- 1Department of Nursing, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
- 2Department of Midwifery, College of Medicine and Health Science, Wolaita Sodo University, Sodo, Ethiopia
- 3Department of Emergency Nursing, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
- 4Department of Pediatrics and Child Health Nursing, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
- 5School of Nursing, College of Health Science, Woldia University, Woldia, Ethiopia
Introduction: Prior primary studies have examined the prevalence and factors associated with glycaemic control among patients with type 2 diabetes mellitus, but studies with evidence-based synthesis of the primary data remained unknown. Hence, we aimed to determine the prevalence of poor glycemic control and identify determinants of poor glycemic control in patients with type 2 diabetes in Ethiopia.
Methods: We performed searches in the online databases of PubMed, Google Scholar, Scopus, Science Direct, and the Cochrane Library. Microsoft Excel was used to extract data, and STATA statistical software (v. 16) was used for analysis. Publication bias was explored by forest plots, Begg’s rank test, and Egger’s regression test. To check for heterogeneity, I2 was computed. Subgroup analysis was conducted based on region and publication year. In addition, the pooled odds ratio for associated factors was calculated.
Results: Out of 1,045 studies assessed, 23 studies were included fulfilling our inclusion criteria. In all, 6,643 individuals were enrolled in the study. It was estimated that 61.11% of type 2 diabetes patients had poor glycemic control (95% CI, 57.14–65.19). The subgroup analysis by study region and publication year revealed that the highest prevalence was observed in the Addis Ababa region (68.57%) and studies published before 2019 (61.76%), respectively. Poor glycemic control was associated with older age > 50 years (AOR = 2.12; 95% CI: 1.27–2.97), not attending formal education (AOR = 3.60; 95% CI: 2.75, 4.46), having diabetes for longer duration (10 years; AOR = 2.57; 95% CI: 1.65–3.49), having comorbidity (AOR = 2.43; 95% CI: 2.05–2.80), and low adherence to diabetes management (AOR = 3.67; 95% CI: 2.41–4.92).
Conclusion: Our findings indicate a high prevalence of poor glycemic control among people with type 2 diabetes in Ethiopia. Being older, not attending formal education, having a longer duration of diabetes, having comorbidity, and having low adherence to diabetes management were all associated. Therefore, we recommend health organizations implement measures to monitor and control patients’ blood glucose levels. Patient education and training of healthcare professionals could serve as a short-term strategy to achieve adequate glycemic control.
Systematic review registration: PROSPERO, identifier CRD42022349792, https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022349792.
Background
Diabetes mellitus (DM) is a rapidly rising global health challenge with a huge burden of diseases (1). It is a common metabolic disorder caused by either insufficient insulin secretion from the pancreas, reduced insulin action, or both (2). The latest data show that in 2019, 463 million individuals are affected by diabetes worldwide. This number is projected to increase to 578 million patients by 2030 and further rise to 700 million by 2045 (3). The estimated number of adults living with diabetes in sub-Saharan Africa (SSA) in 2017 was 15.5 million. Reports found that approximately 69% of SSA adults living with diabetes remained undiagnosed (3, 4). Ethiopia has recorded 2.6 million diabetic patients, the highest number of diabetes cases in Africa (5). Therefore, effective management is the priority for these patients in Ethiopia.
Type 2 diabetes mellitus (T2DM) is characterized by the inability of the pancreas to secrete insulin and peripheral insulin resistance (2). T2D represents 90–95% of all diabetes cases. Despite increased global attention and healthcare efforts, its prevalence continues to increase (6). Nowadays, new methods of evaluating glycemic control are underway. Inadequate diabetes management and its complications can result in recurrent hospital admissions and premature death. Glycemic control plays a key role in the prognosis of diabetes and possible complications (7). A reasonable glycated hemoglobin (A1C) goal for glycemic control is 7%. However, less stringent (A1C of 8%) or more stringent (e.g., A1C of 6.5%) goals might be considered for some patients (2).
Despite the observed benefits of adequate glycemic control, evidence suggests that the majority of patients did not meet targets for reasonable HbA1C according to the recommendations of consensus treatment panels. According to combined regional estimates of North Africa and the Middle East, only approximately 37% of the patients with T2D had an HbA1C < 7.0% in 2021 (8). Furthermore, studies have also suggested that glycemic control in Ethiopia is suboptimal, which indicates most patients (65.5%) had poor glycemic control (9).
Previous meta-analyses of glycemic control in Ethiopia have provided a comprehensive report on all diabetes patients (9). However, a meta-analysis of factors of poor glycemic control in T2DM is still lacking. In Ethiopia, several individual studies have investigated the level of glycemic control and its associated factors among T2D patients. However, most of these studies are single-centered and have relatively small sample sizes. Thus, systematic review and meta-analysis are required, as they provide a comprehensive overview of glycemic control in T2D as a country-level burden. Estimating the national level of glycemic control and identifying associated factors is invaluable to inform strategy design and policy-making to mitigate the burden of T2D. Therefore, this systematic review and meta-analysis aimed to evaluate the level and factors of poor glycemic control among T2D patients in Ethiopia.
Methods
We prepared and presented this study according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Supplementary Table S1) (10) and registered on PROSPERO under a registration number of CRD42022349792.
Search strategy
We identified potentially eligible studies by systematically searching the databases of PubMed, Science Direct, Scopus, and Google Scholar. The keywords used during the search were: ((((((((((((((Glycemic control) OR (poor glycemic control)) OR (blood glucose)) OR (Hemoglobin A1C)) OR (HBA1C)) AND (Diabetes mellitus)) OR (Type 2)) OR (Type II diabetes)) OR (Type 2 diabetes)) AND (associated factors)) OR (determinants)) OR (predictors))) AND (Adult)) AND (Ethiopia). Search terms were based on PICO principles to retrieve relevant articles through the databases mentioned above. We have searched for articles from 1 May 2022 to 30 May 2022.
Outcome measurement
Patients with an FPG level of ≤130 mg/dL or an A1C level of ≤7% were considered to have good glycemic control. On the other hand, patients with an FPG level of >130 mg/dL or an A1C level of >7% were considered to have poor glycemic control (2).
Eligibility criteria
This meta-analysis includes studies that reported the level of glycemic control in adult T2D as study participants, published in English as full-length articles, both published and unpublished studies with full text available for search, and studies that took place in Ethiopia. Studies published between 1 January 2000 and 30 May 2022 were included. We excluded duplicated studies, conference papers or abstracts, articles without full texts, and studies with data that could not be obtained from the corresponding authors.
Quality appraisal
A set of standardized critical appraisal instruments from the Joanna Briggs Institute for observational studies was used to evaluate the quality of the included studies (11). The instrument assesses whether the original studies provided adequate information regarding population characteristics, exposures, confounders, outcomes, follow-up details (where applicable), and statistical analysis. The answers to each instrument item were labeled as yes, no, unclear, or not applicable. Any inconsistencies were resolved through discussion led by the third author (GAA). The critical appraisal tool is shown in Supplementary Table S2.
Data extraction
Using a standard data extraction form, two investigators (KDT and NAG) independently extracted the following information from the included studies. This information includes the name of the first author, year of publication, study region, study setting, study design, the prevalence of poor glycemic control, sample size, and quality of each study. Any disagreements that arose during data extraction were resolved through a discussion led by the third author (LTY). Finally, the argument was solved and an agreement reached. The data automation tool was not used due to this study’s absence of the paper form (manual data).
Data analysis
After extracting all relevant findings in a Microsoft Excel spreadsheet, the data were exported into STATA software version 16 for analysis. Random effect models (DerSimonian and Laird methods) were used to pool individual studies. The possibility of publication bias was explored by the visual inspection of the funnel plots and more objectively by Begg’s and the Egger test (12) and a value of p less than 0.05 indicates it is statistically significant (13). The presence of between-study heterogeneity was checked by using the Cochrane Q statistic. Between studies, heterogeneity was investigated using I2, in which a value of 25, 50, and 75% represented low, medium, and high heterogeneity, respectively (14). To identify the subgroup differences and potential sources of the observed heterogeneity, we carried out subgroup analysis based on the study region and publication year (before 2019 and 2019 onwards). To evaluate the robustness of the overall estimates, we performed sensitivity analyses, leaving out each study consecutively and observing any notable changes in the pooled result. All statistical analyses were conducted in STATA 14.0 (Stata Corp., College Station, TX, United States).
Results
Study selection
We identified 1,045 records through the electronic databases of PubMed, Scopus, Google Scholar, ScienceDirect, and the Cochrane library. Removing duplicates resulted in 523 articles. Then, full title and abstract screening excluded 362 studies, and 523 studies remained. Therefore, 161 full-text studies were assessed for eligibility, which further excluded 138 studies due to the lack of reported outcomes of interest and studies other than the study area. Finally, 23 articles were included in the systematic review and meta-analysis (Figure 1).

Figure 1. Flow chart illustrating the process of search and selection of studies included in the present systematic review and meta-analysis.
