- 1Department of Biostatistics and Epidemiology, Hudson College of Public Health, University of Oklahoma Health Sciences Center, Oklahoma City, OK, United States
- 2Oklahoma State Department of Health, Oklahoma City, OK, United States
Introduction: Susceptibility predicts subsequent uptake of e-cigarettes (EC) by youth. This study identified factors associated with EC susceptibility among high school students who have never used a tobacco/nicotine product.
Methods: The Oklahoma Youth Tobacco Survey was administered to a random sample of 36 Oklahoma High Schools during the 2021–2022 school year (n = 1,220 participating students). Associations between EC susceptibility and covariates were identified using stepwise logistic regression for weighted survey data.
Results: More than one third of Oklahoma high school students who had never used tobacco or nicotine products (36.4%) were susceptible, and males had higher susceptibility than females (38.8 and 33.9%, respectively). In males, EC susceptibility was associated with race (Black, American Indian, and other were less susceptible), psychological distress (aOR = 2.4, 95% CI = 1.1, 4.8), disagreement that all tobacco products are dangerous (aOR = 3.1, 95% CI = 1.2, 7.9), and perception of little/no harm from secondhand vapor (aOR = 3.4, 95% CI = 2.1, 5.3). In females, identifying as gay, lesbian, or bisexual (aOR = 2.1, 95% CI = 1.1, 3.9), poor academic performance (aOR = 4.5, 95% CI = 1.6, 12.6), psychological distress (aOR = 2.6, 95% CI = 1.2, 5.5) and interacting with EC content on social media (aOR = 5.9, 95% CI = 1.9, 18.1) were associated with EC susceptibility.
Conclusion: Males and females had different patterns of susceptibility to EC use. Understanding groups of adolescents most susceptible to using nicotine products can help target prevention efforts at home, in schools, and within communities.
Background/Introduction
Electronic cigarette (EC) use among youth remains problematic and can lead to other forms of nicotine dependence, including smoking (1, 2). Previous research suggests adolescents who regularly used vaping products are up to four times more likely to have smoked in the past 30-days or to have initiated smoking (1). Similarly, there is a strong association between smoking initiation and regular vaping product use among youth (2).
Most adult tobacco use begins with tobacco experimentation during adolescence (1, 2). Of the wide array of tobacco products available, current high school (HS) students most often choose to experiment with ECs. In 2018, Gentzke and associates reported an adolescent 30-day EC prevalence of 27.7% using data from the National Youth Tobacco Survey (YTS) (3). This prevalence dropped to 19.6% in 2020 (4), 11.3% in 2021, and is currently 14.1% in 2022 (5, 6). While this drop in 30-day prevalence during the last 2 years is encouraging, EC use continues to be a concern, and a significant proportion of adolescents remain susceptible to initiation.
Several research studies have documented factors associated EC use in youth, including identifying as White, using other tobacco products, and having family members who use tobacco of any kind (7). Stress is also associated with both EC and tobacco use and can be related to school grades, peer pressure, gender diversity, and other stressors (7–10). Harm perception or the perception that ECs are less harmful and/or addictive than smoking traditional tobacco products is strongly associated with EC use among youth (8–10), as is exposure to EC advertisement and marketing. Alternatively, television, radio, and social media messaging exposing the dangers associated with tobacco use can increase the perception of harm and decrease susceptibility to tobacco initiation (11, 12).
Preventing initiation is an important step in averting nicotine dependence (1). Susceptibility precedes initiation of tobacco use of any kind (1). EC susceptibility is defined as a lack of firm, decisive, and robust denial of interest in initiating EC use among never users (1, 13, 14). Several studies have reported a strong association between EC susceptibility and initiation within youth (15–17).
A number of studies have evaluated susceptibility to EC use among adolescents, and findings vary based on sampling methods and measures. EC susceptibility has been associated with believing that ECs are less harmful than combustible tobacco products (18–20), believing that ECs are less addictive than combustible tobacco products (21), and having higher affluence (19, 22). Additional factors associated with EC susceptibility include being exposed to EC advertising (22), living in a household where members use ECs (18), and having family members or friends who smoke or vape (21, 22). Conversely, identifying as Black (18), Hispanic (18, 20), and female (18, 20) have been associated with a protective effect with regard to EC susceptibility. Studies limiting the analytic sample to youth who have never used any nicotine product are uncommon. The aim of this study was to determine variables associated with EC susceptibility among high school youth in Oklahoma who have never used any tobacco or nicotine product, including ECs.
Methods
Data
Data for this study were obtained from the Oklahoma Youth Tobacco Survey (OYTS), administered from November 2021 through May 2022. A multi-stage sampling design was used to draw the sample of students. The first stage involved selecting a random sample of public high schools. The second stage involved selecting three classes from each school, using simple random sampling without replacement. Finally, all students in each class were offered the opportunity to take the online survey. The OYTS included a final sample of 36 public high schools with a total sample size of 1,220 students. The analytic sample used in this study was students who never used any tobacco or nicotine product, and with complete information about grade level and age required for accurate weighting (n = 780).
