
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 18 January 2024
Sec. Children and Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1323263
This article is part of the Research Topic X-raying Zero Hunger (SDG2) Targets in Africa and Other Regions: Progress, Synergies, Opportunities, and Challenges View all 9 articles
Background: Child and maternal malnutrition (CMM) caused heavy disability-adjusted life years (DALY) and deaths globally. It is crucial to understand the global burden associated with CMM in order to prioritize prevention and control efforts. We performed a comprehensive analysis of the global DALY and deaths attributable to CMM from 1990 to 2019 in this study.
Methods: The age-standardized CMM related burden including DALY and death from 1990 to 2019 were accessed from the Global Burden of Disease study 2019 (GBD 2019). The changing trend were described by average annual percentage change (AAPC). The relationship between sociodemographic factors and burden attributable to CMM were explored by generalized linear model (GLM).
Results: Globally, in 2019, the age-standardized DALY and death rates of CMM were 4,425.24/100,000 (95% UI: 3,789.81/100,000–5,249.55/100,000) and 44.72/100,000 (95% UI: 37.83/100,000–53.47/100,000), respectively. The age-standardized DALY rate (AAPC = −2.92, 95% CI: −2.97% to −2.87%) and death rates (AAPC = −3.19, 95% CI: −3.27% to −3.12%) presented significantly declining trends during past 30 years. However, CMM still caused heavy burden in age group of <28 days, Sub-Saharan Africa and low SDI regions. And, low birth weight and short gestation has identified as the primary risk factors globally. The GLM indicated that the highly per capita gross domestic product, per capita current health expenditure, physicians per 1,000 people were contributed to reduce the burden attributable to CMM.
Conclusion: Although global burden attributable to CMM has significantly declined, it still caused severe health burden annually. To strengthen interventions and address resources allocation in the vulnerable population and regions is necessary.
Despite significant progress have been achieved in improving global poverty and food security during past few decades, child and maternal malnutrition (CMM) still affects millions of women and children worldwide. It estimated that over 122 million people are experiencing hunger due to the pandemic, economic stagnation, climate change, and conflicts, with the Global Hunger Index (GHI) stands at a moderate 18.3 in 2023. Particularly, South Asia and Africa South of the Sahara are confronting severe hunger (GHI score 27.0). Africa South of the Sahara is experiencing the highest level of undernourishment at 21.7% (1). In the UNICEF-WHO low birthweight estimates for the 2023 edition, it is estimated that 19.8 million newborns were classified as low birthweight globally (2). Furthermore, 148.1 million children under the age of 5 were stunted, and 45 million were wasted (3). Previous study also highlights the significant impact on children in Sub-Saharan Africa, with a prevalence of 19.1% stunting in Senegal and 54.6% in Burundi of 2020 (4).
The World Health Assembly endorsed a comprehensive plan to reduce low birth weight, childhood stunting and wasting, anemia in women, and to increase exclusive breastfeeding during the first 6 months of life (5). However, there remains a significant gap while implementation to achieve the 2030 Sustainable Development Goal (SDG) targets. Given the current progress, it is projected that the 2030 target will be missed by 39.5 million children suffering from stunting (3). According to estimation, more than 20 million newborns are affected by low birth weight every year, and anemia rates among girls and women of childbearing age still remains worrisome. Moreover, anemia rates among women also remain high and are increasing in many countries (5). About 60% of children under the age of 5 years are anemic (with a higher proportion among children aged 6–24 months) in LMICs (6). Additionally, the prevalence of vitamin A deficiency and zinc deficiency remains stubbornly high in many regions and should not be ignored.
The evidence have shown that CMM increase the risk of negative health outcomes, causes heavy disability-adjusted life years (DALYs) and high mortality rates, particularly in low-and middle-income countries (LMICs) (7–10). It concluded that maternal malnutrition was associated with maternal anemia, mortality, brain defects, neuropsychiatric disorders, altered cognition, visual impairment, and motor deficits (2). Currently, more than half of all deaths of children under five can be attributed to malnutrition in globally (9, 10). For example, malnutrition accounts for 68.2% of total deaths in children under the age of 5 years, and also serves as the leading risk factor for health loss in all age groups, accounting for 17.3% of total DALY in India (11). In Africa, the prevalence of malnutrition among maternal was 23.5% (12), moreover, hunger is responsible for 45% of all childhood mortality (13). According to another national report from Papua New Guinea, roughly 33% of all hospital deaths among children under the age of 5 are directly or indirectly attributed to malnutrition (14).
Previous CMM studies have assessed its prevalence and trends (4, 15), its influence on health outcomes (16), associate factors (17), effective interventions (7), and the GBD-related study in specific region (11). Tracking the burden and changing trend attributed to CMM by sex, age, social development index (SDI), risk factors, and location can help countries/regions in comprehending the present status and advancements in addressing CMM-related diseases. This understanding can assist local governments, international organizations, civil society organizations and other stakeholders in identifying priorities for preventing and controlling of CMM. However, there is a lack of comprehensive studies from an integrated perspective. Therefore, this study aimed to evaluate the global burden and trends of disease attributable to CMM from 1990 to 2019.
The data of burden attributable to CMM used in this study were derived from the GBD 2019,1 which is collected and analyzed by a consortium of more than 9,000 researchers. The data are collected from various sources, including census, household surveys, civil registration, disease registration, national health service records, air pollution surveillance, satellite imaging, cause of death testing and reporting, and high-quality literature (18, 19). GBD 2019 employs comprehensive methods to quantify health losses such as years of life lost (YLLs), years lived with disability (YLDs), DALY, and death of 87 risk factors in 204 countries and territories from 1990 to 2019. The following data were included in this study: DALY and death cases, age-standardized rates of DALY and age-standardized rates of death (ASDR) attributable to CMM by sex, 5 SDI quintiles (high, high-middle, middle, low-middle, and low SDI), and 21 GBD regions.
We aggregated a list of country-level covariates hypothesized to be directly or indirectly associated with the burden of CMM, including Gross Domestic Product (GDP) per capita, current health expenditure per capita, population, urban population (% of total population), population density, and physicians per 1,000 people (20).
In GBD 2019, CMM includes six following specific risk factors: low birth weight and short gestation, child growth failure, suboptimal breastfeeding, iron deficiency, vitamin A deficiency and zinc deficiency. Low birth weight refers to any birth weight less than the population level birth weight TMREL (the birth weight that minimizes risk), and short gestation refers to all gestational ages below the gestational age TMREL. Stunting, wasting, and underweight were used to estimate child growth failure based on the growth standards for children aged 0–59 months by WHO (21). Suboptimal breastfeeding includes two distinct categories: non-exclusive breastfeeding (children under 6 months of age who are not exclusively breastfeed) and discontinued breastfeeding (children between 6 and 23 months) (22). Iron deficiency is defined as inadequate iron to meet the body’s needs (IDA women had a hemoglobin concentration lower than 115 g/L, 100 g/L for children) (23), while vitamin A deficiency is defined as serum retinol <70 μmol/L for women, 50 μmol/L for children. Zinc deficiency is defined as blood test below 0.60 mcg/mL (24).
