- 1Department of Pharmacy Practice, Faculty of Pharmacy, Bahauddin Zakariya University, Multan, Pakistan
- 2Department of Political Sciences, Bahauddin Zakariya University, Multan, Pakistan
- 3School of Management Sciences, University Sains Malaysia, Penang, Malaysia
- 4Department of Pharmacy Practice, Faculty of Pharmaceutical Sciences, Government College University, Faisalabad, Pakistan
- 5Department of Health Science, Faculty of Public Governance and Business, Mykolas Romeris University, Vilnius, Lithuania
- 6Faculty of Medicine, University of Oslo, Oslo, Norway
- 7Infectious Diseases Department, Alnoor Specialist Hospital, Ministry of Health, Makkah, Saudi Arabia
- 8Pharmacy Department, Alnoor Specialist Hospital, Ministry of Health, Makkah, Saudi Arabia
- 9Department of Clinical Pharmacy, Faculty of Pharmacy, Al-Baha University, Al-Baha, Saudi Arabia
- 10Department of Pharmaceutical Practices, College of Pharmacy, Umm Al-Qura University, Makkah, Saudi Arabia
- 11OPD Pharmacy, Security Forces Hospital, Dammam, Saudi Arabia
- 12Department of Pharmacology and Toxicology, Faculty of Medicine in Al-Qunfudah, Umm Al-Qura University, Makkah, Saudi Arabia
- 13Pharmaceutical Care Department, Ministry of National-Guard Health Affairs, Jeddah, Saudi Arabia
- 14Department of Clinical Pharmacy, College of Health Sciences and Nursing, Al-Rayan Colleges, Al-Madinah Al-Munawarah, Saudi Arabia
Background: The COVID-19 comorbid population is at higher risk of developing severe health issues like acute respiratory distress syndrome, coagulation syndrome, metabolic acidosis, and septic shock, potentially leading to patient death. Patients’ knowledge, attitudes, and practices (KAP) significantly influence their response to the pandemic and aid in enhancing health policy implementation.
Objective: To identify and evaluate the pattern and associated factors to COVID-19 knowledge, attitude, and practice among individuals with comorbidities.
Methodology: The systematic review followed the PRISMA guidelines. Relevant studies assessing the KAP of comorbid patients were retrieved by carefully searching the PubMed and Google Scholar databases. The appraisal tool for cross-sectional studies was used to determine the quality of the included studies and the risk of biases.
Results: Eighteen studies met the inclusion criteria and were included in the review. The pooled sample size of the included studies was 9,104. Different comorbidities reported in the studies include hypertension, diabetes, psychological disorders, and cancer. Pooled analysis showed that 65% of patients showed good knowledge, 57% of patients showed a positive attitude and 51% of patients followed good practices to manage the COVID-19 in presence of their comorbid condition. Significant factors impacting knowledge, attitude and practice in COVID-19 comorbid patients were ethnicity OR 1.78 [95% CI 1.35–2.32]; educational status 3.2 [2.79–3.58]; urban residence 2.43 [1.65–3.02]; employment Status 1.67[1.34–2.12]; financial Status 4.02[3.66–4.38]; occupation 3.65[3.31–4.25]; information Source 2.64[2.19–3.26]; comorbidity 3.28[2.78–3.61]; and duration of chronic illness 1.59[1.31–2.04].
Conclusion: Comorbid COVID-19 patients showed good knowledge, positive attitude and good practice towards the management of the disease.
Introduction
The coronavirus disease is an extremely contagious and infectious pulmonary disease, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-COV2). The first outbreak was initiated in Wuhan, China, in December 2019, and soon it blew out throughout the globe due to a higher spread rate (1). It infected a large population of the world in a short time interval. The emergence and widespread prevalence of coronavirus disease have resulted in severe consequences in different dimensions. According to the World Health Organization (WHO), COVID-19 has affected almost 470 million people throughout the globe, with a death rate of 3.4% (2, 3). Due to the high infection rate and associated mortality, COVID-19 was declared as Public Health Emergency of International Concern by the WHO at the start of 2020 (4).
The SARS-CoV-2-infected patients are mostly asymptomatic or generally experience mild symptoms that include fever, dry cough, sore throat, myalgia, fever, and fatigue. Comorbidities may cause different complications in patients suffering from COVID-19. In addition to the above-mentioned symptoms, the comorbid COVID-19 population is more vulnerable to developing acute respiratory distress syndrome, coagulation syndrome, metabolic acidosis, and septic shock, which may result in patient death (5). Thus, COVID-19 patients with associated comorbid conditions, including hypertension, pregnancy, cardiovascular diseases, diabetes, renal disease, and respiratory diseases, are categorized as high-risk patients (6). These high risk comorbid COVID-19 Patients experience a twofold increase in the necessity for mechanical ventilation, and a threefold elevation in the likelihood of developing severe disease or requiring admission to the intensive care unit (ICU) (7, 8). Comorbid COVID-19 patients are at increased risk of mortality as compared to COVID-19 patients without comorbidity. Data collected from several global locations, encompassing both news outlets and scientific publications, has indicated that the overall case-fatality rate of COVID-19, standing at 3.4%, is more than three times greater (7.3%) in people with preexisting co-morbidities (5, 9–11).
Given the lack of a targeted therapeutic intervention for COVID-19, it is imperative that individuals with underlying health conditions adopt additional precautions and rigorously adhere to recommended practices of maintaining physical distance and practising proper hand hygiene. This approach is essential for facilitating the most effective management of their health. The acceptance of these preventive and therapeutic measures is contingent upon an individual’s level of awareness and knowledge regarding the infection caused by COVID-19 (12). KAP surveys are commonly employed in health behavior research to gather data on the knowledge, attitudes, and practices of individuals regarding a specific scientific topic. They exhibit characteristics that are representative of the specific demographic under study. The collected data serves as a means of assessing the state of community education (13). The role of citizens’ knowledge, attitudes, and practices (KAP) has been widely acknowledged as crucial in effectively managing previous pandemics (13). In the context of the 2009 Swine Flu pandemic, health officials were informed by KAP surveys and systematic evaluations about the necessary measures to implement to contain the transmission of emerging viruses and mitigate the impact of future pandemics (14).
The comprehension of individuals’ attitudes helps predict and influence their behavior. Understanding disease states can contribute to improving patient well-being, mitigating disease advancement, and reducing the likelihood of hospitalization and mortality (15, 16). Consequently, it is anticipated that the knowledge, attitudes, and practices (KAP) levels among individuals with comorbidities will serve as the determining factor in their battle against the COVID-19 pandemic and to effectively tailor educational interventions aimed at enhancing the application of health policies (17). This approach is crucial in mitigating the transmission and proliferation of diseases (12).