Outcome variable
Susceptibility to EC use was defined using the susceptibility index previously developed and validated for smoking susceptibility (1) and determined from the following four questions: “Have you ever been curious about using an e-cigarette?,” “Do you think you will try an e-cigarette soon?,” “Do you think you will use an e-cigarette in the next year?,” and “If one of your best friends were to offer you an e-cigarette, would you use it?” Possible answers included “definitely yes,” “probably yes,” “probably not,” and “definitely not.” Students were considered susceptible if they responded with any answer except “definitely not” to any of those questions.
Measures
Demographic variables
Covariates included ethnicity, categorized as Hispanic or non-Hispanic; race, categorized as American Indian, Black, White, or other; grade level categorized as freshman/sophomore or junior/senior; and sex, categorized as male or female. Finally, students were asked if they spoke a language other than English in the home, with responses dichotomized as yes or no.
Sexual identity
When asked, “Which of the following best describes you?,” respondents self-identified into the following categories: straight; gay, lesbian, or bisexual; and unsure.
Grades in school
Respondents were asked, “During the last 12 months, how would you describe your grades in school?” Responses were coded as “As and Bs”; “C’s or lower”; and “graded on another scale or unsure.” Students graded on another scale were either on a pass/fail grading scale or using an individualized education plan for special education purposes.
Family affluence score
An affluence score was assigned based on four questions; “Does your family own a vehicle?” (no = 0, one = 1, and two or more = 2), “Do you have your own bedroom?” (no = 0 and yes = 1), “How many computers does your family own?” “(none = 0, one = 1, two = 2, and more than two = 3),” and “how many times in the last 12 months have you traveled on vacation with your family?” (Not at all = 0, once = 1, twice = 2, and more than twice = 3). Responses were summed with scores of five or less coded “low affluence,” and scores of six or more coded “high affluence,” consistent with prior studies (3–6).
Psychological distress
A psychological distress score was assigned based on four questions; “During the past 2 weeks, how often have you been bothered by having little interest or pleasure in doing things?,” “During the past 2 weeks, how often have you been bothered by feeling down, depressed, or hopeless?,” “During the past 2 weeks, how often have you been bothered by feeling nervous, anxious, or on edge?,” and “During the past 2 weeks, how often have you been bothered by feeling like you are not able to stop or control worrying?” Each question was coded not at all = 0, several days = 1, more than half of the days = 2, and nearly every day = 3. Consistent with prior literature, responses were summed with scores of five or less coded “none or low distress,” and scores six or more coded “moderate or severe” (3–6).
Harm perception
Four questions were used to determine EC harm perception. First, “How much do you think people harm themselves when they use ECs some days but not every day?” Responses of “No harm” or “a little harm” were combined and compared to “some harm” or “a lot of harm” combined. Next, responses to “Do you believe that ECs are (less addictive, equally addictive, or more addictive) than cigarettes?” were dichotomized as “equally/less/do not know” combined and compared to “more addictive.” Third, agreement with the statement “All tobacco products are dangerous” was assessed. Those who responded, “strongly agree” or “agree” were combined and compared to those who responded “disagree” or “strongly disagree.” Fourth, Do you think that breathing the vapor from other people’s EC causes “no harm,” “a little harm,” “some harm,” or “a lot of harm.” Respondents answering, “no harm” or “a little harm” were combined and compared to those who answered, “some harm” or “a lot of harm” (3–6).
Anti-tobacco messaging
Respondents were asked two questions about anti-tobacco messaging. Youth who responded yes to seeing or hearing The Real Cost ads in the past 12 months, and those selecting one or more anti-tobacco names or slogans they may have seen in the past 12 months were considered to have been exposed. Answers were summed and then dichotomized into 0 or 1 and 2 or more (3–6).
EC and tobacco product marketing
Exposure to EC and other tobacco marketing was assessed separately and from questions about four different sources: retail stores; internet; television, streaming services, or movies; and newspapers or magazines. Respondents were asked, “When you are using ‘each of these services’ how often do you see ads or promotions (for ECs; for cigarettes or tobacco products)?” Respondents could answer never, rarely, sometimes, most of the time, or always. They received one point for each answer of sometimes, most of the time, or always. Answers were summed and then dichotomized into 0 or 1 and 2 or more (2–4).
Social media
Among students responding they use social media, we captured social media exposure based on four questions. First, we asked “How often do you use social media?” Second, we asked “When you use social media, how often do you see posts of content related to e-cigarettes?” To assess interaction with social media, we then asked the following two questions: “When you use social media, how often do you post pictures of yourself or someone else using e-cigarettes?” and “When you use social media, how often have you liked, commented, or shared posts or content related to e-cigarettes?” We dichotomized each question separately, with those responding monthly or more frequently combined and compared to those responding, “less than monthly or never to these questions” (3–6). Those responding that they do not use social media were categorized in the “less than monthly or never” category.
