- 1School of Nursing, Wenzhou Medical University, Zhejiang, China
- 2Department of Neurology, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Zhejiang, China
Background: Affiliate stigma experienced by family caregivers of individuals with dementia may seriously affect home care and prognosis of these patients. This study aimed to explore the levels of perceived affiliate stigma and its influencing factors among family caregivers of patients with dementia in mainland China, which remains a relatively unexplored topic.
Methods: In this cross-sectional study, purposive sampling was used to recruit dementia family caregivers from an online communication group between April and May 2022. A total of 727 eligible caregivers were included and asked to complete the demographic questionnaire, the affiliate stigma scale, and the caregiver burden inventory. Descriptive statistics, independent sample t-test, one-way analysis of variance, Pearson correlation analysis, and multiple linear regression were used to explore the factors that influence perceived affiliate stigma among dementia family caregivers.
Results: The mean score for affiliate stigma of dementia family caregivers was 48.09 ± 16.38 (range: 22–86). Whether there were regular breaks during patient care, time-dependent burden, developmental burden, physical burden, and social burden were significant factors influencing the affiliate stigma of dementia family caregivers.
Conclusion: Dementia family caregivers showed a moderate to high level of affiliate stigma. Those who had regular breaks during patient care, higher time-dependent burden, developmental burden, and physical burden and lower social burden exhibited higher levels of affiliate stigma.
1 Introduction
Dementia is a highly prevalent disease in people older than 65 years and has been diagnosed in increasingly younger individuals in recent years (1–3). There are currently approximately 600,000 people with dementia in China, which means that 7 out of every 100 people older than 65 years have dementia (4). As dementia progresses, patients gradually lose the ability to perform daily activities and require the assistance of healthcare professionals and caregivers. Thus, dementia is recognized as a huge social and healthcare challenge in China (5). With the advancement of the universal medical insurance system in China, the financial burden of treatment and care faced by patients with dementia has eased (5). However, the medical insurance coverage for long-term care is limited, and most families in China cannot afford expensive commercial care services. As a result, patients with dementia still rely heavily on informal home care (5). It is estimated that 75% of patients with dementia are predominantly cared for by family caregivers (6, 7). Owing to the lack of well-developed family support services in China (5), most family caregivers have limited knowledge and skills in caring for patients with dementia (5, 8). As a result, family caregivers suffer from increased negative emotions when caring for patients with dementia who exhibit symptoms of delusions, hallucinations, and aggressive behaviors (9–11). Specifically, a meta-analysis reported a high prevalence of depression (34.0%) and anxiety (43.6%) among dementia family caregivers (12), and they were particularly vulnerable to affiliate stigma (11, 13–15).
Affiliate stigma is defined as the process by which the stigmatized individual internalizes the negative reactions of others to him or her (16). Affiliate stigma has a further negative impact on family caregivers’ physical and mental health (17). In addition, affiliate stigma increases social withdrawal in dementia family caregivers and is an important cause of negative emotions (11, 15). Specifically, family caregivers with affiliate stigma experience high level of stress, high caregiver burden, and engage less in help-seeking behaviors, which, in turn, affects the quality of care they provide to patients with dementia (18–20). Moreover, researchers conducting in-depth interviews with child caregivers found that they experienced feelings of shame and disgust due to the caring activity while feeling guilt and self-blame for their shame and disgust toward their parents (19). These perceptions contribute to a growing sense of stigma among dementia family caregivers, which must be urgently alleviated (19). Although the mental health needs of dementia family caregivers are gaining widespread attention, research examining affiliate stigma in this context is still in its infancy. Understanding the levels of affiliate stigma among dementia family caregivers and the influencing factors involved is necessary for healthcare professionals to develop effective strategies to reduce affiliate stigma in this group. To address this gap, two research questions were proposed: (1) What is the level of affiliate stigma among dementia family caregivers in China? (2) What are the factors that influence affiliate stigma among dementia family caregivers in China?
2 Background
2.1 Levels of affiliate stigma of dementia family caregivers
Affiliate stigma has been reported to occur among dementia family caregivers in many regions, such as Iran, China, Vietnam, Singapore, Ethiopia, the United Kingdom, Belgium, Taiwan, Israel, America, Hong Kong, Malaysia, South Korea, Brazil, Nigeria, Indonesia, and Ghana (16, 21–36). Although the specific rates of incidence have rarely been reported, some studies have indicated the high incidence of affiliate stigma among dementia family caregivers. According to a study from Israel, 50% of a sample of dementia family caregivers experienced affiliate stigma as a result of caring for a relative with dementia-like conditions (28). Furthermore, a qualitative study reported that 91% of Asian-American dementia family caregivers mentioned about stigma (21). In addition, stigmatization of primary caregivers for individuals with mental illness was reported to be 94 and 75% in studies from Singapore (22) and Ethiopia (23), respectively. Moderate to high levels of affiliate stigma have been reported among dementia family caregivers in mainland China (27), while the affiliate stigma levels of dementia family caregivers in Iran are found to be even higher (16). However, dementia family caregivers’ affiliate stigma levels were lower in Taiwan, United Kingdom, and Belgium (24–26).
2.2 Influencing factors of dementia family caregivers’ affiliate stigma
Levels of affiliate stigma among dementia family caregivers were found to be influenced by demographic characteristics (such as caregivers’ gender, age, place of residence, relationship with patient, and patients’ gender) and psychological characteristics (such as anxiety and depression). Specifically, female caregivers experienced more affiliate stigma than male caregivers (37), although another study reported the opposite result (14). Younger caregiver age was associated with higher affiliate stigma (38). Caregivers living in rural areas showed higher scores for affiliate stigma than caregivers living in urban areas (39). Children caregivers experienced higher affiliate stigma than spouse caregivers (37). In addition, male patients with dementia are more aggressive and disruptive, exacerbating the stigma perceived by female spouse caregivers (40). In addition to these demographic variables, anxiety was significantly associated with affiliate stigma (14), while depression predicted affiliate stigma either directly (13) or indirectly through caregiver burden (41). Furthermore, a qualitative study of dementia family caregivers in the Asian-American population found that stigma is strongly associated with negative stereotypes of older adult care and progression of chronic disease (21).
