
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 12 February 2024
Sec. Aging and Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1302783
 Yongqiang Zhang1†
Yongqiang Zhang1† Xia Liu2*†
Xia Liu2*†Aim: The aim of this study was to respectively explore the relationships between physical activity and sedentary behaviors and cardiovascular disease (CVD) and all-cause mortality risk in overweight/obese middle-aged and older patients, and also assess the interaction between physical activity and sedentary behaviors.
Methods: Data of middle-aged and older adults with body mass index (BMI) ≥25 kg/m2 were extracted from the National Health and Nutrition Examination Surveys (NHANES) database in 2007–2018 in this retrospective cohort study. Weighted univariate and multivariate logistic regression analyses were used to explore the associations between physical activity and sedentary behaviors and CVDs; weighted univariate and multivariate Cox regression analyses were used to explore the relationships between physical activity and sedentary behaviors with the risk of all-cause mortality. The interaction effect between physical activity and sedentary behaviors on CVD and all-cause mortality was also assessed. We further explored this interaction effect in subgroups of age and BMI. The evaluation indexes were odds ratios (ORs), hazard ratios (HRs), and 95% confidence intervals (CIs).
Results: Among 13,699 eligible patients, 1,947 had CVD, and 1,560 died from all-cause mortality. After adjusting for covariates, patients who had high sedentary time seemed to have both high odds of CVD [OR = 1.24, 95% CI: (1.06–1.44)] and a high risk of all-cause mortality [HR = 1.20, 95% CI: (1.06–1.37)]. Furthermore, being insufficiently active was linked to high odds of CVD [OR = 1.24, 95% CI: (1.05–1.46)] as well as a high risk of all-cause mortality [HR = 1.32, 95% CI: (1.15–1.51)]. High sedentary time and being insufficiently active had an interaction effect on both high odds of CVD [OR = 1.44, 95% CI: (1.20–1.73)] and high risk of all-cause mortality [HR = 1.48, 95% CI: (1.24–1.76)]. Individuals of different ages with/without obesity need to focus on the potential CVD/mortality risk of high sedentary time and low physical activity (all P < 0.05).
Conclusion: Reducing sedentary time combined with increasing physical activity may benefit health by reducing both the risk of CVD and all-cause mortality in overweight or obese middle-aged and older adults.
Obesity and being overweight are major public health problems currently affecting the global population. Since 1980, the prevalence of obesity has increased twofold in more than 70 countries and continues to rise in most of them (1). In the United States, the prevalence of adult obesity was as high as 42.4% in 2017–2018 and shows a higher prevalence in the middle-aged and older populations aged 40 years and older (2). Obesity contributes to an estimated 4 million deaths globally, more than two-thirds of which are caused by cardiovascular diseases (CVDs) (1). Studies have indicated that obesity or being overweight increases the risk of CVDs in middle-aged and older adults (3, 4). Therefore, ameliorating the pathophysiologic effects of obesity and being overweight and reducing the associated risk of CVDs and mortality are important propositions that need to be addressed.
Physical activity level is an important modifiable factor affecting human health (5). It has been reported that physical activity is negatively associated with the risk of obesity, CVDs, and mortality (6–8). Both the World Health Organization (WHO) and the American College of Cardiology (ACC)/American Heart Association (AHA) have recommended appropriate physical activity for health promotion (9, 10). In 2020, the WHO updated and provided new recommendations for reducing sedentary behaviors in addition to increasing physical activity, although the current evidence is insufficient to quantify the threshold of sedentary behaviors (10). Sedentary behavior represents the lowest level of the physical activity spectrum and is generally defined as an energy expenditure of <1.5 metabolic equivalents (METs) when sitting or lying down during waking hours. The associations between sedentary behaviors and CVDs and the risk of mortality are influenced by the level of physical activity, and as physical activity increases, the risk of mortality from sedentariness diminishes or even cancels out (11–13). A longitudinal cohort study in Japan showed an interaction between physical activity levels and sedentary behaviors on the risk of all-cause mortality in older adults (14). Nevertheless, in middle-aged and older adults who are overweight or obese, who are at high risk for CVDs, the combined effects of physical activity and sedentary behaviors on CVD and mortality are still unclear.
Herein, we speculated that physical activity and sedentary behaviors have a combined effect on CVD as well as the all-cause mortality risk in middle-aged and older patients who are overweight/obese. We hope the research findings could provide some references for lifestyle intervention and management among those at risk of CVD or mortality.
