- 1Palliative Care Unit, Azienda USL – IRCCS di Reggio Emilia, Reggio Emilia, Italy
- 2Department of Medicine and Surgery, University of Parma, Parma, Italy
- 3Local Health Unit of Modena, Modena, Italy
Background: To understand palliative care needs and their changes perceived by health professionals (HPs) of the Infectious Diseases Unit who participated in palliative care (PC) intensive training during the pandemic and behind/during the pandemic and one year after the outbreak.
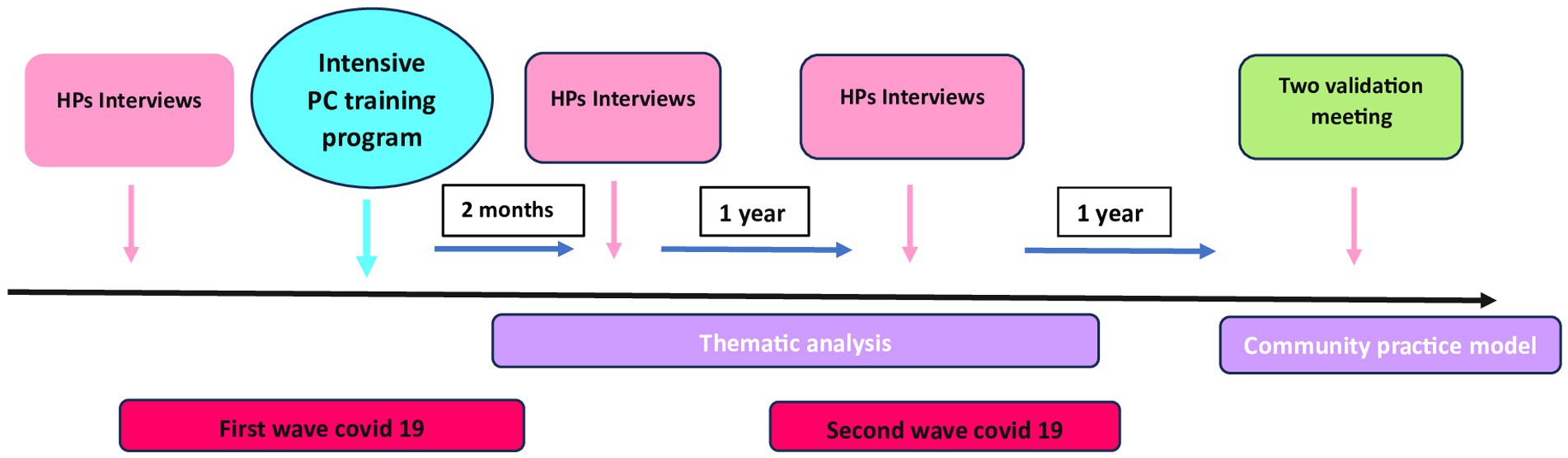
Methods: A longitudinal qualitative study. Thematic analysis and meaning shift were two months after training to one year. This specific thematic approach enabled the researchers to fully understand the experiences of the HPs after they participated in the intensive PC training program during the pandemic. Participant validation meeting with the ward’s staff one year after the end of the course was performed. The two last validation meetings were used as a triangulation source to plan the new education projects.
Results: From March 9 to 28, 2020, the Palliative Care Services (PCS) developed intensive experiential training. Thirty-one HPs of the Infectious Diseases Unit (physicians and nurses) who were facing the COVID-19 emergency participated in the training. We conducted eight semi-structured interviews with HPs who participated in intensive training during the first wave of the pandemic (T0), two months (T1) after training and after one year (T2), during the second wave. Two validation meetings were performed as suggested by the best practices in medical education. Twenty-two infectious disease staff members participated, 8 physicians and 14 nurses. Our data show a meaning shift on five overarching themes (defined within the sub-themes): (1) Recognizing patients’ palliative care needs; (2) Responses to palliative care needs; (3) Increasing attention to intervention and care choices; (4) The suffering of health professionals; (5) Training evaluations and future expectations. At the end of Pandemic period, new training needs and acquisition have emerged. Palliative care needs changed over time: the COVID-19 themes are now far from their perception, and somehow the skills acquired during the intensive training are less present.
Conclusion: The pandemic led to a rapid acquisition of competencies and changes in the professionals’ behaviors, maintenance of professionals’ knowledge and competencies at two months and one year. COVID has improved relationships and increased interactions with the infectious world but that it has not been enough. The integration between PC and Infectious world needs models of integration to implement.
Introduction
The role and response of palliative care services (PCS) around the world during the pandemic were exceptional, especially in the hospital setting (1–4). Moreover, in emergency departments (EDs), PCS largely contributed to physical/spiritual/social symptom control, staff support and decision-making for COVID-19 patients (5–9).
This substantial effort was realized by reorganizing PCS to better respond to the increasing patient and hospital needs (10). Flexibility and adaptability by PCS have shown key characteristics to counteract the pandemic (6, 8). Even during the pandemic, PCS exercised their advanced skills on other healthcare professionals (HPs), according to the model from the 2nd level (specialist) to the 1st level (non-specialist) professionals (11). Educational activities have the goal of improving both the quality of patient care in their specific ward and the medical education that novice professionals receive (12).
Training on basic palliative care (PC) competencies and the knowledge of other specialists was also essential to expand the health care system to provide PC; on the other hand, adapting PC competencies, preferably with short and focused teaching or tutoring, was important due the emerging new scenarios, including patients’ use of communication devices, the limited time available for the delivery of care and managing death inside the hospital and relationships with family members outside of the hospital (5, 6, 13–15).
The published literature on models of integration between palliative and infectious care is non-existent; there are several calls for CP for HIV (16–19) patients in light of the great palliative care needs but no model already implemented (20). The literature between these two worlds focuses very much on the appropriateness of prescribing antibiotics in certain special situations such as the advanced cancer patient (21) or the patient with advanced dementia (22–25) or in infectious control in PC setting (22, 23). PC is underrepresented in global guidelines for responding to infectious disease outbreaks (24). Most of the literature has flourished in the last years due to the COVID pandemic.
Our PCS is a specialized hospital-based unit with no dedicated beds in a Comprehensive Cancer Center in Northern Italy. The PCS was established in 2013, and its goals included developing and implementing training programs to improve health professionals’ PC competencies (25, 26).
In March 2020, during the first wave of the pandemic, we joined a strong collaboration with the Infectious Disease Unit, a front-line department, to implement protocols for symptom control (especially dyspnea, delirium and end of life), support staff in delivering bad news and advance care planning, and control emotional distress and communication with families through intensive training (15). Following the PCS intervention, we explored the experience of HPs in PC. Our study suggests that a PCS can help in managing symptoms and answering the new needs emerging due to the COVID-19 outbreak: both supporting staff and having an educational role in training non specialist HPs; dealing with atypical relationship of care and giving difficult news to isolated patients and to their family members; guaranteeing personalized care (15).