Statistical methods
Data were weighted to adjust for nonresponse and varying probabilities of selection with the underlying population of interest, with extreme weights trimmed. The weighting procedures included base weight, nonresponse adjustment, calibration, and trimming; done to incorporate sampling randomness, reduce nonresponse bias, and improve efficiency. Bivariate associations between covariates and the outcome variable, EC susceptibility, were examined using a Rai-Scott Chi-square test. Weighted multivariable logistic regression was conducted, analyzing the association between EC susceptibility and the series of independent variables using a stepwise selection procedure. Collinearity and interactions were examined in building the final model. Adjusted odds ratios were obtained for the association between EC susceptibility and independent variables. Respondents with missing outcome values were excluded from bivariate and multivariate analysis. Because there was an interaction with sex, all results are presented separately for males and females. All statistical analyses were conducted in SAS® 9.4 (Carey, NC) with an alpha = 0.05. All statistical analyses incorporate design information including final weight, stratification, and clustering. The protocol was approved by Institutional Review Boards at both the Oklahoma State Department of Health (#21–12) and the University of Oklahoma Health Sciences Center (#13847).
Results
Among students who had never used a tobacco or nicotine product, 24% self-identified as American Indian, 11% as Black, 60% as White, and 5% as a member of another race. Most students (82%) self-identified as being “straight” regarding sexual identity, and 78% reported earning A or B grades in school. A high percentage of female students were experiencing psychological distress compared to males (22.1% versus 8.4%). Most students (90%) agreed or strongly agreed that “all tobacco products are dangerous.” More than one-third (37%) responded that breathing vapor from other people’s ECs causes “little” or “no” harm. About half (48%) had seen two or more anti-tobacco advertisements in the past 12 months, and 92% were exposed to e-cigarette advertising in the past 12 months. Regarding social media, 41% of students had seen EC content on social media “monthly or more often,” while 8% had posted pictures, commented on, or shared posts about ECs (Table 1).
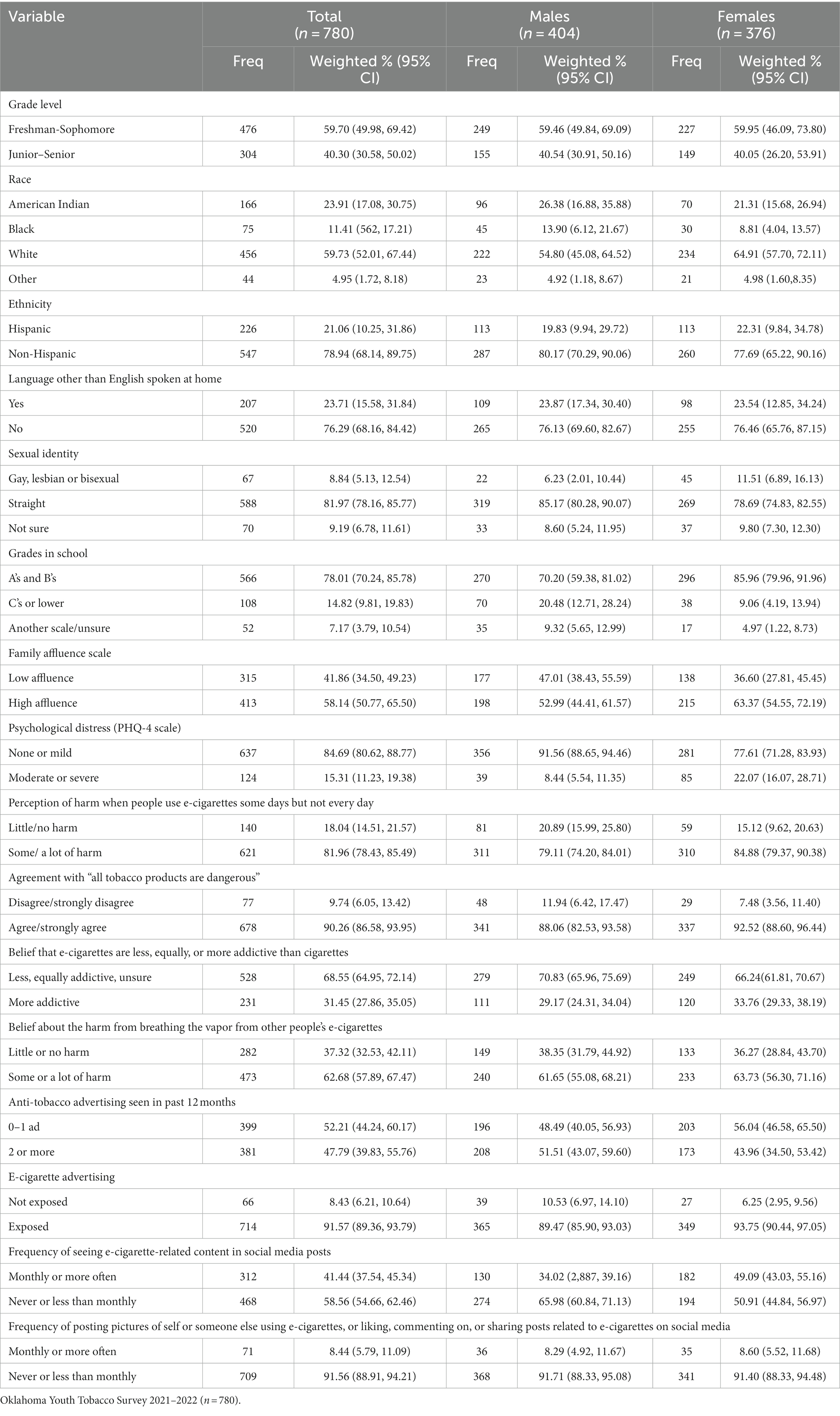
Table 1. Characteristics of high school students who have never used tobacco/nicotine products, by sex.
