
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 23 February 2024
Sec. Occupational Health and Safety
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1340920
 Danielle Wing Lam Ng1,2
Danielle Wing Lam Ng1,2 Serana Chun Yee So1,2
Serana Chun Yee So1,2 Richard Fielding1,2
Richard Fielding1,2 Anja Mehnert-Theuerkauf3
Anja Mehnert-Theuerkauf3 Ava Kwong4
Ava Kwong4 Dacita Suen4
Dacita Suen4 Ling Wong5
Ling Wong5 Sara Wai Wun Fung6
Sara Wai Wun Fung6 Oi Kwan Chun6
Oi Kwan Chun6 Daniel Y. T. Fong7
Daniel Y. T. Fong7 Sharon Chan8
Sharon Chan8 Alex Molasiotis9,10
Alex Molasiotis9,10 Winnie K. W. So11
Winnie K. W. So11 Wendy Wing Tak Lam1,2*
Wendy Wing Tak Lam1,2*Introduction: Existing evidence of returning-to-work (RTW) after cancer comes predominately from Western settings, with none prospectively examined since the initial diagnostic phase. This study prospectively documents RTW-rate, time-to-RTW, work productivity loss, and activity impairment, within the first-year post-surgery among Chinese women with breast cancer (BCW) and identify potential causal co-variants.
Methods: This observational longitudinal study followed 371 Chinese BCW who were employed/self-employed at the time of diagnosis at 4-week post-surgery (baseline). RTW-status and time-to-RTW were assessed at baseline (T1), 4-month (T2), 6-month (T3), and 12-month (T4) post-baseline. WPAI work productivity loss and activity impairment were assessed at T4. Baseline covariates included demographics, medical-related factors, work satisfaction, perceived work demand, work condition, RTW self-efficacy, B-IPQ illness perception, COST financial well-being, EORTC QLQ-C30 and QLQ-BR23 physical and psychosocial functioning, and HADS psychological distress.
Results: A 68.2% RTW-rate (at 12-month post-surgery), prolonged delay in RTW (median = 183 days), and significant proportions of T4 work productivity loss (20%), and activity impairment (26%), were seen. BCW who were blue-collar workers with lower household income, poorer financial well-being, lower RTW self-efficacy, poorer job satisfaction, poorer illness perception, greater physical symptom distress, impaired physical functioning, and unfavorable work conditions were more likely to experience undesired work-related outcomes.
Discussion: Using a multifactorial approach, effective RTW interventions should focus on not only symptom management, but also to address psychosocial and work-environmental concerns. An organizational or policy level intervention involving a multidisciplinary team comprising nurses, psychologists, occupational health professionals, and relevant stakeholders in the workplace might be helpful in developing a tailored organizational policy promoting work-related outcomes in BCW.
Breast cancer affects women worldwide, with a 2020 incidence of 2.26 million cases (1–3). Of these women ~67% were aged <65, with 56% being between 40 and 64 years old, considered the prime working years (4, 5). Increased incidence, improving 5-year survival (~80% in developed countries) (1) and extending retirement ages (6), mean growing numbers of working-age women are diagnosed with breast cancer (BCW) (5, 7). However, cancer patients have 1.6x and 1.3x higher risks for early retirement (8) and unemployment (9), respectively, and a lower incidence of reemployment than do healthy controls (10–12). Consequently, returning to work (RTW) and job retention are crucial unmet needs of this population, and of major concern in the field of cancer survivorship (5). For many, RTW after a cancer diagnosis and treatment is needed for financial stability and regaining normalcy, contributing to patients' wider recovery and quality of life (5, 11, 13–15). Societally, RTW for BCW has extrinsic economic value in terms of reduced direct and indirect medical and welfare costs, and from less disease-related productivity loss, especially in light of increasing female labor force participation (5, 11, 16, 17).
Data reporting global mean RTW rates for cancer patients (63.5%) ranges from 24 to 94%, depending on time since diagnosis (12). In Hong Kong, 6-month and 12-month post-cancer treatment RTW rates were 39 and 63%, respectively (17). A recent systematic review reported RTW rate among BCW within 12 months of diagnosis of between 43–93% (18), with a steadily rising trend observed over the survivorship trajectory (19), suggesting a majority eventually reentered the workforce. Yet, BCW may experience a prolonged delay in RTW compared to individuals with other forms of cancer (20). The average duration of work absence due to BC ranged from 86 to 349 days, with a median of 210 days (e.g. compared to 125 days for gynecological cancer patients) (18, 20). BCW's RTW is associated with work environment, physical and psychosocial functioning, educational level, personal finances, and illness perception, medical/treatment-related factors and social support (7, 11, 12, 15, 18–22). However, evidence is mixed regarding whether these determinants either facilitate or hinder RTW (15). Different regional contexts between studies may account for the reported conflicting evidence and varied RTW rates, reflecting differences in healthcare provision, employment policies, social security, and cultural perspectives on gender across regions (7, 17, 19, 21, 23). For example, in Hong Kong up to 120 paid sick leave days can be accumulated when supported by a valid medical certificate whereas in the United States no federal law guarantees the right to paid sick leave (17). Most existing RTW studies on BCW have studied Caucasian populations in western cultural settings post-treatment or during survivorship (21). Even among the scant evidence on East Asian populations (22, 24, 25), the RTW rates varied across countries; 37%-59% in Korea (22, 26), 41% in Malaysia (25), and 21–33% in China (27, 28). More importantly, there are no prospective studies following BCW from the initial diagnostic stage of the cancer journey to RTW and, thereafter, productivity in work, indicating an important gap in the RTW literature. Understanding BCW's employment experiences in different setting and tracking their RTW status longitudinally from the immediate aftermath of primary surgery more comprehensively illuminates the entire decision-making processes in RTW, clarifying associated long-term facilitators and barriers, enabling efficacious tailored interventions or supportive resources to be developed, and refining relevant laws and regulations to meet specific needs and promote early RTW, ultimately improving rehabilitation outcomes for this population (15, 17, 22). In this regard this study significantly advances the existing literature.
