- 1Department of Pediatrics, Yale University, New Haven, CT, United States
- 2Department of Medicine, Harvey Cushing/John Hay Whitney Medical Library, New Haven, CT, United States
- 3University of North Carolina at Greensboro, Greensboro, NC, United States
- 4Department of Epidemiology of Microbial Diseases, Yale School of Public Health, New Haven, CT, United States
Introduction: Point-of-Care Tests (POCTs) are utilized daily in resource abundant regions, however, are limited in the global south, particularly in the prehospital setting. Few studies exist on the use of non-malarial POCTs by Community Health Workers (CHWs). The purpose of this scoping review is to delineate the current diversity in and breadth of POCTs evaluated in the prehospital setting.
Methods: A medical subject heading (MeSH) analysis of known key articles was done by an experienced medical librarian and scoping searches were performed in each database to capture “point of care testing” and “community health workers.” This review was guided by the PRISMA Extension for scoping reviews.
Results: 2735 publications were returned, 185 were nominated for full-text review, and 110 studies were confirmed to meet study criteria. Majority focused on malaria (74/110; 67%) or HIV (25/110; 23%); 9/110 (8%) described other tests administered. Results from this review demonstrate a broad geographic range with significant heterogeneity in terminology for local CHWs.
Conclusion: The use of new POCTs is on the rise and may improve early risk stratification in limited resource settings. Current evidence from decades of malaria POCTs can guide future implementation strategies.
1 Introduction
The use of point-of-care tests (POCT) in the healthcare setting has exponentially advanced in the last decade given the number of novel biomarkers discovered with potential clinical significance (1–4). Advanced POCTs are utilized daily in resource abundant regions, however, are limited in the global south, particularly in the prehospital setting (1, 2, 5). Community health worker (CHW) programs often employ POCTs for rapid malaria diagnosis, however, there are few studies on the use of other non-malarial POCTs by CHWs (5–8). Additionally, although various training curricula and methods exist, no standardized evaluation process to assess POCT competency has been published.
CHWs are traditionally community members without formal training in healthcare who serve as appointed health representatives for frontline community health concerns, including emergencies (5, 9, 10). Heterogeneity between the definitions and roles of CHWs exists across the globe; CHWs are often trained to meet specific community health needs of a local population, and in low-and middle-income countries (LMIC) serve as the liaison between village and clinic (5, 9, 10). This is critical in LMICs, where it is common to have fewer than 1 physician per 100,000 residents (10, 11). Some programs have standardized the role of CHWs for subsets of patients; for example, the World Health Organization and United Nations Children’s Fund recommended the deployment of integrated community case management (iCCM) programs in 2004 that focus on prehospital evaluation and management of sick children (6–8). A component of the iCCM is the prehospital diagnosis of malaria using a rapid diagnostic test (RDT). Programs such as the iCCM bring training to CHWs and expand early access to emergency triage and treatment to extremely rural regions across the world (6–8). These regions typically have the highest pediatric and maternal mortality rates (6–8).
mHealth, a form of electronic health (eHealth) that uses portable technology such as cellular phones and tablet computers, is one method used to disseminate public health education in limited resource settings (12–15). Pedagogically, mHealth can combine multiple learning styles and apply innovative forms of education tailored to specific populations (14–17). Further, mHealth empowers its users and can harness the power of technology to provide culturally tailored and linguistically appropriate health education to rural communities (16, 17). Historically, mHealth has been underutilized due to the infrastructure required to purchase, connect, and maintain portable devices; however, over the last decade its cost has dropped significantly concurrent with the development of infrastructure for electricity, cellular service, and internet (14, 15). mHealth applications can provide more than innovative forms of education. Step-by-step algorithms for clinical decision management with POCTs have been developed with mHealth, applying current standard of care guidelines for various diseases (14–17). For example, an application can guide its users to input cardiovascular risk data points and serve as a screening tool for patients (16, 17). This can be expanded and tailored to community health workers in LMICs, where both chronic and neglected tropical diseases significantly impact healthy living (16, 17).
Similarly, medical technological advances that leapfrog from well-resourced industrial networks to low health resource settings hold the capacity to transform healthcare systems in LMICs (1–3, 16–18). For example, the development of portable ultrasound technology to identify high risk deliveries in rural villages exemplifies how technology can help decrease health disparity (18, 19). This allows a population’s socioeconomic status to improve by reducing unnecessary death and disability. POCTs are no different. A POCT is a test that can be completed at the patient’s bedside with nearly immediate results, all of which implies advanced portability (1, 2). With POCTs, the early diagnosis of serious illness improves triage decision-making and early treatment of infectious diseases (1–3). Malaria is a prime example. The clinical utility in detecting prehospital malaria with a rapid diagnostic test (RDT), a POCT, allows for prehospital providers to initiate life-saving treatment in their communities (6–8). Given the lack of health resources and potential impact of advancing POCTs in LMICs, this review will outline the current diversity in and breadth of POCTs that have been evaluated in the prehospital setting.
2 Methods
2.1 Search strategy
An experienced medical librarian (MCF) was consulted on methodology. A medical subject heading (MeSH) analysis [mesh.med.yale.edu] of known key articles was completed and scoping searches performed in each database. An iterative process was used to translate and refine searches. To maximize sensitivity, the formal search used controlled vocabulary terms and synonymous free-text words to capture the concepts of “point of care testing” and “community health workers.” The search strategy was peer reviewed by a second librarian, not otherwise associated with the project, using the PRESS standard (20). This scoping review is informed by the framework described by the Joanna Briggs Institute (JBI) (21). In addition, the reporting of this scoping review was guided by the PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation (22).
On June 21, 2022, the librarian performed a comprehensive search of multiple databases: MEDLINE, Embase, PsycInfo, Global Health, CINAHL, Web of Science, and Cochrane. To capture recently published articles, a second database search was repeated on September 13, 2023. No date or language limits were imposed on the search. All search strategies are included in Supplementary material. The final search retrieved a total of 2,735 results which were pooled in EndNote 201 and de-duplicated using the Yale Reference Deduplicator [library.medicine.yale.edu/reference-deduplicator]. This set was uploaded to Covidence2 for screening.
2.2 Inclusion/exclusion criterion
Articles were included if POCTs were administered:
• in the prehospital/clinic setting
• by an individual in the same community
Participants may work both in a healthcare setting and as a community health worker; but must be providing POCT at the community level for inclusion. No age or gender was excluded. The overarching concept of interest for this scoping review is POCTs administered by community health workers in out of hospital environments for any medical purposes.
2.3 Selection of sources of evidence
Two screeners independently reviewed the titles, abstracts and full text of the eligible articles that met inclusion criteria. Any conflicts were resolved through consensus.
3 Results
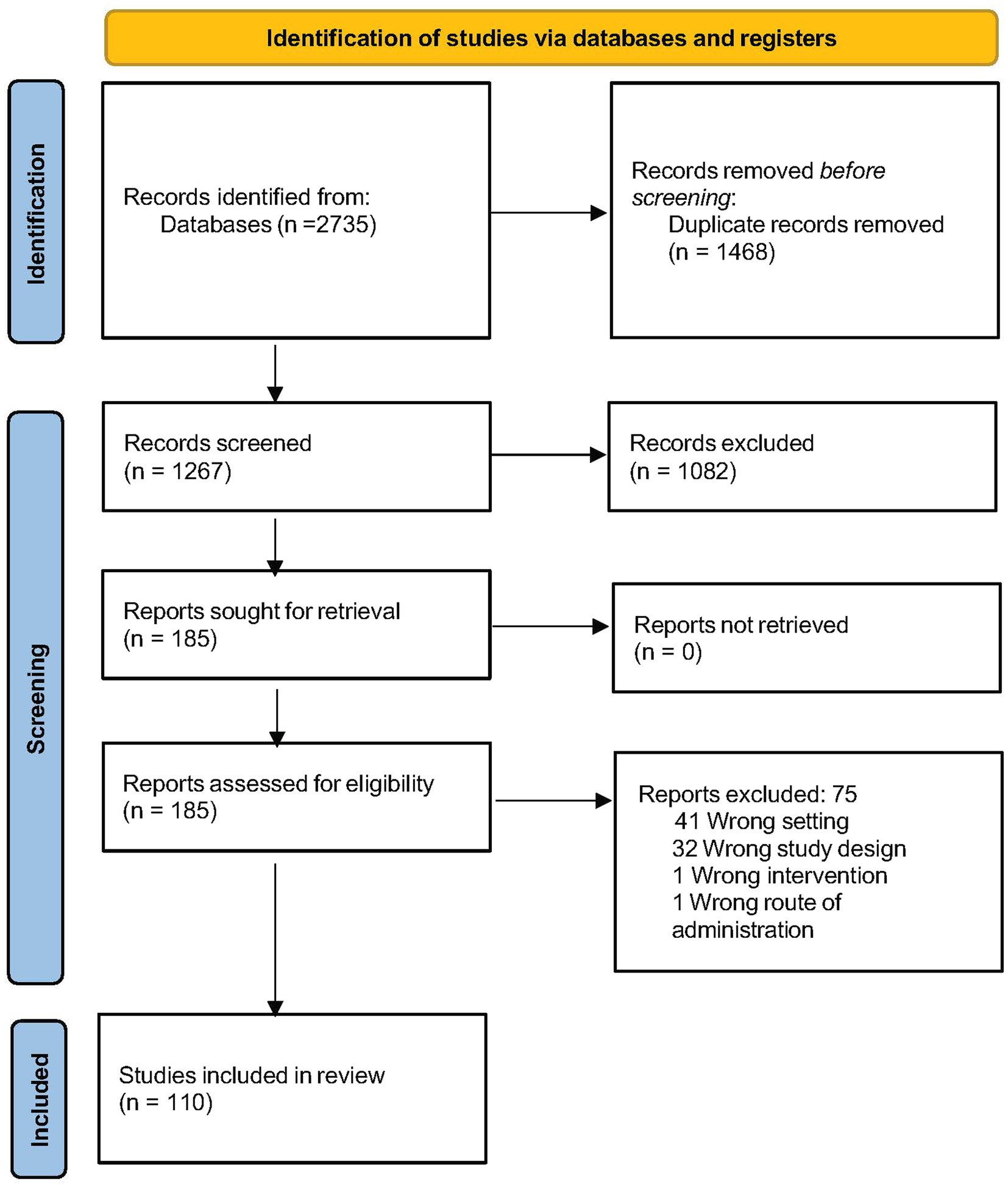
Queries across multiple data bases returned 2,735 publications, of which 1,468 were duplicates. After a two-stage screening process, 185 potentially relevant articles were nominated for full-text review, after which 110 studies were confirmed to meet study criteria and underwent qualitative analysis (Flow Chart in Figure 1) (16, 24–133).
