
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 03 July 2024
Sec. Public Mental Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1397392
 Kiara Herrmann1,2
Kiara Herrmann1,2 Florian Beese2
Florian Beese2 Lina Wollgast2
Lina Wollgast2 Elvira Mauz2
Elvira Mauz2 Christina Kersjes2
Christina Kersjes2 Jens Hoebel2
Jens Hoebel2 Benjamin Wachtler2*
Benjamin Wachtler2*Background: The existence of socioeconomic inequalities in the prevalence of symptoms of depression and anxiety is widely acknowledged, and individuals from lower socioeconomic backgrounds tend to exhibit higher rates of symptoms. However, the direction in which the COVID-19 pandemic has influenced these disparities remains uncertain. We therefore aimed to systematically outline the available evidence on the temporal dynamics of socioeconomic inequalities in symptoms related to depression and anxiety during the COVID-19 pandemic across high-income countries.
Methods: A scoping review was conducted by searching the databases Embase, Scopus and PsycINFO. According to pre-defined eligibility criteria, two reviewers independently screened titles and abstracts as well as full texts of the compiled records. Data from the included studies were extracted using a standardised data-extraction form and analysed numerically and narratively. The scoping review followed the PRISMA-ScR guidelines.
Results: A total of 49 studies comprising 149 analyses of socioeconomic indicators in relation to symptoms of depression and anxiety were included. Despite heterogeneous study designs and results, there was a tendency of increasing (40.9%; n = 61) or persistent (38.2%; n = 57) inequality trends to the detriment of those in socially more disadvantaged positions. Increasing inequalities were most pronounced when income was used as a socioeconomic indicator. Groups with lower socioeconomic status appeared most vulnerable in the initial phase of the COVID-19 pandemic. Throughout the pandemic, dynamics were diverse, with persistent trends most frequently reported.
Conclusion: Overall, to the detriment of those with lower socioeconomic status, mental-health inequalities persisted or increased in most analyses. Continually monitoring socioeconomic inequalities over time is crucial, since this makes it possible to adapt prevention and intervention strategies to specific pandemic phases. Interventions targeting job security, income security and educational attainment could reduce mental-health inequalities. The results can contribute to preparedness plans for future pandemics and crises.
Socioeconomic inequalities in the prevalence of common mental-health disorders, such as depression and anxiety disorders, are well known, with individuals from more disadvantaged socioeconomic backgrounds having higher prevalence of symptoms (1, 2). Individuals suffering from material deprivation, unemployment, limited access to education and social isolation are particularly vulnerable to symptoms of depression and anxiety (3).
On March 11, 2020, the World Health Organization declared COVID-19 a pandemic (4). As one of the consequences, the COVID-19 Mental Disorders Collaborators predicted a global rise of 27.6% in cases of major depressive disorder and a 25.6% increase in anxiety disorder cases in 2020 (5). Reviews showed that symptoms of common mental disorders increased during the first period of the COVID-19 pandemic (6–8). A decline in symptoms was observed in the course of the pandemic, but figures did not return to pre-pandemic levels (7).
The increase in common mental-health disorders (5) was attributed to many changes in daily routines and the associated stress. Many people experienced resource depletion when being furloughed, dismissed or forced to work under new conditions (9, 10). In addition, policy measures were implemented to curb the spread of the virus, encompassing actions such as the closure of childcare facilities and educational institutions, disrupting routine family dynamics (11). In addition, face-to-face psychosocial services were severely compromised (12). It is plausible that the compounding stressors arising from the COVID-19 pandemic amplified pre-existing mental-health challenges (13). Investigations have indicated a notable global escalation in the occurrence of psychopathologies associated with common mental disorders since the onset of the pandemic (5, 12, 14, 15).
The stressors created by the COVID-19 pandemic may have affected certain socioeconomic groups more severely and may also have had different effects depending on socioeconomic status (SES) (16). As with health inequalities in general, socioeconomic inequalities in symptoms of depression and anxiety disorders may change or reproduce over time, leading to specific social-epidemiological patterns of disease distribution at different stages of the pandemic (17).
In the context of the possibly differential increase in symptoms of mental disorders depending on individuals’ socioeconomic status during the COVID-19 pandemic, the following two theories may serve as theoretical background. The conservation of resources (COR) theory (18) posits that individuals strive to amass and safeguard resources to shield themselves from adversity and manage the requisites of daily life. Resources include valuable circumstances or contexts, personal attributes like self-efficacy, and tangible assets like financial means. A fundamental tenet of this theory underscores that the loss of – or perceived threat to – resources can impact on well-being (19). Despite its apparent paradox, the COR theory acknowledges that individuals with more resources might encounter diminished well-being in specific contexts. The extent of well-being impairment hinges upon how much their personal resources contract within that context (20). In the context of the COVID-19 pandemic, individuals with a higher SES might have experienced a greater detrimental impact on mental health due to greater resource depletion (11).
The second theory is the vulnerability-stress model (21). This model delineates the interactions between vulnerability and stress. The central premise is that both elements are prerequisites for the onset of a mental disorder (21). Vulnerability factors encompass (neuro) biological, psychological and environmental elements of vulnerability (22), contributing to an individual’s susceptibility to mental disorders. The COVID-19 pandemic and its containment measures can be construed as stressors. Assuming heightened vulnerability among individuals with more disadvantaged SES (23), e.g., due to limited financial resources etc., experiences during the COVID-19 pandemic might have more frequently led to symptoms of common mental disorders (24).
First results from studies into changing socioeconomic inequalities in common mental disorders are inconclusive and sometimes contradictory. Some studies from the early stages of the COVID-19 pandemic suggested that socially disadvantaged groups were disproportionately affected by the COVID-19 pandemic and were at increased risk of developing common mental symptoms (13, 25, 26). However, contrasting findings from the USA suggest, for instance, that individuals with a higher education in the USA experienced a significant surge in depressive symptoms during the COVID-19 pandemic (11). Conversely, some studies indicate no differentiation in escalating mental-health problems and depressive symptoms across various SES groups (16, 27). However, comparisons were made between different periods, with some studies comparing to pre-pandemic levels (11, 16, 27) and some exclusively using peri-pandemic data (28–30). Understanding the time-dependent patterns of socioeconomic inequalities in mental-health complaints during the COVID-19 pandemic could help identify high-risk groups at different stages of the pandemic and enable timely public-health interventions to reduce mental-health inequalities and the overall burden of disease.
We therefore conducted a systematic scoping review to address the following research question: what is the evidence relating to trends in socioeconomic inequalities in symptoms of common mental-health disorders in high-income countries during the COVID-19 pandemic? To the best of our knowledge, this is the first systematic review of the evidence on SES-specific changes in symptoms of common mental disorders during the COVID-19 pandemic.
We conducted a systematic scoping review by searching the databases Scopus, Embase and PsycINFO in order to identify, collate, map and finally synthesise the available evidence (31, 32). Scopus offered a comprehensive compilation of international medical and social scientific publications relevant to the research question (33). Embase covered biomedical journals and included Medline records from 2010 onwards (34), while PsycINFO complemented the database search with psychology-related publications (35). A detailed study protocol was published on the Open Science Framework (36) prior to the start of the study. This review follows the preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) guidelines (37).
This review concentrated on four main concepts: (1) socioeconomic inequalities, (2) symptoms of common mental-health disorders, (3) COVID-19, and (4) longitudinal design. Due to comparability concerns (38, 39), low- and middle-income countries were excluded based on the World Bank’s list published in 2021 (40). Database-specific search strings were developed for each concept (see Supplementary material S2), tailored to the respective databases, including relevant expanding terms like Emtree thesaurus for the Embase search. A scientific librarian was consulted during the search string development process. An additional filter was used to restrict the publication time from 2020 until the day of the search in 2023. Search terms were applied to search within titles and abstracts. The search in the electronic databases Scopus, Embase and PsycINFO was conducted on 14 May 2023.
The review only considered literature meeting predefined eligibility criteria (Table 1).
