- 1College of Nursing, Jinzhou Medical University, Jinzhou, China
- 2Department of Science and Technology, Jinzhou Medical University, Jinzhou, China
Introduction: Chronic diseases are becoming a serious threat to the physical and mental health of older people in China as their aging process picks up speed. Home hospice care addresses diverse needs and enhances the quality of life for older adult individuals nearing the end of life. To ensure the well-being of chronically ill older adults at the end of life, it is vital to explore and assess the multidimensional hospice needs of terminally ill older individuals in their homes. The aim of this study was to investigate the current situation of home hospice care needs of Chinese older adults with chronic diseases at the end of life, and to analyze the influencing factors (sociodemographic and disease-related factors).
Methods: In this cross-sectional study, 247 older adult people with chronic diseases at the end of life were selected from the communities of 4 community health service centers in Jinzhou City, Liaoning Province from June to October 2023 by random sampling method. A general information questionnaire and the home hospice care needs questionnaire developed by our research group were used to investigate. Independent samples t-test or one-way ANOVA was used to compare the differences in the scores of different characteristics, and the factors with significant differences were selected for multivariate linear regression analysis to determine the final influencing factors.
Results: The total score of home hospice needs of the dying older adult was 115.70 ± 12, with the mean scores for each dimension in descending order being Information Needs (3.96 ± 0.61), Social Support Needs (3.96 ± 0.44), Spiritual Needs (3.92 ± 0.43), Physical Needs (3.60 ± 0.59), Psychological Needs (3.37 ± 0.65). Status of residence, duration of illness (year), the type of disease, and self-care ability were influential factors in the total score of home hospice needs.
Discussion: The need for hospice care for the terminally ill older adult is high, and healthcare professionals should implement services according to the influencing factors of need to meet their multidimensional needs and improve their quality of life.
1 Introduction
Chronic diseases are non-communicable diseases with a long duration and slow progression, characterized by widespread prevalence, high costs, disability and mortality (1). Since the 1990s, the most common non-communicable diseases, including stroke, ischemic heart disease, cancer and chronic obstructive pulmonary disease, have become the leading causes of death in China (2). Increasing age is the primary risk factor for the increased morbidity and mortality of most chronic diseases (3). China currently has the largest older adult population in the world, with 264 million individuals over 60 making up 18.7% of the overall population (4). It is projected that by 2050, the number of older people in China will reach 400 million, with an aging level of more than 30% (5). With the further intensification of the aging process in China, the issue of end-of-life care for the older adult with chronic diseases is imminent.
In China, most end-of-life patients prefer to spend their final stages of life at home due to limited medical resources and the traditional cultural concept of returning to one’s roots (6, 7). Since 2017, China has explicitly referred to hospice care, end-of-life care and palliative care collectively as hospice care (8). As a type of hospice service, home hospice provides palliative and supportive care to end-of-life patients and their families in their own homes by a team of community medical professionals and social volunteers (9, 10), aiming to meet the multifaceted needs of end-of-life patients and their families and optimize the quality of life of end-of-life patients. Bužgová and Sikorová confirmed that a patient’s overall quality of life can be impacted by unmet hospice needs (11). Therefore, it’s critical to evaluate the multifaceted hospice needs of terminally ill older persons in their homes in order to ensure the well-being of these individuals with chronic illnesses in their latter years. Furthermore, identifying the hospice needs of older adults with complex chronic illnesses is becoming an important concern for health systems (12).
Currently, there are many research investigations on the end-of-life needs of older adult people with cancer at home, such as the physiological need for pain control (13), the psychological need for worry and terror relief (14), the spiritual need for peace of mind (15), and other economic support (16). The complexity and intractability of the needs of senior non-cancer terminally ill patients contribute to the relative paucity of research addressing the needs of these individuals with complicated chronic multimorbidity. Most of the reported needs were related to emotional and/or psychological dimensions (social isolation, depression) (17, 18). Bajwah et al. (19) and Ryan et al. (20) both emphasize the supportive need to address clinical symptoms and maintain their activities of daily living. Older adult people with non-cancer chronic disease at the end of life are likely to experience a heavier symptom burden than those with advanced cancer, meaning that more care needs will be presented.
Western studies have reported sociodemographic and disease-related factors that primarily influence the need for home hospice care for the chronically ill older adult. The majority of research indicates women have a higher need for hospice care than men (21, 22). As older adults age, their physiologic functioning and health levels decline, which may increase the need for hospice care. Relevant research also suggests that economic level, education level, and health insurance are also influential factors in the need for hospice care (21, 23). Disease-related factors indicate that older adults with serious illnesses, such as malignant tumors, or multiple coexisting illnesses, face significant physical, psychological, and spiritual challenges, resulting in more urgent needs in all areas (23). The need for hospice care is often closely related to cultural traditions and social systems, and cultural differences between China and the West have led to differences in the factors influencing the need for home hospice care. Nevertheless, home hospice care has paid relatively little attention in China, and there has not been much research done on the variables that affect it.
This study aims to investigate the multi-dimensional hospice care needs of older adults with end-stage chronic diseases in China’s home environment, taking into account the country’s unique aging conditions. Additionally, it analyzes the sociodemographic and disease-related characteristics influencing factors to provide a basis for the provision of high-quality home hospice services.
2 Materials and method
2.1 Design and samples
This study was a cross-sectional study. A random sampling method was used to include the older adult with chronic diseases at the end of life in the communities belonging to four community health centers (providing home hospice services) in Jinzhou City, Liaoning Province, from June to October 2023, as study subjects. Inclusion criteria for end-of-life older adult: (1) age ≥ 60 years; (2) chronic non-tumor diseases, with 1 or more organs severely impaired in function, no effective means of cure into the terminal stage or patients with malignant tumors into the terminal stage (expected survival ≤6 months); (3) choose to die at home (hospice); (4) clear consciousness, with normal language communication, understanding ability. Exclusion Criteria for end-of-life older adult: (1) hospitalized or living in nursing homes; (2) dying in the middle or withdrawing for reasons. The Jinzhou Medical University College of Nursing Ethics Committee gave its approval to the study (No. JZMULL2023062). Every older adult person who was recruited for the study was required to give written informed consent before taking part. G*Power 3.1 was used to calculate the sample size. The effect size was 0.15 (medium size), the significance level α was set at 0.05, and the statistical power (1-β) was 0.90. The minimum sample size was 183 cases. A total of 260 questionnaires were finally distributed.
2.2 Measurement
2.2.1 General information questionnaire
The general information questionnaire was developed by searching the relevant literature and the clinical experience of the investigators. It covers data on disease-related as well as sociodemographic characteristics. Sociodemographic characteristics included gender, age, marital status, education level, medical insurance payment method, religion, status of residence, and household incomes per capita (yuan). Disease-related information comprised the duration of illness (year), number of comorbidities (kind), the type of disease, and self-care ability. Socio-demographic characteristics were collected by self-reporting, and part of the disease-related data (duration of illness, the type of disease) were filled in by the researcher through medical records.
