- 1Postgraduate Master's Programme: Health and Social Care Services Management, Faculty of Health Sciences, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 2Laboratory of Forensic Medicine & Toxicology (Division: Medical Law and Ethics), Faculty of Health Sciences, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 3Master of Science in Business Administration Programme, Faculty of Economics and Business, Katholieke Universiteit Leuven, Brussels, Belgium
- 4Postgraduate Master's Programme: Health and Social Care Services Management, Faculty of Health Sciences, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 5Department of Cardiothoracic Surgery, Faculty of Health Sciences, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
The management of health supplies in public hospitals has been a major concern of national and European institutions over time, often being a field of reforms and regulatory interventions. Health procurement systems constitute complex decision-making and supply chain management mechanisms of public hospitals, involving suppliers, health providers, administrators and political bodies. Due to this complexity, the first important decision to be taken when designing a procurement system, concerns the degree of centralization, namely to what extent the decision-making power on the healthcare procurement (what, how and when) will be transferred either to a central public authority established for this purpose, or to the competent local authorities. In this perspective, we attempt to analyse the types of public procurement in the healthcare sector of the European Union, in terms of degree of centralization. Employing a narrative approach that summarizes recent interdisciplinary literature, this perspective finds that the healthcare procurement systems of the EU Member States, based on the degree of centralization, are categorized into three types of organizational structures: Centralized, Decentralized and Hybrid procurement. Each structure offers advantages and disadvantages for health systems. According to this perspective, a combination of centralized and decentralized purchases of medical supplies represents a promising hybrid model of healthcare procurement organization by bringing the benefits of two methods together.
1 Introduction
The health systems worldwide are faced with the increasing cost of medical care, the limitation of available resources and the failure to meet the legitimate and reasonable expectations of patients-users in relation to the quality of services provided. Addressing costs, supply shortages and treatment disruption in complex settings can be critical to strengthening health systems (1). Nowadays, the users of health services, worldwide, seek equal access to increasingly better quality healthcare and expect the use of medical equipment and modern medical diagnostic tools to them that incorporate the latest technology (2). Implementing the equal access obligation (3) and ensuring the provision of high-quality public health services, requires a strategic approach to sourcing, which depends to a large extent on modern and efficient public procurement procedures (4).
For all the reasons above, the management of healthcare supplies in public hospitals has been a serious concern for the Member-States (M-S) of the European Union (EU). Changes in healthcare procurement include centralizing or decentralizing procurement, improving information systems to track and update data, improving infrastructure and processes along the supply chain (1). Therefore, the solution to successfully address these problems in the healthcare sector lies in the rational management of public hospitals' supplies or otherwise in the effective management of their supply chain (5).
