
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 24 January 2024
Sec. Health Economics
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1322949
Objectives: China has implemented reforms to enhance the operational efficiency of three-level medical services through medical consortiums (MCs). This study evaluated the impact of MCs reform on health services in Sanming, China.
Methods: An interrupted time-series analysis (ITSA) was conducted to assess the impact of MCs on changes in health service levels and trends across the overall situation of MCs and different institutional types within MCs, including county hospitals and grassroots medical institutions. The evaluation focused on various indicators such as outpatient and emergency visits, inpatients, average length of stay, occupancy rate of hospital beds, and hospital bed turnover times. Monthly data were collected from April 2015 to June 2019 through reports on the Sanming Municipal Health Commission website and the Sanming public hospital management monitoring platform.
Results: After the intervention of MCs reform, a significant increase was observed in the total number of inpatients (β3 = 174.28, p < 0.05). However, no statistically significant change was observed in the total number of outpatient and emergency visits (β3 = 155.82, p = 0.91). Additionally, the implementation of MCs reform led to an amplification in service volumes provided by county hospitals, with significant increases in the number of outpatient and emergency visits (β3 = 1376.54, p < 0.05) and an upward trend in the number of inpatients (β3 = 98.87, p < 0.01). However, no significant changes were observed under the MCs policy for grassroots medical institutions regarding the number of outpatient and emergency visits (β3 = −1220.72, p = 0.22) and number of inpatients (β3 = 75.42, p = 0.09).
Conclusion: The Sanming MCs reform has achieved some progress in augmenting service volumes. Nevertheless, it has not led to an increase in service volumes at the grassroots medical institutions. There persists an insufficiency in the efficiency of services and a need for further improvement in primary healthcare. To address these concerns, it is imperative for county hospitals to offer targeted assistance that can enhance motivation among grassroots medical institutions. Besides the MCs should explore initiatives, including improved management of medical equipment, allocation of funding, and personnel resources.
Given the rapidly advancing age demographics among its population, rising burden of chronic disease, increasing prevalence of risk factors, and changing environmental conditions, efficiently allocating health resources for improved patient outcomes has become a policy priority and challenge within the realm of health (1, 2). China has undertaken numerous substantial health policies and initiatives to establish a robust functioning healthcare service infrastructure over recent decades. However, despite incremental enhancements stemming from ongoing comprehensive reforms within China’s healthcare system, scholars’ analysis revealed that approximately 82% of available resources remain concentrated in tertiary and secondary hospitals, whereas merely 18% is allocated toward primary care facilities (3). Consequently, China’s current healthcare system framework grapples with unsustainable predicaments, such as the insufficient distribution of medical resources. Therefore, addressing these concerns becomes an urgent necessity.
As the cornerstone of China’s integrated medical delivery system, the primary objective of medical consortiums (MCs) is to optimize health resource allocation and bolster the capabilities of primary medical institutions. The Chinese government has implemented a series of policies to enhance the efficiency of China’s healthcare system, particularly focusing on MCs. In April 2017, the General Office of the State Council issued “Guidelines on Promoting the Construction and Development of Medical Consortia” (4). Subsequently, in July 2020, the National Health Commission and National Administration of Traditional Chinese Medicine released a policy titled “The Notice on Releasing Management Measures for a Medical Consortium (trial)” (5). Several provinces and cities in China, including Hainan (6), Zhejiang (7), and Guangdong (8), have explored various reforms related to MCs. As of 2020, 4,028 MCs had been established in China (9). However, the formation of MCs is still at an early stage and faces several challenges, such as a lack of clarity regarding institutions and responsibilities and limited primary care capacity (10, 11).
In 2012, the city of Sanming in Fujian Province embarked on a comprehensive healthcare system reform, and has since become a leading healthcare reform model in China. In 2021, the National Health Commission issued the “Notice on the Promotion of Experience in the Construction of Hierarchical Diagnosis and Treatment and Medical Consortium in Sanming,” which summarized the experience of developing compact MCs in Sanming and provided many practical insights into how this could be accomplished. In 2017, Sanming implemented a reform of MCs that relied on county hospitals to form the foundation. This reform oversaw several grassroots medical institutions, including township hospitals and community health centers, to improve regional resource allocation and optimize medical resource utilization. The objectives of Sanming’s MCs policy can be summarized in two aspects: First, to promote the equalization of health resources and hierarchical diagnosis and treatment, as well as resolve issues with unreasonable medical treatment orders, to provide health services “at their doorsteps” for the public and establish an orderly system for medical care. Second, to encourage county hospitals to take the lead in implementing precise management policies and expanding technology and services at the grassroots level, thereby comprehensively enhancing the overall capacities of grassroots medical institutions. In order to achieve the above objectives, the following major measures have been undertaken. First, county hospitals within the compact MCs are responsible for resource allocation. Second, MCs should standardize internal management, including human resources management, funding and asset allocation, performance measurement and information construction. Third, payment reform related to the medical insurance package should create an economic incentive to retain a balance in the medical insurance fund. To date, MCs have been formed in all counties in Sanming, involving 18 county-level hospitals and 144 township hospitals and community health centers, making 10 compact county-level MCs. This would ultimately improve the service capabilities and operational efficiency of county hospitals and grassroots medical institutions in MCs. Therefore, paying more attention to the effects before and after implementing the MCs policy is important.
Several studies have previously reported on the status of China’s MCs reform (8), regional practical experiences (12), theoretical frameworks (13), and development pathways (14). Although some studies have examined the effects of MCs policy using quantitative analyses, most of them have been conducted from a single perspective, such as assessing inpatient numbers (15), hospitalization rates (16), hospitalization expenses (17), physician flows (18), informatization construction (19), and health professionals’ views and satisfaction with regard to MCs reform (20). For example, Özkaytan et al. (21) found that integrated care models could address complicated healthcare needs and enhance service continuity and coordination. Ye et al. (22) used the super-efficiency slack-based measure–data envelopment analysis (SBM-DEA) model to demonstrate that MCs reform could improve the efficiency of medical services provided by county-level public general hospitals. Similarly, using the standardized patient approach, Su and Zhou (23) found that the MCs model could improve the quality of primary medical services. After the MCs reform, Yuan et al. (24) found that county-level public hospitals improved their service efficiency and capability.
Many scholars also researched the effects of the Sanming Model after its comprehensive healthcare system reform (25). For instance, Fu et al. focused on medical costs (26), Meng et al. analyzed drug expenses (27), and Hu et al. paid attention to the use of antibiotics (28), which confirmed that the Sanming medical model has positive effects. Researchers have paid attention to Sanming’s MCs reforms as a research topic and analyzed the current situation (29), governance mechanism (9), and practical experience (30). However, only a few studies have measured the effects of Sanming MCs reform. Liao et al. conducted a descriptive analysis to report that the MCs model helped optimize the hospital income structure (31). Li et al. used a stepwise regression model to demonstrate that the MCs reform positively affected the structure of medical expenses (32). Some studies have examined the effects of MCs reform in a particular county. For example, Zheng et al. interviewed 15 key informants and found that establishing compact MC in Youxi County helped prompt professional integration (33). Zhong ZD et al. used an interrupted time-series analysis (ITSA) to report that the number of surgeries had decreased in county hospitals (34). Zhong ZC et al. employed an ITSA to analyze that the cost of outpatient and emergency patients per time in Youxi County hospitals increased after the medical insurance payment reform (35). Xiong et al. researched the overall, grassroots, and hospitals, which used an ITSA to find that economic incentives of MCs policy have influenced the number of inpatient, outpatient and emergency visits (36). However, they mostly focused on the overall effects or a specific medical institution. Therefore, quantitative research focusing on evaluating the observable effects on health services after the MCs policy implementation, considering both the overall situation of MCs and the different types of institutions within MCs, could provide a more accurate picture of the overall impact of MCs reform.
This study aimed to analyze the effects of Sanming’s MCs reform on health services as judged by the overall situation of MCs and different institutional types (county hospitals and grassroots medical institutions) within MCs to understand the problems and limitations of China’s MCs policy. The findings from this research will serve as a valuable reference for MCs reform in China and other developing countries, facilitating the comprehensive and effective implementation of an integrated health service system.
Sanming is a prefecture-level city in Fujian province, with a residential population of 2.455 million, and a gross domestic product (GDP) per capita of ¥126,044 in 2022. As of 2022, 7,463 registered physicians/physician assistants, 9,118 registered nurses, and 16,843 hospital beds were available in Sanming (37).
