- 1Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
- 2HIV/AIDS Prevention Treatment and Care, Amhara Regional State Health Bureau, Bahir Dar, Ethiopia
Background: The COVID-19 pandemic has presented new challenges to adhering to ART, and its influence on adherence and related factors has not been thoroughly studied. This study examines ART adherence and its associated factors during the COVID-19 pandemic.
Methods: A cross-sectional study was conducted on HIV-positive individuals receiving care and treatment in public health facilities. A total of 612 participants were selected using a multi-stage sampling procedure. Data were collected through interviewer-administered questionnaires and chart reviews. We used Epi-data for data entry and Stata for data analysis.
Results: Good adherence to antiretroviral therapy in this study was 76.5% (95% CI, 72.9, 79.7). Divorced marital status (AOR = 0.45,95%CI:0.22,0.90), regular follow-up (AOR = 3.01,95%CI:1.81,5.01), adherence counseling and information in the context of COVID-19 pandemic (AOR = 2.57,95%CI:1.63,4.08), and knowledge about ART (AOR = 1.81,95%CI:1.11,2.94) were significantly associated with adherence to antiretroviral therapy.
Conclusion: The observed adherence rate in this study was lower than the World Health Organization recommendation and previous studies. The study highlighted the importance of addressing adherence to ART among HIV-positive adults during the COVID-19 pandemic and other upcoming emerging and reemerging outbreaks. Strategies to improve adherence should consider factors such as marital status, regular follow-up, provision of counseling and information, and enhancing knowledge about ART.
Background
As per the Federal HIV/AIDS Prevention and Control Office (FHAPCO) in Ethiopia, there is an estimated total of 613,000 people living with HIV (PLHIV) in the country. Among them, 30% are reported from the Amara region (1). The World Health Organization (WHO) advises an ART adherence rate of at least 95% to prevent the emergence of drug-resistant strains and transmission. Unfortunately, the reported adherence rates are frequently below this recommended threshold (2).
The emergence of the COVID-19 pandemic has added a health burden to PLHIV (3). In the era of the COVID-19 pandemic, the provision of ART services may be affected due to overwhelmed healthcare systems, interruptions in services, and reduced clinic visits by PLHIV due to fear or financial constraints, resulting in suboptimal adherence to treatment. There is limited available data on PLHIV in the context of the ongoing SARS-CoV-2 pandemic (4). Managing COVID-19 directly impacts the local HIV prevention and care landscape, which heavily relies on digital HIV intervention programs (5). Owing to their immunosuppressed state, PLHIV are presumed to be more susceptible to COVID-19 infection and may experience worse clinical outcomes (6).
Factors such as the adverse effects of certain ARVs, lack of social support, stigma, inadequate knowledge about ART, opportunistic infections, and limited access to healthcare services significantly contribute to challenges in adhering to ART (7–12).
The COVID-19 pandemic disrupted the supply chain of HIV-related products from the global to local levels. This disruption may exacerbate the occurrence of severe illnesses and increase mortality rates (13). Investigating if the COVID-19 pandemic affects adherence to antiretroviral treatment is essential (14).
There is limited understanding of how COVID-19 affects the clinical progression of individuals living with HIV in Ethiopia. Although various studies have explored factors related to adherence to ART, there is a lack of documentation on the impact of COVID-19 pandemic-related factors on ART adherence. Therefore, the primary objective of this study was to evaluate the influence of the COVID-19 pandemic on ART adherence and its associated factors among adults living with HIV who receive care and treatment at public health facilities.
Methods
Study designe and setting
An institutional-based cross-sectional study was carried out among adult clients receiving ART follow-ups at public health facilities in Bahir Dar city from November 29 to December 28, 2020. Bahir Dar’s city administration includes three public hospitals and ten public health centers, all offering comprehensive HIV prevention, treatment, and care services. The total count of clients receiving ART in Bahir Dar health facilities was 14,502.
Data collection and participants
The sample size was determined using EPI info software. Assuming a 95% confidence level, a 5% margin of error, and a proportion of good adherance 56% (15). An additional 10% was added to account for non-response and incomplete follow-up charts. Additionally, a design effect of 1.5 was used, resulting in 626 study participants. Multi-stage sampling was employed to select participants. The study included two hospitals and four health centers, chosen through a simple random (lottery) method from a pool of three hospitals and nine health centers, respectively. The sample size was then allocated proportionally to each selected health facility based on the number of adults currently undergoing ART treatment. Participants were selected using a systematic sampling technique with an interval of every fourth individual. The first participant to arrive at the ART unit for follow-up on each day and at each facility was selected as the initial interviewee. Subsequent participants were selected at every fourth interval based on their order of arrival until the required sample size for each selected health facility was achieved. To assess adherence to ART, good adherence was defined as taking at least 95% [≤ 2 missed drug doses out of 30 or ≤ 3 missed drug doses out of 60 doses (16)] of prescribed medication within one month before data collection (2, 17). Adequate knowledge was determined based on respondents correctly answering questions that assess their knowledge at or above the mean level (12). Problematic alcohol use was identified if the respondent scored ≥2 on the CAGE tool (18). A client is considered to have experienced a side effect if they encounter any adverse medical event during their treatment with a pharmaceutical product, which is duly documented in their patient chart. A client is classified as having a history of hospitalization if there is documented evidence of any prior hospital admissions related to HIV in their medical records. Clients categorized as having regular ART follow-up adhere to their scheduled appointments for ART refills, as indicated by their attendance based on the predetermined schedule outlined in their patient follow-up chart, either as scheduled or unscheduled visits recorded by the care provider. A client is considered to have been exposed to stigma if they encounter any from of adverse attitudes, beliefs, behaviors, or actions directed toward them or their community due to their HIV/AIDS status.
