- Department of Population Medicine, Ontario Veterinary College, University of Guelph, Guelph, ON, Canada
Effective and precise public health practice relies on a skilled and interdisciplinary workforce equipped with integrated knowledge, values, skills, and behaviors as defined by competency frameworks. Competency frameworks inform academic and professional development training, support performance evaluation, and identify professional development needs. The aim of this research was to systematically identify and examine trends in the extent, nature, and range of the literature related to developing competencies in public health. This includes developing public health competency frameworks, and how competencies are developed and maintained in students and practitioners. We used a scoping review methodology to systematically identify and report on trends in the literature. Two independent reviewers conducted title and abstract and full-text screening to assess the literature for relevance. Articles were included if they were original primary research or gray literature and published in English. No date or geographic restrictions were applied. Articles were included if they focused on developing competency statements or frameworks for public health and/or training public health students or practitioners to develop competencies. The review encompassed a range of methods and target populations, with an emphasis on building competencies through student and professional development. Foundational competency development was a primary focus, and we found a gap in discipline-specific competency research, especially within developing discipline-specific competency statements and frameworks. Several evidence-based practices for competency development were highlighted, including the importance of governance and resources to oversee competency framework development and implementation, and workforce planning. Experiential learning and competency-based training were commonly identified as best practices for building competencies. A comprehensive understanding of public health competency development—through developing and incorporating foundational and discipline-specific competencies, mapping student and practitioner training to competency frameworks, and incorporating best practices—will enable public health to create skills and an adaptable workforce capable of addressing complex public health issues.
1 Introduction
Health professionals require a specific set of skills, values, and knowledge–commonly referred to as core competencies–to be highly effective in their respective sectors. Core competencies represent a baseline standard of the knowledge, skills, and attitudes required among professionals in the field (1). Competency statements and frameworks are generated by allied health organizations and regulatory bodies globally, including core competencies for incoming medical students (2), entry-to-practice competencies for registered nurses (3, 4), core competencies for clinical pharmacists (5), and professional competencies for veterinarians (6, 7). While they vary across professions, these competencies encompass a set of agreed-upon interpersonal, clinical, scientific, and logical reasoning skills, values, and knowledge that practitioners should exhibit.
Specific to public health, competency statements and frameworks exist across public health organizations and institutions internationally. Governing bodies in Canada (1), the United States (8), the United Kingdom (9), the European Union (10), and Australia (11) have all released competency frameworks to guide public health workforce planning. Although each framework differs in its content and context, they all aim to strengthen the public health sector’s ability to prepare for and respond to public health challenges-- today and in the future (12).
Core competencies provide standards for training the public health workforce (1, 8, 12). These frameworks can inform academic and professional development curricula (1), assess workforce performance (13), and identify professional development needs. Core competencies can also help public health organizations maintain consistency, identify program needs, and help facilitate interdisciplinary work (1, 8). Competency statements and frameworks can ensure public health practitioners have a shared understanding of their roles and responsibilities and that they are working toward a common goal of contributing to a healthier population (1).
Competency frameworks can become outdated as workforce needs evolve in response to changing population health demands. As such, there have been global calls (14–16) to strengthen and transform the public health workforce to adapt to evolving public health challenges like the COVID-19 pandemic (17), climate change (18), and economic inflation (17). In Canada, the Canadian Public Health Association (CPHA) explicitly called on the government to refresh their public health core competency framework to encompass these challenges (14). Further, Canada’s Chief Public Health Officer called for modernized and improved core competencies and curriculum in graduate public health education, and transformation of the public health workforce to better address complex public health challenges such as climate change and the COVID-19 pandemic (16, 18).
Competency-based education and training guide curriculum planning, accreditation, and performance evaluation to enhance outcomes of public health practice (19, 20). Further, competency frameworks bridge the gap between evidence and practice and allow for interdisciplinary skill set development (12, 21). Flexible learning, mentorship, and feedback are key factors in effective competency-based education in healthcare (20). Experiential learning, practice-based learning, and reflective practices are also effective pedagogical practices for developing competencies in public health students (22). In Canada, graduate-level training matched to public health competencies is especially important given the lack of a national, comprehensive competency training program (23).
As Canada and other countries around the world begin to transform their public health workforce, agencies must draw on evidence-based practices for building competencies. There are currently gaps in understanding best practices for developing, implementing, and evaluating public health competency frameworks, and there are no published reviews that capture the breadth of this process. Related research has described the process for developing public health competency frameworks including the need for transparent reporting, validated instruments, and consensus-building approaches (24), but no such reviews exist examining the full scope of research on building competencies in public health. Thus, there is a need for synthesized results to inform evidence-based practices related to developing public health competencies going forward.
The aim of this research is to systematically identify and examine trends in the extent and nature of the literature related to developing competencies in public health. The scope includes developing public health competency frameworks, and identifying how competencies are developed and maintained in students and practitioners. The objectives of this research are:
1. To conduct a scoping review of the relevant literature regarding developing competencies in public health; and,
2. To report on trends in the extent and nature of the literature identified.
2 Materials and methods
This scoping review followed the framework by Arskey and O’Malley (25), and updated by Levac et al. (26) to examine the extent, nature, and range of research related to developing public health competencies. Initially, the review intended to focus on health communication competencies; however, the literature was limited in this area, so the review reflects the full range of developing public health competencies. This research adheres to the PRISMA for Scoping Reviews reporting guidelines (27).