In April 2017, the Sanming Municipal Committee and Municipal Government issued the “Opinions on Implementation of General Hospitals in the Establishment,” aiming to establish high-level general hospitals in the region. This helped select the intervention point for evaluating the effects of the MCs policy in the present study. Considering the time required for the reforms to be implemented, May 2017 was set as the time boundary, as the county hospitals and grassroots medical institutions needed to prepare for the implementation of MCs, including establishment of organizational structures, division of responsibilities and operational mechanisms. April 2015 was selected as the initial date of pre-MCs adoption, and June 2019 was the end date of post-MCs adoption, ensuring equal time (25 months) before and after the adoption of the MCs reforms to facilitate a meaningful comparison (38). We used an ITSA to assess the impact of the MCs policy in Sanming on trend changes in health services provision from April 2015 to June 2019. It ensured that this study had enough data points to assess the intervention’s effect (39).
Based on the policy objectives proposed by the Sanming MCs reform, this study aimed to assess the effects of constructing MCs from two aspects. One focused on the fact that the construction of MCs should serve as an integration mechanism between different health institutions in the county, helping to form an orderly system for medical care. Therefore, this study used two indicators, the total number of outpatient and emergency visits and the total number of inpatients, to focus on intra-county integration based on the overall situation of county and township medical institutions in the region (40). The other was to improve the health service efficiency of county hospitals and grassroots medical institutions under the MCs. Therefore, this study also analyzed the changes in service indicators for county hospitals and grassroots medical institutions separately. The analysis and evaluation of outpatient and inpatient services were representative for assessments of the hospitals’ efficiency and management levels. In summary, indicators such as the number of outpatient and emergency visits, number of inpatients, average length of stay, occupancy rate of hospital beds, and hospital bed turnover times were utilized (41, 42). The relevant formulas used are as follows:
The indicators used in this study are routinely collected by the medical statistics department in county public hospitals and grassroots medical institutions and reported to the Municipal Health Commission in Sanming. It was assumed that the trend changes in these indicators resulted from Sanming’s implementation of MCs.
Monthly data were collected from 10 county MCs, including 18 county-level public hospitals and 144 grassroots medical institutions from April 2015 to June 2019. The post-policy period was 25 months from June 2017 to June 2019, and the baseline data period was 25 months, covering the period from April 2015 to April 2017. All indicators were collected from monthly reports on the Sanming Municipal Health Commission website and the Sanming public hospital management monitoring platform.
ITSA is commonly used to analyze the effects of interventions in situations where a control group is difficult or impossible to find, and the period for data collection can be divided into two time segments (pre- and post-intervention) to be analyzed using a regression model (38, 39, 43). Because no control group was available, we used an ITSA to evaluate the impact of the MCs policy intervention. Accordingly, we constructed the following model:
where Y is the dependent variable representing the number of outpatient and emergency visits, number of inpatients, average length of stay, occupancy rate of hospital beds, and hospital bed turnover times. The independent variables included time, intervention, and time after intervention. “Time” refers to each month from April 2015 to June 2019. “Intervention” is a binary variable coded as 0 for the period before and 1 for the period after the intervention. “Time after intervention” equals 0 before policy implementation and increases monthly afterward. Moreover, GDP per quarter and quarterly dummy variables were included as control variables. C refers to the control variable. As we only collected annual GDP data from 2015 to 2016 and quarterly GDP data from 2017 to 2019, we extrapolated the quarterly GDP from 2015 to 2016 based on the quarterly GDP composition ratios from 2017 to 2019. β0, β1, β2, and β3 reflect the baseline level, time trend without considering the intervention, immediate effects of the intervention on the level of selected indicators, and continuous effect of the intervention on the trend of indicators, respectively. ε is the error term.
In this study, ITSA was performed with Newey-West standard errors, and all indicators were investigated for autocorrelations using the Cumby-Huizinga test (44). If autocorrelation was present at higher lag orders (up to the six lags tested), the lag orders accounted for it. All analyses were performed using Stata version 15 (StataCorp., College Station, TX, United States), and a p-value < 0.05 was considered statistically significant.
Table 1 presents the descriptive statistics. The mean total number of outpatient and emergency visits and the mean total number of inpatients increased after the reforms. In county hospitals, the mean number of outpatient and emergency visits, the number of inpatients, the average length of stay, and the occupancy rate of hospital beds increased. However, during the policy’s implementation, the mean hospital bed turnover times gradually decreased from 3.16 to 2.95. Correspondingly, the mean number of outpatient and emergency visits for grassroots medical institutions increased from 232135.08 to 356592.04. The mean number of inpatients, average length of stay, occupancy rate of hospital beds, and hospital bed turnover time were 8739.80, 5.19, 47.30, and 2.79, before the reform and 8498.20, 5.17, 46.87, and 2.75 afterward, respectively.
All evaluation results of ITSA are presented in Table 2. Model 1 is a crude model. Model 2 is the adjusted model, in which we control for quarterly GDP and quarterly dummy variables. Table 2 and Figure 1 indicate that, after the policy intervention, the trend change of the total number of inpatients significantly increased (β3 = 174.28, 95% confidence interval [CI] = 37.62–310.94, p < 0.05). However, no significant changes were observed in the total number of outpatient and emergency visits for the trend (β3 = 155.82, 95% CI = −2536.03 to 2847.66, p = 0.91).
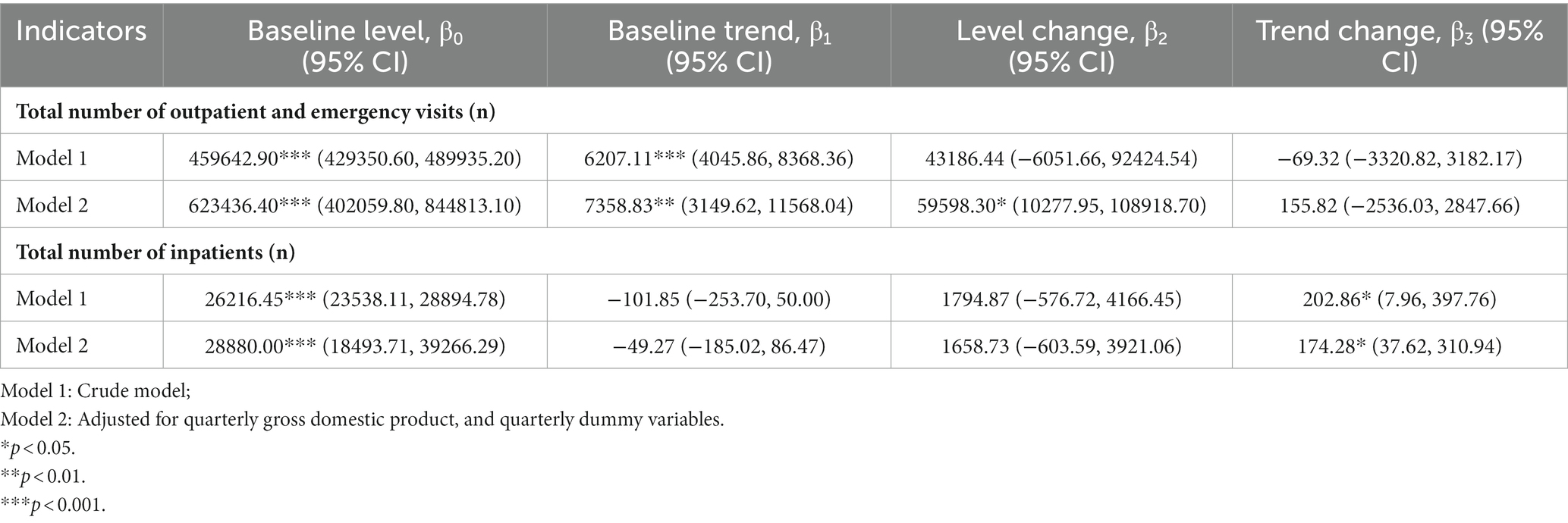
Table 2. Evaluation results of interrupted time-series analysis for the policy effects on the health services indicators in county and grassroots medical institutions.
