- 1The Second Hospital of Jilin University, Jilin, China
- 2School of Nursing, Jilin University, Jilin, China
- 3National Center for Children’s Health, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Background: Medical staff play a crucial role in delivering healthcare services, especially during epidemics of infectious diseases such as coronavirus disease 2019 (COVID-19). However, there is a growing issue of burnout and low wellbeing among this group. While it is widely recognized that burnout has a negative impact on subjective wellbeing, the exact relationship between the two is not yet completely understood. The purpose of this study is to explore the chain mediating role of psychological capital and perceived social support between burnout and subjective wellbeing among medical staff.
Methods: Using the convenient sampling method, 604 medical staff were selected for a cross-sectional study. All participants completed a self-report questionnaire that collected demographic information, as well as data from the Maslach Burnout Inventory-Human Services Survey, General Wellbeing Schedule, Psychological Capital Questionnaire, and Perceived Social Support Scale. SPSS 27.0 and SPSS PROCESS macro were used for data analysis.
Results: There was a significant correlation between burnout, psychological capital, perceived social support, and subjective wellbeing (p < 0.01). Burnout not only has a direct negative impact on the subjective wellbeing of medical staff (effect: −0.2045; Bootstrap 95%CI: −0.2506, −0.1583), but also exerts an indirect influence on subjective wellbeing through three pathways: the independent mediating effect of psychological capital (effect: −0.0481; Bootstrap 95%CI: −0.0876, −0.0109), the independent mediating effect of perceived social support (effect: −0.0092; Bootstrap 95%CI: −0.0203, −0.0003), and the chained mediating effect of psychological capital and perceived social support (effect: −0.0092; Bootstrap 95%CI: −0.0183, −0.0019).
Conclusion: High burnout in medical staff can impair the level of psychological capital, leading to diminished perceived social support and ultimately reduced subjective wellbeing. The findings of this study contribute to understanding the potential pathways between burnout and subjective wellbeing and provide preliminary data support for developing strategies to improve the mental health of medical staff.
1 Background
With the sudden emergence of the coronavirus disease 2019 (COVID-19) pandemic and its continuously evolving variants posing significant challenges to the healthcare system, along with the advancements in the increasingly complex medical environment today, there are progressively higher demands placed on medical staff (1, 2). It is emphasized as a necessary condition to achieve universal health coverage to have a competent and qualified healthcare workforce to address epidemiological challenges and evolving health needs (3). However, there is a global shortage of medical staff (4, 5), leading to heavy workloads and decreased focus on the job. This can easily jeopardize physical and mental health, create burnout, and cause a decline in wellbeing.
Positive psychology is a pioneering method for dealing with burnout and enhancing wellbeing. It utilizes individuals’ potential, strengths, and functions to foster personal thriver (6, 7). In the field of positive psychology, the construction of wellbeing is attributed to the first pillar (i.e., positive subjective experiences), and subjective (or “hedonic”) wellbeing (SWB) is one of its important concepts (6). It pertains to how individuals assess the overall quality of their lives based on their criteria. It is widely used as a measure to evaluate mental health (8). This encompasses both reflective cognitive judgments (e.g., life satisfaction) and emotional reactions to one’s present circumstances (i.e., pleasant and unpleasant emotions) (9). SWB has gradually been recognized as a symbol of national prosperity (10). Since the introduction of positive psychology, research on individuals’ SWB has become increasingly popular, especially within specific organizational contexts (11). Medical staff are responsible for saving lives and caring for patients, serving as the backbone of healthcare services. Given the prominence of the healthcare system in social services, ensuring the quality of the work life of medical staff is an important factor in maintaining its stability. Medical staff’s sense of achievement and satisfaction in their professional lives has been conceptualized as occupational wellbeing (12), which is closely related to broader psychological wellbeing or SWB (13). Therefore, exploring the factors influencing the SWB of medical staff is essential for improving their SWB and further enhancing the level of medical care. To date, a large number of studies at home and abroad have explored the influencing factors of SWB (14–16).
Among the many factors that influence SWB, burnout is an important variable. The World Health Organization (WHO) defines burnout as an “occupational phenomenon” in the International Classification of Diseases 11th revision (17, 18). It is a syndrome caused by chronic work stress that has not been successfully managed and is a serious health problem (17, 18). It has three characteristics: feelings of energy depletion or exhaustion; increased psychological distance from one’s job, feelings of negativism or cynicism related to one’s job; and feelings of ineffectiveness and lack of accomplishment (17, 18). Studies show that burnout is common among medical staff, and this is a global phenomenon (19–22). During the COVID-19 pandemic, studies show that around two-thirds of medical staff experience high levels of burnout, which has become a crucial issue to consider (23, 24). According to a nationwide cross-sectional survey, the prevalence of burnout among Chinese medical staff is 60.8% (25), far higher than the global prevalence (21). The high incidence of medical staff burnout is directly reflected in personal physical health (26) (e.g., alcohol abuse or alcohol dependence), and work level (27) (e.g., negative work attitude, turnover intention). This will directly lead to a decline in the quality of patient care and an increase in medical malpractice litigation, resulting in direct economic costs and indirect reputation costs (28, 29). Not only that, but burnout has become one of the important factors hindering SWB (11), and it has a significant negative predictive effect on SWB (30–32). However, the potential impact path between burnout and SWB is not yet completely clear. Some studies have found that burnout has a predictive effect on mental health, and positive mental health can reduce burnout (27, 33). Therefore, it is necessary to understand the mechanisms, whether internal and external factors such as psychological capital (PsyCap) and social support are involved as mediators, to take effective measures based on positive psychology to prevent and reduce burnout and increase SWB.
The second pillar of positive psychology (i.e., positive individual traits) proposes that character strengths can enrich and promote various aspects of wellbeing (6, 34). PsyCap, as an extension of positive psychology ideas in the field of organizational behavior, refers to the positive psychological state or mental energy of an individual in the process of development or growth and contains four core components: self-efficacy, optimism, hope, and resilience (35). Specifically, it fosters confidence to succeed in the face of challenging tasks (self-efficacy), optimism about current and future success (optimism), and adherence to a positive motivational state that can re-establish pathways to achieve goals when needed (hope) (36). In addition, PsyCap provides a flexible ability to recover from failure, adversity, uncertainty, or overwhelming change (resilience) (36). Theoretical and practical evidence demonstrates that the malleability of PsyCap implies that its four components are sustainable and can have a wide-ranging impact on individuals’ attitudes and behaviors (37). For example, PsyCap can improve nursing burnout (38), alleviate depression (39), and influence wellbeing (40). Existing research has shown that PsyCap of medical staff has a significant negative impact on burnout (41–43). Furthermore, PsyCap plays a mediating role in the outcomes of nursing staff burnout, such as nursing performance (44). Medical staff’s PsyCap positively predicts occupational wellbeing (40). However, few studies have considered how burnout, PsyCap, and SWB are interrelated and interacted with each other. Therefore, it suggests that PsyCap can not only directly negatively impact medical staff’s burnout and positively predict SWB, but also serve as a mediating variable among relevant factors. Based on this, this study proposes Hypothesis 1 (H1): burnout can affect SWB through the mediating effect of PsyCap.
A positive social environment is the third pillar of positive psychology, manifested as positive groups and social institutions that are important for individual health (6). Social support as a powerful external factor refers to experiences valued, nurtured, and respected by those closest to the individual, who may receive support from various sources, including people and society. Perceived social support (PSS) refers to the degree to which individuals feel subjectively understood, respected, and supported by others in the social environment. It emphasizes individuals’ subjective perception, experience, and understanding of different types of social support, and influences their psychological wellbeing more than the actual social support (45). Research has found that through the help and protection provided by others, medical staff can to some extent avoid the occurrence of burnout (46, 47). Higher PSS is associated with lower burnout (48), higher wellbeing (49), higher PsyCap (43), and lower psychological distress (50). A review conducted among workers during the COVID-19 pandemic found a correlation between organizational support and the mental health of this population (51). The investigation of female physicians in Yantai City, Shandong Province, China, indicates that perceived family support plays a moderating role between burnout and SWB (49). Although previous studies have suggested the connection between PSS, burnout, and SWB among medical staff, there is still a need for further exploration due to the limited sample size and narrow research focus. Therefore, we propose Hypothesis 2 (H2): burnout can affect SWB through the mediating effect of PSS. In addition, considering the significant correlation between PSS and PsyCap among medical staff (43), as well as the positive predictive role of PsyCap on PSS in volunteers (52). Our Hypothesis 3 (H3) is that among medical staff, burnout can affect SWB through the chain intermediary effect of PsyCap and PSS.
