- 1Department of Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, United Kingdom
- 2School of Medicine, Cardiff University, Cardiff, United Kingdom
- 3School of Healthcare Sciences, Cardiff University, Cardiff, United Kingdom
Background: Systematic review evidence suggests preconception health interventions may be effective in improving a range of outcomes. However, few studies have explored women’s views on potential content and delivery methods for these interventions.
Methods: Participants were purposively sampled from respondents (n = 313) of a survey. Semi-structured, in-depth interviews were conducted to explore their views on seven candidate delivery methods for preconception health interventions: general practitioners (GPs), nurse practitioners, pharmacists, social media, personal texts and emails, pregnancy tests, and health education in schools. Data were analyzed using a data-driven framework analysis.
Results: Twenty women were interviewed. Women wanted interventions to be easily accessible but allow them to conceal their pregnancy plans. They preferred to choose to receive preconception interventions but were receptive to health professionals raising preconception health during ‘relevant’ appointments such as contraceptive counseling and cervical smear tests. They wanted intervention content to provide trustworthy and positively framed information that highlights the benefits of good preconception health and avoids stigmatizing women for their weight and preconception actions. The inclusion of support for preconception mental health and the use of visual media, personalization, simple information, and interesting and unfamiliar facts were viewed favorably.
Conclusion: Interventions to improve preconception health should reflect the sensitivities of pregnancy intentions, be easy to access in a way that enables discretion, and be designed to seek consent to receive the intervention. These interventions should ideally be tailored to their target populations and provide trustworthy information from reputable sources. The potential for unintended harmful effects should be explored.
1 Introduction
Worldwide, there are around 23 million miscarriages (1), 2.4 million neonatal deaths (2), and 260,000 neural tube defect-affected pregnancies each year (3). There is high- and moderate-certainty evidence that maternal exposures before conception, such as a lack of dietary folate, high body mass index (BMI), interpregnancy weight gain and physical inactivity increase the risk of these outcomes and others (4). However, most women do not begin folate supplementation before pregnancy (5), 32% of reproductive-age women are not sufficiently active (6), and, in high-income countries, one in two reproductive-age women have an overweight or obese BMI (7, 8). These risk factors are more prevalent among minoritized ethnic and socioeconomically deprived women (8–10). Limited systematic review evidence suggests preconception health interventions may be effective in reducing the risk of congenital anomalies and alcohol-exposed pregnancies and in improving infants’ birth weight and women’s diets, physical activity and weight loss (11, 12). National health organizations have called for further research on preconception health interventions, and recommend that this research includes the views of the public (13–15) to increase intervention success and government buy-in (16, 17).
Few studies have explored reproductive-age women’s views and experiences of preconception health interventions. Most previous studies have focused on preconception care delivered in healthcare settings (18–25), of which half have focused on women with diabetes (18–21). Women with diabetes have reported fears of being judged, labeled or lectured and encountering an unsupportive or authoritative healthcare provider to be barriers to their engagement with preconception care, and reassuring and approachable healthcare staff to be facilitators (18–20). They value receiving high-quality information (20, 21) and seeing a healthcare professional who knows and understands them and has dedicated time for preconception counseling (19, 21). Studies with women without chronic conditions have reported cost, accessibility issues (e.g., for rural residents) (22), a lack of time (20), and a reluctance to disclose pregnancy intentions (23, 24) as barriers to their engagement with preconception care. They have reported the reliability of information from a health professional and being able to see a familiar and respectful female professional as facilitators (23, 24).
An issue with the literature’s primary focus on preconception care delivery in healthcare settings is that healthcare providers have consistently highlighted low patient demand for preconception care and a lack of contact with women planning a pregnancy (26–28). ‘Broader strategies’ involving a wider spectrum of stakeholders and community-based methods may therefore be required to promote preconception health (29, 30). This approach is supported by the findings of our recent survey of 835 women in England (31). We found social media, texts and emails, health education in schools, and pregnancy test packaging to be highly acceptable methods for delivering preconception health interventions, as well as doctors, midwives and nurses. Similarly, women in a qualitative study in England (24) expressed that information about preconception health should be more widely available in the community, particularly in schools. A subsequent focus group study in Northern Ireland (25) reported that women and men generally favored non-medical sources of preconception health information, such as family and friends, the internet and social media.
A limitation of these previous qualitative studies was their use of convenience samples, where participants were opportunistically recruited via posters and university-wide emails (25) and pre-existing social groups (24). This meant their authors did not purposively recruit women representing a range of socio-demographic characteristics and attitudes toward candidate methods for preconception health interventions. Nor did they explore women’s views on content for these interventions. This qualitative study therefore aimed to explore reproductive-age women’s views on potential delivery methods and content for interventions to improve preconception health.
2 Materials and methods
2.1 Study design and researcher characteristics
This exploratory qualitative study constituted the second phase of a mixed methods project investigating acceptable preconception health intervention designs (31) and involved semi-structured, in-depth interviews with women aged 18–48 years. The study was undertaken from a position of critical realism (32). Data were iteratively collected and analyzed using a data-driven, framework analysis approach (33), which complemented this position (34). The study received ethical approval from the South West – Frenchay Research Ethics Committee before its conduct (19/SW/0235) and is reported following Standards for Reporting Qualitative Research guidelines (35). The study team comprised investigators with backgrounds in public health research and practice, epidemiology, psychology and midwifery. All had prior experience of qualitative research.
2.2 Study population and participant selection
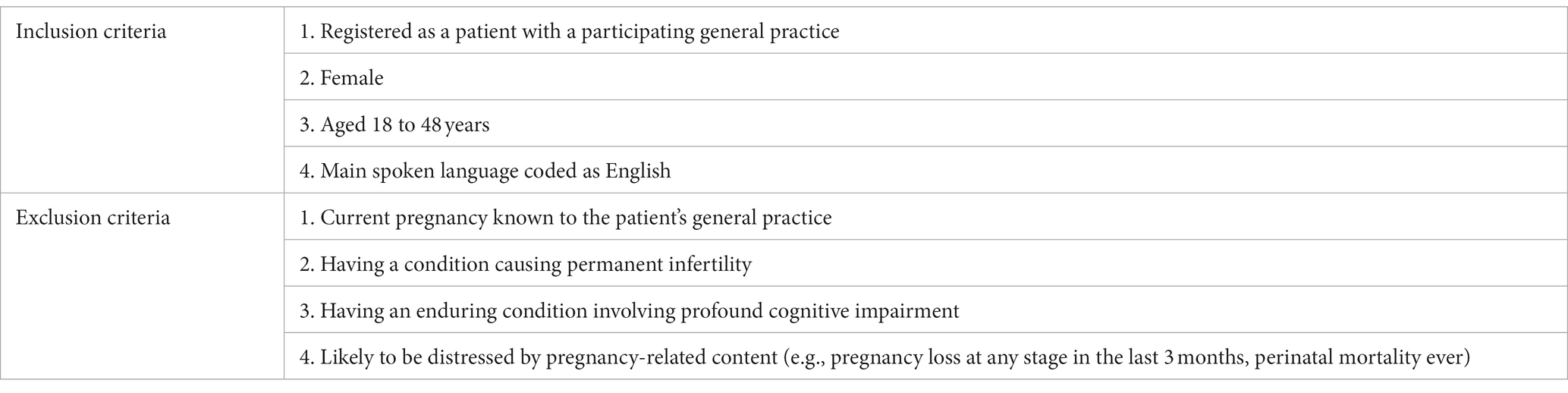
2.2.1 Eligibility criteria
Participants were eligible for inclusion (Table 1) if they participated in our prior survey of women registered with seven general practices in the West of England (31), and expressed interest in being interviewed about their responses. Further information on the survey’s sampling methods is available elsewhere (31).
2.2.2 Participant sampling
Of the 835 survey participants, 313 (37.5%) expressed interest in being interviewed. To promote diversity between participants (36) and enhance the transferability of our findings (37), we used a maximum variation purposive sampling approach (38). Our sampling criteria (39) (Supplementary Material S1) were informed by our survey findings (31). The strongest correlates of low knowledge and less positive attitudes toward preconception health were younger age, lower household income and nulligravidity; we aimed to achieve an approximately even split for these criteria. We monitored secondary criteria while recruiting participants to ensure diversity in their coverage (39). These included: ethnicity; country of birth; pregnancy intentions (including women who were ambivalent about or did not want a future pregnancy); attitudes toward preconception health; and acceptability ratings for the seven intervention delivery methods explored in this study.