In this article, we focused on PC needs and their changes perceived by HPs before the pandemic and after intensive training. We qualitatively evaluated the impact of the training itself and the maintenance of professionals’ knowledge and competences at two months and one year. We used individual, semistructured interviews to get a deeper understanding of the professional’s experience, while the two validation meetings were used to confirm and/or challenge our findings, adding a group (entire ward’s staff of infectious disease) perspective to what we previously found and to assess the educational needs to support future training. Knowledge of PC needs and their changes could be an element to implement a new integration model between PC and the infectious world.
To the best of our knowledge, this is the first longitudinal qualitative study on meaning shifts in PC needs and competencies before, during and after COVID-19. We believe that this longitudinal research could provide new insight into PC delivery in emergency situations and beyond.
Materials and methods
Study design and participants
We developed a satellite, qualitative study to add detail to what was retrieved in a first case study published in 2020. From March 9 to 28, 2020, the PCS developed intensive experiential training with specific component: supervision of 18 daily briefings with nine Infectious Diseases Unit physicians; 48 PC bedside consultations together with the referring physician; two brief (30–40 min) lectures on PC topics, with a PC expert answering the Infectious Diseases Unit physicians’ and nurses’ questions; a booklet addressing the assessment and treatment of PC needs based on issues emerging during the first week of the intervention and elaborated for use by professionals (15). Thirty-one HPs of the Infectious Diseases Unit (physicians and nurses) participated in the training. The intervention was applied to all staff of the Infectious Diseases Unit who were facing the COVID-19 emergency. In 2020 and 2021, these HPs visited approximately 1,022 and 1,401 COVID cases, respectively. No one refused the intervention.
A longitudinal qualitative research design using semi-structured interviews followed by thematic analysis (27–29) was utilized. This specific thematic approach enabled the researchers to fully understand the experiences of the HPs after they participated in the intensive PC training program. Study procedures and reporting followed the Consolidated Criteria for Reporting Qualitative Research (CoreQ) guidelines (30).
Figure 1 describes the timeline of the whole intervention along with its evaluation.
Data collection
Eight HPs (four physicians and four nurses), accounting for 25% of the professionals who participated in the intensive training realized in 2020 (15), were recruited by researchers drawing numbers. No one refused the invitation to participate in the interviews and no HPs were lost to follow up. Eight semi-structured interviews of the same professionals were performed during the first wave, two months (June 2020) after training (T1), and during the second wave (T2), one year (May/June 2021) after training (also referred as “participant validation”) (31). The last two interviews did not yield new data but served to confirm the analysis (data saturation).
The individual interviews were structured to follow a topic guide (the interested reader can find it in Supplementary material online) to explore the PC issues that the professionals encountered in clinical practice before the COVID-19 pandemic and during the pandemic, with a specific focus on the training that was carried out. All interviews were conducted by a researcher (GA) experienced in qualitative research methods (32). Written informed consent was obtained from all the participants. The date, time and site of the interview were agreed upon by the researcher and HPs. Explicit permission was given for the interview to be audio-recorded. The interviewer did not meet or know the participants before the study.
One year after T2, we presented the results of our analysis to the ward’s staff through two “validation meetings.” These validation meetings were focus groups opened to the entire ward’s staff, one year after T2, in order to plan new, future education projects targeting the Infectious Disease Unit.
The meetings were agreed upon with the formal leadership of the ward. We scheduled two editions of each meeting, to maximize participation.
Each meeting had two facilitators, co-authors of the previous paper, and one observer. Twenty-two HPs participated, 8 physicians and 14 nurses.
Our effort was aimed at gaining a deeper understanding of the perception of their current educational needs as a “community of practice” (as described in the “discussion” section), and not only at an individual level (see Figure 1).
Data analysis
The results of the interviews were analyzed through thematic analysis to identify any possible changes in the meanings attributed to that phenomenon from T1 to T2 (27, 28). The same researcher who conducted the interviews conducted the verbatim transcription. On average, each interview lasted for 25 min. The interviewer did not return the transcripts to the participants. Each transcript was labeled independently by two researchers (SA; ST). Through an iterative process during the analysis, the researchers verified that, from time to time, the main sub-themes and the themes of the content that comprised them were consistent with the transcribed interviews and identified significant sentences that condensed and represented the meanings of the identified sub-themes and themes. Then, the labels were combined to identify the central themes and sub-themes. The two researchers compared their analyses and proposed a shared naming. The themes were further reviewed by G.A. to ensure accuracy. The list of identified themes was discussed and refined by the entire team of researchers to ensure internal consistency. The central themes were accurately described to identify their meanings and the change in their meanings over time (29, 32, 33).
All the identified final themes were saturated, with the last interviews not yielding new insight or new data but serving to confirm the analysis.
The validation meetings were performed in according with the best practices in medical educational (as described in Kern, Thomas and Hughes, having a collective, formative evaluation of the group perception of the previous training is helpful in planning a better future training’s edition) (34). In the meetings we presented our results and gathered their perception of their current educational needs. To do so, we asked them to describe clinical cases where they detected palliative care needs.
These data were then compared with the previous results in search for any significant shift.
This study received ethical approval from the Ethics Committee AVEN of the Azienda USL-IRCCS Reggio Emilia in May 2020 (n° 2020/0047973).
Results
The participants’ mean age was 46 years, their time since graduation ranged from one month to 31 years, and the median years of work experience were 21 years (see Supplementary material online).