Current research on the factors influencing dementia family caregivers’ affiliate stigma has mainly focused on demographic variables, and few psychological factors have been explored. In this study, the dimensions of caregiver burden were additionally considered as main variables that may influence dementia family caregivers’ affiliate stigma. Caregiver burden refers to caregivers’ multifaceted stress levels arising from caring for a relative and includes time-dependent burden, developmental burden, physical burden, social burden, and emotional burden (3, 42). Caregivers with the same total burden score may experience different patterns of burden and therefore require differing interventions (43). In addition, different burden dimensions may have varying degrees of influence on affiliate stigma. Therefore, we attempted to explore the impact of caregiver burden on affiliate stigma from the perspective of the various dimensions of this burden. Caregiver burden was confirmed to be positively related to affiliate stigma, and both variables were positively correlated with all dimensions (13, 14, 37). Specifically, caregivers with higher caregiver burden experienced higher affiliate stigma and were unable to provide high-quality care (14). Furthermore, highly burdened caregivers may experience more public stigma, which may lead to high levels of affiliate stigma (44). Furthermore, another study (26) suggested that dementia caregivers caring for a family member with disruptive behavior may experience embarrassment and shame. This could be regarded as emotional burden, which was also associated with affiliate stigma. Although the relationship between caregiver burden and affiliate stigma has been addressed by some researchers, few studies focus on its impact on affiliate stigma from the perspective of the dimensions of caregiver burden.
In summary, current research on affiliate stigma levels is limited. In addition, extant studies report inconsistent findings in regard to the factors that influence affiliate stigma. Furthermore, perceived affiliate stigma levels and their influencing factors among dementia family caregivers in mainland China remain a relatively unexplored topic, especially from the perspective of burden dimensions. Hence, the purpose of this study was to explore the levels of affiliate stigma and its influencing factors from the perspective of burden dimensions among dementia family caregivers in mainland China.
3 Methods
3.1 Study design
This was a cross-sectional study conducted to examine the level of affiliate stigma and its influencing factors among dementia family caregivers in mainland China.
3.2 Setting and sample
Purposive sampling was used to recruit dementia family caregivers from April to May 2022. In purposive sampling, the characteristics of the sample are defined for a purpose that is relevant to the study. The rationale of using purposive sampling is as follows (45): First, purposive sampling avoids random forms of sampling and ensures that the specific types of cases included are part of the final sample for the study. Second, purposive sampling enhances transferability by identifying study participants in terms of inclusion and exclusion criteria, which helps determine the applicability of study findings to other situations and populations. In this study, specific inclusion and exclusion criteria were defined to recruit dementia family caregivers from an online communication group. All members in the online communication group were dementia family caregivers from mainland China who were eligible to represent the target population. For inclusion in this study, caregivers were required to meet the following criteria: (1) primary caregivers of the dementia patient; (2) aged 20 years or older; (3) able to understand the purpose of the study and the content of the study questionnaires; (4) only cared for the dementia patient, and (5) cared for the dementia patient for more than 3 months. The exclusion criterion was receipt of money from caregiving activities. The sample size was determined by combining the following two methods: (1) Power analysis was conducted using G*Power 3.1.9.2 software (46, 47), with an effect size of 0.15, a significance level of 0.05, and a power of 0.80. The sample was calculated to be 117 cases after setting a sample loss rate of 20%. (2) Rough sample size estimation method was adopted, which required the sample size to be 10 to 20 times of the number of study variables (48). In total, 32 variables were included in this study, and the sample size was calculated to be at least 320 to 640 cases. Taking into account invalid questionnaires, the sample size was further expanded by 20% as 384 to 768 cases. In summary, to obtain more robust statistical results, we attempted to collect as much data as possible and set the sample size to at least 384 cases. Finally, 1,024 questionnaires were collected, out of which 727 questionnaires were valid. The effective response rate was 71.0%.
3.3 Measures
3.3.1 The demographic questionnaire
The demographic questionnaire was designed by the researchers based on a literature review (22, 37, 49–51), to collect information on the dementia family caregivers’ gender, age, ethnic group, religious beliefs, educational level, marital status, employment status, whether regular breaks were taken during patient care, monthly household income, relationship with the patient, whether the carer lived with the patient, whether the carer received assistance in caring for the patient, average time spent caring for the patient per day, and knowledge of dementia. In addition, questions regarding the patients’ gender, age, ethnic groups, religious beliefs, marital status, type of medical insurance, course of disease, and self-care ability were included in the demographic questionnaire.
3.3.2 Affiliate stigma scale
The affiliate stigma scale, which was developed to assess affiliate stigma levels of dementia caregivers by Mak and Cheung (52) in Cantonese, comprises 22 items with three dimensions, namely, affective, behavioral, and cognitive. All items are rated on a four-point Likert scale ranging from 1 (not at all) to 4 (always). The total score ranged from 22 to 88, with higher scores indicating higher levels of affiliate stigma. The affiliate stigma scale was reliable, as evidenced by Cronbach’s α of 0.94 (52). The Cantonese version of the affiliate stigma scale was converted into the Mandarin version by the research team, without any modification, as requested by the original author. The Mandarin version was used in this study. In this study, Cronbach’s α of total affiliate stigma scale was 0.970, and Cronbach’s α for the dimensions of affective, behavioral, and cognitive dimensions were 0.901, 0.927, and 0.927, respectively.
3.3.3 Caregiver burden inventory
The caregiver burden inventory, which was developed by Novak and Guest (43) and was translated into Chinese by Yue (53), was used to assess dementia family caregivers’ burden. The caregiver burden inventory consists of 24 items with five dimensions, namely, emotional burden, social burden, time-dependent burden, developmental burden, and physical burden. All items are rated on a five-point Likert scale ranging from 0 (not at all) to 4 (always). The total score ranges from 0 to 96, with higher scores indicating higher levels of caregiver burden. Cronbach’s α of total caregiver burden inventory was 0.92, and the range of each dimension was 0.68 to 0.93 (time-dependent burden = 0.93, developmental burden = 0.83, physical burden = 0.83; social burden = 0.68; and emotional burden = 0.78) (53). In this study, Cronbach’s α of total caregiver burden inventory was 0.958, and the range of each dimension was 0.852 to 0.890 (time-dependent burden = 0.890, developmental burden = 0.879, physical burden = 0.852, social burden = 0.849, and emotional burden = 0.889).
3.4 Data collection
Data were collected using online electronic questionnaires, with the consent of the administrator of a dementia family caregiver online communication group. The questionnaires were entered into China’s largest online survey platform to generate a quick response code for distributing the questionnaires. Then, the quick response code was sent to the dementia family caregiver online communication group. Potential participants scanned the quick response code with their mobile phones and responded to the questionnaires online. To ensure that all questions were answered, the online survey rules were set to refuse the submission of a survey if any questions had not been answered. Questionnaires could be submitted from a single internet protocol address only once.