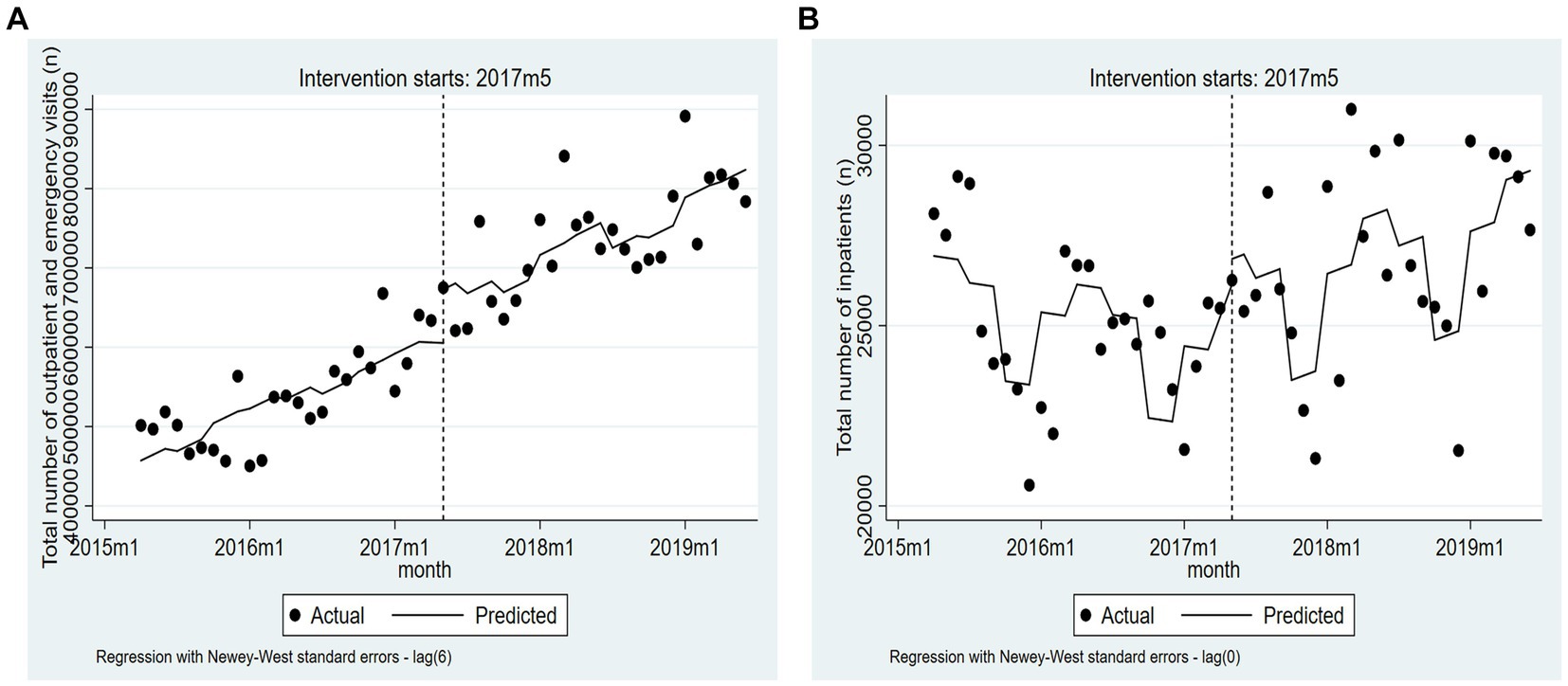
Figure 1. The trend changes of two indicators based on the adjusted model (from April 2015 to June 2019). (A) Total number of outpatient and emergency visits. (B) Total number of inpatients.
Table 3 and Figure 2 show the effects of the MCs policy implementation on health service indicators in county hospitals. The baseline trend in outpatient and emergency visits before the policy intervention showed a significant increase (β1 = 2179.84, 95% CI = 965.87–3393.82, p < 0.01). Meanwhile, the number of outpatient and emergency visits (β3 = 1376.54, 95% CI = 70.88–2682.19, p < 0.05) showed an increasing trend after the policy intervention. Additionally, the number of inpatients also showed an increasing trend, with a statistically significant β3 of 98.87 (95% CI = 32.68–165.05, p < 0.01). No significant differences were observed in the trend change for average length of stay, occupancy rate of hospital beds, or hospital bed turnover times.
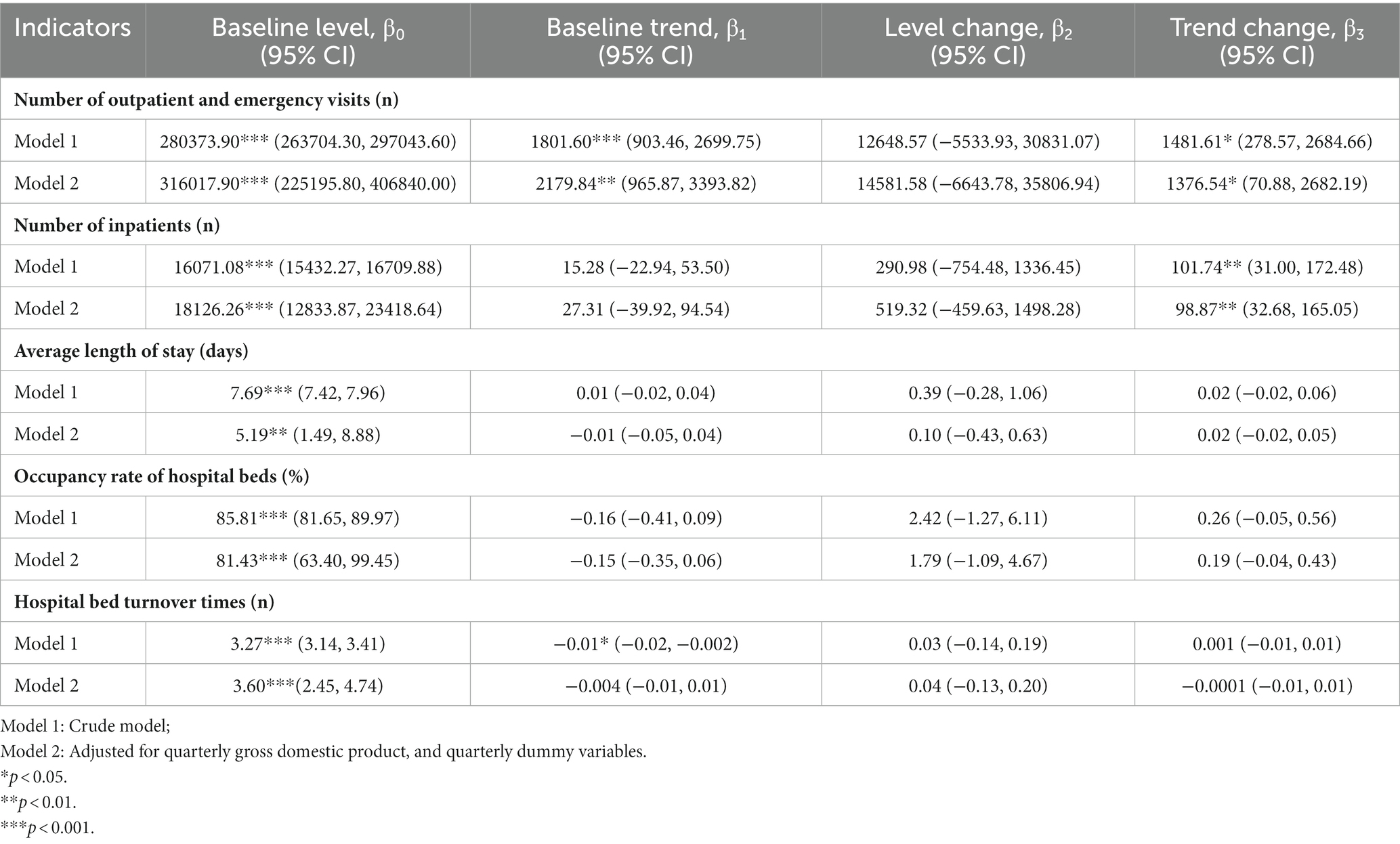
Table 3. Evaluation results of the interrupted time-series analysis for the policy effects on the health services indicators of county hospitals.