Following successful work resumption, BCW face employment-related challenges, including activity impairment and work productivity loss (absenteeism: time lost from work, and presenteeism: reduced work performance) (12), potentially preceding work cessation (17, 22). Greater activity impairment and work limitation, and poorer work performance, is reported by BCW than by healthy controls (12, 19, 29). However, we lack empirical evidence that disentangles whether BC and its treatments affect activity impairment and longer-term work productivity loss, and predictors thereof.
RTW after cancer is a complex process requiring the consideration of multiple factors (5). Mehnert (12) identified six influences on work-related outcomes: (i) demographic factors; (ii) impairments to health status such as physical symptoms; (iii) psychosocial factors like psychological well-being and social support; (iv) motivational factors like work satisfaction; (v) work-related factors like job type, work environment, employer accommodation, and relationship with co-workers; and (vi) work-related interventions like counseling and vocational training services. Given the varying regional contexts that may shape these influences, the next question is if this European model of BCW survivorship is applicable to Chinese BCW. For example, legal protection, medical costs and employer accommodation of employee needs, and perceptions of sick roles may vary, affecting both RTW delay and productivity.
Here we prospectively examine work-related outcomes (RTW rate, time to RTW, work productivity loss, and activity impairment) among Chinese BCW in the first year following primary surgery and identify factors predicting these outcomes. We hypothesized that certain sociodemographics (older age, lower educational attainment, being married, and higher personal financial toxicity), medical factors (cancer stage and treatment type), impaired physical and psychosocial functioning, lower work satisfaction and RTW self-efficacy, and unfavorable work-related factors (higher work demand and poorer work conditions) would be associated with poorer work-related outcomes. Negative illness perceptions affecting the “sick role” of cancer patients may hinder RTW and also lead to a greater loss of work productivity (17, 19), so illness perception was also assessed.
Following ethical approval (ref: UW 17-527), the recruitment was conducted at three dedicated breast centers in government-funded public hospitals in Hong Kong between December 2018 and August 2021. Cantonese- or Mandarin-speaking Chinese patients who (i) were newly diagnosed with curable BC, (ii) were aged 18 or above, (iii) were in paid- or self-employment at the time of diagnosis, and (iv) had completed surgery as primary treatment within the past 4 weeks were eligible. Patients with metastatic BC and linguistic or intellectual difficulties were excluded.
Potential participants were identified by surgical oncologists and approached by a trained research assistant during their postsurgical follow-up consultation. After obtaining fully informed written consent from patients who agreed to participate in the study, patients completed a standardized face-to-face baseline questionnaire immediately (within 1-month post-surgery, T1) and three follow-up assessments at 4-month (T2), 6-month (T3), and 12-month (T4) post-baseline through phone interviews.
Return to work (RTW), defined as time to RTW after an absence from work due to cancer (i.e., paid and unpaid time off from work) (9, 30), was assessed from 1-month post-surgery onwards (T1-T4). At each assessment, patients were asked to indicate if they had taken time off since the first day of sick leave. Those who reported having RTW were asked to specify the date of RTW. Time to RTW was calculated as the number of days between the first day of sick leave and the first day of RTW, irrespective of any job nature changes (e.g., changed job, reduced working hours) (20, 21). For those not taking time off from work, the time of RTW was set to zero.
Work productivity loss and activity impairment were assessed at 12-month post-surgery (T4) using the Chinese version of the Work Productivity and Activity Impairment (WPAI) questionnaire (31). The 6-item WPAI measures work productivity loss (the extent to which current health condition induced work inability) and activity impairment (the extent to which current health condition affected regular activities other than job-related work). Items assessing work productivity loss are only relevant to those who have returned to work. Both work productivity loss and activity impairment were expressed in percentages, with higher values indicative of greater productivity loss and impaired functioning (31).
Potential covariates include: (i) work satisfaction, assessed using a 12-item work satisfaction scale (32); (ii) perceived job strain/work demand, assessed using a 10-item measures (32); (iii) perceived work condition, assessed in terms of unfavorable work conditions such as physically heavy work, incorrect one-side posture, and excessive demand, using an 8-item measure (32); (iv) RTW self-efficacy, assessed using the 11-item Return-to-Work Self-Efficacy scale (RTW-SE scale) (32); (v) cognitive and emotional representations of illness, assessed using the Chinese version of the Brief Illness Perception Questionnaire (B-IPQ) (33, 34); (vi) cancer-related financial well-being, as assessed by the 11-item Comprehensive Score for Financial Toxicity (COST) (35); (vii) physical and psychosocial functioning, assessed by the standard Chinese version of the European Organization Research Treatment Caner (EORTC) general Quality of Life questionnaire (QLQ-C30) and the breast cancer specific module (QLQ-BR23) (36, 37); (viii) psychological distress, assessed by the 14-item Hospital Anxiety and Depression Scale (HADS) (38); (ix) demographics including age, marital status, education level, occupation, health insurance, and social welfare allowance details, collected through self-report; and (x) medical data including diagnosis, cancer stage, and treatment received, retrieved from hospital medical records after the completion of the study. All of which otherwise were assessed only once at baseline.
