
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 17 April 2024
Sec. Public Mental Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1322742
This article is part of the Research TopicCommunity Series in Mental Illness, Culture, and Society: Dealing with the COVID-19 Pandemic, volume VIIIView all 63 articles
Background: Resident physicians at the standardized training stage had undergone significant physical and mental stress during the release of the COVID-19 pandemic restrictions at the end of 2022 in China. This study aimed to investigate the psychological status (including anxiety, depression, somatic symptoms, job burnout, and vicarious trauma) of resident physicians and identify its influencing factors under these special periods.
Methods: Survey was conducted one month after the release of the COVID-19 pandemic restrictions on resident training physicians from a tertiary first-class hospital in Zhejiang, China. Resident physicians completed the psychological status questionnaire. Chi-square tests, Mann–Whitney U tests, and logistic regression analyses were used to estimate the group differences and variable associations.
Results: The prevalence of anxiety, depression, and somatic discomfort in this study was 20.88, 28.53, and 41.47%, respectively. Female resident physicians were more likely to experience somatic symptoms [adjusted odds ratio (OR) = 2.36, 95% confidence interval (CI): 1.33–4.18]. Resident physicians with problem-focused coping styles were less prone to psychological health issues [depression (adjusted OR = 0.92, 95% CI: 0.88–0.96), anxiety (adjusted OR = 0.94, 95% CI: 0.90–0.98), somatic symptoms (adjusted OR = 0.93, 95% CI: 0.89–0.97), job burnout (adjusted OR = 0.91, 95% CI: 0.87–0.96) and vicarious trauma (adjusted OR = 0.94, 95% CI: 0.90–0.98)]. Inversely, resident physicians with emotion-focused coping styles and experienced negative life events were more prone to psychological health issues.
Conclusion: Resident training physicians had a high risk of anxiety, depression, and somatic symptoms under the special COVID-19 pandemic restriction release period. Females, with lower training stages, degrees, negative life events, and emotion-focused coping styles had a disadvantaged effect on psychological status. The medical teaching management department needs to monitor and reduce the workload and working hours of resident physicians, ensure sufficient sleep time, and pay attention to the psychological status of resident physicians. By strengthening regular communication and mental health education or intervention, which can help them improve their ability to cope with complex tasks.
In the past three COVID-19 pandemic years, medical workers have endured extreme psychological pressure. A series of studies have been conducted about the psychological health status of medical workers (1, 2), including medical students (3, 4). During the study period, medical workers were actively involved in the care of COVID-19 patients (1, 2). Both were found a high prevalence of anxiety and depression, but there were few studies on resident training physicians. The resident physicians refer to medical graduates who make medical practices under the direct or indirect supervision of a senior clinician for three years in a qualified hospital training base. As is well known, outbreaks of infectious diseases have psychological influences on medical workers and the general population (1). Medical workers often encounter various mental problems under high pressure and high-risk epidemic prevention situations (5). At the beginning of the outbreak of COVID-19, there has a study found that one-sixth of people reported moderate to severe depressive symptoms and more than a quarter of people reported moderate to severe anxiety symptoms (6); Further longitudinal study found that there was no remarkable difference in anxiety and depressive levels (7).
Standardized training for resident physicians is the most critical stage from medical students to independent doctors (8, 9), residents would face multiple pressures not only in daily life and work but also in various training and assessments. Some physicians are prone to job burnout, which is a mental syndrome caused by persistent work pressure leading to emotional exhaustion, personality disintegration, and impaired personal achievement (10). The topic of burnout has dominated research on medical personnel (11). Previous studies have shown that the prevalence of burnout among physicians was particularly high. The prevalence of job burnout among medical workers (12), primary care practitioners (13), practicing physicians (14), and medical students (15) reached 24, 40.3, 50, and 71%, respectively. Medical workers experienced unprecedented stress related to work since the outbreak of COVID-19 (16). At the end of 2022, China released the COVID-19 epidemic restriction, and a widespread pandemic trend emerged. Resident physicians assumed important responsibilities for the treatment of COVID-19 patients. Due to the lack of human resources, the workload was increased significantly, for instance, during the outbreak of the epidemic, many frontline medical staff worked an average of 16 h or more per day (17). Some resident physicians persisted in work and practice tasks despite their own infections.
In this situation, the likelihood of psychological problems among medical workers increased. As mentioned earlier, there have been studies of anxiety, depression, and job burnout among medical workers, but there was relatively little discussion on vicarious trauma for resident physicians during the epidemic. In addition to common psychological problems such as anxiety and depression, vicarious trauma was also within the scope of our research. Previous studies on major traumatic events (such as post-disaster studies) usually involved the assessment of vicarious trauma (18). When medical workers took care of patients infected with COVID-19, the risk of infection increased sharply. They had empathy for patients’ uncomfortable symptoms and pain, and were prone to vicarious trauma symptoms, further leading to serious physical and mental distress (19, 20).
The outbreak of infectious diseases meant that resident physicians were facing many stressful events. The epidemic itself was a negative life event for everyone, and its impact on medical workers was even greater (16). The consequences faced on the pandemic were all negative events such as inconvenient living, increased work pressure, and shortage of medical resources (21). A longitudinal study of medical workers found that outcomes such as depression, hopelessness, fatigue, fear of going to work, fear of missing work, and worry about caring for family members that worsened at the start of the pandemic did not statistically improve over time (22). Different individuals may have different outcomes when dealing with negative events in different coping ways. Coping is defined as the cognitive and behavioral strategy to deal with the internal and external needs of an interaction with the environment when he or she judges that such interaction may be trouble to him/herself, even beyond the self-resources (23). Coping includes five conceptual domains: social support, avoidance strategies, a positive attitude, problem orientation and transcendent orientation (24). A study revealed that avoidance, problem orientation, and social support coping worsened professional quality of life, whereas a positive attitude improved it (24). A review of the psychological health condition of medical personnel during COVID-19 pointed out that many situations were normal reactions to the pandemic. They also had negative psychological effects such as burnout, compassion fatigue, anxiety, and depression (25).