Given the nature of the COVID-19 pandemic, it is imperative to regularly update scientific literature to facilitate the production of empirical research on interventions and strategies that can enhance the efficacy of efforts aimed at mitigating the impact of the COVID-19 pandemic (18). To achieve this objective, it is imperative to conduct a comprehensive and up-to-date systematic evaluation of the existing body of data. There are a limited number of systematic reviews and meta-analyses available that have examined the knowledge, attitudes, and practises (KAP) related to COVID-19. All the available systematic reviews on KAP of COVID-19 have their own limitations. Few reviews focused on KAP of general population (19–22), some are about KAP of healthcare professionals (20), some are focused on the KAP of specific country (America and Ethiopia) (23, 24). To the best of authors’ knowledge, there has been no comprehensive review conducted to assess the effects of KAP on patients with comorbidities. Taking into consideration the constraints outlined in the existing body of literature, the present systematic review and meta-analysis aimed to identify and evaluate the pattern and associated factors to COVID-19 knowledge, attitude, and practice among individuals with comorbidities. This study has the potential to inform the formulation of policies aimed at providing support to vulnerable groups, particularly individuals with comorbidities, to mitigate mortality rates, minimise the adverse effects on the healthcare system, and prevent economic downturn.
Methodology
Search process
The systematic review followed the PRISMA guidelines (25). Relevant studies assessing the KAP of comorbid patients were retrieved by carefully searching the PubMed and Google Scholar databases until September 15, 2023 (the date last searched). For PUBMED Search terms used were, “COVID-19” OR “SARS-CoV-2” OR “2019 nCoV” OR “novel coronavirus” OR “new coronavirus” OR “severe acute respiratory syndrome coronavirus 2” OR “Wuhan and coronavirus” OR “pathogenesis” OR “infection” OR “transmission” AND “KAP” OR “knowledge” OR “attitude” OR “perception” OR “practice” OR “awareness” OR “action” AND “comorbidity” OR “diabetes” OR “hypertension” OR “pulmonary disorder” OR “renal failure” OR “cancer” OR “chronic disorder.” Moreover, included reference lists were manually searched to address all the published evidence.
Eligibility criteria
The systematic review included all the studies meeting the set inclusion criteria (1) cross-sectional studies, (2) well defined COVID-19 patients, (3) reporting at least one comorbid condition (diabetes, hypertension, pulmonary disorder, renal failure, and cancer), (4) investigating at least one or all components of KAP (knowledge, attitude and practice) model in COVID-19 patients, (5) published in peer reviewed journal. KAP studies in the general population, healthcare workers, systematic reviews, and any study published in a language other than English were excluded. The results measured in the included studies were knowledge, attitudes, and practices related to COVID-19 in comorbid patients.
The study selection approach employed the explicit method to prevent biases (26, 27). Explicit method involves rigorously adhering to stated inclusion criteria during the search process. The objective is to offer more dependable conclusions. The papers that met the inclusion and exclusion criteria, as determined by the abstract and title, were carefully examined by three reviewers. Any disagreements between the reviewers were resolved through discussion until a consensus was achieved.
Selection of studies and data extraction
Titles and abstracts were screened to assess articles for inclusion in the study. Two reviewers independently extracted data in a predesigned data extraction sheet in Excel software. Extracted information included author name, country, year, study period, study design, inclusion and exclusion criteria, method, target population, number and age of participants, study outcomes (knowledge, attitude, practice) and their associated factors. Any discrepancies between the two reviewers were resolved through discussion or by the involvement of the third reviewer (principal investigator) unless consensus was reached.
Study outcomes
The primary outcomes of the meta-analysis focused on three key areas: knowledge (including understanding of symptoms, transmission methods, high risk populations, incubation and isolation periods, virus fatality rates, and prevention and treatment of COVID-19 infection), attitude (regarding the control and management of COVID-19), and practice (such as hand hygiene, social distancing, using face masks, avoiding crowded places, and adhering to isolation measures). The included studies collected responses using “Yes/No/Do not know” or “Strongly agree/Agree/Neutral/Disagree/Strongly disagree” items. The responses of “Yes,” “True,” or “Strongly agree/Agree” were considered positive responses for the analysis. The secondary outcomes encompassed the reported factors that affect the knowledge, attitude, and practice of comorbid COVID-19 patients towards the management of disease.
Quality assessment and risk of biasness
The appraisal tool for cross-sectional studies (AXIS) was used to determine the quality of the included studies and the risk of biases (28). The tool has 20 questions, and each question carries one score. Based on the quality assessment tool scores, the studies were categorized as follows: scores (>15) were considered to have less biasness and good quality, (10–15) were considered to have moderate biasness and fair quality while (<10) were considered to have higher biasness and poor quality.
Statistical analysis
The retrieved studies provided quantitative data on the percentage of knowledge, attitudes, and practices (KAP) related to COVID-19 among patients with comorbidities. The pooled proportion of COVID-19 knowledge, attitudes, and practises (KAP) was computed and displayed using forest plots. The data on KAP-related factors was presented in the form of odds ratios (95% CI) for each component. The analysis was performed using a random effects model. The I2 index was utilized to examine the heterogeneity of the study. Values of I2 ≥ 50% show higher heterogeneity. Sensitivity tests were conducted to assess the impact of the quality score categories of the included studies (results not shown). No missing data were reported in the study. A significance level of p < 0.05 was deemed as statistically significant. Statistical software package Stata V.16 (StataCorp, United States) was used for statistical analyses.
Results
Search results
Originally, 468 articles were obtained after the initial search. After removing 23 duplicates, the remaining 445 articles were screened by title and abstract to retain 47 articles for full-text review. Eighteen studies met the inclusion criteria and were included in the review. The detailed inclusion and exclusion process is shown in Figure 1.