3.1 Heterogeneity in language used for the point-of-care test administrator
Among the included studies, there were various names used to refer to non-medical professionals trained to employ POCTs in the pre-hospital setting. Over 50% of included studies used the terminology “Community Health Worker,” with a smaller but substantial minority of studies using other terms, including Village Health Worker (VHW), Village Malaria Worker (VMW), Peers, Lay Health Provider, Lay Health Worker, and Community Health Volunteer.
3.2 Types of point-of-care tests employed
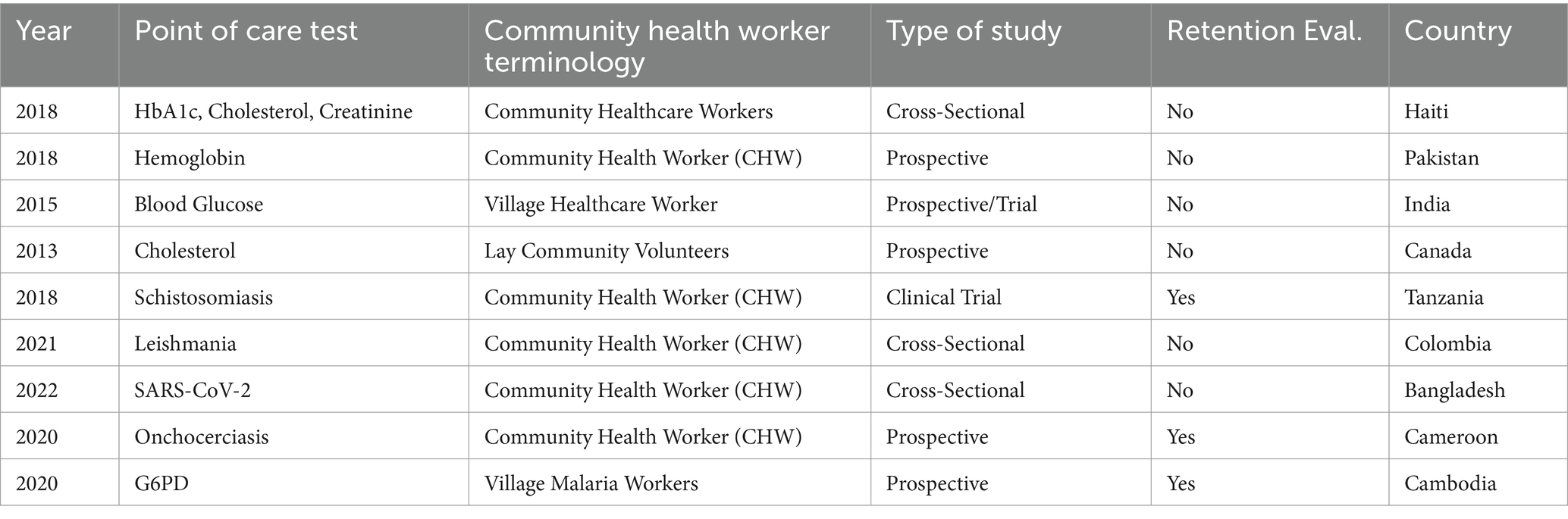
Ninety-nine of the 110 POCTs utilized in the included studies tested for malaria and HIV. Of the POCTs designated as “other,” these included the routine health markers blood glucose, hemoglobin A1c, cholesterol, and hemoglobin, as well as diagnostics for infectious pathogens such as Loa Loa, Schistosomes, SARS-COV-2 and Leishmania (37, 43, 47, 74, 83, 92, 107, 109). Additionally, one abstract evaluated the use of G6PD as a POCT (100). All 9 articles for ‘other’ POCTs were published in the last 10 years, with four in the last 3 years (Table 1). Three articles explicitly described skill retention for the POCT as followed over a set time-period.
3.2.1 Routine health marker POCTs
Degennaro et al. evaluated the community diagnosis of non-communicable diseases, specifically the prevalence of chronic kidney disease, hyperlipidemia, and diabetes among communities in rural and urban Haiti (43). This is a unique, cross-sectional study that demonstrates prevalence of common non-communicable diseases and the successful application of community-based screening via CHWs. The article described a one-week training for the CHWs and limited details on the use of the POCTs which required a finger-stick blood sample.
McCormack et al. trained CHWs to obtain hemoglobin POCTs among a rural mountain community in Pakistan (47). CHWs diagnosed and treated community members who met the diagnostic criteria for anemia. After 8 weeks, repeat hemoglobin levels were obtained via POCTs to evaluate their intervention (education, mebendazole, oral iron). This study found a significant baseline prevalence of anemia among women (53%) and children (47%), as well as a significant reduction in anemia post-intervention.
Raghu et al. developed and piloted SMARTHealth, a mobile point-of-care clinical decision support tool in rural India, designed to facilitate the identification and management of cardiovascular disease in regions with limited health resources (107). This pilot study included the point-of-care measurement of blood glucose by Village Healthcare Workers via capillary puncture. This pilot was subsequently expanded to a stepped-wedge cluster randomized clinical trial that included blood glucose POCTs administered by Village Healthcare Workers.
Jones et al. evaluated cardiovascular risk factors in a high-risk group of South Asian Canadians in Calgary managed by lay community volunteers and applied community based participatory methodology (92). Lay community volunteers completed cardiovascular health assessments that included prehospital point-of-care cholesterol screening. Unique to this study is the screening sites, which were local religious facilities; additionally, this is the only non-HIV, non-malaria, ‘other’ prehospital POCT published in North America.
3.2.2 Infectious disease POCT
Mazigo et al. introduced the first published prehospital POCT for diagnosing a trematode parasitic infection, Schistosomiasis, via circulating cathodic antigen (74). This cluster community randomized clinical trial proposes an alternate to mass drug administration for Schistosomiasis: a diagnostic test first and treat if recommended approach. This is a clinical trial protocol and data from this clinical trial is yet to be published.
Cossio et al. completed the first study evaluating the early, ‘community’ diagnosis of cutaneous leishmaniasis in Colombia via a method they developed, Isothermal Recombinase Polymerase Amplification targeting Leishmania kinetoplast DNA combined with lateral flow immunochromatography (109). A reference laboratory reviewed all samples and were blinded to prehospital results. Study findings demonstrated similar accuracy in diagnosis and highlighted the feasibility of this test to be conducted by CHWs in a community setting.
Sania et al. trained CHWs to complete SARS-COV-2 rapid antigen testing via nasal/saliva swabs in low-income communities near Dhaka, Bangladesh (37). This timely cross-sectional study addressed barriers to access to care by bringing testing directly to communities and their families via CHWs. The authors noted that by introducing CHWs for POCT administration, testing of symptomatic patients with concern for SARS-COV-2 increased fourfold. Notably, nasal swabs demonstrated higher accuracy than saliva samples.
Pion et al. published the first prehospital POCT to evaluate parasite load (concentration of microfilariae) prior to onchocerciasis treatment (83). Given that adverse events typically occur with high levels of microfilaremia (>20,000 per ml), the authors described the use of a novel tool to detect prehospital concentrations prior to treatment: the LoaScope. This study concluded that for individuals with previous microfilariae concentrations <20,000 per ml, and treated with ivermectin, retesting is not required given minimal risk of substantial change over 2 years. Therefore, if patients are tracked, treatment protocols in the future can be streamlined without testing in the community via CHWs.