2.2.2 Home hospice care needs questionnaire for the dying older adult
The home hospice care needs questionnaire for the dying older adult (HHCNQ-DE) was an assessment tool developed by our research group to assess the home hospice care needs of the dying older adult in China. From April to September 2023, a total of 5 hospice pilot community health service centers were selected from 7 administrative districts in Jinzhou City, Liaoning Province by stratified sampling method. Secondly, a simple random sampling method was used to select a total of 199 terminally older adult people from the communities of pilot community service centers for psychological verification. The questionnaire had been psychologically validated and the instrument was found to have good reliability and validity. The Cronbach’s alpha coefficient of the total questionnaire was 0.832, the Cronbach’s alpha coefficients of the dimensions were 0.845–0.942, and the re-test reliability was 0.806. The content validity index of the questionnaire was 0.982, and the content validity index of the items was 0.83–1.00. The exploratory factors were extracted from the five common factors, and the cumulative variance contribution was 68.811%. The questionnaire included physiological needs (9 items), spiritual needs (7 items), psychological needs (6 items), social support needs (5 items) and information needs (4 items) 5 dimensions, a total of 31 items. Likert 5-point scale was used for each item, ranging from 1 to 5 points from “not needed” to “very needed.” The total questionnaire scores ranged from 31 to 155, with higher scores indicating higher levels of need. Among them, < 104 was defined as low need, 104–115 was defined as medium need, and > 115 was defined as high need.
2.3 Data collection
The household survey was carried out by the researcher as the investigator, and the community nurses in charge of home follow-up in each community health center assisted in the survey implementation. Before the survey, the purpose and significance of the study were explained to the respondents, and an informed consent form was signed. Then, we explained the requirements for filling out the questionnaire and asked the older adult to fill out the questionnaire on their own after they fully understood it. For those who were illiterate or physically weak, the researchers would read and explain the questionnaire item by item to the respondents, and finally record the survey results truthfully. The time limit for answering the questionnaire was 20 min. The survey was conducted at a time when the older adult had enough sleep and were not undergoing nursing care or treatment. Incomplete or single-option questionnaires were considered invalid.
2.4 Statistical analysis
Epidata 3.1 software was used for double entry of raw values and SPSS22.0 (IBM Corp, Armonk, NY) software was used for statistical analysis of data. The two-sided test level was α = 0.05, and the difference was statistically significant at p < 0.05.
General information about the study participants was described using frequency and component ratio, and the HHCNQ-DE total and dimension need scores were described using mean and standard deviation. To analyze differences, first, independent samples t-tests (variables grouped into two groups) and one-way ANOVA (variables grouped into three or more groups) were used to initially explore the relationship between the home hospice need dimension scores and general information about study participants. Second, using the HHCNQ-DE total score and the scores of the five dimensions as dependent variables, the statistically significant independent variables in the one-way analysis of variance were selected for multiple linear regression analyses (α in = 0.05, α out = 0.10) to find out the influencing factors of the total needs and the needs of the dimensions.
3 Results
3.1 Participant characteristics
A total of 260 questionnaires were distributed in this study, and 247 meeting the requirements were recovered, with a response rate of 95%. 13 invalid questionnaires were excluded, among which 9 refused to answer part of the questions in the questionnaire due to personal reasons, resulting in incomplete questionnaires. Four were excluded because the subjects filled in their errors.
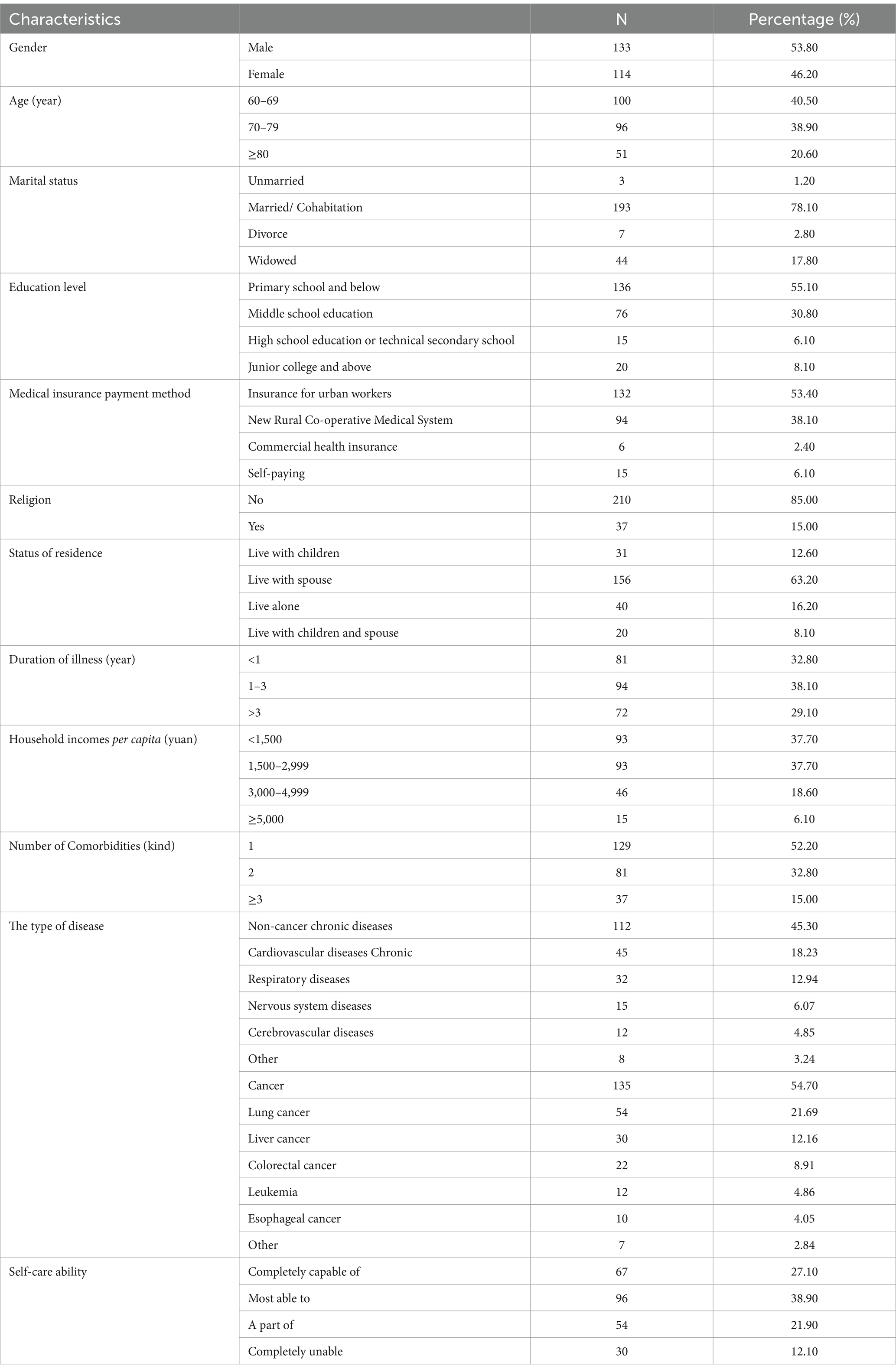
More than half (53.80%) of the older adult dying of chronic diseases were women. The majority were 60–69 years old (40.50%), married or cohabiting (78.10%), with a primary school education or below (55.10%), using medical insurance for urban workers (53.40%), not practicing any religion (85.00%), and living with their spouses (63.20%). The most common type of disease was cancer (54.70%), of which lung cancer was more prevalent (40.00%). Among non-cancer chronic diseases, Cardiovascular diseases were more prevalent (40.18%). Table 1 displayed more general study population data.