The selected studies were required to examine temporal dynamics in symptoms of common mental disorders during the COVID-19 pandemic, i.e., measures against depression or anxiety associated with socioeconomic factors had to be assessed at least at two different time points. Depressive and anxiety disorders are known to be frequently underdiagnosed in healthcare settings, and diverse access barriers might lead to an undertreatment (41). We therefore exclusively included studies that systematically ascertained symptoms via primary data collection in the general population and studies that used only secondary data; e.g. settlement data from health insurances were excluded to reduce selection bias. The initial time points may have preceded the onset of the COVID-19 pandemic, while the subsequent time points can have been during the pandemic. Alternatively, data collection might have taken place at two time points during the COVID-19 pandemic. Hence, cohort studies and repeated cross-sectional studies were eligible for inclusion. In scoping reviews there is typically no assessment of the quality of evidence conducted due to the heterogeneity of the included studies (31, 32). Peer-reviewed studies are generally subject to a minimum standard level of quality control. In contrast, non-peer reviewed publications, such as study preprints, do not have such requirement and hence were excluded. The target population encompassed the general population at a national or at least regional level. Studies with relatively homogeneous study populations (e.g., specific occupational cohorts) were excluded, as they did not permit systematic comparisons of risks between socioeconomic groups and might be particularly prone to collider bias.
Two reviewers (KH and LW) independently screened the titles and abstracts of the records obtained from the database search and the full texts of the identified studies. The software Rayyan (42) supported the title and abstract screening. To assess interrater reliability, Cohen’s Kappa coefficient was calculated for both stages of study selection (43). In cases of disagreement, the records were discussed until a consensus was reached. A PRISMA flow chart summarised and visually represented the selection process. Microsoft Excel was used for all descriptive statistical analyses and the calculation of the Cohen’s Kappa coefficient.
A standardised data-extracting chart was designed in an iterative process. After agreement on the data chart was reached, the following information was extracted from each included full-text article: author (year), country, number of participants, study design, observation period, outcome, socioeconomic indicator, outcome measures (e.g., odds ratio), most-affected SES-group, inequality trend, absolute or relative outcome measure. The results of temporal dynamics in socioeconomic inequalities were categorised into four groups: (1) persistent, (2) increasing, (3) decreasing or (4) crossing over time. For example, increasing inequalities were assumed if the prevalence difference between the highest and lowest socioeconomic category increased over time. Socioeconomic indicators were categorised based on income, education, occupation (including employment) or index-based socioeconomic measures. In the following, the term study refers to the published study, including all analyses, and the term analysis refers to the one particular analysis that was reported by the study.
First, all the articles were summarised in a table based on these previously defined components and adjusted in an iterative process. This table provided an overview of the temporal patterns observed for each outcome and socioeconomic indicator. Second, the principal descriptive results were summarised graphically or numerically. Finally, these preliminary descriptive results were used to narratively synthesise the evidence (44).
Out of all 8,664 database records identified by our search, 49 articles met all the eligibility criteria comprising a total of 149 analyses that combined different socioeconomic indicators with symptoms of depression and anxiety over time. The study selection process is presented in detail in Figure 1.
The Cohen’s Kappa coefficient in the title and abstract screening was 0.931. The interrater percent agreement was 99.8%. In the full-text screening, Cohen’s Kappa coefficient was 0.799. The interrater percent agreement was 90.0%.
An overview of the included studies and their main findings is presented in Table 2.
Most of the included studies came from the USA (n = 14). 5 studies were conducted in the UK and 4 were from the Netherlands and Hong Kong. Three studies were conducted in Germany and Korea, respectively. One study was conducted in each of the following countries: Norway, Italy, Romania, Luxembourg, Switzerland, Portugal, Canada, Chile, Qatar, Israel and Japan. In addition, there were 2 cross-continental studies and 3 studies relating to multiple European countries.
Of the included studies, 32 were cohort studies and 17 were repeated cross-sectional studies. Six studies were published in 2020, 14 in 2021, 23 in 2022, and 6 in 2023.
The size of the sample populations varied substantially with a mean number of participants of 143,222 and a median number of participants of 7,160.
A comprehensive overview of the socioeconomic indicators used in the included studies can be found in Supplementary material S3. Income (n = 54) and education (n = 52) were the most frequently used socioeconomic indicators. Occupation, or employment, was used in 41 analyses. Two analyses assessed the SES by using the Index of Multiple Deprivation (IMD). Socioeconomic inequalities were most frequently assessed via relative measures (n = 90, 60.4%). In 22 (7.4%) analyses, only absolute measures and in 37 (24.8%) analyses, both relative and absolute measures were presented.
The scores used to measure symptoms of depression and anxiety disorders are shown in Supplementary material S4. Among the included studies, depression was the most frequently investigated outcome (n = 38). 24 studies investigated anxiety as an outcome. No study exclusively examined anxiety. In 24 studies, both depressive symptoms and symptoms of anxiety were assessed independently, and 11 studies measured a combined outcome of depression and anxiety.
The instrument most frequently used to measure symptoms of depression was the “Patient Health Questionnaire (PHQ)-9” (n = 16), and the second most used was the PHQ-2 (n = 8), a short version of the PHQ-9 (88). The “Depression Anxiety Stress Scale (DASS)-21 depression subscale” (n = 3) was used third most frequently.
To measure anxiety, the “Generalised Anxiety Disorder Scale (GAD)-2” (n = 8) was commonly used as an abbreviation of GAD-7 (88). The GAD-7 itself was used in seven studies. The DASS-21 anxiety subscale (n = 2) was used third most frequently.
If symptoms of depression and anxiety were measured in combination, the most frequently used instrument was the PHQ-4 (n = 6). All other instruments were used only once.
For the PHQ-9 and GAD-7 instruments, cut-off scores greater than or equal to 10 were used, or the cut-off score was not reported. For the short forms of these instruments, the PHQ-2 and GAD-2 questionnaires, cut-off scores ≥3 were used or not reported. The cut-off score for the PHQ-4 was generally ≥6, except for two studies, which set the cut-off score to 3 (78) or compared the average score over time (47).
Most studies (n = 31) used at least two comparison time points during the COVID-19 pandemic, while 15 studies compared at least one time point before the pandemic with at least one time point during the pandemic. In three studies, multiple time points were used for comparison, so that analyses were possible both before-to-during and during the COVID-19 pandemic (54, 69, 82). The earliest start of the observation period compared from before to during the pandemic in the included studies was in 1999, while the latest start was in November 2019. The earliest onset for a comparison period within the pandemic was March 2020, while the latest beginning was June 2021. All studies’ mean duration of the observation period was 736 days, with a median of 365 days and a range from 32 days to 20 years. Frequently, studies used data showing temporal dynamics based on monthly or yearly outcome rates. Multiple studies, however, compared several pandemic waves or specific time points associated with contextual factors, such as the introduction of containment orders. Additional details on the observation periods can be found in Supplementary material S5.
In almost all analyses, socially disadvantaged groups were most affected at baseline. Most often, the lowest category was the most affected, rarely the second-lowest category, and occasionally also the middle category of the respective component of SES. However, there were some exceptions. Three studies from Hong Kong (59, 65, 81), two cohort studies from Chile and the UK (49, 71) and two studies across several European countries (56, 57) showed heterogenous results regarding the most affected socioeconomic group at baseline.
Of all analyses, 40.9% (n = 61) indicated increasing and 38.2% (n = 57) showed persistent inequalities. 17.4% (n = 26) found decreasing inequalities over time (Figure 2). Among the five analyses showing crossover dynamics in inequalities, four demonstrated a transition from initially higher prevalences in more deprived populations to higher prevalences in more affluent populations over time. One analysis showed crossover dynamics to the detriment of more deprived parts of the population. Considering the initial situation, most of the analyses (63.8%, n = 95) showed either persistent or increasing inequalities, with socioeconomically disadvantaged populations being the most affected.