During this special period, resident physicians’ psychological health status deserved attention. Most of the psychological health data of medical staff related to the COVID-19 epidemic were during the early stages of the pandemic outbreak. To the best of our knowledge, not much research has been done on mental health in China since the COVID 19 restrictions were lifted. Therefore, our study investigated the prevalence of anxiety, depression, and somatic symptoms among resident physicians around one month after the COVID-19 pandemic was lifted from lockdown, and the relationship between anxiety, depression, somatic symptoms, job burnout, vicarious trauma, and different backgrounds, negative events, social support, coping styles which were factors that might be related to the occurrence of the psychological health issues. The study investigated protective and risk factors for psychological status following China’s lifting of lockdown due to the COVID-19 pandemic. Targeted interventions to enhance the well-being of residents can be guided by identifying populations at higher risk for anxiety, depression, burnout, and secondary traumatic stress.
A cross-sectional survey using designed questionnaires including Generalized Anxiety Disorder 7-item (GAD-7), Patient Health Questionnaire 9-item (PHQ-9), Patient Health Questionnaire 15-item (PHQ-15), Maslach Burnout Inventory-General Survey (MBI-GS), vicarious traumatization questionnaire, negative event questionnaire, Perceived Social Support Scale (PSSS) and coping style scale, was conducted one month after the release of the COVID-19 pandemic restrictions among resident training physicians of a tertiary first-class hospital in Zhejiang. The data was collected online from January 21 to February 9, 2023, through a mobile online questionnaire format1 (one widely used electronic survey platform in China). According to the official list of resident physicians in the hospital, we stented the QR code of the questionnaire to every resident physician one by one through an online work platform (“Ding-Ding”). The inclusion criteria were: resident physicians, working in a tertiary first-class hospital in Zhejiang, obtaining informed consent. The exclusion criteria were: any other general or specialty physicians, or medical students or other medical workers. The survey platform did not allow the participants to left blank in the question, which helped us exclude the result of those participants. And we had checked the data, ensuring all the results we got were most-likely logical.
The data was gathered using an online, self-administered, anonymous survey method. At the beginning of the questionnaire, the informed consent form was placed to ensure every participant should provide their informed consent and make sure they are suitable for this survey before completing the survey questions. If the resident physicians did not offer their consent, they could not answer the following questions to finish this survey. The goal of the study and the procedures for completing it were explained in detail to the participants. The main part of the questionnaires consisted of general personal information and measure scales. General personal information included: age, gender, year of residency, marital status, training type, and educational level.
This study has been approved by the ethics committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (the ethical committee’s reference number: 20230216).
Anxiety was evaluated via GAD-7 (26) which is an effective tool for sifting anxiety and evaluating its degree in clinical practice and study. It’s a 7-item scale with a 4-point rating system. It’s calculated by assigning scores of 0, 1, 2, and 3, to the response categories of “not at all,” “several days,” “more than half the days,” and “nearly every day,” respectively, and adding together the scores for the seven questions. Total scores range from 0 to 21. In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.9389) and the scale was used in the study by Chen et al. (27). In our study, participants with GAD-7 scores ≥10 indicated remarkable anxious symptoms.
The PHQ-9 (28) was employed to assess the level of depressive symptoms among resident physicians. It’s a 9-item scale developed for assessing depressive disorders in primary care populations. It’s calculated by assigning scores of 0, 1, 2, and 3, to the response categories of “not at all,” “several days,” “more than half the days,” and “nearly every day,” respectively, and adding together the scores for the nine questions. Total scores range from 0 to 27. In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.9234) and the scale was used in the study by Chen et al. (27). In our study, participants with PHQ-9 scores≥10 were considered as having depression status.
The PHQ-15 (29) was employed to assess somatic symptoms. Each item is calculated by assigning scores of 0, 1, and 2, to the response categories of “not at all,” “a little,” and “often,” respectively, and adding together the scores for the 15 questions. Total scores range from 0 to 30. In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.9081) and the scale was used in the study by Xuedong et al. (30). In our study, participants with PHQ-15 scores≥10 were considered as having somatic symptoms.
The Maslach Burnout Inventory-General Survey (MBI-GS) (31) was used to assess the job burnout of resident physicians. There are 22 items with a 7-point rating system. The items of the scale are divided into three dimensions including emotional exhaustion, personal accomplishment and depersonalization, the scores are calculated separately. Resident physicians select relevant items based on their own situation in the past month. In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.8839) and the scale was used in the study by Gao et al. (32). In our study, participants defined the presence of job burnout symptoms by the median of the scale.
The vicarious trauma section of this study consisted of 29 questions, which were developed by the Department of Psychology and Behavioral Science of Zhejiang University specifically for medical personnel (33). Response options were “very mismatched,” “relatively mismatched,” “neutral,” “relatively matched,” and “very matched” scored as 0, 1, 2, 3 and 4. In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.9679). In our study, participants defined the presence of vicarious trauma symptoms by the median of the scale.
In this survey, we measured the impact of negative events, social support, coping style, vicarious trauma, and job burnout. To fit the clinical work environment discussed in this study, the scales we have chosen were as follows:
The negative event assessment was a series of 9 questions closely related to residents, namely, “relatives and friends are ill/seriously injured/dead,” “spouse is ill/seriously injured/dead,” “I am ill/seriously injured,” “financial difficulties,” “work and study pressure,” “conflict with colleagues or superiors,” “major changes in life rules (such as diet, sleep, and exercise),” “death of the patient in charge” and “other events.” Select “yes” or “no.” If “yes” was selected, further evaluation of the impact of the negative event was needed from 0 to 10.
The social support section used the Perceived Social Support Scale (PSSS), consisting of 12 questions (34). Response options were “strongly disagree,” “very disagree,” “slightly disagree,” “neutral,” “slightly agree,” “very agree,” and “strongly agree,” which were scored as 0, 1, 2, 3,4,5,6,7. The total score ranges from 12 to 84. A score between 12 and 36 indicates low support, 37–60 indicates medium support and 61–84 indicates high support (35). In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.9278) and the scale was used in the study by Guo et al. (36).
