
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 08 April 2024
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1376404
This article is part of the Research Topic World TB Day 2023: Yes! We can end TB View all 30 articles
 Rui Ge1†
Rui Ge1† Guoying Zhu1†
Guoying Zhu1† Min Tian2†
Min Tian2† Zhigang Hou1
Zhigang Hou1 Weizhe Pan1
Weizhe Pan1 Hao Feng1
Hao Feng1 Kui Liu3*
Kui Liu3* Qinfeng Xiao4*
Qinfeng Xiao4* Zhongwen Chen1*
Zhongwen Chen1*Background: Tuberculosis (TB) is recognized as a significant global public health concern. Still, there remains a dearth of comprehensive evaluation regarding the specific indicators and their influencing factors of delay for adolescents and young adults.
Methods: All notified pulmonary TB (PTB) patients in Jiaxing City were collected between 2005 and 2022 from China’s TB Information Management System. Logistic regression models were conducted to ascertain the factors that influenced patient and health system delays for PTB cases, respectively. Furthermore, the impact of the COVID-19 pandemic on local delays has been explored.
Results: From January 1, 2005 to December 31, 2022, a total of 5,282 PTB cases were notified in Jiaxing City, including 1,678 adolescents and 3,604 young adults. For patient delay, female (AOR: 1.18, 95%CI: 1.05–1.32), PTB complicated with extra-pulmonary TB (AOR: 1.70, 95% CI: 1.28–2.26), passive case finding (AOR: 1.46, 95% CI: 1.07–1.98) and retreatment (AOR: 1.52, 95% CI: 1.11–2.09) showed a higher risk of delay. For health system delay, minorities (AOR: 0.69, 95% CI: 0.53–0.90) and non-students (AOR: 0.83, 95% CI: 0.71–0.98) experienced a lower delay. Referral (AOR: 1.46, 95% CI: 1.29–1.65) had a higher health system delay compared with clinical consultation. Furthermore, county hospitals (AOR: 1.47, 95% CI: 1.32–1.65) and etiological positive results (AOR: 1.46, 95% CI: 1.30–1.63) were associated with comparatively high odds of patient delay. Contrarily, county hospitals (AOR: 0.88, 95% CI: 0.78–1.00) and etiological positive results (AOR: 0.67, 95% CI: 0.59–0.74) experienced a lower health system delay. Besides, the median of patient delay, health system delay, and total delay during the COVID-19 pandemic were significantly lower than that before.
Conclusion: In general, there has been a noteworthy decline in the notification rate of PTB among adolescents and young adults in Jiaxing City while the declining trend was not obvious in patient delay, health system delay, and total delay, respectively. It also found factors such as gender, case-finding method, and the hospital level might influence the times of seeking health care and diagnosis in health agencies. These findings will provide valuable insights for refining preventive and treatment strategies for TB among adolescents and young adults.
Tuberculosis is a chronic respiratory infectious disease caused by Mycobacterium tuberculosis (Mtb), which seriously endangers human health (1). Prior to the COVID-19 pandemic, TB held the unfortunate distinction of being the primary cause of death caused by a single infectious agent, surpassing even HIV/AIDS in terms of mortality rates (2). An estimated 2.28 million adolescents and young adults were diagnosed with TB worldwide in 2022, which accounted for approximately 21.5% of all newly reported TB patients (2). Adolescents and young adults are particularly susceptible to TB, as this age group commonly experiences a significant increase in both exposure to TB and rising pressure derived from learning and work (3). In the high burden countries, adolescents and young adults make up a substantial proportion of the general population and a substantial proportion of TB patients. The incidence of TB in China ranks third around the world, and it is also listed as one of the 22 high-burden countries (2). According to the release of the Global TB Report in 2023, there were an estimated 748,000 TB patients and 30,000 died from the disease in 2022 in China, while the reported rate of TB among young and older people was higher than other subgroups (2, 4). Thus, controlling TB among adolescents and young adults is of paramount importance for effectively managing the TB epidemic in China.
Although the strategy of passive case-finding was the mainstream of prevention and control of TB in most countries, it could not hold back TB epidemic and realize the goal of ending TB (5). To ensure effective control of TB and minimize its impact, it is crucial to diagnose the disease early and prompt sufficient treatment. By promptly identifying TB in individuals, treatment could be initiated without delay and prevent further progression of the TB within their body (6). Moreover, timely treatment initiation also plays a significant role in reducing the risk of community transmission. Various factors contribute to the delay (7–9). Consequently, it is imperative to identify them to implement interventions that will optimize the effectiveness of TB control programs.
This study aimed to analyze the changed trend of delay and its influencing factors of TB among adolescents and young adults in Jiaxing City, which would provide a basis for formulating corresponding prevention and control measures, to promote early detection and treatment of TB.