The join-point regression model, developed by U.S Surveillance Research Program of the National Cancer Institute (25), is utilized to identify the join-point in time series data. It conducts statistical modeling and analysis to determine the timing of trend changes and the changes in slope at these points, revealing critical moments of data change and patterns of trend variation (26).
In this study, join-point regression model was used to examine the changing trend of the age-standardized DALY rate and ASDR by sex, age, SDI, specific risk factor and geographical region from 1990 to 2019. The regression model was as follow: ln (age-standardized rate of DALY or death) = α + βX + ε, where X for the calendar year (27). The average annual percentage change (AAPC) was calculated by 100 × [exp (β) − 1]. When AAPC tested significantly greater than zero, the trend was defined as increased, by the contrary, it was defined the decreased trend. Meanwhile, we used “stable” to describe non-significant AAPC trend.
Generalized Linear Model is an extension of linear models, consisting of dependent variables, linear components, and link functions, and is applied to various types of data and scenarios. In this study, the log-linear generalized linear model was used to fit the age-standardized rates of DALY and ASIR and sociodemographic factors. The details were as follows: Log (ASR) = β0 + β1 * Log per capita GDP + β2 * Log per capita current health expenditure + β3 * Urban population (% of total population) + β4 * Log Population + β5 * Log Population density + β6 * Log physicians (per 1,000 people). The best-fitting model was determined according to the Akaike information criterion (28).
Globally, there were 294,779,309 (95% UI: 252,994,742–349,534,865) DALY cases and 2,937,804 (95% UI: 2,489,636–3,512,073) death cases attributable to CMM in 2019. The global age-standardized DALY and death rates of CMM were 4,425.24/100,000 (95% UI: 3,789.81/100,000–5,249.55/100,000) and 44.72/100,000 (95% UI, 37.83/100,000–53.47/100,000), respectively (Table 1; Supplementary Table 1; Figures 1A,B).
Compared to females, males have higher age-standardized rates of DALY (4,552.18/100,000, 95% UI: 3,865.31/100,000–5,418.67/100,000) and death (46.96/100,000, 95% UI: 39.38/100,000–56.97/100,000). The <28 days age group had the highest age-standardized DALY and death rates of CMM (1,554,055.35/100,000, 95% UI: 1,322,830.84/100,000–1,845,976.9/100,000 and 17,464.36/100,000, 95% UI: 14,860.36/100,000–20,754.84/100,000; Table 1).
Maternal and neonatal disorders were the leading causes of DALY (52.47%) and death (55.95%) attributable to CMM (Supplementary Figure 1). For death, the second and third rankings were respiratory infections and tuberculosis (19.26%) and enteric infections (15.40%), respectively. For DALY, the second and third rankings were respiratory infections and tuberculosis (16.88%) and nutritional deficiencies (15.26%), respectively (Supplementary Figure 1).
In 2019, Western Sub-Saharan Africa had the highest age-standardized rates of DALY (10,333.99/100,000, 95% UI: 8,464.8/100,000– 12,698.94/100,000) and death (112.97/100,000, 91.45/100,000–139.98/100,000) of CMM followed by Eastern Sub-Saharan Africa (6,616.55/100,000 for DALY and 77.78/100,000 for death) and South Asia (6,323.59/100,000 for DALY and 59.01/100,000 for death; Table 1; Figures 1A,B).
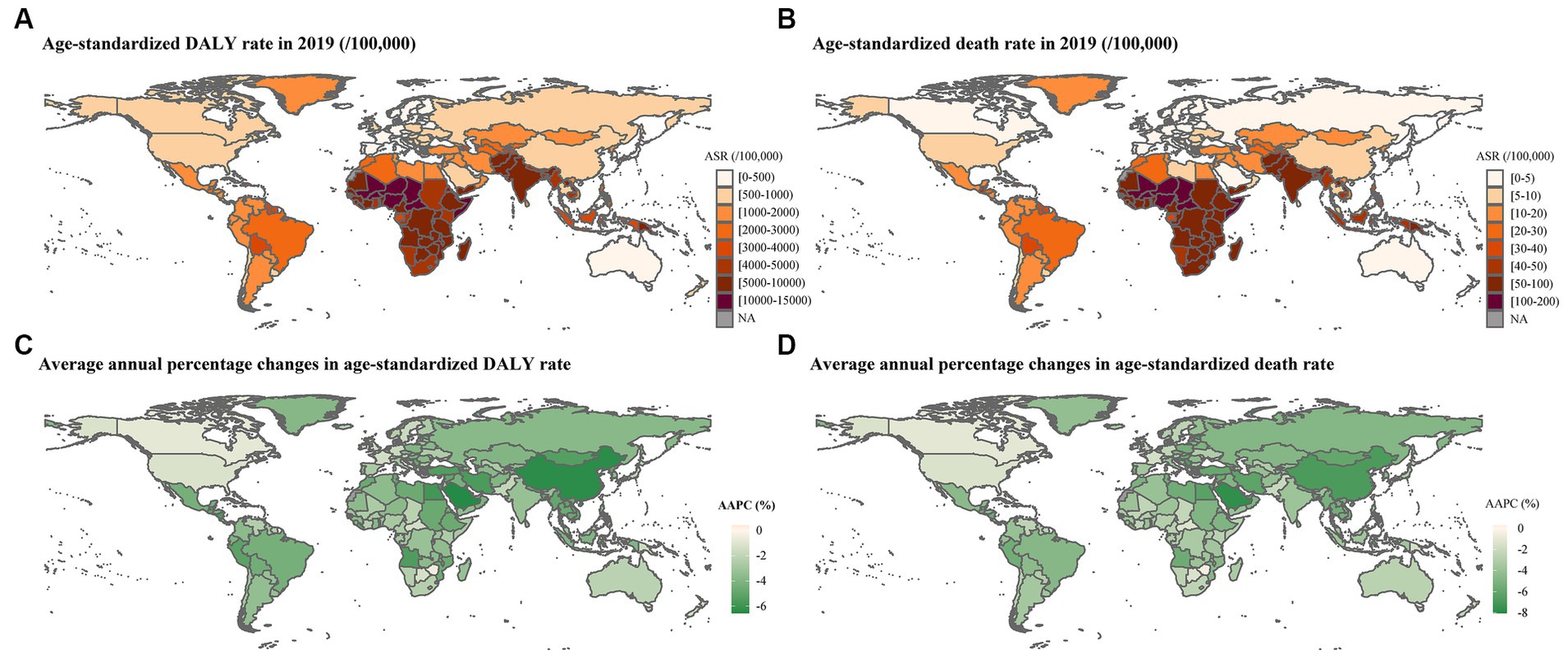
Figure 1. Global burden attributable to CMM in 2019 and average annual percentage change of age-standardized rates from 1990 to 2019. (A) Age-standardized DALY rate in 2019; (B) ASDR in 2019; (C) AAPC of age-standardized DALY rate from 1990 to 2019; (D) AAPC of ASDR from 1990 to 2019. ASR: age-standardized rate. An AAPC less than 0 indicates a significant decrease, an AAPC equal to 0 signifies stability, and an AAPC greater than 0 represents a significant increase.