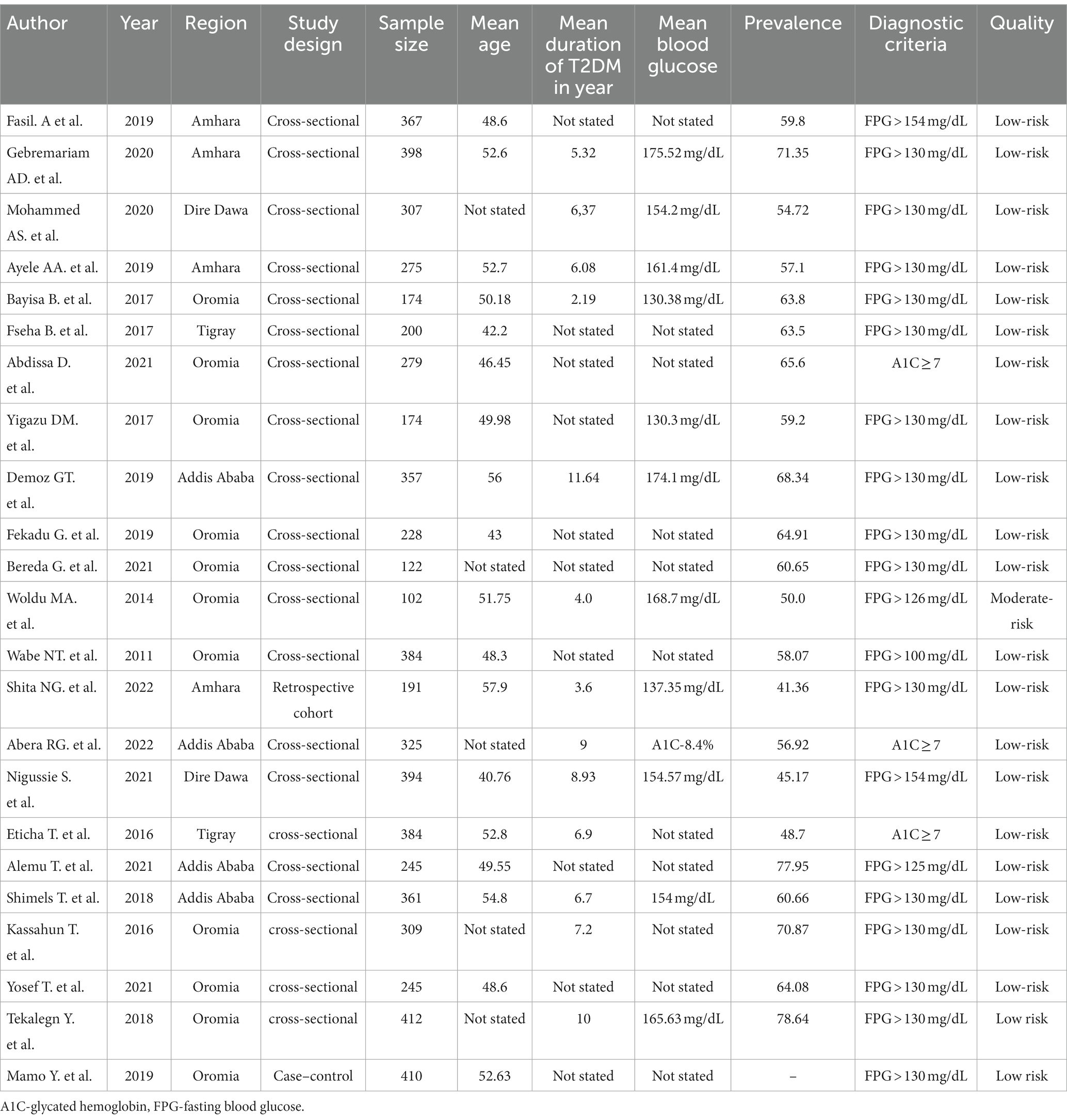
Characteristics of included studies
A total of 23 studies, including 6,643 participants, were identified. The included studies were published between 2011 and 2022. All studies were institutional observational studies, of which 21 were cross-sectional study designs, 1 was a retrospective cohort, and 1 was a case–control. Ten studies were conducted in the Oromia region (7, 15–23), five in Addis Ababa (24–28), four in Amhara (29–32), two in Tigray (33, 34), and two in Dire Dawa (35, 36). The sample sizes ranged from 102 to 412. The prevalence of poor glycemic control ranges from 41.36 to 78.64. Selected articles were deemed to have satisfactory methodological quality as per the critical appraisal process (Table 1).
Glycemic control
Glycemic control was evaluated commonly based on fasting blood glucose (FBG), as reported in 20 studies (7, 16–23, 25–32, 34–36), whereas only 3 studies assessed glycemic control using HbA1C (15, 24, 33). Fifteen studies considered poor glycemic control above 130 mg/dL (7, 16–19, 22, 23, 26–29, 31, 32, 34, 35), three studies considered it at 126 mg/dL (20, 21, 25), and two studies defined poor glycemic control as higher than 154 mg/dL (30, 36). As of the level of A1C, three studies considered poor glycemic control at A1C ≥ 7% (15, 24, 33). A total of 11 studies reported participants’ mean duration of T2D starting from diagnosis, and based on these studies, the mean duration of T2D was 7.42 years. Similarly, the mean FBG level was reported in 11 studies, and the overall mean FBG was 155.08 mg/dL.
Meta-analysis
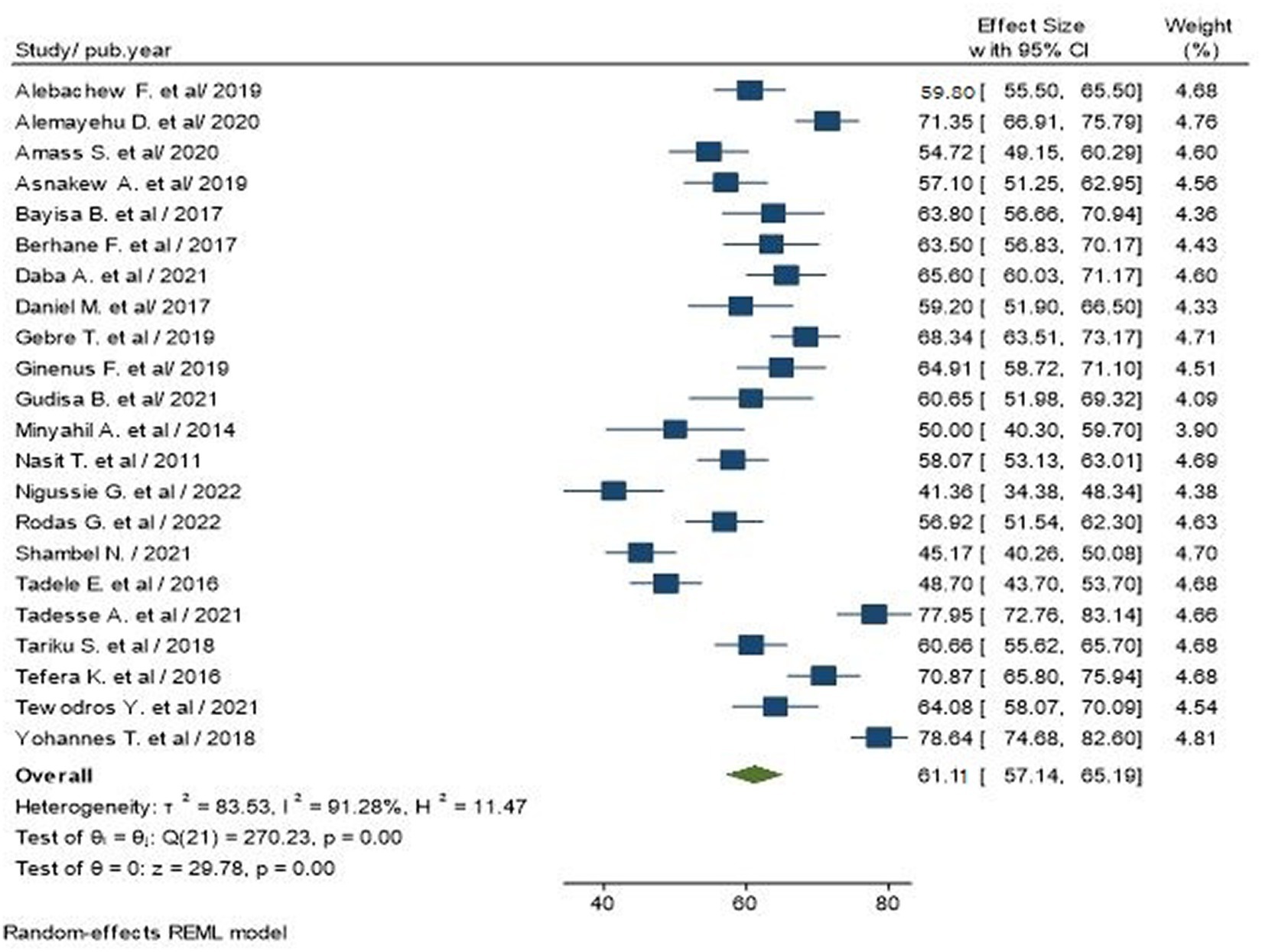
Prevalence of poor glycemic control among T2D in Ethiopia
Out of the 23 studies included in our review, 1 study did not report the prevalence estimates. Thus, 22 studies, including 6,233 participants, reported the prevalence of poor glycemic control, ranging from 41.36 to 78.64%. The pooled prevalence of poor glycemic control among T2D in Ethiopia was 61.11% (95% CI: 57.14–65.19; I2 = 91.28%, p < 0.00; Figure 2).