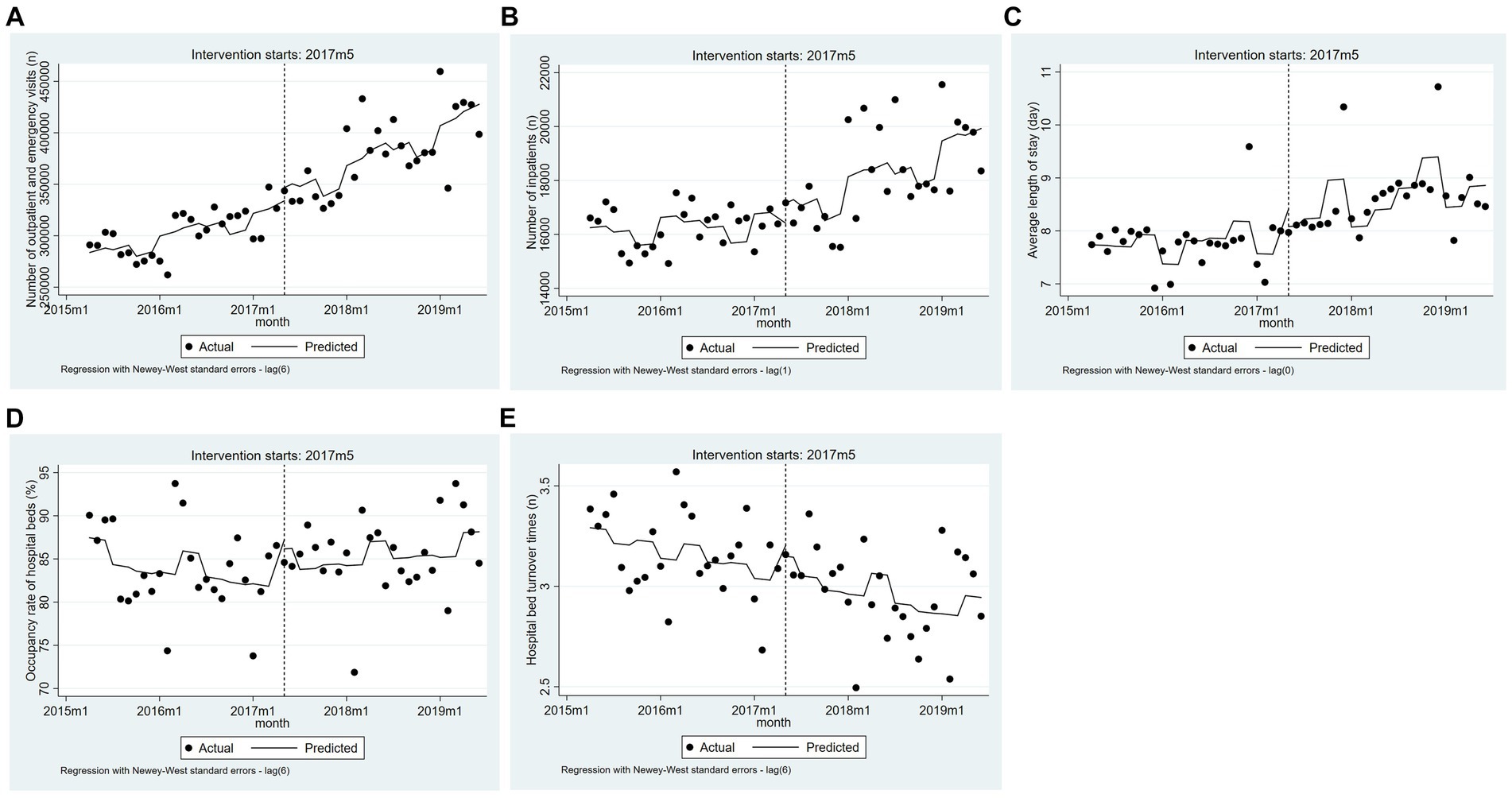
Figure 2. The trend changes of five indicators in county hospitals based on the adjusted model (from April 2015 to June 2019). (A) Number of outpatient and emergency visits. (B) Number of inpatients. (C) Average length of stay. (D) Occupancy rate of hospital beds. (E) Hospital bed turnover times.
As Table 4 shows, after the MCs policy implementation, the average length of stay at grassroots medical institutions recorded a statistically significant decrease, with a β3 of −0.04 (95% CI = −0.05 to −0.02, p < 0.001). Meanwhile, the ITSA did not show significant differences in the trend changes for other indicators (Figure 3).
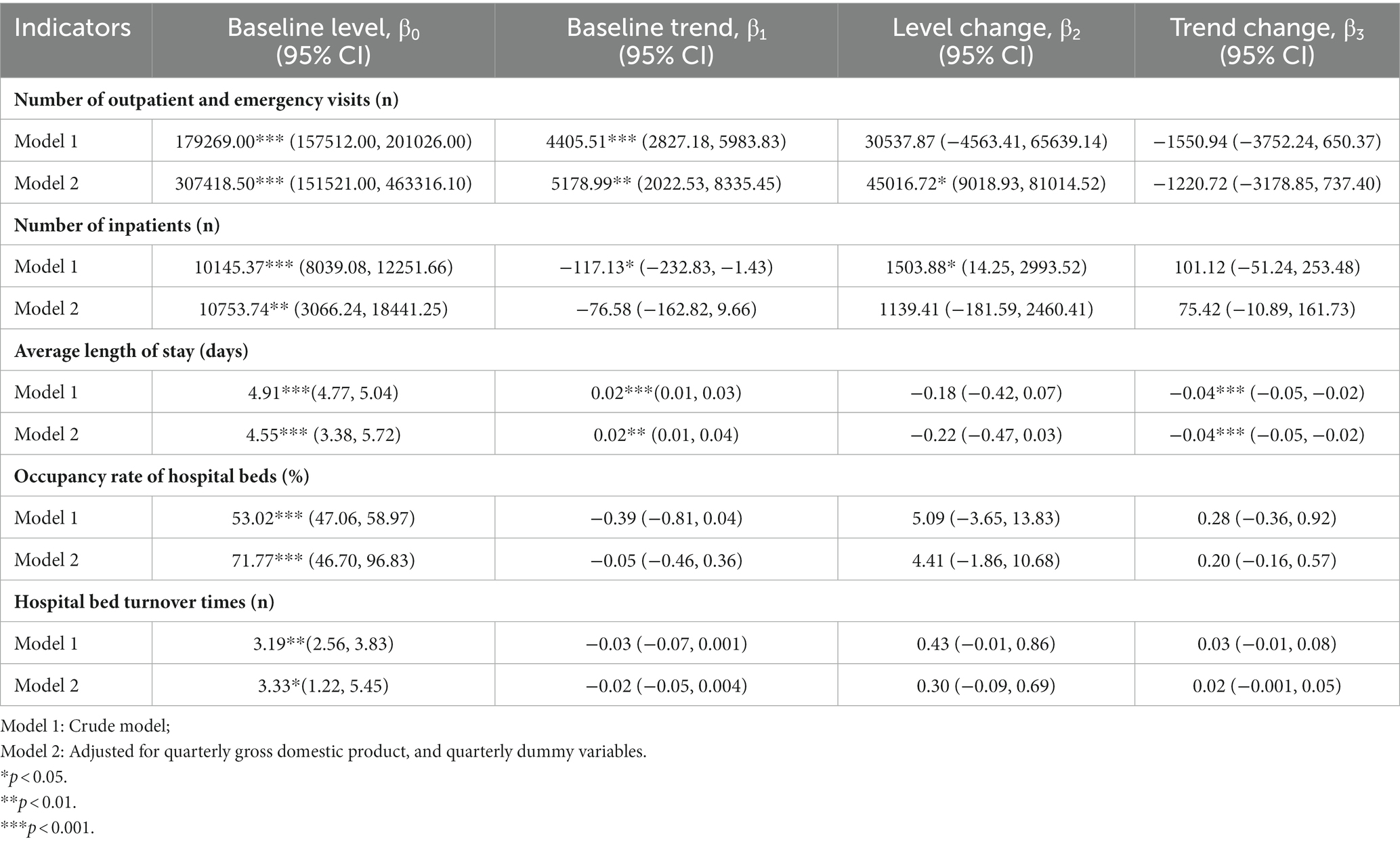
Table 4. Evaluation results of the interrupted time-series analysis for the policy effects on the health services indicators of grassroots medical institutions.
