
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
METHODS article
Front. Public Health , 23 May 2024
Sec. Aging and Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1342562
This article is part of the Research Topic International Perspectives on Older Adult Social Isolation and Loneliness View all 54 articles
 R. Ogrin1*
R. Ogrin1* E. Robinson1
E. Robinson1 K. Rendell1
K. Rendell1 S. Alrababah1
S. Alrababah1 D. Fineberg2
D. Fineberg2 K. Fiddes3
K. Fiddes3 A. Yerolemou4
A. Yerolemou4 M. H. Lim5,6
M. H. Lim5,6 L. Engel7
L. Engel7 J. A. Lowthian1,7
J. A. Lowthian1,7Background: There is wide acknowledgement in the literature that social connection is protective against loneliness and depression. More robust research, however, is needed to evaluate interventions that promote social connection. This protocol paper outlines the evaluation of a community-wide social connection program, Connect Local, in metropolitan Melbourne, Australia to support people 65 years and older to increase access to local community services/activities; and to ascertain impact on social connection, loneliness, depressive symptoms, physical and mental wellbeing, and use of health services.
Methods: A Type 1 Hybrid design, including program effectiveness, cost-effectiveness, and implementation evaluation of the Connect Local program, will be undertaken. Eighty-eight participants aged ≥65 years with one or more chronic health condition, who are also either experiencing or at risk of loneliness, social isolation and depressive symptoms will be invited to participate in the evaluation. Outcomes, measured at baseline, 3, 6 and 12 months, include loneliness, social isolation, depressive symptoms, social anxiety, goal attainment, wellbeing, quality of life and health care utilisation. A gender and age matched comparator group of 88 individuals will be recruited from outside the intervention local government area. Impact of the intervention on community service providers in the target region will be evaluated using mixed methods, where triangulation will be used to combine the qualitative and quantitative data using a deductive-simultaneous design. Changes in wellbeing and quality of life of community volunteers will also be measured. All groups will be interviewed to ascertain their experience and perceptions of the program. The economic evaluation will use a Social Return on Investment (SROI) approach, to include outcomes at the individual, community, and system levels. Implementation outcomes will consider Reach, Adoption, Feasibility, Acceptability, Appropriateness, Fidelity, and Sustainability of the intervention.
Discussion: This study will provide a better understanding of the impacts of a community-wide social connection approach in older adults, the community and broader system.
Clinical trial registration: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=385192; Identifier ACTRN12623000968673.
Many older people live with chronic health conditions, with the prevalence and number of chronic health conditions rising with increasing age (1–3). In addition to chronic health conditions, many older people also report loneliness and social isolation (4). The Global Initiative on Loneliness and Connection defines loneliness as a subjective unpleasant or distressing feeling of a lack of connection to other people, along with a desire for more, or more satisfying, social relationships (5). Loneliness is different to social isolation, defined as having objectively fewer social relationships, social roles, group memberships, and infrequent social interaction (5). Prolonged periods of social isolation and loneliness can negatively impact a person’s mental, physical and social wellbeing, leading to increased risks of developing social anxiety, clinical depression and suicidal ideation (6) and is associated with developing dementia (7, 8), cardiovascular disease (9) and early mortality (10). This may have been compounded by recurrent COVID-19 pandemic lockdowns (8, 11). Susceptibility to depression and anxiety increases with the cumulative impact of social isolation and loneliness on an individual’s mental health and social wellbeing (12, 13). Currently, healthcare systems are focused on treating illness and disease, rather than adopting a preventative approach that enables people to keep healthy and well, such as supporting social connections (6, 14–16). Addressing social needs is critical not just for improving health and wellbeing, but also to ensure improved, appropriate, and efficient use of finite healthcare resources; as older people who are lonely are more likely to seek medical attention in order to satisfy social needs (17). The subsequent long-term impact of unaddressed loneliness on health (7, 9, 15) will further increase healthcare system utilisation (18).
Optimal healthcare delivery is holistic, following the biopsychosocial model, considering social, psychological, and biological factors (19). This approach is designed to enable care that meets the needs of the individual, including enabling continuity of care, with early medical and psychosocial intervention to prevent escalation to more significant health issues (20). Unfortunately, holistic care is lacking, with current models of care being siloed and predominantly focusing on biomedical aspects (14, 16). Loneliness has been found to be more detrimental for mental health correlates and social isolation for physical health (21, 22) but the presence of both loneliness and social isolation further exacerbates poor health outcomes and increases mortality (21, 22).
One intervention that has the potential to address both social isolation and loneliness is social prescribing (23), defined as:
A means for trusted individuals in clinical and community settings to identify that a person has non-medical, health-related social needs and to subsequently connect them to non-clinical supports and services within the community by co-producing a social prescription – a non-medical prescription, to improve health and wellbeing and to strengthen community connections (24).
Social prescribing is currently receiving increased interest; however robust evaluations are limited.
To date, existing studies on effectiveness of social prescribing interventions are of varying quality, where a rapid review found mixed results with some positive, mixed and negative outcomes reported (25). Other reviews identified that the majority of studies focus on positive qualitative outcomes (23, 26). There have been limited quantitative outcome studies, focusing mainly on health-related outcomes, showing inconsistent results (23, 26). This may be because the quantitative measures used for evaluation of outcomes may not adequately capture more complex outcomes, such as community connectedness, social engagement, confidence, willingness to give and receive peer-support, and confidence to access services and self-determination and self-care. These ‘hard to quantify concepts’ were captured in qualitative studies, which predominantly reported positive outcomes for participants (23, 26, 27). Additionally, only a few social prescribing interventions measure loneliness (28).
In the UK, the National Academy for Social Prescribing has undertaken systematic reviews on social prescribing and social connection activities with international evidence (23, 29). Existing evidence highlights more robust research is needed and suggests:
a) The most effective models comprise a collaboration of local partner organisations working together;
b) Social prescribing can have a positive immediate impact on a wide range of outcomes, including reductions in loneliness, and improvements in mental health, social connections and overall wellbeing;
c) Social prescribing can reduce pressure on primary care and save healthcare costs;
d) Social prescribing generates a favourable Social Return on Investment (SROI) in most cases;
e) More research is needed that includes more diverse populations; and
f) There is less evidence on the medium and long-term impact of social prescribing, and research in this area is required.
Recent systematic reviews findings have indicated that future research has to include evaluations on intervention outcomes at the individual, community and system levels, implementation outcomes and cost effectiveness (30, 31).
Specific to health economics, there is a need to understand and quantify the social and economic value that community-based assets generate, for example, whether enabling reciprocity and building mutual trust amongst community members promotes social wellbeing that leads to cost saving by reducing escalation of health issues requiring health service use. Loneliness is associated with a substantial economic burden, where individuals who are lonely are more likely to seek medical attention to satisfy social needs (17, 18). A report from 2021 (32) estimated the cost of loneliness at AUD$2.7 billion each year, which equates to an annual cost of AUD$1,565 for each person experiencing loneliness. Therefore, interventions that aim to alleviate loneliness are likely to be cost saving and cost-effective but there is currently limited evidence that this is the case (33, 34).
To enable the delivery of an evidence-based, person-centred approach to social prescribing in Australia, we have codesigned a new program, Connect Local, based on current UK models.
Connect Local is a newly-developed, codesigned program where community members living in one south-eastern metropolitan Melbourne local government area (LGA), will be supported to connect with local social services and/or activities through a paid trained Community Connector role, with the aim of reducing loneliness, social isolation and/or depressive symptoms; and improving wellbeing (35). This is a whole of community approach to promote social connection incorporating social prescribing, in addition to network building, awareness raising, volunteer and peer support, and other social capital building activities. The program will be evaluated, considering program effectiveness, cost-effectiveness, and implementation summative and process outcomes.
The Connect Local initiative represents a collaboration led by an aged and community care provider, Bolton Clarke; with a tertiary healthcare provider, Alfred Health; a primary care organisation, South Eastern Melbourne Primary Health Network; and a multi-sector and multi-discipline network, the Australian Disease Management Association, called Connecting Communities to Care. Stage 1 comprised co-designing a community-wide approach to facilitate older community members to link with local social supports in one LGA of Eastern metropolitan Melbourne, Australia.
Stage 2 involves implementing and evaluating the Connect Local early intervention program that links older Australians with local social supports, in the Glen Eira LGA.
In this project, we aim to evaluate a program that will support older community members with at least one chronic condition who are at risk or experiencing loneliness, social isolation and/or depressive symptoms to optimise their wellbeing through building their capacity to socially connect. This will be done by enabling their access to local, relevant, social supports using a paid Community Connector role, supplemented with volunteer and peer support to help them do this.