Subgroup analysis
A subgroup analysis was conducted to observe variations across potential covariates and explore the sources of heterogeneity. As a result, subgroup analysis was conducted in terms of study region and publication year. In terms of region, the highest prevalence of poor glycemic control was observed in Addis Ababa (68.57%), and subgroup analysis by publication year revealed a higher pooled prevalence of 61.76% across studies published before 2019 (Table 2).
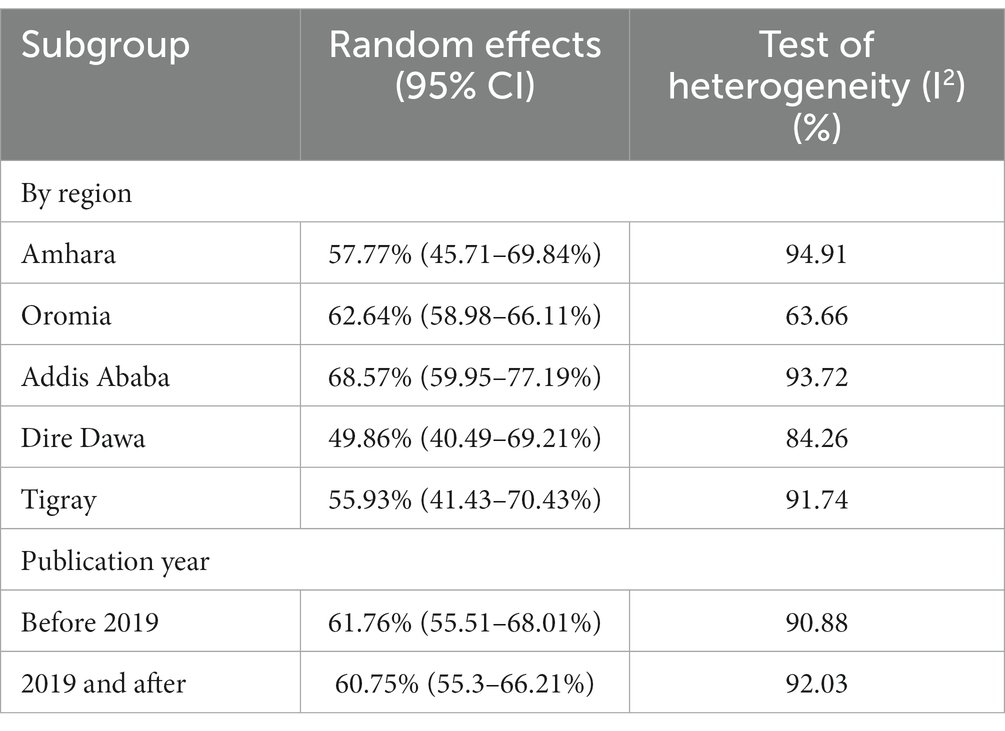
Table 2. Subgroup analysis of studies included in the meta-analysis on poor glycemic control and associated factors among T2D in Ethiopia.
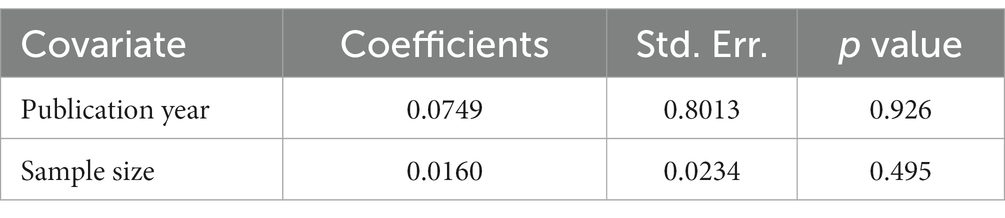
Meta regression
We have performed meta-regression to further explore sources of heterogeneity among studies. A meta-regression using publication year and sample size as covariates indicated non-significant results. The results of meta-regression are presented in Table 3.
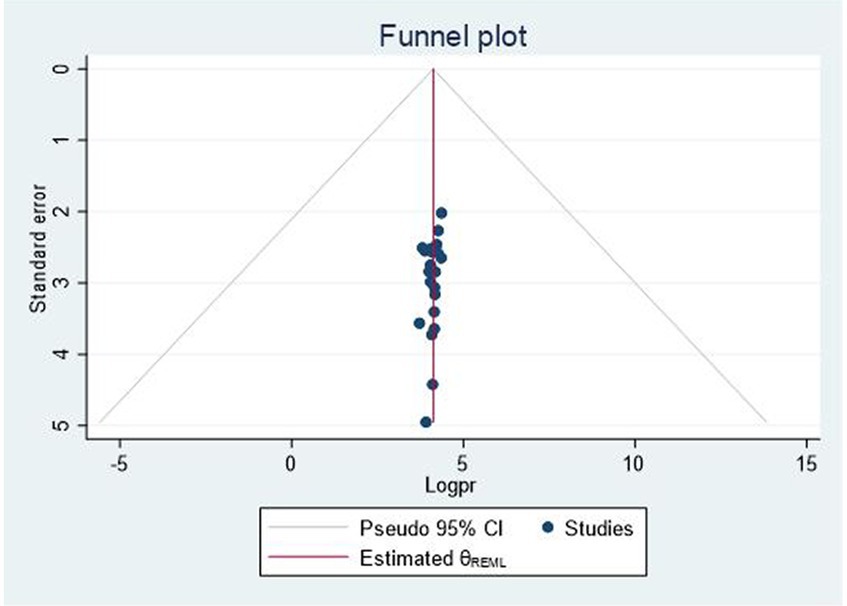
Publication bias
Visual inspection of the funnel plot indicated no evidence of publication bias. Further investigation of Egger’s (p = 0.0783) and Begg’s regression tests (p = 1.7637) did not confirm the presence of publication bias (Figure 3).
Sensitivity analysis for the studies included
To examine the effect of a single study on the overall prevalence estimates, sensitivity analysis was performed using a random effect model. The result revealed that the overall estimate was not affected when studies were alternatively omitted from the model. The pooled estimated prevalence of poor glycemic control is estimated to range from 60.29 (56.35–64.22) to 62.07 (57.94–66.19) after the omission of a single study (Figure 4).
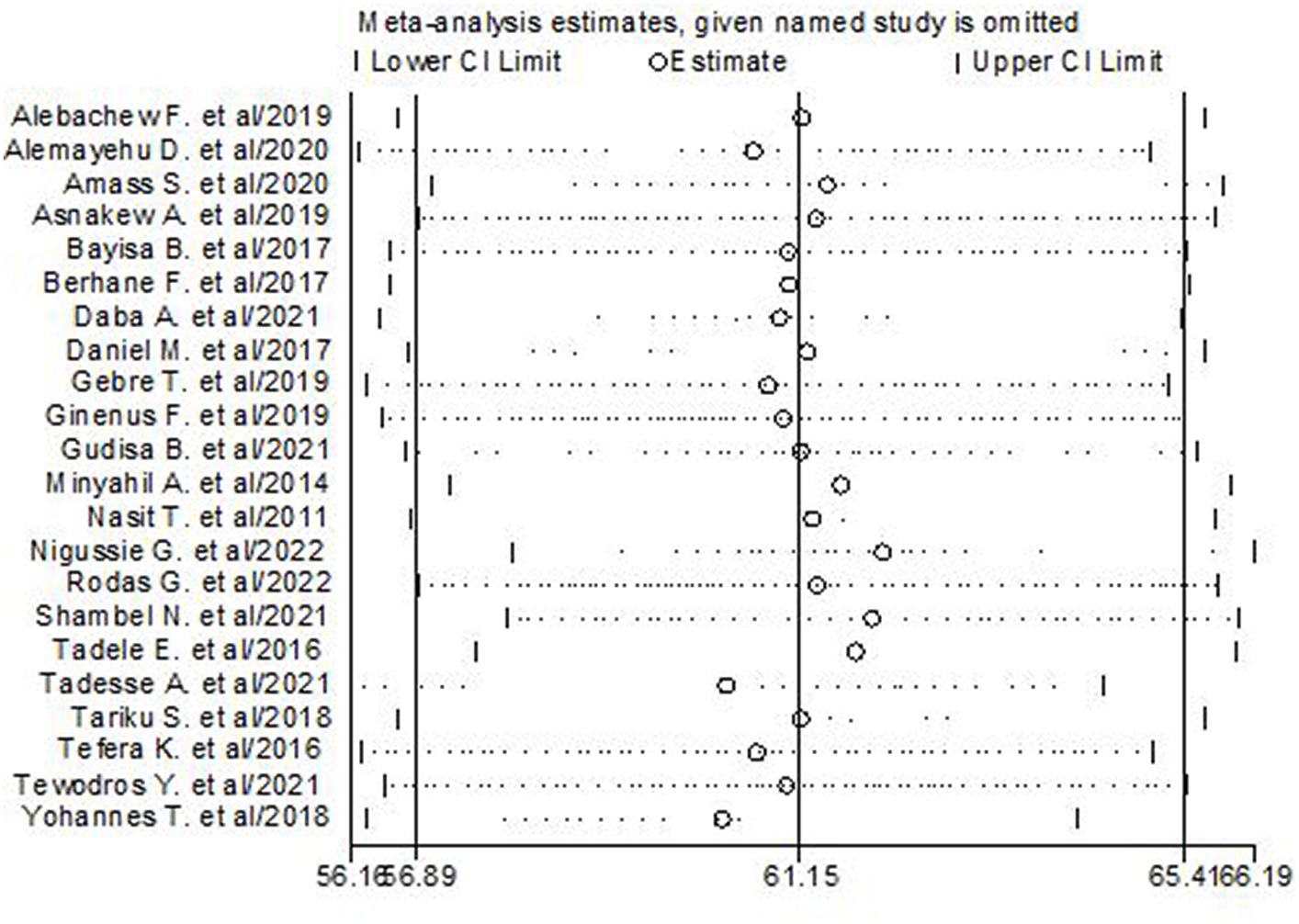
Figure 4. Results of the sensitivity of the 22 studies in the meta-analysis of glycemic control in T2DM.