Jiaxing City, one of the 11 cities under the jurisdiction of Zhejiang Province, is located in the southeast coastal area of China. It consists of 7 counties like Nanhu, Xiuzhou, Haining, Tongxiang, Jiashan, Pinghu, and Haiyan. The total area of Jiaxing City is 3,915 km2. According to the seventh population census, the permanent population in Jiaxing City was 5,400,868, with nearly 722,920 people aged 10–24 years, accounting for 13.39% of the total population. Additionally, Jiaxing City has an average annual temperature of 15.9°C and an annual cumulative precipitation of 1168.6 mm. The location of Jiaxing City is shown in Figure 1.
In this study, we collected all notified pulmonary TB (PTB) cases aged 10–24 years between 2005 and 2022 from China’s TB information management system, which included the details of demographic, treatment, and laboratory testing information of patients (10).
All included pulmonary PTB patients were diagnosed according to the National Diagnostic Criteria for Pulmonary Tuberculosis (WS288-2008 and WS288-2017) and the Classification of Tuberculosis (WS196-2001 and WS196-2017) in China, including laboratory-confirmed TB and clinically diagnosed TB (11, 12). Laboratory-confirmed PTB was defined as people who were diagnosed with bacteriological evidence from a sputum smear, sputum culture, or suitable rapid diagnostic technology such as Gene-Xpert. These tests are instrumental in identifying and confirming cases of PTB through the detection of specific pathogens. Additionally, clinically diagnosed PTB refers to the comprehensive diagnosis based on the patient’s epidemiological history, clinical symptoms, imaging manifestations, and negative sputum smear results (13).
Patient delay was defined as the interval days between the first appearance of PTB symptoms and the first visit to a medical institution. Health system delay refers to the interval days between the first visit to a medical institution and the confirmed diagnosis of PTB (14). Total delay consisted of patient delay and health system delay (15). The distribution of different delays at various time points did not follow a normal pattern, therefore median days were utilized as a threshold to define delays. Case-finding methods were divided into active and passive methods: (1) Active method included active screening and physical examination; (2) Passive method included directly seeking medical care and recommendations from other health institutions, etc.
Descriptive analysis was conducted to present the general epidemiological characteristics of the demographic information. Continuous variables were reported using the median and interquartile range (IQR), while categorical variables were presented as counts and proportions. The Mann–Whitney test was utilized to compare two groups, while the Kruskal-Wallis test was employed for comparing three or more groups. The influencing factors of delay were analyzed using univariate and multivariate logistic regression models. Additionally, the annual percentage change (APC) of TB incidence among adolescents and young adults from 2005 to 2022 was calculated by Joinpoint 5.0.2. The geographic information of Jiaxing City was visualized using ArcGIS 10.9. SPSS 26.0 was used for statistical analysis. All variables significantly associated with the delay were identified based on a p-value less than 0.05.
From January 1, 2005 to December 31, 2022, a total of 5,282 PTB cases were notified in Jiaxing City, including 1,678 adolescents and 3,604 young adults. This accounts for approximately 15.32% (5,282/34487) of the total number of PTB cases during that period. The gender ratio was 1.61:1, with males slightly outnumbering females. Students accounted for approximately 17% of all cases, and the majority of cases (92.3%) were of Han nationality. Additionally, migrant PTB cases made up a significant proportion, accounting for 84.17% of the total cases. The notification rate of this specific group showed two distinct stages of change during this period. Initially, the notification rate increased from 32.59 per 100,000 in 2005 to 59.84 per 100,000 in 2007 (APC = 37.76%, p < 0.05). However, the notification rate then decreased from 64.76 per 100,000 in 2008 to 12.86 per 100,000 in 2022, indicating a downtrend (APC = −7.43%, p < 0.05).
The median of total delay was 13 (7–34) in Jiaxing City and the proportion of total delay was 54.17% (2,861/5,282). Meanwhile, the median for patient delay was 11 (3–30) and the proportion of patient delay was 48.85% (2,580/5,282). The median of health system delay was 1 (0, 4) and the proportion of health system delay was 46.19% (2,440/5,282). The annual proportion of delays is presented in Figure 2. There were no significant annual differences in patient delay, health system delay, and total delay during the study period (all p > 0.05). The results are shown in Table 1.

Table 1. Demographic characteristics of adolescents and young adults with PTB from 2005 to 2021 in Jiaxing City.
The univariate and multiple logistic models were conducted to estimate the influencing factors of patient delay and health system delay. For patient delay, female (AOR: 1.18, 95%CI: 1.05–1.32), PTB complicated with extra-pulmonary TB (AOR: 1.70, 95% CI: 1.28–2.26), passive case-finding (AOR: 1.46, 95% CI: 1.07–1.98) and retreatment (AOR: 1.52, 95% CI: 1.11–2.09) showed a higher delay. For health system delay, minorities (AOR: 0.69, 95% CI: 0.53–0.90) and non-students (AOR: 0.83, 95% CI: 0.71–0.98) experienced a lower delay. Referral (AOR: 1.46, 95% CI: 1.29–1.65) had a higher health system delay compared with clinical consultation.