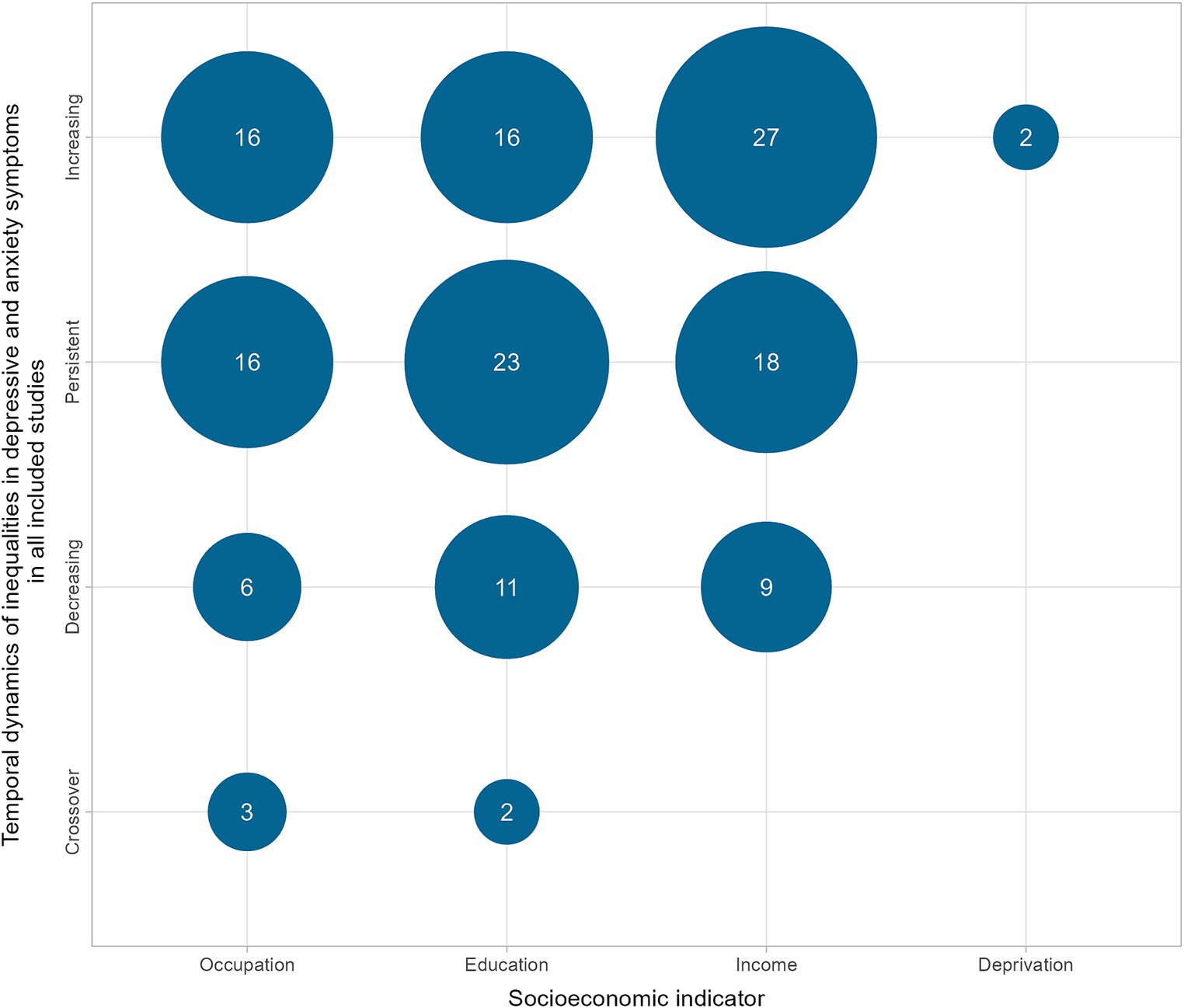
Figure 2. Number of analyses showing temporal dynamics of socioeconomic inequalities in depressive and anxiety symptoms in all included studies.
Similar to the overall proportions of all analyses, among the analyses that specifically focused on comparisons between periods before and during the COVID-19 pandemic (n = 56), 46.4% (n = 26) revealed increasing inequalities, 30.4% (n = 17) indicated persistent inequalities, 19.6% (n = 11) showed decreasing inequalities, and 3.6% (n = 2) found crossover dynamics over time (Figure 3).
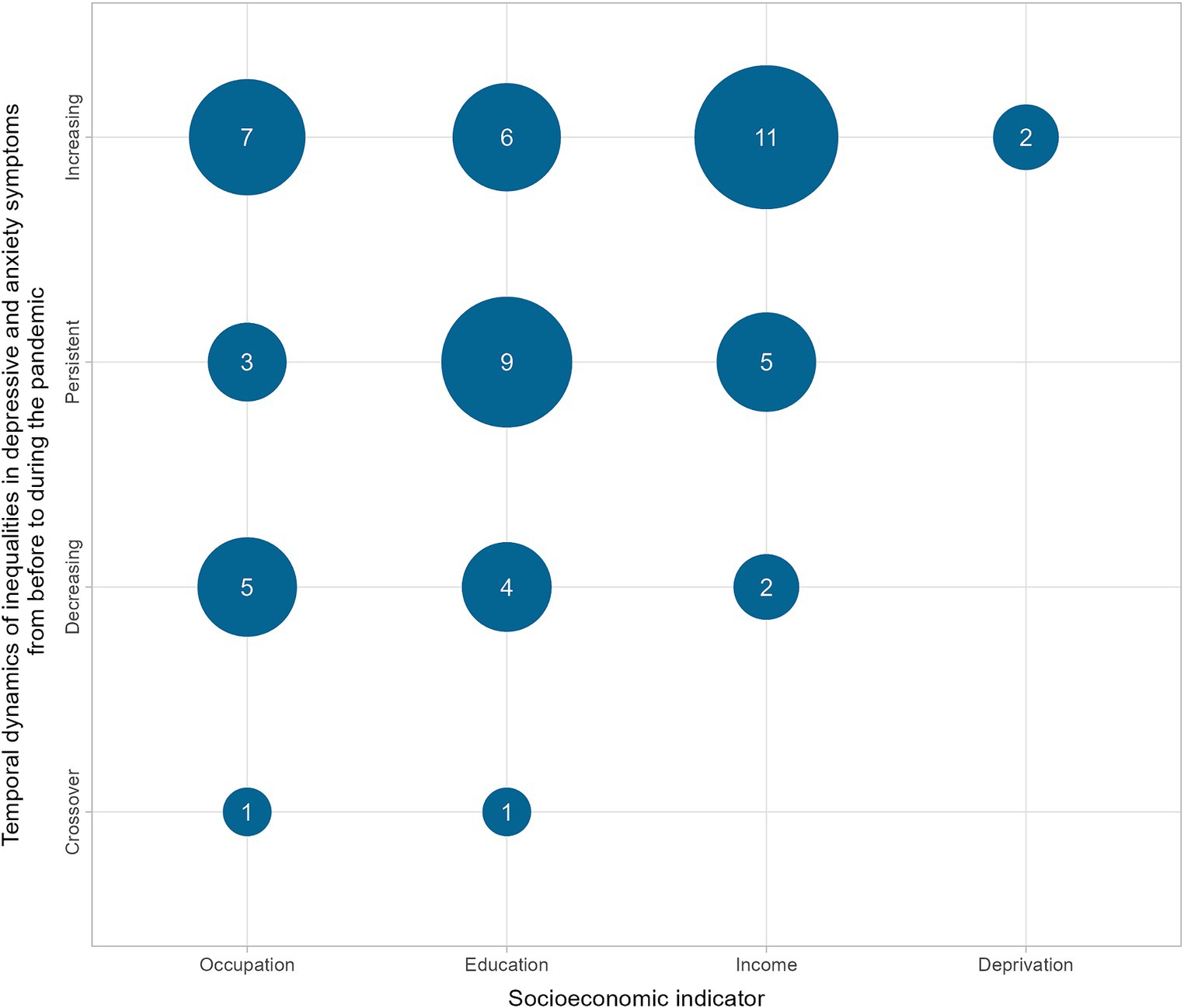
Figure 3. Number of analyses showing temporal dynamics in depressive and anxiety symptoms from before the pandemic to during the pandemic.
Increasing and persistent inequalities combined accounted for more than three-quarters of the findings (76.8%). Specifically, with regard to income, the majority of the analyses (n = 11) indicated an increase in inequalities. In addition, we identified a trend of increasing or persistent inequalities during the early stages of the pandemic (March or April 2020) that negatively affected low SES groups (51, 82–86) in our more detailed analyses studies.
