- 1Department of Emergency Nursing, School of Nursing, Navy Military Medical University, Shanghai, China
- 2905th Hospital of the PLA Navy, Shanghai, China
- 3School of Nursing, Navy Military Medical University, Shanghai, China
Background: Hospital resilience is essential in responding to disasters, but current research focuses mainly on frameworks and models rather than the protection of resilience and analysis of risk factors during public health emergencies. This study aims to examine the development of resilience in Chinese frontline hospitals during the initial COVID-19 outbreak in 2020, providing insights for future disaster response efforts.
Objectives: We conducted interviews with 26 hospital staff members who were involved in the initial response to the COVID-19 outbreak in China. We used a semi-structured interview approach and employed purposive sampling and snowball sampling techniques. The interview outline was guided by the ‘Action Framework’ proposed by the World Health Organization (WHO) for responding to infectious disease emergencies. This framework includes dimensions such as command, surveillance, risk communication, medical response, and public health response. We analyzed the collected data using Colaizzi’s seven-step data analysis method and the template analysis method.
Results: WHO’s ‘action framework’ effectively highlights the factors that contribute to hospital resilience. While medical response, including the availability of materials and facilities, the use of information technology, and the capacity for infectious disease diagnosis and treatment, remains crucial, other important aspects include awareness and beliefs about infections, treatment experience, interdisciplinary collaboration, and more. Additionally, it is essential to establish an intelligent command system, foster trusting partnerships between teams, improve monitoring capabilities for infectious disease agents, enhance risk communication through information synchronization and transparency, strengthen infection control planning, and improve environmental disinfection capabilities for effective public health emergency response. These contradictions significantly impact the enhancement of hospital resilience in dealing with major infectious disease outbreaks.
Conclusion: In responding to sudden major infectious diseases, hospitals play a vital role within the healthcare system. Enhancing hospital resilience involves more than just improving treatment capabilities. It also requires effective command coordination at the hospital level, infection control planning, and the deployment of intelligent equipment. Additionally, planning for effective communication and coordination between hospitals, communities, and the national healthcare system can further enhance hospital resilience.
1 Introduction
With the continuous expansion and deepening of human activities in the natural environment, the contact and interaction between various organisms and humans have increased. This has led to a higher likelihood of unknown infectious disease pathogens invading the human body and causing mass transmission. The insufficient understanding of the pathogenic characteristics, epidemic patterns, and treatment methods of newly emerging infectious diseases has made it challenging to control such events, posing a significant threat and challenge to human health and social stability (1, 2). The COVID-19 pandemic in 2019 serves as a prime example, revealing the global response capabilities to major infectious diseases and emphasizing the importance of building resilient healthcare systems (3). Hospitals, as a crucial component of the healthcare system, play a vital role in epidemic response and serve as the primary point of contact for communities during emergencies. Therefore, ensuring the stability and resilience of hospitals in the face of major infectious diseases is essential (4). Scholars have proposed the concept framework of hospital resilience for disaster response, which includes hospital safety, disaster preparedness and resources, continuous basic medical services, and recovery and adaptation as the four key elements (5). Additionally, some scholars have studied the development of hospital resilience after the Nepal earthquake (6). However, literature specifically focusing on hospital resilience related to biosafety was mainly published after 2019 and is predominantly centered around COVID-19 (7). Despite the increasing attention given to hospital resilience and the gradual enrichment of its concept, the numerous conceptual definitions and model constructions make it challenging to provide practical guidance for hospitals at the operational level. Furthermore, there is a lack of empirical research on the actual participation of frontline hospitals in major infectious disease emergencies.
The concept of resilience has undergone three stages of development. Initially, resilience was used in mechanical research to describe the strength and ductility of materials, referring to their ability to resist or absorb external forces. In the second stage, resilience was seen as the capacity of a system to withstand external disturbances while maintaining its basic function, structure, identity, and feedback (8). The third stage was influenced by Bronfenbrenner’s bioecological theory, which highlights the interdependence between individual development and the environment they are in (9). This theory has contributed to the understanding of resilience in ecology, suggesting that a system’s resilience at a specific level is influenced by the dynamics and states of other levels, resulting in a complex interplay of resilience (10). In this stage, the concept of resilience in systems has evolved from solely focusing on the system’s ability to resist external disturbances and return to its original state or function, to recognizing the mutual influence of various elements within systems, which continuously drive adaptability, reorganization, and development.
Hospitals, like any other systems, are influenced by community management capabilities, healthcare system policies, and various other factors (11, 12). In particular, hospitals can be considered as microsystems, the communities they are located in as mesosystems, other hospitals and communities they do not directly interact with as ecosystems, and health management departments as macrosystems. These macrosystems have an impact on hospitals through their policies and institutions. Our team is currently researching this area. However, the true role of these different systems is reflected in the adaptive capacity of hospitals. After being affected, hospitals will activate and mobilize protective factors to maintain their stability. The interaction between risk factors and protective factors gives rise to four different states: imbalance, obstruction, recovery, and activation. This process is also known as the process model of resilience (13). When hospitals respond to major infectious diseases such as COVID-19, there are factors that influence their response to such events, which can be presented as protective or risk factors.
The process model of resilience includes the “Pressure-State-Response” proposed by Rapport and Friend, which vividly describes the logical relationship between the causes of problems, the changes caused by the problems, and the resulting states and responses through three stages: pressure, state, and response (14). Based on the adaptive cycle’s chaotic model, it is believed that systems are in a state of dynamic change and constantly go through four stages of development: growth or development stage, conservation stage, release or creative destruction stage, and reorganization stage. In the field of disasters, Fink’s life cycle theory is often adopted, which divides the response cycle of emergencies into the latent period, onset period, spread period, and decline period. However, the above models have limitations when applied to the response to infectious disease emergencies. In this study, we explore the generation of protective or risk factors in the five stages of hospital response to infectious diseases: command, surveillance, communication, health care response, and public health intervention, based on the ‘Framework for Action’ proposed by the WHO for responding to infectious disease emergencies (15). This will provide practical references for future hospital responses to major infectious diseases.
2 Methods
2.1 Study setting
On December 31, 2019, the World Health Organization (WHO) reported cases of a new type of pneumonia caused by a novel coronavirus, which is currently named 2019-nCoV (16). Subsequently, a pandemic outbreak occurred, but it is currently under effective control. Our research specifically examines the early stages of the pandemic, focusing on the direct involvement of healthcare workers in hospitals in Wuhan, China in the initial response to the infectious disease. The experiences and contributions of these healthcare workers serve as valuable primary data for our research on the infectious disease response.