3.2.3 G6PD POCT
Patients with glucose-6-phosphate dehydrogenase deficiency (G6PD) are at risk for serious hemolysis when treated for Plasmodium vivax with primaquine. Given this risk, Wojnarski et al. deployed a G6PD POCT via Village Malaria Workers in rural Cambodia (100). This study is the first published that utilizes a prehospital G6PD POCT and demonstrated reliable accuracy in results among prehospital vs. laboratory settings.
3.3 Geographical distribution of prehospital point-of-care testing
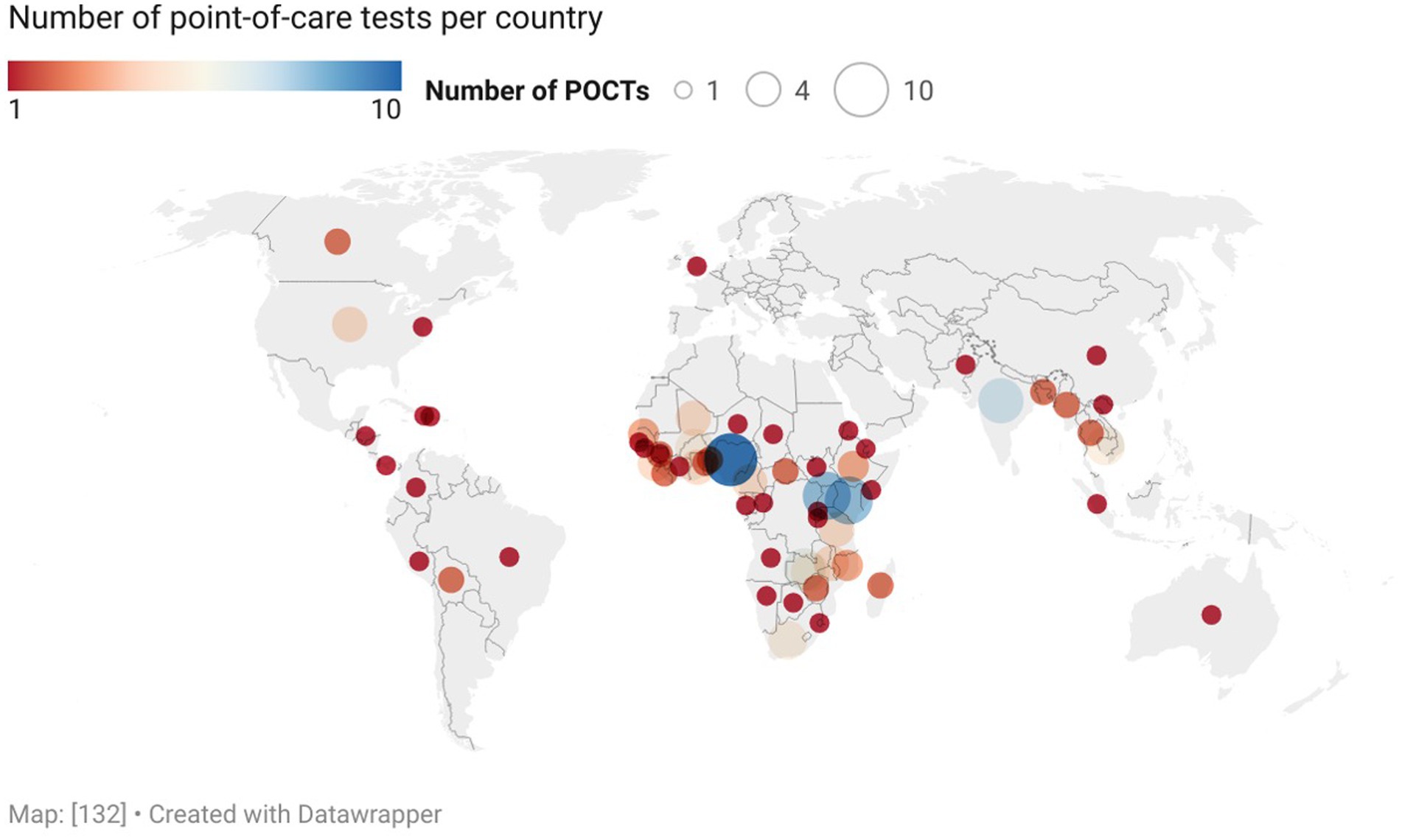
Review of country-level locations of study interventions showed that a majority of POCT evaluations occurred in the Global South (Figure 2) (134). Specifically, in decreasing order by continent, 67 studies occurred in Africa (predominantly in the Sub-Saharan region), 24 in Asia (predominantly in Southeast Asia), 10 in North America (including Caribbean islands and Central American countries), 5 in South America, 1 in Europe, 1 in Australia, and 2 in unspecified areas.
3.4 Type of study design
Articles were characterized by type; for prehospital POCTs, 56/110 (51%) of articles were prospective studies without clinical trials, 10/110 (9%) were clinical trials, and 29/110 (26%) were abstracts. Of note, we reviewed and included three clinical trial protocols that met inclusion criterion. None of the 29 abstracts were non-malaria, non-HIV POCTs (Table 1).
4 Discussion
Simultaneous to the rapid development of novel biomarkers for disease, the capacity to implement POCTs at the community level has changed (1, 6, 7). The findings in this review demonstrate that a diversity of non-malarial prehospital POCTs are being utilized to identify endemic diseases in specific geographic regions. The review also determined that prehospital POCTs are primarily being studied in LMICs. Finally, this review outlines the need for a standardized approach to implementation, monitoring, and evaluation of new POCTs and finds significant heterogeneity between prehospital provider terminology globally.
Although only 11 studies in this review were focused on non-malaria, non-HIV POCTs, 10 (91%) of these studies were published in the last 10 years, and eight (73%) of these in the last 5 years. Portability, decreased cost, and wider accessibility aligned with ease of use in the prehospital setting, has promoted the use of POCTs outside the hospital setting. However, the clinical utility of prehospital POCTs remains unknown. Practical considerations and expert opinion both advocate in favor of implementing POCTs in LMICs; however, after decades of malaria RDT use and subsequent treatment in the prehospital setting, many challenges were identified (1, 6–8). Particularly, financial constraints, limits to supervision and monitoring of CHWs, and a paucity of evidence related to clinical outcomes, constrains progress and possible transformation adaptation (5–8, 23). To improve evaluation for navigating these complexities, a recent content analysis of iCCM programs proposed several frameworks to manage and evaluate programs (23). This overview allows program managers to prepare for process evaluation, sustainability, adequate monitoring, and outcome measurements. This is the necessary first-step in overcoming the many barriers to outcomes research for prehospital POCTs in LMICs.
Primary care in limited health resource settings can be minimal to nonexistent (135). With aging populations, chronic disease becomes more prevalent and there is a need for innovative solutions to address this need in LMICs (135, 136). mHealth offers a unique and timely solution. mHealth applications that use stepwise clinical decision algorithms can incorporate risk factors and POCTs (136). Three studies in this review evaluated risk factors for cardiovascular disease with the input of POCTs (43, 92, 107). Raghu et al. trialed a SMARTHealth mobile POCT application that uses a clinical decision support tool to help guide prehospital providers (107). With advances in telecommunication, decision tools of the alike can be tailored to communities with real-time referral of patients who are at risk and require medical attention. Additionally, telehealth can be integrated into this framework; clinicians may review records and provide online consultation for diagnosis, education, and treatment at the community level. Both Jones et al. and Degennaro et al. also integrated prehospital POCTs to evaluate risk factors and potential benefit of prehospital screening, albeit without a mHealth component (43, 92).
Under the umbrella definition used to identify a CHW in this review, over 30 alternate community definitions were discovered (Figure 3). The majority of CHWs are appointed by local leaders or a quorum of community members to serve as health access points among their communities; the heterogeneity in specific terminology has deep cultural and historical context (8, 9). This variability in terminology is critical to note for future studies or reviews, as standardization is imperative when evaluating prehospital providers in different regions of the world. Further investigation on this variability can help identify potential influences on POCT successes or failures.
This review is limited to available manuscripts and may underrepresent the current diversity in prehospital POCTs. CHW training programs exist across the world and may not have the resources or current interest in publishing on POCT use. This is more limiting for standard POCTs like malaria RDTs, as novel POCTs generally can be identified in early implementation stages when their utility is under investigation. This review included trial protocols and abstracts to capture POCTs that may not be widely disseminated and/or are in development.
This is the first scoping review to evaluate the use of prehospital POCTs by CHWs. The findings in this review demonstrate that prehospital POCTs have increased in number and type over the last two decades with a particular focus on novel, ‘other’ POCTs evaluated over the last 5 years. This review also highlights the under-utilization of mHealth in LMICs and the potential impact of clinical decision support tools that incorporate POCTs for chronic disease management. Overall, it is imperative that POCT use is standardized in the prehospital setting in LMICs, as this may bring early access to care to marginalized communities.