The coping style section included 36 questions (37). Response options were “never taken,” “occasionally taken,” “sometimes taken,” and “often taken” scored as 0, 1, 2, 3. Determine whether the resident physicians were problem-centered or emotional coping styles based on this scale. In this sample, the scale demonstrated good internal consistency (Cronbach’s alpha = 0.8788).
Other information collected in the questionnaire included work status (whether you were at work after lifting the lockdown), service category (whether there was a temporary change of job position in the past month), workload (average clinical working hours per week in the past month), daily sleep duration (average sleep time on working days in the past month).
Data analysis was conducted using STATA15.1. The Shapiro–Wilk test was used to examine the normality of continuous variables. Spearman correlation analysis was used to evaluate the correlation coefficients between various variables. According to the above scale norms, we have divided depression, anxiety, somatic symptoms, job burnout, and vicarious trauma scores into two types. The proportion of anxiety, depression, and somatic symptoms was calculated among resident physicians. To examine the differences between independent variables and the risk of depression, anxiety, somatic symptoms, job burnout, and vicarious trauma, Chi-square tests, and U-tests were used. A collinearity test was performed on the independent variable, and the variance expansion factor was calculated; we analyzed between independent variables and anxiety, depression, somatic symptoms, job burnout, and vicarious trauma in univariate logistic regression and multivariate logistic regression and calculated OR (odds ratio) and 95% CI (confidence interval). All tests were two-tailed, with a significance level of p < 0.05.
In this survey, 340 resident physicians completed all the required questionnaires. The demographic details are presented in Table 1. The mean age of the participants was 26.02 ± 2.90 years. The proportion of females (54.12%) was slightly higher than males (45.88%). Among the participants, different year of residency accounted for 41.76% (first), 33.53% (second), and 24.71% (third) respectively. 87.35% of them were unmarried. About half of the resident physicians were commissioned by other hospitals to receive training at our Hospital. 76.18% of them had a bachelor’s degree. During this period, 92.65% of resident physicians participated in the medical care for COVID-19 patients; 85.59% of resident physicians worked more than 40 h per week, 39.41% worked more than 49 h per week; 55.29% of resident physicians had less than 7 h of sleep per day. The results of the current study showed that there was a significant relationship between the year of residency and the prevalence of depression symptoms (p = 0.019), with the highest percentage of symptoms occurring in the third year of residency (39.29%). There were significant relationships between the age (p = 0.022), year of residency (p = 0.033), workload (p = 0.011) and the prevalence of anxiety symptoms, with the highest percentage of symptoms occurring in the third year of residency (30.95%) and workload>49 h (29.10%). There were significant relationships between the educational level (p = 0.037), daily sleep duration (p < 0.001), and the prevalence of somatic symptoms, with the highest percentage of symptoms occurring in the master (51.35%) and daily sleep duration<7 h (51.06%). There were significant relationships between the educational level (p = 0.014), work status (p = 0.014), daily sleep duration (p = 0.037) and the prevalence of job burnout, with the highest percentage of symptoms occurring in the undergraduate (55.60%), absent from work (76.00%), daily sleep duration<7 h (58.51%). There was a significant relationship between the gender and the prevalence of vicarious trauma (p = 0.015), with the higher percentage of symptoms occurring in man (58.33%).
The prevalence of anxiety (GAD-7 ≥ 10), depression (PHQ-9 ≥ 10), and somatic symptoms (PHQ-15 ≥ 10) in this study reached 20.88, 28.53, and 41.47%, respectively. Details are shown in Table 2.
Female resident physicians were more likely to experience somatic symptoms [adjusted OR = 2.36, 95% CI: 1.33–4.18] compared with males. The second-year resident physicians were less likely to report depression (adjusted OR = 0.41, 95% CI: 0.19–0.91) compared with the first-year resident physicians. Compared with resident physicians with a bachelor’s degree, resident physicians with a doctoral degree were less likely to experience somatic symptoms and job burnout (adjusted OR = 0.25, 95% CI: 0.09–0.67; adjusted OR = 0.31, 95% CI: 0.11–0.89). Resident physicians who were not on duty or had not been transferred were less likely to experience vicarious trauma symptoms (adjusted OR = 0.21, 95% CI: 0.06–0.73; adjusted OR = 0.35, 95% CI: 0.18–0.64). Resident physicians’ problem-focused coping styles were less prone to depression (adjusted OR = 0.92, 95% CI: 0.88–0.96), anxiety (adjusted OR = 0.94, 95% CI: 0.90–0.98), somatic symptoms (adjusted OR = 0.93, 95% CI: 0.89–0.97), job burnout (adjusted OR = 0.91, 95% CI: 0.87–0.96), and vicarious trauma (adjusted OR = 0.94, 95% CI: 0.90–0.98). Resident physicians’ emotion-focused coping styles and who experienced negative life events were more prone to anxiety (adjusted OR = 1.13, 95% CI: 1.08–1.17; adjusted OR = 1.05, 95% CI: 1.03–1.08), depression (adjusted OR = 1.11, 95% CI: 1.07–1.16; adjusted OR = 1.05, 95% CI: 1.03–1.07), somatic symptoms (adjusted OR = 1.10, 95% CI: 1.06–1.14; adjusted OR = 1.06, 95% CI: 1.04–1.08), job burnout (adjusted OR = 1.16, 95% CI: 1.11–1.20; adjusted OR = 1.03, 95% CI: 1.01–1.06), and vicarious trauma (adjusted OR = 1.13, 95% CI: 1.09–1.17; adjusted OR = 1.05, 95% CI: 1.02–1.07). Details are shown in Table 3.