In this perspective, we approach the issue of healthcare procurement in the EU M-S in light of the degree of centralization and we attempt to compare the types of organizational structures, in order to draw useful conclusions about their advantages and disadvantages. The aim of this discussion is to inform policymakers on promising cost containment policies as well as best practices to improve the efficiency, transparency, and competition of their healthcare procurement systems.
2 The importance of degree of centralization in public healthcare procurement
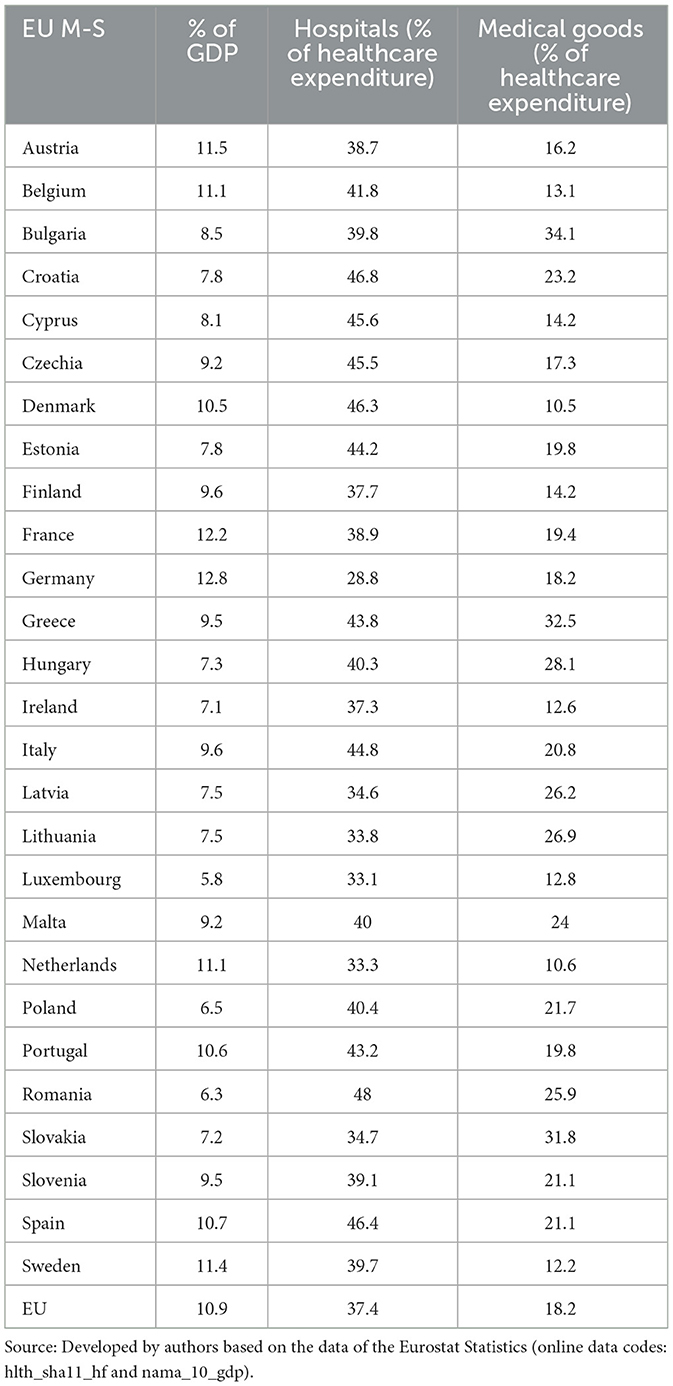
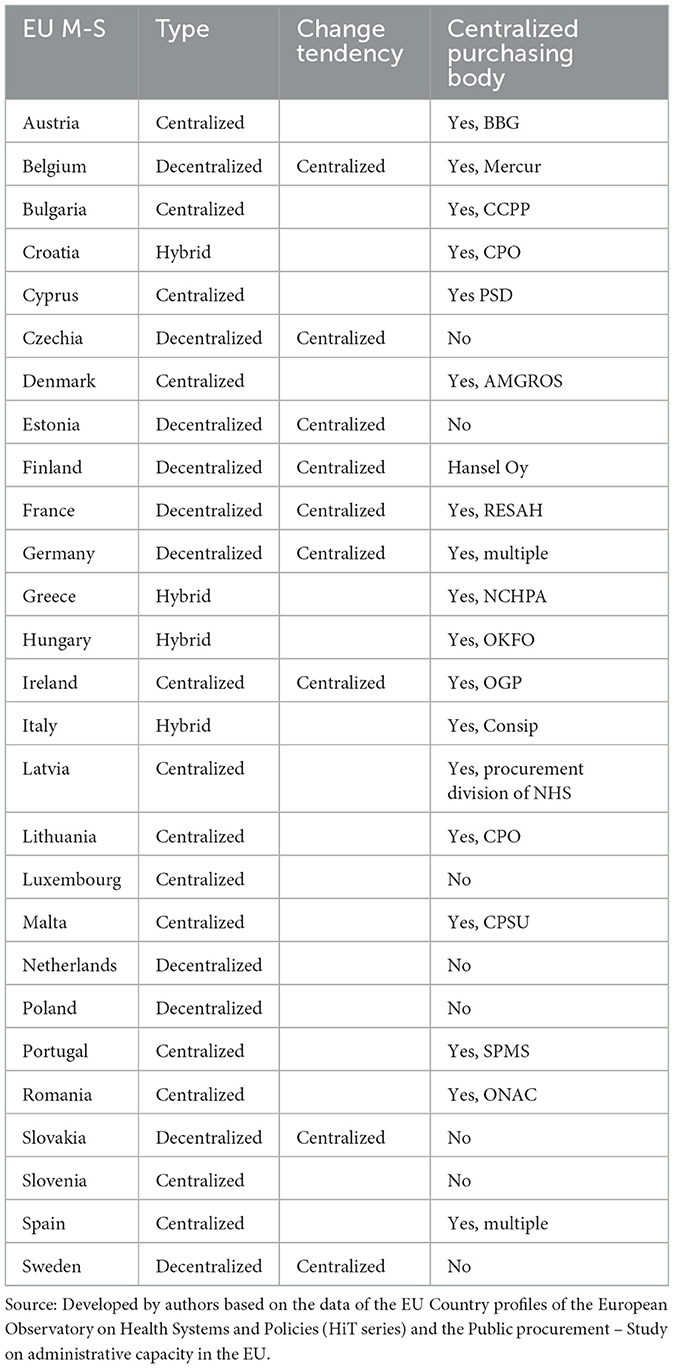
The total volume of EU healthcare expenditure in 2020 amounted to 10.91% of its total gross domestic product (GDP) (6, 7). Hospitals accounted for the highest proportion (37.4%) of healthcare expenditure in 2020 in the EU (8). Medical goods were the second largest function in the EU in 2020, with an 18.2% share of current healthcare expenditure (9). An analysis of current healthcare expenditure in the EU M-S is shown in Table 1.
Due to the significant volume of healthcare expenditure, the main objective of M-S is to optimize their supplies so that health systems offer maximum efficiency in relation to the financial, material and human resources used. Their initiatives include centralized or decentralized supplies, the enhancement of information systems for monitoring and updating data and the improvement of infrastructures and processes along the supply chain (10). On public procurement in particular, the European Parliament and the Council adopted in 2014 a new package of measures, which includes Directive 2014/24/EU (11).
The efficiency and budget control at a public healthcare provider can vary significantly depending on how their procurement is organized and managed. One way to increase the efficiency and effectiveness of public procurement is to choose either between a centralized system, where a central body is responsible for managing all purchasing and procurement activities (selecting suppliers, negotiating prices and terms, making a purchase decision) for final recipients (i.e., local units), who are simply asked to send their requests to it, or a decentralized system; where local units procure themselves (12).
Therefore, the first important decision to be taken in designing the procurement system of a complex organization, such as the health system, concerns its degree of centralization (13). This decision falls under the more general issue of award, an issue that has been widely explored, although not very extensively in public procurement. The issue of centralization vs. decentralization of procurement, due to both the need to control costs and the rationalization of procedures, attracts the interest of researchers, professionals and public administration executives from various angles and is becoming increasingly important for many organizations (14).
3 The three types of healthcare procurement systems based on the degree of centralization
With the aforementioned research approach, we will examine the various models of healthcare procurement based on the degree of centralization and we will review the arguments for and against centralized and decentralized procurement operations. Then we will try to consider the possible impact of such systems in the healthcare sector. In this perspective, the procurement systems based on the degree of centralization and the extent of the powers of contracting authorities are classified into three main types (15).
3.1 Centralized procurement
A procurement system is fully centralized when all relevant decisions (what, how and when) on the purchasing of products, whether through tendering procedures or negotiations, are taken by a central purchasing body set up for this purpose, as shown in Figure 1A (16).
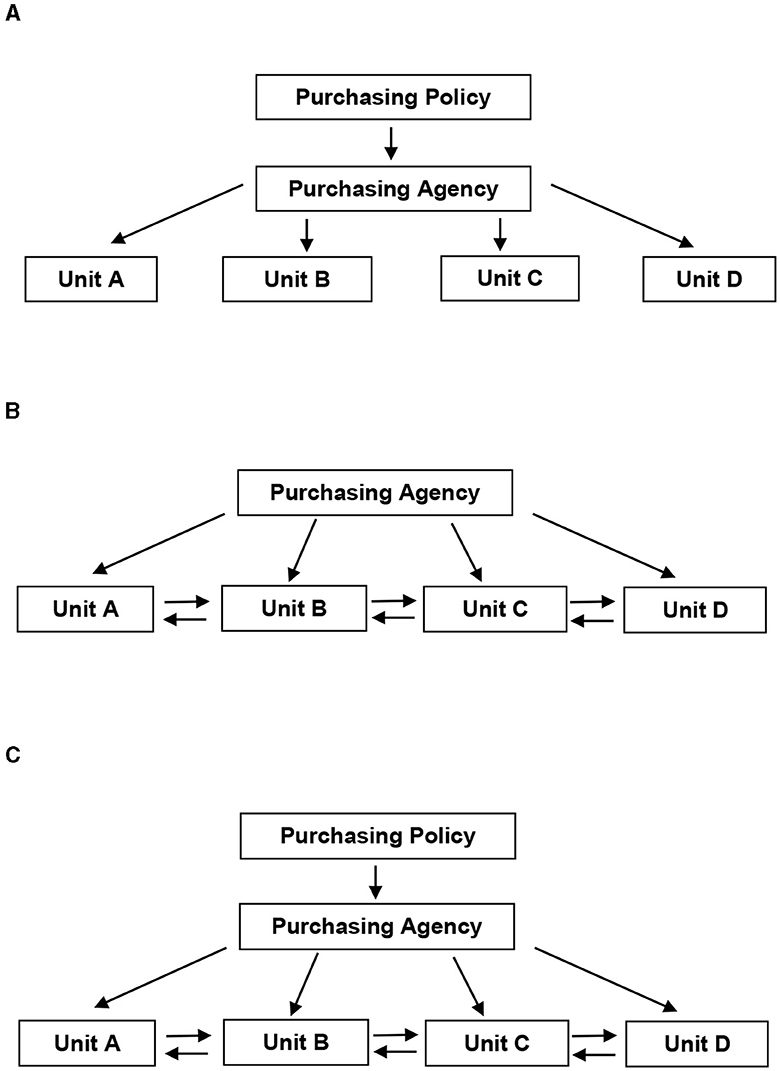
Figure 1. Schematic diagrams of decision-making authority. (A) Centralized model. (B) Decentralized model. (C) Hybrid model. Source: McCue and Pitzer (16).
