- 1Department of Gastroenterology, China-Japan Friendship Hospital, Beijing, China
- 2Research Center for Physical Fitness at High Altitude, Chengguan District Culture and Tourism Bureau, Lhasa Tibet, China
- 3Department of Quality, Health, Safety and Environmental Protection, China National Petroleum Corporation, Beijing, China
- 4Evaluation Research Center, Renmin University of China, Beijing, China
- 5Endoscopy Center, Liaoyang Gastroenterological Hospital, Liaoyang, China
- 6Department of Rehabilitation Medicine, China-Japan Friendship Hospital, Beijing, China
- 7Center for Disease Control and Prevention, Shuanghu County Health Commission, Nagqu Tibet, China
- 8Nursing Department, China-Japan Friendship Hospital, Beijing, China
Background: Our study was designed to determine the incidence and risk factors of severe acute high-altitude illness (AHAI) in healthy adults first entering the northern Tibetan Plateau of over 5,000 m.
Methods: In our prospective observational study, we enrolled 500 people who were scheduled for fast ascension to the northern Tibetan Plateau. The primary outcome variable was severe AHAI, defined as the presence of serious symptoms that could not be ameliorated by general treatment and required evacuation to lower altitudes. According to the inclusion and exclusion criteria, a cohort of 383 healthy people was included in the statistical analysis. We calculated the incidence of severe AHAI, identified the risk factors, and the differences in the most severe symptoms experienced.
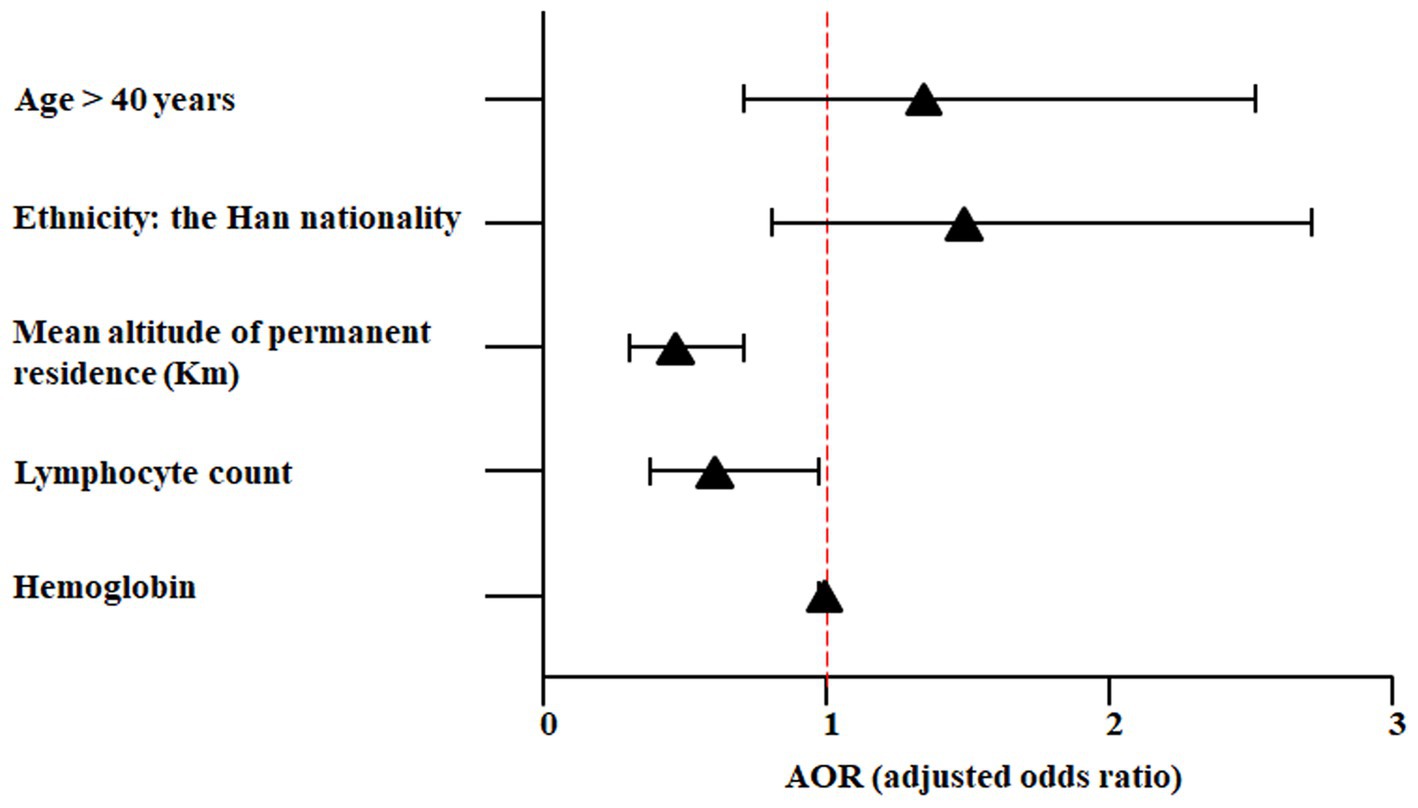
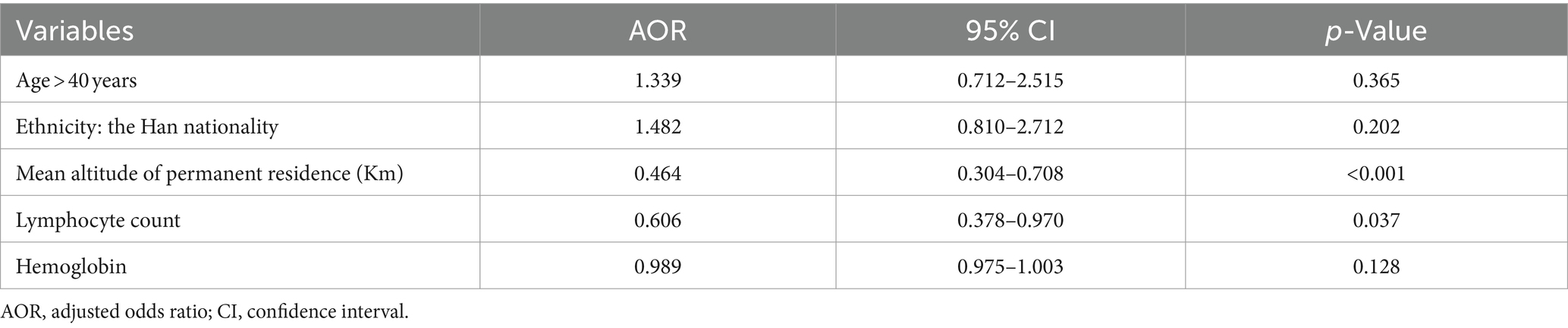
Results: Sixty-eight people were diagnosed with severe AHAI, and the incidence was 17.8%. Compared to individuals without severe AHAI, those with severe AHAI were more likely to be over the age of 40 years, of Han Chinese nationality, and living at an altitude of <1,500 m. They were less likely to belong to the Yi nationality, had a lower altitude of permanent residence, and exhibited decreased levels of lymphocyte count and hemoglobin concentration. Multivariable logistic regression showed that the mean altitude of permanent residence [per kilometer, adjusted odds ratio (AOR) = 0.464; 95% confidence interval (CI), 0.304–0.708; p < 0.001] and lymphocyte count (AOR = 0.606; 95% CI, 0.378–0.970; p = 0.037) were the independent risk factors. Headache and dyspnea ranked in the top two of the most severe symptoms for people with severe AHAI.
