- Department of Anaesthesia, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Patients in Intensive Care Unit (ICU) are at high risk of developing delirium. Lack of early detection and the inability to provide prompt management of delirium remain challenges of ICU patient care. This study aimed to assess the level of knowledge, attitude, and associated factors toward delirium among healthcare providers working in ICU.
Methods: A multicenter, cross-sectional survey was conducted in comprehensive specialized hospitals from 15 April to 5 June 2023. Data were collected using a pretested, self-administered questionnaire. Ordinal logistic regression analysis was performed at p < 0.05 with a 95% confidence interval (CI). The odds ratio with 95% CI was calculated to determine the strength of the association between independent and outcome variables.
Results: A total of 202 health professionals were included in this study, with a response rate of 87%. The proportions of good, moderate, and poor knowledge about delirium in ICU were 29.21 (95% CI: 23–36), 52.48 (95% CI: 45.3–59.5) and 18.32 (95% CI:13.2–24.4), respectively. The overall proportion of negative, neutral and positive attitude were 13.9 (95% CI: 9.4–19.4), 65.8 (95% CI: 58.9–72.4) and 20.3 (95% CI: 15–26.5) respectively. Being an anesthetist and exposure to training were positively associated with a good knowledge while belief in screening tool to change care and reading, and using guidelines were positively associated with a positive attitude. However, believing the impossibility of changing the practice of delirium care, and negative attitudes were delaying factors for a good knowledge. Also, workload and poor knowledge were hindering factors for a positive attitude.
Conclusion: More than half of health professionals had moderate knowledge and neutral attitude toward delirium. However, some of them had poor knowledge and a negative attitude. We recommend stakeholders prepare regular training for delirium care. Also, we urge health professionals to update themselves by reading guidelines and to use screening protocols for delirium.
1 Introduction
Delirium is defined as an acute confounding state with a complex clinical syndrome characterized by disturbance of consciousness, attention, cognitive function, or perception that develops within a short period of time and tends to fluctuate during the course of the day (1). It is a common incidental problem in intensive care unit (ICU), which accounted for 68% in India (2); 51% in Uganda (3); 80% in USA (4) and 22.9% in Mexico, of which 12% of the victims ended up with death (5). Delirium would be high in older patients, immobilized patients, patients on multiple medications, patients with sepsis, medical illnesses, and those on mechanical ventilation (6–8). Even though delirium is usually transient and a reversible syndrome, when left untreated, it will expose patients to prolonged hospital stays, prolonged mechanical ventilation, long-term cognitive dysfunction, and increased mortality (6, 9). The incidence and duration of delirium in ICU patients could be effectively reduced by using multicomponent interventions such as physical activity, family participation, cognitive stimulation, reorientation, sensory stimulation, environmental control, clinical adjustment, and reorientation (10). Assessment of the patient’s conscious level and use of validated detection tools are paramount for the diagnosis and treatment of delirium (11).
However, this condition is often underrecognized and not addressed effectively (12).
As knowledge of delirium and its management approach has changed significantly, professionals those are unaware of it might have a poor level of knowledge, and bad attitude, and poor practice on their patient care (13). Studies also reported that health care providers frustrated to provide care for delirium patients, with arguable reasons of lack of confidence on assessment and dislike of delirium management (14). Reports showed patients with delirium being viewed as underestimated, ignored, and considered a “burden.” This can lead to negative outcomes for patients, hospital staff, and the system of health care because of increased hospitalization and the need for expensive interventions in the event of complications (15). Problems in early detection and management of delirium by health professionals working in the ICU has been reported (2). Lack of knowledge on diagnosis and screening tools, poor attitudes toward delirium care, communication challenges, time restraints, and workload were among the barriers to poor detection and management of delirium (9). The use of validated assessment tools can ensure early detection and the provision of appropriate care to achieve good outcomes (16). To the best of our knowledge, there is no previous study that determines health professionals’ knowledge, attitude, and barriers toward the diagnosis and monitoring of delirium in the study region. It is well understood that the use of updated assessment tools for the measurement of delirium relies on health care providers’ beliefs, perceptions, and attitudes toward delirium. In the present study, we carried out a multi-center survey involving critical care physicians, non-physician anesthetists and ICU nurses regarding their current knowledge and attitude of delirium as well as perceived barriers to the screening and monitoring of delirium. The results of our study may be used us a source for future researchers, and it can also help policymakers to restructure the working environment and improve the management of delirious patients.
2 Methods
A hospital-based, multicenter cross-sectional study was followed. The study was conducted on surgical and medical ICUs at four comprehensive specialized hospitals located in Amhara National Regional State, north-west Ethiopia. The duration of the research was from 15 April to 5 June 2023. Before data collection, we communicate with the ICU leaders of the four hospitals to ensure the homogeneity of the study participants. We found 232 eligible study participants working in almost similar surgical and medical ICU setups.
Inclusion criteria:
• Physicians (Internists, surgeons, surgical and medical residents involved in ICU patient care).
• Anesthetists/Anesthesiologist (Anesthesia and critical care providers working in the ICUs).
• ICU nurses (Intensive care specialist nurses working in the ICUs).
Part-time workers, volunteers, and carers on leave during the data collection period were excluded from the study. Sociodemographic variables, cultural variables, and work-related variables were included in the self-administered questionnaire. Levels of knowledge and attitude were the main outcome variables. Knowledge was defined as the familiarity or awareness of someone or something, such as facts, skills, or objects contributing to understanding. Overall knowledge score was categorized using Bloom’s cut-off points for KAP study 80%–100% for good knowledge 60%–79% for moderate knowledge, and ≤59% for poor knowledge (17). Attitude was defined as critical care providers’ thinking and feeling about the diagnosis and the clinical significance of delirium. A total of 22 items were included in the questionnaire, which was subdivided into three domains (emotion, behavior, and belief). It was measured using five point-Likert scale (from completely disagree to completely agree). The overall attitude score was categorized using Bloom’s cut-off points for KAP study 80%–100% for positive attitude, 60%–79% for neutral attitude, and ≤59% for negative attitude (17). Many studies adapted this cutoff point to determine the level of knowledge, attitude, and practice for their respective studies (18–22).
In this survey, the total study population in the study areas was 232 and easily accessible, so we took the whole population in the four aforesaid hospitals.
After completion of data collection, the variables were entered, coded, and cleaned for errors using Epi-data software. Then the data were transformed into SPSS version 25 software and analyzed. Descriptive data were expressed with frequency and percentage. The Shapiro–Wilk test was checked for the distribution of data. Non-normally distributed data were presented with a median and interquartile range. The model goodness of fit test, multi-collinearity test and parallel line test were checked.
Ordinal logistic regression analysis was conducted to assess the association between dependent and independent variables. The odds ratio with the corresponding 95% CI was calculated to determine the strength of the association of the independent factors with outcome variables. A p-value < 0.05 was considered as statistically significant predictive factors. Finally, the results were presented with texts, tables, and graphs.
Ethical clearance was obtained from Ethical Review Committee of the respective hospitals. Informed consent was obtained from each study participant after a clear explanation of the merits of the study, and confidentiality and anonymity were ensured.