Author contributions
DE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. MT: Investigation, Writing – original draft. MF: Data curation, Formal analysis, Resources, Software, Writing – original draft. MO’D: Writing – original draft. MC: Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. DE acknowledges support from NIH T32: AI007210-39 and Yale Pediatric Scholars Award.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1360322/full#supplementary-material
Footnotes
References
1. Drain, PK, Hyle, EP, Noubary, F, Freedberg, KA, Wilson, D, Bishai, WR, et al. Diagnostic point-of-care tests in resource-limited settings. Lancet Infect Dis. (2014) 14:239–49. doi: 10.1016/S1473-3099(13)70250-0
2. Larsen, FF, and Petersen, JA. Novel biomarkers for sepsis: a narrative review. Eur J Intern Med. (2017) 45:46–50. doi: 10.1016/j.ejim.2017.09.030
3. Leite, AR, Borges-Canha, M, Cardoso, R, Neves, JS, Castro-Ferreira, R, and Leite-Moreira, A. Novel biomarkers for evaluation of endothelial dysfunction. Angiology. (2020) 71:397–410. doi: 10.1177/0003319720903586
4. Ballard, M, and Montgomery, P. Systematic review of interventions for improving the performance of community health workers in low-income and middle-income countries. BMJ Open. (2017) 7:e014216. doi: 10.1136/bmjopen-2016-014216
5. Awor, P, Miller, J, and Peterson, S. Systematic literature review of integrated community case management and the private sector in Africa: relevant experiences and potential next steps. J Glob Health. (2014) 4:1–10. doi: 10.7189/jogh.04.020414
6. Amouzou, A, Morris, S, Moulton, LH, and Mukanga, D. Assessing the impact of integrated community case management (iCCM) programs on child mortality: review of early results and lessons learned in sub–Saharan Africa. J Glob Health. (2014) 4:1–9. doi: 10.7189/jogh.04.020411
7. Sunguya, BF, Mlunde, LB, Ayer, R, and Jimba, M. Towards eliminating malaria in high endemic countries: the roles of community health workers and related cadres and their challenges in integrated community case management for malaria: a systematic review. Malar J. (2017) 16:10–4. doi: 10.1186/s12936-016-1667-x
8. Perry, HB, Zulliger, R, and Rogers, MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. (2014) 35:399–421. doi: 10.1146/annurev-publhealth-032013-182354
9. Scott, K, Beckham, SW, Gross, M, Pariyo, G, Rao, KD, Cometto, G, et al. What do we know about community-based health worker programs? A systematic review of existing reviews on community health workers. Hum Resour Health. (2018) 16:39–7. doi: 10.1186/s12960-018-0304-x
10. Uganda, D. Survey health, Uganda Bureau of Statistics: Key indicators report. Uganda: Kampala, Uganda Ministry of Health (2016).
11. Saluja, S, Rudolfson, N, Massenburg, BB, Meara, JG, and Shrime, MG. The impact of physician migration on mortality in low and middle-income countries: an economic modelling study. BMJ Glob Health. (2020) 5:e001535. doi: 10.1136/bmjgh-2019-001535
12. Early, J, Gonzalez, C, Gordon-Dseagu, V, and Robles-Calderon, L. Use of mobile health (mHealth) technologies and interventions among community health workers globally: a scoping review. Health Promot Pract. (2019) 20:805–17. doi: 10.1177/1524839919855
13. Mahmood, H, Mckinstry, B, Luz, S, Fairhurst, K, Nasim, S, Hazir, T, et al. Community health worker-based mobile health (mHealth) approaches for improving management and caregiver knowledge of common childhood infections: a systematic review. J Glob Health. (2020) 10:1–22. doi: 10.7189/jogh.10.020438
14. Betjeman, TJ, Soghoian, SE, and Foran, MP. mHealth in sub-Saharan Africa. Int J Telemed Appl. (2013) 2013:1–7. doi: 10.1155/2013/482324
15. Colaci, D, Chaudhri, S, and Vasan, A. mHealth interventions in low-income countries to address maternal health: a systematic review. Ann Glob Health. (2016) 82:922–35. doi: 10.1016/j.aogh.2016.09.001
16. Praveen, D, Patel, A, Raghu, A, Clifford, GD, Maulik, PK, Abdul, AM, et al. SMARTHealth India: development and field evaluation of a mobile clinical decision support system for cardiovascular diseases in rural India. JMIR Mhealth Uhealth. (2014) 2:e3568. doi: 10.2196/mhealth.3568
17. Sutton, RT, Pincock, D, Baumgart, DC, Sadowski, DC, Fedorak, RN, and Kroeker, KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ digital medicine. (2020) 3:17. doi: 10.1038/s41746-020-0221-y
18. Wanyonyi, SZ, Mariara, CM, Vinayak, S, and Stones, W. Opportunities and challenges in realizing universal access to obstetric ultrasound in sub-Saharan Africa. Ultrasound Int Open. (2017) 3:E52–9. doi: 10.1055/s-0043-103948
19. Becker, DM, Tafoya, CA, Becker, SL, Kruger, GH, Tafoya, MJ, and Becker, TK. The use of portable ultrasound devices in low-and middle-income countries: a systematic review of the literature. Trop Med Int Health. (2016) 21:294–311. doi: 10.1111/tmi.12657
20. McGowan, J, Sampson, M, Salzwedel, DM, Cogo, E, Foerster, V, and Lefebvre, C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. (2016) 75:40–6. doi: 10.1016/j.jclinepi.2016.01.021
21. Peters, MD, Godfrey, C, McInerney, P, Munn, Z, Tricco, AC, and Khalil, H. Chapter 11: scoping reviews. JBI manual for evidence synthesis. (2020) 169:467–73. doi: 10.46658/JBIMES-20-12
22. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of internal medicine. (2018) 169:467–73. doi: 10.7326/M18-0850
23. Karim, A, de Savigny, D, Awor, P, Muñoz, DC, Mäusezahl, D, Tshefu, AK, et al. The building blocks of community health systems: a systems framework for the design, implementation and evaluation of iCCM programs and community-based interventions. BMJ Glob Health. (2022) 7:e008493. doi: 10.1136/bmjgh-2022-008493
24. Ti, L, Hayashi, K, Kaplan, K, Suwannawong, P, Wood, E, Montaner, J, et al. Willingness to access peer-delivered HIV testing and counseling among people who inject drugs in Bangkok, Thailand. J Community Health. (2013) 38:427–33. doi: 10.1007/s10900-012-9635-z
25. Canavati, SE, Lawpoolsri, S, Quintero, CE, Nguon, C, Ly, P, Pukrittayakamee, S, et al. Village malaria worker performance key to the elimination of artemisinin-resistant malaria: a Western Cambodia health system assessment. Malar J. (2016) 15:282. doi: 10.1186/s12936-016-1322-6
26. Diallo, DA, Konate, M, Traore, I, Bahrambegi, R, and Coulibaly, A. Utility of reporting presumed malaria for improving malaria case management in Mali [conference abstract embase]. Am J Trop Med Hyg. (2020) 103:183.
27. Ikhimioya, U, Adeyoju, T, Okolo, C, Shekarau, E, Hyeladendu, N, Bello, BA, et al. Use of lay health personnel in the implementation of malaria case management within the internally displaced persons community in Nigeria [conference abstract embase]. Am J Trop Med Hyg. (2020) 103:338.
28. Choko, AT, MacPherson, P, Webb, EL, Willey, BA, Feasy, H, Sambakunsi, R, et al. Uptake, accuracy, safety, and linkage into care over two years of promoting annual self-testing for HIV in Blantyre, Malawi: a community-based prospective study. PLoS Med / Public Library of Sci. (2015) 12:e1001873. doi: 10.1371/journal.pmed.1001873
29. Wulandari, LPL, Kaldor, J, and Guy, R. Uptake and acceptability of assisted and unassisted HIV self-testing among men who purchase sex in brothels in Indonesia: a pilot intervention study. BMC Public Health. (2020) 20:14. doi: 10.1186/s12889-020-08812-4
30. Bock, P, Phiri, C, Piwowar-Manning, E, Kosloff, B, Mandla, N, Young, A, et al. Understanding low sensitivity of community-based HIV rapid testing: experiences from the HPTN 071 (PopART) trial in Zambia and South Africa. J Int AIDS Soc. (2017) 20:1–7. doi: 10.7448/IAS.20.7.21780
31. Amutuhaire, M, Rutazaana, D, Opigo, J, Karungi, S, Abwaimo, F, Abbo, S, et al. Test and treat; community outreach strategy improves outcome in a malaria upsurge situation in Gulu district, northern Uganda in 2019 [conference abstract embase]. Am J Trop Med Hyg. (2020) 103:339–40.