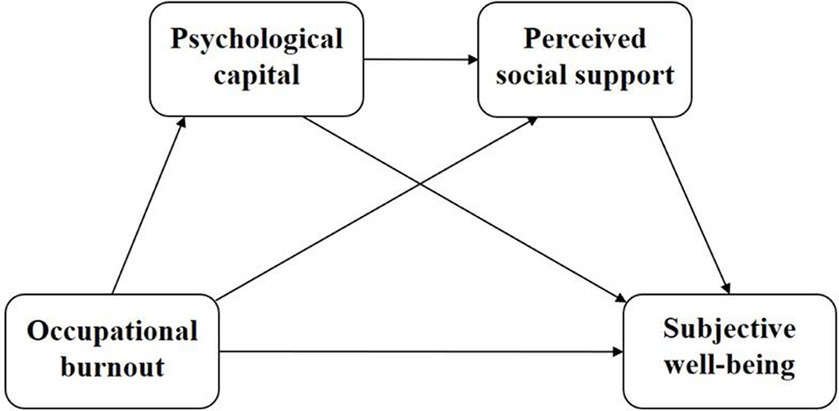
Previous research on medical staff burnout has focused on negative aspects (e.g., stress, depression), with less research on positive psychological emotion aspects. At the same time, despite previous research indicating the association between physician or nurse burnout, SWB, PsyCap, and PSS, in the actual clinical environment, physicians, technicians, and nurses in various departments do not exist independently but rather act as a unified whole in a division of labor and cooperation to play a therapeutic role. Currently, there is still a lack of in-depth exploration of the intrinsic structural relationships between these variables in the real clinical environment. Given the high prevalence of burnout among medical staff and the importance of SWB, exploring potential pathways between the two will contribute to a thriving medical workforce. In summary, this study has established a hypothetical model (Figure 1) aimed at clarifying the pathways and impact of the roles of medical staff burnout, SWB, PsyCap, and PSS, to provide a certain reference for future exploration of pathways to reduce medical staff burnout and enhance wellbeing.
2 Methods
2.1 Study design and participants
A cross-sectional study was conducted using a convenient sampling method from March to June 2022, involving 631 medical staff. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (53) (Supplementary Table S1). Participants were involved in the treatment or support work of the largest designated hospital for epidemic prevention and control in Changchun, China. Their original working units were, respectively, the First Hospital of Jilin University, the Second Hospital of Jilin University, the China-Japan Union Hospital of Jilin University, the Jilin Province People’s Hospital, the Affiliated Hospital of Changchun University of Traditional Chinese Medicine, and the Changchun Hospital of Traditional Chinese Medicine, a total of 6 tertiary medical institutions. They were invited to complete an online survey on the Questionnaire Star platform.1 The survey included self-reported questionnaires on demographic information, burnout, SWB, PsyCap, and PSS. The inclusion criteria were: (1) Medical staff who have worked in designated hospitals for infectious diseases including COVID-19 and were involved in treatment or support work for a minimum of 1 month; (2) Medical staff with practicing qualifications recognized by the National Health Commission and currently employed at the investigated hospitals; (3) Individuals capable of reading and understanding Chinese. The exclusion criteria were: (1) Participants with a confirmed history of mental illness; (2) Individuals who refused to participate.
2.2 Measures
2.2.1 SWB
The revised version of the General Wellbeing Schedule (GWBS) developed by Fazio (54) and adapted by Duan et al. (55) was used to measure SWB. The scale is divided into 6 dimensions: satisfaction and interest in life, concerns about health, energy status, happy or depressed mood, control over emotions and behavior, and degree of tension or relaxation. The higher the total score on the scale, the stronger the SWB (55). A total score of ≤48 is considered “low SWB,” 49–72 is “moderate SWB,” and ≥ 73 is “high SWB” (56). The Cronbach’s α was 0.856.
2.2.2 Burnout
The 22-item Maslach Burnout Inventory-Human Services Survey (MBI-HSS) (57) was used to measure burnout, which was divided into 3 dimensions: emotional exhaustion (EE), depersonalization (DP), and personal achievement (PA). The Chinese version was translated by Li et al. (58) and has good reliability and validity. The higher the score of EE and DP, the more serious the burnout; the higher the score of PA, the lower the degree of burnout. If the score of any dimension reaches or exceeds the threshold, the subject will detect burnout (59). The critical value of each dimension is defined as EE: low ≤16; moderate 17–26; high ≥27; DP: low ≤6; moderate 7–12; high ≥13; PA: low ≥39; moderate 32–38; high ≤31 (60). In this study, the Cronbach’s α was 0.781.
2.2.3 PsyCap
PsyCap was measured using the Psychological Capital Questionnaire (PCQ-24) compiled by Luthans et al. (36). This questionnaire contains 4 dimensions of self-efficacy, hope, resilience, and optimism. Higher scores indicate higher levels of PsyCap. The Cronbach’s α of the total scale was 0.933.
2.2.4 PSS
PSS was measured using the Perceived Social Support Scale (PSSS) developed by Zimet et al. (61) and revised by Qianjin (62). The scale includes perceived family, friends, and other support dimensions. The higher the score, the higher the PSS. The Cronbach’s α was 0.957.
2.3 Data analysis
All data were exported from the Questionnaire Star platform to SPSS (version 27.0, IBM Corp) for statistical analysis. All analyses were based on complete data. Before data analysis, Harman univariate tests were used to test for biases in common methods. Descriptive analysis (e.g., median, interquartile range (IQR), frequency, percentage) was used to present sample characteristics. Due to the non-normality of the data, Spearman correlation analysis was used to assess the relationship between variables. The SPSS macro PROCESS program (version 4.1) designed by Hayes (63) was used for mediation analysis using Model 6 to explore the relationship between burnout, PsyCap, PSS, and SWB. The Bootstrap confidence interval (CI) was set at 95%, with a Bootstrap sample size of 5,000. If the interval of the 95% CI did not include zero, it indicated a significant mediation effect. Type I error for all statistical analyses was p < 0.05 (two-sided).
2.4 Ethical considerations
This study was approved by the Ethics Committee of the School of Nursing, Jilin University (approval number: 2020030201). The survey was anonymous, confidential, and voluntary. Written informed consent was obtained from the participants before the survey (electronically, e.g., by clicking “yes”), and participants could choose to terminate the survey at any time.
3 Results
3.1 Common method deviation test
The data collected in this study comes from self-reports of the participants, so common method bias may exist. To reduce the impact of this bias on the study results, the Harman one-factor model method was used to test the degree of method bias in the data (64). The results showed that there were 12 factors with eigenvalues (i.e., the variances of the data in the directions of the eigenvectors) greater than 1, with the first factor explaining 29.56% of the variance, which was less than the critical standard of 40%, indicating that there was no serious homoscedasticity bias in the variables in this study (i.e., there was no serious variance attributable to the measurement method rather than the constructs of the measures in this study).