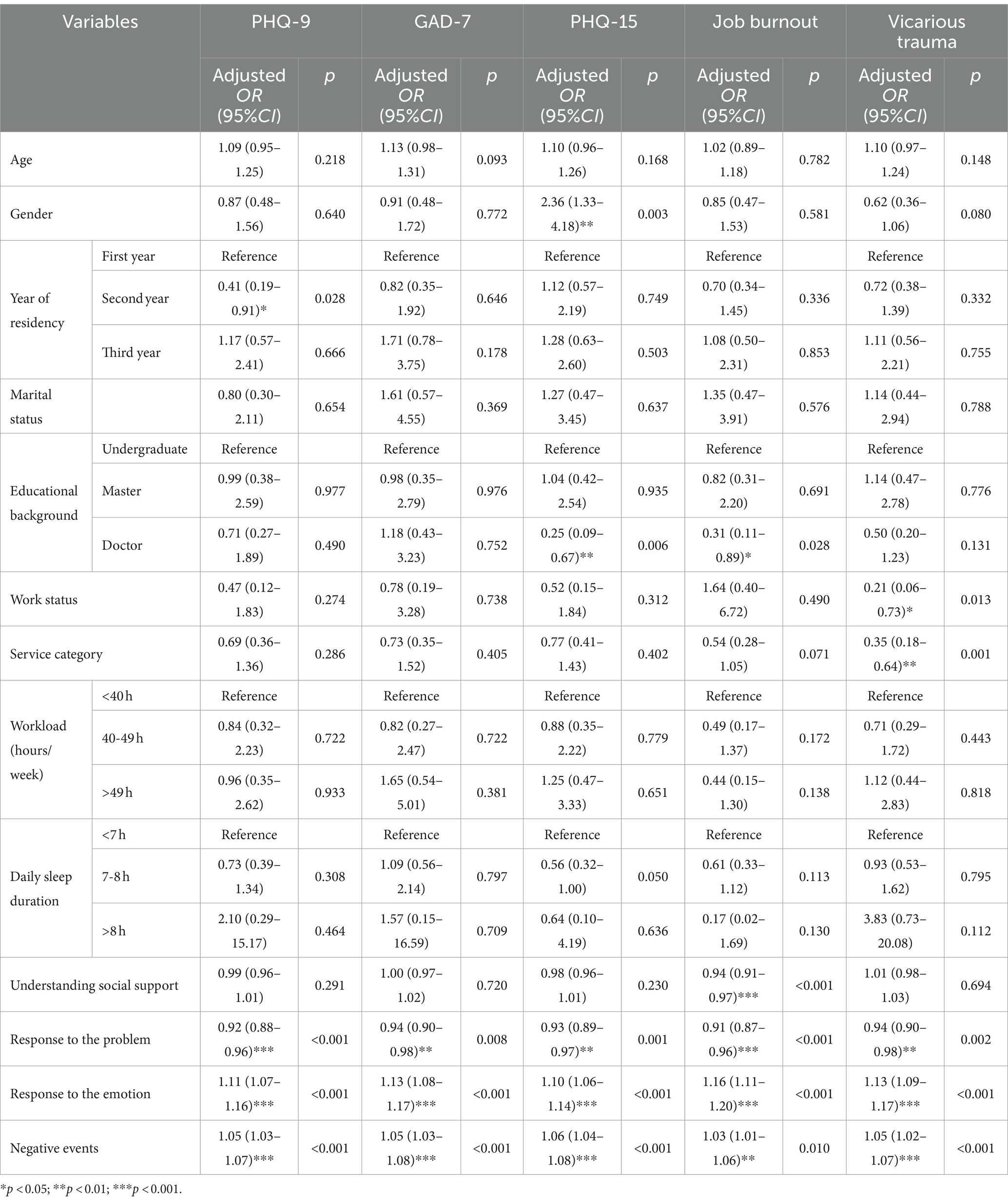
Table 3. Multivariate logistic regression analysis on resident physicians of factors influencing psychological status.
This online survey investigates the psychological status of resident physicians in a tertiary hospital in the early stages of lifting the COVID-19 lockdown in China. The uniqueness of this study lay in the series of questionnaire surveys we conducted on a specific population in a special background, in addition to evaluating anxiety and depression, it also included relevant assessments of somatic symptoms, job burnout, and vicarious trauma among resident physicians. The main findings of this study are as follows. Firstly, in the early stages of lifting the COVID-19 lockdown in China, the prevalence of anxiety, depression, and somatic symptoms among resident physicians in the standardized training stage was high. An important finding was that 41.47% of resident physicians had significant somatic symptoms. We also found that there was a correlation between sleep time and somatic symptoms, and the shorter the sleep time, the more likely to experience somatic symptoms such as fatigue. Secondly, the study also found a correlation between certain psychological problems and age, gender, year of residency, and educational level. Thirdly, resident physicians who were not on duty or had not been transferred were less likely to experience vicarious trauma symptoms. Fourthly, adequate social support was less likely to lead to job burnout. Lastly, resident physicians’ problem-focused coping styles were less prone to depression, anxiety, somatic symptoms, job burnout, and vicarious trauma; Resident physicians’ emotion-focused coping styles and experienced negative life events were more prone to anxiety, depression, somatic symptoms, job burnout, and vicarious trauma. Then, we will discuss our findings separately.
After the outbreak of COVID-19, China has been prevented and controlled for nearly three years, and there has been no large-scale spread. On December 26, 2022, the National Health Commission issued a notice: With the approval of the State Council, as of January 8, 2023, the measures for the prevention and control of Class A infectious diseases stipulated in the Law of the People’s Republic of China on the Prevention and Control of Infectious Diseases against COVID-19 would be lifted. COVID-19 outburst in the short term. Almost everyone was infected with COVID-19. All wards were receiving patients with COVID-19. Medical workers face multiple physical and psychological challenges. In our study, we found that in the early stages of lifting the COVID-19 lockdown in China, the prevalence of anxiety, depression, and somatic symptoms among resident physicians in the standardized training stage were 20.88, 28.53, and 41.47%. Previous studies have also shown that resident physicians had high levels of depression and emotional problems (8, 9, 38). The results of one system review showed that 20.9–43.2% of resident physicians had depression and depressive symptoms (9). An important finding was that about half of resident physicians had more somatic symptoms. We analyzed that this phenomenon might be related to a sharp increase in workload and a decrease in sleep time. Correlation analysis in our study indeed found a remarkable negative association between daily sleep time and somatic symptoms. Research has found that in addition to working hours (10), the sleep time (39) and poor sleep quality (40) of resident physicians were also related to fatigue. Fortier’s study has shown a potential cross-sectional relationship between insomnia and fatigue (41). Many studies confirmed that sleep time was an important predictor of fatigue the next day (42, 43). Insufficient sleep (≤ 6 h per night) increases the risk of depression among resident physicians and might lead to higher medical error rates (39, 44, 45).
