- 1Department of Emergency and Critical Care Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 2National Center For Occupational Safety and Health, National Health Commission of the People’s Republic of China, Beijing, China
- 3Department of Internal Medicine Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 4Obstetrics and Gynecology Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 5Department of Surgical Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 6Department of Pediatric Nursing, School of Nursing, Wannan Medical College, Wuhu, China
- 7Rehabilitation Nursing, School of Nursing, Wanna Medical College, Wuhu, China
- 8Student Health Center, Wannan Medical College, Wuhu, China
Objective: Frailty and activities of daily living (ADL) disability are common conditions among older population. Studies on the bidirectional relationship between frailty and ADL are limited. The current study examined the cross-sectional and longitudinal associations between frailty and ADL in middle-aged and older Chinese individuals.
Methods: The data was collected through the China Health and Retirement Longitudinal Study (CHARLS), conducted in 2011, 2013, and 2015, encompassing 17,284 individuals aged ≥45 years. We excluded individuals without follow-up data. 2,631 participants finished the baseline survey. The definition of ADL disability encompasses difficulty in engaging in either basic activities of daily living (BADL) or instrumental activities of daily living (IADL). Frailty was assessed according to the Fried criteria. Logistic regression was utilized to examine odds ratios (ORs) and 95% confidence intervals (CIs) for assessing the cross-sectional relationships between ADL with frailty at baseline. The prediction effects were explored using Cox proportional hazards analysis, testing hazard ratios (HRs) and 95%CIs.
Results: In cross-sectional analysis, BADL [OR = 6.660 (4.519–9.815)], IADL [OR = 5.950 (4.490–7.866)], and ADL [OR = 5.658 (4.278–7.483)] exhibited significant associations with frailty; frailty demonstrated significant associations with BADL [OR = 6.741 (4.574–9.933)], IADL [OR = 6.042 (4.555–8.016)] and ADL [OR = 5.735 (4.333–7.591)]. In longitudinal analysis, IADL and ADL were significantly associated with frailty in participants without baseline frailty in the short-term period [IADL: HR = 1.971 (1.150–3.379), ADL: HR = 1.920 (1.146–3.215)], IADL exhibited a significant association with frailty in the long-term period [HR = 2.056 (1.085–3.895)]. There was no significant link observed between frailty and an elevated risk of disability onset in BADL, IADL and ADL during the short-term period. When considering the long-term perspective, frailty exhibited a significant association with an elevated risk of disability onset in BADL [HR= 1.820 (1.126–2.939)] and IADL [HR = 1.724 (1.103–2.694)].
Conclusion: In middle-aged and older adults, ADL and IADL disability predicted frailty after 2-year follow-up, IADL disability predicted frailty after 4-year follow-up. Moreover, frailty did not predict BADL, IADL and ADL disability after 2-year follow-up. However, frailty predicted BADL and IADL disability after 4-year follow-up.
Introduction
Frailty is a geriatric syndrome with multiple dimensions, characterized by an increased vulnerability to different stressors. Frailty is associated with poor health outcomes and signifies a decline in physiological reserve and function, which becomes increasingly prevalent with advancing age (1, 2). Frailty is prevalent among middle-aged and older people. Previous studies have reported varying prevalence rates of frailty in middle-aged and older population of 3% in United Kingdom (3), 4.1% in Europe (4), 11.8% in Chilean and 3.1% in China (5). Older population has a higher prevalence of frailty. According to a comprehensive meta-analysis (included studies of cross-sectional and cohort), the prevalence of frailty among Chinese older community-dwelling population was 7–20% (2, 6–8), 11% for females and 8% for males (6). The presence of frailty is associated with elevated rates of hospitalization, dementia, disability, and early mortality (9–11), and presents significant challenges to global healthcare systems. With the aging of China’s population, frailty has emerged as one pressing concern for healthcare systems, posing a significant public health burden. Relevant literature have extensively documented a large number of risk factors for frailty, such as advanced ages, unmarried, women, rural areas, living alone, lower levels of education, worse economic conditions, three or more chronic diseases, and ADL disability (2, 6, 7, 12).
According to the explanations provided in medical and rehabilitation literature, the Activities of Daily Living (ADL) refers to activities focused on self-care and personal hygiene (13). ADL are widely acknowledged as reliable indicators of functional restrictions among older individuals and are commonly categorized into basic activities of daily living (BADL) and instrumental activities of daily living (IADL) (14). BADL reflects the fundamental self-care ability that individual must consistently perform repeatedly every day to maintain their independence, while IADL refers to the more complex ability to participate in social activities and live independently (15). The adverse outcomes of ADL disability encompass hospitalization (16), mortality (17), and diminished levels of quality of life (18), among others. Several factors were associated with ADL disability, including age, chronic pain, polypharmacy, being separated/divorced, physical activity, and frailty (19–21). Most of the studies encompassed individuals aged ≥65 years, 26% of community-dwelling older people in China exhibited limitations in ADL (17), 19.02% limitations in BADL and 25.29% limitations in IADL (22). The prevalence rate of BADL disability among middle-aged and older community-dwelling adults in China was found to be 16.7%, IADL disability was 21.5% (23), and ADL disability was 19.4% (24). 2006–2018 study in United States including middle-aged and older participants showed that 25.4% presented IADL impairments, and the prevalence of impairments in IADL was highest among females and older individuals (25). A cross-sectional study of older adults residing in Brazilian communities in 2015–2016 found that the prevalence of IADL and BADL disabilities was 45.1 and 13.5%, respectively (26). A study conducted in India population aged ≥60 years revealed the prevalence of ADL and IADL were 19.89 and 45.00%, respectively (27). Other studies have described a prevalence rate of 48.5% for ADL disability among middle-aged and older individuals with chronic obstructive pulmonary disease (COPD) (28), the prevalence of IADL and BADL disability among cancer patients was reported as 54.6 and 36.7%, respectively (29).
Previous studies have researched the association of ADL and frailty. A meta-analysis performed for 31 prospective studies (9) showed a prospective association between frailty and ADL disability, with frailty leading to a significantly higher risk of BADL disability (OR: 2.05, 95% CI: 1.73–2.44) and IADL disability (OR: 2.52, 95% CI: 2.08–3.06); frailty increases the risk of losing ADL by 1.6 to 2.0 times. Another meta-analysis also showed that associations persisted among community-dwelling middle-aged and older population (30). Meta-analysis encompassed 20 studies that examined the risks of disability in IADL and ADL, it was found that frail older individuals were more prone to developing or exacerbating disability in IADL and ADL, the pooled OR and pooled HR exhibited statistically significant results (31). The cross-sectional study reported that frailty group exhibited significantly worse scores for the ADL than the non-frailty group in community-dwelling older adults (p < 0.05) (32). Analysis of Italian population cohort, the incident risk of IADL disability was increased in frailty individuals (HR: 2.56, 95%CI: 1.58–4.16) and ADL (HR: 3.58, 95%CI: 1.97–6.52) after a four-year follow-up; pre-frailty participants displayed a higher incidence of frailty compared to those without frailty at follow-up entry (33). On the other side, a meta-analysis comprising 14 studies (encompassing cross-sectional studies and cohort studies) (6) reported that having ADL disability was a risk factor for frailty among the older Chinese population in communities. Another meta-analysis collected cross-sectional data on the frailty prevalence among rural older individuals and revealed that ADL disability was significantly associated with frailty (34).
However, the existing studies mostly focus on the prevalence and risk factors of frailty (2, 6, 7, 34), whereas the effect of ADL on the incidence of frailty in longitudinal studies has been poorly understood (1). In addition, previous research primarily examined the unidirectional associations between ADL and frailty, and were limited by cross-sectional designs or small sample sizes. Considering the shared risk factors and pathophysiological mechanisms involved, our study hypothesizes a bidirectional relationship between frailty and ADL. It is imperative to prospectively investigate the bidirectional association of frailty and ADL disability utilizing a large and representative sample, to provide new references for the development of frailty and ADL disability interventions.
In the study, we utilized a four-year (2011 to 2015) longitudinal dataset from a nationally representative sample of community-dwelling adults in China, aged middle-aged and older. We aimed to explore the bidirectional relationship of ADL and frailty over short-term (2-year, 2011–2013) and long-term (4-year, 2011–2015) periods. We hypothesized that baseline ADL disability is predictive of the following frailty occurrence. Similarly, baseline frailty is predictive of subsequent changes in ADL disability.
Method
Participants
The research is based on the China Health and Retirement Longitudinal Study (CHARLS), which collected data from a cohort of 17,284 individuals aged ≥45 years in 2011 (Wave 1). Subsequent data collection occurred in 2013 and 2015 (Waves2 and Waves3). Participants were selected for in-person interviews, computer-aided personal interview (CAPI), and structured questionnaires conducted biennially. This study utilized longitudinal data from individuals who participated in Wave1, Wave2, and Wave3. The following exclusion criteria were formulated for this study: (1) lack of components of frailty data, (2) lack of components of activities of daily living disability data, and (3) lack of sex/age/current residence/educational level/marital status/alcohol drinking/smoking status/taking activities/physical exercise/BMI/chronic diseases data. Furthermore, participants without follow-up data were excluded. A total of 2,631 participants finished the baseline assessments, with 1936 participants finished the short-term follow-up surveys (spanning from 2011 to 2013) and 1879 participants finished the long-term follow-up surveys (spanning from 2011 to 2015).
Frailty assessment
Frailty assessment was conducted based on the widely accepted criteria initially proposed by Fried et al. (35), which were subsequently refined based on the data available in CHARLS. The definition of frailty comprised five essential elements, including exhaustion, slowness, weight loss, weakness, and low physical activity. The evaluation and definition of the five components of frailty were conducted in our study as follows: (1) Slowness: Participants were asked to self-report whether they had difficulty while walking 100-meter or climbing multiple flights of stairs without taking breaks, following a methodology similar to previous studies (30). Individuals who faced difficulty in performing climbing or walking were classified as slowness, (2) Weakness: it was assessed through self-report question “having difficulty in carrying or lifting weights exceeding 10 jin, such as heavy grocery bags” (36), (3) Exhaustion: it was considered present if the individuals responded with either “Most or all of the time” or “Occasionally or a moderate amount of the time” to anyone questions of the Center for Epidemiologic Studies-Depression scale in the Chinese version (CES-D) (37): “I could not get going during last week” or “I felt everything I did was an effort during last week.” The construction of this component was identical to that initially suggested by Fried et al. (35), (4) Weight loss: it was characterized as the inadvertent reduction of ≥5 kilograms within the past year (36), or a present body mass index (BMI) ≤ 18.5 kg/m2 (38), and (5) Low physical activity: WALK was defined as walking by CHARLS, referred to recreational, sporting, exercise or leisure purposes within workplaces and residences, pedestrian travel between different locations, and other forms of walking. Low physical activity represented the absence of any physical activity or WALK ≥10 min at a time in a typical week. Although differing from the component proposed by Fried et al. (35), similar treatment variables have been previously utilized to assess low physical activity (39). In our study, frailty was defined as the existence of three or more components.