3 Results
3.1 Socio-demographic characteristics
Among 232 eligible study participants, 202 of them were included in the final analysis with a response rate of 87%. Fifty (24.1%) physicians, 77 (38.1%) anesthetists and 75 (37.1%) nurses participated in the study. Thirty study subjects were excluded from the analysis: nine due to incomplete data and 21 due to refusal to fill out the data. Among participants, 147 (72.8%) were males, while 55 (27.2%) were females. The median age of the study participants was 31 (28.75–35). The majority of the health professionals had work experience of 5 to 9 years in their profession (Table 1).
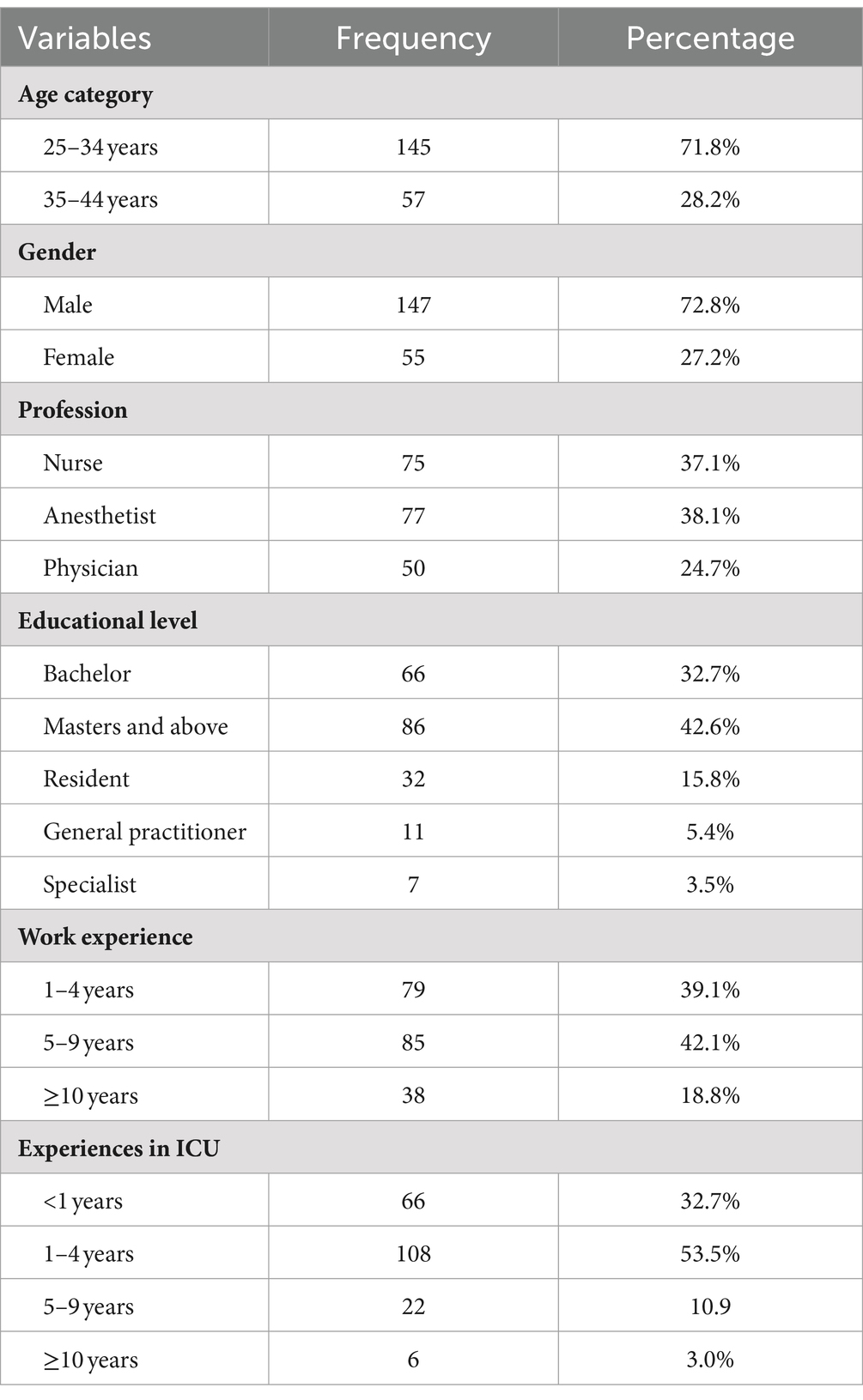
Table 1. Socio-demographic characteristics of health professionals working in ICU, Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
3.2 Work-related characteristics and beliefs of health professionals
Most, 172 (85.1%) of the study subjects acknowledged the usefulness of a screening tool for delirium while 165 (81.7%) of them had no prior experiences at institutions where protocols or guidelines were implemented.
The overall median responses to knowledge and attitude questions were 73 (63–80) and 71 (64–78), respectively.