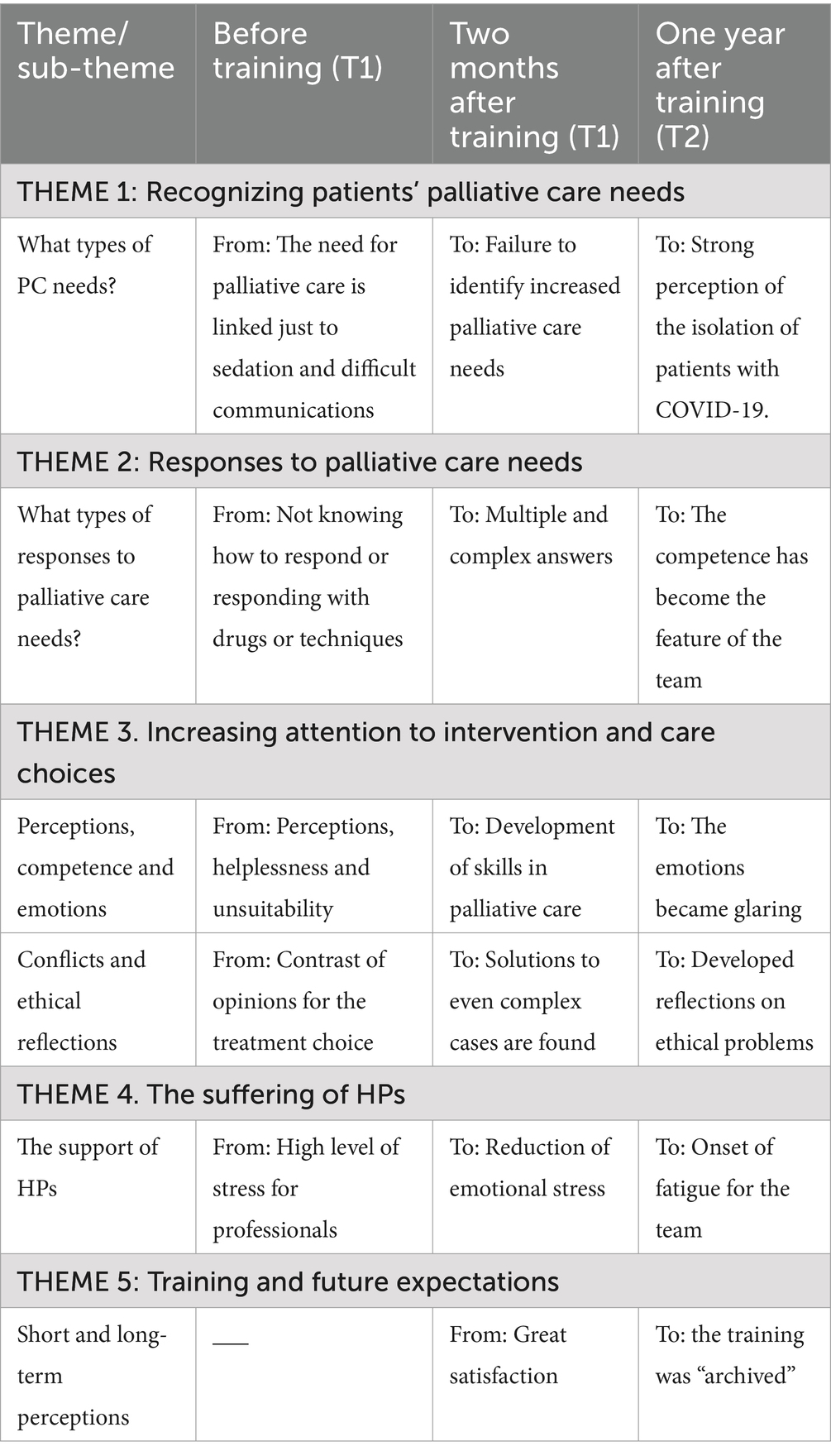
We present the results in two sections: in the first section, we describe the themes identified in the analysis of the longitudinal interviews, at T1 and T2 (see Table 1). In the second section, we describe the feedback on our analysis and the new educational needs declared by the ward’s staff 12 months after T2, at the beginning of a new educational project.
We decided to present results in such form, as the trainee needs and attitudes changed significantly over time, and the group feedback meetings from the staff were upmost informative and helped us to developing a plausible explanation of the perceived, relatively low retention of the training contents.
Interviews thematic analysis
The analysis of the interviews led us to identify five overarching themes (Table 2) (1): Recognizing patients’ PC needs (2); Responses to PC needs (3); Increasing attention to intervention and care choices (4); The suffering of HPs; and (5) Training evaluations and future expectations. These themes emerged with different meanings (defined within the subthemes) in relation to pretraining and two months and one year post-training.
Theme 1. Recognizing patients’ palliative care needs
In this theme, we denominated the meaning shift changing from “The need for palliative care is linked just to sedation and difficult communications” to “failure to identify increased palliative care needs” two months after training, to “strong perception of the isolation of patients with COVID-19” one year after training. We identified a subtheme denominated “What types of PC needs?.” Before training, the HPs identified various types of palliative care needs and the need to receive basic relevant information on PC. For example, the HPs identified palliative sedation, difficulty communicating with patients and their families, symptoms that are difficult to treat, and managing patients’ psychological problems.
“The difficulty communicating with patients was very lacking…” (T1 Cod. 7.24-Physician)
“They needed more intensive care and there was a need to set up a sedative therapy quickly…” (T1 Cod. 1.14—Physician).
After training, the HPs identified the isolation of patients as PC need:
“…one problem is patient isolation…has not been resolved and no major interventions have been made” (T2 Cod. 2.23—Nurse).
Theme 2. Responses to palliative care needs
In this theme, we identified a sub-themes called: “What types of responses to PC needs?.” As a result of the training, the meanings shifted from what we denominated “Not Knowing how to respond or responding with drug or techniques” to “multiple and complex answers” to “the competence has become the feature of the team.” Before the training, the HPs primarily emphasized the lack of a specific approach to PC needs. They recognized responding with only pharmacological interventions or technical interventions for acute symptoms. They often employed psychologists to address other dimensions of quality of life.
“more than with elastomer or long-term therapies, we dispensed medications as needed…” (T1 Cod. 1.18—Physician)
“…empirically, we talk to family members, we try to understand if they are aware” (T1 Cod. 7.24—Physician).
After training, the HPs recognized that they responded more effectively and comprehensively to PC needs:
“…we have improved dyspnea management…pain management…generalized pain related to the lack…you pass me the term…of life” (T1 Cod. 3.24—Nurse);
“…we have acquired expertise in the management of delirium and agitation” (T1 Cod. 5.4—Nurse).
One year after training, the acquired skills were assets for the team, and the situation was more manageable: “we were already tested, organized and we knew what it was all about…” (T2 Cod. 8.17—Nurse). Nevertheless, the problem of identifying psychosocial and spiritual needs remained in both the pre- and post-training interviews.
Theme 3. Increasing attention to intervention and care choices
In this theme, two sub-themes were identified (1): perceptions, competence and emotions and (2) conflicts and ethical reflections.
Perceptions, competence and emotions
The participants shifted from what we called “Perceptions, helplessness and unsuitability” to the “Development of skills in palliative care” to “the emotions become glaring.” Before training, the HPs perceived a great sense of inadequacy and discomfort, mainly due to their lack of knowledge of the new situation. Furthermore, they realized that their interventions were not very effective.
“It was considerably uneasy for us as professionals because we could not…how to say…to manage the…the pain of that moment because it was completely new for us” (T1 Cod 3.20—Nurse).