2.2 Data collection
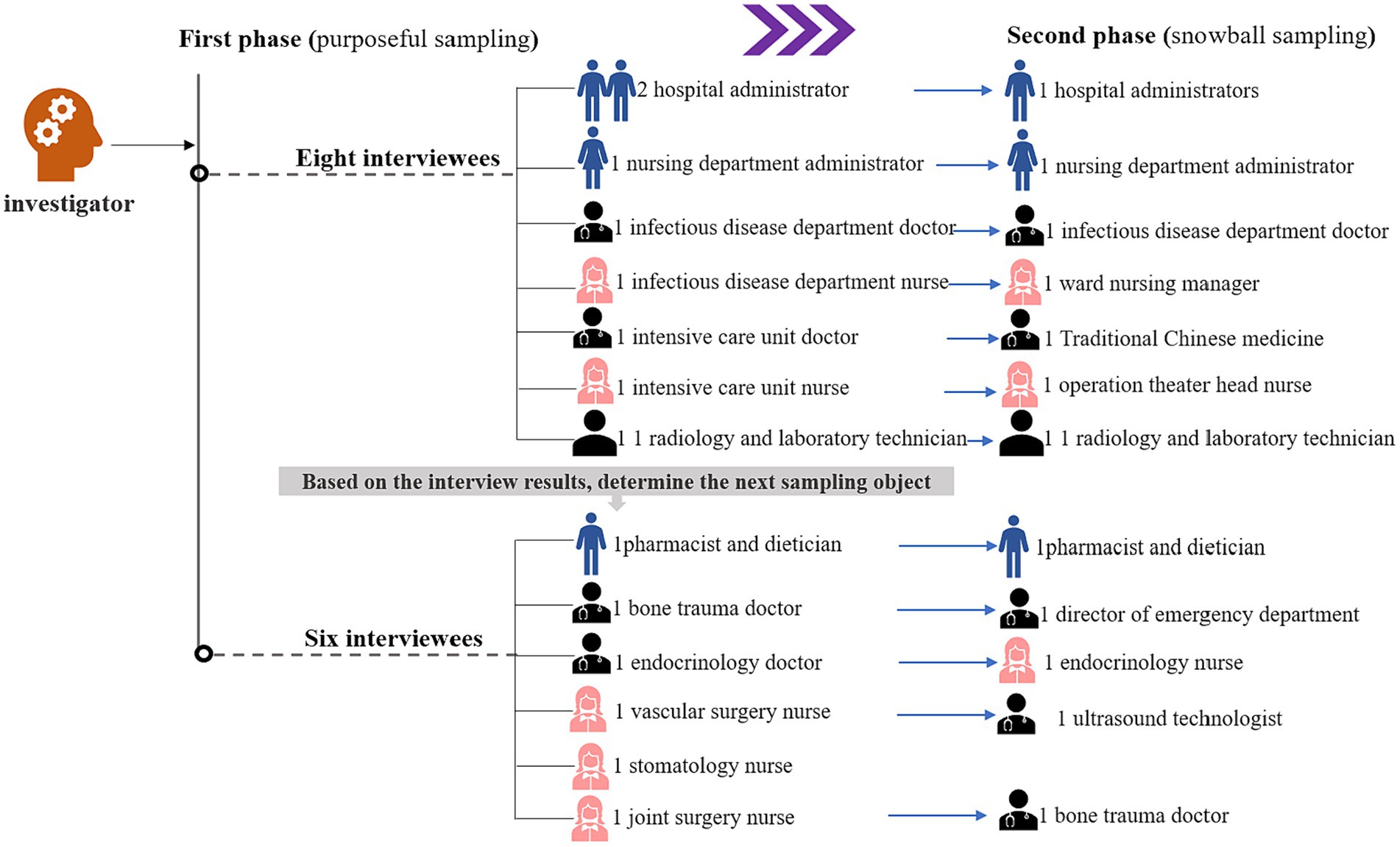
The operation of hospitals relies on the collaboration of different departments. Therefore, it is essential to analyze the protective or risk factors that impact the resilience of hospitals from the perspective of various positions of hospital workers. This study employed purposive sampling and snowball sampling principles to recruit the initial group of medical staff (see Figure 1), hospital administrators, and other personnel from our affiliated hospital who actively participated in the prevention and control of the Wuhan epidemic. A total of 26 interviews were conducted with personnel who had been to Wuhan to provide support before December 31, 2019. These interviews took place between August and December 2022, with the consent of the interviewees, in quiet meeting rooms. The duration of each interview ranged from 40 to 60 min.
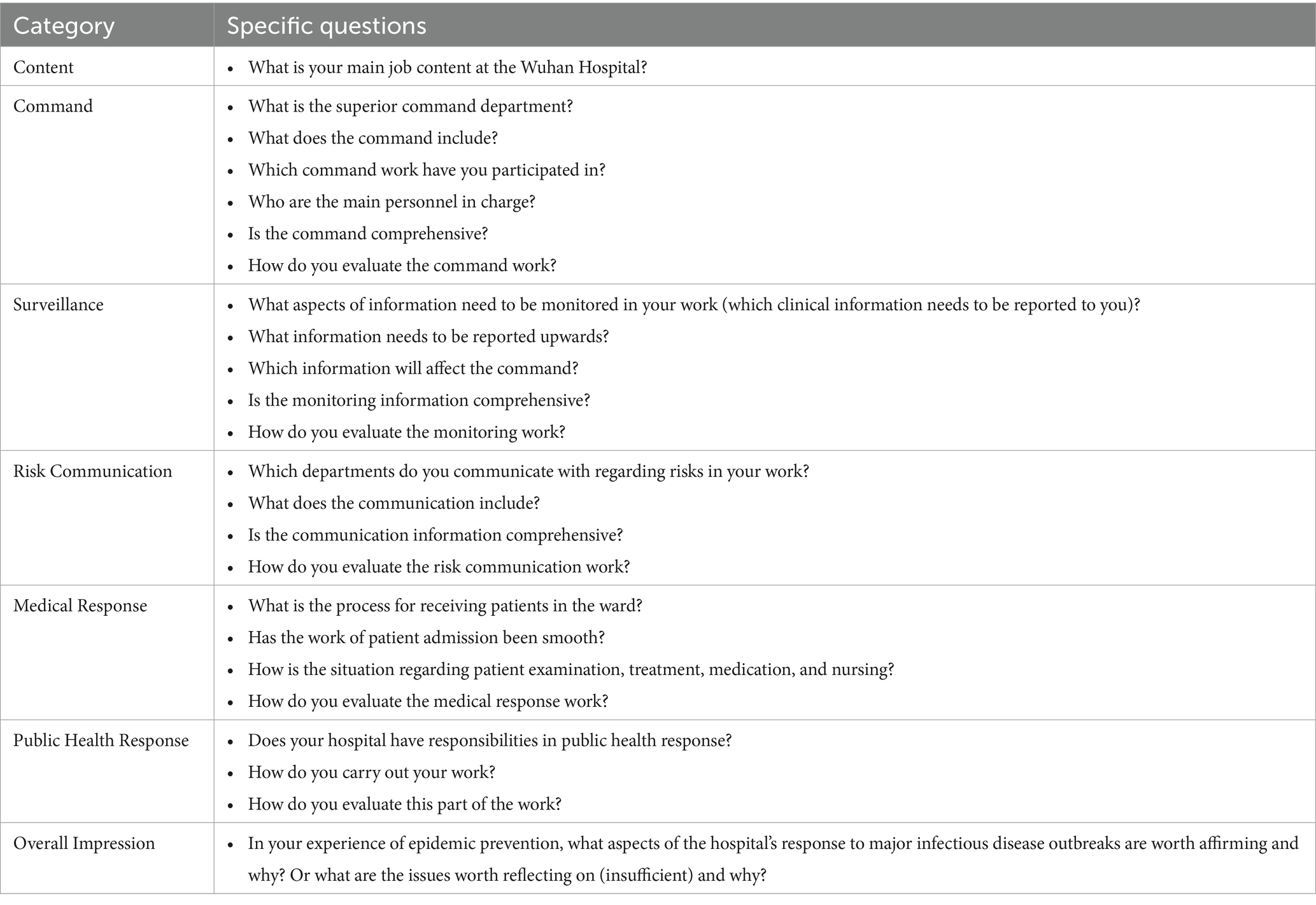
Before each interview, the first author introduced the research content and purpose of the research team to the interviewees, obtained their consent again, and then issued an informed consent form. The interviewees read the form, signed it, and filled out a general information report. Simultaneously, a standardized interview outline was provided for reference. The interview usually began with simple questions to help the interviewees relax and encourage them to express their true feelings. For example, they were asked about their profession and the department they worked in at the hospital in Wuhan. The formal interview outline was based on the ‘Action Framework’ for infectious disease outbreaks by the World Health Organization (refer to Table 1). It covered topics such as command, surveillance, risk communication, medical response, public health response, and overall opinions and suggestions regarding their main work at the hospital in Wuhan. With the interviewee’s consent, the interview was recorded using a voice recorder and transcribed verbatim. Notes were also taken during the interview and included in the initial coding process. The interview records were returned to the interviewees for verification, but no changes were required.