Conclusion: Living at lower altitudes and having a decreased lymphocyte level were the risk factors of severe AHAI in healthy adults first entering the plateau of over 5,000 m.
1 Introduction
The northern Tibetan Plateau, which is also named the “Qiangtang Plateau,” is the highest altitude region of the Qinghai-Tibetan Plateau, covering an area of approximately 0.6 million square kilometers with an average elevation of over 4,500 m and an annual mean temperature below 0°C (1–3). The climate characteristics of this plateau were severe hypoxia, extreme cold, strong ultraviolet radiation exposure, and extremely low absolute humidity (4–6). Permanently living in or temporarily traveling to high altitudes may induce a series of physiological and pathological changes in humans, and the main affecting factor is hypobaric hypoxia (4, 7). When people enter an altitude of over 3,000 m, they usually begin to develop symptoms of hypoxia, for example, headache, dyspnea, insomnia, fatigue, abdominal distension, and loss of appetite (8, 9).
AHAI comprises acute mountain sickness (AMS), high-altitude cerebral edema, and pulmonary edema. AMS is the most common type of AHAI, affecting more than 25% of individuals after exposure to altitudes above 3,500 m and over 50% of individuals at altitudes of 6,000 m (10, 11). Although AMS is usually self-limited for most people and the symptoms can be relieved by rest and oxygen inhalation, approximately 1% of them can progress to severe ailments such as pulmonary edema and cerebral edema (12, 13). Extensive research has been conducted on the pathophysiological processes, but the precise pathogenesis of AHAI has not been explained clearly (14–17). Hypobaric hypoxia has been taken as the main contributing factor, leading to hyperventilation, fluid retention, inflammation, increased pulmonary artery pressure, and raised intracranial pressure (16, 17).
Recently, there has been a growing trend of people ascending to high altitudes worldwide for tourism, work, sports, or military activities (11, 18). Therefore, to reduce the incidence rate of AHAI, early recognition of risk factors and identification of susceptible individuals at low altitudes are especially important. Some risk factors of AHAI have been identified, for example, the altitude reached, fast ascent, older age, obesity, a history of AMS, and lack of pre-acclimatization (13, 18, 19). Several pieces of literature have found an association between lymphocyte level and high altitude (20–23). One in vitro study used isolated peripheral blood lymphocytes as biosensors to test the effect of hypobaric hypoxia and suggested that peripheral blood lymphocytes could be used for monitoring adaptive responses to environmental challenges (20). Another study showed that high altitude (HA) hypobaric hypoxia exacerbates the severity of ulcerative colitis in a mouse model by upregulating CD4+ Th1 and Th 17 lymphocytes (23). In this study, a cohort of people was scheduled for a rapid ascent to the northern Tibetan Plateau, reaching altitudes of over 5,000 m. Our study was designed to determine the incidence and risk factors of severe AHAI in these healthy adults first entering this plateau.
2 Materials and methods
2.1 Study design and screening flow
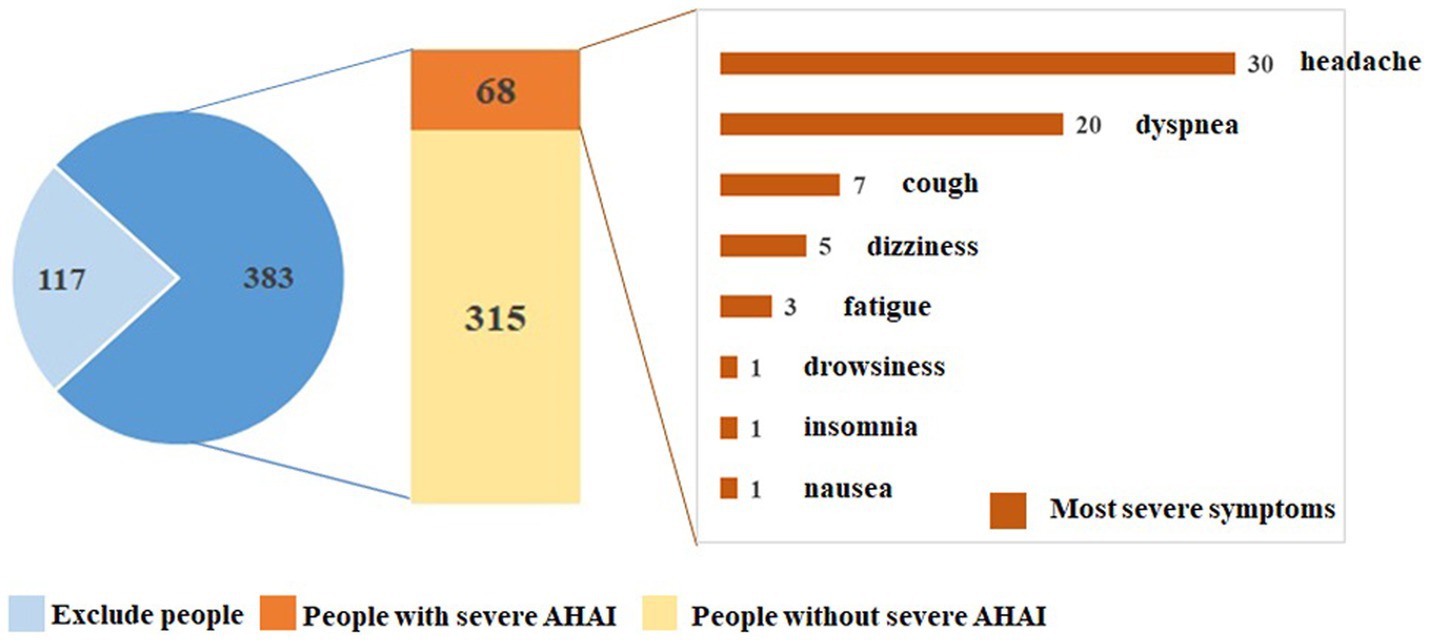
Shuanghu County of the Tibet Autonomous Region is situated at the northern Tibetan Plateau between north latitude 30–36° and east longitude 83–90°, with an average elevation of over 5,000 m. A cohort of 500 people was scheduled for the assignment to Shuanghu County in 3–5 days. The screening flow is shown in Figure 1. They would be divided into two groups based on the presence or absence of severe AHAI. Our prospective observational study was designed to determine the incidence and risk factors of severe AHAI in healthy adults first entering the plateau of over 5,000 m. Our study was conducted in accordance with the Declaration of Helsinki and approved by the Chengguan District Culture and Tourism Bureau, Lhasa, Tibet. Written informed consent was obtained from all the participants.