2.1 Search strategy
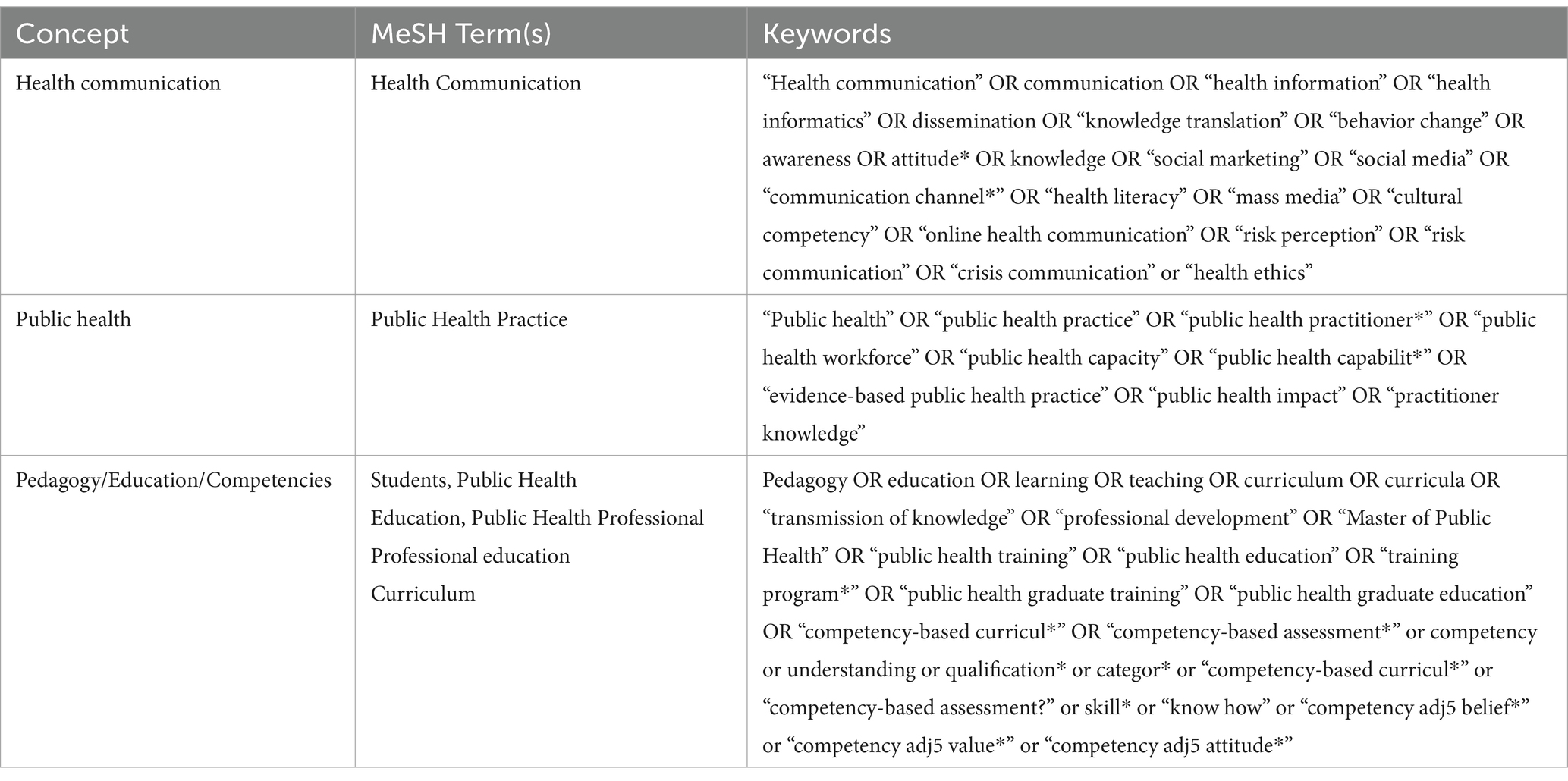
A comprehensive search strategy was developed by the research team in collaboration with a Specialist Librarian from the University of Guelph. The search contained three concepts: health communication, public health, and pedagogy/education/competencies (Table 1). The search was piloted in Ovid via MEDLINE, as well as by screening the reference lists of relevant articles. Six databases were searched including Ovid via MEDLINE, PsycINFO, Web of Science, Communication and Mass Media Complete, ERIC, and CAB Direct to identify relevant literature. The search was conducted on November 24, 2022. The search was verified by hand searching the following journals, which were most often cited in the database search results: Journal of Public Health Management & Practice, American Journal of Public Health, Journal of Health Communication, Health Promotion Practice, and Health Communication.
Using appropriate combinations of concepts and keywords, Google was also searched to identify relevant gray literature. The first 10 pages were searched for each of the following keyword/phrase combinations: “public health” AND core competencies, core competencies AND “public health workforce,” core competencies AND “public health students,” and teaching and learning AND “public health.”
All citations obtained in the database and gray literature search were downloaded to Mendeley (28), where the deduplication tool was used. The deduplicated references were then uploaded into DistillerSR (29) to manage the screening and data extraction processes.
2.2 Study inclusion criteria
To be included, literature had to be published in English from any location, and focused on competency development in public health practitioners and/or students Literature also had to focus on developing competency statements or frameworks for public health and/or training public health practitioners or students to develop competencies. No date restrictions were used, and original primary research and gray literature were included.
Studies were excluded if they focused on competency development in other disciplines (e.g., nursing, medicine, dentistry, etc.) unless it was public health competency-focused (e.g., public health nursing). Research on public health interventions aimed at individuals, communities, groups, etc. that did not feed into knowledge about effective training or education of students and the workforce were also excluded. Finally, descriptive studies about a public health program, training opportunity, or workshop without some basis in program development theory or frameworks were excluded.
2.3 Study selection
Two researchers conducted a pilot test before screening began. Articles were screened in two stages by two independent reviewers. First, the title and abstracts of each article were screened for relevance to the inclusion criteria using a structured form. Kappa was 0.81 for this screening stage, indicating high agreement (30). All conflicts were resolved through discussion.
Next, the full text of articles found to be potentially relevant to this review were independently screened by the same reviewers. Several steps were taken to obtain the full text of all articles if they were not available through traditional means including searching the University of Guelph Library, using Google and Google Scholar, and contacting the researcher directly via ResearchGate and/or their institutional email if available. Articles were screened using a structured form that contained the following criteria: literature type, language, population, measurement, evaluation, or detailed report of competency statement or framework development in public health students and/or the workforce. Kappa was 0.80 for this stage of screening, indicating high agreement (30), and all conflicts were resolved through discussion.
2.4 Data extraction and analysis
This review focused on mapping prominent trends in developing competencies in public health, including competency frameworks and competency development in students and practitioners. The data extraction form was developed by the lead researcher, piloted by the two independent reviewers, and finalized by the research team prior to data extraction. The following fields were extracted using a structured form in DistillerSR: title, author(s), year, article type, country/region of origin, study design, study aim, methods, theories or frameworks included, pedagogy identified, institutions involved in the research, institutions involved in the professional or student training, existing competency frameworks included, focus of competency development (e.g., developing a competency framework, workforce development, student development), focus of competency framework (e.g., general or discipline-specific), target population (e.g., graduate student, general public health practitioner), focus of practitioner or student training, focus on public health communication, recommendations for improved competency development, bias identified, and future research directions.