According to Directive 2014/24/EU “Central purchasing body means a contracting authority providing centralized purchasing activities and, possibly, ancillary purchasing activities” (Directive 2014/24/EU of the European Parliament and of the Council of 26 February 2014 on Public Procurement and Repealing Directive 2004/18/EC Text with EEA Relevance, 2014). At this point, we have to highlight that Directive 2014/24/EU pursuant to recital no. 59 et seq., establishes the separation between aggregation and centralization. The distinction between centralization and aggregation, is that the “centralization” is related to the preparation of a Public Procurement Framework Agreement, whereas the “aggregation” is linked to the concept of quantity or the batch size of procedures. This Directive also emphasizes Dynamic Acquisition Systems, having adjusted the rules applicable to this contracting instrument so that entities adjudicators can take advantage of this instrument. Pursuant to article 37 of the Directive referred to in the previous paragraph, thus becomes one of the possible instruments for use in the scope of centralized purchasing. Furthermore, the terms of the contract for the products under supply are the same in all local public bodies. Centralized procurement and competitive tendering can achieve cost savings across multiple sectors by reaping economies of scale and improved purchasing power. Moreover, the benefits are not only lower prices and savings but also they include improved transparency and governance such as enhanced equity (17). According to Coe centralization of procurement procedures is necessary, both to prevent waste and inefficiency, and to establish control systems (18). It also helps to reduce the situations of exceptional purchases, which usually occur when staff are not sufficiently trained at professional level in purchasing methods.
Undoubtedly, the centralization of public procurement is becoming established throughout the EU. After a period of skepticism, where central procurement was seen as a factor of monopsony and reduced competition, central purchasing bodies, as aggregators, are now managing increasing shares of public procurement. In this spirit, the European Commission's Communication explicitly recognizes the possibility of setting up central purchasing bodies with a general mandate at national level, targeting specific sectors, including health. Given the large volume of public procurement achieved by central purchasing bodies, they can be used to leverage strategic procurement, such as targeting public procurement. They could also play an important role in standardization of public procurement procedures. Central purchasing bodies, by virtue of their specialized knowledge and expertise in purchasing issues, may provide support and advisory services to other contracting authorities and thus contribute indirectly to improving the professional character of public administrations (4).
For the healthcare sector in particular, centralization of procurement is not a new idea. Research by Board on Global Health (BGH) illustrates the benefits of a centralized international malaria drug procurement system (19). Similarly, the Supply Division of United Nations Children's Fund (UNICEF) in Copenhagen has many years of experience in the fully centralized vaccine market under the umbrella of the public-private health partnership Global Alliance for Vaccines and Immunization (GAVI), established in 2000 with aim to increase equitable access to immunization in lower income countries (20). Similarly, the World Health Organization (WHO) proposed similar initiatives at international level to reduce costs in tackling malaria, tuberculosis and HIV/AIDS (21).
In summary, the main arguments in favor of the centralized procurement systems are the following (22):
(a) Significant price reductions.
(b) Better goods and services at lower cost.
(c) Increased purchasing power.
(d) Need for technical standardization (e.g., in the field of information systems and software applications).
(e) Definition and inclusion in the terms of environmental standards for public procurement.
(f) No cost benefits, including greater attention to contract management and better problem solving (e.g., defective products, substandard services, inadequate after-sales services).
(g) Lower staff training costs because they are numerically less and centrally located.
(h) Easier management of staff performance.
(i) Encourage the issuance of transparency regulations, such as effective recording and reporting of procurement and transaction contracts, effective management controls.
On the other hand, the opponents of centralization contend that the expenses related to time and effort necessary to establish and maintain cooperative interactions, such as transaction costs (e.g., information, negotiation, and enforcement costs), could surpass the potential advantages of centralization. Moreover, as centralization takes place, there is a growing concern that it might gradually exclude peripheral actors from participating in governance. This exclusion can potentially limit the ability of central governments to effectively address disputes or develop policies that require local input (23).
3.2 Decentralized procurement
Fully decentralized is the procurement system in which the power of decision making on the purchasing of products (what, how and when) has been transferred to the relevant local administrations, as shown in Figure 1B (16).
The decentralization of the health system can be implemented in various forms and to different degrees, depending on the existing policy, the public administrative structure and the organization of the health system of each country. The most effective programs that improve supply chain and procurement processes address the root causes of system inefficiencies and may provide specific interventions (24).
The logic of decentralization is based on the fact that smaller organizations, properly organized and managed, are inherently more flexible and responsible than larger organizations. Another rationale is that by placing procurement management closer to end-user needs, it is likely to be more cost-effective and able to promote the growth of the private sector, including small and medium-sized enterprises (22). Even the German sociologist Max Weber, who first formulated the basic features of the bureaucratic model and who himself reluctantly concluded that bureaucracy was inevitable in human organization, considered that the only alternative to bureaucracy is a return to small-scale organization (25). Given the strength of this view, it is not surprising that from time to time, and especially since World War II, in an effort to restructure the health sector in various European countries, many national and regional policymakers have introduced decentralization strategies.
Moreover, another important reason for the attractiveness of the idea of decentralization of systems is its adaptability, which allows it to fit simultaneously into the many different national and local health policies. Thus, the decentralized bodies in the health sector can either be public institutions financed by taxes, or non-profit private entities such as sickness funds in countries that have the social health insurance system or even private companies listed on the stock exchange, for example insurance companies.
In summary, the main arguments of the proponents of the idea of decentralization of public procurement are the following (22):
(a) Reduced incentives for corruption through protectionism or large-scale favoritism.
(b) A better responsiveness of procured goods to the detailed end-user requirements.
(c) Reduced margin of error in contrast to those of large purchases resulting in wasteful and excessive spending.
(d) Less bureaucracy, due to shorter time frames and fewer required forms (applications, supporting documents) for both buyers and suppliers.
(e) Greater opportunities for successful competition for small and medium-sized enterprises.
(f) Opportunities for local buying authorities to purchase at lower prices the locally manufactured products.
(g) Increased scope for work responsibility by employees and development of a spirit of “service.”