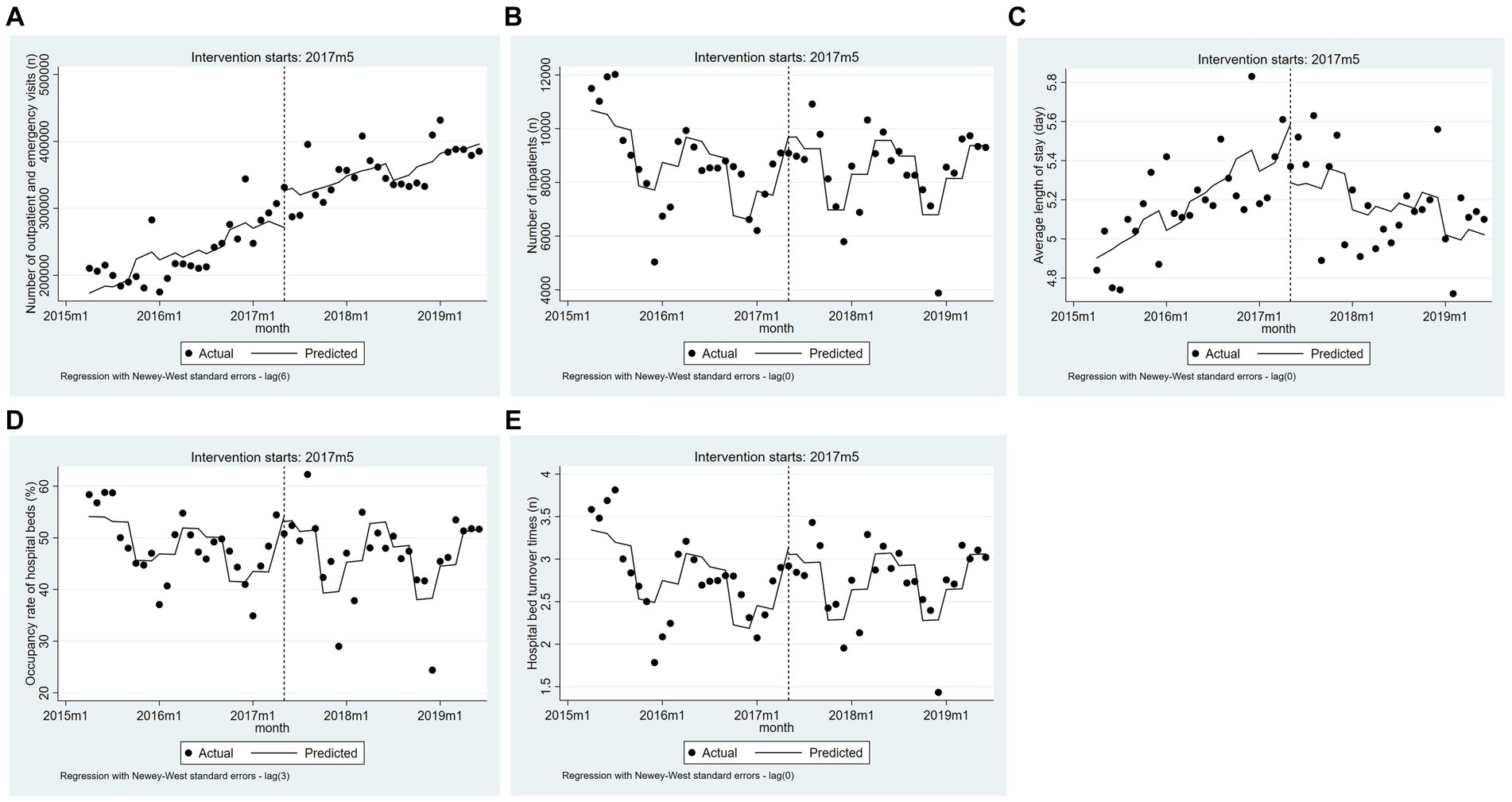
Figure 3. The trend changes of five indicators for grassroots medical institutions based on the adjusted model (from April 2015 to June 2019). (A) Number of outpatient and emergency visits. (B) Number of inpatients. (C) Average length of stay. (D) Occupancy rate of hospital beds. (E) Hospital bed turnover times.
Our study focused on Sanming, a prefecture-level city in China. A 51-month data series and ITSA were employed to evaluate the effects of the MCs’ policy implementation on seven health service indicators. This study presented novel empirical evidence regarding the effects of the MCs reform in China and provided scientifically grounded recommendations for other prefecture-level cities aiming to enhance their policy implementation efforts.
This study found no statistically significant change in the total number of outpatient and emergency visits after the MCs reform. However, further analysis revealed a noteworthy increase in such visits at county hospitals while observing no substantial alteration at grassroots medical institutions. These contrasting findings challenged prior research reporting an evident surge in outpatient and emergency visits at grassroots medical institutions after the establishment of MCs. For example, Gong et al. reported that following the implementation of the Luohu Model, the number of patients in grassroots medical institutions increased from 530,000 to 1.99 million people from 2014 to 2019 (45). Similarly, Wang et al. revealed that outpatient and emergency visits at the primary care level increased after implementing the Zhenjiang Model (46). The result of this study suggested inadequate patient retention within these establishments and highlighted deficiencies in establishing appropriate healthcare protocols. There may be several reasons to explain this phenomenon. First, the payment reform of the medical insurance package has created an effective incentive for Samnang’s MCs to improve their health service capabilities and retain a balance in the medical insurance fund. However, county hospitals, leading hospitals with management rights over the fund, have not motivated grassroots medical institutions enough. Second, county hospitals exhibit deficiencies in managing grassroots medical institutions within MCs (47). In Sanming, county hospitals mainly manage grassroots medical institutions by establishing of primary management departments, comprising two to eight employees with diverse professional backgrounds including nursing and pharmacy. However, this approach lacks sufficient professional management talent. Third, county hospitals in Sanming primarily focus on the assessment and fund allocation of grassroots medical institutions instead of prioritizing the long-term development of regional medical institutions. As a result, there is a failure to motivate grassroots medical institutions to enhance their service capabilities adequately. Unlike the Zhenjiang Model, which set up the joint consultation sessions of general practitioners and specialists at the primary. Upper-level hospitals provided management and business cooperation to improve the technical level of grassroots medical institutions (48).
Our findings revealed a decrease in the average length of stay at grassroots medical institutions during the intervention of MCs, aligning with the findings of Lao et al. (49). Generally, the reduction in the average length of stay indicates an optimization in health service allocation and an improvement in the quality of medical services. Consequently, it raises awareness, enhances competitiveness, encourages more patients to seek medical treatment, and promotes sustainable development. This positive outcome may be attributed to the establishment of a unified management system between county hospitals and grassroots medical institutions under the MCs policy implementation. This facilitated the transfer of medical equipment, personnel, technical skills and management expertise from county hospitals to grassroots facilities, enhancing the service capacity of grassroots medical institutions and contributing to the improvement (50). Additionally, the reform in payment for medical insurance packages standardized the diagnosis and treatment process (51). Furthermore, it effectively addressed issues such as excessive treatment for common diseases and unnecessary healthcare services provided by grassroots medical institutions (52).
In the MCs policy implementation context, the total number of inpatients showed a statistically significant increase. The similar finding could also be found in post-MCs reform in Deqing County, Zhejiang (53), and in Youxi County, Sanming (34). From 2017 to 2019, the hospitalization rate for transfer among urban workers’ medical insurance patients in Sanming decreased from 6.84, 6.63% and then to 6.41%. This downward trend may be attributed to the implementation of a medical insurance package, enabling MCs to control transferred inpatients and retain more inpatients within the county hospitals. Furthermore, no significant change was observed in the number of inpatients at grassroots medical institutions, which was consistent with the findings of another study considering the effect of Sanming’s MCs reform (36). It also could be seen that there was a substantial increase in the number of inpatients at county hospitals, consistent with previous studies by Zhao et al. (54) and Tao et al. (55). The findings indicated that county hospitals effectively retained inpatients within their respective counties and exerted control over patients’ outflow. Tertiary hospitals with robust, comprehensive capabilities in provincial and municipal areas could offer valuable support to county hospitals. For example, Fujian Province stipulated that 47 tertiary hospitals at the provincial and municipal level deploy 516 medical personnel to assist county hospitals. This measure aimed to enhance the medical service capacity of county hospitals while promoting local treatment-seeking behavior (56). However, the implementation of MCs policy had little impact on the number of inpatients at grassroots medical institutions. This could be attributed to several reasons. First, a previous study revealed that most incremental inpatient service volumes at grassroots medical institutions were derived from transfers from specialized departments at county hospitals (57). County hospitals heavily relied on inpatient revenue as a significant source of their overall medical revenue. County hospitals in Sanming generated the largest proportion of their total revenue from inpatient services, accounting for 50.61, 49.23, and 46.33%, respectively, in 2017, 2018, and 2019. Community interest consciousness is lacking, resulting in county hospitals’ unwillingness to transfer inpatients to grassroots medical institutions. Consequently, the integration of medical institutions within MCs may further deplete the resources of grassroots medical institutions as higher-level hospitals are reluctant to transfer patients downward. This situation led to inadequate treatment at lower-tiered healthcare centers. Moreover, outpatient and inpatient services have distinct functional roles in disease prevention and the medical service chain. Diseases that require hospitalization pose greater challenges in terms of treatment. However, the limited availability of medical services at grassroots medical institutions led residents to prefer seeking care at higher-level medical institutions with more advanced medical technology and guaranteed quality for hospitalization (58). As a result, their healthcare-seeking behaviors were less significantly affected by the MCs policy (36).