The SDI level and burden of CMM demonstrate a clear negative correlation, with the highest age-standardized rates of DALY (8,411.63/100,000, 95% UI: 7,020.74/100,000–10,230.56/100,000) and death (90.03/100,000, 95% UI: 74.34/100,000–110.95/100,000) in the lowest SDI regions. In high SDI regions, both age-standardized rates of DALY (580.86/100,000, 95% UI: 517.96/100,000–649.96/100,000) and death (4.43/100,000, 95% UI: 4/100,000–4.89/100,000) are the lowest (Table 1; Figure 2).
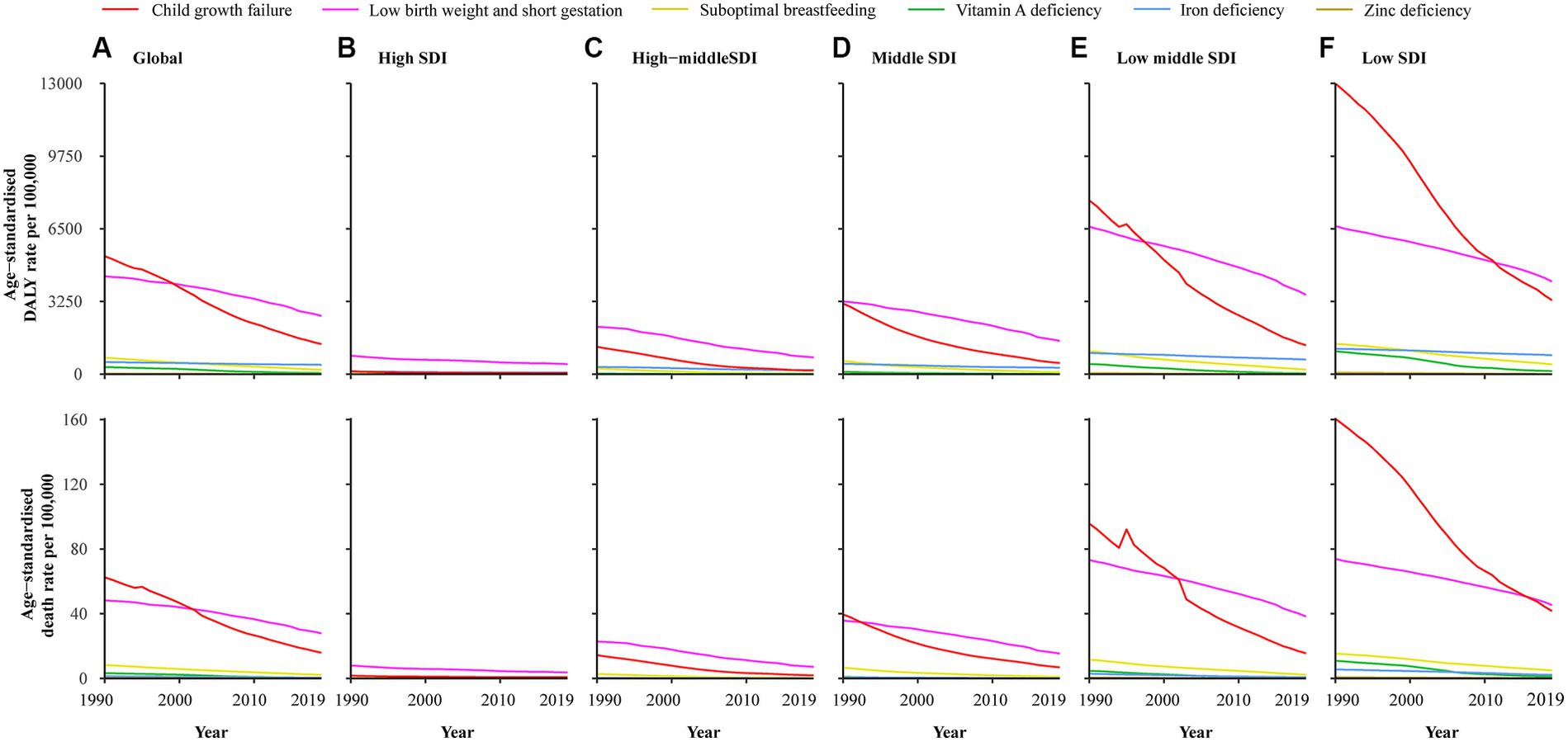
Figure 2. Age-standardized DALY and death rate attributable to CMM among SDI quintiles from 1990 to 2019. (A) Global; (B) High SDI; (C) High-middle SDI; (D) Middle-SDI; (E) Low middle SDI; (F) Low SDI.
Globally, the age-standardized DALY and death rates showed significantly declining trends from 1990 to 2019 (AAPC = −2.92, 95% CI:2.97% to −2.87% and AAPC = −3.19, 95% CI: −3.27 to 3.12%). Furthermore, significantly declining trends were also observed in all of six specific risk factors (Table 1; Supplementary Figure 2). The age-standardized DALY and death rates attributed to CMM decreased from 1990 to 2019 in almost all countries and regions, age groups, and SDI quintiles (Figures 1C,D, 3).
