- 1Centre for Psychosocial Health, The Education University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2Shouyilu Street Community Health Service Center, Wuhan, Hubei, China
- 3Department of Social Medicine and Health Management, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China
- 4Department of Administrative Management, Shanggang Community Health Service Center, Shanghai, China
- 5Department of Administrative Management, Laoshan Community Health Service Center, Qingdao, Shandong, China
- 6Department of Administrative Management, Jinsong Community Health Service Center, Beijing, China
- 7Department of Administrative Management, Xinhua Shaocheng Community Health Service Center, Chengdu, Sichuan, China
- 8Department of Administrative Management, Tianshui Wulin Street Community Health Service Center, Hangzhou, Zhejiang, China
- 9Department of Administrative Management, Jiexin Village Community Health Service Center, Lanzhou, Gansu, China
- 10Department of Administrative Management, Xinglin Street Community Health Service Center, Hefei, Anhui, China
- 11Department of Psychology, The Education University of Hong Kong, Hong Kong, Hong Kong SAR, China
Introduction: This study examined the prevalence and correlates of probable mental health disorders, including psychological distress, somatization, depression, anxiety, phobic anxiety (PHO), obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and insomnia among Chinese primary health care (PHC) physicians and nurses amid the post-pandemic period in 2022.
Method: Region-stratified sampling was conducted to recruit a national sample of 4,246 respondents from 31 July 2022 to 12 August 2022. A total of 692 primary healthcare institutions were identified in 30 provincial-level administrative regions of China. An online questionnaire was used for assessing probable mental health disorders using Symptoms Checklist-90-Revised (SCL-90-R) and PTSD Checklist for DSM-5 (PCL-5), and sleeping problems using Insomnia Severity Index (ISI). Data on demographics and work were also collected. Bivariate analysis and multiple logistic regression were conducted to identify significant correlates of probable mental health disorders.
Results: A total of 4,246 valid questionnaires were identified. Results showed that relative to the prevalence of probable mental health disorders among health care workers at the early stage of the pandemic in China, there was an overall decreased prevalence except for somatization, PHO, and OCD among the current PHC physicians and nurses. Multiple logistic regressions showed that significant risk factors of common probable mental health disorders, namely psychological distress, SOM, DEP, ANX, PHO, OCD, PTSD, and insomnia, were female gender, multimorbidity, history of psychiatric disorders, quarantine experience, never asking anyone for help, and overtime work.
Conclusion: Attention should be given to preexisting psychiatric and multimorbid conditions, social support, and work-related stressors. Regular assessment and psychological interventions are needed to enhance the mental health of PHC professionals even after public health crisis.
1 Introduction
Starting from the lockdown of Wuhan on January 23rd, 2020, China adopted some of the most prolonged and stringent infection control policies compared with other countries, including widespread regional lockdown, large-scale quarantine, mass temperature screening, community closed management, and extensive public health education in the community (1). China further implemented a dynamic zero-COVID policy to minimize COVID-19 transmission starting August 2021 until the abrupt lifting of all infection control rules on 26th December, 2022 (2). The outbreak of the COVID-19 pandemic has brought a substantial and prolonged crisis across the globe, characterized by high infection risk and death rates and could be defined as a traumatic event to all affected people especially those who have either been infected or have suffered from serious medical conditions due to the pandemic, including primary health care (PHC) workers (3–5). The prolonged infection control created significant challenges for Chinese PHC physicians and nurses. Different from the medical professionals at secondary and tertiary hospitals in China, PHC physicians and nurses were the important cornerstone of the healthcare system and the first point of contact for individuals and families in the community, who have taken up the key role of implementing the infection control rules such as diagnosis, triage, and monitoring in collaboration with hospitals and the health department (6–8). Prolonged infection control has been found to create extra challenges to PHC physicians and nurses (6, 9), including overtime work (working hours ≥50 h per week) (10), night duty number ≥10 (11), long shift workhours (8–12 h) (12), working in high-risk environment (e.g., working front-line, working in hardest hit area, or providing direct care to infected patients) (6), and providing direct care to infected patients in ICU or Fangcang shelter hospitals (13, 14).
During the pandemic, frontline healthcare workers could experience continued physical and psychological distress due to prolonged control rules and challenges in multiple stressful and high-risk work environments (6, 11, 15–22). Initial evidence has been gathered upon high probable mental health disorders among Chinese PHC physicians and nurses (5, 23, 24), consistent with the high prevalence of probable mental health disorders across different stages of the pandemic among Chinese medical workers (4). It remains unclear whether the high prevalence was consistent across regions, urban and rural settings, and demographic and occupational characteristics (8, 25). Such evidence will be of global relevance for optimizing the resilience of the primary care system for any future pandemic or large-scale disasters (26, 27).
Previous studies in other regions have identified sociodemographic factors of mental health disorders including younger age, female gender, being unmarried, having children or dependents to care, preexisting chronic disease(s), and histories of psychiatric disorders (13, 15, 20, 21, 27, 30, 31). Apart from demographics, risk factors could be significant risk factors of mental health disorders. Among healthcare professionals in Canada, other health care workers relative to physicians have been found to report higher levels of symptoms of depression, anxiety, and perceived (28). Specifically, nurses have been consistently found to be more vulnerable to psychological problems than physicians across regions (6, 14, 23, 29). Technical and administrative staff have been demonstrated to experience higher odds of common mental disorders, including depression, anxiety disorders, post-traumatic stress disorder, panic attacks, and substance use disorder (13). In addition, redeployment, lack of specialized training, and insufficient relevant medical work experience were found to be associated with higher symptoms of anxiety, burnout, depression, and PTSD (15, 18, 21).
The current study aims to investigate the prevalence of probable mental health disorders, including, somatization, depression, anxiety, phobic anxiety, obsessive-compulsive disorder, PTSD, and insomnia and their sociodemographic and occupational correlates among a national sample of PHC physicians and nurses amid the post-pandemic era in China. This study hypothesizes that probable mental health disorders are more common among PHC physicians and nurses in regions with a more significant impact of the pandemic and concomitant infection control (15, 32) and the prevalence of probable mental disorders are positively associated with sociodemographic and work-related risk factors.