Standard descriptive analyses assessed sample characteristics and the RTW rate at each assessment timepoint. Kaplan-Meier survival analysis estimated the mean time to RTW. Cox regression and linear regression analyses were performed to identify potential covariates of the RTW rates, time to RTW, T4 work productivity loss, and T4 activity impairment, respectively (9, 20, 23, 39). Each of the potential covariates was entered into the regression model individually. Significant variables achieving a p-value of <0.05 were subsequently included in a multivariate regression model (20).
Based on our previous pilot study of RTW and work productivity among BCW, we expected 65–70% of BCW to return to work after BC diagnosis. To examine the RTW at 1 year after breast cancer diagnosis, with a 5% error margin and a confidence level of 95%, a sample of 352 patients was needed. To examine the change in work productivity and activity impairment, a standardized effect size of 0.4 was expected (9). With 80% power and a 5% maximum false positive error rate, at least 89 patients were needed after adjusting for multiplicity by Bonferroni correction.
Of eligible patients, 71% (378/532) gave informed consent. Follow-up attrition ranged from 24%-40%. Seven participants died or/and were diagnosed with metastatic disease and excluded from analyses, leaving a final sample size of 371 (Figure 1). Excepting baseline QLQ-C30 nausea and constipation, neither demographic, clinical, nor baseline variables otherwise differentiated these two groups (Supplementary Table S1). The final sample had a mean age of 52.6 years. Most participants were married (60%), were at least secondary-level educated (85%), having a monthly household income <US$3,850 (57%), and undergoing active treatment at baseline (61%) (Table 1).
RTW rates were 23.2% (n = 86/371, 95%CI = 18.9–27.5%) at baseline, 49.6% (n = 141/284, 95%CI = 43.8–55.5%) at 4-month; 54.3% (n = 152/280, 95%CI = 48.4–60.2%) at 6-month, and; 68.2% (n = 165/242, 95%CI = 62.3–74.1%) at 12-month post-baseline.
Univariate analyses identified potential correlates of RTW status (Supplementary Table S2). In the final multivariable Cox regression model (Table 2), status with job title, monthly household income, receipt of post-operative chemotherapy and radiotherapy, RTW self-efficacy, B-IPQ illness perception, and work condition with long hours in sitting position were significant predictors of RTW. White collar (HR = 1.71, 95%CI = 1.19–2.45, p = 0.004) or professionals (HR = 1.62, 95%CI = 1.06–2.46, p = 0.025) vs. blue collar work, a higher monthly household income of >US$3,850 per month (<US$1,280: HR = 0.64, 95%CI = 0.41–0.98, p < 0.001; US$1,280–3,850: HR = 0.53, 95%CI = 0.39–0.73, p < 0.001), greater RTW self-efficacy (HR = 1.41, 95%CI = 1.20–1.87, p < 0.001), and more prolonged sitting at work (HR = 1.38, 95%CI = 1.17–1.62, p < 0.001) facilitated work resumption within 12 months after surgery. Chemotherapy (HR = 0.53, 95%CI = 0.39–0.70, p < 0.001), radiotherapy (HR = 0.45, 95%CI = 0.46–0.90, p = 0.010), and more negative cognitive representations of illness (HR = 0.97, 95%CI = 0.95–0.98, p < 0.001) hindered work resumption.
Using Kaplan-Meier survival analysis, the average time to RTW was 261 days, with a median of 183 days (Supplementary Figure S1).
Among correlates of time to RTW examined in univariate analyses (Supplementary Table S3), only monthly household income, the receipt of post-operative chemotherapy and radiotherapy, RTW self-efficacy, work conditions with long hours in sitting position, and QLQ-30 physical functioning retained significance in the final multiple linear regression model (Table 3). BCW with higher monthly household incomes of >US$3,850/month (<US$1,280: B = 68.82, 95%CI = 9.63–128.01, p = 0.022; US$1,280–3,850: B = 83.67, 95%CI = 38.57–128.77, p < 0.001), greater RTW self-efficacy (B = −53.77, 95%CI = −81.64 to −25.90, p < 0.001), more prolonged sitting at work (B = −47.52, 95%CI = −69.54 to −25.50, p < 0.001), and better physical functioning (B = −1.56, 95%CI = −2.67 to −0.46, p = 0.006) had taken shorter time to RTW. Delayed time to RTW was predicted by receipt of chemotherapy (B = 89.30, 95%CI = 46.30–132.30, p < 0.001) and/or radiotherapy (B = 61.72, 95%CI = 14.01–109.44, p = 0.011).
Patients successfully resuming work by 12 months following surgery (n = 161) reported an average 20.2% loss in work productivity. The final multiple linear regression model, which took into account significant covariates from univariate regression analyses (Supplementary Table S4), demonstrated that lower work satisfaction (B = −13.07, 95%CI = −18.79 to −7.35, p < 0.001), physically demanding work conditions (B = 11.48, 95%CI = 6.18–16.78, p < 0.001), higher QLQ-C30 role functioning (B = 0.52, 95%CI = 0.20–0.83, p = 0.002), and higher levels of pain (B = 0.75, 95%CI 0.43–1.08, p < 0.001) were all associated with greater work productivity loss at 12 months following surgery (Table 4).