The dataset was split in half so that the two reviewers were each the primary extractors for half and verified the other half. The recommendations for improved competency development were captured deductively based on a related review (24), and inductively to capture approaches for developing competencies in public health practitioners and students found in the included literature. The inductively captured approaches were analyzed by uploading the open text responses into NVivo Plus 12 (31) and conducting an automatic thematic analysis. Codes with multiple references were explored by the lead researcher to generate overall promising approaches for developing competencies and were verified by a second researcher and the research team.
Descriptive statistics demonstrate the trends in the collected information relevant to the review aim. Microsoft Excel (Microsoft, Redmond, USA) was used to analyze and visualize the data.
3 Results
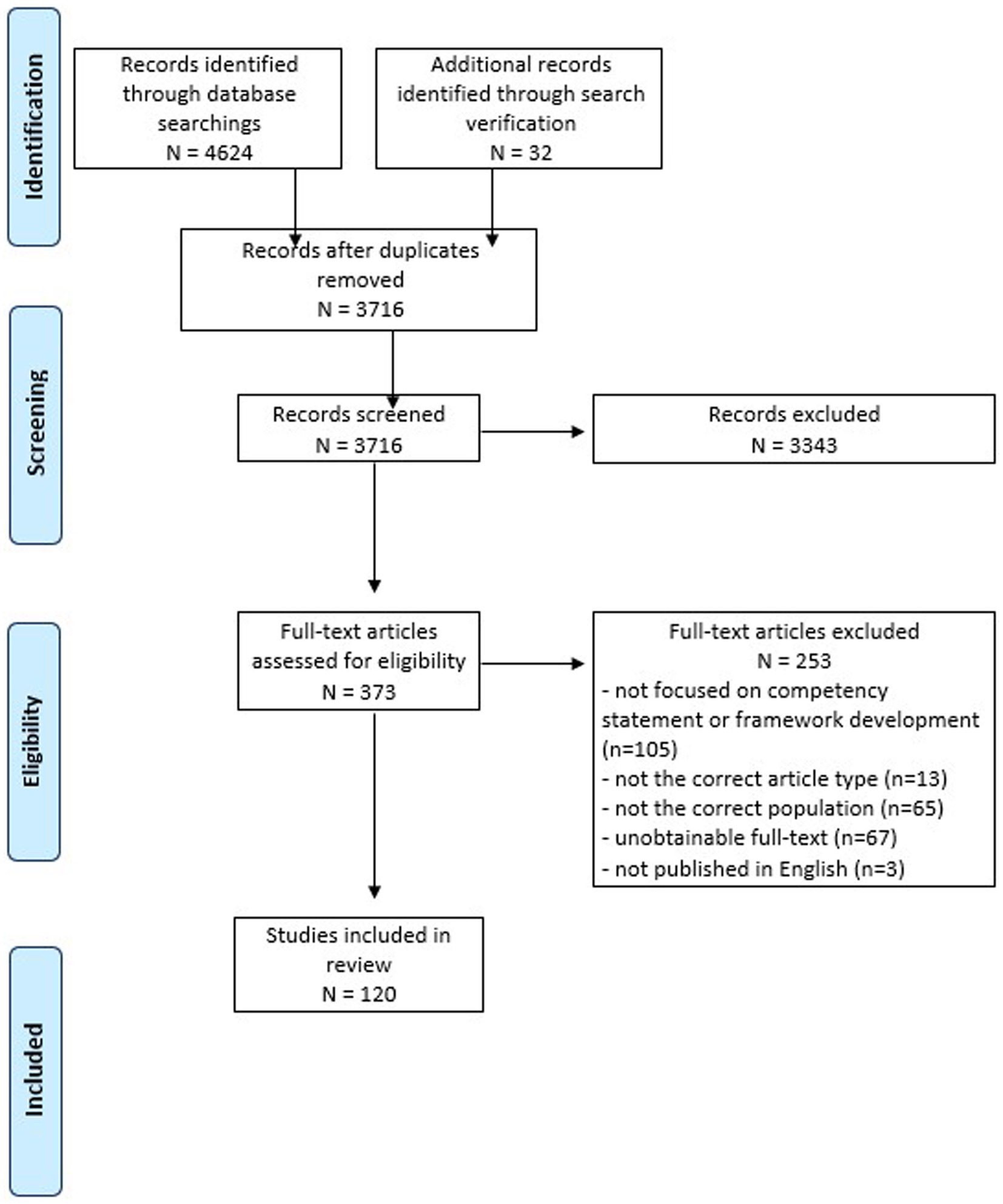
The search identified 3,716 articles after deduplication and a total of 120 articles met the inclusion criteria and underwent data extraction and analysis (Figure 1). Generally, articles either described the development of competency statements and frameworks or the development of competencies through training and professional development.