3.3 Level of attitude and knowledge across hospitals
In the University of Gondar comprehensive specialized hospital (UOGCSH), 45 (22.2%) study subjects had moderate knowledge, while 19 (9.4%) of them had good knowledge (Figure 1). In Tibebe Ghion Comprehensive Specialised Hospital (TGCSH), 32 (15.8%) study subjects had neutral attitude, whereas 12 (5.9%) had a positive attitude (Figure 2).
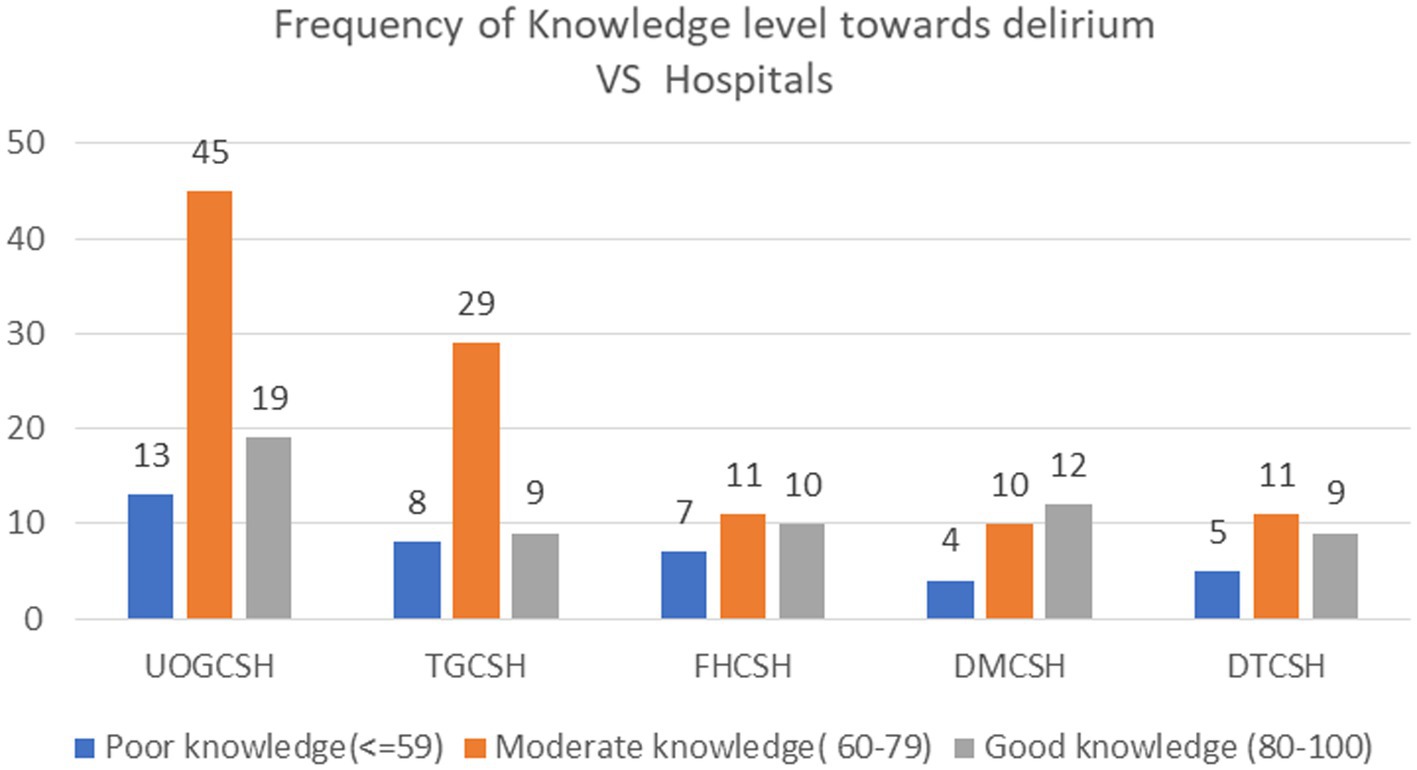
Figure 1. Frequency of Knowledge level toward delirium vs. Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
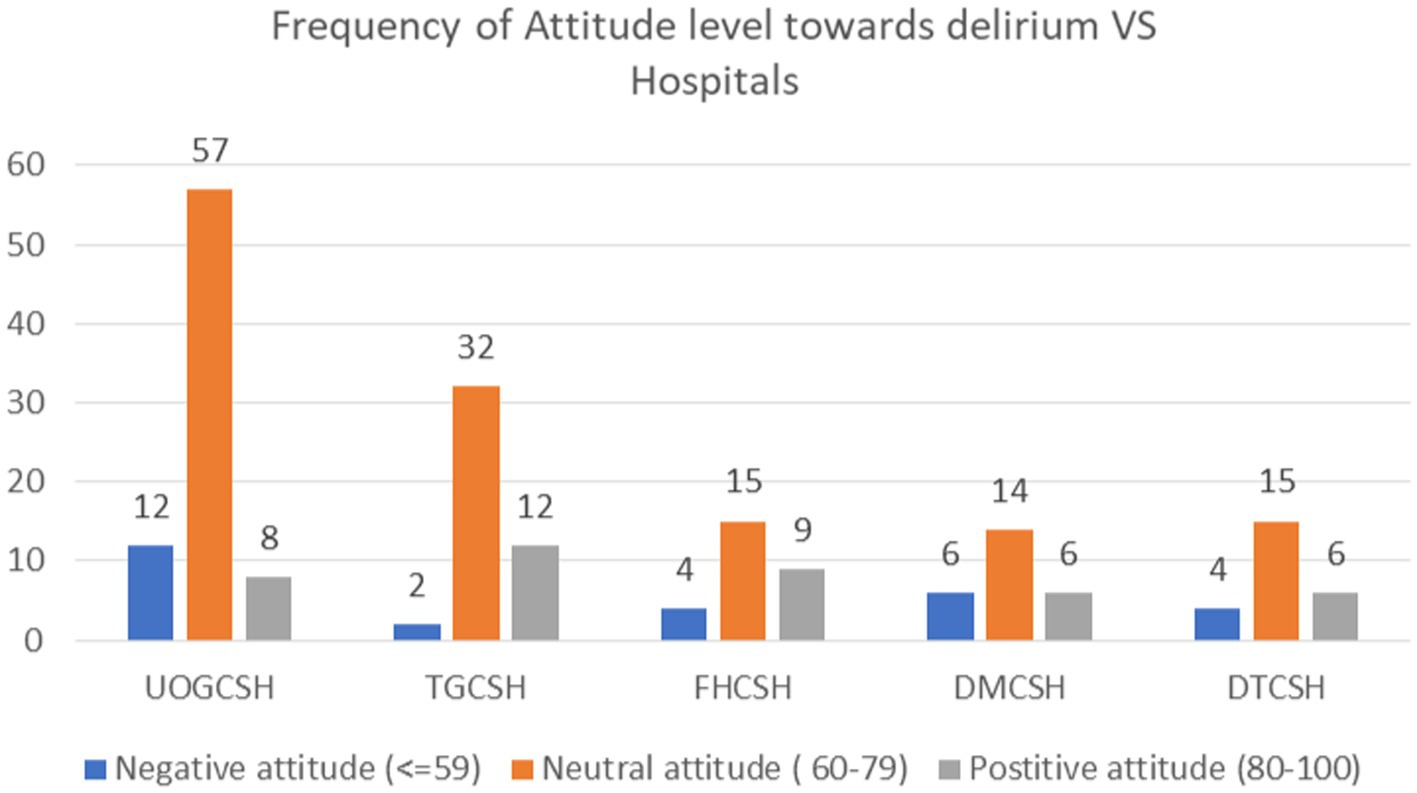
Figure 2. Frequency of Attitude level toward delirium vs. Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
3.4 Overall proportions of knowledge and attitude toward delirium
The overall proportion of good, moderate, and poor knowledge was 29.21 (95% CI: 23–36), 52.48 (95% CI: 45.3–59.5), and 18.32 (95% CI: 13.2–24.4), respectively (Figure 3). The overall proportion of negative, neutral, and positive attitudes was 13.9 (95% CI: 9.4–19.4), 65.8 (95% CI: 58.9–72.4) and 20.3 (95% CI:15–26.5) respectively (Figure 4).