2.3 Data analysis
Following guidelines for qualitative data analysis in health services research, we utilized a combination of deductive and inductive thematic coding (17). The coding and discussion of the results were collectively completed by the team. In the specific coding process, a coding team consisting of the corresponding author and two researchers is formed. Firstly, the two researchers strictly conduct data coding and classification in a double-blind manner. The corresponding author then reads the coding and proposes questions and suggestions. Any discrepancies that arise during the coding process are verified and resolved through supplemental background knowledge and group discussions, aiming to reach a consensus. If a consensus cannot be reached, the coding is deleted. Additionally, weekly group meetings are held to report and discuss the coding process, aiming to improve the accuracy of the analysis results.
Initially, we provide an overview of the research findings, outlining the impact of infectious diseases on hospitals and the corresponding changes observed at each stage. By employing a standardized outline that encompasses multiple dimensions, we observed that the interviewees’ responses largely align with the five dimensions defined by the WHO’s action framework: command, surveillance, risk communication, medical response, and public health response. However, certain aspects of the interview content deviate from the five dimensions. To clarify their attribution to a specific dimension, we conducted a structured reanalysis of these elements.
This study opts for manual analysis rather than computer software for the qualitative data analysis, with the aim of identifying protective or risk factors within the foundational dimensions of the model. To achieve this, we employed a template analysis method based on the WHO’s “Behavioral Framework” for responding to outbreaks of infectious diseases, which encompasses five key elements. The data analysis process adheres to Colaizzi’s seven-step method for data analysis: (1) detailed recording and careful reading of interview data. (2) excerpting meaningful statements that match the research phenomenon. (3) summarizing and extracting meaning from the meaningful statements. (4) searching for common concepts or characteristics of meaning to form themes, theme clusters, and categories. (5) connecting the themes to provide a complete narrative of the research phenomenon. (6) stating the essential structure of the phenomenon. (7) returning the obtained results to the interviewees to verify the authenticity of the content. If new data emerged, it was integrated into the comprehensive description. This study adhered to the Consolidated Criteria for Reporting Qualitative Research (COREQ) (18).
Finally, two situations were identified regarding the protective and risk factors of hospital resilience. In most cases, the protective factors (P) and risk factors (R) were interdependent, with a mutually exclusive relationship. As the protective factors (P) increased, the risk factors (R) gradually disappeared. However, in some cases, the protective factors and risk factors were independent of each other. Increasing the protective factors (P) had no impact on the risk factors (R).
3 Results
3.1 Characteristics of study participants
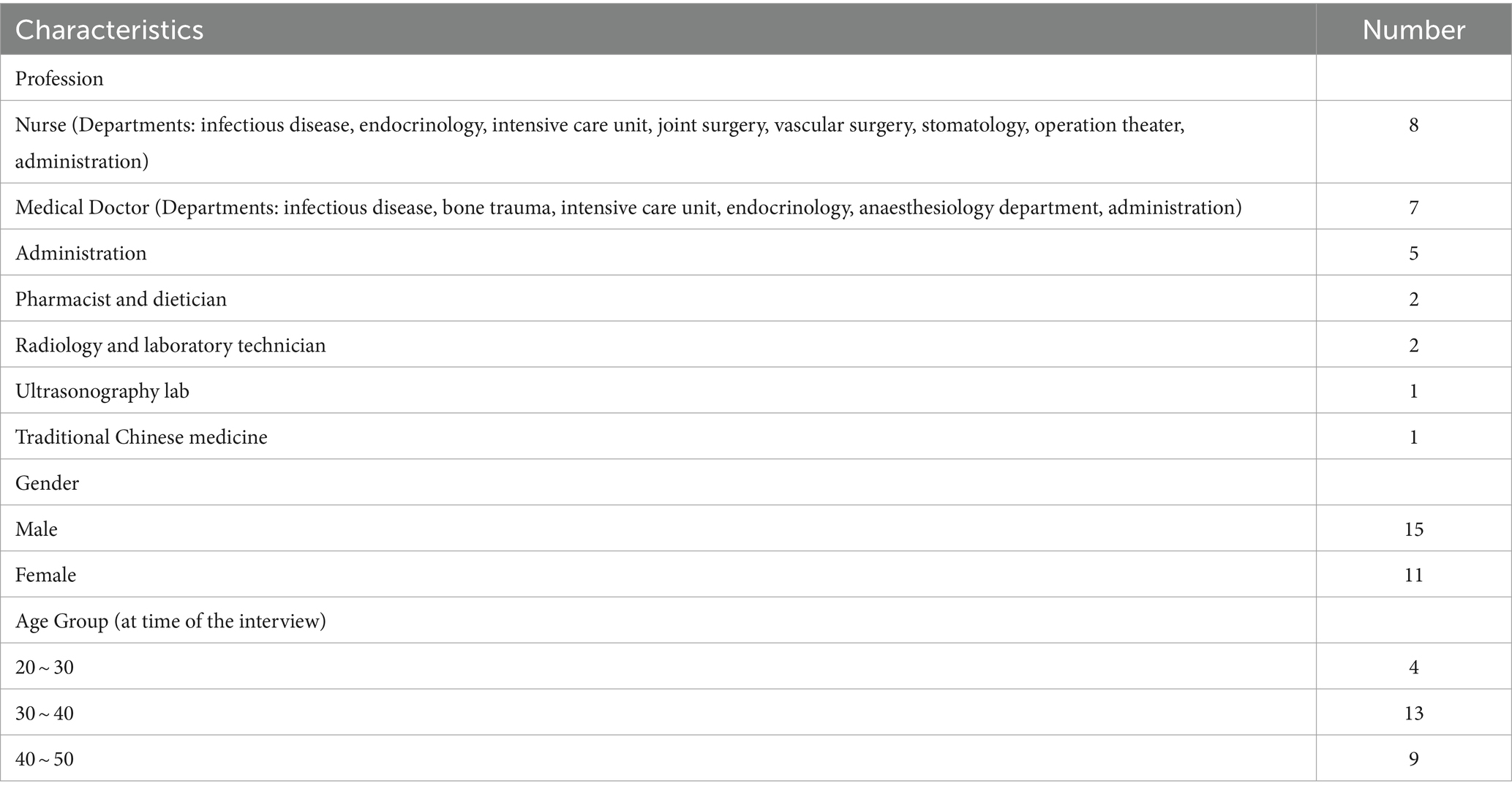
We conducted interviews with 26 hospital staff members from various functions and demographic backgrounds, as outlined in Table 2. The subsequent interview objects are represented by I1 to I27.