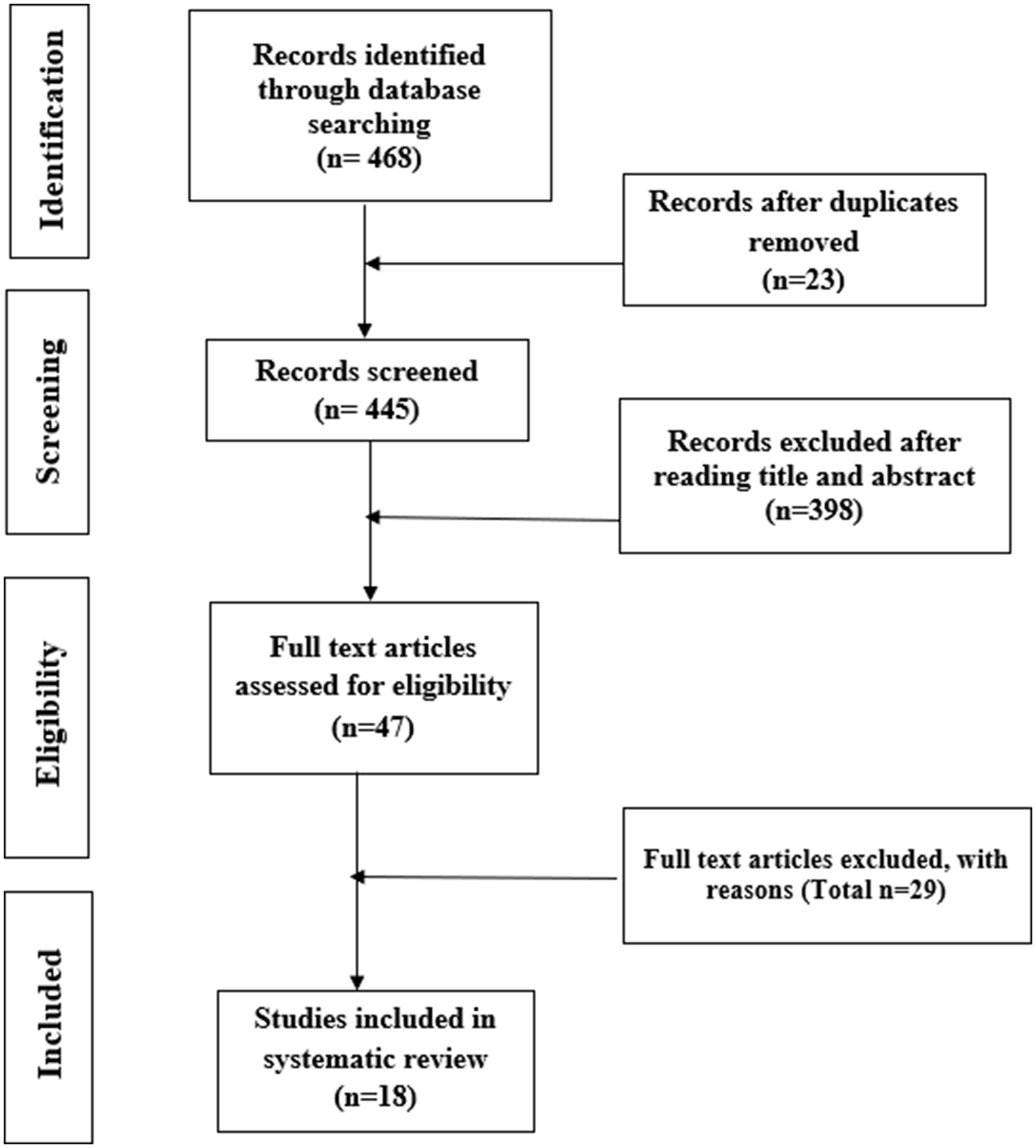
Figure 1. Systematic study selection process, in line with the PRISMA guidelines (25).
Characteristics of selected studies
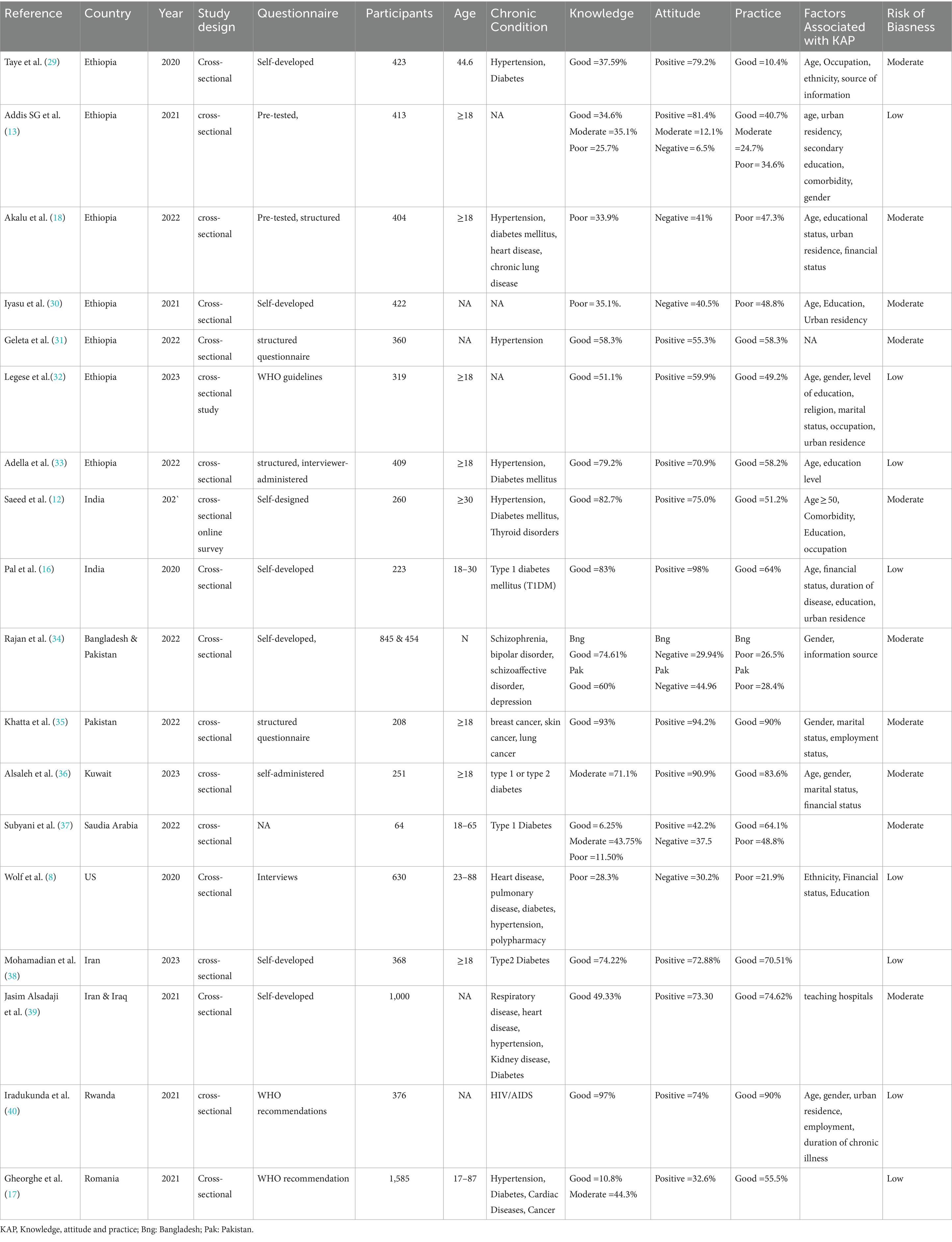
Among the included studies, seven were performed in Ethiopia, two each in India, Pakistan, and Iran, and one each in Kuwait, Saudi Arabia, the US, Rwanda, and Romania. All the studies were cross-sectional. The pooled sample size of the included studies was 9,104, ranging from 64 to 1,585. The ages of the included patients range from 18 to 80 years. Different comorbidities reported in the studies were hypertension, diabetes type 1 and 2, thyroid disorders, psychological disorders, depression, cancer, chronic pulmonary disease, heart disease, kidney disease, and HIV/AIDS. Eight studies show a low risk of bias, whereas 10 studies show a moderate risk of bias. The summaries of the included studies are demonstrated in Table 1.
The pattern of knowledge towards COVID-19
Figure 2 demonstrates the pooled proportion of the comorbid population with good knowledge about COVID-19 in the presence of their comorbid condition. Overall, 65% of the comorbid patients acquired good knowledge about COVID-19 and associated comorbidity (95% CI 43–79%, p < 0.001, I2 = 87%). Pooled analysis showed that in Ethiopia the comorbid population with knowledge was 49 to 84%. Country-wise, India 81% [95% CI 55–89%], Bangladesh 71% [95% CI 42–87%], Pakistan 83% [95% CI 49–97%], Kuwait 65% [95% CI 37–79%], Saudia Arabia 77% [95% CI 52–82%], US 45% [95% CI 31–58%], Iran 63% [95% CI 29–77%], Iraq 58% [95% CI 36–69%], Rwanda 51% [95% CI 31–62%], Romania 52% [95% CI 33–67%] population acquire good knowledge regarding management of COVID-19 along with comorbid condition. High Heterogenicity (I2 = 87%) was reported among studies.