Social capital theoretical constructs will underpin this work. Social capital is a broad, umbrella concept with many components and difficult to define, attempting to map the value of relationship networks (36). Basically, social capital is ‘something social’ (called “Form”), drawn from a Source (be it individual competencies, history and culture, education and others) that has the potential/ability/capacity to produce Outcomes that are productive, beneficial and important (36–39). Social capital exists between people, in groups and communities and in communities and society, and can benefit individuals, the collective and/or both. The ‘something social’ requires a structural dimension be in place to enable cognitive and relational dimensions to occur (36). More specifically, the structural category facilitates cooperation (enabling it to occur), but the cognitive category predisposes cooperation (so people actively seek out and participate in social engagement) (40). These three dimensions are connected and mutually reinforcing, so cannot be treated separately. In addition, the context within which these activities are implemented is important, which includes the resources necessary to enable them to occur. Resources can be defined as information, trust, support (41), as well as the traditional wealth, status, power and social ties linked to the individual (42) – context (including resources) mediate the ability to achieve the desired outcomes. Our approach focuses on the pro-social aspects (giving, sharing, helping, caring, supporting) provided within a network of social connection, which will lead to reduced loneliness, social isolation and depressive symptoms and improved psychological and physical wellbeing. All of which will eventually lead to reduced health system use (such as reduced hospitalisations). Putting this all together, the social capital approach that we will utilise can be depicted in Figure 1.
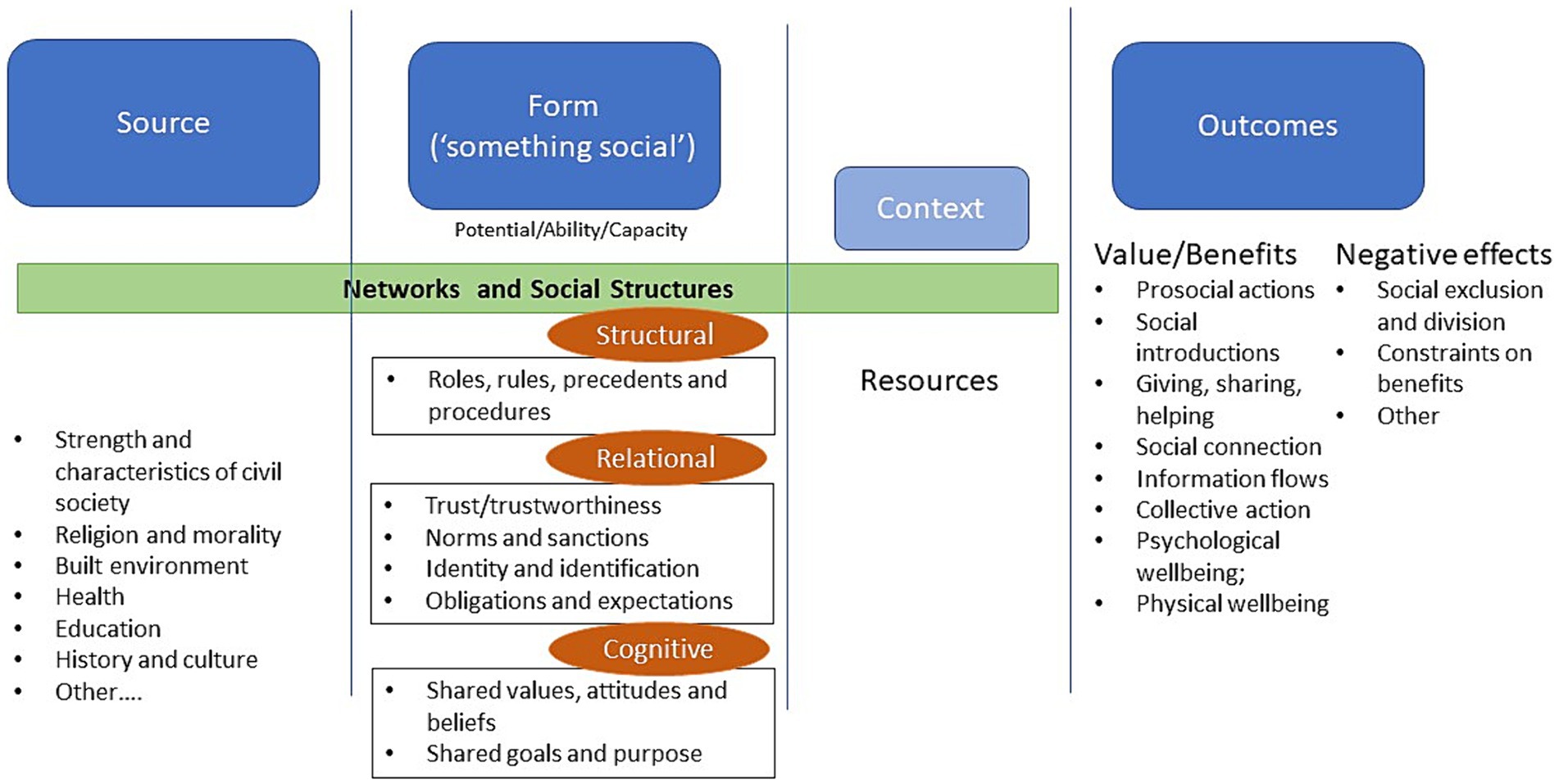
Figure 1. Social capital approach adapted from a model developed by Claridge (43) from the Institute for Social Capital.
Specific to loneliness, we refer to the conceptual model developed by Lim et al. (44) which guided the different types of variables collected in our evaluation but also provide a more comprehensive socioecological approach to reducing loneliness. The Conceptual Model of Loneliness articulates the different risk factors and correlated for loneliness in three parts: demography (i.e., age, gender, marital status, living states, socioeconomic status), health (physical, mental, cognitive, brain and biology), and socio-environmental (e.g., workplaces, digital use) (44). It is assumed that everyone holds at least some risk factors of loneliness and these risk factors interact and may lead to problematic levels of loneliness (44). Therefore, it is critical to consider how different types of factors (such as individual, relationship, and community factors) can also contribute to the severity of loneliness.
Finally, program development was underpinned by a Theory of Change, generated according to the changes stakeholders aspired to achieve as a consequence of delivery of programs to promote holistic wellbeing, shown in Figure 2. Table 1 shows the participants of the stakeholder engagement and level of engagement that led to the development of the Theory of Change. Participants included those involved in codesign from previous studies aiming to promote holistic wellbeing through community supports: Older Women Living Alone (OWLA) (45) and Peer support for Older WomEn to pRomote wellbeing and independence (POWER) (46). These elements were then refined from codesign sessions in Stage 1 of this study.
We propose to contribute to the evidence-base by undertaking an evaluation to measure program effectiveness, health economic outcomes and the implementation of the Connect Local program. This evaluation will include medium- and longer-term loneliness, social isolation, depressive symptoms, and wellbeing outcomes of the community-wide social connection initiative with a comparator group. The evaluation will also include a comprehensive economic evaluation, using a Social Return on Investment (SROI) approach (47), to cover outcomes at the individual, community and system levels. Finally, implementation outcomes will also be evaluated to consider Reach, Adoption, Feasibility, Acceptability, Appropriateness, Fidelity and Sustainability of the intervention.
At the end of the project we aim to contribute to the greater understanding of how a social connection program for older people functions, building on the middle conceptual and grand theories used to underpin this work. We anticipate this will enable a greater conceptualisation of how implementation of this program impacts the included stakeholders and is in turn impacted by the multiple contextual components.
The research team is using a pragmatic approach, where all necessary approaches will be used to understand the research problems. There are a number of different components that will be considered, and each component will be using a different approach.
The outcomes related to the impact of the Connect Local intervention on older individuals and cost effectiveness will include a post-positivist ontological approach, where there is a single reality, imperfectly known (48, 49). Following on from this, our epistemological approach considers that we can only establish probable truths, as obtaining knowledge is subject to human error (48, 49). Axiomatically, we are considering that our intervention will make the community a better place by reducing loneliness, social isolation and/or depressive symptoms, leading to wellbeing, increased community activity/program use and reductions on health system use. The evaluation team aims to observe and measure the changes resulting from the Connect Local intervention, therefore position themselves outside the context of the intervention.
The outcomes related to the impact of the Connect Local intervention on the community, health system and the implementation of the program will be using a critical theory approach, where there are multiple subjective realities, influenced by power relations in society (48, 49). The knowledge is subjective, and co-constructed between individuals and groups (48, 49). The aim is to understand the relationships and these groups. The evaluation team is part of the implementation process, actively engaging and therefore position themselves inside the context of the intervention.
The ten members of the research team (nine female), consist of eight researchers, with research experience varying from early career (E.R., K.F., and S.A.) midcareer (R.O., D.F.), to highly established (M.L., L.E, and J.L.). The two non-research team members have work roles that support delivery of care in health (A.Y) and aged and community (K.R.) systems.