This study also found no statistically significant differences in the average length of stay, occupancy rate of hospital beds, or hospital bed turnover times before and after the MCs reform in county hospitals. This result differed from that in other studies. Ye and Jiang found that, in the long term, the Luohu Model reduced the length of stay in inpatient care (59). These findings indicated that the service capacity of county hospitals has not yet improved, and their leading function has not been adequately emphasized. Therefore, further promotion of county hospitals is necessary to achieve the goal of “county hospitals taking a leading position” in the MCs reform (60). There are still some challenges due to variations in medical care levels, population sizes, economic development between counties, as well as the relatively short period since implementing reform in most county hospitals (61). Given the inadequate infrastructure, weak technology and professionalism, insufficient medical equipment and health personnel, and the lack of interconnected information systems within the county, it was challenging to meet residents’ multilevel and multiple healthcare service demands (62–64). Unlike the Luohu Model, technologies, such as Internet Plus, were utilized to facilitate the sharing of diagnosis and treatment information in the Luohu Medical Group, improving medical services’ efficiency (65). According to the MCs policy, county hospitals play a vital role in ensuring major diseases which can be treated without patients leaving their counties (66). The above findings suggested that county hospitals should define their positioning and expand their diagnosis coverage by strengthening the comprehensiveness of diagnosis and treatment projects. At the same time, improvements are needed in infrastructure, information systems, health personnel, medical equipment, and discipline construction (64).
No significant differences were found in the occupancy rates or turnover times for hospital beds during the MCs policy implementation, indicating a need to strengthen healthcare efficiency in grassroots health institutions (54). These findings may be attributed to several factors, including inadequate health personnel at the grassroots level and uneven distribution of their skills (67). As seen from the MCs monitoring index value of Fujian Province, Sanming had a higher number of daily visits per grassroots doctor at 13.00 compared to the provincial level (11.21). Moreover, some researchers have revealed that Sanming lacks attractive programs to motivate medical personnel to serve at the grassroots level (68). The demanding workload of grassroots health personnel in Sanming increases the likelihood of burnout and turnover among healthcare workers, making recruiting staff for grassroots medical institutions difficult and leading to a personnel shortage and a vicious circle (69). Furthermore, despite receiving technical support from professionals at county-level or tertiary hospitals, the service capacity of grassroots medical institutions remains low. Consequently, professionals in grassroots medical institutions were in subordinate positions (33), thereby limiting the role of primary medical staff and diminishing their motivation to engage actively in the establishment of MCs. Another contributing factor could be patients’ lack of confidence in grassroots hospitals’ quality of care. Patients were not aware of the enhanced convenience offered by grassroots medical institutions for managing non-critical conditions, particularly prevalent chronic diseases (67, 70). Therefore, it is imperative for the governmental health department to formulate human resource policies and measures to augment intrinsic motivation and elevate service standards in grassroots medical institutions. This can be accomplished by implementing incentive policies, bolstering development programs, augmenting remuneration packages, and enhancing working conditions (68). Meanwhile, grassroots medical practitioners must establish robust patient connections by providing guidance and policy advocacy in basic public health services (71), thereby fostering a greater willingness to attend grassroots medical institutions (70).
Compared to other studies evaluating the effect of the Sanming’s MCs, this study assessed the effects considering the overall situation of MCs and the diverse institutions within them. This comprehensive perspective sheds light on the evaluation of MCs. Our study revealed that implementing the MCs policy in Sanming has partially contributed to the development of healthcare system capabilities. However, it is evident that an appropriate medical order has not yet been established. As key healthcare providers and leaders in the tertiary medical system, county hospitals must strengthen their leading roles further. In addition, grassroots medical institutions have been unable to effectively serve as gatekeepers. This resulted in a siphoning effect whereby patients prefer higher-level hospitals. Addressing this issue is crucial when implementing the MCs policy in other areas. County hospitals and grassroots medical institutions within MCs should formulate long-term development plans for enhancing policy coordination through allocating resources such as medical equipment, funds, and personnel. This approach aims to strengthen health service capacity, improving the service quality and efficiency, reshape patients’ healthcare-seeking habits, and promote comprehensive and continuous medical services in county hospitals and grassroots medical institutions.
This study had some limitations. First, the samples used in this study were limited to a single city in eastern China, which restricts the generalizability of the findings. Second, other policies may have influenced the results of ITSA, and its application could not fully mitigate this impact (72). For example, the implementation of diagnosis-related group reform or high-quality related hospital reform in Sanming could have affected health service efficiency. This might have led to an overestimation of the intervention effects of the MCs policy. Third, due to the limitations in data availability, we only collected annual GDP data from 2015 to 2016 and quarterly GDP data from 2017 to 2019 in Sanming. This may influence the results obtained from the adjusted ITSA model. Lastly, evaluating the implementation effect of the MCs policy in Sanming for only approximately 4 years may somewhat compromise the stability of evaluation results. Future research should conduct more in-depth analysis by collecting additional data and comparing it with other Chinese provinces.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
XY: Data curation, Writing – original draft. YC: Writing – original draft, Data curation. CL: Conceptualization, Supervision, Writing – review & editing. MH: Conceptualization, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Three-Year Action Plan of Shanghai Municipality Strengthens Public Health System Construction [Grant numbers: GWIV-32 and GWV-12], and the Shanghai Foundation for Talents Development [Grant number: 2020128].
The authors thank the Sanming Municipal Health Commission for the support of data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chai, PP, Zhang, YH, Zhou, MG, Liu, SW, and Kinfu, Y. Technical and scale efficiency of provincial health systems in China: a bootstrapping data envelopment analysis. BMJ Open. (2019) 9:e27539. doi: 10.1136/bmjopen-2018-027539
2. Zhang, LY, Cheng, G, Song, SH, Yuan, BB, Zhu, WM, He, L, et al. Efficiency performance of China's health care delivery system. Int J Health Plann Manag. (2017) 32:254–63. doi: 10.1002/hpm.2425
3. Yip, W, Fu, HQ, Chen, AT, Zhai, TM, Jian, WY, Xu, R, et al. 10 years of health-care reform in China: Progress and gaps in universal health coverage. Lancet. (2019) 394:1192–204. doi: 10.1016/S0140-6736(19)32136-1
4. General Office of the State Council. Guidance on promoting the construction and development of medical consortiums. (2017). Available at: http://www.gov.cn/zhengce/content/2017-04/26/content_5189071.htm (Accessed August 30, 2023).
5. National Health Commission, National Administration of Traditional Chinese Medicine. Notice on releasing management measures for medical consortium (trial). (2020). Available at: http://www.nhc.gov.cn/yzygj/s3594q/202007/62e9df95714741fa95f9074828848f05.shtml (Accessed August 30, 2023).
6. Ke, Z, Xiao, SZ, Lai, GX, and Xian, ZD. Influence of county medical community on equity of health resource allocation in Hainan Province. Chin Primary Health Care. (2023) 37:1–6. doi: 10.3969/j.issn.1001-568X.2023.07.0001
7. Wu, C, Tu, YX, Li, ZX, and Yu, JX. An early assessment of the county medical community reform in China: a case study of Zhejiang Province. J Chin Gov. (2021) 6:463–85. doi: 10.1080/23812346.2021.1978722
8. Zheng, CY, Huang, YX, and Wang, X. Current situation analysis and operation effect evaluation of county medical community in Guangdong Province: based on two-step cluster and rank-sum ratio method. Mod Prev Med. (2022) 49:4132–8. doi: 10.20043/j.cnki.MPM.202205700
9. Lin, KH, Liu, X, Zhong, ZD, Xiong, YB, Zhou, J, and Xiang, L. Research on the governance of merged county medical community in Sanming based on the integration of principal-agent theory and stewardship theory. Chin Health Econ. (2022) 41:1–5. doi: 10.7664/j.issn.1003-0743.2022.8.zgwsjj202208002
10. Wu, J, Du, XN, Fu, XL, Hua, BY, Ma, Z, Dong, WY, et al. Analysis of the formation mechanism of the vulnerability of the compact healthcare alliance and the key governance strategies during the "14th five-year plan" period. Chin Hosp. (2022) 26:21–3. doi: 10.19660/j.issn.1671-0592.2022.2.07
11. Li, X, Zhang, L, Li, Z, and Tang, WX. Patient choice and willingness toward gatekeepers as first-contact medical institutions in Chinese tiered healthcare delivery system: a cross-sectional study. Front Public Health. (2021) 9:665282. doi: 10.3389/fpubh.2021.665282
12. Yang, JK, Wang, L, Lu, SS, Liao, XH, and Wang, SR. Practice and exploration of high-quality development of compact county-level medical community in Guizhou Province——taking the construction of county-level medical sub centers as a means. Health Econ Res. (2023) 40:75–8. doi: 10.14055/j.cnki.33-1056/f.2023.08.006
13. Chen, XY, Wang, XH, Peng, ZY, Qian, Y, Pan, WW, Cheng, GM, et al. Research on the theoretical framework of performance evaluation of traditional Chinese medicine preventive treatment of diseases in county medical community based on grounded theory. Chin Hosp Manage. (2023) 43:15–8.