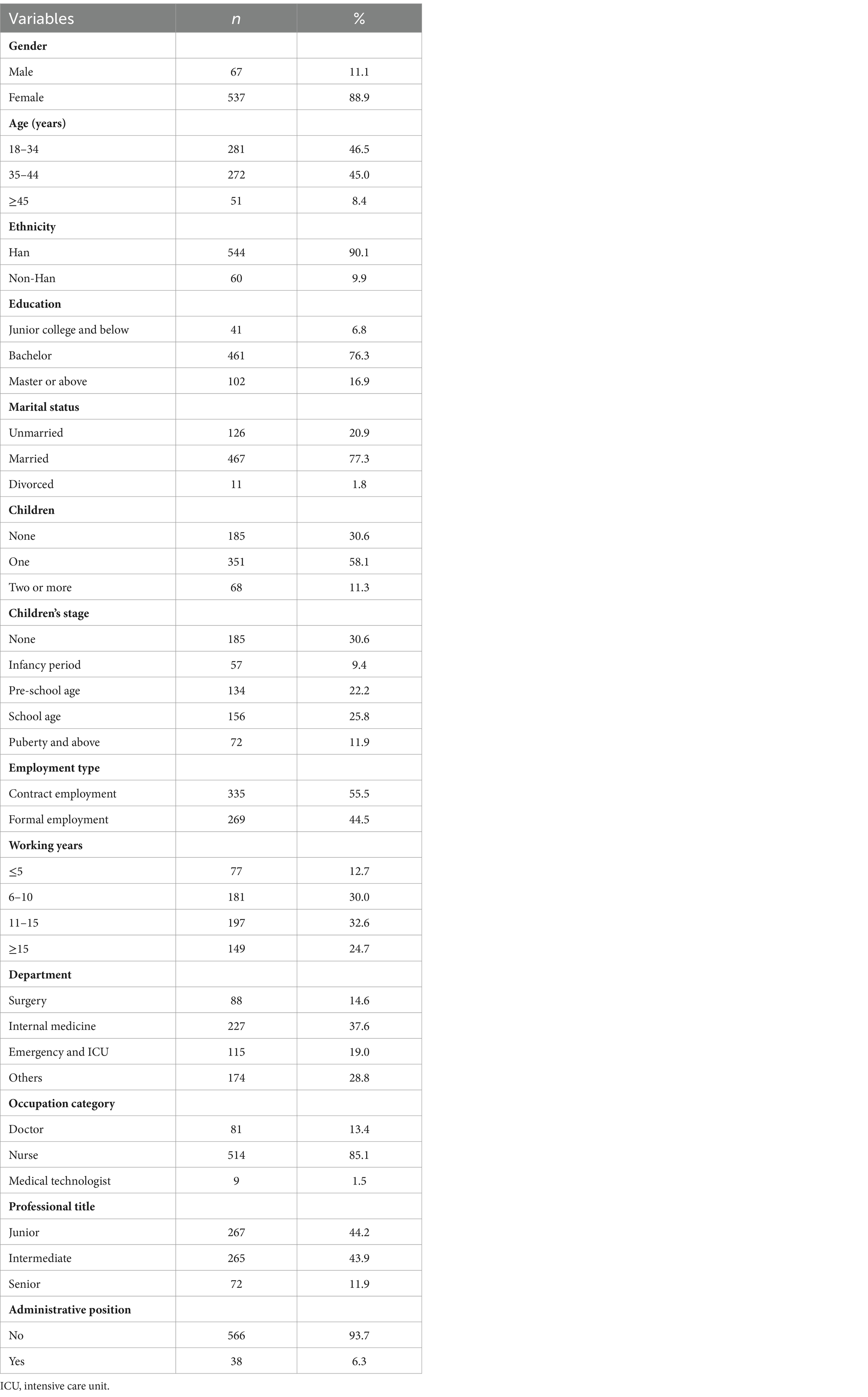
3.2 Demographic characteristics of participants
In this study, a total of 631 questionnaires were distributed. After eliminating 5 questionnaires with one or more missing answers and 22 questionnaires with 10 or more consecutively repeated responses, a total of 604 valid questionnaires were collected, achieving an effective response rate of 95.7%. The age of participants ranged from 19 to 64; 3.4% were physicians, 85.1% were nurses, and 1.5% were medical technologists (Table 1).
3.3 Descriptive analysis of participants’ scale scores
Among the surveyed medical staff, the GWBS total score had a median of 78.00 (IQR: 68.00–89.00), with 1.8% reporting low SWB, 34.9% reporting moderate SWB, and 63.2% reporting high SWB. The lowest scored dimensions were “Satisfaction and interest in life” with a score of 7.00 (IQR: 6.00–8.00) and “Concerns about health” with a score of 6.00 (IQR: 5.00–8.00). The MBI-HSS total score had a median of 56.00 (IQR: 47.00–67.00), with a burnout detection rate of 52.5%, including 35.8% experiencing low burnout, 12.9% experiencing moderate burnout, and 3.8% experiencing high burnout. The PCQ total score had a median of 90.00 (IQR: 81.25–94.00), and the PSSS total score had a median of 65.00 (IQR: 54.00–72.00). The dimension scores of the scale are detailed in Table 2.
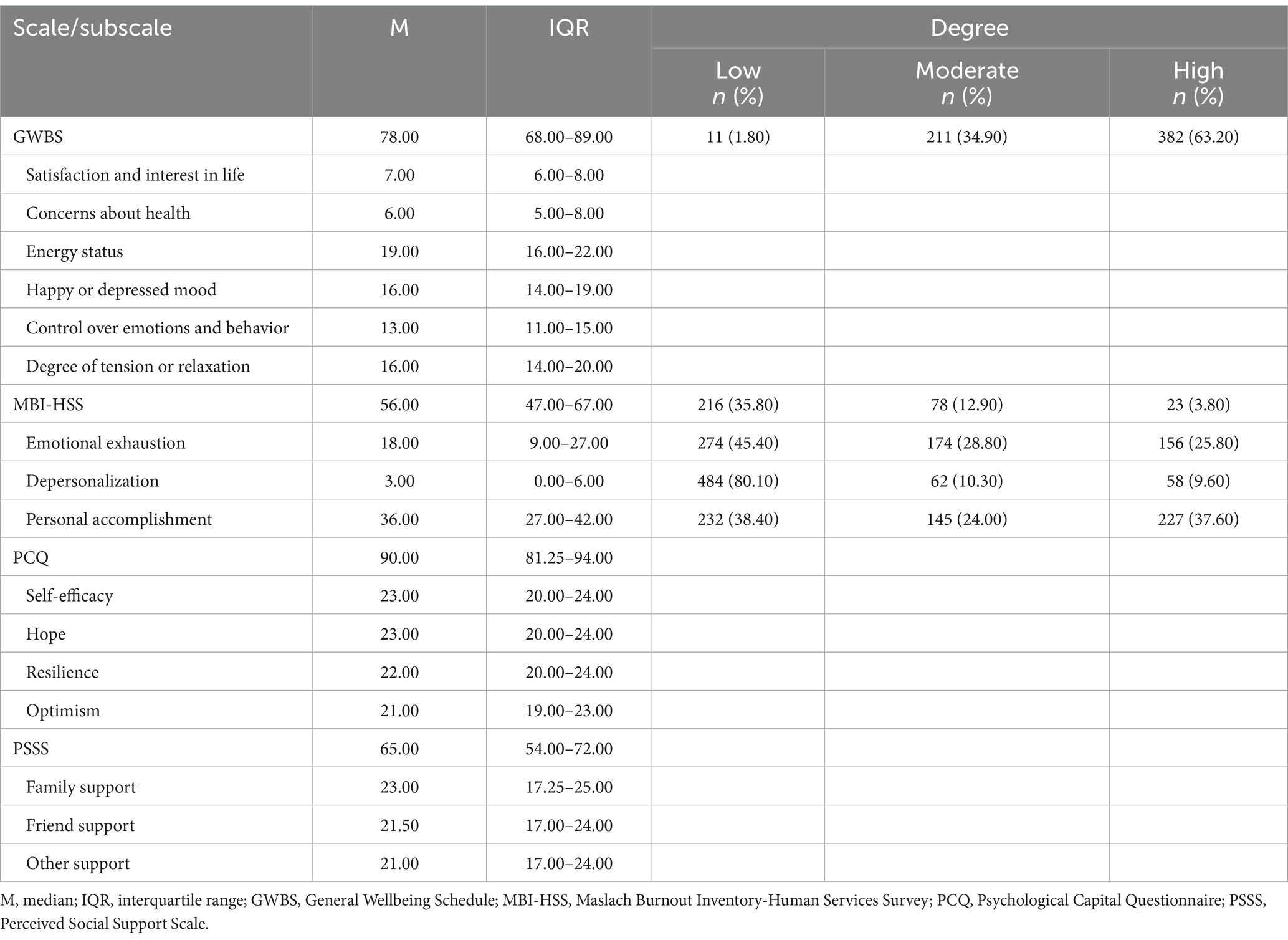
Table 2. Descriptive summary of subjective wellbeing, occupational burnout, psychological capital, and perceived social support (n = 604).
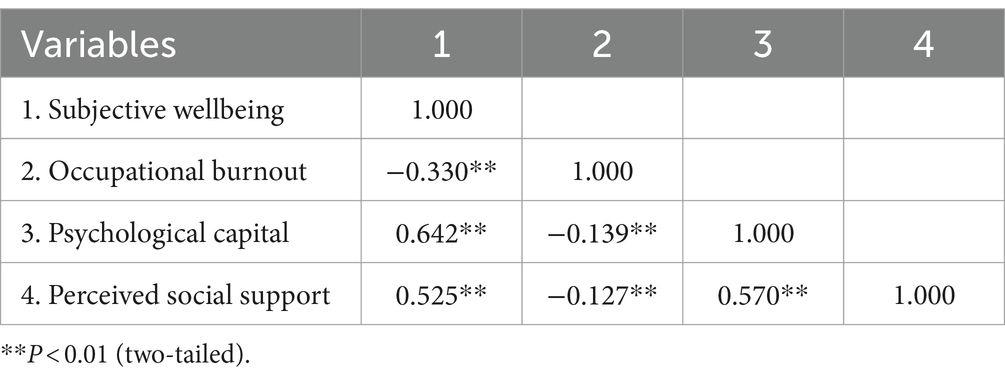
3.4 Correlation analysis
The Spearman correlation analysis results indicated that burnout among medical staff was negatively correlated with SWB (r = −0.330, p < 0.01), PsyCap (r = −0.139, p < 0.01), and PSS (r = −0.127, p < 0.01); PsyCap was positively correlated with SWB (r = 0.642, p < 0.01) and PSS (r = 0.570, p < 0.01), thus meeting the requirements for intermediary effect analysis. Additionally, all correlation coefficients were below 0.700, indicating that there was no multicollinearity in the data (i.e., no high correlations between two or more variables) (see Table 3 for details).