In our study, we found a positive association between age and anxiety. Medical students in the higher (>22 years) age group in Nepal suffered from elevated levels of anxiety and/or depression during COVID-19 (46). The age of resident physicians in our study was similar to that of medical students in Nepal and similar conclusions were found. The reason for similar conclusions might be related to the similarity of research background and population. We also found gender and grade differences in certain assessment content. For example, compared to males, female resident physicians were more likely to experience somatic symptoms. In the past, many studies focused on the somatic symptoms of peri-menopausal (47) and older females (48), and compared to males, the prevalence of somatic symptoms in females during this period were higher. Although this conclusion was similar to ours and had some reference value, comparability decreased due to other factors such as age and occupation. However, there was also a study that suggested that females were seeking medical help more frequently due to somatic symptoms (49). We also found similar conclusions regarding the specific female population in our study, which was also a part of the female population. Compared with first-year resident physicians, resident physicians in the second year of training stage were less likely to report depression, which was related to the fact that second-year resident physicians had a relatively easy year, unlike the first-year resident physicians who just arrived in the new environment and was in the adaptation stage, also unlike the third-year resident physicians who at the last year of standardized training and faced more challenges and tests, bore more work responsibilities and also faced more pressure in terms of assessment. Moreover, we found that compared with resident physicians with a bachelor’s degree, resident physicians with a doctoral degree were less likely to experience somatic symptoms and job burnout; More research on PhD students showed that PhD students demonstrated a remarkably higher level of emotional problems, somatic symptoms and sleep issues compared to persons who had not received further education after obtaining a master’s degree (50). A previous study about academic medicine faculty found that teachers with master’s and doctoral degrees had a higher risk of depression and anxiety (51). Our research conclusions seemed to be inconsistent with many previous research conclusions. One possible reason was that our research subjects were resident physicians who had already worked and were not students on campus. Additionally, we concluded that resident physicians were less likely to experience somatic symptoms and job burnout. Previous studies have focused more on anxiety and depression symptoms. Further research is needed to analyze the specific reasons in the future.
Our study found that resident physicians who were not on duty or had not been transferred were less likely to experience vicarious trauma symptoms; some resident physicians were not on duty due to policy reasons or COVID-19 infection, they seldom contacted or managed COVID-19 patients, so they were less impacted and less likely to have vicarious trauma symptoms. Many resident physicians have been transferred from their original posts to emergency, infection department, intensive care unit, and other departments due to work needs, and were more likely to have vicarious trauma symptoms when facing COVID-19 patients directly.
Good social support was less likely to lead to job burnout; Similar to a previous study that found that organizational support reduced burnout (52). Cardozo et al. also found that social support and healthy coping strategies were protective factors for depression, anxiety, and burnout (53). Extremely amount of work, document burden, declined regulation over workload, difficulty integrating into work and life, and loss of meaning in work were elements related to burnout (14). A multicenter prospective study on the pressure, anxiety, and job burnout of medical workers during COVID-19 in Singapore found that long working hours were closely related to anxiety and job burnout (12). A reasonable response to external stress and sufficient social support might reduce the occurrence of emotional problems and job burnout.
The study suggested that resident physicians’ problem-focused coping styles were less prone to depression, somatic symptoms, job burnout, and vicarious trauma; while resident physicians were more prone to feel anxiety, depression, somatic symptoms, job burnout, and vicarious trauma through emotion-focused coping styles. The found were similar to many researches. Cruz et al. found that problem-focused coping was negatively associated with depressive symptoms and impairments of social. And there was a remarkable positive association between emotion-focused coping and depressive symptoms (54). When facing negative stress events, positive coping styles were protective factors for anxiety and depression, while avoidance coping styles were risk factors for anxiety and depression (55, 56). Yan et al. also found that people who used positive coping measures felt fewer symptoms of depression, obsessive-compulsive anxiety, and neurasthenia under stress, while negative coping measures aggravated mood distress (57). Our study found a correlation between job burnout and coping styles. A major factor that might influence job burnout is a person’s coping style, which is the cognitive and behavioral efforts they make to cope with stress (54). Coping has two primary roles: adjusting unstable emotions and resolving emotional distress through cognitive and behavioral changes (58–60). The use of adaptive coping strategies has a positive impact on the body and mental health, stress management, and overall performance of medical staff (61). We can improve the psychological health status of resident physicians by educating them on reasonable coping strategies.
Negative life events were adverse factors for anxiety, depression, somatic symptoms, job burnout, and vicarious trauma. The more negative events, the easier it was to experience anxiety, depression, somatic discomfort, job burnout, and vicarious trauma. One study related to negative life events and mental health in adolescents, found the more frequent and intensive negative life events that adolescents experienced, the more likely they were to experience symptoms of depression and anxiety (62). Our study also collected and analyzed the negative events experienced by resident physicians within one month of the release of the COVID-19 pandemic restrictions. In the early stages of lifting the COVID-19 lockdown, everyone more or less experienced negative events related to the disease, and psychological health is hypersensitive to trauma incidents and their social and commercial outcomes (60). The pandemic was a crash process that endangered individual’s life and survival, with many traumatic effects on everyone’s physical and psychological well-being (59). Compared to the general population, resident physicians needed to undertake more work tasks and faced greater risks of infection, even had to work with diseases, in such difficult situation. The negative events experienced during this period were more frequent than usual, which might lead to a higher prevalence of anxiety, depression, somatic symptoms, job burnout, and vicarious trauma.
