
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 04 April 2024
Sec. Aging and Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1292289
 Hongji Zeng1
Hongji Zeng1 Chen Miao2
Chen Miao2 Rui Wang1
Rui Wang1 Weijia Zhao1
Weijia Zhao1 Wenjuan Wang1
Wenjuan Wang1 Yahui Liu1
Yahui Liu1 Shufan Wei1
Shufan Wei1 Anqi Liu1
Anqi Liu1 Huibing Jia1
Huibing Jia1 Guoxin Li1
Guoxin Li1 Junge Zhou1
Junge Zhou1 Xuejiao Chen1
Xuejiao Chen1 Qingfeng Tian1*
Qingfeng Tian1*Rationale: With the accelerating process of population aging, the comorbidity of chronic disease (CCD) has become a major public health problem that threatens the health of older adults.
Objective: This study aimed to assess whether CCD is associated with basic activities of daily living (BADL) and explore the factors influencing BADL in older adults.
Method: A cross-sectional community health survey with stratified random sampling among older residents (≥60 years old) was conducted in 2022. A questionnaire was used to collect information on BADL, chronic diseases, and other relevant aspects. Propensity score matching (PSM) was used to match the older adults with and without CCD. Univariate and multivariate logistic regression analyses were used to explore the factors influencing BADL. PSM was used to match participants with single-chronic disease (SCD) and CCD.
Results: Among the 47,720 participants, those with CCD showed a higher prevalence of BADL disability (13.07%) than those with no CCD (6.33%) and SCD (7.39%). After adjusting for potential confounders with PSM, 6,513 pairs of cases with and without CCD were matched. The univariate analysis found that the older adults with CCD had a significantly higher prevalence of BADL disability (13.07%, 851 of 6,513) than those without CCD (9.83%, 640 of 6,513, P < 0.05). The multivariate logistic regression analysis revealed that CCD was a risk factor for BADL in older adults [OR = 1.496, 95% CI: 1.393–1.750, P < 0.001]. In addition, age, educational level, alcohol intake, social interaction, annual physical examination, retirement benefits, depression, weekly amount of exercise, and years of exercise were related to BADL disability (P < 0.05). PSM matching was performed on participants with CCD and SCD and showed that the older adults with CCD had a significantly higher prevalence of BADL disability (13.07%, 851 of 6,513) than those with SCD (11.39%, 742 of 6,513, P < 0.05).
Conclusion: The older adults with CCD are at a higher risk of BADL disability than their counterparts with no CCD or SCD. Therefore, we advocate paying attention to and taking measures to improve the health and quality of life of these individuals.
The challenge of an aging population is a relatively recent phenomenon in historical terms, but its acceleration has become increasingly apparent since the beginning of the 21st century (1). As of 2020, the total number of Chinese adults aged ≥60 years has reached 264.02 million, accounting for 18.70% of the total population (2). Research indicates that China will enter a highly aging society in 2035, with the proportion of older individuals exceeding 20% (3).
With the global population aging, there is a growing emphasis on chronic diseases due to the increasing life expectancy (4). The World Health Organization (WHO) reports that chronic diseases account for 38 million deaths annually (5). In the United States, half of all adults are affected by chronic diseases (6). Similarly, in Europe, a study found that over one-third of European adults suffer from chronic diseases, which contribute to more than 80% of total deaths (7). In China, over 300 million individuals have been diagnosed with chronic diseases, representing 86.8% of all-cause mortality each year. Additionally, chronic diseases have become the primary cause of disability among Chinese adults (8).
According to the WHO, comorbidity of chronic diseases (CCD) refers to the presence of two or more chronic diseases in a single individual (9). As chronic diseases continue to be prevalent, CCD has emerged as a significant global public health concern (10). The complex causes of chronic diseases, including the correlation with various behavioral factors and the existence of common risk factors shared among different diseases, contribute to CCD (11). Previous studies have shown that 38% of American adults have experienced CCD (12), while around three-quarters of European Union citizens aged 65 and above have been affected (13). With the rapid aging of the population, CCD is expected to pose significant challenges and threats to healthcare systems (10).