2.2 Study population and physical examination
Five hundred people were enrolled, and finally, a cohort of 383 healthy people was included in the statistical analysis (Figure 1). The inclusion criteria included: (1) age between 18 and 59 years old; (2) never having visited this plateau or entered high-altitude areas of over 5,000 m; (3) not having stayed at high altitudes of over 3,000 m in the past 2 years; and (4) having obtained written informed consent, sufficient data for statistical analysis, and completing follow-up. The exclusion criteria included: (1) physical examination findings that were independently assessed by two team doctors and considered to be unsuitable for entering the plateau of over 5,000 m and (2) a history of serious medical conditions based on their self-reported records. Their physical examinations included demographic data, blood parameters, biochemical parameters, electrocardiogram (ECG), chest computed tomography (CT) scan, echocardiography, lung function test, and skull magnetic resonance imaging (MRI) examination. The examinations were conducted at hospitals near the participants’ permanent residences, and the resulting data were treated as baseline characteristics. The normal reference values of routine blood and liver function tests are listed in Supplementary Table S1.
2.3 Definition of severe AHAI and study parameters
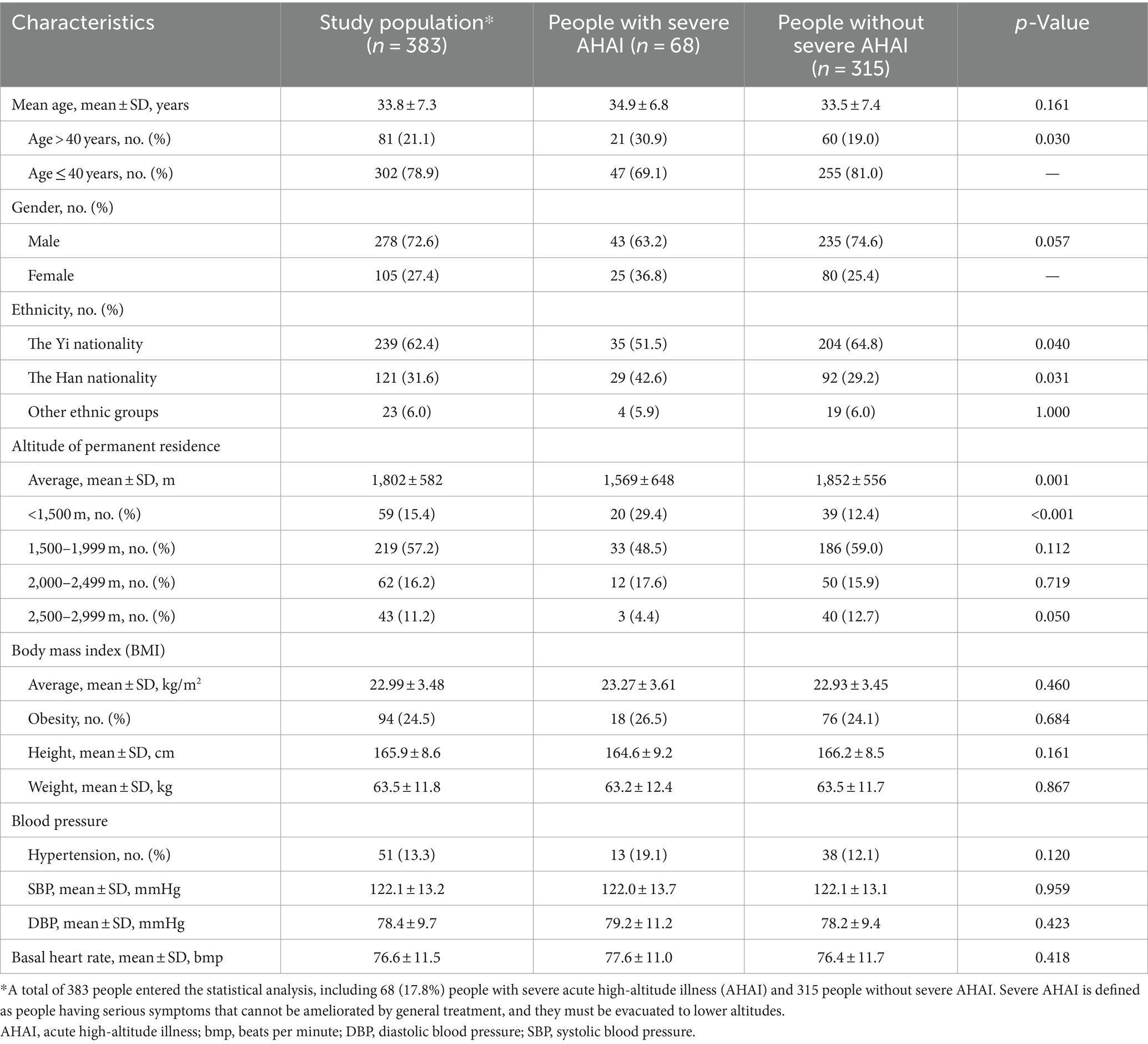
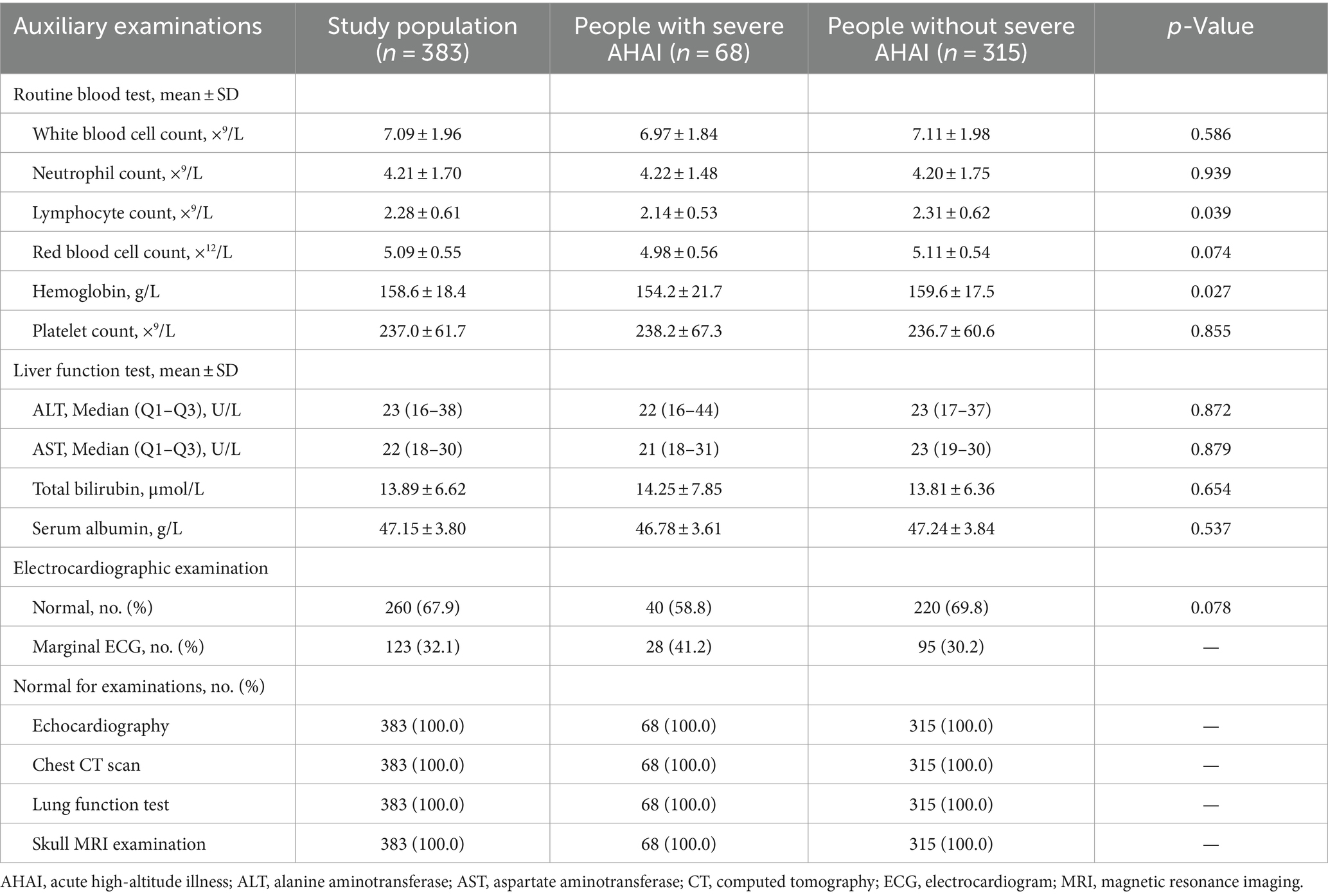
Instead of the Lake Louise AMS score (LLS), we gave close attention to the primary outcome. Severe AHAI is defined as people having serious symptoms that cannot be ameliorated by general treatment and required evacuation to lower altitudes. Study parameters are outlined in Tables 1, 2. For age, the mean ± SD and percentage of age over 40 were described. Given that 360 (94.0%) participants were of Han Chinese or Yi nationality, ethnicities were divided into three groups: Yi, Han, and other. The altitudes of permanent residence were split into four groups: <1,500 m, 1,500–1,999 m, 2,000–2,499 m, and 2,500–2,999 m. Routine blood and liver function tests included 10 indices: white blood cell count, lymphocyte count, neutrophil count, hemoglobin, red blood cell count, platelet count, ALT, AST, total bilirubin, and serum albumin.