3.5 Data analysis
SPSS 26.0 was used to analyze the data. Categorical variables were described as frequencies and percentages. Numerical variables were described by means and standard deviations. Independent sample t-test and one-way analysis of variance were used to investigate the differences in dementia family caregivers’ affiliate stigma based on the family caregivers’ and patients’ demographic characteristics. Pearson correlation analysis was used to detect the correlation between dementia family caregivers’ burden and affiliate stigma and the relationship between the numerical demographic variables and affiliate stigma. Multiple linear regression was used to explore the factors influencing dementia family caregivers’ affiliate stigma. Nominal variables were converted into dummy variables before entering the regression model. A difference of p < 0.05 was considered to indicate statistical significance.
4 Results
4.1 Demographic characteristics of dementia family caregivers and patients with dementia
The demographic characteristics of the family caregivers and patients with dementia are shown in Table 1. The average age of the family caregivers was 39.12 years (standard deviation = 9.67, range: 21–77), and their average time spent caring for patients per day was 5.44 h (standard deviation = 3.01, range: 1–15). Slightly more than half of the family caregivers were women (50.5%). More than two-fifths of the family caregivers had an undergraduate educational level (40.3%) and a monthly household income of more than 5,001 RMB (41.1%). More than one-third of the family caregivers had a basic knowledge of dementia (35.5%). The majority of the family caregivers were of Han ethnicity (99.6%), with no religious beliefs (73.5%), married (85.1%), employed (84.0%), children of the patients with dementia (78.4%), took regular breaks during patient care (85.0%), living with the patients with dementia (87.2%), and received assistance in caring for the patients with dementia (91.5%). The average age of the patients with dementia was 65.21 years (standard deviation =8.17, range: 52–92), and the average course of disease was 5.56 years (standard deviation =3.29, range: 1–20). The majority of the patients were male (54.9%) of Han ethnicity (99.6%), with no religious beliefs (70.4%), married (72.2%), having new rural cooperative medical insurance (51.3%), and had partial self-care abilities (76.3%).
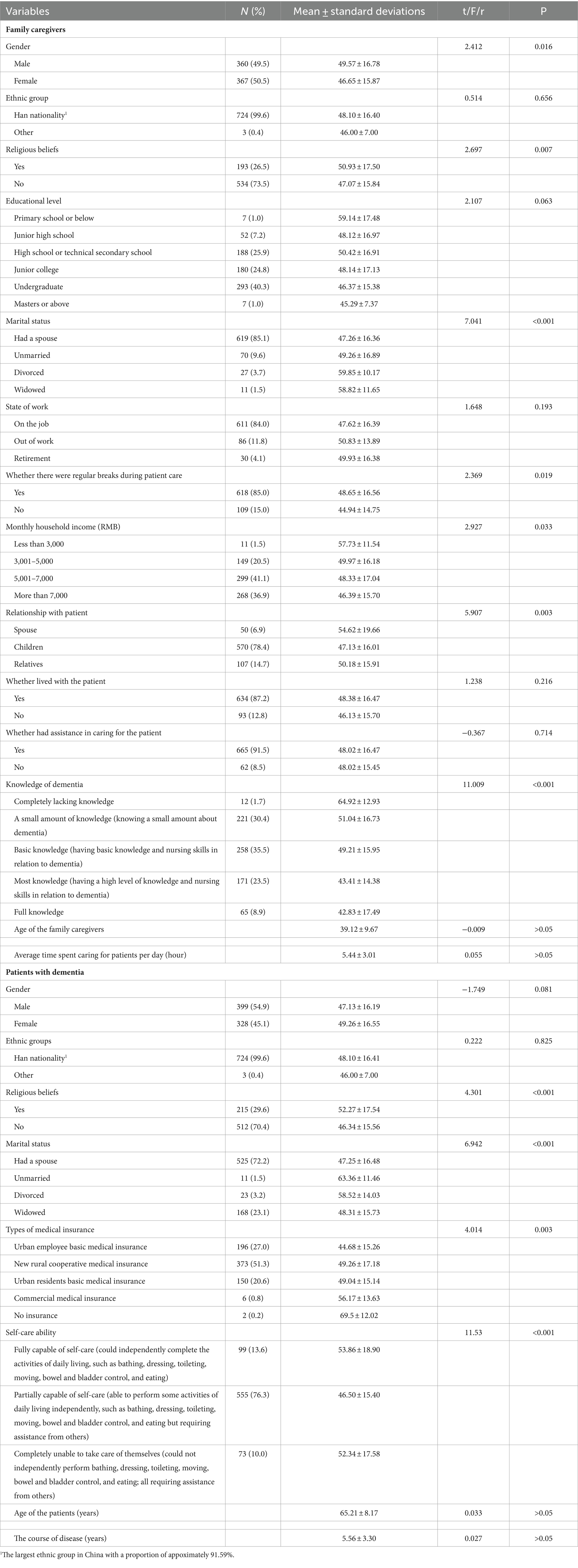
Table 1. Demographic characteristics and univariate analysis of affiliated stigma among family caregivers and patients with dementia (N = 727).
4.2 Level of dementia family caregivers’ affiliate stigma and burden
The mean scores of total affiliate stigma and each dimension are presented in Table 2. The total affiliate stigma score of dementia family caregivers was 48.09 (standard deviation = 16.38), which corresponded to a moderate to high level. The mean scores for the affective, behavioral, and cognitive dimensions were 16.03 (standard deviation = 5.31), 17.25 (standard deviation = 6.18), and 14.81 (standard deviation = 5.33), respectively. In addition, the total caregiver burden score of dementia family caregivers was 47.35 (standard deviation = 21.41), which corresponded to a high level. The mean scores of its dimensions are shown in Table 2.