BADL refers to the basic daily movements that individuals perform to maintain their independence, such as dressing and grooming (14). It is a crucial indicator of physical and cognitive ability in older adults and is considered a vital component of healthy aging and independent living (15). Therefore, a comprehensive understanding of BADL is essential for future health-service planning. However, most studies of BADL in the older adults worldwide are based on a single chronic disease. There is insufficient research on the association between CCD and BADL. Therefore, the current study was carried out to analyze the impact of CCD on BADL in older adults to provide references for improving their quality of life.
In 2021, we conducted a preliminary survey in Zhongmou County, Henan Province, to estimate the sample size required for the formal survey. The preliminary survey lasted 1 month with the same selection criteria as the formal study. During this period, 3,245 participants were included, and the prevalence of CCD was 15.79%. Additionally, we conducted reliability and validity tests based on the preliminary survey because some of the assessments may be affected by subjective factors. The results showed Cronbach's α of 0.932 and a KMO of 0.969. Based on the CCD prevalence of 15.79%, we estimated the sample size, assuming that the probability of type I error was α = 0.05, P = 15.79, and the margin of error was 0.05. The formula was as follows:
Based on the expected data loss rate of 20%, we estimated that at least 24,518 participants were required.
In 2022, we conducted a community health survey using a stratified random sampling method among the older adults (aged ≥60 years) from 635 communities in county-level administrative regions under the jurisdiction of Zhengzhou City, Henan Province, including Zhongyuan, Erqi, Guancheng, Jinshui, Shangjie, Huiji, Gongyi, Xingyang, Xinmi, Dengfeng, and Zhongmou. This study was approved by the Ethics Committee of Zhengzhou University (Ethical Number: ZZUIRB2022-07) and conducted in accordance with the relevant guidelines and local regulations. Written informed consent was obtained from each patient before enrollment in the study.
During the survey, we conducted a dynamic data entry for CCD prevalence to monitor the sample saturation rate throughout the study. Sample saturation refers to the point at which the sample size reaches a certain level, and there is no significant change in CCD prevalence with further increases in the sample size. We found that the sample began to saturate when the sample size reached 45,289. We then stopped the survey after 2 weeks.
The invited participants were informed of the topic before their tentative consent to complete the survey. Participants were excluded if they met the following criteria: (1) < 60 years of age and (2) unable to cooperate or complete the survey due to aphasia, severe psychological disorders, or cognitive impairments. Finally, 48,232 participants were enrolled. After excluding 512 incomplete cases, 47,720 cases were included in this study. PSM was used to eliminate the endogeneity of control variables and the interference of confounding factors and to improve the accuracy of the results. In the first PSM, 6,513 pairs of cases with CCD and no CCD were matched, while in the second PSM, 6,513 pairs of cases with CCD and SCD were matched. None of the variables used in the final analysis contained missing data. The flowchart is shown in Figure 1.
This study used a self-designed questionnaire, which has been reviewed and approved by experts at Zhengzhou University. All components of the questionnaire were derived from standardized sub-questionnaires.
BADL is the explained variable, which was assessed using the modified Barthel Index (MBI). The scores range from 0 to 100, with higher scores indicating greater BADL. The scale covers 10 subscales, namely, fecal continence, micturition continence, eating, dressing, bathing, personal hygiene, toileting, moving, walking, and climbing stairs (16). It was reported that when the score was above 60, most older adults could manage their daily lives independently, while the older adults with an MBI < 60 could not independently complete many daily activities (17). As a result, participants were divided into two groups according to whether or not their MBI scores were higher than 60. Cronbach's α for the MBI was 0.916. The assessment of BADL was based on a face-to-face investigation (Appendix A).
The condition of chronic disease was the explanatory variable. CCD refers to an individual simultaneously suffering from two or more chronic diseases. No CCD refers to an individual suffering from < 1 chronic disease. SCD refers to an individual with a chronic disease. First, the participants were divided into CCD and no CCD groups for the first PSM. For further analysis, the participants were divided into the CCD and SCD groups for the second PSM. In this study, 16 chronic diseases, namely hypertension, diabetes, heart disease, stroke and cerebrovascular disease, emphysema, asthma or pneumonia, prostate disease, gastrointestinal ulcer, Parkinson's disease, dementia, epilepsy, dyslipidemia, cholecystitis or gallstone, chronic nephritis, hysteromyoma, and hepatitis, were included. Throughout the study, we requested primary healthcare institutions to provide patients' medical records to ensure the accuracy of the disease status documentation (18).