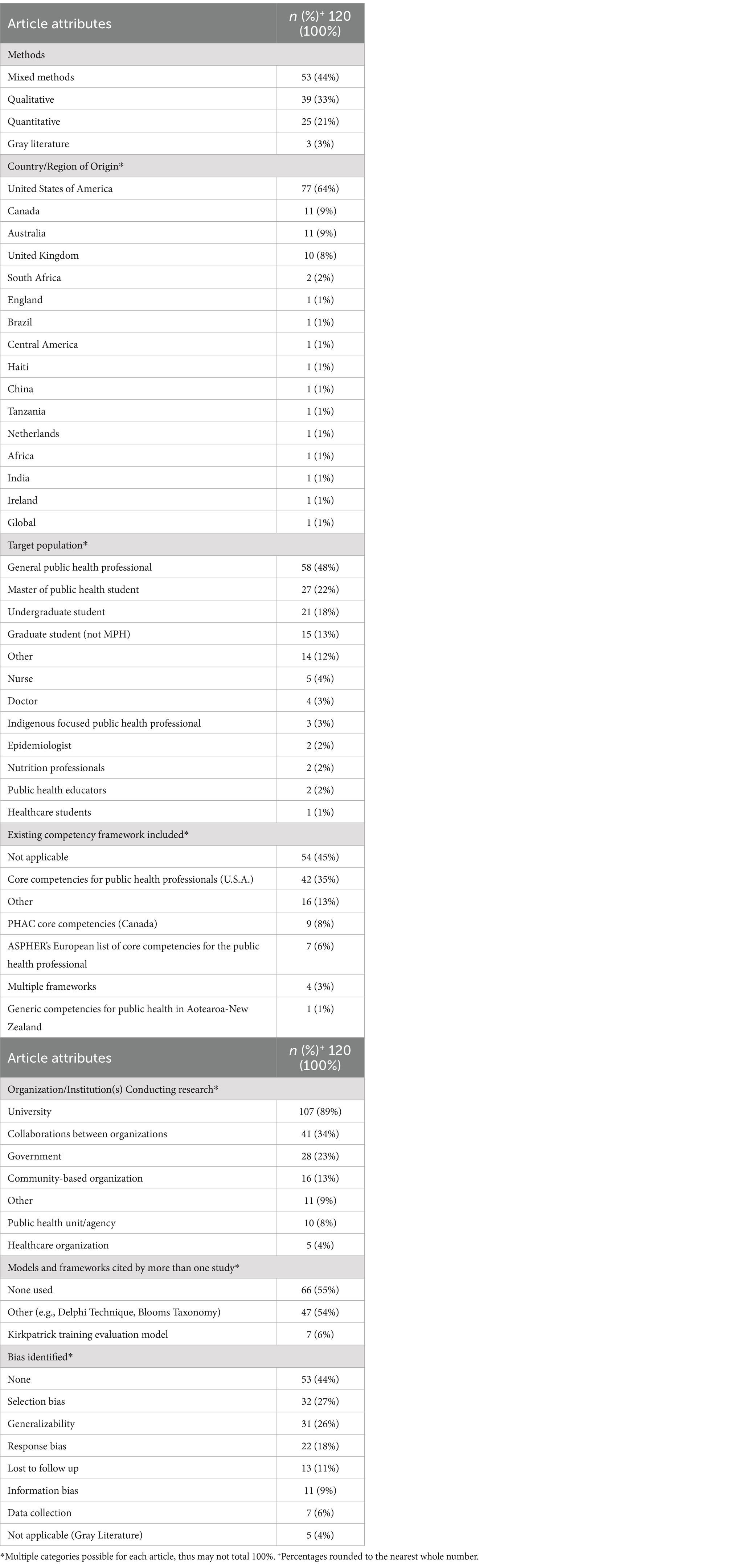
Most included articles used mixed method designs (44%) and were conducted in the United States of America (64%) (Table 2). Supplementary Table S1 provides the authors, year, article title, and study details of all the included literature (n = 120). General public health practitioners (48%), followed by Master of Public Health (MPH) students (22%), were the common target populations for the included articles. Other public health practitioners commonly cited (12%) include public health leaders, environmental public health practitioners, public health nurses, public health nutritionists, and Indigenous health workers. Universities (89%) conducted most of the included research, followed by collaborations between the cited institutions and organizations (e.g., universities and governments) (34%). Other organizations (9%), including research funders and networks, government-funded and/or operated training centers, and consultants also conducted the research. Existing competency frameworks were often not included (45%) in the articles, but when they were, the framework by the US Core Competencies for Public Health Professionals (35%) was the most frequently incorporated. Finally, bias was not identified (44%) in some studies; however, other studies cited participant bias (27%).
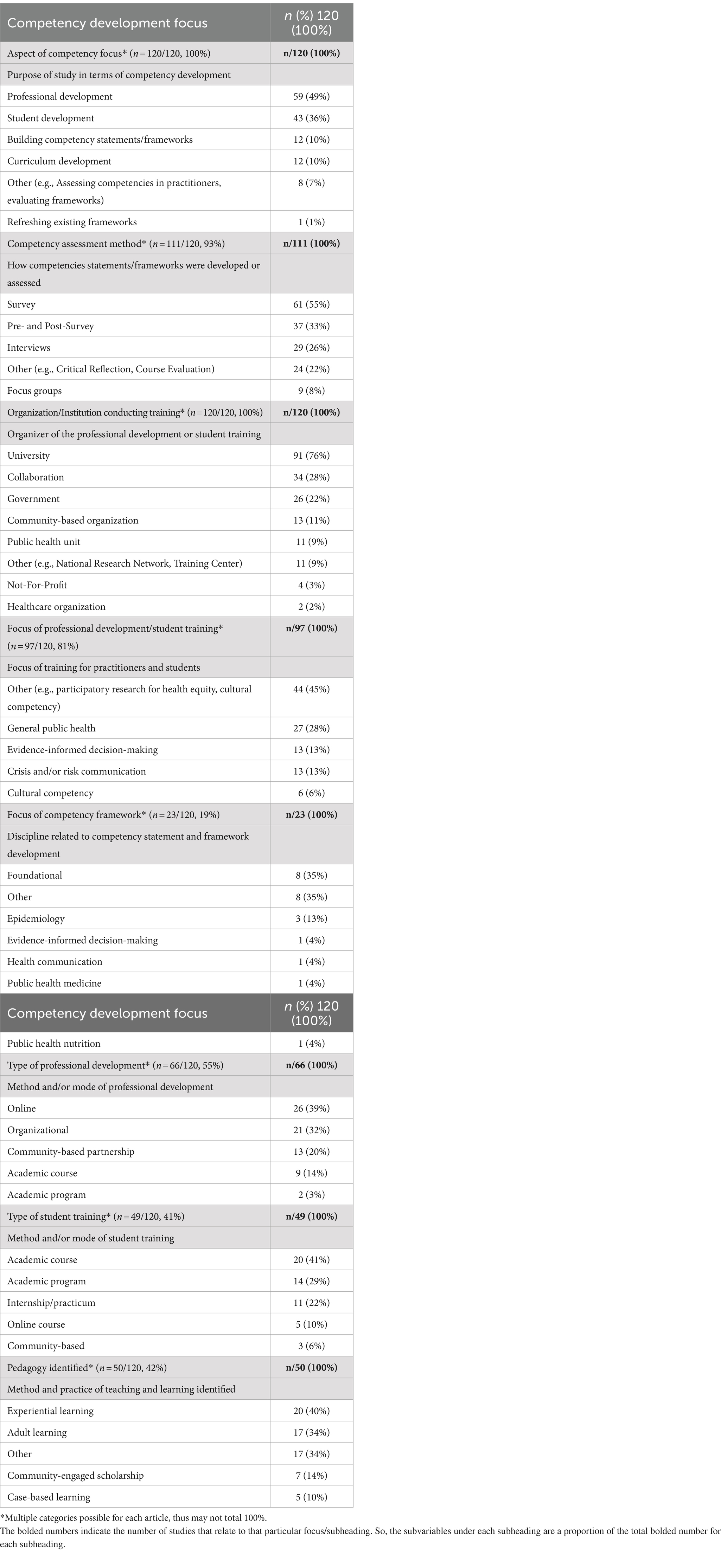
Table 3 describes the range of competency development work in public health from building competency statements and frameworks to student education and professional training. Professional development (49%) was often the focus of the included literature, followed by developing competencies in public health students (36%). Of the studies that assessed competencies, general surveys (55%) and pre- and post-surveys (33%) were employed as a step within building competency frameworks, as well as to assess self-rated competency changes after student and professional training. Universities (76%) were the institutions that most commonly conducted training in the included articles; however, collaborations (28%) between cited institutions and organizations were also common. Other organizations (9%) who participated in developing and conducting training included federally funded organizations and consultants. Of the studies that included professional development/training opportunities, some are conducted online (39%) and focused on a variety of other topics (45%) including cultural competency, health equity and literacy, and epidemiology. When student training was the focus, it was often centered within an academic course (41%) and incorporated experiential learning (40%). Articles that focused on development of competency statements and frameworks are limited (10%), but when present are focused on foundational competencies, epidemiology, leadership, and other discipline-specific areas. One article (1%) focused on refreshing an existing competency framework.