Overall, 36% of students were susceptible to EC use: 39% of males and 34% of females. In males, susceptibility to EC use was higher among White students (44%) than Black (24%), or American Indian (36%) students. A higher proportion of students who self-identified as gay, lesbian, or bisexual (53%) were susceptible to EC use compared to those who self-identified as “straight” (34%). A larger proportion of students earning “C” grades or less were susceptible to EC use (52%) compared to those earning grades of “A” and “B” (34%) grades. More than half of students reporting high levels of psychological distress (53%) were susceptible to EC use compared to those reporting mild or no stress (34%). Overall, a large percentage of students who disagreed or strongly disagreed with the statement that “all tobacco” products are dangerous (51%) were susceptible to EC use compared to those who agreed or strongly agreed (34%). While almost half of all students who thought that “breathing vapor” from other people’s vaping products causes “little” or “no harm” were susceptible (46%), susceptibility was higher in males (52%), compared to females (39%). Of students who posted pictures of themselves or someone else using vaping products on social media, or who commented on, or shared posts related to ECs monthly or more often, 62% were susceptible overall (65% of males and 58% of females) (Table 2).
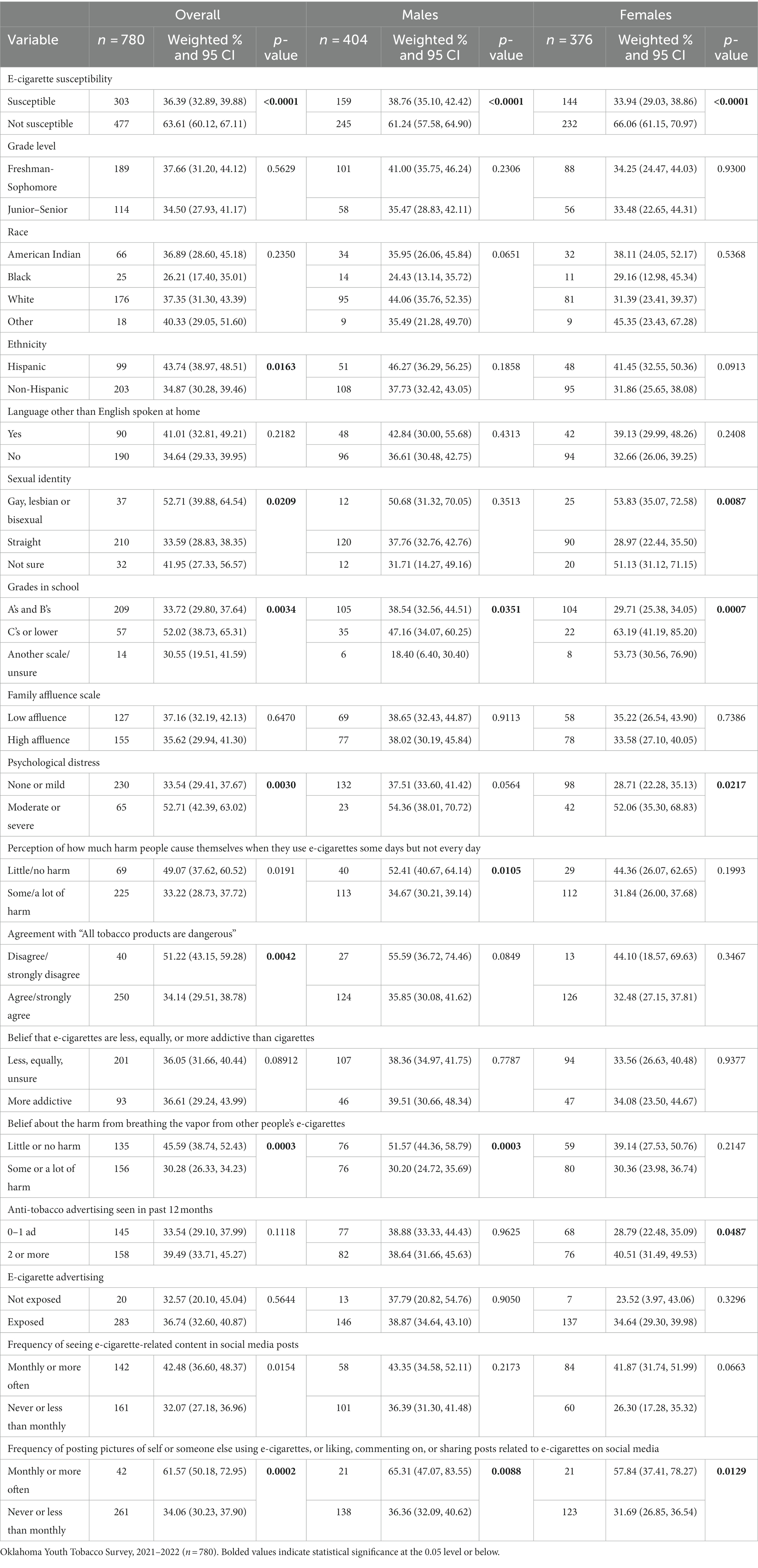
Table 2. E-cigarette susceptibility among high school students who never used tobacco/nicotine products by sex and variables of interest.