In this retrospective cohort study, data on middle-aged and older persons were extracted from the National Health and Nutrition Examination Surveys (NHANES) database between 2007 and 2018. The NHANES surveys are conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC) to assess the nutritional and health status of the civilian non-institutionalized population in the United States. It includes a complex, multistage stratified probability sample based on selected counties, blocks, households, and persons within households. The well-trained NCHS professionals conduct interviews in participants' homes, and extensive physical examinations are conducted at mobile exam centers (MECs). More details are available on the NAHENS webpage: https://www.cdc.gov/nchs/nhanes/index.htm.
Initially, 15,076 adults aged 40–79 years with a body mass index (BMI) of ≥25 kg/m2 were included. The exclusion criteria were (1) missing information on CVD, sedentary behaviors, or all-cause mortality (n = 225) and (2) missing information on the potential covariates, including marital status, education level, smoking, healthy eating index 2015 (HEI-2015) (15), and chronic kidney disease (CKD) (n = 1,152). Finally, 13,699 individuals were deemed eligible. The NHANES was approved by the Institutional Review Board (IRB) of the NCHS. The data were anonymized, and all the participants provided informed consent. No ethical approval of our agency's IRB was required since this database was publicly available.
Physical activity was converted into MET, which was calculated based on the information collected via the NHANES physical activity questionnaire (PAQ). The corresponding questions were as follows: “In a typical week, do you do any vigorous-intensity sports, fitness, or recreational activities that cause large increases in breathing or heart rate like running or basketball for at least 10 min continuously?” and “In a typical week, do you do any moderate-intensity sports, fitness, or recreational activities that cause a small increase in breathing or heart rate such as brisk walking, bicycling, swimming, or volleyball for at least 10 min continuously?” Energy expenditure (MET·min) = recommended MET × exercise time of corresponding activity (min). According to a previous study, we classified physical activity into two levels: energy expenditure <450 MET·min/week was defined as insufficiently active; otherwise, it was defined as sufficiently active (9).
The information on sedentary behavior was also self-reported through the PAQs, with the question “How much time do you usually spend sitting on a typical day?” In specific, sedentary behavior was defined as the time spent sitting at school or home and getting to and from places, including sitting at a desk, traveling in a car or bus, reading, playing cards, watching television, or using a computer, which does not include time spent sleeping. The cutoff value for sedentary behaviors was 6 h/day, according to a previous study (16).
The study outcomes were CVD and all-cause mortality. CVD was self-reported based on the NHANES multiple-choice question (MCQ) with the question: “Have you ever been told you had (congestive) heart failure, coronary heart disease, angina/angina pectoris, heart attack, stroke?” An individual who gave a positive answer was considered a patient with CVD (17).
We used the NHANES publicly linked mortality file as of 31 December 2019, which was correlated with the NCHS with the National Death Index (NDI) through a probability matching algorithm to determine the mortality status of the patients: https://ftp.cdc.gov/pub/health_statistics/NCHS/datalinkage/linked_mortality/. The follow-up ended when an individual died or on 31 December 2019.
We extracted data from the database of the following variables: age, sex, race, education level, marital status, poverty income ratio (PIR), alcohol consumption, smoking, diabetes mellitus (DM), dyslipidemia, hypertension, CKD, BMI, estimated glomerular filtration rate (eGFR), urinary albumin to creatinine ratio (UACR), HEI-2015, total energy intake, cardiovascular drugs use, cancer, arthritis, human immunodeficiency virus (HIV) infection, and glutamic oxaloacetic transaminase to serum glutamic pyruvic transaminase ratio (AST/ALT).
During the NHANES household interview, smokers were individuals who self-reported having smoked more than 100 cigarettes in their lives. The pattern of alcohol consumption was also captured by the NHANES questionnaires (18). Persons with total cholesterol (TC) ≥200 mg/dl (5.2 mmol/L), triglycerides (TG) ≥150 mg/dl (1.7 mmol/L), low-density lipoprotein cholesterol (LDL-C) ≥130 mg/dl (3.4 mmol/L), high-density lipoprotein cholesterol (HDL-C) ≤ 40 mg/dl (1.0 mmol/L), self-reported hypercholesteremia, or receiving lipid-lowering therapy were identified as patients with dyslipidemia (19). DM was defined according to a self-reported diagnosis, the use of oral hypoglycemic agents or insulin, glycosylated hemoglobin (HbAlc) ≥6.5%, a plasma glucose level ≥200 mg/dl at 2 h after the oral glucose tolerance test (OGTT), or a fasting glucose level ≥126 mg/dl. CKD was defined as eGFR <60 ml/min per 1.73 m2 or UACR ≥30 mg/g (20). In addition, cancer, arthritis, and HIV infections were self-reported. Dietary total energy intake was calculated through information on “total nutrient intakes” and “total dietary supplements” collected from two 24-h dietary recalls in the NHANES. BMIs were divided into four levels according to the WHO criteria, including underweight (BMI <18.5 kg/m2), normal weight (BMI = 18.5–24.9 kg/m2), overweight (BMI = 25–29.9 kg/m2), and obese (BMI ≥30 kg/m2). Participants who aged <65 years were considered middle-aged adults, whereas those who aged ≥65 years were considered older adults (21).