Five team members currently work within an aged and community care service organisation (R.O., K.R., E.R., S.A., and J.L.). Two team members work as clinicians, one in a hospital (D.F) and one in primary care with a university position (M.L.). One works within a university environment only (L.E.) and one team member works at a peak health organisation (K.F.). The professional backgrounds of the research team are also diverse, with clinical training of six team members [in the fields of podiatry (R.O.), optometry (S.A.), nursing (K.F.), psychology (M.L.), speech pathology (J.L.), endocrinology and general medicine physician (D.F.)] and fields of health economics (L.E.) and business and management (K.R. and A.Y.).
This manuscript includes the relevant elements from the Standard Protocol Items for Clinical Trials (SPIRIT) guidelines (50), and the consolidated criteria for reporting qualitative research COREQ (51) and Standards for reporting implementation studies (STARI) (52).
The evaluation will be a Type 1 Hybrid effectiveness-implementation study design (53), with research objectives to ascertain program effectiveness, program cost-effectiveness; and implementation summative and process outcomes. This evaluation comprises Stage 2 of a two-stage project, with Stage 1, codesign of the program, being published separately. Hypotheses and research questions in the form of PICO [participants, intervention, comparator and outcome(s)] (54) have been generated for the research components involving a comparator group for quantitative data. Propositions and research questions in the form of SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) (54) have been generated when data is mixed method or qualitative.
Hypotheses are proposed for the first two evaluation components:
Compared to the comparator group, older people receiving the intervention will, when compared to baseline, report at 3-, 6- and 12-months follow-up:
(i) a reduction in loneliness, social isolation and/or depressive symptoms;
(ii) improvement in wellbeing and quality of life;
(iii) increased access to activities/services in the community.
Three months after participation in the program, community volunteer participants will have improved wellbeing and quality of life when compared to baseline.
It is hypothesised that all stakeholders: intervention, volunteer and service provider participants will also have a positive perception of and experience with the program.
Research question for older participant cohort using PICO:
Does participation in the Connect Local social connection program reduce loneliness, social isolation and/or depressive symptoms, improve wellbeing and quality of life and increase access to activities/services in community of older Australians when compared to a similar group who do not have access to a similar program?
Research question components for stakeholders using SPIDER:
Sample: volunteers and service provider participants;
Phenomenon of interest: perception and experience of program;
Design: prospective surveys and semi-structured interviews;
Evaluation: impact on community and health services, and perceptions of the program;
Research type: mixed methods.
Question: What are the perceptions and experiences of volunteers/service provider participants after being a part of the Connect Local program?
(i) Among the target cohort within the study LGA, Connect Local will generate improvements in the health, wellbeing, and quality of life of participants that can be translated into monetary values. This will be established by comparing the situation before and after the Connect Local intervention and comparing outcomes with the comparator group.
(ii) When comparing the cost of the intervention with the social and economic outcomes, including health service utilisation, the SROI ratio will yield a return greater than the investment.
Research question using PICO:
Is Connect Local more cost effective to address loneliness, social isolation, depressive symptoms and wellbeing in older community members compared to no Connect Local?
A proposition is proposed for the third research component:
The program effectiveness and cost-effectiveness components will be evaluated in a prospective, cohort quasi-experimental (non-randomised), pragmatic trial, using a convenience sample of participants, with the intervention group drawn from those living in the target LGA who access the community connector.
Research question components using SPIDER:
Sample: older community members, volunteers and service provider participants;
Phenomena of interest: reach, adoption, feasibility, appropriateness, fidelity, sustainability.
Design: prospective surveys, semi-structured interviews, administrative data;
Evaluation: implementation of program as planned;
Research type: mixed methods.
Question: What are the perceptions and experiences of [participants] about the Connect Local program and it being implemented as planned?
The Connect Local program will involve eligible individuals to access a trained and paid Community Connecter professional. Community Connectors are individuals with a counselling, community development, health/allied health professional and/or life coaching background, who receive training in social prescribing (55), wellness and reablement and positive ageing, diversity in ageing, mental health first aid and trauma informed care.
Once a referral/contact is received, the Connect Local program manager contacts the community member and first discusses the program, to ascertain that it is what they are seeking. If so, the community member is screened for eligibility, namely, they live in target geographic location, are aged 65 or older, have a chronic health condition, and are in need of social connection. If appropriate, the program manager organises the Community Connector to contact the individual to organise a time to meet face to face and commence the program. As shown in Figure 3, the Community Connector will work with eligible community members to:
1. Identify what matters to the individual and screen for loneliness, social isolation and depressive symptoms: the Community Connector holds a rapport-building conversation, involving open-ended questions and using motivational interviewing techniques guided by the NHS document ‘What matters to me?’ (56). The question topics have previously been codesigned with Community Connectors and community members to ensure they are fit-for-purpose for the local population, and include: expectations of the program, personal history in the area, past activities of interest, and when they remember being happy – where they were, who they were with, and what they were doing;
2. Work together on generating goals that address a social need/s, and a develop a plan to achieve these goals by linking the individual to activities and/or services being offered in the target geographic area. This is based on the discussion on “What matters to me?” and what existing available programs and activities are in the region, as well as the community member’s level of digital engagement and any transportation requirements. Usually three or four programs/activities are generated for pursuing;
3. Support the individual to access these activities/services using local resources such as volunteer support including transport. This involves the Community Connector reaching out to program/activity providers agreed to in point 2, and organising to meet with the community member at the program/activity location. This serves as an introduction and, if possible, have the community member participate or at least view the program/activity, to ascertain whether this is something they are interested in engaging with. If the community member is interested, the Community Connector facilitates ongoing engagement in the program/activity, as needed. If the community member is not interested in this program/activity, they pursue an alternative program/activity discussed previously; and.
4. Review follow up to ensure that the activities and/or services are addressing their needs. Should there be any issues, the Community Connector may either engage with the service/activity provider to address them or work with the individual to develop a new goal, plan and access new activity/service.
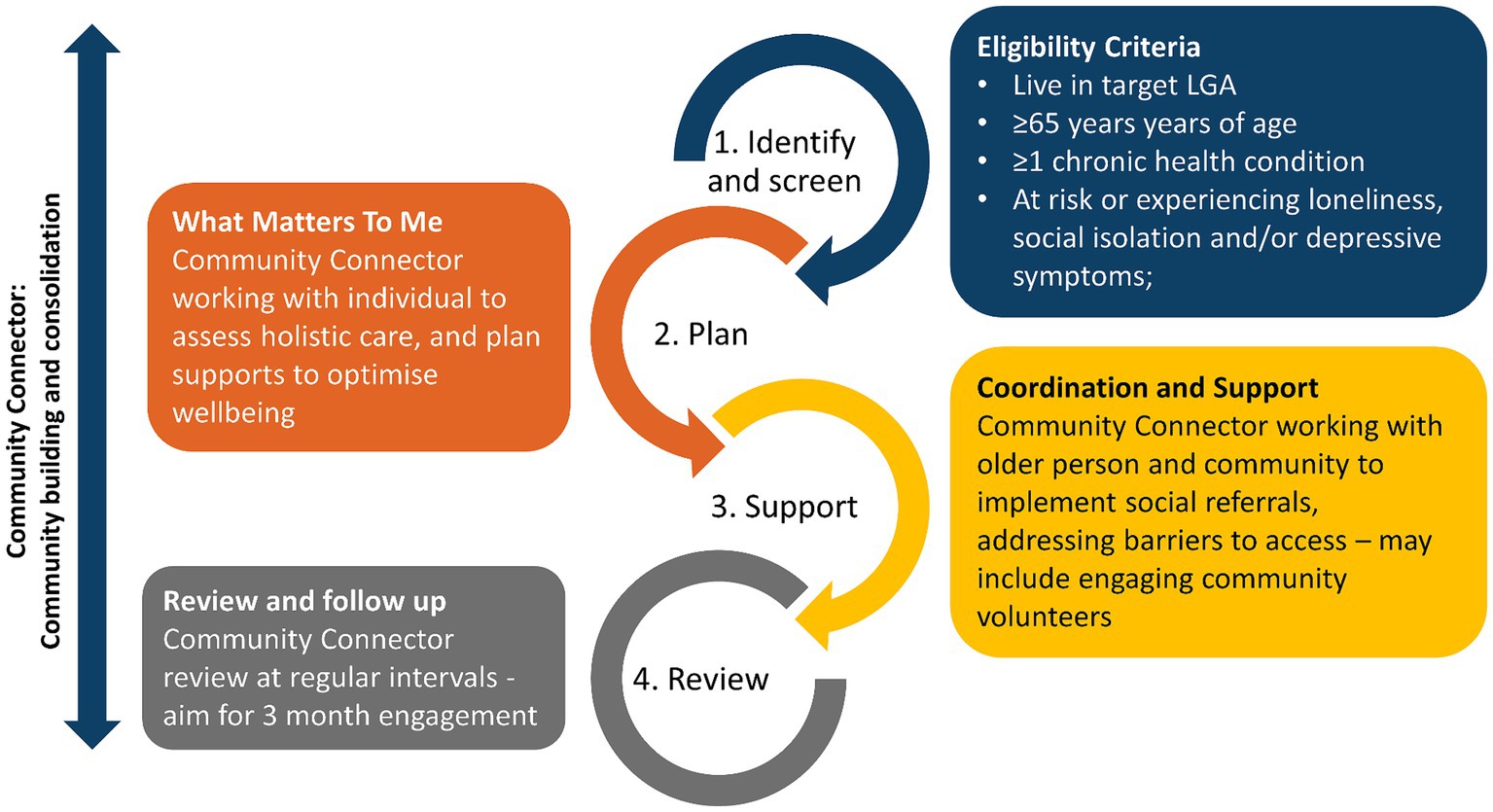
Figure 3. Service flow of Connect Local. Adapted from Mann et al. (20).