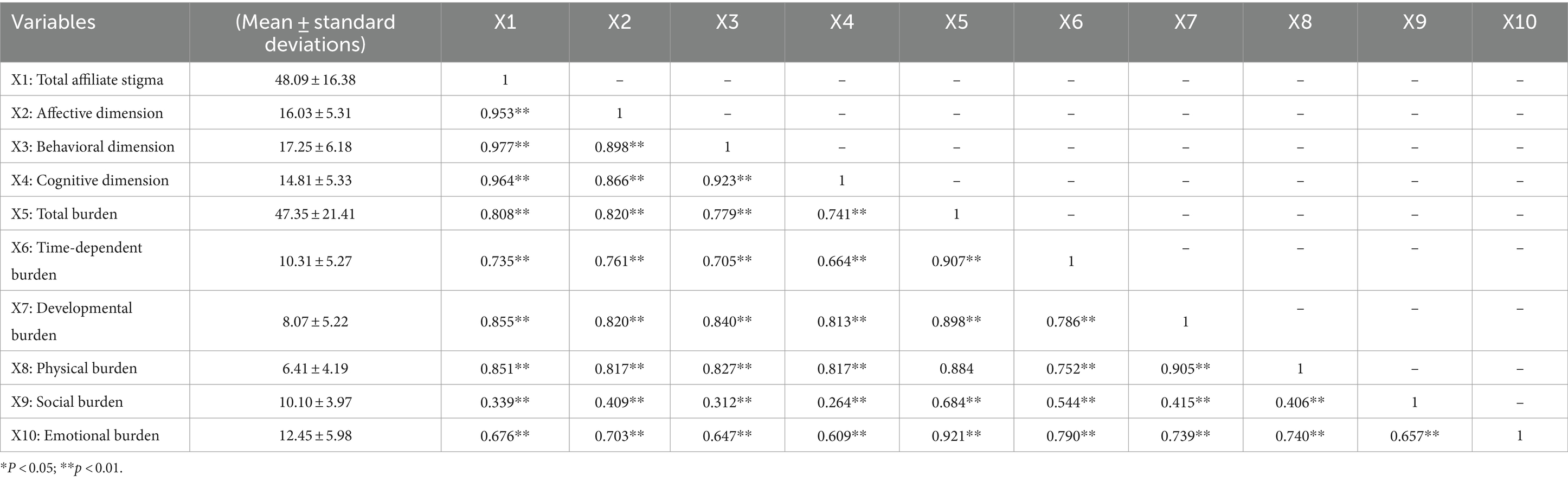
Table 2. The means and standard deviations of dementia family caregivers’ burden and affiliate stigma and the relationship between them (N = 727).
4.3 Factors influencing dementia family caregivers’ affiliate stigma
The univariate analysis showed that dementia family caregivers’ gender, religious beliefs, marital status, whether regular breaks were taken during patient care, monthly household income, relationship with patients, and knowledge of dementia were associated with their levels of affiliate stigma. Furthermore, the patients’ religious beliefs, marital status, types of medical insurance, and self-care ability were also associated with dementia family caregivers’ affiliate stigma (Table 1). The reference values of the non-continuous variables above are shown in Table 3. In addition, Pearson correlation analysis showed that the total and dimension scores of dementia family caregivers’ burden were all significantly and positively correlated with the total and dimension scores of their affiliate stigma (Table 2).
Factors associated with dementia family caregivers’ affiliate stigma in the univariate analysis and Pearson correlation analysis were included in the multiple linear regression model. The results showed that time-dependent burden, developmental burden, physical burden, social burden, and whether regular breaks were taken during patient care influenced dementia family caregivers’ affiliate stigma. In descending order of their magnitude of influence, the five variables were developmental burden (β = 0.393), physical burden (β = 0.392), time-dependent burden (β = 0.176), social burden (β = −0.080) and whether regular breaks were taken during patient care (yes) (β = −0.036). See Table 4 for details.
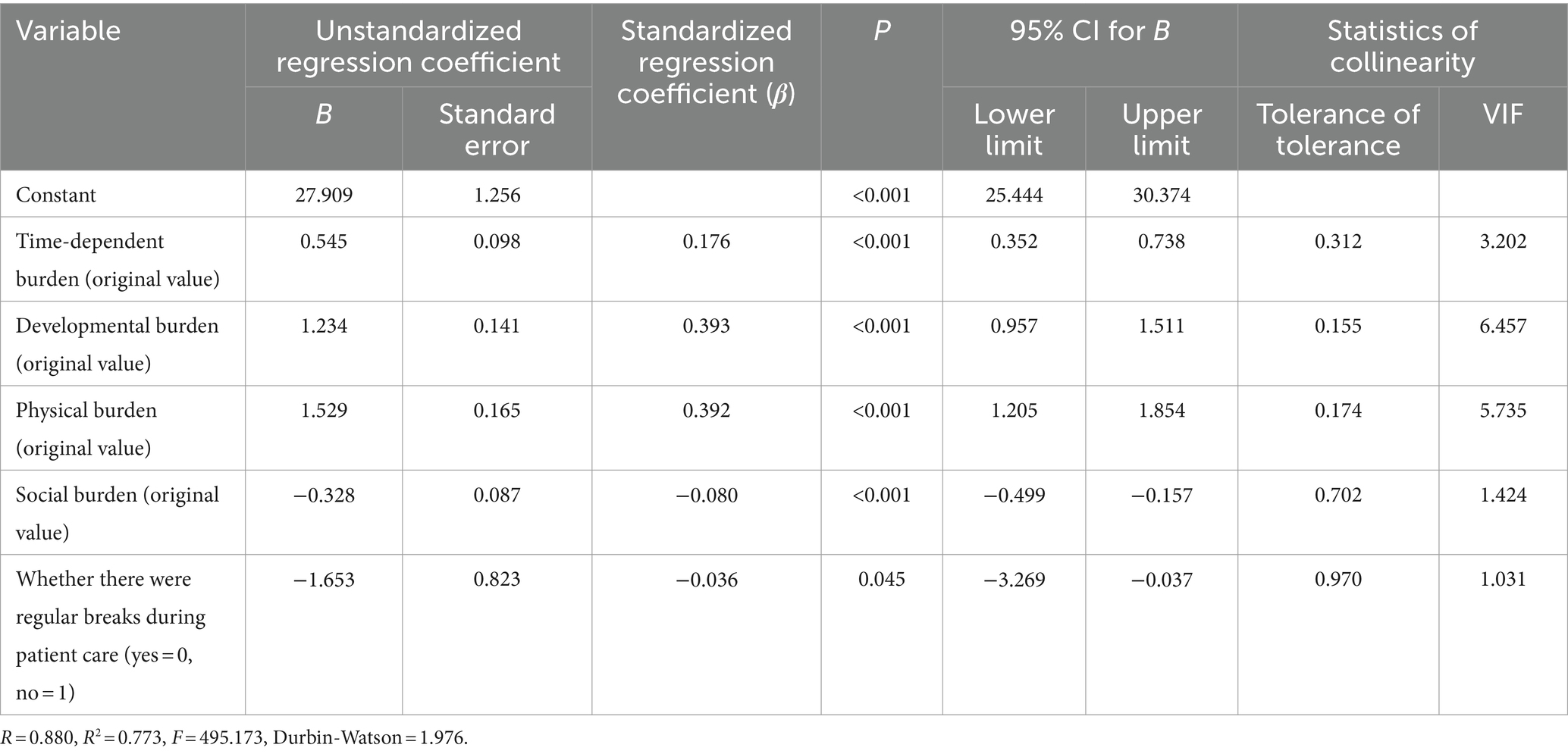
Table 4. Multiple linear regression analysis of dementia family caregivers’ affiliate stigma (N = 727).