Factors associated with poor glycemic control among T2D
In this systematic review and meta-analysis, factors that are associated with poor glycemic control in T2D patients have been identified. Subsequently, older people >50 years, not attending formal education, longer duration of diabetes (10 years), having comorbidity, and low adherence to diabetes management are the factors linked with poor glycemic control among T2DM patients. However, the combined use of oral anti-diabetics and oral insulin was not a significant factor in poor glycemic control among T2D patients.
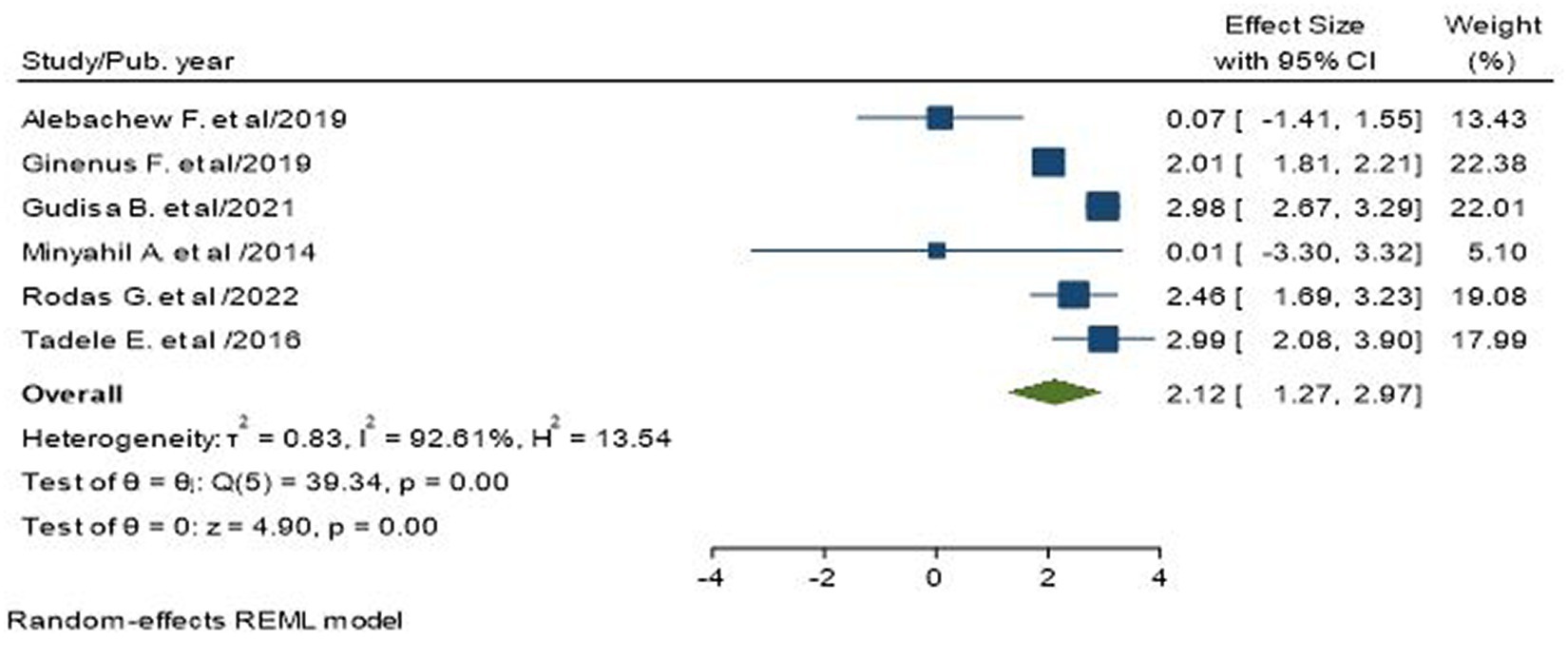
Association of older age with poor glycemic control
Six studies, including 1,528 participants, provided data for this analysis (17, 18, 21, 24, 30, 33). Accordingly, older age (over 50 years) was found to be a factor associated with poor glycemic control. The pooled result indicated that older people >50 years were two times more likely to have poor glycemic control than younger people (AOR = 2.12; 95% CI: 1.27, 2.97; I2 = 92.61%, p < 0.001; Figure 5).
Association of educational status with poor glycemic control
Educational status, more specifically, not attending formal education, was reported as a significant factor influencing glycemic control among T2D patients in four primary studies (17–19, 23, 31). A total of 1,302 subjects were included to analyze the association between not attending formal education and poor glycemic control. The odds of poor glycemic control among uneducated type 2 diabetics were 3.6 times higher as compared to their educated counterparts (AOR = 3.60; 95% CI: 2.75, 4.46; I2 = 87.81%, p < 0.001; Figure 6).
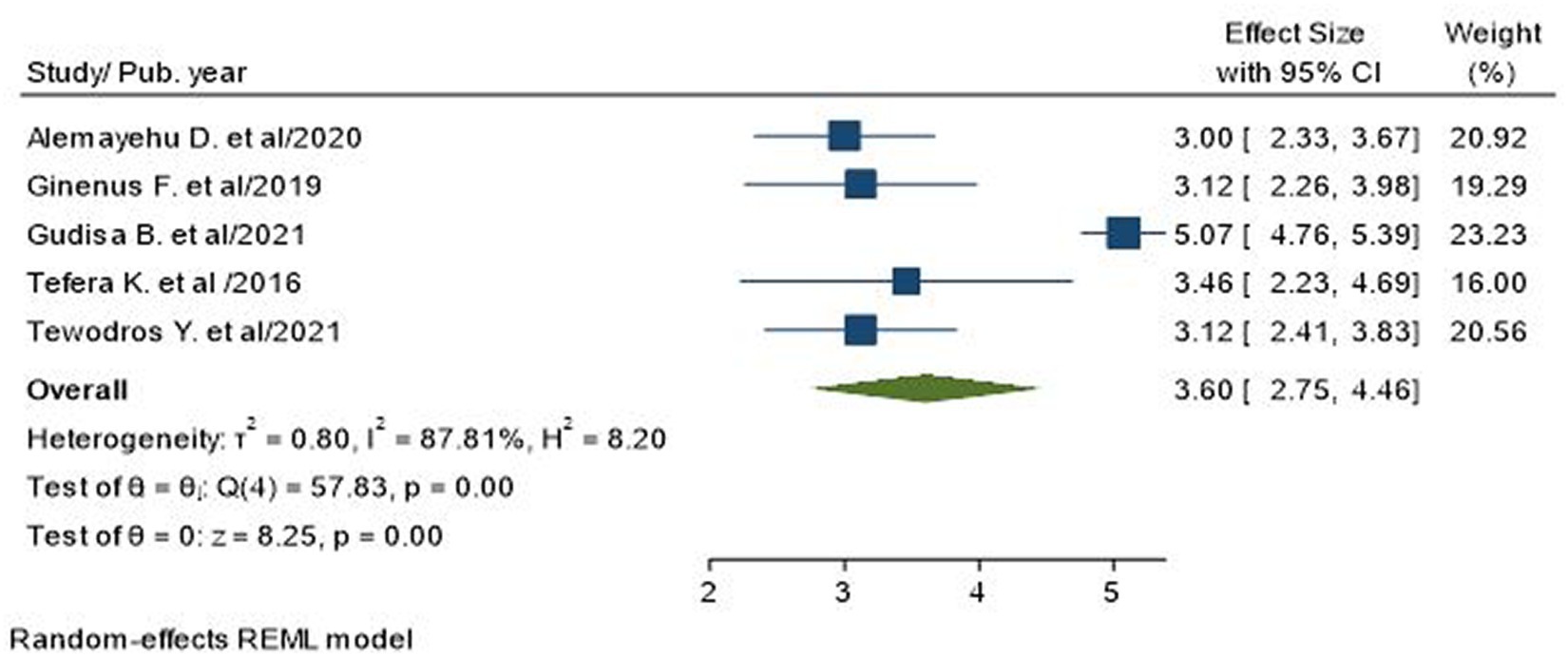
Figure 6. Association between educational status and poor glycemic control in type 2 diabetic patients.
