- 1Beijing Chest Hospital, Capital Medical University, Beijing, China
- 2Beijing Tuberculosis and Thoracic Tumor Research Institute, Clinical Center on Tuberculosis, China CDC, Beijing, China
- 3Department of Epidemiology, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 4Institute of Tuberculosis Prevention and Control, Tongzhou District Center for Disease Prevention and Control, Beijing, China
- 5Beijing Changping Institute for Tuberculosis Prevention and Treatment, Beijing, China
Background: Tuberculosis (TB) remains a significant public health challenge in China. Early detection and diagnosis of TB cases are crucial to interrupt disease transmission and prevent its progression. This study aims to describe the delay in seeking care and diagnosis among patients with pulmonary tuberculosis (PTB) and identify the influencing factors in two counties in Beijing.
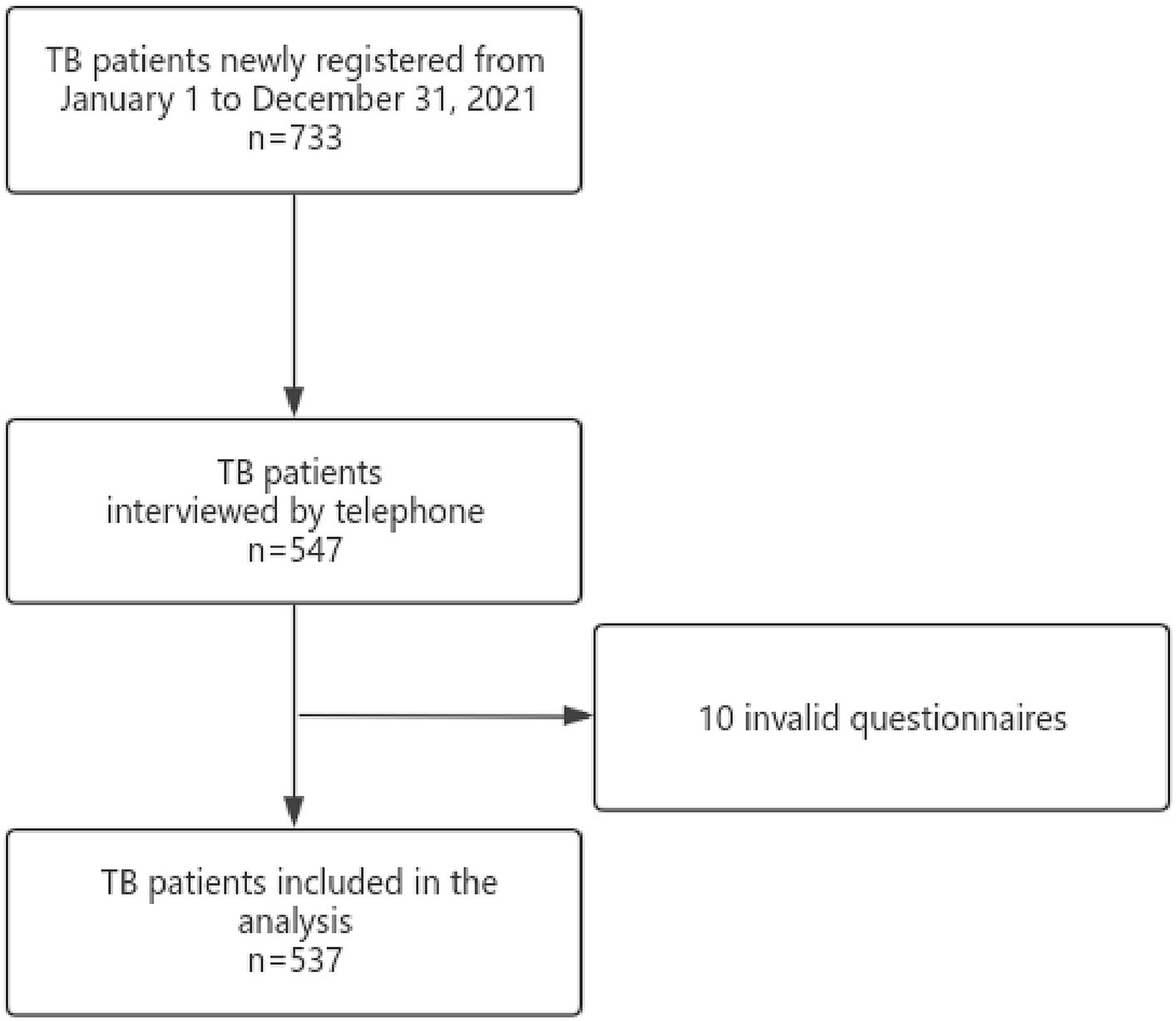
Methods: A retrospective analysis was carried out to investigate care-seeking and diagnosis delay in two counties in Beijing. Basic information of PTB patients from January 1 to December 31, 2021, was extracted from the Tuberculosis Information Management System of China (TBIMS), and all enrolled patients were interviewed via telephone using a standard questionnaire. Statistical description was performed using the median and interquartile range (IQR). Chi-square test and multivariate logistic regression model were used to analyze the influencing factors.
Results: 537 patients were enrolled. The median duration of care-seeking and diagnosis delay was 11 (IQR: 5–26) days and 8 (IQR: 0–18) days, with 41.71 and 35.20% of patients experiencing delays (>14 days). The study found that being asymptomatic (OR = 2.791, 95%CI: 1.710–4.555) before seeking medical care and not attending work during treatment (OR = 2.990, 95%CI: 1.419–6.298) were identified as risk factors for care-seeking delay. Patients who were tracked (OR = 2.632, 95%CI: 1.062–6.521) and diagnosed at tuberculosis control and prevention institutions (OR = 1.843, 95%CI: 1.061–3.202) had higher odds of diagnostic delays. 44.69% of patients presented a total delay (>28 days), with a median duration of 25 (IQR: 13–39) days. A multivariate logistic regression analysis showed that healthy examination (OR = 0.136, 95%CI: 0.043–0.425) was a protective factor for total delay.
