- 1School of Physical Education, Southwest University, Chongqing, China
- 2Key Laboratory of Cognition and Personality, Faculty of Psychology, Ministry of Education, Southwest University, Chongqing, China
Objective: The objective of this systematic review and meta-analysis was to evaluate the overall efficacy of cognitive behavioral therapy for insomnia (CBT-I) in treating insomnia in adolescents, and to examine the efficacy of CBT-I on different sleep-related outcomes in this population.
Methods: Randomized controlled trials (RCTs) of CBT-I on insomnia in adolescents were identified using electronic databases and manual searches. The Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) was used to assess risk of bias in RCTs. A standardized mean difference (SMD) with a 95% confidence interval (CI) was used to combine effect sizes. A sensitivity analysis was performed for each outcome using a stepwise elimination method to assess whether the pooled results were significantly affected by individual studies.
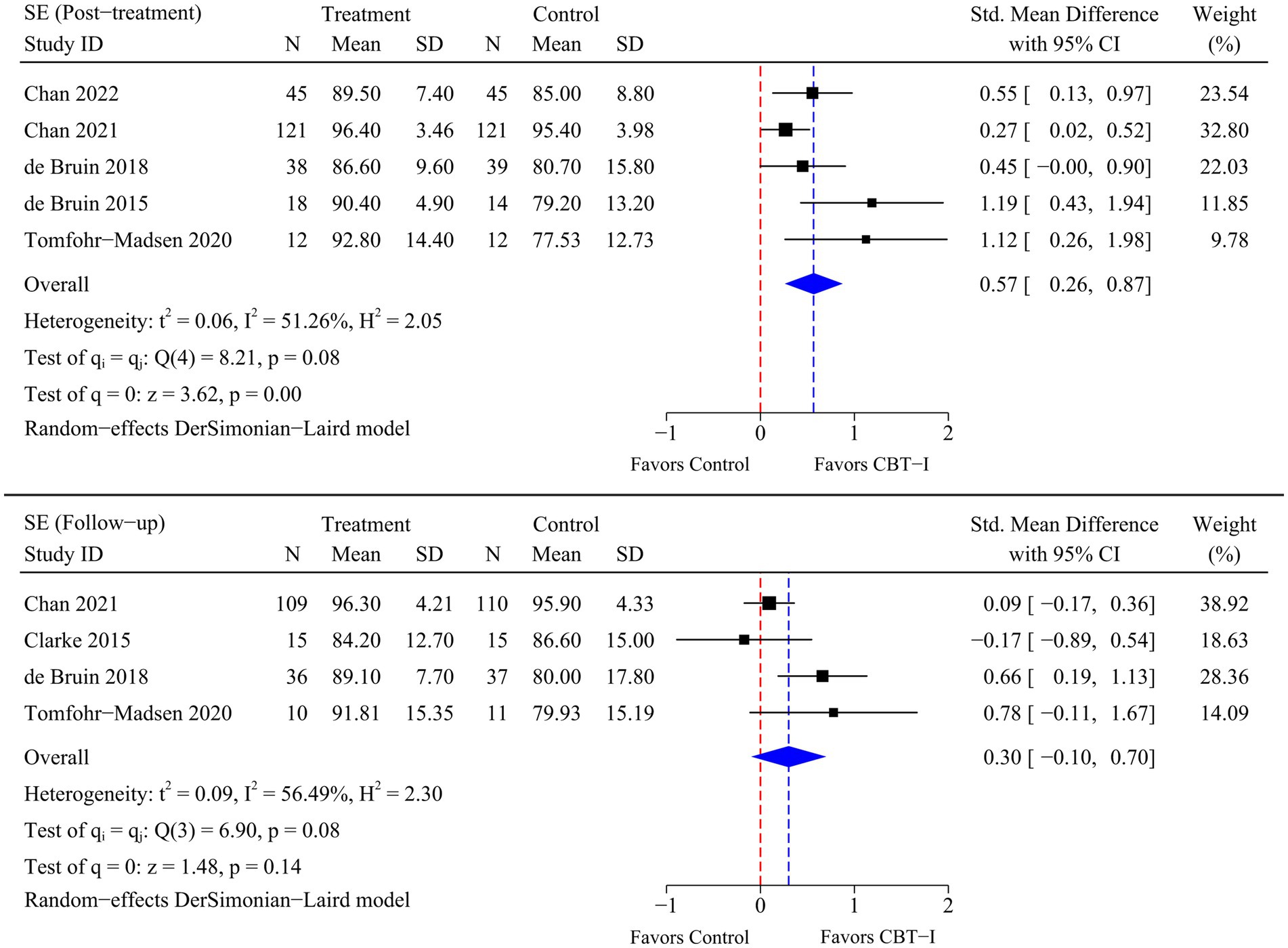
Results: The analysis included 8 RCTs involving a total of 599 participants. The meta-analysis indicated that marked and statistically significant improvements in insomnia (SMD = −1.06; 95% CI -1.65 to −0.47; p < 0.01), sleep onset latency (SMD = −0.99; 95% CI -1.65 to −0.32; p < 0.01), total sleep time (SMD = 0.50; 95% CI 0.10 to 0.90; p = 0.01), and sleep efficiency (SMD = 0.57; 95% CI 0.26 to 0.87; p < 0.01) were observed at post-treatment time point following CBT-I. At follow-up time point, a statistically significant improvement in insomnia (SMD = −0.79; 95% CI -1.42 to −0.17; p = 0.01) was observed following CBT-I.
Conclusion: CBT-I was effective in improving insomnia in adolescents and some sleep-related outcomes, including sleep onset latency, total sleep time, and sleep efficiency. CBT-I was characterized by low risk and high therapeutic benefits and could serve as alternative or adjuvant approaches to medication for the treatment of insomnia. Considering the advantages in terms of safety and efficacy, CBT-I should be the preferred intervention for the treatment of insomnia in adolescents.
Systematic Review Registration:
1 Introduction
Insomnia refers to a sleep disorder caused by physical, psychological and social stressors, usually accompanied by non-adaptive behaviors and hyperarousal, leading to the subjective experience of disturbed sleep (1). Worldwide, insomnia is the most common sleep disorder among adolescents, with a prevalence rate ranging from 7.8% to 23.8% (2–5). In addition, according to the White Paper on Sleep Health of Chinese Residents 2024, more than half of adolescents used to fall asleep after midnight, and accompanied by difficulties in falling asleep, restless sleep and nocturia, with insomnia being a major concern. Insomnia is predominantly characterized by dissatisfaction with sleep duration or quality and difficulties initiating or maintaining sleep, along with substantial distress and impairments of daytime functioning (6). Based on the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-V), diagnosis of insomnia is made when sleep difficulties are present for ≥3 nights per week and last for >3 months (7). Adolescence is not only a critical stage for changes in their sleep needs (8), but also a vulnerable period for the development of insomnia (9). During this period, adolescents are often exposed to various stressors, including academic stress (2), parent-adolescent relationship (10), parental conflicts (11), parental psychological control (12), and parenting styles (13). The cumulative effect of these stressors may increase the risk of insomnia in adolescents. There is a vast amount of evidence that insomnia is prevalent among adolescents (2, 3, 14–17), and that insomnia is associated with a variety of problematic behaviors and psychiatric disorders, including suicidal tendency (18), substance abuse (19), mobile phone use addiction (20), and symptoms of depression and anxiety (21, 22). These facts underline that insomnia not only severely affects adolescents’ physical and mental health, but also places a heavy burden on society and family.
Several countermeasures have been developed to help adolescents cope successfully with stress and improve insomnia, including Benzodiazepines (23), Ramelteon (24), Melatonin (25), and Suvorexant (26), which have been proved to be effective in treating insomnia. However, the prolonged use of such drugs can result in several side effects, such as long-term dependence, tolerance, and even rebound insomnia upon discontinuation (27–29). In this context, cognitive behavioral therapy for insomnia (CBT-I) may help to address these limitations. CBT-I is a psychotherapy focused on improving sleep quality and designing to guide patients to modify their behavioral and thinking patterns (6). Common CBT-I includes cognitive therapy, stimulus control therapy, sleep restriction therapy, sleep hygiene education, and relaxation therapy (6, 30–32). The feasibility and efficacy of CBT-I in treating insomnia in adolescents have been supported by numerous evidence (33–37). For instance, sleep hygiene education has been found to be effective in reducing sleep onset latency, regulating sleep cycles, and improving the duration of insomnia in adolescents (38, 39). Relaxation therapy is thought to have beneficial effects on wake time after sleep onset, sleep efficiency and quality, and can improve poor sleep symptoms in adolescents (40).
In terms of evaluating the overall efficacy of CBT-I in treating insomnia in adolescents, it can be assessed directly using the Insomnia Severity Index (ISI) and Holland Sleep Disorder Questionnaire (HSDQ), and indirectly through measuring different sleep-related outcomes, including sleep onset latency (SOL), total sleep time (TST), and sleep efficiency (SE). However, the scales to evaluate insomnia and sleep-related outcomes in published randomized controlled trials (RCTs) on CBT-I that improves insomnia in adolescents vary, resulting in different effect sizes. For adolescents exposed to many stressors, treating insomnia with CBT-I rather than medication may help them improve their quality of life (41) and some of the psychiatric disorders (e.g., depression, anxiety) that are highly associated with insomnia (36, 42), thereby mitigating the potential adverse effects caused by stressful situations. The objective of this systematic review and meta-analysis was to evaluate the overall efficacy of CBT-I in treating insomnia in adolescents, and to examine the efficacy of CBT-I on different sleep-related outcomes in this population.
2 Methods
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) and was registered in the International Prospective Register of Systematic Reviews (PROSPERO), under number CRD42024526102.