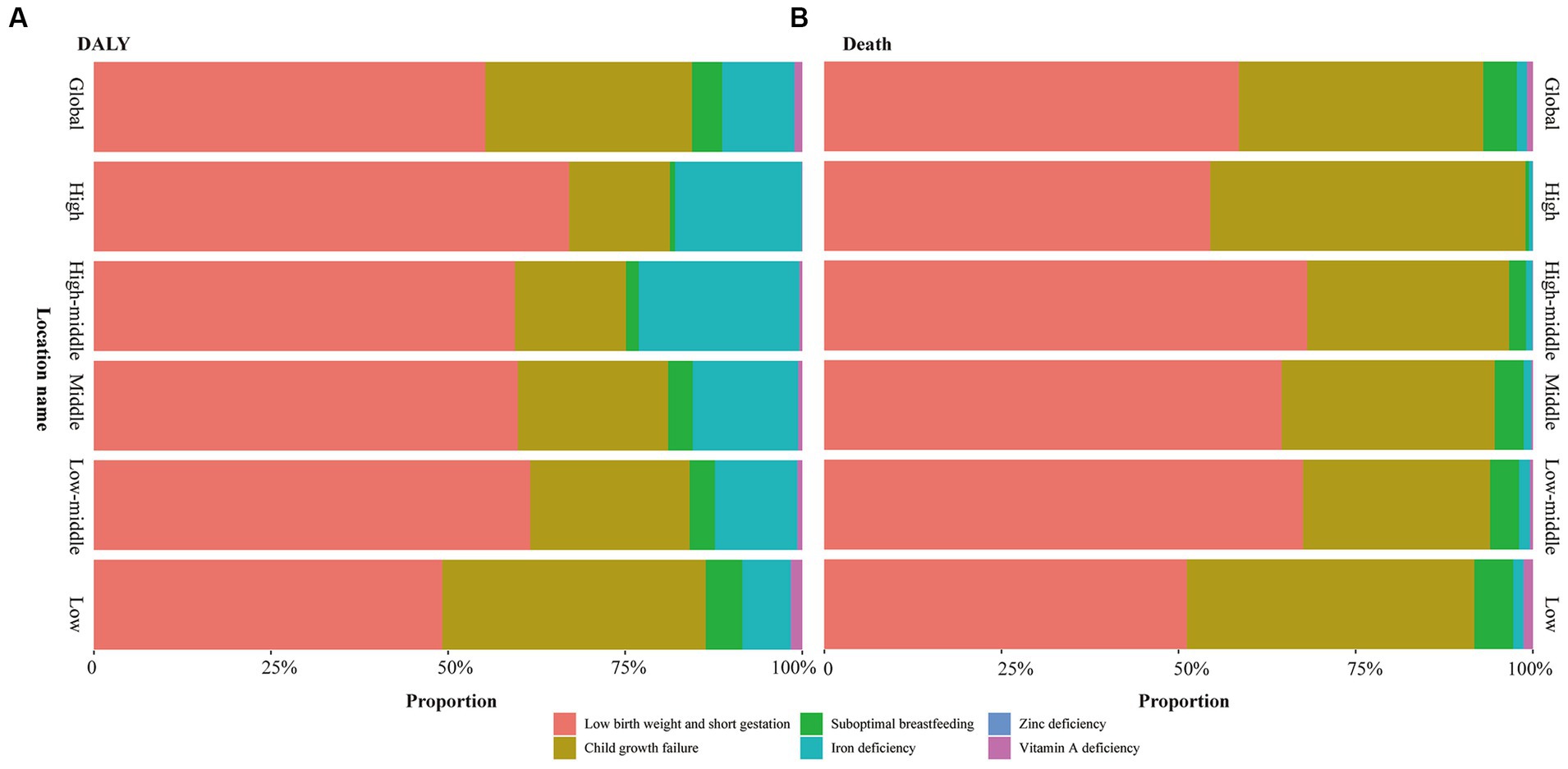
Figure 3. Contribution of each specific risk factor for DALY and death of global and each SDI regions. (A) DALY; (B) Death.
In 2019, low birth weight and short gestation and was primary type of the CMM globally, which accounted for 55.25% and 58.51% of the total DALYs and deaths cases (Figure 3), respectively. In 2019, the global age-standardized DALY and death rates of low birth weight and short gestation were 2,604.41/100,000 (2,232.22/100,000–308,5.68) and 27.87/100,000 (23.73/100,000–33.09/100,000), respectively (Table 1). Subsequently, the second and third rankings were child growth failure and iron deficiency, respectively (Figure 3).
In the past three decades, though, low birth weight and short gestation has been on a downward trend in most countries and regions (Supplementary Figure 3). It still caused heavy burden in Sub-Saharan Africa and low SDI regions, and there is an upward trend in Dominica, Guam and Zimbabwe (Figure 4; Supplementary Figure 3).

Figure 4. Global burden attributable to low birth weight and short gestation in 2019. (A) Age-standardized DALY rate of low birth weight and short gestation; (B) Age-standardized DALY rate of low birth weight; (C) Age-standardized DALY rate of short gestation; (D) ASDR of low birth weight and short gestation; (E) ASDR of low birth weight; (F) ASDR of short gestation.
We found that the age-standardized DALY and death rates were negatively correlated with the SDI scores in the 21 GBD regions, with correlation coefficients of 0.89 (p < 0.05; Figure 5). The GLM results indicated that the GDP per capita (β = −0.1968 for age-standardized DALY rate, β = −0.271 for ASDR), current health expenditure per capita (β = −0.2841 for age-standardized DALY rate, β = −0.2889 for ASDR), physicians per 1,000 people (β = −0.242 for age-standardized DALY rate, β = −0.2943 for ASDR) were contributed to reduce the burden attributable to CMM (Table 2).