32. Dandge, S, Jeemon, P, and Reddy, PS. Technology enabled non-physician health workers extending telemedicine to rural homes to control hypertension and diabetes (TETRA): a pre-post demonstration project in Telangana, India. PLoS ONE [Electronic Resource]. (2019) 14:e0211551. doi: 10.1371/journal.pone.0211551
33. Tagbor, H, Antwi, GD, Acheampong, PR, Bart Plange, C, Chandramohan, D, and Cairns, M. Seasonal malaria chemoprevention in an area of extended seasonal transmission in Ashanti, Ghana: an individually randomised clinical trial. Trop Med Int Health. (2016) 21:224–35. doi: 10.1111/tmi.12642
34. Otshudiema, J, Embeke, N, Hernandez, F, Tchofa, J, Modiri, CM, and Mwema, FX. Scaling-up malaria rapid diagnostic tests and artemisinin-based combination therapy into integrated community case management sites: results from two remote and low-resource settings in the democratic republic of Congo [conference abstract embase]. Am J Trop Med Hyg. (2013) 1:382.
35. Akogun, O. Robotic health assistant (Feverkit) for the rational management of fevers among nomads in Nigeria. Nurs Leadersh. (2011) 24:58–67. doi: 10.12927/cjnl.2011.22465
36. Camara, A, Guilavogui, T, Keita, K, Dioubate, M, Barry, Y, Camara, D, et al. Rapid epidemiological and entomological survey for validation of reported indicators and characterization of local malaria transmission in Guinea, 2017. Am J Trop Med Hyg. (2018) 99:1134–44. doi: 10.4269/ajtmh.18-0479
37. Sania, A, Alam, AN, Alamgir, ASM, Andrecka, J, Brum, E, Chadwick, F, et al. Rapid antigen testing by community health workers for detection of SARS-CoV-2 in Dhaka, Bangladesh: a cross-sectional study. BMJ Open. (2022) 12:e060832. doi: 10.1136/bmjopen-2022-060832
38. Jackson, D, Naik, R, Tabana, H, Pillay, M, Madurai, S, Zembe, W, et al. Quality of home-based rapid HIV testing by community lay counsellors in a rural district of South Africa. J Int AIDS Soc. (2013) 16:18744. doi: 10.7448/IAS.16.1.18744
39. Hamer, DH, Brooks, ET, Semrau, K, Pilingana, P, MacLeod, WB, Siazeele, K, et al. Quality and safety of integrated community case management of malaria using rapid diagnostic tests and pneumonia by community health workers. Pathogens and Global Health. (2012) 106:32–9. doi: 10.1179/1364859411Y.0000000042
40. Bell, D, Bwanika, JB, Cunningham, J, Gatton, M, Gonzalez, IJ, Hopkins, H, et al. Prototype positive control Wells for malaria rapid diagnostic tests: prospective evaluation of implementation among health Workers in Lao People’s Democratic Republic and Uganda. Am J Trop Med Hyg. (2017) 96:319–29. doi: 10.4269/ajtmh.16-0498
41. Awide, HH. Proactive community case Management of Malaria in children aged 6-59 months: results of a pilot project in northern Benin, West Africa, 2018. Am J Trop Med Hyg. (2019) 101:288–9.
42. Gaye, S, Kibler, J, Ndiaye, JL, Diouf, MB, Linn, A, Gueye, AB, et al. Proactive community case management in Senegal 2014-2016: a case study in maximizing the impact of community case management of malaria. Malar J. (2020) 19:166. doi: 10.1186/s12936-020-03238-0
43. Degennaro, V, Malcolm, S, Crompton, L, Vaddiparti, K, Mramba, LK, Striley, C, et al. Community-based diagnosis of non-communicable diseases and their risk factors in rural and urban Haiti: a cross-sectional prevalence study. BMJ Open. (2018) 8:1–8. doi: 10.1136/bmjopen-2017-020317
44. Rogers, AL, Lee, AXT, Joseph, JG, Starnes, JR, Odhong, TO, Okoth, V, et al. Predictors of under-five healthcare utilization in Rongo sub-county of Migori County, Kenya: results of a population-based cross-sectional survey. Pan Afr Med J. (2022) 41:108. doi: 10.11604/pamj.2022.41.108.31618
45. Mischlinger, J, Dudek, V, and Ramharter, M. Predictive performance of rapid diagnostic tests for falciparum malaria and its modeled impact on integrated community case Management of Malaria in sub-Saharan African febrile children. Clin Infect Dis. (2021) 73:e1158–67. doi: 10.1093/cid/ciaa1942
46. Thomas, H, Hann, K, Vandi, M, Sesay, JB, Alpha, KS, and Najjemba, R. Post-Ebola Community Health Worker programme performance in Kenema District, Sierra Leone: A long way to go! F1000Research. (2019). Available from: http://f1000research.com/articles?tab=ALL&articleType=&subjectArea=&subtopic=&show=50 https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed20&AN=2003259636 http://wa4py6yj8t.search.serialssolutions.com/?url_ver=Z39.88-2004&rft_val_fmt
47. McCormack, T, Ayub, R, Aziz, F, Motta, L, Spaeth, B, and Shephard, M. Point-of-care testing facilitates screening and treatment for anaemia in women and children in rural Pakistan. Aust J Rural Health. (2018) 26:194–8. doi: 10.1111/ajr.12395
48. Pascom, AR, Dutra de Barros, CH, Lobo, TD, Pasini, EN, Comparini, RA, and Caldas de Mesquita, F. Point-of-care HIV tests done by peers, Brazil. Bull World Health Organ. (2016) 94:626–30. doi: 10.2471/BLT.15.162461
49. Yan, H, Zhang, R, Wei, C, Li, J, Xu, J, Yang, H, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. (2014) 90:388–93. doi: 10.1136/sextrans-2013-051397
50. Sakolsatayadorn, P, Wattanayingcharoenchai, S, Kanjana-Wattana, S, Tanprasertsuk, S, Sirinirund, P, Janyam, S, et al. A pathway to policy commitment for sustainability of a key population-led health services model in Thailand [conference abstract embase]. Journal of the International AIDS Society Conference: 10th IAS Conference on HIV Science Mexico City Mexico. (2019). Available from: https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed20&AN=629011285 http://wa4py6yj8t.search.serialssolutions.com/?url_ver=Z39.88-2004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&rfr_id=info:sid/Ovid:emed20&rft.genre=article&rft_id=info
51. Boakye, MDS, Owek, CJ, Oluoch, E, Atakora, SB, Wachira, J, and Afrane, YA. Needs assessment of community health workers to enhance efficient delivery of their services for community case management of malaria in Kenya. Malar J. (2021) 20:102. doi: 10.1186/s12936-021-03640-2
52. Oliphant, NP, Muniz, M, Guenther, T, Diaz, T, Lainez, YB, Counihan, H, et al. Multi-country analysis of routine data from integrated community case management (iCCM) programs in sub-Saharan Africa. J Glob Health. (2014) 4:020408. doi: 10.7189/jogh.04.020408
53. Landoh, ED, Tchamdja, P, Saka, B, Tint, KS, Gitta, SN, Wasswa, P, et al. Morbidity and mortality due to malaria in Est mono district, Togo, from 2005 to 2010: a times series analysis. Malar J. (2012) 11:1–7. doi: 10.1186/1475-2875-11-389
54. Briet, OJT, Angluben, R, Torno, M, Navarro, MAH, Deray, R, and Schapira, A. Modelling to support the planning of malaria elimination in southern Palawan, the Philippines [conference abstract embase]. Trop Med Int Health. (2017) 22:55.
55. Laktabai, J, Platt, A, Menya, D, Turner, EL, Aswa, D, Kinoti, S, et al. A mobile health technology platform for quality assurance and quality improvement of malaria diagnosis by community health workers. PLoS ONE [Electronic Resource]. (2018) 13:e0191968. doi: 10.1371/journal.pone.0191968
56. Kinoti, S, Mbogo, C, Hayim, R, Ferro, S, Hirji, Z, Yeung, E, et al. A mobile digital technology (FionetTM) to improve accuracy, completeness and timeliness of research data compared with a non-digital system in Kenya. Bollettino delle malattie veneree, sifilitiche, e della pelle. (2020) 1:1–10. doi: 10.37425/eajsti.v1i3.154
57. Fomba, S, Kone, D, Doumbia, B, Diallo, D, Druetz, T, Florey, L, et al. Management of uncomplicated malaria among children under five years at public and private sector facilities in Mali. BMC Public Health. (2020) 20:1888. doi: 10.1186/s12889-020-09873-1
58. Mubi, M, Janson, A, Warsame, M, Martensson, A, Kallander, K, Petzold, MG, et al. Malaria rapid testing by community health workers is effective and safe for targeting malaria treatment: randomised cross-over trial in Tanzania. PLoS ONE [Electronic Resource]. (2011) 6:e19753. doi: 10.1371/journal.pone.0019753
59. Falade, CO, Ajayi, IO, Nsungwa-Sabiiti, J, Siribie, M, Diarra, A, Serme, L, et al. Malaria rapid diagnostic tests and malaria microscopy for guiding malaria treatment of uncomplicated fevers in Nigeria and Prereferral cases in 3 African countries. Clin Infect Dis. (2016) 63:S290–7. doi: 10.1093/cid/ciw628
60. Kim, S, Nhem, S, Dourng, D, and Menard, D. Malaria rapid diagnostic test as point-of-care test: study protocol for evaluating the VIKIA (R) malaria ag pf/Pan. Malar J. (2015) 14:8. doi: 10.1186/s12936-015-0633-3
61. Thomas, A, Doutchi, M, Issaley, A, Kanta, I, Daures, M, Ouattara, A, et al. Malaria prevention with nutrient supplementation in addition to seasonal chemoprevention in children aged 6-59 months in rural Mali [conference abstract embase]. Am J Trop Med Hyg. (2017) 97:87.