Control variables included (1) sociodemographic characteristics: age (years), sex (male/female), type of residence (urban/rural), body mass index (BMI, body weight divided by squared of height, kg/m2), educational level (under junior high school/junior high school or above), and ethnicity (Han/minority nationality); (2) social support: cohabitation (living alone/living with others), daily care from offspring (more than once per week), and social interaction (more than once per week); (3) health behavior: smoking (one cigarette at least a day for at least 6 months), alcohol intake (at least once a week for at least 6 months), balanced diet, weekly amount of exercise (min), years of exercise (year), and annual physical examination (at least for 3 years); (4) economic status: retirement benefits; and (5) mental health: depression. The specific assignments are shown in Appendix B.
The assessment of a balanced diet was subjective, and we explained to each participant that a diet high in oil and salt or imbalanced in meat and vegetables was considered unbalanced. According to relevant definitions, exercise was considered a heart rate higher than 50% * (220–age). However, it was not always possible to completely follow this point. We generally adopted conventional practices and believed that brisk walking or higher-intensity activities were qualified as exercises (19, 20). Finally, we used the Geriatric Depression Scale (GDS) to assess mental health and considered scores above 9 points to indicate the presence of depression (18). The assessment of control variables was based on ID information or self-reports.
The counting data were expressed as the number of cases and percentage (n, %), and the comparison between groups was conducted using a chi-square test if applicable. After passing the tests for normality and homogeneity of variance, the measurement data were expressed as mean (SD), and a t-test was performed between the groups. The Mann–Whitney U-test was used when the data were skewed and the variance was homogeneous. The values were expressed as median (interquartile range). PSM can eliminate the endogeneity and confounding factors of control variables to improve the accuracy of the results. A probit regression model was used to estimate the propensity scores for CCD vs. no CCD and SCD vs. CCD participants. After matching, univariate and multivariate logistic regression analyses were performed to test factors influencing BADL. The second PSM was performed with the same setting between the CCD and SCD groups to test the influence of CCD on BADL compared to SCD. The formula for prevalence was the number of individuals with the disease (CCD or SCD) divided by the total number of individuals in the group. SPSS 21.0 was used for statistical analysis. Differences were considered statistically significant if P-values were < 0.05.
A total of 47,720 participants were enrolled in the study (13.65% CCD, 86.35% no CCD, and 35.87% SCD). The characteristics of the participants are shown in Table 1.
A total of 3,459 (7.25%) participants expressed BADL disabilities. The prevalence of BADL disability in the older adults with CCD (13.07%) was significantly higher (P < 0.05) than that in their counterparts without CCD (6.33%). Of the 23,632 elderlies with chronic diseases, 2,116 cases (8.95%) expressed BADL disability. The older adults with CCD (13.07%) showed a significantly higher (P < 0.05) prevalence of BADL disability than those with SCD (7.39%).
A total of 6,513 participants (13.64%) had CCD. Before PSM, the age, sex, cohabitation, BMI, educational level, ethnicity, social situation interaction, smoking, alcohol intake, balanced diet, weekly amount of exercise, years of exercise, annual physical examination, pension, and retirement benefits between participants with and without CCD showed significant differences (P < 0.05). After PSM matching, 6,513 pairs of cases with and without CCD were matched. There were no significant differences (P > 0.05) in the above variables between the two matched groups, as shown in Table 2 and Appendix C.
After PSM, among a total of 13,026 participants, 11,535 (88.55%) expressed BADL no disability and 1,491 (11.45%) BADL disability. Participants with CCD showed a significantly higher prevalence of BADL disability than those with no CCD (13.07% vs. 9.83%, 1.330 times, P < 0.001). There was a statistically significant difference in age, cohabitation, type of residence, educational level, ethnicity, daily care from offspring, social interaction, alcohol intake, balanced diet, weekly amount of exercise, years of exercise, annual physical examination, retirement benefits, and depression (P < 0.05), as shown in Tables 3.1, 3.2.