2.4 Treatment of severe AHAI and follow-up
Our study participants were accompanied by two team doctors who could help to treat the possible AHAI. After the people entered the northern Tibetan Plateau, they were asked to monitor their heart rates, blood pressure, fingertip arterial oxygen saturation (SaO2), and the top three cardinal symptoms. During the first week, monitoring was conducted three times a day, with results reported to the team doctors. If participants exhibited serious symptoms, the doctors could provide appropriate treatments, such as oxygen inhalation, sleep medications, and painkilling drugs. Those did not experience sufficient relief after these treatments were rushed to Shuanghu County Hospital. After diagnosis and general treatment, individuals with severe AHAI were evacuated to lower altitudes and categorized as the case group.
The follow-up lasted for at least 4 weeks. Individuals with severe AHAI were followed up by investigators at least once a week and for a minimum of 1 month via phone. During the follow-up period, cardinal symptoms, the progression of AHAI, recovery, and prognosis were recorded. For individuals without severe AHAI, the contents of monitoring remained unchanged, and the frequency of monitoring decreased gradually. The frequency was twice a day in the second week and once a day in the next 2 weeks.
2.5 Statistical analysis
SPSS 23.0 for Windows (Chicago, IL, USA) was used for the statistical analysis. Based on the variable types, data were described as the mean ± standard deviation, median (interquartile range), or number and proportion. To compare the baseline characteristics and results of auxiliary examinations, Student’s t-test, the Mann–Whitney U-test, and the chi-square test were used for continuous variables with normal distribution, continuous variables with skewed distribution, and categorical variables, respectively. Univariate and multivariable analyses were conducted using unconditional logistic regression to determine risk factors of severe AHAI. Stepwise analysis (backward: Wald; entry: 0.05; removal: 0.10) was adopted. The results were expressed as odds ratios and 95% confidence intervals. The chi-square test was used to compare the differences in the most severe symptoms between the two groups.
3 Results
3.1 People’s baseline characteristics and auxiliary examination results
Figure 1 shows the screening flow and 500 people were enrolled. Based on the inclusion and exclusion criteria, a cohort of 383 healthy people was included in the statistical analysis. Their baseline characteristics and auxiliary examination results are listed in Tables 1, 2. The mean age was 33.8 ± 7.3 years and 81 (21.1%) participants were over 40 years. Two hundred and seventy-eight (72.6%) participants were male and 360 (94.0%) participants were Han Chinese or Yi nationality. For the altitude of permanent residence, the mean altitude was 1,802 ± 582 m, with 219 participants living at altitudes of 1,500–1,999 m. Routine blood tests revealed average lymphocyte counts of 2.28 ± 0.61 × 9/L and hemoglobin levels of 158.6 ± 18.4 g/L. All participants had normal results from echocardiography, chest CT scan, lung function, and skull MRI examinations.
3.2 Incidence of participants diagnosed with severe AHAI
Sixty-eight participants diagnosed with severe AHAI were evacuated to the lower altitudes, and the incidence of severe AHAI was 17.8% (Figure 1). Among these 68 participants, the mean age was 34.9 ± 6.8 years, and 25 (36.8%) participants were female. For ethnicity, 35 (51.5%) participants were of the Yi nationality and 29 (42.6%) were of the Han Chinese nationality. Twenty (29.4%) participants lived at altitudes of less than 1,500 m. The results of routine blood and liver function tests are shown in Table 2. Electrocardiographic examination showed that 28 (41.2%) participants were diagnosed with marginal ECG.
3.3 Comparative analysis between participants with and without severe AHAI
Using Student’s t-test, the chi-square test, and the Mann–Whitney U-test, a comparative analysis of baseline characteristics and auxiliary examination results between participants with and without severe AHAI are shown in Tables 1, 2. Compared to those without severe AHAI, those with severe AHAI had higher percentages of age over 40 (30.9% vs. 19.0%, p = 0.030), Han Chinese nationality (42.6% vs. 29.2%, p = 0.031), and living at an altitude of <1,500 m (29.4% vs. 12.4%, p < 0.001), a lower percentage of Yi nationality (51.5% vs. 64.8%, p = 0.040), a lower altitude of permanent residence (1,569 ± 648 m vs. 1,852 ± 556 m, p = 0.001), and decreased levels of lymphocyte count (2.14 ± 0.53 × 9/L vs. 2.31 ± 0.62 × 9/L, p = 0.039) and hemoglobin concentration (154.2 ± 21.7 g/L vs. 159.6 ± 17.5 g/L, p = 0.027).