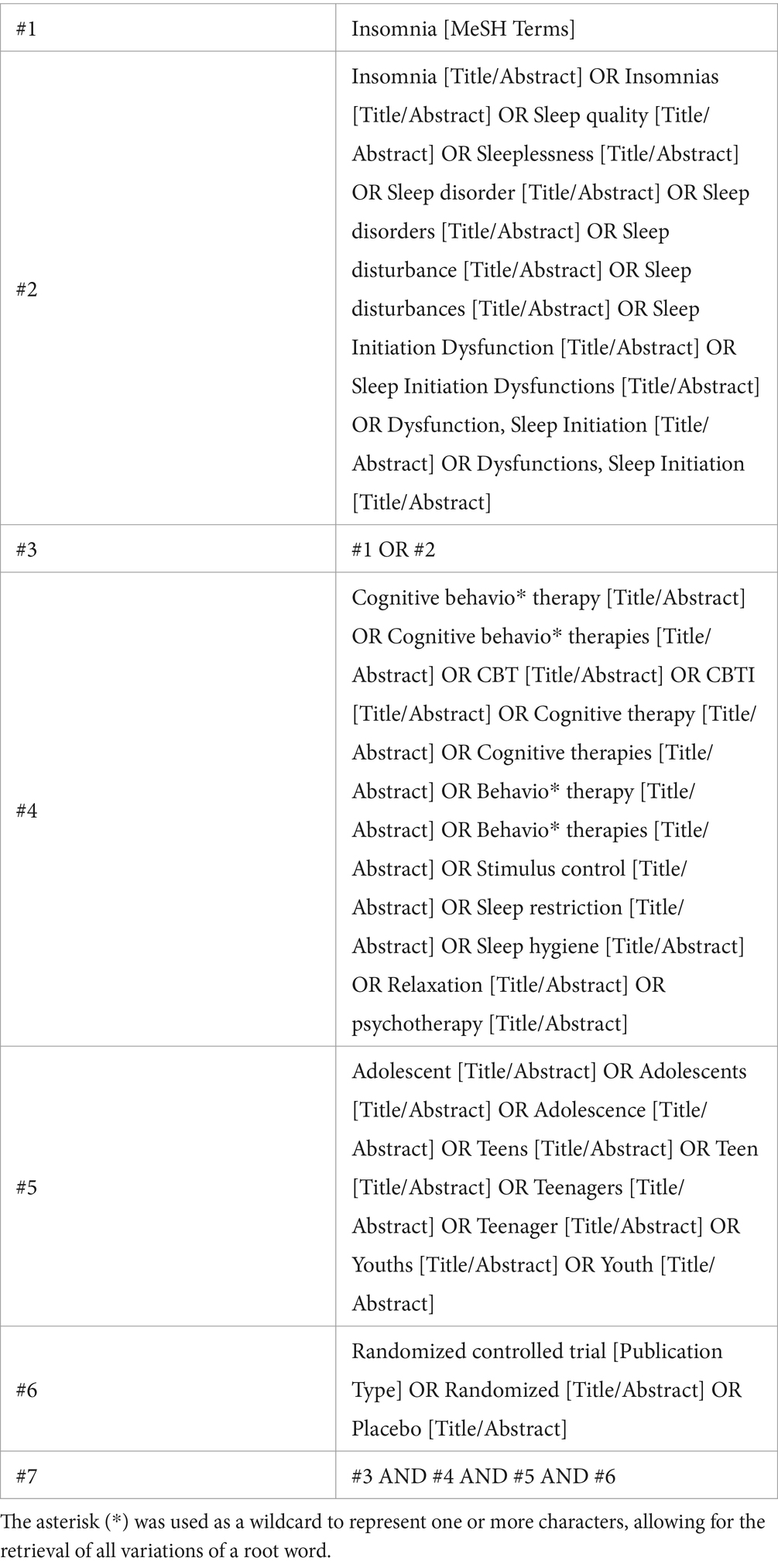
2.1 Search strategy
Based on medical subject headings and free-text terms, a search was conducted across six databases: PubMed, Embase, EBSCOhost, Scopus, Web of Science, and APA PsycINFO. Additionally, the Google database was manually searched for relevant studies. The search timeframe was from the inception of each database to March 2024. The search strategy is presented in Table 1, per the PubMed database.
2.2 Inclusion and exclusion criteria
The inclusion and exclusion criteria followed the PICOS principle. Specifically, studies were included in the present systematic review and meta-analysis if they met the following criteria: (P) population: adolescent and youth groups (ages between 6 and 19 years); (I) intervention: CBT-I was used as the generic term for interventions including cognitive behavioral therapy, stimulus control therapy, sleep restriction therapy, sleep hygiene education, and relaxation therapy; (C) control: control group received only routine treatment or appropriate rehabilitation intervention; (O) outcome: any assessment for insomnia or sleep-related outcomes; and (S) study design: randomized controlled trials.
Studies were excluded in the present systematic review and meta-analysis if they met the following criteria: (P) population: not adolescents; (I) intervention: interventions that were not CBT-I; (C) control: inappropriate control conditions; (O) outcome: studies that did not assess insomnia or sleep-related outcomes; and (S) study design: non-randomized controlled trials, such as quasi-experiments, study protocols, review, conference proceedings, comments, etc.
2.3 Study selection and quality assessment
According to the predetermined inclusion and exclusion criteria, two independent researchers (ZYM and CYC) used EndNote 20.6 bibliographic software for evidence selection. Duplicates were excluded when the references were imported into EndNote 20.6 and the remaining duplicates were manually removed. Two independent researchers screened and checked the references based on information such as the title, abstract, and full text. During the study selection process, any controversies were discussed and addressed by consulting the third author (SL).
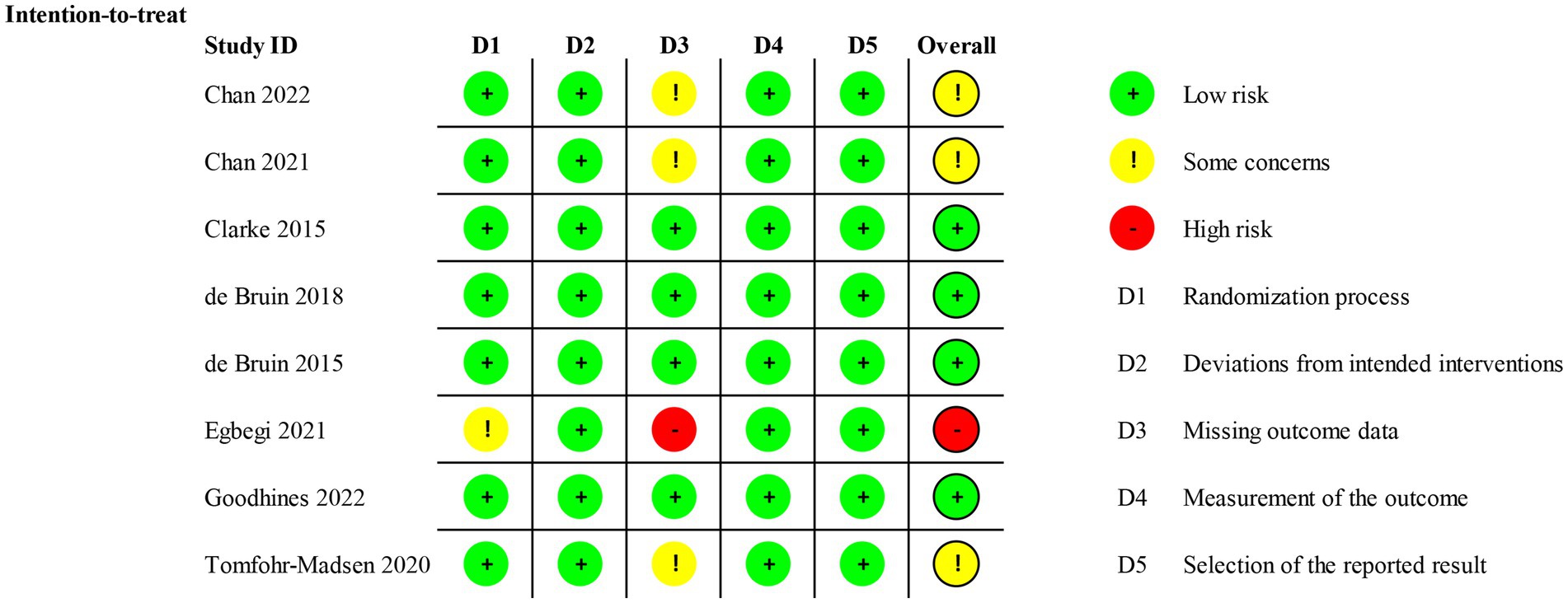
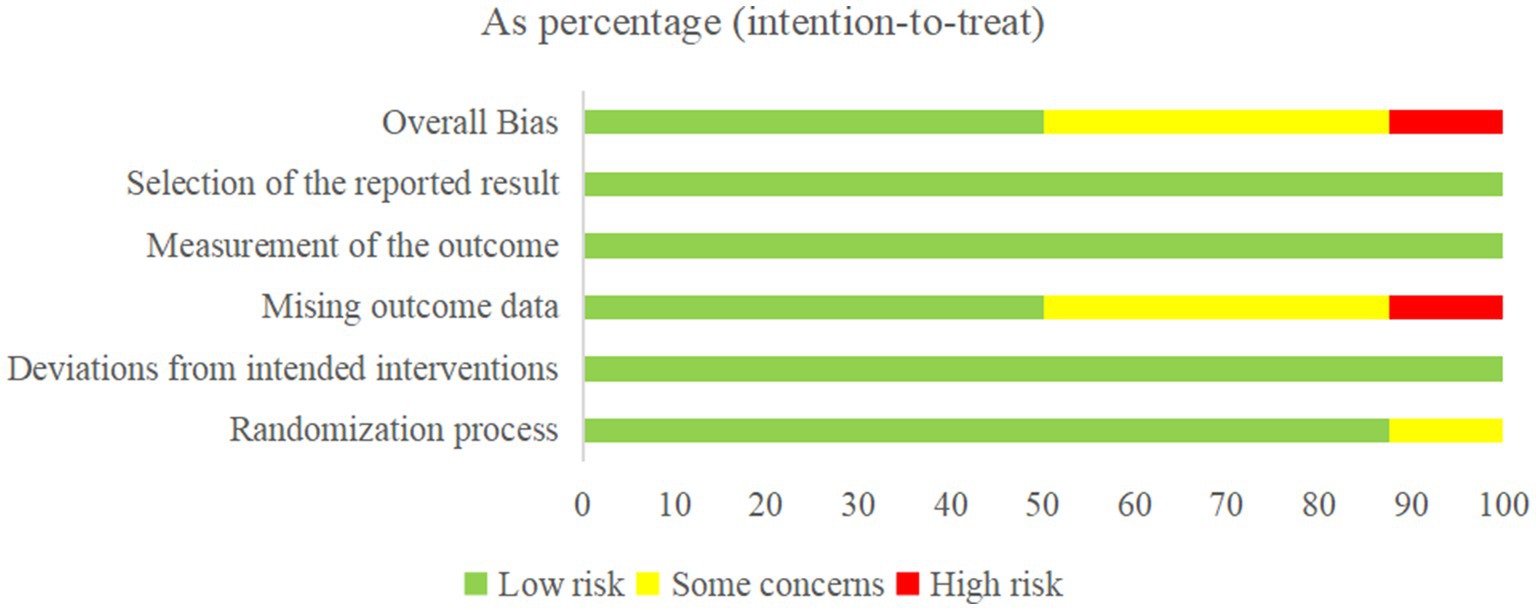
The Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) was used to assess the risk of bias in RCTs, in the following five respects: (1) randomization process, (2) deviations from intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported result. For each eligible study, the overall risk of bias was assessed as either low risk of bias, with some concerns, or high risk of bias. During the quality assessment process, any controversies were discussed and addressed by consulting the third author (SL).