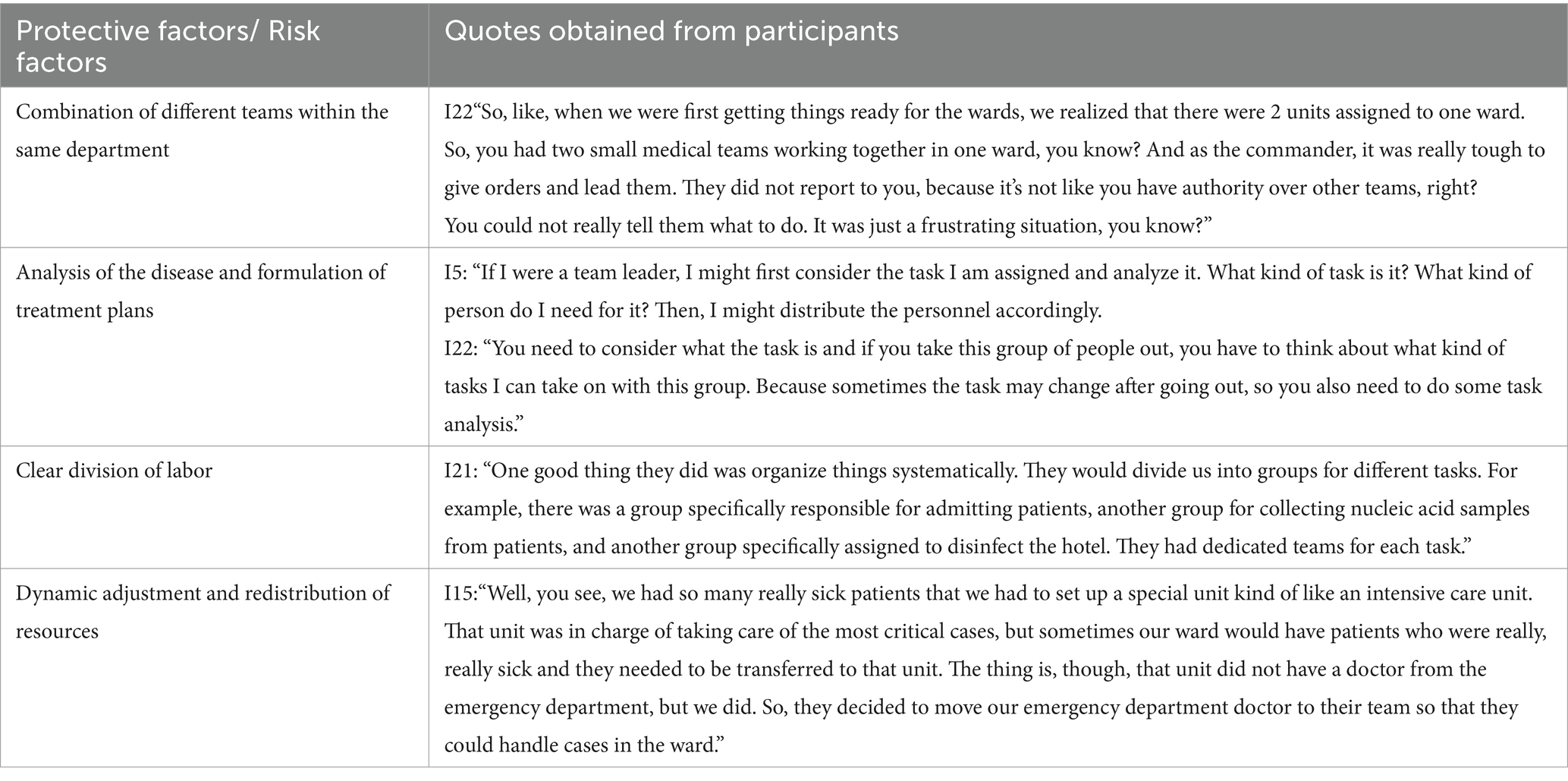
Based on the information gathered from these interviews, we identified five dimensions that encompass the protective factors and risk factors contributing to hospital resilience. These dimensions effectively capture the approaches, strategies, and perspectives of the interviewees in addressing major infectious disease outbreaks. Additionally, we observed that the interviewees not only analyzed the response from the hospital’s standpoint but also shared their personal perspectives. Consequently, we have included several personal-level protective factors and/or risk factors in Table 3, building upon the aforementioned five dimensions.
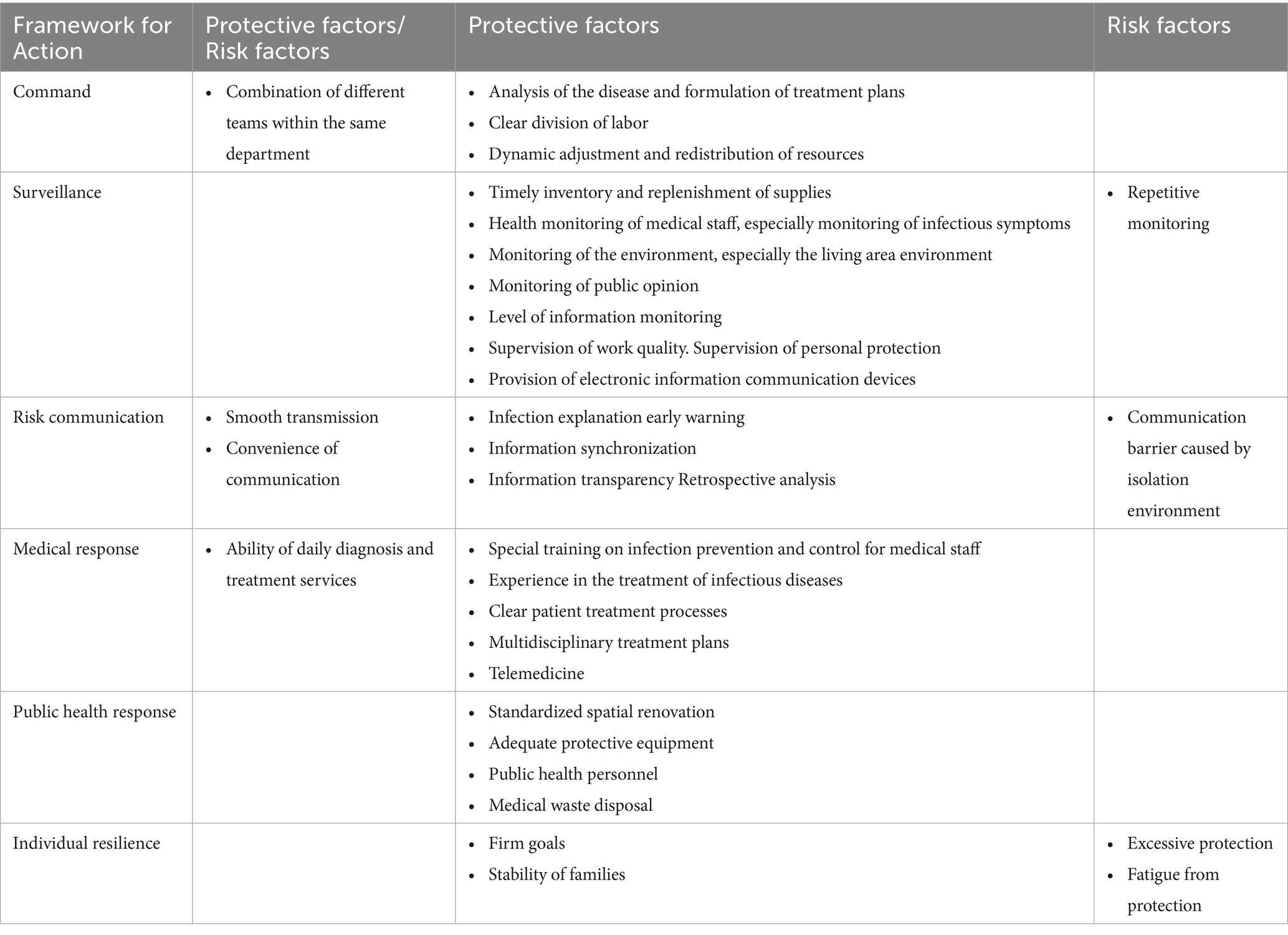
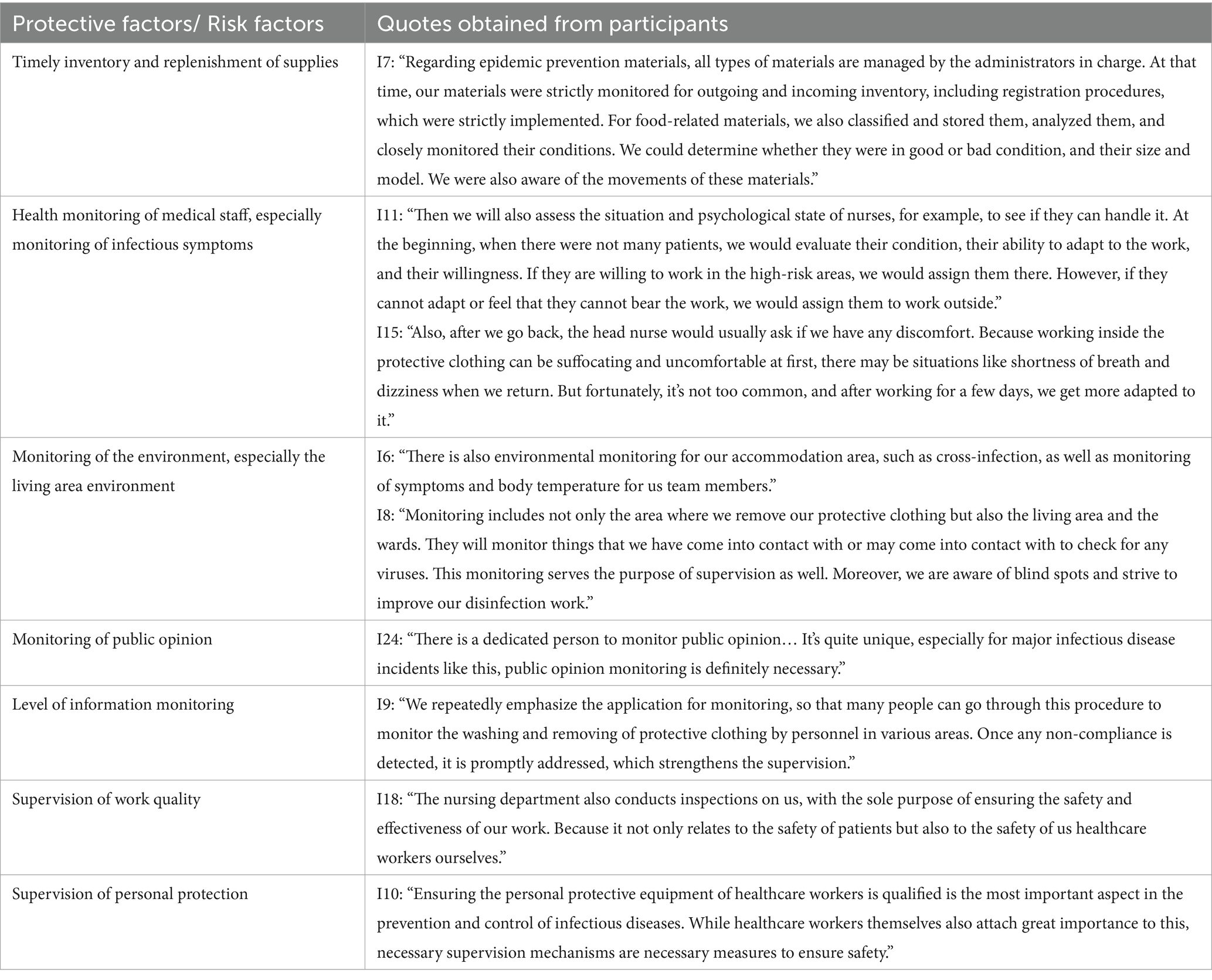
Table 3. Overview of hospital resilience protective and risk factors: content analysis based on interview information.
3.2 Protective and risk factors for hospital resilience
3.2.1 Command dimension
During the initial phase of a pandemic outbreak, hospitals often have personnel from various units working together. The amalgamation of different teams within the same department can have both positive and negative effects. On one hand, effective collaboration can result in a synergistic effect that surpasses the individual contributions. On the other hand, lack of familiarity among personnel can hinder coordination and impact the seamless progression of work.
The hospital command system’s command work is built upon a thorough analysis of the epidemic situation. This analysis serves as the basis for formulating appropriate treatment plans and defining roles. Furthermore, hospitals may need to dynamically adjust and control various aspects such as medical staff, departments, and the number of admitted patients to maintain a balance in internal operations, especially when faced with limited medical resources and nursing services (Table 4).
3.2.2 Surveillance dimension