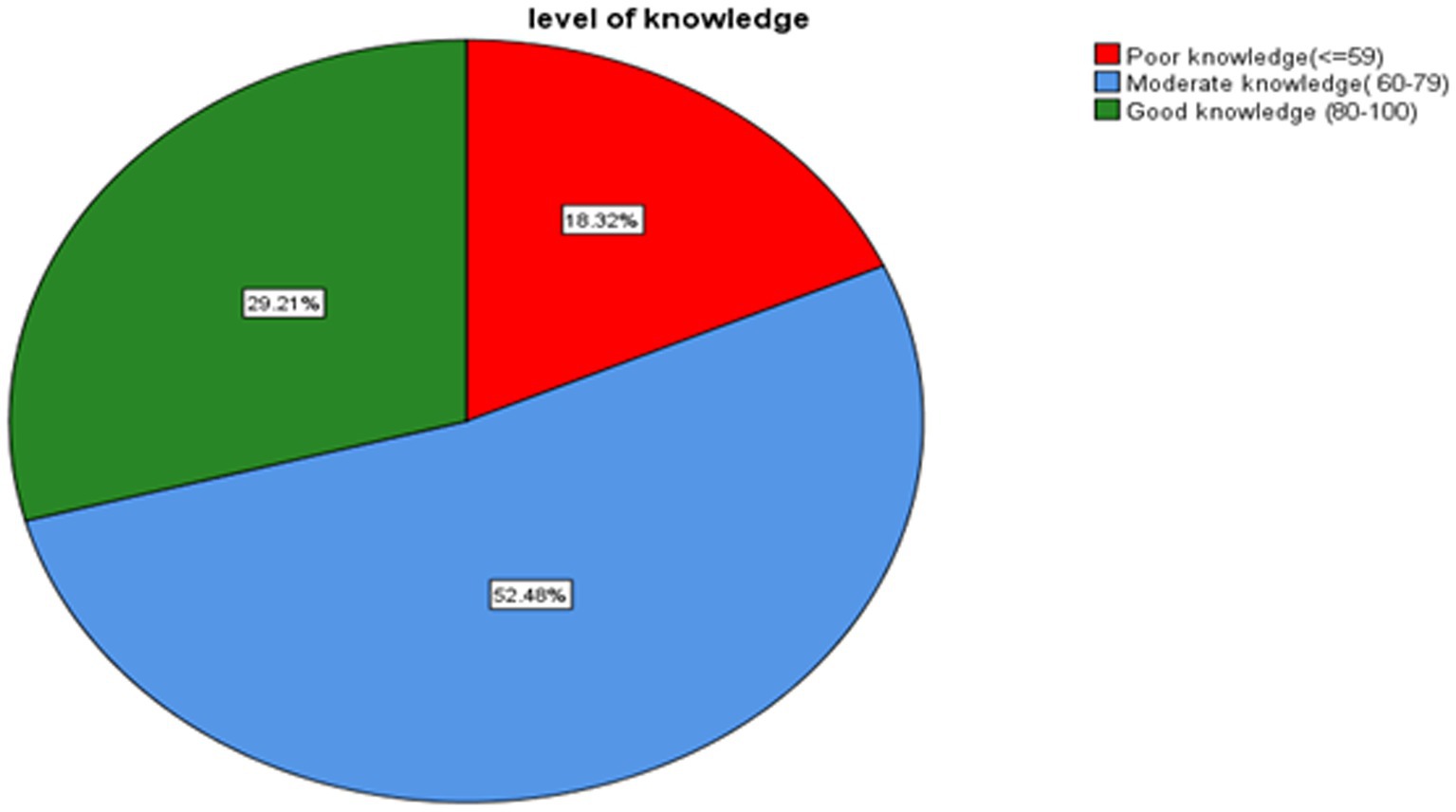
Figure 3. Proportions of knowledge level toward delirium among health professionals working in ICU, Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
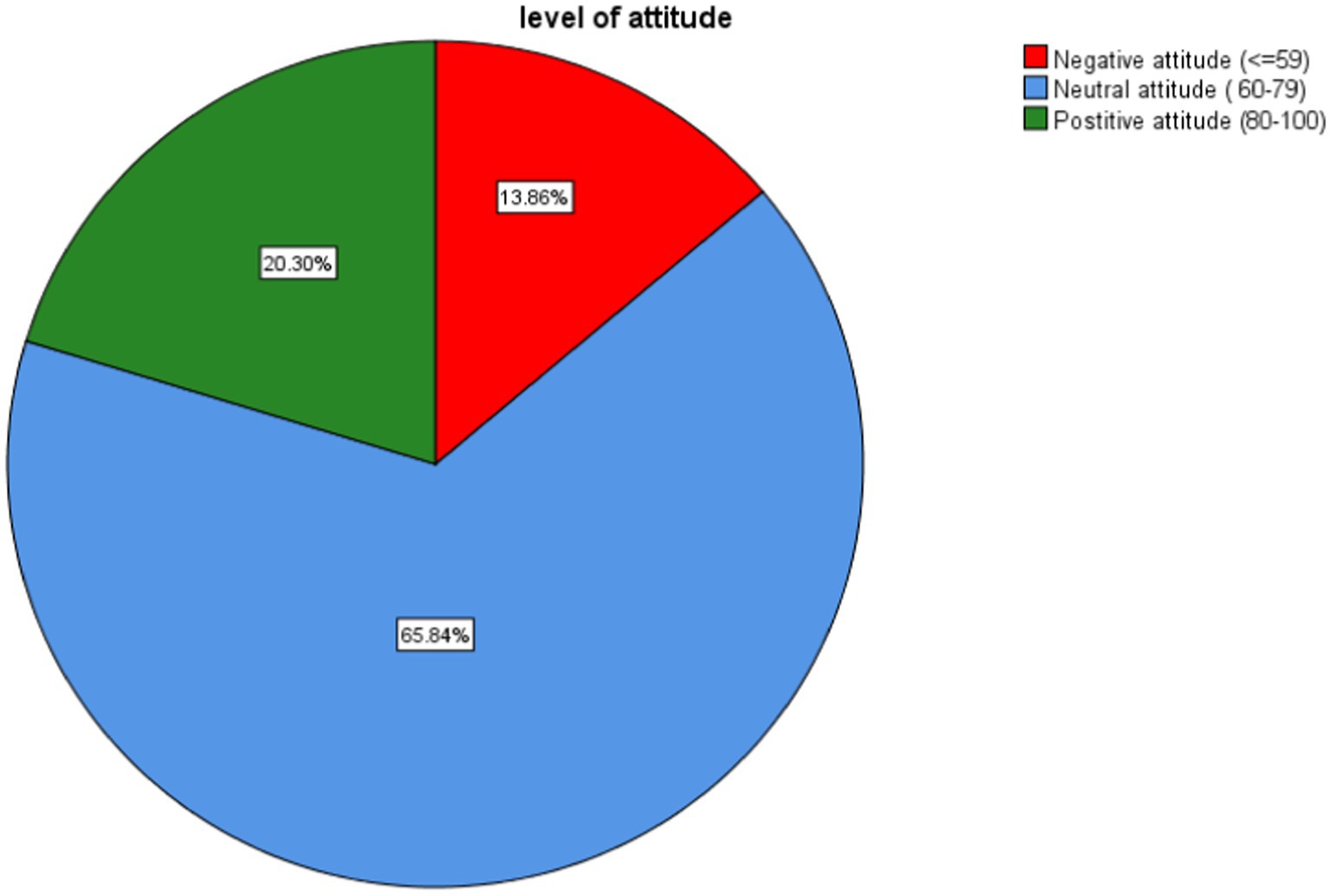
Figure 4. Proportions of attitude level toward delirium among health professionals working in ICU, Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
3.5 Factors associated with knowledge level toward delirium
Factors showing an association with knowledge in bivariable ordinal logistic regression analysis were entered into multivariable ordinal logistic regression. Anesthetists were more likely to have good knowledge as compared to physicians holding all other variables constant (AOR = 2.8, 95% CI =1.25–6.26, p = 0.012). Believing the possibility of changing the practice of delirium care was less likely to have good knowledge than believing possibility of change (AOR = 0.48, 95% CI =0.24–0.97, p = 0.041).
Health professionals engaged in training about delirium were more likely to have good knowledge as compared to those lacking the training (AOR = 2.16, 95% CI =1.14–4.1, p = 0.018). The odds of having a negative attitude were less likely to have good knowledge than having a positive attitude (AOR = 0.06, 95% CI = 0.02–0.19, P ≤ 0.001).
Professionals with neutral attitude were less likely to have good knowledge than having positive attitude (AOR = 0.13, 95% CI = 0.05–0.29, P ≤ 0.001; Table 2).