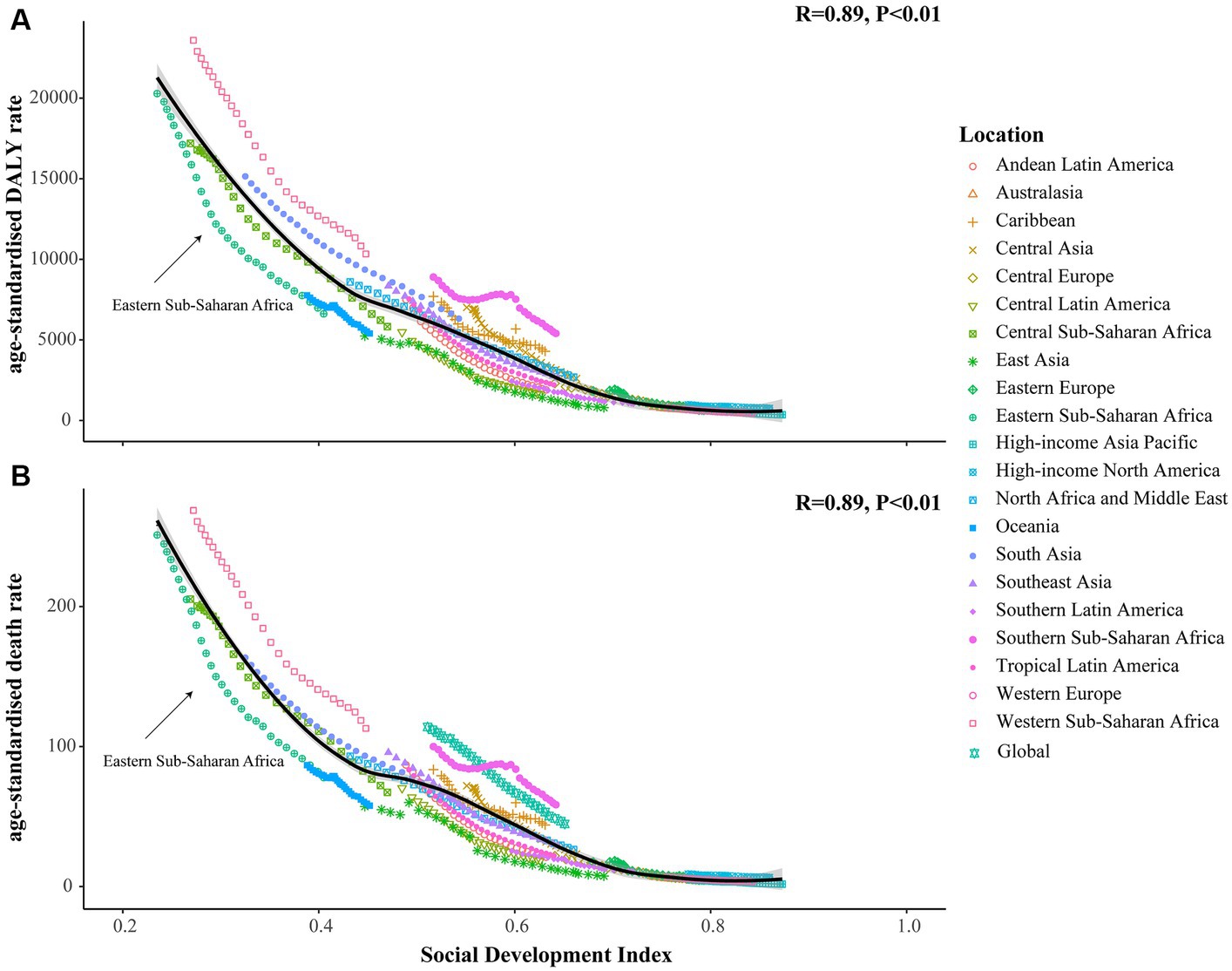
Figure 5. The correlation between SDI scores and the age-standardized rates of DALY and death in 21 GBD regions. (A) The correlation between SDI scores and the age-standardized DALY rate; (B) The correlation between SDI scores and ASDR. The horizontal axis represents the score of the social development index, ranging from 0 for low to 1 for high. Meanwhile, the vertical axis represents the age-standardized rates of DALY and death, with distinct shapes denoting different GBD regions.
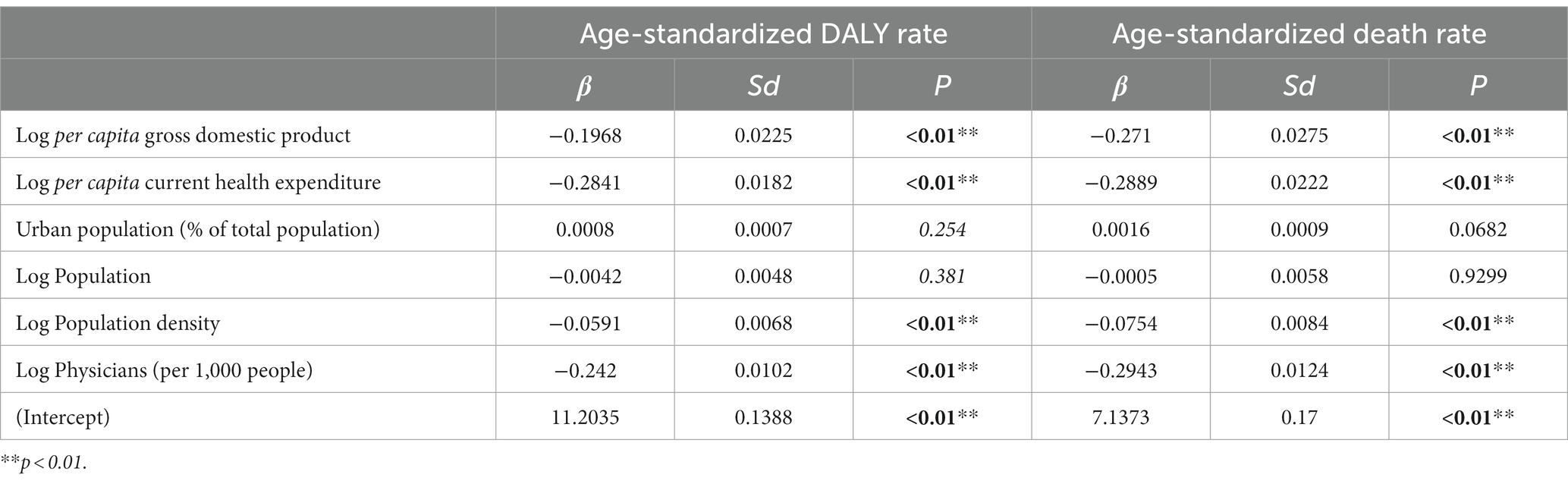
Table 2. The correlation between sociodemographic factors and DALY and death rates attributable to CMM.
In this study, we examined the global burden and trends of disease attributable to CMM during the past 30 years. We also explored the sociodemographic factors associated with burden attributable to CMM. Our findings showed that global age-standardized DALY and death rates have continuously decreased. However, there are still substantial DALYs and death cases occurring annually, especially in infants aged <28 days, Sub-Saharan Africa, and low SDI regions. The burden attributable to CMM was significantly negatively correlated with SDI scores. Higher GDP per capita, current health expenditure per capita, and physicians were found to significantly contribute to reducing the burden attributable to CMM.
The downward trend observed in the burden attributed to CMM is a result of joint efforts made by people worldwide. Previous study has summarized evidence-based interventions that have been effective in reducing CMM over the past decade, including providing preventive zinc, preventive small-quantity lipid-based nutrient supplements, maternal and child multiple micronutrient powder (MMN), maternal calcium vitamin A supplementation, promotion of breastfeeding, farm input subsidies, appropriate complementary feeding and management of moderate and severe acute malnutrition, etc. (7, 29, 30). These measures have considerably improved the nutritional health of children and pregnant women, thereby decreasing the disease burden caused by CMM (31–33). For instance, during food crises, community-based supplementary food is provided and locally produced complementary and therapeutic foods are used to handle acutely malnourished children (34, 35). Additionally, some newly launched interventions, such as preventive low-dose lipid supplements for children aged 6–23 months, have demonstrated with positively impacts on children’s growth and development (36–38). Indirect nutrition strategies implemented by the healthcare sector or other sectors, such as malaria prevention, pre-pregnancy care, water, sanitation, and hygiene improvement, have also contributed significantly to reducing the disease burden of CMM (39–42). Between 1980 and 2000, the mortality rate of babies in the first month of life from 2 months to 5 years decreased by 1/3, while the neonatal mortality rate decreased by about 1/4 (43).
