- 1Physical Education School, Putian University, Putian, Fujian, China
- 2School of Physical Education, Shenzhen University, Shenzhen, Guangdong, China
- 3School of Physical Education and Sport Science, Fujian Normal University, Fuzhou, Fujian, China
- 4School of Exercise Science, Physical and Health Education, University of Victoria, Victoria, BC, Canada
Background: The spread of Covid-19 and resultant infection prevention strategies have disturbed the life routine of Chinese young adults, led to reduced physical activity (PA), prolonged screen time (ST) and inadequate sleep duration (SP), and made immense influence on their mental health (MH) and quality of life (QoL). E-Health literacy (EHL) can enable citizens to use available online information to respond to the highly complex information environment and make appropriate health decisions.
Objective: This study aims to examine associations between adhering to 24-h movement (24HM) guidelines and MH and QoL among young adults, as well as to identify any mediating or moderating role of EHL in these associations.
Methods: 1742 young adults (20.03 ± 1.54 years old, 68.6% females) from north and south China completed self-report measures of 24HM (PA, ST and SP), health indicators (MH and QoL), EHL and demographic information through an online survey between 4 Apr and 16 Jun 2022. Generalized linear mixed models were applied for data analysis.
Results: Results showed that adhering to PA, ST and SP guidelines were all positively connected with QoL while MH was associated with adhering ST or SP guidelines. Adhering to more of 24HM guidelines was linked to better MH and QoL. EHL significantly mediated the association of guideline adherence and QoL and moderate that of guideline adherence and MH.
Conclusion: This is the first study to investigate the role of EHL on the associations between 24HM and MH as well as QoL during the Covid-19. The findings may contribute to further empirical research or intervention that aims to promote MH or QoL among young adults more effectively or provide valuable references for developing relevant strategies or policy of health promotion or public health events in China.
Introduction
In order to control the coronavirus disease 2019 (Covid-19) swiftly, infection prevention strategies such as quarantine and travel limitation were performed across China (1). During the performance of these strategies, Chinese young adults had to go through the isolation in or outside of the campus while taking online courses (2). Most aspects of their lives were affected by quarantines, which subsequently lead to negative impacts on their mental health (MH) as well as quality of life (QoL) (3). For most Chinese young adults, entering college is the first chance to live independently (4), and they may not have been psychologically mature enough to face such a severe public health emergency (5). Additionally, young adults had especially high rates of internet usage (6) and were likely exposed to a multitude of information online that contributed to psychological distress because of the information overload (7). Moreover, the isolated environment limited the social activities (8), strengthened academic pressures (9), and increased the likelihood of psychological problems (10). Thus, the MH and QoL of Chinese young adults have deteriorated since the Covid-19 outbreak (11).
Prior studies have shown that Covid-19 has resulted in less physical activity (PA) (12, 13), more screen time (ST) (13, 14), and insufficient sleep (SP) (10, 14), and it is well-known that these could negatively influence people’s physical and mental health as well as QoL (10, 12–14). Importantly, individuals may carry out multiple health behaviors in a day (15), thus the health impact of these behaviors should be given integrated consideration. In line with this reasoning, the Canadian Society for Exercise Physiology (CSEP) created the premiere 24-h movement (24HM) recommendations for adults aged under 65, provided the “healthy threshold” for adult’s PA, ST and SP (16). While these guidelines were primarily based on the impact of 24HM on physical health outcomes (16), limited research examined the relationship between 24HM and MH as well as QoL (17).
As introduced before, associations may exist between 24HM and MH together with QoL. Since e-Health literacy (EHL) has effects on health behaviors, MH and QoL, it is reasonable to assume that EHL could play a role in the linkages of 24HM and MH together with QoL. Yet, it is uncertain whether EHL is a mediator or a moderator in these linkages. For the mediating effect, theoretically, EHL is an integrated set of knowledge-based context-specific capabilities which may show variation due to circumstances (18, 19). According to the daily experience, sleep quality may influence individuals’ capability of health-related communication, people who are more attached to screen behaviors may tend to avoid health advice with plenty of physical activities. Besides, more physical activities provide practitioners more chances to obtain health-related experience such as how to stretch and strengthen muscles. These cases imply that EHL does not remain constant and would be influenced by context. Thus, it is possible that 24HM may have impacts on EHL and indirectly influence MH and QoL. For the moderating effect, EHL may relieve the negative impacts of inadequate 24HM on MH or QoL. A recent study found that EHL may help safeguard MH and enhance QoL for those exhibiting Covid-19 symptoms (20).
EHL encompasses the skills to search for, comprehend, evaluate, and apply health information from digital sources in order to address a health issue or make health-related decisions (18). Due to social distancing protocols and increased demand for health resources during Covid-19, individuals are more prone to access health information electronically compared to before the pandemic (21, 22). EHL therefore becomes crucial. Previous research proved that adequate EHL is significantly linked healthy behavior engagement (19, 23, 24). Recently, scholars have also shown that EHL can have a positive effect on MH by protecting people from unreliable or poor-quality health information during the Covid-19 (21, 22, 25). Additionally, EHL represents individuals’ ability to cope with health problems and manage their health status via the electronic resources or tools, thus it is closely associated with QoL. While several studies have validated that EHL could significantly enhance MH (22, 25) and QoL (20, 26) during the pandemic, scarce research has analyzed the interrelationships between 24HM, EHL, MH, and QoL.
Given the above, the current study aims to: (1) examine adherence to 24HM guidelines in Chinese young adults; (2) investigate associations between meeting 24HM guidelines and MH as well as QoL; and (3) analyze the mediating and moderating roles of EHL in the connections between adherence to 24HM guidelines and MH/QoL, while controlling for key demographic factors. We hypothesized that (1) participants who met individual or the specific combination of two 24HM guidelines would potentially exhibit superior MH and QoL versus non-adherers; (2) meeting more 24HM guidelines would correlate with decreased MH symptoms and improved QoL; (3) EHL would be a salient mediator and moderator in the associations of the 24HM guidelines adherence and MH together with QoL.
Methods
Participants and design
A cross-sectional design as well as the convenience sampling were utilized (27). Participants were recruited from four colleges in Hebei and Fujian of China. The cities were selected based on contrasts in regional geography (northern vs. southern) and administrative level (provincial capital vs. prefecture). The issue of convenience and feasibility were also considered when selecting the target cities (28). The inclusion criteria required that young adults (≥18 years): (1) were fluent in Chinese, (2) provided informed consent and willingness to take part in the survey, (3) had no disabilities or disorders in their physical or mental function, and (4) had persisted in China after the onset of the Covid-19. This study received ethical approval from the Research Ethics Committee at Putian University, China.
Procedures
The data collection was conducted with the help of lecturers from the target colleges from 4 Apr to 16 Jun 2022. The survey was administered after obtaining informed consent from participants. They were notified of their right to withdraw at any time. The questionnaire was delivered via a QR code linking to an online survey platform. Participants spent approximately 10 min completing the questionnaires.