However, such a wide variety of decentralized institutional forms raises a number of questions about the key features of decentralization and the ability of smaller decentralized units to respond effectively to the demands of modern healthcare, such as the provision of integrated care to patients with chronic diseases or older adult patients. Questions also arise regarding both the managerial ability of decentralized units to organize and their financial ability to procure key new technologies for their clinical and information systems (26). Collusion and corruption at local level can be another thorny issue, as decentralization can result in a loss of public oversight and quality assurance of products in procurements and the supply chain. But also from an economic aspect, a decentralized approach may promote the development of the private sector and SMEs as mentioned above, but on the other hand may sacrifice the potential advantages of centralized purchasing and the achievement of economies of scale.
In recent years, the above concerns have created a reversal of the trend of decentralization of health systems in some countries to more centralized systems. In particular, the Nordic countries of the EU, such as Sweden, Denmark and Finland but also Central European countries such as Poland and Slovakia which had adopted strategies of decentralization in the health sector, are beginning to recentralize basic functions in their health systems (22).
3.3 Hybrid procurement
Between the decentralized and centralized procurement system, there is also an intermediate system, the hybrid system, in which the central authority and the competent local administrations share decision-making power, as shown in Figure 1C (16).
A quite common example of a hybrid procurement system, is the framework agreement that central purchasing body may conclude on behalf of their regional public administrations (15). According to Directive 2014/24/EU“ framework agreement means an agreement between one or more contracting authorities and one or more economic operators, the purpose of which is to establish the terms governing contracts to be awarded during a given period, in particular with regard to price and, where appropriate, the quantity envisaged” (Directive 2014/24/EU of the European Parliament and of the Council of 26 February 2014 on Public Procurement and Repealing Directive 2004/18/EC Text with EEA Relevance, 2014).
A framework agreement may be concluded:
(a) By a contracting authority to meet its own needs (e.g., the Ministry of Health concludes a framework agreement with three suppliers for the supply of stationery for its departments).
(b) By several contracting authorities or by a contracting authority operating on behalf of several contracting authorities (e.g., the Regional Health Agency concludes a framework agreement with a contractor for the supply of needles to hospitals in its jurisdiction).
(c) By a central purchasing body, acting on behalf of other contracting authorities (e.g., the National Central Health Procurement Authority concludes a framework agreement for all hospitals in the country, with five suppliers for the supply of specific medical equipment).
At this point, it should be noted that the framework agreement is not a new type of public contract, but a contractor selection method, which is not legally binding, unlike individual contracts concluded on the basis of such agreements (27). Therefore, in such a mild centralized arrangement as hybrid, the individual implementing contracts, concluded on the basis of the framework agreement make available to all regional public administrations, various goods to be procured for a given period of time at a specific (often renegotiated) price. Public administrations have the discretion to decide whether to conclude an individual implementing contract on the basis of the framework agreement (recommended), unless the required goods are not available or local suppliers are able to provide similar products in a better price and quality.
For the healthcare sector in particular, the hybrid procurement system can benefit the performance of the healthcare system with some decentralized functions. For example, it can benefit the financing and the programming-drafting of budget, since these functions are likely to require greater flexibility so that they respond to local information. It can also benefit other more centralized functions, such as inventory control, warehousing, product transportation, logistics management information systems, since these functions can benefit from supervision, storage capacity, etc. In addition, the hybrid procurement system can serve national and regional programmes, with central government playing an essential role in the procurement, storage and distribution of selected public health products, such as vaccines (24).
4 Discussion on healthcare procurement systems in the European Union countries
In light of the degree of centralization, we analyse the healthcare procurement system of the European Union countries. Performing a theoretical literature research in combination with the collection, recording, processing and comparison of EU healthcare procurement policies, we attempt to ascertain which type of healthcare procurement is implemented by each EU country and whether or not a central purchasing body (CPB) has been established. The theoretical literature research conducted through valid search engines (PUBMED, Google Scholar) includes scientific articles and electronic repositories, relevant and appropriate publications from primary and secondary sources, bibliography, press articles, conference summaries, legislation and jurisprudence.
The results obtained by the analysis of the healthcare procurement systems of the EU countries, regarding the type of health procurement system based on the degree of centralization as well as the operation of CPBs are as follows (see Table 2):
(a) The EU countries implementing the “centralized” healthcare procurement system are Austria (28–30), Bulgaria (29, 31–33), Cyprus (17, 34, 35), Denmark (17, 36–39), Ireland (29, 40–42), Latvia (29, 43–46), Lithuania (29, 47, 48), Luxembourg (29, 49–51), Malta (29, 52, 53), Portugal (17, 29, 54–58), Romania (29, 59–61), Slovenia (29, 62, 63) and Spain (64–67). There is no tendency toward decentralization in the above countries. Almost all EU countries operating a centralized health procurement system (except Luxembourg and Slovenia) have established central purchasing bodies which are contracting authorities providing centralized purchasing activities.
(b) The EU countries implementing the “decentralized” healthcare procurement system are Belgium (29, 68–72), Czechia (29, 73–75), Estonia (76–78), Finland (29, 38, 43, 79), France (29, 80–82), Germany (29, 83–85), Poland (29, 74, 86), Slovakia (29, 87, 88) and Sweden (29, 89, 90). The vast majority of these countries have in recent years implemented policies of gradual centralization of their procurement in order to achieve economies of scale, save resources, increase transparency of public spending and fight corruption.
(c) The EU countries implementing the “hybrid” healthcare procurement system are Croatia (10, 91–93), Greece (94–97), Italy (12, 29, 38, 98–101) and Hungary (29, 74, 102, 103)).
Procurement is seldom exclusively centralized or decentralized in its entirety (104, 105). In order to classify the healthcare procurement on the basis of centralization, we must first identify the range of capabilities offered within a gradual scale, ranging from minimal coordination between healthcare providers to full bulk purchasing. The choice between a fully centralized and a fully decentralized procurement system comprises some different intermediate forms of operation (106). For example, in the case of Portugal, which applies a mild centralized type of procurement, whose characteristics are quite similar to the hybrid one (107), we have identified four levels of centralization as below:
(a) Centralized
The Centralized model concerns only the development of Framework Agreements, with activity being directed toward issues of market assessment and establishment of technical requirements. This activity is carried out in conjunction with experts from other institutions, whose objective is to regulate the purchase, through the standardization of the technical requirements of the product or service to be purchased. Through this process, the market operators who are able to meet the terms of the agreement are selected and committed to supply their products with the required technical requirements and the agreed prices during the validity of the framework agreement. Healthcare providers develop their respective acquisition procedures under the Framework Agreements.
(b) Centralized aggregate
In the Centralized Aggregate model, in accordance with the Framework Agreements, acquisition processes are developed for a group of institutions, acting on their behalf and as a purchasing center.
(c) Aggregate
In the Aggregate model, a competent body acts as a purchasing center, but the contracting instrument used is not the Framework Agreement, but other public contracting instruments such as public tenders.