Activities of daily living
In CHARLS, the ADL scale was employed to assess the level of disability among older people. The assessment of ADL was categorized into BADL and IADL. BADL disability was described as difficulty in eating, bathing, dressing, indoor moving, toileting and continence control. IADL disability was described as difficulty in performing housework, shopping, cooking, taking medicine, and financial management. Each question is categorized into 4 possible responses: “I cannot do it,” “Yes, I have difficulty and need help,” “I have difficulty but still can do it” and “No, I do not have any difficulty” (40). The individuals were classified as experiencing ADL disability if they had inability or difficulty to complete any of the 11 items, BADL disability and IADL disability represented inability or difficulty to complete any of the items about BADL and IADL, respectively (28).
Body measurement
The body mass index (BMI) is calculated by dividing weight (kilograms) by the square of height (meters). BMI is easy to measure and widely recorded in research, clinical nutrition, and epidemiology. We used the cut-off points standard of BMI for Chinese adults (41). BMI can be classified into 4 categories: BMI < 18.5 kg/m2 for underweight, BMI 18.5-24 kg/m2 for normal weight, BMI 24-28 kg/m2 for overweight and BMI ≥ 28 kg/m2 for obese (42–44).
Covariates
Age/sex (female and male)/marital status/educational level/current residence /alcohol drinking/smoking status/taking activities/ physical exercise/BMI data/chronic diseases at baseline were included as covariates in our study. (1) The age groups were categorized as four groups: 45–54, 55–64, 65–74, and ≥ 75 years old, (2) Marital status was classified into married or single (including never married, divorced, separated, or widowed), (3) Educational levels range from illiterate (no formal education), below elementary school (incomplete primary education but capable of writing or reading, to graduates of home school/sishu, middle or elementary school), high school, and above vocational school (holding a two- or three-year associate/college degree, as well as a postgraduate or doctoral degree/Ph. D), (4) Current residence encompassing urban and rural, (5) Alcohol drinking encompassing more than once a month, less than once a month, and never drinker, (6) Smoking status encompassing never smoked, former-smoker and current smoker, (7) Taking activities (such as socializing with friends, providing unpaid assistance to non-cohabiting family members, neighbors or friends, participating in social/sports/other kinds of club, playing cards/chess/mahjong/participating in community club, attending the organization of community-related, engaging in charity or voluntary work, caregiving for an uncohabiting disabled or sick people without receiving compensation, attending a training or educational course, using the Internet, stocking investment) were classified into two categories: ever (at least once a month) and never, (8) Physical exercise encompassing regular physical exercises, less than regular physical exercises, and no physical exercise, and (9) Chronic diseases, including 1) hypertension, 2) high blood or sugar diabetes, 3) dyslipidemia, 4) stroke, 5) chronic lung diseases, 6) malignant tumor or cancer (excluding minor skin cancers), 7) kidney disease(except for cancer or tumor), 8) liver disease (except cancer, tumors, and fatty liver), 9) stomach or other digestive diseases (except for cancer or tumor), 10) angina, congestive heart failure, heart attack, coronary heart disease, or other heart problems, 11) nervous, emotional, or psychiatric problems, 12) asthma of self-reported (diagnosed by a doctor), 13) memory related disease, and 14) arthritis or rheumatism. By our previous criteria (45, 46), a continuous variable ranging from 0 to 14 was employed to quantify the chronic health issues in 14 common diseases. The numbers representing the chronic disease condition were categorized into 3 groups: 0, 1–2, and 3–14. These categories have been extensively employed in our prior research (39, 43–45, 47–50).
Statistical analysis
The statistical analyses were conducted using IBM SPSS version 23.0. Categorical variables were compared using the χ2 test and presented as frequencies and percentages. Logistic regression was employed to analyze the odds ratios (ORs) and 95% confidence intervals (CIs) to examine the cross-sectional relationships of ADL disability and frailty in the individuals at baseline. The binary dependent variable of frailty (no-frailty and frailty) and ADL disability (no and yes) were subjected to analysis, with the regression models sequentially incorporating covariates, which were also used in our previous studies (50–52). Model 1 comprised activities of daily living disability and frailty, while model 2 additionally incorporated characteristics of socio-demographic (age, sex, marital status, educational level, current residence). Model 3 additionally encompassed health conditions and behaviors (alcohol drinking, smoking status, taking activities, physical exercise, chronic diseases). Lastly, model 4 incorporated BMI as an additional covariate. The Cox proportional hazards analysis was performed using hazard ratios (HRs) and 95% CIs to examine the prospective associations between baseline ADL disability in individuals without frailty at baseline, as well as the prospective associations between baseline frailty in individuals without ADL disability at baseline. The covariates were modeled through the same methods as those employed in cross-sectional analyses. The statistical significance of the results was determined based on a p-value<5%. The VIF (Variance Inflation Factor) multicollinearity diagnostic test in linear regression was conducted to detect collinearity among independent variables (53), and no collinear relationships were found between frailty and ADL (VIF < 5).
Results
Table 1 presents the baseline characteristics of individuals according to frailty status. The mean age of participants was 61.21 (SD ± 10.19), 37.74% were male; 2.62% were above vocational school, 3.88% were in high school, and 58.27% were less than elementary school; 83.88% were single; 92.02% were living in rural; 19.35% were drinking more than once a month, and 6.96% were drinking less than once a month. 48.99% were taking activities; 24.33% were current smoking, and 8.97% were former smoking; 45.12% were regular physical exercises, and 42.80% were less than regular physical exercises; 27.48% had 3–14 chronic diseases, and 51.24% had 1–2 chronic diseases; 6.16% had BADL disability, 17.71% had IADL disability, and 19.84% had ADL disability. The frequency of frailty was 11.78%. The distribution of age, age groups, sex, educational level, marital status, alcohol drinking, taking activities, physical exercise, chronic diseases, BADL, IADL, and ADL exhibited significant differences between individuals with or without frailty.
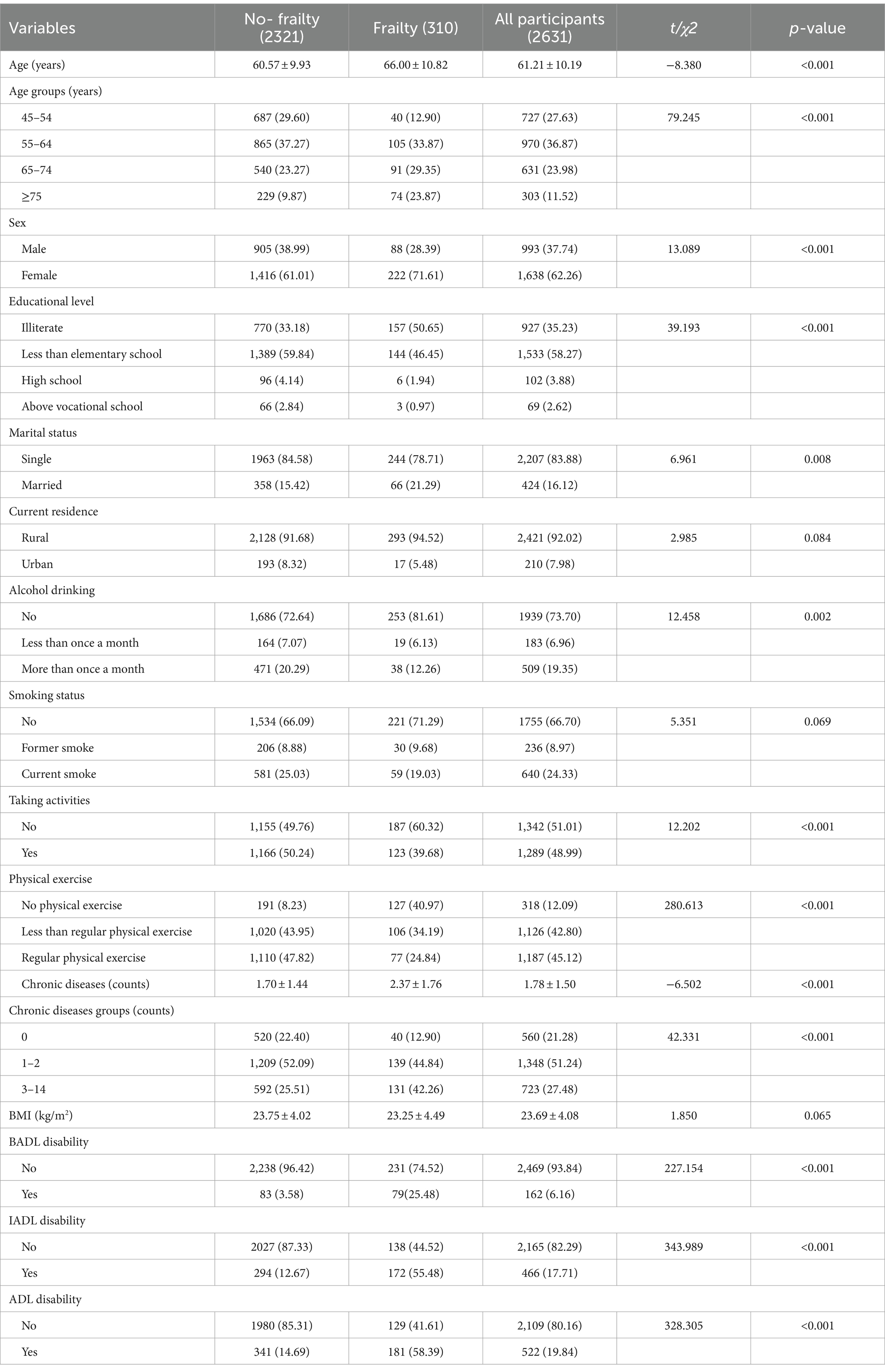
Table 1. Baseline characteristics of participants according to the status of frailty in CHARLS Waves 2011 (N, %).