Measurements
Demographic information to obtain demographic information, the survey asked for gender, age, academic year, major, BMI, family economic status (monthly family income: RMB < 6,000; RMB 6000–10,000; RMB 10000–14,000; RMB 14000–18,000; RMB > 18,000), parents’ highest education level, and geographical region.
Physical activity (PA) was assessed by the abridged Chinese edition of the International Physical Activity Questionnaire (IPAQ-C) [International Physical Activity Questionnaire, (29); IPAQ-C, (30)], and a self-designed question, asking participants how many times of muscle strengthen activities they have performed per week. The IPAQ-C comprises 6 items assessing self-reported PA across three intensities (vigorous, moderate, mild) over the past week. For each intensity, participants indicated how many days per week and how many minutes per day they took part in the activities. Total weekly PA time and time in each intensity category (minutes/week) were calculated based on responses (31). The 24HM Guidelines (16) define meeting PA recommendations as ≥150 min weekly of moderate-to-vigorous PA (MVPA) plus twice weekly muscle strengthening (16).
Sleep (SP) was measured by three items extracted from the Pittsburgh Sleep Quality Index (PSQI) (32). Questions include: “Thinking about the previous week, what were your average wake-up and bedtimes each day? How many hours did you sleep nightly on average?” Meeting SP recommendations per the 24HM guidelines (16) requires 7–9 h daily.
Screen time (ST) was measured using the Chinese translated Sedentary Behavioral Questionnaire (33). Six questions were asked: “Considering the last 7 days, what was your mean time allotted on weekdays/weekends for activities such as videos, gaming, chatting, web searches, email, and studying?” The 24HM Guidelines (16) recommend limiting ST time to ≤8 h daily.
Mental health (MH) was quantified via the 21-question Chinese ‘Depression Anxiety Stress Scale’ (DASS-21) (34, 35), which has demonstrated validity among the adult mainland Chinese population. The 21-item DASS comprises three 7-item subscales assessing participants’ feeling of depression, anxiety and stress regarding the previous week (Cronbach’s α = 0.79–0.89). Each item uses a 4-point response format from 0 (“irrelevant to me”) to 3 (“extremely relevant to me”). Subscale values are obtained by totaling the item responses and doubling the sum. Cutoffs classify depression as normal (0–9) or symptomatic (>9), anxiety as normal (0–7) or symptomatic (>8), and stress as normal (0–14) or symptomatic (>15). Symptomatic levels include mild, moderate, severe and extremely severe (36).
Quality of life (QoL) was measured utilizing the brief Chinese edition of the World Health Organization Quality of Life scale (37) (Cronbach’s α = 0.82). Participants rated their perceptions over the previous 4 weeks. They firstly measured their overall QoL with a 5-point scale from 1 (“very poor”) to 5 (“very good”), then completed 7 items evaluating satisfaction with physical health subdomains on a 5-point scale from 1 (“very dissatisfied”) to 5 (“very satisfied”).
e-Health literacy (EHL) was assessed using the e-Health literacy scale in Web 3.0 context (eHLS-Web3.0) developed by Liu et al. (38), consisting of 24 items assessing EHL across three dimensions: acquisition, verification and application utilizing a 5-point scale from 1 (strongly disagree) to 5 (strongly agree). The tool demonstrates validity via exploratory and confirmatory factor analyses. Its reliability, validity, and measurement invariance have been established among young adult populations. Compared to previous EHL measures, the eHLS-Web3.0 captures modern technological engagement including social media and mobile internet. Recently developed, it shows high internal consistency for the overall scale (α = 0.971) and subscales (α = 0.913–0.962) in Chinese young adults.