A multivariate logistic regression analysis was carried out with BADL as the dependent variable and variables showing statistical significance in the univariate analysis as the independent variables. The results showed that CCD was a risk factor for BADL in older adults (OR = 1.496, 95% CI: 1.393–1.750). Moreover, age (OR = 1.102, 95% CI: 1.021–1.316), educational level (OR = 2.253, 95% CI: 1.290–2.705), weekly amount of exercise (OR = 0.996, 95% CI: 0.989–0.998), years of exercise (OR = 0.836, 95% CI: 0.652–0.941), alcohol intake (OR = 2.242, 95% CI: 1.939–2.688), social interaction (OR = 0.136, 95% CI: 0.058–0.464), annual physical examination (OR = 0.480, 95% CI: 0.152–0.772), retirement benefits (OR = 0.319, 95% CI: 0.196–0.669) and depression (OR = 0.124, 95% CI: 0.049–0.726) were influencing factors of BADL in older adults (P < 0.05), as shown in Table 4.
A total of 23,632 participants with chronic diseases were further analyzed using PSM. Before PSM, there were significant differences in sex, educational level, balanced diet, smoking, alcohol intake, social interaction, daily care from offspring, annual physical examination, age, BMI, and weekly amount of exercise (P < 0.05). After PSM, there were 6,513 pairs of cases with CCD and SCD while no significant differences were observed in the above variables (P > 0.05), as shown in Table 5 and Appendix D. Furthermore, the prevalence of BADL disability in the older adults with CCD was significantly higher than that in the older adults with SCD (13.07% vs. 11.39%, 1.179 times, P < 0.05).
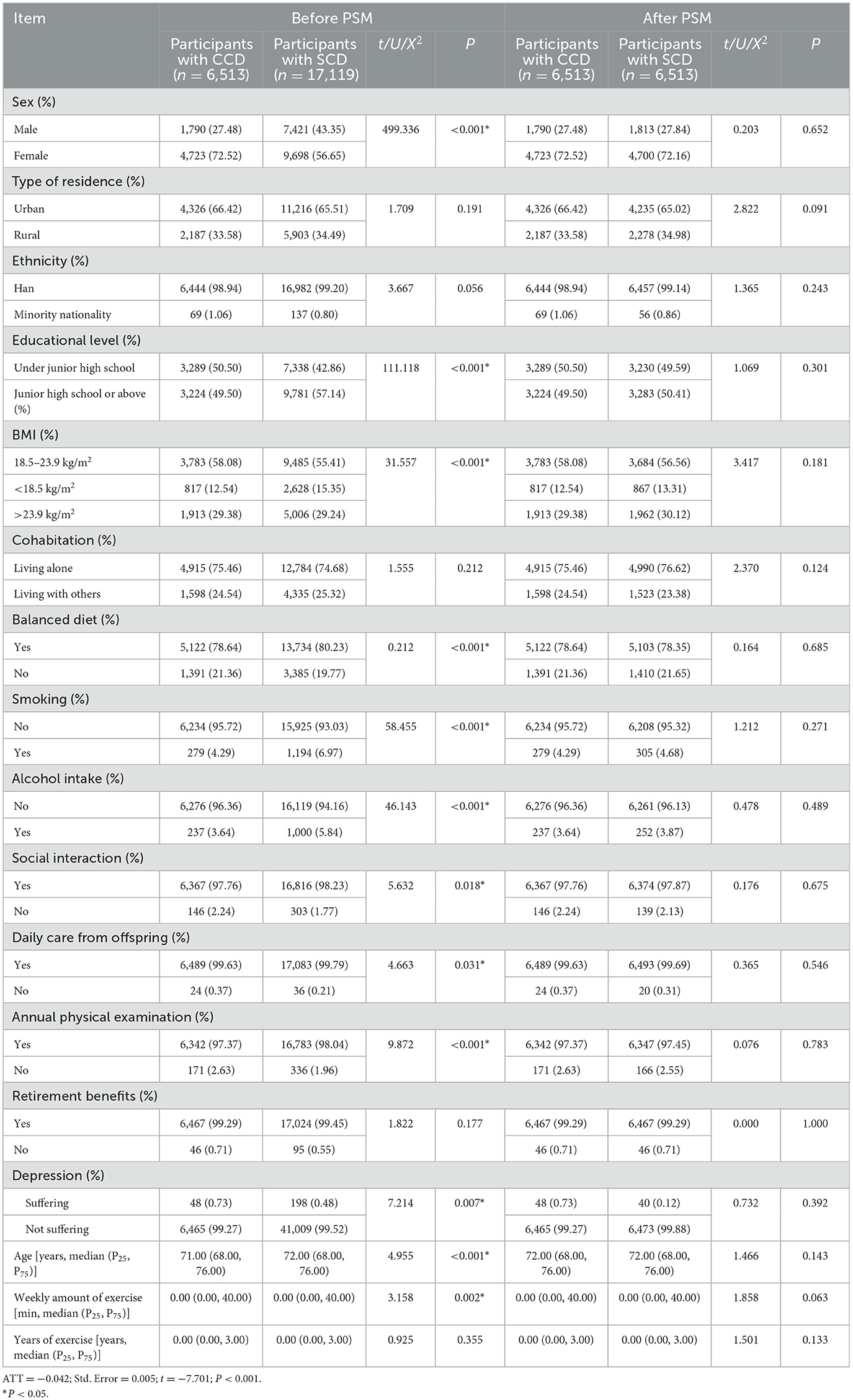
Table 5. Comparison of the general information of the group with CCD and with SCD before and after PSM.