Table 2 demonstrates the baseline characteristics of individuals according to the status of BADL, IADL and ADL. A total of 2,638 BADL disability individuals 162 (6.14%) and BADL normal 2,476 (93.86%) at baseline were incorporated into the cross-sectional analysis. The distribution of age groups, educational level, smoking status, taking activities, physical exercise, and chronic diseases exhibited variations among the components of BADL. A total of 2,671 IADL disability individuals 466 (17.45%) and IADL normal 2,205 (82.55%) at baseline were incorporated into the cross-sectional analyses. The distribution of age groups, sex, educational level, current residence, alcohol drinking status, taking activities, physical exercise, chronic diseases, and BMI exhibited significant variations among the components of IADL. A total of 2,631 ADL disability individuals 522 (19.84%) and ADL normal 2,109 (80.16%) at baseline were incorporated into the cross-sectional analysis. The distribution of age groups, educational level, current residence, smoking status, taking activities, physical exercise, chronic diseases, and BMI exhibited significant differences among components of ADL.
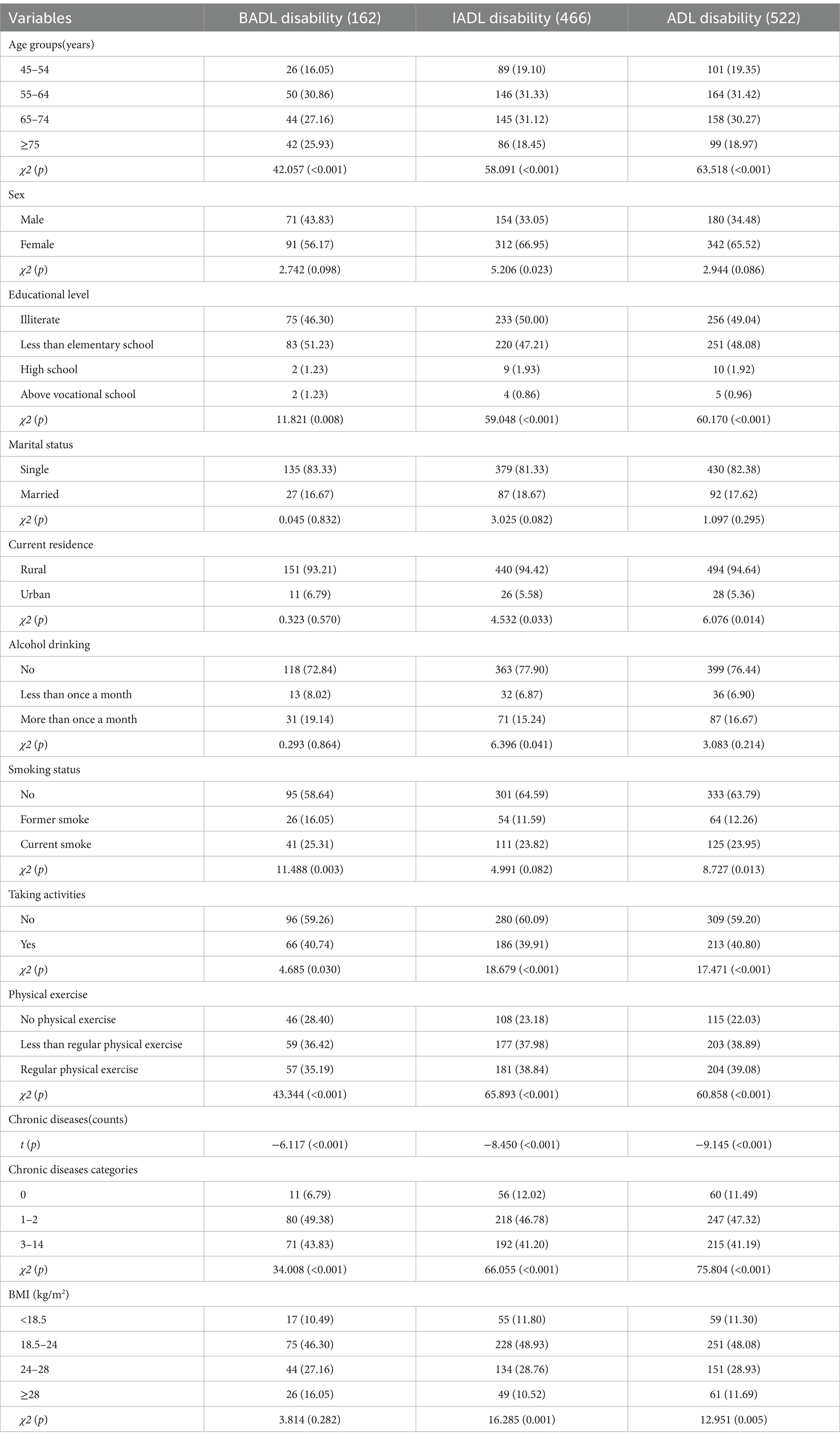
Table 2. Baseline characteristics of participants according to the level of BADL, IADL and ADL in CHARLS Waves 2011 (N, %).
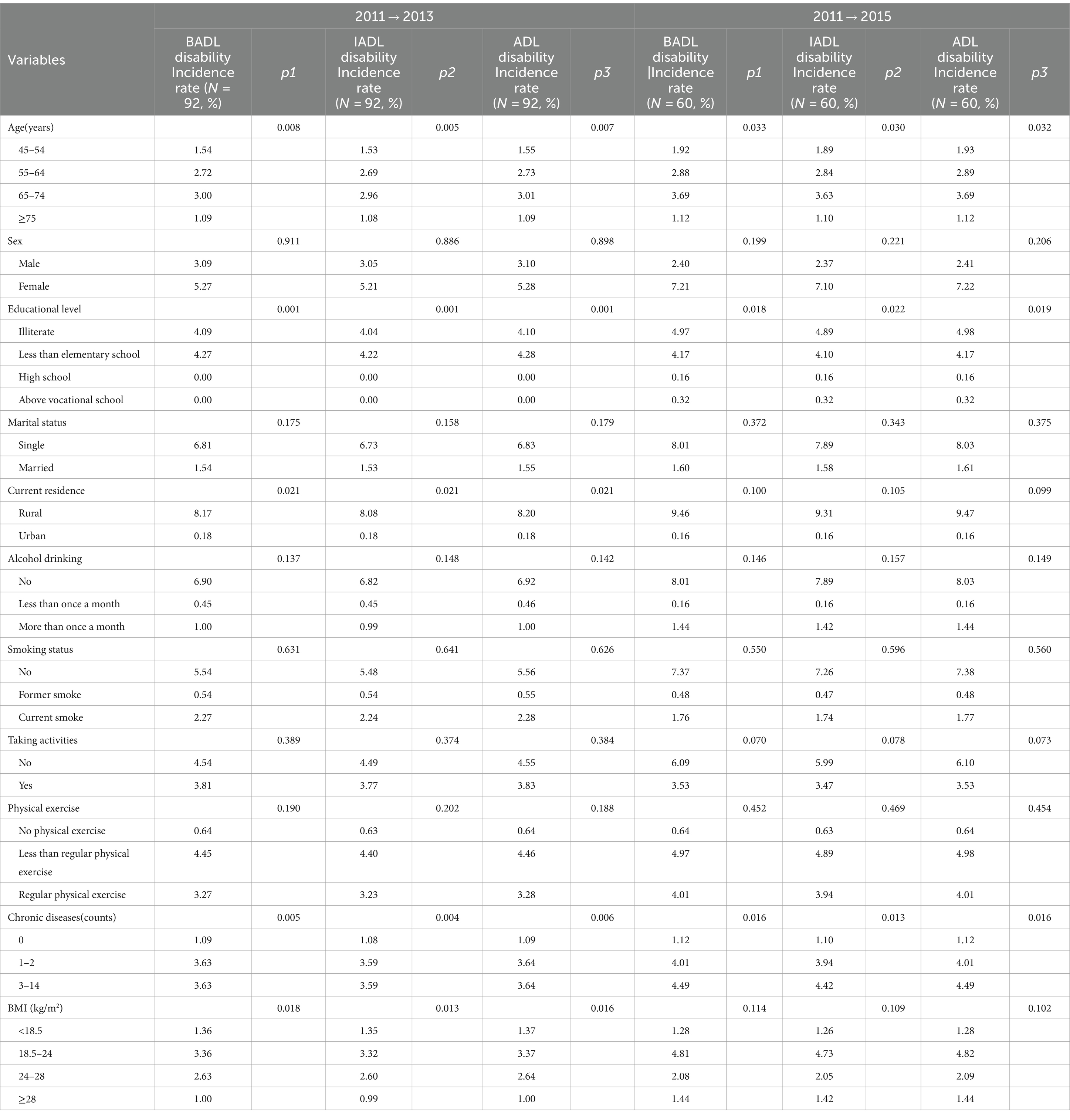
Table 3 demonstrates baseline characteristics categorized based on the subsequent onset of frailty in short-term period (2011–2013) and long-term period (2011–2015) in BADL, IADL, and ADL cohorts. In short-term period, the likelihood of developing frailty was higher among individuals aged 65–74, residing in rural areas, having chronic diseases, and with a BMI ranging from 18.5 to 24 kg/m2. In long-term period, the likelihood of developing frailty was higher among individuals aged 65–74, educational level in illiterate, and having chronic diseases.
Table 4 reports baseline characteristics classified according to the subsequent onset of BADL, IADL, and ADL disability in short-term period (2011–2013) and long-term period (2011–2015). In short-term period, the likelihood of developing BADL disability was higher among individuals aged 65–74, male, single, never smoking, having less than regular physical exercises, and having 1–2 chronic diseases. The likelihood of developing IADL disability was higher among individuals single, aged 55–64, educational level less than elementary school, having regular physical exercises, and having 1–2 chronic diseases. They tended to take no activities. The likelihood of developing ADL disability was higher among individuals aged 55–64, female, single, educational level less than elementary school, having regular physical exercises, and having 1–2 chronic diseases. They tended to never smoke and take no activities. In long-term period, the likelihood of developing BADL disability was higher among individuals aged 65–74, educational level less than elementary school, having less than regular physical exercises, and having 1–2 chronic diseases. The likelihood of developing IADL disability was higher among individuals aged 55–64, educational level less than elementary school, residing in rural areas, having less than regular physical exercises, having 1–2 chronic diseases, and with a BMI ranging from 18.5 to 24 kg/m2. The likelihood of developing ADL disability was higher among individuals aged 55–64, educational level with illiterate or above vocational school, residing in rural areas, having less than regular physical exercises, having 1–2 chronic diseases, and BMI ranging from 18.5 to 24 kg/m2.