Upon closer examination of single countries, the USA stands out due to the highest number of included studies and contradictory results. Using the PHQ-9, Ettman et al. (51) showed that depressive symptoms tripled from 2017 to April 2020 in the USA, and low income and little savings were a risk for depressive symptoms in the initial stage of the COVID-19 pandemic. The population-representative survey study showed a stronger increase in depressive symptoms in the lowest and second-lowest income categories (51). In contrast, Wanberg et al. (11) came to different results, reporting that people with higher education had a higher risk of developing depressive symptoms in the USA between April 2019 and April 2020. The two studies differed in their pre-pandemic comparison date, screening tools, and methodology.
Regarding symptoms of common mental disorders and the dimension of educational attainment, a study conducted by Zhao et al. (86) in Hong Kong showed results similar to those of Ettman et al. in the USA. Specifically, Zhao et al. (86) analysed data on depression and anxiety symptoms from 2016 to April 2020 and found that individuals with low levels of formal education were particularly vulnerable to developing symptoms in the early stages of the pandemic. Mauz et al. (69) examined temporal trends in depressive symptoms based on educational attainment in Germany. Over the entire observation period from spring/summer 2019 to 2022, they observed an increase in the standardised proportions of individuals with a positive screen (69). A social gradient to the detriment of those with the lowest educational attainment was apparent throughout the whole observation period (69). In the high-level education group, there was a 5.2% increase (from 5.5%), while in the middle group, there was a 4.6% increase (from 10.6%), and in the low-level education group a 4.8% increase (from 16.2%) (69). Although all education groups had higher values at the end, the progression during the pandemic differed (69). The middle education group benefited at the beginning, and the higher education group was more affected as the pandemic progressed (69).
In the dimension of income or financial situation and inequality in symptoms of common mental-health disorders, a cohort study combining two different population cohorts from the UK ending in May 2020 found that socioeconomically disadvantaged people had higher levels of anxiety and depression, even when pre-pandemic levels were taken into account (64). Lower income, financial problems and deprivation were associated with a greater risk of symptoms of depression and anxiety. Anxiety symptoms exhibited a more profound increase compared to depressive symptoms. This surge was attributed to the uncertainty and sudden disruptions in daily life, coupled with health-related apprehensions (64).
Among the analyses investigating the dynamics of socioeconomic inequalities in symptoms of common mental disorders during the COVID-19 pandemic (n = 93), 43.0% (n = 40) showed persistent inequalities, 37.6% (n = 35) increasing inequalities, 16.1% (n = 15) decreasing inequalities, and 3.2% (n = 3) crossover dynamics (Figure 4).
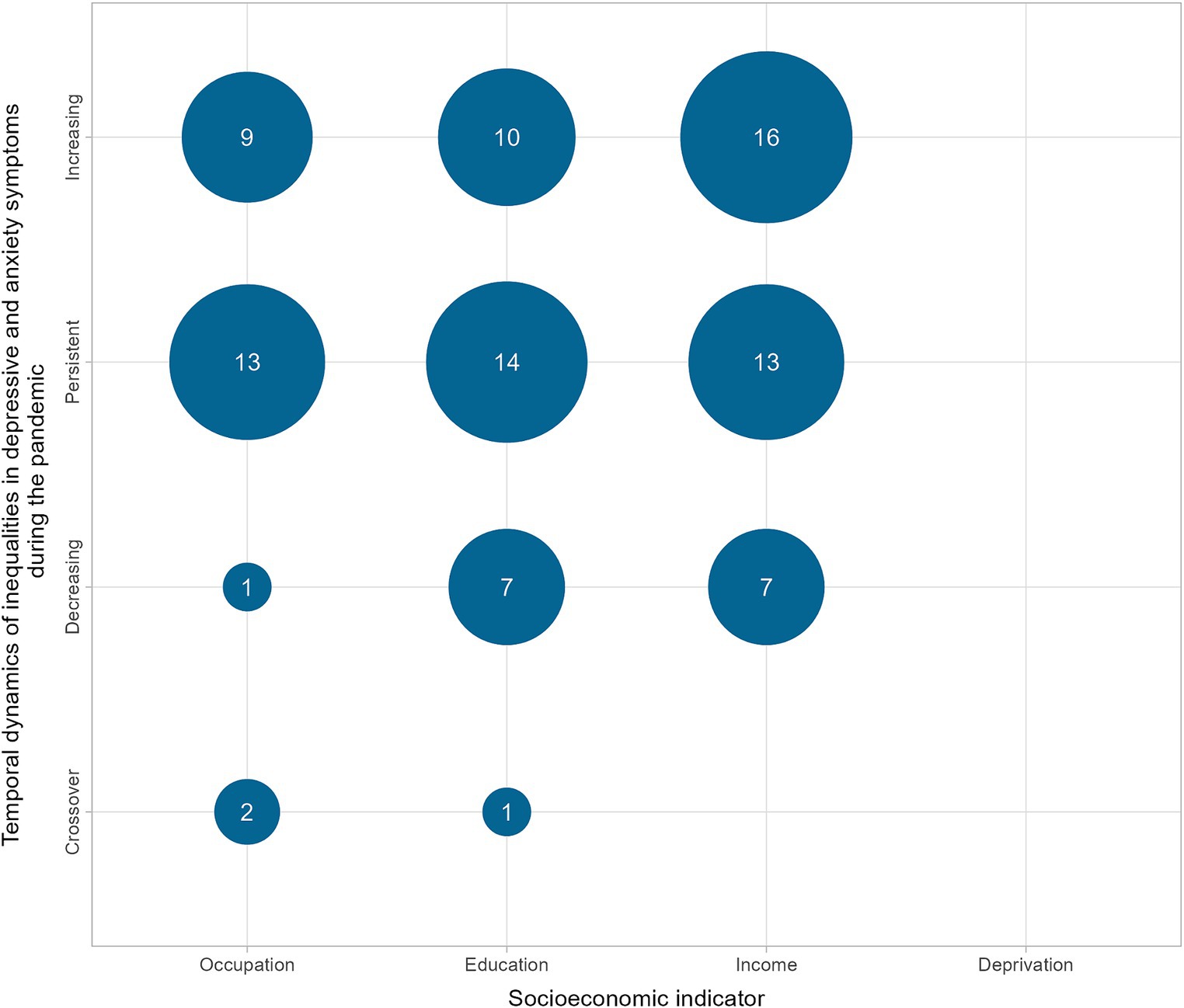
Figure 4. Number of analyses showing temporal dynamics of socioeconomic inequalities in depressive and anxiety symptoms during the pandemic.
Regarding symptoms of common mental disorders and the dimension of educational attainment, there were contrasting results in the USA, highlighted in the following section. Educational inequalities in depressive symptoms increased in the USA in May 2020 and then stabilised, according to Coley and Baum (46). In the case of symptoms of anxiety disorders, on the other hand, after an increase in May 2020, there was a decrease in educational inequality in autumn 2020 (46). Twenge et al. (82) reported that the relative increase in anxiety and depression in the USA was greater among those with higher education and income. However, those with lower education and income still had a higher prevalence (82). By contrast, Vahratian et al. (29) reported that the percentage of adults who had symptoms of anxiety disorder and depression increased during the pandemic, as did unmet mental-health needs. The most significant increases were among those aged between 18 and 29 and those with less than a high-school education (29).
In the dimension of income or financial situation and inequality in symptoms of common mental-health disorders, most studies concluded that inequalities have worsened or remained unchanged. In the UK, Saunders et al. (30) reported that from March to July 2020, individuals with lower incomes had higher symptoms at baseline, which then increased steadily during and after the relaxation of restrictions. Between May 2020 and February/March 2021, Moreno-Agostino et al. (71) examined self-reported financial difficulties, depression and anxiety in five existing UK adult cohorts. Large inequalities were observed and remained constant throughout the examined period (71). This finding aligned with previous research that found large inequalities employing various indicators of household economic conditions (16, 30, 53, 64). Riehm et al. (78) conducted a longitudinal study examining mental distress (PHQ-4) in a nationally representative sample of USA adults from March to August 2020. Prevalence of mental distress reached its highest point in mid-April to early May 2020 and subsequently declined (78). The trajectories of mental distress over the duration of the 4.5 months study period displayed a general resemblance across various sociodemographic subgroups, one of the investigated socioeconomic indicators being the distinction between individuals living below or above the federal poverty line (78).