Multivariate analysis results for males and females
Males
When compared to white male students, after adjusting for other variables in the model, the odds of susceptibility to EC use in American Indian and Black male students were lower (aOR = 0.46, 95% CI = 0.23, 0.90 and 0.44, 95% CI = 0.20, 0.96, respectively). In male students, the odds of EC susceptibility were also considerably lower among those who were graded on a different grading scale (aOR = 0.31 with 95% CI = 0.14, 0.70) compared to those who made “A” or “B” grades. After adjusting for other variables in the model, the odds of EC susceptibility in male students who reported moderate or severe levels of psychological stress were more than twice as high as for those reporting mild or no stress (aOR = 2.35, 95% CI = 1.14, 4.81). Likewise, the odds of EC susceptibility among male students who disagreed or strongly disagreed with the statement “all tobacco products are dangerous” were three times higher (aOR = 3.07, 95% CI = 1.19, 7.92) compared to those who agreed or strongly agreed. The odds EC susceptibility among those who perceived little or no harm from breathing vapor from other people’s ECs were more than three times higher when compared to those who perceived some or a lot of harm (aOR = 3.35 with 95%CI = 2.12, 5.30) (Table 3).
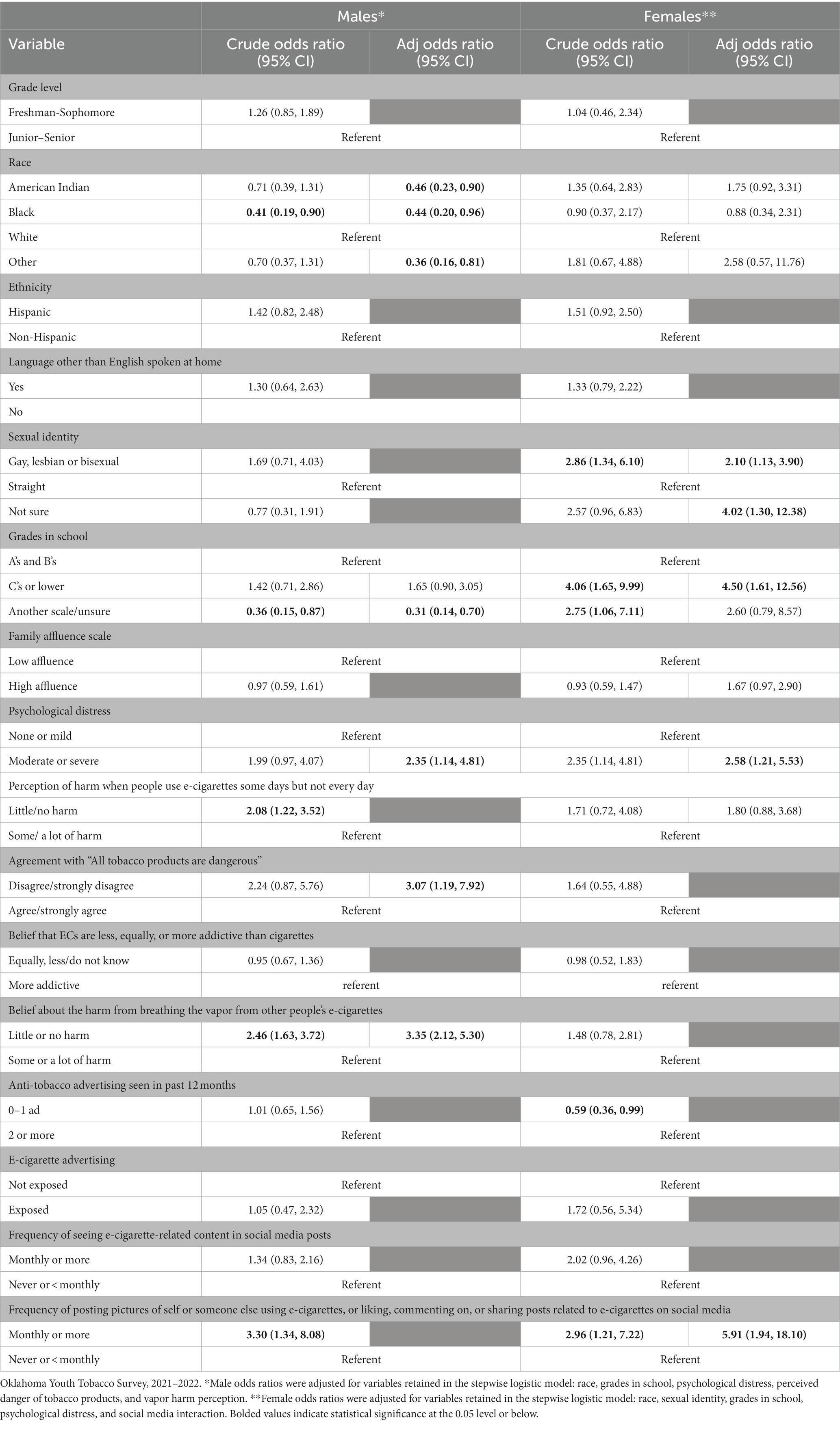
Table 3. Factors associated with e-cigarette susceptibility, by sex, crude, and adjusted odds ratios with 95% CIs.