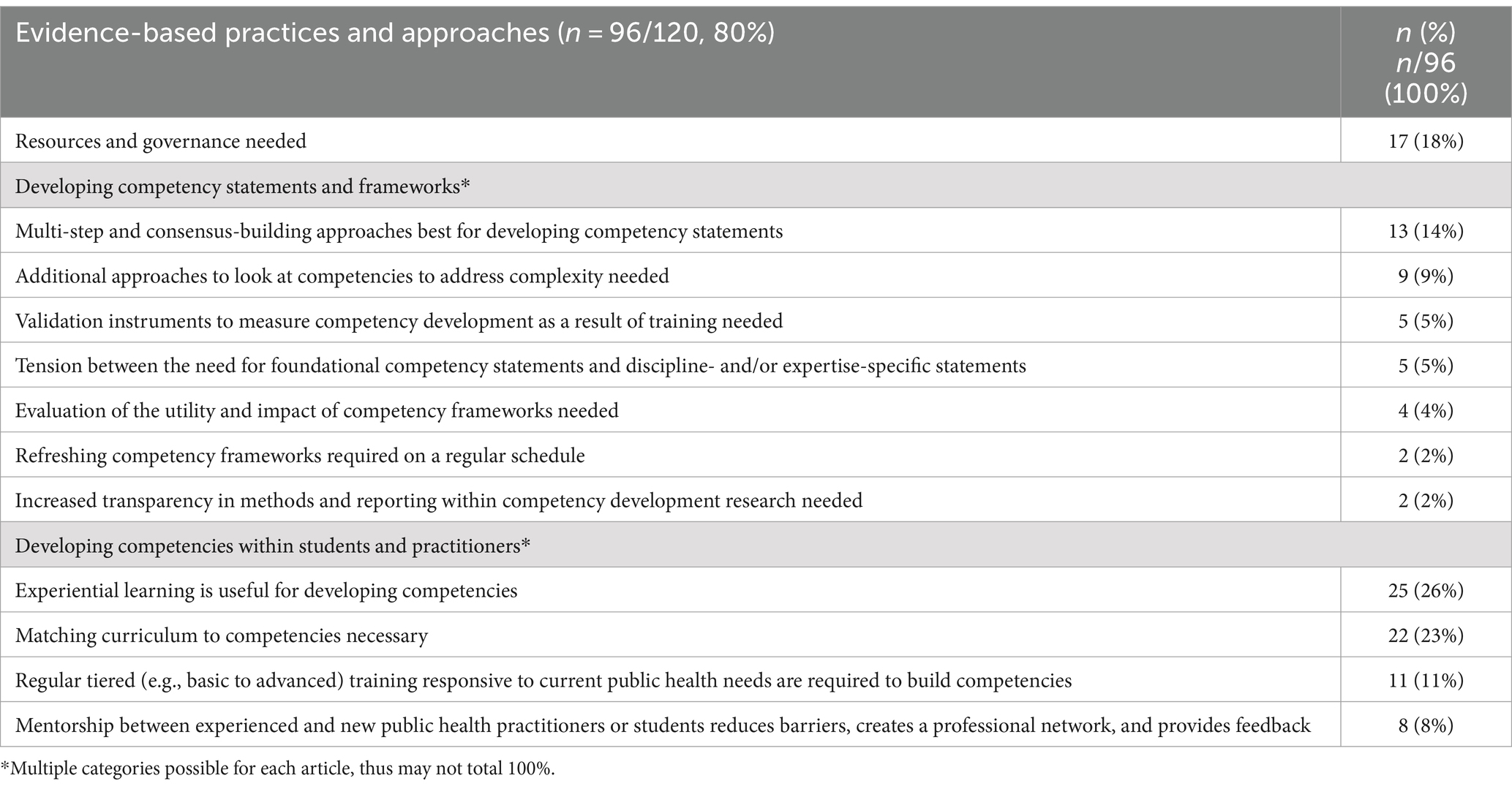
Evidence-based practices and recommendations for developing competency frameworks and for building competencies within public health students and practitioners are identified (Table 4). Of the studies that identified evidence-based practices and approaches, the need for governance and resources to oversee competency framework development, refreshing, implementation across the workforce, and evaluation are included (18%). Multi-step and consensus-building approaches (14%) are recommended by studies that focused on building competency statements and frameworks, followed by a call for additional approaches to address complex public health issues (e.g., health inequities, Indigenous health). Experiential learning (26%), including practicum and community-based learning, was found to be best for developing competencies in public health students and practitioners. Matching training curricula to competencies (23%) was also found to be an effective practice for developing competencies in public health students and practitioners.
4 Discussion
Effective public health practice requires a skilled interdisciplinary public health workforce. Competencies describe the integrated knowledge, values, skills, and behaviors required for practitioners and organizations across the practice of public health (1, 8, 10, 16, 32). Competency frameworks allow for workforce planning and development, including identifying gaps in training, evaluating performance, and developing professional development opportunities (32). Key components in developing the public health workforce include developing competency-based curricula and a comprehensive and coordinated lifelong learning system (33). Understanding successes, shortfalls, and lessons learned from previous literature on competency development is important for developing a strong public health workforce going forward. However, the lack of consistency in methods across the body of literature on this topic, the focus on foundational competencies and general practitioners, along with limited reporting on best practices, may make it challenging for public health researchers and organizations to develop competencies effectively and efficiently within the workforce.