14. Xu, Y, Hu, L, and Liu, YL. Multiple realization pathways of county-level medical alliances to improve service capacity: a fuzzy set qualitative comparative analysis. Chin Gen Pract. (2023) 26:3140–6. doi: 10.12114/j.issn.1007-9572.2023.0058
15. Ran, YF, Gao, HX, Han, D, Hou, GL, Chen, YC, and Zhang, Y. Comparison of inpatient distribution amongst different medical alliances in a county: a longitudinal study on a healthcare reform in rural China. Int J Equity Health. (2020) 19:142. doi: 10.1186/s12939-020-01260-x
16. Zheng, Y, Guo, YH, Zhu, LY, Huang, ED, and Nong, S. Estimation of the impact of medical community reform on intra-county hospitalization rate in Guangdong Province based on differences-in-differences. Chin Health Econ. (2023) 42:26–8.
17. Rong, WR, and Yang, YJ. Study on the impact of countywide medical alliance reform on hospitalization expenses: take Funan county in Anhui province as an example. Soft Sci Health. (2021) 35:40–4. doi: 10.3969/j.issn.1003-2800.2021.06.010
18. Zhou, LJ, and Tao, HB. Research on the incentive mechanism of county-level specialists outreach the grassroots level in the county medical community. Chin J Health Policy. (2023) 16:24–9. doi: 10.3969/j.issn.1674-2982.2023.03.004
19. Tian, SH, and Chen, Y. Vertical integration of electronic health records in medical consortiums: dynamic modeling approach based on the evolutionary game theory. JMIR Serious Games. (2023) 11:e41528. doi: 10.2196/41528
20. Gao, QS, Ma, Y, Zhu, PH, and Chen, DW. Healthcare professionals' views of the integrated county healthcare consortium in Zhejiang, China. Int J Integr Care. (2022) 22:25. doi: 10.5334/ijic.5690
21. Özkaytan, Y, Schulz-Nieswandt, F, and Zank, S. Acute health care provision in rural long-term care facilities: a scoping review of integrated care models. J Am Med Dir Assoc. (2023) 24:1447–57. doi: 10.1016/j.jamda.2023.06.013
22. Ye, Y, Evans, R, Jing, L, Rizwan, M, Xuan, Y, and Lu, W. The impact of county medical community reform on the medical service efficiency of county-level public general hospitals in China: a case study of Shanxi Province. Int J Env Res Pub Health. (2022) 19:13827. doi: 10.3390/ijerph192113827
23. Su, M, and Zhou, ZL. A study on the impacts from medical service complex and its models on the quality of primary medical services in urban China: based on the standardized patient approach. Chin J Health Policy. (2021) 14:41–6. doi: 10.3969/j.issn.1674-2982.2021.09.007
24. Yuan, BY, Lin, K, and Dong, HJ. Impact of county-level medical alliance on the performance of county-level public hospitals: a case study of Zhejiang Province. Chin Hosp Manage. (2020) 40:26–9.
25. He, YZ, Dou, GS, Huang, QY, Zhang, XY, Ye, YF, Qian, MC, et al. Does the leading pharmaceutical reform in China really solve the issue of overly expensive healthcare services? Evidence from an empirical study. PLoS One. (2018) 13:e190320. doi: 10.1371/journal.pone.0190320
26. Fu, HQ, Li, L, Li, MQ, Yang, CY, and Hsiao, W. An evaluation of systemic reforms of public hospitals: the Sanming model in China. Health Policy Plann. (2017) 32:1135–45. doi: 10.1093/heapol/czx058
27. Meng, ZL, Zhu, M, Cai, YY, Cao, XH, and Wu, HZ. Effect of a typical systemic hospital reform on inpatient expenditure for rural population: the Sanming model in China. BMC Health Serv Res. (2019) 19:231. doi: 10.1186/s12913-019-4048-7
28. Hu, L, Fu, MY, Wushouer, H, Ni, BY, Li, HQY, Guan, XD, et al. The impact of Sanming healthcare reform on antibiotic appropriate use in county hospitals in China. Front Public Health. (2022) 10:936719. doi: 10.3389/fpubh.2022.936719
29. Liao, DP. The practice of medical insurance package payment and C-DRG under medica alliance. Chin Health Econ. (2022) 41:49–52.
30. Yang, XD, and Huang, CJ. A report on operation mechanism of compact medical union in counties. Mod Hosp Manage. (2022) 20:19–21. doi: 10.3969/j.issn.1672-4232.2022.03.005
31. Liao, DP, Lan, Z, Jing, L, Zheng, LY, and Ren, W. Research on the impact of medical insurance package payment for merged county medical alliance. Chin Health Econ. (2023) 42:29–33.
32. Li, XM, and Li, YP. Structural analysis of the increase in medical expenses of public hospitals under medical alliance in Sanming. Chin Health Econ. (2021) 40:30–5.
33. Zheng, Y, Hu, J, Li, L, and Dai, T. Practice and enlightenment of chronic disease management at the county level in China from the perspective of professional integration: a qualitative case study of Youxi County, Fujian Province. Int J Integr Care. (2023) 23:1–13. doi: 10.5334/ijic.7550
34. Zhong, ZD, Yang, XD, Wu, DW, Wu, XH, Lin, KH, Liu, X, et al. Collaborative governance model and effect analysis of the reform of county medical alliance payment method in Sanming: taking Youxi general hospital as an example. Chin J Health Policy. (2022) 15:1–8. doi: 10.3969/j.issn.1674-2982.2022.03.001
35. Zhong, ZC, Yao, Q, Chen, SQ, Jiang, JN, Lin, KH, Yao, YF, et al. China promotes Sanming's model: a national template for integrated medicare payment methods. Int J Integr Care. (2023) 23:1–11. doi: 10.5334/ijic.7011
36. Xiong, YB, Zhong, ZD, Lin, KH, Liu, X, Zhou, J, and Xiang, L. Research on the influence of internal and external economic incentives of Sanming county medical alliance on medical service supply. Chin J Health Policy. (2022) 15:66–73. doi: 10.3969/j.issn.1674-2982.2022.07.009
37. Sanming Municipal Bureau of Statistics. Statistical bulletin on national economic and social development of Sanming in 2022. (2022). Available at: http://tjj.sm.gov.cn/xxgk/tjgb/ndgb/202303/t20230317_1888106.htm (Accessed August 30, 2023).