After training, the HPs recognize that they have developed skills in symptom management and acquired the importance of multidisciplinary work.
“…the experience of COVID-19 has taught that this pathology must be managed in a multidisciplinary way” (T1 Cod 7.20—Physician).
The HPs lead the patients’ pathways with other departments and developed “awareness that older adult patients, with dementia, die with dignity.” (T1 Cod. 7.13—Physician).
After one year, despite the skills acquired, the emotions of the HPs become evident for “not seeing a way out soon” (T2 Cod. 1.24—Physician).
The HPs are tired of always managing and only managing this pathology and “…often you felt helpless because you could not find any positive feedback.” (T2 Cod. 8.30—Nurse).
Conflicts and ethical reflections
The participants shifted from what we called “Contrast of opinions for the treatment choice” to “Solutions to even complex cases are found” to “Developed reflections on ethical problems.” Before the training, palliative sedation was a cause of conflict among the nurses and physicians. The HPs had difficulty managing ventilated patients and patients who asked to be sedated.
“…doctor, this patient is too agitated and if we put C-PAP, she will not tolerate it! The doctor replied: ‘Let us try without sedation’. After a few hours, the patient had torn C-PAP and bladder catheter…” (T2 Cod. 2.20—Nurse)
“I remember a patient…who said: ‘I absolutely do not want to feel difficulty of breathing, if it goes badly, fall asleep, fall asleep’” (T1 Cod. 1.16—Physician).
After training, the HPs described the capacity to manage complex cases and greater knowledge of the indications for palliative sedation. The participants discovered the importance of end-of-life (EoL) treatments, as higher sensitivity and attention were given to patients.
“An old woman began to breathe poorly…she was beginning to be delirious…making phone calls her daughter saying ‘They keep me prisoner’…we used elastomer and she said ‘I’m better, I breathe better.’ She died, but she died quietly” (T1 Cod. 1.27—Physician).
Over time, after training, the HPs begin to ask ethical questions, and they were more critical of decision-making. The HPs began to investigate ethical issues such as the need for some invasive treatment, respect for the dignity of the person and not ventilating patients. The HPs claimed:
“[In the second wave] the situation seemed much clearer to us. In the first wave age was a dramatic factor and there were many discussions…” (T2 Cod. 1.12—Physician)
“We have discussed several times about the use of the nasogastric tube during ventilation… also for an invasiveness and dignity of the body” (T2 Cod. 2.16–17—Nurse).
Theme 4. The suffering of HPs
Another theme emerging from interviews regarded the difficulty of the HPs in sustaining, over time, the emotional charge of daily contact with patients who have COVID-19 and their families. The sub-theme is represented by the support to HPs. The participants shifted from what we called “High level of stress for professionals” to “Reduction of emotional stress” to “Onset of fatigue for the team.”
Before the training, there was evident suffering on the part of the professionals, especially nurses, due to the reduced use of the appropriate drugs for sedation.
“I suffered a lot because if you have the opportunity, I did not understand why not being able to use them [the drugs] and not being able to give the patient less suffering” (T1 Cod. 3.19—Nurse).
Following training, the HPs recognized, above all, the need to receive psychological support themselves to face complex COVID-19 and EoL situations. The HPs recognized the training as an occasion for discussion and sharing of their most complex problems: “In my opinion, the shared decision-making helped me a lot, it personally helped me a lot.” (T1 Cod. 1.22—Physician).
Furthermore, the help of the PCS in reducing the patients’ suffering “…reduced the medical and nursing staff’s suffering who were the ones most in contact… (T1 Cod. 1.25—Physician).
Over time, the HPs’ fatigue developed. The participants were tired of managing only this disease: “It lasted little over two months and then we started again…we are worn out by a situation that has destabilized us.” (T2 Cod. 8.10–20—Nurse); “It’s quite frustrating, to see new cases again…” (T2 Cod. 1.24—Physician).
Theme 5. Training and future expectations
In this theme, the sub-theme identified has been called “short and long-term perceptions.” The participants shifted from what we called “Great satisfaction” to “the training was ‘archived’” (T2 Cod. 4.16—Physician). The HPs recognized that they have acquired some skills to deal with the needs of PC, and they appreciated the method based on clinical practice. The collaboration with PCS has brought greater well-being for patients and also HPs.
“For me it was useful…it dissolved my doubts about sedation, being unable to understand why the physicians are so reluctant, I had confirmation…” (T1 Cod. 2.30—Nurse)
“…this is new, very, very useful…” (T1 Cod. 3.33—Nurse) “A huge thank you” (T1 Cod. 1.35—Physician).
The HPs’ perceptions were that the second wave of COVID-19 “…canceled everything that was done before because getting back into the COVID routine was difficult” (T2 Cod. 4.15—Physician) and “In my opinion it was archived” (T2 Cod. 4.16—Physician). After one year of training, they feel the need for continuous training that could promote a change in their mentality with respect to palliative medicine.
“We abandoned it too quickly…From too much to zero; there was a challenging gap” (T2 Cod. 7.33—Physician)
“…for some situations every now and then, some refresh is useful…” (T2 Cod. 1.10—Physician).