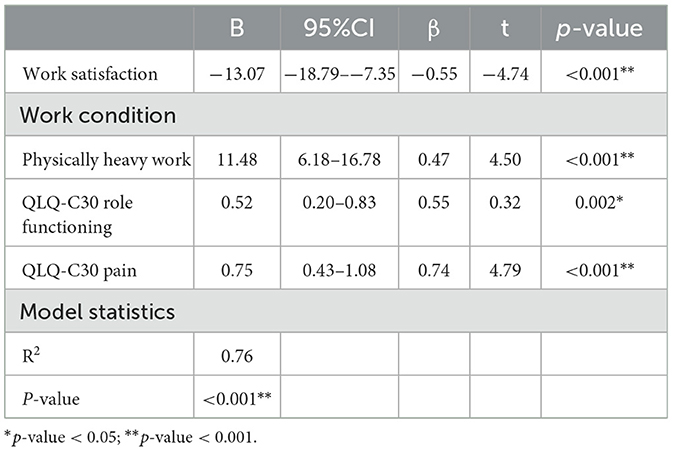
Table 4. Multiple forward linear regression on work productivity loss at 12-month post-surgery (n = 161).
Patients reported an average 26.1% activity limitation at 12-month after surgery. The final multiple linear regression model of activity impairment, adjusted for significant covariates (Supplementary Table S5), showed that the receipt of hormonal therapy (B = 8.33, 95%CI 1.72–14.94, p = 0.014), poorer financial well-being (B = –0.47, 95%CI –0.78– –0.15, p = 0.004), a more B-IPQ negative cognitive representation of illness (B = 0.89, 95%CI = 0.46–1.32, p < 0.001), a higher level of QLQ-C30 insomnia (B = 0.10, 95%CI = 0.001–0.20, p = 0.048), and lower RTW self-efficacy (B = –6.09, 95%CI = –10.13– –2.06, p = 0.003) were all associated with greater activity impairment at 12 months after surgery (Table 5).
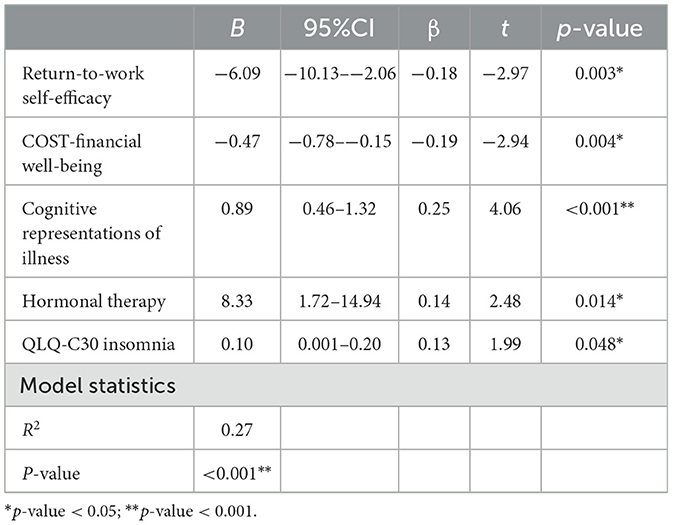
Table 5. Multiple forward linear regression on activity impairment at 12-month post-surgery (n = 227).
In this first longitudinally documented RTW study of Chinese BCW during the initial recovery stage following primary breast surgery, we observed upward trending RTW rates over time (12, 19) from 23.2% at 4-weeks to 68.2% at 12-month post-surgery. Approximately 2-in-3 BCW (68%) successfully RTW at the first year following surgery, comparable with the global mean RTW rates of 63.4% regardless of time since diagnosis from a systematic review of mixed cancer types (12), and within the 43%-93% BCW RTW range reported within 12 months of diagnosis elsewhere (18); both reviews being of predominantly western contexts. The observed RTW rate was relatively higher compared to other studies of Asian populations that reported rates of 21–59% (22, 24, 25). However, direct comparisons are challenging due to ambiguous or different RTW assessment timepoints used across these studies. Median time to RTW after BC in this study was ~183 days, comparable with BCW RTW studies in the early diagnostic and active treatment phases in developed countries such as France (155 days) (40) and the United Kingdom (210 days) (20), where statutory sick pay is available.
Adjuvant radiotherapy and chemotherapy, and physical impairment were associated with poor RTW outcomes, partially consistent with Mehnert's model (12). Radiotherapy can cause arm pain and limit movement. Chemotherapy-induced neuropathy or fatigue may impair to return to work (19, 21, 41). Poorer physical functioning is associated with RTW delay (17). Body image concerns, and societal expectations and stigmas surrounding BC can damage self-esteem and psychological well-being, resulting in the decision not to RTW (11, 18, 33).
In contrast, higher household income, white-collar work, favorable work conditions, and greater RTW self-efficacy promoted RTW outcomes. While higher household income can reflect employment (21, 26), it may also imply higher educational attainment, potentially higher job security, flexibility and less manual work, facilitating earlier resumption (7, 26). Similarly, favorable work conditions such as desk work, are less physically demanding, alleviating physical handicaps from BC treatments, smoothing return into the workforce (18, 21). Enhanced RTW self-efficacy also significantly contributed to early RTW, substantiating reports of lower self-efficacy among those not RTW in previous qualitative studies (27, 42). Poorer RTW self-efficacy reflects both perceived impaired working capability, and worries about potential workplace demands, impeding RTW (43). Job type influenced decisions on RTW but not duration of RTW. White-collar workers were more able to RTW after BC than were blue-collar workers (36). Blue-collar workers may face job loss and/or challenges in finding new employment due to both cancer and treatment impacts restricting more physically-skilled work (44, 45).