38. Yang, P, Cao, Y, Liu, DH, Bai, YX, Pan, F, and Xu, YY. The effect of electronic medical record application on the length of stay in a Chinese general hospital: a department- and disease-focused interrupted time-series study. J Med Syst. (2014):38. doi: 10.1007/s10916-014-0053-x
39. Bernal, JL, Cummins, S, and Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2021) 50:1045. doi: 10.1093/ije/dyaa118
40. Wang, Y, Zhu, YL, Shi, H, Sun, XL, Chen, N, and Li, X. The effect of the full coverage of essential medicines policy on utilization and accessibility of primary healthcare service for rural seniors: a time series study in Qidong, China. Int J Env Res Pub Health. (2019) 16:4316. doi: 10.3390/ijerph16224316
41. Zhao, N, and Chen, K. Equity and efficiency of medical and health service system in China. BMC Health Serv Res. (2023) 23:33. doi: 10.1186/s12913-023-09025-2
42. Aloh, HE, Onwujekwe, OE, Aloh, OG, and Nweke, CJ. Is bed turnover rate a good metric for hospital scale efficiency? A measure of resource utilization rate for hospitals in Southeast Nigeria. Cost Eff Resour Alloc. (2020) 18:21. doi: 10.1186/s12962-020-00216-w
43. Linden, A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. (2015) 15:480–500. doi: 10.1177/1536867X1501500208
44. Cumby, RE, and Huizinga, J. Testing the autocorrelation structure of disturbances in ordinary least squares and instrumental variables regressions. Econometrica. (1992) 60:185–95. doi: 10.2307/2951684
45. Gong, FF, Sun, XZ, and Li, YN. Building a world-class integrated high-quality healthcare system with Chinese features: an analysis of the experience of Shenzhen Luohu hospital group. Chin Gen Pract. (2021) 24:2408–11. doi: 10.12114/j.issn.1007-9572.2021.00.178
46. Wan, XB, Zhu, F, and Yang, Y. Exploration and practice of establishing the campact medical consortium in Zhenjiang City. Chin J Hosp Admin. (2013) 29:263–6. doi: 10.3760/cma.j.issn.1000-6672.2013.04.009
47. Niu, YD, and Zhang, L. Analysis in the development and problems of county medical alliance. Chin Health Econ. (2020) 39:22–5. doi: 10.7664/CHE20200205
48. Zhu, F, Wan, XB, and Yang, Y. Hierarchical medical system piloted by Zhenjang rehabilitation group: practice and reflections. Chin J Hosp Admin. (2017) 33:275–7. doi: 10.3760/cma.j.issn.1000-6672.2017.04.010
49. Lao, YQ, Li, JH, Liu, MQ, Xie, FS, Tang, YT, and Guo, ZY. Research on the influence of compact county medical consumption linkage on the operation efficiency of county and township medical institutions. Chin. Hospitals. (2022) 26:5–8. doi: 10.19660/j.issn.1671-0592.2022.12.02
50. Lu, ZH, Li, YW, Guo, D, and Wang, LJ. Evaluation on the completion of the goals for the pilot construction of the county-level medical community in a certain province — empirical research based on DID. Health Econ Res. (2023) 40:54–6. doi: 10.14055/j.cnki.33-1056/f.2023.09.018
51. Kalanj, K, Marshall, R, Karol, K, and Oreskovic, S. The effects of diagnosis-related groups payment on efficiency of the hospital health care in Croatia. Croat Med J. (2021) 62:561–8. doi: 10.3325/cmj.2021.62.561
52. Altman, SH. The lessons of medicare's prospective payment system show that the bundled payment program faces challenges. Health Affair. (2012) 31:1923–30. doi: 10.1377/hlthaff.2012.0323
53. Dong, JX, Xu, XQ, Dong, ZX, and Wu, SX. Analysis on the effectiveness of county medical community reform-based on the empirical study of medical community a in Deqing County. J Huzhou Univ. (2022) 44:78–84. doi: 10.3969/j.issn.1009-1734.2022.08.012
54. Zhao, YX, Yuan, CL, and Liu, MZ. Effect and evaluation of compact medical consortium. Mod Bus Trade Ind. (2023) 44:30–2. doi: 10.19311/j.cnki.1672-3198.2023.06.012
55. Tao, LL, Shi, W, Yang, H, Sun, LL, and Song, Y. Implementation status of hierarchical medical system in Chaoyang District, Beijing. Chin Gen Pract. (2017) 20:3876–9. doi: 10.3969/j.issn.1007-9572.2017.31.009
56. Fujian Provincial Health Commission. Notice of the 2019-2020 rural-urban hospital peer-to-peer support program. (2018). Available at: https://wjw.fujian.gov.cn/xxgk/zfxxgkzl/zfxxgkml/wszh/yzgl/201811/t20181121_4677918.htm (Accessed September 6, 2023).
57. Jia, M, Wang, F, Tian, MM, Yuan, SS, and Zhao, MJ. Pilot projects of county-level healthcare community in China: its early impacts on primary health institutions. Chin Rural Health Serv Adm. (2020) 40:482–5. doi: 10.3969/j.issn.1005-5916.2020.07.007
58. Li, J, Zhao, N, Zhang, HY, Yang, H, and Yang, J. Patients' willingness of first visit in primary medical institutions and policy implications: a national cross-sectional survey in China. Front Public Health. (2022) 10:842950. doi: 10.3389/fpubh.2022.842950
59. Ye, ZJ, and Jiang, YW. The impact of a pilot integrated care model on the quality and costs of inpatient care among Chinese elderly: a difference-in-difference analysis of repeated cross-sectional data. Cost Eff Resour Alloc. (2022) 20:28. doi: 10.1186/s12962-022-00361-4
60. Li, Q, Tian, LQ, Jing, XL, Chen, XH, Li, JF, and Chen, HX. Efficiency and scale effect of county public hospitals in Shandong Province, China: a cross-sectional study. BMJ Open. (2020) 10:e35703. doi: 10.1136/bmjopen-2019-035703
61. Liu, J, He, BB, Xu, XL, Zhou, LM, Li, J, Wang, GR, et al. Determinants of efficiency growth of county-level public hospitals-evidence from Chongqing, China. BMC Health Serv Res. (2019) 19:858. doi: 10.1186/s12913-019-4609-9
62. Zhao, L, Wang, L, Li, S, and Zhang, Y. Evaluation and analysis of hospital efficiency in China based on macro- and micro-level analyses. J Public Health UK. (2020) 28:191–7. doi: 10.1007/s10389-019-01048-6
63. Wang, ML, Fang, HQ, Tao, HB, Cheng, ZH, Lin, XJ, Cai, M, et al. Bootstrapping data envelopment analysis of efficiency and productivity of county public hospitals in eastern, central, and Western China after the public hospital reform. J Huazhong Univ Sci Technolog Med Sci. (2017) 37:681–92. doi: 10.1007/s11596-017-1789-6
64. Fang, PQ, Chen, JY, Liu, SL, and Zhang, Q. Challenges and reflection on challenges of public hospitals under the hierarchical diagnosis and treatment system. Chin Hosp Manage. (2018) 38:1–3.
65. Xia, JJ, Zhao, ZQ, Sun, XZ, Gong, FF, Hou, WL, Gan, Y, et al. Effectiveness analysis of "sharing economy" on "Luohu model". Chin J Soc Med. (2019) 36:630–4. doi: 10.3969/j.issn.1673-5625.2019.06.020
66. Yin, G, Ning, J, Peng, YR, Yue, JK, and Tao, HB. Configurational paths to higher efficiency in county hospital: evidence from qualitative comparative analysis. Front Public Health. (2022) 10:918571. doi: 10.3389/fpubh.2022.918571
67. Xu, JF, Zhou, YY, Liu, RY, Cheng, F, and Liang, WN. Primary health institutions and service quality in China: implications for health policy. Int J Env Res Pub Health. (2022) 19:12063. doi: 10.3390/ijerph191912063
68. Wu, QD, Xie, XY, Liu, WB, and Wu, Y. Implementation efficiency of the hierarchical diagnosis and treatment system in China: a case study of primary medical and health institutions in Fujian province. Int J Health Plann Manag. (2022) 37:214–27. doi: 10.1002/hpm.3333
69. Qin, LL, Li, S, Chen, YW, Chen, S, Fan, XL, Luo, BG, et al. Analysis of work willingness and its influencing factors of mental illness prevention and control personnel of grassroots institutions in China: a cross-sectional study. Trans R Soc Trop Med Hyg. (2022) 116:807–13. doi: 10.1093/trstmh/trac010
70. Feng, D, Zhang, DL, Li, BY, Zhang, Y, Serrano, R, Shi, DX, et al. Does having a usual primary care provider reduce patient self-referrals in rural China’s rural multi-tiered medical system? A retrospective study in Qianjiang District, China. BMC Health Serv Res. (2017) 17:778. doi: 10.1186/s12913-017-2673-6
71. Wu, YX, and Li, YP. Effect of medical insurance package payment in compact county medical community on patient flows. J Nanjing Med Univ (Soc Sci). (2023) 23:144–9. doi: 10.7655/NYDXBSS20230208
Keywords: medical consortium, health services, county hospitals, grassroots medical institutions, interrupted time series analysis
Citation: Yang X, Chen Y, Li C and Hao M (2024) Effects of medical consortium policy on health services: an interrupted time-series analysis in Sanming, China. Front. Public Health. 12:1322949. doi: 10.3389/fpubh.2024.1322949
Received: 17 October 2023; Accepted: 10 January 2024;
Published: 24 January 2024.
Edited by:
Minghui Li, University of Tennessee Health Science Center (UTHSC), United StatesReviewed by:
Dai Su, Capital Medical University, ChinaCopyright © 2024 Yang, Chen, Li and Hao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengyue Li, bGljaGVuZ3l1ZUBmdWRhbi5lZHUuY24=; Mo Hao, aGFvbW8wM0BmdWRhbi5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.