2.4 Data extraction
Using a data extraction form that included relevant information, two independent researchers collected the following data from each included study: (1) basic information, including the first author, country, and year of publication, (2) participant characteristics, including mean (standard deviations) age, sample size, and percentage of boys, (3) diagnostic criteria of insomnia, (4) intervention and control, and (5) sleep-related outcomes.
2.5 Statistical analysis
All the outcomes of this systematic review and meta-analysis were insomnia, sleep onset latency (SOL), total sleep time (TST), and sleep efficiency (SE). The endpoints for the outcomes were assessed at two time points, which were defined for this analysis: immediate post-treatment and follow-up (1 month to 6 months after completion of the intervention). As there were differences in the measurement tools used in the different RCTs, the standardized mean difference (SMD) with a 95% confidence interval (CI) was used to combine effect sizes (43). For all meta-analyses, heterogeneity among studies was assessed using the Chi-square test based on Q-test and I2 statistics with a significance level of p-value <0.05 (44). According to the recommendations of Cochran’s handbook, when p-value <0.10 or I2 > 50%, there was a significant heterogeneity, and a random-effect model was used to merge the results. Otherwise, a fixed-effect model was used to merge the results when there was no significant heterogeneity (p-value >0.10 or I2 < 50%) (43). Since the number of trials included was less than 10, the publication bias was not assessed. A sensitivity analysis was performed for each outcome using a stepwise elimination method to assess whether the pooled results were significantly affected by individual studies (43). All statistical analyses of this study were performed using Stata 18.0 software.
3 Results
3.1 Literature search and eligible studies
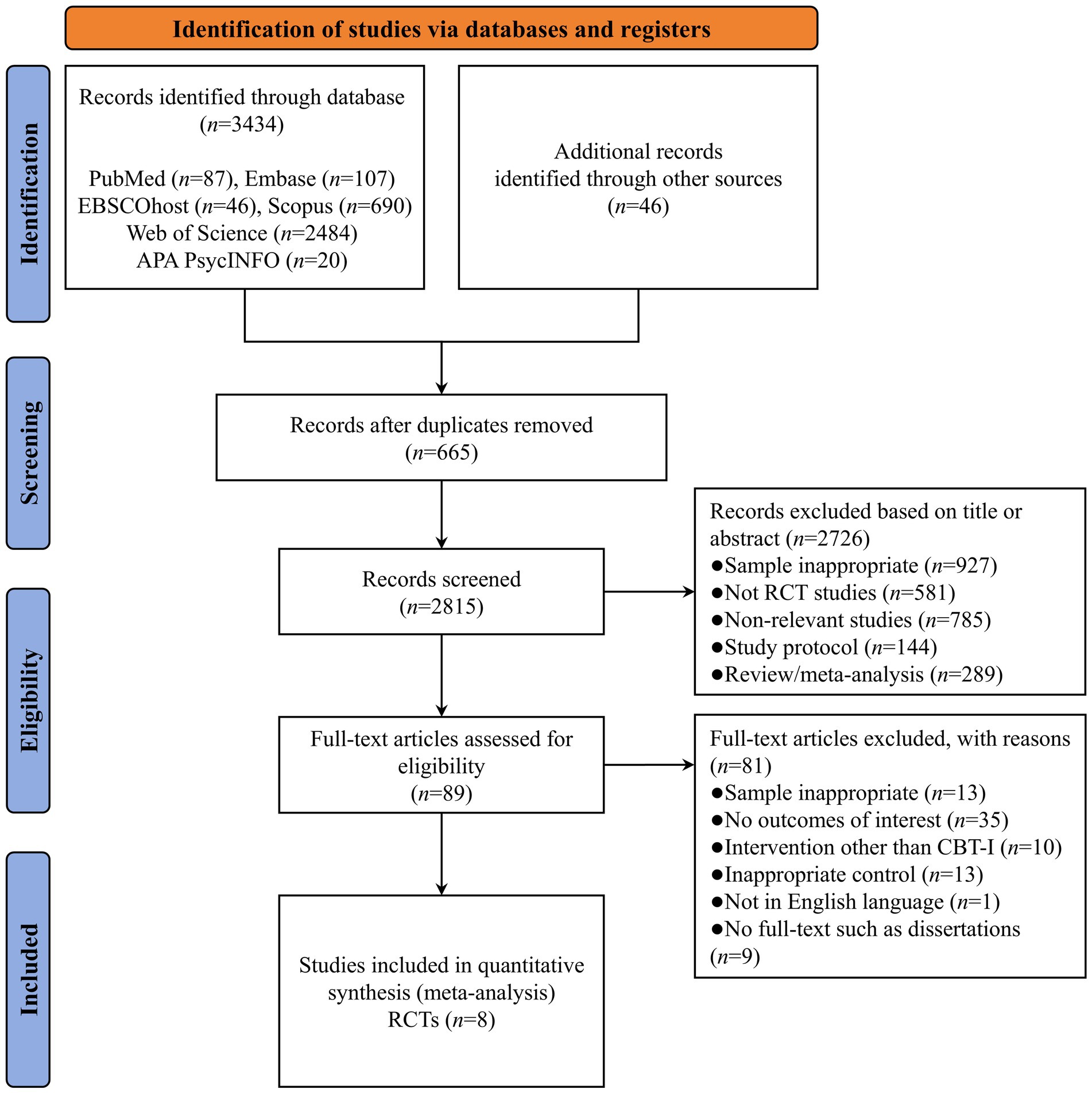
A total of 3,480 studies were identified through database searches, including PubMed (n = 87), Embase (n = 107), EBSCOhost (n = 46), Scopus (n = 690), Web of Science (n = 2,484), APA PsycINFO (n = 20), and other sources (n = 46). After removing duplicate studies (n = 665), the titles and abstracts of 2,815 studies were screened for eligibility, and 2,726 references were eliminated due to samples inappropriate (n = 927), not RCT studies (n = 581), non-relevant studies (n = 785), study protocol (n = 144), and review/meta-analysis (n = 289). Therefore, 89 studies were subjected to full-text review, 81 of which were deemed ineligible because the sample was inappropriate (n = 13), no outcomes of interest (n = 35), intervention other than CBT-I (n = 10), inappropriate control (n = 13), not in English language (n = 1), and no full-text such as dissertations (n = 9). Finally, 8 studies met the inclusion criteria and were included in the meta-analysis (45–52). A PRISMA flowchart of the literature search is presented in Figure 1.