Association of longer duration of diabetes with poor glycemic control
Six primary studies, involving a total of 1987 subjects, reported longer duration with diabetes (10 years) as a factor for poor glycemic control in T2D patients (7, 18, 24, 25, 28, 30). The pooled odds ratio showed that longer duration of T2D was 2.57 times more likely to have poor blood glucose control than their counterparts (AOR = 2.57; 95% CI: 1.65–3.49; I2 = 85.43%, p < 0.001; Figure 7).
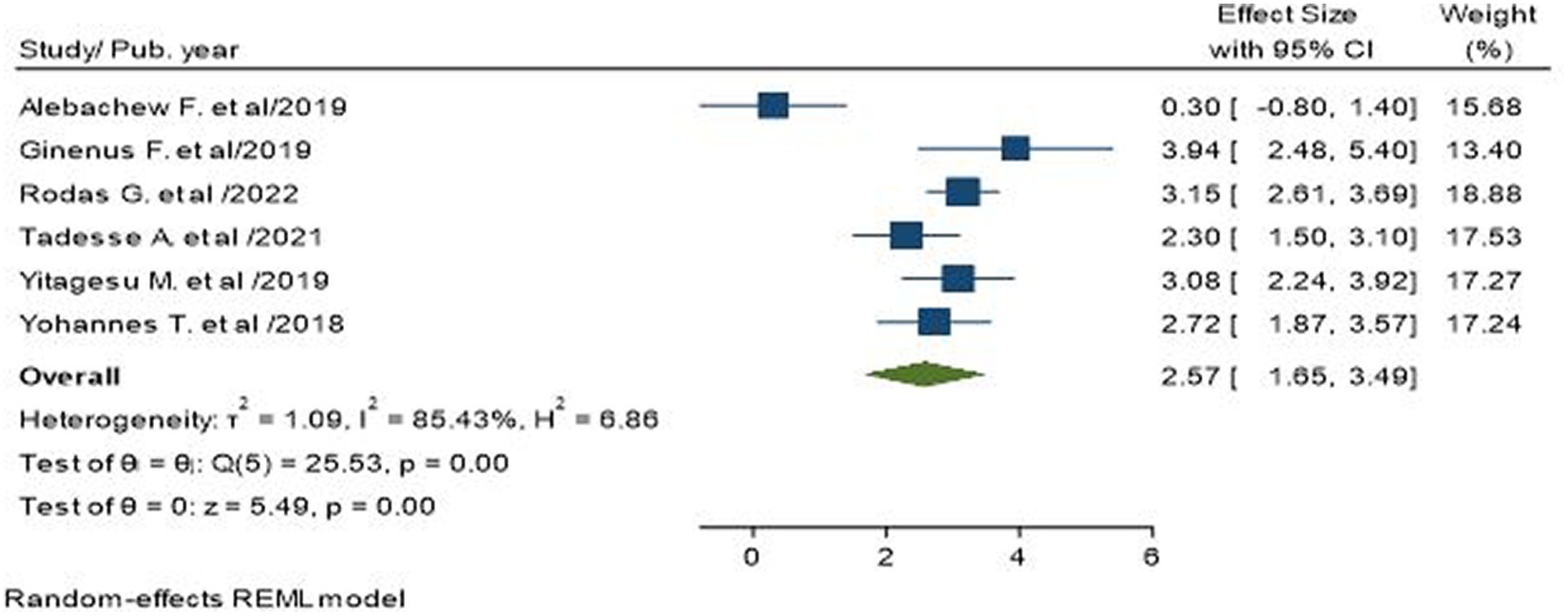
Figure 7. Association between longer duration of diabetes and poor glycemic control in type 2 diabetic patients.
Association of comorbidity with poor glycemic control
Three studies, involving a total of 916 subjects, reported longer duration with diabetes (10 years) as a factor for poor glycemic control in T2DM patients (7, 17, 33). The pooled odds ratio showed that T2D with comorbidity was 2.43 times more likely to have poor blood glucose control than T2D without comorbidity (AOR = 2.43; 95% CI: 2.05–2.80; I2 = 0.00%, p < 0.001; Figure 8).
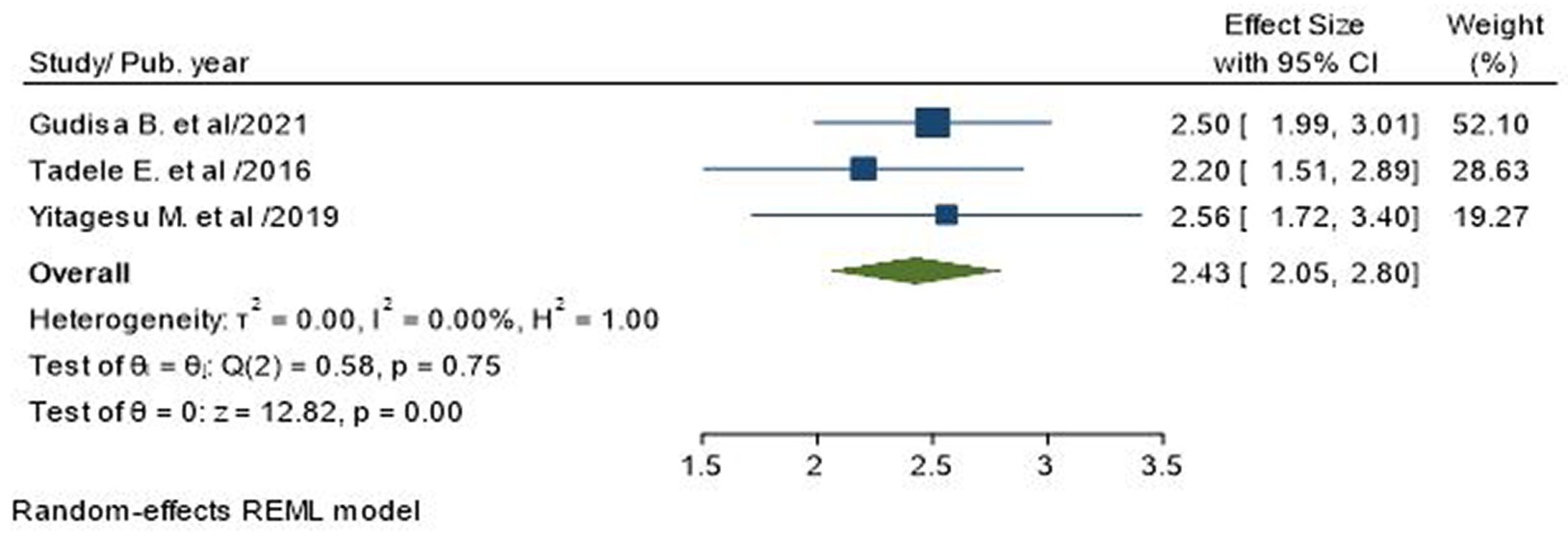
Figure 8. Association of combined use of oral anti-diabetics and insulin with poor glycemic control in type 2 diabetic patients.
Association of low self-care adherence with poor glycemic control
Five studies, including 1,358 study subjects, reported low self-care adherence as a factor in poor glycemic control in T2D patients (17, 19, 24–26). The pooled odds ratio showed that T2D with low self-care adherence had 3.67 times more odds to control blood glucose than T2D with good self-care adherence (AOR = 3.67; 95% CI: 2.41–4.92; I2 = 93.53%, p < 0.001; Figure 9).