Continuous data were described using mean ± standard error (mean ± SE), and a weighted t-test was used for comparison between the two groups. Categorical data were expressed as frequency with constituent ratio [N (%)] and chi-square test (χ2) for the comparison.
We used the MEC 2-year sample weights (WTMEC2YR) for combined analyses of NHANES data from 2007 to 2018 (22). A weighted univariate logistic regression analysis was used to screen the covariates associated with CVD, and a weighted Cox regression analysis was used to screen those associated with all-cause mortality. The associations of physical activity and sedentary behaviors with CVD in middle-aged and older patients who were overweight/obese were explored using weighted univariate and multivariate logistic regression analyses. The relationships between physical activity and sedentary behaviors and the risk of all-cause mortality were investigated using weighted univariate and multivariate Cox regression analyses (23). The interaction effects between physical activity and sedentary behaviors on CVD and the risk of all-cause mortality were also assessed. We further explored these relationships in subgroups of age and BMI.
When the study outcome was CVD, the multivariate model adjusted for age, sex, race, education level, marital status, PIR, alcohol consumption, BMI, smoking, DM, dyslipidemia, hypertension, CKD, HEI-2015, total energy intake, cardiovascular drugs use, cancer, arthritis, HIV infection, and AST/ALT. When the outcome was all-cause mortality, the multivariate model adjusted for age, sex, race, education level, marital status, PIR, BMI, smoking, DM, hypertension, CKD, total energy intake, cardiovascular drugs use, CVD, cancer, arthritis, HIV infection, and AST/ALT.
The evaluation indexes were odds ratios (ORs), hazard ratios (HRs), and 95% confidence intervals (CIs). A two-sided P < 0.05 was considered a significant statistical association. Statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). The variables, including missing values, are shown in Supplementary Table S1, and they have been deleted.
Figure 1 shows the flowchart of participant screening. We initially included 15,076 individuals aged 40–79 years with a BMI of ≥25 kg/m2 from the NHANES. Then, we excluded patients without information about CVD (n = 88), sedentary time (n = 100), or all-cause mortality (n = 37). Those who had missing data on education level (n = 11), smoking (n = 7), HEI-2015 (n = 956), CKD (n = 174), or marital status (n = 4) were also excluded. Finally, 13,699 individuals were eligible.
A comparison of characteristics between the non-CVD group (n = 11,752) and the CVD group (n = 1,947) is shown in Table 1. After an average of 88.5-month follow-up, 1,560 (9.17%) participants died from all-cause. We found that 8,008 (62.96%) middle-aged and older adults were sufficiently active, whereas 6,577 (54.19%) had high sedentary time.
We first screened the covariates associated with CVD and all-cause mortality, respectively (Supplementary Table S2). Then, we respectively explored the relationships of physical activity and sedentary behaviors with CVD (Table 2) and of physical activity with sedentary behaviors and all-cause mortality (Table 3). After adjusting for covariates, we found that compared with low sedentary time, patients who had a higher sedentary time seemed to have both higher odds of CVD [OR = 1.24, 95% CI: (1.06–1.44)] and a higher risk of all-cause mortality [HR = 1.20, 95% CI: (1.06–1.37)]. Furthermore, being insufficiently active was linked to both high odds of CVD [OR = 1.24, 95% CI: (1.05–1.46)] and a high risk of all-cause mortality [HR = 1.32, 95% CI: (1.15–1.51)] among overweight or obese middle-aged and older adults.