Conclusion: Public interventions are necessary to improve the efficiency of PTB patients detection and treatment in Beijing. Medical services should focus on the target population and improve access to medical care to further reduce delays for PTB patients.
1 Introduction
Tuberculosis (TB) is an airborne infectious disease caused by Mycobacterium tuberculosis (M.tb.) (1, 2). It is concerning that TB has reemerged as the primary cause of death among infectious diseases globally, following the decline in mortality rates due to COVID-19 (3). According to global statistics, around a quarter of the world’s population is infected with M.tb. (4). The 2023 Tuberculosis Report by the World Health Organization (WHO) states that the COVID-19 pandemic resulted in 7.5 million new tuberculosis cases globally in 2022, the highest number since the WHO began global TB epidemic surveillance in 1995. China is among the countries with a high burden of TB and drug-resistant TB. Among the 30 countries with a significant TB burden, China ranks third globally in estimated TB cases, accounting for 7.1% of the total TB cases worldwide, following India (27%) and Indonesia (10%) (5).
During the period from symptom onset to treatment initiation, patients with pulmonary tuberculosis (PTB) pose a substantial risk for transmission due to their high infectivity (6, 7). However, inadequate awareness among PTB patients significantly contributes to delays in seeking medical care and diagnosis, thereby greatly amplifying the risk of M.tb. transmission within populations (8). The Fifth TB Epidemiological Sample Survey in China found that over 50% of patients with symptomatic PTB did not promptly seek medical care (9).
Delay in seeking medical help, diagnosis and treatment by healthcare institutions are prevalent among PTB patients in both high and low TB burden regions globally (10–12). In low- and middle-income countries, up to 42% of patients exhibit delayed healthcare-seeking behavior upon experiencing TB-related symptoms (13), with diagnosis delay ranging from 47 to 63% (14–16). Untreated sputum positive patients can infect an average of 10 contacts per year and over 20 contacts throughout the natural course of their disease until death (17). The low detection rate in China suggests that either the healthcare system’s ability to diagnose PTB early falls short of expectations or symptomatic individuals are not actively seeking care.
Delays in seeking care from healthcare facilities and the health system’s inefficiency in identifying TB patients are the main reasons for the high burden of tuberculosis in China (18). This situation also places unnecessary economic burdens on patients’ families. In 2019, around 20% of tuberculosis patients worldwide experienced catastrophic health expenditures, which means that the costs associated with tuberculosis diagnosis and treatment exceeded 20% of the household’s annual income, both directly and indirectly (19). The tuberculosis epidemic is a significant public health issue and a complex socio-economic challenge that has significantly hindered the rapid economic and social progress of developing nations. Therefore, it is crucial to comprehend the characteristics linked to delayed diagnosis among patients with PTB and analyze the factors that affect this delay.
The objective of this study was to investigate the factors of care-seeking delay, diagnostic delay, and total delay among PTB patients in two counties of Beijing in 2021, and to propose corresponding measures for the early detection and effective management of PTB patients.
2 Methods
2.1 Study patients
A retrospective observational cross-sectional analysis was conducted on care-seeking, diagnosis, and total delay of PTB patients, based on existing study. Tuberculosis Information Management System of China (TBIMS) was used to collect all notified PTB cases in Tongzhou and Changping Counties from January 1 to December 31, 2021. Patients with extrapulmonary tuberculosis, impaired hearing, language expression and comprehension, and incorrect registration information were excluded from this study.
2.2 Data collection
Patient demographics, including gender, age (age groups: ≤29, 30–49, 50–69, ≥70 years), occupation, high-risk population, household registration, patient source, sputum examination results, comorbidity, time of symptoms onset, time of visit, and time of diagnosis, were collected based on TBIMS. Symptoms prior to treatment, first contact unit, unit of diagnosis, number of referral hospitals, attendance at work during treatment, and number of people living together were obtained through telephonic interviews by the trained investigators using the designed standard questionnaire (Figure 1). To ensure objectivity, the investigators underwent strict and uniform training to control for bias. If patients were uncertain about their answers, we used corresponding terms to help them recall memories. If their answers were still ambiguous, they would not be included in the study. All questionnaires were coded and double-checked before entering them into the database. Epidata was used to establish the database. Each questionnaire was entered in duplicate by different entry staff, and the double database was checked and corrected to ensure the accuracy and integrity of the questionnaire data entry software.
2.3 Relevant definitions
According to the WHO, care-seeking delay is the time between the onset of symptoms associated with PTB and the patient’s first visit to a healthcare facility. Diagnosis delay is the duration between the patient’s first care-seeking encounter and receiving a definitive diagnosis of PTB. The total duration of both care-seeking delay and diagnosis delay is referred to as total delay (17). Following previous studies, a delay in care-seeking and diagnosis was defined as more than 14 days, while a total delay was defined as more than 28 days (20, 21).
High-risk population: This study defines the high-risk population as individuals who are HIV/AIDS patients, diabetes patients, school and kindergarten personnel, regulatory personnel, breeding personnel, dust exposure personnel/pneumoconiosis patients, residents of nursing homes/welfare homes, close contacts of pathogenic positive tuberculosis patients, medical staff, or people in other crowded places.
Household registration: It refers to whether individual is a local resident of Beijing.
According to the “Guidelines for Tuberculosis prevention and control in China” (22), register the source of tuberculosis infection through transfer, direct visit, healthy examination, referral, and tracking. (1) Transfer: It refers to the individual who went to medical and health institutions (excluding tuberculosis prevention and control institutions) after experiencing suspicious symptoms of TB, and was diagnosed as TB or suspected TB by chest X-ray or sputum examination, and brought the transfer form filled by the doctor to the tuberculosis prevention and control institutions for treatment. (2) Direct visit: It refers to the individual who proactively seek medical treatment at tuberculosis prevention and control institutions after experiencing suspicious symptoms that suggest TB. (3) Referral: It refers to the medical staff or relevant personnel who will find suspicious symptoms of TB and encourage them to go to tuberculosis prevention and control institutions for examination. (4) Tracking: It refers to the disease prevention and control institutions encouraging TB and suspected TB patients who have been reported but have not yet visited designated TB medical institutions for diagnosis and treatment.