Inclusion and exclusion criteria
The study included all HIV-positive adults aged 18 or older receiving follow-up care at public health facilities, excluding those receiving treatment for less than a month.
Survey instrument and data quality assurance
Data collection involved the utilization of structured questionnaires administered by the interviewer, and additional information was extracted from client charts as secondary data. The questionnaire was prepared by selecting, modifying, and adapting relevant evaluation tools from previous studies conducted in English. Dose adherence was calculated by subtracting missed doses from prescribed doses, dividing the result by prescribed doses, and multiplying by 100 to determine the outcome variable (2, 17). Different measures were implemented to ensure high-quality data, such as conducting a pretest on 5% of participants, providing extensive training to data collectors, translating the questionnaire from English to Amharic (the local language), and back-translating it into English to ensure consistency. The principal investigator was responsible for supervising the entire data collection process.
Statistical analysis
The collected data were coded, cleaned, and entered into EpiData version 4.6 before being exported to Stata version 14 for processing and analysis. Descriptive statistics were used to describe respondent characteristics. Frequency, proportion, and summary statistics were computed and reported in tables. The bivariate analysis identified candidate variables (p-value ≤0.25) for the multivariable analysis. Multicollinearity among independent variables was assessed using standard error, variance inflation factor (VIF), and tolerance. Adjusted odds ratios (AOR) were used to measure the strength of associated factors, with a p-value <0.05 considered statistically significant. The Hosmer-Lemeshow statistic test was utilized to assess the fitness of the model.
Results
Socio-demography characteristics of participants
In this study, 612 adult respondents participated, making a 97.8% response rate. The mean age of the participants were 39 ± 0.55 standard deviation (SD) years. Considering sex, more than half, 367 (60%) of the participants were females. Among participants, about 421(68.8%) of the study participants were urban residents (Table 1).
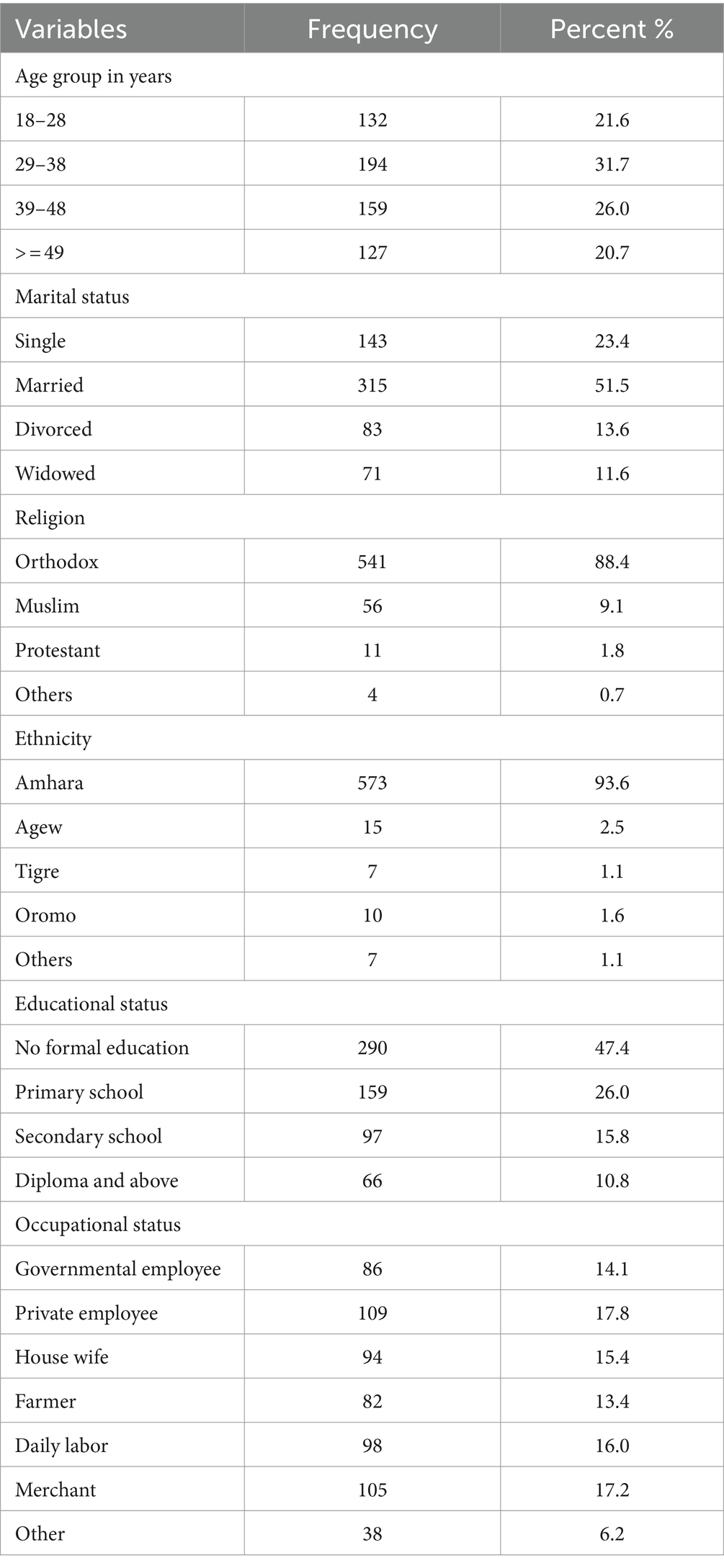
Table 1. Socio-demographic characteristics of ART clients in public health facilities of Bahir Dar city administration, Northwest Ethiopia, 2020 (n = 612).