3.2 Home hospice care needs score
The older adult with chronic diseases had a total score of 115.70 ± 12.79 for home hospice needs, with a mean score of 3.73 ± 0.41 for all items. The mean scores of the items of the dimensions of the needs in descending order were Information Needs (3.96 ± 0.61), Social Support Needs (3.96 ± 0.44), Spiritual Needs (3.92 ± 0.43), Physical Needs (3.60 ± 0.59), Psychological Needs (3.37 ± 0.65). More specific details are displayed in Table 2.
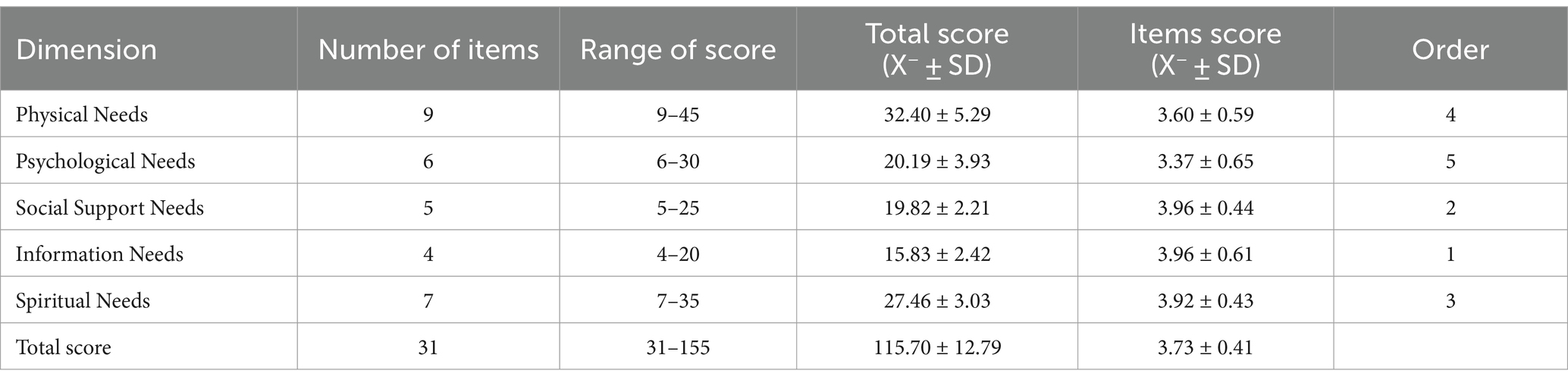
Table 2. Scores for items on dimensions of need for home hospice care for older adult with end-stage chronic disease (N = 247).
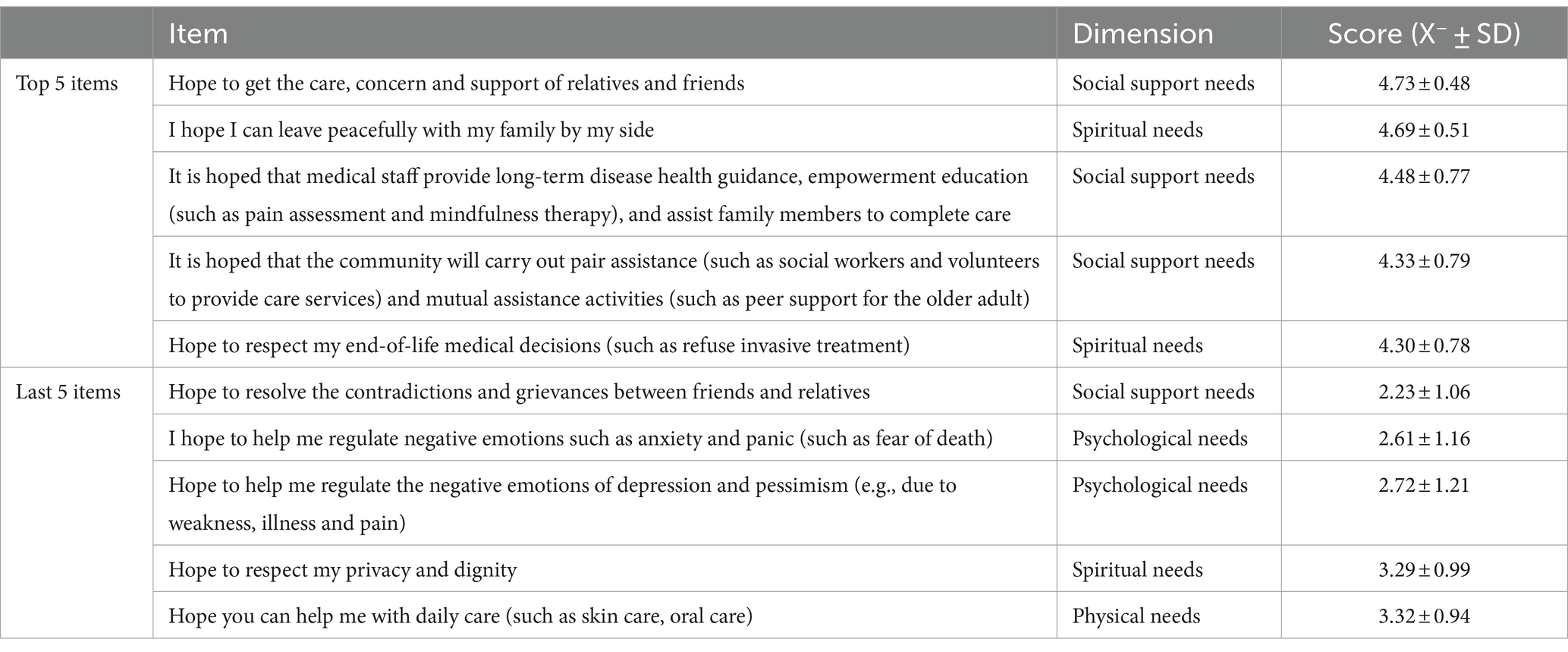
The top and bottom five scoring items for each dimension are displayed in Table 3. The top 5 items were related to the dimensions of Information Needs and Social Support Needs, of which the top 2 need items were “Hope to get the care, concern and support of relatives and friends” (4.73 ± 0.48) and “I hope I can leave peacefully with my family by my side” (4.69 ± 0.51). The last 5 items in the ranking were primarily related to the Psychological Needs dimension, of which the last 2 need items were “Hope to resolve the contradictions and grievances between friends and relatives” (2.23 ± 1.06) and “I hope to help me regulate negative emotions such as anxiety and panic (such as fear of death)” (2.61 ± 1.16).