Individuals who participate in all four elements will be considered to have completed the full program. Meetings between the Community Connector and the participant will be undertaken in a mutually agreed upon location, including local community houses, local spaces such as libraries, local cafés, or in the participant’s home.
People will be engaged in the program through multiple sources: the local tertiary hospital, aged care provider, general practices, allied health providers, community health providers, through the program website, and general community access.
These individuals will receive usual care (regular access to activities in their LGA), and will not be engaged in the Connect Local program.
There are three participant groups involved in this evaluation: older community members, community volunteers, and health and social care providers.
The inclusion criteria include being aged 65 years or older; understand and speak English sufficiently to understand and be involved in the program; live in the target LGA; community dwelling (including those experiencing homelessness); have at least one chronic health condition; are at risk or experiencing loneliness, social isolation and/or depressive symptoms. Screening tools are summarised in Table 2, loneliness will be assessed using both the Single Item Measure and UCLA-3 as per recommended national indicators of loneliness (66).
The exclusion criteria include living in residential aged care; individuals who do not speak English sufficiently to understand the program; and individuals who do not have the cognitive capacity to consent [assessed using a Cognitive Capacity to Consent Checklist (67)].
All eligible individuals will be made aware of the evaluation by the Community Connector and asked if their details can be shared with the researchers to contact them about the study. The researchers will contact the individuals to obtain consent. If consent is obtained, individuals will be asked if they would like to be informed of trial results.
Given the proposed whole of community impact of Connect Local program, the inclusion criteria for the comparator group are the same as for the intervention group, except that they do not live in the target LGA. These participants will be recruited from the local tertiary hospital and aged and community care provider. All eligible individuals will be made aware of the program through their care provider and will be asked if their details can be shared with the researchers to contact them about the study. The researchers will contact the individuals to obtain consent. Recruitment will be monitored in blocks of five to match comparator participants by age and gender to the intervention participant group.
Inclusion criteria include: any age (including younger people of school age); Live, work or are willing to regularly come to the target LGA; currently a volunteer engaging with community members receiving Connect Local program; and understand and speak English sufficiently to understand the program.
Organisations engaging volunteers will share the information on the evaluation, and all volunteers who have been involved in supporting individuals engaging in Connect Local will be invited to reach out to researchers and participate in the evaluation.
Inclusion criteria are individuals who work at health and social services that support eligible older participants or volunteers in the target LGA, including the Connect Local program and the Community Connectors. Researchers will obtain information on health and service providers engaged in the program from the Community Connector and contact them directly to ask them to participate in the evaluation.
Data will be collected either by researchers via the phone, in-person, in paper-based surveys, or by Community Connectors during program operations. Study data will be collected and managed using REDCap electronic data capture tools hosted on a secure server at Bolton Clarke (68), which only researchers will have access by password. Table 2 outlines the different levels and the data collected, while Table 3 outlines the time points of data collection. If data collection causes distress to participants, interviewing will be immediately halted and existing escalation procedures will be followed, including referral back to the referring healthcare provider (community members), service responsible (volunteers), or external mental health services.
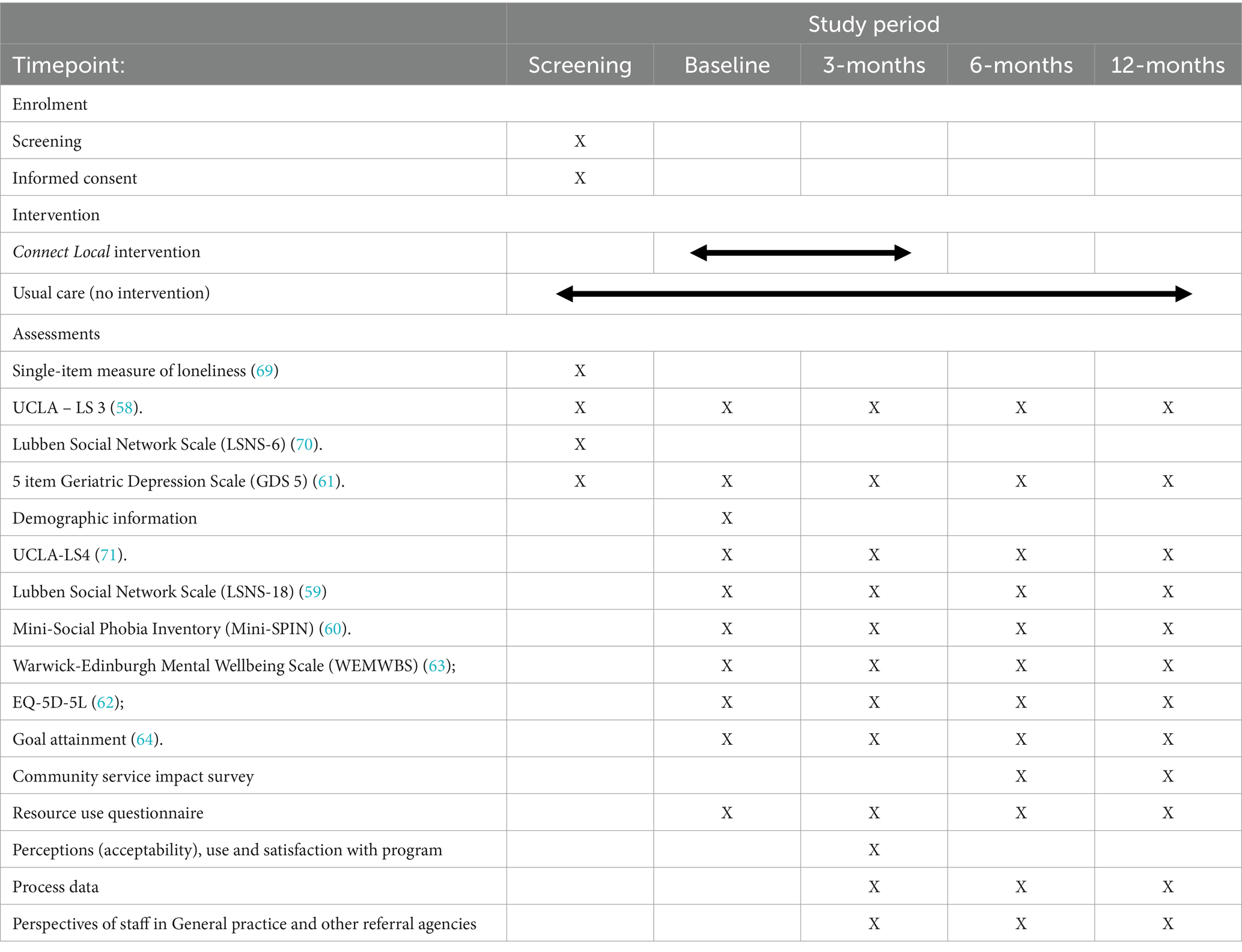
Table 3. Schedule of enrolment, interventions and assessments, per SPIRIT guidelines (50).
The aim of this evaluation is to assess the participant outcomes, and program effectiveness and impact from the Individual, Community and Health Service perspectives.
This is the level at which individuals are impacted directly, including older community members, volunteers and health and social service providers.
For older community members, we will consider the primary outcome as a mean change in loneliness, from baseline at 3, 6 and 12 months for participants receiving the Connect Local program, when compared to the comparator group. This will be measured using UCLA-3 as informed by previous research that support the sample size calculations (58). At this stage, there is insufficient research data to calculate sample size when using UCLA-4 (57), however this tool has been recommended for use by community organisations by Australia’s national network, Ending Loneliness Together (71), therefore we will also utilise this tool to capture loneliness to ascertain whether it can be utilised with this cohort in future studies.