Behavioral characteristics of study participants
Of the participants, 427 (69.8%) individuals openly disclosed their HIV status. Additionally, 439 (71.7%) participants utilized reminder aids to take ART medication. In terms of experiencing stigma, 319 (52.1%) respondents reported facing it. Regarding awareness about ART, 420 (68.6%) participants had knowledge about it. Moreover, problematic alcohol use was reported by 103 (16.8%) respondents (Table 2).
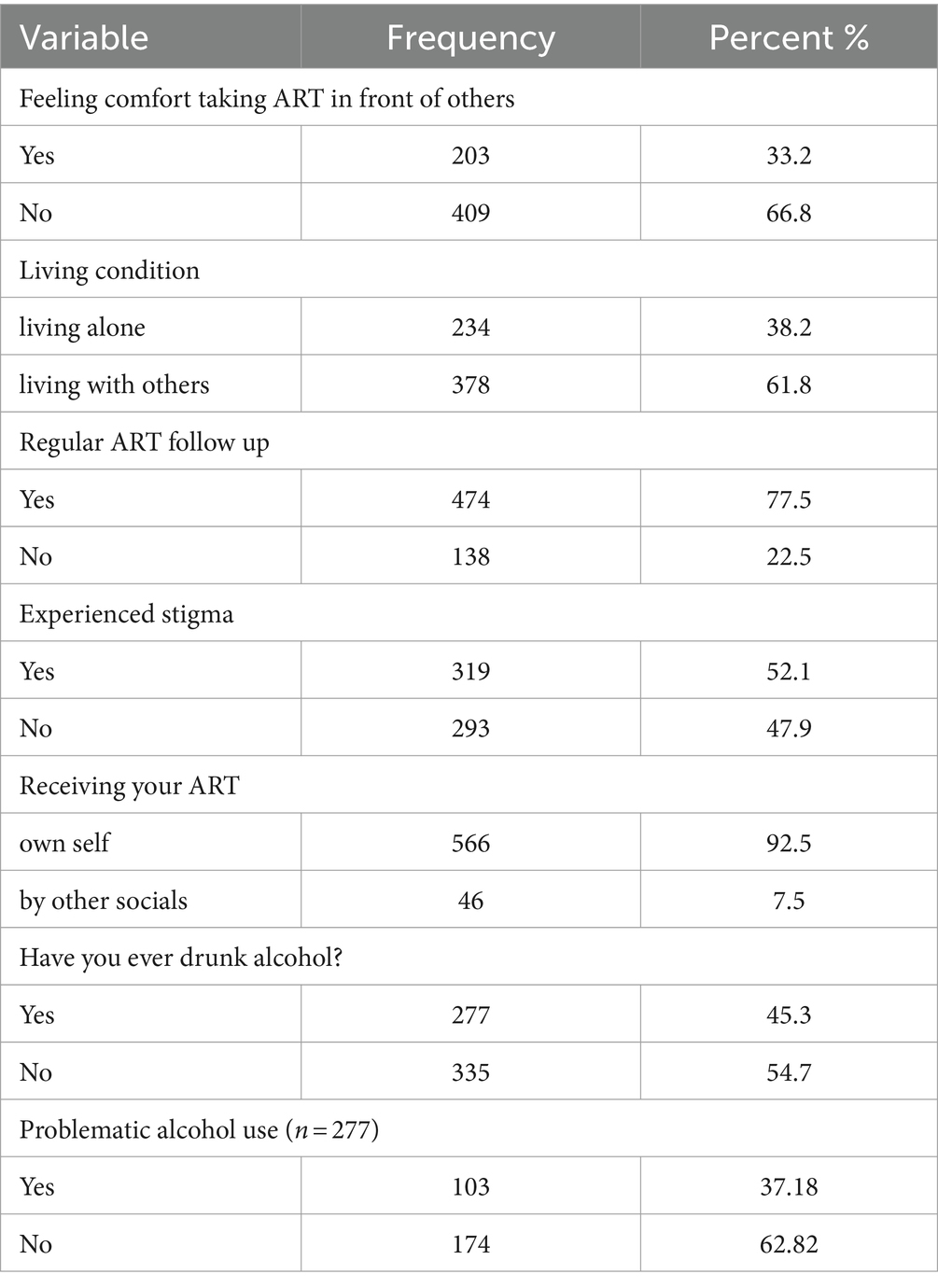
Table 2. Behavioral characteristics of ART clients in public health facilities of Bahir Dar city administration, Northwest Ethiopia, 2020 (n = 612).
Clinical and health care system-related factors
The average treatment duration of the respondents were 59.6 ± 2 SD months. Among respondents, 32 (53.1%) had ≤350 CD4 counts at the base-line. The majority, 569 (93.0%) of respondents, were on a first-line ART regimen. Two hundred fifty-seven (42.0%) of the participants experienced high viral load. The mean time duration since HIV positive was 68 (SD ± 2.6) months. Five hundred seventy-eight (94.4%) participants had one pill daily and one hundred forty-one (23.0%) had additional medications other than ARVs. Two hundred twenty-four (36.6%) participants developed opportunistic infections (Table 3).