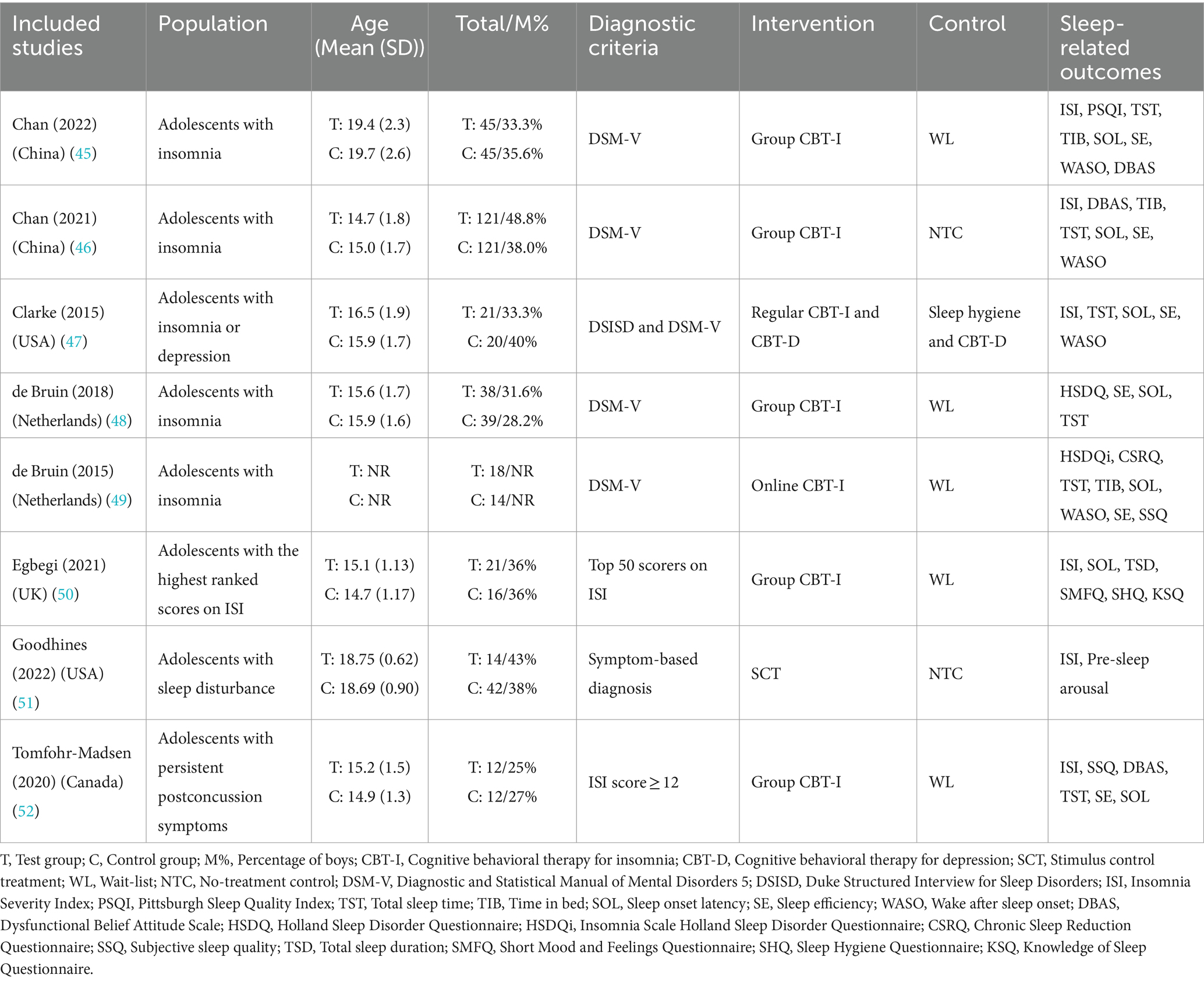
3.2 Study characteristics
Eight full-text RCTs met the inclusion criteria, conducted in various countries: two in China (45, 46), two in the USA (47, 51), two in the Netherlands (48, 49), one in the UK (50), and one in Canada (52). The study populations comprised adolescents with insomnia disorder (6 RCTs) (45–49, 51), adolescents with the highest ranked scores on ISI (1 RCT) (50), and adolescents with persistent postconcussion symptoms (1 RCT) (52). In total, 290 adolescents were assigned to the experimental group, with a mean age ranging from 14.7 to 19.4 years, while 309 were assigned to the control group, with a mean age ranging from 14.7 to 19.7 years.
Most trials referenced accepted diagnostic criteria for insomnia, most commonly the DSM-V (5 RCTs) (45–49), ISI (2 RCTs) (50, 52), and one trial diagnosed insomnia by sleep onset latency and wake after sleep onset (51). Experimental groups comprised group CBT-I (5 RCTs) (45, 46, 48, 50, 52), regular CBT-I and CBT-D (1 RCT) (47), online CBT-I (1 RCT) (49), and SCT (1 RCT) (51). Control groups comprised a wait-list (5 RCTs) (45, 48–50, 52), a no-treatment control (2 RCTs) (46, 51), and sleep hygiene and cognitive behavioral therapy for depression (1 RCT) (47). The main characteristics of the eight RCTs are presented in Table 2.
3.3 Risk of bias
Seven trials showed a low risk of bias in the randomization process (45–49, 51, 52), and one trial was assessed as having some concerns owing to the random allocation sequence (50). For deviations from intended interventions, all trials were considered low risk because there were no deviations from intended interventions that arose because of the experimental context. For missing outcome data, four trials were of low risk because the data for the outcome were available for all or nearly all randomized participants (47–49, 51). Three trials had some concerns (45, 46, 52) and one had high risk because participant data were incomplete and there was no evidence that the result was not biased by missing outcome data (50). The measurement of the outcome and selection of the reported result were low risk because all trials used appropriate