Restricted by special periods and populations, some limitations should be considered when explaining the findings of the present study. Firstly, all information was based on the self-report of the resident physicians. Secondly, all resident physicians’ data comes from only one large hospital, due to the impact of special period, the number of collected samples was relatively small, which may not represent all resident physicians in the standardized training stage. A larger multicenter sample size was needed to increase the representativeness of the data. Thirdly, this was a descriptive study, and confirming causal relationships was relatively difficult. Further longitudinal research should be utilized to address this relationship. Nevertheless, our study has added a survey of favorable factors related to psychological health status, which could provide a basis for developing relevant psychological intervention measures. Cognitive behavioral therapy (CBT) and crisis intervention have been considered helpful intervention strategies for managing the psychological health results of medical staff (63). In addition, protective and risk factors for anxiety, depression, somatic symptoms, job burnout, and vicarious trauma identified among resident physicians provided valuable information for developing relevant psychological intervention measures to improve the psychological health of relevant groups after the outbreak of infectious diseases. Further longitudinal researches also need to be confirmed.
This study found that resident physicians had a high prevalence of anxiety, depression, and somatic symptoms during the release of COVID-19 pandemic restrictions. Internal and external factors of residents were correlated with the occurrence of anxiety, depression, somatic symptoms, job burnout, and vicarious trauma. Risk and protective factors related to the psychological health of residents have been proposed. These findings suggested that interventions aimed at reducing working hours and workload, ensuring sufficient sleep time, promoting problem-focused coping strategies, strengthening regular communication and mental health education or intervention, might help improve the psychological health status of resident physicians and their ability to cope with complex tasks.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the ethics committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
QZ: Conceptualization, Writing – original draft, Writing – review & editing. RP: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. QP: Data curation, Formal analysis, Writing – review & editing. YQ: Formal analysis, Writing – review & editing. XZ: Conceptualization, Writing – review & editing. QC: Conceptualization, Methodology, Project administration, Resources, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research is partly sponsored by grants from the National Science Foundation of China (NSFC) under Grant Number 82090030, 82372013.
We sincerely thank all the participants in this study. The views expressed in this paper are not necessarily those of departments or institutions. Any omission or negligence is the responsibility of the author.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
COVID-19, Corona Virus Disease 2019; GAD-7, Generalized Anxiety Disorder Assessment; PHQ-9, Patient Health Questionnaire-9; PHQ-15, Patient Health Questionnaire-15; PSSS, Perceived Social Support Scale; MBI-GS, The Maslach Burnout Inventory-General Survey.
1. Chew, NWS, Lee, GKH, Tan, BYQ, Jing, M, Goh, Y, Ngiam, NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
2. Lee, BEC, Ling, M, Boyd, L, Olsson, C, and Sheen, J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: a systematic review and meta-analysis. J Affect Disord. (2023) 330:329–45. doi: 10.1016/j.jad.2023.03.012
3. Yuan, L, Lu, L, Wang, X, Qu, M, Gao, Y, and Pan, B. Comorbid anxiety and depressive symptoms and the related factors among international medical students in China during COVID-19 pandemic: a cross-sectional study. BMC Psychiatry. (2023) 23:165. doi: 10.1186/s12888-023-04638-7
4. Zhang, M, Qin, L, Zhang, D, Tao, M, Han, K, Chi, C, et al. Prevalence and factors associated with insomnia among medical students in China during the COVID-19 pandemic: characterization and associated factors. BMC Psychiatry. (2023) 23:140. doi: 10.1186/s12888-023-04556-8
5. Kang, J, Wang, D, Duan, Y, Zhai, L, Shi, L, and Guo, F. Aerobic exercise prevents depression via alleviating hippocampus injury in chronic stressed depression rats. Brain Sci. (2020) 11:9. doi: 10.3390/brainsci11010009
6. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, Ho, CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
7. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, McIntyre, RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
8. Ishak, WW, Lederer, S, Mandili, C, Nikravesh, R, Seligman, L, Vasa, M, et al. Burnout during residency training: a literature review. J Grad Med Educ. (2009) 1:236–42. doi: 10.4300/JGME-D-09-00054.1
9. Mata, DA, Ramos, MA, Bansal, N, Khan, R, Guille, C, Di Angelantonio, E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. (2015) 314:2373–83. doi: 10.1001/jama.2015.15845
10. Maslach, C, Schaufeli, WB, and Leiter, MP. Leiter MP, Job burnout. Annu Rev Psychol. (2001) 52:397–422. doi: 10.1146/annurev.psych.52.1.397
11. Mihailescu, M, and Neiterman, E. A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America. BMC Public Health. (2019) 19:1363. doi: 10.1186/s12889-019-7661-9
12. Teo, I, Chay, J, Cheung, YB, Sung, SC, Tewani, KG, Yeo, LF, et al. Healthcare worker stress, anxiety and burnout during the COVID-19 pandemic in Singapore: a 6-month multi-centre prospective study. PLoS One. (2021) 16:e0258866. doi: 10.1371/journal.pone.0258866