We further investigated the interaction effects between physical activity and sedentary behaviors on CVD and all-cause mortality (Table 4). After adjusting for covariates, the results showed that middle-aged and older adults who were overweight/obese had high sedentary time combined with insufficient physical activity and seemed to have both high odds of CVD [OR = 1.44, 95% CI: (1.20–1.73)] and a high risk of all-cause mortality [HR = 1.48, 95% CI: (1.24–1.76)], compared with those who had low sedentary time combined with sufficient physical activity.
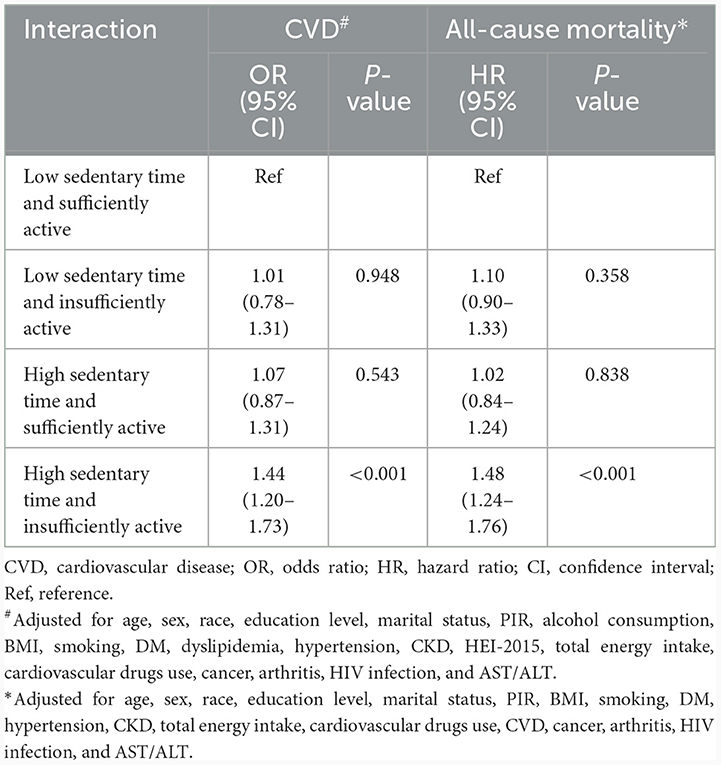
Table 4. Interaction between physical activity, sedentary behaviors in CVD, and all-cause mortality.
Table 5 shows the subgroup analyses of the combined effect between physical activity and sedentary behaviors on CVD and all-cause mortality. For patients aged ≥65 years, high sedentary time [OR = 1.41, 95% CI: (1.11–1.78)] and being insufficiently active [OR = 1.25, 95% CI: (1.02–1.54)] were both associated with high odds of CVD, whereas these relationships in the <65-year-old subgroup were not significant (all P > 0.05). Similarly, in the BMI ≥30 kg/m2 group, patients with high sedentary time [OR = 1.29, 95% CI: (1.02–1.61)] or who were insufficiently active [OR = 1.27, 95% CI: (1.04–1.57)] had high odds of CVD, while these associations were not significant among those whose BMI was <30 kg/m2 (all P > 0.05). In addition, the interaction effect between physical activity and sedentary behaviors on CVD was found in patients in the subgroups of <65 years, ≥65 years, and with a BMI of ≥30 kg/m2 (all P < 0.05).
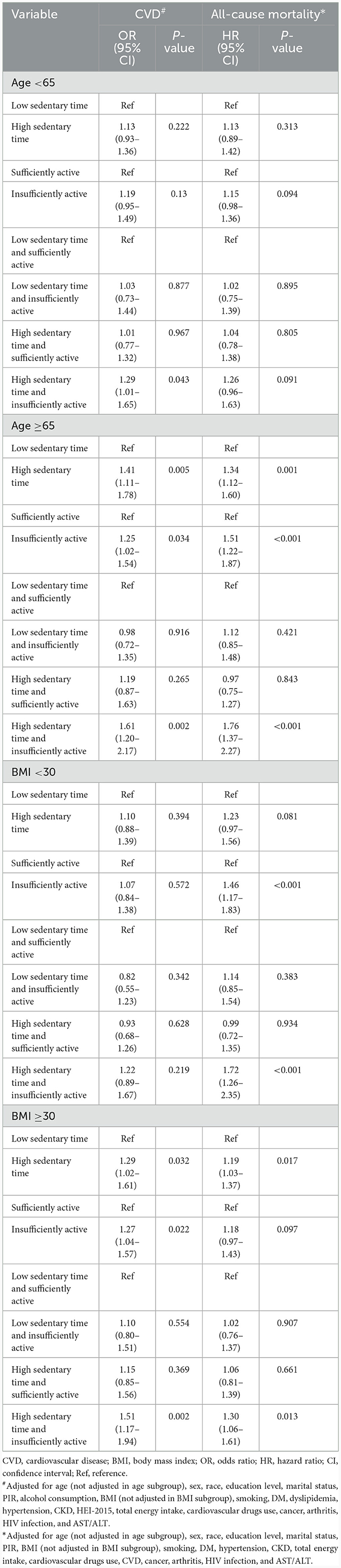
Table 5. Association between physical activity, sedentary behaviors, CVD, and all-cause mortality in age and BMI subgroups.