The prevalence of BADL disability among the older adults ranged from 6% to 40% (14, 15, 17, 21, 22). These differences may be attributed to inconsistent evaluation criteria and economic inequality across regions (23). In the current study, the prevalence of BADL disability was 7.25%, which was similar to 8.78% reported by Cui et al. (21) and 6% by Zhang et al. (14) and slightly lower than 13% obtained by Connolly et al. (22) using data from the Irish longitudinal study on aging. This may be due to different definitions of older individuals. In this study, the participants were 60 years and older, whereas Connolly's study focused on individuals aged >65 years. According to a previous study (24), age has been identified as an influencing factor of BADL among older adults, which aligns with the present study. Tissues and organs, including the brain, tend to exhibit signs of aging as a person grows older. Age-related changes may manifest as a decline in the quantity and quality of information processing, leading to a decrease in physical strength, balance, memory, and other cognitive functions. These factors collectively contribute to BADL disability.
The older population commonly experiences deterioration in physical condition, an increased prevalence of chronic diseases, mobility difficulties, and a reduction in daily activities. This study showed that the prevalence of BADL disability in older individuals with CCD was 1.330 times higher than that in those without CCD (13.07% vs. 9.83%, P < 0.001). To further investigate the association between CCD and BADL, we conducted PSM analysis on SCD and CCD groups. The analysis revealed a significant difference in the prevalence of BADL disability between the two groups (13.07% vs. 11.39%, 1.179 times, P < 0.05). To analyze the possible reasons: first, compared to SCD, CCD has longer courses of disease and complex conditions that would cause long-term suffering (25), thus leading to BADL decline. Second, CCD can lead to multiple uses of drugs, for which compliance is poor. This can cause weakness and obstacles in the management of health (26). Third, the older adults with CCD might consume excessive β receptor blockers and sulfonamides from prescription, which can have side effects including decreased vitality, anorexia, and negative emotions (27). This further causes a decline in quality of life and mobility, leading to BADL disability. In addition, it is worth noting that the older population with CCD often exhibits a lack of health knowledge, which can result in inadequate attention to maintaining a healthy lifestyle. This can contribute to the exacerbation of chronic diseases, the development of complications, and ultimately the decline in BADL.
CCD significantly increases the risk of BADL disability, which is associated with reduced physical exercise and increased negative emotions. In turn, these factors can contribute to the poor prognosis of existing diseases (28, 29). The bidirectional correlation between CCD and BADL disability creates a vicious cycle in the older population. Additionally, it is important to recognize that different combinations of chronic diseases may share common risk factors. In summary, comprehensive measures should be taken to break the vicious circle, including strengthening the dynamic monitoring of chronic disease prevalence, improving community clinic services, and raising awareness among older adults (30). Considering these findings, it is imperative to prioritize the training of general practitioners working in grassroots healthcare institutions. Equipping them with the necessary knowledge and skills is crucial to ensure adequate care for older individuals with BADL disabilities. Furthermore, efforts should be made to disseminate relevant knowledge among the general population, particularly caregivers and family members, to enhance their understanding of the needs and challenges faced by older adults.