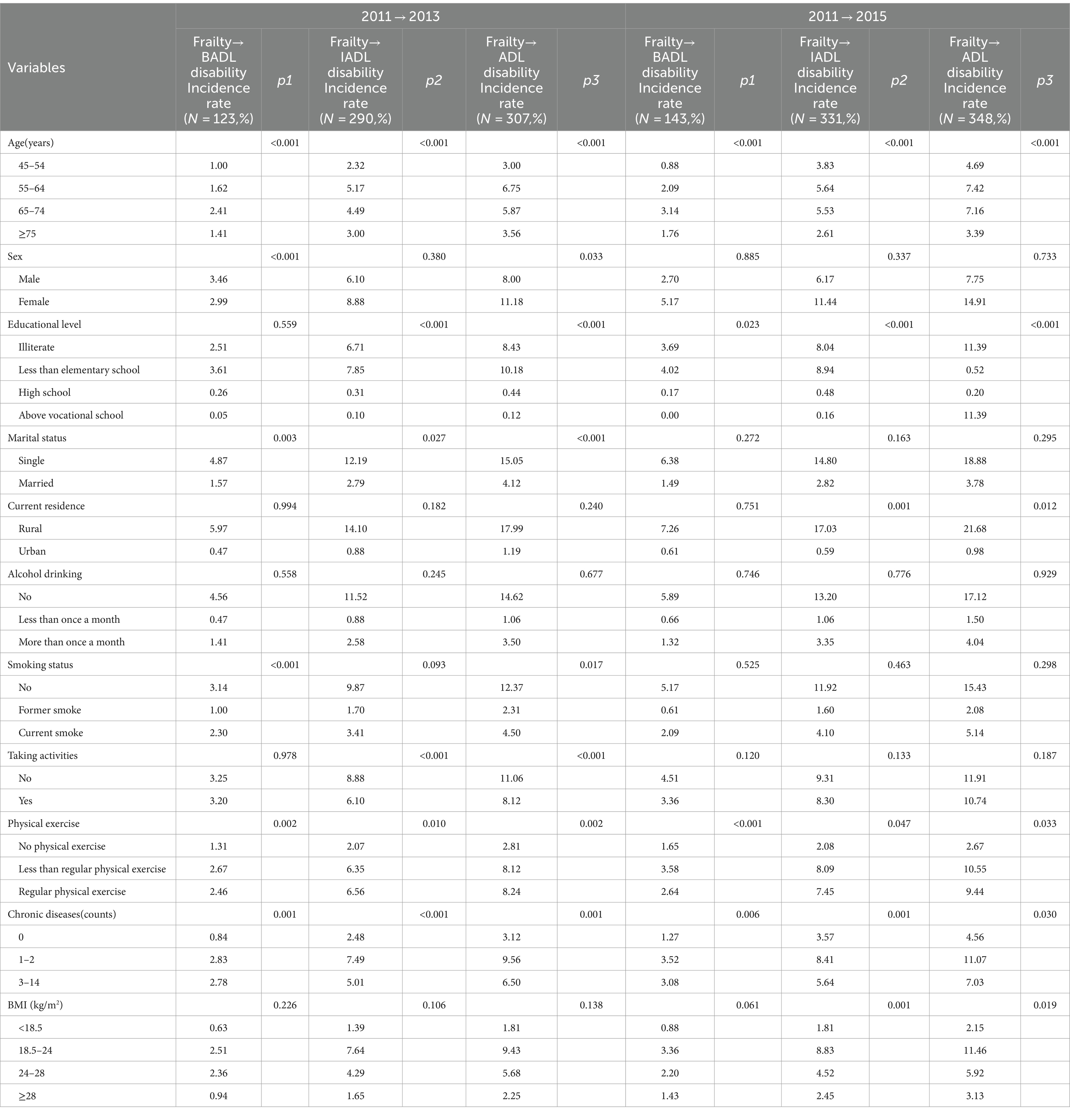
Table 4. Baseline characteristics classified according to subsequent onset of BADL, IADL, and ADL disability.
Table 5 presents the cross-sectional relationship between ADL in baseline and frailty, frailty as the dependent variable. Both BADL (OR = 6.660, 95% CI 4.519–9.815), IADL (OR = 5.950, 95% CI 4.490–7.886), and ADL (OR = 5.658, 95% CI 4.278–7.483) disability were associated with frailty significantly after controlling for covariates of sex, age, educational level, marital status, current residence, alcohol drinking, smoking status, taking activities, physical exercise, chronic diseases, and BMI (adjusted model 4).
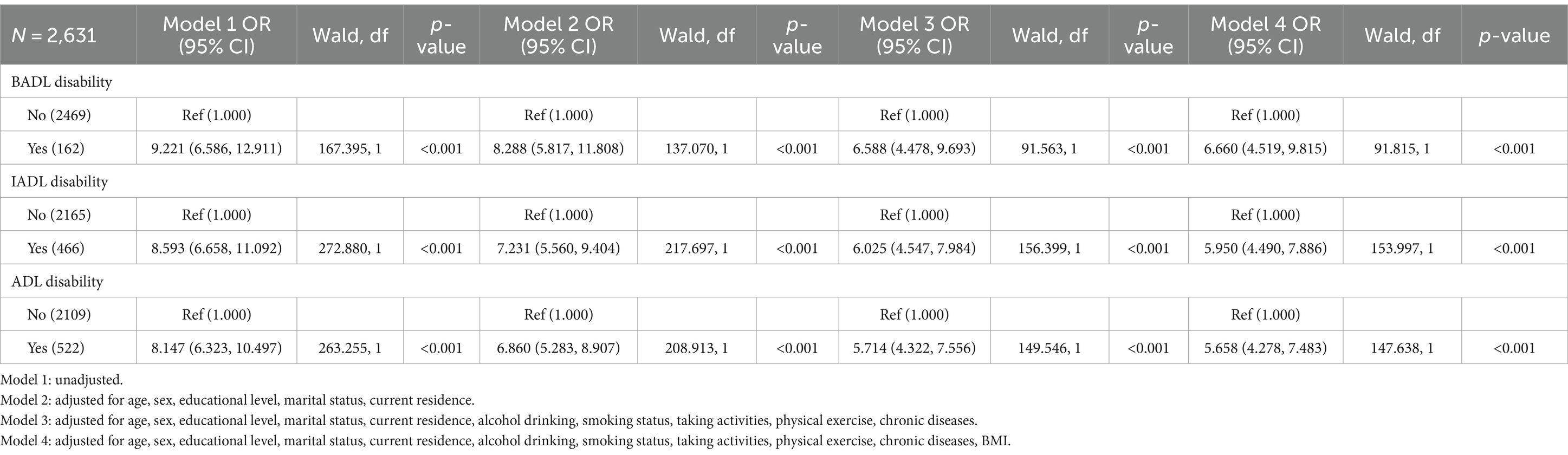
Table 5. Odds ratios (ORs) and 95% confidence interval (CIs) for frailty at baseline associated with BADL, IADL, and ADL disability at baseline.
Table 6 presents the cross-sectional relationship between baseline frailty and ADL, ADL as the dependent variable. Frailty was significantly associated with BADL (OR = 6.741, 95% CI 4.574–9.933), IADL (OR = 6.042, 95% CI 4.555–8.016) and ADL (OR = 5.735, 95% CI 4.333–7.591) disability after controlling for covariates of sex, age, marital status, educational level, current residence, alcohol drinking, smoking status, taking activities, physical exercise, chronic diseases, and BMI (adjusted model 4).
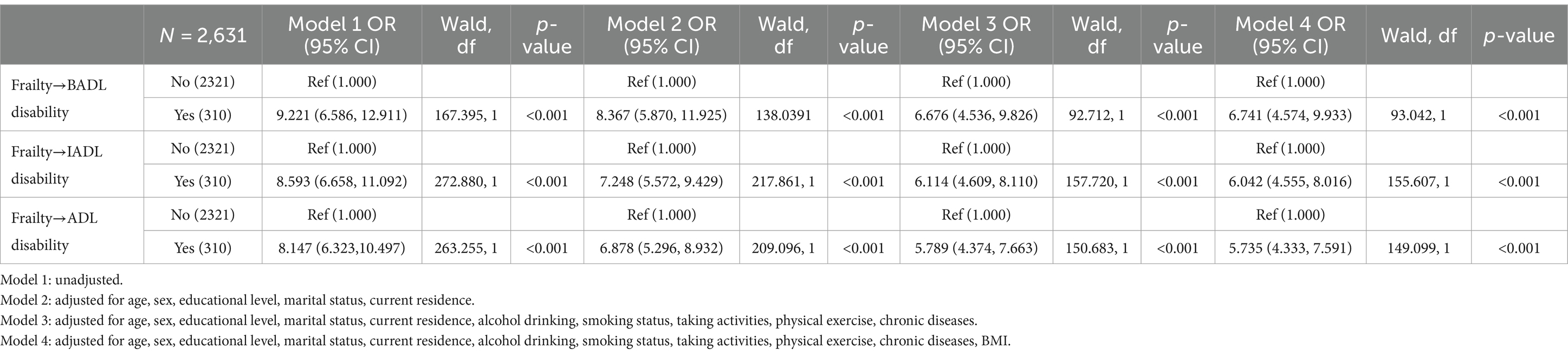
Table 6. Odds ratios (ORs) and 95% confidence interval (CIs) for BADL, IADL, and ADL disability at baseline associated with frailty at baseline.
Table 7 reports the prospective associations between baseline ADL and frailty after 2 years and 4 years of follow-up in the individuals without frailty at baseline. First, in crude analysis, IADL and ADL disability showed a significant association with incident frailty during the short-term [IADL disability: HR = 2.603 (1.563, 4.335); ADL disability: HR = 2.499 (1.533, 4.072)]. After controlling for covariates of age, sex, marital status, educational level, current residence, alcohol drinking, smoking status, taking activities, physical exercise, chronic diseases, and BMI, IADL disability [HR = 1.971 (1.150, 3.379)] and ADL disability [HR = 1.920 (1.146, 3.215)] showed a significant association with incident frailty during the short-term. Second, in crude analysis, IADL and ADL disability showed a significant association with incident frailty during the long-term [IADL disability: HR = 2.685 (1.472, 4.898); ADL disability: HR = 2.111 (1.165, 3.826)]. After controlling for covariates of age, sex, educational level, marital status, and current residence, IADL and ADL disability showed significant association with incident frailty [IADL disability: HR = 2.498 (1.349, 4.626); ADL disability: HR = 1.873 (1.018, 3.448)] (adjusted model 2). After adjusting for all covariates, IADL disability [HR = 2.056 (1.085, 3.895)] still showed a significant association with incident frailty, but the ADL disability [HR = 1.556 (0.830, 2.917)] did not show significant association with incident frailty (adjusted model 4).