3.3 Univariate analyses of the home hospice care needs
In Table 4, there were significant differences in the home care needs of older adults with end-stage chronic disease based on several sociodemographic and disease-related factors. Regarding the overall needs score, the dying older adult with older age, lower education, commercial health insurance, religious beliefs, living with children and spouse, long illness duration, monthly household income of 3,000–4,999 yuan, many chronic illnesses, non-cancer chronic disease, and partial able to care had higher HHCNQ-DE scores.
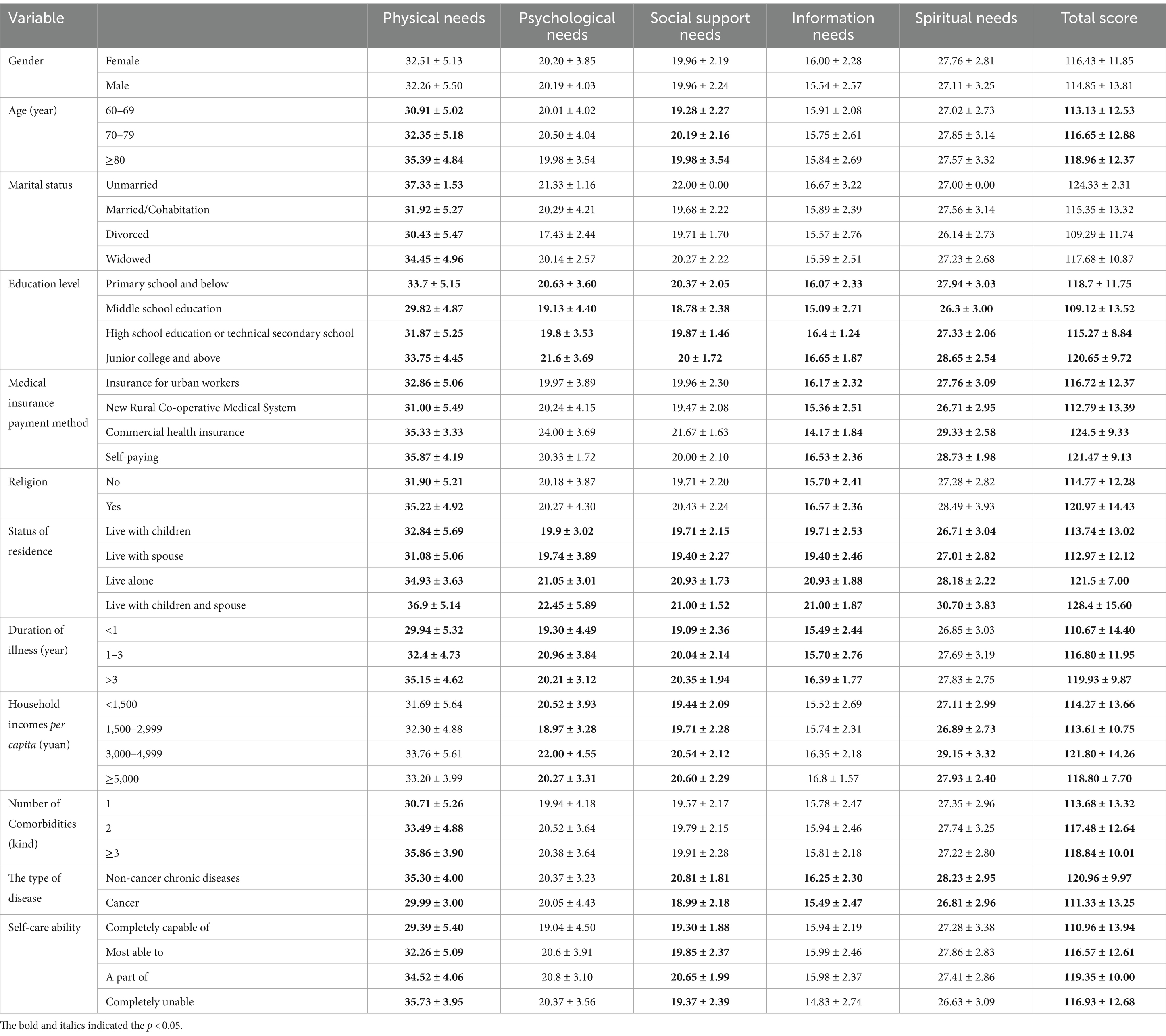
Table 4. Univariate analysis of home hospice care needs (independent samples t-test or one-way analysis of variance, x̄ ±s).
3.4 Multiple linear regression analysis of factors influencing the need for home hospice care
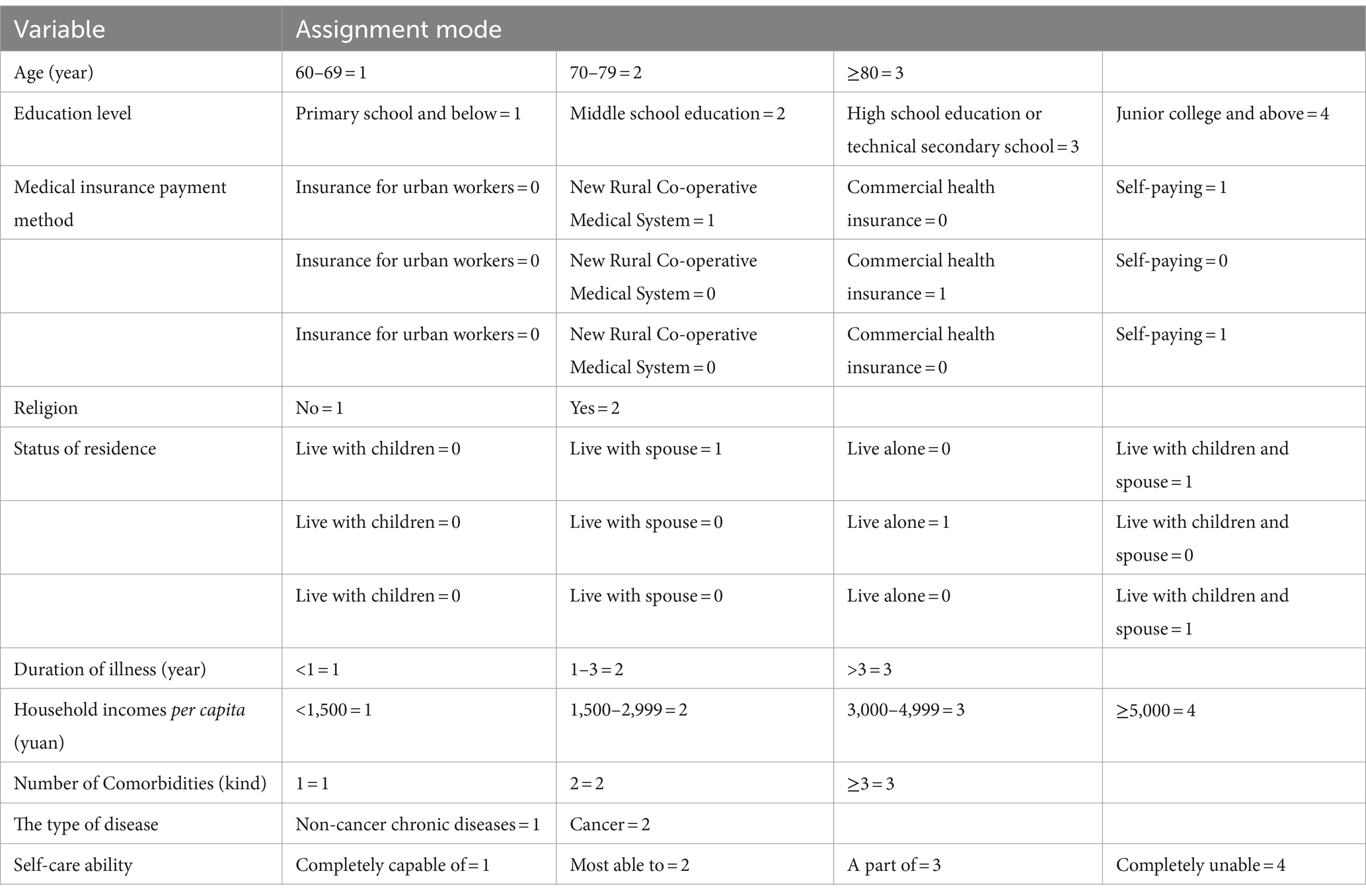
The independent variables medical insurance payment method (based on Insurance for urban workers) and status of residence (based on living with children) were set as dummy variables. Other independent variables were assigned values, like age, which was coded as 1 for 69–69 years, 2 for 70–79 years, and 3 for ≥80 years. The independent variable assignments and dummy variable settings are shown in Table 5.