Furthermore, county hospitals (AOR: 1.47, 95% CI: 1.32–1.65) and etiological positive (AOR: 1.46, 95% CI: 1.30–1.63) were associated with high odds of patient delay. Contrarily, county hospitals (AOR:0.88, 95% CI: 0.78–1.00) and etiological positive (AOR: 0.67, 95% CI: 0.59–0.74) experienced a lower health system delay. This information is presented in Tables 2, 3.
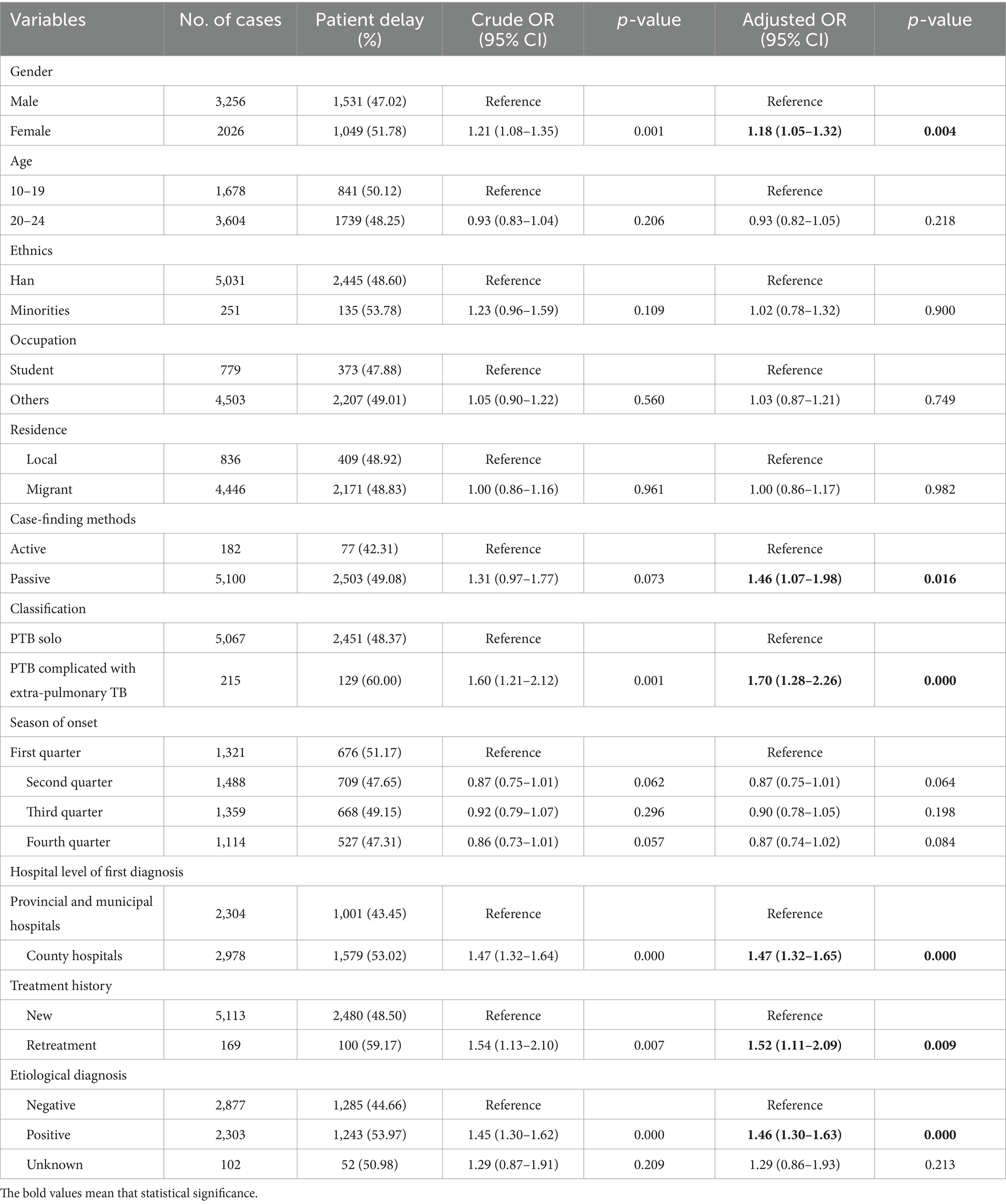
Table 2. The influencing factors analysis of patient delay among adolescents and young adults with PTB.