13. Goehring, C, Bouvier Gallacchi, M, Künzi, B, and Bovier, P. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners a cross-sectional survey. Swiss Med Wkly. (2005) 135:101–8. doi: 10.4414/smw.2005.10841
14. Shanafelt, TD, Dyrbye, LN, and West, CP. Addressing physician burnout: the way forward. JAMA. (2017) 317:901–2. doi: 10.1001/jama.2017.0076
15. Mazurkiewicz, R, Korenstein, D, Fallar, R, and Ripp, J. The prevalence and correlations of medical student burnout in the pre-clinical years: a cross-sectional study. Psychol Health Med. (2012) 17:188–95. doi: 10.1080/13548506.2011.597770
16. Si, MY, Su, XY, Jiang, Y, Wang, WJ, Gu, XF, Ma, L, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. (2020) 9:113. doi: 10.1186/s40249-020-00724-0
17. Wang, K, Yang, B, Wu, C, and Zheng, L. The moderation of satisfaction with working conditions in the association between workload and mental health among healthcare workers collecting test samples in the post-COVID-19 era. Front Public Health. (2023) 11:1106299. doi: 10.3389/fpubh.2023.1106299
18. Kim, J, Chesworth, B, Franchino-Olsen, H, and Macy, RJ. A scoping review of vicarious trauma interventions for service providers working with people who have experienced traumatic events. Trauma Violence Abuse. (2022) 23:1437–60. doi: 10.1177/1524838021991310
19. Ruiz-Fernández, MD, Ramos-Pichardo, JD, Ibáñez-Masero, O, Cabrera-Troya, J, Carmona-Rega, MI, and Ortega-Galán, ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. (2020) 29:4321–30. doi: 10.1111/jocn.15469
20. Werner, EA, Aloisio, CE, Butler, AD, D'Antonio, KM, Kenny, JM, Mitchell, A, et al. Addressing mental health in patients and providers during the COVID-19 pandemic. Semin Perinatol. (2020) 44:151279. doi: 10.1016/j.semperi.2020.151279
21. Jia, L, Ye, M, Wang, H, and Wang, H. Physical discomforts, feeling of the high work intensity and the related risk factors of the frontline medical staff during COVID-19 epidemic: an early-outbreak, national survey in China. Front Public Health. (2023) 11:1270366. doi: 10.3389/fpubh.2023.1270366
22. Patel, R, and Foster, T. Longitudinal assessment of physician wellness during the COVID-19 pandemic. Psychiatry Res. (2022) 316:114739. doi: 10.1016/j.psychres.2022.114739
23. Folkman, S, and Moskowitz, JT. Coping: pitfalls and promise. Annu Rev Psychol. (2004) 55:745–74. doi: 10.1146/annurev.psych.55.090902.141456
24. Calegari, JG, Russo, S, Luciani, M, Strepparava, MG, Di Mauro, S, and Ausili, D. Association between coping strategies and professional quality of life in nurses and physicians during COVID-19: a cross-sectional study. J Nurs Manag. (2022) 30:4054–63. doi: 10.1111/jonm.13845
25. Walton, M, Murray, E, and Christian, MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. (2020) 9:241–7. doi: 10.1177/2048872620922795
26. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
27. Chen, H, Feng, H, Liu, Y, Wu, S, Li, H, Zhang, G, et al. Anxiety, depression, insomnia, and PTSD among college students after optimizing the COVID-19 response in China. J Affect Disord. (2023) 337:50–6. doi: 10.1016/j.jad.2023.05.076
28. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9 validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
29. Kroenke, K, Spitzer, RL, Williams, JB, and Lowe, B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
30. Xuedong, AN, Qing, Z, Junxiu, T, Li, LI, Yun, C, Kejian, LI, et al. Shugan Jieyu capsule improve sleep and emotional disorder in coronavirus disease 2019 convalescence patients: a randomized, double-blind, placebo-controlled trial. J Tradit Chin Med. (2022) 42:803–9. doi: 10.19852/j.cnki.jtcm.20220719.003
31. Maslach, C, and Jackson, SE. The measurement of experienced burnout. J Organ Behav. (1981) 2:99–113. doi: 10.1002/job.4030020205
32. Gao, X, Ma, KL, Wang, H, Gao, Q, Lei, LJ, and Wang, T. Association of sleep quality with job burnout among Chinese coal mine staff: a propensity score weighting analysis. Sci Rep. (2019) 9:8737. doi: 10.1038/s41598-019-45329-2
33. Zhang, Q.Q. (2022) Development of the scale and the influencing mechanism of medics’ vicarious traumatization, in Zhejiang University, Hang Zhou (CHN)
34. Dahlem, NW, Zimet, GD, and Walker, RR. The multidimensional scale of perceived social support a confirmation study. J Clin Psychol. (1991) 47:756–61. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l
35. Liu, Y, Zhang, L, Guo, N, and Jiang, H. Postpartum depression and postpartum post-traumatic stress disorder: prevalence and associated factors. BMC Psychiatry. (2021) 21:487. doi: 10.1186/s12888-021-03432-7
36. Guo, K, Zhang, X, Bai, S, Minhat, HS, Nazan, A, Feng, J, et al. Assessing social support impact on depression, anxiety, and stress among undergraduate students in Shaanxi province during the COVID-19 pandemic of China. PLoS One. (2021) 16:e0253891. doi: 10.1371/journal.pone.0253891
37. Chen, SL, Zheng, OQ, Pan, JN, and Zhen, SS. Preliminary development of coping style scale for middle school students. Chin J Clin Psych. (2000) 8:211–2. doi: 10.1186/s12913-016-1423-5
38. Fang, Y, Bohnert, ASB, Pereira-Lima, K, Cleary, J, Frank, E, Zhao, Z, et al. Trends in depressive symptoms and associated factors during residency, 2007 to 2019: a repeated annual cohort study. Ann Intern Med. (2022) 175:56–64. doi: 10.7326/M21-1594
39. Gopal, R, Glasheen, JJ, Miyoshi, TJ, and Prochazka, AV. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. (2005) 165:2595–600. doi: 10.1001/archinte.165.22.2595
40. Jaradat, R, Lahlouh, A, and Mustafa, M. Sleep quality and health related problems of shift work among resident physicians: a cross-sectional study. Sleep Med. (2020) 66:201–6. doi: 10.1016/j.sleep.2019.11.1258