2 Materials and methods
2.1 Study design and respondents
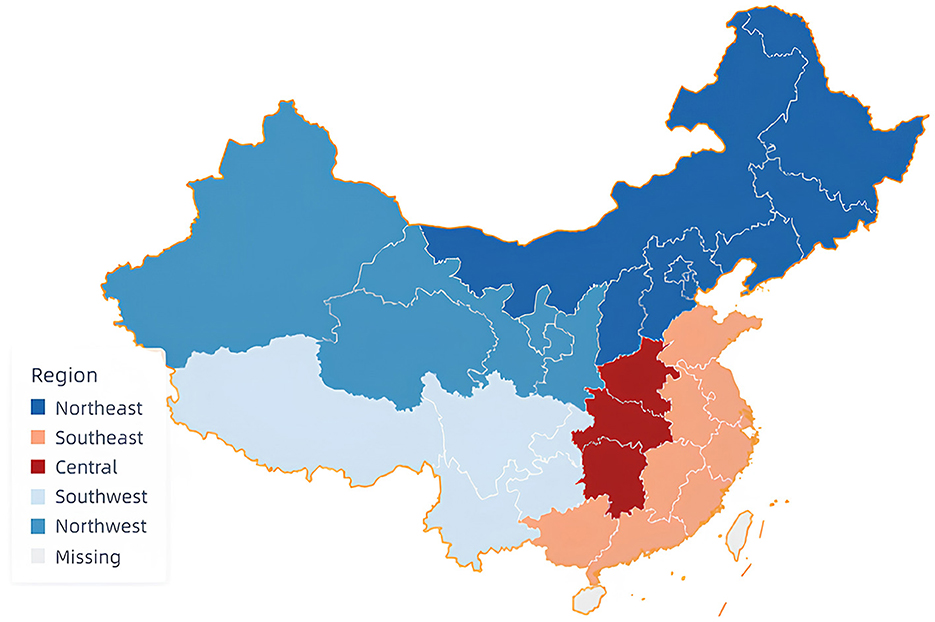
Upon obtaining the ethics committee's approval from The 7th Hospital of Wuhan (220701), respondents were recruited using region-stratified sampling. The sampling regions are shown in Figure 1. Five geographical regions of China were covered, including the central (3 provinces), southeast (7 provinces, 1 autonomous region, 1 municipality), southwest (3 provinces, 1 autonomous region, 1 municipality), northeast (5 provinces, 1 autonomous region, 2 municipalities), and northwest (3 provinces, 2 autonomous regions) (33). A total of 30 administrative regions (21 provinces, 5 autonomous regions, 4 municipalities) were covered.
Recruitment of respondents and administration of the survey was conducted online via Wenjuanxing, a widely used platform in China, from July 31-August 12, 2022. Electronic questionnaires were delivered through the Community Health Center Directors' Alliance affiliated with the Community Health Association of China, which is a national first-level organization under the management of the Ministry of Civil Affairs and the National Health Commission. Inclusion criteria were (1) age 18 years or above and (2) PHC physicians and nurses. Respondents were randomly selected using a disproportionate stratified sampling design with nine strata defined according to gender (male and female), occupation (physician and nurse), and technician title (none, junior, intermediate, associate senior, and senior). To ensure that the current sample was representative of PHC physicians and nurses in China (34), the current study (1) oversampled female respondents, (2) recruited physicians and nurses in the ratio of approximately 1:1, and (3) recruited respondents with junior and intermediate technician title based on the proportion of healthcare professionals as outlined in previous PHC national sample in China (35). Electronic informed consent was obtained from all respondents before the survey. All questions in the questionnaire needed to be answered before submission resulting in the absence of missing data. A returned survey was considered invalid if (1) no electronic informed consent, (2) the average response time on each item was < 2 s (34), or (3) maximum long string (i.e., consecutive identical responses) was equal to or larger than half of the item number (35, 36).
2.2 Measurements
2.2.1 Background variables
Demographic data were collected, including gender, age, province, residence (rural or urban), workplace (i.e., community health center or station, village and township clinics), education level (i.e., below bachelor, bachelor, and master or above), marital status (i.e., unmarried and married), childcare responsibility (yes or no, age of the child is required to be indicated), and any diagnosed chronic medical conditions (i.e., no, hypertension, diabetes, chronic obstructive pulmonary disease, pneumonia, chronic bronchitis, stroke, and others). They also reported their occupation (i.e., doctor, nurse), technical title (i.e., none, junior, intermediate, associate senior, and senior), and frequency of overtime/longer than 8 hours of work (not at all, sometimes, more than half the time, and almost every day). Respondents also rated fear of infecting COVID-19 on duties (strongly disagree, disagree, neutral, agree, strongly agree) and the cumulative number of quarantines (0, 1, 2, 3, or more than 3).
2.2.2 Probable mental health disorders
Probable mental health disorders were measured using the Chinese version of Symptoms Checklist-90-Revised (SCL-90-R) (37), the 20-item PTSD Checklist for DSM-5 (PCL-5) (38), and the 7-item Insomnia Severity Index (ISI) (39).
2.2.2.1 SCL-90-R
Respondents rated on a 5-point scale (0 = not at all, 1 = a little bit, 2 = moderately, 3 = quite a bit, 4 = extremely) for nine dimensions of psychological distress, including somatization (SOM), obsessive-compulsive disorder (OCD), interpersonal sensitivity, depression (DEP), anxiety (ANX), hostility, phobic anxiety (PHO), paranoid ideation, psychoticism, and seven additional items that assess appetite and sleep disturbances. The scores of all 90 items were averaged to form the Global Severity Index (GSI) to indicate overall psychological distress. GSI scores ≥1 indicated probable general psychological distress (37). Average scores were also calculated for SOM, DEP, ANX, PHO, and OCD. Raw average scores were then converted into T-scores (mean = 50, SD = 10) based on the mean scores of prior representative samples of Chinese medical workers (40). Subscale T-scores ≥63 were identified as high psychological distress/probable mental disorders (subscales) (41). SCL-90-R has been found to be valid and reliable for assessing mental health symptoms in Chinese populations (42). In the current study, Cronbach's α of the SCL-90-R = 0.990. The Cronbach's α for the selected subscales showed good internal consistency: SOM = 0.929, DEP = 0.942, ANX = 0.935, PHO = 0.898, and OCD = 0.922.