Females
After adjusting for other variables in the model, the odds of EC susceptibility among females self-identifying as gay, lesbian, or bisexual were two times higher (aOR = 2.10, 95% CI = 1.13, 3.90), and for those who were unsure of their sexual identity, the odds were four times higher (aOR = 4.02, 95% CI = 1.30, 12.38) compared to those who self-identified as “straight.” The odds of susceptibility among female students who made “C” grades or lower were more than four times higher than for those making “A” or “B” grades (aOR = 4.50, 95% CI = 1.61, 12.56) and were almost three times higher for those under moderate or severe psychological stress compared to those with mild or no stress (aOR = 2.58, 95% CI = 1.21, 5.53). The odds of susceptibility to EC use in female students who interacted about EC use on social media were almost six times higher than for those who did not (aOR = 5.91, 95%CI = 1.94, 18.10) (Table 3).
Discussion
More than one third of HS students who never used tobacco products were found to be susceptible to EC use. Patterns of susceptibility differed between male and female students. White males were more likely to be susceptible than Black or American Indian males. As reported by others (18, 20), this study found an association between identifying as White and EC susceptibility; however, in our study this only occurred with male students. Male students with low levels of EC/tobacco harm perception were more likely to be susceptible to EC initiation. Females, however, demonstrated an association between susceptibility and both psychological stress, as well as poorer academic performance. Females who interacted in social media about EC products were also more likely to be susceptible to EC initiation. Understanding these differences can assist with focused and evidence-based tobacco/nicotine prevention measures. An important step in tobacco prevention is averting tobacco initiation and susceptibility among youth, especially with popular tobacco products like ECs (1, 2).
Amrock and associates reported a study suggesting that adolescents cannot accurately assess the potential danger of ECs. They noted those who believe ECs are less harmful than combustible tobacco products are more likely to initiate their use (9). In our study, harm perception was only associated with EC susceptibility in male students and in only two of the four harm perception questions, agreeing that “all tobacco products are dangerous,” and that “breathing vapor from other’s ECs causes some or a lot of harm.” Because other authors have reported associations between harm perception and 30-day vaping prevalence (7, 17, 23, 24), continued public health education efforts are warranted. Previous research has reported that heightened harm perception is associated with lower EC susceptibility (with odds ratios between 0.60 and 0.23) (20, 21), while lower levels of harm perception have been associated with increases EC susceptibility (with odds ratios ranging from 2.2 to 4.9) (18).
Students experience a wide variety of stressors during their high school years. In this study, a higher percentage of female students demonstrated psychological distress, which in turn was associated with a higher level of susceptibility to EC use, after controlling for other covariates. Both male and female students experiencing distress had a higher prevalence of susceptibility. Female students demonstrated an association between grades earned in school and susceptibility; and had a higher odds of EC susceptibility when their grades dropped lower than a “B” level. Interestingly, Jha and associates found youth who needed stress relief were more likely to use ECs (13). However, the youth who attempted EC use as a form of stress relief reported higher stress levels after use. Research suggests EC prevention strategies for high school students should focus on stress reduction and healthy coping strategies (9, 22, 25).
While exposure to EC advertising on social media was not associated with EC susceptibility in either male or female students, active interaction on social media sites was. In female students, posting pictures, making comments about, or interacting with others about EC use was highly associated with EC susceptibility. A similar finding was reported by Vogel and associates, who found students who engaged in social media on a regular basis demonstrated higher intent to use ECs, along with a lower perception of the danger of EC use (26). This finding warrants further investigation about the potential success of monitoring social media sites in youth at risk for tobacco use, and providing intervention before initiation occurs.