As outlined in Tables 2, 3, secondary outcomes, including social isolation, social anxiety, depressive symptoms, and improvement in quality of life and wellbeing, are a mean change from baseline at 3, 6 and 12 months for participants receiving the Connect Local program, when compared to the comparator. Achieved goals, as measured by the Goal Attainment scale (64), will also be gathered from the intervention group.
For community volunteers involved in the Connect Local program, as per Tables 2, 3, we will collect health-related quality of life and wellbeing measures at baseline, 3, 6 and 12 months.
Perceptions of the program will be collected from community members in the intervention group, volunteers and service providers involved in referred to the Connect Local program through interviews or focus groups at three months from participant baseline. Questions will invite participants to share their thoughts around the following aspects of the program: Relational (trust and trustworthiness, obligations and expectations, identity and identification), Cognitive (shared language, codes and narratives; shared values, attitudes and beliefs; and shared goals and purpose), and Structural (roles, rules, precedents and procedures).
As per Table 2 the following indicators will be collected to evaluate the impact of the program on the broader community: the number of participants who access community activities/services, the number and types of services offered to and used by participants in both the intervention and comparator groups at baseline, 3, 6 and 12 months using the Resource Use Questionnaire [adapted from Fletcher (65)].
We will also ask community service and/or activity providers about the impact of the program on their services six monthly, using the Community Service Impact Survey (72), and their perspectives of the program through interviews or focus groups at three months from when participants were engaged in their program.
To evaluate impact of Connect Local on health services use such as hospitalisations, General Practitioner (GP) visits and other health service visits, several health service-related indicators will be collected from participants in both the intervention and comparator groups at baseline, 3, 6 and 12 months using the Resource Use Questionnaire [adapted from Fletcher (65)], as per Tables 2, 3. Using interviews, the service provider morale in general practice and other referral agencies and healthcare provider satisfaction will also be gathered at three months from when their patients engaged in the Connect Local program.
The primary outcome is a reduction in loneliness at 3 months for participants receiving the Connect Local program, when compared to the comparator group. A program conducting similar activities found a statistically significant reduction in mean UCLA-3 scores of 0.85, with a medium effect size of 0.37 (73). Using this effect size at 0.05 alpha, 76 participants are required in the intervention group to reach 0.9 power. Allowing for 15% attrition at the 3 month follow up, we have increased the sample size to 88. A matched comparator group will be recruited at a 1:1 ratio, as such a total of 176 participants will be recruited to the intervention and comparator groups.
To consider the social value generated by the initiative, a triple bottom line of social, economic and environmental value through Social Returns on Investment (SROI) will be considered (74). Economic evaluation is a tool used to guide resource allocation decisions in health care, where effects are often expressed in health-related units. However, it is anticipated that interventions that alleviate loneliness are not only associated with health benefits but also broader societal benefits, where benefits often accrue across sectors. As such, a broader evaluation framework is required to determine the social and economic value of the Connect Local intervention, such as Social Return on Investment (47).
The scope of the health economic evaluation will involve data collected as part of this evaluation between May 2023 and May 2025 (8 quarters), during which time the program will be fully established and running in the target LGA. The categories of stakeholders that will be operationalised will be:
1. Beneficiaries: those who experience the outcomes of an intervention (community members) involved in Connect Local;
2. Implementers: suppliers and subcontractors (Bolton Clarke, Social Service providers);
3. Promoters: those who provide support and a conducive environment for implementation of the intervention (health care providers); and
4. Funders: those who directly and indirectly finance the project (The Ian Potter Foundation, Department of Health, target LGA City Council).
The theory of change, shown in Figure 3, developed for this study, was used to underpin this cost-effectiveness evaluation.
The evaluation component will involve the following SROI process steps:
Data on loneliness, social connection, depressive symptoms, wellbeing, quality of life and health service use at baseline, 3, 6 and 12 months will provide evidence of outcomes, drawing comparisons between the intervention and comparator groups. Each outcome will be then monetised using financial proxies. Costs and benefits that occur at different time points will be made comparable by adjusting for inflation in order to calculate net present value (47).
This stage will determine those aspects of change that would have happened anyway or are a result of other factors. Such aspects will be eliminated from consideration. Qualitative and quantitative data (surveys on loneliness, social connection, depressive symptoms, wellbeing and quality of life at baseline, 3, 6 and 12 months) will provide this evidence. Monetised outcomes will be discounted on the basis of what would have happened without the intervention (deadweight), what outcomes are displaced by the intervention (displacement), who else has contributed to the outcomes aside from the funder (attribution), and whether experience of the outcomes declines over time (drop off).
This will involve adding up all benefits. Investment into the Connect Local will be compared to the discounted, monetised value of benefits. The discounted, monetised value of benefits and outcomes will be divided by total investment (inputs) to estimate the SROI ratio.
In order to ascertain the effectiveness of the implementation of the program, the following methods will be used:
To ascertain the useability of the intervention (does it reach the right people? Are they using it?), we will collect demographic data of participants, number of clients who engage with the Community Connector and number of participants who complete the program, using administrative data from the Connect Local program, stored in Bolton Clarke’s client record system.
To ascertain the perceived fit and relevance of the intervention, the extent to which it can be used in the participating organisations, and acceptability (overall experience), we will collect: time taken to complete the program (collected through administrative data), perception/attitudes of all stakeholders as to the ease of use, usefulness of, and satisfaction with, the program (through interviews), and organisational support systems and processes also through interviews as well as the Resource Use Questionnaire [adapted from Fletcher et al. (65)] collected at 3, 6 and 12 months.
To ascertain the uptake of the intervention into practice as planned, and the extent to which it can be embedded into practice to promote sustainability, we will use administrative data on the delivery of all four program components outlined in section 2.2 above, and organisational support systems and processes to enable this. We will supplement this information with in-depth data from interviews/focus groups with all participant groups, using open-ended questions around the participant experiences of the program components by participants. These questions will include sharing thoughts on: being made aware of the program and signing up; the engagement with the community connector – the process of finding out ‘what matters to you?’; How they connected with the programs/activities; Whether this went well and what happened then.
For all quantitative, repeated, continuous individual level variables (loneliness, social isolation, social anxiety, depressive symptoms, wellbeing, quality of life) the main research question will be whether the study intervention is effective at improving the outcome of interest compared with usual care. Modelling these data will focus on fitting linear mixed models using different covariance matrices such as: unstructured, an exchangeable-changeable and AR level-1 residual matrices, where the mean structure of all fitted models include a term for intervention group and a term for time and an interaction term for time and intervention. Non-linear outcomes will be fitted using Generalised Estimating Equations (GEE) analysis which requires that the missingness mechanism is Missing Completely At Random (MCAR). Alternatively, polynomials and/or piecewise linear functions will be utilised for modelling outcomes with non-linear growth trajectories if responses are Missing At Random (MAR). To ascertain whether the missing data is MCAR or MAR, we will utilise methods such as data inspection, applying domain knowledge and comparing summary statistics between cases with complete data and those with missing data to determine the missing data mechanism. An understanding of the mechanism will enable an appropriate statistical method to be chosen to handle the missing values in the data set.
For quantitative, binary or dichotomous individual level outcomes (scales that have cut-off scores: loneliness (UCLA-3), social anxiety, depressive symptoms) additional analysis will be undertaken addressing the research question: do the interventions differ in their effectiveness, such that individuals in the intervention group experience a greater improvement in their probability of achieving the desired outcome compared to those receiving usual care. Generalised linear mixed models (GLMMs) for dichotomous outcomes will be used as well as GEE. The typology of missing data will be investigated to make sure that the assumptions of the adopted statistical technique are not violated. Our choice of GLMMs is based on the specific characteristics of the data, as well as the advantages provided by GLMMs in handling dependent responses in longitudinal or repeated measures studies. As highlighted in Breslow and Clayton (75), GLMMs incorporate random effects into the linear predictors and are particularly well-suited for modelling the dependence among response variables in such study designs.
Selection of the model that best fits the data will be based on the low goodness-of-fit measures such as the Akaike information criterion (AIC) and Bayesian information criterion (BIC). Additionally, the log-likelihood ratio test will be employed as another method for evaluating model fit.
All quantitative community and system level variables, as well as the goal attainment will be analysed descriptively. Descriptive statistics will be presented as proportions, means (standard deviations) or, for variables that did not conform to a normal or log-normal distribution, medians (interquartile range).
Statistical analysis will be performed using STATA V.15.0 (STATA Corp LP., College Station, Texas, United States). We will use a Type I error rate of 5% to indicate statistical significance, with 95% confidence intervals (CI).