methods to measure outcomes, and all measurements and data analyses were available and none of the trials reported results selectively. The overall risk was low risk in four trials (47–49, 51), with some concerns in three trials (45, 46, 52), and high risk in one trial (50). The Cochrane risk-of-bias assessment is presented in Figures 2, 3.
3.4 Meta-analysis
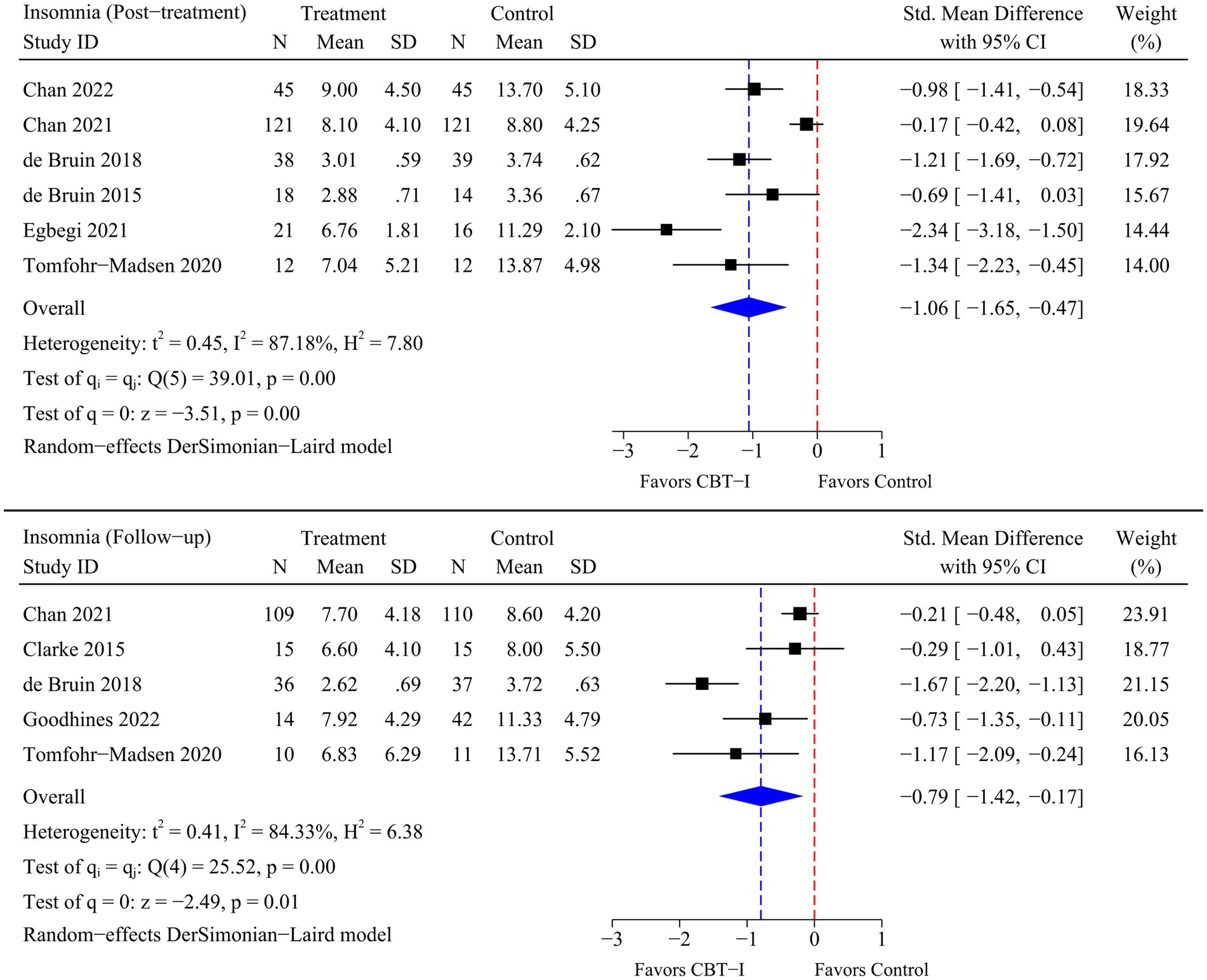
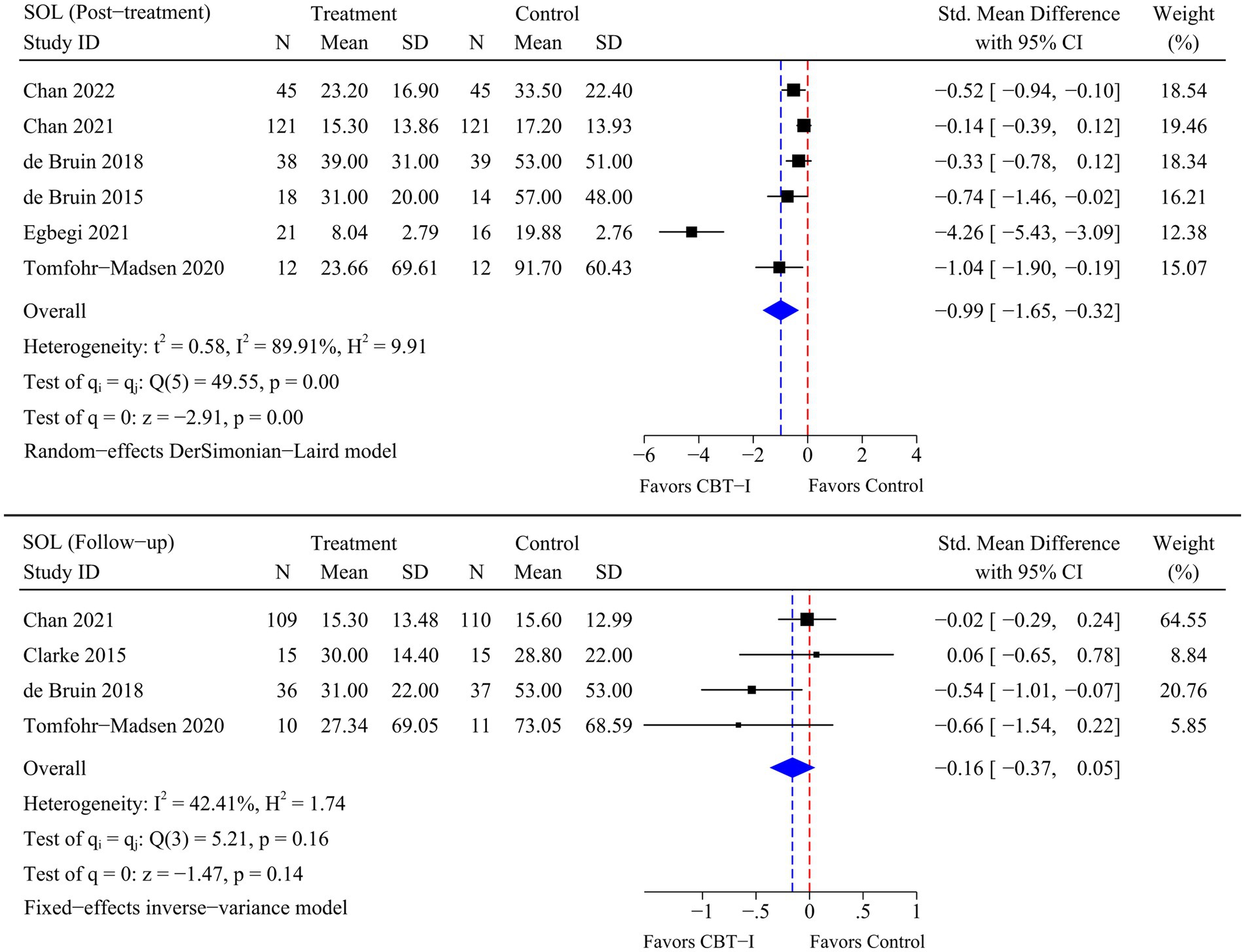
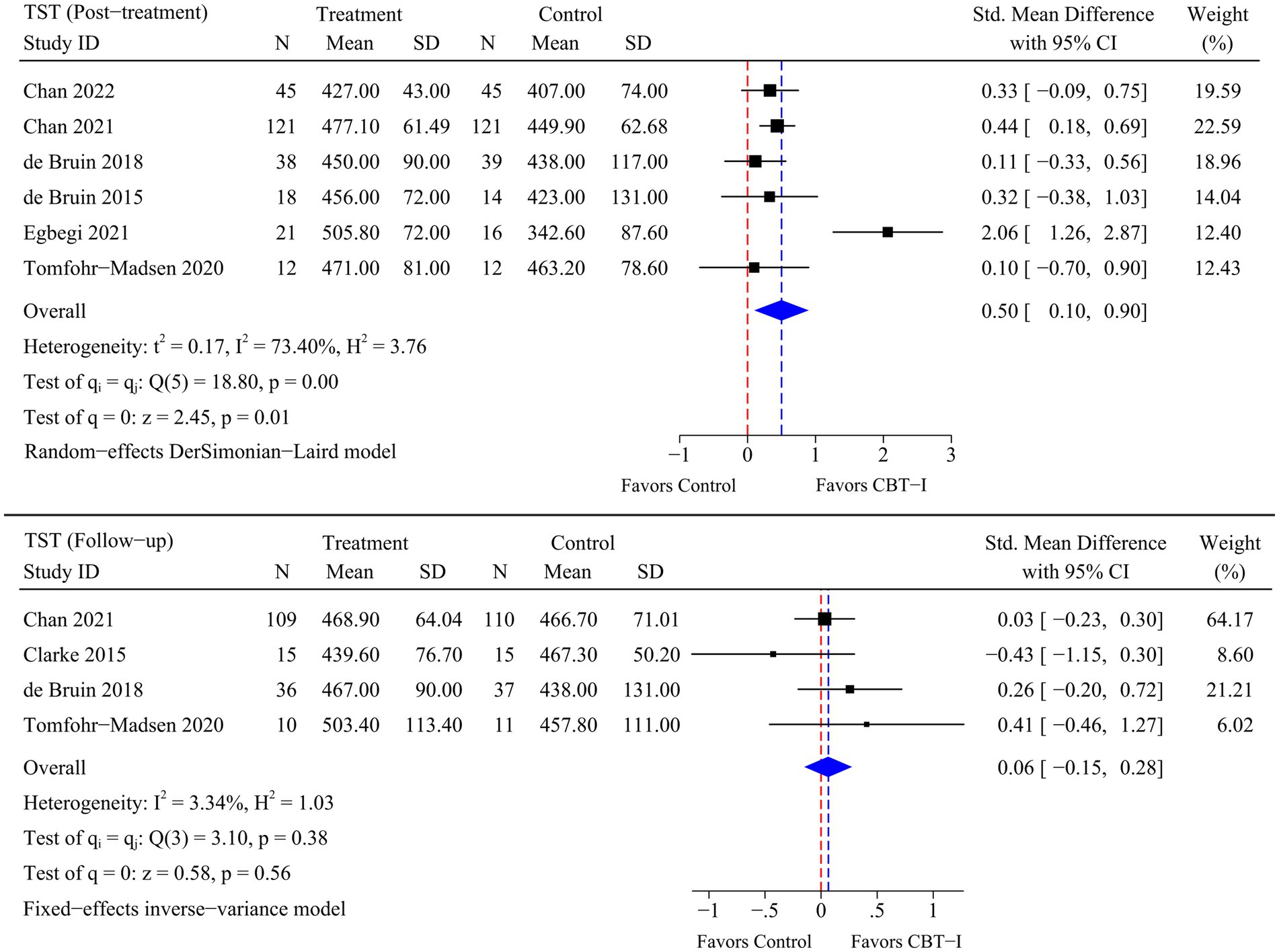
A total of eight RCTs were included in the meta-analysis, and heterogeneity was examined using the Chi-square test based on Q-test and I2 statistics. Marked and statistically significant improvements in insomnia (SMD = −1.06; 95% CI -1.65 to −0.47; p < 0.01), SOL (SMD = −0.99; 95% CI -1.65 to −0.32; p < 0.01), TST (SMD = 0.50; 95% CI 0.10 to 0.90; p = 0.01), and SE (SMD = 0.57; 95% CI 0.26 to 0.87; p < 0.01) were observed at post-treatment time point following CBT-I. At follow-up time point, a statistically significant improvement in insomnia (SMD = −0.79; 95% CI -1.42 to −0.17; p = 0.01) was observed following CBT-I. Although there were no significant improvements in the remaining sleep-related outcomes, statistical significance was borderline as there were fewer RCTs available for the meta-analysis at follow-up time point. The results of the meta-analysis for each outcome are presented in Figures 4– 7.
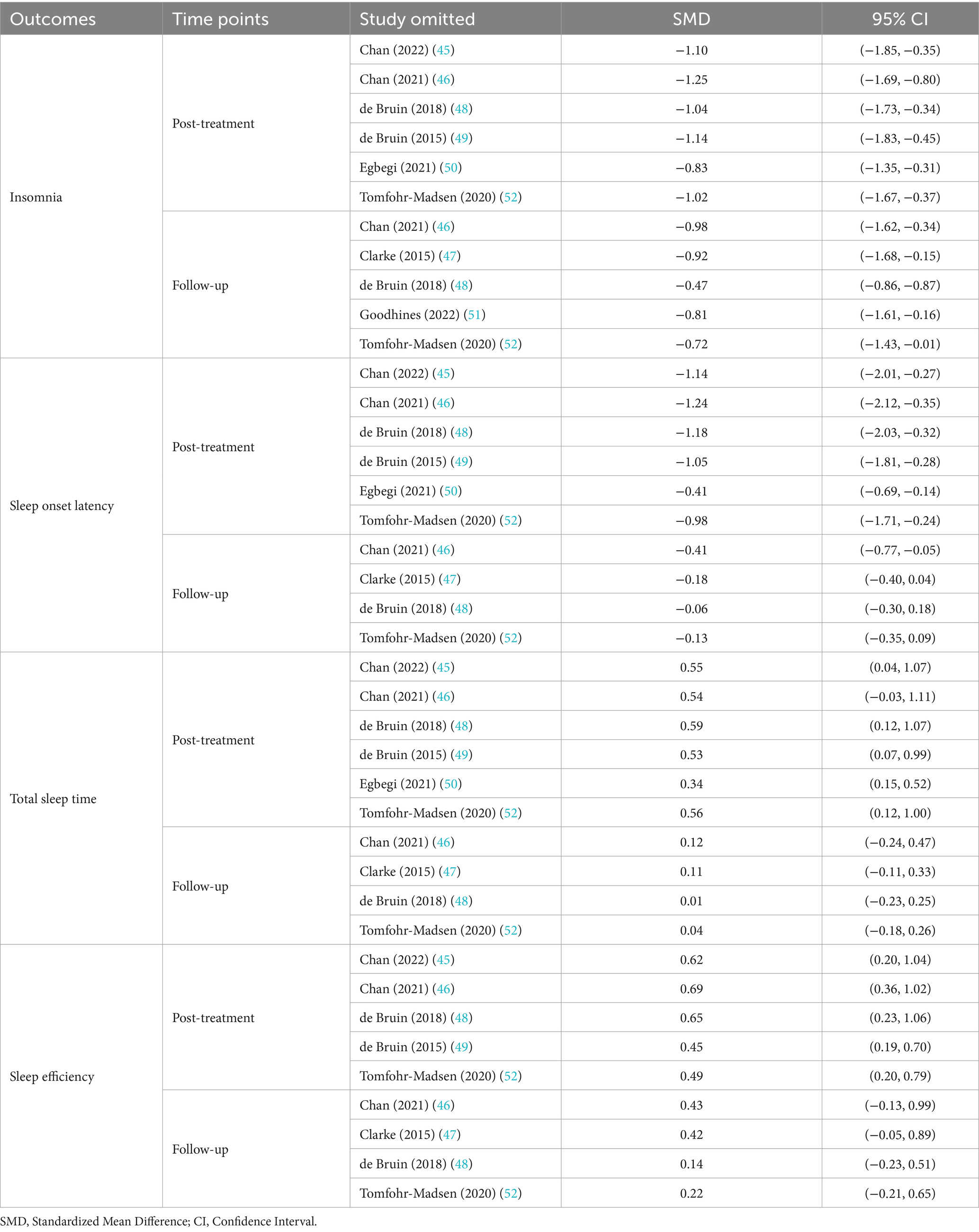
3.5 Sensitivity analysis
The results of the sensitivity analysis indicated that the pooled results for insomnia, SOL, and SE remained stable at post-treatment time point after excluding individual studies, indicating that these results were insensitive to study selection. However, the pooled results of TST were statistically changed and sensitive to study selection when the Chan et al. (46) study was excluded (SMD = 0.54; 95% CI -0.03 to 1.11; p > 0.05). At follow-up time point, the pooled results for insomnia, TST, and SE were more insensitive to study selection. However, the pooled results of SOL were statistically changed and sensitive to study selection when the Chan et al. (46) study was excluded (SMD = −0.41; 95% CI -0.77 to −0.05; p < 0.05).