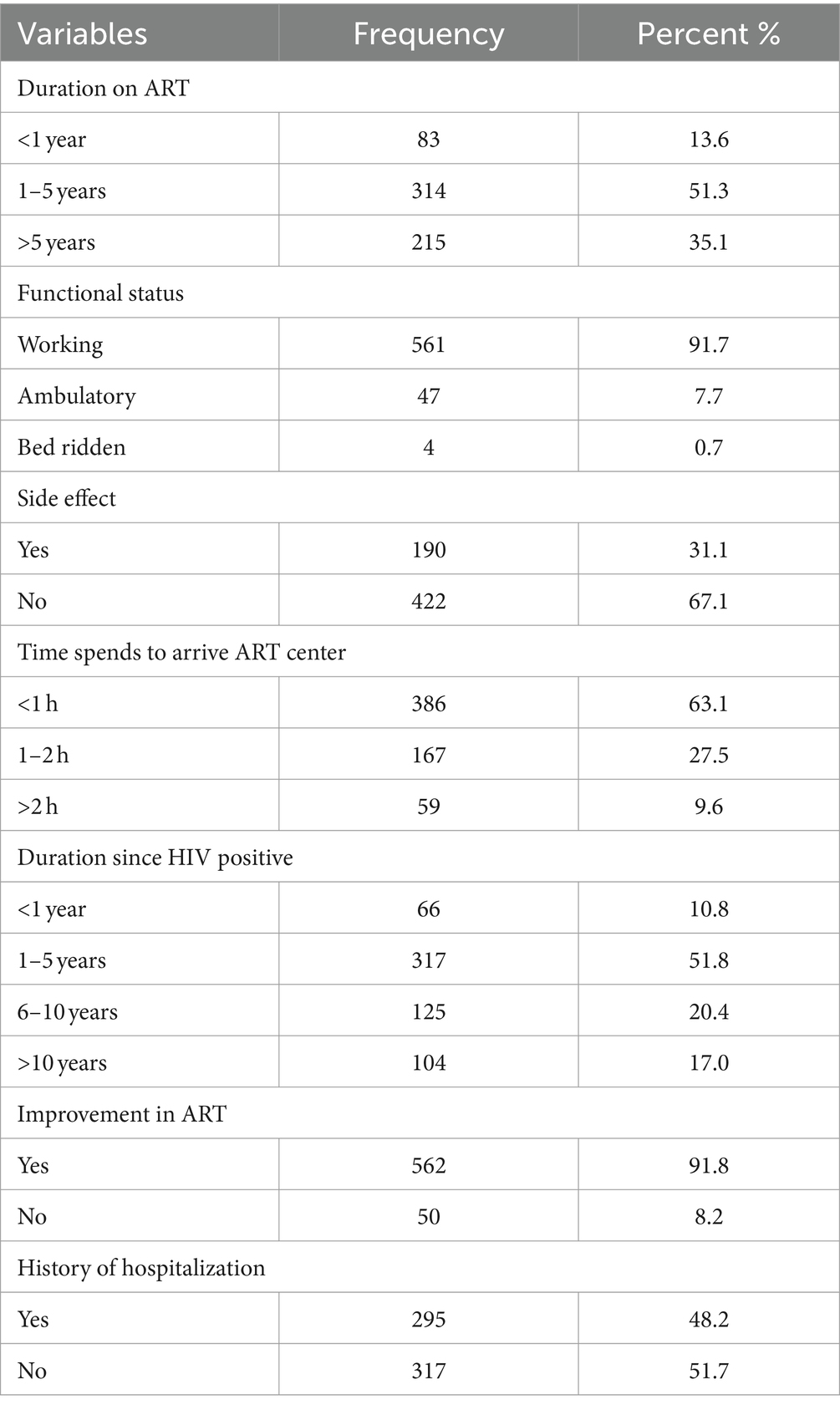
Table 3. Clinical and health care system related factors of ART clients in public health facilities of Bahir Dar city administration Northwest Ethiopia, 2020 (n = 612).
COVID-19 related characteristics
Out of the participants, 160 individuals, accounting for 26%, did not attend ART follow-up appointments because of the COVID-19 pandemic. The most significant portion, comprising 348 participants or 57%, had their follow-up schedules altered due to the pandemic (Table 4).
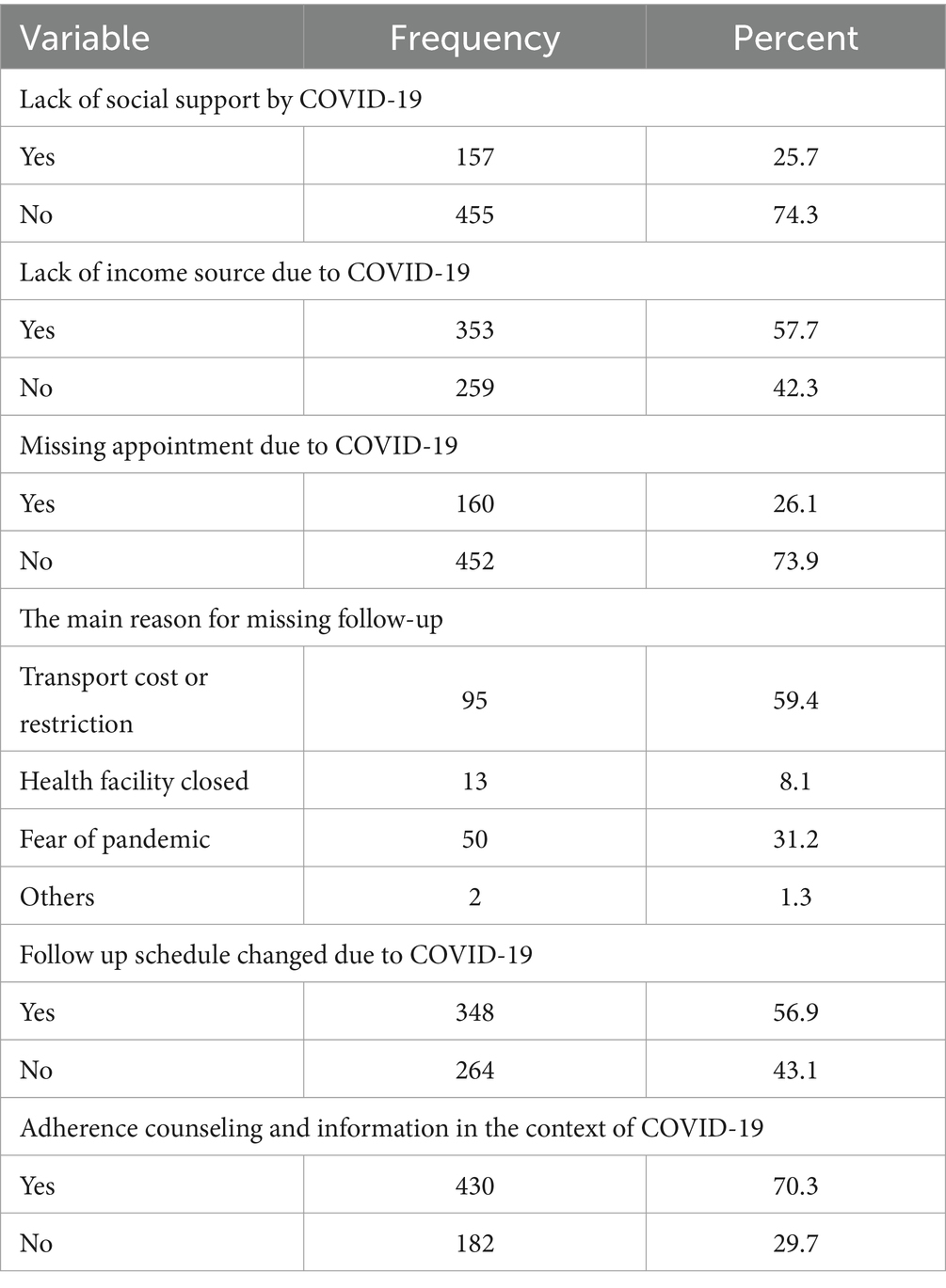
Table 4. COVID-19 pandemic-related factors of ART clients in public health facilities of Bahir Dar city administration Northwest Ethiopia, 2020 (n = 612).
Adherence to antiretroviral therapy
Of the total 612 study participants, 468 had good adherence to AR. In this study, good adherence to antiretroviral therapy was 76.5% (95% CI: 72.9, 79.7).
Factors associated with adherence to ART
The variables shown as an association at bi-variable analysis could not remain significant at multivariable analysis. Only marital status, regular ART follow-up, adherence counseling & support in the context of the COVID-19 pandemic, and knowledge about ART persist as significantly associated with adherence to ART in both bi-variable and multivariable logistic regression analysis.