3.5 Mediation effect analyses
As shown in Table 4 and Figure 2, firstly, burnout significantly negatively predicted the SWB of medical staff (β = −0.3432, p < 0.001, Model 1). Secondly, burnout had significant negative predictive effects on PsyCap (β = −0.1223, p < 0.01, Model 2) and PSS (β = −0.0724, p < 0.05, Model 3). Thirdly, PsyCap significantly positively predicted PSS (β = 0.5967, p < 0.001, Model 3). Fourthly, when burnout, PsyCap, and PSS simultaneously entered the regression equation (Model 4), the predictive effect of burnout remained significant (β = −0.2590, p < 0.001), and PsyCap (β = 0.4980, p < 0.001) and PSS (β = 0.1602, p < 0.001) both significantly positively predicted SWB.
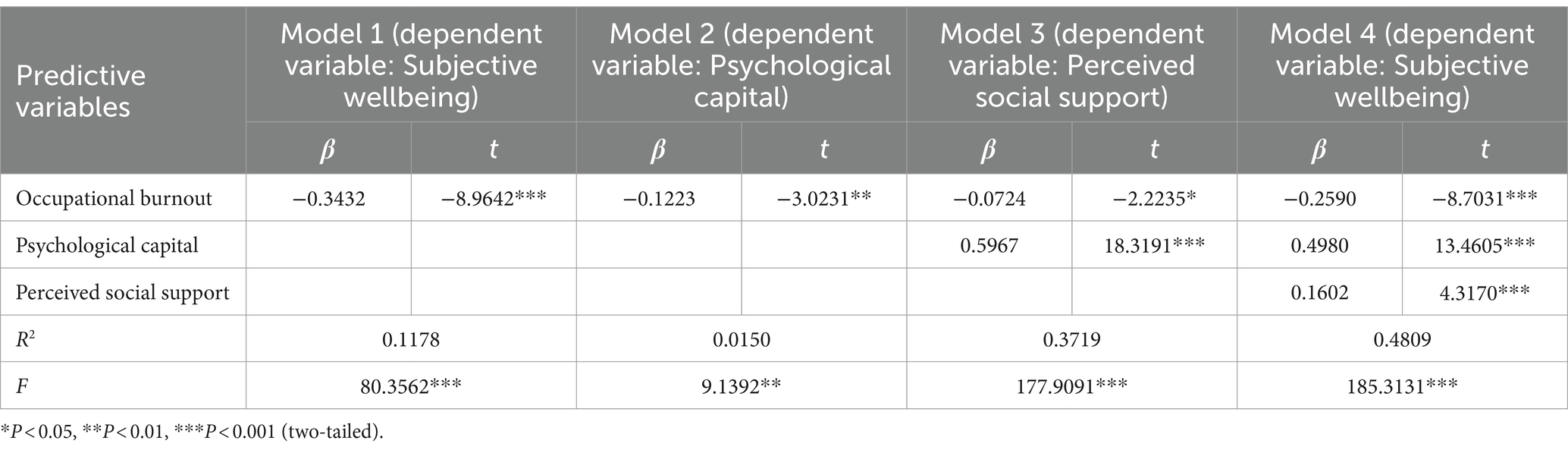
Table 4. Regression analysis of the relationship between variables in the mediation effect model (n = 604).

Figure 2. The chain mediating model of psychological capital and perceived social support on occupational burnout and subjective well-being. *P < 0.05, **P < 0.01, ***P < 0.001 (two-tailed).
Finally, we used the Bootstrap method with percentile bias correction to test the mediating effects of PsyCap and PSS on the relationship between burnout and SWB. The results indicated that the mediating effects of PsyCap and PSS were significant, with the total indirect effect of 0.0665, accounting for 24.55% of the total effect (0.2709). Specifically, the mediating effect consisted of three paths supporting H1, H2, and H3. Firstly, the path coefficient of the indirect effect of burnout on SWB through PsyCap was −0.0481 (Bootstrap 95%CI: −0.0876, −0.0109). Secondly, the path coefficient of the indirect effect of burnout on SWB through PSS was −0.0092 (Bootstrap 95%CI: −0.0203, −0.0003). Thirdly, the path coefficient of the indirect effect of burnout on SWB through PsyCap and PSS was −0.0092 (Bootstrap 95%CI: −0.0183, −0.0019). Detailed results are available in Table 5 and Figure 2.
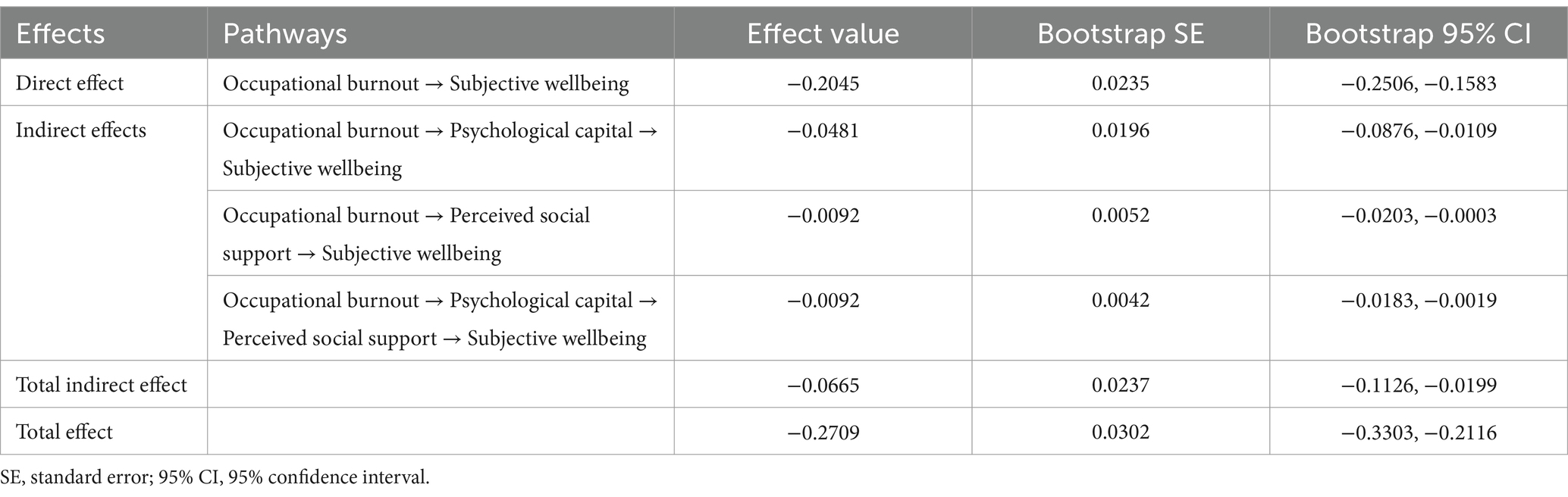
Table 5. Direct, indirect, and total effects of occupational burnout on subjective wellbeing (n = 604).
4 Discussion
In this study, we examined the relationship between medical staff’s burnout and SWB, as well as the mediating roles of PsyCap and PSS. Our findings indicate that PsyCap and PSS mediate the relationship between burnout and SWB. Therefore, the model suggests that burnout negatively influences PsyCap and PSS, leading to a decrease in SWB.
4.1 Current state of SWB of medical staff
In this study, the SWB of medical staff was slightly lower than that of the study results of Aggar et al. (65), indicating that the overall SWB of medical staff in China is slightly lower. The reason for this difference may be that their study participants were nurses in Australia, while China is a country with a large population base. With the opening of the two-child policy and the increasing aging population, the number of patients and the demand for medical care in tertiary public hospitals in China has reached an unprecedented level. There are only 6.94 professional public health personnel per 10,000 people, which is significantly lower than in other developed countries, causing each medical staff to provide services to more patients, requiring Chinese medical staff to work overtime frequently, with long working hours and heavy workloads (66). In addition, more than three-quarters of our research subjects are married, and the conflict between family and work may further lead to lower life satisfaction. Furthermore, the dimensions with the lowest scores are “Satisfaction and interest in life” and “Concerns about health,” which is similar to several studies (67–69), indicating that our study sample may experience a decrease in satisfaction and interest in life due to frequent shift work, disrupted circadian rhythms, and unresolved physical fatigue. At the same time, this study was conducted during the COVID-19 pandemic, during which medical staff frequently come into contact with highly infectious and critically ill patients, which may exacerbate their concerns about their health. A meta-analysis of the SWB of medical staff in China showed that the SWB of medical staff declined more significantly compared to other populations (e.g., college students, and older adults) (70).