5 Discussion
5.1 Levels of affiliate stigma among dementia family caregivers
The affiliate stigma scores of dementia family caregivers in China indicated that this group experienced a moderate to high level of affiliate stigma, which was higher than that reported in previous studies (24–26). This finding may be explained by the following reasons: First, a review suggested that much of the research studies on family stigma has focused on Asian countries, with Chinese culture emphasizing collectivism (54). As a result, the impact of affiliate stigma on Chinese family caregivers is obviously greater. Second, highly abnormal behaviors in people with dementia, such as agitation, irritability, defiance, wandering, cognitive impairment, and unintentional injuries (55–58), may all contribute to affiliate stigma of family caregivers. Third, the majority of the caregivers in this study were adult children of patients—a group that has previously been reported to experience high levels of affiliate stigma (37). This may also explain the higher scores of affiliate stigma observed in this study. Notably, Iranian dementia family caregivers’ level of affiliate stigma was higher than the levels found in our study (16). This may be due to the difference in the proportion of female caregivers in the samples of the two studies, i.e., two-thirds of the dementia family caregivers were women in the Iran study (16), while only half were women in this study. It is worth noting that women in both Iranian and traditional Chinese culture are expected to assume the role of caregivers. Given that researchers have found that female caregivers generally experience higher affiliate stigma (25), it is not surprising that the level of affiliate stigma was higher in the Iran study as it included more female caregivers.
5.2 Factors influencing dementia family caregivers’ affiliate stigma
The multiple linear regression analysis revealed that dementia family caregivers’ affiliate stigma was influenced by their time-dependent burden, developmental burden, physical burden, social burden, and whether they took regular breaks during patient care (yes).
This study found that dementia family caregivers with higher time-dependent burden exhibited higher level of affiliate stigma. Time-dependent burden is a measure of the cost of the caregivers’ time spent on caring for the patients (42). A previous study showed that time-dependent burden is associated with dementia severity (42), and the time spent by caregivers significantly increases as dementia worsens. In this case, the caregivers spend significantly more time at home, and they may even need to take the patients along with them, for the patients’ own safety, when they have to leave home. These factors reinforce the affiliated stigma of the caregivers.
Family caregivers with higher developmental burden exhibited higher affiliate stigma in our study. Developmental burden explains the sense of failure generated by caregivers compared with their peers during development (42). Dementia family caregivers may perceive themselves at a stage in life which does not match their expectations of their development at that stage. Owing to their caregiving duties, their development and progression, in terms of life goals, may have stagnated relative to their peers, which may trigger psychological imbalance. They may then strive harder to pursue their unfulfilled ambitions to meet their developmental expectations (59) and suffer more affiliate stigma in the process of socializing with their peers who are more developmentally advanced.
Our study showed that caregivers with higher physical burden reported higher affiliate stigma. Physical burden describes the caregivers’ perception of chronic fatigue and harm to physical health (42). A previous study has shown that behavioral disorders among dementia patients, such as increased nocturnal activity, incontinence, and impaired mobility, resulted in physical stress for caregivers (60), which subsequently added to their physical burden (61). In addition, with increased cognitive impairment of patients, caregivers perceive more conflict and less resilience and support in the family (62, 63). The increased physical burden and prolonged exposure to a non-supportive environment may result in incremental affiliate stigma of caregivers.
This study also found that family caregivers with higher social burden had lower levels of affiliate stigma. Social burden refers to the caregivers’ perception of role conflict (42). Higher social burden was correlated with lower affiliate stigma, which may be explained as follows: The majority of the family caregivers were the children of the patients (78.4%) who experienced higher social burden owing to a variety of social roles they performed, such as filial duties, employees, and parental duties. Multiple roles may keep them busy with their families and work, giving them little time to develop perceptions of affiliate stigma. Thus, family caregivers with higher social burden exhibited lower affiliate stigma. Conversely, family caregivers with lower social burden may not take on more social roles and focus on caring for patients with dementia, leading to higher affiliate stigma.
In contrast to findings from a previous study (49), dementia family caregivers who had regular breaks during caregiving experienced higher affiliate stigma in this study. The reason may be that caregivers with regular rest have more opportunities to socialize with the outside world, with higher engagement in interpersonal relationships. As a result, they often feel anxiety and shame owing to perceptions of being discriminated by others, which, in turn, leads to affiliate stigma. Conversely, caregivers who do not take regular breaks are more physically tired and have less contact with the outside world and are thus less likely to feel judged by others. This may explain their lower level of affiliate stigma relative to caregivers who had regular rest.
In summary, this study examined dementia family caregivers’ affiliate stigma levels from the perspective of dimensions of caregiver burden. The results may provide a basis for formulating targeted intervention strategies. Notably, demographic variables, such as family caregivers’ gender, religious beliefs, marital status, monthly household income, relationship with patients, knowledge of dementia and patients’ religious beliefs, marital status, types of medical insurance, and self-care ability did not enter the regression model, although they were found to have a significant influence on affiliate stigma in the univariate analysis. The reason may be that there are correlations between these variables; therefore, their effects on affiliate stigma are counteracted in the regression model. Future studies are recommended to further explore the relationship between these demographic variables. In addition, there may be other mediating variables between these demographic variables and affiliate stigma, which must also be further explored.
6 Limitations
This study has some limitations. First, the cross-sectional design did not allow us to determine causality between variables. Future longitudinal studies are necessary to further explore the causal relationship between variables. Second, the data were collected using self-reported questionnaires, which might be susceptible to self-report bias. Indicators that are more objective should be used in future studies. Third, only one main variable was included in addition to the demographic variables, which may not fully explain the factors that influence affiliate stigma in the present group. Studies involving more variables are necessary in the future. Fourth, the purposive sampling method was used to recruit target participants; however, the participants were sourced from only one dementia family caregiver online communication group. Future studies should aim to recruit participants from multiple centers to improve the generalizability of the study results. Finally, the online data collection method made it impossible to control the quality of the data filling process. Future research should adopt the on-site questionnaire collection method to ensure the quality of data.