Compared with previous studies in specific country (11, 12), this study offers a more comprehensive perspective for exploring global trends. Furthermore, it is capable of examining the most vulnerable populations and regions. We found that newborns, Sub-Saharan Africa, and regions with a low level of SDI require more attention. For infants <28 days, their bodies are adapting to the external environment. During this process, infants with poor physical conditions may become sick or die because they cannot adjust to the surroundings. Research has shown that although the neonatal period only lasts for 28 days, it accounts for 38% of all deaths among children under the age of 5 (43). Especially in Sub-Saharan Africa, which takes the highest neonatal mortality rates, and the neonatal mortality rate among children under the age of five is 26%. Among 18 countries, of 14 have a neonatal mortality rate of 45 per 1,000 people (43). With a few exceptions, countries in Sub-Saharan Africa have accomplish little progress in reducing neonatal deaths over the past decade (43). For a long time, agriculture and animal husbandry production in Sub-Saharan Africa has lagged behind, leading to low output of agricultural products, and a growth rate of food production that is much lower than that of population growth. Consequently, inadequate food supply has become a common problem in Sub-Saharan Africa. For the past two decades, these regions have consistently had the highest levels of hunger with high GHI score. In all of Sub-Saharan Africa, there exists the highest level of undernourishment (44) with undernutrition hotspots (45). The same situation has also been observed in India, malnutrition served as the predominant risk factor for death in children under the age of 5 in whole region (11).
In previous GBD studies, SDI as a comprehensive index measuring the developmental status of a country or region, is frequently used to analyze its correlation with the burden of disease (18, 19, 46). It measures social development and provides an overall assessment of a country or region’s level of development, including per capita GDP, the average length of education of adults, and the fertility rate of women under the age of 25 (47). As countries and regions increase sustainable development indicators through higher levels of education, particularly for women, we can look forward to progress on these risks (48). While public health interventions such as immunization, breastfeeding, and improved sanitation can reduce neonatal and late neonatal deaths, moreover, the provision of personalized clinical care also supply as a significant decrease in early neonatal (and maternal) deaths (43).
Our results reveal that national economic level, medical expenditure, and the allocation of medical resources are crucial factors influencing the disease burden attributed to CMM. Countries with higher per capita GDP have better economic conditions, greater availability of health resources, improved accessibility and diversity of food, and a reduced likelihood of malnutrition among their residents compared to countries with low per capita GDP (48). Countries with higher per capita GDP also have greater capacity to achieve universal healthcare, reduced inequality in health status and determinants among residents, and more access to medical services (49, 50). Research indicates that every 1% increase in per capita government health expenditure increases life expectancy by 0.0169%, and every 1% increase in per capita private health expenditure increases life expectancy by 0.0032% (51). GDP and domestic health expenditure are common macroeconomic indicators used to measure living standards and public health policies. The number of doctors per thousand population is the main index used to measure the development of medical human resources in the region. A larger number of doctors per thousand population means more adequate medical human resources, greater possibilities for residents to get medical help, and a reduced incidence of disease burden (52). Therefore, expanding coverage of care during childbirth and early postpartum can significantly reduce neonatal mortality in this environment, benefiting the poorest and underserved groups. In areas with heavy burdens, increasing investment in medical resources and allocation of medical resources per capita can effectively reduce the burden attributed to CMM.
This study retrieved data from public database of GBD, and the data collected from various sources, potentially containing errors, anomalies, or uncertainties, which may introduce some bias. Nevertheless, the GBD database still remains one of the most comprehensive and widely used database. Furthermore, strengthening collaboration and data sharing, especially among governments, across regions, and among scholars, is also a crucial pathway to enhance data quality and accessibility. Secondly, considering the latest update in GBD as of 2019, our study was unable to account for the long term impacts of the pandemic and regional conflicts on CMM, as well as their subsequent effects (53, 54). In the future, by obtaining the latest update by GBD, along with more comprehensive and relevant data, and conducting in-depth research, we can explore these issues, thereby obtaining more valuable and worthwhile findings.
Despite the continuous decrease in global age-standardized DALY and death rates attributable to CMM, there are still significant DALYs and deaths occurring annually, especially among infants aged <28 days, in Sub-Saharan Africa, and in low SDI regions. Further research could examine the specific factors contributing to CMM in high burden regions, aiming to develop region-specific interventions. Among the CMM, low birth weight and short gestation has become the primary risk factors globally. The burden attributable to CMM showed a significant negative correlation with SDI scores, while higher per capita GDP, per capita current health expenditure, and physicians per 1,000 people significantly contributed to reducing the burden, it provides the insights into effective resource allocation and healthcare policies. Therefore, our study offers valuable insights to guide targeted interventions and shape future research endeavors in addressing the burden of CMM and enhancing maternal and child health globally.
All data are open-access and are available from The Global Burden of Disease 2019 (https://vizhub.healthdata.org/gbd-results/).
RL: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. LP: Data curation, Formal analysis, Writing – original draft. FL: Writing – original draft. QS: Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Zhejiang Provincial Philosophy and Social Science Planning Project (24NDJC021YB).
We gratefully acknowledge the generous contributions of time and insight of Global Burden of Disease Collaboration for collecting and sharing the data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1323263/full#supplementary-material
1. Moumen, H. State of Food Security and Nutrition in the World (SOFI) 2023. UNICEF DATA. (2023). Available at: https://data.unicef.org/resources/sofi-2023/ (accessed December 24, 2023).
2. WHO. (2023). Joint low birthweight estimates. Available at: https://www.who.int/teams/nutrition-and-food-safety/monitoring-nutritional-status-and-food-safety-and-events/joint-low-birthweight-estimates (Accessed December 24, 2023).
3. WHO. (2023). Joint low birthweight estimates. (n.d.). Available at: https://www.who.int/teams/nutrition-and-food-safety/monitoring-nutritional-status-and-food-safety-and-events/joint-low-birthweight-estimates (Accessed December 24, 2023).