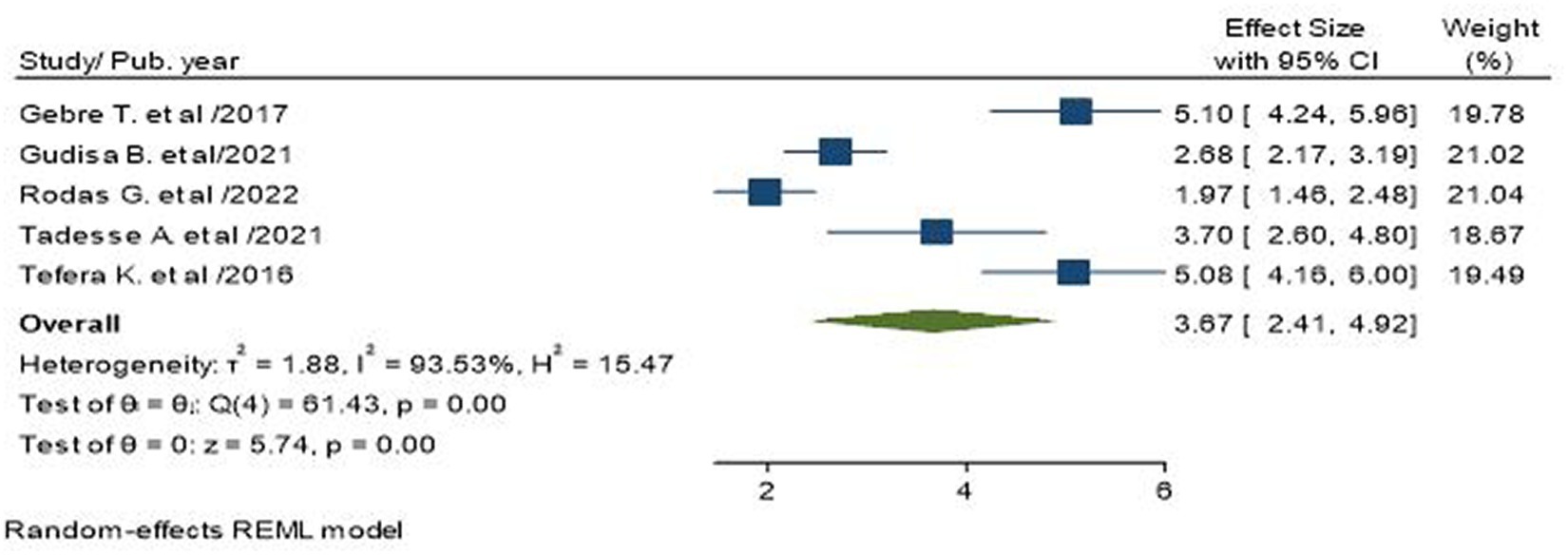
Figure 9. Association between low self-care adherence and poor glycemic control in type 2 diabetic patients.
Association of taking the combination of oral anti-diabetes and insulin with poor glycemic control
Four studies with 1,474 participants reported the association between receiving a combination of oral anti-diabetic drugs and insulin and poor glycemic control in T2D patients (7, 19, 27, 36). The pooled odds ratio showed that there are no significant associations between receiving both oral anti-diabetics and insulin and poor glycemic control (AOR = 4.04; 95% CI: 0.26–7.83; I2 = 98.36%, p = 0.06; Figure 10).
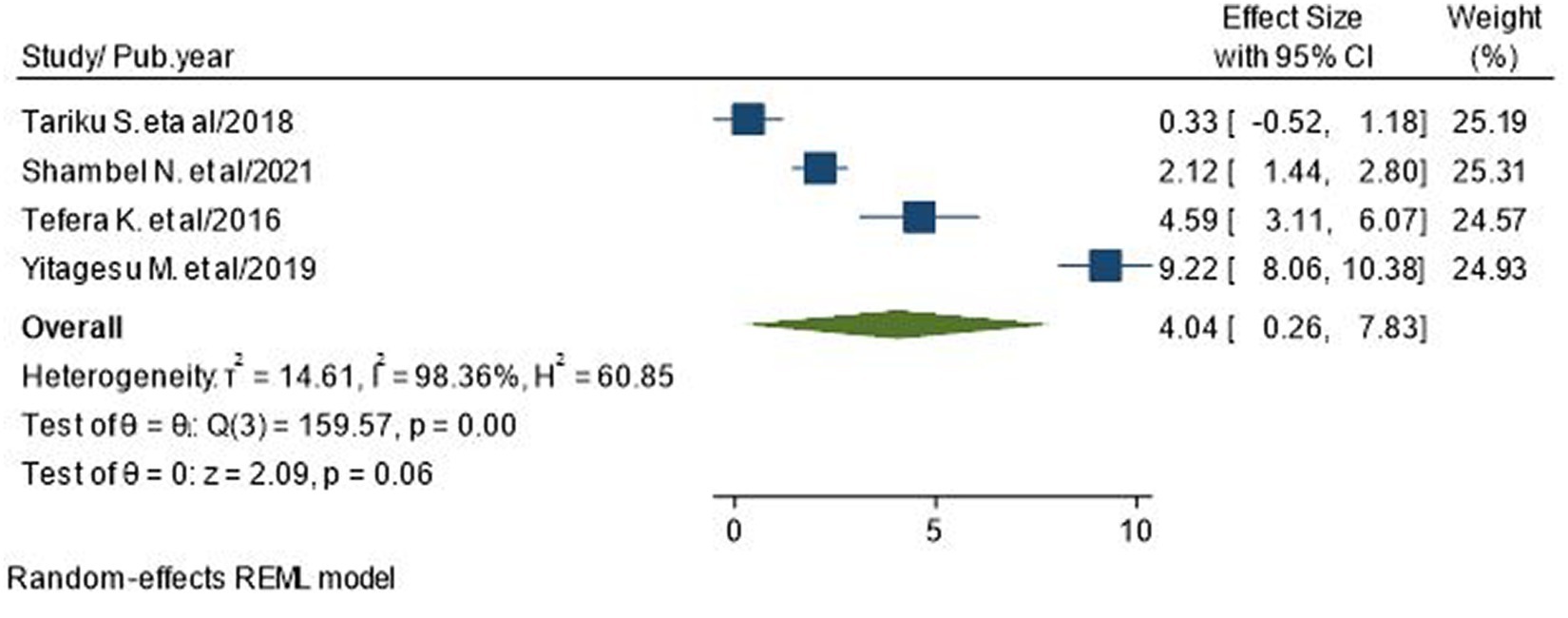
Figure 10. Association between low self-care adherence and poor glycemic control in type 2 diabetic patients.
Discussion
In this study, we have conducted a comprehensive review to evaluate the pooled estimates and factors of poor glycemic control among T2D adults aged 18 years and older in Ethiopia. This systematic review and meta-analysis is, as far as we are aware the first meta-analysis on the prevalence and associated factors of poor glycemic control among people with T2D in Ethiopia. In this meta-analysis, 23 articles with a total of 6,643 study subjects were included. The overall prevalence of poor glycemic control among T2D in this study was 61.11% (95% CI: 57.14–65.19).
In accordance with our findings, a recent meta-analysis in the Middle East and North Africa reported 63% poor glycemic control in T2D (8). Similarly, a large cross-sectional study from Morocco revealed that 66.3% of T2D patients had poor glycemic control (37). A previous review on glycemic control for overall diabetes in Ethiopia also confirmed that 65.6% of patients had poor glycemic control based on fasting blood glucose measurement (9). On the contrary, our result is higher than a study reported in China (44%). The lower poor glycemic control prevalence observed in China might be due to higher literacy rates in industrialized nations, which likely leads to a better understanding of the disease (38). Having adequate knowledge about diabetes is essential for improving blood glucose and preventing acute and chronic complications.
The observed high heterogeneity of the studies included in this review could be largely attributed to a broad range of poor glycemic control prevalence across the studies. Thus, we further conducted subgroup analyses stratified by study region and publication year. In terms of region, Addis Ababa had the highest prevalence of poor glycemic control (68.57%). Addis Ababa is the capital city of the country, where economic growth and development are relatively higher compared to other areas of the country. Individuals residing in urban and industrialized areas often become physically inactive, consume highly processed and energy-rich foods, and experience stressful environments with inadequate sleep, which could all make controlling blood glucose difficult in T2D (39–41). Hence, healthcare professionals who manage diabetes should pay more attention to patients who live in towns to improve their blood glucose levels and overall health. With regard to subgroup analysis by publication year, we have observed a closer prevalence of poor glycemic control between studies published before 2019, which is 61.76, and 60.75% in 2019 and after.
Our findings show that older age, not attending formal education, longer duration with diabetes (>10 years), comorbidity, and low adherence to diabetes management were the factors contributing to poor glycemic control in T2D. Furthermore, this study demonstrated that older people >50 years were more likely to have poor glycemic control. This finding was supported by previous studies (15, 42, 43). In contrast, some studies have reported a contrary association between age and glycemic control. A previous review on glycemic control in diabetic patients reported that younger ages are more vulnerable to poor glycemic control (9). Therefore, future studies should consider focusing on age-specific factors for glycemic control.
Diabetes in people who had not attended formal education was also linked to poor glycemic control. This result is in line with previous meta-analyses in Ethiopia (9), a review in Gulf Cooperation Countries (44), and a study in Brazil (45). A low educational level leads to low health literacy, resulting in less knowledge about the disease and glycemic control (46). Hence, health professionals are advised to include a comprehensive health education program on glycemic control in their patient care routine for T2D.