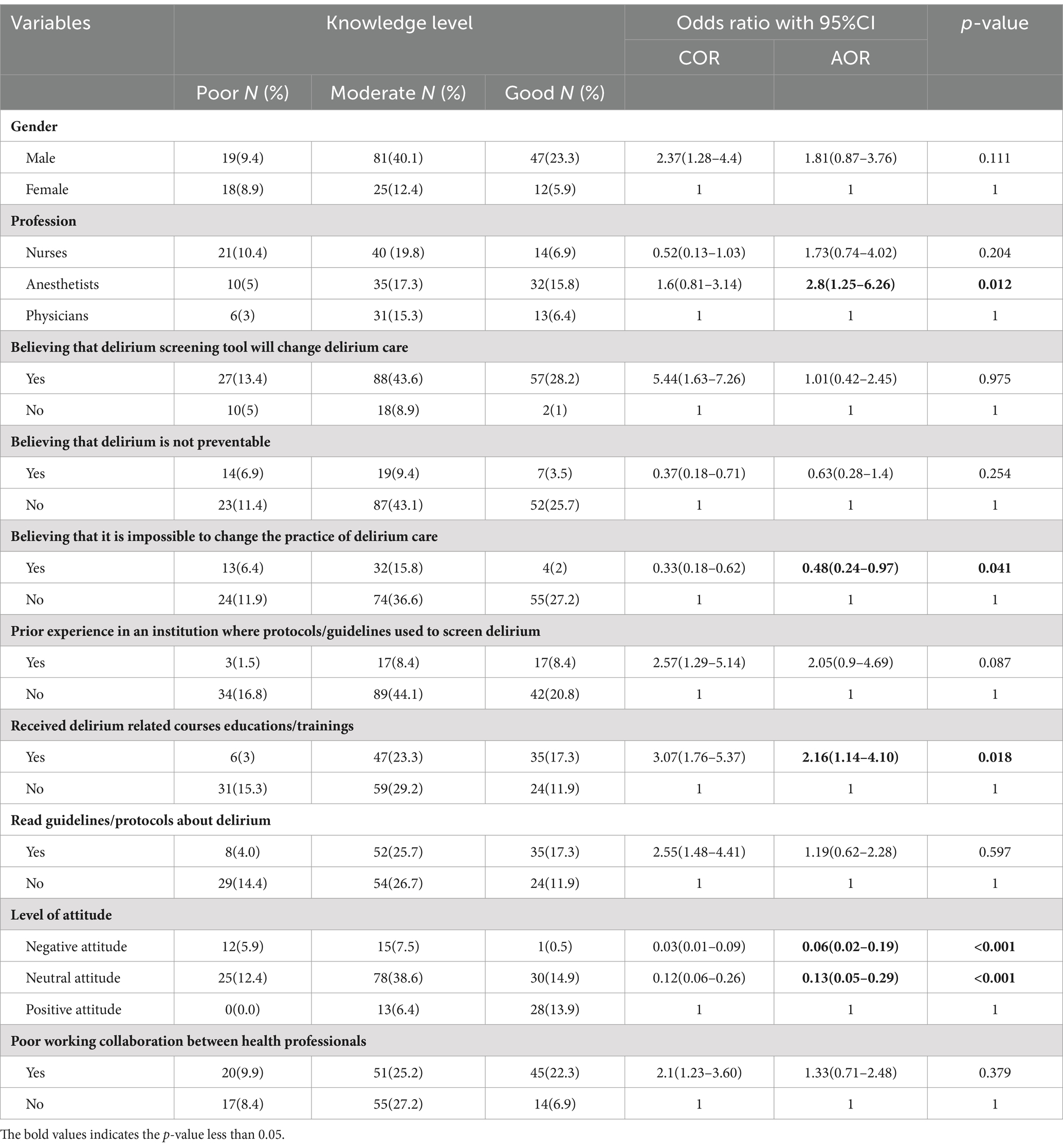
Table 2. Ordinal logistic regression for knowledge level toward delirium among health professionals working in ICU, Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
3.6 Factors associated with attitude level toward delirium
Factors showing an association with attitude in bivariable ordinal logistic regression analysis were entered into multivariable ordinal logistic regression. Believing that the screening tool will change delirium care was more likely to have a positive attitude as compared to those who did not believe, holding all other variables constant (AOR = 3.71, 95% CI =1.35–10.15, p = 0.011). The estimated odds ratio (AOR = 2.7, 95% CI =1.23–5.92, p = 0.013) indicated that health professionals who use protocols or guidelines to screen delirium were more likely to have a positive attitude than those who do not use them.
Reading updated guidelines and protocols was more likely to have a positive attitude as compared to not reading (AOR = 2.55, 95% CI =1.17–5.59, p = 0.019). Professionals with overloaded work were less likely to have a positive attitude when compared to those with a lower workload (AOR = 0.41, 95% CI = 0.17–0.96, p = 0.04). Working in the surgical ICU was less likely to have a positive attitude than working in the mixed ICU (AOR = 0.41, 95% CI = 0.18–0.96, p = 0.04). Having poor knowledge was less likely to a have a positive attitude than having good knowledge (AOR = 0.04, 95% CI = 0.01–0.13, P ≤ 0.001). Having a moderate knowledge was times less likely to have positive attitude than having a good knowledge (AOR = 0.15, 95% CI = 0.06–0.36, P ≤ 0.001; Table 3).
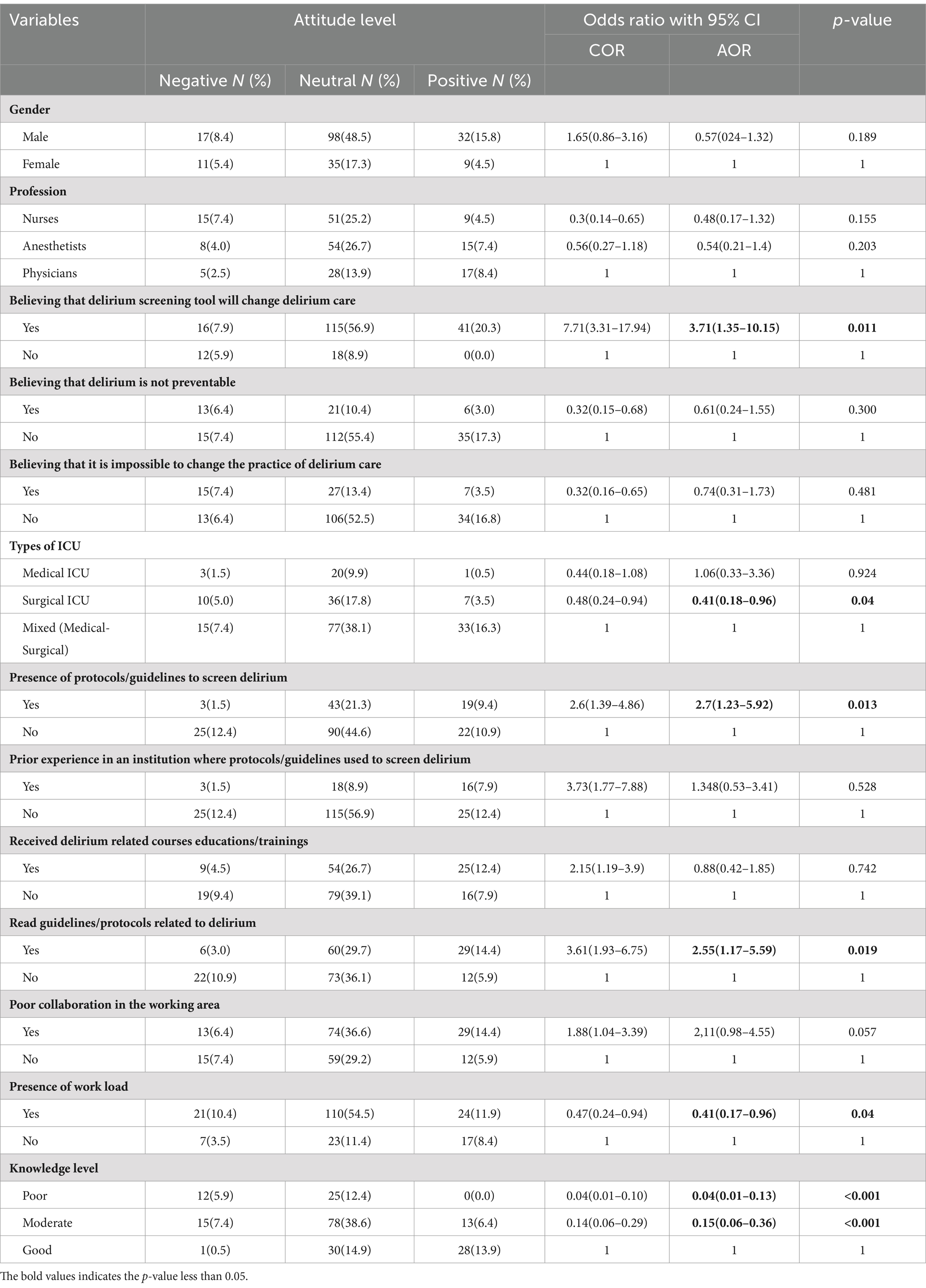
Table 3. Ordinal logistic regression for attitude level toward delirium among health professionals working in ICU, Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2023, (N = 202).