Data analysis
IBM SPSS 27.0 (Armonk, NY) facilitated data analyses. Initial diagnostics were conducted including outlier and distribution analyses. Skewed variables were log-transformed or replaced with median (interquartile range). Participant characteristics were summarized using descriptive statistics: mean, standard deviation (SD), and frequencies (%). Generalized linear mixed models were used to examine the relationships of meeting the 24HM guidelines with MH and QoL, controlling for all demographic covariates (i.e., gender, age, year of study, major, BMI, family economic status, parents’ education levels and region).1 The sample size was sufficient to detect an effect size of (Cohen f2) 0.01, with an alpha of 0.05 and 1-β of 0.8 in the regression model (42). A two-tailed p-value under 0.05 denoted statistical significance. Model 1 and Model 4 of PROCESS was utilized in SPSS to test the mediating and moderating effect of e-Health literacy. To confirm the significance of the indirect effect, bias-corrected bootstrapped of 95% confidence intervals with 5,000 resamples were also applied. We established statistical significance as p < 0.05 (two-tailed). Effect sizes for model predictors were calculated using Cohen’s f2, computed by the formula “f2 = R2/(1-R2).” Values of 0.02, 0.15, and 0.35 indicate small, medium and large effects, respectively (43).
Results
Demographic characteristics and guideline adherence
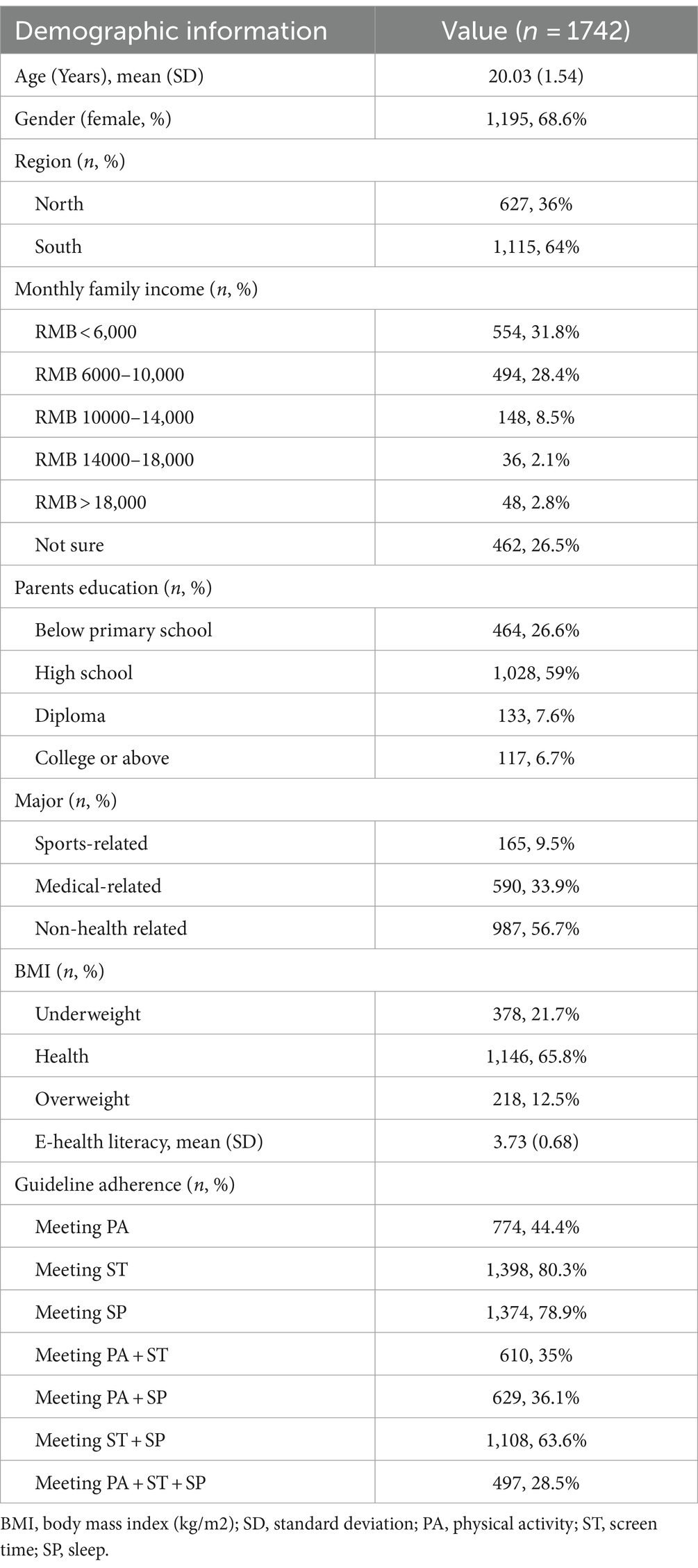
A summary of participants’ demographic information and guideline adherence are described in Table 1. Out of 1,862 young adults approached, 1,850 gave written informed consent to participate. After eligibility check and data screening, the final analytical sample comprised 1,742 participants. The sample comprised 547 males and 1,195 females, aged 18 to 25 years (M = 20.03, SD = 1.54). A considerable proportion of the sample reported a health-related major (43.3%). In terms of body mass index (BMI, kg/m2), most of the participants were in a healthy level. 44.4% of participants reported meeting the PA guideline, 80.3% meeting ST, and 78.9% meeting SP. Percentages of participants adhering to a combination of two 24HM guidelines ranged from 35 to 63.6%. 28.5% of participants meet all the 24HM recommendations. An adequate level of EHL (M = 3.73, SD = 0.68) was demonstrated among the participants.
24HM guideline adherence and health outcomes (MH and QoL)
Table 2 displays the links between compliance with guidelines and health indicators (individual and in combination). After adjusting the covariates (i.e., gender, age, year of study, major, BMI, family economic status, parents’ education levels and region), meeting the guideline of PA was associated with QoL (β = 0.176, 95%CI = 0.114, 0.239); meeting the guideline of ST was associated with QoL (β = 0.092, 95%CI = 0.017, 0.166) and lower depression symptoms (β = −1.872, 95%CI = -2.441, −1.304), anxiety (β = −1.582, 95%CI = -2.138, −1.027) and stress (β = −1.576, 95%CI = -2.154, −0.99); meeting the guideline of SP was associated with QoL (β = 0.280, 95%CI = 0.208, 0.353), as well as lower stress (β = −1.102, 95%CI = -1.666, −0.538), depression symptoms (β = −0.595, 95%CI = -1.149, −0.041) and anxiety (β = −0.842, 95%CI = -1.384, −0.300) (all p < 0.05).
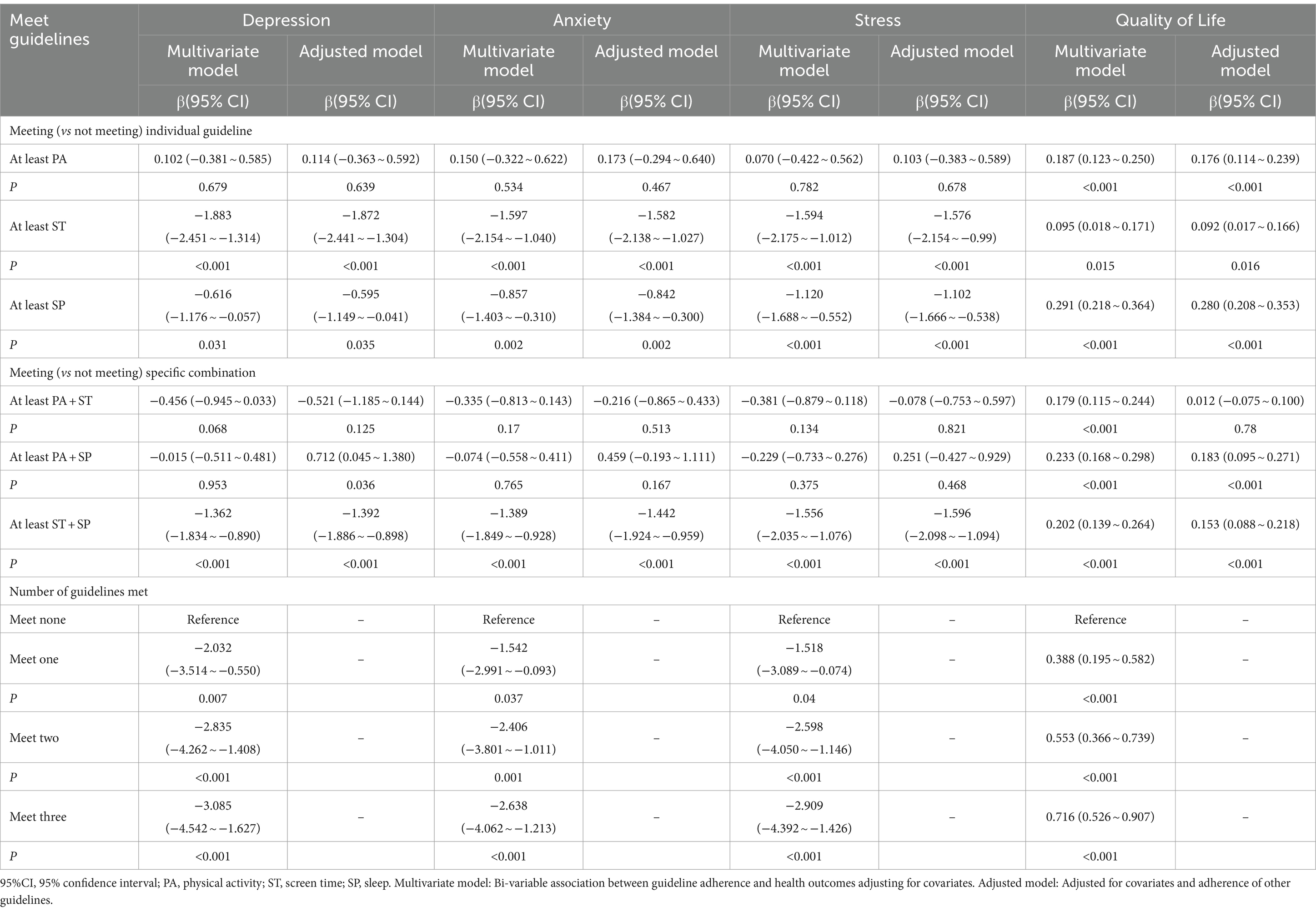
Table 2. Associations between guideline adherence and stress, depression, anxiety and quality of life.