4.2 The direct effect of burnout on SWB of medical staff
Wellbeing is broader than wellness and mainly focuses on personal responsibility (71). At present, research mainly measures the level of wellbeing in terms of SWB. SWB fluctuates throughout life (72) and is influenced by life events (73). This suggests that exploring potential pathways to improve the level of SWB is valuable, and understanding the factors and pathways that affect the level of SWB of medical staff is crucial for targeted interventions. Multiple studies have shown that burnout among medical staff is closely related to decreased SWB (25, 30, 49, 74). This indicates to healthcare system managers that the SWB of medical staff is not high and that their burnout is closely linked. It is important to pay attention to the relationship between the two and understand the factors and pathways that affect the level of SWB of medical staff to carry out targeted interventions. This study found that burnout significantly predicts a decrease in SWB among medical staff. This is consistent with previous findings in populations such as physicians, athletic coaches, and police officers (11, 75, 76), and this phenomenon may be related to the following factors. The Conservation of resources theory (77) posits that individuals have a natural inclination to seek and preserve valuable resources, such as time, wealth, optimism, and support. Whether a resource has been lost or is at risk of loss, it can cause stress to the individual (77). In the workplace, when individuals become aware that their resources are at risk and struggle to adjust to their jobs, it leads to a cycle of resource loss. This cycle creates job stress and eventually results in burnout (78). The progression of burnout amplifies an individual’s detrimental actions (e.g., heightened tobacco consumption, insufficient physical exercise, and lack of sleep), which subsequently results in various physiological manifestations; moreover, burnout tends to generate more frequent adverse emotions, giving rise to psychological symptoms like anxiety and depression (79). Burnout results in the exhaustion of both physical and mental resources. This exhaustion then makes it difficult for individuals to effectively allocate time and effort toward other responsibilities (e.g., family roles). It also creates conflicts and disruptions in their ability to balance their work and family life (80, 81). SWB is primarily comprised of cognitive and affective elements, which encompass evaluations of life satisfaction and positive/negative emotional reactions (9). Burnout can cause damage to physical and mental health, and work–family conflict can lead to a decrease in SWB. Current research provides supportive evidence for this hypothesis. The research results also inspire us to strengthen the improvement of burnout among medical staff, which is very necessary for enhancing SWB.
4.3 Mediation effects of PsyCap and PSS
This study demonstrates that PsyCap plays an important mediating role in the relationship between burnout and SWB among Chinese medical staff, confirming H1. This means that medical staff with high levels of burnout are more likely to have lower PsyCap, leading to a decrease in SWB. This is similar to previous findings in the nursing population (44, 82). The mechanisms may be related to the following factors: the Job Demands-Resources model (JD-R) suggests that the interaction between job demands and job resources affects the development of burnout (83). Job resources, which include a combination of internal and external resources, can reduce the impact of job demands on burnout (84). As an important internal positive psychological resource, individuals with high levels of PsyCap generally have a positive attitude and confidence in their work, and offer more positive interpretations of work events, making it easier for them to recover from setbacks and failures (85, 86). Additionally, the broaden hypothesis in the Broaden-and-Build theory proposes that positive emotions increase an individual’s focus and awareness of their environment, allowing them to have a broader range of thoughts and perceptions than normal (87). This enhances wellbeing due to increased physical, psychological, and social resources (87). In this sense, PsyCap gives individuals the ability to innovate, etc. (88, 89), which improves the SWB in terms of individual psychological ability and strength. In addition, those with high levels of PsyCap are better able to overcome stress appropriately, feel more comfortable physically and mentally, and tend to have positive outcomes on SWB (90). This is similar to a cross-sectional study result conducted by Ravikumar among medical staff and police personnel during the COVID-19 pandemic (91). They found that positive PsyCap helps reduce occupational stress and improve mental health. This finding suggests that despite the negative impact of burnout on SWB, medical staff with sufficient PsyCap resources can mitigate this impact and reduce the damage to SWB.
This study also found that the PSS is an intermediate variable between burnout and SWB among Chinese medical staff, confirming H2. This is consistent with previous research findings (92). The underlying mechanism may be related to the following factors: firstly, the PSS as an important external resource may improve burnout by reducing job demands and supporting the JD-R model perspective from another angle (84). When individuals receive support from their work group, external work resources increase, effectively reducing the occurrence of burnout. Additionally, previous research has shown that work relationships characterized by lack of support and trust increase the risk of burnout (93). Conversely, when work relationships are positive and there is a high level of social support, employees are more likely to resolve conflicts effectively and be more engaged in their work. For medical staff, perceiving support from family, friends, or others can reduce negative emotions such as fatigue or indifference, increase personal achievement or confidence, and thereby reduce the occurrence and development of burnout. A narrative review highlighted that during the COVID-19 pandemic, peer support as one of the sources of social support, is a key factor in managing work stress (51). Furthermore, the theory of subjective wellbeing homeostasis indicates that SWB is maintained by stable forces such as adaptation and positive emotions (94). At the same time, the maintenance of SWB is influenced by emotional responses, and if internal stable resources are strong, SWB will remain within a normal range (94). As a positive social psychological resource for individuals, PSS can help buffer stress sources in the body’s balancing system, thereby maintaining the relative stability of an individual’s SWB. Therefore, for medical staff, PSS as a buffer for burnout can help individuals cope with burnout, reduce the negative effects of burnout on physical and mental health, and thus affect SWB.
In addition, this study provides small but significant support for the chain intermediary role of PsyCap and PSS between burnout and SWB among medical staff, which has not been explored in previous studies. In the mediation path of burnout and SWB, PsyCap plays a partial mediating role in the relationship between burnout and PSS, indicating that positive PsyCap can serve as an important buffer to prevent the impact of burnout on the PSS among medical staff. Positive emotions can lead individuals to a growth trajectory, enabling them to identify and build their resources, and these resources are enduring (87). As an inherent positive psychological resource within individuals, multiple studies (95, 96) have confirmed that individuals with high levels of PsyCap generally perceive more prominent material and emotional support between family members and peers, which provides support for the build hypothesis in the broaden-and-build theory. Furthermore, the burnout experienced by medical staff can lead to a decrease in positive psychological resources such as low hope levels and low self-efficacy. At the same time, psychological resources serve as an important mediator for PSS. Faced with the vast work system and personnel structure of tertiary hospitals, individuals with low psychological resources are more likely to show social detachment from colleagues and experience a decrease in PSS, which in turn leads to lower SWB. Therefore, burnout can affect the SWB among medical staff through the chain intermediary role of PsyCap and PSS.
Existing intervention research has found that positive psychology interventions can enhance the PsyCap level of primary care physicians, change work behavior (e.g., coping with work more effectively), improve work-related outcomes (e.g., burnout), and thus influence wellbeing (97). Moreover, interventions including a module that enhances PSS can improve certain components of wellbeing, particularly work stress (98). This result inspires us to develop positive psychology interventions or to develop psychological interventions that include enhancing PsyCap and PSS components, to improve medical staff’s burnout and promote SWB.
4.4 Relevance to clinical practice
In China, even if they do not have serious illnesses, patients tend to prefer seeking medical treatment at large public hospitals (99). This results in a high outpatient volume and a large number of hospitalized patients at tertiary hospitals, which can easily lead to burnout among medical staff (100), but the clinical demand for healthcare services is increasing. Therefore, it has become particularly important to improve the SWB of medical staff who are the main body for saving lives. This study has certain theoretical significance and practical value for improving the SWB of medical staff. Given the important mediating role of PsyCap and PSS in the relationship between burnout and SWB, we propose the following suggestions to improve medical staff burnout and ultimately enhance their level of SWB. Firstly, it is important to focus on and enhance individuals’ level of PsyCap. Luthans et al. (101) argue that PsyCap is a state-like individual resource that can be changed and improved. The methods proposed by Luthans et al. (35, 101) for developing PsyCap include: allowing employees to experience success to develop self-efficacy and confidence; accepting their past mistakes, failures, and setbacks; encouraging them to appreciate the present and be grateful for positive aspects of life, etc. Secondly, it is important to prioritize and enhance the individual’s PSS as much as possible. This is closely related to the level of individual PsyCap and the harmonious organizational atmosphere. Therefore, we hope to strengthen the attention to burnout and wellbeing among medical staff at the policy-making level, create a positive work atmosphere at the organizational leadership level, and focus on enhancing positive psychological resources at the individual level.