Diagnostic results: Laboratory confirmed PTB included sputum smear positive, M.tb. culture positive, and molecular biology positive PTB. Not laboratory confirmed PTB was defined as sputum smear and M.tb. culture negative PTB and tuberculosis without sputum examination (23).
Comorbidities: Patients with diabetes, pneumoconiosis and HIV/AIDS.
2.4 Statistical analysis
Descriptive epidemiological methods were used to analyze the demographic characteristics. Continuous variables were presented as median and interquartile range (IQR), while categorical variables were presented as ratios and proportions. The statistical analysis was conducted using IBM SPSS 25.0 software. The Chi-squared test and multivariate logistic regression model were used to investigate the relationship between relevant influencing factors and delay among PTB patients. A p-value of less than 0.05 was considered statistically significant.
2.5 Ethical considerations
Ethics approval was obtained from the Ethics Committee, Beijing Chest Hospital, Capital Medical University, Beijing, China (2018-30-01 dated 21 August 2018). All study participants provided informed consent.
3 Results
3.1 Study population
A total of 537 patients with PTB were enrolled in this study, of whom 344 (64.1%) were male. The mean age was 40.68 ± 17.23 years. Among them, 168 (31.3%) were workers or farmers, while 334 (62.2%) were non-local. The majority of patients, 388 (72.3%) were transferred from other healthcare facilities. A total of 264 (49.2%) patients were laboratory confirmed PTB. Complications other than TB were observed in 51 (9.5%) patients. Before their visit, 199 (37.1%) patients were asymptomatic. The majority of individuals initially sought medical care at non-specialized TB hospitals, comprising 417 (77.7%), while only 87 (16.2%) patients directly visited TB specialized hospitals. Among the diagnosed institutions, TB specialized hospitals accommodated 226 (42.1%) of all the patients involved in this study. Out of all the patients, only 37 (6.9%) received a direct diagnosis at the initial medical institution. During their care-seeking process, 116 (21.6%) continued to attend work. Additionally, 85 (15.8%) of the patients resided alone, while 203 (37.8%) cohabited with one other individual (Table 1).

Table 1. Characterization of the studied population and univariate analysis of care-seeking, diagnosis and total delay of pulmonary tuberculosis cases (n = 537).
3.2 Influencing factors of care-seeking delay for PTB patients
The median duration for seeking medical care was 11 (IQR: 5–26) days, with 41.71% of patients experiencing a care-seeking delay (>14 days). The results of the univariate analysis showed statistically significant differences in patient source, pre-visit symptoms, first contact unit, and whether patients attended work during treatment (p < 0.05).
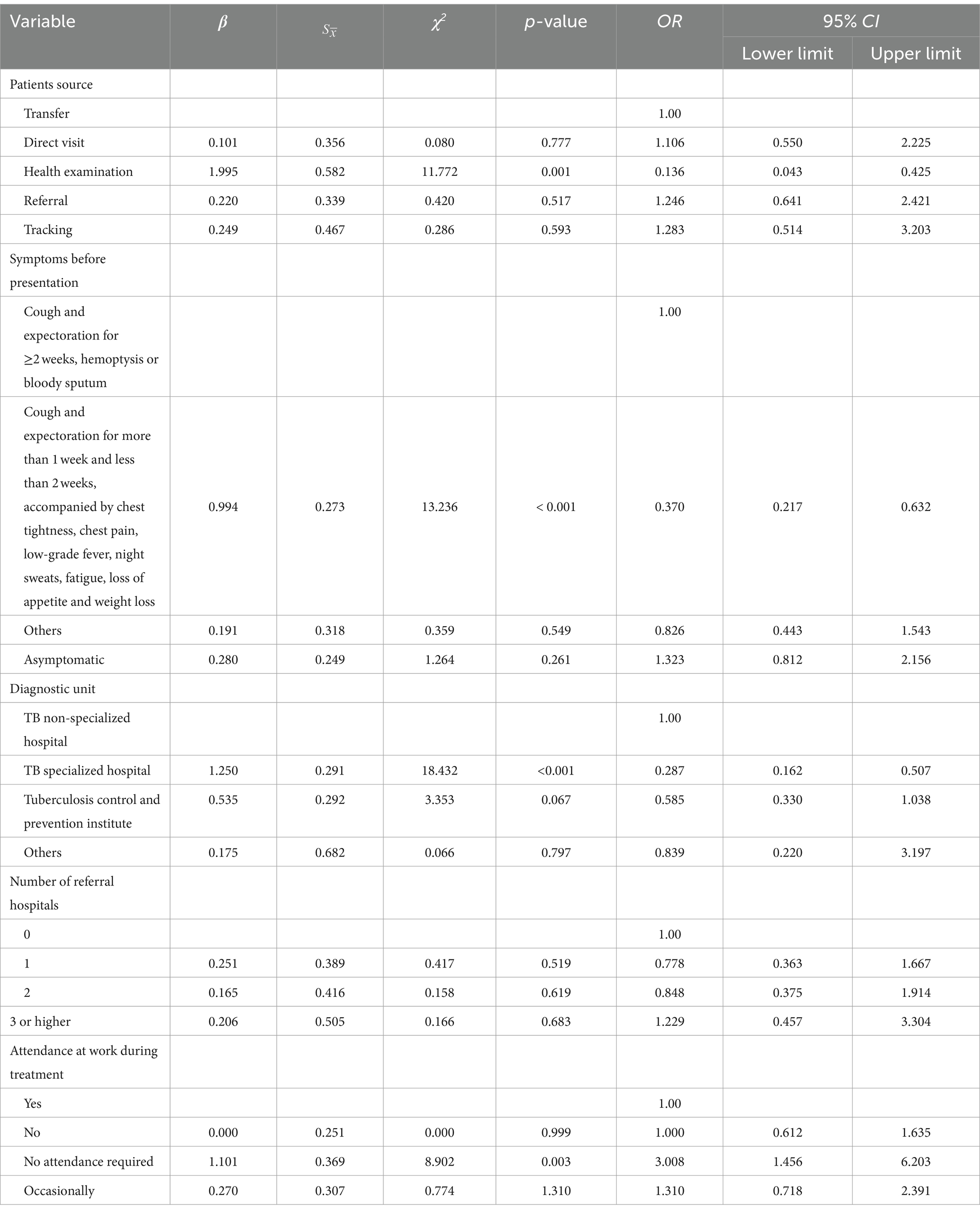
The results of the multivariate analysis results showed that health examination (OR = 0.033, 95%CI: 0.008–0.147), experiencing cough and expectoration for a duration of more than one but less than 2 weeks prior to the visit, as well as presenting with symptoms such as chest tightness, chest pain, low fever, night sweats, fatigue, loss of appetite, and weight loss (OR = 0.378, 95%CI: 0.215–0.665) were identified as protective factors associated with delayed care-seeking behavior. Conversely, the study found that being asymptomatic (OR = 2.791, 95%CI: 1.710–4.555) and not needing to attend work during treatment (OR = 2.990, 95%CI: 1.419–6.298) were identified as risk factors for delaying care-seeking (Table 2).