2.2.3 Participant recruitment
Invitation emails were sent with the study’s participant information sheet (PIS) and consent form to 46 women. We aimed to include approximately 10 participants in each grouping of our dichotomous primary criteria (20 overall), informed by guidance that datasets involving 10 interviews or fewer are conducive to theme development where participant groups are homogenous (37). However, we continuously assessed the dataset during data collection to ensure the final sample was sufficient to justify claims of patterned meaning, validity and information power (37, 40).
2.3 Data collection
2.3.1 Interview schedule
We used in-depth, semi-structured interviews to support participants to freely express their views, reduce the risk of socially desirable responding, and facilitate probing of participants’ responses (41–43). We developed an interview topic guide (Supplementary Material S2) informed by our survey findings (31), a review of the literature (18–25) and through consulting academic researchers. The topic guide included questions to elicit participants’ views on seven candidate delivery options for preconception health interventions, found to be acceptable to women in our survey (31), and acceptable and appealing content for these interventions. The options were: general practitioners (GPs), nurse practitioners, pharmacists, social media, personal texts and emails, pregnancy tests, and health education in schools. MD conducted pilot interviews with five women, approached as peers or via a local public involvement network. Commonly misunderstood phrasings were re-worded. The topic guide was refined as new areas of interest emerged from the interviews.
2.3.2 Interviews
Interviews (N = 20; September–December 2021) lasted an average of 57 min (range: 37–79 min, reflecting the diversity in views and experiences). All participants chose a telephone interview. MD conducted 19 (95%) interviews. JS interviewed the final participant, who requested a female interviewer. Interviews were audio-recorded using an encrypted audio-recorder after consent was confirmed. Participants received a £20 shopping voucher to thank them for participating (44).
2.4 Ethical considerations
Participants provided consent for the publication and sharing of anonymized information. We anticipated that the topic of pregnancy might induce distress in participants who had experienced adverse pregnancy outcomes or infertility. We thus stated in the PIS and interview pre-briefing that participants could skip questions, stop the interview and/or withdraw from the study at any point.
2.5 Data analysis
Data were analyzed according to the framework method (33). Interviews were transcribed verbatim, transcripts were anonymized and imported into the NVivo 11 software package, and familiarization was undertaken (33). Deductive code labels (Supplementary Material S3) were applied to all relevant excerpts (45), as were inductive codes developed from the first three transcripts (coded in duplicate by the research team) (33) if these were agreed to be sufficiently relevant to the research questions. All investigators agreed on an initial analytical framework to index the remaining transcripts, and discussed potential refinements (33). The data were charted into matrices using Microsoft Excel, with each matrix representing an intervention delivery method (33). Data for each code were paraphrased and added to the corresponding participant’s matrix cell with reference to salient quotations (33). Candidate themes were developed by identifying data patterns within and between matrices. Themes were chosen based on prevalence, the study’s aims and deductive codes, and inductively-derived concepts, and elaborated through analytical memos (33). The transcripts were reviewed to confirm candidate themes formed a ‘coherent narrative’ of the data and addressed the research questions (37). The final themes and subthemes were written up as an analytic narrative (45).
2.6 Data quality
As rigor and quality are considered requisite considerations for framework analysis (33), we incorporated the concept of data trustworthiness, a theorisation of data quality developed for thematic analysis (46). Supplementary Material S4 outlines our quality-assurance measures for each data trustworthiness criterion.
3 Results
3.1 Participant characteristics
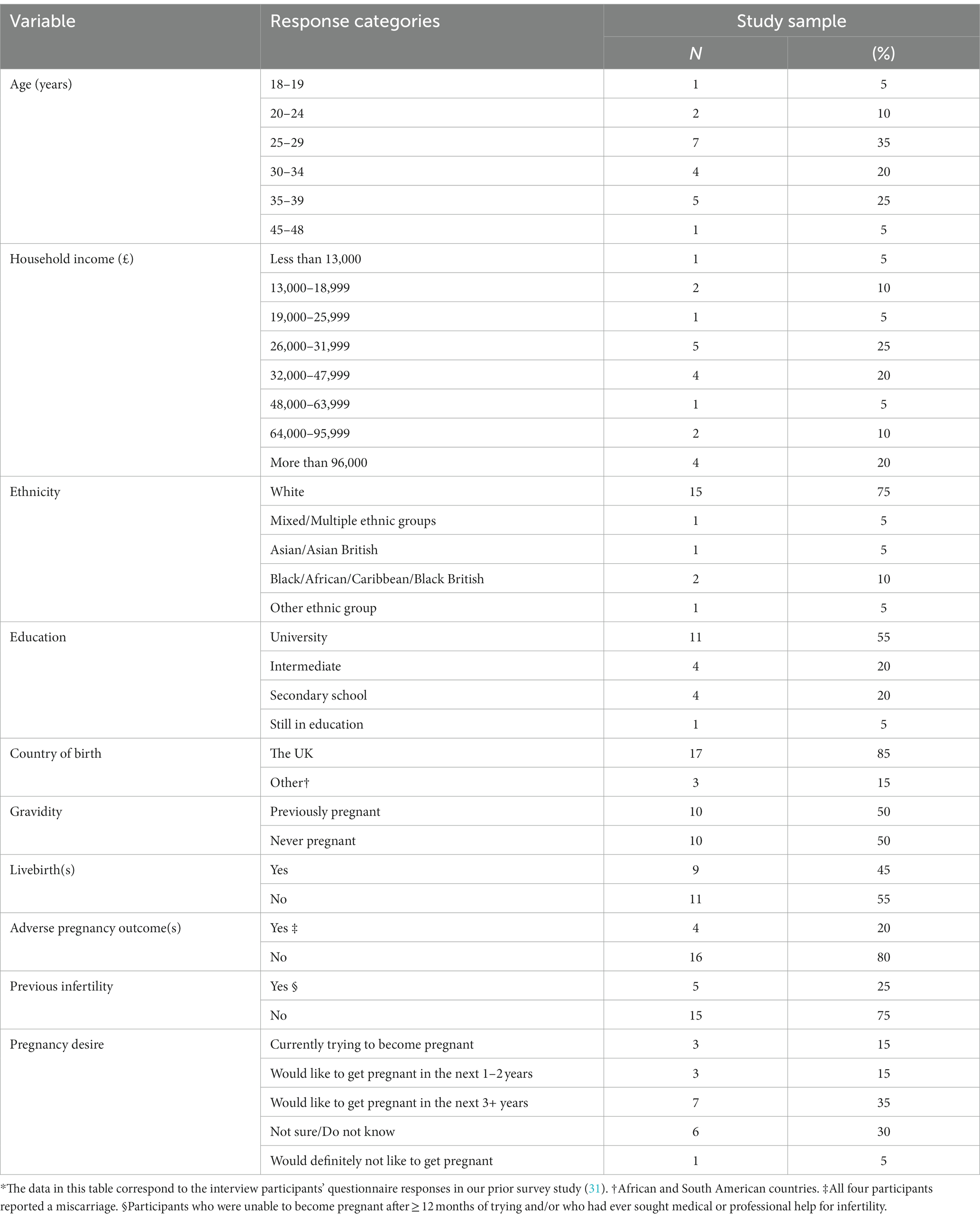
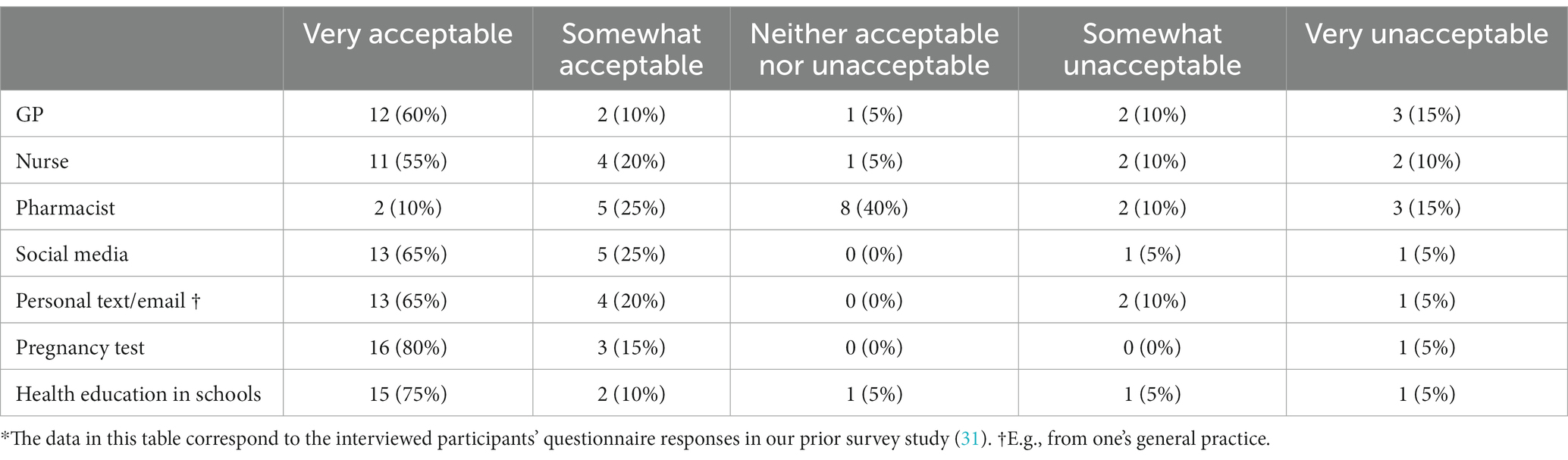
Twenty women took part (43.5% of invitees). Table 2 shows there was an even split of gravid and nulligravid participants and 18–29 and 30–48-year-old participants. Half (45%) of participants had experienced at least one live birth and a fifth (20%) had experienced a miscarriage. Two-thirds (65%) reported a desire for a future pregnancy. Almost half (45%) had household incomes below £32,000, compared with 43% of the UK population (47). The proportion of participants who were UK-born was similar to the national average (85% vs. 84.3%) (48). A greater proportion of participants had a minority ethnicity (25% vs. 15.2%) (49) and were university graduates (65% vs. 42%) (50) than the national average. We recruited participants with a range of acceptability ratings for the discussed intervention delivery methods (Table 3). There was a broadly even split of participants with ‘low’ knowledge of preconception health (n = 9; listed ≤2 of the preconception risk factors assessed in our survey (31)) and ‘high’ knowledge (n = 11; listed ≥3 assessed risk factors). We recruited participants with a range of attitudes toward preconception health (Supplementary Material S5).