High sedentary time was linked to a high risk of all-cause mortality in patients aged ≥65 years [HR = 1.34, 95% CI: (1.12–1.60)]. Being insufficiently active was associated with a high risk of all-cause mortality in patients aged ≥65 years [HR = 1.51, 95% CI: (1.22–1.87)] and with BMI <30 kg/m2 [HR = 1.46, 95% CI: (1.17–1.83)]. Moreover, the interaction effect between high sedentary time and being insufficiently active on having a high risk of all-cause mortality was found in patients aged ≥65 years, with BMI <30 kg/m2, and BMI ≥30 kg/m2 subgroups (all P < 0.05).
In this study, we explored the relationships between physical activity and sedentary behaviors with CVD and all-cause mortality risk in middle-aged and older patients who were overweight/obese, respectively. We also assessed the interaction effects between physical activity and sedentary behaviors on CVD as well as all-cause mortality. The results showed that high sedentary time and being insufficiently active had an interaction effect on both high odds of CVD and a high risk of all-cause mortality. These associations were also found in patients with different ages and BMI levels.
To the best of our knowledge, no study has explored the interaction effect between physical activity and sedentary behaviors on CVD and all-cause mortality in middle-aged and older adults who are overweight or obese. A prospective cohort study in 70-year-old populations showed that objectively measured light-intensity physical activity and moderate-intensity physical activity were each associated with a lower risk of all-cause mortality, while sedentary time was associated with increased risk (24). Liang et al. (25) found that long-term sedentary behaviors increased the risk of CVDs in healthy adults, whereas physical activity reduced the risk of CVDs and improved indicators associated with CVDs. Our findings relatively further verified these relationships in middle-aged and older adults who were overweight/obese, and differently, we based them on the NHANES database, which includes representative populations in the United States. Some studies indicated a potential regulating effect of physical activity on the sedentary behaviors associated with CVD or all-cause mortality risk. However, they often focus on older populations or obese populations. Han et al. (26) considered that despite increased time spent on sedentary behaviors, maintaining physical activity could reduce the occurrence of CVD in healthy Korean adults. Furthermore, physical activity and sedentary behaviors are associated with adiposity-related traits, apparently in a bidirectional manner (27). Therefore, the current study combined their study populations and investigated and suggested that high sedentary time combined with low physical activity was linked to a high risk of both CVD and all-cause mortality in middle-aged and older patients who were overweight/obese.
The mechanisms through which sedentary behaviors combined with physical activity influence CVD and all-cause mortality are complex and multifaceted. Sedentary behaviors have been identified as a risk factor for CVD, which was suggested to have the strongest association with all causes of CVD mortality (28, 29). Sedentary behaviors result in a lack of physical activity, leading to a decreased turnover of endogenous energy stores, myogenic glycogen, and intracellular lipids, which in turn can lead to skeletal muscle insulin resistance (25). The increased adipogenesis promotes the production of very low-density lipoproteins and lower high-density lipoprotein levels in the liver in hyperinsulinism, which may contribute to the development of metabolic syndrome and also CVDs. Additionally, steatosis may cause hyperglycemia, which not only causes DM but also potentially increases the risk of CVD (30, 31). Several behavioral and biological pathways could explain the potential regulating effect of physical activity on CVD and the all-cause mortality risk associated with sedentary behaviors, including metabolic and sex hormones, inflammation, and immunity (32). Prolonged, uninterrupted sitting is related to impaired glucose metabolism and increased systemic inflammation, which can be attenuated by physical activities (33, 34). Moreover, sitting may induce exercise resistance and diminish the benefits of physical activity (35). Nevertheless, additional studies are needed to evaluate whether the observed interaction between sedentary behaviors and physical activity on CVD and all-cause mortality is causal.