Monitoring plays a crucial role in responding to infectious disease outbreaks, encompassing surveillance, supervision, and various aspects of hospital resilience. It is important to monitor the presence of the virus in the environment, particularly in the living areas of healthcare workers. Additionally, monitoring the usage of supplies and ensuring timely replenishment are also essential protective measures. Furthermore, during the initial stages of a pandemic outbreak, healthcare workers face significant challenges and stress, primarily due to the requirement of wearing protective equipment. Therefore, it becomes imperative to monitor their health closely. It is worth noting that this situation differs from other emergency response scenarios.
In major infectious disease outbreaks, various media platforms become avenues for public assistance. Hospitals actively pay attention to epidemic-related public opinions to gain insights into the public’s medical condition and verify the accuracy of hospital-related information. This proactive approach helps prevent the dissemination of misleading information that may lead to unnecessary panic.
Information monitoring devices can aid hospitals in remotely supervising the quality of work and ensuring that healthcare workers are wearing appropriate protective equipment. However, determining the optimal scale of monitoring poses a challenge. Excessive monitoring within a short timeframe can increase workload and reduce efficiency (Table 5).
“We focus on using surveillance in our work. Apart from the red zone, we can keep an eye on the movement of staff in different non-red zones using a program. If we notice any irregularities, we can promptly remind them as we can engage in dialogue and consultation. This has improved our supervision compared to how things were done in the past.”
3.2.3 Risk communication dimension
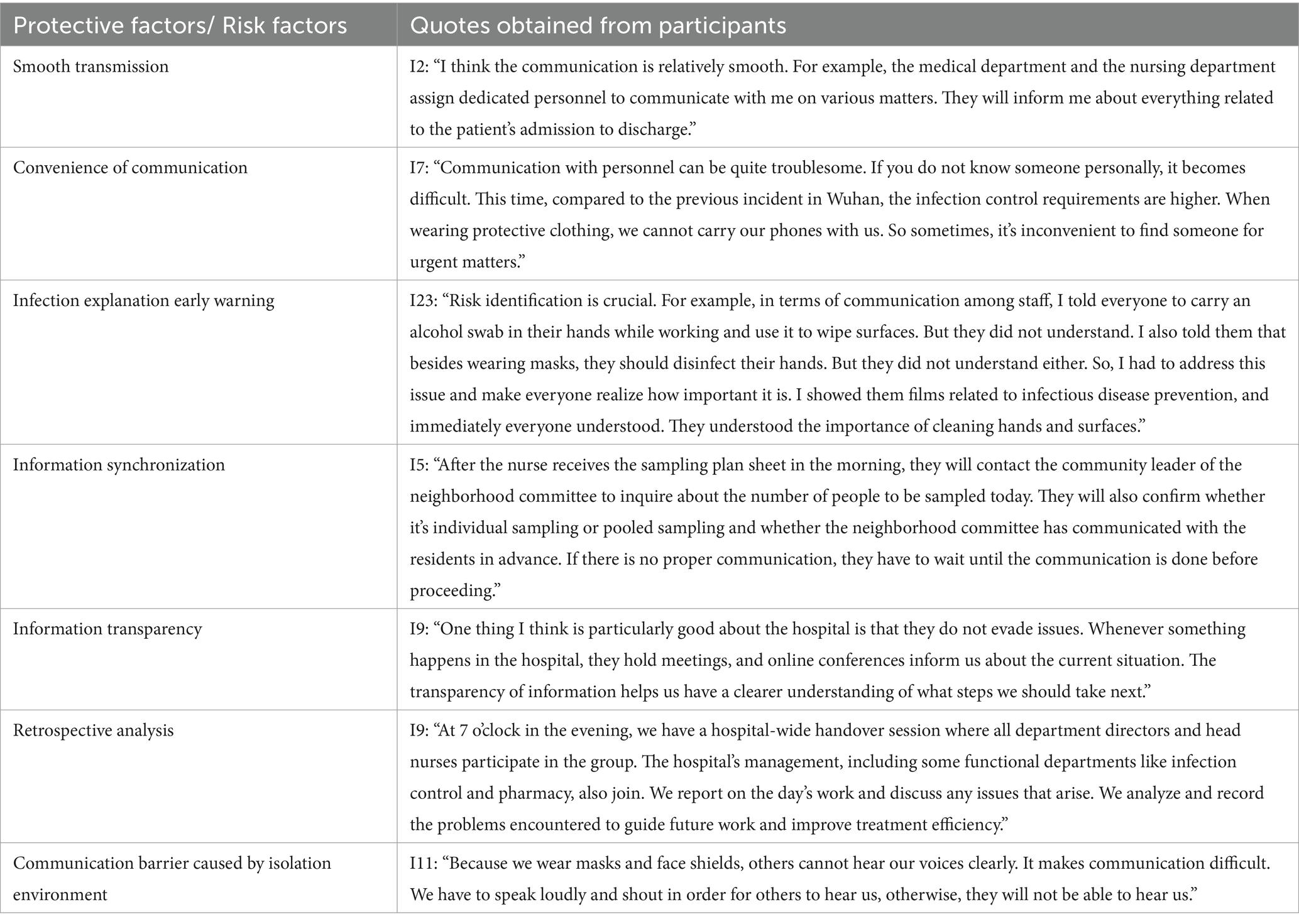
During the initial phases of a significant outbreak, the use of protective equipment and quarantine measures can create communication barriers that pose a risk to hospital resilience. To mitigate this, hospitals can implement electronic communication devices, which can enhance resilience. However, the effectiveness of these devices relies on the smooth transmission of information and communication.