62. Valdez, D, Keys, H, Urena, K, Cabral, D, Camilo, F, Ogando, EC, et al. Malaria outbreak response in urban Santo Domingo, Dominican Republic: lessons learned for community engagement. Pan Am J Public Health. (2020) 44:e92. doi: 10.26633/RPSP.2020.92
63. McLean, ARD, Hla Phyo, W, Aung Myat, T, Zay Soe, K, Indrasuta, C, Ashley, EA, et al. Malaria elimination in remote communities requires integration of malaria control activities into general health care: an observational study and interrupted time series analysis in Myanmar. BMC Med. (2018) 16:1–10. doi: 10.1186/s12916-018-1172-x
64. Pradhan, MM, Sahu, PK, Ranjit, M, Datta, A, and Pati, S. Malaria elimination in high transmission hard-to-reach areas in the state of Odisha India [conference abstract embase]. BMC Proceedings Conference: 1st Field Epidemiology Training Programs India Conference, FETP ICON. (2020). Available from: https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emexa&AN=635914946 http://wa4py6yj8t.search.serialssolutions.com/?url_ver=Z39.88-2004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&rfr_id=info:sid/Ovid:emexa&rft.genre=article&rft_id=info:d
65. Kasereka, CM, Katsuva, JPM, and Hawkes, M. Malaria case-finding and treatment strategies in an internally displaced persons (IDP) camp in the democratic republic of Congo [conference abstract embase]. Am J Trop Med Hyg. (2014) 1:105.
66. Davlantes, E, Salomao, C, Wate, F, Sarmento, D, Rodrigues, H, Halsey, ES, et al. Malaria case management commodity supply and use by community health workers in Mozambique, 2017. Malar J. (2019) 18:47. doi: 10.1186/s12936-019-2682-5
67. Anand, A, Favero, R, Dentinger, C, Ralaivaomisa, A, Ramamonjisoa, S, Rabozakandraina, O, et al. Malaria case management and elimination readiness in health facilities of five districts of Madagascar in 2018. Malar J. (2020) 19:351. doi: 10.1186/s12936-020-03417-z
68. Tiono, AB, Diarra, A, Sanon, S, Nebie, I, Konate, AT, Pagnoni, F, et al. Low specificity of a malaria rapid diagnostic test during an integrated community case management trial. Infectious Dis Therapy. (2013) 2:27–36. doi: 10.1007/s40121-013-0006-6
69. Thomson, A, Khogali, M, de Smet, M, Reid, T, Mukhtar, A, Peterson, S, et al. Low referral completion of rapid diagnostic test-negative patients in community-based treatment of malaria in Sierra Leone. Malar J. (2011) 10:94. doi: 10.1186/1475-2875-10-94
70. Hamze, H, Charchuk, R, Jean Paul, MK, Claude, KM, Leon, M, and Hawkes, MT. Lack of household clustering of malaria in a complex humanitarian emergency: implications for active case detection. Pathogens and Global Health. (2016) 110:223–7. doi: 10.1080/20477724.2016.1220730
71. Zeh, C, Rose, CE, Inzaule, S, Desai, MA, Otieno, F, Humwa, F, et al. Laboratory-based performance evaluation of PIMA CD4+ T-lymphocyte count point-of-care by lay-counselors in Kenya. J Immunol Methods. (2017) 448:44–50. doi: 10.1016/j.jim.2017.05.006
72. Ngo, H, Vu, NB, Green, K, Phan, H, Vo, HS, Ngo, MT, et al. Key population-led health services: Community-based organizations and lay health workers transform HIV testing in Vietnam [conference abstract embase]. Journal of the International AIDS Society Conference: 22nd International AIDS Conference, AIDS. (2018). Available from: https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed19&AN=623485765 http://wa4py6yj8t.search.serialssolutions.com/?url_ver=Z39.88-2004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&rfr_id=info:sid/Ovid:emed19&rft.genre=article&rft_id=info
73. Huy, R, Canavati, SE, Leang, R, Richards, JS, Miotto, O, and Dondorp, AM. Intensifying surveillance of antimalarial multidrug resistance in the Cambodian national control program by integrating genetic epidemiology into routine activities of village malaria workers [conference abstract embase]. Am J Trop Med Hyg. (2015) 93:265.
74. Mazigo, HD, Amuasi, JH, Osei, I, and Kinung’hi, SM. Integrating use of point-of-care circulating cathodic antigen rapid diagnostic tests by community health workers during mass drug administration campaigns to improve uptake of praziquantel treatment among the adult population at Kome Island, North-Western Tanzania: a cluster randomized community trial. BMC Public Health. (2018) 18:840. doi: 10.1186/s12889-018-5732-y
75. Ochom, E, Meyer, AJ, Armstrong-Hough, M, Kizito, S, Ayakaka, I, Turimumahoro, P, et al. Integrating home HIV counselling and testing into household TB contact investigation: a mixed-methods study. Public Health in Action. (2018) 8:72–8. doi: 10.5588/pha.18.0014
76. Linzey, D, Shaheen, S, Macleod, O, Chen, F, Booth, J, and Evans, A. PTU-098 an innovative model to increase uptake of hepatitis C testing in the pakistani population in reading, England. Gut. (2015) 64:A104.1–A104. doi: 10.1136/gutjnl-2015-309861.213
77. Kheang, ST, Duong, S, and Olkkonen, A. Increasing access to early malaria diagnosis and prompted treatment in remote cambodian villages. Am J Public Health. (2011) 101:e6–8. doi: 10.2105/AJPH.2011.300228
78. Brennan, AT, Thea, DM, Semrau, K, Goggin, C, Scott, N, Pilingana, P, et al. In-home HIV testing and nevirapine dosing by traditional birth attendants in rural Zambia: a feasibility study. J Midwifery Womens Health. (2014) 59:198–204. doi: 10.1111/jmwh.12038
79. Smith, CMJ, De Urriola, L, Cerezo, L, Vizcaino, F, Victoria, C, Cortes, D, et al. Improving malaria case management and surveillance through a community-based pilot in Panama [conference abstract embase]. Am J Trop Med Hyg. (2017) 97:528.
80. Badolo, O, Nebie, SP, Bonkoungou, M, Dodo, M, Waxman, R, Burke, D, et al. The improving malaria care (IMC) project’s contribution to follow up a pilot to use rapid diagnostic tests (RDTS) at the community level in Burkina Faso [conference abstract embase]. Am J Trop Med Hyg. (2016) 95:69.
81. Rozelle, JW, Korvah, J, Wiah, O, Kraemer, J, Hirschhorn, LR, Price, MR, et al. Improvements in malaria testing and treatment after a national community health worker program in rural Liberia. J Global Health Reports. (2021) 5:e2021073. doi: 10.29392/001c.25979
82. Ahmed, S, Kim, MH, Dave, AC, Sabelli, R, Kanjelo, K, Preidis, GA, et al. Improved identification and enrolment into care of HIV-exposed and -infected infants and children following a community health worker intervention in Lilongwe, Malawi. J Int AIDS Soc. (2015) 18:19305. doi: 10.7448/IAS.18.1.19305
83. Pion, SD, Nana-Djeunga, H, Niamsi-Emalio, Y, Chesnais, CB, Deleglise, H, Mackenzie, C, et al. Implications for annual retesting after a test-and-not-treat strategy for onchocerciasis elimination in areas co-endemic with Loa loa infection: an observational cohort study. Lancet Infect Dis. (2020) 20:102–9. doi: 10.1016/S1473-3099(19)30554-7
84. Ajibaye, O, Balogun, EO, Olukosi, YA, Orok, BA, Oyebola, KM, Iwalokun, BA, et al. Impact of training of mothers, drug shop attendants and voluntary health workers on effective diagnosis and treatment of malaria in Lagos, Nigeria. Tropical Parasitol. (2019) 9:36–44. doi: 10.4103/tp.TP_36_18
85. Hopkins, H, West, P, Yeung, S, and Chandler, C. Impact of malaria rapid diagnostic tests on patients’ subsequent treatment-seeking, costs and health outcomes: results from the act consortium [conference abstract embase]. Am J Trop Med Hyg. (2015) 93:520.