The joint association between sedentary behaviors and physical activity on CVD and mortality outcomes has been explored in healthy populations. A harmonized meta-analysis summarized evidence from 13 studies of more than 1 million adults and showed that long sedentary time was associated with increased all-cause mortality among adults who engaged in <30 MET hour/week of physical activity (11). In 2018, the United States Department of Health and Human Services clearly acknowledged the health risks associated with sedentary behavior and suggested that people of all ages would benefit from more regular physical activity and less sedentary behavior for the first time in the Physical Activity Guidelines for Americans (36). Despite the limited evidence available, the WHO strongly recommends limiting the amount of sedentary time and substituting it with any physical activity to improve health, particularly for individuals with long-term diseases (10).
We also explored the associations of sedentary behaviors and physical activity with CVD and all-cause mortality risk in individuals of different ages and BMIs. The subgroup analysis results showed that the combined effect of physical activity and sedentary behaviors on CVD was significant in patients aged <65 and ≥65 years, with BMI ≥30 kg/m2. Furthermore, this interaction on risk of all-cause mortality was found in patients in the subgroups aged ≥65 years with BMI <30 kg/m2 and BMI ≥30 kg/m2. Physical activity is a protective factor of successful aging in middle-aged and older populations, which can prevent the development of many chronic diseases, such as metabolic syndrome, DM, hypertension, dyslipidemia, depression, osteoarthritis, osteoporosis, and non-alcoholic fatty liver disease (37). In fact, there is a dose-response relationship between physical activity and a decrease in mortality in middle-aged and older people (38). In the current research, we found that long sedentary time combined with low physical activity levels was associated with high odds of CVD in overweight/obese adults aged <65 years, while this combined effect was associated with a high risk of all-cause mortality in those aged ≥65 years. It was inferred that middle-aged people who were overweight or obese may pay more attention to improving and preventing the development of CVD because their basic health condition may be better than that of older people. Likewise, older adults should take care of their sedentary time and increase appropriate physical activity to reduce the risk of mortality. Moreover, in patients with obesity (BMI ≥30 kg/m2), high sedentary time as well as low physical activity may increase the risk of both CVD and all-cause mortality in our study. Clark et al. (39) concluded that total physical activity habits, including time spent being sedentary and lower-intensity physical activity, impact the levels of lipoprotein-associated phospholipase A2, an important inflammatory marker and marker of CVD risk. Wanders et al. (40) confirmed a beneficial association between physical activity and whole-body insulin resistance. These findings indicated that the potential mechanisms of the relationship between sedentary behaviors and physical activity, CVD, and all-cause mortality may be varied. Therefore, the causal associations and specific mechanisms between sedentary behaviors, physical activity, and CVD/mortality need to be clarified in the future, which may be beneficial management and preventive measures for chronic disease and mortality in obese patients.
This study is based on the NHANES database, which has large samples with good representativeness in the United States. We analyzed the combined effect between physical activity and sedentary behaviors on CVD and all-cause mortality risk, which may provide some references for behavioral interventions in overweight/obese middle-aged and older adults (e.g., appropriate physical activity to antagonize the risks associated with prolonged sedentary time). However, there are also some limitations to our study. The information about CVD was collected according to self-reported diagnosis, and that of physical activity as well as sedentary behaviors was obtained through questionnaires, which cannot avoid the reporting bias. Additionally, although we have tried our best to include possible confounding factors, such as diet, lifestyle, comorbidities, and treatment, due to the limitations of the NHANES database, other potential covariates, including place of abode (urban or rural), changes in lifestyle, and treatment regimen during the follow-up, could not be obtained and included in this exploration.
Low physical activity and long sedentary time were associated with both high odds of CVDs and a high risk of all-cause mortality in middle-aged and older adults who were overweight or obese, and there was an interaction effect between them.
Publicly available datasets were analyzed in this study. This data can be found at: NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
The requirement of ethical approval was waived by the People's Hospital of Lincang for the studies involving humans because the database is publicly available. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing—original draft, Writing—review & editing. XL: Writing—original draft, Writing—review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1302783/full#supplementary-material
1. Afshin A, Reitsma MB, Murray CJL. Health effects of overweight and obesity in 195 countries. N Engl J Med. (2017) 377:1496–7. doi: 10.1056/NEJMc1710026
2. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. (2020) 360:1–8.