Work productivity loss in RTW BCW is common. Our sample reported a 20% reduction of their work productivity at 12-month post-surgery. Pain was weakly associated with work productivity loss, resonating with previous studies that unmanaged physical symptoms distress reduced working hours (46) and hindered work productivity (17, 47–49). Physically demanding work may exacerbate treatment-induced physical symptoms including pain, limiting work performance (12, 47, 50). Concern about physically demanding work causing upper-body lymphedema might further impair BCW productivity (49). Higher role functioning seemingly enhances work productivity loss, contradicting previous reports (51). Better role functioning may lead to taking on more responsibilities, generating more work-related stress and exhaustion (52), adversely affecting work performance (53). In contrast, job satisfaction was the sole protective predictor of work productivity among BCW. A supportive work environment and better interpersonal relationships at work facilitate work commitment and motivation, enhancing productivity (23, 54).
BCW commonly report cancer/treatment impacts on daily physical activities (55), affecting work-related outcomes (56). At 12-month post-surgery, BCW reporting reduced activity functioning had received hormonal therapy, experiencing severe sleep disturbance symptoms, lower RTW self-efficacy, poorer financial well-being, and negative cognitive representation of illness. Lymphedema is a common side effect of hormonal therapy (57) that cause swelling, pain, and limit range of motion in the affected arm or shoulder (58), impairing physical functioning and routine task performance (59). Sleep disturbance was inversely related to daytime alertness and quality of life (60), which might further worsen capacity to perform daily activities especially during daytime (61). Financial constraints restrict utilization of healthcare, social welfare and other resources (62). Post-hoc analysis suggested that patients experiencing greater financial difficulties tended not to have health insurance. Financial stress likely amplifies psychological distress in BCW, compounding cancer's impact on daily activities (62). Furthermore, negative illness perceptions were associated with greater activity impairment, perhaps attributable to lower perceived social support and well-being (63). Negative illness perception might also reflect residual symptoms which compound psychological distress (63), further impairing recovery.
Supporting BCW in RTW and other work-related outcomes (5), particularly during early recovery stage after primary surgery is feasible and necessary. In Hong Kong, as elsewhere, few cancer rehabilitation resources exist or are outside routine clinical practice. A multifactorial RTW intervention would manage physical symptoms and side-effects but also address psychosocial (RTW self-efficacy), and work-environmental (promoting favorable work environments) issues at organizational or even policy levels, particularly for manual labor workers (5). RTW is context-specific, involving workplace policies, insurance protocol, culture, and resource availability—all of which could be regulated by legislation (5, 64). The Disability Discrimination Ordinance in Hong Kong guarantees people with chronic diseases including cancer, equal employment opportunities and reasonable workplace accommodation. However, challenges remain in effectively implementing and enforcing these regulations often due to employer intransigence (5, 64). In-house or external occupational health services, such as educational programs for employers might help. Occupational health professionals should also collaborate closely with occupational stakeholders to tailor organizational policy for creating supportive work environments and preventing work-related problems for BCW after RTW (64).
Study limitations include, first, BCW sampling was from government-funded public hospitals only. Being where most local patients received oncological care, the representativeness of our sample thus remains favorable. Second, an ideal control condition, such as RTW after acute coronary syndrome would clarify if the observed work-related outcomes were cancer-specific (65). Third, the COVID-19 pandemic may have influenced the RTW rate and duration (66). Furthermore, 31% of our sample had unspecified cancer staging (just 2% of participants with known disease stages had non-localized disease), but it is highly probable that almost all had early-stage cancer. Lastly, to minimize recall bias of self-reported RTW dates, averaged time to RTW was used in the analysis.
Early RTW after BC was relatively uncommon, with prolonged RTW delays, significant work productivity loss and activity impairment reported within the first year following surgery, highlighting the need for evidence-based rehabilitation interventions to support RTW and facilitate social reintegration (17). Work-related outcomes after BC evidenced multidimensional relationships with demographics, treatment-induced side effect and physical symptoms, financial well-being, work environment and satisfaction, RTW self-efficacy, and illness perception. These findings suggest that the development of a multifactorial, multidisciplinary RTW intervention might benefit Chinese BCW rehabilitation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by HKU/HA HKW Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
DN: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft. SS: Data curation, Writing – review & editing. RF: Conceptualization, Supervision, Writing – review & editing. AM-T: Conceptualization, Validation, Writing – review & editing. AK: Resources, Writing – review & editing. DS: Resources, Writing – review & editing. LW: Resources, Writing – review & editing. SF: Resources, Writing – review & editing. OC: Resources, Writing – review & editing. DF: Writing – review & editing. SC: Resources, Writing – review & editing. AM: Writing – review & editing. WS: Writing – review & editing. WL: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project was supported by the Health and Medical Research Fund (Project No. 15161641).
Our sincere gratitude to the participants for their time and support, as well as the study sites that coordinated the recruitment of subjects, are appreciated.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1340920/full#supplementary-material
1. Wilkinson L, Gathani T. Understanding breast cancer as a global health concern. Br J Radiol. (2022) 95:20211033. doi: 10.1259/bjr.20211033
2. Arnold M, Morgan E, Rumgay H, Mafra A, Singh D, Laversanne M, et al. Current and future burden of breast cancer: global statistics for 2020 and 2040. Breast. (2022) 66:15–23. doi: 10.1016/j.breast.2022.08.010
3. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
4. Ferlay JEM, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, et al. Global Cancer Observatory: Cancer Today. Lyon: International Agency for Research on Cancer 2020.