General and generalised linear mixed models use maximum likelihood estimation which produces robust/unbiased estimates as they make implicit corrections for missing data, hence they are likely to retain more power if participants are lost to follow-up than traditional repeated-measures ANOVA/ANCOVA approaches which use “complete-case-analysis” approach that only includes cases with no missing data in the analysis. Maximum likelihood estimation (MLE) for incomplete longitudinal data (continuous or categorical) uses all available information, which means all participants will be included in the analysis regardless of whether they had complete responses for all occasions/timepoints or not. The MLE estimates are consistent if the assumption of data missingness is MAR and is more robust than using imputed values.
If more than 5% of the outcome data are missing, a sensitivity analysis will be conducted comparing fitted models in terms of estimates and corresponding standard errors using maximum likelihood estimation with and without considering different imputation techniques.
For all qualitative individual, community and system level variables, interviews with participants will be audio-recorded, transcribed and then analysed utilising thematic analysis. Thematic analysis based on grounded theory involves finding repeated patterns of meaning within qualitative data (76) and will be facilitated with the use of qualitative management and analysis software such as NVivo (77). In addition, an interview summary will be created for each interview and circulated to the research team, facilitating the team’s ongoing knowledge of the data being collected. An inductive approach will be used within the project, which allows for themes and findings to emerge from the data, grounding the findings in the perspectives and experiences of participants. Finally, situational analyses will be used to supplement basic grounded theory with situation-centred approaches, enabling the consideration of all of the collective actors and the arena’s within which they engage to develop and fully articulate an ordered situational map (78).
Triangulation will be used to combine the qualitative and quantitative data using a deductive-simultaneous design (79) where the core component is quantitative, and the supplemental component is qualitative.
The following accepted systematic approach to analyses of the SROI approach will be undertaken (47, 80).
The research team will identify and categorise the stakeholders, and the outcomes most relevant for each, and then apply the following tools of SROI (outlined below): consideration of deadweight, displacement, attribution and drop off. We will do this through discussion between team members undertaking evaluation and program implementation in relation to each of the outcomes considered in the SROI. See the Box 1 re: tools of SROI.
BOX 1 Tools used to calculate Social Return on Investment (SROI)
Tools of SROI
Establishing impact (attribution, deadweight, displacement, drop-off):
To minimise the risk of overclaiming the benefits it was necessary to account for deadweight, displacement, attribution, and attrition.
Deadweight: responds to the question: ‘How much of the outcome would still be attained without the activity delivered?’
We will use the quantitative data captured in the comparator group to ascertain this information, measured as a percentage, and then that percentage of the outcome will be deducted from the total quantity of the outcome.
Displacement responds to the question: ‘Were there any activities with the same outcome displaced by the intervention being evaluated?’
We will capture this information when collecting service information from participants involved in the program and comparing them to what was captured in the comparator group – using a percentage and deducted from the total outcomes.
Attribution responds to the question; ‘Who else contributed to the attainment of the outcome?
The research team will identify all relevant stakeholders and to assess how much of each outcome could be attributed to the delivery of Connecting Communities to Care with due circumspection. This will be calculated as a percentage.
Drop-off responds to the question: ‘How much of the outcome is lost in the years post intervention?’
To calculate the percentage of the outcome lost in the years after delivery of the intervention. It is calculated by deducting a fixed percentage from the remaining level of outcome at the end of each year. This will be calculated as a percentage.
Calculating the SROI:
The calculation of the SROI will consider the total value of the inputs in the program. The discounted, monetised value of benefits and outcomes will be divided by total investment (inputs) to estimate the SROI ratio.
The process evaluation aims to assess the effectiveness of the implementation process on reach, adoption, feasibility, acceptability, appropriateness, fidelity, and sustainability.
1. Reach and adoption: this will include quantitative data that will be reported descriptively, using frequencies and proportions.
2. Feasibility, acceptability and appropriateness: this will include quantitative data that will be reported descriptively, using frequencies and proportions. Qualitative data will be analysed thematically using an inductive approach, as described above, to ascertain themes around feasibility, acceptably and appropriateness of the program. Process data regarding organisational support systems and processes will also be reviewed by the research team, discussed as a group, considering the content in light of the qualitative data analysis results to form synthesised outcomes. This information will be reported narratively.
3. Fidelity and sustainability: interview qualitative data will be analysed deductively, to ascertain whether program components were delivered as planned. Further, information on organisational support systems and process will be reviewed by the research team to consider the sustainability of the program. This information will be reported narratively.
Expansion method, using simultaneous design where the core component is quantitative and the supplemental component is qualitative (79).
The Connect Local early intervention model is designed with end users to positively impact the wellbeing and quality of life for an older population at risk or experiencing loneliness, social isolation and/or depressive symptoms, by utilising a social prescribing approach. Our intervention evaluation will determine impacts on community members involved in the program, as well as volunteers and service providers involved, over 12-months. The SROI evaluation will highlight social, economic and health outcomes for the beneficiaries, the healthcare system and wider society. The implementation evaluation will observe and gather information on the implementation of the program to support future implementation of similar programs. Collectively this mixed method evaluation of effectiveness, cost-effectiveness and implementation will add to the evidence base, providing much needed long-term data in a large sample group (30, 31).
The number of people aged 65 years and older is expected to rise (81), and therefore the number of people with chronic health conditions is also expected to rise. The consequences will increase pressure on the health system, with public expenditure on health and social care likely to struggle to meet demands. Therefore, to ensure people with health and social care needs can continue to access appropriate and timely care, we need to address any issues early, before they escalate, and support people to stay well. The World Health Organization is focusing on promoting health and wellbeing (82) including promoting social connection, where human beings adopt a collaborative and equitable approach in their relationships with fellow human beings, building bridges between medicine, public health and social sciences, where programs are codesigned with those who will benefit (82). Social prescribing involves the delivery of more holistic, person -centred care, aiming to empower individuals to take care of their own health and well-being and ultimately reduce stress on health systems. This work will contribute to building the evidence-base through implementation and evaluation of Connect Local, an approach using social prescribing.
We anticipate that our Connect Local early intervention program will lead to sustainable and life-changing improvements among the participants, particularly on reducing loneliness. By preventing escalation to more significant health issues and using a preventative approach, the model may also reduce the development of associated downstream societal and economic costs. The SROI evaluation and consolidation of our Connect Local model will enable decision makers to allocate resources and replicate such evidence-based programs.
We aim to disseminate these findings through multiple avenues including reports to funders, peer reviewed articles and presentations of research findings, and broader dissemination to stakeholders including local older community members, as well as volunteers, service providers and decision makers. We aim to provide robust information to enable decision makers to select and implement this approach more broadly.
Social prescribing programs have shown promise in potentially combatting a number of health conditions and reducing loneliness (23), while leveraging off, and developing networks between existing services to develop more connected, supportive communities. We anticipate that this multi-pronged evaluation of Connect Local program will not only determine the effects on all program stakeholders, but also provide robust evidence to policy makers about the potential health and economic impact to enable optimisation of our health and social care systems. Further, this research will contribute to the development of a conceptual model to improve understanding of how program promoting social connection for older people can lead to improved health outcomes, wellbeing and reduced health service use.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
RO: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing, Funding acquisition. ER: Methodology, Writing – original draft, Writing – review & editing. KR: Writing – review & editing, Methodology. SA: Methodology, Writing – review & editing, Writing – original draft. DF: Writing – review & editing, Funding acquisition, Methodology. KF: Writing – review & editing, Funding acquisition, Methodology. AY: Writing – review & editing, Methodology. ML: Writing – review & editing, Methodology. LE: Methodology, Writing – review & editing, Writing – original draft. JL: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Funding acquisition.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The project was funded by The Ian Potter Foundation, and Perpetual’s Impact Philanthropy Grant program on behalf of the Ian Rollo Currie Estate Foundation, Felton Bequest, managed by Equity Trustees and Perpetual Trustees. The funders did not contribute to or influence the design of the study or writing of the protocol.
David Menzies – for contribution to development of the initial funding proposal.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer AJ declared a shared affiliation with the author(s) ML to the handling editor at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Australian Institute of Health and Welfare. Chronic conditions and multimorbidity. Canberra: AIHW (2020).