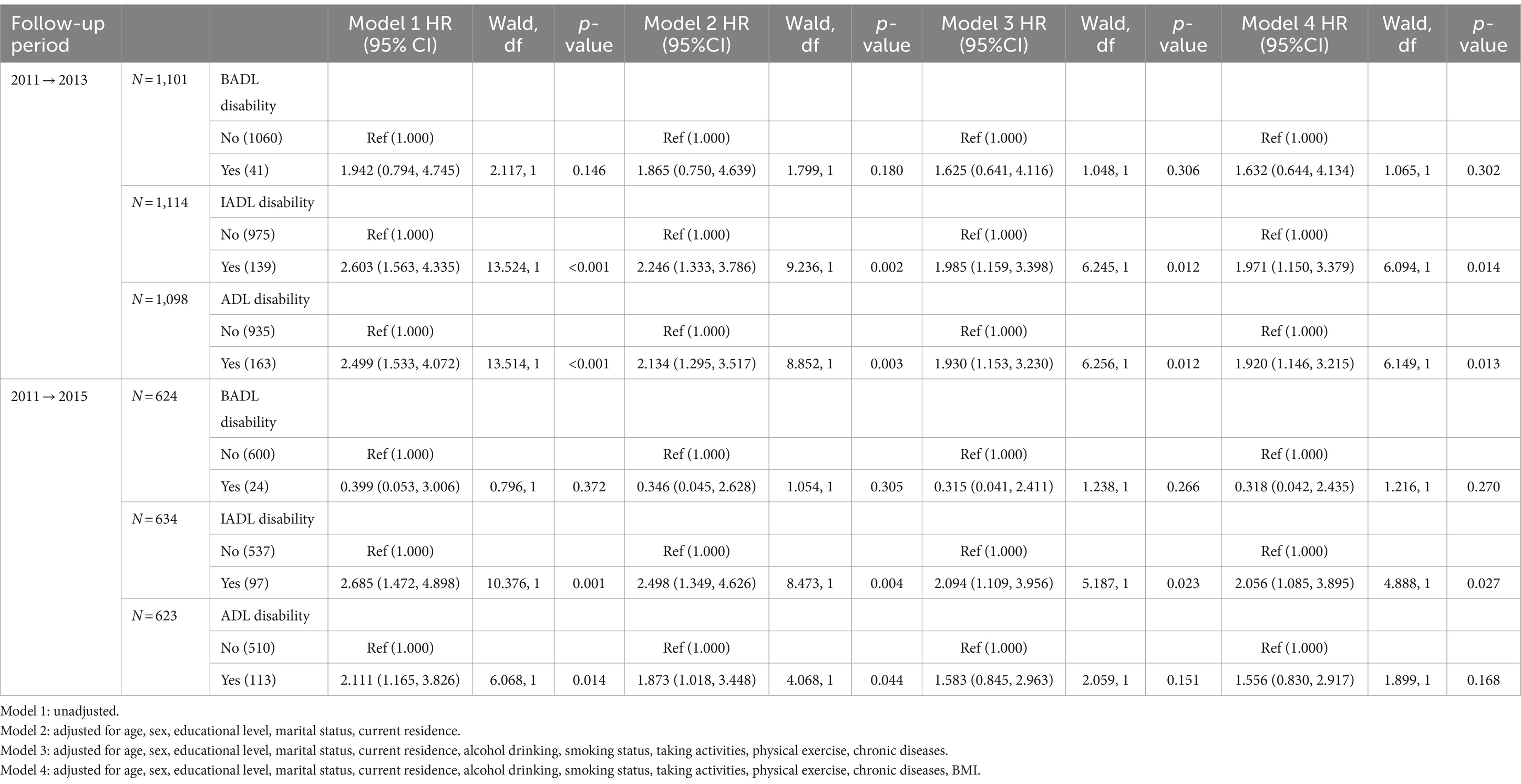
Table 7. Association between BADL, IADL, and ADL disability and incident frailty without frailty at baseline.
Table 8 reports the prospective associations between frailty in baseline and ADL after 2 years and 4 years of follow-up in individuals without ADL disability in baseline. First, in crude analysis, frailty showed a significant association with incident BADL disability [frailty: HR = 2.044 (1.256, 3.327)], IADL disability [frailty: HR = 2.069 (1.348, 3.177)] and ADL disability [frailty: HR = 1.865(1.209, 2.876)] during the short-term. After controlling for covariates of age, sex, marital status, educational level, and current residence, frailty was significantly associated with incident BADL disability [frailty: HR = 2.008 (1.210, 3.334)], IADL disability [frailty: HR = 1.740 (1.110, 2.725)], and ADL disability [frailty: HR = 1.703 (1.085, 2.671)] (adjusted model 2). After adjusting for all covariates, frailty was not significantly associated with incident BADL disability [frailty: HR = 1.573 (0.912, 2.712)], IADL disability [frailty: HR = 1.437 (0.901, 2.291)], and ADL disability [frailty: HR = 1.393 (0.873, 2.225)] during the short-term (adjusted model 4). Second, in crude analysis, frailty was significantly associated with incident BADL disability [frailty: HR = 3.042 (1.982, 4.669)], IADL disability [frailty: HR = 2.364 (1.560, 3.582)] and ADL disability [frailty: HR = 1.840 (1.187, 2.852)] during the long-term. After adjusting for all covariates, frailty was significantly associated with incident BADL disability [frailty: HR = 1.820 (1.126, 2.939)] and IADL disability [frailty: HR = 1.724 (1.103, 2.694)]. However, frailty did not show a significant association with incident ADL disability [frailty: HR = 1.351 (0.846, 2.158)] during the long-term (adjusted model 4).
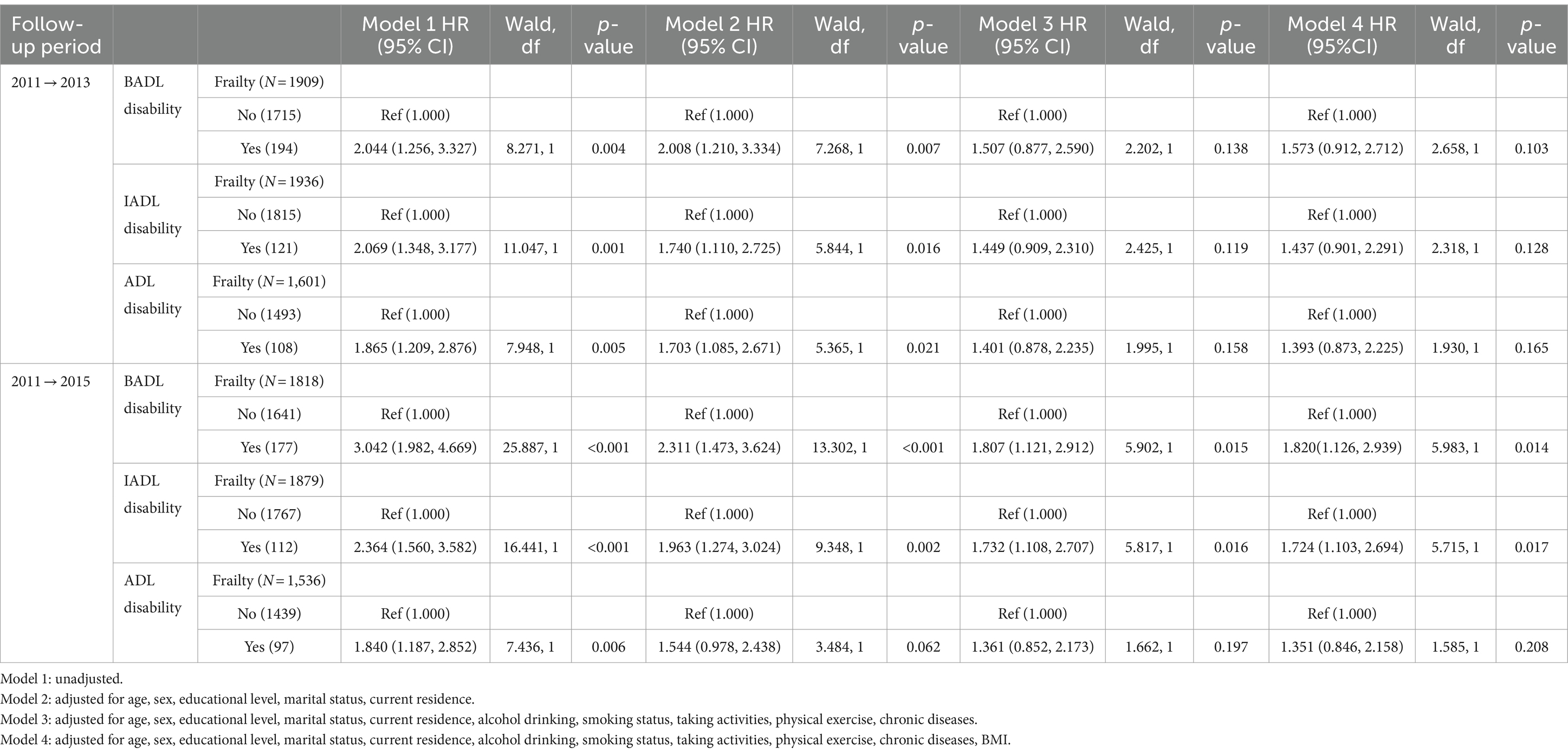
Table 8. Association between frailty and incident BADL, IADL and ADL disability without disability at baseline.
Discussion
The study based on a representative sample from CHARLS reveals ADL disability and frailty are common among middle-aged and older individuals in China (6). There is a positive, reciprocal, time-varying association between ADL disability and frailty. The present study provides the comprehensive analysis of the reciprocal associations between ADL/IADL/BADL and frailty, both longitudinally and cross-sectionally. First, there was a confirmed correlation between baseline ADL/IADL/BADL disability and frailty, as well as between baseline frailty and ADL/BADL/IADL disability. Second, ADL/IADL disability at baseline was reported to be associated with the onset of frailty significantly after a two-year follow-up. However, no significant associations were found between baseline frailty and the onset of ADL/BADL/IADL disability after a two-year follow-up. Last, Baseline IADL disability was significantly associated with the onset of frailty after a four-year follow-up. In contrast, the baseline frailty was significantly associated with the onset of BADL and IADL disability after a four-year follow-up.
The meta-analysis study (9) including cross-sectional and cohort studies, comprehensive analysis showed that frailty increased the likelihood of developing IADL and BADL disabilities. In terms of follow-up time, frailty was significantly associated with an elevated risk of disability onset in BADL and IADL after 2-5 years and above 5 years of follow-up, which was in line with our results after 4 years of follow-up; but no relevant data was found at 1–2 years of follow-up. Thus, further studies during short-term and long-term follow-up are needed to explore the dynamic association between frailty and incidence of ADL disability in middle-aged and older adults. Previous meta-analysis (30, 31) including studies from United States, the United Kingdom, Europe, Australia, Mexico, Korea and China revealed that during 1–15 years of follow-up, frailty individuals had a higher risk of both ADL and IADL disability compared to those without frailty among middle-aged and older people. In contrast, there was no significant association between frailty in baseline and the onset of ADL/BADL/IADL disability after a short-term (2-year) period in our study. The occurrence can be elucidated by the cumulative effect, demonstrating significant association between frailty and the longitudinal onset of BADL and IADL disability over a long-term (4-year) period.