Six multivariate linear regression analyses were performed to identify significant correlates of overall home hospice needs and five dimensions of needs (see Table 6). The diagnostic test independent variables had all variance inflation factor (VIF) values less than 10, indicating no multicollinearity issue existed before the analysis was conducted. Furthermore, residual analysis provided support for the equation models’ linearity, normality, and homogeneity of variance. The terminal older adult lived with children and spouse (β = 16.385, p = 0.000), had a disease duration ≥3 years (β = 2.721, p = 0.007), had a non-cancer chronic disease (β = −5.874, p = 0.002), and were completely unable to care for themselves (β = 1.919, p = 0.031) may have a higher total need for home hospice care, with 30% of the variance explained. The terminal older adult who used commercial health insurance to pay for health care (β = 3.808, p = 0.031), lived with children and spouse (β = 5.566, p = 0.000), had a disease duration ≥3 years (β = 1.154, p = 0.001), had a comorbid combination of ≥3 chronic diseases (β = 1.302, p = 0.001), with non-cancer chronic diseases (β = −5.874, p = 0.000), and completely unable to care for themselves (β = 1.463, p = 0.031) were more likely to have Physical Needs, explaining 49.6% of the variance. The terminal older adult used commercial medical insurance to pay medical expenses (β = 4.384, p = 0.031), lived with children and spouse (β = 3.925, p = 0.000) and were completely unable to take care of themselves (β = 0.814, p = 0.008) were significantly correlated with Psychological Needs, which explained 11.4% of the variance. Duration of illness ≥3 years (β = 0.421, p = 0.019), comorbidity of ≥3 chronic disease (β = −0.561, p = 0.003), and suffering from non-cancer chronic disease (β = −1.537, p = 0.000) were higher in the terminally ill older adult Social Support Needs, explaining 25.5% of the variance. The use of urban workers’ insurance to pay for medical expenses (β = −2.925, p = 0.005) and living with children and spouse (β = 2.145, p = 0.003) among the terminally ill older adult were significantly associated with Information Needs, explaining 17.2% of the variance. Terminally ill older adult were more likely to express Spiritual Needs by paying for healthcare out-of-pocket (β = 1.689, p = 0.043), living with children and spouse (β = −3.551, p = 0.000), and having a non-cancer chronic disease (β = −1.001, p = 0.037), explaining 19.5% of the variance.
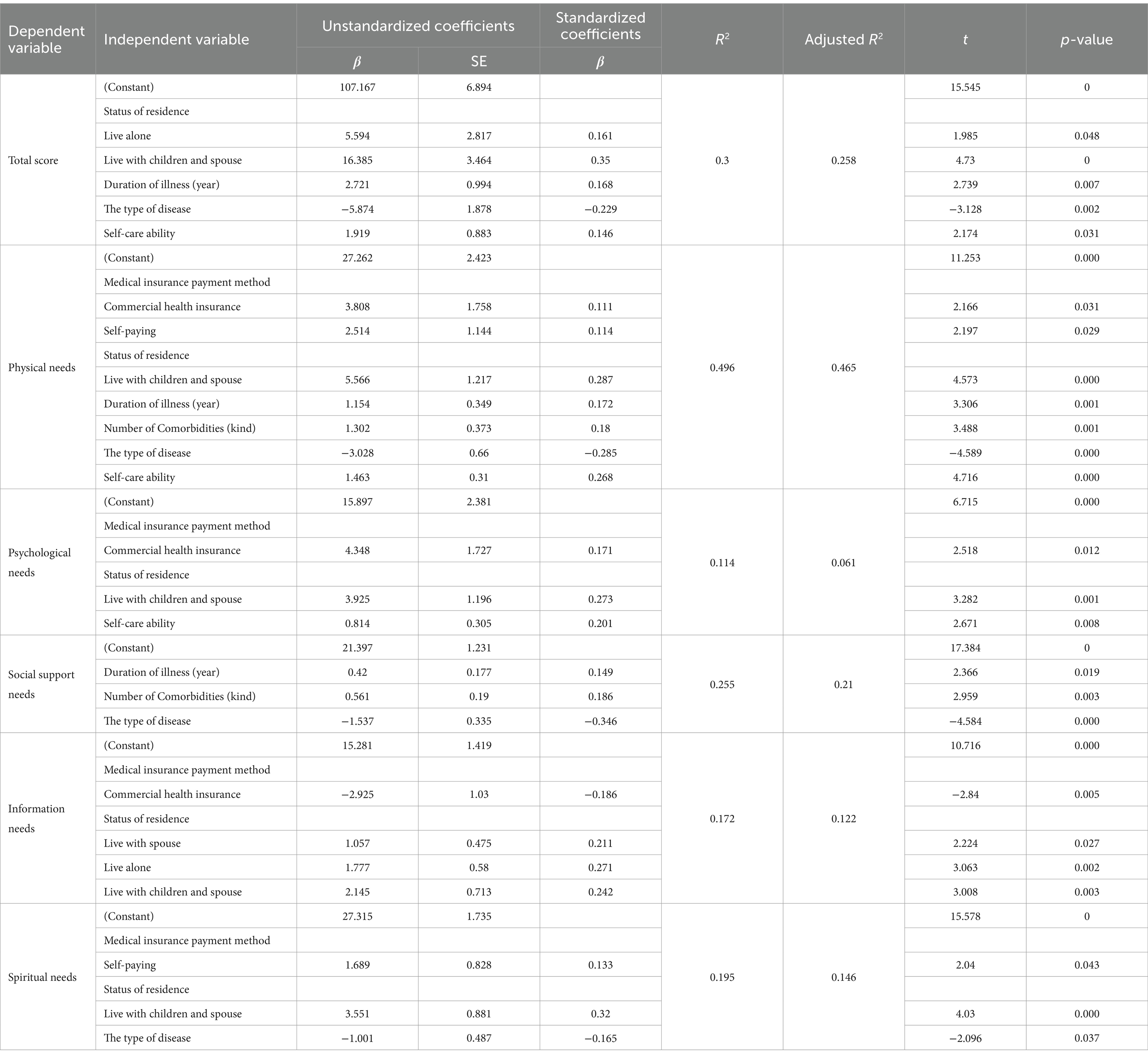
Table 6. Multiple linear regression analysis of total home hospice need and factors influencing need by dimension.