3.2 Themes
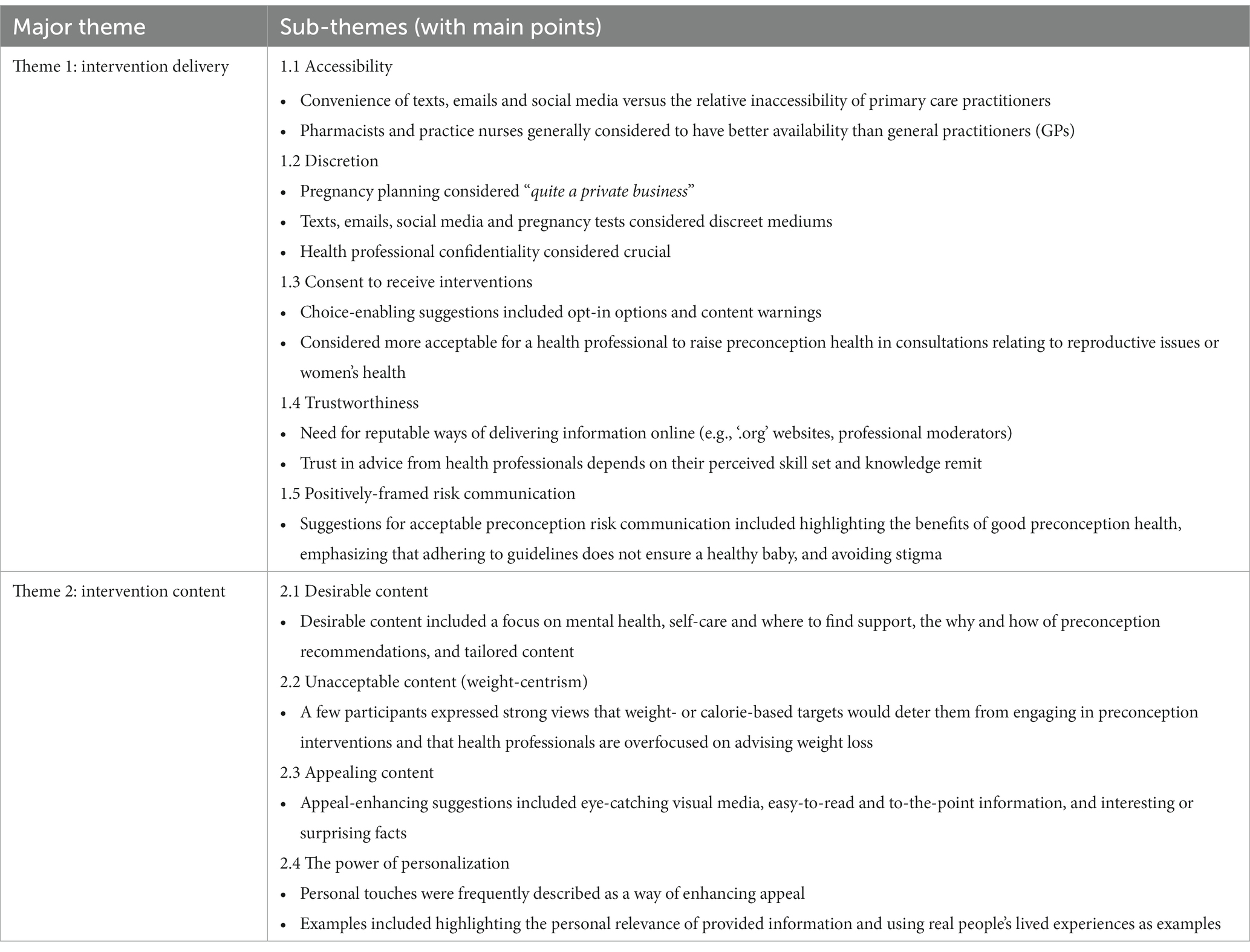
The themes and sub-themes developed from the data are shown in Table 4; these are the focus of the analytic narrative presented below. The specific points participants made about each of the seven intervention delivery methods are presented in Supplementary Material S6.
3.2.1 Theme 1: intervention delivery
3.2.1.1 Accessibility
Participants commonly highlighted the importance of accessible interventions. For instance, a perceived advantage of sending information by personal text or email was the convenience for recipients:
“I think it’s brilliant… He’s [GP] sent me the information [by text/email] and I’ve got it there in front of me within minutes. Instead of me having to go up to the surgery...” (p. 04, 30–34 years, previously pregnant).
Participants also spoke about how “accessible” (p. 13) information provided through social media can be and how passive, unintentional information receipt can often lead to real engagement:
“[Social media] is one of the best ways you can communicate with people. Because it comes up accidentally. People get really bored on their phones, so they click on things they do not really want to click on, but they end up reading and engaging in.” (p. 03, 25–29 years, nulligravid).
Conversely, primary care practitioners were widely perceived to be relatively inaccessible. Participants reported that they only contact these professionals about illnesses and medical emergencies, as they lack the time to merely provide “information” about issues like preconception health:
“…we tend to avoid contacting the GP if you are not unwell because you feel like you are wasting a doctor’s time, that they could be looking after people that are actually unwell… Whereas this is more: ‘I just need a chat and information’.” (p. 01, 35–39 years, previously pregnant).
The brevity of primary care appointments was also considered a barrier to exploring issues in depth:
“…the appointment times are just not long enough and I do prefer to read more deeply around different things.” (p. 18, 25–29 years, nulligravid).
This perceived lack of availability was particularly apparent in discussions about general practitioners (GPs). Participants expressed that they would be willing to discuss their preconception health with GPs if there was “an opportunity” (p. 02). However, they felt it’s “very noticeable” that GPs do not have “very much time” (p. 03), meaning “you do not feel like you can have a proper conversation” (p. 03) and it’s not “appropriate” to ask GPs questions such as “‘shall I take this vitamin?’”(p. 10). Pharmacists were considered to have better availability than GPs. Nurses were also generally considered to have “more time” (p. 03) and be “a lot easier to see” (p. 09) than a GP. It was thus felt that topics such as preconception health can be raised in a nurse consultation, alongside other care:
“…I could bring that up in a blood test or my flu jab… to me, there’s a lot more downtime in a nurse’s appointment than there is in a GP [appointment].” (p. 09, 20–24 years, nulligravid).
Finally, participants commonly demonstrated a desire to avoid adding additional burden to the national health service (NHS) and for access to “services that specialize in women’s health” (p. 08) to be improved:
“With the NHS being so under-resourced... it’s what we are always encouraged to do, isn’t it? Minor things, go to a pharmacy first.” (p. 10, 20–24 years, nulligravid).