Respondents with divorced marital status were 55% less likely to adhere to ART than participants with married marital status (AOR = 0.45, 95%CI: 0.22, 0.90).
The odds of good adherence were three times higher among respondents who had regular follow-ups for clinical appointments compared with those who did not have regular follow-ups (AOR = 3.01, 95%CI: 1.81, 5.01).
Participants who had adherence counseling and information in the context of the COVID-19 pandemic were 2.57 times more likely to adhere to ART as compared with those who had not (AOR =2.57, 95%CI: 1.63, 4.08).
The odds of good adherence were 1.81 times higher among respondents with adequate knowledge than their counterparts (AOR = 1.81, 95%CI:1.11, 2.94) (Table 5).
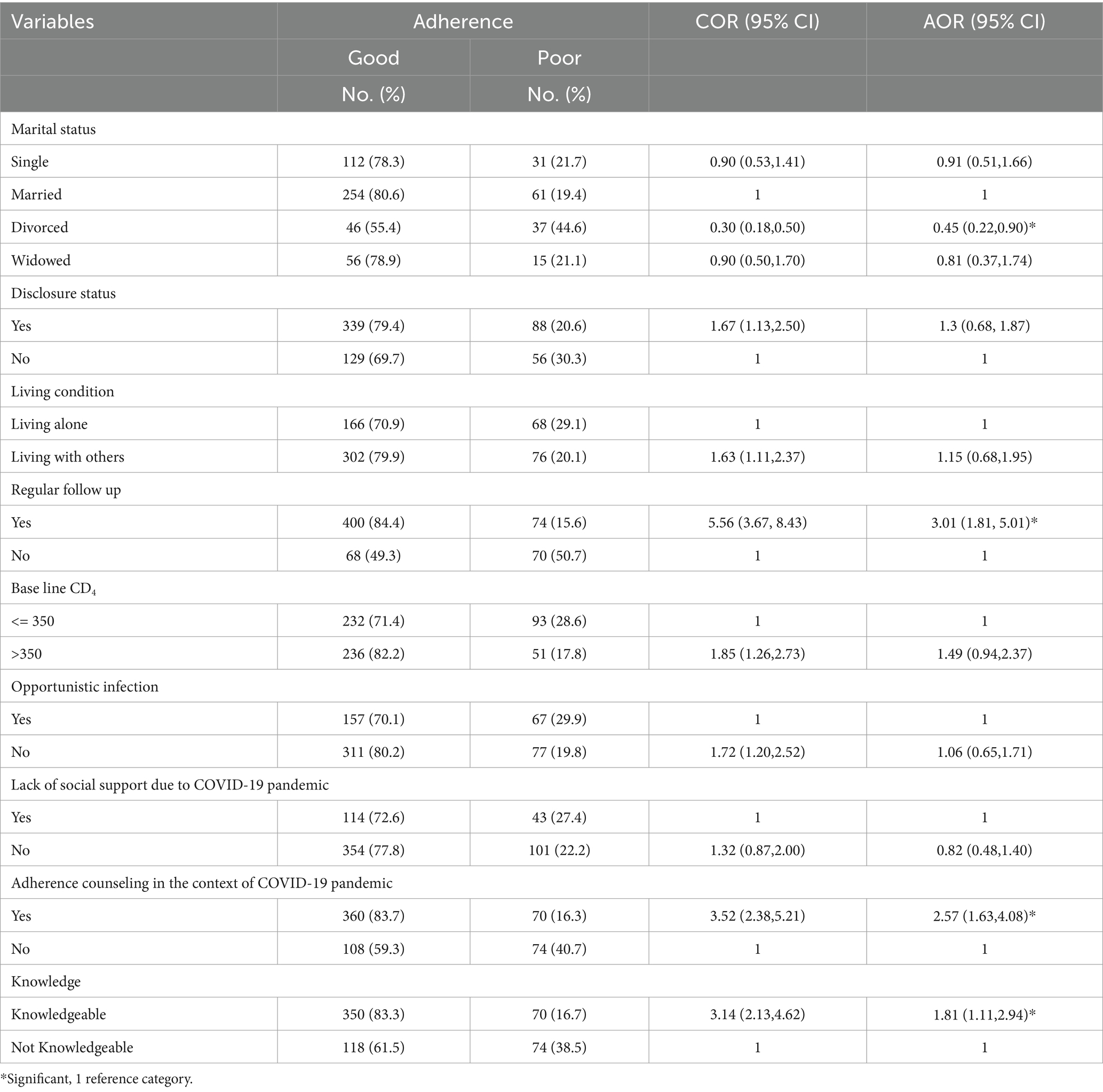
Table 5. Bivariable and multivariable analysis between explanatory and adherence to ART among HIV-positive adults attending care and treatment in public health facilities of Bahir Dar city administration, Northwest Ethiopia, 2020 (n = 612).