Meeting PA + ST has no significant association with mental health or quality of life. Meeting PA + SP guideline was associated with depression symptoms (β = 0.712, 95%CI = 0.045, 1.380) and QoL (β = 0.183, 95%CI = 0.095, 0.271); meeting ST + SP guidelines was connected to relieved depression (β = −1.392, 95%CI = -1.886, −0.898), anxiety (β = −1.442, 95%CI = -1.924, −0.959) and stress (β = −1.596, 95%CI = -2.098, −1.094) symptoms, and higher QoL (β = 0.153, 95%CI = 0.088, 0.218). Meeting all guidelines was related to higher level of QoL (β = 0.716, 95%CI = 0.526, 0.907) and lower symptoms of depression (β = −3.085, 95%CI = -4.542, −1.627), anxiety (β = −2.638, 95%CI = -4.062, −1.213) and stress (β = −2.909, 95%CI = -4.392, −1.426).
The mediating and moderation effects of EHL
A significant moderating effect of EHL emerged in the analysis between adhering to guidelines and stress, depression, and anxiety symptoms (see Table 3). The moderation effect of EHL on the association of guideline adherence and QoL was not significant. Regarding the association between guideline adherence and stress, significant interactions emerged between EHL and meeting one guideline (β = 0.374, p = 0.015) as well as EHL and meeting two guidelines (β = 0.334, p = 0.024). The interactions contributed a significant change in the explained variance (△R2 = 0.007, p < 0.01). Overall, the moderation model explained 8% of variance in stress scores (R2 = 0.08, p < 0.001). On the association between guideline adherence and depression, results indicated a significant interaction between EHL and adhering to one guideline (β = 0.344, p = 0.025). The interaction contributed to a significant change in the explained variance (△R2 = 0.006, p = 0.010). Overall, the moderation model explained 8% of variance in depression scores (R2 = 0.08, p < 0.001). On the association between guideline adherence and anxiety, the interaction between EHL and compliance with one guideline (β = 0.322, p = 0.037) contributed to a significant change in the explained variance (△R2 = 0.007, p = 0.007). Total variance explained in anxiety was 7% (R2 = 0.07, p < 0.001). For students adhering to more behavioral guidelines, the moderating effect of EHL was mild, whereas for those adhering fewer behavioral guideline, a higher level of EHL was associated with the negative impact of health-compromising behavior and mental health.
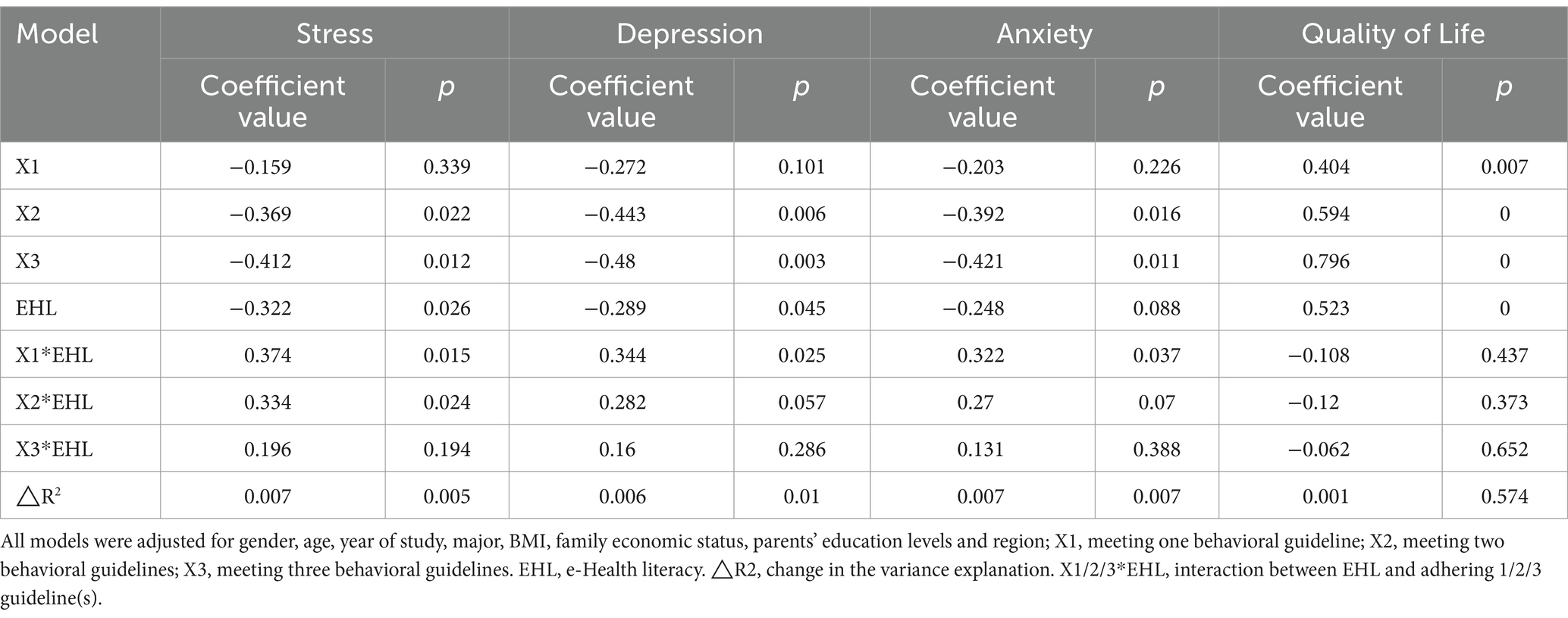
Table 3. Moderating effect of e-Health literacy on the association between guideline adherence and stress, depression, anxiety and quality of life (N = 1,742).
Table 4 shows the results of the mediation analyses conducted to determine whether guideline adherence predicted stress, depression, anxiety and QoL through EHL. The relationships between EHL and anxiety/depression/stress were not significant (βanxiety = −0.016, p = 0.503; βdepression = −0.038, p = 0.102; βstress = −0.029, p = 0.215), indicating that EHL did not mediate the relationship between guideline adherence and mental health. The mediating effect of EHL was found for the association between guideline adherence and QoL, no matter how many guidelines were complied. Further, the direct effect of guideline adherence on QoL (c’) remained significant after EHL and other covariates were controlled for, indicating a partial mediation of EHL. The total mediation model accounted for 25% of the variance in QoL (R2 = 0.25, p < 0.001).