41. Fortier-Brochu, E, Beaulieu-Bonneau, S, Ivers, H, and Morin, CM. Relations between sleep, fatigue, and health-related quality of life in individuals with insomnia. J Psychosom Res. (2010) 69:475–83. doi: 10.1016/j.jpsychores.2010.05.005
42. Smith, RA, Lack, LC, Lovato, N, and Wright, H. The relationship between a night's sleep and subsequent daytime functioning in older poor and good sleepers. J Sleep Res. (2015) 24:40–6. doi: 10.1111/jsr.12237
43. Harris, AL, Carmona, NE, Moss, TG, and Carney, CE. Testing the contiguity of the sleep and fatigue relationship: a daily diary study. Sleep. (2021) 44:zsaa252. doi: 10.1093/sleep/zsaa252
44. Wallace, JE, Lemaire, JB, and Ghali, WA. Physician wellness a missing quality indicator. Lancet (London, England). (2009) 374:1714–21. doi: 10.1016/S0140-6736(09)61424-0
45. Kalmbach, DA, Arnedt, JT, Song, PX, Guille, C, and Sen, S. Sleep disturbance and short sleep as risk factors for depression and perceived medical errors in first-year residents. Sleep. (2017) 40:zsw073. doi: 10.1093/sleep/zsw073
46. Risal, A, Shikhrakar, S, Mishra, S, Kunwar, D, Karki, E, Shrestha, B, et al. Anxiety and depression during COVID-19 pandemic among medical students in Nepal. Kathmandu Univ Med J (KUMJ). (2020) 18:333–9. doi: 10.3126/kumj.v18i4.49241
47. McCall-Hosenfeld, JS, Winter, M, Heeren, T, and Liebschutz, JM. The association of interpersonal trauma with somatic symptom severity in a primary care population with chronic pain: exploring the role of gender and the mental health sequelae of trauma. J Psychosom Res. (2014) 77:196–204. doi: 10.1016/j.jpsychores.2014.07.011
48. Eslami, B, Di Rosa, M, Barros, H, Torres-Gonzalez, F, Stankunas, M, Ioannidi-Kapolou, E, et al. Lifetime abuse and somatic symptoms among older women and men in Europe. PLoS One. (2019) 14:e0220741. doi: 10.1371/journal.pone.0220741
49. Ballering, AV, Olde Hartman, TC, Verheij, R, and Rosmalen, JGM. Sex and gender differences in primary care help-seeking for common somatic symptoms: a longitudinal study. Scand J Prim Health Care. (2023) 41:132–9. doi: 10.1080/02813432.2023.2191653
50. Pizunska, D, Golinska, PB, Malek, A, and Radziwillowicz, W. Well-being among PhD candidates. Psychiatr Pol. (2021) 55:901–14. doi: 10.12740/PP/OnlineFirst/114121
51. Uristemova, A, Myssayev, A, Meirmanov, S, Migina, L, Pak, L, and Baibussinova, A. Prevalence and associated factors of depression, anxiety, and stress among academic medicine faculty in Kazakhstan: a cross-sectional study. J Prev Med Hyg. (2023) 64:E215–25. doi: 10.15167/2421-4248/jpmh2023.64.2.2932
52. Gomez-Urquiza, JL, Monsalve-Reyes, CS, San Luis-Costas, C, Fernandez-Castillo, R, Aguayo-Estremera, R, and Canadas-de la Fuente, GA. Risk factors and burnout levels in primary care nurses: a systematic review. Aten Primaria. (2017) 49:77–85. doi: 10.1016/j.aprim.2016.05.004
53. Lopes Cardozo, B, Gotway Crawford, C, Eriksson, C, Zhu, J, Sabin, M, Ager, A, et al. Psychological distress, depression, anxiety, and burnout among international humanitarian aid workers: a longitudinal study. PLoS One. (2012) 7:e44948. doi: 10.1371/journal.pone.0044948
54. Portero de la Cruz, S, Cebrino, J, Herruzo, J, and Vaquero-Abellan, M. A multicenter study into burnout, perceived stress, job satisfaction, coping strategies, and general health among emergency department nursing staff. J Clin Med. (2020) 9:1007. doi: 10.3390/jcm9041007
55. Chen, J, Liu, X, Wang, D, Jin, Y, He, M, Ma, Y, et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:47–55. doi: 10.1007/s00127-020-01954-1
56. Wang, C, Havewala, M, and Zhu, Q. COVID-19 stressful life events and mental health: personality and coping styles as moderators. J Am Coll Heal. (2022) 1-10:1–10. doi: 10.1080/07448481.2022.2066977
57. Yan, L, Gan, Y, Ding, X, Wu, J, and Duan, H. The relationship between perceived stress and emotional distress during the COVID-19 outbreak: effects of boredom proneness and coping style. J Anxiety Disord. (2021) 77:102328. doi: 10.1016/j.janxdis.2020.102328
58. Guo, M, Gan, Y, and Tong, J. The role of meaning-focused coping in significant loss. Anxiety Stress Coping. (2013) 26:87–102. doi: 10.1080/10615806.2011.627507
59. Pfefferbaum, B, and North, CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMp2008017
60. Altundal Duru, H, Yılmaz, S, Yaman, Z, Boğahan, M, and Yılmaz, M. Individuals’ coping styles and levels of depression, anxiety, and stress during the COVID-19 pandemic in Turkey: a web-based cross-sectional study. SAGE Open. (2023) 13:21582440221148628. doi: 10.1177/21582440221148628
61. Abraham, LJ, Thom, O, Greenslade, JH, Wallis, M, Johnston, AN, Carlstrom, E, et al. Morale, stress and coping strategies of staff working in the emergency department: a comparison of two different-sized departments. Emerg Med Australas. (2018) 30:375–81. doi: 10.1111/1742-6723.12895
62. Sarbu, EA, Iovu, MB, and Lazar, F. Negative life events and internalizing problems among Romanian youth. Clin Child Psychol Psychiatry. (2022) 27:399–411. doi: 10.1177/13591045211055674
Keywords: COVID-19, anxiety, depression, somatic symptoms, job burnout, vicarious trauma, resident physicians
Citation: Zhang Q, Pan R, Pan Q, Qian Y, Zhou X and Chen Q (2024) Psychological status and related factors of resident physicians during the release of COVID-19 pandemic restrictions in China. Front. Public Health. 12:1322742. doi: 10.3389/fpubh.2024.1322742
Received: 16 October 2023; Accepted: 11 March 2024;
Published: 17 April 2024.
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Muna Ahmead, Al-Quds University, PalestineCopyright © 2024 Zhang, Pan, Pan, Qian, Zhou and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiaozhen Chen, Y3JhemlsQHpqdS5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.