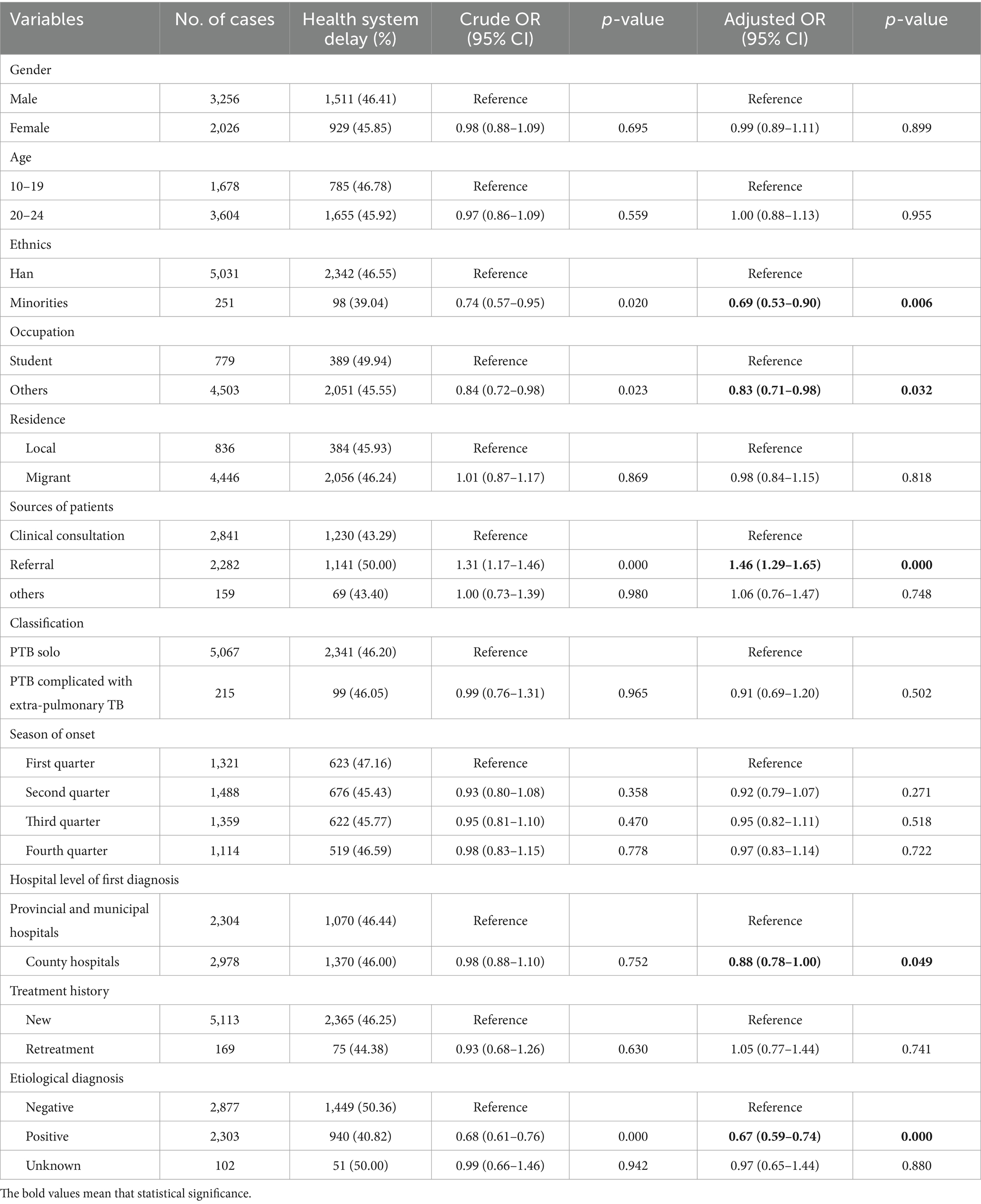
Table 3. The influencing factors analysis of health system delay among adolescents and young adults with TB.
Considering the impact of the COVID-19 pandemic, we classified the cases notified around 2020 and compared the differences in delays using the Mann–Whitney test. The median of patient delay, health system delay, and total delay of 2020–2022 were significantly lower than those of 2005–2019, respectively. This information is presented in Table 4.
In this study, we conducted a comprehensive analysis of the PTB notification rate among adolescents and young adults in Jiaxing City over the last dozen years, as well as patient delay and health system delay. From 2005 to 2022, a total of 5,282 PTB patients aged 10–24 years were notified in Jiaxing City, accounting for 15.32% of the overall cases. This percentage aligns with the global estimates (2). In recent years, China has implemented the directly observed treatment short-course (DOTS) and the “End TB strategy” to enhance the prevention and control of tuberculosis (16–18). As a result of these strategies, the incidence rate and number of notified cases among individuals aged 10–24 years in Jiaxing City have shown a declining trend since 2008. The median patient delay and health system delay in Jiaxing were 11 and 1, respectively, which were lower than the overall levels observed in China and some findings from other countries (19–22). Despite the median time of PTB delay in Jiaxing City being consistently low, there was no significant decrease in the risk of delay between 2005 and 2022. Given seeking medical care with delay exacerbating the burden of tuberculosis and escalating the financial strain on patients, families, and the wider public health system, it therefore highlighted the ongoing need for improved control measures to reduce delays across various stages (23). Besides, a series of specific interventions such as targeted educational campaigns, community outreach programs, the improvement of healthcare infrastructure, and innovative approaches to case detection and treatment initiation also should be strengthened in the future.