3.2.1.2 Discretion
Participants considered pregnancy planning to be “quite a private business” (p. 12) and felt that “a lot of women would not necessarily tell anybody they were going to try for a baby” (p. 19). Providing preconception health information and services discreetly was thus commonly considered advantageous or necessary. For instance, personal texts and emails were viewed as “a nice and discreet way” (p. 18) to provide information, websites were considered “a good resource” that “anyone can access in the privacy of their own homes” (p. 19), and information in pregnancy test packaging was considered “quite private” (p. 13).
The importance of discretion was also evident in suggestions for enhancing the acceptability of interventions. For instance, participant 18 favored placing information about preconception health “inside the packaging” of pregnancy tests over a vendor “loudly waving a leaflet and talking about pregnancy.” Participant 05 emphasized the importance of preconception health information provided through social media being “visible just to you” and was reluctant to “respond to something on social media about pre-pregnancy” because ‘basically anyone could see… and pin it back to you.” The importance of providing information to school pupils that they can access discreetly was also highlighted:
“Leaflets in school are good but not great because everyone can see you picking it up… more of an online resource is best.” (p. 10, 20–24 years, nulligravid).
Discretion was also a consideration for methods involving health professionals. Unlike the above examples, this tended to relate more to the importance of confidentiality, highlighting a need to consider the many forms of discretion. For instance, a perceived advantage of discussing preconception health with a GP was that they are bound “by various confidentiality rules” (p. 16) and can be trusted not to share personal information:
“I think the GP… for a lot of people, is a safe person. Somebody who is a healthcare professional, somebody they trust.” (p. 19, 45–48 years, previously pregnant).
Some divergent views on this were noted, including the security of GP medical records and confidentiality concerns for patients with family or friends working “within the GP practice” (p. 08). Participants commonly reported that enabling privacy may be an issue if pharmacists were used as an intervention medium. This mainly related to the public nature of discussions with a pharmacist:
“…there would probably be certain things I would not want to just discuss [with a pharmacist] when potentially someone could just walk through the door.” (p. 13, 18–19 years, nulligravid).
Participants reported that they might therefore “shut the conversation down” (p. 08) if a pharmacist attempted to raise the topic of preconception health. However, some felt this would be more acceptable if pharmacists had “time to take someone aside” (p. 03) and consult them in a “private room” (p. 19), and allowed this private consultation to be anonymous and booked discreetly online:
“If you could book a private appointment online so you do not have to physically go in and physically ask for a private session… then it’s no different than just booking a doctor’s appointment.” (p. 12, 35–39 years, nulligravid).
“You could go to any pharmacy if you did not want to speak to someone that may know you… if you wanted to, give a false name.” (p. 05, 35–39 years, previously pregnant).
3.2.1.3 Consent to receive interventions
Participants expressed mixed views on whether individuals need to consent to receive preconception health interventions. Some felt this wasn’t necessary, as it’s “definitely something that women need to know” (p. 06) and recipients can “ignore” (p. 08) provided information. However, others felt it would be an issue if recipients “have not chosen to see” (p. 10) this information as it might feel “intrusive” and “triggering” (p. 19) for some, such as those who have “just had a miscarriage” (p. 10), and that people should therefore be given “the choice” (p. 15). Suggested methods for enabling this choice included a scoping message asking “are you happy to receive emails on this topic?” (p. 13), a “click to find out more” (p. 14) or “opt-in” (p. 03) option, and asking patients “is it okay if I send you this stuff?” (p. 13) in healthcare appointments. Participants also suggested having a content warning, for example at the “very top of the email” (p. 05), so that recipients can make an informed decision about whether to delete or read it. A further choice-enabling suggestion for pregnancy test packaging was to provide leaflets by rather than in the boxes and use these leaflets to signpost to “where [one] can look” (p. 17) for information. This contradicted the suggestion for a leaflet to be inside the box to enable discretion.
A perceived benefit of social media as an intervention medium was that people choose to use social media and have some control over the content they see and engage with. Participants therefore felt this method is not as invasive as having “information sent straight to your phone” (p. 10):
“…it [social media] never feels imposing… you can just choose to scroll past something if you are not comfortable with it.” (p. 13, 18–19 years, nulligravid).
Some participants also considered that targeted social media advertisements would be acceptable as these tend to relate to relevant online “searches or conversations” (p. 01), social media algorithms are “very for that person” (p. 09), and you can choose not to see similar advertisements again:
“Targeting people with specific ads if they are in the right age group or they have thought about pregnancy before would be good… if it affects you… you can say that you do not want to see the ad anymore.” (p. 14, 25–29 years, nulligravid).
Others disagreed with this view. They felt the use of targeted social media advertisements would be “invading people’s privacy if they have had bad pregnancy experiences” (p. 18), and that the imperfection of algorithms means there would be targeting issues. They thus felt it would only be appropriate to provide this information to those who had explicitly sought it out:
“You might have spoken about pregnancy tests and started getting things about children and how to conceive, when actually that’s the opposite.” (p. 08, 25–29 years, nulligravid).
Some participants also felt that health professionals raising the topic of preconception health would be inappropriate as this might be seen as disregarding the wishes of women who cannot have or do not want children and “panic” those who “do not have all the time in the world” (p. 11) left to become pregnant. Conversely, other participants felt it would be acceptable for health practitioners to initiate a conversation about preconception health, and that questions like “Do you feel well equipped with the knowledge to have a successful pregnancy?” should be “standard” (p. 03). In support of this view, participants argued that “a lot of people will not open up” or “want to admit that they do not know” (p. 03) this information. It was also argued that there are “so many missed opportunities” (p. 03) for this information to be provided to patients and “there needs to be a way” to know that GPs “offer these kinds of services” (p. 05). Some participants suggested that it would be more acceptable for a health professional to raise these topics in consultations relating to reproductive issues or women’s health, such as contraception counseling and cervical smear tests:
“…nobody ever says to me [during smear tests]: ‘And are you trying for a baby?’… that would be an ideal time” (p. 12, 35–39 years, nulligravid).
Others felt that providing preconception health information would be more appropriate if the recipient was purchasing or had mentioned a product (e.g., folate supplements) or issue related to pregnancy, or had indicated their pregnancy intentions:
“… if there was a setting on there [the NHS app] to say that ‘yes, I want a child at some point in my life’…. I think that setting would then give GPs the option to bring it up.” (p. 09, 20–24 years, nulligravid).
Participants also suggested ways that healthcare service providers could advertise preconception health information and services so that patients can choose whether they engage with these. These suggestions included “a welcome pack” (p. 05) for new registrations and other promotional materials, such as posters, webpages and leaflets inserted into shopping bags by pharmacists when selling related products such as “ovulation tests, pregnancy tests” (p. 08):
“Even if you just stuck it on the back of folic acid, as a: ‘go to this website’… You just need to raise the awareness of where to go...” (p. 17, 35–39 years, previously pregnant).
3.2.1.4 Trustworthiness
Participants commonly spoke of the importance of trustworthy information and reputable sources. For instance, participants frequently highlighted the considerable amount of poor-quality information available through social media and the internet, which can be “hard to filter through” (p. 16) to find legitimate information. Some participants therefore felt that communicating preconception health information through social media would be problematic as it may get “lost amongst all of the reams of misinformation” (p. 18) and “with pregnancy, you have got to be so careful” (p. 06). Others felt this highlighted a need for using “reputable ways” (p. 03) of delivering preconception health advice on social media and the internet. These included partnerships between trusted institutions and subject experts and the use of ‘.org’ websites (p. 07), peer-reviewed scientific literature (p. 18), professional moderators (p. 15), and recommendations from reputable health organizations:
“They [period tracking app] go by NHS guidelines and WHO [World Health Organization] and all that kind of stuff. So they are a really good source of information.” (p. 03, 25–29 years, nulligravid).
Some participants favored advice from a recognized health professional over receiving information online. They felt that with health professionals, you can be more sure you have “got the right information” (p. 06) and that they would not make a health behavior change “unless a health professional tells [them] to” (p. 10). However, many participants expressed that their trust in a health professional’s advice would depend on their perceived skill set and knowledge remit. For instance, participants commonly saw pharmacists as the “medicine person” (p. 08) with whom they would feel comfortable discussing preconception supplements and the potential impact of “any other medication” (p. 01). While some said they would speak to pharmacists about “any kind of [preconception] topics” (p. 07), others stated they would not seek or trust their advice on more general “lifestyle changes” (p. 09). Some felt it would only be acceptable for a pharmacist to initiate a discussion about preconception health “if they are trained” to (p. 06) or if their pharmacy “had a specific interest in maternal health” (p. 19).