7 Conclusion
Dementia family caregivers showed a moderate to high level of affiliate stigma, warranting urgent attention and efforts to mitigate this burden. Dementia family caregivers who had regular breaks during patient care, higher time-dependent burden, developmental burden, and physical burden and lower social burden exhibited higher levels of affiliate stigma.
8 Implications for practice
Dementia family caregivers’ affiliate stigma can be reduced by regulating their breaks during patient care, time-dependent burden, developmental burden, physical burden, and social burden. Specifically, we recommend that healthcare providers: (1) help dementia family caregivers understand the characteristics of the disease and establish an appropriate attitude toward dementia so as to enable them to reduce the impact of external bias; (2) provide development advice and help identify better development opportunities for dementia family caregivers; (3) provide professional caring knowledge and skill training in regard to dementia care to reduce the harm caused by the caring process to the family caregivers’ physical health; (4) build a social support system with multiple subjects (medical staff, community workers, and social workers) collaborating to relieve affiliate stigma of the family caregivers and reduce their social burden.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Review Board of Wenzhou Medical University (NO.2022–003). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YS: Data curation, Investigation, Supervision, Validation, Writing – original draft, Writing – review & editing. SD: Supervision, Writing – original draft, Writing – review & editing. ZL: Data curation, Writing – original draft. MX: Investigation, Writing – original draft. HZ: Investigation, Writing – original draft. SL: Investigation, Writing – original draft. JL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Innovation and Entrepreneurship Training program for College Students (Nos. 202110343045 and 202210343008) and the Undergraduate Student Research Project of Wenzhou Medical University (Nos. wyx2022102009 and wyx2022102010).
Acknowledgments
The authors would like to acknowledge all of the participants and researchers in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brown, AD, Kelso, W, Velakoulis, D, Farrand, S, and Stolwyk, RJ. Understanding Clinician's experiences with implementation of a younger onset dementia telehealth service. J Geriatr Psychiatry Neurol. (2023) 36:295–308. doi: 10.1177/08919887221141653
2. Koopmans, RT, Reinders, R, van Vliet, D, Verhey, FR, de Vugt, ME, Bor, H, et al. Prevalence and correlates of psychotropic drug use in community-dwelling people with young-onset dementia: the Needyd-study. Int Psychogeriatr. (2014) 26:1983–9. doi: 10.1017/s1041610213002330
3. Liu, Z, Sun, W, Chen, H, Zhuang, J, Wu, B, Xu, H, et al. Caregiver burden and its associated factors among family caregivers of persons with dementia in Shanghai, China: a cross-sectional study. BMJ Open. (2022) 12:1–11. doi: 10.1136/bmjopen-2021-057817
4. Li, J, Li, Y, and Li, P. Perceived grief among caregivers of patients with dementia in China. Clin Nurs Res. (2019) 30:70–81. doi: 10.1177/1054773819839265
5. Wang, H, Xie, H, Qu, Q, Chen, W, Sun, Y, Zhang, N, et al. The continuum of Care for Dementia: needs, resources and practice in China. J Glob Health. (2019) 9:1–13. doi: 10.7189/jogh.09.020321
6. Li, J, Gao, G, Zeng, Y, Wu, Y, Zhu, X, and Xu, H. Perceived social support in Chinese family caregivers of patients with dementia. Int J Nurs Pract. (2021) 28:e12945. doi: 10.1111/ijn.12945
7. Brodaty, H, and Donkin, M. Family caregivers of people with dementia. Dialogues Clin Neurosci. (2009) 11:217–28. doi: 10.31887/DCNS.2009.11.2/hbrodaty
8. Liu, D, Cheng, G, An, L, Gan, X, Wu, Y, Zhang, B, et al. Public knowledge about dementia in China: a National Wechat-Based Survey. Int J Environ Res Public Health. (2019) 16:1–14. doi: 10.3390/ijerph16214231
9. Baharudin, AD, Din, NC, Subramaniam, P, and Razali, R. The associations between behavioral-psychological symptoms of dementia (Bpsd) and coping strategy, burden of care and personality style among low-income caregivers of patients with dementia. BMC Public Health. (2019) 19:1–12. doi: 10.1186/s12889-019-6868-0
10. Qiu, D, Hu, M, Yu, Y, Tang, B, and Xiao, S. Acceptability of psychosocial interventions for dementia caregivers: a systematic review. BMC Psychiatry. (2019) 19:1–14. doi: 10.1186/s12888-018-1976-4
11. Saffari, M, Koenig, HG, O'Garo, KN, and Pakpour, AH. Mediating effect of spiritual coping strategies and family Stigma stress on caregiving burden and mental health in caregivers of persons with dementia. Dementia. (2018) 1–18. doi: 10.1177/1471301218798082
12. Sallim, AB, Sayampanathan, AA, Cuttilan, A, and Ho, R. Prevalence of mental health disorders among caregivers of patients with Alzheimer disease. J Am Med Dir Assoc. (2015) 16:1034–41. doi: 10.1016/j.jamda.2015.09.007
13. Chang, C-C, Su, J-A, and Lin, C-Y. Using the affiliate Stigma scale with caregivers of people with dementia: psychometric evaluation. Alzheimers Res Ther. (2016) 8:45. doi: 10.1186/s13195-016-0213-y
14. Su, JA, and Chang, CC. Association between family caregiver burden and affiliate Stigma in the families of people with dementia. Int J Environ Res Public Health. (2020) 17:1–10. doi: 10.3390/ijerph17082772
15. Weisman de Mamani, A, Weintraub, MJ, Maura, J, Martinez de Andino, A, and Stigma, BCA. Expressed emotion, and quality of life in caregivers of individuals with dementia. Fam Process. (2018) 57:694–706. doi: 10.1111/famp.12325