Discussion
The primary objective of this study was to evaluate the influence of COVID-19 on adherence to ART and identify the factors associated with it. After conducting a multivariable analysis, it was determined that factors such as marital status, consistent ART follow-up, adherence counseling, support during the COVID-19 pandemic, and knowledge about antiretroviral therapy were significantly associated with adherence to ART.
The Good adherence to ART in this study was 76.5% (95% CI = 72.9,79.7). This aligns with previous research conducted in various locations, including China (72%) (7), Nekemt 77.9% (19), Jima Zone (73.6%) (20), Hara 71.8% (21), and Dubbo St. Marry Hospital, Areka Town, southern Ethiopia 78% (22). However, it surpasses the adherence rates reported in studies from Zimbabwe (65%) (23), Dre Dawa 65% (24), Jima university hospital 63.8% (25), and Nigst Eleni Mohammed memorial hospital 56% (15). The differences in adherence rates could be attributed to several factors, such as variations in study populations, timing of the studies, and specific healthcare settings. Socio-demographic characteristics, availability of healthcare services and support systems, and cultural factors could all influence ART adherence rates in these diverse settings. Additionally, differences in how adherence was assessed and what constitutes good adherence may have contributed to the variations observed across the studies.
The observed adherence rate of 76.5% in this study is lower than the rates reported in other studies conducted in different regions, including, Nepal 87.4% (26), India 89.5% (9), Indonesia 84.6% (27), Oromia regional state 98.8% (28), Hoshana 90.7% (11), Goba hospital 90.8% (29), Debre Birhan 95.5% (30), Gondar university specialized teaching hospital 88.2% (12), and Debre Markos referral hospital 88.6% (31). This disparity in adherence rates might be attributed to the specific study settings and contexts. Furthermore, the impact of the COVID-19 pandemic could be a contributing factor to lower adherence rates in this study. It’s possible that ART clients missed their routine HIV care appointments due to the pandemic, leading to interruptions in their ART medication. Additionally, the heightened focus on the COVID-19 pandemic may have diverted attention and resources away from HIV care and adherence, potentially affecting the results of this study.
Divorced clients exhibited reduced odds of achieving good adherence to ART compared to those who were married. This result is consistent with findings from studies conducted in Nigeria (32), Hoshana (11), and Nigst Eleni Mohammed memorial hospital (15). A possible potential explanation for this is that divorced individuals often face increased emotional and financial stress, which has been worsened by the uncertainties created by the COVID-19 pandemic. Due to the social isolation measures and disruptions in routine healthcare services, the stress levels of these individuals may further increase, making it challenging for them to prioritize and stick to their ART regimen. Moreover, divorced individuals may lack the social support systems that married individuals typically rely on during times of crisis, which could make it more difficult for them to cope with the pandemic’s challenges and maintain consistent adherence to ART.
Consistent attendance to ART follow-up appointments increased treatment adherence among HIV-positive adults compared to those who did not maintain regular clinical visits. This is comparable with studies done in Dre Dawa (24), Nigst Eleni Mohammed Memorial Hospital Hoshana (15), Nekemt Hospital (19), and Bale Goba Hospital (29). Maintaining regular attendance at ART follow-up appointments is critical for promoting treatment adherence among HIV-positive adults, which is supported by various studies. However, the COVID-19 pandemic has led to significant disruptions in healthcare services, which may hinder access to these appointments due to altered clinic schedules, transportation restrictions, and concerns about virus transmission. Despite these challenges, individuals who have continued to attend appointments have likely benefited from ongoing support and monitoring from healthcare providers. This continuity of care may have facilitated the timely identification and management of treatment-related issues, reinforcing adherence behaviors. Therefore, prioritizing regular clinical visits remains essential for promoting treatment adherence and enhancing health outcomes among HIV-positive individuals, even amid pandemic-related challenges.
The likelihood of achieving good adherence to ART was greater among individuals who received adherence counseling and information during the COVID-19 pandemic than those who did not receive such support. The finding is supported by the Federal Ministry of Health Ethiopia’s interim guidance for the provision of HIV services in the context of the COVID-19 pandemic in Ethiopia (13). A possible explanation for this observation is that providing up-to-date information and adherence support can enhance clients’ awareness and knowledge about their antiretroviral therapy and the ongoing pandemic, thereby contributing to better adherence.