The pattern of attitude towards COVID-19
Figure 3 demonstrates the pooled proportion of the comorbid population with a positive attitude toward COVID-19 in the presence of their comorbid condition. Overall, 57% of the comorbid patients showed a positive attitude to managing COVID-19 and associated comorbidity (95% CI 49–69%, p < 0.0001, I2 = 83%). Pooled analysis showed that in Ethiopia the comorbid population with a positive attitude to manage COVID-19 and associated comorbidity were 37 to 72%. Country-wise, India 91% [95% CI 75–97%], Bangladesh 41% [95% CI 34–49%], Pakistan 82% [95% CI 71–98%], Kuwait 81% [95% CI 69–88%], Saudia Arabia 42% [95% CI 35–49%], US 48% [95% CI 38–66%], Iran 72% [95% CI 64–82%], Iraq 41% [95% CI 32–63%], Rwanda 39% [95% CI 32–57%] and Romania 43% [95% CI 33–49%] population showed positive attitude to manage COVID-19 along with comorbid condition. High Heterogenicity (I2 = 83%) was reported among studies.
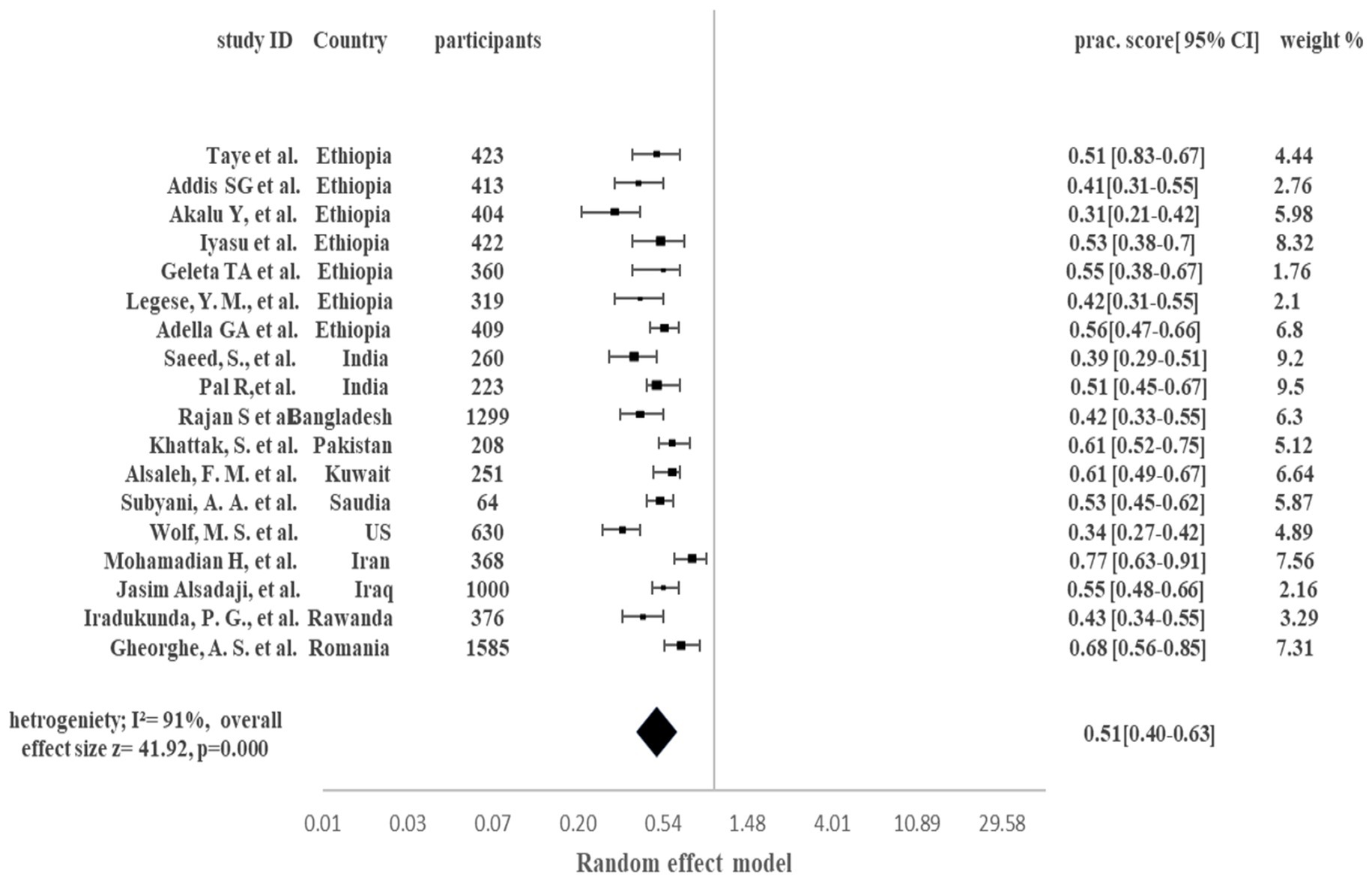
The pattern of practice towards COVID-19
Figure 4 demonstrates the pooled proportion of the comorbid COVID-19 population following good preventive practices to manage the COVID-19 in presence of their comorbid condition. Overall, 51% of the comorbid COVID-19 patients adopted good preventive practices to manage the COVID-19 in presence of their comorbid condition (95% CI 40–63%, p < 0.0001, I2 = 91%). Pooled analysis showed that in Ethiopia 31 to 56% of patients adopted good preventive practices. Country-wise, India 51% [95% CI 45–67%], Bangladesh 42% [95% CI 33–55%], Pakistan 61% [95% CI 52–75%], Kuwait 61% [95% CI 49–67%], Saudia Arabia 53% [95% CI 45–62%], US 34% [95% CI 27–42%], Iran 77% [95% CI 63–91%], Iraq 55% [95% CI 48–66%], Rwanda 43% [95% CI 34–55%] and Romania 68% [95% CI 56–85%] population were following good preventive practices to manage the COVID-19 in presence of their comorbid condition. Higher heterogenicity (I2 = 91%) was reported among studies.
Factors related to COVID-19 knowledge attitude and practice
Different factors affecting the knowledge, attitude, and preventive practices to manage the COVID-19 in presence of comorbidity are shown in Figure 5 with odd ratios, 95% CI, p values, I2 statistics and forest plot. Significant factors (OR [95% CI]) impacting knowledge, attitude and practice in COVID-19 comorbid patients were ethnicity 1.78 [1.35–2.32]; educational status 3.2 [2.79–3.58]; urban residence 2.43 [1.65–3.02]; employment Status 1.67[1.34–2.12]; financial Status 4.02[3.66–4.38]; occupation 3.65[3.31–4.25]; information Source 2.64[2.19–3.26]; comorbidity 3.28[2.78–3.61]; and duration of chronic illness 1.59[1.31–2.04].