The longer duration of diabetes, known to increase the risk of poor glycemic control, has been identified as a key factor contributing to poor glycemic control in diabetes (37). Our finding confirmed previous reports associating longer durations of diabetes with poor glycemic control. Odai Hamed et al. demonstrated that patients with longer durations of diabetes were associated with the occurrence of poor glycemic control (8). The unfavorable effect of a longer duration of diabetes on glycemic control could be possibly due to inadequate insulin secretion resulting from gradual dysfunction of the β-cell (47). Considering this, people with T2D should be classified as high risk due to the higher probability of losing control over their blood glucose levels. They require more specific and close attention to control blood glucose levels at the optimal level. In addition, our study revealed that T2D patients with comorbidities are more likely to poorly control their blood glucose, and this result is supported by a meta-analysis (48). Studies suggest that diabetes coupled with comorbidities has an adverse effect on the control of blood glucose in diabetes (49). This implies clinicians should design strategies emphasizing the management of diabetes with comorbidities. Low-level adherence is the other important factor leading to inadequate blood glucose control.
We found that T2D with a low level of adherence has 3.67 times higher odds of poor glycemic control compared to diabetes with good glycemic control. Low-level adherence has become a popular challenge over the past few years, which could have a paramount contribution to poor glycemic control in diabetes. Previous studies also mentioned low adherence as a factor in poor glycemic control (9, 50). It is highly recommended that greater effort be focused on counseling and improving adherence rather than changing medications and adjusting the dose (51). Another study showed that improving adherence results in better glycemic control, and better glycemic control was observed in highly adherent patients than in non-adherent patients (52). This indicates that activities such as health education and continuous glycemic control that improve adherence levels are priorities. Overall, the result implies that policymakers, health professionals, and concerned bodies should encourage better control of blood glucose to reduce complications related to poor glycemic control and improve the overall quality of life.
Conclusion
To conclude, our study indicated a high prevalence of poor glycemic control. Factors such as older age, not attending formal education, longer duration of diabetes, comorbidity, and low adherence were associated with poor glycemic control. As diabetes is a progressive chronic disease, complications arise from inadequate diabetes management. This is an issue of concern, as these patients face more challenges in controlling the disease process, which might lead to the worst health outcome. To that end, health professionals should be aware of the need for special emphasis on specific groups such as older diabetics, individuals with low educational status, those with a longer duration of diabetes, diabetes with comorbidities, and those who are not adherent to treatments. One way is to evaluate all diabetes patients with respect to the individualized needs of glycemic targets, lifestyles, and the medications needed to achieve those targets. Efforts to lower A1c should be carried out considering patient characteristics such as age, educational status, duration of diabetes mellitus, comorbidity, and adherence to ensure long-term glycemic control. Further longitudinal cohort studies evaluating the prevalence and factors of poor glycemic control among T2D are required.
Strength and limitations
This study has some limitations. First, articles were restricted to only the English language, which could potentially exclude other relevant articles. Second, the meta-analyses showed high heterogeneity in the pooled prevalence. Sample size variations across studies, different geographical areas, and other unknown factors in the studies might explain the high heterogeneity of estimates. Third, compared to other articles, two articles have used FPG > 154 mg/dL as screening criteria for poor glycemic control; this may have an influence on the overall estimates. Despite all these limitations, this study also has strengths. Several factors associated with poor glycemic control were identified. In addition, the authors followed systematic approaches to include more studies and maintain the quality of the study.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
KT: Conceptualization, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. NG: Conceptualization, Supervision, Investigation, Validation, Writing – review & editing. LY: Methodology, Validation, Writing – review & editing. YY: Project administration, Validation, Writing – review & editing. MK: Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1256024/full#supplementary-material
Abbreviations
DM, Diabetes mellitus; FBG, Fasting blood glucose; A1C, Glycated hemoglobin; JBI, Joanna Briggs Institute; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; T2D, Type 2 diabetes; WHO, World Health Organization
References
1. Azzam, MM, Ibrahim, AA, El-Ghany, A, and Mohammed, I. Factors affecting glycemic control among Egyptian people with diabetes attending primary health care facilities in Mansoura District. Egyptian J Internal Med. (2021) 33:1–10. doi: 10.1186/s43162-021-00065-w
2. Committee ADAPP. 2. Classification and diagnosis of diabetes: standards of medical Care in Diabetes—2022. Diabetes Care. (2022) 45:S17–38. doi: 10.2337/dc22-S002
3. Cho, NH, Shaw, J, Karuranga, S, Huang, Y, da Rocha, FJ, Ohlrogge, A, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. (2018) 138:271–81. doi: 10.1016/j.diabres.2018.02.023
4. Hall, V, Thomsen, RW, Henriksen, O, and Lohse, N. Diabetes in sub Saharan Africa 1999-2011: epidemiology and public health implications. A systematic review. BMC public health. (2011) 11:1–12. doi: 10.1186/1471-2458-11-564
5. International diabetes federation. IDF diabetes atlas 2021. Brussels, Belgium: International Diabetes Federation; (2022). p. 905–911.
6. Hegazi, R, El-Gamal, M, Abdel-Hady, N, and Hamdy, O. Epidemiology of and risk factors for type 2 diabetes in Egypt. Ann Glob Health. (2015) 81:814–20. doi: 10.1016/j.aogh.2015.12.011
7. Mamo, Y, Bekele, F, Nigussie, T, and Zewudie, A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University medical center, Jimma zone, south West Ethiopia: a case control study. BMC Endocr Disord. (2019) 19:1–11. doi: 10.1186/s12902-019-0421-0
8. Al-ma'aitah, OH, Demant, D, Jakimowicz, S, and Perry, L. Glycaemic control and its associated factors in patients with type 2 diabetes in the Middle East and North Africa: an updated systematic review and meta-analysis. J Adv Nurs. (2022) 78:2257–76. doi: 10.1111/jan.15255
9. Gebreyohannes, EA, Netere, AK, and Belachew, SA. Glycemic control among diabetic patients in Ethiopia: a systematic review and meta-analysis. PloS One. (2019) 14:e0221790. doi: 10.1371/journal.pone.0221790
10. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DGGroup* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
11. Institute JB. JBI critical appraisal checklist for studies reporting prevalence data. Adelaide: University of Adelaide (2017).
12. Egger, M, Smith, GD, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
14. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
15. Abdissa, D, and Hirpa, D. Poor glycemic control and its associated factors among diabetes patients attending public hospitals in west Shewa zone, Oromia, Ethiopia: an institutional based cross-sectional study. Metabolism Open. (2022) 13:100154. doi: 10.1016/j.metop.2021.100154
16. Bayisa, B, and Bekele, M. Glycemic control and associated factors among type II diabetic patients on chronic follow up at Southwest Ethiopia. J Med Health Sci. (2017) 6:13–20.