Fancourt et al. (53) demonstrated with a prospective longitudinal observational study that inequalities in the UK tended to converge over 20 weeks after the lockdown was announced but persisted until the end of the study period. 36,520 participants had at least three measurements at different time points, and their data were analysed using latent growth models. Numerous risk factors associated with worse mental-health outcomes, such as female gender, younger age and lower educational attainment, were prominently observable during the early stages of the lockdown (53). As mental health gradually improved, the inequalities between these vulnerable demographic groups and those without these risk factors diminished. However, the inequalities in mental health persisted, and vulnerable groups have remained at risk (53).
This is the first systematic scoping review of the international evidence on the temporal dynamics of socioeconomic inequalities in symptoms of depression and anxiety disorders during the COVID-19 pandemic. Trends became evident despite the marked heterogeneity of the studies in terms of observation periods, outcomes, socioeconomic indicators and methods. Overall, most analyses showed increasing or persistent inequality trends. In the narrative synthesis of the studies, we identified a trend of increasing inequalities during the early stage of the pandemic that negatively affected low SES groups (46, 50, 51, 64). During the pandemic, there were very heterogeneous developments, with persistent inequalities reported most frequently (46, 69, 71). Large inequalities were observed concerning income, including financial situation using different indicators of household economic situation (16, 30, 53, 64, 71, 75, 80).
The included studies discussed potential explanations for the observed trends. In the initial phase of the COVID-19 pandemic, socioeconomic inequality in symptoms of depression and anxiety increased in many analyses. One reason proposed was that segments of the population with lower SES were disproportionately affected, experiencing job losses, reduced working hours, having to continue to work despite increased exposure, and particularly suffering from the deteriorating economic conditions (9, 10). A Canadian study reported that a third of their sample reported losing household income or occupational status (67). Those who moved down the social gradient and those who were always disadvantaged had a higher prevalence of symptoms of mental disorders (58, 80, 89). Dragano et al. (48) described that mental health was negatively influenced by pandemic-related job loss, reduction in working hours without short-time allowance, increase in working hours, switch to home-based work, increased job insecurity, and a worsening financial situation. The increase in mental-health problems was significantly lower after statistically controlling for work-related changes and financial strain (48). This indicates that the mean increase in symptom severity during the pandemic was primarily due to increased occupational and financial stress (48). Most pandemic-related job changes, except for increased home office work (76), may have particularly affected individuals with a low SES (26, 59, 73). Financial strain might have particularly afflicted individuals with lower incomes, which, in accordance with the vulnerability-stress model, might have led to deteriorating mental health (16, 90).
As the COVID-19 pandemic progressed, there were reports of increased depressive or anxiety symptoms among population groups with higher SES. One cited reason was the prevalence of remote work conditions (11). Min et al. (70) suggested that differential access to information may have contributed to the fact that people with higher SES were increasingly affected by the pandemic. Previous studies reported that people were exposed to anxiety-provoking information via social media, and more frequent exposure to such information may have led to higher vulnerability to mental-health deterioration when the future was unpredictable (91). In this regard, young, middle-aged, highly educated and high-income individuals were more likely to be exposed to negative information from the internet and social media than the general population (70). In addition, in several studies, the COR theory (18) was invoked to rationalise the fact that individuals with higher SES experienced relatively greater losses (11, 81). Higher SES could have been associated with a greater loss of interpersonal resources, as individuals with higher SES were likelier to work at home during the pandemic than those with lower SES (11).
Even in high-income countries, substantial heterogeneity existed in initial conditions, outcomes and mitigation measures during the COVID-19 pandemic. Some authors have suggested that this variability could account for divergent findings and conclusions, emphasising the importance of caution when extrapolating results across nations (13, 77, 83). Maffly-Kipp et al. (13) concluded that the severity of the COVID-19 pandemic influenced the relationship between socioeconomic factors and mental-health outcomes. In addition, van der Velden et al. (83) mentioned that differences in unemployment rates in March and April 2020 differed drastically between the USA and the Netherlands and might explain differences in results. A study from Luxembourg mentioned that Luxembourg implemented many policy measures to mitigate the spread of the disease and its economic consequences (77). Therefore, the authors emphasised that the mental-health impact should not be underestimated in other less affluent countries that were more seriously affected (77). A rapid review from 2021 in Germany showed that mental health was stable or advantageous for low SES groups during the first phase of the pandemic (92). The pronounced heterogeneity between countries could explain the discrepancy between the rapid review (92) and this scoping review.
Some studies identified demographic subgroups at higher risk for mental-health problems during the COVID-19 pandemic. Concerning generational inequality, young adults were frequently mentioned as disproportionally vulnerable during the COVID-19 pandemic (29, 30, 50, 54, 55, 62, 66, 70, 71, 75, 77, 78, 87, 91, 93). This could be related to SES, as young people often have yet to reach a higher level of education, are still studying or in training, and consequently have a lower income (94). They are pursuing their education instead of working in a full-time paid job (94). For this age group, the literature discusses the greater overall disruption of life during the pandemic (57) against the background of the particularly great importance of social contacts with peers when leaving home. If we also take a look at family health, which is still important for young adults, a scoping review of mediators of health inequalities in children and adolescents pointed to the role of parental mental health, parenting practices, and the parent–child relationship, which could also serve as targets for interventions (95). The majority of studies suggested future pandemic-preparedness measures, including health-care access and targeted interventions for disadvantaged populations (53, 64, 71, 74, 76). Identifying at-risk populations and collecting data on subgroups enables targeted support, as highlighted by multiple studies (30, 66, 69, 86).
Both relative and absolute measures of inequality were presented in only 24.8% of the analyses from the included studies. Research should precisely assess the magnitude and changes in socioeconomic health inequalities by consistently employing summary metrics for absolute and relative inequalities (96). This approach helps prevent biased interpretations of health-inequality trends resulting from the selective reporting of inequality measures (96). In future cohort or cross-sectional study publications, it would be desirable to present relative and absolute measures to view the development in its entirety. The measurement instruments of depressive symptoms and symptoms of anxiety disorders and their corresponding cut-off values were relatively uniform using the PHQ-9 and GAD-7 and their short forms. By contrast, the study designs and methodology were very heterogeneous. Standardised study designs and methodology would be desirable to answer social-epidemiological questions. Subsequent investigations are imperative to quantitatively elucidate the extent of the correlation between socioeconomic indicators and symptoms of common mental disorders over time. Addressing this inquiry will necessitate forthcoming reviews to concentrate on narrower sets of socioeconomic indicators (e.g., household income categories), outcomes (e.g., PHQ-9, GAD-7) and periods (e.g., specific waves during the pandemic). Continuous, unified monitoring and comprehension of developments might help to develop more targeted support.
This is the first systematically conducted scoping review investigating the temporal dynamics of socioeconomic inequalities related to symptoms of depression and anxiety disorders during the COVID-19 pandemic in high-income countries. The systematic literature search contributed to achieving a high degree of comprehensiveness and ensured the replicability of the results. However, it could not be entirely ruled out that additional relevant records were perhaps obtained via supplementary databases or manual searches. Systematic assessment of methodological limitations of the included studies was not possible due to the heterogeneity of the studies, which might have introduced bias into the narrative synthesis (97). Nevertheless, this approach of a scoping review appeared most fitting considering the review’s objectives of compiling a first and comprehensive overview. Potential selection and publication bias are concerns due to the review’s exclusive focus on peer-reviewed publications. Studies that found null results were possibly neglected and not published. This bias could have been mitigated by incorporating non-peer-reviewed literature. However, since a structured assessment of evidence quality could not be executed (32), the eligibility criteria were confined to peer-reviewed articles to enhance the quality of the findings encompassed in the study. For reasons of comparability, this review was limited to high-income countries (38, 39), which should be borne in mind when interpreting the results. In addition, this study included only articles published in English or German. This approach can limit the generalisability of the results.