Lack of understanding among healthcare workers regarding protective measures and treatment protocols in infectious disease environments, as well as the public’s limited comprehension of the necessity for frequent nucleic acid testing, contribute to the challenges of infection explanation and early warning. To address these issues, hospitals can provide explanations, demonstrations, and education to clarify the reasons for and risks associated with infection.
“If you just give healthcare workers instructions, they might follow them, but not necessarily do a great job. But if you explain why they should do it, once they grasp the reasons, they can perform their tasks more smoothly and find better solutions to problems. They will also have a stronger sense of initiative to accomplish these tasks.”
During major infectious disease outbreaks, there is a significant need for healthcare workers and the public to access information about disease transmission and updates on prevention and control measures. It is crucial to ensure that information is acquired and disseminated in a synchronized and transparent manner to enhance the trust of healthcare workers and the public in the hospital.
Healthcare workers involved in treating infectious diseases face various challenges and issues in their work, including treatment plans, infection control, emergencies, and protective procedures. Conducting post-incident reviews and making timely improvements based on the experiences and lessons learned can help prevent the occurrence of risky events (Table 6).
3.2.4 Medical response dimension
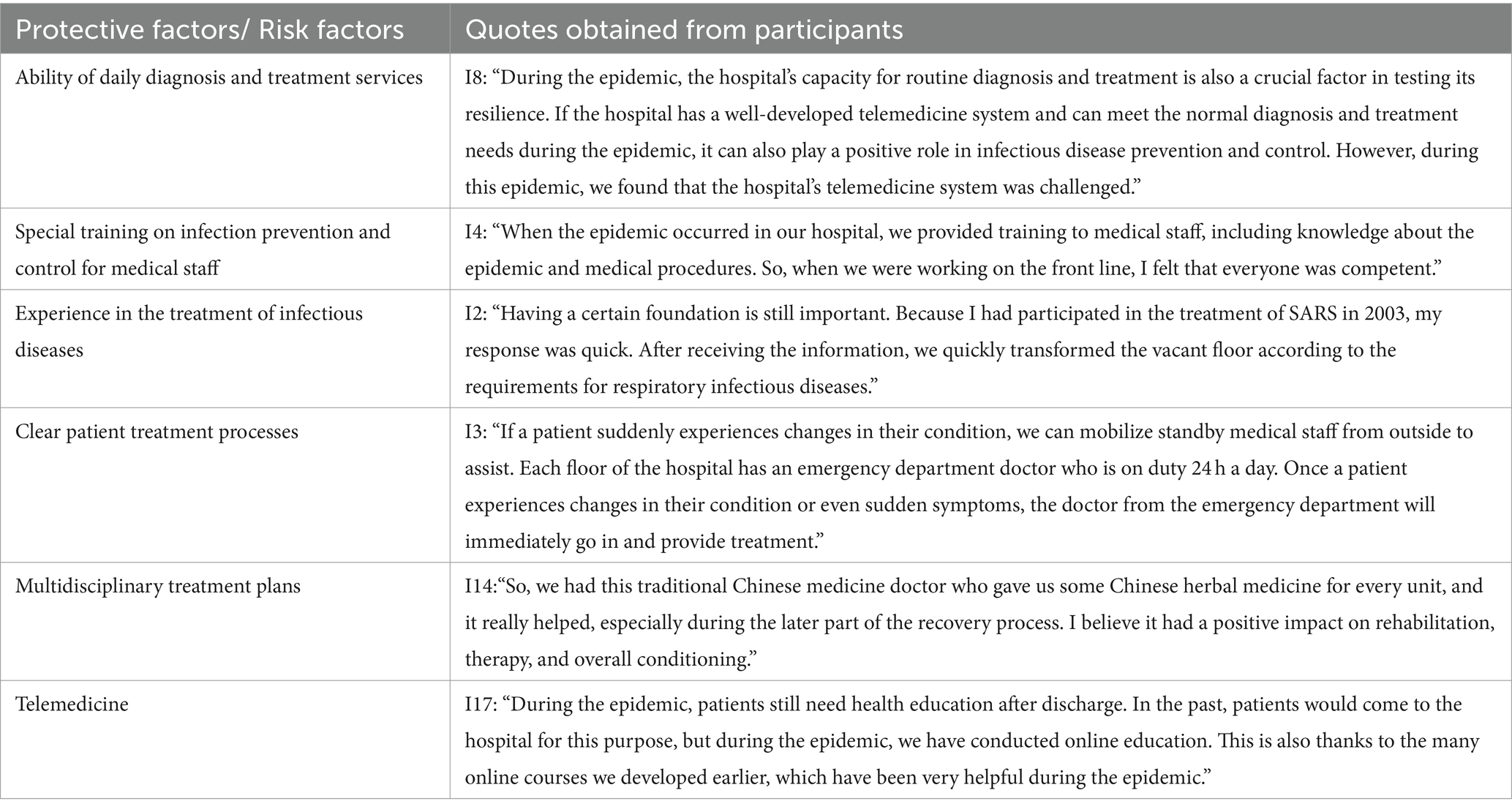
Proper training is essential for healthcare workers who are not specialized in handling infectious diseases. Incorporating previous experiences in managing infectious diseases like SARS can help healthcare workers quickly improve their skills. It is important for hospitals to establish clear patient treatment processes to ensure that healthcare workers understand the patient’s access and flow. Multidisciplinary treatment plans, such as traditional Chinese medicine and hyperbaric oxygen chambers, have demonstrated good efficacy in responding to COVID-19 and other similar emergencies.
“So, we had this traditional Chinese medicine doctor who gave us some Chinese herbal medicine for every unit, and it really helped, especially during the later part of the recovery process. I believe it had a positive impact on rehabilitation, therapy, and overall conditioning.”
During a pandemic, the diagnostic and treatment capacity of hospitals may be overwhelmed. In such situations, telemedicine can serve as an alternative means to assist the public with medical issues and ensure the smooth operation of hospitals. This is particularly relevant during infectious disease outbreaks (Table 7).