The included literature was divided into literature that describes how competency statements and frameworks have been developed and refreshed (n = 13, 11%) and literature describing how to develop competencies within public health students and practitioners (n = 107, 89%). Studies were most often mixed methods research conducted in the United States by academia and spanned various target populations within public health students and professionals. Most of the included literature focused on building competencies through student and professional development, with the former most often offered through academic courses and the latter most often offered online. Surveys, including pre- and post-surveys, are used for self-assessment of competency development among students and practitioners. The included literature had a limited focus on approaches and best practices for developing competency statements and frameworks. Within the relevant literature, experiential and adult learning were the most applied pedagogical approaches.
4.1 Competency literature focused on a general public health audience and foundational competencies
The focus on foundational and core competencies is necessary to provide the cross-cutting knowledge, values, and skills integrated by a practitioner to perform broad functions across public health (34). These studies provide the basis by which practitioners and students can engage in critical thinking and reflection and allow for the development of more advanced and discipline-specific knowledge, values, skills, and behaviors (35). Thus, as more is understood about developing core competency frameworks and foundational competencies across the workforce, discipline-specific competency frameworks and training programs that support depth in knowledge, skills, and behaviors can be built more efficiently.
Specific public health audiences varied across the included literature, with the majority focusing on general public health practitioners. The public health workforce is comprised of practitioners who engage in public health work as the primary part of their role (33). Within the public health workforce, there are diverse disciplines and professional backgrounds that require unifying competencies and professional development to ensure optimal individual and organizational performance (14). A focus on general public health practitioners provides the evidence-base required for understanding and applying best practices for workforce development across the public health system.
Similarly, most of the literature focused on approaches for developing foundational or core competency frameworks, and professional development across foundational competencies. There was an overall lesser focus on professional development on the topics of cultural competency, evidence-informed decision-making, crisis and risk communication, epidemiology, and public health leadership. However, discipline-specific competencies, coupled with foundational competencies are necessary to address complex and multifaceted public health issues including social determinants of health, health equity, and climate change (36, 37).
4.2 Gaps exist in competency research including a limited focus on discipline-specific competency research
The modest amount of discipline-specific competency research uncovered in the current review was mainly in the realm of professional development, including a focus on health equity, health literacy, epidemiology, evidence-informed decision-making, crisis and risk communication, and cultural competency. System-level improvement requires developing and maintaining a trained public health workforce. Key aspects of providing effective professional development include mapping competencies to curricula and understanding training gaps in the workforce (38). A recent study identified communication, change management, budgeting, and reporting as gaps in the U.S. public health workforce (39). Similarly, communication was identified as a gap among Israeli public health practitioners, along with responding to current and emerging public health issues (38). However, studies examining competency gaps in public health practitioners at the country level are limited. An understanding of the strengths and gaps in public health competencies both today and in the future is required to be able to map professional development opportunities, such as in public health communication, to strengthen the workforce.
Further, few included studies focused on discipline-specific competency statements and framework development. Both foundational and discipline-specific competencies are necessary to provide the cross-cutting knowledge, values, skills, and behaviors necessary for core public health functions. Public health encompasses a range of disciplines and backgrounds and requires not only a grounding foundational set of competencies, but also discipline-specific competencies used by public health specialists (12). Key public health disciplines requiring a specialized competency framework through which the foundational competencies are integrated include epidemiology, infectious disease, global health, nursing, communication, and others (40). Additional literature on developing discipline-specific competency frameworks, including health communication competencies, and competency-based training would add to our understanding of additional professional development and workforce planning requirements across the public health workforce.
Within the literature on developing competency statements and frameworks, gaps were also identified related to the trustworthiness of the research. More than half the included literature emphasized the need for validated instruments to measure change in competencies as a result of education or professional development to increase the trustworthiness of research. Further, studies reporting on competency statements and framework development should aim to increase their transparency to allow for replication and the ability to better contextualize and understand the results. Recent recommendations for reporting competency framework development in health professions (CONFRED-HP) echo this as demonstrated by the inclusion of a number of key items related to transparency in their checklist (41). Finally, evaluation of the utility and impact of competency frameworks is lacking and should be undertaken to better understand how to develop frameworks that meet the needs of public health organizations. Very few evaluations of public health competency frameworks exist, but those that do provide an important contribution to related literature and workforce development (42). Evaluation and implementation are also areas of focus within the CONFRED-HP checklist to support this key recommendation (41).
4.3 Evidence-based practices and approaches for competency development point toward a need for resources, governance, and real-world application
Several best practices and approaches for public health competency development were found in the included literature. The need for resources and governance to oversee competency framework development, revitalization, and workforce planning was commonly identified. Governance of competency frameworks by federal governments is needed to provide oversight and resources for public health workforce planning and development and to ensure equal access to an effective workforce for all communities. In Canada, the Canadian Public Health Association and others have called on the federal government to create a new Public Health Act that supports public health, oversees competency framework development and implementation, and provides resources to the system (14, 43). In the United States, the Council on Linkages between Academia and Public Health Practice is comprised of 24 national organizations that collaborate to support public health competence development in the workforce (44). Governance ensures competency frameworks stay up to date, are incorporated into practice, are adequately financed, and are mapped to professional development opportunities. Ensuring the public health workforce has modern competencies to fulfill its functions requires dedicated resources and an interdisciplinary and collaborative governance structure to oversee the renewal, implementation, and evaluation of competency frameworks.
Multi-step and consensus-building approaches for developing competency statements and frameworks in public health are identified as best practices by all the related included literature. The Delphi technique is a method often used for competency framework development to gain consensus from a group of experts (45). Delphi techniques contain a number of rounds that may include expert consultation, surveys, interviews, and focus groups, depending on the literature in the area and the number of rounds required for consensus or agreement. There are no specific recommendations on the number of rounds or the order of methods included in Delphi technique; however, it is clear that a multi-step process that builds consensus is key to ensure rigor (45, 46).
Within competency development for public health students and practitioners, experiential learning and curriculum-based training were commonly identified as evidence-based practices. Experiential learning provides real-world public health experiences as a means of developing competencies beyond the classroom and is often incorporated in practicums, capstone courses, and sometimes within individual courses and assessments (47, 48). Experiential learning centers practical experiences within the education, allowing for the integration of knowledge, values, skills, and behaviors (47). Further, competency-based training embeds competencies within the curricula, assessments, and structure of the training opportunity. Competency-based education and training complements experiential learning through orienting the application of knowledge, values, skills, and behaviors in the real world (49). Importantly, it also accelerates graduate’s to job readiness, thereby enhancing public health capacity. The focus on the real-world application of competency-based education and training and experiential learning bridges the gap between the public health workplace, evidence, and the education or training setting (49).