16. Saffari, M, Lin, C-Y, Koenig, HG, O’Garo, K-GN, Broström, A, and Pakpour, AH. A Persian version of the affiliate Stigma scale in caregivers of people with dementia. Health promotion. Perspectives. (2019) 9:31–9. doi: 10.15171/hpp.2019.04
17. Meichsner, F, Köhler, S, and Wilz, G. Moving through Predeath grief: psychological support for family caregivers of people with dementia. Dementia. (2017) 18:2474–93. doi: 10.1177/1471301217748504
18. Sun, F . Caregiving stress and coping: a thematic analysis of Chinese family caregivers of persons with dementia. Dementia. (2014) 13:803–18. doi: 10.1177/1471301213485593
19. Werner, P, Goldstein, D, and Buchbinder, E. Subjective experience of family Stigma as reported by children of Alzheimer's disease patients. Qual Health Res. (2010) 20:159–69. doi: 10.1177/1049732309358330
20. Xiao, LD, Habel, L, and De Bellis, A. Perceived challenges in dementia care by Vietnamese family caregivers and Care Workers in South Australia. J Cross Cult Gerontol. (2015) 30:333–52. doi: 10.1007/s10823-015-9264-y
21. Liu, D, Hinton, L, Tran, C, Hinton, D, and Barker, JC. Reexamining the relationships among dementia, Stigma, and aging in immigrant Chinese and Vietnamese family caregivers. J Cross Cult Gerontol. (2008) 23:283–99. doi: 10.1007/s10823-008-9075-5
22. Zhang, Y, Subramaniam, M, Lee, SP, Abdin, E, Sagayadevan, V, Jeyagurunathan, A, et al. Affiliate Stigma and its association with quality of life among caregivers of relatives with mental illness in Singapore. Psychiatry Res. (2018) 265:55–61. doi: 10.1016/j.psychres.2018.04.044
23. Shibre, TNA, Kullgren, G, Kebede, D, Alem, A, Fekadu, A, Fekadu, D, et al. Perception of Stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Soc Psychiatry Psychiatr Epidemiol. (2001) 36:299–303. doi: 10.1007/s001270170048
24. Bhatt, J, Scior, K, Stoner, CR, Moniz-Cook, E, and Charlesworth, G. Stigma among Uk family Carers of people living with dementia. BJPsych Open. (2022) 8:1–7. doi: 10.1192/bjo.2022.585
25. Van den Bossche, P, and Schoenmakers, B. The impact of Dementia's affiliate Stigma on the mental health of relatives: a cross section survey. Front Psychol. (2022) 12:12. doi: 10.3389/fpsyg.2021.789105
26. Chen, Y-J, Su, J-A, Chen, J-S, Liu, C-h, Griffiths, MD, Tsai, H-C, et al. Examining the association between neuropsychiatric symptoms among people with dementia and caregiver mental health: are caregiver burden and affiliate Stigma mediators? BMC Geriatr. (2023) 23:27. doi: 10.1186/s12877-023-03735-2
27. Hengxiao, L, Yaxin, W, Mengyuan, M, Yuchen, D, Huifang, Z, and Qiaoju, Y. Study on the relationship between Stigma, social support and general self-efficacy of family caregivers with Alzheimer's disease. Chinese Evidence-Based Nursing. (2023) 9:1409–1413. doi: 10.12102/j.issn.2095-8668.2023.08.012
28. Werner, P, and Abo, JH. Who internalizes courtesy Stigma and how? A study among Israeli Arab family caregivers of persons with dementia. Aging Ment Health. (2019) 24:1153–60. doi: 10.1080/13607863.2019.1584790
29. Velilla, L, Acosta-Baena, N, Allen, I, Lopera, F, and Kramer, J. Analysis of family Stigma and socioeconomic factors impact among caregivers of patients with early-and late-onset Alzheimer's disease and frontotemporal dementia. Sci Rep. (2022) 12:12663. doi: 10.1038/s41598-022-16400-2
30. Yun, YSJS, Fadzil, NA, and Cheng, KY. Validation of the Malay version of the affiliate Stigma scale among caregivers of patients with mental illness. Malays J Med Sci. (2018) 25:127–36. doi: 10.21315/mjms2018.25.6.13
31. Mak, WWS, and Cheung, RYM. Psychological distress and subjective burden of caregivers of people with mental illness: the role of affiliate Stigma and face concern. Community Ment Health J. (2011) 48:270–4. doi: 10.1007/s10597-011-9422-9
32. Jeong, JS, Kim, SY, and Kim, JN. Ashamed caregivers: self-Stigma, information, and coping among dementia patient families. J Health Commun. (2020) 25:870–8. doi: 10.1080/10810730.2020.1846641
33. Oliveira, D, da Mata, F, Mateus, E, Musyimi, CW, Farina, N, Ferri, CP, et al. Experiences of Stigma and discrimination among people living with dementia and family Carers in Brazil: qualitative study. Ageing Soc. (2023) 43:447–68. doi: 10.1017/s0144686x21000660
34. Nwakasi, CC, de Medeiros, K, and Bosun-Arije, FS. "we are doing these things so that people will not laugh at us": Caregivers' attitudes about dementia and caregiving in Nigeria. Qual Health Res. (2021) 31:1448–58. doi: 10.1177/10497323211004105
35. Theresia, I, Sani, TP, Evans-Lacko, S, Farina, N, Augustina, L, and Turana, Y. Experiences of caregivers of people with dementia in Indonesia: a focus group study. Int J Geriatr Psychiatry. (2023) 38:e6038. doi: 10.1002/gps.6038
36. Duodu, PA, Simkhada, B, Okyere, J, Akrong, R, Barker, C, Gillibrand, W, et al. Primary Caregivers' experiences of caring for people living with dementia in Ghana: a phenomenological study. BMC Geriatr. (2024) 24:304. doi: 10.1186/s12877-024-04894-6
37. Kahn, PV, Wishart, HA, Randolph, JS, and Santulli, RB. Caregiver Stigma and burden in memory disorders: An evaluation of the effects of caregiver type and gender. Curr Gerontol Geriatr Res. (2016) 2016:1–5. doi: 10.1155/2016/8316045
38. Dongmei, Z . Status quo and analysis of influencing factors of Stigma among family caregivers for dementia patients. J Qilu Nur. (2019) 25:58–61. doi: 10.3969/j.issn.1006-7256.2019.13.017
39. Girma, E, Möller-Leimkühler, AM, Dehning, S, Mueller, N, Tesfaye, M, and Froeschl, G. Self-Stigma among caregivers of people with mental illness: toward Caregivers' empowerment. J Multidiscip Healthc. (2014) 7:37–43. doi: 10.2147/jmdh.S57259