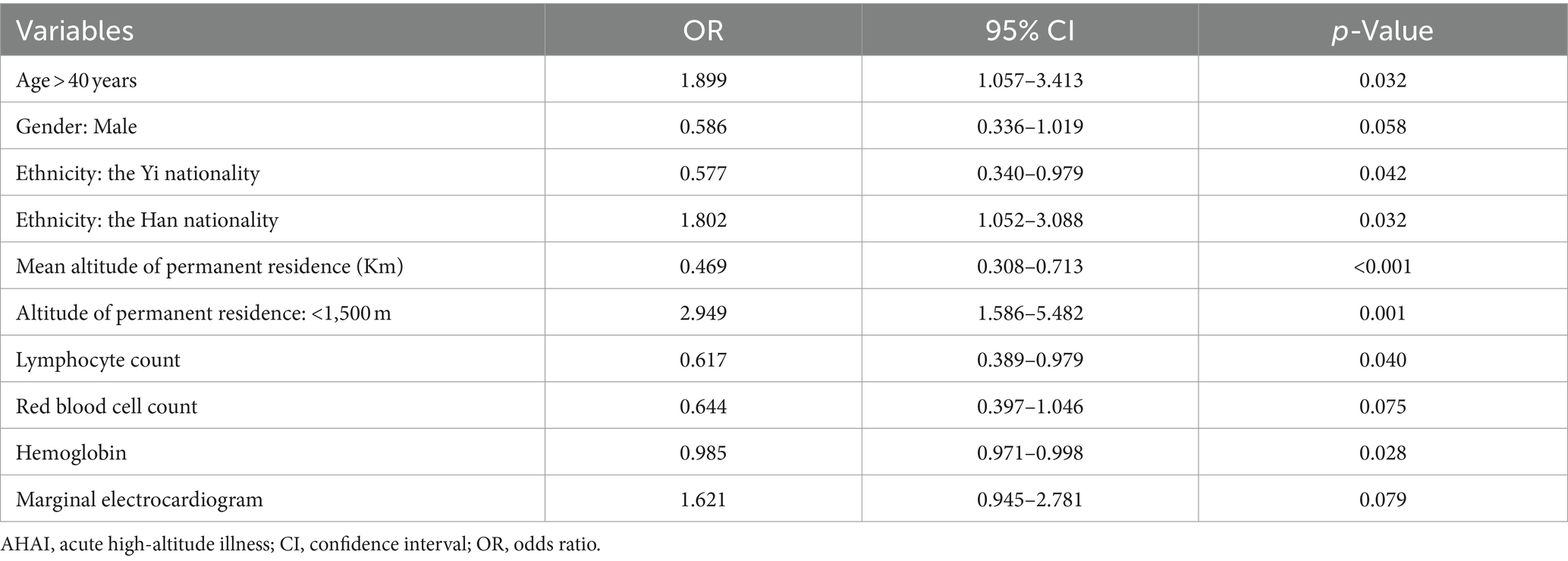
3.4 Risk factors of severe AHAI by univariate analysis
Logistic regression analysis, including both univariate and multivariable analyses, was used to determine risk factors. Based on the results of the comparative analysis (Tables 1, 2), 10 variables were considered potential predicting factors. The univariate analysis (Table 3) showed that seven variables had significant differences, including age > 40 years (OR = 1.899; 95% CI, 1.057–3.413; p = 0.032), the Yi nationality (OR = 0.577; 95% CI, 0.340–0.979; p = 0.042), the Han nationality (OR = 1.802; 95% CI, 1.052–3.088; p = 0.032), the mean altitude of permanent residence (OR = 0.469; 95% CI, 0.308–0.713; p < 0.001), living at the altitude of <1,500 m (OR = 2.949; 95% CI, 1.586–5.482; p = 0.001), lymphocyte count (OR = 0.617; 95% CI, 0.389–0.979; p = 0.040), and hemoglobin concentration (OR = 0.985; 95% CI, 0.971–0.998; p = 0.028).
3.5 Multivariable analysis for risk factors of severe AHAI
Since the Yi nationality and living at an altitude of <1,500 m were repetitive variables, they were excluded from the final analysis. Five variables were included in the multivariable analysis: age > 40 years, Han nationality, mean altitude of permanent residence (in kilometers), lymphocyte count, and hemoglobin concentration (Figure 2 and Table 4). The results showed that only two variables had statistical differences, including the mean altitude of permanent residence (per kilometer, AOR = 0.464; 95% CI, 0.304–0.708; p < 0.001) and lymphocyte count (AOR = 0.606; 95% CI, 0.378–0.970; p = 0.037), indicating that living at lower altitudes and having a decreased lymphocyte level were the risk factors of severe AHAI in healthy adults first entering the plateau of over 5,000 m. A comparative analysis of routine blood and liver function tests at different altitude levels is shown in Supplementary Table S2.
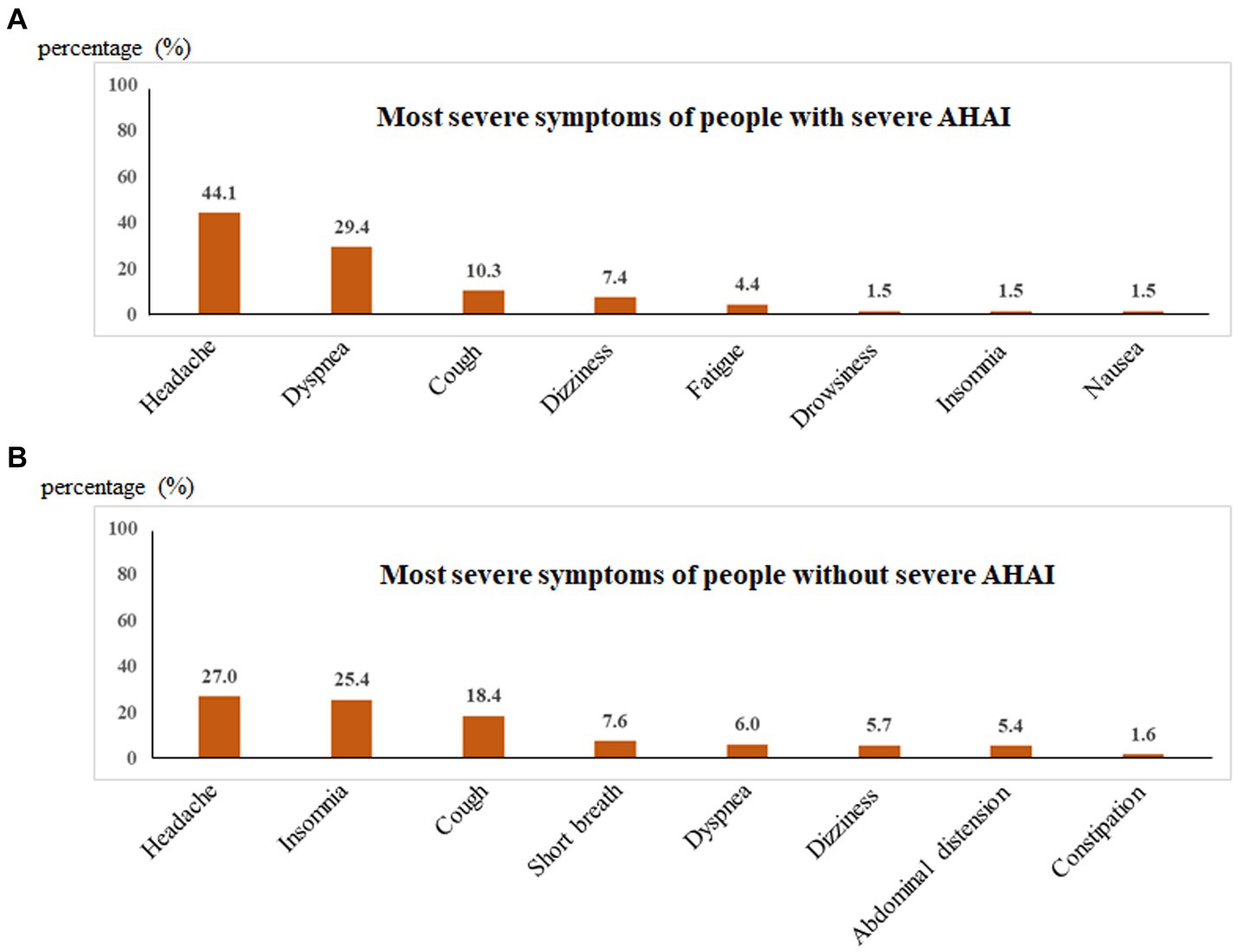
3.6 Most severe symptoms between participants with and without severe AHAI
The most severe symptoms were recorded, including headache, dyspnea, dizziness, cough, fatigue, drowsiness, insomnia, nausea, abdominal distension, constipation, shortness of breath, anorexia, and toothache. For participants with severe AHAI, the top five most severe symptoms were headache (44.1%), dyspnea (29.4%), cough (10.3%), dizziness (7.4%), and fatigue (4.4%), whereas for the participants without severe AHAI, they were headache (27.0%), insomnia (25.4%), cough (18.4%), shortness of breath (7.6%), and dyspnea (6.0%) (Table 5 and Figure 3). Headache and dyspnea ranked in the top two for participants with severe AHAI and the percentages were higher than those without severe AHAI. The chi-square test showed that significant differences were found in headache (p = 0.005), dyspnea (p < 0.001), and insomnia (p < 0.001) (Table 5).