Similarly, previous studies have also reported that disability in ADL/BADL/IADL is associated with frailty in cross-section (6, 34, 54, 55), which aligns with our results. Other research reported that BADL and IADL disability at baseline did not serve as predictors for the occurrence of frailty after one-year follow-up in community-dwelling older adults (1). This study is conducted in middle-aged and older people, IADL and ADL disability at baseline serve as predictors for the occurrence of frailty after short-term follow-up, IADL disability at baseline serves as predictors for the onset of frailty after long-term follow-up among middle-aged and older individuals. The occurrence can be ascribed to the cumulative effect.
In theory, two directions of this relationship are reasonable according to middle-aged and older individuals. Through various potential mechanisms, frailty can exert an impact on ADL disability. For instance, frailty individuals commonly had a higher prevalence of chronic diseases than non-frailty people (56). People with chronic conditions demonstrated higher incidence rates of disability across all ADL items (57–59), our results also supported this view. Over time, the decline of BADL such as bathing, walking, toileting, dressing, transferring and eating, as well as IADL such as performing housework, shopping, cooking, taking medicine and financial management will increase. IADL represent the functional competence required for complex everyday tasks, such as shopping or meal preparation, and are recognized to decline before BADL associated with self-care (60). Besides, frailty phenotype demonstrated independent predictability for ADL disability. The presence of frailty syndrome may serve as an etiologic factor and physiological precursor in the development of disability, owing to its primary characteristics encompassing weakness, exhaustion, weight loss, slowness, and low physical activity. Frailty was likely to primarily impact functions reliant on energy expenditure and speed of execution (e.g., mobility), frailty initially affected mobility tasks before manifesting difficulties in BADL and IADL (9, 35, 56). Additionally, a 2-year longitudinal study revealed that individuals with weakness faced a significantly incidence risk of ADL disability compared to those without weakness individuals at baseline in the older (61). A cohort study indicated that frailty acts as a significant negative factor in the recovery process of disability in ADL among newly disabled Chinese older people (62). Furthermore, frailty is characterized by a decline in the body’s reserve capacity, implying physiological decrements and adverse health outcomes can be anticipated (63). The underlying mechanism involves a multifaceted interaction, including a lower activity level, malnutrition, sarcopenia, weight loss, and difficulty maintaining homeostasis (35). This multiorgan system imbalance manifests as impaired energy metabolism and neuromuscular alterations (64), along with the growth of age, potentially leading to a decline in physical functioning as well as an increased occurrence of ADL (65). Simultaneously, existing research has reported that engagement in physical activities can reduce the risk of ADL disability and functional limitations among older individuals (66, 67), our findings also support this view, one of the characteristics of frailty is a decrease in physical activity, which would increase the risk of ADL disability.
Similarly, previous studies have also demonstrated that disability in ADL is a necessary predictor of frailty (6, 34). Individuals who had difficulty with ADL were more likely to show having frailty (55). Through a variety of underlying mechanisms, ADL disability can affect frailty. For example, having more difficulties with BADL and IADL increases the risk of frailty by limiting older people’s social participation and physical activity. People with higher levels of ADL functioning tend to experience more social participation (68), and individuals with ADL disabilities experience the opposite pattern. Disability in BADL, e.g., eating, bathing, dressing, and toileting, etc., as well as IADL, e.g., shopping, taking medicine and financial management, etc., can act as a hindrance that causes or exacerbates low level of social participation (69), may results social isolation and loneliness (70), accordingly promoting the frailty progression (71, 72). Low physical activity poses a significant risk factor for the development of frailty (73, 74). Difficulties in ADL can impede mobility and hinder flexibility, inevitably leading to insufficient levels of physical activity and reduced function of extremities, and therefore increasing the risk of physical frailty as people age (75, 76). People with ADL difficulties tend to experience more negative affect (68), which is a risk factor for frailty (77). Disability in ADL, such as continence control, housework and cooking, can serve as a stressor due to the loss of independence and decline in self-care abilities, causing or exacerbating high level of negative affect (69), and increasing the incidence risk of frailty (21, 72). The inability to perform essential ADL leads to dependence on others and/or mechanical aids, and negatively affects daily activities, safe conditions and quality of life (78), all those increase slowness, weakness, low physical activity, and exhaustion resulting in frailty (79, 80). In addition, the middle-aged and older participants with disability in ADL often suffer from chronic diseases (59), and the ability to take medicine in IADL may be restricted, which is not conducive to disease control, thus aggravating physical weakness and presenting frailty (3, 6).
Frailty is characterized by a condition of increased vulnerability to both exogenous and endogenous stressors, impacting the quality of life and raising the risk of adverse health-related outcomes for individuals (81, 82), and frailty is significantly associated with mortality (3). Frailty is described as a transition state between ADL disability and successful aging (83). Identifying potential frailty in middle-aged and older population is essential for early prevention and management. Special attention should be given to middle-aged and older person with ADL disability to prevent the incidence of their frailty. Besides, ADL disability is one independent risk factor for 7 years mortality in middle-aged and older adults in China (84), and ADL skills can facilitate successful aging (85). Frailty serves as a strong predictor for disability in ADL, while disability in ADL is also a strong predictor of frailty among middle-aged and older population. The findings of our research demonstrate that middle-aged and older individuals with ADL disability and frailty are both at high risk and require increased attention. The present study just examines the bivariate bidirectional association between frailty and ADL disability. Further studies are necessary to determine the impact of this relationship in order to break this vicious cycle.
Strengths and limitations of the study
This study possesses several strengths. It is based on a nationwide representative cohort with a relatively large sample size, which includes individuals aged ≥45 years. It explores the bidirectional association between frailty and ADL disability across two different time intervals and provides help to understand the short-term and long-term effects further. Certain limitations should be noted in the current study. Some predictors in our study, such as ADL, frailty, and disease history, were self-reported and potentially introduced partial information bias. The exclusion of some participants with incomplete data resulted in a reduced sample size and would affect the analysis results. This study did not investigate how certain lifestyles might relate to ADL disabilities, which should be carried out in the follow-up study.
Conclusion
In summary, this study established bidirectional cross-sectional and longitudinal associations between frailty and ADL using a nationwide representative sample in China. This study suggested that disability in ADL increased the risk of frailty and vice versa. They may create a vicious circle, negatively reinforcing each other. Early interventions targeting ADL disability or frailty for middle-aged and older adults will be beneficial to improving their health status. Accordingly, in the context of increasing aging, the interaction between ADL disability and frailty should be explored to prevent the development of a vicious cycle.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: https://charls.charlsdata.com/pages/data/111/zh-cn.html.
Author contributions
XiaopL: Writing – original draft, Writing – review & editing. XiaogL: Writing – review & editing. LS: Writing – review & editing. LY: Writing – review & editing. CW: Writing – review & editing. TY: Writing – review & editing. YL: Writing – review & editing. JL: Writing – review & editing. ML: Writing – review & editing. DZ: Writing – review & editing. YH: Writing – review & editing. HL: Writing – review & editing. LZ: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. CHARLS was supported by the NSFC (70910107022 and 71130002) and National Institute on Aging (R03-TW008358-01 and R01-AG037031-03S1) and World Bank (7159234).
Acknowledgments
We thank the members of the CHARLS as well as all participants for their contribution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ADL, activities of daily living; BADL, basic activities of daily living; IADL, instrumental activities of daily living; CHARLS, China Health and Retirement Longitudinal Study; BMI, Body mass index; CI, Confidence interval; OR, Odds ratios; HR, hazard ratio
References
1. Costenoble, A, Knoop, V, Debain, A, Bautmans, I, Van Laere, S, Lieten, S, et al. Transitions in robust and Prefrail octogenarians after 1 year: the influence of activities of daily living, social participation, and psychological resilience on the frailty state. BMC Geriatr. (2023) 23:485. doi: 10.1186/s12877-023-04178-5
2. Zhou, Q, Li, Y, Gao, Q, Yuan, H, Sun, L, Xi, H, et al. Prevalence of frailty among Chinese community-dwelling older adults: a systematic review and Meta-analysis. Int J Public Health. (2023) 68:1605964. doi: 10.3389/ijph.2023.1605964
3. Hanlon, P, Nicholl, BI, Jani, BD, Lee, D, McQueenie, R, and Mair, FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 Uk biobank participants. Lancet Public Health. (2018) 3:e323–32. doi: 10.1016/s2468-2667(18)30091-4
4. Santos-Eggimann, B, Cuénoud, P, Spagnoli, J, and Junod, J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. (2009) 64A:675–81. doi: 10.1093/gerona/glp012
5. Fan, J, Yu, C, Guo, Y, Bian, Z, Sun, Z, Yang, L, et al. Frailty index and all-cause and cause-specific mortality in Chinese adults: a prospective cohort study. Lancet Public Health. (2020) 5:e650–60. doi: 10.1016/s2468-2667(20)30113-4
6. He, B, Ma, Y, Wang, C, Jiang, M, Geng, C, Chang, X, et al. Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and Meta-analysis. J Nutr Health Aging. (2019) 23:442–50. doi: 10.1007/s12603-019-1179-9
7. Wu, C, Smit, E, Xue, QL, and Odden, MC. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. (2017) 73:102–8. doi: 10.1093/gerona/glx098
8. Sun, J, Kong, X, Li, H, Chen, J, Yao, Q, Li, H, et al. Does social participation decrease the risk of frailty? Impacts of diversity in frequency and types of social participation on frailty in middle-aged and older populations. BMC Geriatr. (2022) 22:553. doi: 10.1186/s12877-022-03219-9
9. Vermeiren, S, Vella-Azzopardi, R, Beckwée, D, Habbig, AK, Scafoglieri, A, Jansen, B, et al. Frailty and the prediction of negative health outcomes: a Meta-analysis. J Am Med Dir Assoc. (2016) 17:1163.e1–1163.e17. doi: 10.1016/j.jamda.2016.09.010
10. Liu, KY, and Mukadam, N. Frailty and dementia: what can the body tell us about the brain? Int Psychogeriatr. (2021) 33:1001–3. doi: 10.1017/s1041610220004160
11. Bartosch, PS, Kristensson, J, McGuigan, FE, and Akesson, KE. Frailty and prediction of recurrent falls over 10 years in a community cohort of 75-year-old women. Aging Clin Exp Res. (2020) 32:2241–50. doi: 10.1007/s40520-019-01467-1
12. Mendiratta, P, Schoo, C, and Latif, R. Clinical frailty scale. Statpearls. Treasure Island (FL) ineligible companies. Disclosure: Caroline Schoo declares no relevant financial relationships with ineligible companies. Disclosure: Rafay Latif declares no relevant financial relationships with ineligible companies. St. Petersburg, FL: StatPearls Publishing (2023).