This mix of views was also observed for GPs. Some participants expressed a reluctance to discuss “lifestyle changes” with a GP (p. 06). This was associated with a view that GPs’ knowledge is “spread over so many things” (p. 17) and that someone else who is “very specialized” (p. 13) in reproductive health might know more. A contrasting view was that GPs are “the real medical practitioners” (p. 02) who “give you the facts that you can trust” (p. 10). Nurse practitioners were generally considered to have a more practical skillset. For some, this meant that nurses are a less acceptable source of guidance:
“Some nurses have a very, very, very low knowledge of nutrition and they are more practical. So they are more wound care.” (p. 03, 25–29 years, nulligravid).
Others felt this practical skillset means that nurses often have more “hands-on experience of how things have affected people” (p. 10) and are “a bit more down-to-earth” (p. 12) than GPs. Some participants felt that “the more appropriate person” would be “whoever is more of a specialist on the topic” (p. 18) of preconception health.
3.2.1.5 Positively-framed risk communication
Participants suggested several ways to enhance the acceptability of information about preconception risk factors. One suggestion was to emphasize that adhering to all preconception health guidelines does not guarantee a healthy baby, to minimize the potential for people to “think that they are the problem” (p. 09) and self-blame for adverse outcomes. A further suggestion was to strike “the right balance” (p. 13) between acknowledging the different emotions women may feel toward pregnancy and ensuring the provided information is factual and non-euphemistic:
“You do not want to dress up the facts so much that they get lost…it’s information that you want to deliver quite softly but still factually.” (p. 13, 18–19 years, nulligravid).
Some participants also spoke of the importance of positive framing and highlighting the benefits of good preconception health rather than focusing on risks, harms and actions to avoid (i.e., “‘do not do this, this is the risk’” (p. 12)). These participants felt this approach is more effective and memorable, and that people “like aiming for the positives” (p. 17):
“…when I was smoking, it made absolutely zero difference to me… that doom and gloom stuff… I’ve responded a lot better to stuff that’s been much more positive.” (p. 12, 35–39 years, nulligravid).
Participants also felt a risk-averse, “better to be safe than sorry” (p. 20) approach to health messaging may be desirable as people’s risk perceptions vary greatly, and that people are more likely to disregard information that relates to risk rather than guaranteed health outcomes:
“If you said to someone: ‘If you exercise, you’ll have an extremely healthy pregnancy’… everyone would be exercising. But because that’s not true, it’s just: ‘Yes, you are going to be reducing any potential health risks’… Do people really understand what that means?” (p. 03, 25–29 years, nulligravid).
Further, some expressed that people should not be judged for their preconception actions or pressured into changing their behavior, as this is unacceptable and unlikely to affect change. Preferred strategies included acknowledging that behavior changes are “difficult for everyone” (p. 05), accepting people’s circumstances, and focusing on risk mitigation:
“The work that I’ve seen done best is about… harm reduction. ‘Okay, we accept where you are, how can we help you to minimize risk?’… I do not think the other way of doing it, of just saying: ‘Oh, well, just stop’ makes a difference.” (p. 12, 35–39 years, nulligravid).
Participant 17 also alluded to the importance of respecting the reproductive choices of women whose health conditions are associated with greater risk of adverse outcomes. This would mean tailoring messages to ensure acceptable risk communication for these women:
“….[At a discussion] someone had said that women with diseases should not reproduce, which was a bit harsh to take in… I think there can be an outcome, but I’ve actually seen quite a lot of…. [people] with diseases like epilepsy, like diabetes… and the babies have been fine.” (p. 17, 35–39 years, previously pregnant).
The importance of acceptance was also evoked in participants’ views on GPs as potential interventionists. Some participants expressed that they would “feel comfortable discussing basically anything with a GP because it feels confidential and without judgement” (p. 13). Others highlighted that they would be comfortable discussing preconception health with a GP “as long as they keep their personal opinions to themselves” (p. 10). Participant 16 described an experience where she considered not telling her GP about skiing while pregnant because she “knew that they’d not really approve.”
3.2.2 Theme 2: intervention content
3.2.2.1 Desirable content
Participants highlighted a range of content they felt should be included in preconception health interventions. This commonly included “general advice” (p. 02) on “what to do if you want to be pregnant” (p. 09) and preconception “changes” (p. 05) to consider. Others suggested this guidance should include the specifics of recommended preconception practices, such as the exact “dosage” (p. 17) of folic acid and safe alcohol consumption limits, so that women can make decisions “with a bit more knowledge behind them” (p. 20).
Mental health was highlighted by some as an important focus for preconception health interventions. Participants felt that factors like “stress” are a “big problem” (p. 04) for outcomes such as miscarriage and that the importance of people’s mental preparedness for pregnancy is typically overlooked, despite mental health being “just as important as physical health” (p. 04):
“It’s not so much of a main focus when you are trying to have a baby… [that] you and your mental [health] are ready.” (p. 09, 20–24 years, nulligravid).
Some participants expressed that they would be more interested in preconception health interventions if they included a focus on “self-care” (p. 09) and signposted to where people “can find support” (p. 14), including support for individuals “struggling to get pregnant” (p. 14). A perceived advantage of social media as a delivery method was its ability to help users to “find support with other women” (p. 09).
Participants also suggested that intervention content should be tailored to its target population, particularly with regard to age. All participants agreed that providing at least some information about preconception health through schools would be appropriate. Specifically, participants suggested providing pupils with “some really basic detail” that “links with good health advice” (p. 12) but includes something specific to preconception health. They also suggested making pupils aware of relevant services and information sources, and highlighting the preconception period as a unique phase of the pregnancy journey:
“…breaking it down into the different phases… living a normal life, then the preconception phase, then you are pregnant but you are not necessarily aware of it, and then you have got the trimesters of pregnancy… building up that awareness that it’s not just as simple as not pregnant, pregnant.” (p. 16, 30–34 years, previously pregnant).
Participant 04 also spoke of the importance of highlighting the “problems that can occur” in the preconception period, including infertility, as this “should not be a taboo subject.” She felt this had not been communicated in her education at school, which resulted in a conflict between her reproductive expectations and reality:
“I assumed that by the age of twenty-eight, I would have two children… I’m now [in my early thirties] and I’ve not got none... I do not think that’s made clear enough, about infertility...” (p. 04, 30–34 years, previously pregnant).
Some participants felt information about preconception health should be communicated to pupils, particularly older teenagers, in the same way it would to adults, as “making everything very kiddy and funky” (p. 06) can be off-putting and impair understanding:
“…being factual and realistic can just be the best way of delivering things to kids, especially when you are talking about sixteen-year-olds.” (p. 06, 35–39 years, previously pregnant).
Others felt it may be better for the focus of this information to be “women’s health” (p. 12) or the importance of preconception health more generally, as topics like “babies” (p. 12) and pregnancy may be off-putting or of little interest to this cohort:
“Just give them: ‘Okay, this is important… to have good pre-pregnancy health for these reasons’. Just general. Not being too specific. Because they are sixteen, I do not think they want to get pregnant.” (p. 07, 25–29 years, nulligravid).
Participants who felt younger children should be given some level of information about preconception health noted that “a fun way” (p. 09) of relaying this information to this age group may be required:
“…almost like a game, like ‘oh, this woman, or this person, wants to have a baby… in six months. What should they be doing to make sure that their pregnancy is as healthy as can be?’.” (p. 09, 20–24 years, nulligravid).
3.2.2.2 Unacceptable content (weight-centrism)
A few participants expressed strong views that it’s important for preconception health interventions to “not be weight-centric” or even “mention weight” (p. 09). These participants expressed that repeatedly being advised to lose weight “gets to you, massively” (p. 04) and that the possibility that a healthcare provider might “mention anything about weight” would make them “anxious” (p. 09). Participant 09 (20–24 years, nulligravid) felt body weight is not a “fair determinant of health,” that body mass index (BMI) is “outdated, sexist” (p. 09), and that there’s “so much pressure on women… to fit a certain box of ideals” (p. 09). She described how she was “stepping away” from having “so much of [her] medical care and [her] life revolve around” her weight and that weight-, BMI- or calorie-based targets “would a hundred per cent” deter her from engaging with preconception health interventions. Conversely, she expressed that she would be interested in interventions that focused on “healthy habits” such as finding a way to be physically active that “makes your body feel good” or making meals more “nutritional.” Participant 04 described prior expectations from health professionals for her to lose weight as “ridiculous,” and the way she had been spoken to about this as “awful.” She felt health professionals are overly focused on advising weight loss and lack the ability to support patients beyond this:
“They just tell you to lose weight…. But if you cannot lose weight, what else can you do?... they do not seem to be able to help you.” (p. 04, 30–34 years, previously pregnant).