4 Discussion
The results of this study showed that the total score for home hospice needs was 115.70 ± 12.79, indicating that there is a high level of hospice needs for the older adult at the end of life with chronic diseases in the home setting. The highest scoring items were Information Needs, Social Support Needs, and Spiritual Needs in that order, indicating that these three dimensions are of particular concern to the older adult dying at home in China, and that there are still many unmet needs in these three dimensions with the existing medical resources. The three items with higher scores in Social Support Needs implied that the dying older adult longed for assistance from family members, medical staff, social workers, and senior peers, which was similar to the results of Hu et al. (24). The item that received the lowest score in terms of Social Support Needs was “Hope to resolve the contradictions and grievances between friends and relatives,” which suggests that the dying older adult in this study had harmonious relationships with their friends and relatives. Dunham et al. believed that harmonious interpersonal relationships could help older adult cancer patients enhance their sense of self-worth and reduce psychological anxiety (25). Two Spiritual Needs items with higher scores expressed the dying older adult’s need for increased autonomy. Since the older adult are respected in their right to die at home and have essentially had their wish to pass away with dignity fulfilled, the low score for “Hope to respect my privacy and dignity” can be explained.
The dimensions of physical and psychological needs had the lowest mean scores among the items. Ghesquiere demonstrated that older people who had multiple chronic illnesses experienced more depressive feelings along with a greater number of physical symptoms (e.g., pain, and fatigue) (26). Therefore, it is not implied that these two dimensions were met by the study’s low results. The low scores may be because China is deeply influenced by Confucian culture, which is family-centered, and not being a burden to the family is the greatest expectation of the dying older adult (27), which is reflected in the item “Hope to help me with daily care (such as skin care, oral care).” Family members are responsible for personal care, symptom management, and emotional support for the dying older adult, and the responsibility of caring for them makes the caregiver’s burden of care heavy. In order to minimize the burden and indebtedness to the family, the dying older adult conceal their actual feelings and tolerate their physical discomfort.
Next, we determined a number of variables pertaining to the need for home hospice care for the older adult dying of chronic illness. The study’s findings demonstrated that the status of residence was an influential factor of needs, with those who live with their spouse and children reporting higher levels of physical, psychological, informational, and spiritual needs. Contrary to the results of several scholars (28, 29). One potential explanation could be the low monthly household income of the study’s population, of which 75.4% earn less than ≤3,000 yuan per month. This amount of money is far less than the monthly per capita income of Liaoning Province’s urban residents in 2022 (3,667 yuan) (30). Higher costs are associated with more people living together, and older people’s access to high-quality healthcare is restricted by the state of the economy. At present, home hospice care is not covered in its whole by medical insurance in China (31). Due to financial constraints, older patients who are terminally ill only accept a portion of the home hospice care service program, so the fact cannot meet their basic physiological needs. According to Maslow’s Hierarchy of Needs Theory, unmet physiological needs make it difficult to meet other needs at a higher level (32). Furthermore, this study discovered that due to differences in reimbursement rates, different types of insurance are linked to various needs. In order to relieve financial strain, it is advised that healthcare professionals help family members apply for grants and benefits, as well as applications for donations from individuals and social organizations for the older adult with terminal illnesses. China needs to reform its health insurance system in the future, intending to break down the barriers of the home hospice medical system and provide institutional safeguards for the development of the home hospice care business.
In this study, end-of-life older adult with longer illness duration and more comorbidities had higher physical and social support needs, which was consistent with the findings of Wyld et al. (33). The reason for this analysis is the progressive aggravation of symptoms brought about by the disease as the duration of the disease increases. Studies have shown that cancer patients with longer disease duration experience more symptoms than patients with shorter disease duration (28), which suggests that the duration of the disease is closely related to the patient’s quality of life. Relevant studies have found that heart failure is often complicated by diabetes mellitus, arrhythmia, hypertension and other diseases (34). The combination of chronic diseases in older adult patients can cause multi-system damage, leading to a decline in physiologic function, increasing the burden of medication (increased adverse drug reactions, decreased medication adherence), and severely reducing the quality of life. Wang et al. have found that a higher level of social support can positively affect patients (35). Support from healthcare professionals in relation to physical symptoms and moral support from family and friends ultimately improved their quality of life. Consequently, healthcare professionals should provide early home hospice care for the older adult chronic population can effectively reduce disease distress. Simultaneously, we should highlight the function and influence of social support on older persons with chronic illnesses and their families, as well as develop practical strategies to offer social interventions to patients.
According to the study’s findings, older adult with non-cancer chronic diseases had higher home hospice care needs than those with cancer, particularly in terms of their physical, social, and spiritual needs. This agrees with Llop-Medina et al.’s (36) findings. Theoretical trajectories of dying of patients with advanced cancer, proposed by Glaser and Strauss, can predict changes in the condition of cancer patients in advance (37). Healthcare professionals can make appropriate end-of-life care decisions based on changes in symptoms. In contrast, non-cancer-diagnosed patients are characterized by long-term, progressive and rapid deterioration (38), and the difficulty in grasping the course of the disease makes it more difficult to carry out nursing care. Burt believes that it is difficult to meet the physiological needs of the patient without effective symptom management or adequate nursing care (39). Repeated changes in disease not only increase physical pain but also mental suffering and a diminished sense of confidence and meaning in life. Roughly half of patients with severe heart failure will pass away suddenly from sudden cardiac death (40); this suggests that a professional hospice team is necessary due to the disease’s rapid deterioration. Therefore, community healthcare professionals should encourage seniors and their families to develop advanced care planning as early as possible to cope with the unpredictability of chronic disease at the end of life. It is also possible to establish a hospice care multidisciplinary chronic disease specialist team, according to different types of chronic diseases, through division of labor and cooperation, to improve the sense of meaning in life based on relieving physical pain, and provide timely professional help when the disease deteriorates rapidly.