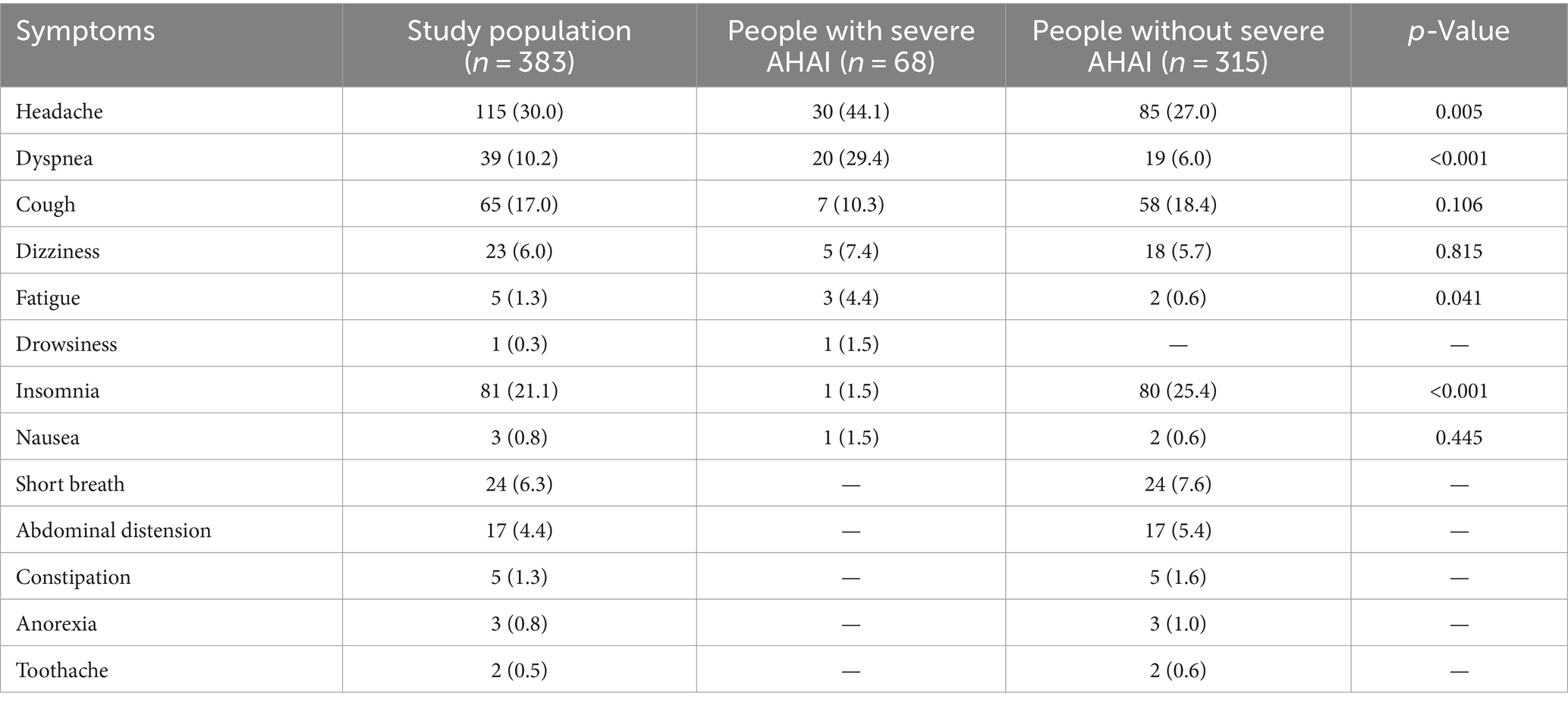
Table 5. Comparative analysis of the most severe symptoms between people with and without severe AHAI.
4 Discussion
With the increasing number of individuals ascending to high altitudes for work, tourism, sports, or military activities, people diagnosed with AHAI are gradually increasing (11, 18). If the susceptible individuals who had the likelihood of developing AHAI could be identified prior to ascending to high altitudes, they could receive intensive monitoring, and preventative treatment, even avoid rapid ascents or entering high altitudes. Our study was designed to determine the incidence and risk factors of severe AHAI in healthy adults first entering the northern Tibetan Plateau. We showed that living at lower altitudes and having a decreased lymphocyte count were independent risk factors.
Shuanghu County is situated in the northern Tibetan Plateau at an average altitude of over 5,000 m. Most humans may develop symptoms of hypoxia at this altitude (10, 11) and usually avoid rapid ascents to this elevation. In this study, 500 people were scheduled for the assignment, fast ascending to this plateau in 3–5 days. This assignment gave us the chance to conduct this prospective study, and the major contribution of our study was that we obtained the incidence and risk factors of severe AHAI in healthy adults upon rapid ascent to over 5,000 m. The identified risk factors can be used to construct a prediction model to identify susceptible individuals, allowing for targeted monitoring and preventative treatment before ascending to higher altitudes, for work, tourism, sports, or military activities. The authors wish that future studies could help to advance these goals.
Currently, the diagnosis of AMS can be assessed using rating scales, such as the LLS, the AMS-Cerebral (AMS-C) score, the clinical functional score (CFS), the visual analog scale (VAS) score, the Chinese AMS score (CAS), and the Hackett clinical score (10, 13, 24). The LLS has been widely used in clinical and research practice and is regarded as a gold standard in the diagnosis of AMS (10). One study included 143 young Chinese men and found that the prevalence of AMS was 54% after exposure at 3,800 m (13). Another study showed that the prevalence of AMS was 14.8 and 10.1% at 3,650 m and 21.9 and 15% at 4,559 m, assessed using the LLS and AMS-C scores, respectively (24). The prevalence of AMS varied significantly across different populations and rating scales, primarily due to the fact that these rating scales were established on the grounds of subjective self-evaluation. In our study, we used an objective outcome variable, defining severe AHAI as serious symptoms that cannot be ameliorated by general treatment and require evacuation to lower altitudes. The incidence of severe AHAI was 17.8%.