5. Butow P, Laidsaar-Powell R, Konings S, Lim CYS, Koczwara B. Return to work after a cancer diagnosis: a meta-review of reviews and a meta-synthesis of recent qualitative studies. J Cancer Survivor. (2020) 14:114–34. doi: 10.1007/s11764-019-00828-z
6. Figueredo JM, García-Ael C, Gragnano A, Topa G. Well-being at work after return to work (RTW): a systematic review. Int J Environ Res Public Health. (2020) 17:7490. doi: 10.3390/ijerph17207490
7. Schmidt ME, Scherer S, Wiskemann J, Steindorf K. Return to work after breast cancer: the role of treatment-related side effects and potential impact on quality of life. Eur J Cancer Care. (2019) 28:e13051. doi: 10.1111/ecc.13051
8. Carlsen K, Oksbjerg Dalton S, Frederiksen K, Diderichsen F, Johansen C. Cancer and the risk for taking early retirement pension: a Danish cohort study. Scand J Public Health. (2008) 36:117–25. doi: 10.1177/1403494807085192
9. De Boer A, Verbeek J, Spelten ER, Uitterhoeve ALJ, Ansink AC, De Reijke TM, et al. Work ability and return-to-work in cancer patients. Br J Cancer. (2008) 98:1342–7. doi: 10.1038/sj.bjc.6604302
10. Tamminga SJ, De Boer A, Verbeek J, Frings-Dresen MHW. Return-to-work interventions integrated into cancer care: a systematic review. Occup Environ Med. (2010) 67:639–48. doi: 10.1136/oem.2009.050070
11. Tan FSI, Shorey S. Experiences of women with breast cancer while working or returning to work: a qualitative systematic review and meta-synthesis. Supportive Care Cancer. (2022) 30:2971–82. doi: 10.1007/s00520-021-06615-w
12. Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. (2011) 77:109–30. doi: 10.1016/j.critrevonc.2010.01.004
13. Stergiou-Kita M, Grigorovich A, Tseung V, Milosevic E, Hebert D, Phan S, et al. Qualitative meta-synthesis of survivors' work experiences and the development of strategies to facilitate return to work. J Cancer Survivor. (2014) 8:657–70. doi: 10.1007/s11764-014-0377-z
14. Wells M, Williams B, Firnigl D, Lang H, Coyle J, Kroll T, et al. Supporting ‘work-related goals' rather than ‘return to work'after cancer? A systematic review and meta-synthesis of 25 qualitative studies. Psycho Oncol. (2013) 22:1208–19. doi: 10.1002/pon.3148
15. Forbes D, Lisy K, Wood C, White V, Evans S, Afshar N, et al. Factors beyond diagnosis and treatment that are associated with return to work in Australian cancer survivors—a systematic review. Asia Pac J Clin Oncol. (2023). doi: 10.1111/ajco.13973
16. Thandrayen J, Joshy G, Stubbs J, Bailey L, Butow P, Koczwara B, et al. Workforce participation in relation to cancer diagnosis, type and stage: Australian population-based study of 163,556 middle-aged people. J Cancer Surviv. (2021) 2021:1–13. doi: 10.1007/s11764-021-01041-7
17. So SCY, Ng DWL, Liao Q, Fielding R, Soong I, Chan KKL, et al. Return to work and work productivity during the first year after cancer treatment. Front Psychol. (2022) 13:866346. doi: 10.3389/fpsyg.2022.866346
18. Cocchiara RA, Sciarra I, D'Egidio V, Sestili C, Mancino M, Backhaus I, et al. Returning to work after breast cancer: a systematic review of reviews. Work. (2018) 61:463–76. doi: 10.3233/WOR-182810
19. Sun Y, Shigaki CL, Armer JM. Return to work among breast cancer survivors: a literature review. Supp Care Cancer. (2017) 25:709–18. doi: 10.1007/s00520-016-3446-1
20. Cooper AF, Hankins M, Rixon L, Eaton E, Grunfeld EA. Distinct work-related, clinical and psychological factors predict return to work following treatment in four different cancer types. Psycho-Oncology. (2013) 22:659–67. doi: 10.1002/pon.3049
21. Islam T, Dahlui M, Majid HA, Nahar AM, Mohd Taib NA, Su TT. Factors associated with return to work of breast cancer survivors: a systematic review. BMC Public Health. (2014) 14:1–13. doi: 10.1186/1471-2458-14-S3-S8
22. Lee MK, Kang HS, Lee KS, Lee ES. Three-year prospective cohort study of factors associated with return to work after breast cancer diagnosis. J Occup Rehabil. (2017) 27:547–58. doi: 10.1007/s10926-016-9685-7
23. Mehnert A, de Boer A, Feuerstein M. Employment challenges for cancer survivors. Cancer. (2013) 119:2151–9. doi: 10.1002/cncr.28067
24. Yang ZY, Chen WL, Wu WT, Lai CH, Ho CL, Wang CC. Return to work and mortality in breast cancer survivors: a 11-year longitudinal study. Int J Environ Res Public Health. (2022) 19:14418. doi: 10.3390/ijerph192114418
25. Su TT, Azzani M, Tan FL, Loh SY. Breast cancer survivors: return to work and wage loss in selected hospitals in Malaysia. Support Care Cancer. (2018) 26:1617–24. doi: 10.1007/s00520-017-3987-y