Older individuals with higher levels of education tend to have a stronger awareness of disease prevention and healthcare. Educational level is also related to social status and economic resources. These factors can contribute to better health outcomes and wellbeing (31). Furthermore, this study revealed a positive correlation between engagement in regular exercise and BADL levels. Exercise can help maintain muscle mass, improve cardiovascular function, and regulate mental wellbeing, all of which contribute to improving BADL (32). It is important to note that alcohol intake has detrimental effects on the digestive and neurological systems. Excessive alcohol intake can increase the burden on the liver and kidneys, potentially leading to BADL decline (33). High participation in social interaction can help avoid negative emotions and improve neurological function (34), which might help maintain BADL. The annual physical examination can help to discover changes in health status and to take preventive measures promptly, which is beneficial to BADL maintenance. Moreover, adequate retirement pension allows older individuals to allocate relatively sufficient resources to quality of life and medical services (35). Finally, this study found that depression was a risk factor for BADL, consistent with a previous study (36). A possible reason might be that depression could cause brain damage and cognitive impairment, which would further lead to BADL decline.
In practical terms, this study provides valuable insights into fostering collaboration among individuals, family members, society, and healthcare institutions. First, it is recommended that older individuals cultivate a healthy lifestyle by engaging in regular physical activity and minimizing alcohol intake. Second, family members should prioritize active communication with older adults, including regular check-ups, attention to their mental wellbeing, and the provision of social support. Third, from a societal standpoint, it is crucial to strengthen welfare benefits for older adults. Diverse activities that enrich the lives of older individuals should be implemented to prevent depression and alleviate feelings of isolation. Finally, healthcare institutions should publicize the significance of the prevention and treatment of chronic diseases through primary care, actively carry out disease screening, and facilitate early detection and intervention to safeguard BADL.
By collaboratively addressing these issues, strong support can be provided to enhance the BADL of the older population. This approach not only helps improve the quality of life of older adults but also alleviates the burden on families and society.
In our study, we observed a progressive relationship between no CCD, SCD, and CCD. PSM was used to eliminate the confounding factors and enhance the reliability of the results. However, this study had several weaknesses. The cross-sectional design used in this study makes it difficult to infer causality. Therefore, bidirectional causality cannot be ruled out. Considering this, future research endeavors are planned to adopt tracking designs and randomized interventions to further explicate the causal relationships between variables. Second, it is worth mentioning that all samples included in this study were drawn from Zhengzhou. Caution must be exercised when attempting to generalize the findings to other populations. To address this issue, future research endeavors should aim to expand the coverage of survey objects and collect data from a wider range of provinces.
The prevalence of BADL disability in the older adults with CCD is significantly higher than that of the older adults with SCD and no CCD. CCD, age, educational level, weekly amount of exercise, years of exercise, alcohol intake, social interaction, annual physical examination, retirement benefits, and depression are the factors associated with BADL.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of Zhengzhou University (Ethical number: ZZUIRB2022-07). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