In addition, we performed a thorough analysis of various factors, such as gender, age, ethnicity, occupation, and the mode of case-finding, to examine the relationship of influencing factors and delay. Our findings indicated that there was a higher proportion of patient delay among females than males. That is to say, females tend to delay the behavior of seeking health care when presenting PTB symptoms (24). This result was consistent with some available study that listed females emerged as a significant factor associated with a reduced likelihood of seeking diagnosis and treatment for TB (25). In general, airborne pathogens are expected to pose an equal biological risk to all individuals. The reasons for the discrepancy of delay among gender might be attributed to the susceptibility of stigma and vulnerability to PTB. Females were found to have a higher level of TB-related stigma compared to males, which can limit their access to medical care (26). Additionally, due to their vulnerability and unique physiological characteristics, female patients may present milder symptoms than their male counterparts, potentially leading to delays in seeking medical care (27). Thus, the stigma caused by TB needs to be eliminated through extensive and effective health education and health promotion. PTB patients with extra-pulmonary TB demonstrated a higher likelihood of experiencing patient delay. Specifically, patients with extra-pulmonary TB were found to be 1.70 times more likely to delay the diagnosis compared to PTB (AOR = 1.70, 95%CI: 1.28–2.26). Tuberculosis, as a disease associated with poverty, is linked to the timeliness of disease detection, severity, and prognosis with the economic status of patients (28). It is speculated that PTB patients with extra-pulmonary TB may be constrained by their economic conditions and understanding of the disease, thereby increasing the risk of patient delay. Furthermore, the presence of PTB along with extra-pulmonary TB could also lead to the complex clinical presentations and make the PTB diagnosis difficult (29). These findings align with similar studies indicating that PTB patients with extra-pulmonary TB are more prone to delay seeking medical care compared to those with only PTB (29, 30). This emphasizes the importance of providing specific attention in clinical practice to PTB patients with extra-pulmonary TB to enhance the early detection to prevent further complications and transmission.
Retreatment was identified as an independent risk factor for patient delay in our study. Retreatment PTB refers to patients who have received inconsistent anti-TB treatment for more than 1-month, experienced treatment failure, and subsequently relapsed (31). These individuals tend to undervalue their health status and lack the motivation to actively seek medical care. This reminder highlights the importance of paying attention to retreated patients in TB surveillance and active case finding, as this is also important in preventing the emergence of drug resistance (31). Moreover, this study found that active case-finding has been demonstrated to be more effective in reducing patient delay compared to passive case-finding.
Our study also revealed several findings regarding the factors influencing health system delay. We observed that minorities and non-students had a lower risk of experiencing health system delay. Our further analysis found that 90% of minorities and non-students were from workers. In Zhejiang Province, nearly all employees were requested for the pre-employment physical examinations and annual health check-ups. Once people with suspected PTB were considered, the company will require them to seek medical care for a definitive diagnosis, thereby reducing potential health system delay among these groups. Meanwhile, student population generally had heavy study loads, and faced with potential suspension of schooling and possible stigma, leading to poor pre-diagnostic compliance and exacerbating health system delay. In this study, the risk was 1.46 times higher for referral patients compared to those who sought clinical consultation directly. This could be attributed to the fact that referral patients seek medical care across different healthcare institutions, leading to a prolonged diagnostic process. Despite the median health system delay in Jiaxing City being only 1 day, in the context of rapid diagnostic technology taking only 4 h to diagnose, there is still a need for improvement in implementing control measures aimed at reducing health system delay across various stages.
Patient delay at the county level of first diagnosis was found to be higher compared to city-level and higher medical institutions, which might be attributed to characteristics of the visiting population. Patients seeking medical care in county-level hospitals generally have limited economic conditions, milder symptoms, and lower awareness of the disease compared to those in higher-level hospitals. Nevertheless, county hospitals presented a lower health system delay than higher-level hospitals. With the development of primary healthcare services and improved TB screening capabilities in China (16, 18), the health system delay in county-level hospitals are relatively low. People with TB can receive timely TB diagnosis and treatment services when seeking medical care. Conversely, higher-level hospitals receive mainly referrals with complicated condition resulting in a longer time to diagnosis than county hospitals. Our study has indicated that patients with positive etiology are at a higher risk of patient delay and a lower health system delay. The patient delay may be related to the interactive influence and causal transformation between etiology and outcome (32). Meanwhile, with improved etiological detection in hospitals and the availability of Mtb testing, people with a positive etiology are more likely to receive confirmation.