26. Ahn E, Cho J, Shin DW, Park BW, Ahn SH, Noh D-Y, et al. Impact of breast cancer diagnosis and treatment on work-related life and factors affecting them. Breast Cancer Res Treat. (2009) 116:609–16. doi: 10.1007/s10549-008-0209-9
27. Hou W, Li Q, Liu X, Zeng Y, Cheng ASK. Exploring the employment readiness and return to work status of breast cancer patients and related factors. Int J Nurs Sci. (2021) 8:426–31. doi: 10.1016/j.ijnss.2021.09.001
28. Li M, Gao J, Li M, Wang L. The assessment of returning to work following treatment and the associated personal, disease, and treatment factors among breast cancer survivors in central China. Supportive Care Cancer. (2021) 29:7627–36. doi: 10.1007/s00520-021-06354-y
29. Liu S, Wang F, Yang Q, Wang Q, Feng D, Chen Y, et al. Work productivity loss in breast cancer survivors and its effects on quality of life. Work. (2021) 70:199–207. doi: 10.3233/WOR-213565
30. Mehnert A, Koch U. Predictors of employment among cancer survivors after medical rehabilitation-a prospective study. Scand J Work Environ Health. (2013) 39:76–87. doi: 10.5271/sjweh.3291
31. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. (1993) 4:353–65. doi: 10.2165/00019053-199304050-00006
32. Lagerveld SE, Blonk RWB, Brenninkmeijer V, Schaufeli WB. Return to work among employees with mental health problems: development and validation of a self-efficacy questionnaire. Work Stress. (2010) 24:359–75. doi: 10.1080/02678373.2010.532644
33. Zhang N, Fielding R, Soong I, Chan KKK, Tsang J, Lee V, et al. Illness perceptions among cancer survivors. Support Care Cancer. (2016) 24:1295–304. doi: 10.1007/s00520-015-2914-3
34. Zhang N, Fielding R, Soong I, Chan KKK, Lee C, Ng A, et al. Psychometric assessment of the Chinese version of the brief illness perception questionnaire in breast cancer survivors. PLoS ONE. (2017) 12:e0174093. doi: 10.1371/journal.pone.0174093
35. De Souza JA, Yap BJ, Wroblewski K, Blinder V, Araújo FS, Hlubocky FJ, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer. (2017) 123:476–84. doi: 10.1002/cncr.30369
36. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. JNCI J Nat Cancer Instit. (1993) 85:365–76. doi: 10.1093/jnci/85.5.365
37. Sprangers MA, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol. (1996) 14:2756–68. doi: 10.1200/JCO.1996.14.10.2756
38. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
39. Endo M, Haruyama Y, Takahashi M, Nishiura C, Kojimahara N, Yamaguchi N. Returning to work after sick leave due to cancer: a 365-day cohort study of Japanese cancer survivors. J Cancer Survivor. (2016) 10:320–9. doi: 10.1007/s11764-015-0478-3
40. Arfi A, Baffert S, Soilly AL, Huchon C, Reyal F, Asselain B, et al. Determinants of return at work of breast cancer patients: results from the OPTISOINS01 French prospective study. BMJ Open. (2018) 8:e020276. doi: 10.1136/bmjopen-2017-020276
41. Johnsson A, Fornander T, Rutqvist L-E, Olsson M. Work status and life changes in the first year after breast cancer diagnosis. Work. (2011) 38:337–46. doi: 10.3233/WOR-2011-1137
42. Rangabashyam M, Koh SQ, Sultana R, Tan NC, Iyer NG, Soo KC, et al. Factors associated with returning to work in head and neck cancer survivors in Singapore: A preliminary exploratory mixed-methods approach study. Head Neck. (2021) 43:1451–64. doi: 10.1002/hed.26644
43. Cheng ASK, Lee S, Li N, Tsang S, Zeng Y. Chinese translation and cross-cultural adaptation of the return-to-work self-efficacy scale among chinese female breast cancer survivors. Int J Environ Res Public Health. (2023) 20:4225. doi: 10.3390/ijerph20054225
44. Takahashi M, Tsuchiya M, Horio Y, Funazaki H, Aogi K, Miyauchi K, et al. Job resignation after cancer diagnosis among working survivors in Japan: timing, reasons and change of information needs over time. Jpn J Clin Oncol. (2018) 48:43–51. doi: 10.1093/jjco/hyx143
45. Mizuno M, Munezawa N, Onizuka M, Kashiwa S, Inoue Y, Kataoka J, et al. Health related quality of life and factors relevant to return to work in cancer survivors after hospital discharge: a descriptive cross-sectional study. Discover Soc Sci Health. (2022) 2:23. doi: 10.1007/s44155-022-00026-w
46. Alleaume C, Bendiane M-K, Bouhnik A-D, Rey D, Cortaredona S, Seror V, et al. Chronic neuropathic pain negatively associated with employment retention of cancer survivors: evidence from a national French survey. J Cancer Surviv. (2018) 12:115–26. doi: 10.1007/s11764-017-0650-z
47. Tan FL, Loh SY, Tin TS, Veloo VW, Ng LL. Return to work in multi-ethnic breast cancer survivors-a qualitative inquiry. Asian Pac J Cancer Prev. (2012) 13:5791–7. doi: 10.7314/APJCP.2012.13.11.5791