The differences mentioned above may be attributed to the larger sample size of the excluded study, which was significantly weighted in the meta-analysis and therefore had a greater impact on the pooled results. In addition, statistical significance was generally borderline due to the limited number of trials that met the inclusion criteria, resulting in the pooled results for some sleep-related outcomes being sensitive to study selection. The results of the sensitivity analysis for each outcome are presented in Table 3.
4 Discussion
Addressing sleep disorders in adolescents through effective psychological interventions, such as CBT-I, is crucial for their physical and mental health, as these disorders are associated with various adverse outcomes, especially suicidal ideation (53), emotional regulation disorder (54), and substance abuse (55). The objective of this systematic review and meta-analysis was to evaluate the overall efficacy of CBT-I in treating insomnia in adolescents, and to examine the efficacy of CBT-I on different sleep-related outcomes in this population. The pooled results of the meta-analysis indicated that CBT-I, at post-treatment time point, effectively improved insomnia (SMD = −1.06; 95% CI -1.65 to −0.47; p < 0.01) and some sleep-related outcomes, including SOL (SMD = −0.99; 95% CI -1.65 to −0.32; p < 0.01), TST (SMD = 0.50; 95% CI 0.10 to 0.90; p = 0.01), and SE (SMD = 0.57; 95% CI 0.26 to 0.87; p < 0.01) in adolescents. At follow-up time point, although SOL, TST, and SE failed to improve, CBT-I still showed an improvement effect on insomnia in adolescents (SMD = −0.79; 95% CI -1.42 to −0.17; p = 0.01).
Considering that circadian rhythm delay is prominent in adolescence and can be easily confused with insomnia, this study adhered strictly to pre-established criteria during the study selection process to eliminate the potential influence of other factors on the research results. Specifically, participants in five trials were diagnosed with insomnia using instruments such as the DSM-V (45–49). Additionally, they were required to engage in structured screening interviews (including assessments of sleep patterns and sleep disorders) with clinical professionals or related experts, to ascertain their eligibility for an insomnia diagnosis. One trial utilized the Morningness-Eveningness Questionnaire to control for potential circadian rhythm/phase disorders (51). Furthermore, in terms of participant characteristics, all trials excluded participants who were using sleep medications. However, two trials diagnosed insomnia solely based on ISI without considering the impact of circadian rhythm delay (50, 52). The results of the sensitivity analysis indicated that excluding these trials did not significantly affect the pooled results of the outcomes, suggesting that the potential influence of circadian rhythm delay on the findings of this study can be ruled out.
In fact, the mechanisms by which CBT-I improves insomnia primarily rely on behavioral and cognitive strategies. Behavioral strategies for insomnia aim to modify sleep-incompatible behaviors in the bedroom and consolidate sleep architecture (56, 57). Cognitive strategies target erroneous beliefs maintaining insomnia (56). For instance, in terms of behavioral strategies, sleep restriction therapy improves insomnia primarily by reducing the tendency to remain in bed while awake (58). Specifically, by restricting time in bed (TIB), sleep restriction therapy curtails sleep opportunity, resulting in partial sleep deprivation, which contributes to an increase in sleep need, thereby enhancing sleep efficiency and quality (59). Stimulus control therapy can regulate the relationship between TIB and bedtime through sleep instructions, such as “Lie down, intending to go to sleep only when you are sleepy,” thereby reinforcing sleep behaviors while inhibiting non-sleep behaviors (60–62). In terms of cognitive strategies, cognitive therapy is able to identify, challenge, and replace dysfunctional beliefs and attitudes about sleep and insomnia, such as “If I cannot sleep all the time, I may crash” (63). This intervention may help individuals fall asleep faster, and improve their sleep quality (63, 64). Furthermore, insomniacs have greater activation in cognitive, emotional, and cortical domains, and CBT-I can decrease such activation by diverting attention from sleep difficulties, thereby alleviating sleep disturbances in these patients (65, 66). Finally, insomnia is usually associated with hyperactivation of the hypothalamic–pituitary–adrenal (HPA) axis (2, 67, 68), and impaired heart rate variability (HRV) (69, 70). Evidence suggests that CBT-I helps to suppress hyperactivation of the HPA axis, reduce hyperarousal, and improve HRV during sleep (71, 72). It is important to note that the aforementioned physiological changes represent correlational rather than causal relationships, and are primarily based on data from studies of adult populations. For adolescents whose brains are still developing, these physiological changes may exhibit different relevance and applicability. Therefore, the specific physiological mechanisms by which CBT-I improves insomnia in adolescents require further investigation and validation to comprehensively clarify the efficacy of this therapy in this population.
The pooled results of the current systematic review and meta-analysis indicated that CBT-I was effective in improving insomnia in adolescents compared with the control group, both at post-treatment time point and at follow-up time point. For some sleep-related outcomes, including SOL, TST, and SE, none of the CBT-I group showed a statistically significant difference in therapeutic efficacy compared with the control group at follow-up time point. It has been hypothesized that this may be due to the fact that CBT-I strategies implemented throughout the course of therapy were not used by adolescent patients any more to manage sleep disorders over time, leading to a “sharp decline” in the improvement of sleep-related outcomes at follow-up time point (73). This “sharp decline” suggests that adolescent adherence to CBT-I strategies may decrease over time. Effectively managing this decline in adherence and maximizing the long-term efficacy of CBT-I on insomnia and sleep-related outcomes in adolescents are critical issues that warrant further investigation. Furthermore, the confidence intervals for some pooled results were close to the margin of statistical significance, which implies that the pooled results may vary in the case of a change in the study selection or in certain conditions. This suggests the sample size and experimental design should be further expanded and optimized, in order to assess the long-term effects of CBT-I on these outcomes more accurately.
In summary, the findings of this study suggest that CBT-I was effective in improving insomnia in adolescents and some sleep-related outcomes, including SOL, TST, and SE. Adolescents are at a critical stage in healthy physical and mental development, during which they are often exposed to physical, psychological and, social stressors. The cumulative effect of these stressors may increase the risk of insomnia in adolescents. CBT-I was characterized by low risk and high therapeutic benefits and could serve as alternative or adjuvant approaches to medication for the treatment of insomnia. In a direct comparison, CBT-I has been shown to be more effective than medication in managing insomnia, with effects lasting for at least 6 months of follow-up (74). Therefore, considering the advantages in terms of safety and efficacy, CBT-I should be the preferred intervention for the treatment of insomnia in adolescents. Appropriate medication can be adopted in accordance with specific conditions to further enhance the therapeutic effects, and the improvement in sleep quality and related disorders can be maximized though this comprehensive treatment in adolescent patients.
5 Limitations
The findings of the current systematic review and meta-analysis must be interpreted in the context of limitations. First, due to the limited number of trials that met the inclusion criteria, some additional sleep-related outcomes, including TIB, WASO, and SSQ were not covered in this study. Second, the follow-up time point range was limited to 6 months or less due to the different follow-up time points among the included trials. The therapeutic efficacy of CBT-I for insomnia in adolescents beyond 6 months was not investigated. Therefore, future research should be encouraged to increase sample sizes and extend follow-up periods based on these findings, in order to explore the more comprehensive and long-term effects of CBT-I on sleep-related outcomes in adolescents. It is important to note that this study did not conduct subgroup analyses based on demographic data, which means that the specific efficacy of CBT-I on sleep-related outcomes in adolescents remains unconfirmed. Addressing this gap will contribute to a more nuanced understanding of the differential benefits of CBT-I in this field, which could further facilitate the development of personalized CBT-I strategies. Finally, the confidence intervals for some of the pooled results were close to the margin of statistical significance. This suggests that the pooled results may vary in the case of a change in the study selection or in certain conditions, and these findings should be interpreted cautiously.
6 Conclusion
The objective of this systematic review and meta-analysis was to evaluate the overall efficacy of CBT-I in treating insomnia in adolescents, and to examine the efficacy of CBT-I on different sleep-related outcomes in this population. CBT-I was effective in improving insomnia in adolescents and some sleep-related outcomes, including SOL, TST, and SE. Moreover, CBT-I was characterized by low risk and high therapeutic benefits and could serve as alternative or adjuvant approaches to medication for the treatment of insomnia. Therefore, considering the advantages in terms of safety and efficacy, CBT-I should be the preferred intervention for the treatment of insomnia in adolescents.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ZYM: Conceptualization, Data curation, Methodology, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. CYC: Writing – review & editing, Conceptualization, Formal analysis, Software. SLL: Data curation, Methodology, Software, Visualization, Writing – original draft. YZZ: Formal analysis, Validation, Writing – review & editing. CFL: Methodology, Software, Visualization, Writing – review & editing. SL: Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Social Science Fund of China (project 24BTY098).