2. Djukic, M, Jun, J, and Fletcher, J. An examination of the factors associated with implementation of evidence-based management practices for improving nurse work environments. Worldviews Evid-Based Nurs. (2021) 18:129–37. doi: 10.1111/wvn.12497
3. Marengoni, A, Angleman, S, Melis, R, Mangialasche, F, Karp, A, Garmen, A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. (2011) 10:430–9. doi: 10.1016/j.arr.2011.03.003
4. Teo, RH, Cheng, WH, Cheng, LJ, Lau, Y, and Lau, ST. Global prevalence of social isolation among community-dwelling older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. (2023) 107:104904. doi: 10.1016/j.archger.2022.104904
5. Badcock, JC, Holt-Lunstad, J, Garcia, E, Bombaci, P, and Lim, MH. Position statement: Addressing social isolation and loneliness and the power of human connection. Global Initiative on Loneliness and Connection (GILC) (2022). Available at: https://www.gilc.global/general-6
6. Holt-Lunstad, J. Loneliness and social isolation as risk factors: the power of social connection in prevention. Am J Lifestyle Med. (2021) 15:567–73. doi: 10.1177/15598276211009454
7. Wang, S, Molassiotis, A, Guo, C, Leung, ISH, and Leung, AYM. Association between social integration and risk of dementia: a systematic review and meta-analysis of longitudinal studies. J Am Geriatr Soc. (2023) 71:632–45. doi: 10.1111/jgs.18094
8. Lazzari, C, and Rabottini, M. COVID-19, loneliness, social isolation and risk of dementia in older people: a systematic review and meta-analysis of the relevant literature. Int J Psychiatry Clin Pract. (2022) 26:196–207. doi: 10.1080/13651501.2021.1959616
9. Hakulinen, C, Pulkki-Råback, L, Virtanen, M, Jokela, M, Kivimäki, M, and Elovainio, M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK biobank cohort study of 479 054 men and women. Heart. (2018) 104:1536–42. doi: 10.1136/heartjnl-2017-312663
10. Long, RM, Terracciano, A, Sutin, AR, Creaven, AM, Gerstorf, D, D'Arcy-Bewick, S, et al. Loneliness, social isolation, and living alone associations with mortality risk in individuals living with cardiovascular disease: a systematic review, Meta-analysis, and Meta-regression. Psychosom Med. (2023) 85:8–17. doi: 10.1097/PSY.0000000000001151
11. Lim, M, Lambert, G, Thurston, L, Argent, T, Eres, R, Qualter, P, et al. Survey of health and wellbeing – Monitoring the impact of COVID-19. Melbourne: Swinburne University (2020) 28th March 2023.
12. Lim, MH, Rodebaugh, TL, Zyphur, MJ, and Gleeson, JF. Loneliness over time: the crucial role of social anxiety. J Abnorm Psychol. (2016) 125:620–30. doi: 10.1037/abn0000162
13. Hämmig, O. Health risks associated with social isolation in general and in young, middle and old age. PLoS One. (2019) 14:e0219663. doi: 10.1371/journal.pone.0219663
14. Department of Health. National Preventive Health Strategy 2021–2030. Canberra, Australia: Commonwealth of Australia (2021).
15. Holt-Lunstad, J, Robles, TF, and Sbarra, DA. Advancing social connection as a public health priority in the United States. Am Psychol. (2017) 72:517–30. doi: 10.1037/amp0000103
16. World Health Organization. Integrated care for older people (ICOPE) implementation framework: Guidance for systems and services. Geneva: World Health Organisation (2019) Report No.: Licence: CC BY-NC-SA 3.0 IGO.
17. Kung, CSJ, Kunz, JS, and Shields, MA. Economic aspects of loneliness in Australia. Aust Econ Rev. (2021) 54:147–63. doi: 10.1111/1467-8462.12414
18. Gerst-Emerson, K, and Jayawardhana, J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. (2015) 105:1013–9. doi: 10.2105/AJPH.2014.302427
19. Engel, GL. The need for a new medical model: a challenge for biomedicine. Science (New York, NY). (1977) 196:129–36. doi: 10.1126/science.847460
20. Mann, J, Quigley, R, Harvey, D, Tait, M, Williams, G, and Strivens, E. OPEN ARCH: integrated care at the primary–secondary interface for the community-dwelling older person with complex needs. Aust J Prim Health. (2020) 26:104–8. doi: 10.1071/PY19184
21. Beller, J, and Wagner, A. Disentangling loneliness: differential effects of subjective loneliness, network quality, network size, and living alone on physical, mental, and cognitive health. J Aging Health. (2018) 30:521–39. doi: 10.1177/0898264316685843
22. Beller, J, and Wagner, A. Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychol. (2018) 37:808–13. doi: 10.1037/hea0000605
23. Polley, M, Chatterjee, H, Asthana, S, Cartwright, L, Husk, K, Burns, L, et al. Measuring outcomes for individuals receiving support through social prescribing. London: National Academy for Social Prescribing (2022).
24. Muhl, C, Mulligan, K, Bayoumi, I, Ashcroft, R, and Godfrey, C. Establishing internationally accepted conceptual and operational definitions of social prescribing through expert consensus: a Delphi study. BMJ Open. (2023) 13:e070184. doi: 10.1136/bmjopen-2022-070184
25. Zurynski, Y, and Vedovi, A. Smith K-l. social prescribing: A rapid literature review to inform primary care policy in Australia. Sydney: NHMRC Parternship Centre for Health System Sustainability, Australian Institute of Health Innovation, Macquarie University (2020).
26. Chatterjee, HJ, Camic, PM, Lockyer, B, and Thomson, LJM. Non-clinical community interventions: a systematised review of social prescribing schemes. Arts Health. (2018) 10:97–123. doi: 10.1080/17533015.2017.1334002
27. Liebmann, M, Pitman, A, Hsueh, YC, Bertotti, M, and Pearce, E. Do people perceive benefits in the use of social prescribing to address loneliness and/or social isolation? A qualitative meta-synthesis of the literature. BMC Health Serv Res. (2022) 22:1264. doi: 10.1186/s12913-022-08656-1
28. Reinhardt, GY, Vidovic, D, and Hammerton, C. Understanding loneliness: a systematic review of the impact of social prescribing initiatives on loneliness. Perspect Public Health. (2021) 141:204–13. doi: 10.1177/1757913920967040
29. Kimberlee, R, Bertotti, M, Dayson, C, Asthana, S, Polley, M, Burns, L, et al. The economic impact of social prescribing. London: National Academy for Social Prescribing (2022).
30. Percival, A, Newton, C, Mulligan, K, Petrella, RJ, and Ashe, MC. Systematic review of social prescribing and older adults: where to from here? Family Med Commun Health. (2022) 10:e001829. doi: 10.1136/fmch-2022-001829
31. Calderón-Larrañaga, S, Greenhalgh, T, Finer, S, and Clinch, M. What does the literature mean by social prescribing? A critical review using discourse analysis. Sociol Health Illn. (2022) 44:848–68. doi: 10.1111/1467-9566.13468
32. Duncan, A, Kiely, D, Mavisakalyan, A, et al. Stronger together: Loneliness and social connectedness in. Australia: Bankwest Curtin Economics Centre (2021).
33. Mihalopoulos, C, Le, LK-D, Chatterton, ML, Bucholc, J, Holt-Lunstad, J, Lim, MH, et al. The economic costs of loneliness: a review of cost-of-illness and economic evaluation studies. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:823–36. doi: 10.1007/s00127-019-01733-7
34. Engel, L, Lee, YY, Le, LK-D, Lal, A, and Mihalopoulos, C. Reducing loneliness to prevent depression in older adults in Australia: a modelled cost-effectiveness analysis. Mental Health Prev. (2021) 24:200212. doi: 10.1016/j.mhp.2021.200212
35. Greenhalgh, T, Jackson, C, Shaw, S, and Janamian, T. Achieving research impact through co-creation in community-based health services: literature review and case study. Milbank Q. (2016) 94:392–429. doi: 10.1111/1468-0009.12197
36. Nahapiet, J, and Ghoshal, S. Social capital, intellectual capital, and the organizational advantage. Acad Manag Rev. (1998) 23:242–66. doi: 10.2307/259373
37. Bourdieu, P. The forms of capital In: J Richardson, editor. Handbook of theory and research for the sociology of education. Westport, Conneticut: Greenwood Press (1986). 241–58.
38. Putnam, R, Leonardi, R, and Nanetti, R. Making democracy work: Civic traditions in modern Italy. Princeton: Princeton University Press (1993).
39. Lin, N. Building a network theory of social capital In: N Nin, K Cook, and R Burt, editors. Social capital: Theory and research. New York: Aldine de Gruyter (2001). 3–30.
40. Uphoff, N. Understanding social capital: learning from the analysis and experience of participation In: P Dasgupta and I Serageldin, editors. Social capital: A multifaceted perspective. Washington DC: World Bank (1999). 215–53.