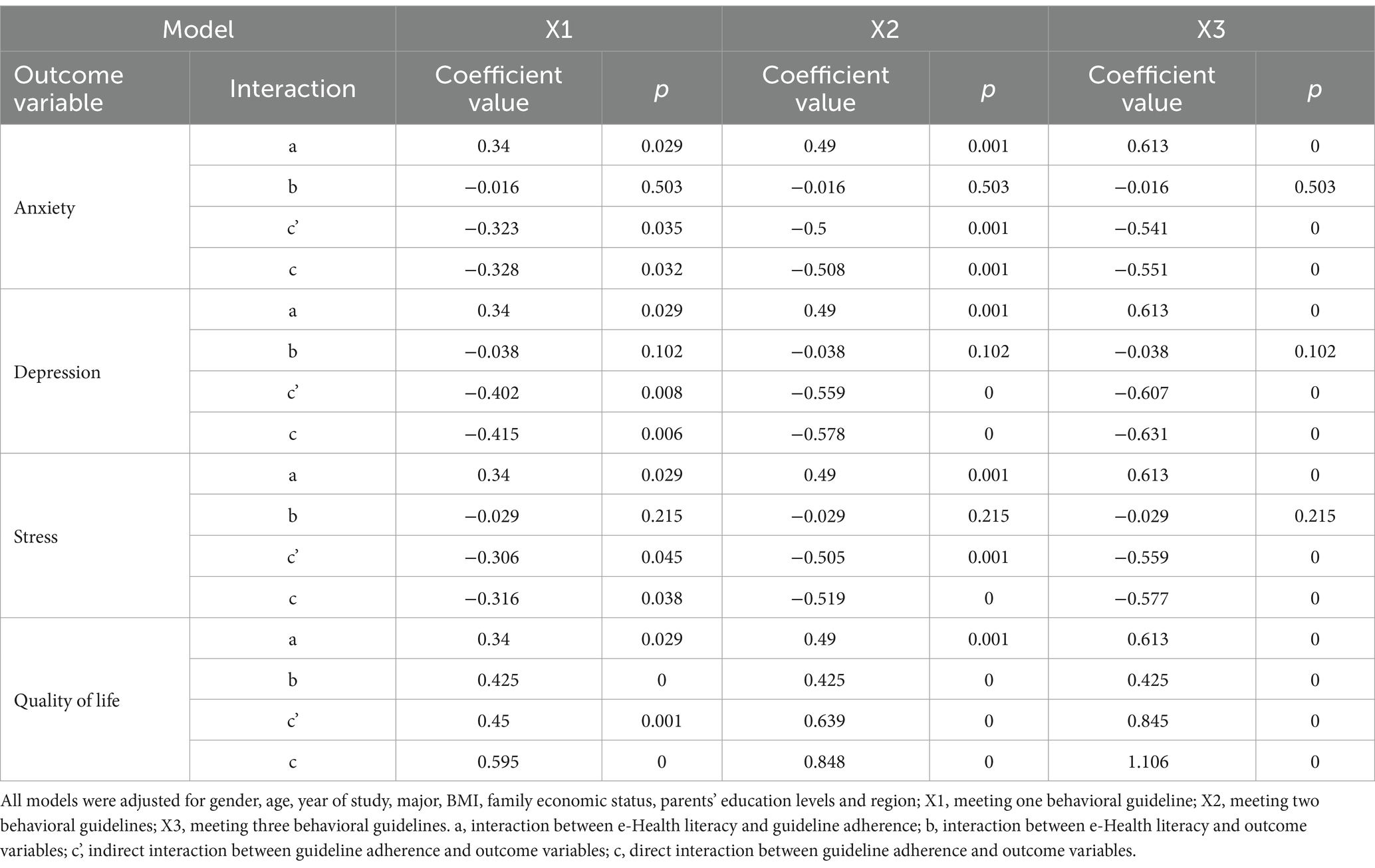
Table 4. Mediating effect of e-Health literacy on the association between guideline adherence and stress, depression, anxiety and quality of life (N = 1,742).
Discussion
This research analyzed adherence to recommendations for 24HM among Chinese university students, examined the relationship between guideline adherence and MH and QoL, and identified the mediating or moderating role of EHL. Findings showed that meeting PA, ST and SP guidelines were all positively connected with QoL while MH was associated with meeting ST or SP guidelines. Furthermore, adhering to more 24HM guidelines was associated with improved MH and QoL, but meeting different combinations of guidelines also led to different relationships with MH and QoL. EHL is also found to be a mediator of the relationship between guideline adherence and QoL and a moderator of the relationship between guideline adherence and MH.
Among the three movement guidelines, the PA guideline had the lowest compliance rate. This might be because the study was conducted in April 2022, during the outbreak of Omicron in China. Omicron is one of the most easily spread variants of Covid-19 (44) and some infection prevention strategies were taken by universities during this time, including entry-school restrictions, social distancing and lockdown inside school (2). The adherence to the PA guidelines might have been influenced by pandemic restrictions. Still, compared to previous research (17, 45, 46), the compliance in the current study was higher. The possible reason is that the participants are all college students living on campus, nearly half of whom (43.3%) where from health-related major. Life on campus is usually comprised of a regular routine, and students’ health behaviors may be positively influenced by their interests in their health major and their peers. Environmental factors such as peer support or perceived social norms should be considered in further relevant studies.
Meeting ST and SP guidelines were associated with better MH and QoL, which partially supported our hypothesis. However, a linkage was not significant between PA guideline adherence and mental health. This unexpected result is inconsistent with previous research that has established PA as an effective therapy for mental illness symptoms (47, 48). However, several articles reported a similar finding with the current study (49–52). A review on PA intervention among young people demonstrated that there was limited evidence for PA intervention to benefit mental illness (53). Consistent with the current study, research by Walsh et al. (49) and Guerrero et al. (50) showed no link between adherence to PA recommendations and better MH among American youth. Rebar et al. (54) suggested that the effect of PA on MH was smaller among non-clinical groups than the clinical ones, which might explain this finding. The sample characters in this study may have contribute to the lack significant association with PA. Additionally, most college students were required to take PE courses, and on-campus compulsory quarantine in April 2022 (2) also required students to take extra walk to arrive the quarantine station at least three times per week. These ‘compulsory tasks’ may also limit the positive effect of PA on MH observed in a more autonomous situation.
Consistent with hypothesis 2, increased compliance with guidelines corresponded to better MH and QoL outcomes. Meanwhile, meeting different combinations of guidelines had different effects on students’ MH and QoL. Among the three combinations (PA + ST, PA + SP, ST + SP), meeting ST + SP guidelines showed the most significant positive effects on both MH and QoL, which is consistent with previous studies (45, 46). Surprisingly, meeting PA + SP guideline was found to increase the symptoms of depression with a moderate effect size. This result might again be another demonstration of the negative impact of unhealthy ST on depression during Covid-19. There were infection peaks in April 2022 because of the spread of Omicron and subsequently an overwhelming influx of information about emerging infectious disease was booming online. For students who were having a lockdown inside the school, the internet was the main channel for them to learn about the situation outside (55). The enormous amount of information and messages about the infection may have created a huge challenge to their mental health (21). Additionally, meeting PA + ST had no significant impact on either MH or QoL. Several previous studies have highlighted the relative importance of meeting SP guideline (45, 46, 56), indicated that the SP guideline had a stronger connection to MH compared to the other guidelines. It is possible that the negative impact of not meeting SP guideline inhibits the positive effect of meeting PA + ST guideline. Furthermore, the mandatory PA may also be limiting the findings of PA in this population. Overall, the findings of this study reveal that PA, ST and SP are three codependent behaviors which may impact each other and occupy each other’s time within 24 h. Future research should continue to consider the differences in these combinations when implementing behavioral interventions, and priority should be given to which behavioral guideline should also be further studied so as to provide greater impact on various health benefits.