This scoping review can contribute to improving preparedness for future pandemics or crises. It became apparent that social inequality in mental health increased or at least persisted in most cases to the disadvantage of the deprived population. Considering the temporal dynamics of mental-health inequalities can help prevent harmful effects on the mental health of specific population groups during different pandemic stages. Job security, income security, educational attainment and community-based initiatives, including targeted prevention and intervention programmes that consider diverse socioeconomic backgrounds, could be important targets for interventions to address health inequalities. Socioeconomic inequalities must be monitored to adapt prevention and intervention measures to specific phases. Reducing socioeconomic inequalities is crucial to improving population health and achieving equity in the face of a significant burden of common mental-health disorders and existing inequalities.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
KH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. FB: Conceptualization, Methodology, Visualization, Writing – review & editing. LW: Writing – review & editing, Data curation. EM: Writing – review & editing. CK: Writing – review & editing. JH: Writing – review & editing. BW: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was part of the research project “Socioeconomic Inequalities during the COVID-19 Pandemic (INHECOV) – Empirical Analyses and Implications for Pandemic Preparedness” funded by the German Research Foundation (Grant number 458531028).
We would like to thank Dr. Franziska Klatt, head of the Teaching Library at the Technical University of Berlin, for the search string consultation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1397392/full#supplementary-material
1. WHO . Depression and other common mental disorders – Global Health estimates. Geneva: World Health Organization (2017).
2. Freeman, A, Tyrovolas, S, Koyanagi, A, Chatterji, S, Leonardi, M, Ayuso-Mateos, JL, et al. The role of socio-economic status in depression: results from the COURAGE (aging survey in Europe). BMC Public Health. (2016) 16:1098. doi: 10.1186/s12889-016-3638-0
3. WHO & CGF . Social determinants of mental health – 1.Mental health. 2.Socioeconomic factors. 3.Mental disorders – Prevention and control. Geneva: World Health Organization (2014).
4. Mahase, E . Covid-19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. BMJ. (2020) 368:m1036. doi: 10.1136/bmj.m1036
5. Santomauro, DF, Herrera, AMM, Shadid, J, Zheng, P, Ashbaugh, C, Pigott, DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
6. Kunzler, AM, Rothke, N, Gunthner, L, Stoffers-Winterling, J, Tuscher, O, Coenen, M, et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Glob Health. (2021) 17:34. doi: 10.1186/s12992-021-00670-y
7. Richter, D, Riedel-Heller, S, and Zurcher, SJ. Mental health problems in the general population during and after the first lockdown phase due to the SARS-Cov-2 pandemic: rapid review of multi-wave studies. Epidemiol Psychiatr Sci. (2021) 30:e27. doi: 10.1017/S2045796021000160
8. Salari, N, Hosseinian-Far, A, Jalali, R, Vaisi-Raygani, A, Rasoulpoor, S, Mohammadi, M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. (2020) 16:57. doi: 10.1186/s12992-020-00589-w
9. Lee, H, and Singh, GK. Monthly trends in self-reported health status and depression by race/ethnicity and socioeconomic status during the COVID-19 pandemic, United States, April 2020 – may 2021. Ann Epidemiol. (2021) 63:52–62. doi: 10.1016/j.annepidem.2021.07.014
10. Kimhi, S, Eshel, Y, Marciano, H, Adini, B, and Bonanno, GA. Trajectories of depression and anxiety during COVID-19 associations with religion, income, and economic difficulties. J Psychiatr Res. (2021) 144:389–96. doi: 10.1016/j.jpsychires.2021.10.043
11. Wanberg, CR, Csillag, B, Douglass, RP, Zhou, L, and Pollard, MS. Socioeconomic status and well-being during COVID-19: a resource-based examination. J Appl Psychol. (2020) 105:1382–96. doi: 10.1037/apl0000831
12. WHO . Mental health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022. (2022):[13 p.]. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 Accessed January 30, 2024).
13. Maffly-Kipp, J, Eisenbeck, N, Carreno, DF, and Hicks, J. Mental health inequalities increase as a function of COVID-19 pandemic severity levels. Soc Sci Med. (2021) 285:114275. doi: 10.1016/j.socscimed.2021.114275
14. Jones, EAK, Mitra, AK, and Bhuiyan, AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. (2021) 18:2470. doi: 10.3390/ijerph18052470
15. Min, S, Jeong, YH, Kim, J, Koo, JW, and Ahn, YM. The aftermath: post-pandemic psychiatric implications of the COVID-19 pandemic, a south Korean perspective. Front Psych. (2021) 12:671722. doi: 10.3389/fpsyt.2021.671722
16. Pierce, M, Hope, H, Ford, T, Hatch, S, Hotopf, M, John, A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. (2020) 7:883–92. doi: 10.1016/S2215-0366(20)30308-4
17. Lampert, T, Kroll, LE, Kuntz, B, and Hoebel, J. Health inequalities in Germany and in international comparison: trends and developments over time. J Health Monit. (2018) 3:1–24. doi: 10.17886/RKI-GBE-2018-036
18. Hobfoll, SE, Tirone, V, Holmgreen, L, and Gerhart, J. Conservation of resources theory applied to major stress. In: Fink G, editor. Stress: concepts, cognition, emotion, and behavior. Handbook of stress. San Diego, CA, US: Elsevier Academic Press (2016). 65–71.
19. Hobfoll, SE . Conservation of resources. A new attempt at conceptualizing stress. Am Psychol. (1989) 44:513–24. doi: 10.1037/0003-066X.44.3.513
20. Hobfoll, SE ed. Conservation of resources theory: Its implications for stress, health, and resilience. New York, NY: Oxford University Press (2010).
21. Wittchen, H-U, and Hoyer, J. Klinische Psychologie & Psychotherapie (German). “Clinical psychology & psychotherapy”. Springer Berlin, Heidelberg: Springer (2011).
22. Brakemeier, EL, Normann, C, and Berger, M. Atiopathogenese der unipolaren Depression. Neurobiologische und psychosoziale Faktoren (German). “The etiopathogenesis of unipolar depression. Neurological and psychosocial factors”. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2008) 51:379–91. doi: 10.1007/s00103-008-0505-x
23. Patel, JA, Nielsen, FBH, Badiani, AA, Assi, S, Unadkat, VA, Patel, B, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. (2020) 183:110–1. doi: 10.1016/j.puhe.2020.05.006
24. Tham, WW, Sojli, E, Bryant, R, and McAleer, M. Common mental disorders and economic uncertainty: evidence from the COVID-19 pandemic in the U.S. PLoS One. (2021) 16:e0260726. doi: 10.1371/journal.pone.0260726
25. Iob, E, Frank, P, Steptoe, A, and Fancourt, D. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2026064. doi: 10.1001/jamanetworkopen.2020.26064
26. Witteveen, D, and Velthorst, E. Economic hardship and mental health complaints during COVID-19. Proc Natl Acad Sci USA. (2020) 117:27277–84. doi: 10.1073/pnas.2009609117
27. Reme, BA, Worn, J, and Skirbekk, V. Longitudinal evidence on the development of socioeconomic inequalities in mental health due to the COVID-19 pandemic in Norway. Sci Rep. (2022) 12:3837. doi: 10.1038/s41598-022-06616-7
28. Vancea, F, and Apostol, M. Changes in mental health during the COVID-19 crisis in Romania: a repeated cross-section study based on the measurement of subjective perceptions and experiences. Sci Prog. (2021) 104:368504211025873. doi: 10.1177/00368504211025873
29. Vahratian, A, Blumberg, SJ, Terlizzi, EP, and Schiller, JS. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic – United States, august 2020–February 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:490–4. doi: 10.15585/mmwr.mm7013e2
30. Saunders, R, Buckman, JEJ, Fonagy, P, and Fancourt, D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol Med. (2022) 52:4049–57. doi: 10.1017/S0033291721000957
31. Arksey, H, and O'Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
32. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18:2119–26. doi: 10.11124/JBIES-20-00167
33. Burnham, JF . Scopus database: a review. Biomed Digit Libr. (2006) 3:1. doi: 10.1186/1742-5581-3-1
34. Lam, MT, De Longhi, C, Turnbull, J, Lam, HR, and Besa, R. Has Embase replaced MEDLINE since coverage expansion? J Med Libr Assoc. (2018) 106:227–34. doi: 10.5195/jmla.2018.281
35. Bramer, WM, Rethlefsen, ML, Kleijnen, J, and Franco, OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. (2017) 6:245. doi: 10.1186/s13643-017-0644-y
36. Herrmann, KM . Socioeconomic inequalities in symptoms of common mental health disorders during SARS-CoV-2 pandemic in high-income countries –a scoping review protocol Open Science Framework (2023). doi: 10.17605/OSF.IO/NKQSD
37. Tricco, AC, Lillie, E, Zarin, W, O'Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
38. Aung, MN, Koyanagi, Y, and Yuasa, M. Health inequality among different economies during early phase of COVID-19 pandemic. J Egypt Public Health Assoc. (2021) 96:3. doi: 10.1186/s42506-021-00067-0
39. Bernardini, F, Attademo, L, Rotter, M, and Compton, MT. Social determinants of mental health as mediators and moderators of the mental health impacts of the COVID-19 pandemic. Psychiatr Serv. (2021) 72:598–601. doi: 10.1176/appi.ps.202000393
40. The World Bank Group . The world by income and region (2021) [2023 March 3]. Available at: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html (Accessed January 30, 2024).