(d) Free
The Free model is used by institutions to acquire goods or services that are not included in the other three models, with each institution developing its own acquisition processes.
Several studies have shown that centralized and hybrid procurement systems perform better with respect to decentralized systems (12, 100, 108–110). Based on numerical experimentation, it is generally found that a hybrid combination of the centralized and decentralized procurement types tends to yield the optimal results (104, 110).
5 Conclusions
In this perspective article, employing a narrative approach that summarizes recent interdisciplinary literature on healthcare procurement systems of the European Union countries based on the degree of centralization, we identified three types of organizational structures: Centralized, Decentralized and Hybrid procurement. We discussed the three different ways to organize the procurement function, as well as the advantages and disadvantages of each structural organization. We found that the implementation of healthcare procurement centralization or decentralization in the EU can vary in terms of its forms and levels, influenced by the political and administrative structure of a M-S and the organization of its health system. By consolidating procurement and tendering processes, centralization can generate cost savings in various settings through the advantages of scale and enhanced purchasing ability. For this reason, there has been a growing strategic trend toward centralizing purchases, especially within the EU healthcare systems. Health system performance can be improved through a hybrid procurement model, where certain functions are decentralized, such as financing and planning/budgeting and conversely, other functions, such as control, storage and logistics can be centralized. In this perspective, a combination of centralized and decentralized purchases of medical supplies could represent a promising hybrid type of healthcare procurement organization by bringing the benefits of two systems together. But, striking the appropriate equilibrium between centralization and decentralization is a highly intricate challenge. To effectively combine the potential advantages of both approaches, it is necessary to carefully establish a balance and define the relationships between local and central management of hospital supplies. Policymakers should consider the best practices and lessons learned from each country to improve the efficiency, transparency, and competition of their healthcare procurement systems.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
NG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. PV: Formal analysis, Supervision, Validation, Writing – review & editing. MG: Data curation, Formal analysis, Writing – review & editing. FT: Formal analysis, Validation, Writing – review & editing. GT: Formal analysis, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1359155/full#supplementary-material
References
1. Seidman G, Atun R. Do changes to supply chains and procurement processes yield cost savings and improve availability of pharmaceuticals, vaccines or health products? A systematic review of evidence from low-income and middle-income countries. BMJ Global Health. (2017) 2:e000243. doi: 10.1136/bmjgh-2016-000243
2. WHO. World Report on the Health of Refugees and Migrants. (2022). Available online at: https://www.who.int/publications-detail-redirect/9789240054462 (accessed May 26, 2023).
3. Scholz N. The Public Health Dimension of the European Migrant Crisis. (2016). Available online at: https://www.europarl.europa.eu/RegData/etudes/BRIE/2016/573908/EPRS_BRI(2016)573908_EN.pdf (accessed June 10, 2023).
4. European Commission. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions Making Public Procurement work in and for Europe. (2017). Available online at: https://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:52017DC0572 (accessed May 26, 2023).
5. World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva: World Health Organization (2010). Available online at: https://apps.who.int/iris/handle/10665/258734 (accessed June 12, 2023).
6. Eurostat. Healthcare Expenditure Statistics. (2022). Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthcare_expenditure_statistics (accessed Jun 21, 2023).
7. Current Healthcare Expenditure, 2020 Health2022.png. Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Current_healthcare_expenditure,_2020_Health2022.png (accessed Jun 21, 2023).
8. Healthcare Expenditure, Analysed by Provider, 2020 (% of current healthcare expenditure) Health2022.png. Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Healthcare_expenditure,_analysed_by_provider,_2020_(%25_of_current_healthcare_expenditure)_Health2022.png (accessed Jun 21, 2023).
9. Healthcare Expenditure, Analysed by Function, 2020 (% of current healthcare expenditure) Health2022.png. Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Healthcare_expenditure,_analysed_by_function,_2020_(%25_of_current_healthcare_expenditure)_Health2022.png (accessed Jun 21, 2023).
10. European Commission DG for M and HA, Weistra K, Swart L, Oortwijn W, Raets T, Slot B. Updated Study on Corruption in the Healthcare Sector: Final Report. LU: Publications Office of the European Union (2017). Available online at: https://data.europa.eu/doi/10.2837/68580 (accessed May 26, 2023).
11. European Parliament, Council of the EU. Directive 2014/24/EU of the European Parliament and of the Council of 26 February 2014 on public procurement and repealing Directive 2004/18/EC Text with EEA relevance. OJ L, Directive 2014/24/EU. Available online at: http://data.europa.eu/eli/dir/2014/24/oj/eng (accessed February 26, 2014).
12. Baldi S, Vannoni D. The impact of centralization on pharmaceutical procurement prices: the role of institutional quality and corruption. Reg Stud. (2017) 51:426–38. doi: 10.1080/00343404.2015.1101517
13. Bakker E, Walker H, Schotanus F, Harland C. Choosing an organisational form: the case of collaborative procurement initiatives. Int J Procure Manage. (2008) 1:297–317. doi: 10.1504/IJPM.2008.017527
14. Petersen OH, Jensen MD, Bhatti Y. The effect of procurement centralization on government purchasing prices: evidence from a field experiment. Int Public Manage J. (2022) 25:24–42. doi: 10.1080/10967494.2020.1787278
15. Dimitri N, Dini F, Piga G. When should procurement be centralized? In:Nicola Dimitri G, Spagnolo G, editors. Handbook of Procurement. Cambridge, MA: Cambridge University Press (2006), p. 47–81. doi: 10.1017/CBO9780511492556.004
16. McCue CP, Pitzer JT. Centralized vs. decentralized purchasing: current trends in governmental procurement practices. J Public Budg Account Financial Manag. (2000) 12:400–20. doi: 10.1108/JPBAFM-12-03-2000-B003
17. Vogler S, Bauer E, Habimana K. Centralised pharmaceutical procurement: learnings from six European countries. Appl Health Econ Health Policy. (2022) 20:637–50. doi: 10.1007/s40258-022-00729-w
18. Coe CK. Public financial management / Charles K. Coe. - Vanderbilt University. Prentice Hall (1989). Available online at: https://catalog.library.vanderbilt.edu/discovery/fulldisplay/alma991004559539703276/01VAN_INST:vanui (accessed May 27, 2023).
19. Institute of Medicine. Saving Lives, Buying Time: Economics of Malaria Drugs in an Age of Resistance. Washington, DC: National Academies Press; 2004. Available online at: http://www.nap.edu/catalog/11017 (accessed May 27, 2023).
20. UNICEF. UNICEF's Engagement with Gavi, the Vaccine Alliance | UNICEF. (2020). Available online at: https://www.unicef.org/documents/unicefs-engagement-gavi-vaccine-alliance (accessed May 27, 2023).