4.5 Limitations
This study also has notable limitations. Firstly, it is a cross-sectional survey design, which cannot establish a causal model. Therefore, further investigation and validation should be conducted by combining longitudinal studies and in vitro and in vivo experiments to further uncover the specific mechanisms of the mediating effect in this study. Secondly, the data is sourced from a sample of medical staff in Changchun, Jilin Province, China, which limits the generalizability of the research findings. Lastly, the assessment of variables is based on self-reported results, which cannot exclude response bias.
5 Conclusion
Based on determining the current status of medical staff’s burnout and SWB, this study constructed a mediation model to investigate the processes and mechanisms by which burnout affects medical staff’s SWB. The research findings indicate that high levels of burnout not only lead to a decrease in the SWB of medical staff but also affect their PsyCap and PSS. Additionally, burnout decreases the PsyCap and PSS among medical staff, thereby reducing their SWB. Furthermore, a novel contribution of this current study is the exploration of PsyCap and PSS as chain intermediary roles in burnout and SWB. This study provides initial data support for the design of intervention strategies targeting medical staff burnout and SWB. Enhancing PsyCap and PSS are potential strategies for reducing burnout and improving SWB. Hospital managers should take corresponding measures to enhance medical staff’s PsyCap and PSS, thereby improving their SWB. This will play a certain role in promoting the quality and level of medical staff’s services, while ensuring the vigorous and stable development of the national healthcare system. In addition, this will provide hospital administrators and medical staff with better reference for coping with potential sudden public health emergencies in the future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the School of Nursing, Jilin University (approval number: 2020030201). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JF: Conceptualization, Methodology, Writing – original draft. YC: Conceptualization, Formal analysis, Investigation, Writing – original draft. LL: Data curation, Investigation, Writing – original draft. NJ: Investigation, Resources, Writing – original draft. ZQ: Data curation, Resources, Writing – original draft. JZ: Formal analysis, Resources, Writing – original draft. ML: Formal analysis, Visualization, Writing – original draft. BL: Supervision, Writing – review & editing. DQ: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge the support and contributions of all the medical staff and researchers involved in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1408006/full#supplementary-material
Footnotes
References
1. Jia, L, Ye, M, Wang, H, and Wang, H. Physical discomforts, feeling of the high work intensity and the related risk factors of the frontline medical staff during COVID-19 epidemic: an early-outbreak, national survey in China. Front Public Health. (2023) 11:1270366. doi: 10.3389/fpubh.2023.1270366
2. Chang, Q, Su, H, Xia, Y, Gao, S, Zhang, M, Ma, X, et al. Association between clinical competencies and mental health symptoms among frontline medical staff during the COVID-19 outbreak: a cross-sectional study. Front Psych. (2022) 13:760521. doi: 10.3389/fpsyt.2022.760521
3. World Health Organization. Sixty-ninth World Health Assembly. Resolution WHA.69.19: Global strategy on human resources for health: workforce 2030. (2016). Available at: http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_R19-en.pdf?ua=1&ua=1
4. Haakenstad, A, Irvine, CMS, Knight, M, Bintz, C, Aravkin, AY, Zheng, P, et al. Measuring the availability of human resources for health and its relationship to universal health coverage for 204 countries and territories from 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2022) 399:2129–54. doi: 10.1016/s0140-6736(22)00532-3
5. World Health Organization. State of the world's nursing 2020: investing in education, jobs and leadership. (2020). Available at: https://www.who.int/publications/i/item/9789240003279.
6. Seligman, ME, and Csikszentmihalyi, M. Positive psychology. An introduction. Am Psychol. (2000) 55:5–14. doi: 10.1037//0003-066x.55.1.5
7. Seligman, ME. Flourish: a visionary new understanding of happiness and well-being. New York, NY: Free Press (2011).
8. Diener, E, Suh, EM, Lucas, RE, and Smith, HL. Subjective well-being: three decades of progress. Psychol Bull. (1999) 125:276–302. doi: 10.1037//0033-2909.125.2.276
9. Diener, E, Oishi, S, and Tay, L. Advances in subjective well-being research. Nat Hum Behav. (2018) 2:253–60. doi: 10.1038/s41562-018-0307-6
10. Dolan, P, and Metcalfe, R. Measuring subjective wellbeing: recommendations on measures for use by National Governments. J Soc Policy. (2012) 41:409–27. doi: 10.1017/S0047279411000833
11. Fu, Y, Huang, D, Zhang, S, and Wang, J. Job burnout on subjective wellbeing among clinicians in China: the mediating role of mental health. Front Psychol. (2023) 14:1227670. doi: 10.3389/fpsyg.2023.1227670
12. Doble, SE, and Santha, JC. Occupational well-being: rethinking occupational therapy outcomes. Can J Occup Ther. (2008) 75:184–90. doi: 10.1177/000841740807500310
13. National Academies of Sciences E, Medicine, National Academy of M, Committee on Systems Approaches to Improve Patient Care by Supporting Clinician W-B. Taking action against clinician burnout: a systems approach to professional well-being. Washington, DC: National Academies Press (2019).
14. Anglim, J, Horwood, S, Smillie, LD, Marrero, RJ, and Wood, JK. Predicting psychological and subjective well-being from personality: a meta-analysis. Psychol Bull. (2020) 146:279–323. doi: 10.1037/bul0000226
15. Stone, AA, Broderick, JE, Wang, D, and Schneider, S. Age patterns in subjective well-being are partially accounted for by psychological and social factors associated with aging. PLoS One. (2020) 15:e0242664. doi: 10.1371/journal.pone.0242664
16. Zou, W, Zeng, Y, Peng, Q, Xin, Y, Chen, J, and Houghton, JD. The influence of spiritual leadership on the subjective well-being of Chinese registered nurses. J Nurs Manag. (2020) 28:1432–42. doi: 10.1111/jonm.13106
17. World Health Organization. Burn-out an "occupational phenomenon": international classification of Diseases. Available at: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases.
18. World Health Organization. International classification of diseases - eleventh revision. (2022). Available at: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281.
19. Wright, T, Mughal, F, Babatunde, OO, Dikomitis, L, Mallen, CD, and Helliwell, T. Burnout among primary health-care professionals in low- and middle-income countries: systematic review and meta-analysis. Bull World Health Organ. (2022) 100:385–401a. doi: 10.2471/blt.22.288300
20. Low, ZX, Yeo, KA, Sharma, VK, Leung, GK, McIntyre, RS, Guerrero, A, et al. Prevalence of burnout in medical and surgical residents: a meta-analysis. Int J Environ Res Public Health. (2019) 16:1479. doi: 10.3390/ijerph16091479
21. Woo, T, Ho, R, Tang, A, and Tam, W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. (2020) 123:9–20. doi: 10.1016/j.jpsychires.2019.12.015
22. Wang, Z, Koenig, HG, Tong, Y, Wen, J, Sui, M, Liu, H, et al. Moral injury in Chinese health professionals during the COVID-19 pandemic. Psychol Trauma. (2022) 14:250–7. doi: 10.1037/tra0001026
23. Hassan, MEG, Elsehrawy, MG, Eltayeb, MM, Ebrahim, EE, and Abd-Elsalam, NAE. Burnout and stress among healthcare Workers at Primary Healthcare Centers: the role of COVID-19 pandemic. Int J Biomed. (2022) 12:256–64. doi: 10.21103/Article12(2)_OA10
24. Khosravi, M, Ghiasi, Z, and Ganjali, A. A narrative review of research on healthcare staff’s burnout during the COVID-19 pandemic. Proc Sing Healthcare. (2021) 31:201010582110405. doi: 10.1177/20101058211040575
25. Xiao, Y, Dong, D, Zhang, H, Chen, P, Li, X, Tian, Z, et al. Burnout and well-being among medical professionals in China: a National Cross-Sectional Study. Front Public Health. (2021) 9:761706. doi: 10.3389/fpubh.2021.761706
26. Oreskovich, MR, Kaups, KL, Balch, CM, Hanks, JB, Satele, D, Sloan, J, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. (2012) 147:168–74. doi: 10.1001/archsurg.2011.1481
27. West, CP, Dyrbye, LN, and Shanafelt, TD. Physician burnout: contributors, consequences and solutions. J Intern Med. (2018) 283:516–29. doi: 10.1111/joim.12752
28. Hodkinson, A, Zhou, A, Johnson, J, Geraghty, K, Riley, R, Zhou, A, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. (2022) 378:e070442. doi: 10.1136/bmj-2022-070442
29. Han, S, Shanafelt, TD, Sinsky, CA, Awad, KM, Dyrbye, LN, Fiscus, LC, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. (2019) 170:784–90. doi: 10.7326/m18-1422
30. Kim, G, Yu, H, and Ryu, E. Social group membership, burnout, and subjective well-being in new nurses in the life transition period: a cross-sectional study. Nurs Open. (2023) 10:3295–304. doi: 10.1002/nop2.1581
31. Poulsen, MG, Poulsen, AA, Khan, A, Poulsen, EE, and Khan, SR. Factors associated with subjective well-being in cancer workers in Queensland. J Med Imaging Radiat Oncol. (2012) 56:347–53. doi: 10.1111/j.1754-9485.2012.02368.x
32. Safiye, T, Vukcevic, B, and Cabarkapa, M. Resilience as a moderator in the relationship between burnout and subjective well-being among medical workers in Serbia during the COVID-19 pandemic [article]. Vojnosanit Pregl. (2021) 78:1207–13. doi: 10.2298/VSP210517070S
33. Kumar, S. Burnout and doctors: prevalence, prevention and intervention. Healthcare. (2016) 4:37. doi: 10.3390/healthcare4030037
34. Peterson, C, and Seligman, M. Character strengths and virtues: a handbook and classification. New York, NY; Washington, DC: Oxford University Press (2004).