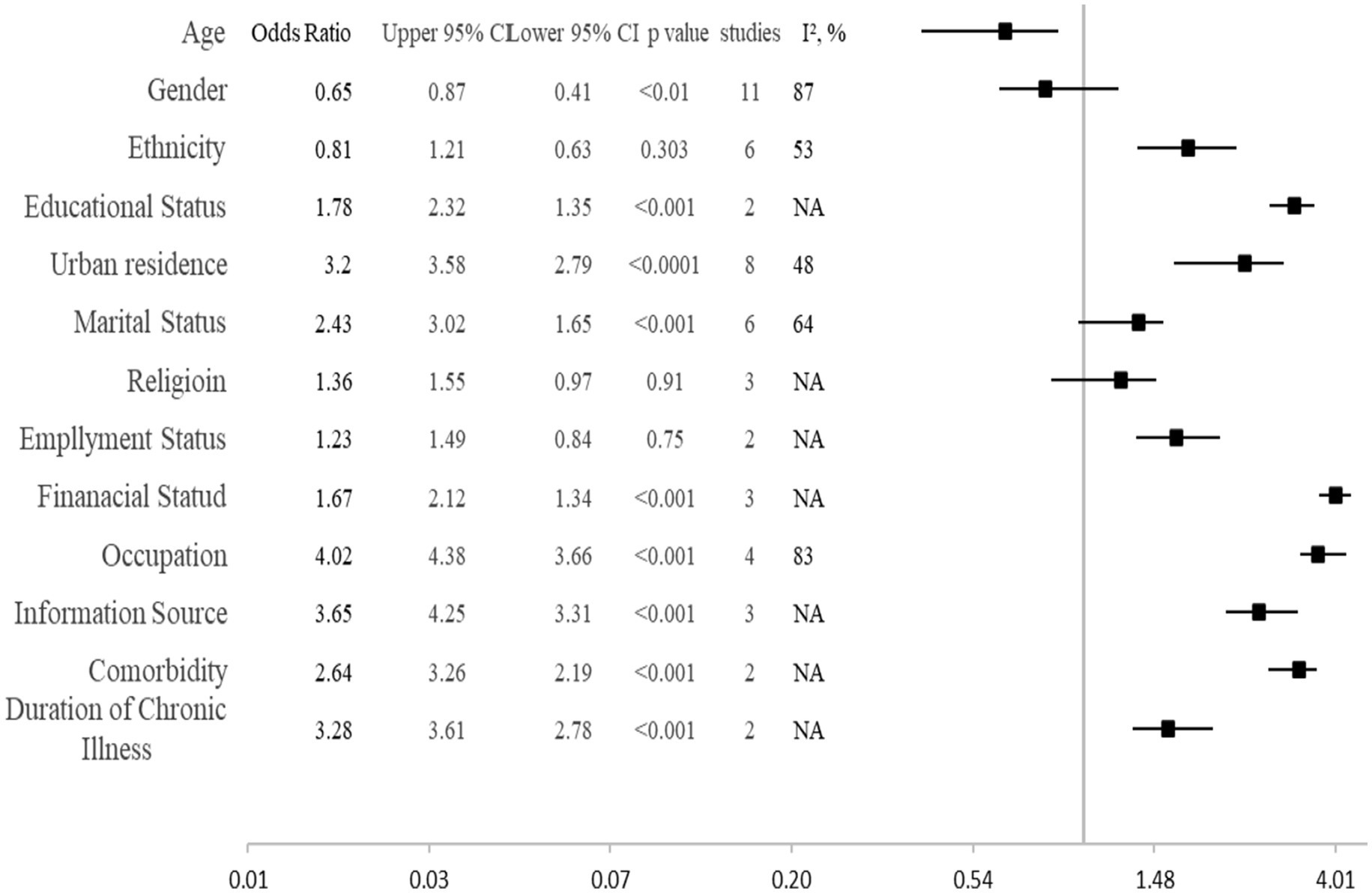
Figure 5. Factors affecting the knowledge, attitude, and preventive practices to manage the COVID-19 in presence of comorbidity.
Discussion
We recognized a limited body of evidence determining the pattern and associated factors of COVID-19 knowledge, attitude, and practice among comorbid COVID-19 patients. Our results showed good knowledge, a positive attitude and good practice to manage COVID-19 in the presence of comorbidity. In addition, good knowledge, positive attitude and good practice were related to age, ethnicity, educational status, urban residence, employment status, financial status, occupation, information Source, comorbidity and duration of chronic illness. Age was reported as an important factor in 11 studies, educational status in eight studies, urban residence and gender in six studies, financial status in four studies, employment status, marital status and occupation in three studies and ethnicity, religion, information source, comorbidity and duration of chronic illness in two studies each.
Adequate knowledge and awareness of preventive strategies are important to manage COVID-19 in comorbid patients (41). Our results showed good knowledge about COVID-19 in 65% of the COVID-19 comorbid patients. Most of the patients were aware of the symptoms of COVID-19 including dyspnea, sore throat, fever, chills, and associated risks due to the comorbid conditions. Cancer patients and diabetes patients’ cardiovascular patients were able to distinguish the COVID-19 symptoms and their respective disease symptoms. Our results are in line with the previous research that shows higher knowledge about COVID-19 management in comorbid patients (35, 36). This may be due to the fact chronic disease patients are in regular contact with healthcare professionals due to their disease condition. Frequent contact with healthcare providers and discussions may improve their knowledge of the pandemic COVID-19.
In our results, 57% of the comorbid patients showed a positive attitude to managing COVID-19 and associated comorbidity. Most of the patients knew COVID-19 may cause more harmful effects in the presence of their disease. Cancer patients believe that COVID-19 increases the risk of mortality so they must adopt extra preventive measures to avoid COVID-19 exposure. Diabetic patients think that they need to manage their diet and physical activity to improve immunity against COVID-19. Our results are in line with the previous literature which shows a positive attitude of 58 and 47% of hypertension and diabetic patients, respectively, toward COVID-19 management (31, 32). Usually, chronic disease patients have better disease management knowledge as compared to healthy people (42–44). So, most of them believe that government policies and restrictions to prevent COVID-19 are for the benefit of the people and can control the pandemic.
Overall, published articles showed the constructive attitude of the participants about COVID-19, which is consistent with the findings of the study conducted in Indonesia (96%) (45). It could be due to better health policies and knowledge about the disease. However, the study done in Northern Ethiopia revealed that 40.5% of the included participants showed a negative attitude towards the prevention of COVID-19 (30). The possible reason for negative attitudes can be poor knowledge about the disease and the unfamiliar nature of COVID-19. Our finding demonstrated that a substantial part of the comorbid patients were concerned about the probability of COVID-19 infection and mortality due to infection. These findings were consistent with those in the Philippines and the United States (8, 46).
Regarding practice, in most studies, participants adopted regular measures to prevent COVID-19 disease. In pooled analysis, 57% of comorbid patients adopted preventive measures to avoid COVID-19. Diabetic patients believe regular physical activity is necessary for them to manage diabetes but they must avoid parks and crowded places to avoid COVID-19 exposure. Comorbid patients need to visit the pharmacy regularly to refill prescriptions or take insulin. Most of the comorbid patients left their houses to visit pharmacies. Policies to provide insulin and other medicines at doorsteps can reduce pharmacy visits and further improve preventive practices in comorbid patients.