4.4 Limitations and future research
With regards to the included literature, selection bias and generalizability of results were identified within the included literature as the most common biases. These biases can threaten the validity of the research and impact the generalizability of findings.
Within the methods used to conduct the scoping review, limitations also exist including the selection of databases. Language bias is also present as included articles needed to be in English.
Future research using robust mixed methods to assess how competencies are developed and the best instrument to measure changes in competencies reliably and efficiently is needed. Additional research on developing, implementing, and evaluating discipline-specific competency frameworks is also needed. With regards to experiential learning, additional evaluation of various opportunities in public health should be conducted to increase the validity of findings and contribute to an increased understanding of best practices.
5 Conclusion
This scoping review highlights the importance of competency frameworks and professional development in improving public health practice and developing a skilled, interdisciplinary public health workforce. Competency frameworks are essential tools for workforce planning and development, including identifying training gaps, evaluating performance, and creating professional development opportunities. Much of the included literature focused on foundational competency framework development and professional development for general public health practitioners. While this provides an important broad understanding of the essential competencies needed, there is a gap in discipline-specific research. Public health is a diverse field comprising a range of disciplines that require competency development and frameworks for specialized areas of practice. This review also highlights several best practices for competency development, including the importance of governance and resources to oversee competency framework development and workforce planning, as well as experiential learning and competency-based training for students and practitioners.
Author contributions
MM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CF: Writing – review & editing, Formal analysis, Investigation, Validation. LG: Funding acquisition, Validation, Writing – review & editing. AP: Conceptualization, Funding acquisition, Validation, Writing – review & editing. JM: Writing – review & editing, Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Funding for this research was provided by the Canadian Institutes for Health Research (CIHR) in the form of a CIHR Catalyst Grant (FRN 184647).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1332412/full#supplementary-material
References
1. Public Health Agency of Canada. (2008). Core competencies for public health in Canada: Government of Canada. Available at:https://www.canada.ca/content/dam/phac-aspc/documents/services/public-health-practice/skills-online/core-competencies-public-health-canada/cc-manual-eng090407.pdf
2. Association of American Medical Colleges. (2017). Anatomy of an applicant: competency resources and self-assessment guide for medical school applicants. Available at:https://students-residents.aamc.org/media/10606/download
3. Nursing & Midwifery Council. (2014). Standards for competence for registered nurses. Available at:https://www.nmc.org.uk/globalassets/sitedocuments/standards/nmc-standards-for-competence-for-registered-nurses.pdf
4. Ontario College of Nurses of Ontario. (2023). Entry-to-practice competencies for registered nurses. Available from: https://www.cno.org/globalassets/docs/reg/41037-entry-to-practice-competencies-2020.pdf
5. Saseen, JJ, Ripley, TL, Bondi, D, Burke, JM, Cohen, LJ, McBane, S, et al. ACCP clinical pharmacist competencies. Pharmacotherapy. (2017) 37:630–6. doi: 10.1002/phar.1923
6. American Association of Veterinary Medical Colleges. (2010). Core competency multi-species clinical expertise. Available at:http://www.aavmc.org/assets/data-new/files/NAVMEC/NAVMECCoreCompetencies.pdf
7. Ontario Veterinary College. Professional competencies of Canadian veterinarians: a basis for curriculum development. Guelph: University of Guelph (1996).
8. Public Health Foundation. (2023). Core competencies for public health professionals: domains. Available at:https://www.phf.org/programs/corecompetencies/Pages/Core_Competencies_Domains.aspx
9. Office for Health Improvement & Disparities. GOV.UK. (2023). Public Health Skills and Knowledge Framework: August 2019 Update. Available at:https://www.gov.uk/government/publications/public-health-skills-and-knowledge-framework-phskf/public-health-skills-and-knowledge-framework-august-2019-update
10. World Health Organization. WHO-ASPHER competency framework for the public health workforce in the European region. Copenhagen, Denmark: WHO Regional Office for Europe (2020).
11. Council of Academic Public Health Institutions of Australia. (2016). Foundation competencies for public health graduates in Australia. Available at:https://caphia.com.au/wp-content/uploads/2016/07/CAPHIA_document_DIGITAL_nov_22.pdf
12. Hunter, MB, Ogunlayi, F, Middleton, J, and Squires, N. Strengthening capacity through competency-based education and training to deliver the essential public health functions: reflection on roadmap to build public health workforce. BMJ Glob Health. (2023) 8:e011310. doi: 10.1136/bmjgh-2022-011310
13. Al Jabri, YM, Kvist, T, Azimirad, M, and Turunen, H. A systematic review of healthcare professionals’ core competency instruments. Nurs Health Sci. (2021) 23:87–102. doi: 10.1111/nhs.12804
14. Canadian Public Health Association. Strengthening public health Systems in Canada. Ottawa, Canada: Canadian Public Health Association (2022).