35. Luthans, F, Luthans, KW, and Luthans, BC. Positive psychological capital: beyond human and social capital. Bus Horiz. (2004) 47:45–50. English. doi: 10.1016/j.bushor.2003.11.007
36. Luthans, F, Youssef, CM, and Avolio, BJ. Psychological capital: developing the human competitive edge. New York, NY: Oxford University Press (2007).
37. Peterson, SJ, Luthans, F, Avolio, BJ, Walumbwa, FO, and Zhang, Z. Psychological capital and employee performance: a latent growth modeling approach [article]. Pers Psychol. (2011) 64:427–50. doi: 10.1111/j.1744-6570.2011.01215.x
38. Li, Y, Wu, Q, Li, Y, Chen, L, and Wang, X. Relationships among psychological capital, creative tendency, and job burnout among Chinese nurses. J Adv Nurs. (2019) 75:3495–503. doi: 10.1111/jan.14141
39. Sun, L, Zhang, Y, He, J, Qiao, K, Wang, C, Zhao, S, et al. Relationship between psychological capital and depression in Chinese physicians: the mediating role of organizational commitment and coping style. Front Psychol. (2022) 13:904447. doi: 10.3389/fpsyg.2022.904447
40. Hao, C, Zhu, L, Zhang, S, Rong, S, Zhang, Y, Ye, J, et al. Serial multiple mediation of professional identity, and psychological Capital in the Relationship between Work-Related Stress and Work-Related Well-Being of ICU nurses in China: a cross-sectional questionnaire survey. Front Psychol. (2020) 11:535634. doi: 10.3389/fpsyg.2020.535634
41. Zhou, J, Yang, Y, Qiu, X, Yang, X, Pan, H, Ban, B, et al. Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. (2018) 83:75–82. doi: 10.1016/j.ijnurstu.2018.03.016
42. Sui, G, Liu, G, Jia, L, Wang, L, and Yang, G. Associations of workplace violence and psychological capital with depressive symptoms and burn-out among doctors in Liaoning, China: a cross-sectional study. BMJ Open. (2019) 9:e024186. doi: 10.1136/bmjopen-2018-024186
43. Tang, Y, Wang, Y, Zhou, H, Wang, J, Zhang, R, and Lu, Q. The relationship between psychiatric nurses' perceived organizational support and job burnout: mediating role of psychological capital. Front Psychol. (2023) 14:1099687. doi: 10.3389/fpsyg.2023.1099687
44. An, M, Shin, ES, Choi, MY, Lee, Y, Hwang, YY, and Kim, M. Positive psychological capital mediates the association between burnout and nursing performance outcomes among hospital nurses. Int J Environ Res Public Health. (2020) 17:5988. doi: 10.3390/ijerph17165988
45. Hefner, J, and Eisenberg, D. Social support and mental health among college students. Am J Orthopsychiatry. (2009) 79:491–9. doi: 10.1037/a0016918
46. Sampei, M, Okubo, R, Sado, M, Piedvache, A, Mizoue, T, Yamaguchi, K, et al. Emotional exhaustion of burnout among medical staff and its association with mindfulness and social support: a single center study during the COVID-19 pandemic in Japan. Front Psych. (2022) 13:774919. doi: 10.3389/fpsyt.2022.774919
47. Song, X, Li, H, Jiang, N, Song, W, Ding, N, and Wen, D. The mediating role of social support in the relationship between physician burnout and professionalism behaviors. Patient Educ Couns. (2021) 104:3059–65. doi: 10.1016/j.pec.2021.04.025
48. Hamama, L, Hamama-Raz, Y, Stokar, YN, Pat-Horenczyk, R, Brom, D, and Bron-Harlev, E. Burnout and perceived social support: the mediating role of secondary traumatization in nurses vs. physicians. J Adv Nurs. (2019) 75:2742–52. doi: 10.1111/jan.14122
49. Wang, L, Wang, H, Shao, S, Jia, G, and Xiang, J. Job burnout on subjective well-being among Chinese female doctors: the moderating role of perceived social support. Front Psychol. (2020) 11:435. doi: 10.3389/fpsyg.2020.00435
50. Feng, D, Su, S, Wang, L, and Liu, F. The protective role of self-esteem, perceived social support and job satisfaction against psychological distress among Chinese nurses. J Nurs Manag. (2018) 26:366–72. doi: 10.1111/jonm.12523
51. Lulli, LG, Giorgi, G, Pandolfi, C, Foti, G, Finstad, GL, Arcangeli, G, et al. Identifying psychosocial risks and protective measures for Workers' mental wellbeing at the time of COVID-19: a narrative review [article]. Sustain For. (2021) 13:13869. doi: 10.3390/su132413869
52. Xu, LP, Liao, JB, Wu, YS, and da Kuang, H. Effect of psychological Capital of Volunteers on volunteering behavior: the chained mediation role of perceived social support and volunteer motivation. Front Psychol. (2021) 12:657877. doi: 10.3389/fpsyg.2021.657877
53. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. (2007) 147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010
54. Fazio, AF. A concurrent validational study of the NCHS general well-being schedule. Vital Health Stat. (1977) 73:1–53.
55. Duan, J. Results and analysis of the general well-being schedule in Chinese college students. Chin J Clin Psychol. (1996) 4:56–7.
56. Yan, S. Study on the status and influencing factors of subjective well-being among nurses of a classified 3A hospital. Qiqihaer: Jilin University (2018).
57. Maslach, C, and Jackson, SE. The measurement of experienced burnout. J Organ Behav. (1981) 2:99–113. doi: 10.1002/job.4030020205
58. Li, C, Shi, K, Luo, Z, Li, L, and Yang, Y. An investigation on job burnout of doctor and nurse. Chin J Clin Psychol. (2003) 11:170–2.
59. Li Yongxin, LY. Developing the diagnostic Ctiterion of job burnout. J Psychol Sci. (2006) 1:148–50.
60. Maslach, C, Jackson, SE, and Leiter, MP. Maslach burnout inventory In: Evaluating stress: a book of resources. 3rd ed. Lanham, MD: Scarecrow Education (1997). 191–218.
61. Zimet, GD, Powell, SS, Farley, GK, Werkman, S, and Berkoff, KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55:610–7. doi: 10.1207/s15327752jpa5503&4_17