This study adds information not yet published about differences in susceptibility in male and female adolescent students. Because this study was conducted with students who had never used any type of nicotine or tobacco product, these results are also unique. Limitations of the current study warrant discussion. This is a cross sectional study, and as such, causal inferences are not valid. While this study involved youth in Oklahoma, the sample of high school students never using nicotine and tobacco products was relatively small (n = 780) and from a single state; thus, generalizability may be limited. Sample sizes for several sub-groups of interest in this study were small, specifically those involving racial and sexual minority groups. Although weighting procedures intend to account for non-response, the overall response rate of schools and classrooms was less than optimal (44%). Finally, all estimates are based on self-reported data, which might be affected by information bias. As is typical with most surveys, data for all factors likely to be associated with susceptibility were not included.
Understanding EC susceptibility can assist with focused and evidence-based tobacco/nicotine prevention measures. An important step in tobacco prevention is averting tobacco initiation and susceptibility among youth.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the University of Oklahoma Health Sciences Center. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SJ: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft. AW: Formal analysis, Investigation, Writing – review & editing. FK: Funding acquisition, Supervision, Validation, Writing – review & editing. NM: Formal analysis, Investigation, Supervision, Writing – review & editing. SC: Formal analysis, Software, Supervision, Writing – review & editing. LB: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. SC was partially supported by the Oklahoma Shared Clinical and Translational Resources (U54GM104938) with an Institutional Development Award (IDeA) from NIGMS. The content was solely the responsibility of the authors and does not necessarily represent official views of the National Institutes of Health or the Indian Health Service.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Soneji, S, Barrington-Trimis, JL, Wills, TA, Leventhal, AM, Unger, JB, Gibson, LA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. (2017) 171:788–97. doi: 10.1001/jamapediatrics.2017.1488
2. O’Brien, D, Long, J, Quigley, J, Lee, C, McCarthy, A, and Kavanagh, P. Association between electronic cigarette use and tobacco cigarette smoking initiation in adolescents: a systematic review and meta-analysis. BMC Public Health. (2021) 21:954. doi: 10.1186/s12889-021-10935-1
3. Gentzke, AS, Creamer, M, Cullen, KA, Ambrose, BK, Willis, G, Jamal, A, et al. Vital signs: tobacco product use among middle and high school students - United States, 2011-2018. MMWR Morb Mortal Wkly Rep. (2019) 68:157–64. doi: 10.15585/mmwr.mm6806e1
4. Gentzke, AS, Wang, TW, Jamal, A, Park-Lee, E, Ren, C, Cullen, KA, et al. Tobacco product use among middle and high school students - United States, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1881–8. doi: 10.15585/mmwr.mm6950a1
5. Gentzke, AS, Wang, TW, Cornelius, M, Park-Lee, E, Ren, C, Sawdey, MD, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021. MMWR Surveill Summ. (2022) 71:1–29. doi: 10.15585/mmwr.ss7105a1
6. Park-Lee, E, Ren, C, Cooper, M, Cornelius, M, Jamal, A, and Cullen, KA. Tobacco product use among middle and high school students—United States, 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:1429–35. doi: 10.15585/mmwr.mm7145a1
7. Moustafa, AF, Rodriguez, D, Mazur, A, and Audrain-McGovern, J. Adolescent perceptions of E-cigarette use and vaping behavior before and after the EVALI outbreak. Prev Med. (2021) 145:106419. doi: 10.1016/j.ypmed.2021.106419
8. Ma, J, Kraus, AJ, Owens, C, Moskowitz, DA, Birnholtz, J, and Macapagal, K. Perspectives on cigarette use, vaping, and Antitobacco campaigns among adolescent sexual minority males and gender diverse youth. LGBT Health. (2022) 9:479–88. doi: 10.1089/lgbt.2021.0460
9. Amrock, SM, Zakhar, J, Zhou, S, and Weitzman, M. Perception of e-cigarette harm and its correlation with use among U.S. adolescents. Nicotine Tob Res. (2015) 17:330–6. doi: 10.1093/ntr/ntu156
10. Vogel, EA, Henriksen, L, Schleicher, NC, and Prochaska, JJ. Young people’s e-cigarette risk perceptions, policy attitudes, and past-month nicotine vaping in 30 U.S. cities. Drug Alcohol Depend. (2021) 229:109122. doi: 10.1016/j.drugalcdep.2021.109122