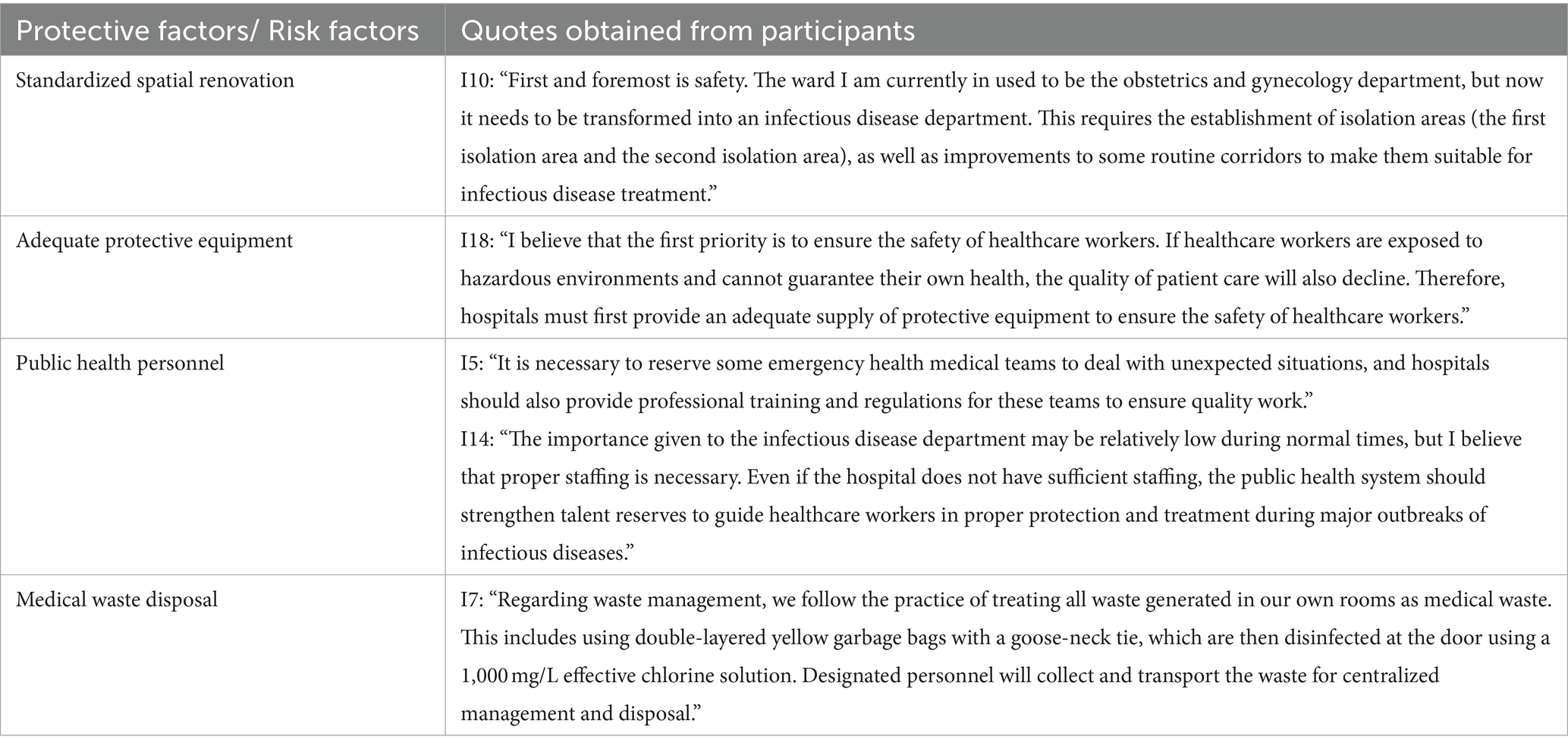
3.2.5 Public health response dimension
Hospitals can enhance the conditions for treating infectious diseases by remodeling their facilities and installing negative pressure wards, fresh air systems, and other air purification devices. This helps in preventing nosocomial infections. Additionally, hospitals should ensure the availability of personal protective equipment, strictly follow infection control measures, and promptly manage medical waste to prevent further spread and transmission of infectious diseases. Public health professionals play a crucial role in providing solutions and support for hospitals’ scientific public health response (Table 8).
3.2.6 Individual level
The resilience of healthcare workers is crucial for maintaining the resilience of hospitals. In the early stages of a pandemic outbreak, healthcare workers not only face the risk of infection but also experience significant work pressure, all while worrying about the safety of their families. Despite these challenges, they express pride and gratitude for their commitment to frontline work. The support from their families provides them with courage and strengthens their determination to overcome the epidemic. However, it is important to note that some healthcare workers may underestimate the severity of the outbreak, leading to a lax approach toward protective measures, which can further increase their psychological stress.
“I never expected something like this to happen to us, and all of a sudden, we had to deal with it without being mentally prepared.”
“There is excessive protection in some cases, and this situation is very common, where people wear three or four layers of masks.”
4 Discussion
Our study aims to investigate the actual experiences and emotions of healthcare workers in hospitals during the initial phases of a significant pandemic outbreak. Following the World Health Organization’s ‘Action Framework’ for responding to infectious diseases, we examine the factors that contribute to hospital resilience at each stage, both in terms of protection and risk. In contrast to current hospital resilience frameworks or models, our study offers more precise operational recommendations for enhancing hospital resilience.
At the onset of the COVID-19 pandemic, the concept of hospital resilience was relatively underexplored, primarily with a focus on disaster response. The Multidisciplinary Center for Earthquake Engineering Research (MCEER) in the United States proposed the classic 4R resilience theory, which subsequently served as a theoretical framework for subsequent resilience studies (19). With the outbreak of the pandemic, hospital resilience gained attention; however, most literature examined hospital resilience within the broader healthcare system rather than as a distinct entity. In our study, we specifically concentrate on the hospital system and conduct interviews with healthcare workers from various positions to gain insights into their experiences during the early stages of the pandemic. Building upon Richardson et al.’s resilience process model, we place emphasis on exploring protective and risk factors in establishing hospital resilience and offer practical operational guidance (13).
In this study, healthcare workers were temporarily assigned from different units, which is a common model in emergency response to infectious diseases (20). This model facilitates collaboration among healthcare professionals from various disciplines to deliver comprehensive treatment. However, it also presents challenges for command and management personnel, as the effectiveness of management directly affects the development of hospital resilience. Therefore, management should be guided by timely analysis of the pandemic situation, the development of scientific treatment plans, and the rational allocation of personnel.
Resilience development necessitates ongoing adaptation (21). Numerous studies have highlighted the dynamic nature of resilience (22, 23). Our findings indicate that responding to major infectious disease outbreaks, particularly in their early stages, demands continuous adjustment and optimization of response plans. This represents a significant departure from the routine operations of hospitals, which have well-established systems in place. However, during major infectious disease outbreaks, the situation is often characterized by uncertainty and unknown factors. As a result, management personnel must adjust resources based on the trajectory of the disease, necessitating regular review. Experienced personnel, including those who have dealt with previous infectious disease outbreaks, as well as professionals in public health, play a crucial role in guiding this process.
We have also identified several unique aspects related to major infectious disease outbreaks. One crucial aspect is the continuous monitoring of healthcare workers’ health, particularly for symptoms of infection, to ensure their ability to work under normal conditions. Previous studies have highlighted the dual burden faced by healthcare workers during disaster response, as they juggle family responsibilities and hospital duties (24, 25). However, our study revealed that healthcare workers expressed positive coping strategies, such as having clear goals and receiving support from their families. This reflects the unity among the people during that national crisis. Given the extensive scope and rapid spread of the pandemic, both the general public and healthcare workers paid close attention to news updates, and the timely and transparent dissemination of information became crucial factors influencing the resilience of hospitals. The increased demand for online consultations by the public during the pandemic underscored the importance of continuous routine healthcare in bolstering hospital resilience. Consequently, telemedicine emerged as a protective factor in the development of hospital resilience.
Quality control in response to infectious diseases should not be neglected. Regular inspections by internal and external stakeholders, such as hospitals, health authorities, and other relevant organizations, are necessary to evaluate the effectiveness of the hospital’s epidemic prevention and treatment measures, identify potential risks, and implement necessary improvements. Information monitoring devices within hospitals can provide a convenient means of monitoring, enhancing efficiency, and minimizing personnel movement, thereby preventing cross-infection. However, it is important to strike a balance as excessive monitoring during an epidemic can significantly burden healthcare workers.
The public health response is a crucial factor that distinguishes major infectious disease outbreaks from other disasters. In order to prevent further spread and transmission, hospitals should prioritize the provision of personal protective equipment and diligently enforce infection control measures. These measures include thorough surface cleaning and disinfection, as well as proper management of medical waste, to prevent nosocomial infections (26). The unique characteristics of protective equipment present challenges in communication among healthcare workers, as restrictions may limit verbal communication and the use of mobile phones. Consequently, there has been a focus on developing and enhancing information communication devices.
5 Limitations
Although our selection of interviewees was diverse, it is possible that we overlooked certain roles, such as hospital directors and personnel from disease control centers, that could have provided valuable insights and enriched our analysis. Additionally, it is important to note that the protective and risk factors for hospital resilience identified in this study may be influenced by the broader community, healthcare system, and other hospitals, which were not included in our research. Therefore, it is crucial for future studies to thoroughly investigate these factors to gain a more comprehensive understanding.