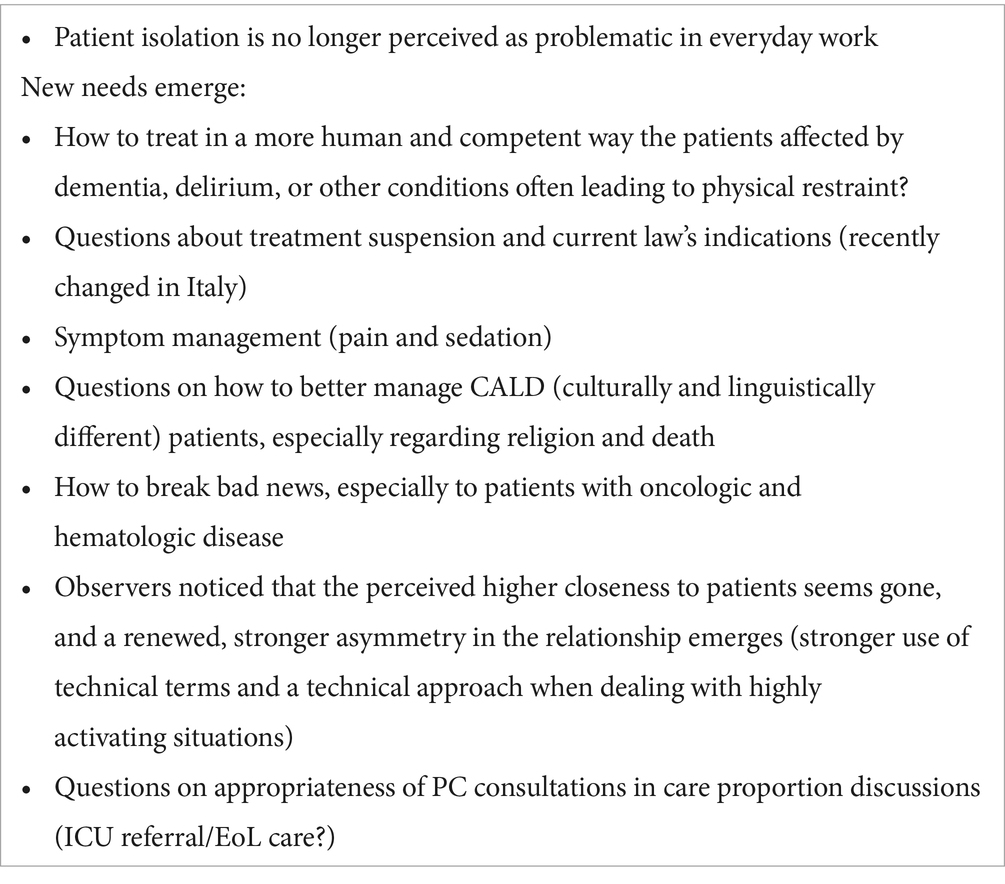
Ward’s staff group feedback at 12 months from T2
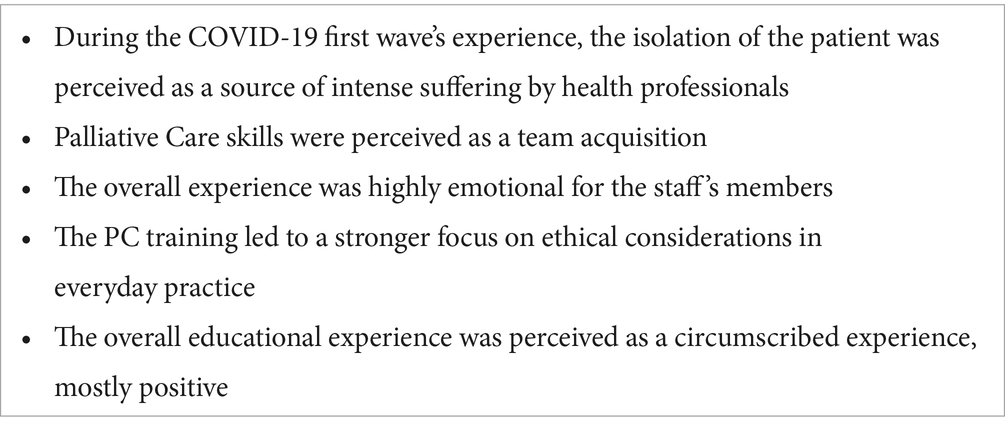
We inquired the ward’s staff feedback in two validation meetings: in the first meeting we presented the results of previous interviews and study (15) (Table 2) and asked for their current perception of these results and how much they might have changed over time.
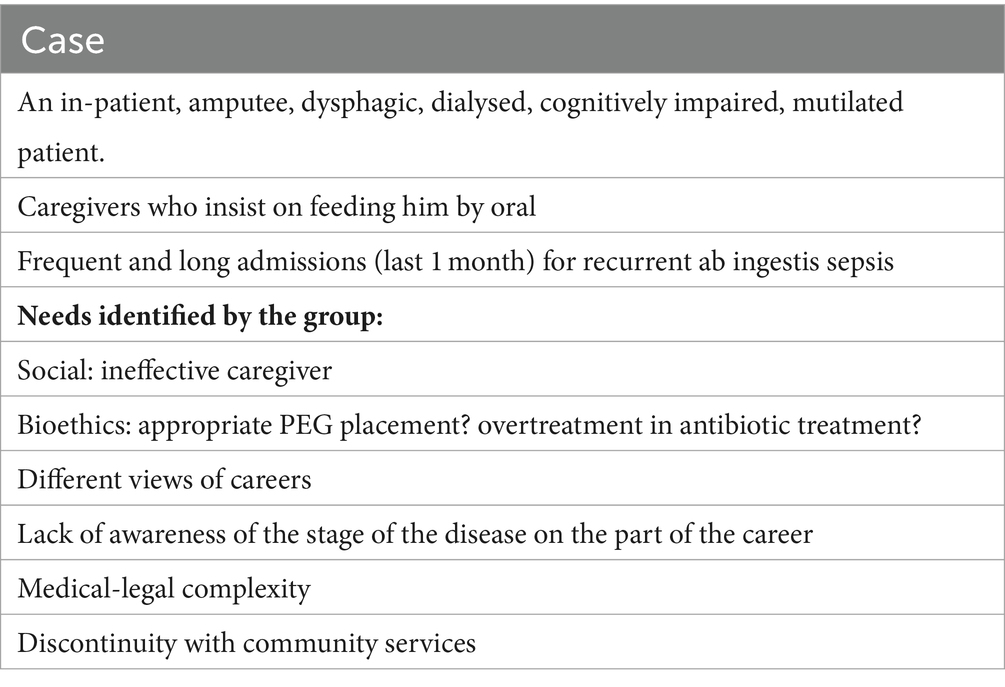
In the second meeting we asked them to define Palliative Care from their perspective and to present real life situations and cases where they faced palliative care needs as a ward (Table 3).
When asked to define their perception of palliative care needs, they focused mainly on treatment of pain (nine staff members), and psychological end of life needs (four staff members), and most of the participants referred to palliative care as EoL care (12 of them).
Table 4 summarizes the perceived current needs at T2 + 12 months, (compared to Table 2, reporting the needs at T1 and T2).
As you can see, palliative care needs changed back significantly over time: the COVID-19 themes are now far from their perception, and somehow the skills acquired during the intensive training are less present.
Discussion
Our findings describe the experience of the HPs of the Infectious Diseases Unit after intensive training in PC; the study explored the participants’ learning needs prior to the pandemic, during the first wave and one year later. We explored their perceptions, in terms of educational needs and feedback 12 months after T2, at the beginning of a new educational project (Table 4), and their palliative care perception was in part back to a EoL care and symptoms management perception.
Few studies have reported whether educational interventions have longitudinal impacts on behaviors and results (35). A longitudinal evaluation was useful, for example, to underline PC competences.
Although PCS has implemented a short training, HPs expressed great satisfaction with the method based on clinical practice with quick responses. The HPs recognized the training as an occasion for the discussion and sharing of the most complex problems. The shared search for common solutions became a support strategy, and the help of the PCS unit in reducing the patients’ suffering also led to a reduction in the staff’s suffering (36).