3.2.2.3 Appealing content
Participants expressed a range of views on whether and how to maximize the appeal of intervention content delivered through the discussed intervention mediums. Some felt appeal-enhancing strategies are not needed, as women wishing to become pregnant will already be interested in this topic:
“It’s [pregnancy] not something that you do by invitation. It’s more like something you have already planned and the information just happens to be there to help you along the way. Rather than it being something that entices you.” (p. 01, 35–39 years, previously pregnant).
Participant 08 expanded on this view by saying that appeal may only be needed for people who have ambivalent pregnancy intentions:
“…[for people wishing to become pregnant]a simple leaflet would do. But if it was a resource for women that were maybe on the fence then, yeah, it might be.” (p. 08, 25–29 years, nulligravid).
A multitude of methods for enhancing intervention appeal were suggested by participants who felt this could be beneficial. These included the use of “eye-catching” (p. 10) visual media involving images, video and color. Participants expressed that this media can turn “a very boring, factual [social media] post into something that catches people’s attention” (p. 13) and that it’s “almost not even worth” (p. 03) putting information on social media without it:
“…all the communication [on social media], pretty much, has to be through a really quick video or graphics that lead to information that is simple to digest… You always want that stimulation first.” (p. 03, 25–29 years, nulligravid).
Participants also highlighted the importance of “simple” (p. 08), “easy-to-read” (p. 17), and “to the point” (p. 04) information that is free from “medical jargon” (p. 08), as information that is “really complicated… puts people off” (p. 19):
“You don’t want a video that’s five minutes long, right? It has to be appealing and short.” (p. 07, 25–29 years, nulligravid).
However, some suggested that this initial, brief information could be supplemented with signposting to “more complex bits of information” (p. 03) for people who “want to read more” (p. 19). The use of interesting or “surprising” facts was another suggested way of ensuring recipients “want to find out more” (p. 03). Participants also described that appeal can be enhanced by ensuring the provided information has clear “themes and a narrative” (p. 03) and explains the why and how of preconception recommendations:
“I really like to know how things work. So why am I going to be taking the folic acid? How is that going to be helping me?” (p. 09, 20–24 years, nulligravid).
3.2.2.4 The power of personalization
Participants frequently described the use of personal touches as a way of enhancing the appeal of preconception health interventions. This included suggestions to offer or signpost to more individualized information and making the provided information “more personal” (p. 15) through, for instance, using a patient’s name, following on from a relevant conversation, or tailoring information to the recipient’s personal risk factors. Highlighting the personal relevance of preconception health information was another suggested way of enhancing engagement:
“It could even be a very transparent leaflet saying: ‘a lot of women… [of] childbearing age have reduced knowledge of nutritional interventions and exercise interventions’… I think people are more inclined to know more once they think: ‘Oh, I’m in that category…’” (p. 03, 25–29 years, nulligravid).
Participants also valued the “personal touch” (p. 12) of a health professional-initiated conversation, as they “would not pay any attention to” a leaflet (p. 12), and expressed that they would be more comfortable having this conversation with a familiar professional:
“I do not want to share something that’s quite so personal with someone I do not know.” (p. 17, 35–39 years, previously pregnant).
Finally, participants widely considered real people’s lived experiences to be a more “personal” (p. 09), “relatable” (p. 03) and memorable way of communicating health information than “textbook” (p. 02), scientific information:
“… if I read someone’s experience, I would take that into account more than just information, information, information.” (p. 04, 30–34 years, previously pregnant).
4 Discussion
National health organizations such as England’s Department of Health and Social Care have called for more research with women to explore how best to engage them in preconception health interventions (13–15). This is the first qualitative study to explore views on content and delivery methods for preconception health interventions delivered in both healthcare- and community-based settings, with purposively-recruited women to capture a variety of experiences and perspectives. To increase appeal and acceptability, women suggested preconception interventions should ensure privacy, sensitivity, easy access and appropriate consent, and provide positively-framed information that highlights the benefits of good preconception health. They favored the use of visual media, ‘trustworthy’ information from reputable sources, interesting and unfamiliar facts, simple information with signposting to more complex information, and the use of personalized information.
4.1 Integration with prior research
Participants felt individuals should choose to receive preconception health interventions, but that it may be acceptable for health professionals to raise preconception health with patients. One of the justifications for this was that this may address the ‘missed opportunities’ for improving preconception health (14, 51). This opportunistic delivery was considered more acceptable in encounters relating to reproductive issues or women’s health, such as cervical smear tests and contraceptive counseling. This view was also identified in Tuomainen et al.’s (24) qualitative study of 41 women; collectively these findings support policy recommendations that healthcare services should meet women’s full range of reproductive health needs at the same time and place (14, 15). Some women favored advice provided by a health professional, preferably with specialist training in preconception health, over online information, due to their greater credibility. This mirrors prior findings that women with diabetes value high-quality information relating to pregnancy (20, 21). However, we also found that, due to their perceived inaccessibility, participants commonly felt it was inappropriate to consult GPs for information retrievable online. This echoes McGowan et al.’s findings that men and women are reluctant to seek preconception care from a physician due to a perceived lack of availability and a view that this would be ‘wasting an appointment’ (25). Collectively, these findings suggest that an awareness of primary care capacity issues may drive some women to less credible but more accessible information sources, and highlight the trade-offs women may make when seeking reproductive health information.
Participants also reported that they did not want preconception health discussions with a health professional to be judgmental. This echoes prior findings that fears of being judged, labelled or lectured (19, 20) can impede the receipt of preconception care by women with diabetes, suggesting these findings may be generalizable to other reproductive-age populations. Women also favored positively-framed information that highlights the benefits of good preconception health rather than risks and harms. This replicates McGowan et al.’s (25) finding that participants were uncomfortable with messages that link parental preconception behaviors with adverse infant outcomes. Similarly, women in our study recommended emphasizing that adhering to all preconception health guidelines does not guarantee a healthy baby, to minimize the potential for self-blame for adverse outcomes. Participants also widely considered real people’s lived experiences to be more relatable and memorable than textbook, scientific information. This can be seen to reflect the tenets of Fisher’s narrative paradigm, that people draw on an innate narrative logic to assess new information, and that all meaningful communication happens via storytelling (52).
There were some notable tensions between the views expressed in this study and the epidemiological literature on preconception health. For instance, our finding that some women felt preconception health interventions should include support for preconception mental health contrasts with the lack of systematic reviews reporting associations between this factor and reproductive outcomes (4). This suggests that women may want the focus of preconception interventions to extend beyond risk factors that have currently demonstrable adverse health impacts to also encompass a broader range of social, mental health and well-being factors.
4.2 Implications for policy, practice and future research
Researchers, policymakers and practitioners should seek to develop and implement preconception interventions informed by the strategies we identified to enhance the appeal and acceptability of their delivery and content (16, 17). Our finding that women commonly considered GPs and practice nurses to be relatively trustworthy but inaccessible intervention delivery methods has implications for the English government’s aim for primary care professionals to have a role in supporting women’s preconception health (13). It suggests that to achieve this, strategies are needed to persuade women that seeking this support is an appropriate reason to see a GP or nurse. As primary care professionals have repeatedly reported capacity issues to be a major barrier to providing preconception care (27, 28), innovative, light-touch interventions may be required to build capacity for this. This could include raising the topic of preconception health in existing encounters relating to reproductive issues or women’s health, such as cervical smear tests and contraceptive counseling; participants considered this more acceptable than raising the topic ‘out of the blue’. If this approach is taken, future research should seek to identify the training and resources these professionals require to deliver this opportunistic preconception care in an acceptable way. An alternative interpretation of women’s reluctance to seek preconception care from primary care is that this further highlights a need to consider online and community-based opportunities for preconception health interventions (9, 31).
Our findings highlight complexities for preconception health interventions and trade-offs that may be needed to tackle these. The possibility that a focus on weight may deter some women from engaging in preconception interventions is one such challenge. Obesity is considered a major public health issue (53) and pre-pregnancy obesity is a risk factor for common adverse pregnancy outcomes including pre-eclampsia and gestational diabetes (4). On this basis, it is understandable that preconception health interventions should aim to reduce weight in mothers-to-be with obesity. However, policymakers and practitioners should consider the relative benefits of this approach against the risk of deterring these women from engaging in these interventions and potentially seeing improvements in other risk factors. They should be mindful of the stigma mothers with obesity already experience (54) and of concerns that medical practice draws on prevailing “biomedical discourse” to justify controlling women’s bodies (55). This highlights the potential merits of using ‘dark logic’ models in the early development of preconception health interventions, to explore the potential for unintended harmful effects (56). Future research should explore whether it may be more acceptable for these interventions to focus on weight-related behaviors, such as diet and exercise, rather than having explicit weight-based goals.