17. Bereda, G, and Bereda, G. The incidence and predictors of poor glycemic control among adults with type 2 diabetes mellitus in ambulatory Clinic of Mettu Karl Referral Hospital, South Western, Ethiopia: a prospective cross sectional study. Int Arch Endocrinol Clin Res. (2021) 7:024. doi: 10.15761/DU.1000155
18. Fekadu, G, Bula, K, Bayisa, G, Turi, E, Tolossa, T, and Kasaye, HK. Challenges and factors associated with poor glycemic control among type 2 diabetes mellitus patients at Nekemte referral hospital, Western Ethiopia. J multidisciplinary healthcare. (2019) 12:963–74. doi: 10.2147/JMDH.S232691
19. Kassahun, T, Eshetie, T, and Gesesew, H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: a cross-sectional survey in Ethiopia. BMC Res Notes. (2016) 9:1–6. doi: 10.1186/s13104-016-1896-7
20. Wabe, NT, Angamo, MT, and Hussein, S. Medication adherence in diabetes mellitus and self management practices among type-2 diabetics in Ethiopia. N Am J Med Sci. (2011) 3:418–23. doi: 10.4297/najms.2011.3418
21. Woldu, MA, Wami, CD, Lenjisa, JL, Tegegne, G, Tesafye, G, and Dinsa, H. Factors associated with poor glycemic control among patients with type 2 diabetes mellitus in ambo hospital, Ambo. Ethiopia Endocrinol Metab Synd. (2014) 3:2161–1017. doi: 10.4172/2161-1017.1000143
22. Yigazu, DM, and Desse, TA. Glycemic control and associated factors among type 2 diabetic patients at Shanan gibe hospital. Southwest Ethiopia BMC research notes. (2017) 10:1–6. doi: 10.1186/s13104-017-2924-y
23. Yosef, T, Nureye, D, and Tekalign, E. Poor glycemic control and its contributing factors among type 2 diabetes patients at Adama hospital medical College in East Ethiopia. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. (2021) 14:3273–80. doi: 10.2147/DMSO.S321756
24. Abera, RG, Demesse, ES, and Boko, WD. Evaluation of glycemic control and related factors among outpatients with type 2 diabetes at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia: a cross-sectional study. BMC Endocr Disord. (2022) 22:1–11. doi: 10.1186/s12902-022-00974-z
25. Alemu, T, Tadesse, T, and Amogne, G. Glycemic control and its determinants among patients with type 2 diabetes mellitus at Menelik II referral hospital. Ethiopia SAGE open medicine. (2021) 9:205031212110230. doi: 10.1177/20503121211023000
26. Demoz, GT, Gebremariam, A, Yifter, H, Alebachew, M, Niriayo, YL, Gebreslassie, G, et al. Predictors of poor glycemic control among patients with type 2 diabetes on follow-up care at a tertiary healthcare setting in Ethiopia. BMC Res Notes. (2019) 12:1–7. doi: 10.1186/s13104-019-4248-6
27. Shimels, T, Abebaw, M, Bilal, AI, and Tesfaye, T. Treatment pattern and factors associated with blood pressure and fasting plasma glucose control among patients with type 2 diabetes mellitus in police referral hospital in Ethiopia. Ethiop J Health Sci. (2018) 28:461–472. doi: 10.4314/ejhs.v28i4.12
28. Tekalegn, Y, Addissie, A, Kebede, T, and Ayele, W. Magnitude of glycemic control and its associated factors among patients with type 2 diabetes at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. PloS one. (2018) 13:e0193442. doi: 10.1371/journal.pone.0193442
29. Ayele, AA, Tegegn, HG, Ayele, TA, and Ayalew, MB. Medication regimen complexity and its impact on medication adherence and glycemic control among patients with type 2 diabetes mellitus in an Ethiopian general hospital. BMJ Open Diabetes Res Care. (2019) 7:e000685. doi: 10.1136/bmjdrc-2019-000685
30. Fasil, A, Biadgo, B, and Abebe, M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar Hospital, Northwest Ethiopia. Diabetes, metabolic syndrome and obesity: targets and therapy. (2019) 12:75–83. doi: 10.2147/DMSO.S185614
31. Gebermariam, AD, Tiruneh, SA, Ayele, AA, Tegegn, HG, Ayele, BA, and Engidaw, M. Level of glycemic control and its associated factors among type II diabetic patients in Debre Tabor general hospital, Northwest Ethiopia. Metabolism Open. (2020) 8:100056. doi: 10.1016/j.metop.2020.100056
32. Shita, NG, and Iyasu, AS. Glycemic control and its associated factors in type 2 diabetes patients at Felege Hiwot and Debre Markos referral hospitals. Sci Rep. (2022) 12:1–9. doi: 10.1038/s41598-022-13673-5
33. Eticha, T, Mulu, A, Gebretsadik, H, Kahsay, G, and Ali, D. Factors associated with poor glycemic control in type 2 diabetic patients investigated at Ayder referral hospital, Mekelle. Ethiopia Ijppr Human. (2016) 6:160–71.
34. Fseha, B. Glycemic control and it’s associated factors in type 2 diabetic patients in Suhul hospital, Northwest Tigray. Ethiopia J Diabetes Metab. (2017) 8:1–6. doi: 10.4172/2155-6156.1000729
35. Mohammed, AS, Adem, F, Tadiwos, Y, Woldekidan, NA, and Degu, A. Level of adherence to the dietary recommendation and glycemic control among patients with type 2 diabetes mellitus in eastern Ethiopia: a cross-sectional study. Diabetes, metabolic syndrome and obesity: targets and therapy. (2020) 13:2605–12. doi: 10.2147/DMSO.S256738
36. Nigussie, S, Birhan, N, Amare, F, Mengistu, G, Adem, F, and Abegaz, TM. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: a cross sectional study. PloS one. (2021) 16:e0251506. doi: 10.1371/journal.pone.0251506
37. Chetoui, A, Kaoutar, K, Elmoussaoui, S, Boutahar, K, El Kardoudi, A, Chigr, F, et al. Prevalence and determinants of poor glycaemic control: a cross-sectional study among Moroccan type 2 diabetes patients. Int Health. (2022) 14:390–7. doi: 10.1093/inthealth/ihz107
38. Liu, X, Xia, Q, Fang, H, Li, R, Chen, Y, Yan, Y, et al. Effect of health literacy and exercise-focused interventions on glycemic control in patients with type 2 diabetes in China. Zhonghua liu xing bing xue za zhi= Zhonghua liuxingbingxue zazhi. (2018) 39:357–62. doi: 10.3760/cma.j.issn.0254-6450.2018.03.021
39. Gozashti, MH, Eslami, N, Radfar, MH, and Pakmanesh, H. Sleep pattern, duration and quality in relation with glycemic control in people with type 2 diabetes mellitus. Iranian J Medical Sci. (2016) 41:531–8.
40. Hamasaki, H. Daily physical activity and type 2 diabetes: a review. World J Diabetes. (2016) 7:243–51. doi: 10.4239/wjd.v7.i12.243
41. Sadiya, A, and Mnla, R. Impact of food pattern on glycemic control among type 2 diabetic patients: a cross-sectional study in the United Arab Emirates. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. (2019) 12:1143–50. doi: 10.2147/DMSO.S209320
42. Reza, HM, Hasan, T, Sultana, M, and Faruque, MO. Glycemic control and its associated factors among patients with diabetes mellitus: a cross-sectional study in Bangladesh. Nutrit Food Sci. (2020) 51:936–46. doi: 10.1108/NFS-09-2020-0343
43. Smith, NL, Heckbert, SR, Bittner, VA, Savage, PJ, Barzilay, JI, Dobs, AS, et al. Antidiabetic treatment trends in a cohort of elderly people with diabetes. The cardiovascular health study, 1989-1997. Diabetes Care. (1999) 22:736–42. doi: 10.2337/diacare.22.5.736
44. Alramadan, MJ, Afroz, A, Hussain, SM, Batais, MA, Almigbal, TH, Al-Humrani, HA, et al. Patient-related determinants of glycaemic control in people with type 2 diabetes in the gulf cooperation council countries: a systematic review. J Diabetes Res. (2018) 2018:1–14. doi: 10.1155/2018/9389265
45. Khattab, M, Khader, YS, Al-Khawaldeh, A, and Ajlouni, K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complications. (2010) 24:84–9. doi: 10.1016/j.jdiacomp.2008.12.008
46. King, A. Poor health literacy: a'hidden'risk factor. Nat Rev Cardiol. (2010) 7:473–4. doi: 10.1038/nrcardio.2010.122
47. Group UPDS. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. (1998) 352:837–53. doi: 10.1016/S0140-6736(98)07019-6
48. Sanal, T, Nair, N, and Adhikari, P. Factors associated with poor control of type 2 diabetes mellitus: a systematic review and meta-analysis. J Diabetology. (2011) 3:1–10.
49. Luijks, H, Biermans, M, Bor, H, van Weel, C, Lagro-Janssen, T, de Grauw, W, et al. The effect of comorbidity on glycemic control and systolic blood pressure in type 2 diabetes: a cohort study with 5 year follow-up in primary care. PloS one. (2015) 10:e0138662. doi: 10.1371/journal.pone.0138662
50. Khan, H, Lasker, SS, and Chowdhury, TA. Exploring reasons for very poor glycaemic control in patients with type 2 diabetes. Prim Care Diabetes. (2011) 5:251–5. doi: 10.1016/j.pcd.2011.07.001
51. Bezie, Y, Molina, M, Hernandez, N, Batista, R, Niang, S, and Huet, D. Therapeutic compliance: a prospective analysis of various factors involved in the adherence rate in type 2 diabetes. Diabetes Metab. (2006) 32:611–6. doi: 10.1016/S1262-3636(07)70316-6
Keywords: poor glycemic control, determinants, meta-analysis, type 2 diabetes, Ethiopia
Citation: Tegegne KD, Gebeyehu NA, Yirdaw LT, Yitayew YA and Kassaw MW (2024) Determinants of poor glycemic control among type 2 diabetes in Ethiopia: a systematic review and meta-analysis. Front. Public Health. 12:1256024. doi: 10.3389/fpubh.2024.1256024
Edited by:
Joao Raposo, Associacao Protectora dos Diabeticos de Portugal, PortugalReviewed by:
Dulce Ó, Portuguese Diabetes Association-APDP, PortugalSudhanshu Kumar Bharti, Patna University, India
Copyright © 2024 Tegegne, Gebeyehu, Yirdaw, Yitayew and Kassaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kirubel Dagnaw Tegegne, a2lydWJlbGRhZ25hd0BnbWFpbC5jb20=
 Kirubel Dagnaw Tegegne
Kirubel Dagnaw Tegegne Natnael Atnafu Gebeyehu
Natnael Atnafu Gebeyehu Lehulu Tilahun Yirdaw
Lehulu Tilahun Yirdaw Yibeltal Asmamaw Yitayew
Yibeltal Asmamaw Yitayew Mesfin Wudu Kassaw
Mesfin Wudu Kassaw