As suggested by other authors (37), the presence of a mentor meant that these questions and insights could be explored and clarified quickly, thus leading to a faster learning process (38, 39).
Once again, this confirms the supporting role of the PCS that stimulates reflection on complex cases, but also an important role in simultaneous care.
In support of this important role, it should be emphasized that one year after the training, it emerged that the professionals have seen the training archived too quickly. Having lost the continuous and lasting comparison over time has brought out glaring emotions and fatigue for the team. Some physicians’ competences seem to decrease, and some clinical confidences increase (40).
Moreover, as in other published experiences (26, 41, 42), the participants experienced an impact of the team training program on interprofessional collaboration in the ward and suggested that team-based learning supports the transferability of knowledge to clinical practice and the need for continuing CP training.
The main changes analyzed in this study such as patient isolation, staff support, maintenance of basic CP skills and ability to recognize complexity and ethical issues are the subject of a new training program for HPs, initiated by the two meetings at T2 + 12 months. It’s important to notice that this perception seems to be somehow lost over time, as well as training effect.
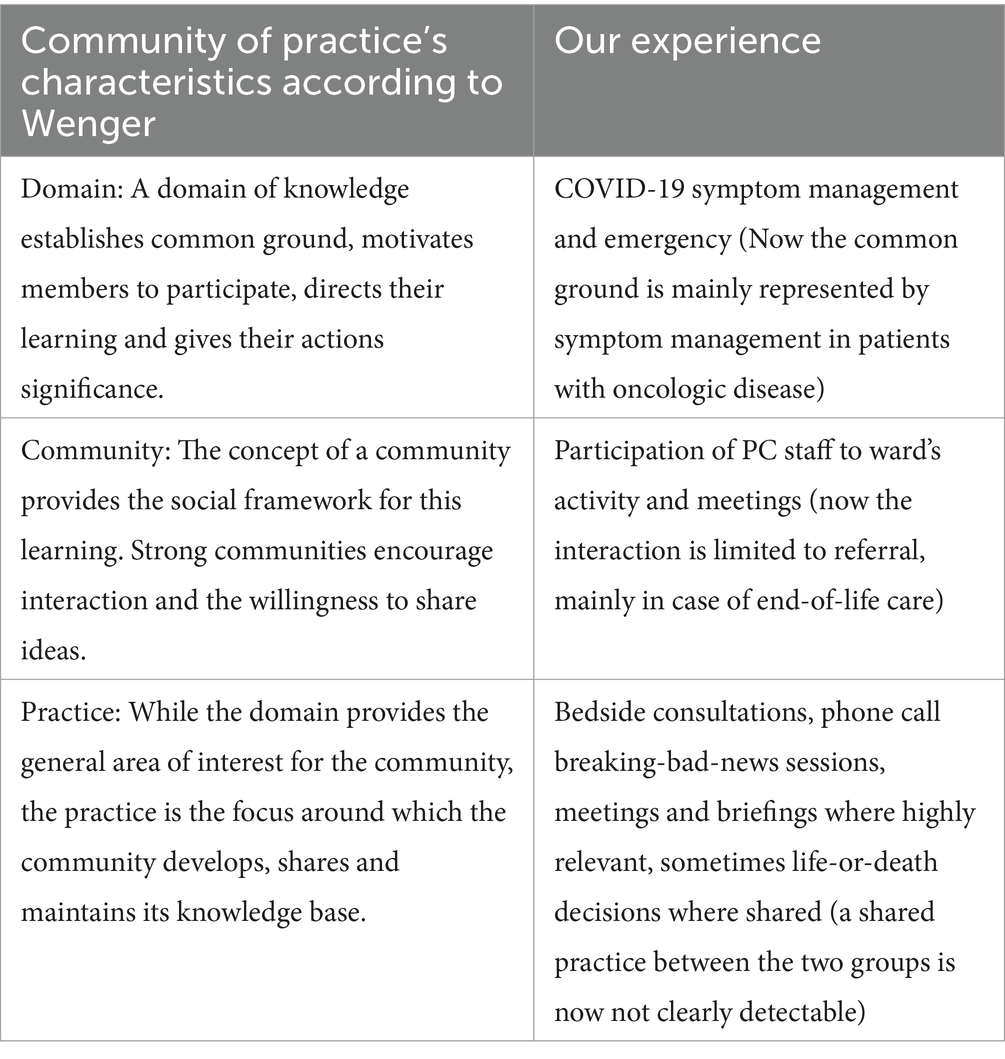
While many explanations are possible, we’d like to highlight some considerations in terms of “community of practice.” J. Lave and E. Wenger describe learning as a mainly social process, “situated” in the participation of a social context. A community of practice is “group of people who “share a concern or a passion for something they do and learn how to do it better as they interact regularly,” and have some structural characteristics (see Table 5) (43).
We believe that the intense COVID-19 experience led to the provisional creation of a real “community of practitioners,” where PC professionals were perceived as part of the same social group as the infectious disease ward’s staff.
We can find many possible explanations for why this phenomenon faded, at least partially. According to Wenger’s theorization, one possible explanation might be: the identity of the infectious disease ward’s staff dramatically changed, but is now back to an “older version,” as COVID-19 has a significantly smaller social impact. In 2020, when they were living the new identity of professionals facing an unprecedented social danger, this new identity facilitated the creation of a new community of practice.
While the relationship between the two Units is still good and well-functioning, it’s not possible to distinguish the same characteristics of a shared community of practitioners (see Table 5).
Probably, the local, temporary change of identity did not match an equivalent change of identity at a more global level (i.e., the infectious disease staff worldwide did not change their attitude toward PC as a group) and the specific needs of that time catalyzed a quick change, that wasn’t sustained by the same needs over time. From 2020 to 2022, the initial consultations carried out by the PCS have decreased. Especially way, in 2020, the PCS performed 63 initial consultations, while in 2022 performed 19 initial consultations.
Our experience shows that COVID has improved relationships and increased interactions with the infectious world but that it has not been enough; as in all educational experiences, continuous supervision of needs, monitoring and evaluation over time is necessary. The needs of patients admitted to these wards are multiple and infectious specialist clinicians perceived themselves unable to respond to them. Moreover, the data indicated that PC education may need to be tailored to meet the needs of different medical specialties (42) so all HPs can provide primary palliative care (6).
Our model, consisting of a cycle of assessment of educational needs and training, suggested an effective way to assess the real retention of interest, skills and knowledge in PC in an infectious disease ward after COVID-19. In such an innovative and uncertain field, the iterative evaluation of educational needs might effectively support the training of HPs, and help PCS maintain flexibility and adaptability mentoring approach without taking for granted the acquisition of skills. Furthermore, analyzing how the needs of the ward’s staff change over time will allow the PCS to reorganize itself to create the conditions for more effective and long-lasting collaborations with infectious disease word.