41. Handy, A, Mangal, R, Stead, TS, Coffee, RL Jr, and Ganti, L. Prevalence and impact of diagnosed and undiagnosed depression in the United States. Cureus. (2022) 14:e28011. doi: 10.7759/cureus.28011
42. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
43. McHugh, ML . Interrater reliability: the kappa statistic. Biochem Med (Zagreb). (2012) 22:276–82. doi: 10.11613/BM.2012.031
44. Rodgers, M, Sowden, A, Petticrew, M, Arai, L, Roberts, H, Britten, N, et al. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews. SAGE Publications (Los Angeles, London, New Delhi and Singapore). (2009);15:047–071.
45. Cha, WT, Joo, HJ, Park, YS, Park, EC, and Kim, SY. Depression before and during-COVID-19 by Gender in the Korean Population. Int. J. Environ. Res. Public Health. (2022) 19:3477.
46. Coley, RL, and Baum, CF. Trends in mental health symptoms, service use, and unmet need for services among US adults through the first 8 months of the COVID-19 pandemic. Transl Behav Med. (2022) 12:273–83. doi: 10.1093/tbm/ibab133
47. Daly, M, and Robinson, E. Psychological distress and adaptation to the covid-19 crisis in the United States. J Psychiatr Res. (2020) 136:603–9. doi: 10.1016/j.jpsychires.2020.10.035
48. Dragano, N, Reuter, M, and Berger, K. Increase in mental disorders during the COVID-19 pandemic—the role of occupational and financial strains. An analysis of the German National Cohort (NAKO) study. Dtsch Arztebl Int. (2022) 119:179–87. doi: 10.3238/arztebl.m2022.0133
49. Duarte, F, and Jimenez-Molina, A. A longitudinal Nationwide study of psychological distress during the COVID-19 pandemic in Chile. Front Psych. (2022) 13:744204. doi: 10.3389/fpsyt.2022.744204
50. Ebrahimi, OV, Bauer, DJ, Hoffart, A, and Johnson, SU. A critical period for pandemic adaptation: the evolution of depressive symptomatology in a representative sample of adults across a 17-month period during COVID-19. J Psychopathol Clin Sci. (2022) 131:881–94. doi: 10.1037/abn0000786
51. Ettman, CK, Abdalla, SM, Cohen, GH, Sampson, L, Vivier, PM, and Galea, S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
52. Ettman, CK, Cohen, GH, Abdalla, SM, Sampson, L, Trinquart, L, Castrucci, BC, et al. Persistent depressive symptoms during COVID-19: a national, population-representative, longitudinal study of U.S. adults. The Lancet Regional Health - Americas. (2022) 5.
53. Fancourt, D, Steptoe, A, and Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. (2021) 8:141–9. doi: 10.1016/S2215-0366(20)30482-X
54. Gigantesco, A, Minardi, V, Contoli, B, and Masocco, M. Depressive symptoms among adults in 2018-2019 and during the 2020 COVID-19 pandemic in Italy. J Affect Disord. (2022) 309:1–8. doi: 10.1016/j.jad.2022.04.131
55. Goodwin, RD, Dierker, LC, Wu, M, Galea, S, Hoven, CW, and Weinberger, AH. Trends in US depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. (2022) 63:726–33. doi: 10.1016/j.amepre.2022.05.014
56. Hajek, A, Neumann-Bohme, S, Sabat, I, Torbica, A, Schreyogg, J, Barros, PP, et al. Depression and anxiety in later COVID-19 waves across Europe: new evidence from the European COvid survey (ECOS). Psychiatry Res. (2022) 317:114902. doi: 10.1016/j.psychres.2022.114902
57. Hajek, A, Sabat, I, Neumann-Böhme, S, Schreyögg, J, Barros, PP, Stargardt, T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the European COvid survey (ECOS). J Affect Disord. (2022) 299:517–24. doi: 10.1016/j.jad.2021.12.029
58. Hertz-Palmor, N, Moore, TM, Gothelf, D, DiDomenico, GE, Dekel, I, Greenberg, DM, et al. Association among income loss, financial strain and depressive symptoms during COVID-19: evidence from two longitudinal studies. J Affect Disord. (2021) 291:1–8. doi: 10.1016/j.jad.2021.04.054
59. Hou, WK, Lee, TMC, Liang, L, Li, TW, Liu, H, Tong, H, et al. Psychiatric symptoms and behavioral adjustment during the COVID-19 pandemic: evidence from two population-representative cohorts. Transl Psychiatry. (2021) 11:174. doi: 10.1038/s41398-021-01279-w
60. Jeong, H, Park, S, Kim, J, Oh, K, and Yim, HW. Mental health of Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey. Epidemiology and Health. (2022) 44:e2022042.
61. Kessler, RC, Ruhm, CJ, Puac-Polanco, V, Hwang, IH, Lee, S, Petukhova, MV, et al. Estimated prevalence of and factors associated with clinically significant anxiety and depression among US adults during the first year of the COVID-19 pandemic. JAMA Netw. Open. (2022) 5:E2217223.
62. Khaled, SM, Davis, V, Amro, I, Ali, AAM, Woodruff, PW, and Haddad, PM. Trends in prevalence of depression and anxiety symptoms and effects of sociodemographic variables before and after the first wave of COVID-19 in Qatar. J Affect Disord. (2022) 310:412–21. doi: 10.1016/j.jad.2022.04.019
63. König, H-H, Neumann-Böhme, S, Sabat, I, Schreyögg, J, Torbica, A, van Exel, J, et al. Health-related quality of life in seven european countries throughout the course of the covid-19 pandemic: Evidence from the european covid survey (ecos). Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation. (2023).
64. Kwong, ASF, Pearson, RM, Adams, MJ, Northstone, K, Tilling, K, Smith, D, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br J Psychiatry. (2021) 218:334–43. doi: 10.1192/bjp.2020.242
65. Lai, FTT, Chan, VKY, Li, TW, Li, X, Hobfoll, SE, Lee, TMC, et al. Disrupted daily routines mediate the socioeconomic gradient of depression amid public health crises: a repeated cross-sectional study. Aust N Z J Psychiatry. (2022) 56:1320–31. doi: 10.1177/00048674211051271
66. Lim, MH, Qualter, P, Thurston, L, Eres, R, Hennessey, A, Holt-Lunstad, J, et al. A global longitudinal study examining social restrictions severity on loneliness, social anxiety, and depression. Front Psych. (2022) 13:818030. doi: 10.3389/fpsyt.2022.818030
67. Lowe, C, Keown-Gerrard, J, Ng, CF, Gilbert, TH, and Ross, KM. COVID-19 pandemic mental health trajectories: patterns from a sample of Canadians primarily recruited from Alberta and Ontario. Can J Behav Sci. (2023) 55:113–29. doi: 10.1037/cbs0000313
68. Mangot-Sala, L, Smidt, N, and Liefbroer, AC. Changes in anxiety and depression symptoms during the covid-19 lockdown in the netherlands – The moderating role of pre-existing mental health, employment situation and alcohol consumption. Social Psychiatry and Psychiatric Epidemiology: The International Journal for Research in Social and Genetic Epidemiology and Mental Health Services. (2023).