As far as we know, this is the first cross-sectional study examining the role of EHL in the relationship between 24HM and MH as well as QoL among Chinese young adults during the Covid-19. Prior studies have discussed various possibilities for how health literacy links to health outcomes (57, 58), although actual research on these mechanisms is scant. EHL is a concept developed on the basis of health literacy (18) and the mechanism of it influencing health might be similar. Health literacy is frequently found as a mediator or a moderator of the relationship between other determinants and health (57). The results of this study support EHL as a mediator between guideline adherence and QoL, and a moderator between guideline adherence and MH. Overall these findings thus partially support hypotheses 3. Health literacy has long been seen as a mediating factor between behavior and health because it has a potentially adaptable impact on social factors determining health outcomes (58). As a key element of public health surveillance, QoL had long be seen as an integrated predictor for individual’s perceived physical, mental and social health (59). This result supports the intervening effect of EHL on social-life-related QoL, proposing that improve EHL can potentially strengthen the positive health impacts of adhering behavioral guidelines. It is worthwhile to explore the relationship between 24HM and QoL among young adults during the Covid-19, which could help obtain a whole picture for the health impact of 24HM guideline.
In terms of the moderating effect, EHL was found to be a stronger moderator among students who were adhering to less guidelines. This finding might have been because that students adhering to more behavioral guidelines had better competency in health management and perceive better controllability when facing health threats (i.e., Covid-19) (60). However, for students adhering less to guidelines, they may have had limited health-managing personal experiences to draw upon, and had to rely on messages mainly from the internet. Among this group, EHL may substantially influence their understanding of such messages, thus creating stronger moderating effect between behavioral guidelines and MH. A Romanian study also found EHL acted as a protective factor against emotional distress related to searching for health information online (61). This finding indicates the necessity of providing EHL workshop or intervention for young adults, especially for those from non-health-related majors.
Limitations
Despite this study’s innovative and interesting findings, some limitations exist. First, the cross-sectional design of this study precludes the causality assumptions, and a reverse causation might be equally plausible. Further longitudinal research is needed to confirm these results. Second, the use of self-report measures may have contributed to recall bias, as well as the over/under-reporting and social desirability biases common in surveys. Further, the ST measured in this study was not limited to ‘recreational’ or ‘non-recreational’ ST; therefore, potential inaccuracies in the adherence of ST guideline might occurred. Third, the data collection was conducted during an infection peak of Omicron, so the timing may have influenced participants’ movement behaviors compared to other situations. Fourth, this study applied an online convenience sampling method, which may lead to some selection bias, despite the large sample. Finally, although the focus of this research was on the role of EHL and the relationship between movement guideline adherence and QoL/MH, there may still be other potential mediators that have not been taken into consideration. Continued exploration of key mechanisms linking movement behaviors to QOL and MH are warranted.
Conclusion
The current study examined the relationship between adhering to the 24HM guidelines and MH/QoL during Covid-19 and identified the effect of EHL in mediating the 24HM-QoL association and moderating the 24HM-MH association. It was found that meeting more of the guidelines was related to better MH and QoL among Chinese young adults, while meeting different combinations of the guidelines led to different health outcomes. The findings of this study highlighted the importance of EHL, offered new insights for implementing more effective MH and QoL interventions in the future, and supported guidance of 24HM guidelines when understanding health behaviors.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Research Ethics Committee at Putian University, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LL: Writing – review & editing, Supervision, Resources, Project administration. WL: Writing – review & editing, Writing – original draft, Validation, Resources, Project administration, Methodology, Investigation, Data curation. RW: Writing – review & editing, Supervision, Project administration. RR: Writing – review & editing, Validation, Supervision. HL: Writing – review & editing, Writing – original draft, Validation, Project administration, Investigation, Data curation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Fujian Provincial Social Science Foundation of China (Grant No.: FJ2024bf035) and Putian Municipal Bureau of Ethnic and Religious Affairs (Grant no.: 2022AHX142(L)).
Acknowledgments
The research team extends their gratitude to the individuals who volunteered their time and experiences for this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BMI, body mass index; CI, confidence interval; Covid-19, the coronavirus disease 2019; CSEP, the Canadian Society for Exercise Physiology; DASS21, the Depression Anxiety Stress Scale - 21; EHL, e-Health literacy; eHLS-Web3.0, the e-Health literacy scale in Web 3.0 context; IPAQ-C, the Chinese short version of the International Physical Activity Questionnaire; MH, mental health; MVPA, moderate-to-vigorous intensity physical activity; PA, physical activity; PSQI, the Pittsburgh Sleep Quality Index; QoL, quality of life; SD, standard deviation; SP, Sleep duration; ST, screen time; 24HM, 24-h Movement.
Footnotes
1. ^Previous research demonstrated that these variables were associate with people’s 24-h movement, e-Health literacy and diverse health outcomes (39–41).
References
1. Ding, D, and Zhang, R. China's COVID-19 control strategy and its impact on the global pandemic. Front Public Health. (2022) 10:483. doi: 10.3389/fpubh.2022.857003
2. Leung, M, and Sharma, Y. All Shanghai universities in lockdown in COVID-19 wave. (2022). Available at: https://www.universityworldnews.com/post.php?story=20220317152658532 (Accessed February 20, 2023).