Strengths and limitations
As typical in qualitative research, these data can help researchers and decision-makers generate hypotheses for those who face similar challenges but are not strongly generalisable in contexts different from ours.
Our study described an experience of a single institute. The number of interviews was small but sufficient to have a saturation of the results and not have new themes to explore. Another limitation of our study was the potential recall bias and possible selection bias in the participants. However, at the same time, the longitudinal characteristic and the analysis with different methodologies may have reduced these limits.
The results provide an in-depth understanding of HPs’ experiences with the implementation of a longitudinal team training program that may also offer relevant knowledge for other similar health-care settings.
Conclusion
Palliative care is a complex and difficult discipline to be learned. The pandemic led to a rapid acquisition of competences and changes in the professionals’ behaviors.
PC professionals should maintain a mentoring approach over time and tailor training to the changing needs of HPs.
Specific models of integration between palliative care and infectious diseases are needed, to be tailored to the specific needs of these patients, which are not limited to COVID Pandemic moments.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Ethics statement
The studies involving humans were approved by the Ethics Committee AVEN of the Azienda USL-IRCCS Reggio Emilia in May 2020 (n° 2020/0047973). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SA: Conceptualization, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing, Data curation, Supervision. GA: Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. GM: Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. ST: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing, Supervision.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to pay tribute to all the HPs of the Infectious Disease Unit who gave their time to participate in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1393770/full#supplementary-material
References
1. Chidiac, C, Feuer, D, Naismith, J, Flatley, M, and Preston, N. Emergency palliative care planning and support in a COVID-19 pandemic. J Palliat Med. (2020) 23:752–3. doi: 10.1089/jpm.2020.0195
2. Etkind, SN, Bone, AE, Lovell, N, Cripps, RL, Harding, R, Higginson, IJ, et al. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. J Pain Symptom Manag. (2020) 60:e31–40. doi: 10.1016/j.jpainsymman.2020.03.029
3. Powell, RA, Schwartz, L, Nouvet, E, Sutton, B, Petrova, M, Marston, J, et al. Palliative care in humanitarian crises: always something to offer. Lancet. (2017) 389:1498–9. doi: 10.1016/S0140-6736(17)30978-9
4. Xu, Y, Zhang, LK, Smeltz, RL, and Cohen, SE. A vital layer of support: one safety net hospital’s palliative care response to the pandemic. J Palliat Med. (2021) 24:1474–80. doi: 10.1089/jpm.2020.0571
5. Aaronson, EL, Daubman, BR, Petrillo, L, Bowman, J, Ouchi, K, Gips, A, et al. Emerging palliative care innovations in the ED: a qualitative analysis of programmatic elements during the COVID-19 pandemic. J Pain Symptom Manag. (2021) 62:117–24. doi: 10.1016/j.jpainsymman.2020.10.035
6. Blinderman, CD, Adelman, R, Kumaraiah, D, Pan, CX, Palathra, BC, Kaley, K, et al. A comprehensive approach to palliative care during the coronavirus pandemic. J Palliat Med. (2021) 24:1017–22. doi: 10.1089/jpm.2020.0481
7. Fadul, N, Elsayem, AF, and Bruera, E. Integration of palliative care into COVID-19 pandemic planning. BMJ Support Palliat Care. (2021) 11:40–4. doi: 10.1136/bmjspcare-2020-002364
8. Gips, A, Daubman, BR, Petrillo, LA, Bowman, J, Ouchi, K, Traeger, L, et al. Palliative care in the emergency department: a qualitative study exploring barriers, facilitators, desired clinician qualities, and future directions. Palliat Support Care. (2022) 20:363–8. doi: 10.1017/S1478951521001012
9. Lee, J, Abrukin, L, Flores, S, Gavin, N, Romney, ML, Blinderman, CD, et al. Early intervention of palliative care in the emergency department during the COVID-19 pandemic. JAMA Intern Med. (2020) 180:1252–4. doi: 10.1001/jamainternmed.2020.2713
10. Apoeso, O, Kuwata, C, Goldhirsch, SL, Piracha, N, Reyes-Arnaldy, A, De Leon, J, et al. Creating a colocation unit for end-of-life care during a pandemic. J Palliat Med. (2021) 24:574–9. doi: 10.1089/jpm.2020.0502
11. Quill, TE, and Abernethy, AP. Generalist plus specialist palliative care--creating a more sustainable model. N Engl J Med. (2013) 368:1173–5. doi: 10.1056/NEJMp1215620
12. Gelfman, LP, Morrison, RS, Moreno, J, and Chai, E. Palliative care as essential to a hospital system’s pandemic preparedness planning: how to get ready for the next wave. J Palliat Med. (2021) 24:656–8. doi: 10.1089/jpm.2020.0670
13. Glass, M, Rana, S, Coghlan, R, Lerner, ZI, Harrison, JD, Stoltenberg, M, et al. Global palliative care education in the time of COVID-19. J Pain Symptom Manag. (2020) 60:e14–9. doi: 10.1016/j.jpainsymman.2020.07.018
14. Hanson, LC. We will all be changed: palliative care transformation in the time of COVID-19. J Palliat Med. (2020) 23:1145–6. doi: 10.1089/jpm.2020.0446
15. Tanzi, S, Alquati, S, Martucci, G, and De Panfilis, L. Learning a palliative care approach during the COVID-19 pandemic: a case study in an infectious diseases unit. Palliat Med. (2020) 34:1220–7. doi: 10.1177/0269216320947289
16. Harding, R. Palliative care as an essential component of the HIV care continuum. Lancet HIV. (2018) 5:e524–30. doi: 10.1016/S2352-3018(18)30110-3
17. Kutzen, HS. Integration of palliative care into primary care for human immunodeficiency virus-infected patients. Am J Med Sci. (2004) 328:37–47. doi: 10.1097/00000441-200407000-00006
18. Ruiz, M, and Cefalu, C. Palliative care program for human immunodeficiency virus-infected patients: rebuilding of an academic urban program. Am J Hosp Palliat Care. (2011) 28:16–21. doi: 10.1177/1049909110371468