This study’s findings, which are in line with those of Kun Zhang and Chaoying Wang’s (28, 29) study, show that the poorer the self-care ability of the terminal older adult, the higher the need for home hospice care, especially physical needs and psychological needs. With the increase of age, the self-care ability of the older adult gradually decreases. According to the current survey, 72.9% of older persons have defective self-care ability, which means that they greatly depend on the assistance of others. Influenced by the traditional Chinese concept of “raising children to prevent old age,” most of the dying older adult tend to choose family members to provide care for them (41). Due to the lack of caregiving knowledge, it is difficult for family members to manage their symptoms effectively while providing basic care such as daily living. For instance, Tarter’s research revealed that informal caregivers were inefficient in managing dementia patients’ pain (42). In addition, dying older adult have restricted activities due to their illness (dyspnea, heart failure), which often keeps them indoors and isolates them from the outside world. This creates psychological needs like loneliness. As a result, community medical staff use both online and offline techniques to instruct caregivers on caregiving skills. If the condition permits, assist family members in transferring the patient to the outdoor area to talk with others and participate in social activities together, to reduce the sense of social alienation; When the illness does not allow outdoor activities, assist family members in arranging home activities, such as having dinner together or accompanying the patient to catch up with old times.
5 Limitations
The following are the limitations of this study. First, the classification of chronic illness categories and comorbidities was overly simple and rough due to the small sample size. To determine the differences in need, the classification of chronic diseases can be further differentiated in the future using a sizable sample size. Second, this study was conducted in Jinzhou City, Liaoning Province, which is useful for studies under the same economic and cultural conditions, but whether the conclusions are representative of the chronic terminal older adult population in other regions needs to be further explored. Future studies can collect data in different regions to make the findings more generalizable. Finally, this study was a cross-sectional survey that investigated the need for and factors influencing home hospice care for this population at a certain point in time. In the future, a longitudinal study could be conducted to investigate trends in home hospice needs and influencing factors as their condition changes. Based on this study, we need to continue to explore cultural differences in hospice needs at home or evaluate the effectiveness of different hospice interventions in the future.
6 Conclusion
In summary, the need for home hospice care in China is high for the older adult with end-stage chronic disease, who need care in physical, psychological, spiritual, and social support. Among them, status of residence, duration of illness (year), the type of disease, and self-care ability were the main factors influencing the need for home hospice care. In the process of providing hospice care services for the dying older adult and their families, healthcare professionals should assess their needs and fully consider the influencing factors of needs, so as to promote the improvement of the level of hospice care services. Moreover, the provision of personalized and comprehensive care and nursing care centered on the dying older adult can improve their quality of life within a limited period of time. It is also necessary for government departments to standardize and formulate a comprehensive hospice policy so that older adult patients can finish their final journey in a home environment, quietly and comfortably.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Jinzhou Medical University College of Nursing Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LW: Writing – original draft. YL: Writing – original draft. RZ: Writing – review & editing. JL: Writing – review & editing. XG: Writing – original draft. HL: Writing – review & editing. YC: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project has received funding from the Chinese Association of Gerontology and Geriatrics, Action for Health Promotion in the Elderly (2021–2025), First Action Program Fund (No. CAGG-2021-04-01).
Acknowledgments
We are very grateful to the terminally ill seniors and their families who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Namisango, E, Powell, RA, Taylor, S, Radbruch, L, Freeman, R, Haufiku, D, et al. Depressive symptoms and palliative care concerns among patients with non-communicable diseases in two southern African countries. J Pain Symptom Manag. (2023) 65:26–37. doi: 10.1016/j.jpainsymman.2022.09.008
2. Zhou, M, Wang, H, Zeng, X, Yin, P, Zhu, J, Chen, W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/s0140-6736(19)30427-1
3. Kennedy, BK, Berger, SL, Brunet, A, Campisi, J, Cuervo, AM, Epel, ES, et al. Geroscience: linking aging to chronic disease. Cell. (2014) 159:709–13. doi: 10.1016/j.cell.2014.10.039
4. Chen, X, Giles, J, Yao, Y, Yip, W, Meng, Q, Berkman, L, et al. The path to healthy ageing in China: a Peking University-lancet commission. Lancet. (2022) 400:1967–2006. doi: 10.1016/s0140-6736(22)01546-x
5. Pot, AM, Oliveira, D, and Hoffman, J. Towards healthy ageing in China: shaping person-centred long-term care. Lancet. (2022) 400:1905–6. doi: 10.1016/s0140-6736(22)02361-3
6. Gu, X, Cheng, W, Cheng, M, Liu, M, and Zhang, Z. The preference of place of death and its predictors among terminally ill patients with cancer and their caregivers in China. Am J Hosp Palliat Care. (2015) 32:835–40. doi: 10.1177/1049909114542647
7. Xu, T. Survey of feasibility on foundation of home hospice center in Chenngdu city. Chin Nurs Res. (2014) 28:3113–5. doi: 10.3969/j.issn.10096493.2014.25.016
8. Xia, CF, and Chen, WQ. Fractions and trends of cancer burden attributable to population ageing in China. Zhonghua Zhong Liu Za Zhi. (2022) 44:79–85. doi: 10.3760/cma.j.cn112152-20211012-00756
9. Hui, D, Nooruddin, Z, Didwaniya, N, Dev, R, de la Cruz, M, Kim, SH, et al. Concepts and definitions for "actively dying," "end of life," "terminally ill," "terminal care," and "transition of care": a systematic review. J Pain Symptom Manag. (2014) 47:77–89. doi: 10.1016/j.jpainsymman.2013.02.021
10. Agarwal, A, Alshakhs, S, Luth, E, Dignam, R, Reid, MC, Adelman, RD, et al. Caregiver challenges seen from the perspective of certified home hospice medical directors. Am J Hosp Palliat Care. (2022) 39:1023–8. doi: 10.1177/10499091211056323
11. Bužgová, R, and Sikorová, L. Association between quality of life, demographic characteristics, physical symptoms, and unmet needs in inpatients receiving end-of-life care: a cross-sectional study. J Hosp Palli Nur. (2015) 17:325–32. doi: 10.1097/njh.0000000000000170