21. WHO. Malaria and HIV/AIDS Interactions and Implications: Conclusions of a Technical Consultation Convened by WHO, 23-25 June 2004. World Health Organization; 2004. Report No.: WHO/HIV/2004.08. Available online at: https://apps.who.int/iris/handle/10665/70076 (accessed May 27, 2023).
22. OECD. Centralised and Decentralised Public Procurement. (2000). Available online at: https://www.oecd-ilibrary.org/governance/centralised-and-decentralised-public-procurement_5kml60w5dxr1-en (accessed May 27, 2023).
23. Abimbola S, Baatiema L, Bigdeli M. The impacts of decentralization on health system equity, efficiency and resilience: a realist synthesis of the evidence. Health Policy Plan. (2019) 34:605–17. doi: 10.1093/heapol/czz055
24. Millington KA, Bhardwaj M. Evidence and Experience of Procurement in Health Sector Decentralisation - GSDRC. (2017). Available online at: https://gsdrc.org/publications/evidence-and-experience-of-procurement-in-health-sector-decentralisation/ (accessed May 27, 2023).
25. Weber M. The Theory of Social and Economic Organization, 1st American ed. (Parsons T, editor). New York, NY: Oxford University Press (1947), 436.
26. Saltman RB, Bankauskaite V, Vrangbæk K. Decentralization in Health Care: Strategies and Outcomes. McGraw-Hill; 2007. (European Observatory on Health Systems and Policies Series). Available online at: https://eurohealthobservatory.who.int/publications/m/decentralization-in-health-care-strategies-and-outcomes (accessed May 27, 2023).
27. OECD. Manual for Framework Agreements. (2014). Available online at: https://www.oecd.org/gov/ethics/manual-framework-agreements.pdf (accessed May 27, 2023).
28. Bundesbeschaffung GmbH. Information about the Company | Federal Procurement GmbH. Available online at: https://www.bbg.gv.at/unternehmen/infos-zum-unternehmen (accessed June 6, 2023).
29. European Commission. Inforegio - Stock-Taking of Administrative Capacity, Systems and Practices Across the EU to Ensure the Compliance and Quality of Public Procurement Involving European Structural and Investment (ESI) Funds. (2016). Available online at: https://ec.europa.eu/regional_policy/information-sources/publications/studies/2016/stock-taking-of-administrative-capacity-systems-and-practices-across-the-eu-to-ensure-the-compliance-and-quality-of-public-procurement-involving-european-structural-and-investment-esi-funds_en (accessed May 27, 2023).
30. Bachner F, Bobek J, Habimana K, Ladurner J, Lepuschutz L, Ostermann H, et al. Austria: health system review. Health Syst Transit. (2018) 20:1–254.
31. Republic of Bulgaria. Public procurement agency - AOP. Available online at: https://www2.aop.bg/aop/agenciya-po-obshtestveni-porychki/ (accessed June 6, 2023).
32. Republic of Bulgaria. Ministry of Finance: Centralised Contracting and Public Procurement. Available online at: https://www.minfin.bg/en/52 (accessed June 6, 2023).
33. Dimova A, Rohova M, Koeva S, Atanasova E, Koeva-Dimitrova L, Kostadinova T, et al. Bulgaria: health system review. Health Syst Transit. (2018) 20:1–230.
34. Tsiolas TA. Cypriot MoH. MINISTRY OF HEALTH - Purchasing and Supply Directorate. Available online at: https://www.moh.gov.cy/moh/moh.nsf/page67_en/page67_en?OpenDocument (accessed May 28, 2023).
35. Theodorou M, Charalambous C, Petrou C, Cylus J. Cyprus health system review. Health Syst Transit. (2012) 14:1–128.
36. International Trade Administration. Healthcare Resource Guide - Denmark. Available online at: https://www.trade.gov/healthcare-resource-guide-denmark (accessed June 6, 2023).
37. European Health Public Procurement Alliance. Denmark - AMGROS. Available online at: https://www.ehppa.com/Members/3/5/1010 (accessed June 6, 2023).
38. OECD. Centralised Purchasing Systems in the European Union. Paris: OECD (2011). Available online at: https://www.oecd-ilibrary.org/governance/centralised-purchasing-systems-in-the-european-union_5kgkgqv703xw-en (accessed June 6, 2023).
39. Olejaz M, Juul Nielsen A, Rudkjøbing A, Okkels Birk H, Krasnik A, Hernández-Quevedo C. Denmark health system review. Health Syst Transit. (2012) 14:i–xxii, 1–192.
40. Government of Ireland. Department of Health Statement of Strategy 2021-2023. (2021). Available online at: https://www.gov.ie/en/organisation-information/0fd9c-department-of-health-statement-of-strategy-2021-2023/ (accessed June 6, 2023).
41. Health Service Executive. Procurement. Available online at: https://www.hse.ie/eng/about/who/finance/nationalfinance/procurement/procurement.html (accessed June 6, 2023).
42. McDaid D, Wiley M, Maresso A, Mossialos E. Health systems in transition Ireland: health system review. Health Syst Transit. (2009) 11:1–268.
43. Finnish Ministry of Economic Affairs and Employment. Työ- ja elinkeinoministeriö. Public Procurement Legislation. Available online at: https://tem.fi/en/public-procurement-legislation (accessed June 10, 2023).
44. Vogler S, Haasis MA, van den Ham R, Humbert T, Garner S, Suleman F. European collaborations on medicine and vaccine procurement. Bull World Health Organ. (2021) 99:715–21. doi: 10.2471/BLT.21.285761
45. Latvian Ministry of Health. Centralised Procurement of Personal Protective Equipment | COVID-19. (2020). Available online at: http://covid19.gov.lv/en/atbalsts-sabiedribai/ekonomika/uznemejiem/centralised-procurement-personal-protective-equipment (accessed June 10, 2023).
46. Behmane D, Dudele A, Villerusa A, Misins J, Klavina K, Mozgis D, et al. Latvia: health system review. Health Syst Transit. (2019) 21:1–165.
47. Murauskiene L, Thomson S. Can People afford to Pay for health Care?: New Evidence on Financial Protection in Lithuania: Summary. Copenhagen: World Health Organization. Regional Office for Europe (2018). Available online at: https://apps.who.int/iris/handle/10665/345679 (accessed June 6, 2023).
48. Murauskiene L, Janoniene R, Veniute M, van Ginneken E, Karanikolos M. Lithuania: health system review. Health Syst Transit. (2013) 15:1–150.
49. Luxembourg- Luxembourg Hospital Federation (FHL). Available online at: https://www.ehppa.com/Members/3/5/5 (accessed June 6, 2023).
50. Portail des Marchés Publics. Direction des Marchés Publics. (2021). Available online at: http://marches.public.lu/fr/acteurs/direction.html (accessed June 6, 2023).