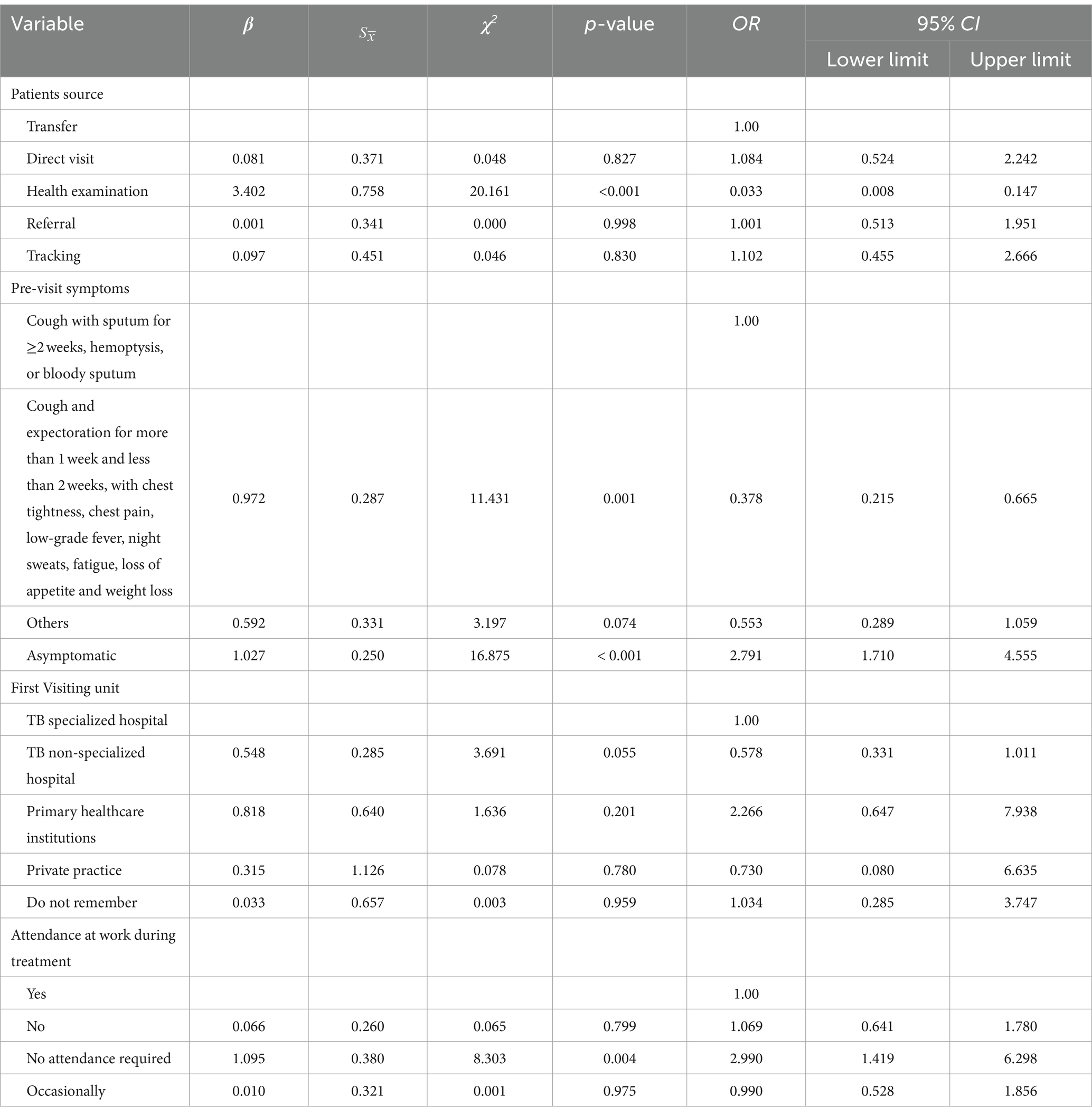
Table 2. Multivariate logistic analysis of care-seeking delay of pulmonary tuberculosis cases (n = 537).
3.3 Influencing factors of diagnosis delay for PTB patients
The median time for diagnosing PTB patients was 8 (IQR: 0–18) days, with 35.20% of patients experiencing a diagnosis delay (>14 days). Univariate analysis results showed statistically significant differences in the delay rate of diagnosis based on household registration, diagnosing hospital unit, number of referral hospitals, and number of cohabiting patients (p < 0.05).
The multivariate analysis results showed that being admitted to a tuberculosis specialized hospital (OR = 0.426, 95%CI: 0.236–0.767) acted as a protective factor against diagnosis delay. Additionally, tracking (OR = 2.632, 95%CI: 1.062–6.521) and receiving the final diagnosis from an institution within the tuberculosis control and prevention institute (OR = 1.843, 95%CI: 1.061–3.202) were identified as risk factors for delayed diagnosis (Table 3).