2.2.2.2 PCL-5
Respondents reported their experiences and responses to the threat of traumatic events in the past month on a 5-point scale (0 = not at all, 4 = extremely). A cutoff score of 33 or above was used to indicate probable PTSD (43). PCL-5 has been shown to have excellent internal consistency, test-retest reliability, and convergent and discriminant validity (44). The valid and reliable Chinese version of PCL-5 was widely used across Chinese populations (45). The Cronbach's α was 0.978 in the current administration.
2.2.2.3 ISI
The index assessed the nature, severity, and impact of insomnia on a 5-point scale (0 = none, 1 = mild, 2 = moderate, 3 = severe, and 4 = very severe). A cutoff score of 10 was used to indicate probable insomnia (39). ISI is a valid and reliable instrument for detecting insomnia among Chinese health care workers (6). In the present study, the Cronbach's α = 0.822.
2.2.3 Workplace social support
Social support in the workplace was assessed using selected items from the Social Support Rating Scale (46), including emotional support from colleagues (You and your colleagues: 1 = Never care for each other, just nod to each other, 4 = Most colleagues care about you), seeking emotional support (The way you confide when you have trouble: 1 = Never tell anyone, 4 = Confide your troubles voluntarily to get support and understanding), and seeking instrumental support (The way you seek help when you are in trouble: 1 = Only rely on themselves and do not accept help from others, 4 = Frequently ask for help from family, relatives, and organizations when in trouble). Higher scores indicated higher levels of social support and support-seeking. Social Support Rating Scale has shown good validity and reliability across Chinese populations (26, 47). In the present study, the alpha was 0.788.
2.3 Statistical analysis
First, we examined the prevalence of different probable mental health disorders. Nonparametric Mann-Whitney U tests were conducted to investigate sociodemographic and occupational correlates of mental health disorders. Next, multiple logistic regressions were conducted to test the correlates that were significant in previous bivariate analyses within a multivariable environment. Adjusted odds ratios (aORs) with 95% CI were reported. SPSS 26.0 (RRID:SCR_002865) was used for all analyses.
3 Results
3.1 Respondents and descriptive characteristics
The sampling frame consisted of 692 primary healthcare institutions, with 518 in urban areas and 174 in rural areas. A total of 5,826 online surveys were received, among which 4,246 (72.9%) were identified as valid data. Demographics did not differ between respondents with and without a valid survey (gender: p = 0.565, age: p = 0.046, marital status: p = 0.006, education level: p = 0.423, region: p = 0.037, residence: p = 0.785). The sample (37.8 ± 9.2 years of age) consisted of 2,120 physicians (49.9%) and 2,126 nurses (50.1%), among which 3,429 (80.8%) were female. The gender ratio was consistent with the ratio of 1:3 among Chinese primary medical workers (48). A total of 2,095 (49.3%) were in general practice; 3,575 (84.2%) worked in community health service centers and the remainder (n = 671, 15.8%) in village and township clinics. The majority of the respondents had never been quarantined (n = 3,113, 73.3%) and did not indicate fear of COVID-19 (n = 1,133, 88.9%). More than 60% reported overtime work sometimes (n = 2,744, 64.6%) and about 10% reported overtime work almost every day (n = 420). Demographics and study variables are summarized in Table 1.
3.2 Prevalence of mental health disorders
As shown in Table 2, among the 4,246 respondents, 11.5% of the respondents reported general psychological distress (95%CI = 10.6, 12.5), 11.2% (95%CI = 10.3, 12.2) reported somatization, 8.2% (95%CI = 7.4, 9.1) reported probable depression, 5.9% (95%CI = 5.2, 6.6) reported probable anxiety, 6.2% (95%CI = 5.5, 7.0) reported probable phobic anxiety, 7.9% (95%CI = 7.1, 8.8) reported probable OCD, 6.8% (95%CI = 6.0, 7.6) reported probable interpersonal sensitivity, 9.0% (95%CI = 8.2, 8.9) reported probable hostility, 6.2% (95%CI = 5.5, 6.9) reported probable paranoid ideation, 7.0% (95%CI = 6.2, 7.7) reported probable psychoticism, 6.9% (95%CI = 6.1, 7.7) reported probable PTSD, and 18% (95%CI = 16.9, 19.2) reported probable insomnia.
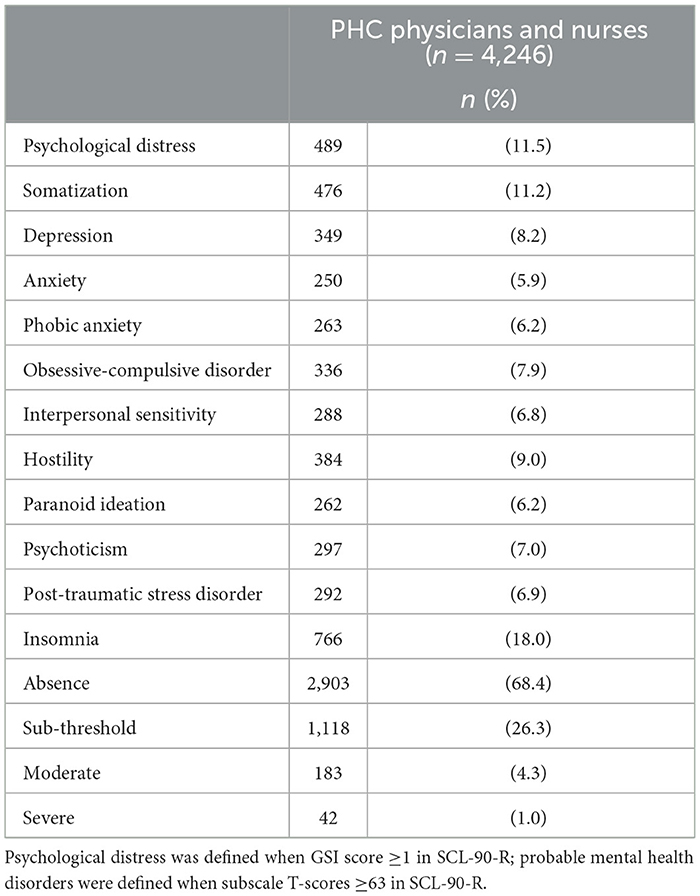
Table 2. Prevalence of current probable mental health disorders among primary health care physicians and nurses.