4 Discussion
Our research found that good knowledge and a positive attitude toward delirium remain lower, at 29.1 and 20.3%, respectively. Delirium is the main incidental problem in ICU settings (23–25). Physicians, nurses, and anesthetists were the direct healthcare providers for critically ill patients. Moreover, management of delirium in the ICU should be multidisciplinary approach “including physicians, nurses, and possibly other healthcare professionals (26–28). Lack of knowledge and attitude toward delirium among health professionals would affect the quality of healthcare and preventive measures (29).
This study discovered that the overall proportion of good, moderate, and poor knowledge about delirium was 29.21, 52.48, and 18.32, respectively. The proportion of good knowledge was in line with a study conducted in Iran, which found a proportion of 24.6%. However, the moderate level of knowledge was higher than in this study, with a proportion of 68.3% (29). A study done in Egypt reported a higher level of good knowledge with a proportion of 83.1% as compared to our study. However, a poor level of knowledge was comparable with this study with a proportion of 16.9% (30). A previous study that used a similar levels of knowledge category as ours found moderate and poor level of knowledge of 31 (91.2%) and 3 (8.8%), respectively, which is different from the result of this study (31). The discrepancy might be due to the small sample size they used and the fact that it was conducted only on nurse professionals.
In this study, the overall proportion of negative, neutral, and positive attitude toward delirium was 13.9 (95% CI: 9.4–19.4), 65.8 (95% CI: 58.9–72.4) and 20.3 (95% CI: 15–26.5), respectively. The proportion of positive attitudes in this study was lower as compared to reports from Egypt (66.2%) and Sri Lanka (80%) (29, 30). A study done in UK and Canada reported that most nurses had a negative attitude toward delirium in the ICU (14). However, only 13.9% of health professionals had negative attitude in our study. The possible reasons for the difference in level of attitude might be due to the categorization of the attitude section as negative, neutral, and positive in this study, while negative and positive attitudes were found in previous studies (30). The composition of study participants regarding of profession, in-service training, measurement tool, and sample size might also be possible reasons for the differences in knowledge and attitude level.
This study found that engagement in training about delirium was more likely to have an association with good knowledge, which is consistent with previous studies (30, 32, 33). A study conducted in Poland found that lack of education about delirium control had negative effect on knowledge of delirium symptoms, risk factors and complications associated with delirium in ICU patients (34). Educational interventions with inter-professional involvement increased the knowledge of clinicians about delirium in ICU (35). A focused session of delirium education for junior health professionals would increase the overall screening, investigation, and management of patients with delirium (32). Moreover, educational exposure to delirium in the form of lectures or discussions during training had a significant contribution to the improvement of the level of knowledge (36). Contrary to this fact, one study reported that the quantity of prior education about delirium did not improve the confidence, competence, and knowledge of clinicians (37).
In our study, anesthetists were more likely to have good knowledge on delirium as compared to physicians. This is supported by previous studies justifying that anesthetists spent their maximum time working in a high-level ICU (9, 26). Possibly, anesthetists might be more familiar with delirium, as it is one of the post-anesthesia complications and complications for patients with mechanical ventilators behind having good knowledge about delirium than other disciplines. Cross-sectional studies found that nurses lack the knowledge and skill to assess delirium. The difficulty of assessing delirium in intubated patients, nurses’ lack of confidence in their ability to use delirium assessment, poor organization and management, and the complexity of patients’ conditions were mentioned as potential barriers to the assessment of delirium (38).
Study participants those reporting the impossibility of changing the practice of delirium care were less likely to have good knowledge than reported the possibility to change. In agreement with this, reluctance to change delirium care practice was the possible factor that negatively affected the level of knowledge (9).
Those with a negative or neutral attitude toward delirium were less likely to have good knowledge about delirium than those with a positive attitude. These findings are supported by previous studies (29, 39). In line with this study, an earlier study reported that better knowledge was correlated with a positive attitude toward delirium (39). Health professionals who believed that the delirium screening tool would change delirium care were more likely to have a positive attitude as compared to those who did not, which is consistent with previous studies (9).
The presence of protocols or guidelines to screen for delirium in the ICU was more likely to have a positive attitude than the absence of the tools (9, 40). Similarly, a previous study identified that inadequate or non-existent use of delirium tools was one contributing factor to the low level of attitude toward delirium (41). In this study, health professionals who had read guidelines and protocols were more likely to have a positive attitude than those who had not read them. In agreement with this, earlier studies identified that reading guidelines and protocols for delirium care had a significant effect on the positive attitude of clinicians working in the ICU (32, 33, 42).
This study confirmed that health professionals those with a high work load were less likely to have a positive attitude than those with no work load. Similarly, previous studies identified that workload was the main determinant factor that negatively affected the level of attitude (9, 40).
Professionals working in the surgical ICU were less likely to have a positive attitude. Probably, the reason might be due to the lack of multidisciplinary collaboration and no proper policy on delirium care. In the surgical ICU, there should be special inter-professional collaborations with surgeons, anesthetists and nurses because multiple hands are applied on the patient’s perioperative care (43). Additionally, interrelating the manifestations of delirium with anesthesia and surgery independent of other comorbid features may lead to a negative attitude, and the patient may be left untreated (44).
Study participants with poor and moderate knowledge were less likely to have a positive attitude than those with good knowledge. This finding is in congruence with earlier study that knowledge played a significant role in improving the quality of healthcare and preventive measures, as well as the attitude toward dealing with delirious patients. Also, another study stated the positive correlation between attitude and knowledge toward delirium (29, 39).