51. World Health Organization, Regional Office for Europe, European Observatory on Health Systems and Policies, Berthet F, Calteux A, Wolter M, et al. Luxembourg: HiT in Brief. World Health Organization; Regional Office for Europe (2015). Available online at: https://iris.who.int/handle/10665/333260
52. health.gov.mt. Central Procurement & Supplies Unit. Available online at: https://healthservices.gov.mt/en/cpsu/Pages/Home.aspx (accessed June 6, 2023).
53. Azzopardi-Muscat N, Buttigieg S, Calleja N, Merkur S. Malta: health system review. Health Syst Transit. (2017) 19:1–137.
54. EHPPA. European Health Public Procurement Alliance. Portugal- SPMS. Available online at: https://www.ehppa.com/Members/3/5/9 (accessed May 28, 2023).
55. República D da. Decree Law No. 19/2010. Republic Diary. Sect. 1, 19 Mar 22, 2010, p. 900–6. Available online at: https://dre.pt/dre/en/detail/decree-law/19-2010-611341
56. About Public Procurement - SPMS. Available online at: https://www.spms.min-saude.pt/as-compras-publicas/ (accessed May 28, 2023).
57. Vogler S, Habimana K, Haasis MA. Purchasing medicines for the public sector: evaluation of the performance of centralised procurement in Portugal. Int J Health Plann Manage. (2022) 37:2007–31. doi: 10.1002/hpm.3444
58. de Almeida Simoes J, Augusto GF, Fronteira I, Hernandez-Quevedo C. Portugal: health system review. Health Syst Transit. (2017) 19:1–184.
59. Legislative Portal. EMERGENCY ORDER 46 31/05/2018 - Regarding the Establishment, Organization and Operation of the National Office for Centralized Procurement, The Government of Romania. (2018). Available online at: https://legislatie.just.ro/Public/DetaliiDocument/201404 (accessed June 6, 2023).
60. National Office for Centralized Procurement. Legislation. Available online at: https://onac.gov.ro/legislatie/ (accessed June 6, 2023).
61. Vladescu C, Scintee SG, Olsavszky V, Hernandez-Quevedo C, Sagan A. Romania: health system review. Health Syst Transit. (2016) 18:1–170.
62. International Trade Administration. Slovenia - Medical Equipment. Available online at: https://www.trade.gov/country-commercial-guides/slovenia-medical-equipment-0 (accessed June 6, 2023).
63. Albreht T, Polin K, Pribaković Brinovec R, Kuhar M, Poldrugovac M, Ogrin Rehberger P, et al. Slovenia: health system review. Health Syst Transit. (2021) 23:1–183.
64. Ministerio De Sanidad. The Centralized Purchase Web Platform of the SNS Incorporates a New Catalog with 25,000 Medicines and Health Products. (2019). Available online at: https://www.sanidad.gob.es/gabinete/notasPrensa.do?id=4515 (accessed May 28, 2023).
65. Consorci de Salut i Social de Catalunya. Who we are and What we do | Pharmacy and Medication. Available online at: http://www.consorci.org/farmacia-medicament/en_index/ (accessed May 28, 2023).
66. EHPPA. European Health Public Procurement Alliance. Spain-Catalan Health and Social Care Consortium (Consorci CSC). Available online at: https://www.ehppa.com/Members/3/5/1011 (accessed May 28, 2023).
67. Bernal-Delgado E, Garcia-Armesto S, Oliva J, Sanchez Martinez FI, Repullo JR, Pena-Longobardo LM, et al. Spain: health system review. Health Syst Transit. (2018) 20:1–179.
68. The Belgian State Structure & the Language Differences Make an Unitary Structure Almost Impossible | healthproceurope.org. (2020). Available online at: https://healthproceurope.org/country-perspective-belgium/ (accessed June 6, 2023).
69. De Regge M, De Pourcq K, Van de Voorde C, Van den Heede K, Gemmel P, Eeckloo K. The introduction of hospital networks in Belgium: the path from policy statements to the 2019 legislation. Health Policy. (2019) 123:601–5. doi: 10.1016/j.healthpol.2019.05.008
70. European Health Public Procurement Alliance. Belgium-Mercurhosp. Available online at: https://www.ehppa.com/Members/3/5/3 (accessed June 6, 2023).
71. Hebert G. Pooling procurement in the Belgian hospital sector. World Hosp Health Serv. (2011) 47:27–30.
73. International Trade Administration. Healthcare Resource Guide - Czech Republic. Available online at: https://www.trade.gov/healthcare-resource-guide-czech-republic (accessed June 6, 2023).
74. Public Procurement in Poland, Hungary, the Czech Republic, and Ukraine - Трансперенсі Інтернешнл Україна. (2021). Available online at: https://ti-ukraine.org/en/news/public-procurement-in-poland-hungary-the-czech-republic-and-ukraine/ (accessed June 18, 2023).
75. Bryndová L, Šlegerová L, Votápková J, Hrobon P, Shuftan N, Spranger A. Czechia: health system review. Health Syst Transit. (2023) 25:1–216.
76. Figueras J, Robinson R, Jakubowski E. Purchasing to Improve Health Systems Performance. McGraw-Hill Education(2005).
77. Habicht T. Pricing and Reimbursement Policies in Estonian Pharmaceutical Market. World Bank 2(018). 1. (Other Health Study). Available online at: https://elibrary.worldbank.org/doi/abs/10.1596/34189 (accessed June 6, 2023).
78. Habicht T, Reinap M, Kasekamp K, Sikkut R, Aaben L, van Ginneken E. Estonia: health system review. Health Syst Transit. (2018) 20:1–189.
79. Keskimaki I, Tynkkynen LK, Reissell E, Koivusalo M, Syrja V, Vuorenkoski L, et al. Finland: health system review. Health Syst Transit. (2019) 21:1–166.
80. AccParAdmin. Access Partnership. Public Procurement and Cloud Service Providers in France. (2018). Available online at: https://accesspartnership.com/public-procurement-and-cloud-service-providers-in-france/ (accessed May 28, 2023).
81. Le Resah - RESAH. Available online at: https://www.resah.fr/Presentation-resah/2/5 (accessed May 28, 2023).
82. Chevreul K, Berg Brigham K, Durand-Zaleski I, Hernandez-Quevedo C. France: health system review. Health Syst Transit. (2015) 17:1–218, xvii.
83. Van den Mooter B. Linkedn. Comparing Purchasing Processes for Surgical Devices and Medical Equipment in the US, Japan and Germany | LinkedIn. (2017). Available online at: https://www.linkedin.com/pulse/comparing-purchasing-processes-surgical-devices-us-van-den-mooter/ (accessed June 10, 2023).
84. EHPPA. Germany - EK UNICO. Available online at: https://www.ehppa.com/Members/3/5/6 (accessed June 10, 2023).
85. Blümel M, Spranger A, Achstetter K, Maresso A, Busse R. Germany: health system review. Health Syst Transit. (2020) 22:1–272.