3.3 Correlates of probable mental health disorders
The multiple results of the logistic regression analyses are presented in Table 3. Female gender, multimorbidity, psychiatric histories, quarantine experience, working overtime for half of the time or more, and never asking help were associated with increased odds of the following outcomes: probable general psychological distress (aOR = 1.54–7.06, 95%CI = 1.14–4.41, 2.08–11.31), somatization (aOR = 1.86–5.52, 95%CI = 1.37–4.41, 2.52–8.89), depression (aOR = 1.59–8.97, 95%CI = 1.25–5.55, 2.56–14.49), anxiety (aOR = 1.47–9.73, 95%CI = 1.10–5.88, 1.96–16.07), phobic anxiety (aOR = 1.58–6.84, 95%CI = 1.20–4.12, 2.07–11.37), OCD (aOR = 1.50–7.13, 95%CI = 1.17–4.40, 1.92–11.55), PTSD (aOR = 1.48–6.97, 95%CI = 0.99–4.25, 2.21–11.44), and insomnia (aOR = 1.38–5.96, 95%CI = 1.08–3.73, 1.76–9.54). In addition, older age was associated with increased odds of probable somatization (aOR = 1.02, 95%CI = 1.00, 1.03), whereas having a bachelor's degree or above was associated with increased odds of probable general psychological distress (aOR = 1.43, 95%CI = 1.11, 1.82), somatization (aOR = 1.39, 95%CI = 1.08, 1.78), OCD (aOR = 1.39, 95%CI = 1.04, 1.86), interpersonal sensitivity (aOR = 1.25, 95%CI = 1.02, 1.52), psychoticism (aOR = 1.45, 95%CI = 1.12, 1.88), and insomnia (aOR = 1.29, 95%CI = 1.06, 1.57). Relative to respondents living in the Central region, those living and working in the Southeast region were more likely to report probable somatization (aOR = 1.39, 95%CI = 1.08, 1.79), and PTSD (aOR = 1.49, 95%CI = 1.09, 2.04). Those living in the Southwest region were more likely to report probable general psychological distress (aOR = 1.48, 95%CI = 1.10, 2.01), somatization (aOR = 1.52, 95%CI = 1.12, 2.07), hostility (aOR = 1.31, 95%CI = 1.01, 1.70), paranoid ideation, (aOR = 1.43, 95%CI = 1.07, 1.92), psychoticism (aOR = 1.68, 95%CI = 1.21, 2.33), and PTSD (aOR = 1.51, 95%CI = 1.03, 2.21). Respondents with colleagues never caring about each other at work reported increased odds of probable phobic anxiety (aOR = 2.00, 95%CI = 1.30, 3.07), interpersonal sensitivity (aOR = 1.48, 95%CI = 1.05, 2.09), psychoticism (aOR = 1.65, 95%CI = 1.12, 2.42), and PTSD (aOR = 1.72, 95%CI = 1.11, 2.66) relative to respondents with colleagues caring to some extent. Finally, those never confiding their troubles to others reported increased odds of psychological distress (aOR = 1.85, 95%CI = 1.34, 2.56), probable somatization (aOR = 1.73, 95%CI = 1.24, 2.42), depression (aOR = 1.79, 95%CI = 1.24, 2.58), anxiety (aOR = 2.07, 95%CI = 1.37, 3.12), phobic anxiety (aOR = 1.75, 95%CI = 1.17, 2.62), and OCD (aOR = 1.91, 95%CI = 1.32, 2.77). Results from bivariate analyses are summarized in Supplementary material 1.
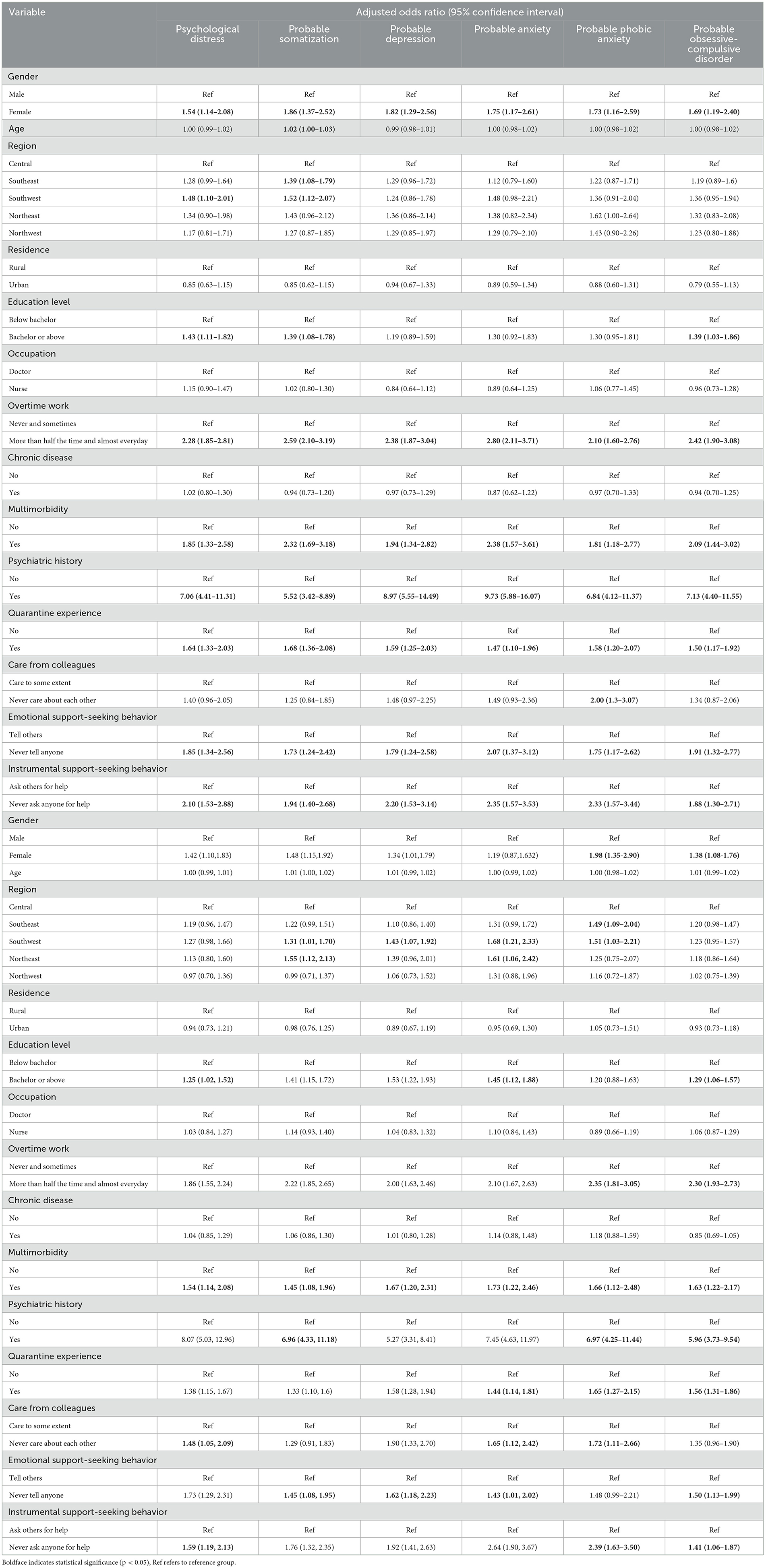
Table 3. Multiple logistic regression of risk factors associated with probable mental health disorders and insomnia.