This systematic review revealed several factors associated with KAP towards COVID-19 among participants including age, ethnicity, educational status, urban residence, employment status, financial status, occupation, information Source, comorbidity and duration of chronic illness. Younger age was associated with better KAP toward COVID-19 than older age. Different studies reported that people younger than 40 years had better knowledge and positive attitudes toward the management of their disease (16). This may be because young people are more frequent users of social media and adopt change easily. Social media is a key source of information these days. So, this may be the reason for better COVID-19-related KAP in young people. Occupation, financial status and education were also reported as significant factors to impact KAP in comorbid COVID-19 patients in previous research. Studies conducted in Ethiopia, India and Egypt reported occupation, financial status and education as contributing factors to the impact of KAP in comorbid COVID-19 patients (12, 30, 47). Comorbidity and duration of chronic illness were also associated with better KAP in comorbid COVID-19 patients. With an increase in the duration of disease self-management practice and knowledge improve. Research shows that compliance increases with the duration of chronic disease. Thus, with the increased duration of the disease, people may become more conscious of the management of a disease.
Higher heterogeneity was reported among COVID-19 KAP studies. The higher heterogeneity may be due to due to variations in illness manifestation, characteristics of the population being studied, and the methodologies employed in the research (48, 49). The diverse demographics of these research participants, regional variations in healthcare systems, environmental variables, population genetics demographic factors, comorbidities, and the varying severity of COVID-19 lead to heterogeneity. Diagnostic and testing methods are also a factor in the diversity. Heterogeneity can also be caused by variations in study design and methodologies (26, 27). The quality of data and the outcomes obtained differ depending on the type of study conducted, such as observational studies, randomised controlled trials, retrospective studies, or prospective studies. The variety of findings is influenced by the variations in data collection procedures, duration of follow-up, and outcome measures. Study outcomes are also influenced by epidemiological factors such as pandemic waves and new variants that have varying levels of transmissibility and pathogenicity (22, 38, 42).
Notwithstanding its robustness, this study has few limitations. Most of the research conducted took place during the epidemic and primarily consisted of online or telephonic questionnaires. Consequently, individuals lacking access to these amenities may have been deprived of participation. The presence of diverse methods resulted in increased heterogeneity in the studies. Furthermore, the exclusion of grey literature, which was not included in this study due to the availability of sufficient peer-reviewed data, may potentially lead to the omission of certain information. Despite a few limitations, this study has several strengths. The study identified a significant portion of the accessible data and yielded valuable insights into the Knowledge, Attitudes, and Practices (KAP) regarding COVID-19 among individuals with comorbidities. To the best of the author’s knowledge, this study was the first systematic review and meta-analysis to evaluate knowledge attitudes and practices towards COVID-19 and its associated factors in comorbid patients. The anticipated outcomes of the study are expected to bring attention to areas of research that have not been well addressed. This information will be valuable for health professionals in making informed decisions and for developing policies and programs that are specifically targeted at addressing these gaps. The findings have the potential to enhance our understanding of the impact of the pandemic on individuals with chronic diseases, in terms of their knowledge, attitudes, and practices (KAP). Consequently, this could potentially contribute to the enhancement of patient safety and the provision of high-quality care, while also mitigating the transmission of COVID-19 among individuals at a heightened risk.
The COVID-19 pandemic has highlighted the importance of prioritizing vulnerable populations, particularly those with chronic conditions. Millions have died due to inadequate preparedness and responses. In addition to the implementation of efficacious solutions for the prevention and treatment of disease, a positive attitude and practice of the population to adopt preventive measures is also important. Our research shows that by giving priority to vulnerable groups, such as individuals with other chronic illnesses, it is possible to implement focused interventions, enhance access to crucial healthcare services, and implement public health policies (50). Implementation of effective strategies to improve knowledge, including information sources, targeted information, and enhanced telecommunication contact with healthcare providers can improve the attitude of comorbid patients toward the pandemic control. Moreover, media partnerships, digital educational materials, online medicine refills, extended medical supply distribution, hotlines, health protocols, and home visits can be effective in protecting individuals and maintaining care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
AR: Conceptualization, Formal analysis, Supervision, Writing – original draft. ZT: Supervision, Writing – review & editing. SM: Software, Writing – review & editing. MFR: Writing – review & editing. SS: Writing – review & editing. GJ: Formal analysis, Writing – review & editing. SA: Formal analysis, Writing – review & editing. LO: Writing – review & editing. YK: Writing – review & editing. SaA: Writing – review & editing. SSA: Writing – review & editing. SK: Writing – review & editing. RA: Writing – review & editing. MH: Writing – review & editing. AA: Writing – review & editing. ME: Writing – review & editing, Resources. AH: Writing – review & editing.
Funding
The author(s) declare no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors are very grateful to the teaching faculty of the Department of Pharmacy Practice, Bahauddin Zakariya University Multan, who gave their valuable feedback on the systematic review and to the library staff for searching and requesting the full-text articles from the authors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wu, F, Zhao, S, Yu, B, Chen, YM, Wang, W, Song, ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. (2020) 579:265–9. doi: 10.1038/s41586-020-2008-3
2. World Health Organization The true death toll of COVID-19: Estimating global excess mortality. (2022) Available at: https://www.who.int/data/stories/the-true-death-toll-of-covid-19-estimating-global-excess-mortality
3. World Health Organization. World Health Organization coronavirus disease (COVID-19) dashboard. Geneva: World Health Organization (2020).