13. Pashmdarfard, M, and Azad, A. Assessment tools to evaluate activities of daily living (Adl) and instrumental activities of daily living (Iadl) in older adults: a systematic review. Med J Islam Repub Iran. (2020) 34:33. doi: 10.34171/mjiri.34.33
14. Zhang, Y, Xiong, Y, Yu, Q, Shen, S, Chen, L, and Lei, X. The activity of daily living (Adl) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
15. Gao, Y, Du, L, Cai, J, and Hu, T. Effects of functional limitations and activities of daily living on the mortality of the older people: a cohort study in China. Front Public Health. (2022) 10:1098794. doi: 10.3389/fpubh.2022.1098794
16. Gill, TM, Robison, JT, and Tinetti, ME. Difficulty and dependence: two components of the disability continuum among community-living older persons. Ann Intern Med. (1998) 128:96–101. doi: 10.7326/0003-4819-128-2-199801150-00004
17. Stineman, MG, Xie, D, Pan, Q, Kurichi, JE, Zhang, Z, Saliba, D, et al. All-cause 1-, 5-, and 10-year mortality in elderly people according to activities of daily living stage. J Am Geriatr Soc. (2012) 60:485–92. doi: 10.1111/j.1532-5415.2011.03867.x
18. Unsar, S, Dindar, I, and Kurt, S. Activities of daily living, quality of life, social support and depression levels of elderly individuals in Turkish society. J. Pak. Med. Assoc. (2015) 65:642–6.
19. Connolly, D, Garvey, J, and McKee, G. Factors associated with Adl/Iadl disability in community dwelling older adults in the Irish longitudinal study on ageing (Tilda). Disabil Rehabil. (2017) 39:809–16. doi: 10.3109/09638288.2016.1161848
20. Sjölund, BM, Wimo, A, Engström, M, and von Strauss, E. Incidence of ADL disability in older persons, physical activities as a protective factor and the need for informal and formal care--results from the SNAC-N project. PLoS One. (2015) 10:e0138901. doi: 10.1371/journal.pone.0138901
21. Al Snih, S, Graham, JE, Ray, LA, Samper-Ternent, R, Markides, KS, and Ottenbacher, KJ. Frailty and incidence of activities of daily living disability among older Mexican Americans. J Rehabil Med. (2009) 41:892–7. doi: 10.2340/16501977-0424
22. Liu, H, Ma, Y, Lin, L, Sun, Z, Li, Z, and Jiang, X. Association between activities of daily living and depressive symptoms among older adults in China: evidence from the Charls. Front Public Health. (2023) 11:1249208. doi: 10.3389/fpubh.2023.1249208
23. Hu, WH, Liu, YY, Yang, CH, Zhou, T, Yang, C, Lai, YS, et al. Developing and validating a Chinese multimorbidity-weighted index for middle-aged and older community-dwelling individuals. Age Ageing. (2022) 51:afab274. doi: 10.1093/ageing/afab274
24. Weng, Y, and Yang, X. Fertility behaviors and mid-late-life health status in China: from a life-course perspective. Soc Sci Med. (2023) 338:116314. doi: 10.1016/j.socscimed.2023.116314
25. Knoll, K, Rhee, Y, Hamm, JM, Hammer, KDP, Heimbuch, H, Holloway, J, et al. The prevalence and trends of instrumental activities of daily living impairments in the United States from 2008-2018. J Alzheimers Dis Rep. (2023) 7:271–8. doi: 10.3233/adr-220107
26. da Rosa, PPS, Marques, LP, Corrêa, VP, De Oliveira, C, and Schneider, IJC. Is the combination of depression symptoms and multimorbidity associated with the increase of the prevalence of functional disabilities in Brazilian older adults? A cross-sectional study. Front Aging. (2023) 4:1188552. doi: 10.3389/fragi.2023.1188552
27. Muneera, K, Muhammad, T, Pai, M, Ahmed, W, and Althaf, S. Associations between intrinsic capacity, functional difficulty, and fall outcomes among older adults in India. Sci Rep. (2023) 13:9829. doi: 10.1038/s41598-023-37097-x
28. Gong, B, Shang, S, and Wu, C. Association between cognitive declines and disability in activities of daily living in older adults with Copd: evidence from the China health and retirement longitudinal study. BMJ Open. (2020) 10:e040098. doi: 10.1136/bmjopen-2020-040098
29. Neo, J, Fettes, L, Gao, W, Higginson, IJ, and Maddocks, M. Disability in activities of daily living among adults with Cancer: a systematic review and Meta-analysis. Cancer Treat Rev. (2017) 61:94–106. doi: 10.1016/j.ctrv.2017.10.006
30. Kojima, G . Quick and simple frail scale predicts incident activities of daily living (Adl) and instrumental Adl (Iadl) disabilities: a systematic review and Meta-analysis. J Am Med Dir Assoc. (2018) 19:1063–8. doi: 10.1016/j.jamda.2018.07.019
31. Kojima, G . Frailty as a predictor of disabilities among community-dwelling older people: a systematic review and Meta-analysis. Disabil Rehabil. (2017) 39:1897–908. doi: 10.1080/09638288.2016.1212282
32. Hirase, T, Kataoka, H, Nakano, J, Inokuchi, S, Sakamoto, J, and Okita, M. Impact of frailty on chronic pain, activities of daily living and physical activity in community-dwelling older adults: a cross-sectional study. Geriatr Gerontol Int. (2018) 18:1079–84. doi: 10.1111/ggi.13314
33. Galluzzo, L, Noale, M, Maggi, S, Feraldi, A, Baldereschi, M, Di Carlo, A, et al. Frailty prevalence, incidence, and association with incident disability in the Italian longitudinal study on aging. Gerontology. (2023) 69:249–60. doi: 10.1159/000525581
34. Xu, R, Li, Q, Guo, F, Zhao, M, and Zhang, L. Prevalence and risk factors of frailty among people in rural areas: a systematic review and Meta-analysis. BMJ Open. (2021) 11:e043494. doi: 10.1136/bmjopen-2020-043494
35. Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.m146
36. Theou, O, Cann, L, Blodgett, J, Wallace, LM, Brothers, TD, and Rockwood, K. Modifications to the frailty phenotype criteria: systematic review of the current literature and investigation of 262 frailty phenotypes in the survey of health, ageing, and retirement in Europe. Ageing Res Rev. (2015) 21:78–94. doi: 10.1016/j.arr.2015.04.001
37. Steptoe, A, Breeze, E, Banks, J, and Nazroo, J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol. (2013) 42:1640–8. doi: 10.1093/ije/dys168
38. Veronese, N, Solmi, M, Maggi, S, Noale, M, Sergi, G, Manzato, E, et al. Frailty and incident depression in community-dwelling older people: results from the Elsa study. Int J Geriatr Psychiatry. (2017) 32:e141–9. doi: 10.1002/gps.4673
39. Xu, W, Li, YX, and Wu, C. Incidence of frailty among community-dwelling older adults: a nationally representative profile in China. BMC Geriatr. (2019) 19:378. doi: 10.1186/s12877-019-1393-7
40. Yaka, E, Keskinoglu, P, Ucku, R, Yener, GG, and Tunca, Z. Prevalence and risk factors of depression among community dwelling elderly. Arch Gerontol Geriatr. (2014) 59:150–4. doi: 10.1016/j.archger.2014.03.014
41. Zhou, BF . Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases--report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. (2002) 15:245–52.