86. Leurent, B, Bruxvoort, K, Grieve, E, Hutchinson, E, Reynolds, J, and Leslie, T. Impact of malaria rapid diagnostic tests on care of febrile patients: cross-project results from the act consortium [conference abstract embase]. Am J Trop Med Hyg. (2014) 1:552.
87. Samuels, AM, Odero, NA, Odongo, W, Otieno, K, Were, V, Shi, YP, et al. Impact of community-based mass testing and treatment on malaria infection prevalence in a high-transmission area of Western Kenya: a cluster randomized controlled trial. Clin Infect Dis. (2021) 72:1927–35. doi: 10.1093/cid/ciaa471
88. van Rooyen, H, Barnabas, RV, Baeten, JM, Phakathi, Z, Joseph, P, Krows, M, et al. High HIV testing uptake and linkage to care in a novel program of home-based HIV counseling and testing with facilitated referral in KwaZulu-Natal, South Africa. J Acquired Immune Deficiency Syndromes: JAIDS. (2013) 64:e1–8. doi: 10.1097/QAI.0b013e31829b567d
89. Bridges, DJ, Miller, JM, Chalwe, V, Moonga, H, Hamainza, B, Steketee, RW, et al. Application of serology in evaluating two reactive response interventions for malaria elimination: results from the core community randomized trial in southern province, Zambia [conference abstract embase]. Am J Trop Med Hyg. (2020) 103:219.
90. Phiri, TB, Kaunda-Khangamwa, BN, Bauleni, A, Chimuna, T, Melody, D, Kalengamaliro, H, et al. Feasibility, acceptability and impact of integrating malaria rapid diagnostic tests and pre-referral rectal artesunate into the integrated community case management programme. A pilot study in Mchinji district, Malawi. Malar J. (2016) 15:177. doi: 10.1186/s12936-016-1237-2
91. Sarkar, A, Mburu, G, Shivkumar, PV, Sharma, P, Campbell, F, Behera, J, et al. Feasibility of supervised self-testing using an oral fluid-based HIV rapid testing method: a cross-sectional, mixed method study among pregnant women in rural India. J Int AIDS Soc. (2016) 19:20993. doi: 10.7448/IAS.19.1.20993
92. Jones, CA, Nanji, A, Mawani, S, Davachi, S, Ross, L, Vollman, A, et al. Feasibility of community-based screening for cardiovascular disease risk in an ethnic community: the south Asian cardiovascular health assessment and management program (SA-CHAMP). BMC Public Health. (2013) 13:160. doi: 10.1186/1471-2458-13-160
93. Penda, CI, Moukoko, CEE, Koum, DK, Fokam, J, Meyong, CAZ, Talla, S, et al. Feasibility and utility of active case finding of HIV-infected children and adolescents by provider-initiated testing and counselling: evidence from the Laquintinie hospital in Douala, Cameroon. BMC Pediatr. (2018) 18:259. doi: 10.1186/s12887-018-1235-3
94. Swana, EK, Makan, GY, Mukeng, CK, Mupumba, HI, Kalaba, GM, Luboya, ON, et al. Feasibility and implementation of community-based malaria case management with integrated vector control in the Democratic Republic of Congo. Malar J. (2016) 15:413. doi: 10.1186/s12936-016-1475-3
95. Zelalem, D, Getaneh, A, Mulat, Y, Chalachew, M, and Banchamlak, T. Evaluation of the performance of health extension workers on malaria rapid diagnostic tests and predictor factors in Bahir Dar Zuria district, Northwest Ethiopia: a cross-sectional study. PLoS One. (2021) 16:1–11. doi: 10.1371/journal.pone.0249708
96. Searle, KM, Hamapumbu, H, Lubinda, J, Shields, TM, Pinchoff, J, Kobayashi, T, et al. Evaluation of the operational challenges in implementing reactive screen-and-treat and implications of reactive case detection strategies for malaria elimination in a region of low transmission in southern Zambia. Malar J. (2016) 15:412. doi: 10.1186/s12936-016-1460-x
97. Garofalo, R, Adetunji, A, Kuhns, LM, Omigbodun, O, Johnson, AK, Kuti, K, et al. Evaluation of the iCARE Nigeria pilot intervention using social media and peer navigation to promote HIV testing and linkage to care among high-risk Young men: a nonrandomized controlled trial. JAMA Netw Open. (2022) 5:e220148. doi: 10.1001/jamanetworkopen.2022.0148
98. Agius, PA, Cutts, JC, Han Oo, W, Thi, A, O’Flaherty, K, Zayar Aung, K, et al. Evaluation of the effectiveness of topical repellent distributed by village health volunteer networks against plasmodium spp. infection in Myanmar: a stepped-wedge cluster randomised trial. PLoS Medicine / Public Library of Science. (2020) 17:e1003177. doi: 10.1371/journal.pmed.1003177
99. Ferdinand, DY, Nadlaou, B, Samuel, N, Oscar, BY, Raphael, M, Christophe, N, et al. Evaluation of the effectiveness of community health workers in the fight against malaria in the Central African Republic (2012-2017). Trans R Soc Trop Med Hyg. (2020) 114:173–84. doi: 10.1093/trstmh/trz104
100. Wojnarski, B, Lon, C, Sea, D, Sok, S, Sriwichai, S, Chann, S, et al. Evaluation of the CareStart TM glucose-6-phosphate dehydrogenase (G6PD) rapid diagnostic test in the field settings and assessment of perceived risk from primaquine at the community level in Cambodia. PLoS ONE [Electronic Resource]. (2020) 15:e0228207. doi: 10.1371/journal.pone.0228207
101. Gidebo, KD, and Mavundla, TR. Evaluation of malaria treatment practice of health extension workers (community health workers): a qualitative study conducted in Damot Gale district, southern Ethiopia. Indian J Community Health. (2015) 27:66–71.
102. Ruizendaal, E, Schallig, H, Scott, S, Traore-Coulibaly, M, Bradley, J, Lompo, P, et al. Evaluation of malaria screening during pregnancy with rapid diagnostic tests performed by community health Workers in Burkina Faso. Am J Trop Med Hyg. (2017) 97:1190–7. doi: 10.4269/ajtmh.17-0138
103. Morris, JL, Prach, L, Gilvydis, J, Naidoo, E, Treves-Kagan, S, Grignon, J, et al. Evaluation of a comprehensive HIV prevention program in north West Province, South Africa: results from the pilot [conference abstract embase]. Ann Glob Health. (2014) 80:242. doi: 10.1016/j.aogh.2014.08.210
104. Garcia, ME, Baird, M, Lana, J, Hanson, K, Park, S, Cartagena, L, et al. Evaluating the community health worker network to achieve and sustain malaria elimination in Gracias a Dios, Honduras [conference abstract embase]. Am J Trop Med Hyg. (2020) 103:347–8.
105. Marita, E, Langat, B, Kinyari, T, Igunza, P, Apat, D, Kimori, J, et al. Implementation of community case management of malaria in malaria endemic counties of western Kenya: are community health volunteers up to the task in diagnosing malaria? Malar J. (2022) 21:73. doi: 10.1186/s12936-022-04094-w
106. Brieger, WR, Orji, BC, Otolorin, E, Ndekhedehe, E, and Nwadike, JU. Establishing integrated community management of malaria, pneumonia and diarrhea in selected two local government areas, Akwa Ibom state Nigeria [conference abstract embase]. Am J Trop Med Hyg. (2011) 1:173.