69. Mauz, E, Walther, L, Junker, S, Kersjes, C, Damerow, S, Eicher, S, et al. Time trends in mental health indicators in Germany's adult population before and during the COVID-19 pandemic. Front Public Health. (2023) 11:1065938. doi: 10.3389/fpubh.2023.1065938
70. Min, J, Kwon, D, Lee, W, Kang, C, Park, C, Heo, S, et al. Individual and regional characteristics associated with changes in mental health before and during the COVID-19 pandemic in South Korea. Sci Rep. (2022) 12:14189. doi: 10.1038/s41598-022-18493-1
71. Moreno-Agostino, D, Fisher, HL, Hatch, SL, Morgan, C, Ploubidis, GB, and Das-Munshi, J. Generational, sex, and socioeconomic inequalities in mental and social wellbeing during the covid-19 pandemic: prospective longitudinal observational study of five Uk cohorts. Psychol Med. (2022) 53:6403–14. doi: 10.1017/S0033291722003348
72. Parsons, CE, Purves, KL, Skelton, M, Peel, AJ, Davies, MR, Rijsdijk, F, et al. Different trajectories of depression, anxiety and anhedonia symptoms in the first 12 months of the covid-19 pandemic in a uk longitudinal sample. Psychol. Med. (2022).
73. Petersen, J, Hettich, N, Baumkötter, R, Wild, PS, Pfeiffer, N, Münzel, T, et al. The burdens of poverty during the COVID-19 pandemic. Front Sociol. (2022) 7:7. doi: 10.3389/fsoc.2022.995318
74. Perez, MP, Fernandes, A, Couto, B, Ferreira, S, and Morgado, P. P.0817 sociodemographic and lifestyle predictors of mental health adaptability during COVID-19 compulsory confinement: a longitudinal study. Eur Neuropsychopharmacol. (2021) 53:S597. doi: 10.1016/j.euroneuro.2021.10.677
75. Probst-Hensch, N, Jeong, A, Keidel, D, Imboden, M, and Lovison, G. Depression trajectories during the COVID-19 pandemic in the high-quality health care setting of Switzerland: the COVCO-Basel cohort. Public Health. (2023) 217:65–73. doi: 10.1016/j.puhe.2023.01.010
76. Qi, Y, Lepe, A, Almansa, J, Ots, P, de Kroon, MLA, Vrooman, JC, et al. Increases in symptoms of depression and anxiety in adults during the initial phases of the COVID-19 pandemic are limited to those with less resources: results from the lifelines cohort study. J Psychiatr Res. (2022) 154:151–8. doi: 10.1016/j.jpsychires.2022.07.011
77. Ribeiro, F, Schröder, VE, Krüger, R, and Leist, AK. The evolution and social determinants of mental health during the first wave of the COVID-19 outbreak in Luxembourg. Psychiatry Res. (2021) 303:114090. doi: 10.1016/j.psychres.2021.114090
78. Riehm, KE, Holingue, C, Smail, EJ, Kapteyn, A, Bennett, D, Thrul, J, et al. Trajectories of mental distress among U.S. adults during the COVID-19 pandemic. Ann Behav Med. (2021) 55:93–102. doi: 10.1093/abm/kaaa126
79. Robinson, E, and Daly, M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: Longitudinal evidence from the Understanding America Study. Br. J. Health Psychol. (2021) 26:570–87.
80. Shuster, A, O'Brien, M, Luo, Y, Berner, LA, Perl, O, Heflin, M, et al. Emotional adaptation during a crisis: decline in anxiety and depression after the initial weeks of COVID-19 in the United States. Transl Psychiatry. (2021) 11:435. doi: 10.1038/s41398-021-01552-y
81. Tao, TJ, Liang, L, Liu, H, Hobfoll, SE, Hou, WK, and Bonanno, GA. The interrelations between psychological outcome trajectories and resource changes amid large-scale disasters: a growth mixture modeling analysis. Transl Psychiatry. (2023) 13:57. doi: 10.1038/s41398-023-02350-4
82. Twenge, JM, McAllister, C, and Joiner, TE. Anxiety and depressive symptoms in U.S. Census Bureau assessments of adults: trends from 2019 to fall 2020 across demographic groups. J Anxiety Disord. (2021) 83:102455. doi: 10.1016/j.janxdis.2021.102455
83. van der Velden, PG, Contino, C, Das, M, van Loon, P, and Bosmans, MWG. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic a prospective national study on prevalence and risk factors. J Affect Disord. (2020) 277:540–8. doi: 10.1016/j.jad.2020.08.026
84. van der Velden, PG, Marchand, M, Das, M, Muffels, R, and Bosmans, M. The prevalence, incidence, and risk factors of mental health problems and mental health service use before and 9 months after the COVID-19 outbreak among the general Dutch population. A 3-wave prospective study. PLoS ONE. (2022) 17:e0276834.
85. Yamamoto, T, Uchiumi, C, Suzuki, N, Sugaya, N, Murillo-Rodriguez, E, Machado, S, et al. Mental health and social isolation under repeated mild lockdowns in Japan. Sci. Rep. (2022) 12.
86. Zhao, SZ, Wong, JYH, Luk, TT, Wai, AKC, Lam, TH, and Wang, MP. Mental health crisis under COVID-19 pandemic in Hong Kong, China. Int J Infect Dis. (2020) 100:431–3. doi: 10.1016/j.ijid.2020.09.030
87. Zhou, Y, Macgeorge, EL, and Myrick, JG. Mental health and its predictors during the early months of the covid-19 pandemic experience in the United States. Int J Environ Res Public Health. (2020) 17:1–19. doi: 10.3390/ijerph17176315
88. Staples, LG, Dear, BF, Gandy, M, Fogliati, V, Fogliati, R, Karin, E, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: the PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. (2019) 56:13–8. doi: 10.1016/j.genhosppsych.2018.11.003
89. Barakat, C, and Konstantinidis, T. A review of the relationship between socioeconomic status change and health. Int J Environ Res Public Health. (2023) 20:6249. doi: 10.3390/ijerph20136249
90. Ahnquist, J, and Wamala, SP. Economic hardships in adulthood and mental health in Sweden. The Swedish National Public Health Survey 2009. BMC Public Health. (2011) 11:788. doi: 10.1186/1471-2458-11-788
91. Marguilho, M, and Nobre, A. Effects of the COVID-19 pandemic on mental health – what do we know so far? Eur Psychiatry. (2021) 64:S312. doi: 10.1192/j.eurpsy.2021.839
92. Mauz, E, Eicher, S, Peitz, D, Junker, S, Holling, H, and Thom, J. Mental health of the adult population in Germany during the COVID-19 pandemic. Rapid review. J Health Monit. (2021) 6:2–63. doi: 10.25646/9537
93. Di Fazio, N, Morena, D, Delogu, G, Volonnino, G, Manetti, F, Padovano, M, et al. Mental health consequences of COVID-19 pandemic period in the European population: an institutional challenge. Int J Environ Res Public Health. (2022) 19:9347. doi: 10.3390/ijerph19159347
94. Liu, S, Haucke, MN, Heinzel, S, and Heinz, A. Long-term impact of economic downturn and loneliness on psychological distress: triple crises of covid-19 pandemic. J Clin Med. (2021) 10:4596. doi: 10.3390/jcm10194596
95. Blume, M, Rattay, P, Hoffmann, S, Spallek, J, Sander, L, Herr, R, et al. Health inequalities in children and adolescents: a scoping review of the mediating and moderating effects of family characteristics. Int J Environ Res Public Health. (2021) 18:7739. doi: 10.3390/ijerph18157739
96. Harper, S, King, NB, and Young, ME. Impact of selective evidence presentation on judgments of health inequality trends: an experimental study. PLoS One. (2013) 8:e63362. doi: 10.1371/journal.pone.0063362
Keywords: mental health, depressive symptoms, anxiety symptoms, COVID-19 pandemic, socioeconomic inequalities
Citation: Herrmann K, Beese F, Wollgast L, Mauz E, Kersjes C, Hoebel J and Wachtler B (2024) Temporal dynamics of socioeconomic inequalities in depressive and anxiety symptoms during the COVID-19 pandemic: a scoping review. Front. Public Health. 12:1397392. doi: 10.3389/fpubh.2024.1397392
Received: 07 March 2024; Accepted: 19 June 2024;
Published: 03 July 2024.
Edited by:
S. M. Yasir Arafat, Biomedical Research Foundation, BangladeshReviewed by:
Birute Strukcinskiene, Klaipėda University, LithuaniaCopyright © 2024 Herrmann, Beese, Wollgast, Mauz, Kersjes, Hoebel and Wachtler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin Wachtler, d2FjaHRsZXJiQHJraS5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.