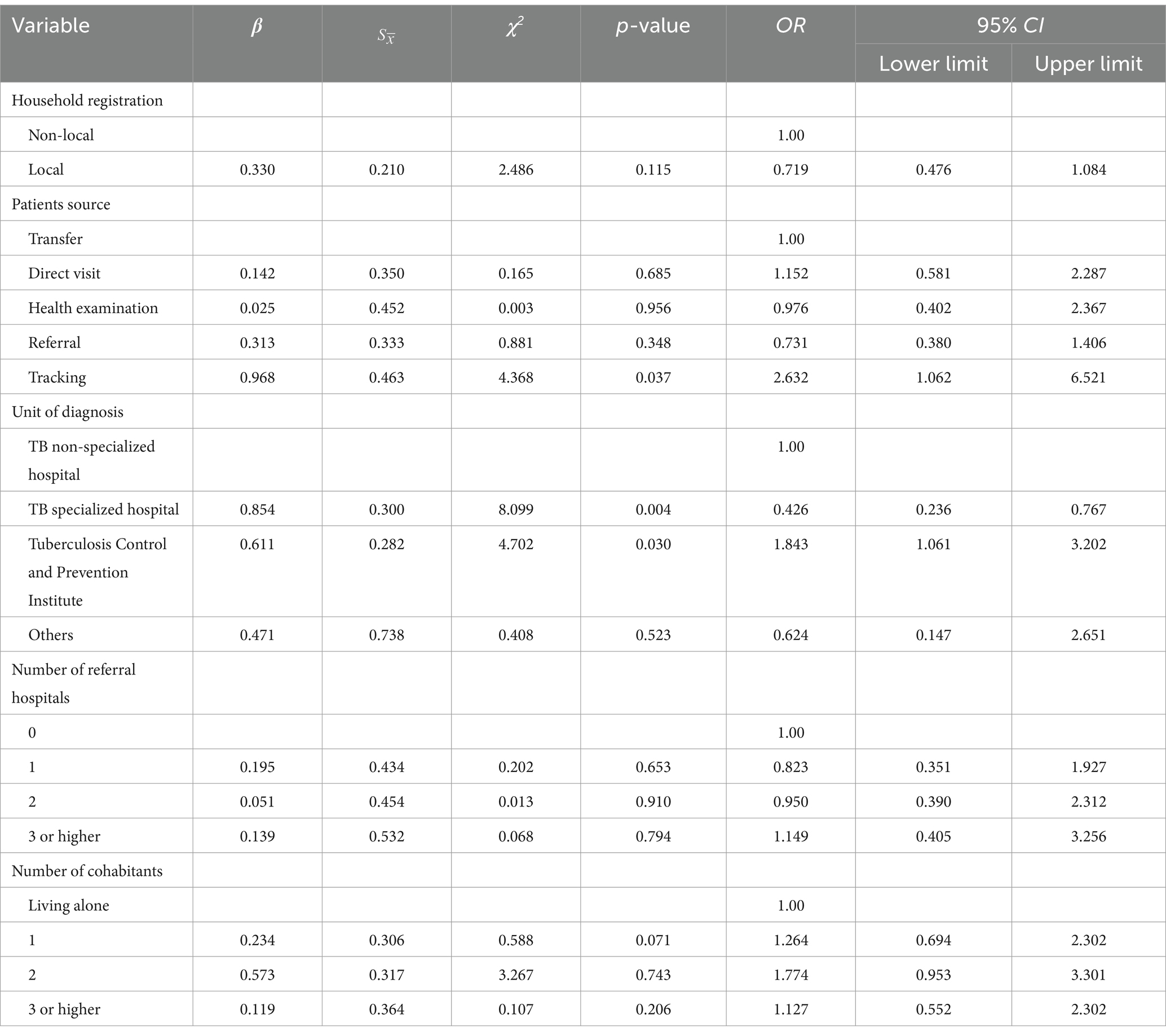
Table 3. Multivariate logistic analysis of diagnostic delay of pulmonary tuberculosis cases (n = 537).
3.4 Influencing factors of total delay for PTB patients
Among 537 patients diagnosed with PTB, the median duration of total delay was 25 days (IQR: 13–39), with 44.69% of patients experiencing a total delay (>28 days). Univariate analysis showed statistically significant differences in delay rates based on patients’ pre-visit symptoms, diagnostic units, number of referral hospitals, and whether they attended work during treatment (p < 0.05).
Multivariate analysis showed that patients who were informed through health examinations (OR = 0.136, 95%CI: 0.043–0.425), experienced cough and expectoration for a duration of more than 1 week but less than 2 weeks prior to hospital visit, and presented with at least one symptom such as chest tightness, chest pain, low fever, night sweats, fatigue, loss of appetite or weight loss (OR = 0.370, 95%CI: 0.217–0.632) had a shorter total delay in seeking medical attention for pulmonary tuberculosis diagnosis. Furthermore, the study found that being diagnosed in a specialized tuberculosis hospital (OR = 0.287, 95%CI: 0.162–0.507) is a protective factor against total delay while not requiring attendance at work during treatment (OR = 3.008; 95%CI: 1.456–6.203) emerged as a risk factor for prolonged delay in seeking medical care (Table 4).
4 Discussion
Based on a global meta-analysis, it was found that the average duration for seeking medical attention among 14 low-income countries with high TB prevalence was 28 days, while it was only 10 days in high-income nations (18). Our study shows that the median duration of seeking care for PTB patients in Tongzhou and Changping Districts of Beijing in 2021 was 11 (IQR: 5–26) days. Compared to international studies, the duration of this data is shorter than that reported in India (25 days) (24) and Portugal (33 days) (25). The median delay in diagnosing PTB patients was 8 (IQR: 0–18) days, which is shorter than the average of 14 (IQR: 4–50) days observed in Switzerland (26) and longer than the average of 4 (IQR: 2–10) days reported in Ethiopia (27). The median time to total delay for PTB patients was 25 (IQR: 13–39) days, which is comparatively shorter than the duration reported in similar surveys and studies conducted both domestically and internationally. For instance, Uzbekistan (28) recorded a median delay of 50 (IQR: 22–92) days, southeast Ethiopia (29) reported a delay of 97 days, while northern Australia (30) observed a delay of 90 (IQR: 60–121) days. The lower reported incidence of PTB in Beijing could be attributed to its higher level of economic development and enhanced accessibility to medical and healthcare services compared to other regions.