4 Discussion
This study aims to investigate the prevalence of probable mental health disorders, and identify sociodemographic and work-related risk factors of the prevalence in a national sample of primary health care (PHC) physicians and nurses after a prolonged period of stringent infection control rules in China. The prevalence of probable mental health disorders ranged from 5.9% to 18%. Female gender, multimorbidity, psychiatric histories, and quarantine experience were related to increased odds of common probable mental health disorders, namely SOM, DEP, ANX, PHO, OCD, PTSD, and insomnia. On top of these sociodemographics were work-related factors including frequent working overtime, and never asking for help at work.
4.1 Prevalence of mental health disorders
Two years after the COVID-19 pandemic outbreak, the prevalence of probable depression (8.2%), anxiety (5.9%), PTSD (6.9%), and insomnia (18%) of Chinese PHC physicians and nurses reduced by over 13.8% compared with previous studies in the acute phase (i.e., 8th December 2019–11th March 2020), which reported a pooled prevalence of 31.0% for probable depression, 29.0% for probable anxiety, and 13.2%-75.2% for PTSD among physicians (30) and nurses (49). However, the prevalence of probable phobic anxiety (6.2%) and OCD (7.9%) slightly increased compared to previous studies (5.3–5.5%) (8, 50). Increased probable anxiety and OCD could be attributable to the traumatic experiences and fear of infection. A sense of uncontrollability, has been found to be related to increased anxiety symptoms (52), whereas the increased OCD symptoms could be related to personal hygiene and protection measures (6, 51). Our findings further suggested that this sense of uncontrollability might persist or heighten even after the traumatic event. PHC physicians and nurses might practice repetitive personal hygiene measures as compulsions to protect from infection or alleviate distress (6). Moreover, PHC physicians and nurses could be exposed to high levels of suffering and death, leading to heightened phobic anxiety (53). It is important to note that the prevalence of probable somatization (11.2%) was higher than that at the early stage of COVID-19 (5.3%) (8). Our findings suggested that somatization symptoms could be one of the most serious mental health disorders in Chinese PHC physicians and nurses during the post-pandemic period, with stress and distress expressed through physical symptoms probably resulting from prior increased workload and demands, exposure to traumatic events, or personal or family stressors related to the pandemic (54).
4.2 Risk factors of probable mental health disorders
4.2.1 Sociodemographics
In line with previous studies (4, 15), the current study similarly found that female gender was a risk factor for different mental health disorders. Adding to the mixed previous evidence on age (8, 15), our study found that older age was associated with higher odds of probable somatization but no other mental health disorders. About 22.0% of the respondents reported chronic diseases and 7.5% reported multimorbidity, which was found to be associated with higher odds of common probable mental health disorders (8, 15, 55). Acknowledging the multicollinearity between multimorbidity and probable mental health disorders (55), the current findings should be replicated with the consideration of this issue. Medical professionals could be more sensitive to somatic symptoms, particularly among people experienced age-related deterioration in physical conditions in conjunction with work stress, burnout, and difficulty in adjustment to overtime work. Existing physical and psychiatric issues could further cause chronic pain and functional impairment (55), and increase physical and psychological burden. The PHC physicians and nurses in Central China reported lower odds of disorders which could be explained by their early exposure to the pandemic outbreak, as they received more support from across the nation (7) and could have more psychosocial resources to buffer against mental ill health (56). Contrarily, physicians/nurses in Southwestern China might be more disadvantaged given the region's developing economy and PHC sectors and the lower socioeconomic status of the physicians/nurses (7).
4.2.2 Work-related characteristics
Job duties and responsibilities were associated with higher odds of multiple probable mental health disorders among PHC physicians and nurses, who shouldered the burden of regular community health care services in conjunction with the implementation of national epidemic prevention and control policies (1, 2). The present findings showed that overtime work was associated with higher odds of common probable mental health disorders. The finding extended previous evidence on the positive association between long working hours and mental illnesses in different occupations (10) to PHC physicians and nurses during prolonged strict COVID-19 quarantine in China. Our results were also consistent with previous evidence (44, 57) on the adverse mental health impact of quarantine experiences among physicians/nurses during COVID-19. People within mandatory and stringent quarantine have reported immediate disruptions to their daily routines of work, exercise, and social activities, and various quarantine-induced stressors concerning health, finance, stigma, and employment could persist even after the pandemic and relate to mental health disorders (57, 58). This study added to previous evidence by assessing quarantine experiences that occurred 1–2 years and showing their prolonged adverse mental health impact in a national sample of PHC physicians and nurses.