11. Wang, L, Chen, J, Ho, SY, Leung, LT, Wang, MP, and Lam, TH. Exposure to e-cigarette advertising, attitudes, and use susceptibility in adolescents who had never used e-cigarettes or cigarettes. BMC Public Health. (2020) 20:1349. doi: 10.1186/s12889-020-09422-w
12. Wang, Y, Duan, Z, Weaver, SR, Self-Brown, SR, Ashley, DL, Emery, SL, et al. Association of e-cigarette advertising, parental influence, and peer influence with US adolescent e-cigarette use. JAMA Netw Open. (2022) 5:e2233938. doi: 10.1001/jamanetworkopen.2022.33938
13. Pierce, JP, Choi, WS, Gilpin, EA, Farkas, AJ, and Merritt, RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. (1996) 15:355–61. doi: 10.1037/0278-6133.15.5.355
14. Cheng, HG, Lizhnyak, PN, Knight, NA, Vansickel, AR, and Largo, EG. Youth susceptibility to tobacco use: is it general or specific? BMC Public Health. (2021) 21:1913. doi: 10.1186/s12889-021-11956-6
15. Cole, AG, Kennedy, RD, Chaurasia, A, and Leatherdale, ST. Exploring the predictive validity of the susceptibility to smoking construct for tobacco cigarettes, alternative tobacco products, and E-cigarettes. Nicotine Tob Res. (2019) 21:323–30. doi: 10.1093/ntr/ntx265
16. Nicksic, NE, and Barnes, AJ. Is susceptibility to E-cigarettes among youth associated with tobacco and other substance use behaviors one year later? Results from the PATH study. Prev Med. (2019) 121:109–14. doi: 10.1016/j.ypmed.2019.02.006
17. Carey, FR, Wilkinson, AV, Harrell, MB, Cohn, EA, and Perry, CL. Measurement and predictive value of susceptibility to cigarettes, e-cigarettes, cigars, and hookah among Texas adolescents. Addict Behav Rep. (2018) 8:95–101. doi: 10.1016/j.abrep.2018.08.005
18. Tackett, AP, Keller-Hamilton, B, Hébert, ET, Smith, CE, Wallace, SW, Stevens, EM, et al. Adolescent susceptibility to E-cigarettes: an update from the 2018 National Youth Tobacco Survey. Am J Health Promot. (2021) 35:551–8. doi: 10.1177/0890117120971121
19. Kaleta, D, Niedzin, M, Jankowska, A, and Polańska, K. Predictors of E-cigarette use susceptibility-a study of young people from a socio-economically disadvantaged rural area in Poland. Int J Environ Res Public Health. (2019) 16:3935. doi: 10.3390/ijerph16203935
20. Margolis, KA, Thakur, SK, Nguyen Zarndt, A, Kemp, CB, and Glover-Kudon, R. E-cigarette susceptibility among U.S. middle and high school students: National Youth Tobacco Survey Data Trend Analysis, 2014-2018. Prev Med. (2021) 143:106347. doi: 10.1016/j.ypmed.2020.106347
21. Kwon, E, Seo, DC, Lin, HC, and Chen, Z. Predictors of youth e-cigarette use susceptibility in a U.S. nationally representative sample. Addict Behav. (2018) 82:79–85. doi: 10.1016/j.addbeh.2018.02.026
22. Pettigrew, S, Santos, JA, Li, Y, Jun, M, Anderson, C, and Jones, A. Short report: factors contributing to young people's susceptibility to e-cigarettes in four countries. Drug Alcohol Depend. (2023) 250:109944. doi: 10.1016/j.drugalcdep.2023.109944
23. Vu, T-HT, Groom, A, Hart, JL, Tran, H, Landry, RL, Ma, JZ, et al. Socioeconomic and demographic status and perceived health risks of E-cigarette product contents among youth: results from a National Survey. Health Promot Pract. (2020) 21:148S–56S. doi: 10.1177/1524839919882700
24. Duke, JC, Farrelly, MC, Alexander, TN, MacMonegle, AJ, Zhao, X, Allen, JA, et al. Effect of a National Tobacco Public Education Campaign on Youth’s risk perceptions and beliefs about smoking. Am J Health Promot. (2018) 32:1248–56. doi: 10.1177/0890117117720745
25. Jha, V, and Kraguljac, A. Assessing the social influences, self-esteem, and stress of high school students who vape. Yale J Biol Med. (2021) 94:95–106.
Keywords: susceptibility, electronic cigarettes (e-cigarettes), vaping, youth tobacco prevention, youth tobacco survey
Citation: James SA, White AH, Kahn FF, Mushtaq N, Chen S and Beebe LA (2024) Susceptibility to e-cigarette use and associated factors in high school youth, Oklahoma Youth Tobacco Survey, 2021–2022. Front. Public Health. 12:1348926. doi: 10.3389/fpubh.2024.1348926
Edited by:
Thivanka Muthumalage, Purdue University, United StatesReviewed by:
Mark A. Gottlieb, Northeastern University, United StatesRobert J. Wellman, UMass Chan Medical School, United States
Copyright © 2024 James, White, Kahn, Mushtaq, Chen and Beebe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shirley A. James, c2hpcmxleS1qYW1lc0BvdWhzYy5lZHU=
 Shirley A. James
Shirley A. James Ashley H. White
Ashley H. White Fahad F. Kahn2
Fahad F. Kahn2 Nasir Mushtaq
Nasir Mushtaq Sixia Chen
Sixia Chen Laura A. Beebe
Laura A. Beebe