As the capital of China, Beijing has one of the lowest TB epidemics in the country and relatively low levels of delay among TB patients. However, our study revealed that 41.7% of patients still experience a delay, and 35.2% of patients encountered a delay in diagnosis. Another study from the Haidian counties of Beijing reported a 54.96% rate of diagnostic delay (31). Our study showed a lower rate of diagnostic delay. This may be related to the timing of our investigation during the COVID-19 pandemic. Screening in health care settings provides an opportunity to find PTB cases and diagnose PTB patients more quickly, as PTB can present with symptoms similar to COVID-19 (32). Additionally, physical examinations such as CT scans are more frequent when screening for COVID-19 in fever clinics, which also aids in detecting PTB cases (33).
The analysis and research findings indicated that passive case finding (PCF), such as transfer, referral, and tracking, are associated with a higher likelihood of delayed diagnosis and medical treatment. These results align with studies conducted in countries with high tuberculosis incidence rates (34, 35). Relevant study has reported that active case finding (ACF) is more effective than PCF in promptly identifying individuals with TB (36). Both the guidelines provided by WHO (37) and China’s tuberculosis prevention and control program (23) emphasize the importance of optimizing the strategy for controlling the source of infection. They suggest added and strengthening new interventions as well as enhancing the screening of high-risk populations and ACF. The investigation findings on factors influencing care-seeking delay and total delay indicate that symptoms such as cough and expectoration lasting for more than 1 week but less than 2 weeks, chest tightness, chest pain, low fever, night sweats, fatigue, loss of appetite, and weight loss were identified as protective factors. These results are consistent with previous studies conducted in Cambodia (38) and Kenya (39). The presence of severe symptoms, such as chest pain, fever, and weight loss, may prompt patients to seek medical treatment (40). Our study also found that being asymptomatic was identified as a risk factor contributing to the delay in seeking medical care. Therefore, it is significant to carry out ACF in high-risk groups for PTB, such as specific populations in high-risk areas of the epidemic. Compared to patients who continued working during their treatment, those who did not need to work were more likely to experience delayed medical treatment and diagnosis. The majority of these individuals were either retired or unemployed, which may have contributed to their reduced inclination to seek medical assistance and limited access to adequate healthcare coverage.
The multivariate analysis results showed that TB specialist hospitals had a lower likelihood of delayed diagnosis. This is because medical personnel and screening technologies in TB specialized hospitals tend to be more vigilant and have a faster ability to identify tuberculosis. In contrast to general medical institutions, they consider whether a patient has tuberculosis after excluding other diseases. Specialized hospitals have higher diagnostic efficiency compared to general health institutions, which often lack the corresponding rapid screening technology. Our study found that the final diagnosis made in tuberculosis control and prevention institutions was a risk factor for diagnosis delay. This may be due to the diagnosis technology of M.tb used in these institutions. Certain tuberculosis control and prevention institutions reportedly still rely on conventional laboratory methods such as sputum smear and culture. GeneXpert is a rapid diagnostic method recommended by WHO. Compared to conventional methods for pathogen detection, GeneXpert offers the advantages of rapid detection speed and high accuracy (positive results can be detected when the number of M.tb is >130/mL) (41). According to a report, the use of GeneXpert reduced diagnostic delay by 1.79 days (95% CI: 0.27–3.85) and treatment initiation delay by 2.55 days (95% CI: 0.54–4.56) compared to sputum microscopy (42). Currently, GeneXpert technology is only available in certain designated tuberculosis hospitals in China. However, most patients initially seek diagnosis at TB non-specialized hospitals or primary healthcare institutions. Therefore, the implementation of molecular biology detection technology will not only improve the efficiency of identifying PTB patients but also reduce the time required for diagnosis.
Our study has several limitations. Firstly, it was conducted only in two counties of Beijing, which may limit its generalizability to the entire city. Secondly, although we have included most of the data in the system, there are still some variables missing. Additionally, there may be recall bias among certain patients, which could lead to potential differences in their responses to specific questions. These limitations require further comprehensive investigation for future research to address these gaps.
5 Conclusion
In summary, PTB patients in Tongzhou and Changping Districts of Beijing are expected to experience relatively low delays in 2021. However, a significant proportion of patients may still face delayed treatment and diagnosis. Therefore, it is crucial to implement effective measures to improve the diagnostic efficiency of tuberculosis, treat patients as early as possible, and reduce patient suffering and economic losses.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee, Beijing Chest Hospital, Capital Medical University, Beijing, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
LZ: Writing – original draft, Visualization, Methodology, Writing – review & editing, Supervision, Project administration, Conceptualization. XM: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Conceptualization. HG: Writing – review & editing, Resources, Data curation. CB: Writing – review & editing, Resources, Data curation. YW: Writing – review & editing, Resources, Data curation. SW: Writing – review & editing, Investigation, Data curation. ML: Writing – review & editing, Investigation, Data curation. YL: Writing – original draft, Writing – review & editing, Visualization, Validation, Supervision, Software, Project administration, Methodology, Funding acquisition, Conceptualization. LL: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Funding acquisition, Conceptualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Thanks to the Key Techniques of Integrated Prevention and Control of Tuberculosis, Beijing, China, and Health Commission high-level public health technical personnel project, Beijing, China, for financial support to conduct this study.
Acknowledgments
Thanks to the TB patients and their physicians for participating in the study. And also thanks to data collectors and supervisors for their commitment.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ACF, Active case finding; MTB, Mycobacterium tuberculosis; PCF, Passive case finding; PTB, Pulmonary tuberculosis; WHO, The World Health Organization; TB, Tuberculosis.