6 Conclusion
This research paper has shed light on the critical role of resilient hospitals in effectively managing major infectious disease outbreaks. By adhering to the World Health Organization’s infectious disease response framework and conducting interviews with frontline healthcare workers, this study has identified protective and risk factors for hospital resilience at each stage. The findings of this research offer valuable guidance to hospitals in their efforts to enhance resilience in future actions. Moreover, this study reinforces the significance of individual well-being in facilitating sustained work and resilience development within hospitals, aligning with prior research. Ultimately, this research paper contributes to the field by presenting a comprehensive approach to addressing the challenges posed by infectious disease outbreaks and fostering hospital resilience.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Navy Military Medical University, the author’s affiliated institution. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
WS: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. RC: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. KW: Data curation, Investigation, Writing – original draft. YW: Writing – review & editing. LG: Conceptualization, Formal analysis, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was funded by National Natural Science Foundation of China (72174205); Deep Blue Nursing Research “Zhuyuan” Talent Program Project (2022KYZ02).
Acknowledgments
We thank Anhua Qiao for her support during the interview and all the hospital staff who participated in the interviews.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ling, E, Larson, E, Macauley, R, Kodl, Y, VanDeBogert, B, Baawo, S, et al. Beyond the crisis: did the Ebola epidemic improve resilience of Liberia’s health system? Health Policy Plan. (2017) 32:40–7. doi: 10.1093/heapol/czx109
2. Kola, L. COVID-19: boost mental-health resilience. Nature. (2022) 601:26. doi: 10.1038/d41586-021-03838-z
3. Carenzo, L, Costantini, E, Greco, M, Barra, FL, Rendiniello, V, Mainetti, M, et al. Hospital surge capacity in a tertiary emergency referral Centre during the COVID-19 outbreak in Italy. Anaesthesia. (2020) 75:928–34. doi: 10.1111/anae.15072
4. Ravaghi, H, Khalil, M, Al-Badri, J, Naidoo, AV, Ardalan, A, and Khankeh, H. Role of hospitals in recovery from COVID-19: reflections from hospital managers and frontliners in the eastern Mediterranean region on strengthening hospital resilience. Front Public Health. (2023) 10:2296–565. doi: 10.3389/fpubh.2022.1073809
5. Zhong, S, Clark, M, Hou, XY, Zang, Y, and FitzGerald, G. Validation of a framework for measuring hospital disaster resilience using factor analysis. Int J Environ Res Public Health. (2014) 11:6335–53. doi: 10.3390/ijerph110606335
6. Moitinho de Almeida, M, van Loenhout, JAF, Singh Thapa, S, Kumar, KC, Prakash Mahara, D, Guha-Sapir, D, et al. Hospital resilience after the 2015 earthquake in Nepal: results from semi-structured interviews with hospital staff. Front Public Health. 9:602509. doi: 10.3389/fpubh.2021.602509
7. Khalil, M, Ravaghi, H, Samhouri, D, Abo, J, Ali, A, Sakr, H, et al. What is "hospital resilience"? A scoping review on conceptualization, operationalization, and evaluation. Front Public Health. (2022) 10:1009400. doi: 10.3389/fpubh.2022.1009400
8. Holling, SC. Resilience and stability of ecological systems. Annu Rev Ecol Evol Syst. (1973) 4:1–23. doi: 10.1146/annurev.es.04.110173.000245
9. Bronfenbrenner, U. Making human beings human: bioecological perspectives on human development. Thousand Oaks, CA: Sage Publications (2005).
10. Paschoalotto, M, Lazzari, EA, Rocha, R, Massuda, A, and Castro, MC. Health systems resilience: is it time to revisit resilience after COVID-19? Soc Sci Med. (2023) 320:115716. doi: 10.1016/j.socscimed.2023.115716
11. Rk, C. Risk factors and effects of the Morbus: COVID-19 through the biopsychosocial model and ecological systems approach to social work practice. Soc Work Public Health. (2021) 36:98–117. doi: 10.1080/19371918.2020.1859035
12. Wernli, D, Clausin, M, Antulov-Fantulin, N, Berezowski, J, Biller-Andorno, N, Blanchet, K, et al. Building a multisystemic understanding of societal resilience to the COVID-19 pandemic. BMJ Glob Health. (2021) 6:e006794. doi: 10.1136/bmjgh-2021-006794
13. Richardson, G, Neiger, B, Jenson, S, and Kumpfer, K. The resilience model. Health Educ. (1990) 21:33–9. doi: 10.1080/00970050.1990.10614589
15. Craig, AT, Kasai, T, Li, A, Otsu, S, and Khut, QY. Getting back to basics during a public health emergency: a framework to prepare and respond to infectious disease public health emergencies. Public Health. (2010) 124:10–3. doi: 10.1016/j.puhe.2009.11.011
16. Phelan, AL, Katz, R, and Gostin, LO. The novel coronavirus originating in Wuhan, China: challenges for Global Health governance. JAMA. (2020) 323:709–10. doi: 10.1001/jama.2020.1097
17. Bradley, EH, Curry, LA, and Devers, KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. (2007) 42:1758–72. doi: 10.1111/j.1475-6773.2006.00684.x
18. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. 10.1093/intqhc/mzm042. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
19. Bruneau, M, Chang, SE, Eguchi, RT, Lee, GC, O'Rourke, TD, Reinhorn, AM, et al. A framework to quantitatively assess and enhance the seismic resilience of communities. Earthquake Spectra. (2003) 19:733–52. doi: 10.1193/1.1623497
20. Tadmor, B, McManus, J, and Koenig, KL. The art and science of surge: experience from Israel and the U.S. Acad Emerg Med. (2006) 13:1130–4. doi: 10.1197/j.aem.2006.06.043
21. Kruk, ME, Myers, M, Varpilah, ST, and Dahn, B. What is a resilient health system? Lessons from Ebola. Lancet. (2015) 385:1910–2. doi: 10.1016/S0140-6736(15)60755-3
22. Norris, FH, Stevens, SP, Pfefferbaum, B, Wyche, KF, and Pfefferbaum, RL. Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. Am J Community Psychol. (2008) 41:127–50. doi: 10.1007/s10464-007-9156-6
23. Schelfaut, K, Pannemans, B, Craats, I, Krywkow, J, Mysiak, J, and Cools, J. Bringing flood resilience into practice: the FREEMAN project. Environ Sci Pol. (2011) 14:825–33. doi: 10.1016/j.envsci.2011.02.009
24. Oh, RN, Hong, N, Ryu, DH, Bae, SG, Kam, S, and Kim, K. Exploring nursing intention, stress, and professionalism in response to infectious disease emergencies: the experience of local public hospital nurses during the 2015 MERS outbreak in South Korea. Asian Nurs Res. (2017) 11:230–6. doi: 10.1016/j.anr.2017.08.005
25. Slykerman, RF, Li, E, and Booth, RJ. Improvement in the psychological health of nurses working during the COVID-19 pandemic. Nurs Forum. (2022) 57:87–93. doi: 10.1111/nuf.12660
Keywords: public health, infectious diseases, hospital resilience, qualitative research, hospital staff
Citation: Shi W, Chen R, Wang K, Wang Y and Gui L (2024) Exploring hospital resilience protective or risk factors: lessons for future disaster response efforts. Front. Public Health. 12:1378257. doi: 10.3389/fpubh.2024.1378257
Edited by:
Davide Rasella, Instituto Salud Global Barcelona (ISGlobal), SpainReviewed by:
Erwin Calgua, Universidad de San Carlos de Guatemala, GuatemalaJerrald Lau, National University of Singapore, Singapore
Copyright © 2024 Shi, Chen, Wang, Wang and Gui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Gui, Z3VpbGkyMDAwQHFxLmNvbQ==
†These authors share first authorship
 Wenwen Shi
Wenwen Shi Rujie Chen1,2†
Rujie Chen1,2†