The findings of this study implies that health professionals who have poor knowledge about delirium may have a negative attitude, and the vice-versa. Even though we did not accurately assess the impact on the patients’ care, it can be concluded that poor knowledge and a negative attitude possibly contribute for poor patient outcomes. Therefore, we suggest educational interventions so as to improve health professionals’ knowledge and attitude to indirectly improve the patient’s outcome. Finally, the findings of this study can form the basis for an intervention module that can address risk factors, assessment, and management of delirium in ICU.
4.1 The strength and limitations of the study
The possible strength of the study would be the use of primary data sources; being a multi-center study, and the research is the first of its type in Ethiopia since we did not access any published evidences, which would create motivation for researchers to do more research on similar studies. As limitations, self-administered responses may have unavoidable inaccuracies due to response bias, which could have been caused by poor recall or misunderstanding of questions and exposed to social desirability bias as respondents may over-report their attitudes.
5 Conclusions and recommendations
More than half of health professionals had moderate knowledge (52.48%) and a neutral attitude (65.8%) toward delirium. However, there was still some proportion of health professionals with poor knowledge (18.32%) and a negative attitude (13.9%). Only (29.21%) and (20.3%) of the study subjects had good knowledge and a positive attitude, respectively. Being anesthetist and having educations training about delirium were positively associated with good knowledge while believing delirium screening tools will change delirium care, using protocols or guidelines to screen delirium, and reading guidelines or protocols were positively associated with a positive attitude. However, it is impossible to change the practice of delirium care; negative attitudes, and neutral attitudes were delaying factors for good knowledge. Similarly, work load, poor knowledge, and moderate knowledge were hindering factors for a positive attitude. So, we recommend that concerned bodies prepare regular trainings and courses related to delirium. Also, we urge health professionals to update themselves by reading recent guidelines and protocols, as well as to prepare and use screening protocols and guidelines.
Data availability statement
The datasets presented in this article will be made available upon request from the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical Review Committee of University of Gondar, school of medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RA: Conceptualization, Formal Analysis, Writing – original draft. TG: Software, Writing – review & editing. WC: Writing – review & editing, Conceptualization, Formal Analysis, Visualization. DY: Writing – review & editing, Methodology, Software, Supervision, Validation. HE: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors’ deepest gratitude goes to the University of Gondar, College of Medicine and Health Sciences.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association (1994).
2. Grover, S, Mehra, A, Sharma, N, Sahoo, S, and Dua, D. Knowledge and attitude of nurses toward delirium. Annals Indian Psychiatry. (2022) 6:73–81. doi: 10.4103/aip.aip_134_21
3. Kwizera, A, Nakibuuka, J, Ssemogerere, L, Sendikadiwa, C, Obua, D, Kizito, S, et al. Incidence and risk factors for delirium among mechanically ventilated patients in an African intensive care setting: an observational multicenter study. Crit Care Res Prac. (2015) 2015:491780. doi: 10.1155/2015/491780
4. Girard, TD, Pandharipande, PP, and Ely, EW. Delirium in the intensive care unit. Crit Care. (2008) 12:S3. doi: 10.1186/cc6149
5. Sánchez-Hurtado, LA, Hernández-Sánchez, N, Moral-Armengol, D, Guevara-García, H, García-Guillén, FJ, Herrera-Gómez, Á, et al. Incidence of delirium in critically ill cancer patients. Pain Res Manag. (2018) 2018:4193275. doi: 10.1155/2018/4193275
6. Bulic, D, Bennett, M, Rodgers, H, Nourse, M, Rubie, P, Looi, JC, et al. Delirium after mechanical ventilation in intensive care units: the cognitive and psychosocial assessment (CAPA) study protocol. JMIR Res Protoc. (2017) 6:e6660. doi: 10.2196/resprot.6660
7. Fong, TG, Tulebaev, SR, and Inouye, SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. (2009) 5:210–20. doi: 10.1038/nrneurol.2009.24
8. Brummel, NE, and Girard, TD. Preventing delirium in the intensive care unit. Crit Care Clin. (2013) 29:51–65. doi: 10.1016/j.ccc.2012.10.007
9. Trogrlić, Z, Ista, E, Ponssen, HH, Schoonderbeek, JF, Schreiner, F, Verbrugge, SJ, et al. Attitudes, knowledge and practices concerning delirium: a survey among intensive care unit professionals. Nurs Crit Care. (2017) 22:133–40. doi: 10.1111/nicc.12239
10. Chen, T-J, Traynor, V, Wang, A-Y, Shih, C-Y, Tu, M-C, Chuang, C-H, et al. Comparative effectiveness of non-pharmacological interventions for preventing delirium in critically ill adults: a systematic review and network meta-analysis. Int J Nurs Stud. (2022) 131:104239. doi: 10.1016/j.ijnurstu.2022.104239
11. Barr, J, Fraser, GL, Puntillo, K, Ely, EW, Gélinas, C, Dasta, JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. (2013) 41:263–306. doi: 10.1097/CCM.0b013e3182783b72
12. Arumugam, S, El-Menyar, A, Al-Hassani, A, Strandvik, G, Asim, M, Mekkodithal, A, et al. Delirium in the intensive care unit. J Emerg Trauma Shock. (2017) 10:37. doi: 10.4103/0974-2700.199520
13. LeBlanc, A, Bourbonnais, FF, Harrison, D, Tousignant, KJI, and Nursing, CC. The experience of intensive care nurses caring for patients with delirium: a phenomenological study. Intensive Crit Care Nurs. (2018) 44:92–8. doi: 10.1016/j.iccn.2017.09.002
14. Zamoscik, K, Godbold, R, Freeman, PJI, and Nursing, CC. Intensive care nurses’ experiences and perceptions of delirium and delirium care. Intensive Crit Care Nurs. (2017) 40:94–100. doi: 10.1016/j.iccn.2017.01.003
15. Inouye, SK. Delirium—a framework to improve acute care for older persons. J Am Geriatr Soc. (2018) 66:446–51. doi: 10.1111/jgs.15296
16. Meunier, JM. Practices and perceptions of delirium assessment by critical care nurses Gardner-Webb University ProQuest Dissertations Publishing (2010).
17. Bloom, BS. Learning for mastery. Instruction and curriculum. Regional education Laboratory for the Carolinas and Virginia, topical papers and reprints, number 1. Eval Comm. (1968) 1:n2.
18. Khaled, A, Siddiqua, A, and Makki, S. The knowledge and attitude of the community from the Aseer region, Saudi Arabia, toward COVID-19 and their precautionary measures against the disease. Risk Manag Healthc Policy. (2020) 13:1825–34. doi: 10.2147/RMHP.S271899
19. Ahmed, N, and Taneepanichskul, S. Knowledge, attitude and practice of dengue fever prevention among the people in male, Maldives. J Health Res. (2008) 22:33–7.