42. Zhang, L, Li, JL, Zhang, LL, Guo, LL, Li, H, and Li, D. Association and interaction analysis of body mass index and triglycerides level with blood pressure in elderly individuals in China. Biomed Res Int. (2018) 2018:8934531–4. doi: 10.1155/2018/8934534
43. Zhang, L, Li, JL, Zhang, LL, Guo, LL, Li, H, Yan, W, et al. Relationship between adiposity parameters and cognition: the "fat and jolly" hypothesis in middle-aged and elderly people in China. Medicine. (2019) 98:e14747. doi: 10.1097/md.0000000000014747
44. Zhang, L, Li, JL, Zhang, LL, Guo, LL, Li, H, and Li, D. Body mass index and serum uric acid level: individual and combined effects on blood pressure in middle-aged and older individuals in China. Medicine. (2020) 99:e19418. doi: 10.1097/md.0000000000019418
45. Zhang, L, Liu, K, Li, H, Li, D, Chen, Z, Zhang, LL, et al. Relationship between body mass index and depressive symptoms: the "fat and jolly" hypothesis for the middle-aged and elderly in China. BMC Public Health. (2016) 16:1201. doi: 10.1186/s12889-016-3864-5
46. Chang, HH, and Yen, ST. Association between obesity and depression: evidence from a longitudinal sample of the elderly in Taiwan. Aging Ment Health. (2012) 16:173–80. doi: 10.1080/13607863.2011.605053
47. Zhang, L, Li, JL, Zhang, LL, Guo, LL, Li, H, and Li, D. No association between C-reactive protein and depressive symptoms among the middle-aged and elderly in China: evidence from the China health and retirement longitudinal study. Medicine. (2018) 97:e12352. doi: 10.1097/md.0000000000012352
48. Zhang, L, Li, JL, Guo, LL, Li, H, Li, D, and Xu, G. The interaction between serum uric acid and triglycerides level on blood pressure in middle-aged and elderly individuals in China: result from a large National Cohort Study. BMC Cardiovasc Disord. (2020) 20:174. doi: 10.1186/s12872-020-01468-3
49. Zhang, L, Yang, L, Wang, C, Yuan, T, Zhang, D, Wei, H, et al. Combined effect of famine exposure and obesity parameters on hypertension in the Midaged and older adult: a population-based cross-sectional study. Biomed Res Int. (2021) 2021:5594717–8. doi: 10.1155/2021/5594718
50. Zhang, L, Yang, L, Wang, C, Yuan, T, Zhang, D, Wei, H, et al. Individual and combined association analysis of famine exposure and serum uric acid with hypertension in the mid-aged and older adult: a population-based cross-sectional study. BMC Cardiovasc Disord. (2021) 21:420. doi: 10.1186/s12872-021-02230-z
51. Liu, H, Yang, X, Guo, LL, Li, JL, Xu, G, Lei, Y, et al. Frailty and incident depressive symptoms during short- and long-term follow-up period in the middle-aged and elderly: findings from the Chinese Nationwide cohort study. Front Psych. (2022) 13:848849. doi: 10.3389/fpsyt.2022.848849
52. Wang, C, Wang, J, Wan, R, Yuan, T, Yang, L, Zhang, D, et al. Relationship between baseline and changed serum uric acid and the incidence of type 2 diabetes mellitus: a National Cohort Study. Front Public Health. (2023) 11:1170792. doi: 10.3389/fpubh.2023.1170792
53. Cheng, J, Sun, J, Yao, K, Xu, M, and Cao, Y. A variable selection method based on mutual information and variance inflation factor. Spectrochim Acta A Mol Biomol Spectrosc. (2022) 268:120652. doi: 10.1016/j.saa.2021.120652
54. Manrique-Espinoza, B, Salinas-Rodríguez, A, Salgado de Snyder, N, Moreno-Tamayo, K, Gutiérrez-Robledo, LM, and Avila-Funes, JA. Frailty and social vulnerability in Mexican deprived and rural settings. J Aging Health. (2016) 28:740–52. doi: 10.1177/0898264315609909
55. Feng, Z, Lugtenberg, M, Franse, C, Fang, X, Hu, S, Jin, C, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: a systematic review of longitudinal studies. PLoS One. (2017) 12:e0178383. doi: 10.1371/journal.pone.0178383
56. Huang, ST, Tange, C, Otsuka, R, Nishita, Y, Peng, LN, Hsiao, FY, et al. Subtypes of physical frailty and their long-term outcomes: a longitudinal cohort study. J Cachexia Sarcopenia Muscle. (2020) 11:1223–31. doi: 10.1002/jcsm.12577
57. Sharma, P, Maurya, P, and Muhammad, T. Number of chronic conditions and associated functional limitations among older adults: cross-sectional findings from the longitudinal aging study in India. BMC Geriatr. (2021) 21:664. doi: 10.1186/s12877-021-02620-0
58. Fong, JH . Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr. (2019) 19:323. doi: 10.1186/s12877-019-1348-z
59. Klinedinst, TC, Terhorst, L, and Rodakowski, J. Chronic condition clusters and associated disability over time. J Multimorb Comorb. (2022) 12:26335565221093569. doi: 10.1177/26335565221093569
60. Coventry, PA, McMillan, D, Clegg, A, Brown, L, van der Feltz-Cornelis, C, Gilbody, S, et al. Frailty and depression predict instrumental activities of daily living in older adults: a population-based longitudinal study using the Care75+ cohort. PLoS One. (2020) 15:e0243972. doi: 10.1371/journal.pone.0243972
61. Duchowny, KA, Clarke, PJ, and Peterson, MD. Muscle weakness and physical disability in older Americans: longitudinal findings from the U.S. health and retirement study. J Nutr Health Aging. (2018) 22:501–7. doi: 10.1007/s12603-017-0951-y
62. Xu, W, Li, YX, Hu, Y, and Wu, C. Association of Frailty with recovery from disability among community-dwelling Chinese older adults: China health and retirement longitudinal study. BMC Geriatr. (2020) 20:119. doi: 10.1186/s12877-020-01519-6
63. Fried, LP, Ferrucci, L, Darer, J, Williamson, JD, and Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. (2004) 59:M255–63. doi: 10.1093/gerona/59.3.m255
64. Fedarko, NS . The biology of aging and frailty. Clin Geriatr Med. (2011) 27:27–37. doi: 10.1016/j.cger.2010.08.006
65. Wang, DXM, Yao, J, Zirek, Y, Reijnierse, EM, and Maier, AB. Muscle mass, strength, and physical performance predicting activities of daily living: a Meta-analysis. J Cachexia Sarcopenia Muscle. (2020) 11:3–25. doi: 10.1002/jcsm.12502
66. Cunningham, CROS, Caserotti, P, and Tully, MA. Consequences of physical inactivity in older adults: a systematic review of reviews and Meta-analyses. Scand J Med Sci Sports. (2020) 30:816–27. doi: 10.1111/sms.13616
67. de Souto Barreto, P, Morley, JE, Chodzko-Zajko, W, H Pitkala, K, Weening-Djiksterhuis, E, Rodriguez-Mañas, L, et al. Recommendations on physical activity and exercise for older adults living in long-term care facilities: a taskforce report. J Am Med Dir Assoc. (2016) 17:381–92. doi: 10.1016/j.jamda.2016.01.021
68. Huang, YW, Chien, CH, Chiang, YH, Liu, CY, and Huang, XY. Social participation, positive affect, and negative affect in postoperative patients with hip fractures: a cross-sectional study. J Health Psychol. (2023) 29:303–16. doi: 10.1177/13591053231200318
69. Beltz, S, Gloystein, S, Litschko, T, Laag, S, and van den Berg, N. Multivariate analysis of independent determinants of Adl/Iadl and quality of life in the elderly. BMC Geriatr. (2022) 22:894. doi: 10.1186/s12877-022-03621-3
70. Kotian, DB, Mathews, M, Parsekar, SS, Nair, S, Binu, VS, and Subba, SH. Factors associated with social isolation among the older people in India. J Geriatr Psychiatry Neurol. (2018) 31:271–8. doi: 10.1177/0891988718796338
71. Ge, L, Yap, CW, and Heng, BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. (2022) 22:26. doi: 10.1186/s12877-021-02745-2
72. Fang, B, Huang, J, Zhao, X, Liu, H, Chen, B, and Zhang, Q. Concurrent and lagged associations of social participation and frailty among older adults. Health Soc Care Community. (2022) 30:e4812–20. doi: 10.1111/hsc.13888
73. Sobhani, A, Sharifi, F, Fadayevatan, R, Kamrani, AAA, Moodi, M, Khorashadizadeh, M, et al. Low physical activity is the strongest factor associated with frailty phenotype and frailty index: data from baseline phase of Birjand longitudinal aging study (Blas). BMC Geriatr. (2022) 22:498. doi: 10.1186/s12877-022-03135-y
74. Zulfiqar, AA, Lorenzo-Villalba, N, Peixoto, A, Rio, J, and Gillibert, A. Frailty of the elderly and physical activity in general practice: a prospective study. Rev Epidemiol Sante Publique. (2020) 68:282–7. doi: 10.1016/j.respe.2020.06.006
75. Ottenbacher, KJ, Graham, JE, Al Snih, S, Raji, M, Samper-Ternent, R, Ostir, GV, et al. Mexican Americans and frailty: findings from the Hispanic established populations epidemiologic studies of the elderly. Am J Public Health. (2009) 99:673–9. doi: 10.2105/ajph.2008.143958
76. Blodgett, J, Theou, O, Kirkland, S, Andreou, P, and Rockwood, K. The association between sedentary behaviour, moderate-vigorous physical activity and frailty in Nhanes cohorts. Maturitas. (2015) 80:187–91. doi: 10.1016/j.maturitas.2014.11.010
77. Mulasso, A, Argiolu, L, Roppolo, M, Azucar, D, and Rabaglietti, E. Emotion experience and frailty in a sample of Italian community-dwelling older adults. Clin Interv Aging. (2017) 12:2017–24. doi: 10.2147/cia.s147121
78. Edemekong, PF, Bomgaars, DL, Sukumaran, S, and Schoo, C. Activities of daily living. Statpearls. Treasure Island (FL) ineligible companies. Disclosure: Deb Bomgaars declares no relevant financial relationships with ineligible companies. Disclosure: Sukesh Sukumaran declares no relevant financial relationships with ineligible companies. Disclosure: Caroline Schoo declares no relevant financial relationships with ineligible companies. St. Petersburg, FL: StatPearls Publishing (2024).
79. Papathanasiou, IV, Rammogianni, A, Papagiannis, D, Malli, F, Mantzaris, DC, Tsaras, K, et al. Frailty and quality of life among community-dwelling older adults. Cureus. (2021) 13:e13049. doi: 10.7759/cureus.13049
80. Provencher, V, Béland, F, Demers, L, Desrosiers, J, Bier, N, Ávila-Funes, JA, et al. Are frailty components associated with disability in specific activities of daily living in community-dwelling older adults? A multicenter Canadian study. Arch Gerontol Geriatr. (2017) 73:187–94. doi: 10.1016/j.archger.2017.07.027
81. Liang, XY, Zhou, QG, Wang, LY, Wang, SL, Xie, YL, Yang, X, et al. Prevalence of frailty and related factors in middle-aged and elderly people in island and mountainous areas of Taizhou, Zhejiang Province. Zhonghua Liu Xing Bing Xue Za Zhi. (2024) 45:139–47. doi: 10.3760/cma.j.cn112338-20230720-00026
82. Rolfson, D . Successful aging and frailty: a systematic review. Geriatrics (Basel, Switzerland). (2018) 3:79. doi: 10.3390/geriatrics3040079
83. Cesari, M, Prince, M, Thiyagarajan, JA, De Carvalho, IA, Bernabei, R, Chan, P, et al. Frailty: an emerging public health priority. J Am Med Dir Assoc. (2016) 17:188–92. doi: 10.1016/j.jamda.2015.12.016
84. Hu, Z, Zheng, B, Kaminga, AC, Zhou, F, and Xu, H. Association between functional limitations and incident cardiovascular diseases and all-cause mortality among the middle-aged and older adults in China: a population-based prospective cohort study. Front Public Health. (2022) 10:751985. doi: 10.3389/fpubh.2022.751985
Keywords: frailty, activities of daily living, bidirectional relationship, middle-aged and older adults, basic activities of daily living, instrumental activities of daily living
Citation: Li X, Li X, Sun L, Yang L, Wang C, Yuan T, Lei Y, Li J, Liu M, Zhang D, Hua Y, Liu H and Zhang L (2024) The bidirectional relationship between activities of daily living and frailty during short-and long-term follow-up period among the middle-aged and older population: findings from the Chinese nationwide cohort study. Front. Public Health. 12:1382384. doi: 10.3389/fpubh.2024.1382384
Edited by:
Xiaolei Liu, Sichuan University, ChinaReviewed by:
Cheng-Hong Yang, National Kaohsiung University of Science and Technology, TaiwanXun Luo, Kerry Rehabilitation Medicine Research Institute, China
Shinji Takahashi, Tohoku Gakuin University, Japan
Copyright © 2024 Li, Li, Sun, Yang, Wang, Yuan, Lei, Li, Liu, Zhang, Hua, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Zhang, eWFvcmFuMjAwOEAxNjMuY29t
 Xiaoping Li
Xiaoping Li Xiaoguang Li2
Xiaoguang Li2 Ting Yuan
Ting Yuan Dongmei Zhang
Dongmei Zhang Lin Zhang
Lin Zhang