4.2.3 Lack of workplace social support in primary health care
Social support has been widely recognized as a protective factor that was associated with lower symptoms of depression, anxiety, PTSD (15, 26), burnout, and quality of life among physicians/nurses. The current study provided additional evidence on the important positive link between social support-seeking behaviors and mental health in the often overlooked primary health care settings. Instead of focusing on the social support PHC professionals received, more attention should be given to facilitating their social support-seeking behaviors, which is an essential coping strategy that helps individuals develop more positive and effective coping strategies and psychological qualities, such as self-efficacy and positive appraisal (26). Such proactive coping with different stressors in PHC could contribute to overall psychological health (59). Despite the potentially important role of social support-seeking behaviors, it was previously found that as low as 12.7% of physicians sought help for their mental health during the COVID-19 outbreak (60), consistent with our findings that 10% of PHC physicians/nurses never sought support. Reluctance to seek help for mental health coupled with a shortage of psychologists (60) should be addressed systematically.
The present study has several limitations. First, causality could not be inferred due to the cross-sectional design. Second, our self-report survey method which could not preclude the possibilities of recall and social desirability biases, although the current instruments were validated and widely used. Third, the traumatic event was not specified in our measurement of PTSD, therefore we could not conclude that the scores reflected respondents' experiences with COVID-19 or related occupational conditions (61). Fourth, apart from the workplace, probable mental health disorders of healthcare professionals could be partially attributable to family issues, such as family distress, family support, and having family members infected (23, 62, 63). Fifth, there could be contextual biases or framing effects which may exist in studies targeting a particular workforce (32). Lower prevalence of mental health disorders was reported in occupation-specific populations with larger sample size compared to those collected in surveys, such as military personnel and police. Last but not least, the current study did not assess other common confounding variables that could influence mental health in COVID-19 such as COVID-19 infection history and perception of COVID-19 information release (64).
4.3 Conclusion and implications
Notwithstanding the limitations, the present study has several strengths. First, this national survey recruited one of the largest samples of nationally representative primary health care physicians and nurses using the stratified sampling method, covering both urban and rural areas across seven geographical regions and 30 provincial-level administrative regions in China. To the best of our knowledge, this is one of the first national studies on the mental health of PHC physicians and nurses in China. Second, our study extended the current literature by demonstrating the prolonged mental health impact of stringent infection control rules in the post-pandemic period, supplementing existing body of evidence for the early phase of the outbreak, within and beyond China.
Two years after the pandemic outbreak, under the prolonged strict quarantine measures in China, we observed an overall decreased prevalence of probable mental health disorders and insomnia in Chinese primary health care physicians and nurses, except for the increased probable in somatization, phobic anxiety, and obsessive-compulsive disorder. Primary health care workers might suffer long-term somatic symptoms despite the improvement in overall mental health. Burden and disrupted schedules due to overtime work and quarantine increased the odds of probable disorders. Mental health of primary health care professionals who were older, female, holding higher education degrees, or suffering from multimorbidity were more affected, especially those who did not seek social support. Our results call for attention from an organizational level to provide intervention and rehabilitation programs targeting primary health care physicians and nurses in need, so with the goal of enhancing their long-term physical and mental health and preparedness for future public health crises.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, upon reasonable request.
Ethics statement
The studies involving humans were approved by The 7th Hospital of Wuhan (220701). The studies were conducted in accordance with the local legislation and institutional requirements. Electronic informed consent for participation in this study was provided before the data collection.
Author contributions
CL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. YZ: Methodology, Conceptualization, Data curation, Project administration, Resources, Writing – review & editing. YG: Conceptualization, Methodology, Writing – review & editing. ZD: Methodology, Writing – review & editing. XC: Methodology, Writing – review & editing. YL: Methodology, Writing – review & editing. WW: Methodology, Writing – review & editing. TJ: Methodology, Writing – review & editing. QZ: Methodology, Writing – review & editing. LN: Methodology, Writing – review & editing. TT: Writing – review & editing. WH: Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Research Grants Council, University Grants Committee, Hong Kong SAR, China [Grant Number 18600320 (WH)]. The funding source had no role in any process of our study.
Acknowledgments
We would like to thank all the respondents who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1392845/full#supplementary-material
Abbreviations
PHC, Primary health care; SOM, Somatization; OCD, Obsessive-compulsive disorder; DEP, Depression; ANX, Anxiety; PHO, Phobic anxiety; PTSD, Post-traumatic stress disorder.