41. Shin, B. Exploring network measures of social capital: toward more relational measurement. J Plan Lit. (2021) 36:328–44. doi: 10.1177/0885412221999415
42. Lin, N, Ensel, WM, and Vaughn, JC. Social resources and strength of ties: structural factors in occupational status attainment. Am Sociol Rev. (1981) 46:393–405. doi: 10.2307/2095260
43. Claridge, T. Guide to Social Capital: The Concept, Theory, and its Research New Zealand2021. Available at: https://www.socialcapitalresearch.com/guide-to-social-capital-the-concept-theory-and-its-research/
44. Lim, MH, Eres, R, and Vasan, S. Understanding loneliness in the twenty-first century: an update on correlates, risk factors, and potential solutions. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:793–810. doi: 10.1007/s00127-020-01889-7
45. Ogrin, R, Dickins, M, Johnstone, G, Mortimer, D, Iezzi, A, and Lowthian, J. Co-creation of services to maintain independence and optimise well-being: learnings from Australia’s older women living alone (OWLA) project. Health Soc Care Community. (2020) 28:494–504. doi: 10.1111/hsc.12882
46. Green, MM, Lowthian, JA, Allgood, H, and Ogrin, R. Volunteer peer support frameworks supporting older women living alone. Health Soc Care Community. (2022) 30:e4252–63. doi: 10.1111/hsc.13818
47. Nicholls, J, Lawlor, E, Neitzert, E, and Goodspeed, T. A guide to social return on investment. London, UK: The office of the third sector (OTS), Cabinet Office (2012).
48. Brown, MEL, and Dueñas, AN. A medical science Educator's guide to selecting a research paradigm: building a basis for better research. Med Sci Educ. (2020) 30:545–53. doi: 10.1007/s40670-019-00898-9
49. Nyein, KP, Caylor, JR, Duong, NS, Fry, TN, and Wildman, JL. Beyond positivism: toward a pluralistic approach to studying “real” teams. Organ Psychol Rev. (2020) 10:87–112. doi: 10.1177/2041386620915593
50. Chan, A-W, Tetzlaff, JM, Gøtzsche, PC, Altman, DG, Mann, H, Berlin, JA, et al. Explanation and elaboration: guidance for protocols of clinical trials. BMJ. (2013) 346:346. doi: 10.1136/bmj.e7586
51. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
52. Pinnock, H, Barwick, M, Carpenter, CR, Eldridge, S, Grandes, G, Griffiths, CJ, et al. Standards for reporting implementation studies (StaRI): explanation and elaboration document. BMJ Open. (2017) 7:e013318. doi: 10.1136/bmjopen-2016-013318
53. Curran, GM, Bauer, M, Mittman, B, Pyne, JM, and Stetler, C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. (2012) 50:217–26. doi: 10.1097/MLR.0b013e3182408812
54. Cooke, A, Smith, D, and Booth, A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. (2012) 22:1435–43. doi: 10.1177/1049732312452938
55. World Health Organization. A toolkit on how to implement social prescribing. Manila: World Health Organization Western Pacific (2022).
56. NHS. Social prescribing and community-based support. London, UK: National Health Service (2019).
57. Russell, D, Peplau, LA, and Cutrona, CE. The revised UCLA loneliness scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. (1980) 39:472–80. doi: 10.1037/0022-3514.39.3.472
58. Hughes, ME, Waite, LJ, Hawkley, LC, and Cacioppo, JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
59. Lubben, J, Blozik, E, Gillmann, G, Iliffe, S, von Renteln, KW, Beck, JC, et al. Performance of an abbreviated version of the Lubben social network scale among three European community-dwelling older adult populations. Gerontologist. (2006) 46:503–13. doi: 10.1093/geront/46.4.503
60. Connor, KM, Kobak, KA, Churchill, LE, Katzelnick, D, and Davidson, JRT. Mini-SPIN: a brief screening assessment for generalized social anxiety disorder. Depress Anxiety. (2001) 14:137–40. doi: 10.1002/da.1055
61. Rinaldi, P, Mecocci, P, Benedetti, C, Ercolani, S, Bregnocchi, M, Menculini, G, et al. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. J Am Geriatr Soc. (2003) 51:694–8. doi: 10.1034/j.1600-0579.2003.00216.x
62. Devlin, N, and Brooks, R. EQ-5D and the EuroQol group: past, present and future. Appl Health Econ Health Policy. (2017) 15:127–37. doi: 10.1007/s40258-017-0310-5
63. Tennant, R, Hiller, L, Fishwick, R, Platt, P, Joseph, S, Weich, S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcome. (2007) 5:63. doi: 10.1186/1477-7525-5-63
64. Hurn, J, Kneebone, I, and Cropley, M. Goal setting as an outcome measure: a systematic review. Clin Rehabil. (2006) 20:756–72. doi: 10.1177/0269215506070793
65. Fletcher, K, Foley, F, Thomas, N, Michalak, E, Berk, L, Berk, M, et al. Web-based intervention to improve quality of life in late stage bipolar disorder (ORBIT): randomised controlled trial protocol. BMC psychiatry. (2018) 2018/07/; 18(1):[221 p.]. Available at: http://europepmc.org/abstract/MED/30001704
66. Benson, T, Sladen, J, Liles, A, and Potts, HWW. Personal wellbeing score (PWS)—a short version of ONS4: development and validation in social prescribing. BMJ Open Qual. (2019) 8:e000394. doi: 10.1136/bmjoq-2018-000394
67. Resnick, B, Gruber-Baldini, AL, Pretzer-Aboff, I, Galik, E, Buie, VC, Russ, K, et al. Reliability and validity of the evaluation to sign consent measure. Gerontologist. (2007) 47:69–77. doi: 10.1093/geront/47.1.69
68. Harris, PA, Taylor, R, Thielke, R, Payne, J, Gonzalez, N, and Conde, JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
69. Snape, D, and Martin, G. Measuring loneliness: Guidance for use of the national indicator on Surveys. United Kingdom: Office for National Statistics (2018).
70. Lubben, JE. Assessing social networks among elderly populations. Fam Commun Health. (1988) 11:42–52. doi: 10.1097/00003727-198811000-00008
71. Badcock, J, and Lim, M. A Guide to Evaluating Loneliness for Community Organisations. Ending Loneliness Together. (2021). Available at: https://api.research-repository.uwa.edu.au/ws/portalfiles/portal/164617872/ELT_2_Guide_to_Evaluating_Loneliness_for_Community_Organisations_Dec_2021.pdf
72. NHS. Personalised care: welcome! An induction guide for social prescribing link Workers in Primary Care Networks. London, UK: Service NH (2021).
73. Brown, C, and Hammond, J., Jones, M., Kimberlee, R, BAB community researchers. Community webs final evaluation report; (2018)
74. NSW Department of Communities and Justice. Social return on investment (SROI) approach by NSW Department of Communities and Justice. Sydney: NSW Department of Communities and Justice (2020).
75. Breslow, NE, and Clayton, DG. Approximate inference in generalized linear mixed models. J Am Stat Assoc. (1993) 88:9–25. doi: 10.1080/01621459.1993.10594284
76. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
77. Lumivero. NVivo (Version 11). (2016). Available at: www.lumivero.com
78. Clarke, AE. Situational analyses: grounded theory mapping after the postmodern turn. Symb Interact. (2003) 26:553–76. doi: 10.1525/si.2003.26.4.553
79. Schoonenboom, J, and Johnson, RB. How to construct a mixed methods research design. Kolner Z Soz Sozpsychol. (2017) 69:107–31. doi: 10.1007/s11577-017-0454-1
80. Hutchinson, CL, Berndt, A, Forsythe, D, Gilbert-Hunt, S, George, S, and Ratcliffe, J. Valuing the impact of health and social care programs using social return on investment analysis: how have academics advanced the methodology? A systematic review. BMJ Open. (2019) 9:e029789. doi: 10.1136/bmjopen-2019-029789
81. Wilson, T, and Temple, J. New population projections for Australia and the states and territories, with a particular focus on population ageing: ARC Centre of Excellence in Population Ageing Research ; (2022).
Keywords: loneliness, social isolation, community, prevention, early intervention, evaluation, older adults, protocol
Citation: Ogrin R, Robinson E, Rendell K, Alrababah S, Fineberg D, Fiddes K, Yerolemou A, Lim MH, Engel L and Lowthian JA (2024) “Connect Local”: protocol for the evaluation of a codesigned whole of community approach to promote social connection in older adults. Front. Public Health. 12:1342562. doi: 10.3389/fpubh.2024.1342562
Received: 22 November 2023; Accepted: 03 May 2024;
Published: 23 May 2024.
Edited by:
Matthew Lee Smith, Texas A and M University, United StatesReviewed by:
Suraj Samtani, University of New South Wales, AustraliaCopyright © 2024 Ogrin, Robinson, Rendell, Alrababah, Fineberg, Fiddes, Yerolemou, Lim, Engel and Lowthian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: R. Ogrin, cm9ncmluQGJvbHRvbmNsYXJrZS5jb20uYXU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.