References
1. Safdar, A. Principles and practice of transplant infectious diseases. New York: Springer (2019). p. 491–502.
2. World Health Organization. Global tuberculosis report 2018. Geneva: World Health Organization (2018).
3. Millington, KA, White, RG, Lipman, M, McQuaid, CF, Hauser, J, Wooding, V, et al. The 2023 UN high-level meeting on tuberculosis: renewing hope, momentum, and commitment to end tuberculosis. Lancet Respir Med. (2024) 12:10–3. doi: 10.1016/S2213-2600(23)00409-5
4. World Health Organization. Global tuberculosis report 2019. Geneva: World Health Organization (2019).
5. World Health Organization. Global tuberculosis report 2023. Geneva: World Health Organization (2023).
6. Peri, AM, Bernasconi, DP, Galizzi, N, Matteelli, A, Codecasa, L, Giorgio, V, et al. Determinants of patient and health care services delays for tuberculosis diagnosis in Italy: a cross-sectional observational study. BMC Infect Dis. (2018) 18:690. doi: 10.1186/s12879-018-3609-4
7. Teo, AKJ, Singh, SR, Prem, K, Hsu, LY, and Yi, S. Delayed diagnosis and treatment of pulmonary tuberculosis in high-burden countries: a systematic review protocol. BMJ Open. (2019) 9:e029807. doi: 10.1136/bmjopen-2019-029807
8. Marks, GB, Nguyen, NV, Nguyen, PTB, Nguyen, TA, Nguyen, HB, Tran, KH, et al. Community-wide screening for tuberculosis in a high-prevalence setting. N Engl J Med. (2019) 381:1347–57. doi: 10.1056/NEJMoa1902129
9. Disease Control Bureau of the Ministry of Health, Chinese Center for Disease Control and Prevention. Report on the 5th national tuberculosis epidemiological survey in China-2010. Beijing, China: Military Medical Science Press (2011).
10. Moyo, N, Tay, EL, Trauer, JM, Burke, L, Jackson, J, Commons, RJ, et al. Tuberculosis notifications in regional Victoria, Australia: implications for public health care in a low incidence setting. PLoS One. (2023) 18:e0282884. doi: 10.1371/journal.pone.0282884
11. Supehia, S, Singh, M, Bahurupi, Y, Aggarwal, P, Chandra, R, and Sharma, N. The extent of delay in diagnosis, treatment and their associated factors among tuberculosis patients attending government hospitals of Rishikesh, Uttarakhand: a cross-sectional study. Recent Adv Antiinfect Drug Discov. (2024) 19:137–47. doi: 10.2174/2772434418666230517151828
12. Alema, HB, Hailemariam, SA, Misgina, KH, Weldu, MG, Gebregergis, YS, Mekonen, GK, et al. Health care seeking delay among pulmonary tuberculosis patients in north west zone of Tigrai region, North Ethiopia. BMC Infect Dis. (2019) 19:309. doi: 10.1186/s12879-019-3893-7
13. Getnet, F, Demissie, M, Assefa, N, Mengistie, B, and Worku, A. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: systematic review and meta-analysis. BMC Pulm Med. (2017) 17:202. doi: 10.1186/s12890-017-0551-y
14. Makwakwa, L, Sheu, ML, Chiang, CY, Lin, SL, and Chang, PW. Patient and heath system delays in the diagnosis and treatment of new and retreatment pulmonary tuberculosis cases in Malawi. BMC Infect Dis. (2014) 14:132. doi: 10.1186/1471-2334-14-132
15. Bojovic, O, Medenica, M, Zivkovic, D, Rakocevic, B, Trajkovic, G, Kisic-Tepavcevic, D, et al. Factors associated with patient and health system delays in diagnosis and treatment of tuberculosis in Montenegro, 2015-2016. PLoS One. (2018) 13:e0193997. doi: 10.1371/journal.pone.0193997
16. Wako, WG, Wasie, A, Wayessa, Z, and Fikrie, A. Determinants of health system diagnostic delay of pulmonary tuberculosis in Gurage and Siltie zones, South Ethiopia: a cross-sectional study. BMJ Open. (2021) 11:e047986. doi: 10.1136/bmjopen-2020-047986
17. World Health Organization. Diagnostic and treatment delay in tuberculosis. (2006). Available at: https://iris.who.int/handle/10665/116501 (Accessed March 15, 2024).
18. Teo, AKJ, Singh, SR, Prem, K, Hsu, LY, and Yi, S. Duration and determinants of delayed tuberculosis diagnosis and treatment in high-burden countries: a mixed-methods systematic review and meta-analysis. Respir Res. (2021) 22:251. doi: 10.1186/s12931-021-01841-6