12. Kingston, A, Robinson, L, Booth, H, Knapp, M, and Jagger, C. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing. (2018) 47:374–80. doi: 10.1093/ageing/afx201
13. Hazelwood, DM, Koeck, S, Wallner, M, Anderson, KH, and Mayer, H. Patients with cancer and family caregivers: management of symptoms caused by cancer or cancer therapy at home. HeilberufeSCIENCE. (2012) 3:149–58. doi: 10.1007/s16024-012-0118-z
14. Moghaddam, N, Coxon, H, Nabarro, S, Hardy, B, and Cox, K. Unmet care needs in people living with advanced cancer: a systematic review. Support Care Cancer. (2016) 24:3609–22. doi: 10.1007/s00520-016-3221-3
15. Höcker, A, Krüll, A, Koch, U, and Mehnert, A. Exploring spiritual needs and their associated factors in an urban sample of early and advanced cancer patients. Eur J Cancer Care (Engl). (2014) 23:786–94. doi: 10.1111/ecc.12200
16. Gott, M, Allen, R, Moeke-Maxwell, T, Gardiner, C, and Robinson, J. 'No matter what the cost': a qualitative study of the financial costs faced by family and whānau caregivers within a palliative care context. Palliat Med. (2015) 29:518–28. doi: 10.1177/0269216315569337
17. Higginson, IJ, Daveson, BA, Morrison, RS, Yi, D, Meier, D, Smith, M, et al. Social and clinical determinants of preferences and their achievement at the end of life: prospective cohort study of older adults receiving palliative care in three countries. BMC Geriatr. (2017) 17:271. doi: 10.1186/s12877-017-0648-4
18. Low, J, Pattenden, J, Candy, B, Beattie, JM, and Jones, L. Palliative care in advanced heart failure: an international review of the perspectives of recipients and health professionals on care provision. J Card Fail. (2011) 17:231–52. doi: 10.1016/j.cardfail.2010.10.003
19. Bajwah, S, Higginson, IJ, Ross, JR, Wells, AU, Birring, SS, Riley, J, et al. The palliative care needs for fibrotic interstitial lung disease: a qualitative study of patients, informal caregivers and health professionals. Palliat Med. (2013) 27:869–76. doi: 10.1177/0269216313497226
20. Ryan, T, Ingleton, C, Gardiner, C, Parker, C, Gott, M, and Noble, B. Symptom burden, palliative care need and predictors of physical and psychological discomfort in two UK hospitals. BMC Palliat Care. (2013) 12:11. doi: 10.1186/1472-684x-12-11
21. Daya, AP, Sarkar, S, and Kar, SS. Estimation of palliative care need in the Urban Community of Puducherry. Indian J Palliat Care. (2017) 23:81–7. doi: 10.4103/0973-1075.197959
22. Elayaperumal, S, Venugopal, V, and Dongre, AR. Identifying people in need of palliative Care Services in Rural Tamil Nadu: a survey. Indian J Palliat Care. (2018) 24:393–6. doi: 10.4103/ijpc.Ijpc_92_18
23. Kozlov, E, Cai, A, Sirey, JA, Ghesquiere, A, and Reid, MC. Identifying palliative care needs among older adults in nonclinical settings. Am J Hosp Palliat Care. (2018) 35:1477–82. doi: 10.1177/1049909118777235
24. Hu, T, Xiao, J, Peng, J, Kuang, X, and He, B. Relationship between resilience, social support as well as anxiety/depression of lung cancer patients: a cross-sectional observation study. J Cancer Res Ther. (2018) 14:72–7. doi: 10.4103/jcrt.JCRT_849_17
25. Dunham, M, Ingleton, C, Ryan, T, and Gott, M. A narrative literature review of older people's cancer pain experience. J Clin Nurs. (2013) 22:2100–13. doi: 10.1111/jocn.12106
26. Ghesquiere, A, Gardner, DS, McAfee, C, Kenien, C, Capezuti, E, Kozlov, E, et al. Development of a community-based palliative care screening tool for underserved older adults with chronic illnesses. Am J Hosp Palliat Care. (2018) 35:929–37. doi: 10.1177/1049909117749467
27. Kastbom, L, Milberg, A, and Karlsson, M. A good death from the perspective of palliative cancer patients. Support Care Cancer. (2017) 25:933–9. doi: 10.1007/s00520-016-3483-9
28. Kun, Z, Yunyun, P, Li, L, and Can, G. The status quo and influencing factors of palliative care needs of the community elderly with chronic diseases Chinese. Nurs Manag. (2023) 23:1306–11. doi: 10.3969/j.issn.1672-1756.2023.09.005
29. Chaoying, W, Wei, Z, Yanju, J, Fuying, Z, and Cuizhen, S. Study on the demand for hospice care and its influencing factors in elderly patients. Shang Med Pharm J. (2017) 38:15–9.
30. Minxin, (2022) Liaoning provincial government work report. (2022) 2:24–30. doi: 10.3969/j.issn.1674-201X.2022.02.015
31. Ying, Y, Chen, D, Zhang, P, Tang, Y, Zhu, Q, and Jiang, S. Status quo of hospice care service in community health service centers in Shanghai. Chin J General Pract. (2023) 22:367–72. doi: 10.3760/cma.j.cn114798-20220729-00808
33. Wyld, MLR, Morton, RL, Clayton, P, Wong, MG, Jardine, M, Polkinghorne, K, et al. The impact of progressive chronic kidney disease on health-related quality-of-life: a 12-year community cohort study. Qual Life Res. (2019) 28:2081–90. doi: 10.1007/s11136-019-02173-1
34. Conrad, N, Judge, A, Tran, J, Mohseni, H, Hedgecott, D, Crespillo, AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. (2018) 391:572–80. doi: 10.1016/s0140-6736(17)32520-5
35. Wang, T, Molassiotis, A, Tan, JY, Chung, BPM, and Huang, HQ. Prevalence and correlates of unmet palliative care needs in dyads of Chinese patients with advanced cancer and their informal caregivers: a cross-sectional survey. Support Care Cancer. (2021) 29:1683–98. doi: 10.1007/s00520-020-05657-w
36. Llop-Medina, L, Fu, Y, Garcés-Ferrer, J, and Doñate-Martínez, A. Palliative Care in Older People with multimorbidities: a scoping review on the palliative care needs of patients, Carers, and health professionals. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19063195
38. Romem, A, Tom, SE, Beauchene, M, Babington, L, Scharf, SM, and Romem, A. Pain management at the end of life: a comparative study of cancer, dementia, and chronic obstructive pulmonary disease patients. Palliat Med. (2015) 29:464–9. doi: 10.1177/0269216315570411
39. Burt, J, Shipman, C, Richardson, A, Ream, E, and Addington-Hall, J. The experiences of older adults in the community dying from cancer and non-cancer causes: a national survey of bereaved relatives. Age Ageing. (2010) 39:86–91. doi: 10.1093/ageing/afp212
40. Jackevicius, CA, de Leon, NK, Lu, L, Chang, DS, Warner, AL, and Mody, FV. Impact of a multidisciplinary heart failure post-hospitalization program on heart failure readmission rates. Ann Pharmacother. (2015) 49:1189–96. doi: 10.1177/1060028015599637
41. van den Berg, B, Brouwer, WB, and Koopmanschap, MA. Economic valuation of informal care. An overview of methods and applications. Eur J Health Econ. (2004) 5:36–45. doi: 10.1007/s10198-003-0189-y
Keywords: home hospice, influencing factors, older adults, chronic diseases, need
Citation: Wang L, Li Y, Zhao R, Li J, Gong X, Li H and Chi Y (2024) Influencing factors of home hospice care needs of the older adults with chronic diseases at the end of life in China: a cross-sectional study. Front. Public Health. 12:1348214. doi: 10.3389/fpubh.2024.1348214
Edited by:
Elena Carrillo-Alvarez, Blanquerna Ramon Llull University, SpainReviewed by:
Sup Amornpinyo, Khon Kaen University, ThailandDaisy Volmer, University of Tartu, Estonia
Copyright © 2024 Wang, Li, Zhao, Li, Gong, Li and Chi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyu Li, cmVkYTQ2NzNAc2luYS5jb20=; Yuan Chi, NzgxMzYzMDlAcXEuY29t
 Lei Wang1
Lei Wang1 Hongyu Li
Hongyu Li