86. Sowada C, Sagan A, Kowalska-Bobko I, Badora-Musial K, Bochenek T, Domagala A, et al. Poland: health system review. Health Syst Transit. (2019) 21:1–234.
87. Ministry of Finance of the Slovak Republic M of H. Ministry of Finance of the Slovak Republic. Healthcare Spending Review II, Final Report. (2020). Available online at: https://www.mfsr.sk/files/archiv/77/HealthcareSpendingReview2_EN.pdf (accessed June 18, 2023).
88. Smatana M, Pazitny P, Kandilaki D, Laktisova M, Sedlakova D, Paluskova M, et al. Slovakia: health system review. Health Syst Transit. (2016) 18:1–210.
89. Carlsson P, Jonsson E, Werkö L, Banta D. Health technology assessment in Sweden. Int J Technol Assess Health Care. (2000) 16:560–75. doi: 10.1017/S0266462300101151
90. Anell A, Glenngård AH, Merkur S. Sweden health system review. Health Syst Transit. (2012) 14:1–159.
91. European Observatory on Health Systems and Policies, Vončina L, Sagan A. New joint hospital procurement programme in Croatia. Eurohealth. (2014) 20:29–32. Available online at: https://iris.who.int/bitstream/handle/10665/332841/Eurohealth-20-2-29-32-eng.pdf (accessed February 7, 2024).
92. Vončina L, Strizrep T, Bagat M, Pezelj-Duliba D, Pavić N, Polašek O. Croatian 2008-2010 health insurance reform: hard choices toward financial sustainability and efficiency. Croat Med J. (2012) 53:66–76. doi: 10.3325/cmj.2012.53.66
93. Džakula A, Vocanec D, Banadinovic M, Vajagic M, Loncarek K, Lukacevic Lovrencic I, et al. Croatia: health system review 2021. Health Syst Transit. (2021) 23:i−146.
94. Economou C, Kaitelidou D, Karanikolos M, Maresso A. Greece: health system review. Health Syst Transit. (2017) 19:1–166.
95. EKAPY. EKAPY-Purpose/Vision. Available online at: https://ekapy.gov.gr/skopos-orama/ (accessed May 28, 2023).
96. Kastanioti C, Kontodimopoulos N, Stasinopoulos D, Kapetaneas N, Polyzos N. Public procurement of health technologies in Greece in an era of economic crisis. Health Policy. (2013) 109:7–13. doi: 10.1016/j.healthpol.2012.03.015
97. Directorate-General for Economic and Financial Affairs (European Commission). Post-Programme Surveillance Report. Greece, Autumn 2022 (European Economy Institutional Papers). Report No.: 191. (2022), p. 1–56. Available online at: https://economy-finance.ec.europa.eu/publications/post-programme-surveillance-report-greece-autumn-2022_en (accessed May 28, 2023).
98. International Trade Administration. Healthcare Resource Guide - Italy. Available online at: https://www.trade.gov/healthcare-resource-guide-italy (accessed May 28, 2023).
99. Italy-SCR Piemonte. Available online at: https://www.ehppa.com/Members/3/5/7 (accessed June 6, 2023).
100. Ferraresi M, Gucciardi G, Rizzo L. Savings from public procurement centralization in the healthcare system. Eur J Polit Econ. (2021) 66:101963. doi: 10.1016/j.ejpoleco.2020.101963
101. Giulio de. Belvis A, Meregaglia M, Morsella A, Adduci A, Perilli A, Cascini F, et al. Italy: health system review. Health Syst Transit. (2022) 24:1–236.
102. Közbeszerzési Hatóság. Welcome to the Website of the Public Procurement Authority of Hungary - Foportál. Available online at: http://www.kozbeszerzes.hu/english/ (accessed June 18, 2023).
103. Gaal P, Szigeti S, Csere M, Gaskins M, Panteli D. Hungary health system review. Health Syst Transit. (2011) 13:1–266.
104. Munson CL. The appeal of partially centralised purchasing policies. Int J Procur Manag. (2007) 1:117–43. doi: 10.1504/IJPM.2007.015358
105. Kanepejs E, Kirikova M. Centralized vs. Decentralized Procurement: A Literature Review. (2018). Available online at: https://www.semanticscholar.org/paper/Centralized-vs.-Decentralized-Procurement%3A-A-Review-Kanepejs-Kirikova/11003631fca882ddd0210ae241d6e607132e7fa3 (accessed Jun 21, 2023).
106. Gianfredi V, Filia A, Rota MC, Croci R, Bellini L, Odone A, et al. Vaccine procurement: a conceptual framework based on literature review. Vaccines. (2021) 9:1434. doi: 10.3390/vaccines9121434
107. Rego N, Claro J, Pinho de Sousa J. A hybrid approach for integrated healthcare cooperative purchasing and supply chain configuration. Health Care Manag Sci. (2014) 17:303–20. doi: 10.1007/s10729-013-9262-y
108. Lucchese A, Marino A, Ranieri L. Minimization of the logistic costs in healthcare supply chain: a hybrid model. Procedia Manuf. (2020) 42:76–83. doi: 10.1016/j.promfg.2020.02.025
109. Karjalainen K. Estimating the cost effects of purchasing centralization—Empirical evidence from framework agreements in the public sector. J Purch Supply Manag. (2011) 17:87–97. doi: 10.1016/j.pursup.2010.09.001
110. Dameri RP, Benevolo C, Rossignoli C, Ricciardi F, De Marco M. Centralization vs. decentralization of purchasing in the public sector: the role of e-procurement in the italian case. In:Khachidze V, Wang T, Siddiqui S, Liu V, Cappuccio S, Lim A, editors. Contemporary Research on E-business Technology and Strategy. Berlin, Heidelberg: Springer (2012), p. 457–70 (Communications in Computer and Information Science). doi: 10.1007/978-3-642-34447-3_41
Keywords: public procurement, health system, medical supplies, centralization, hybrid model, European Union
Citation: Geropoulos N, Voultsos P, Geropoulos M, Tsolaki F and Tagarakis G (2024) Hybrid model: a promising type of public procurement in the healthcare sector of the European Union. Front. Public Health 12:1359155. doi: 10.3389/fpubh.2024.1359155
Received: 20 December 2023; Accepted: 29 January 2024;
Published: 15 February 2024.
Edited by:
Alexandre Morais Nunes, University of Lisbon, PortugalReviewed by:
Nuno Costa, Serviços Partilhados do Ministério da Saúde Ministos, PortugalCopyright © 2024 Geropoulos, Voultsos, Geropoulos, Tsolaki and Tagarakis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nikolaos Geropoulos, bmdlcm9wb3VAYXV0aC5ncg==
 Nikolaos Geropoulos
Nikolaos Geropoulos Polychronis Voultsos
Polychronis Voultsos Miltiadis Geropoulos
Miltiadis Geropoulos Fani Tsolaki4
Fani Tsolaki4 Georgios Tagarakis
Georgios Tagarakis