19. World Health Organization. Global tuberculosis report 2022. Geneva: World Health Organization (2022).
20. Sun, R, Wu, Z, Zhang, H, Huang, J, Liu, Y, Chen, M, et al. Assessing heterogeneity of patient and health system delay among TB in a population with internal migrants in China. Front Public Health. (2024) 12:1354515. doi: 10.3389/fpubh.2024.1354515
21. Liu, K, Ge, R, Luo, D, Zheng, Y, Shen, Z, Chen, B, et al. Delay analysis of pulmonary tuberculosis in the eastern coastal county of China from 2010 to 2021: evidence from two surveillance systems. Front Public Health. (2023) 11:1233637. doi: 10.3389/fpubh.2023.1233637
22. Xia, Y, Chen, H, Zhang, C, Zhao, Y, Cheng, J, and Zhang, H. Guidelines for the prevention and control of tuberculosis in schools: Recommendations from China CDC. China CDC Wkly. (2021) 3:34–8. doi: 10.46234/ccdcw2021.009
23. People’s Republic of China state health and Family Planning Commission. Diagnostic criteria for tuberculosis (WS 288—2017). Electr J Emerg Infect Dis. (2018) 3:59–61. doi: 10.19871/j.cnki.xfcrbzz.2018.01.017
24. Balasubramnian, A, Francis, PT, Leelamoni, K, Rakesh, PS, and Lalu, JS. Diagnostic and treatment delay among new pulmonary tuberculosis patients in Southern India: a cross-sectional study. Indian J Public Health. (2022) 66:S60–s5. doi: 10.4103/ijph.ijph_1079_22
25. Zão, I, Ribeiro, AI, Apolinário, D, and Duarte, R. Why does it take so long? The reasons behind tuberculosis treatment delay in Portugal. Pulmonology. (2019) 25:215–22. doi: 10.1016/j.pulmoe.2019.02.005
26. Auer, C, Kiefer, S, Zuske, M, Schindler, C, Wyss, K, Blum, J, et al. Health-seeking behaviour and treatment delay in patients with pulmonary tuberculosis in Switzerland: some slip through the net. Swiss Med Wkly. (2018) 148:w14659. doi: 10.4414/smw.2018.14659
27. Datiko, DG, Jerene, D, and Suarez, P. Patient and health system delay among TB patients in Ethiopia: Nationwide mixed method cross-sectional study. BMC Public Health. (2020) 20:1126. doi: 10.1186/s12889-020-08967-0
28. Belkina, TV, Khojiev, DS, Tillyashaykhov, MN, Tigay, ZN, Kudenov, MU, Tebbens, JD, et al. Delay in the diagnosis and treatment of pulmonary tuberculosis in Uzbekistan: a cross-sectional study. BMC Infect Dis. (2014) 14:624. doi: 10.1186/s12879-014-0624-y
29. Hussen, A, Biadgilign, S, Tessema, F, Mohammed, S, Deribe, K, and Deribew, A. Treatment delay among pulmonary tuberculosis patients in pastoralist communities in bale zone, Southeast Ethiopia. BMC Res Notes. (2012) 5:320. doi: 10.1186/1756-0500-5-320
30. Vigneswaran, N, Parnis, R, Lowbridge, C, Townsend, D, and Ralph, AP. Factors leading to diagnostic delay in tuberculosis in the tropical north of Australia. Intern Med J. (2023). doi: 10.1111/imj.16223
31. Wu, F, Lai, C, Wang, Y, Zhang, G, Li, Y, Yu, S, et al. Tuberculosis infection and epidemiological characteristics in Haidian District, Beijing, 2005-2018. BMC Public Health. (2020) 20:823. doi: 10.1186/s12889-020-08773-8
32. Zumla, A, Marais, BJ, McHugh, TD, Maeurer, M, Zumla, A, Kapata, N, et al. COVID-19 and tuberculosis-threats and opportunities. Int J Tuberc Lung Dis. (2020) 24:757–60. doi: 10.5588/ijtld.20.0387
33. Zhang, G, Yu, Y, Zhang, W, Shang, J, Chen, S, Pang, X, et al. Influence of COVID-19 for delaying the diagnosis and treatment of pulmonary tuberculosis-Tianjin, China. Front Public Health. (2022) 10:937844. doi: 10.3389/fpubh.2022.937844
34. Harries, AD, Lin, Y, Kumar, AMV, Satyanarayana, S, Takarinda, KC, Dlodlo, RA, et al. What can national TB control programmes in low- and middle-income countries do to end tuberculosis by 2030? F1000Res. (2018) 7:1011. doi: 10.12688/f1000research.14821.1
35. Mbuthia, GW, Olungah, CO, and Ondicho, TG. Health-seeking pathway and factors leading to delays in tuberculosis diagnosis in West Pokot County, Kenya: a grounded theory study. PLoS One. (2018) 13:e0207995. doi: 10.1371/journal.pone.0207995
36. Mhimbira, FA, Cuevas, LE, Dacombe, R, Mkopi, A, and Sinclair, D. Interventions to increase tuberculosis case detection at primary healthcare or community-level services. Cochrane Database Syst Rev. (2017) 11:Cd011432. doi: 10.1002/14651858.CD011432.pub2
37. World Health Organization. WHO operational handbook on tuberculosis. Module 2: screening – systematic screening for tuberculosis disease. Geneva: World Health Organization (2021).
38. Butsorn, A, Suggaravetsiri, P, and Tesana, N. Delay of treatment among new smear-positive pulmonary tuberculosis patients in Thai-Cambodia border: cases study in Surin and Sisaket Province, Thailand. Res J Med Sci. (2010) 4:340–5. doi: 10.3923/rjmsci.2010.340.345
39. Kunjok, DM, Mwangi, JG, Mambo, S, and Wanyoike, S. Assessment of delayed tuberculosis diagnosis preceding diagnostic confirmation among tuberculosis patients attending Isiolo County level four hospital, Kenya. Pan Afr Med J. (2021) 38:51. doi: 10.11604/pamj.2021.38.51.21508
40. Sabawoon, W, Sato, H, and Kobayashi, Y. Delay in the treatment of pulmonary tuberculosis: a report from Afghanistan. Environ Health Prev Med. (2012) 17:53–61. doi: 10.1007/s12199-011-0219-9
41. Zhang, Q, Zhang, Q, Sun, BQ, Liu, C, Su, AN, Wang, XH, et al. GeneXpert MTB/RIF for rapid diagnosis and rifampin resistance detection of endobronchial tuberculosis. Respirology. (2018) 23:950–5. doi: 10.1111/resp.13316
Keywords: pulmonary tuberculosis, delay, diagnosis, influencing factors, logistic regression
Citation: Zhang L, Ma X, Gao H, Bao C, Wu Y, Wu S, Liu M, Liu Y and Li L (2024) Analysis of care-seeking and diagnosis delay among pulmonary tuberculosis patients in Beijing, China. Front. Public Health. 12:1369541. doi: 10.3389/fpubh.2024.1369541
Edited by:
Mathieu Nacher, INSERM CIC1424 Centre d'Investigation Clinique Antilles Guyane, French GuianaReviewed by:
João Almeida Santos, National Health Institute Doutor Ricardo Jorge (INSA), PortugalMathilde Boutrou, Centre Hospitalier de Cayenne, French Guiana
Copyright © 2024 Zhang, Ma, Gao, Bao, Wu, Wu, Liu, Liu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liang Li, bGlsaWFuZzY5QHZpcC5zaW5hLmNvbQ==; Yuhong Liu, bGl1eXVob25nMDUxNkAxMjYuY29t
†These authors share first authorship
‡These authors share last authorship
 Lijie Zhang
Lijie Zhang Xiaoge Ma
Xiaoge Ma Hanqing Gao4
Hanqing Gao4 Liang Li
Liang Li