4. Quamme, SH, and Iversen, PO. Prevalence of child stunting in sub-Saharan Africa and its risk factors. Clin Nutr Open Sci. (2022) 42:49–61. doi: 10.1016/j.nutos.2022.01.009
5. Victora, CG, Christian, P, Vidaletti, LP, Gatica-Domínguez, G, Menon, P, and Black, RE. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet Lond Engl. (2021) 397:1388–99. doi: 10.1016/S0140-6736(21)00394-9
6. Zlotkin, S, and Dewey, KG. Perspective: putting the youngest among us into the nutrition “call for action” for food fortification strategies. Am J Clin Nutr. (2021) 114:1257–60. doi: 10.1093/ajcn/nqab207
7. Keats, EC, Das, JK, Salam, RA, Lassi, ZS, Imdad, A, Black, RE, et al. Effective interventions to address maternal and child malnutrition: an update of the evidence. Lancet Child Adolesc Health. (2021) 5:367–84. doi: 10.1016/S2352-4642(20)30274-1
8. Black, RE, Victora, CG, Walker, SP, Bhutta, ZA, Christian, P, de Onis, M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet Lond Engl. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
9. UNICEF. (2017). Levels and Trends in Child Mortality Report 2017 | UNICEF. Available at: https://www.unicef.org/reports/levels-and-trends-child-mortality-report-2017 (Accessed April 27, 2023).
10. GBD. Risk factor collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Lond Engl. (2017, 2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
11. India State-Level Disease Burden Initiative Malnutrition Collaborators. The burden of child and maternal malnutrition and trends in its indicators in the states of India: the global burden of disease study 1990-2017. Lancet Child Adolesc Health. (2019) 3:855–70. doi: 10.1016/S2352-4642(19)30273-1
12. Desyibelew, HD, and Dadi, AF. Burden and determinants of malnutrition among pregnant women in Africa: a systematic review and meta-analysis. PLoS One. (2019) 14:e0221712. doi: 10.1371/journal.pone.0221712
13. Daniil Filipenco. (2022). Children hunger in Africa – statistics and facts. Development Aid. Available at: https://www.developmentaid.org/news-stream/post/146514/children-hunger-in-africa-statistics-and-facts (Accessed December 25, 2023).
14. Child Health Advisory Committe. (2016). PNG National Department of Health, PNG Paediatric Society. 2015 Annual Child Morbidity and Mortality Report. Available at: https://pngpaediatricsociety.org/wp-content/uploads/2013/05/2015-Annual-Child-Morbidity-and-Mortality-Report.pdf (Accessed December 25, 2023).
15. Ssentongo, P, Ssentongo, AE, Ba, DM, Ericson, JE, Na, M, Gao, X, et al. Global, regional and national epidemiology and prevalence of child stunting, wasting and underweight in low- and middle-income countries, 2006–2018. Sci Rep. (2021) 11:5204. doi: 10.1038/s41598-021-84302-w
16. Cortés-Albornoz, MC, García-Guáqueta, DP, Velez-van-Meerbeke, A, and Talero-Gutiérrez, C. Maternal nutrition and neurodevelopment: a scoping review. Nutrients. (2021) 13:3530. doi: 10.3390/nu13103530
17. Forgie, AJ, Drall, KM, Bourque, SL, Field, CJ, Kozyrskyj, AL, and Willing, BP. The impact of maternal and early life malnutrition on health: a diet-microbe perspective. BMC Med. (2020) 18:135. doi: 10.1186/s12916-020-01584-z
18. Murray, CJL, Aravkin, AY, Zheng, P, Abbafati, C, Abbas, KM, Abbasi-Kangevari, M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
19. GBD. Diseases and injuries collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Lond Engl. (2019, 2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
20. World Bank. World development indicators. (2020). https://datacatalog.worldbank.org/dataset/world-development indicators n.d. https://datacatalog.worldbank.org/dataset/world-development-indicators (accessed August 30, 2021).
21. WHO. Malnutrition in children. (n.d.). Available at: https://www.who.int/data/nutrition/nlis/info/malnutrition-in-children (Accessed July 18, 2023).
22. Institute for Health Metrics and Evaluation. (2020). Suboptimal breastfeeding — Level 3 risk. Inst Health Metr Eval. Available at: https://www.healthdata.org/results/gbd_summaries/2019/suboptimal-breastfeeding-level-3-risk (Accessed May 15, 2023).
23. Murray-Kolb, LE, and Beard, JL. Iron deficiency and child and maternal health. Am J Clin Nutr. (2009) 89:946S–50S. doi: 10.3945/ajcn.2008.26692D
24. Institute for Health Metrics and Evaluation. (2020). Child growth failure — Level 3 risk. Inst Health Metr Eval. Available at: https://www.healthdata.org/results/gbd_summaries/2019/child-growth-failure-level-3-risk (Accessed May 5, 2023).
25. National Cancer Institute. Joinpoint Regression Program. (n.d.). Available at: https://surveillance.cancer.gov/joinpoint/ (Accessed December 24, 2023).