63. Hayes, AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Press (2013).
64. Zhou, H, and Long, L. Statistical remedies for common method biases. Adv Psychol Sci. (2004) 12:942.
65. Aggar, C, Samios, C, Penman, O, Whiteing, N, Massey, D, Rafferty, R, et al. The impact of COVID-19 pandemic-related stress experienced by Australian nurses. Int J Ment Health Nurs. (2022) 31:91–103. doi: 10.1111/inm.12938
66. Guo, Y, Hu, S, and Liang, F. The prevalence and stressors of job burnout among medical staff in Liaoning, China: a cross-section study. BMC Public Health. (2021) 21:777. doi: 10.1186/s12889-021-10535-z
67. Ren, Z, Zhang, X, Sun, Y, Li, X, He, M, Shi, H, et al. Relationships of professional identity and psychological reward satisfaction with subjective well-being among Chinese nurses. J Nurs Manag. (2021) 29:1508–16. doi: 10.1111/jonm.13276
68. Yu, J, Song, H, Shi, H, and Wang, K. Association between work-family conflict and overall well-being among Chinese nurse leaders. J Nurs Manag. (2020) 28:1498–503. doi: 10.1111/jonm.13084
69. Liu, H, Zhang, X, Chang, R, and Wang, W. A research regarding the relationship among intensive care nurses' self-esteem, job satisfaction and subjective well-being. Int J Nurs Sci. (2017) 4:291–5. doi: 10.1016/j.ijnss.2017.06.008
70. Sheng, L, Zhao, T, Liu, J, Gao, J, Peng, H, and Xin, S. Changes of medical staffs' subjective well-being in China (2004-2020): a cross-temporal meta-analysis. Appl Psychol Health Well Being. (2023) 15:425–46. doi: 10.1111/aphw.12387
71. Simons, G, and Baldwin, DS. A critical review of the definition of 'wellbeing' for doctors and their patients in a post Covid-19 era. Int J Soc Psychiatry. (2021) 67:984–91. doi: 10.1177/00207640211032259
72. Fujita, F, and Diener, E. Life satisfaction set point: stability and change. J Pers Soc Psychol. (2005) 88:158–64. doi: 10.1037/0022-3514.88.1.158
73. Gomez, V, Krings, F, Bangerter, A, and Grob, A. The influence of personality and life events on subjective well-being from a life span perspective. J Res Pers. (2009) 43:345–54. doi: 10.1016/j.jrp.2008.12.014
74. Eckleberry-Hunt, J, Kirkpatrick, H, Taku, K, Hunt, R, and Vasappa, R. Relation between Physicians' work lives and happiness. South Med J. (2016) 109:207–12. doi: 10.14423/smj.0000000000000437
75. Pacewicz, CE, Rowley, TW, and Savage, JL. Physical activity and the link among stress, burnout, and well-being in athletic trainers. J Athl Train. (2023) 58:374–80. doi: 10.4085/1062-6050-0160.22
76. Lan, X, Liang, Y, Wu, G, and Ye, H. Relationships among job burnout, generativity concern, and subjective well-being: a moderated mediation model. Front Psychol. (2021) 12:613767. doi: 10.3389/fpsyg.2021.613767
77. Hobfoll, SE. Conservation of resources. A new attempt at conceptualizing stress. Am Psychol. (1989) 44:513–24. doi: 10.1037/0003-066X.44.3.513
78. Hobfoll, SE. The influence of culture, community, and the nested-self in the stress process: advancing conservation of resources theory. Appl Psychol. (2001) 50:337–421. doi: 10.1111/1464-0597.00062
79. Salvagioni, DAJ, Melanda, FN, Mesas, AE, González, AD, Gabani, FL, and Andrade, SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One. (2017) 12:e0185781. doi: 10.1371/journal.pone.0185781
80. Yuan, L, Li, Y, Yan, H, Xiao, C, Liu, D, Liu, X, et al. Effects of work-family conflict and anxiety in the relationship between work-related stress and job burnout in Chinese female nurses: a chained mediation modeling analysis. J Affect Disord. (2023) 324:309–16. doi: 10.1016/j.jad.2022.12.112
81. Adkins, CL, and Premeaux, SF. Spending time: the impact of hours worked on work–family conflict. J Vocat Behav. (2012) 80:380–9. doi: 10.1016/j.jvb.2011.09.003
82. Chen Caifeng, ZD, and Yuhong, L. Mediating effects of social support and psychological capital on job stressors and subjective well-beinoof nurses from perspective of job demands-resources theory. Occupat Health. (2022) 38:1930–1935+1940. doi: 10.13329/j.cnki.zyyjk.2022.0446
83. Demerouti, E, Bakker, AB, Nachreiner, F, and Schaufeli, WB. The job demands-resources model of burnout. J Appl Psychol. (2001) 86:499–512. doi: 10.1037/0021-9010.86.3.499
84. Bakker, AB, Demerouti, E, and Euwema, MC. Job resources buffer the impact of job demands on burnout. J Occup Health Psychol. (2005) 10:170–80. doi: 10.1037/1076-8998.10.2.170
85. Riolli, L, and Savicki, V. Optimism and coping as moderators of the relation between work resources and burnout in information service workers. Int J Stress Manag. (2003) 10:235–52. doi: 10.1037/1072-5245.10.3.235
86. Jackson, D, Firtko, A, and Edenborough, M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. J Adv Nurs. (2007) 60:1–9. doi: 10.1111/j.1365-2648.2007.04412.x
87. Fredrickson, BL. The broaden-and-build theory of positive emotions. Philos Trans R Soc Lond Ser B Biol Sci. (2004) 359:1367–77. doi: 10.1098/rstb.2004.1512
88. Yan, D, Wen, F, Li, X, and Zhang, Y. The relationship between psychological capital and innovation behaviour in Chinese nurses. J Nurs Manag. (2020) 28:471–9. doi: 10.1111/jonm.12926
89. Wang, J, Chen, J, Zheng, L, Zeng, B, Yan, X, Xia, M, et al. Influence of psychological capital on core competency for new nurses. PLoS One. (2023) 18:e0289105. doi: 10.1371/journal.pone.0289105
90. Harolds, JA. Quality and safety in health care, part L: positive psychology and burnout. Clin Nucl Med. (2019) 44:643–5. doi: 10.1097/rlu.0000000000002439
91. Ravikumar, T. Occupational stress and psychological wellbeing during COVID 19: mediating role of positive psychological capital. Curr Psychol. (2022) 42:20157–64. doi: 10.1007/s12144-022-02861-1
92. Ruisoto, P, Ramírez, MR, García, PA, Paladines-Costa, B, Vaca, SL, and Clemente-Suárez, VJ. Social support mediates the effect of burnout on health in health care professionals. Front Psychol. (2020) 11:623587. doi: 10.3389/fpsyg.2020.623587
93. Frögéli, E, Rudman, A, and Gustavsson, P. The relationship between task mastery, role clarity, social acceptance, and stress: an intensive longitudinal study with a sample of newly registered nurses. Int J Nurs Stud. (2019) 91:60–9. doi: 10.1016/j.ijnurstu.2018.10.007
94. Tomyn, AJ, and Cummins, RA. Subjective wellbeing and homeostatically protected mood: theory validation with adolescents. J Happiness Stud. (2011) 12:897–914. doi: 10.1007/s10902-010-9235-5
95. Huang, Y, Lin, X, Yang, J, Bai, H, Tang, P, and Yuan, GF. Association between psychological capital and depressive symptoms during COVID-19: the mediating role of perceived social support and the moderating effect of employment pressure. Front Public Health. (2023) 11:1036172. doi: 10.3389/fpubh.2023.1036172
96. Xu, H, Liu, X, and Zeng, P. The mediating role of social support in the relationship between psychological capital and depression among Chinese emergency physicians. Psychol Res Behav Manag. (2022) 15:977–90. doi: 10.2147/prbm.S360611
97. McGonagle, AK, Schwab, L, Yahanda, N, Duskey, H, Gertz, N, Prior, L, et al. Coaching for primary care physician well-being: a randomized trial and follow-up analysis. J Occup Health Psychol. (2020) 25:297–314. doi: 10.1037/ocp0000180
98. Smoktunowicz, E, Lesnierowska, M, Carlbring, P, Andersson, G, and Cieslak, R. Resource-based internet intervention (med-stress) to improve well-being among medical professionals: randomized controlled trial. J Med Internet Res. (2021) 23:e21445. doi: 10.2196/21445
99. Xie, Z, Wang, A, and Chen, B. Nurse burnout and its association with occupational stress in a cross-sectional study in Shanghai. J Adv Nurs. (2011) 67:1537–46. doi: 10.1111/j.1365-2648.2010.05576.x
100. Wen, J, Cheng, Y, Hu, X, Yuan, P, Hao, T, and Shi, Y. Workload, burnout, and medical mistakes among physicians in China: a cross-sectional study. Biosci Trends. (2016) 10:27–33. doi: 10.5582/bst.2015.01175
Keywords: medical staff, burnout, subjective wellbeing, psychological capital, perceived social support
Citation: Fan J, Chang Y, Li L, Jiang N, Qu Z, Zhang J, Li M, Liang B and Qu D (2024) The relationship between medical staff burnout and subjective wellbeing: the chain mediating role of psychological capital and perceived social support. Front. Public Health. 12:1408006. doi: 10.3389/fpubh.2024.1408006
Edited by:
Shen Liu, Anhui Agricultural University, ChinaReviewed by:
Nicola Mucci, University of Florence, ItalyKathleen Clegg, University Hospitals Cleveland Medical Center, United States
Copyright © 2024 Fan, Chang, Li, Jiang, Qu, Zhang, Li, Liang and Qu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bing Liang, liangbing716@jlu.edu.cn; Danhua Qu, qudh@jlu.edu.cn
†These authors have contributed equally to this work
 Jia Fan
Jia Fan