3. Sun, S, Goldberg, SB, Lin, D, Qiao, S, and Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob Health. (2021) 17:15–4. doi: 10.1186/s12992-021-00663-x
4. Nelson, L, Badger, S, and Wu, B. The influence of culture in emerging adulthood: perspectives of Chinese college students. Int J Behav Dev. (2004) 28:26–36. doi: 10.1080/01650250344000244
5. Yu, M, Tian, F, Cui, Q, and Wu, H. Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatry. (2021) 21:66–8. doi: 10.1186/s12888-021-03066-9
6. Gowin, M, Cheney, M, Gwin, S, and Franklin, WT. Health and fitness app use in college students: a qualitative study. Am J Health Educ. (2015) 46:223–30. doi: 10.1080/19325037.2015.1044140
7. Li, S, Cui, G, Kaminga, AC, Cheng, S, and Xu, H. Associations between health literacy, ehealth literacy, and covid-19–related health behaviors among Chinese college students: cross-sectional online study. J Med Internet Res. (2021) 23:e25600. doi: 10.2196/25600
8. Li, Y, Peng, J, and Tao, Y. Relationship between social support, coping strategy against COVID-19, and anxiety among home-quarantined Chinese university students: a path analysis modeling approach. Curr Psychol. (2021) 42:10629–44. doi: 10.1007/s12144-021-02334-x
9. Shi, Y, Li, C, and Luo, L. Impact of the COVID-19 pandemic on Chinese college students’ information behavior and library needs: a qualitative study. Libr Q. (2021) 91:150–71. doi: 10.1086/713051
10. Tang, W, Hu, T, Hu, B, Jin, C, Wang, G, Xie, C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. (2020) 274:1–7. doi: 10.1016/j.jad.2020.05.009
11. Chen, RN, Liang, SW, Peng, Y, Li, XG, Chen, JB, Tang, SY, et al. Mental health status and change in living rhythms among college students in China during the COVID-19 pandemic: a large-scale survey. J Psychosom Res. (2020) 137:110219. doi: 10.1016/j.jpsychores.2020.110219
12. Han, B, Du, G, Yang, Y, Chen, J, and Sun, G. Relationships between physical activity, body image, BMI, depression and anxiety in Chinese college students during the COVID-19 pandemic. BMC Public Health. (2023) 23:24–1. doi: 10.1186/s12889-022-14917-9
13. Zhang, Y, Wu, X, Tao, S, Li, S, Ma, L, Yu, Y, et al. Associations between screen time, physical activity, and depressive symptoms during the 2019 coronavirus disease (COVID-19) outbreak among Chinese college students. Environ Health Prev Med. (2021) 26:1–2. doi: 10.1186/s12199-021-01025-0
14. Song, Y, Sznajder, K, Cui, C, Yang, Y, Li, Y, and Yang, X. Anxiety and its relationship with sleep disturbance and problematic smartphone use among Chinese medical students during COVID-19 home confinement—a structural equation model analysis. J Affect Disord. (2022) 296:315–21. doi: 10.1016/j.jad.2021.09.095
15. Duan, Y, Liang, W, Wang, Y, Lippke, S, Lin, Z, Shang, B, et al. The effectiveness of sequentially delivered web-based interventions on promoting physical activity and fruit-vegetable consumption among Chinese college students: mixed methods study. J Med Internet Res. (2022) 24:e30566. doi: 10.2196/30566
16. Ross, R, Chaput, JP, Giangregorio, LM, Janssen, I, Saunders, TJ, Kho, ME, et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. (2020) 45:S57–S102. doi: 10.1139/apnm-2020-0467
17. Feng, J, Huang, WY, Lau, PW, Wong, SH, and Sit, CH. Movement behaviors and mental health of caregivers of preschoolers in China during the COVID-19 pandemic. Prev Med. (2022) 155:106913. doi: 10.1016/j.ypmed.2021.106913
18. Norman, CD, and Skinner, HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. (2006) 8:e506. doi: 10.2196/jmir.8.2.e9
19. Xesfingi, S, and Vozikis, A. eHealth literacy: in the quest of the contributing factors. Interact J Med Res. (2016) 5:e4749. doi: 10.2196/ijmr.4749
20. Nguyen, MH, Pham, TT, Nguyen, KT, Nguyen, YH, Tran, TV, Do, BN, et al. Negative impact of fear of COVID-19 on health-related quality of life was modified by health literacy, eHealth literacy, and digital healthy diet literacy: a multi-hospital survey. Int J Environ Res Public Health. (2021) 18:4929. doi: 10.3390/ijerph18094929
21. Chong, YY, Cheng, HY, Chan, HY, Chien, WT, and Wong, SY. COVID-19 pandemic, infodemic and the role of eHealth literacy. Int J Nurs Stud. (2020) 108:103644. doi: 10.1016/j.ijnurstu.2020.103644
22. Brørs, G, Norman, CD, and Norekvål, TM. Accelerated importance of eHealth literacy in the COVID-19 outbreak and beyond. Eur J Cardiovasc Nurs. (2020) 19:458–61. doi: 10.1177/1474515120941307
23. Hsu, W, Chiang, C, and Yang, S. The effect of individual factors on health behaviors among college students: the mediating effects of eHealth literacy. J Med Internet Res. (2014) 16:e287. doi: 10.2196/jmir.3542
24. Mitsutake, S, Shibata, A, Ishii, K, and Oka, K. Associations of eHealth literacy with health behavior among adult internet users. J Med Internet Res. (2016) 18:e192. doi: 10.2196/jmir.5413
25. Yang, BX, Xia, L, Huang, R, Chen, P, Luo, D, Liu, Q, et al. Relationship between eHealth literacy and psychological status during COVID-19 pandemic: a survey of Chinese residents. J Nurs Manag. (2021) 29:805–12. doi: 10.1111/jonm.13221
26. Vu, DN, Phan, DT, Nguyen, HC, Le, LT, Nguyen, HC, Ha, TH, et al. Impacts of digital healthy diet literacy and healthy eating behavior on fear of COVID-19, changes in mental health, and health-related quality of life among front-line health care workers. Nutrients. (2021) 13:2656. doi: 10.3390/nu13082656
28. Denscombe, M. The good research guide: For small-scale social research projects McGraw-Hill Education:UK (2017).
29. Hagströmer, M, Oja, P, and Sjöström, M. The international physical activity questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. (2006) 9:755–62. doi: 10.1079/PHN2005898
30. Macfarlane, DJ, Lee, CCY, Ho, EYK, Chan, KL, and Chan, DTS. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J Sci Med Sport. (2007) 10:45–51. doi: 10.1016/j.jsams.2006.05.003
31. IPAQ Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. (2005). Available at https://www.semanticscholar.org/paper/Guidelines-for-data-processing-analysis-of-the-and-Sjostrom-Ainsworth/efb9575f5c957b73c640f00950982e618e31a7be (Accessed May 13, 2024).
32. Chang, Q, Xia, Y, Bai, S, Zhang, X, Liu, Y, Yao, D, et al. Association between Pittsburgh sleep quality index and depressive symptoms in Chinese resident physicians. Front Psych. (2021) 12:564815. doi: 10.3389/fpsyt.2021.564815
33. Rosenberg, DE, Norman, GJ, Wagner, N, Patrick, K, Calfas, KJ, and Sallis, JF. Reliability and validity of the sedentary behavior questionnaire (SBQ) for adults. J Phys Act Health. (2010) 7:697–705. doi: 10.1123/jpah.7.6.697
34. Gong, X, Xie, XY, Xu, R, and Lu, YJ. Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chin J Clin Psychol. (2010) 4:45–8. doi: 10.16128/j.cnki.1005-3611.2010.04.020
35. Moussa, MT, Lovibond, PF, and Laube, R. Psychometric properties of a Chinese version of the 21-item depression anxiety stress scales (DASS21). Sydney, NSW: Transcultural Mental Health Centre, Cumberland Hospital (2001).
36. Lee, D. The convergent, discriminant, and nomological validity of the depression anxiety stress Scales-21 (DASS-21). J Affect Disord. (2019) 259:136–42. doi: 10.1016/j.jad.2019.06.036
37. Yao, G, and Wu, CH. Similarities and differences among the Taiwan, China, and Hong-Kong versions of the WHOQOL questionnaire. Soc Indic Res. (2009) 91:79–98. doi: 10.1007/s11205-008-9326-4
38. Liu, HX, Chow, BC, Liang, W, Hassel, H, and Huang, YW. Measuring a broad spectrum of eHealth skills in the web 3.0 context using an eHealth literacy scale: development and validation study. J Med Internet Res. (2021) 23:e31627. doi: 10.2196/31627
39. Zhang, Y, Xu, P, Sun, Q, Baral, S, Xi, L, and Wang, D. Factors influencing the e-health literacy in cancer patients: a systematic review. J Cancer Surviv. (2022) 3:1–6.