4. Tang, D, Tou, J, Wang, J, Chen, Q, Wang, W, Huang, J, et al. Prevention and control strategies for emergency, limited-term, and elective operations in pediatric surgery during the epidemic period of COVID-19. World. J Pediatr Surg. (2020) 3:122. doi: 10.1136/wjps-2020-000122
5. Ejaz, H, Alsrhani, A, Zafar, A, Javed, H, Junaid, K, Abdalla, AE, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. (2020) 13:1833–9. doi: 10.1016/j.jiph.2020.07.014
6. Barone, MTU, Ngongo, B, Harnik, SB, de Oliveira, LX, Végh, D, de Luca, PV, et al. COVID-19 associated with diabetes and other noncommunicable diseases led to a global health crisis. Diabetes Res Clin Pract. (2021) 171:108587. doi: 10.1016/j.diabres.2020.108587
7. Oraibi, O, Alamer, A, Zogel, B, Hakami, F, Hakami, K, Gadi, W, et al. Impact of COVID-19 on patients with diabetes standard of Care in the Jazan Region, Saudi Arabia. Mater Sociomed. (2022) 34:272–7. doi: 10.5455/msm.2022.34.272-277
8. Wolf, MS, Serper, M, Opsasnick, L, O'Conor, RM, Curtis, L, Benavente, JY, et al. Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the U.S. outbreak. Ann Intern Med. (2020) 173:100–9. doi: 10.7326/M20-1239
9. Guan, WJ, Ni, ZY, Hu, Y, Liang, WH, Ou, CQ, He, JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
10. Huang, S, Wang, J, Liu, F, Liu, J, Cao, G, Yang, C, et al. COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res. (2020) 43:824–31. doi: 10.1038/s41440-020-0485-2
11. Wang, D, Hu, B, Hu, C, Zhu, F, Liu, X, Zhang, J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
12. Saeed, S, Awasthi, AA, Nandi, D, Kaur, K, Hasan, S, Janardhanan, R, et al. Knowledge, attitude and practice towards COVID-19 among individuals with associated comorbidities. J Med Life. (2021) 14:225–37. doi: 10.25122/jml-2020-0184
13. Addis, SG, Nega, AD, and Miretu, DG. Knowledge, attitude and practice of patients with chronic diseases towards COVID-19 pandemic in Dessie town hospitals, Northeast Ethiopia. Diabetes Metab Syndr Clin Res Rev. (2021) 15:847–56. doi: 10.1016/j.dsx.2021.03.033
14. Lin, L, Savoia, E, Agboola, F, and Viswanath, K. What have we learned about communication inequalities during the H1N1 pandemic: a systematic review of the literature. J BMC public health. (2014) 14:1–13. doi: 10.1186/1471-2458-14-484
15. Magnani, JW, Mujahid, MS, Aronow, HD, Cené, CW, Dickson, VV, Havranek, E, et al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. (2018) 138:e48–74. doi: 10.1161/CIR.0000000000000579
16. Pal, R, Yadav, U, Grover, S, Saboo, B, Verma, A, Bhadada, SK, et al. Knowledge, attitudes and practices towards COVID-19 among young adults with type 1 diabetes mellitus amid the nationwide lockdown in India: a cross-sectional survey. Diabetes Res Clin Pract. (2020) 166:108344. doi: 10.1016/j.diabres.2020.108344
17. Gheorghe, A, Negru, Ş, Nițipir, C, Mazilu, L, Marinca, M, Gafton, B, et al. Knowledge, attitudes and practices related to the COVID-19 outbreak among Romanian adults with cancer: a cross-sectional national survey. Ann Oncol. (2021) 6:100027. doi: 10.1016/j.esmoop.2020.100027
18. Akalu, Y, Ayelign, B, and Molla, MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen hospital Northwest Ethiopia. Infect Drug Resist. (2020) 13:1949–60. doi: 10.2147/IDR.S258736
19. Raquib, A, Raquib, R, Jamil, S, Hossain, A, al-Mamun, F, and Mamun, MA. Knowledge, attitudes, and practices toward the prevention of COVID-19 in Bangladesh: a systematic review and Meta-analysis. Front Med. (2022) 9:856156. doi: 10.3389/fmed.2022.856156
20. Bekele, F, Sheleme, T, Fekadu, G, and Bekele, K. Patterns and associated factors of COVID-19 knowledge, attitude, and practice among general population and health care workers: a systematic review. SAGE Open Med. (2020) 8:205031212097072. doi: 10.1177/2050312120970721
21. Saadatjoo, S, Miri, M, Hassanipour, S, Ameri, H, and Arab-Zozani, MJPH. Knowledge, attitudes, and practices of the general population about coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis with policy recommendations. Public Health. (2021) 194:185–95. doi: 10.1016/j.puhe.2021.03.005
22. Rahman, MM, Marzo, RR, Chowdhury, S, Qalati, SA, Hasan, MN, Paul, GK, et al. Knowledge, attitude and practices toward coronavirus disease (COVID-19) in southeast and South Asia: a mixed study design approach. J Front Public Health. (2022) 10:875727. doi: 10.3389/fpubh.2022.875727
23. Sarria-Guzmán, Y, Fusaro, C, Bernal, JE, Mosso-González, C, González-Jiménez, FE, and Serrano-Silva, N. Knowledge, attitude and practices (KAP) towards COVID-19 pandemic in America: a preliminary systematic review. JIDC. (2021) 15:9–21. doi: 10.3855/jidc.14388
24. Azene, AG, Workie, MS, and Aragaw, AMJCTR. Knowledge, attitude, and prevention practices toward coronavirus disease 2019 in Ethiopia: a systematic review and Meta-analysis. Curr Ther Res Clin Exp. (2021) 94:100633. doi: 10.1016/j.curtheres.2021.100633
25. Liberati, A, Altman, DG, Tetzlaff, J, Mulrow, C, Gøtzsche, PC, Ioannidis, JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. doi: 10.1371/journal.pmed.1000100
26. Anees Ur, R, Ahmad Hassali, MA, Muhammad, SA, Shah, S, Abbas, S, Hyder Ali, IAB, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in the USA, Europe, and Asia: results from a systematic review of the literature. Expert Rev Pharmacoecon Outcomes Res. (2020) 20:661–72. doi: 10.1080/14737167.2020.1678385
27. Rehman, A, Hassali, MAA, Muhammad, SA, Harun, SN, Shah, S, and Abbas, S. The economic burden of chronic obstructive pulmonary disease (COPD) in Europe: results from a systematic review of the literature. Eur J Health Econ. (2020) 21:181–94. doi: 10.1007/s10198-019-01119-1
28. Downes, MJ, Brennan, ML, Williams, HC, and Dean, RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. (2016) 6:e011458. doi: 10.1136/bmjopen-2016-011458
29. Taye, GM, Bose, L, Beressa, TB, Tefera, GM, Mosisa, B, Dinsa, H, et al. COVID-19 knowledge, attitudes, and prevention practices among people with hypertension and diabetes mellitus attending public health facilities in ambo Ethiopia. Infect Drug Resist. (2020) 13:4203–14. doi: 10.2147/IDR.S283999
30. Iyasu, A, Kidanu, BH, and Zereabruk, K. Knowledge, attitude, and practice towards COVID-19 among chronic disease patients at Aksum hospital, northern Ethiopia, 2020: a cross-sectional study. Asthma Res Pract. (2021) 7:1–9. doi: 10.1186/s40733-021-00074-0