40. Brodaty, H, Connors, MH, Xu, J, Woodward, M, and Ames, D. The course of neuropsychiatric symptoms in dementia: a 3-year longitudinal study. J Am Med Dir Assoc. (2015) 16:380–7. doi: 10.1016/j.jamda.2014.12.018
41. Magaña, SM, Ramírez García, JI, Hernández, MG, and Cortez, R. Psychological distress among latino family caregivers of adults with Schizophrenia: The roles of burden and stigma. Psychiatric services (Washington, DC) (2007) 58:378–84. doi: 10.1176/ps.2007.58.3.378
42. Chou, K-R, Jiann-Chyun, L, and Chu, H. The reliability and validity of the Chinese version of the caregiver burden inventory. Nurs Res. (2002) 51:324–31. doi: 10.1097/00006199-200209000-00009
43. Novak, M, and Guest, C. Application of a multidimensional caregiver burden inventory. The Gerontologist. (1989) 29:798–803. doi: 10.1093/geront/29.6.798
44. Werner, P, Mittelman, MS, Goldstein, D, and Heinik, J. Family Stigma and caregiver burden in Alzheimer's disease. The Gerontologist. (2011) 52:89–97. doi: 10.1093/geront/gnr117
45. Stratton, SJ . Purposeful sampling: advantages and pitfalls. Prehosp Disaster Med. (2024) 39:121–2. doi: 10.1017/s1049023x24000281
46. Kang, H . Sample size determination and power analysis using the G*power software. J Educ Eval Health Pro. (2021) 18:18. doi: 10.3352/jeehp.2021.18.17
47. Jan, S-L, and Shieh, G. Sample size calculations for model validation in linear regression analysis. BMC Med Res Methodol. (2019) 19:54. doi: 10.1186/s12874-019-0697-9
48. Ni, P, Chen, J, and Liu, N. The sample size estimation in quantitative nursing research. Chin J Nurs. (2010) 45:378–80. doi: 10.3761/j.issn.0254-1769.2010.04.037
49. Xu, XY, Leung, D, Leung, AYM, Kwan, RYC, Liang, TN, and Chai, AJ. "am I entitled to take a break in caregiving?": perceptions of leisure activities of family caregivers of loved ones with dementia in China. Dementia. (2022) 21:1682–98. doi: 10.1177/14713012221093879
50. Chang, CC, Yen, CF, Jang, FL, Su, JA, and Lin, CY. Comparing affiliate Stigma between family caregivers of people with different severe mental illness in Taiwan. J Nerv Ment Dis. (2017) 205:542–9. doi: 10.1097/NMD.0000000000000671
51. Perlick, DA, Miklowitz, DJ, Link, BG, Struening, E, Kaczynski, R, Gonzalez, J, et al. Perceived Stigma and depression among caregivers of patients with bipolar disorder. Br J Psychiatry. (2007) 190:535–6. doi: 10.1192/bjp.bp.105.020826
52. Mak, W, and Cheung, R. Affiliate Stigma among caregivers of people with intellectual disability or mental illness. J Appl Res Intellect Disabil. (2008) 21:532–45. doi: 10.1111/j.1468-3148.2008.00426.x
53. Yue, P, Fu, Y, Shang, S, Liu, Y, Wang, Z, and Yu, X. Reliability and validity of the caregiver burden inventory. Chin Ment Health J. (2006) 8:562–4. doi: 10.3321/j.issn:1000-6729.2006.08.026
54. Werner, S, Corrigan, P, Ditchman, N, and Sokol, K. Stigma and intellectual disability: a review of related measures and future directions. Res Dev Disabil. (2012) 33:748–65. doi: 10.1016/j.ridd.2011.10.009
55. Rogowska, M, Thornton, M, Creese, B, Velayudhan, L, Aarsland, D, Ballard, C, et al. Implications of adverse outcomes associated with antipsychotics in older patients with dementia: a 2011–2022 update. Drugs Aging. (2022) 40:21–32. doi: 10.1007/s40266-022-00992-5
56. Wilfling, D, Junghans, A, Marshall, L, Eisemann, N, Meyer, G, Möhler, R, et al. Non-pharmacological interventions for sleep disturbances in people with dementia. Cochrane Database Syst Rev. (2023) 1–101. doi: 10.1002/14651858.Cd011881
57. Hugo, J, and Ganguli, M. Dementia and cognitive impairment. Clin Geriatr Med. (2014) 30:421–42. doi: 10.1016/j.cger.2014.04.001
58. Lynds, ME, and Arnold, CM. Fall risk screening and assessment for people living with dementia: a scoping review. J Appl Gerontol. (2023) 42:2025–35. doi: 10.1177/07334648231168983
59. Ziello, A, Pastore, F, Fasanaro, AM, Poderico, C, and Iavarone, A. Caregiver burden and coping strategies in caregivers of patients with Alzheimer&Rsquo;S disease. Neuropsychiatr Dis Treat. (2014) 10:1407–13. doi: 10.2147/ndt.S58063
60. Hope, T, Keene, J, Gedling, K, Fairburn, CG, and Jacoby, R. Predictors of institutionalization for people with dementia living at home with a Carer. Int J Geriatr Psychiatry. (1998) 13:682–90. doi: 10.1002/(sici)1099-1166(1998100)13:10<682::Aid-gps847>3.0.Co;2-y
61. Schnaider Beeri, M, Werner, P, Davidson, M, and Noy, S. The cost of behavioral and psychological symptoms of dementia (Bpsd) in community dwelling Alzheimer's disease patients. Int J Geriatr Psychiatry. (2002) 17:403–8. doi: 10.1002/gps.490
62. Deimling, GT, Smerglia, VL, and Schaefer, ML. The impact of family environment and decision-making satisfaction on caregiver depression. J Aging Health. (2016) 13:47–71. doi: 10.1177/089826430101300103
Keywords: dementia, family caregiver, affiliate stigma, China, caregiver burden
Citation: Shi Y, Dong S, Liang Z, Xie M, Zhang H, Li S and Li J (2024) Affiliate Stigma among family caregivers of individuals with dementia in China: a cross-sectional study. Front. Public Health. 12:1366143. doi: 10.3389/fpubh.2024.1366143
Edited by:
Zahir Vally, United Arab Emirates University, United Arab EmiratesReviewed by:
Farah Purwaningrum, Kalta Bina Insani, IndonesiaMatias E. Rodriguez-Rivas, Universidad de Desarrollo, Chile
Copyright © 2024 Shi, Dong, Liang, Xie, Zhang, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jufang Li, lijufang911@126.com
†These authors have contributed equally to this work and share last authorship
 Yingying Shi
Yingying Shi Shishi Dong
Shishi Dong Zhiqi Liang1†
Zhiqi Liang1† Jufang Li
Jufang Li