4.3 Limitations
Our study has some limitations relating to its sample and design. We recruited a balanced sample with respect to age and gravidity and the proportions of participants who were born outside the UK and had household incomes under £32,000 were in line with the national average (47, 49). However, the actual numbers of participants from these groups were small and university graduates were overrepresented (50). Our findings need to be interpreted with an awareness of this. Further, women who were considered likely to be distressed by pregnancy-related content were not included (31). A finding of this study was that preconception interventions need to be sensitive to the experiences of these women, and their exclusion means their views on how to ensure this were not reflected. Our use of a sequential explanatory mixed methods design, where we analyzed our quantitative data (31) before collecting our qualitative data, allowed us to qualitatively explore our survey’s findings and purposively recruit women from the general population. This overcame many of the limitations and potential bias of prior qualitative studies in this area, which used convenience samples (24, 25). However, it should be noted that only a minority of the women who received a questionnaire took part in our survey (31), which may have introduced a self-selection bias if participants’ experiences and views on preconception health were different to those who did not participate. Further, a sequential exploratory design would have allowed us to quantitatively assess the representativeness of the views participants expressed and the appropriateness of transferring our findings to different samples (156). This is a potential avenue for future research.
Additionally, the positioning of the first author as an outsider researcher may have affected the study’s knowledge production. This likely helped to avoid issues associated with insider research, including over-familiarity, taken-for-granted assumptions and the omission of details from participants’ narratives due to assumed common understanding and experience (57). Placing the participant in a relatively expert position, argued to be an ‘empowering experience’, can also be advantageous when studying marginalized individuals (58). Conversely, MD’s positioning as an outsider researcher may have meant there was information relating to the reproductive experiences of the interviewed women they did not feel comfortable sharing with a man (58).
5 Conclusion
Women favored preconception health interventions that ensure discretion, easy access and sensitivity, seek consent to receive the intervention, and provide trustworthy information that highlights the benefits of good preconception health rather than stigmatizing people for their weight, actions and reproductive choices. The use of visual media, personalization, interesting and unfamiliar facts and simple information with signposting to more detailed information were also viewed favorably. Future research should seek to develop and implement preconception health interventions informed by these findings, and should explore the potential for these interventions to have unintended harmful effects.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by South West – Frenchay Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MD: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing, Funding acquisition. RK: Conceptualization, Funding acquisition, Supervision, Writing – review & editing. JW: Conceptualization, Funding acquisition, Supervision, Writing – review & editing. JS: Conceptualization, Investigation, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported in part by grant MR/N0137941/1 for the GW4 BIOMED DTP, awarded to the Universities of Bath, Bristol, Cardiff and Exeter from the Medical Research Council (MRC)/UKRI. This included funding for open access publication fees. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Acknowledgments
The authors thank the women who took part in this study. We also wish to thank Mike Bell at NIHR ARC West, who facilitated the study’s public involvement, and Judith Stephenson, Jennifer Hall and Geraldine Barrett, who reviewed the study’s topic guide and protocol prior to its conduct. Some of the content of this manuscript has previously appeared online in the first author’s PhD thesis (59).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1303953/full#supplementary-material
Abbreviations
BMI, Body Mass Index; GP, General Practitioner; NHS, National Health Service; PIS, Participant Information Sheet
References
1. Quenby, S, Gallos, ID, Dhillon-Smith, RK, Podesek, M, Stephenson, MD, Fisher, J, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. (2021) 397:1658–67. doi: 10.1016/S0140-6736(21)00682-6
2. United Nations Children's Fund (UNICEF). Neonatal mortality (2020). Available at: https://data.unicef.org/topic/child-survival/neonatal-mortality/. Accessed May, 20 2022.
3. Blencowe, H, Kancherla, V, Moorthie, S, Darlison, MW, and Modell, B. Estimates of global and regional prevalence of neural tube defects for 2015: a systematic analysis. Ann N Y Acad Sci. (2018) 1414:31–46. doi: 10.1111/nyas.13548
4. Daly, M, Kipping, RR, Tinner, LE, Sanders, J, and White, JW. Preconception exposures and adverse pregnancy, birth and postpartum outcomes: umbrella review of systematic reviews. Paediatr Perinat Epidemiol. (2021) 36:288–99. doi: 10.1111/ppe.12855
5. Toivonen, KI, Lacroix, E, Flynn, M, Ronksley, PE, Oinonen, KA, Metcalfe, A, et al. Folic acid supplementation during the preconception period: a systematic review and meta-analysis. Prev Med. (2018) 114:1–17. doi: 10.1016/j.ypmed.2018.05.023
6. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
7. Flegal, KM, Carroll, MD, Kit, BK, and Ogden, CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. (2012) 307:491–7. doi: 10.1001/jama.2012.39
8. Public Health England. Health of women before and during pregnancy: health behaviours, risk factors and inequalities. An updated analysis of the maternity services dataset antenatal booking data (2019). Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/844210/Health_of_women_before_and_during_pregnancy_2019.pdf. Accessed May, 26 2022.
9. Stephenson, J, Patel, D, Barrett, G, Howden, B, Copas, A, Ojukwu, O, et al. How do women prepare for pregnancy? Preconception experiences of women attending antenatal services and views of health professionals. PLoS One. (2014) 9:e103085. doi: 10.1371/journal.pone.0103085
10. Toivonen, KI, Oinonen, KA, and Duchene, KM. Preconception health behaviours: a scoping review. Prev Med. (2017) 96:1–15. doi: 10.1016/j.ypmed.2016.11.022
11. Withanage, NN, Botfield, JR, Srinivasan, S, Black, KI, and Mazza, D. Effectiveness of preconception interventions in primary care: a systematic review. Br J Gen Pract. (2022) 72:e865–72. doi: 10.3399/BJGP.2022.0040
12. Temel, S, Van Voorst, SF, Jack, BW, Denktaş, S, and Steegers, EAP. Evidence-based preconceptional lifestyle interventions. Epidemiol Rev. (2014) 36:19–30. doi: 10.1093/epirev/mxt003
13. Department of Health and Social Care. Maternity disparities taskforce explores women's health before and during pregnancy (2022). Available at: https://www.gov.uk/government/news/maternity-disparities-taskforce-explores-womens-health-before-and-during-pregnancy. Accessed August, 24 2022.
14. Davies, SC. Annual report of the chief medical officer, 2014, the health of the 51%: Women (2015). Available at: https://www.gov.uk/government/publications/chief-medical-officer-annual-report-2014-womens-health. Accessed August, 01 2022.
15. Department of Health and Social Care. Women's health strategy for England (2022). Available at: https://www.gov.uk/government/publications/womens-health-strategy-for-england. Accessed January, 10 2023.