40. Yang, Y, Yuan, S, Liu, Q, Li, F, Dong, Y, Dong, B, et al. Meeting 24-hour movement and dietary guidelines: prevalence, correlates and association with weight status among children and adolescents: a National Cross-Sectional Study in China. Nutrients. (2022) 14:2822. doi: 10.3390/nu14142822
41. Zhou, L, Liang, W, He, Y, Duan, Y, Rhodes, RE, Liu, H, et al. Relationship of 24-hour movement behaviors with weight status and body composition in Chinese primary school children: a cross-sectional study. Int J Environ Res Public Health. (2022) 19:8586. doi: 10.3390/ijerph19148586
42. Cohen, J. Statistical power analysis for the behavioral sciences. Second ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers (1988).
43. Duan, Y, Shang, B, Liang, W, Lin, Z, Hu, C, Baker, JS, et al. Predicting hand washing, mask wearing and social distancing behaviors among older adults during the covid-19 pandemic: an integrated social cognition model. BMC Geriatr. (2022) 22:91. doi: 10.1186/s12877-022-02785-2
44. UC Davis Health. Omicron BA.5: What we know about this COVID-19 strain. (2022). Available at: https://health.ucdavis.edu/coronavirus/covid-19-information/omicron-variant#:~:text=The%20omicron%20subvariant%20of%20COVIDfrom%20COVID%20infection%20and%20vaccination (Accessed February 24, 2023).
45. Luo, L, Cao, Y, Hu, Y, Wen, S, Tang, K, Ding, L, et al. The associations between meeting 24-hour movement guidelines (24-HMG) and self-rated physical and mental health in older adults—cross sectional evidence from China. Int J Environ Res Public Health. (2022) 19:13407. doi: 10.3390/ijerph192013407
46. Liang, K, de Lucena Martins, CM, Chen, ST, Clark, CC, Duncan, MJ, Bu, H, et al. Sleep as a priority: 24-hour movement guidelines and mental health of Chinese college students during the COVID-19 pandemic. Healthcare. (2021) 9:1166). MDPI. doi: 10.3390/healthcare9091166
47. Rosenbaum, S, Tiedemann, A, Sherrington, C, Curtis, J, and Ward, PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. (2014) 75:964–74. doi: 10.4088/JCP.13r08765
48. Schuch, F, Vancampfort, D, Firth, J, Rosenbaum, S, Ward, P, Reichert, T, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord. (2017) 210:139–50. doi: 10.1016/j.jad.2016.10.050
49. Walsh, JJ, Barnes, JD, Cameron, JD, Goldfield, GS, Chaput, JP, Gunnell, KE, et al. Associations between 24-hour movement behaviours and global cognition in US children: a cross-sectional observational study. Lancet Child Adolesc Health. (2018) 2:783–91. doi: 10.1016/S2352-4642(18)30278-5
50. Guerrero, MD, Barnes, JD, Chaput, JP, and Tremblay, MS. Screen time and problem behaviors in children: exploring the mediating role of sleep duration. Int J Behav Nutr Phys Act. (2019) 16:105. doi: 10.1186/s12966-019-0862-x
51. Sampasa-Kanyinga, H, Colman, I, Goldfield, GS, Janssen, I, Wang, J, Podinic, I, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. (2020) 17:72. doi: 10.1186/s12966-020-00976-x
52. Faulkner, G, Rhodes, RE, Vanderloo, LM, Chulak-Bozer, T, O'Reilly, N, Ferguson, L, et al. Physical activity as a coping strategy for mental health due to the COVID-19 virus: a potential disconnect among Canadian adults? Front Commun. (2020) 5:571833. doi: 10.3389/fcomm.2020.571833
53. Biddle, SJ, and Asare, M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. (2011) 45:886–95. doi: 10.1136/bjsports-2011-090185
54. Rebar, AL, Stanton, R, Geard, D, Short, C, Duncan, MJ, and Vandelanotte, C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. (2015) 9:366–78. doi: 10.1080/17437199.2015.1022901
55. Xia, Y, Fan, Y, Liu, TH, and Ma, Z. Problematic internet use among residential college students during the COVID-19 lockdown: a social network analysis approach. J Behav Addict. (2021) 10:253–62. doi: 10.1556/2006.2021.00028
56. Kitano, N, Kai, Y, Jindo, T, Tsunoda, K, and Arao, T. Compositional data analysis of 24-hour movement behaviors and mental health in workers. Prev Med Rep. (2020) 20:101213. doi: 10.1016/j.pmedr.2020.101213
57. Pelikan, JM, Ganahl, K, and Roethlin, F. Health literacy as a determinant, mediator and/or moderator of health: empirical models using the European health literacy survey dataset. Glob Health Promot. (2018) 25:57–66. doi: 10.1177/1757975918788300
58. Nutbeam, D, and Lloyd, JE. Understanding and responding to health literacy as a social determinant of health. Annu Rev Public Health. (2021) 42:159–73. doi: 10.1146/annurev-publhealth-090419-102529
59. Cam, HH, Ustuner Top, F, and Kuzlu, AT. Impact of the COVID-19 pandemic on mental health and health-related quality of life among university students in Turkey. Curr Psychol. (2022) 41:1033–42. doi: 10.1007/s12144-021-01674-y
60. Rhodes, RE, and Courneya, KS. Self-efficacy, controllability and intention in the theory of planned behavior: measurement redundancy or causal independence? Psychol Health. (2003) 18:79–91. doi: 10.1080/0887044031000080665
Keywords: college student, e-Health literacy, mental health, physical activity, quality of time, screen time, sleep
Citation: Lin L, Liang W, Wang R, Rhodes RE and Liu H (2024) Association of 24-hour movement guideline adherence, mental health and quality of life in young adults: the role of e-Health literacy. Front. Public Health. 12:1344718. doi: 10.3389/fpubh.2024.1344718
Edited by:
Pawel Adam Piepiora, Wroclaw University of Health and Sport Sciences, PolandReviewed by:
Magdalena Superson, WSB Universities, PolandBartłomiej Gąsienica-Walczak, Academy of Applied Sciences in Nowy Targ, Poland
Eva Gjorgjievska, Goce Delcev University, North Macedonia
Copyright © 2024 Lin, Liang, Wang, Rhodes and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huaxuan Liu, YmVsbGFfbGl1aHhAZmpudS5lZHUuY24=
†These authors have contributed equally to this work
 Lixin Lin1†
Lixin Lin1† Wei Liang
Wei Liang Ryan E. Rhodes
Ryan E. Rhodes Huaxuan Liu
Huaxuan Liu