The COVID-19 pandemic is bound to have an impact on the detection and diagnosis of tuberculosis. To assess its effect on the identification of PTB among adolescents and young adults in Jiaxing City more accurately, we compared various types of delays between two time periods: 2005–2019 and 2020–2022. An obvious decline of notified PTB cases was observed in our study during 2020–2022, which was consistent with some studies in China (33–35). The reason may be partly attributed to the implementation of COVID-19 prevention and control policies. Some implementations of non-pharmaceutical interventions in China, such as social distancing and community containment measures, effectively prevented the transmission of COVID-19 until the end of 2022 (19, 36). Interestingly, our study found a significant reduction in delays after 2019. We speculated that the increased awareness for seeking health care among young people, especially presenting serious respiratory symptom like COVID-19 may lead to the increased identification of PTB cases, thereby reducing patient delay. Additionally, the enhancement of etiological detection in hospitals also played a pivotal role in mitigating the health system delay. Still, some rigorous containment measures during the pandemic might impeded the access of non-urgent patients or asymptomatic patients to hospitals, lowering the finding of active PTB and thereby increasing the risk of TB infection in household. Besides, the afraid of the stigma associated with COVID-19 might also promote the refuse to seek medical care among some asymptomatic or mildly symptomatic patients (37, 38). Thus, TB epidemic clustered in family or some communities need be taken into account in the context of the post-pandemic era.
It is important to acknowledge certain limitations of this study. Firstly, the onset time of the research subjects was self-reported by the patients, which existed the possibility of recall bias. Meanwhile, the presence of missing data also had an impact on the results of the study. Additionally, the data utilized in this study was obtained solely from the national TB information management system, without conducting further epidemiological investigations. Some variables like income level and access to healthcare services were hard to acquire, which hindered the comprehensive analysis. It is suggested that longitudinal and qualitative research should be conducted in the future. It is also important to explore the multiple reasons that contribute to delays among adolescents and young adults with PTB and to evaluate the effectiveness of interventions.
Over the past decades, there has been a noteworthy decline in the notification rate of PTB among adolescents and young adults in Jiaxing City while the declining trend was not obvious in patient delay, health system delay, and total delay, respectively. It also found factors such as gender, case-finding method, and the hospital level might influence the times of seeking health care and diagnosis in health agencies. These findings will provide valuable insights for refining preventive and treatment strategies for TB among adolescents and young adults.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Ethics Committee of the Jiaxing Municipal Center for Disease Control and Prevention. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
RG: Funding acquisition, Writing – original draft, Formal analysis, Investigation. GZ: Data curation, Investigation, Writing – original draft. MT: Formal analysis, Investigation, Visualization, Writing – original draft. ZH: Data curation, Investigation, Writing – review & editing. WP: Data curation, Investigation, Writing – review & editing. HF: Investigation, Project administration, Writing – review & editing. KL: Funding acquisition, Project administration, Validation, Writing – review & editing. QX: Data curation, Software, Supervision, Writing – review & editing. ZC: Project administration, Resources, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National-Zhejiang Health Commission Major S&T Project (Grant No. WKJ-ZJ-2118), Zhejiang Provincial Medical and Health Project (2021KY618), and Zhejiang Provincial Program for the cultivation of High level Innovative Health Talents (2021-132).
We would like to extend our sincere acknowledgment and gratitude to the local center for disease control and prevention, the local community health centers, and the TB-designated hospitals for their invaluable contribution to the implementation of TB control efforts.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Furin, J, Cox, H, and Pai, M. Tuberculosis. Lancet. (2019) 393:1642–56. doi: 10.1016/S0140-6736(19)30308-3