3. Dhana K, Berghout MA, Peeters A, Ikram MA, Tiemeier H, Hofman A, et al. Obesity in older adults and life expectancy with and without cardiovascular disease. Int J Obes. (2016) 40:1535–40. doi: 10.1038/ijo.2016.94
4. Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. (2018) 3:280–7. doi: 10.1001/jamacardio.2018.0022
5. Kelly RS, Kelly MP, Kelly P. Metabolomics, physical activity, exercise and health: a review of the current evidence. Biochim Biophys Acta Mol Basis Dis. (2020) 1866:165936. doi: 10.1016/j.bbadis.2020.165936
6. Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM, et al. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med Sci Sports Exerc. (2019) 51:1270–81. doi: 10.1249/MSS.0000000000001939
7. Ciumarnean L, Milaciu MV, Negrean V, Orasan OH, Vesa SC, Salagean O, et al. Cardiovascular risk factors and physical activity for the prevention of cardiovascular diseases in the elderly. Int J Environ Res Public Health. (2021) 19. doi: 10.3390/ijerph19010207
8. Yuan F, Gong W, Ding C, Li H, Feng G, Ma Y, et al. Association of physical activity and sitting time with overweight/obesity in chinese occupational populations. Obes Facts. (2021) 14:141–7. doi: 10.1159/000512834
9. Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. (2007) 116:1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649
10. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
11. Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. (2016) 388:1302–10. doi: 10.1016/S0140-6736(16)30370-1
12. Pandey A, Salahuddin U, Garg S, Ayers C, Kulinski J, Anand V, et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease: a meta-analysis. JAMA Cardiol. (2016) 1:575–83. doi: 10.1001/jamacardio.2016.1567
13. Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. (2019) 73:2062–72. doi: 10.1016/j.jacc.2019.02.031
14. Watanabe D, Yamada Y, Yoshida T, Watanabe Y, Hatamoto Y, Fujita H, et al. Association of the interaction between physical activity and sitting time with mortality in older Japanese adults. Scand J Med Sci Sports. (2022) 32:1757–67. doi: 10.1111/sms.14234
15. Shan Z, Wang F, Li Y, Baden MY, Bhupathiraju SN, Wang DD, et al. Healthy eating patterns and risk of total and cause-specific mortality. JAMA Intern Med. (2023) 183:142–53. doi: 10.1001/jamainternmed.2022.6117
16. Cao C, Friedenreich CM, Yang L. Association of daily sitting time and leisure-time physical activity with survival among US cancer survivors. JAMA Oncol. (2022) 8:395–403. doi: 10.1001/jamaoncol.2021.6590
17. Xu JP, Zeng RX, He MH, Lin SS, Guo LH, Zhang MZ. Associations between serum soluble alpha-klotho and the prevalence of specific cardiovascular disease. Front Cardiovasc Med. (2022) 9:899307. doi: 10.3389/fcvm.2022.899307
18. Niezen S, Trivedi HD, Mukamal KJ, Jiang ZG. Associations between alcohol consumption and hepatic steatosis in the USA. Liver Int. (2021) 41:2020–3. doi: 10.1111/liv.15020
19. Jellinger PS, Smith DA, Mehta AE, Ganda O, Handelsman Y, Rodbard HW, et al. American association of clinical endocrinologists' guidelines for management of dyslipidemia and prevention of atherosclerosis. Endocr Pract. (2012) 18(Suppl 1):1–78. doi: 10.4158/EP.18.S1.1
20. Jespersen T, Kruse N, Mehta T, Kuwabara M, Noureddine L, Jalal D. Light wine consumption is associated with a lower odd for cardiovascular disease in chronic kidney disease. Nutr Metab Cardiovasc Dis. (2018) 28:1133–9. doi: 10.1016/j.numecd.2018.06.018
21. Zhang J, Ren Z, Zhang Q, Zhang R, Zhang C, Liu J. Lower hydration status increased diabetic retinopathy among middle-aged adults and older adults: results from NHANES 2005-2008. Front Public Health. (2022) 10:1023747. doi: 10.3389/fpubh.2022.1023747
22. Li Y, Wang J, Cai Y, Chen H. Association of serum vitamin D with periodontal disease. Int Dent J. (2023) 73:777–83. doi: 10.1016/j.identj.2023.06.004
23. Lee SW. Kaplan-Meier and Cox proportional hazards regression in survival analysis: statistical standard and guideline of Life Cycle Committee. Life Cycle. (2023) 3:e8. doi: 10.54724/lc.2023.e8