References
1. Wang X, Shi L, Zhang Y, Chen H, Sun G. Policy disparities in fighting COVID-19 among Japan, Italy, Singapore and China. Int J Equity Health. (2021) 20:33. doi: 10.1186/s12939-020-01374-2
2. Burki T. Dynamic zero COVID policy in the fight against COVID. Lancet Respir Med. (2022) 10:e58–9. doi: 10.1016/S2213-2600(22)00142-4
3. Adjorlolo S, Adjorlolo P, Andoh-Arthur J, Ahiable EK, Kretchy IA, Osafo J. Post-traumatic growth and resilience among hospitalized covid-19 survivors: a gendered analysis. Int J Environ Res Public Health. (2022) 19:10014. doi: 10.3390/ijerph191610014
4. Hu N, Deng H, Yang H, Wang C, Cui Y, Chen J, et al. The pooled prevalence of the mental problems of Chinese medical staff during the COVID-19 outbreak: a meta-analysis. J Affect Disord. (2022) 303:323–30. doi: 10.1016/j.jad.2022.02.045
5. Zeng X, Peng T, Hao X, Zou C, Lin K, Liao X, et al. Psychological distress reported by primary care physicians in china during the covid-19 pandemic. Psychosom Med. (2021) 83:380. doi: 10.1097/PSY.0000000000000939
6. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
7. Li X, Krumholz HM, Yip W, Cheng KK, De Maeseneer J, Meng Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet. (2020) 395:1802–12. doi: 10.1016/S0140-6736(20)30122-7
8. Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
9. Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatry. (2020) 33:e100259. doi: 10.1136/gpsych-2020-100259
10. Ma X. Impact of long working hours on mental health: evidence from China. Int J Environ Res Public Health. (2023) 20:1641. doi: 10.3390/ijerph20021641
11. Peng X, Meng X, Li L, Hu C, Liu W, Liu Z, et al. Depressive and anxiety symptoms of healthcare workers in intensive care unit under the COVID-19 epidemic: an online cross-sectional study in China. Front Public Health. (2021) 9:603273. doi: 10.3389/fpubh.2021.603273
12. Abhiram K, Tan BYQ, Tan M, Tan L, Sia C-H, Chua YX, et al. The effect of COVID-19 endemicity on the mental health of health workers. J Am Med Dir Assoc. (2022) 23:405–13.e3. doi: 10.1016/j.jamda.2022.01.059
13. Aragonès E, Cura-González I, Hernández-Rivas L, Polentinos-Castro E, Fernández-San-Martín MI, López-Rodríguez JA, et al. Psychological impact of the COVID-19 pandemic on primary care workers: a cross-sectional study. Br J Gen Pract. (2022) 72:e501–10. doi: 10.3399/BJGP.2021.0691
14. Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. (2020) 131:132–7. doi: 10.1016/j.jpsychires.2020.09.007
15. Chutiyami M, Cheong AMY, Salihu D, Bello UM, Ndwiga D, Maharaj R, et al. COVID-19 Pandemic and overall mental health of healthcare professionals globally: a meta-review of systematic reviews. Front Psychiatry. (2022) 12:804525. doi: 10.3389/fpsyt.2021.804525
16. Maltezou HC, Pavli A, Tsakris A. Post-COVID syndrome: an insight on its pathogenesis. Vaccines. (2021) 9:497. doi: 10.3390/vaccines9050497
17. Mandal A, Purkey E. Psychological impacts of the COVID-19 pandemic on rural physicians in Ontario: a qualitative study. Healthcare. (2022) 10:455. doi: 10.3390/healthcare10030455
18. Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. (2020) 5:e475–83. doi: 10.1016/S2468-2667(20)30164-X
19. Pavli A, Theodoridou M, Maltezou HC. Post-COVID syndrome: incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch Med Res. (2021) 52:575–81. doi: 10.1016/j.arcmed.2021.03.010
20. Rahman MA, Hoque N, Alif SM, Salehin M, Islam SMS, Banik B, et al. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Glob Health. (2020) 16:95. doi: 10.1186/s12992-020-00624-w
21. Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. (2020) 277:347–57. doi: 10.1016/j.jad.2020.08.034
22. Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the coronavirus disease 2019 epidemic in China. Brain Behav Immun. (2020) 88:60–5. doi: 10.1016/j.bbi.2020.06.002
23. She R, Li L, Yang Q, Lin J, Ye X, Wu S, et al. Associations between COVID-19 work-related stressors and posttraumatic stress symptoms among Chinese doctors and nurses: Application of stress-coping theory. Int J Environ Res Public Health. (2022) 19:6201. doi: 10.3390/ijerph19106201
24. Li Y, Fan R, Lu Y, Li H, Liu X, Kong G, et al. Prevalence of psychological symptoms and associated risk factors among nurses in 30 provinces during the COVID-19 pandemic in China. Lancet Reg Health – West Pac. (2023) 30:100618. doi: 10.1016/j.lanwpc.2022.100618
25. Chersich MF, Gray G, Fairlie L, Eichbaum Q, Mayhew S, Allwood B, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Glob Health. (2020) 16:46. doi: 10.1186/s12992-020-00574-3
26. Shi L, Xu RH, Xia Y, Chen D, Wang D. The impact of COVID-19-related work stress on the mental health of primary healthcare workers: The mediating effects of social support and resilience. Front Psychol. (2022) 12:800183. doi: 10.3389/fpsyg.2021.800183
27. De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz S-A, Ellis L, et al. rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health. (2021) 21:104. doi: 10.1186/s12889-020-10070-3
28. Schechter-Finkelstein T, Plenert E, La Rosa J, McLean J, Chiang KY, Krueger J, et al. Pediatric hematology/oncology healthcare professional emotional health during COVID-19. Cancer Med. (2021) 10:7144–51. doi: 10.1002/cam4.4253
29. Halcomb E, Fernandez R, Mursa R, Stephen C, Calma K, Ashley C, et al. Mental health, safety and support during COVID-19: a cross-sectional study of primary health care nurses. J Nurs Manag. (2022) 30:393–402. doi: 10.1111/jonm.13534
30. Fiest KM, Parsons Leigh J, Krewulak KD, Plotnikoff KM, Kemp LG, Ng-Kamstra J, et al. Experiences and management of physician psychological symptoms during infectious disease outbreaks: a rapid review. BMC Psychiatry. (2021) 21:91. doi: 10.1186/s12888-021-03090-9
31. Sriharan A, Ratnapalan S, Tricco AC, Lupea D, Ayala AP, Pang H, et al. Occupational stress, burnout, and depression in women in healthcare during COVID-19 pandemic: rapid scoping review. Front Glob Womens Health. (2020) 1:596690. doi: 10.3389/fgwh.2020.596690
32. Scott HR, Stevelink SAM, Gafoor R, Lamb D, Carr E, Bakolis I, et al. Prevalence of post-traumatic stress disorder and common mental disorders in health-care workers in England during the COVID-19 pandemic: a two-phase cross-sectional study. Lancet Psychiatry. (2023) 10:40–9. doi: 10.1016/S2215-0366(22)00375-3
33. Fairbank JK, Goldman M. China: A New History, Second Enlarged Edition. Cambridge, MA: Harvard University Press (2006). p. 642
34. Huang JL, Curran PG, Keeney J, Poposki EM, DeShon RP. Detecting and deterring insufficient effort responding to surveys. J Bus Psychol. (2012) 27:99–114. doi: 10.1007/s10869-011-9231-8
35. Curran PG. Methods for the detection of carelessly invalid responses in survey data. J Exp Soc Psychol. (2016) 66:4–19. doi: 10.1016/j.jesp.2015.07.006