48. Hansen JA, Feuerstein M, Calvio LC, Olsen CH. Breast cancer survivors at work. J Occup Environ Med. (2008) 50:777–84. doi: 10.1097/JOM.0b013e318165159e
49. Quinlan E, Thomas-MacLean R, Hack T, Kwan W, Miedema B, Tatemichi S, et al. The impact of breast cancer among Canadian women: disability and productivity. Work. (2009) 34:285–96. doi: 10.3233/WOR-2009-0926
50. Boelhouwer IG, Vermeer W, van Vuuren T. Late effects of cancer (treatment) and work ability: guidance by managers and professionals. BMC Public Health. (2021) 21:1255. doi: 10.1186/s12889-021-11261-2
51. Cleeland CS, Mayer M, Dreyer NA, Yim YM Yu E, Su Z, et al. Impact of symptom burden on work-related abilities in patients with locally recurrent or metastatic breast cancer: results from a substudy of the VIRGO observational cohort study. Breast. (2014) 23:763–9. doi: 10.1016/j.breast.2014.08.004
52. Özer Güçlüel Y, Can G. Evaluation of job stress and quality of life in individuals returning to work after cancer treatment. Eur J Oncol Nurs. (2023) 66:102381. doi: 10.1016/j.ejon.2023.102381
53. Cheng ASK, Lau LOC, Ma YNH, Ngai RH, Fong SSL. Impact of cognitive and psychological symptoms on work productivity and quality of life among breast cancer survivors in Hong Kong. Hong Kong J Occup Ther. (2016) 28:15–23. doi: 10.1016/j.hkjot.2016.11.002
54. RoŽman M, Treven S, Cančer V. Motivation and satisfaction of employees in the workplace. Bus Syst Res Int J Soc Adv Innov Res Econ. (2017) 8:14–25. doi: 10.1515/bsrj-2017-0013
55. Peuckmann V, Ekholm O, Sjøgren P, Rasmussen NK, Christiansen P, Møller S, et al. Health care utilisation and characteristics of long-term breast cancer survivors: nationwide survey in Denmark. Eur J Cancer. (2009) 45:625–33. doi: 10.1016/j.ejca.2008.09.027
56. Hara T, Kogure E, Sugita Y, Ohnuma T, Kubo A. Self-efficacy and Physical Function in Cancer Survivors Receiving Home-visit Rehabilitation. Prog Rehabil Med. (2022) 7:20220042. doi: 10.2490/prm.20220042
57. Garmy-Susini B. Hormone therapy outcome in lymphedema. Aging. (2019) 11:291–2. doi: 10.18632/aging.101772
58. Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, et al. Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. (2012) 118:2237–49. doi: 10.1002/cncr.27467
59. Eaton LH, Narkthong N, Hulett JM. Psychosocial issues associated with breast cancer-related lymphedema: a literature review. Curr Breast Cancer Rep. (2020) 12:216–24. doi: 10.1007/s12609-020-00376-x
60. Le Guen Y, Gagnadoux F, Hureaux J, Jeanfaivre T, Meslier N, Racineux J-L, et al. Sleep disturbances and impaired daytime functioning in outpatients with newly diagnosed lung cancer. Lung Cancer. (2007) 58:139–43. doi: 10.1016/j.lungcan.2007.05.021
61. Jim H, Barata A, Wenham R, Jacobsen P. Fatigue, mood, and sleep, during intraperitoneal chemotherapy: a pilot case control study. Int J Psychol Res. (2013) 6:8–14. doi: 10.21500/20112084.694
62. Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. (2018) 68:153–65. doi: 10.3322/caac.21443
63. Lee Y, Baek J-M, Jeon Y-W, Im E-O. Illness perception and sense of well-being in breast cancer patients. Pat Prefer Adher. (2019) 13:1557–67. doi: 10.2147/PPA.S225561
64. Bosma AR, Boot CRL, Snippen NC, Schaafsma FG, Anema JR. Supporting employees with chronic conditions to stay at work: perspectives of occupational health professionals and organizational representatives. BMC Public Health. (2021) 21:592. doi: 10.1186/s12889-021-10633-y
65. Bansback N, Zhang W, Walsh D, Kiely P, Williams R, Guh D, et al. Factors associated with absenteeism, presenteeism and activity impairment in patients in the first years of RA. Rheumatology. (2012) 51:375–84. doi: 10.1093/rheumatology/ker385
Keywords: return to work, employment, work productivity, activity impairment, breast cancer, work condition, survival analysis
Citation: Ng DWL, So SCY, Fielding R, Mehnert-Theuerkauf A, Kwong A, Suen D, Wong L, Fung SWW, Chun OK, Fong DYT, Chan S, Molasiotis A, So WKW and Lam WWT (2024) Return to work, work productivity loss and activity impairment in Chinese breast cancer survivors 12-month post-surgery: a longitudinal study. Front. Public Health 12:1340920. doi: 10.3389/fpubh.2024.1340920
Received: 19 November 2023; Accepted: 05 February 2024;
Published: 23 February 2024.
Edited by:
Julia Roick, Technical University of Munich, GermanyReviewed by:
Maria Malliarou, University of Thessaly, GreeceCopyright © 2024 Ng, So, Fielding, Mehnert-Theuerkauf, Kwong, Suen, Wong, Fung, Chun, Fong, Chan, Molasiotis, So and Lam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wendy Wing Tak Lam, d3d0bGFtQGhrdS5oaw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.