Some risk factors of AHAI have been identified, for example, older age, fast ascent, obesity, the altitude reached, lack of pre-acclimatization, and history of AMS (13, 18, 19). One study was designed to explore the relationship between anxiety, sleep quality, and AMS and found that the Zung Self-Rating Anxiety Scale (SAS) score and Athens Insomnia Scale (AIS) score were risk factors for AMS (13). However, the risk factors of AHAI may be different in different populations (18, 25). Tang et al. found that older age is an independent risk factor for AMS, whereas Small et al. showed that older age was not associated with AMS. Using univariate analysis, our study showed that older age, Han or Yi nationality, the altitude of permanent residence, lymphocyte count, and hemoglobin concentration were the potential risk factors of severe AHAI.
Having a decreased level of lymphocyte count was the first independent risk factor for severe AHAI identified in our study. Past clinical research has found that lymphocyte count, especially the neutrophil-to-lymphocyte ratio (NLR), is associated with high altitude and AHAI (26–28). He et al. found that the incidence of myocardial injury was increased at high altitudes and NLR was an independent risk factor for myocardial injury (26). Nguyen et al. described that exposure to high altitudes induced increased granulocyte-to-lymphocyte ratio and monocyte-to-lymphocyte ratio (27). Vélez-Páez et al. included 340 patients in Quito-Ecuador (2,850 m) and showed that NLR was an independent predictor of mortality in critically ill obese patients (28).
Several basic studies have revealed the potential underlying mechanisms between lymphocytes and high altitude (20–23). One in vitro study used isolated peripheral blood lymphocytes to test the effect of HA hypobaric hypoxia and revealed that 3 weeks of exposure to a high altitude of 5,000 m could increase intracellular Ca(2+) concentration and intracellular levels of reactive oxygen species (ROS) and decrease mitochondrial membrane potential in lymphocytes (20). Another study discovered that T helper 2 (Th2) lymphocytes could promote erythropoiesis under the hypoxic conditions of HA (21). The authors further demonstrated that Th2 lymphocytes from hypoxic mice could promote the erythroid differentiation of hematopoietic stem/progenitor cells and the growth of erythroblasts via elevated secretion of interleukin-9 and activin A (21).
Considering that a decreased level of lymphocyte count is associated with severe AHAI in our study, we tried to use the ROC curve and Youden index to determine the range or level of lymphocytes that are considered indicative of severe AHAI. Unfortunately, no optimal cutoff point was obtained, and we wish that it could be resolved by in-depth research in the future. Based on current research, combined with the mean and median of lymphocytes, the value of 2.20 × 9/L is recommended as the temporary threshold, indicating that people with lymphocytes <2.20 × 9/L have an increased risk of severe AHAI. Identifying susceptible individuals based on lymphocyte count may still be challenging. More in-depth studies are required to resolve this issue.
Living at lower altitudes was the second independent risk factor of severe AHAI in our study. This result was supported by some previous studies, which suggested that residence at moderate altitude could reduce the risk of suffering AHAI during rapid ascent to higher altitude (29, 30). Some limitations in our study should be acknowledged. The first limitation was that our population was from one single center. The potential impact on generalizability should be considered, and the results should be validated with more people. The second was that the research data were obtained mainly from physical examination data and some new biomarkers were not included. The authors wish that easily available variables can be identified and used widely for risk prediction.
In conclusion, our study showed that living at lower altitudes and having a decreased level of lymphocyte count were the risk factors for severe AHAI in healthy adults first entering this Tibetan Plateau of over 5,000 m. Early identification and management of the risk factors for severe AHAI are especially important in clinical practice and public health interventions. Future research should focus on validating findings in diverse populations and exploring additional biomarkers for predicting AHAI risk.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Chengguan District Culture and Tourism Bureau (No. 20201216cgwlsy(05), date of approval: 21 December 2020). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CG: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. G-DQ: Data curation, Supervision, Writing – review & editing. DW: Methodology, Supervision, Writing – review & editing. Z-HZ: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. Z-XL: Investigation, Methodology, Writing – review & editing. R-DG: Formal analysis, Investigation, Writing – review & editing. ZY: Data curation, Investigation, Writing – review & editing. L-EY: Formal analysis, Investigation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all the participants for their committed participation.
Conflict of interest
G-DQ was employed by China National Petroleum Corporation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1400236/full#supplementary-material
References
1. Yu, J, Hou, G, Shi, P, Zong, N, and Peng, J. Nitrogen rather than phosphorous addition alters the asymmetric responses of primary productivity to precipitation variability across a precipitation gradient on the northern Tibetan Plateau. Sci Total Environ. (2024) 907:167856. doi: 10.1016/j.scitotenv.2023.167856
2. Liu, SW, Zhai, XX, Liu, D, Liu, YY, Sui, LY, Luo, KK, et al. Bioprospecting of actinobacterial diversity and antibacterial secondary metabolites from the sediments of four saline lakes on the northern Tibetan Plateau. Microorganisms. (2023) 11:2475. doi: 10.3390/microorganisms11102475
3. Zhao, Y, Liu, S, Dong, Y, Wang, F, Liu, H, and Liu, Y. Effect of fencing on regional ecological networks in the northern Tibetan Plateau. Front Plant Sci. (2023) 14:1051881. doi: 10.3389/fpls.2023.1051881
4. Gao, C, Ciren, J, Wang, D, Zhang, Z, Ge, R, and Yan, L. Assessment of psychological and social fitness in healthy adults permanently living at very high altitude. Int J Environ Res Public Health. (2023) 20:2013. doi: 10.3390/ijerph20032013
5. Zhang, X, and Zhang, J. The human brain in a high altitude natural environment: a review. Front Hum Neurosci. (2022) 16:915995. doi: 10.3389/fnhum.2022.915995