2. World Health Organization. Global tuberculosis report. Geneva: World Health Organization (2023). Available at: https://www.who.int/publications/i/item/9789240083851
3. Snow, KJ, Cruz, AT, Seddon, JA, Ferrand, RA, Chiang, SS, Hughes, JA, et al. Adolescent tuberculosis. Lancet Child Adolesc Health. (2020) 4:68–79. doi: 10.1016/S2352-4642(19)30337-2
4. Dong, Z, Wang, QQ, Yu, SC, Huang, F, Liu, JJ, Yao, HY, et al. Age-period-cohort analysis of pulmonary tuberculosis reported incidence, China, 2006-2020. Infect Dis Poverty. (2022) 11:85. doi: 10.1186/s40249-022-01009-4
5. Saunders, MJ, Tovar, MA, Collier, D, Baldwin, MR, Montoya, R, Valencia, TR, et al. Active and passive case-finding in tuberculosis-affected households in Peru: a 10-year prospective cohort study. Lancet Infect Dis. (2019) 19:519–28. doi: 10.1016/S1473-3099(18)30753-9
6. Yuen, CM, Amanullah, F, and Dharmadhikari, A. Turning off the tap: stopping tuberculosis transmission through active case-finding and prompt effective treatment. Lancet. (2015) 386:2334–43. doi: 10.1016/S0140-6736(15)00322-0
7. Getnet, F, Demissie, M, Assefa, N, Mengistie, B, and Worku, A. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: systematic review and meta-analysis. BMC Pulm Med. (2017) 17:202. doi: 10.1186/s12890-017-0551-y
8. Finnie, RK, Khoza, LB, van den Borne, B, Mabunda, T, Abotchie, P, and Mullen, PD. Factors associated with patient and health care system delay in diagnosis and treatment for TB in sub-Saharan African countries with high burdens of TB and HIV. Trop Med Int Health. (2011) 16:394–411. doi: 10.1111/j.1365-3156.2010.02718.x
9. Yasobant, S, Bhavsar, P, Kalpana, P, Memon, F, Trivedi, P, and Saxena, D. Contributing factors in the tuberculosis care Cascade in India: a systematic literature review. Risk Manag Healthc Policy. (2021) 14:3275–86. doi: 10.2147/RMHP.S322143
10. Liu, K, Ai, L, Pan, J, Fei, F, Chen, S, Zhang, Y, et al. Survival analysis and associated factors for pulmonary tuberculosis death: evidence from the information system of tuberculosis disease and mortality surveillance in China. Risk Manage Healthcare Policy. (2022) 15:1167–78. doi: 10.2147/rmhp.s368593
11. National Health Commission of the People’s Republic of China. WS 288-2017: diagnostic criteria for pulmonary tuberculosis. (2017). Available at: http://www.nhc.gov.cn/wjw/s9491/201712/a452586fd21d4018b0ebc00b89c06254.shtml
12. National Health Commission of the People’s Republic of China. WS196-2017: classification of tuberculosis. (2017). Available at: http://www.nhc.gov.cn/wjw/s9491/201712/0d3c52de984b4bc4add047f19ccd51b9.shtml
13. Jiang, H, Liu, M, Zhang, Y, Yin, J, Li, Z, Zhu, C, et al. Changes in incidence and epidemiological characteristics of pulmonary tuberculosis in mainland China, 2005-2016. JAMA Netw Open. (2021) 4:e215302. doi: 10.1001/jamanetworkopen.2021.5302
14. Sreeramareddy, CT, Qin, ZZ, Satyanarayana, S, Subbaraman, R, and Pai, M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis. (2014) 18:255–66. doi: 10.5588/ijtld.13.0585
15. Yimer, S, Bjune, G, and Alene, G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infect Dis. (2005) 5:112. doi: 10.1186/1471-2334-5-112
16. Liu, S, Bi, Y, and Liu, Y. Modeling and dynamic analysis of tuberculosis in mainland China from 1998 to 2017: the effect of DOTS strategy and further control. Theor Biol Med Model. (2020) 17:6. doi: 10.1186/s12976-020-00124-9
17. Zhao, Y, and Liu, J. Facing the challenge of tuberculosis: towards “end TB in China by 2035”. China CDC Wkly. (2021) 3:243–6. doi: 10.46234/ccdcw2021.070
18. Long, Q, Guo, L, Jiang, W, Huan, S, and Tang, S. Ending tuberculosis in China: health system challenges. Lancet Public Health. (2021) 6:e948–53. doi: 10.1016/S2468-2667(21)00203-6
19. Li, T, Du, X, Kang, J, Luo, D, Liu, X, and Zhao, Y. Patient, diagnosis, and treatment delays among tuberculosis patients before and during COVID-19 epidemic-China, 2018-2022. China CDC Wkly. (2023) 5:259–65. doi: 10.46234/ccdcw2023.047
20. Batbayar, B, Kariya, T, Boldoo, T, Purevdorj, E, Dambaa, N, Saw, YM, et al. Patient delay and health system delay of patients with newly diagnosed pulmonary tuberculosis in Mongolia, 2016-2017. Nagoya J Med Sci. (2022) 84:339–51. doi: 10.18999/nagjms.84.2.339
21. Owolabi, OA, Jallow, AO, Jallow, M, Sowe, G, Jallow, R, Genekah, MD, et al. Delay in the diagnosis of pulmonary tuberculosis in the Gambia, West Africa: a cross-sectional study. Int J Infect Dis. (2020) 101:102–6. doi: 10.1016/j.ijid.2020.09.029