26. Kim, HJ, Fay, MP, Feuer, EJ, and Midthune, DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. (2000) 19:335–51. doi: 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z
27. Wang, H, Zhao, S, Wang, S, Zheng, Y, Wang, S, Chen, H, et al. Global magnitude of encephalitis burden and its evolving pattern over the past 30 years. J Infect. (2022) 84:777–87. doi: 10.1016/j.jinf.2022.04.026
28. Portnoy, A, Jit, M, Ferrari, M, Hanson, M, Brenzel, L, and Verguet, S. Estimates of case-fatality ratios of measles in low-income and middle-income countries: a systematic review and modelling analysis. Lancet Glob Health. (2019) 7:e472–81. doi: 10.1016/S2214-109X(18)30537-0
29. Tione, G, Gondwe, E, Maonga, BB, Machira, K, and Katengeza, SP. Improving wasting among children under-5 years in Malawi: the role of farm input subsidies. Front Public Health. (2022) 10:862461. doi: 10.3389/fpubh.2022.862461
30. Zavala, E, Rhodes, M, and Christian, P. Pregnancy interventions to improve birth outcomes: what are the effects on maternal outcomes? A scoping review. Int J Public Health. (2022) 67:1604620. doi: 10.3389/ijph.2022.1604620
31. Bhutta, ZA, Das, JK, Rizvi, A, Gaffey, MF, Walker, N, Horton, S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet Lond Engl. (2013) 382:452–77. doi: 10.1016/S0140-6736(13)60996-4
32. Ouedraogo, O, Doudou, MH, Drabo, KM, Garnier, D, Zagré, NM, Sanou, D, et al. Policy overview of the multisectoral nutrition planning process: the progress, challenges, and lessons learned from Burkina Faso. Int J Health Plann Manag. (2020) 35:120–39. doi: 10.1002/hpm.2823
33. Bhutta, ZA, Akseer, N, Keats, EC, Vaivada, T, Baker, S, Horton, SE, et al. How countries can reduce child stunting at scale: lessons from exemplar countries. Am J Clin Nutr. (2020) 112:894S–904S. doi: 10.1093/ajcn/nqaa153
34. Oh, C, Keats, EC, and Bhutta, ZA. Vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low- and middle-income countries: a systematic review and Meta-analysis. Nutrients. (2020) 12:491. doi: 10.3390/nu12020491
35. Peña-Rosas, JP, De-Regil, LM, Gomez Malave, H, Flores-Urrutia, MC, and Dowswell, T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. (2015) 2015:CD009997. doi: 10.1002/14651858.CD009997.pub2
36. Tam, E, Keats, EC, Rind, F, Das, JK, and Bhutta, AZA. Micronutrient supplementation and fortification interventions on health and development outcomes among children under-five in low- and middle-income countries: a systematic review and Meta-analysis. Nutrients. (2020) 12:289. doi: 10.3390/nu12020289
37. Das, JK, Salam, RA, Hadi, YB, Sadiq Sheikh, S, Bhutta, AZ, Weise Prinzo, Z, et al. Preventive lipid-based nutrient supplements given with complementary foods to infants and young children 6 to 23 months of age for health, nutrition, and developmental outcomes. Cochrane Database Syst Rev. (2019) 5:CD012611. doi: 10.1002/14651858.CD012611.pub3
38. Stewart, CP, Wessells, KR, Arnold, CD, Huybregts, L, Ashorn, P, Becquey, E, et al. Lipid-based nutrient supplements and all-cause mortality in children 6-24 months of age: a meta-analysis of randomized controlled trials. Am J Clin Nutr. (2020) 111:207–18. doi: 10.1093/ajcn/nqz262
39. Dangour, AD, Watson, L, Cumming, O, Boisson, S, Che, Y, Velleman, Y, et al. Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children. Cochrane Database Syst Rev. (2013) 8:CD009382. doi: 10.1002/14651858.CD009382.pub2
40. Darvesh, N, Das, JK, Vaivada, T, Gaffey, MF, Rasanathan, K, Bhutta, ZA, et al. Water, sanitation and hygiene interventions for acute childhood diarrhea: a systematic review to provide estimates for the lives saved tool. BMC Public Health. (2017) 17:776. doi: 10.1186/s12889-017-4746-1
41. Bassani, DG, Arora, P, Wazny, K, Gaffey, MF, Lenters, L, and Bhutta, ZA. Financial incentives and coverage of child health interventions: a systematic review and meta-analysis. BMC Public Health. (2013) 13:S30. doi: 10.1186/1471-2458-13-S3-S30
42. Graziose, MM, Downs, SM, O’Brien, Q, and Fanzo, J. Systematic review of the design, implementation and effectiveness of mass media and nutrition education interventions for infant and young child feeding. Public Health Nutr. (2018) 21:273–87. doi: 10.1017/S1368980017002786
43. Lawn, JE, Cousens, S, and Zupan, J. Lancet neonatal survival steering team. 4 million neonatal deaths: when? Where? Why? Lancet Lond Engl. (2005) 365:891–900. doi: 10.1016/S0140-6736(05)71048-5
44. Global Hunger Index. (2023). Global, Regional, and National Trends. Glob Hunger Index GHI - Peer-Rev Annu Publ Des Comprehensively Meas Track Hunger Glob Reg Ctry Levels. Available at: https://www.globalhungerindex.org/trends.html (Accessed December 25, 2023).
45. Amir-Ud-Din, R, Fawad, S, Naz, L, Zafar, S, Kumar, R, and Pongpanich, S. Nutritional inequalities among under-five children: a geospatial analysis of hotspots and cold spots in 73 low- and middle-income countries. Int J Equity Health. (2022) 21:135. doi: 10.1186/s12939-022-01733-1
46. Zheng, Y, Yu, Q, Lin, Y, Zhou, Y, Lan, L, Yang, S, et al. Global burden and trends of sexually transmitted infections from 1990 to 2019: an observational trend study. Lancet Infect Dis. (2022) 22:541–51. doi: 10.1016/S1473-3099(21)00448-5
47. Sean McKee. (2016). A new way to measure progress in global health – Humanosphere. Available at: https://www.humanosphere.org/global-health/2016/10/a-new-way-to-measure-progress-global-health/ (Accessed April 27, 2023).
48. Pienaar, M, Marais, L, Serekoane, M, Marais, K, Cloete, J, Lenka, M, et al. “Being a mother is not child’s play”: the capabilities of mothers in a low-resource setting in South Africa. Health Expect Int J Public Particip Health Care Health Policy. (2023) 26:651–61. doi: 10.1111/hex.13689
49. WHO. (2021). Global expenditure on health: Public spending on the rise? Available at: https://www.who.int/publications-detail-redirect/9789240041219 (Accessed April 27, 2023).
50. OECD/The World Bank. (2020). Health at a Glance: Latin America and the Caribbean 2020. Paris: OECD Publishing. doi: 10.1787/6089164f-en
51. Shen, Y, Sheng, H, Ma, G, and Ma, A. Analysis on health production effectiveness of health resources in OECD countries. Chin Health Econ. (2019) 38:61–3. doi: 10.7664/CHE20190715 (In Chinese).
52. Elhady, GW, Ibrahim, SK, Abbas, ES, Tawfik, AM, Hussein, SE, and Salem, MR. Barriers to adequate nutrition care for child malnutrition in a low-resource setting: perspectives of health care providers. Front Public Health. (2023) 11:1064837. doi: 10.3389/fpubh.2023.1064837
53. Jawad, M, Hone, T, Vamos, EP, Cetorelli, V, and Millett, C. Implications of armed conflict for maternal and child health: a regression analysis of data from 181 countries for 2000–2019. PLoS Med. (2021) 18:e1003810. doi: 10.1371/journal.pmed.1003810
Keywords: trends, sub-Saharan Africa, low SDI, global burden of disease, child and maternal malnutrition
Citation: Liu R, Pi L, Leng F and Shen Q (2024) Global disability-adjusted life years and deaths attributable to child and maternal malnutrition from 1990 to 2019. Front. Public Health. 12:1323263. doi: 10.3389/fpubh.2024.1323263
Received: 18 October 2023; Accepted: 02 January 2024;
Published: 18 January 2024.
Edited by:
Mojisola Olanike Kehinde, Landmark University, NigeriaReviewed by:
Olutosin Ademola Otekunrin, Federal University of Agriculture, NigeriaCopyright © 2024 Liu, Pi, Leng and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qing Shen, c3FAaG1jLmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.