Participants who possessed knowledge about ART were more inclined to adhere to their treatment than those who lacked such knowledge. The finding agreed with the studies conducted at Gondar University Specialized Teaching Hospital (12) and Jima Zone (20). One possible explanation for this trend is that clients with good knowledge are better equipped to comprehend the significance of taking their prescribed medication as directed. Moreover, they have a deeper understanding of the disease progression and its connection with COVID-19 in individuals with compromised immune systems.
Limitations of the study
This study evaluated adherence via self-report, susceptible to social desirability and recall bias. However, participants were well-informed and encouraged to provide honest responses. This awareness likely minimized the effect of this limitation on the study’s findings’ credibility. Moreover, the study did not adequately address the impact of healthcare-related factors on treatment adherence.
Conclusion
Compared to the standards set by the WHO and prior studies in Ethiopia, the level of adherence to antiretroviral therapy in this study was relatively low. According to the findings of this study, individuals who maintained regular ART follow-up appointments received adherence counseling and information specifically related to the COVID-19 pandemic and possessed knowledge about their treatment were more inclined to adhere to their medication regimen. On the other hand, People who identified as divorced had lower adherence to antiretroviral therapy.
Implication
The findings of this study highlight the urgent need for improved efforts to increase adherence to ART among individuals living with HIV. Strategies that prioritize regular follow-up appointments, personalized counseling, and education on HIV treatment and emerging and reemerging health threats like COVID-19 could be beneficial in improving adherence rates.
Furthermore, the study suggests that social and emotional support systems may be crucial in medication adherence, as divorce was associated with lower adherence. Interventions aimed at enhancing support networks, providing psychosocial assistance, and addressing potential emotional distress among divorced individuals could potentially improve their adherence to antiretroviral therapy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Bahir Dar University’s College of Medicine and Health Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CDG: Formal Analysis, Writing – review & editing, Writing – original draft. GWT: Writing – review & editing, Writing – original draft. BFS: Formal Analysis, Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our appreciation to Bahir Dar University’s College of Medicine and Health Sciences, as well as the administrators of healthcare facilities, data collectors, and the participants for their valuable contributions to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; ART, antiretroviral therapy; COR, crude odds ratio; HIV, human immunodeficiency virus; PLHIV, people living with HIV.
References
1. Federal HIV AIDS Prevention and Control Office HIV Prevention in Ethiopia National Road Map 2018–2020. Addis Ababa Ethiopia; Federal HAPCO November (2018). Available at: https://ethiopia.unfpa.org/sites/default/files/pubpdf/HIV%20Prevention%20in%20Ethiopia%20National%20Road%20Map%202018%20%202020%20FINAL_FINAL.pdf
2. World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. 2nd ed. Geneva: World Health Organization (2016).
3. Shiau, S, Krause, KD, Valera, P, Swaminathan, S, and Halkitis, PN. The burden of COVID-19 in people living with HIV: a syndemic perspective. AIDS Behav. (2020) 24:2244–9. doi: 10.1007/s10461-020-02871-9
4. Baye, K. “COVID-19 prevention measures in Ethiopia: Current realities and prospects,” ESSP Working Paper 141. Washington, DC: Addis Ababa, Ethiopia: International Food Policy Research Institute (IFPRI); Federal Democratic Republic of Ethiopia Policy Studies Institute. (2020).
5. Hightow-Weidman, L, Muessig, K, Claude, K, Roberts, J, Zlotorzynska, M, and Sanchez, T. Maximizing digital interventions for youth in the midst of COVID-19: lessons from the adolescent trials network for HIV interventions. AIDS Behav. (2020) 24:2239–43. doi: 10.1007/s10461-020-02870-w
6. Posada-Vergara, MP, Alzate-Ángel, JC, and Martínez-Buitrago, E. COVID-19 and HIV. Colomb Med. (Cali). (2020) 51:e4327. doi: 10.25100/cm.v51i2.4327
7. Kipsang, J, Chen, J, Tang, C, Li, X, and Wang, H. Self reported adherence to antiretroviral treatment and correlates in Hunan province, the Peoples Republic of China. Int J Nurs Sci. (2018) 5:162–7. doi: 10.1016/j.ijnss.2018.04.008
8. Beer, L, and Skarbinski, J. Adherence to antiretroviral therapy among HIV-infected adults in the United States. AIDS Educ Prev. (2014) 26:521–37. doi: 10.1521/aeap.2014.26.6.521
9. Sakthivel, V, Krishnasamy, V, and Mehalingam, V. Level of medication adherence and its associated factors among patients receiving antiretroviral therapy at a tertiary care hospital in South India. J Caring Sci. (2020) 9:93–7. doi: 10.34172/JCS.2020.014
10. Kim, MH, Mazenga, AC, Yu, X, Ahmed, S, Paul, ME, Kazembe, PN, et al. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. J Int AIDS Soc. (2017) 20:21437. doi: 10.7448/IAS.20.1.21437
11. Doyore, F, and Moges, B. Adherence to antiretroviral treatment services and associated factors among clients attending ART clinics in hosanna town, southern Ethiopia. J AIDS Clin Res. (2016) 7:2. doi: 10.4172/2155-6113.1000590
12. Molla, AA, Gelagay, AA, Mekonnen, HS, and Teshome, DF. Adherence to antiretroviral therapy and associated factors among HIV positive adults attending care and treatment in University of Gondar Referral Hospital, Northwest Ethiopia. BMC Infect Dis. (2018) 18:266. doi: 10.1186/s12879-018-3176-8
13. "Ethiopian Minstry of health". Interim Guidance for Provision of HIV Services in the context of COVID-19 Pandemic in Ethiopia. (2020).