15. Centers for Disease Control. (2022). Strengthening the Population & Public Health Workforce Pipeline. Available at:https://www.cdc.gov/apih/workforce/index.html
16. Public Health Agency of Canada. (2021). A vision to transform Canada’s public health system: chief public health officer’s report on the state of public health in Canada 2021. Available at:https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/state-public-health-canada-2021.html
17. Centers for Disease Control. (2022). National workforce capacity to implement the essential public health functions including a focus on emergency preparedness and response. Available at:https://www.who.int/publications/i/item/9789240050402
18. Government of Canada. (2022). Mobilizing public health action on climate change in Canada: chief public health officer’s report on the state of public health in Canada 2022. Available at:https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/state-public-health-canada-2022/report.html
19. Calhoun, JG, Wrobel, CA, and Finnegan, JR. Current state in U.S. public health competency-based graduate education. Public Health Rev. (2011) 33:148–67. doi: 10.1007/BF03391625
20. Imanipour, M, Ebadi, A, Monadi Ziarat, H, and Mohammadi, MM. The effect of competency-based education on clinical performance of health care providers: a systematic review and meta-analysis. Int J Nurs Pract. (2022) 28:e13003. doi: 10.1111/ijn.13003
21. Scharff, DP, Rabin, BA, Cook, RA, Wray, RJ, and Brownson, RC. Bridging research and practice through competency-based public health education. J Public Health Manag Pract. (2008) 14:131–7. doi: 10.1097/01.PHH.0000311890.91003.6e
22. Pham, CN, Cunningham, SD, and Humphries, DL. Action learning and public health pedagogy: student reflections from an experiential public health course. Front Public Health. (2023) 11:1128705. doi: 10.3389/fpubh.2023.1128705
23. Apatu, E, Sinnott, W, Piggott, T, Butler-Jones, D, Anderson, LN, Alvarez, E, et al. Where are we now? A content analysis of Canadian master of public health course descriptions and the public health agency of Canada’s core competencies. J Public Health Manag Pract. (2021) 27:201–7. doi: 10.1097/PHH.0000000000001173
24. MacKay, M, Ford, C, Grant, LE, Papadopoulos, A, and McWhirter, JE. Developing public health competency statements and frameworks: a scoping review and thematic analysis of approaches. BMC Public Health. (2023) 23:2240. doi: 10.1186/s12889-023-17182-6
25. Arksey, H, and O’Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
26. Levac, D, Colquhoun, H, and O’Brien, KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
27. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
28. Mendeley. (2023). Mendeley reference manager. Available at:https://www.mendeley.com/reference-management/reference-manager
29. DistillerSR. (2023). Smarter reviews: trusted evidence. Available at:https://www.distillersr.com/
30. McHugh, ML. Interrater reliability: the kappa statistic. Biochem Med. (2012) 22:276–82. doi: 10.11613/BM.2012.031
31. QSR International Pty Ltd. NVivo. (2020). Available at:https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
32. Centers for Disease Control. Public Health Professionals Gateway. (2023). Competencies for public health professionals. Available at:https://www.cdc.gov/publichealthgateway/professional/competencies.html
33. Otok, R, Richardson, E, Czabanowska, K, and Middleton, J. (2018). The public health workforce. In: Organization and financing of public health services in Europe. European observatory on health systems and policies. Available at:https://www.ncbi.nlm.nih.gov/books/NBK535727/
34. Public Health Foundation. (2021). Revision of the Core Competencies for Public Health Professionals. Available at:http://www.phf.org/programs/corecompetencies/Pages/2021_Revision_of_the_Core_Competencies_for_Public_Health_Professionals.aspx
35. Makhene, A. Use of foundational knowledge as a basis to facilitate critical thinking: nurse educators’ perceptions. Nurs Res Pract. (2022) 2022:1–7. doi: 10.1155/2022/3736322
36. de Beaumount Foundation. (2021). Adapting and aligning public health strategic skills. Available at:https://debeaumont.org/strategic-skills/
37. National Collaborating Centre for Determinants of Health. Do public health discipline-specific competencies provide guidance for equity-focused practice? Antigonish, NS: St Francis Xavier University (2015).
38. Bashkin, O, Otok, R, Kapra, O, Czabanowska, K, Barach, P, Baron-Epel, O, et al. Identifying the gaps between public health training and practice: a workforce competencies comparative analysis. Int J Public Health. (2022) 67:1605303. doi: 10.3389/ijph.2022.1605303
39. Taylor, HL, and Yeager, VA. Core competency gaps among governmental public health employees with and without a formal public health degree. J Public Health Manag Pract. (2021) 27:20–9. doi: 10.1097/PHH.0000000000001071
40. Harvard, T.H. (2021). Chan School of public health. Communications guide. What is public health? Available at:https://www.hsph.harvard.edu/communications-guide/what-is-public-health/
41. Batt, AM, Tavares, W, Horsley, T, Rich, JV, Williams, B, Collaborators, CONFERD-HP, et al. CONFERD-HP: recommendations for reporting COmpeteNcy FramEwoRk development in health professions. Br J Surg. (2023) 110:233–41. doi: 10.1093/bjs/znac394
42. Bornioli, A, Evans, D, and Cotter, C. Evaluation of the UK public health skills and knowledge framework (PHSKF): implications for international competency frameworks. BMC Public Health. (2020) 20:956. doi: 10.1186/s12889-020-09024-6
43. Di Ruggiero, E, Papadopoulos, A, Steinberg, M, Blais, R, Frandsen, N, Valcour, J, et al. Strengthening collaborations at the public health system–academic interface: a call to action. Can J Public Health. (2020) 111:921–5. doi: 10.17269/s41997-020-00436-w
44. Public Health Foundation. Public Health Foundation. (2023). Council on linkages between academia and public health practice. Available at:http://www.phf.org/programs/council/Pages/default.aspx
45. Taylor, E. We agree, Don’t we? The Delphi method for health environments research. HERD. (2020) 13:11–23. doi: 10.1177/1937586719887709
46. Diamond, IR, Grant, RC, Feldman, BM, Pencharz, PB, Ling, SC, Moore, AM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. (2014) 67:401–9. doi: 10.1016/j.jclinepi.2013.12.002
47. Anderson, K, Gupta, S, Nava Buenfil, F, and Verrinder, G. Using experiential learning and authentic assessments to support students to become competent health promotion practitioners. Health Promot J Austr. (2022) 33:27–34. doi: 10.1002/hpja.654
48. Chorazy, ML, and Klinedinst, KS. Learn by doing: a model for incorporating high-impact experiential learning into an undergraduate public health curriculum. Front Public Health. (2019) 7:7. doi: 10.3389/fpubh.2019.00031
Keywords: public health, competencies, competency frameworks, professional development, competency-based education, pedagogy, training
Citation: MacKay M, Ford C, Grant LE, Papadopoulos A and McWhirter JE (2024) Developing competencies in public health: a scoping review of the literature on developing competency frameworks and student and workforce development. Front. Public Health. 12:1332412. doi: 10.3389/fpubh.2024.1332412
Edited by:
Tim Sandle, The University of Manchester, United KingdomReviewed by:
Anthony Paul Breitbach, Saint Louis University, United StatesKristie Cason Waterfield, Georgia Southern University, United States
Copyright © 2024 MacKay, Ford, Grant, Papadopoulos and McWhirter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer E. McWhirter, ai5tY3doaXJ0ZXJAdW9ndWVscGguY2E=
 Melissa MacKay
Melissa MacKay Caitlin Ford
Caitlin Ford Lauren E. Grant
Lauren E. Grant Andrew Papadopoulos
Andrew Papadopoulos