19. Spencer, DC, Krause, R, Rossouw, T, Moosa, MYS, Browde, S, Maramba, E, et al. Palliative care guidelines for the management of HIV-infected people in South Africa. South Afr J HIV Med. (2019) 20:1013. doi: 10.4102/sajhivmed.v20i1.1013
20. Gusev, DA, Leonova, ON, Dugin, SD, Smirnova, NL, and Shelomov, AS. Mobile team performance in integrated palliative care for patients with HIV infection. J Infectol. (2020) 12:58–62. doi: 10.22625/2072-6732-2020-12-2-58-62
21. Yajima, R, Ise, Y, Wako, T, Katayama, S, and Kizu, J. A retrospective study of risk factors for infection in cancer patients receiving specialist palliative care. J Nippon Med Sch. (2013) 80:481–5. doi: 10.1272/jnms.80.481
22. Choi, A, Lemos-Filho, L, Narayana-Jaya, K, and Gasperino, J. Central line-associated bloodstream infections in patients with palliative care needs. Crit Care Med. (2016) 44:374. doi: 10.1097/01.ccm.0000509869.14343.92
23. Schedin, A, Goodrose-Flores, C, Bonn, S, and Björkhem-Bergman, L. Catheter-related bloodstream infections in palliative care patients receiving parenteral nutrition by medical home care. BMJ Support Palliat Care. (2020) 1–6. doi: 10.1136/bmjspcare-2020-002331
24. de Boer, M, Coghlan, RJ, Russell, B, and Philip, JAM. The underrepresentation of palliative care in global guidelines for responding to infectious disease outbreaks: a systematic narrative review. Int Health. (2022) 14:453–67. doi: 10.1093/inthealth/ihab075
25. Artioli, G, Bedini, G, Bertocchi, E, Ghirotto, L, Cavuto, S, Costantini, M, et al. Palliative care training addressed to hospital healthcare professionals by palliative care specialists: a mixed-method evaluation. BMC Palliat Care. (2019) 18:88. doi: 10.1186/s12904-019-0476-8
26. Tanzi, S, De Panfilis, L, Costantini, M, Artioli, G, Alquati, S, and Di Leo, S. Development and preliminary evaluation of a communication skills training programme for hospital physicians by a specialized palliative care service: the ‘teach to talk’ programme. BMC Med Educ. (2020) 20:363. doi: 10.1186/s12909-020-02275-2
27. Braun, V, Clarke, V, Hayfield, N, and Terry, G. Thematic analysis In: P Liamputtong, editor. Handbook of research methods in health social sciences. Singapore: Springer (2019). 843–60.
28. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
29. Calman, L, Brunton, L, and Molassiotis, A. Developing longitudinal qualitative designs: lessons learned and recommendations for health services research. BMC Med Res Methodol. (2013) 13:14. doi: 10.1186/1471-2288-13-14
30. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
31. Birt, L, Scott, S, Cavers, D, Campbell, C, and Walter, F. Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qual Health Res. (2016) 26:1802–11. doi: 10.1177/1049732316654870
32. Drury, A, Eicher, M, and Dowling, M. Experiences of cancer care during COVID-19: phase 1 results of a longitudinal qualitative study. Int J Nurs Stud Adv. (2021) 3:100030. doi: 10.1016/j.ijnsa.2021.100030
33. Balmer, DF, and Richards, BF. Conducting qualitative research through time: how might theory be useful in longitudinal qualitative research? Adv Health Sci Educ Theory Pract. (2022) 27:277–88. doi: 10.1007/s10459-021-10068-5
34. Kern, DE, Thomas, PA, and Hughes, MT eds. Curriculum development for medical education: a six-step approach. 2nd ed. Baltimore, Md.: Johns Hopkins University Press (2009). 253 p.
35. Ballangrud, R, Aase, K, and Vifladt, A. Longitudinal team training program in a Norwegian surgical ward: a qualitative study of nurses’ and physicians’ experiences with implementation. BMC Health Serv Res. (2021) 21:725. doi: 10.1186/s12913-021-06732-6
36. Galiana, L, Sansó, N, Muñoz-Martínez, I, Vidal-Blanco, G, Oliver, A, and Larkin, PJ. Palliative care professionals’ inner life: exploring the mediating role of self-compassion in the prediction of compassion satisfaction, compassion fatigue, burnout and wellbeing. J Pain Symptom Manag. (2022) 63:112–23. doi: 10.1016/j.jpainsymman.2021.07.004
37. Siow, YC, Cheong, MWL, Lim, KS, Mahalinggam, S, and Teoh, CCO. Training physicians to provide basic-level palliative care: an evaluation of a novel training programme. Prog Palliative Care. (2022) 30:69–74. doi: 10.1080/09699260.2021.1963175
38. Krishna, LKR, Tan, LHE, Ong, YT, Tay, KT, Hee, JM, Chiam, M, et al. Enhancing mentoring in palliative care: an evidence based mentoring framework. J Med Educat Curri Develop. (2020) 7:238212052095764. doi: 10.1177/2382120520957649
39. Whitehurst, JL, and Rowlands, J. Helping palliative care healthcare professionals get the most out of mentoring in a low-income country: a qualitative study. BMC Palliat Care. (2016) 15:90. doi: 10.1186/s12904-016-0164-x
40. Grüne, B, Meesters, S, Bausewein, C, and Schildmann, E. Challenges and strategies regarding sedation at the end of life in hospitals and nursing homes. J Pain Symptom Manag. (2022) 63:530–8. doi: 10.1016/j.jpainsymman.2021.12.012
41. Eddy, K, Jordan, Z, and Stephenson, M. Health professionals’ experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. JBI Database System Rev Implement Rep. (2016) 14:96–137. doi: 10.11124/JBISRIR-2016-1843
42. Paulsen, K, Wu, DS, and Mehta, AK. Primary palliative care education for trainees in U.S. medical residencies and fellowships: a scoping review. J Palliat Med. (2021) 24:354–75. doi: 10.1089/jpm.2020.0293
Keywords: COVID-19, palliative care, qualitative research, education, infectious disease
Citation: Alquati S, Artioli G, Martucci G and Tanzi S (2024) Training an infectious disease unit in palliative care during and post COVID-19: a qualitative longitudinal study. Front. Public Health. 12:1393770. doi: 10.3389/fpubh.2024.1393770
Edited by:
Hanne Tønnesen, Copenhagen University Hospital, DenmarkReviewed by:
Kourosh Zarea, Ahvaz Jundishapur University of Medical Sciences, IranOsnat Bashkin, Ashkelon Academic College, Israel
Copyright © 2024 Alquati, Artioli, Martucci and Tanzi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Alquati, c2FyYS5hbHF1YXRpQGF1c2wucmUuaXQ=
†ORCID: Sara Alquati, orcid.org/0000-0001-8696-9602
 Sara Alquati
Sara Alquati Giovanna Artioli
Giovanna Artioli Gianfranco Martucci
Gianfranco Martucci Silvia Tanzi
Silvia Tanzi