22. Saldana, L, Abid, M, McCarthy, N, Hunter, N, Inglis, R, and Anders, K. Factors affecting delay in initiation of treatment of tuberculosis in the Thames Valley. UK Public Health. (2013) 127:171–7. doi: 10.1016/j.puhe.2012.11.010
23. Mesfin, MM, Newell, JN, Madeley, RJ, Mirzoev, TN, Tareke, IG, Kifle, YT, et al. Cost implications of delays to tuberculosis diagnosis among pulmonary tuberculosis patients in Ethiopia. BMC Public Health. (2010) 10:173. doi: 10.1186/1471-2458-10-173
24. Krishnan, L, Akande, T, Shankar, AV, McIntire, KN, Gounder, CR, Gupta, A, et al. Gender-related barriers and delays in accessing tuberculosis diagnostic and treatment services: a systematic review of qualitative studies. Tuberc Res Treat. (2014) 2014:215059. doi: 10.1155/2014/215059
25. Dey, A, Thekkur, P, Ghosh, A, Dasgupta, T, Bandopadhyay, S, Lahiri, A, et al. Active case finding for tuberculosis through TOUCH agents in selected high TB burden wards of Kolkata, India: a mixed methods study on outcomes and implementation challenges. Trop Med Infect Dis. (2019) 4:134. doi: 10.3390/tropicalmed4040134
26. Chen, X, Du, L, Wu, R, Xu, J, Ji, H, Zhang, Y, et al. Tuberculosis-related stigma and its determinants in Dalian, Northeast China: a cross-sectional study. BMC Public Health. (2021) 21:6. doi: 10.1186/s12889-020-10055-2
27. Feng, JY, Huang, SF, Ting, WY, Chen, YC, Lin, YY, Huang, RM, et al. Gender differences in treatment outcomes of tuberculosis patients in Taiwan: a prospective observational study. Clin Microbiol Infect. (2012) 18:E331–7. doi: 10.1111/j.1469-0691
28. Moutinho, S. Tuberculosis is the oldest pandemic, and poverty makes it continue. Nature. (2022) 605:S16–20. doi: 10.1038/d41586-022-01348-0
29. Zão, I, Ribeiro, AI, Apolinário, D, and Duarte, R. Why does it take so long? The reasons behind tuberculosis treatment delay in Portugal. Pulmonology. (2019) 25:215–22. doi: 10.1016/j.pulmoe.2019.02.005
30. Getnet, F, Demissie, M, Worku, A, Gobena, T, Tschopp, R, Girmachew, M, et al. Delay in diagnosis of pulmonary tuberculosis increases the risk of pulmonary cavitation in pastoralist setting of Ethiopia. BMC Pulm Med. (2019) 19:201. doi: 10.1186/s12890-019-0971-y
31. Caminero, JA. Management of multidrug-resistant tuberculosis and patients in retreatment. Eur Respir J. (2005) 25:928–36. doi: 10.1183/09031936.05.00103004
32. Storla, DG, Yimer, S, and Bjune, GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. (2008) 8:15. doi: 10.1186/1471-2458-8-15
33. Xu, J, Wang, Y, Liu, F, and Yang, H. Changes of tuberculosis infection in mainland China before and after the COVID-19 pandemic. J Infect. (2023) 86:154–225. doi: 10.1016/j.jinf.2022.12.008
34. Zhang, G, Yu, Y, Zhang, W, Shang, J, Chen, S, Pang, X, et al. Influence of COVID-19 for delaying the diagnosis and treatment of pulmonary tuberculosis-Tianjin. China Front Public Health. (2022) 10:937844. doi: 10.3389/fpubh.2022.937844
35. Wang, X, He, W, Lei, J, Liu, G, Huang, F, and Zhao, Y. Impact of COVID-19 pandemic on pre-treatment delays, detection, and clinical characteristics of tuberculosis patients in Ningxia Hui autonomous region, China. Front Public Health. (2021) 9:644536. doi: 10.3389/fpubh.2021.644536
36. Visca, D, Ong, CWM, Tiberi, S, Centis, R, D’Ambrosio, L, Chen, B, et al. Tuberculosis and COVID-19 interaction: a review of biological, clinical and public health effects. Pulmonology. (2021) 27:151–65. doi: 10.1016/j.pulmoe.2020.12.012
37. Xia, Y, Huang, F, Chen, H, Wang, N, Du, X, Chen, W, et al. The impact of COVID-19 on tuberculosis patients’ behavior of seeking medical care – China, 2020. China CDC Wkly. (2021) 3:553–6. doi: 10.46234/ccdcw2021.143
Keywords: tuberculosis, delay, patient delay, health system delay, influencing factors, logistic regression
Citation: Ge R, Zhu G, Tian M, Hou Z, Pan W, Feng H, Liu K, Xiao Q and Chen Z (2024) Analysis on time delay of tuberculosis among adolescents and young adults in Eastern China. Front. Public Health. 12:1376404. doi: 10.3389/fpubh.2024.1376404
Received: 25 January 2024; Accepted: 26 March 2024;
Published: 08 April 2024.
Edited by:
Hai-Feng Pan, Anhui Medical University, ChinaReviewed by:
Jizhou Wu, Nanjing Medical University, ChinaCopyright © 2024 Ge, Zhu, Tian, Hou, Pan, Feng, Liu, Xiao and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kui Liu, a2xpdUBjZGMuemouY24=; Qinfeng Xiao, eG8xMzA3QDE2My5jb20=; Zhongwen Chen, Y3p3MjAwN0Bzb2h1LmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.