31. Geleta, TA, Deriba, BS, and Jemal, KJ. Evaluation of the knowledge, attitude, and practice of COVID-19 prevention methods among hypertensive patients in North Shoa, Ethiopia. Risk Manag Healthc Policy. (2022) 15:457–71. doi: 10.2147/RMHP.S347105
32. Legese, YM, Gebru, SB, Gebremariam, AG, and Tesfay, ZAJH. Knowledge, attitude, and practice towards COVID-19 among chronic disease patients visiting public hospitals. Heliyon. (2023) 9:e17734. doi: 10.1016/j.heliyon.2023.e17734
33. Adella, GA, Abebe, K, Atnafu, N, Azeze, GA, Alene, T, Molla, S, et al. Knowledge, attitude, and intention to accept COVID-19 vaccine among patients with chronic diseases in southern Ethiopia: multi-center study. Front Public Health. (2022) 10:917925. doi: 10.3389/fpubh.2022.917925
34. Rajan, S, Paton, LW, Chowdhury, AH, Zavala, GA, Aslam, F, Huque, R, et al. Knowledge and response to the COVID-19 pandemic in people with severe mental illness in Bangladesh and Pakistan: a cross-sectional survey. Front Psych. (2022) 13:785059. doi: 10.3389/fpsyt.2022.785059
35. Khattak, S, Faheem, M, Nawaz, B, Khan, M, Khan, NH, Ullah, N, et al. Knowledge, attitude, and perception of Cancer patients towards COVID-19 in Pakistan: a cross-sectional study. IJERPH. (2022) 19:7926. doi: 10.3390/ijerph19137926
36. Alsaleh, FM, Elzain, M, Alsairafi, ZK, and Naser, AY. Perceived knowledge, attitude, and practices (KAP) and fear toward COVID-19 among patients with diabetes attending primary healthcare centers in Kuwait. IJERPH. (2023) 20:369. doi: 10.3390/ijerph20032369
37. Subyani, AA, Fadel, HA, Bokhary, A, Ghunaim, AM, Alharbi, HH, Alghamdi, KA, et al. Knowledge, attitudes, and practices of COVID-19 safety measures among type 1 diabetes mellitus patients at king Abdulaziz university hospital: a cross-sectional study. Cureus. (2022) 14:e27713. doi: 10.7759/cureus.27713
38. Mohamadian, H, faraji, A, Ghorrabi, AT, Ghobadi-Dashdebi, K, and Salahshouri, A. The COVID-19 pandemic: knowledge, attitudes and practices of coronavirus (COVID-19) among patients with type 2 diabetes. J Diarrhoeal Dis Res. (2023) 42:11. doi: 10.1186/s41043-023-00349-7
39. Jasim Alsadaji, A, Zendeh Talab, HR, Jasim Mohammed, Z, and HJMEB, BV. Comparison of knowledge, attitude, and practice of patients with chronic diseases referred to clinics affiliated with Iranian and Iraqi teaching hospitals regarding COVID-19. Med Edu Bull. (2021) 2:263–74. doi: 10.22034/MEB.2021.312860.1035
40. Iradukunda, PG, Pierre, G, Muhozi, V, Denhere, K, and Dzinamarira, T. Knowledge, attitude, and practice towards COVID-19 among people living with HIV/AIDS in Kigali, Rwanda. J Community Health. (2021) 46:245–50. doi: 10.1007/s10900-020-00938-1
41. Erfani, A, Shahriarirad, R, Ranjbar, K, Mirahmadizadeh, A, and Moghadami, M. Knowledge, attitude and practice toward the novel coronavirus (COVID-19) outbreak: a population-based survey in Iran. Bull World Health Organ. (2020) 30:2471.
42. Rehman, A, Shah, S, Abbas, G, Harun, SN, Shakeel, S, Hussain, R, et al. Assessment of risk factors responsible for rapid deterioration of lung function over a period of one year in patients with chronic obstructive pulmonary disease. Sci Rep. (2021) 11:92968. doi: 10.1038/s41598-021-92968-5
43. Rasool, MF, Rehman, AU, Imran, I, Abbas, S, Shah, S, Abbas, G, et al. Risk factors associated with medication errors among patients suffering from chronic disorders. Front Public Health. (2020) 8:531038. doi: 10.3389/fpubh.2020.531038
44. Rasool, MF, Rehman, A, Khan, I, Latif, M, Ahmad, I, Shakeel, S, et al. Assessment of risk factors associated with potential drug-drug interactions among patients suffering from chronic disorders. PLoS One. (2023) 18:e0276277. doi: 10.1371/journal.pone.0276277
45. Sari, DK, Amelia, R, Dharmajaya, R, Sari, LM, and Fitri, NK. Positive correlation between general public knowledge and attitudes regarding COVID-19 outbreak 1 month after first cases reported in Indonesia. J Community Health. (2021) 46:182–9. doi: 10.1007/s10900-020-00866-0
46. Lau, LL, Hung, N, Go, DJ, Ferma, J, Choi, M, Dodd, W, et al. Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: a cross-sectional study. J Glob Health. (2020) 10:1007. doi: 10.7189/jogh.10.011007
47. Kebede, Y, Yitayih, Y, Birhanu, Z, Mekonen, S, and Ambelu, A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS One. (2020) 15:e0233744. doi: 10.1371/journal.pone.0233744
48. Khattak, M, Rehman, A, Muqaddas, T, Hussain, R, Rasool, MF, Saleem, Z, et al. Tuberculosis (TB) treatment challenges in TB-diabetes comorbid patients: a systematic review and meta-analysis. J Ann Med. (2024) 56:683. doi: 10.1080/07853890.2024.2313683
49. Rehman, A, Khattak, M, Mushtaq, U, Latif, M, Ahmad, I, Rasool, MF, et al. The impact of diabetes mellitus on the emergence of multi-drug resistant tuberculosis and treatment failure in TB-diabetes comorbid patients: a systematic review and meta-analysis. J Front Public Health. (2023) 11:1244450. doi: 10.3389/fpubh.2023.1244450
Keywords: knowledge, attitude, practice, KAP, hypertension, chronic illness, comorbidity, COVID-19
Citation: Rehman Au, Tasleem Z, Muhammad SA, Rasool MF, Shah S, Jabeen G, Arif S, Omar Babkair LS, Kadumi YJ, Alghamdi S, Almarzoky Abuhussain SS, Khayyat SM, Alharthi RHH, Hossain MA, Abbas AA, Elrggal ME and Haseeb A (2024) Pattern and associated factors of COVID-19 knowledge, attitude and practice (KAP) among COVID-19-comorbid patients: a systematic review and meta-analysis. Front. Public Health. 12:1365744. doi: 10.3389/fpubh.2024.1365744
Edited by:
Nyi Nyi Naing, Sultan Zainal Abidin University, MalaysiaReviewed by:
Pragya Sharma, Maulana Azad medical College, IndiaAndrew Omame, Federal University of Technology Owerri, Nigeria
Rizaldy Taslim Pinzon, Duta Wacana Christian University, Indonesia
Dafeng Liu, Public Health and Clinical Center of Chengdu, China
Copyright © 2024 Rehman, Tasleem, Muhammad, Rasool, Shah, Jabeen, Arif, Omar Babkair, Kadumi, Alghamdi, Almarzoky Abuhussain, Khayyat, Alharthi, Hossain, Abbas, Elrggal and Haseeb. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anees ur Rehman, YW5lZXN1cnJlaG1hbkBienUuZWR1LnBr; YW5lZXN1cnJlaG1hbnI5MEBnbWFpbC5jb20=; Zermina Tasleem, emVybWluYXRhc2xlZW1AYnp1LmVkdS5waw==
 Anees ur Rehman
Anees ur Rehman Zermina Tasleem2*
Zermina Tasleem2* Muhammad Fawad Rasool
Muhammad Fawad Rasool Yahya Jaber Kadumi
Yahya Jaber Kadumi Saleh Alghamdi
Saleh Alghamdi Safa S. Almarzoky Abuhussain
Safa S. Almarzoky Abuhussain Raed Hamed Hilal Alharthi
Raed Hamed Hilal Alharthi Asma A. Abbas
Asma A. Abbas Mahmoud Essam Elrggal
Mahmoud Essam Elrggal Abdul Haseeb
Abdul Haseeb