6. Sharma, V, Varshney, R, and Sethy, NK. Human adaptation to high altitude: a review of convergence between genomic and proteomic signatures. Hum Genomics. (2022) 16:21. doi: 10.1186/s40246-022-00395-y
7. Li, Y, and Wang, Y. Effects of long-term exposure to high altitude hypoxia on cognitive function and its mechanism: a narrative review. Brain Sci. (2022) 12:808. doi: 10.3390/brainsci12060808
8. Chen, P, Liu, Y, Liu, W, Wang, Y, Liu, Z, and Rong, M. Impact of high-altitude hypoxia on bone defect repair: a review of molecular mechanisms and therapeutic implications. Front Med. (2022) 9:842800. doi: 10.3389/fmed.2022.842800
9. Georges, T, Menu, P, Le Blanc, C, Ferreol, S, Dauty, M, and Fouasson-Chailloux, A. Contribution of hypoxic exercise testing to predict high-altitude pathology: a systematic review. Life. (2022) 12:377. doi: 10.3390/life12030377
10. Meier, D, Collet, TH, Locatelli, I, Cornuz, J, Kayser, B, Simel, DL, et al. Does this patient have acute mountain sickness? The rational clinical examination systematic review. JAMA. (2017) 318:1810–9. doi: 10.1001/jama.2017.16192
11. Guo, H, Wang, Q, Li, T, Chen, J, Zhang, C, Xu, Y, et al. Potential plasma biomarkers at low altitude for prediction of acute mountain sickness. Front Immunol. (2023) 14:1237465. doi: 10.3389/fimmu.2023.1237465
12. Zhao, Y, Zou, H, Fan, W, Liu, Y, Chen, X, Huang, Y, et al. Patterns of structural changes in the fundus measured by optical coherence tomography angiography as potential markers of acute mountain sickness. Transl Vis Sci Technol. (2023) 12:15. doi: 10.1167/tvst.12.12.15
13. Tang, X, Li, X, Xin, Q, Wang, Q, Li, S, and Yang, Y. Anxiety as a risk factor for acute mountain sickness among young Chinese men after exposure at 3800 m: a cross-sectional study. Neuropsychiatr Dis Treat. (2023) 19:2573–83. doi: 10.2147/NDT.S436438
14. Luks, AM, Swenson, ER, and Bärtsch, P. Acute high-altitude sickness. Eur Respir Rev. (2017) 26:160096. doi: 10.1183/16000617.0096-2016
15. Luks, AM, and Hackett, PH. Medical conditions and high-altitude travel. N Engl J Med. (2022) 386:364–73. doi: 10.1056/NEJMra2104829
16. Liu, M, Jiao, X, Li, R, Li, J, Wang, L, Wang, L, et al. Effects of acetazolamide combined with remote ischemic preconditioning on risk of acute mountain sickness: a randomized clinical trial. BMC Med. (2024) 22:4. doi: 10.1186/s12916-023-03209-7
17. Schober, A, Chinn, G, Eichbaum, Y, Dudley, M, and Sall, JWUniversity of California San Francisco AR36 Working Group. A randomized phase 2 study to evaluate efficacy and safety of AR36 for prevention of acute mountain sickness. Wilderness Environ Med. (2023) 34:498–508. doi: 10.1016/j.wem.2023.09.002
18. Tang, XG, Zhang, JH, Qin, J, Gao, XB, Li, QN, Yu, J, et al. Age as a risk factor for acute mountain sickness upon rapid ascent to 3,700 m among young adult Chinese men. Clin Interv Aging. (2014) 9:1287–94. doi: 10.2147/CIA.S67052
19. Yang, B, Sun, ZJ, Cao, F, Zhao, H, Li, CW, and Zhang, J. Obesity is a risk factor for acute mountain sickness: a prospective study in Tibet railway construction workers on Tibetan Plateau. Eur Rev Med Pharmacol Sci. (2015) 19:119–22.
20. Mariggiò, MA, Falone, S, Morabito, C, Guarnieri, S, Mirabilio, A, Pilla, R, et al. Peripheral blood lymphocytes: a model for monitoring physiological adaptation to high altitude. High Alt Med Biol. (2010) 11:333–42. doi: 10.1089/ham.2009.1097
21. Li, P, Zheng, SJ, Jiang, CH, Zhou, SM, Tian, HJ, Zhang, G, et al. Th2 lymphocytes migrating to the bone marrow under high-altitude hypoxia promote erythropoiesis via activin a and interleukin-9. Exp Hematol. (2014) 42:804–15. doi: 10.1016/j.exphem.2014.04.007
22. Karagiannidis, C, Hense, G, Rueckert, B, Mantel, PY, Ichters, B, Blaser, K, et al. High-altitude climate therapy reduces local airway inflammation and modulates lymphocyte activation. Scand J Immunol. (2006) 63:304–10. doi: 10.1111/j.1365-3083.2006.01739.x
23. Gamah, M, Alahdal, M, Zhang, Y, Zhou, Y, Ji, Q, Yuan, Z, et al. High-altitude hypoxia exacerbates dextran sulfate sodium (DSS)-induced colitis by upregulating Th1 and Th17 lymphocytes. Bioengineered. (2021) 12:7985–94. doi: 10.1080/21655979.2021.1975017
24. Berger, MM, Hüsing, A, Niessen, N, Schiefer, LM, Schneider, M, Bärtsch, P, et al. Prevalence and knowledge about acute mountain sickness in the Western Alps. PLoS One. (2023) 18:e0291060. doi: 10.1371/journal.pone.0291060
25. Small, E, Phillips, C, Marvel, J, and Lipman, G. Older age as a predictive risk factor for acute mountain sickness. Am J Med. (2022) 135:386–392.e1. doi: 10.1016/j.amjmed.2021.10.003
26. He, S, He, S, Yang, Y, Li, B, Gao, L, Xie, Q, et al. Correlation between neutrophil to lymphocyte ratio and myocardial injury in population exposed to high altitude. Front Cardiovasc Med. (2021) 8:738817. doi: 10.3389/fcvm.2021.738817
27. Nguyen, KT, Gates, CA, Hassell, JE Jr, Foxx, CL, Salazar, SN, Luthens, AK, et al. Evaluation of the effects of altitude on biological signatures of inflammation and anxiety- and depressive-like behavioral responses. Prog Neuro-Psychopharmacol Biol Psychiatry. (2021) 111:110331. doi: 10.1016/j.pnpbp.2021.110331
28. Vélez-Páez, JL, Aguayo-Moscoso, SX, Castro-Bustamante, C, Montalvo- Villagómez, M, Jara-González, F, Baldeón-Rojas, L, et al. Biomarkers as predictors of mortality in critically ill obese patients with COVID-19 at high altitude. BMC Pulm Med. (2023) 23:112. doi: 10.1186/s12890-023-02399-3
29. Bernardi, E, Pomidori, L, Cavallari, D, Mandolesi, G, and Cogo, A. Residence at moderate versus low altitude is effective at maintaining higher oxygen saturation during exercise and reducing acute mountain sickness following fast ascent to 4559 m. Wilderness Environ Med. (2017) 28:122–6. doi: 10.1016/j.wem.2017.02.004
Keywords: acute high-altitude illness, risk factor, northern Tibetan Plateau, healthy adults, incidence
Citation: Gao C, Qi G-D, Wang D, Zhang Z-H, Liu Z-X, Ge R-D, Yong Z and Yan L-E (2024) Incidence and risk factors of severe acute high-altitude illness in healthy adults first entering the northern Tibetan Plateau of over 5,000 m. Front. Public Health. 12:1400236. doi: 10.3389/fpubh.2024.1400236
Edited by:
Niroj Kumar Sethy, Defence Institute of Physiology and Allied Sciences (DRDO), IndiaReviewed by:
Sushil Kumar, University of Colorado, United StatesSrikant S., All India Institute of Medical Sciences, Rishikesh, India
Manish Tiwari, National Dairy Research Institute (ICAR), India
Copyright © 2024 Gao, Qi, Wang, Zhang, Liu, Ge, Yong and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun Gao, Z2FvY2h1bkBiam11LmVkdS5jbg==
†ORCID: Chun Gao, https://orcid.org/0000-0003-3477-5886
 Chun Gao
Chun Gao Guo-Dong Qi3
Guo-Dong Qi3 Rui-Dong Ge
Rui-Dong Ge