16. Sekhon, M, Cartwright, M, and Francis, JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. (2017) 17:88–13. doi: 10.1186/s12913-017-2031-8
17. Diepeveen, S, Ling, T, Suhrcke, M, Roland, M, and Marteau, TM. Public acceptability of government intervention to change health-related behaviours: a systematic review and narrative synthesis. BMC Public Health. (2013) 13:1–11. doi: 10.1186/1471-2458-13-756
18. Murphy, HR, Temple, RC, Ball, VE, Roland, JM, Steel, S, Zill-E-Huma, R, et al. Personal experiences of women with diabetes who do not attend pre-pregnancy care. Diabet Med. (2010) 27:92–100. doi: 10.1111/j.1464-5491.2009.02890.x
19. Spence, M, Alderdice, FA, Harper, R, McCance, DR, and Holmes, VA. An exploration of knowledge and attitudes related to pre-pregnancy care in women with diabetes. Diabet Med. (2010) 27:1385–91. doi: 10.1111/j.1464-5491.2010.03117.x
20. O'Higgins, S, McGuire, BE, Mustafa, E, and Dunne, F. Barriers and facilitators to attending pre-pregnancy care services: the ATLANTIC-DIP experience. Diabet Med. (2014) 31:366–74. doi: 10.1111/dme.12370
21. McCorry, NK, Hughes, C, Spence, D, Holmes, VA, and Harper, R. Pregnancy planning and diabetes: a qualitative exploration of women's attitudes toward preconception care. J Midwifery Womens Health. (2012) 57:396–402. doi: 10.1111/j.1542-2011.2011.00143.x
22. Mazza, D, and Chapman, A. Improving the uptake of preconception care and periconceptional folate supplementation: what do women think? BMC Public Health. (2010) 10:1–6. doi: 10.1186/1471-2458-10-786
23. van der Zee, B, de Beaufort, ID, Steegers, EAP, and Denktaş, S. Perceptions of preconception counselling among women planning a pregnancy: a qualitative study. Fam Pract. (2013) 30:341–6. doi: 10.1093/fampra/cms074
24. Tuomainen, H, Cross-Bardell, L, Bhoday, M, Qureshi, N, and Kai, J. Opportunities and challenges for enhancing preconception health in primary care: qualitative study with women from ethnically diverse communities. BMJ Open. (2013) 3:1–9. doi: 10.1136/bmjopen-2013-002977
25. McGowan, L, Lennon-Caughey, E, Chun, C, McKinley, MC, and Woodside, JV. Exploring preconception health beliefs amongst adults of childbearing age in the UK: a qualitative analysis. BMC Pregnancy Childbirth. (2020) 20:1–13. doi: 10.1186/s12884-020-2733-5
26. Goossens, J, De Roose, M, Van Hecke, A, Goemaes, R, Verhaeghe, S, and Beeckman, D. Barriers and facilitators to the provision of preconception care by healthcare providers: a systematic review. Int J Nurs Stud. (2018) 87:113–30. doi: 10.1016/j.ijnurstu.2018.06.009
27. Heyes, T, Long, S, and Mathers, N. Preconception care: practice and beliefs of primary care workers. Fam Pract. (2004) 21:22–7. doi: 10.1093/fampra/cmh106
28. Ojukwu, O, Patel, D, Stephenson, J, Howden, B, and Shawe, J. General practitioners’ knowledge, attitudes and views of providing preconception care: a qualitative investigation. Ups J Med Sci. (2016) 121:256–63. doi: 10.1080/03009734.2016.1215853
29. Dean, SV, Lassi, ZS, Imam, AM, and Bhutta, ZA. Preconception care: closing the gap in the continuum of care to accelerate improvements in maternal, newborn and child health. Reprod Health. (2014) 11:S1. doi: 10.1186/1742-4755-11-S3-S1
30. World Health Organisation. Preconception care: Maximizing the gains for maternal and child health (2013). Available at: https://www.who.int/maternal_child_adolescent/documents/. Accessed August, 24 2022.
31. Daly, MP, White, J, Sanders, J, and Kipping, RR. Women’s knowledge, attitudes and views of preconception health and intervention delivery methods: a cross-sectional survey. BMC Pregnancy Childbirth. (2022) 22:729. doi: 10.1186/s12884-022-05058-3
32. Collier, A. Critical realism: An introduction to Roy Bhaskar's philosophy. New York: Verso (1994). 292 p.
33. Gale, NK, Heath, G, Cameron, E, Rashid, S, and Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:1–8. doi: 10.1186/1471-2288-13-117
34. Smith, J, and Firth, J. Qualitative data analysis: the framework approach. Nurse Res. (2011) 18:52–62. doi: 10.7748/nr2011.01.18.2.52.c8284
35. O’Brien, BC, Harris, IB, Beckman, TJ, Reed, DA, and Cook, DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. (2014) 89:1245–51. doi: 10.1097/ACM.0000000000000388
37. Braun, V, and Clarke, V. Conceptual and design thinking for thematic analysis. Qual Psychol. (2021) 9:3–26. doi: 10.1037/qup0000196
38. Onwuegbuzie, AJ, and Leech, NL. Sampling designs in qualitative research: making the sampling process more public. Qual Rep. (2007) 12:238–54. doi: 10.46743/2160-3715/2007.1636
39. Ritchie, J, Lewis, J, Nicholls, CM, and Ormston, R. Qualitative research practice: a guide for social science students and researchers. 2rd ed. London: SAGE Publications (2013). 456 p.
40. Malterud, K, Siersma, VD, and Guassora, AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. (2016) 26:1753–60. doi: 10.1177/1049732315617444
41. Grimm, P. Social desirability bias In: JN Sheth and NK Malhotra, editors. Wiley International encyclopedia of marketing. Hoboken: Wiley (2010)
42. Bergen, N, and Labonté, R. “Everything is perfect, and we have no problems”: detecting and limiting social desirability bias in qualitative research. Qual Health Res. (2020) 30:783–92. doi: 10.1177/1049732319889354
43. Carruthers, J. A rationale for the use of semi-structured interviews. J Educ Adm. (1990) 28:28. doi: 10.1108/09578239010006046
44. National Institute for Health Research. Budgeting for involvement: Practical advice on budgeting for actively involving the public in research studies (2013). Available at: https://www.invo.org.uk/wp-content/uploads/2013/07/INVOLVEMHRNBudgeting09Jul2013.pdf. Accessed June, 24 2022.
45. Braun, V, and Clarke, V. Thematic analysis: A practical guide. 1st ed. London: SAGE Publications (2021). 376 p.
46. Lincoln, YS, and Guba, EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Program Eval. (1986) 1986:73–84. doi: 10.1002/ev.1427
47. Office for National Statistics. Number of individuals by gross income band in the UK for the financial year ending 2020 (2021). Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/adhocs/13866numberofindividualsbygrossincomebandintheukforthefinancialyearending2020. Accessed April, 26 2022.
48. Office for National Statistics. Population of the UK by country of birth and nationality (July 2020 to June 2021 edition) (2021). Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/datasets/populationoftheunitedkingdombycountryofbirthandnationality. Accessed December, 09 2022.
49. Office for National Statistics. Population estimates by ethnic group and religion, England and Wales: 2019 (2021). Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/populationestimatesbyethnicgroupandreligionenglandandwales/2019. Accessed April, 26 2022.
50. Office for National Statistics. Graduates in the UK labour market: 2017 (2017). Available at: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/articles/graduatesintheuklabourmarket/2017. Accessed April, 26 2022.
51. National Institute for Health Research. Better beginnings - improving health for pregnancy (2017). Available at: https://evidence.nihr.ac.uk/wp-content/uploads/2020/03/Better-beginnings-web-interactive.pdf. Accessed May, 20 2022.
52. Fisher, WR. Human communication as narration: toward a philosophy of reason, value, and action. Columbia: Univ of South Carolina Press (2021). 220 p.
53. Office for Health Improvement and Disparities. Obesity profile (2022). Available at: https://fingertips.phe.org.uk/profile/national-child-measurement-programme. Accessed November, 07 2022.
54. Bombak, AE, McPhail, D, and Ward, P. Reproducing stigma: interpreting “overweight” and “obese” women's experiences of weight-based discrimination in reproductive healthcare. Soc Sci Med. (2016) 166:94–101. doi: 10.1016/j.socscimed.2016.08.015
55. Wray, S, and Deery, R. The medicalization of body size and women's healthcare. Health Care Women Int. (2008) 29:227–43. doi: 10.1080/07399330701738291
56. Bonell, C, Jamal, F, Melendez-Torres, GJ, and Cummins, S. ‘Dark logic’: theorising the harmful consequences of public health interventions. J Epidemiol Community Health. (2015) 69:95–8. doi: 10.1136/jech-2014-204671
57. Hockey, J. Research methods -- researching peers and familiar settings. Res Pap Educ. (1993) 8:199–225. doi: 10.1080/0267152930080205
58. Berger, R. Now I see it, now I don’t: Researcher’s position and reflexivity in qualitative research. Qual Res. (2015) 15:219–34. doi: 10.1177/1468794112468475
Keywords: preconception care, preconception health, women’s health, intervention development, intervention design, qualitative, framework analysis, sequential exploratory design
Citation: Daly MP, Kipping RR, White J and Sanders J (2024) Women’s views on content and delivery methods for interventions to improve preconception health: a qualitative exploration. Front. Public Health. 12:1303953. doi: 10.3389/fpubh.2024.1303953
Edited by:
Evelyn Loo, Singapore Institute for Clinical Sciences (A*STAR), SingaporeReviewed by:
Han Zhang, Singapore Institute for Clinical Sciences (A*STAR), SingaporeCopyright © 2024 Daly, Kipping, White and Sanders. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael P. Daly, bWljaGFlbC5kYWx5QGJyaXN0b2wuYWMudWs=
 Michael P. Daly
Michael P. Daly Ruth R. Kipping
Ruth R. Kipping James White2
James White2