14. Ballester-Arnal, R, and Gil-Llario, MD. The virus that changed Spain: impact of COVID-19 on people with HIV. AIDS Behav. (2020) 24:2253–7. doi: 10.1007/s10461-020-02877-3
15. Billoro, B, Mamo, G, and Jarso, H. Adherence to antiretroviral therapy and associated factors among HIV infected patients in Nigist Eleni Mohammed memorial general hospital, Hossana, southern Ethiopia. J AIDS Clin Res. (2018) 9:2. doi: 10.4172/2155-6113.1000774
16. Ethiopia, F. National consolidated guidelines for comprehensive HIV prevention, care and treatment. Addis Ababa: Fmoh. (2018):1–238.
17. Federal Ministry of Health Ethiopia. National Comprehensive HIV Prevention, Care & Treatment Training for Health care Providers. Participant Manual June, Addis Ababa Ethiopia (2019).
18. Ewing, JA. Detecting alcoholism: the CAGE questionnaire. JAMA. (1984) 252:1905–7. doi: 10.1001/jama.1984.03350140051025
19. Ejigu, SH, Rike, WA, and Angamo, MT. Medication adherence and associated factors among patients on highly active antiretroviral therapy in Nekemte hospital, Ethiopia. Gazi Med J. (2014) 20:199–208. doi: 10.5455/GMJ-30-153681
20. Hassen, A, and Mohammed, Y. Antiretroviral therapy adherence level and associated factors among HIV/AIDS patients in Jimma zone government health facilities, ART clinics, south-West Ethiopia. Int J Multicult Multirelig Understand. (2019) 5:331–41. doi: 10.18415/ijmmu.v5i5.535
21. Legesse, TA, and Reta, MA. Adherence to antiretroviral therapy and associated factors among people living with HIV/AIDS in Hara town and its surroundings, north-eastern Ethiopia: a cross-sectional study. Ethiop J Health Sci. (2019) 29:299–308. doi: 10.4314/ejhs.v29i3.2
22. Koyra, H. Adherence to antiretroviral therapy among adult persons living with HIV/AIDS in southern Ethiopia. Int J Virol AIDS. (2018) 5:38. doi: 10.23937/2469-567X/1510038
23. Gonah, L, and Mukwirimba, A. Determinants of optimal adherence to antiretroviral therapy among people living with HIV/AIDS registered for antiretroviral therapy in Zimbabwe. Med J Zambia. (2016) 43:174–83. doi: 10.55320/mjz.43.4.301
24. Negesa, L, Demeke, E, and Mekonnin, W. Adherence to antiretroviral therapy and factors affecting among people living with HIV/AIDS and taking antiretroviral therapy, Dire Dawa town, eastern Ethiopia. J Infect Dis Treat. (2017) 3:5. doi: 10.21767/2472-1093.100032
25. Abera, A, Fenti, B, Tesfaye, T, and Balcha, F. Factors influencing adherence to antiretroviral therapy among people living with HIV/AIDS at ART Clinic in Jimma University teaching hospital, Southwest Ethiopia. J Pharma Reports. (2015) 1:2.
26. Neupane, S, Dhungana, GP, and Ghimire, HC. Adherence to antiretroviral treatment and associated factors among people living with HIV and AIDS in CHITWAN, Nepal. BMC Public Health. (2019) 19:720. doi: 10.1186/s12889-019-7051-3
27. Ibrahim, K, Lindayani, L, Emaliyawati, E, Rahayu, U, and Nuraeni, A. Factors associated with adherence to antiretroviral therapy among people living with HIV infection in West Java Province, Indonesia. Malaysian Journal of Medicine & Health Sciences. (2020) 16.
28. Chaka, T, Abeya, S, Adlo, A, Abebe, T, Hamuse, S, and Lencha, M. Antiretroviral therapy: level of adherence and its determinants among patients on treatment in different health facilities. A Cross Sectional Study in Oromia Regional State, Ethiopia. J AIDS Clin Res. (2016) 7:1–7.
29. Lencha, B, Hasen, K, Getachew, T, Abdi, M, and Habtamu, M. Adherence to antiretroviral therapy and associated factors among people living with HIV/AIDS at Gobba hospital, Southeast Ethiopia: an institutional based study. Qual Primary Care. (2015) 23:336–41.
30. Ketema, AK, and Weret, ZS. Assessment of adherence to highly active antiretroviral therapy and associated factors among people living with HIV at Debrebrihan referral hospital and health center, Northeast Ethiopia: a cross-sectional study. HIV/AIDS (Auckl). (2015) 7:75. doi: 10.2147/HIV.S79328
31. Asmare, M, Aychiluhem, M, Ayana, M, and Jara, D. Level of ART adherence and associated factors among HIV sero-positive adult on highly active antiretroviral therapy in Debre Markos referral hospital, Northwest Ethiopia. J Antivir Antiretrovir. (2014) 6:120–6.
Keywords: adherence, antiretroviral therapy, COVID-19, HIV-positive adult, Ethiopia
Citation: Gela CD, Tsegaye GW and Shibesh BF (2024) Adherence to antiretroviral therapy and determining factors in adults living with HIV receiving services at public health facilities amidst the COVID-19 crisis in Bahir Dar city, Northwest Ethiopia. Front. Public Health. 12:1380055. doi: 10.3389/fpubh.2024.1380055
Edited by:
Carlos Brites, Federal University of Bahia (UFBA), BrazilReviewed by:
Nilesh Chandrakant Gawde, Tata Institute of Social Sciences, IndiaAhmed Cordie, Cairo University, Egypt
Copyright © 2024 Gela, Tsegaye and Shibesh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Belayneh Fentahun Shibesh, YmVsYXluZWhmZW50YWh1bjQyQGdtYWlsLmNvbQ==
 Chalachew Dessie Gela1
Chalachew Dessie Gela1 Belayneh Fentahun Shibesh
Belayneh Fentahun Shibesh