107. Raghu, A, Praveen, D, Peiris, D, Tarassenko, L, and Clifford, G. Engineering a mobile health tool for resource-poor settings to assess and manage cardiovascular disease risk: SMARThealth study. BMC Medical Info Decision Making. (2015) 15:36. doi: 10.1186/s12911-015-0148-4
108. Yeonji, M, Heunghee, K, Yinseo, C, Jaeeun, L, Degley, JK, Adam, AG, et al. Effects of community health volunteers on infectious diseases of children under five in Volta region, Ghana: study protocol for a cluster randomized controlled trial. BMC Public Health. (2017) 17:95–10. doi: 10.1186/s12889-016-3991-z
109. Cossio, A, Jojoa, J, Castro, MDM, Castillo, RM, Osorio, L, Shelite, TR, et al. Diagnostic performance of a recombinant polymerase amplification test-lateral flow (RPA-LF) for cutaneous leishmaniasis in an endemic setting of Colombia. PLoS Neglected Tropical Dis [electronic resource]. (2021) 15:e0009291. doi: 10.1371/journal.pntd.0009291
110. Singh, MP, Chand, SK, Jaiswal, A, Savargaonkar, D, and Anvikar, AR. Diagnostic ability of community health workers for malaria diagnosis in the field using different variants of bivalent malaria rapid diagnostic test kits. J Vector Borne Dis. (2018) 55:321–3. doi: 10.4103/0972-9062.256569
111. Francis, F, Ishengoma, DS, Mmbando, BP, Rutta, ASM, Malecela, MN, Mayala, B, et al. Deployment and use of mobile phone technology for real-time reporting of fever cases and malaria treatment failure in areas of declining malaria transmission in Muheza district North-Eastern Tanzania. Malar J. (2017) 16:308. doi: 10.1186/s12936-017-1956-z
112. Samir, G, Preeti, G, Mukesh, D, and Prabodh, N. Coverage of community case management for malaria through CHWs: a quantitative assessment using primary household surveys of high-burden areas in Chhattisgarh state of India. Malar J. (2020) 19:1–11. doi: 10.1186/s12936-020-03285-7.pdf
113. Guenther, T, Sadruddin, S, Finnegan, K, Wetzler, E, Ibo, F, Rapaz, P, et al. Contribution of community health workers to improving access to timely and appropriate case management of childhood fever in Mozambique. J Glob Health. (2017) 7:1–12. doi: 10.7189/jogh.07.010402
114. Dziva Chikwari, C, Simms, V, Kranzer, K, Dringus, S, Chikodzore, R, Sibanda, E, et al. Comparison of index-linked HIV testing for children and adolescents in health facility and community settings in Zimbabwe: findings from the interventional B-GAP study. Lancet HIV. (2021) 8:e138–48. doi: 10.1016/S2352-3018(20)30267-8
115. Chowdhury, P, Baidya, S, Paul, D, Kalita, B, Saikia, G, Karmakar, S, et al. A comparative study on knowledge and practice against malaria among accredited social health activists (ASHAs) of low and high endemic regions of Tripura, Northeast India. J Family Med Prim Care. (2020) 9:2420–5. doi: 10.4103/jfmpc.jfmpc_1169_19
116. Latham, NH, Pedrana, A, Doyle, JS, Howell, J, Williams, B, Higgs, P, et al. Community-based, point-of-care hepatitis C testing: perspectives and preferences of people who inject drugs. J Viral Hepat. (2019) 26:919–22. doi: 10.1111/jvh.13087
117. Nelson, AK, Caldas, A, Sebastian, JL, Munoz, M, Bonilla, C, Yamanija, J, et al. Community-based rapid oral human immunodeficiency virus testing for tuberculosis patients in Lima, Peru. Am J Trop Med Hyg. (2012) 87:399–406. doi: 10.4269/ajtmh.2012.12-0036
118. Bungay, V, Kolar, K, Thindal, S, Remple, VP, Johnston, CL, and Ogilvie, G. Community-based HIV and STI prevention in women working in indoor sex markets. Health Promot Pract. (2013) 14:247–55. doi: 10.1177/15248399124471
119. Say, C, Bjorge, S, Sokkhieng, M, Dysoley, L, and Soy, TK. Community level day-3 positive surveillance of plasmodium falciparum malaria in Cambodia [conference abstract embase]. Int J Infect Dis. (2012) 16:e35. doi: 10.1016/j.ijid.2012.05.090
120. Orji, BC, Rao, N, Thompson, E, Brieger, WR, and Dipo, OE. Community health workers provide integrated community case management using malaria rapid diagnostic test kits. Res Soc Adm Pharm. (2017) 13:875–9. doi: 10.1016/j.sapharm.2016.09.006
121. Lal, S, Ndyomugenyi, R, Magnussen, P, Hansen, KS, Alexander, ND, Paintain, L, et al. Referral patterns of community health workers diagnosing and treating malaria: cluster-randomized trials in two areas of high- and low-malaria transmission in southwestern Uganda. Am J Trop Med Hyg. (2016) 95:1398–408. doi: 10.4269/ajtmh.16-0598
122. Hammack, AY, Bickham, JN, Gilliard, I 3rd, and Robinson, WT. A community health worker approach for ending the HIV epidemic. Am J Prev Med. (2021) 61:S26–31. doi: 10.1016/j.amepre.2021.06.008
123. Ajayi, IO, Jegede, AS, Ogunwale, AO, Ogundairo, J, Olaleye, OS, Oshiname, FO, et al. Community acceptance, satisfaction, and support for case management of malaria of various degrees in selected rural communities in Ibadan. Oyo-State Ghana Medical J. (2021) 55:198–205. doi: 10.4314/gmj.v55i3.4
124. Jones, FK, Wesolowski, A, Phru, CS, Hossain, MS, Sullivan, DJ, Khan, WA, et al. Characterization of endemic year-round malaria transmission in the Chittagong Hill tracts of Bangladesh [conference abstract embase]. Am J Trop Med Hyg. (2019) 101:496.
125. Kenya, S, Okoro, IS, Wallace, K, Ricciardi, M, Carrasquillo, O, and Prado, G. Can home-based HIV rapid testing reduce HIV disparities among African Americans in Miami? Health Promot Pract. (2016) 17:722–30. doi: 10.1177/15248399166299
126. Young, B, Rosenthal, A, Escarfuller, S, Shah, S, Carrasquillo, O, and Kenya, S. Beyond the barefoot doctors: using community health workers to translate HIV research to service. AIDS Behav. (2019) 23:2879–88. doi: 10.1007/s10461-019-02636-z
127. Blanas, DA, Ndiaye, Y, Nichols, K, Jensen, A, Siddiqui, A, and Hennig, N. Barriers to community case management of malaria in Saraya, Senegal: training, and supply-chains. Malar J. (2013) 12:95. doi: 10.1186/1475-2875-12-95
128. Ranasinghe, S, Ansumana, R, Lamin, JM, Bockarie, AS, Bangura, U, Buanie, JA, et al. Attitudes toward home-based malaria testing in rural and urban Sierra Leone. Malar J. (2015) 14:80. doi: 10.1186/s12936-015-0582-x
129. Lopez, M, Marca, C, Guarachi, C, Ortiz, H, and Torrez, M. Assessment of the role of volunteers in malaria case management in a rural area of tropical Bolivia. Revista de Salud Ambiental. (2013) 13:120–8.
130. Miller, JS, Mbusa, RK, Baguma, S, Patel, P, Matte, M, Ntaro, M, et al. Assessing Village health workers’ ability to perform and interpret rapid diagnostic tests for malaria 4 years after initial training: a cross-sectional study. Am J Trop Med Hyg. (2021) 104:294–7. doi: 10.4269/ajtmh.20-0747
131. Jegede, AS, Oshiname, FO, Sanou, AK, Nsungwa-Sabiiti, J, Ajayi, IO, Siribie, M, et al. Assessing acceptability of a diagnostic and malaria treatment package delivered by community health Workers in Malaria-Endemic Settings of Burkina Faso, Nigeria, and Uganda. Clin Infect Dis. (2016) 63:S306–11. doi: 10.1093/cid/ciw630
132. Okwen, PM, Ngem, B, Chia, ON, Cheabum, R, and Moola, S. Artemisinin based combination therapy for uncomplicated malaria management among children under five in Cameroon: a best practice implementation project. JBI Database System Rev Implement Rep. (2018) 16:776–90. doi: 10.11124/JBISRIR-2017-003404
133. Mukanga, D, Tibenderana, JK, Peterson, S, Pariyo, GW, Kiguli, J, Waiswa, P, et al. Access, acceptability and utilization of community health workers using diagnostics for case management of fever in Ugandan children: a cross-sectional study. Malar J. (2012) 11:121. doi: 10.1186/1475-2875-11-121
134. Beratarrechea, A, Lee, AG, Willner, JM, Jahangir, E, Ciapponi, A, and Rubinstein, A. The impact of mobile health interventions on chronic disease outcomes in developing countries: a systematic review. Telemedicine and e-Health. (2014) 20:75–82. doi: 10.1089/tmj.2012.0328
135. Kelly, BB, Narula, J, and Fuster, V. Recognizing global burden of cardiovascular disease and related chronic diseases. Mount Sinai J Med: J Trans Personalized Med. (2012) 79:632–40. doi: 10.1002/msj.21345
Keywords: community health worker, point-of-care test, mobile health, rapid diagnostic test, lay health worker
Citation: Ebbs D, Taricia M, Funaro MC, O’Daniel M and Cappello M (2024) Prehospital use of point-of-care tests by community health workers: a scoping review. Front. Public Health. 12:1360322. doi: 10.3389/fpubh.2024.1360322
Edited by:
Monica Catarina Botelho, Universidad do Porto, PortugalReviewed by:
Miguel Ángel Castro Villamor, Universidad de Valladolid, SpainJose Ricardo Navarro Vargas, National University of Colombia, Colombia
Copyright © 2024 Ebbs, Taricia, Funaro, O’Daniel and Cappello. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel Ebbs, ZGFuaWVsLmViYnNAeWFsZS5lZHU=
 Daniel Ebbs
Daniel Ebbs Max Taricia1
Max Taricia1 Melissa C. Funaro
Melissa C. Funaro Maggie O’Daniel
Maggie O’Daniel Michael Cappello
Michael Cappello