HZ: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. CM: Writing – review & editing. RW: Visualization, Writing – review & editing. WZ: Software, Visualization, Writing – review & editing. WW: Visualization, Writing – review & editing. YL: Writing – review & editing. SW: Writing – review & editing. AL: Writing – review & editing. HJ: Writing – review & editing. GL: Writing – review & editing. JZ: Writing – review & editing. XC: Writing – review & editing. QT: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was funded by the National Key R&D Program for Active Health and Aging Science and Technology Response Key Special Project (Grant Number: 2020YFC2006100).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1292289/full#supplementary-material
1. Rudnicka E, Napierala P, Podfigurna A, Meczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. (2020) 139:6–11. doi: 10.1016/j.maturitas.2020.05.018
2. Jiang QB, Feng QS. Aging and health in China. Front Public Health. (2022) 10:998769. doi: 10.3389/fpubh.2022.998769
3. Wei YG, Wang ZC, Wang HW, Li Y, Jiang ZY. Predicting population age structures of China, India, and Vietnam by 2030 based on compositional data. PLoS ONE. (2019) 14:e0212772. doi: 10.1371/journal.pone.0212772
4. Ng R, Sutradhar R, Yao Z, Wodchis WP, Rosella LC. Smoking, drinking, diet and physical activity - modifiable lifestyle risk factors and their associations with age to first chronic disease. Int J Epidemiol. (2020) 49:113–30. doi: 10.1093/ije/dyz078
5. Mobula LM, Fisher ML, Lau N, Estelle A, Wood T, Plyler W. Prevalence of hypertension among patients attending mobile medical clinics in the Philippines after Typhoon Haiyan. PLoS Curr. (2016) 8. doi: 10.1371/currents.dis.5aaeb105e840c72370e8e688835882ce
6. Raghupathi W, Raghupathi V. An empirical study of chronic diseases in the united states: a visual analytics approach to public health. Int J Env Res Public Health. (2018) 15:431. doi: 10.3390/ijerph15030431
7. Krutilová VK, Bahnsen L, De Graeve D. The out-of-pocket burden of chronic diseases: the cases of Belgian, Czech and German older adults. BMC Health Serv Res. (2021) 21:239. doi: 10.1186/s12913-021-06259-w
8. Zhang M, Wang LH, Wu J, Huang ZJ, Zhao ZP, Zhang X, et al. Data resource profile: china chronic disease and risk factor surveillance (CCDRFS). Int J Epidemiol. (2022) 51:E1–8. doi: 10.1093/ije/dyab255
10. Shang XW, Peng W, Hill E, Szoeke C, He MG, Zhang L. Incidence, progression, and patterns of multimorbidity in community-dwelling middle-aged men and women. Front Public Health. (2020) 8:404. doi: 10.3389/fpubh.2020.00404
11. Kshatri JS, Palo SK, Bhoi T, Barik SR, Pati S. Prevalence and patterns of multimorbidity among rural elderly: findings of the AHSETS Study. Front Public Health. (2020) 8:582663. doi: 10.3389/fpubh.2020.582663
12. Huaquía-Díaz AM, Chalán-Dávila TS, Carrillo-Larco RM, Bernabe-Ortiz A. Multimorbidity in Latin America and the Caribbean: a systematic review and meta-analysis. BMJ Open. (2021) 11:e050409. doi: 10.1136/bmjopen-2021-050409
13. Prados-Torres A, Poblador-Plou B, Gimeno-Miguel A, Calderón-Larrañaga A, Poncel-Falcó A, Gimeno-Feliú LA, et al. Cohort profile: the epidemiology of chronic diseases and multimorbidity. The EpiChron Cohort Study. Int J Epidemiol. (2018) 47:382–4. doi: 10.1093/ije/dyx259
14. Zhang YC, Xiong Y, Yu QH, Shen SS, Chen L, Lei X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
15. Wang R, Xiao XY, Tao YL, Luo WX, Zhou T, Wu YN, et al. Health empowerment and health-related quality of life in older individuals with disabilities and their spouse carers: a cross-sectional study. Res Nurs Health. (2023) 46:616–26. doi: 10.1002/nur.22345
16. Leung S, Chan C, Shah S. Development of a Chinese version of the Modified Barthel Index - validity and reliability. Clin Rehabil. (2007) 21:912–22. doi: 10.1177/0269215507077286
17. Sagari A, Tabira T, Maruta M, Miyata H, Han G, Kawagoe M. Causes of changes in basic activities of daily living in older adults with long-term care needs. Australas J Ageing. (2021) 40:E54–61. doi: 10.1111/ajag.12848
18. Wang XR, Zhang D. A study on the impact of comorbidities of chronic diseases on anxiety symptoms in elderly people in China: based on propensity score matching. Chin Gen Pract. (2023) 26:3622–7. doi: 10.12114/j.issn.1007-9572.2023.0140
19. Willadsen TG, Bebe A, Koster-Rasmussen R, Jarbol DE, Guassora AD, Waldorff FB, et al. The role of diseases, risk factors and symptoms in the definition of multimorbidity - a systematic review. Scand J Prim Health. (2016) 34:112–21. doi: 10.3109/02813432.2016.1153242