20. Akalu, Y, Ayelign, B, and Molla, MJS. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen hospital, Northwest Ethiopia. Infect Drug Resist. (2020) 13:1949–60. doi: 10.2147/IDR.S258736
21. Xing, H, Zhu, S, Liu, S, Xia, M, Jing, M, Dong, G, et al. Knowledge, attitudes and practices of ICU nurses regarding subsyndromal delirium among 20 hospitals in China: a descriptive cross-sectional survey. BMJ Open. (2022) 12:e063821. doi: 10.1136/bmjopen-2022-063821
22. Seid, MA, and Hussen, MS. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC Infect Dis. (2018) 18:1–8. doi: 10.1186/s12879-018-3199-1
23. Rowley-Conwy, GJI, and Nursing, CC. Barriers to delirium assessment in the intensive care unit: a literature review. Intensive Crit Care Nurs. (2018) 44:99–104. doi: 10.1016/j.iccn.2017.09.001
24. Colantuoni, E, Koneru, M, Akhlaghi, N, Li, X, Hashem, MD, Dinglas, VD, et al. Heterogeneity in design and analysis of ICU delirium randomized trials: a systematic review. Trials. (2021) 22:354. doi: 10.1186/s13063-021-05299-1
25. Zhang, S, Han, Y, Xiao, Q, Li, H, and Wu, Y. Effectiveness of bundle interventions on ICU delirium: a meta-analysis. Crit Care Med. (2021) 49:335. doi: 10.1097/CCM.0000000000004773
26. Gokmen, N, Iyilikci, L, Kucukguclu, S, Kuvaki, B, Ciftci, L, and Gunerli, A. Approaches of Turkish anesthesiologists to delirium observed in intensive care unit patients. Crit Care. (2007) 11:P418. doi: 10.1186/cc5578
27. Gong, ZP, Liu, XW, Zhuang, YY, Chen, XP, Xie, GH, Cheng, BL, et al. Survey of attitudes and behaviors of healthcare professionals on delirium in ICU. Chin J Traumatol. (2009) 12:328–33. doi: 10.3760/cma.j.issn.1008-1275.2009.06.002
28. Pisani, MA, Araujo, KL, Van Ness, PH, Zhang, Y, Ely, EW, and Inouye, S. A research algorithm to improve detection of delirium in the intensive care unit. Crit Care. (2006) 10:1–8. doi: 10.1186/cc5027
29. Monfared, A, Soodmand, M, and Ghasemzadeh, G. Knowledge and attitude of intensive care units nurses towards delirium working at Guilan University of Medical Sciences in 2015. Prev Care Nurs. (2017) 7:1–7.
30. YEE-S, H, Mahmoud, BH, and Hamza, MF. Nurses’ performance toward patients with delirium in intensive care unit. Int J Novel Res Healthc Nurs. 8:222–33.
31. Ismail, MA, and Fadhil, I. Assessment of nurses knowledge regarding delirium in adult critical care units in Baqubah. Mosul J Nurs. (2021) 9:232–47. doi: 10.33899/mjn.2021.169850
32. Hancock, Sara, "Nurses' Knowledge of Delirium in the ICU" (2022). DNP Projects. 405. Available at: https://uknowledge.uky.edu/dnp_etds/405.
33. Yıldırım, F, Türkleş, S, and Altundal, DH. The effect of delirium information training given to intensive care nurses on patient care: quasi-experimental study. PeerJ. (2022) 10:e13143. doi: 10.7717/peerj.13143
34. Lange, S, Medrzycka-Dabrowska, W, Tomaszek, L, Wujtewicz, M, and Krupa, S. Nurses' knowledge, barriers and practice in the care of patients with delirium in the intensive care unit in Poland—a cross-sectional study. Front Public Health. (2023) 11:1119526. doi: 10.3389/fpubh.2023.1119526
35. Ramoo, V, Abu, H, Rai, V, Surat Singh, SK, Baharudin, AA, Danaee, M, et al. Educational intervention on delirium assessment using confusion assessment method-ICU (CAM-ICU) in a general intensive care unit. J Clin Nurs. (2018) 27:4028–39. doi: 10.1111/jocn.14525
36. Arachchi, TMJ, and Pinto, VOfficial Publication of Indian Society of Critical Care Medicine. Understanding the barriers in delirium care in an intensive care unit: a survey of knowledge, attitudes, and current practices among medical professionals working in intensive care units in teaching hospitals of Central Province, Sri Lanka. Indian J Crit Care Med. (2021) 25:1413. doi: 10.5005/jp-journals-10071-24040
37. Ormonde, C, Igwe, EO, Nealon, J, O’Shaughnessy, P, Traynor, V, and Research, E. Delirium education and post-anaesthetics care unit nurses’ knowledge on recognising and managing delirium in older patients. Aging Clin Exp Res. (2023) 35:995–1003. doi: 10.1007/s40520-023-02390-2
38. Gao, Y, Zhang, C, Liao, C, and Gan, X. Nurses' assessment of subsyndromal delirium and barriers to assessment: a cross-sectional survey in the intensive care unit. J Nurs Manag. (2022) 30:4491–502. doi: 10.1111/jonm.13887
39. Papaioannou, M, Papastavrou, E, Kouta, C, Tsangari, H, and Merkouris, A. Investigating nurses’ knowledge and attitudes about delirium in older persons: a cross-sectional study. BMC Nurs. (2023) 22:10. doi: 10.1186/s12912-022-01158-9
40. Xing, J, Sun, Y, Jie, Y, Yuan, Z, and Liu, W. Perceptions, attitudes, and current practices regards delirium in China: a survey of 917 critical care nurses and physicians in China. Medicine. (2017) 96:e8028. doi: 10.1097/MD.0000000000008028
41. El Hussein, M, Hirst, S, and Salyers, V. Factors that contribute to underrecognition of delirium by registered nurses in acute care settings: a scoping review of the literature to explain this phenomenon. J Clin Nurs. (2015) 24:906–15. doi: 10.1111/jocn.12693
42. Ista, E, Trogrlic, Z, Bakker, J, Osse, RJ, van Achterberg, T, and van der Jagt, M. Improvement of care for ICU patients with delirium by early screening and treatment: study protocol of iDECePTIvE study. Implement Sci. (2014) 9:143. doi: 10.1186/s13012-014-0143-7
43. Oosterhouse, KJ, Vincent, C, Foreman, MD, Gruss, VA, Corte, C, and Berger, B. Intensive care unit nurses’ beliefs about delirium assessment and management. AACN Adv Crit Care. (2016) 27:379–93. doi: 10.4037/aacnacc2016535
Keywords: attitude, delirium, intensive care, knowledge, professionals
Citation: Ayanaw Eyayu R, Gudayu Zeleke T, Chekol WB, Yaregal Melesse D and Enyew Ashagrie H (2024) Assessment of level of knowledge, attitude, and associated factors toward delirium among health professionals working in intensive care unit multicenter, cross-sectional study, Amhara region comprehensive specialized hospitals, Northwest Ethiopia, 2023. Front. Public Health. 12:1338760. doi: 10.3389/fpubh.2024.1338760
Edited by:
Mark Servis, University of California, Davis, United StatesReviewed by:
Clement Dubost, Hôpital d'Instruction des Armées Bégin, FranceSabina Krupa, University of Rzeszow, Poland
Sandra Lange, Medical University of Gdansk, Poland
Copyright © 2024 Ayanaw Eyayu, Gudayu Zeleke, Chekol, Yaregal Melesse and Enyew Ashagrie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Henos Enyew Ashagrie, aGVueWVueTExQGdtYWlsLmNvbQ==
 Ruth Ayanaw Eyayu
Ruth Ayanaw Eyayu Wubie Birlie Chekol
Wubie Birlie Chekol Debas Yaregal Melesse
Debas Yaregal Melesse Henos Enyew Ashagrie
Henos Enyew Ashagrie