36. Landers RN. Calculating LongString in Excel to Detect Careless Responders. Hoboken, NJ: Authorea (2020).
38. Yehuda R. Post-traumatic stress disorder. N Engl J Med. (2002) 346:108–14. doi: 10.1056/NEJMra012941
39. Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
40. Xie J, Liu Q, Jiang X, Manandhar U, Zhu Z, Li Y, et al. Psychological health issues of medical staff during the COVID-19 outbreak. Front Psychiatry. (2021) 12:611223. doi: 10.3389/fpsyt.2021.611223
42. Tian F, Li H, Tian S, Yang J, Shao J, Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. (2020) 288:112992. doi: 10.1016/j.psychres.2020.112992
43. Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, et al. Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. (2016) 28:1392–403. doi: 10.1037/pas0000260
44. Chamaa F, Bahmad HF, Darwish B, Kobeissi JM, Hoballah M, Nassif SB, et al. In the COVID-19 era. Curr Neuropharmacol. (2021) 19:2164–79. doi: 10.2174/1570159X19666210113152954
45. Cheng P, Xu L-Z, Zheng W-H, Ng RMK, Zhang L, Li L-J, et al. Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. J Affect Disord. (2020) 277:368–74. doi: 10.1016/j.jad.2020.08.038
46. Xiao S. Theoretical basis and application of the social support rating scale. J Clin Psychiatry. (1994) 4:98–100.
47. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit Int Med J Exp Clin Res. (2020) 26:e923549-1–e923549-8. doi: 10.12659/MSM.923549
48. Yu Y, Kong C, Zhang W, Yuan B. A study on the chain mediating effect of job motivation in job satisfaction and work performance of primary medical workers. Chin J Health Policy. (2021) 14:21–8.
49. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
50. Zhang J, Deng X, Liu H, Xu X, Fang R. Evaluation of the mental health status of community healthcare workers during the COVID-19 outbreak. Medicine (Baltimore). (2021) 100:e24739. doi: 10.1097/MD.0000000000024739
51. Greenberg N, Brooks SK, Wessely S, Tracy DK. How might the NHS protect the mental health of health-care workers after the COVID-19 crisis? Lancet Psychiatry. (2020) 7:733–4. doi: 10.1016/S2215-0366(20)30224-8
52. Myhr G, Sookman D, Pinard G. Attachment security and parental bonding in adults with obsessive-compulsive disorder: a comparison with depressed out-patients and healthy controls. Acta Psychiatr Scand. (2004) 109:447–56. doi: 10.1111/j.1600-0047.2004.00271.x
53. Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J Affect Disord. (2020) 275:48–57. doi: 10.1016/j.jad.2020.06.022
54. Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson AE, et al. comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage. (2020) 60:e60–5. doi: 10.1016/j.jpainsymman.2020.04.008
55. Ronaldson A, Arias de la Torre J, Prina M, Armstrong D, Das-Munshi J, Hatch S, et al. Associations between physical multimorbidity patterns and common mental health disorders in middle-aged adults: A prospective analysis using data from the UK biobank. Lancet Reg Health - Eur. (2021) 8:100149. doi: 10.1016/j.lanepe.2021.100149
56. Li S, Rao L-L, Ren X-P, Bai X-W, Zheng R, Li J-Z, et al. Psychological typhoon eye in the 2008 Wenchuan earthquake. PLoS ONE. (2009) 4:e4964. doi: 10.1371/journal.pone.0004964
57. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
58. Liu H, Tao TJ, Chan SKY, Ma JCH, Lau AYT, Yeung ETF, et al. Daily routine disruptions and psychiatric symptoms amid COVID-19: a systematic review and meta-analysis of data from 0.9 million individuals in 32 countries. BMC Med. (2024) 22:49. doi: 10.1186/s12916-024-03253-x
59. Zhang N, Bai B, Zhu J. Stress mindset, proactive coping behavior, and posttraumatic growth among health care professionals during the COVID-19 pandemic. Psychol Trauma Theory Res Pract Policy. (2022) 15:515. doi: 10.1037/tra0001377
60. She R, Wang X, Zhang Z, Li J, Xu J, You H, et al. Mental health help-seeking and associated factors among public health workers during the COVID-19 outbreak in China. Front Public Health. (2021) 9:622677. doi: 10.3389/fpubh.2021.622677
61. Muysewinkel E, Stene LE, Van Deynse H, Vesentini L, Bilsen J, Van Overmeire R. Post-what stress? A review of methods of research on posttraumatic stress during COVID-19. J Anxiety Disord. (2024) 102:102829. doi: 10.1016/j.janxdis.2024.102829
62. Yuan K, Zheng Y-B, Wang Y-J, Sun Y-K, Gong Y-M, Huang Y-T, et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. (2022) 27:3214–22. doi: 10.1038/s41380-022-01638-z
63. Parthasarathy R, Ts JKT, Murthy P. Mental health issues among health care workers during the COVID-19 pandemic – a study from India. Asian J Psychiatry. (2021) 58:102626. doi: 10.1016/j.ajp.2021.102626
Keywords: COVID-19, mental health disorder, primary healthcare physician and nurse, post-pandemic, SCL-90-R, post-traumatic stress disorder, insomnia
Citation: Li CJ, Zheng Y, Gan Y, Du Z, Cai X, Li Y, Wang W, Jiang T, Zhang Q, Niu L, Tao TJ and Hou WK (2024) Mental health of primary health care physicians and nurses following prolonged infection control rules: a national survey in China. Front. Public Health 12:1392845. doi: 10.3389/fpubh.2024.1392845
Received: 28 February 2024; Accepted: 18 July 2024;
Published: 23 August 2024.
Edited by:
Yuka Kotozaki, Iwate Medical University, JapanReviewed by:
Roel Van Overmeire, Vrije University Brussels, BelgiumParandis Pourdehghan, Tehran University of Medical Sciences, Iran
Copyright © 2024 Li, Zheng, Gan, Du, Cai, Li, Wang, Jiang, Zhang, Niu, Tao and Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wai Kai Hou, d2tob3VAZWR1aGsuaGs=
†These authors share first authorship
 Crystal Jingru Li
Crystal Jingru Li Yanling Zheng2†
Yanling Zheng2† Yong Gan
Yong Gan Xuemin Cai
Xuemin Cai Tiffany Junchen Tao
Tiffany Junchen Tao Wai Kai Hou
Wai Kai Hou