20. Cao M, Li Y, Tian Q. Comorbidity of chronic diseases and its impact on activities of daily living among the elderly in Henan province. China J Public Health. (2022) 38:395–8. doi: 10.11847/zgggws1132913
21. Cui L, Ding D, Wang M, He F, Ma J, Chen J. The relationship between different types of daily living abilities and depression among older adults. Chin J Dis Control Prev. (2023) 27:717–21. doi: 10.16462/j.cnki.zhjbkz.2023.06.017
22. Connolly D, Garvey J, McKee G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil Rehabil. (2017) 39:809–16. doi: 10.3109/09638288.2016.1161848
23. Qian JH, Ren XH. Association between comorbid conditions and BADL/IADL disability in hypertension patients over age 45 Based on the China health and retirement longitudinal study (CHARLS). Medicine. (2016) 95:e4536. doi: 10.1097/MD.0000000000004536
24. Sieber S, Roquet A, Lampraki C, Jopp DS. Multimorbidity and quality of life: the mediating role of ADL, IADL, loneliness, and depressive symptoms. Innov Aging. (2023) 7:igad047. doi: 10.1093/geroni/igad047
25. Kojima T, Mizokami F, Akishita M. Geriatric management of older patients with multimorbidity. Geriatr Gerontol Int. (2020) 20:1105–11. doi: 10.1111/ggi.14065
26. Birk JL, Kronish IM, Moise N, Falzon L, Yoon S, Davidson KW. Depression and multimorbidity: considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. (2019) 38:802–11. doi: 10.1037/hea0000737
27. Giannakou K, Kyprianidou M, Chrysostomou S, Christophi CA. The associations of lifestyle factors and behaviors with multimorbidity. Front Public Health. (2023) 11:1227381. doi: 10.3389/fpubh.2023.1227381
28. Soares W, Lopes AD, Nogueira E, Candido V, de Moraes SA, Perracini MR. Physical activity level and risk of falling in community-dwelling older adults: systematic review and meta-analysis. J Aging Phys Activ. (2019) 27:34–43. doi: 10.1123/japa.2017-0413
29. Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995-2015. Arch Public Health. (2020) 78:20. doi: 10.1186/s13690-020-00402-5
30. Cunningham C, O' Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: a systematic review of reviews and meta-analyses. Scand J Med Sci Spor. (2020) 30:816–27. doi: 10.1111/sms.13616
31. Alvarez-Gálvez J, Ortega-Martín E, Carretero-Bravo J, Pérez-Muñoz C, Suárez-Lledó V, Ramos-Fiol B. Social determinants of multimorbidity patterns: a systematic review. Front Public Health. (2023) 11:1081518. doi: 10.3389/fpubh.2023.1081518
32. Tang SL, Liu MX, Yang TL, Ye CY, Gong Y, Yao L, et al. Association between falls in elderly and the number of chronic diseases and health-related behaviors based on CHARLS 2018: health status as a mediating variable. BMC Geriatr. (2022) 22:374. doi: 10.1186/s12877-022-03055-x
33. Milne-Ives M, Lam C, De Cock C, Van Velthoven MH, Meinert E. Mobile apps for health behavior change in physical activity, diet, drug and alcohol use, and mental health: systematic review. JMIR Mhealth Uhealth. (2020) 8:e17046. doi: 10.2196/17046
34. Wang RY, Chen HS, Liu Y, Lu Y, Yao Y. Neighborhood social reciprocity and mental health among older adults in China: the mediating effects of physical activity, social interaction, and volunteering. BMC Public Health. (2019) 19:1036. doi: 10.1186/s12889-019-7385-x
35. Weida EB, Phojanakong P, Patel F, Chilton M. Financial health as a measurable social determinant of health. PLoS ONE. (2020) 15:e0233359. doi: 10.1371/journal.pone.0233359
Keywords: basic activities of daily living, comorbidities of chronic disease, chronic disease, older adults, quality of life
Citation: Zeng H, Miao C, Wang R, Zhao W, Wang W, Liu Y, Wei S, Liu A, Jia H, Li G, Zhou J, Chen X and Tian Q (2024) Influence of comorbidity of chronic diseases on basic activities of daily living among older adults in China: a propensity score-matched study. Front. Public Health 12:1292289. doi: 10.3389/fpubh.2024.1292289
Received: 11 September 2023; Accepted: 14 March 2024;
Published: 04 April 2024.
Edited by:
Soham Al Snih, University of Texas Medical Branch at Galveston, United StatesReviewed by:
Ivana Simic Vukomanovic, University of Kragujevac, SerbiaCopyright © 2024 Zeng, Miao, Wang, Zhao, Wang, Liu, Wei, Liu, Jia, Li, Zhou, Chen and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingfeng Tian, enp1dHFmQDEyNi5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.