Acknowledgments
Research team would like to thank Southwest University for the support of this research, and also thank Shi Luo for the help in developing the research program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Riemann, D, Spiegelhalder, K, Feige, B, Voderholzer, U, Berger, M, Perlis, M, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. (2010) 14:19–31. doi: 10.1016/j.smrv.2009.04.002
2. de Zambotti, M, Goldstone, A, Colrain, IM, and Baker, FC. Insomnia disorder in adolescence: diagnosis, impact, and treatment. Sleep Med Rev. (2018) 39:12–24. doi: 10.1016/j.smrv.2017.06.009
3. Johnson, EO, Roth, T, Schultz, L, and Breslau, N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. (2006) 117:e247–56. doi: 10.1542/peds.2004-2629
4. Chung, KF, Kan, KKK, and Yeung, WF. Insomnia in adolescents: prevalence, help-seeking behaviors, and types of interventions. Child Adolesc Ment Health. (2014) 19:57–63. doi: 10.1111/camh.12009
5. Hysing, M, Pallesen, S, Stormark, KM, Lundervold, AJ, and Sivertsen, B. Sleep patterns and insomnia among adolescents: a population-based study. J Sleep Res. (2013) 22:549–56. doi: 10.1111/jsr.12055
6. Morin, CM, Drake, CL, Harvey, AG, Krystal, AD, Manber, R, Riemann, D, et al. Insomnia disorder. Nat Rev Dis Primers. (2015) 1:1–18. doi: 10.1038/nrdp.2015.26
7. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association (2013).
8. Madrid-Valero, JJ, Ronald, A, Shakeshaft, N, Schofield, K, Malanchini, M, and Gregory, AM. Sleep quality, insomnia, and internalizing difficulties in adolescents: insights from a twin study. Sleep. (2020) 43:1–9. doi: 10.1093/sleep/zsz229
9. Zhang, J, Chan, NY, Lam, SP, Li, SX, Liu, Y, Chan, JW, et al. Emergence of sex differences in insomnia symptoms in adolescents: a large-scale school-based study. Sleep. (2016) 39:1563–70. doi: 10.5665/sleep.6022
10. Kapetanovic, S, Skoog, T, Bohlin, M, and Gerdner, A. Aspects of the parent–adolescent relationship and associations with adolescent risk behaviors over time. J Fam Psychol. (2019) 33:1–11. doi: 10.1037/fam0000436
11. Mastrotheodoros, S, van der Graaff, J, Deković, M, Meeus, WH, and Branje, S. Parent–adolescent conflict across adolescence: trajectories of informant discrepancies and associations with personality types. J Youth Adolesc. (2020) 49:119–35. doi: 10.1007/s10964-019-01054-7
12. Yan, F, Zhang, Q, Ran, G, Li, S, and Niu, X. Relationship between parental psychological control and problem behaviours in youths: A three-level meta-analysis. Child Youth Serv Rev. (2020) 112:104900–9. doi: 10.1016/j.childyouth.2020.104900
13. Moreno–Ruiz, D, Martínez–Ferrer, B, and García–Bacete, F. Parenting styles, cyberaggression, and cybervictimization among adolescents. Comput Hum Behav. (2019) 93:252–9. doi: 10.1016/j.chb.2018.12.031
14. Gradisar, M, Gardner, G, and Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. (2011) 12:110–8. doi: 10.1016/j.sleep.2010.11.008
15. Zhou, HQ, Shi, WB, Wang, XF, Yao, M, Cheng, GY, Chen, PY, et al. An epidemiological study of sleep quality in adolescents in South China: a school-based study. Child Care Health Dev. (2012) 38:581–7. doi: 10.1111/j.1365-2214.2011.01300.x
16. Crowley, SJ, Acebo, C, and Carskadon, MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. (2007) 8:602–12. doi: 10.1016/j.sleep.2006.12.002
17. Åslund, L, Lekander, M, Wicksell, RK, Henje, E, and Jernelöv, S. Cognitive-behavioral therapy for insomnia in adolescents with comorbid psychiatric disorders: A clinical pilot study. Clin Child Psychol Psychiatry. (2020) 25:958–71. doi: 10.1177/1359104520929376
18. Chan, NY, Zhang, J, Tsang, CC, Li, AM, Chan, JWY, Wing, YK, et al. The associations of insomnia symptoms and chronotype with daytime sleepiness, mood symptoms and suicide risk in adolescents. Sleep Med. (2020) 74:124–31. doi: 10.1016/j.sleep.2020.05.035
19. Bootzin, RR, and Stevens, SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin Psychol Rev. (2005) 25:629–44. doi: 10.1016/j.cpr.2005.04.007
20. Honglv, X, Jian, T, Jiaxing, Y, Yunpeng, S, Chuanzhi, X, Mengdie, H, et al. Mobile phone use addiction, insomnia, and depressive symptoms in adolescents from ethnic minority areas in China: A latent variable mediation model. J Affect Disord. (2023) 320:381–9. doi: 10.1016/j.jad.2022.09.156
21. Blake, MJ, Trinder, JA, and Allen, NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin Psychol Rev. (2018) 63:25–40. doi: 10.1016/j.cpr.2018.05.006
22. Alvaro, PK, Roberts, RM, and Harris, JK. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. (2014) 15:934–41. doi: 10.1016/j.sleep.2014.03.019
23. Holbrook, A, Crowther, R, Lotter, A, and Endeshaw, Y. The role of benzodiazepines in the treatment of insomnia: meta-analysis of benzodiazepine use in the treatment of insomnia. J Am Geriatr Soc. (2001) 49:824–6. doi: 10.1046/j.1532-5415.2001.49161.x
24. Kuriyama, A, Honda, M, and Hayashino, Y. Ramelteon for the treatment of insomnia in adults: a systematic review and meta-analysis. Sleep Med. (2014) 15:385–92. doi: 10.1016/j.sleep.2013.11.788
25. Choi, K, Lee, YJ, Park, S, Je, NK, and Suh, HS. Efficacy of melatonin for chronic insomnia: systematic reviews and meta-analyses. Sleep Med Rev. (2022) 66:101692–15. doi: 10.1016/j.smrv.2022.101692
26. Kuriyama, A, and Tabata, H. Suvorexant for the treatment of primary insomnia: a systematic review and meta-analysis. Sleep Med Rev. (2017) 35:1–7. doi: 10.1016/j.smrv.2016.09.004
27. Atkin, T, Comai, S, and Gobbi, G. Drugs for insomnia beyond benzodiazepines: pharmacology, clinical applications, and discovery. Pharmacol Rev. (2018) 70:197–245. doi: 10.1124/pr.117.014381
28. Werner-Seidler, A, Johnston, L, and Christensen, H. Digitally-delivered cognitive-behavioural therapy for youth insomnia: A systematic review. Internet Interv. (2018) 11:71–8. doi: 10.1016/j.invent.2018.01.007
30. Williams, J, Roth, A, Vatthauer, K, and McCrae, CS. Cognitive behavioral treatment of insomnia. Chest. (2013) 143:554–65. doi: 10.1378/chest.12-0731
31. Matthews, EE, Arnedt, JT, McCarthy, MS, Cuddihy, LJ, and Aloia, MS. Adherence to cognitive behavioral therapy for insomnia: a systematic review. Sleep Med Rev. (2013) 17:453–64. doi: 10.1016/j.smrv.2013.01.001
32. Krystal, AD, Prather, AA, and Ashbrook, LH. The assessment and management of insomnia: an update. World Psychiatry. (2019) 18:337–52. doi: 10.1002/wps.20674
33. de Bruin, EJ, Bögels, SM, Oort, FJ, and Meijer, AM. Efficacy of cognitive behavioral therapy for insomnia in adolescents: a randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep. (2015) 38:1913–26. doi: 10.5665/sleep.5240
34. de Bruin, EJ, Oort, FJ, Bögels, SM, and Meijer, AM. Efficacy of internet and group-administered cognitive behavioral therapy for insomnia in adolescents: a pilot study. Behav Sleep Med. (2014) 12:235–54. doi: 10.1080/15402002.2013.784703
35. Lah, S, Phillips, NL, Palermo, TM, Bartlett, D, Epps, A, Teng, A, et al. A feasibility and acceptability study of cognitive behavioural treatment for insomnia in adolescents with traumatic brain injury: A–B with follow up design, randomized baseline, and replication across participants. Neuropsychol Rehabil. (2021) 31:345–68. doi: 10.1080/09602011.2019.1693404
36. Cliffe, B, Croker, A, Denne, M, Smith, J, and Stallard, P. Digital cognitive behavioral therapy for insomnia for adolescents with mental health problems: feasibility open trial. JMIR Ment Health. (2020) 7:e14842–11. doi: 10.2196/14842
37. Conroy, DA, Czopp, AM, Dore-Stites, DM, Dopp, RR, Armitage, R, Hoban, TF, et al. Modified cognitive behavioral therapy for insomnia in depressed adolescents: a pilot study. Behav Sleep Med. (2019) 17:99–111. doi: 10.1080/15402002.2017.1299737
38. Weiss, MD, Wasdell, MB, Bomben, MM, Rea, KJ, and Freeman, RD. Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. J Am Acad Child Adolesc Psychiatry. (2006) 45:512–9. doi: 10.1097/01
39. Tan, E, Healey, D, Gray, AR, and Galland, BC. Sleep hygiene intervention for youth aged 10 to 18 years with problematic sleep: a before-after pilot study. BMC Pediatr. (2012) 12:1–9. doi: 10.1186/1471-2431-12-189
40. Means, MK, Lichstein, KL, Epperson, MT, and Johnson, CT. Relaxation therapy for insomnia: nighttime and day time effects. Behav Res Ther. (2000) 38:665–78. doi: 10.1016/S0005-7967(99)00091-1
41. Palermo, TM, Beals-Erickson, S, Bromberg, M, Law, E, and Chen, M. A single arm pilot trial of brief cognitive behavioral therapy for insomnia in adolescents with physical and psychiatric comorbidities. J Clin Sleep Med. (2017) 13:401–10. doi: 10.5664/jcsm.6490
42. Reddy, A, Mansuri, Z, Vadukapuram, R, Shah, K, Thootkur, M, and Trivedi, C. Efficacy of cognitive behavioral therapy for insomnia for the treatment of child and adolescent anxiety and depression: a systematic review from randomized controlled trials. J Nerv Ment Dis. (2023) 211:238–43. doi: 10.1097/NMD.0000000000001613
43. Deeks, JJ, Higgins, JP, and Altman, DG. Analysing data and undertaking meta-analyses In: VA Welch, editor. Cochrane handbook for systematic reviews of interventions. Hoboken: Wiley (2019). 241–84.
44. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
45. Chan, NY, Lam, SP, Zhang, J, Chan, JWY, Yu, MMW, Suh, S, et al. Efficacy of email-delivered versus face-to-face group cognitive behavioral therapy for insomnia in youths: a randomized controlled trial. J Adolesc Health. (2022) 70:763–73. doi: 10.1016/j.jadohealth.2021.11.005
46. Chan, NY, Li, SX, Zhang, J, Lam, SP, Kwok, APL, Yu, MWM, et al. A prevention program for insomnia in at-risk adolescents: a randomized controlled study. Pediatrics. (2021) 147:1–9. doi: 10.1542/peds.2020-006833
47. Clarke, G, McGlinchey, EL, Hein, K, Gullion, CM, Dickerson, JF, Leo, MC, et al. Cognitive-behavioral treatment of insomnia and depression in adolescents: a pilot randomized trial. Behav Res Ther. (2015) 69:111–8. doi: 10.1016/j.brat.2015.04.009
48. de Bruin, EJ, Bögels, SM, Oort, FJ, and Meijer, AM. Improvements of adolescent psychopathology after insomnia treatment: results from a randomized controlled trial over 1 year. J Child Psychol Psychiatry. (2018) 59:509–22. doi: 10.1111/jcpp.12834
49. de Bruin, EJ, Dewald-Kaufmann, JF, Oort, FJ, Bögels, SM, and Meijer, AM. Differential effects of online insomnia treatment on executive functions in adolescents. Sleep Med. (2015) 16:510–20. doi: 10.1016/j.sleep.2014.12.009
50. Egbegi, DR, Bella-Awusah, T, Omigbodun, O, and Ani, C. A controlled trial of cognitive Behavioural therapy-based strategies for insomnia among in-school adolescents in southern Nigeria. Child Adolesc Psychiatry Ment Health. (2021) 15:52–11. doi: 10.1186/s13034-021-00406-1
51. Goodhines, PA, Svingos, AM, Gerish, S, Park, A, and Gellis, LA. Randomized controlled trial of cognitive refocusing versus stimulus control treatment for college insomnia: feasibility of a brief, electronic-based, and peer-led approach. J Am Coll Health. (2022) 72:2229–41. doi: 10.1080/07448481.2022.2109031
52. Tomfohr-Madsen, L, Madsen, JW, Bonneville, D, Virani, S, Plourde, V, Barlow, KM, et al. A pilot randomized controlled trial of cognitive-behavioral therapy for insomnia in adolescents with persistent Postconcussion symptoms. J Head Trauma Rehabil. (2020) 35:E103–12. doi: 10.1097/htr.0000000000000504
53. Baldini, V, Gnazzo, M, Rapelli, G, Marchi, M, Pingani, L, Ferrari, S, et al. Association between sleep disturbances and suicidal behavior in adolescents: a systematic review and meta-analysis. Front Psych. (2024) 15:01–10. doi: 10.3389/fpsyt.2024.1341686
54. Palmer, CA, Oosterhoff, B, Bower, JL, Kaplow, JB, and Alfano, CA. Associations among adolescent sleep problems, emotion regulation, and affective disorders: findings from a nationally representative sample. J Psychiatr Res. (2018) 96:1–8. doi: 10.1016/j.jpsychires.2017.09.015
55. Logan, RW, Hasler, BP, Forbes, EE, Franzen, PL, Torregrossa, MM, Huang, YH, et al. Impact of sleep and circadian rhythms on addiction vulnerability in adolescents. Biol Psychiatry. (2018) 83:987–96. doi: 10.1016/j.biopsych.2017.11.035
56. Morin, CM. Insomnia: Psychological assessment and management. New York, NY: Guilford press (1993).
57. Morin, CM, and Espie, CA. Insomnia: a clinical guide to assessment and treatment. Berlin: Springer Science and Business Media (2007).
58. Spielman, AJ, Saskin, P, and Thorpy, MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. (1987) 10:45–56. doi: 10.1093/sleep/10.1.45
59. Maurer, LF, Espie, CA, and Kyle, SD. How does sleep restriction therapy for insomnia work? A systematic review of mechanistic evidence and the introduction of the triple-R model. Sleep Med Rev. (2018) 42:127–38. doi: 10.1016/j.smrv.2018.07.005
61. Verreault, MD, Granger, É, Neveu, X, Delage, JP, Bastien, CH, and Vallières, A. The effectiveness of stimulus control in cognitive behavioural therapy for insomnia in adults: a systematic review and network meta-analysis. J Sleep Res. (2024) 33:e14008–20. doi: 10.1111/jsr.14008
62. Jansson-Fröjmark, M, Nordenstam, L, Alfonsson, S, Bohman, B, Rozental, A, and Norell-Clarke, A. Stimulus control for insomnia: a systematic review and meta-analysis. J Sleep Res. (2024) 33:e14002–13. doi: 10.1111/jsr.14002
63. Trauer, JM, Qian, MY, Doyle, JS, Rajaratnam, SM, and Cunnington, D. Cognitive behavioral therapy for chronic insomnia. Ann Intern Med. (2015) 163:191–204. doi: 10.7326/M14-2841
64. Schwartz, DR, and Carney, CE. Mediators of cognitive-behavioral therapy for insomnia: a review of randomized controlled trials and secondary analysis studies. Clin Psychol Rev. (2012) 32:664–75. doi: 10.1016/j.cpr.2012.06.006
65. Kim, SJ, Lee, YJ, Kim, N, Kim, S, Choi, J-W, Park, J, et al. Exploration of changes in the brain response to sleep-related pictures after cognitive–behavioral therapy for psychophysiological insomnia. Sci Rep. (2017) 7:12528–10. doi: 10.1038/s41598-017-13065-0
66. Kim, N, Kang, SG, Lee, YJ, Kim, SJ, Kim, S, Choi, JW, et al. Decreased regional brain activity in response to sleep-related sounds after cognitive behavioral therapy for psychophysiological insomnia. Psychiatry Clin Neurosci. (2019) 73:254–61. doi: 10.1111/pcn.12822
67. Vgontzas, AN, Fernandez-Mendoza, J, Liao, D, and Bixler, EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. (2013) 17:241–54. doi: 10.1016/j.smrv.2012.09.005
68. van Dalfsen, JH, and Markus, CR. The influence of sleep on human hypothalamic–pituitary–adrenal (HPA) axis reactivity: A systematic review. Sleep Med Rev. (2018) 39:187–94. doi: 10.1016/j.smrv.2017.10.002
69. da Estrela, C, McGrath, J, Booij, L, and Gouin, J-P. Heart rate variability, sleep quality, and depression in the context of chronic stress. Ann Behav Med. (2021) 55:155–64. doi: 10.1093/abm/kaaa039
70. McCall, WV, Looney, SW, Zulfiqar, M, Ketcham, E, Jones, M, Mixson, C, et al. Daytime autonomic nervous system functions differ among adults with and without insomnia symptoms. J Clin Sleep Med. (2023) 19:1885–93. doi: 10.5664/jcsm.10704
71. Buckley, TM, and Schatzberg, AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. (2005) 90:3106–14. doi: 10.1210/jc.2004-1056
72. Jarrin, DC, Chen, IY, Ivers, H, Lamy, M, Vallières, A, and Morin, CM. Nocturnal heart rate variability in patients treated with cognitive–behavioral therapy for insomnia. Health Psychol. (2016) 35:638–41. doi: 10.1037/hea0000347
73. Hertenstein, E, Trinca, E, Wunderlin, M, Schneider, CL, Züst, MA, Fehér, KD, et al. Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: a systematic review and meta-analysis. Sleep Med Rev. (2022) 62:101597–14. doi: 10.1016/j.smrv.2022.101597
Keywords: adolescents, cognitive behavioral therapy, insomnia, sleep, meta-analysis
Citation: Mei Z, Cai C, Luo S, Zhang Y, Lam C and Luo S (2024) The efficacy of cognitive behavioral therapy for insomnia in adolescents: a systematic review and meta-analysis of randomized controlled trials. Front. Public Health. 12:1413694. doi: 10.3389/fpubh.2024.1413694
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Giorgia Varallo, University of Modena and Reggio Emilia, ItalyLeisha Cuddihy, University of Rochester, United States
Copyright © 2024 Mei, Cai, Luo, Zhang, Lam and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shi Luo, bHVvc2hpMDYwNEAxMjYuY29t
 Zhengyang Mei
Zhengyang Mei Chenyi Cai1
Chenyi Cai1 Shulai Luo
Shulai Luo Yuanzhuo Zhang
Yuanzhuo Zhang Chifong Lam
Chifong Lam Shi Luo
Shi Luo