24. Ballin M, Nordstrom P, Niklasson J, Nordstrom A. Associations of objectively measured physical activity and sedentary time with the risk of stroke, myocardial infarction or all-cause mortality in 70-year-old men and women: a prospective cohort study. Sports Med. (2021) 51:339–49. doi: 10.1007/s40279-020-01356-y
25. Liang ZD, Zhang M, Wang CZ, Yuan Y, Liang JH. Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-a meta-analysis and systematic review. Front Public Health. (2022) 10:1018460. doi: 10.3389/fpubh.2022.1018460
26. Han J, Ju YJ, Lee SY. Physical activity, sedentary behavior, and cardiovascular disease risk in Korea: a trajectory analysis. Epidemiol Health. (2023) 45:e2023028. doi: 10.4178/epih.e2023028
27. Schnurr TM, Stallknecht BM, Sorensen TIA, Kilpelainen TO, Hansen T. Evidence for shared genetics between physical activity, sedentary behaviour and adiposity-related traits. Obes Rev. (2021) 22:e13182. doi: 10.1111/obr.13182
28. Young DR, Hivert MF, Alhassan S, Camhi SM, Ferguson JF, Katzmarzyk PT, et al. Sedentary behavior and cardiovascular morbidity and mortality: a science advisory from the American Heart Association. Circulation. (2016) 134:e262–279. doi: 10.1161/CIR.0000000000000440
29. Katzmarzyk PT, Powell KE, Jakicic JM, Troiano RP, Piercy K, Tennant B, et al. sedentary behavior and health: update from the 2018 physical activity guidelines advisory committee. Med Sci Sports Exerc. (2019) 51:1227–41. doi: 10.1249/MSS.0000000000001935
30. Leiter LA. From hyperglycemia to the risk of cardiovascular disease. Rev Cardiovasc Med. (2006) 7(Suppl 2):S3–9.
31. Booth FW, Laye MJ, Lees SJ, Rector RS, Thyfault JP. Reduced physical activity and risk of chronic disease: the biology behind the consequences. Eur J Appl Physiol. (2008) 102:381–90. doi: 10.1007/s00421-007-0606-5
32. Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, et al. American college of sports medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc. (2019) 51:2391–402. doi: 10.1249/MSS.0000000000002117
33. Dogra S, Wolf M, Jeffrey MP, Foley RCA, Logan-Sprenger H, Jones-Taggart H, et al. Disrupting prolonged sitting reduces IL-8 and lower leg swell in active young adults. BMC Sports Sci Med Rehabil. (2019) 11:23. doi: 10.1186/s13102-019-0138-4
34. Dunstan DW, Dogra S, Carter SE, Owen N. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol. (2021) 18:637–48. doi: 10.1038/s41569-021-00547-y
35. Akins JD, Crawford CK, Burton HM, Wolfe AS, Vardarli E, Coyle EF. Inactivity induces resistance to the metabolic benefits following acute exercise. J Appl Physiol (1985) 126.(2019) 1088–94. doi: 10.1152/japplphysiol.00968.2018
36. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
37. Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. (2012) 2:1143–211. doi: 10.1002/cphy.c110025
38. Gebel K, Ding D, Chey T, Stamatakis E, Brown WJ, Bauman AE. Effect of moderate to vigorous physical activity on all-cause mortality in middle-aged and older Australians. JAMA Intern Med. (2015) 175:970–7. doi: 10.1001/jamainternmed.2015.0541
39. Clark K, Sharp S, Womack CJ, Kurti SP, Hargens TA. Increased sedentary time and decreased physical activity increases lipoprotein associated phospholipase A(2) in obese individuals. Nutr Metab Cardiovasc Dis. (2022) 32:1703–10. doi: 10.1016/j.numecd.2022.04.023
Keywords: age, BMI, lifestyle, mortality, cardiovascular disease
Citation: Zhang Y and Liu X (2024) Effects of physical activity and sedentary behaviors on cardiovascular disease and the risk of all-cause mortality in overweight or obese middle-aged and older adults. Front. Public Health 12:1302783. doi: 10.3389/fpubh.2024.1302783
Received: 27 September 2023; Accepted: 17 January 2024;
Published: 12 February 2024.
Edited by:
Mihnea-Alexandru Găman, Carol Davila University of Medicine and Pharmacy, RomaniaReviewed by:
Dong Keon Yon, Kyung Hee University, Republic of KoreaCopyright © 2024 Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xia Liu, bGl1eGlhZGN0QG91dGxvb2suY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.