- Department of Infectious Disease, Suzhou Hospital of Integrated Traditional Chinese and Western Medicine, Suzhou, China
Background: China is among the 10 high-burden tuberculosis (TB) countries in the world; thus, investigation and management of household contacts is an essential part of TB prevention strategy.
Objective: To explore the knowledge, attitude, and practice (KAP) toward TB prevention and management among household contacts of TB patients.
Methods: This cross-sectional study enrolled household contacts in Suzhou Hospital of Integrated Traditional Chinese and Western Medicine between September 2022 and January 2023; KAP and demographic characteristics were assessed with the self-designed questionnaire and analyzed by multivariate logistic regression.
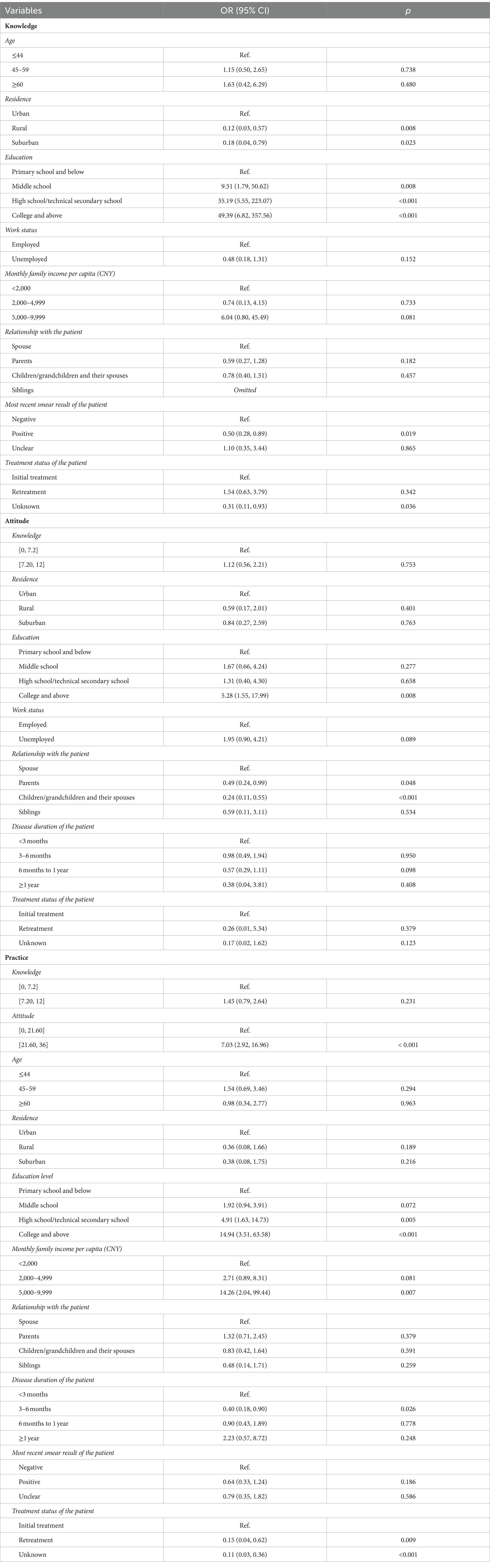
Results: A total of 503 participants were included; of them, 280 (55.78%) were female, and 303, (60.36%) aged ≥45 years. The KAP scores were 6.24 ± 2.20 (possible range: 0–12), 18.69 ± 2.80 (possible range: 0–36), and 20.37 ± 5.15 (possible range: 0–36), respectively. Suburban (OR = 0.18, 95% CI: 0.04–0.79, p = 0.023) and rural (OR = 0.12, 95% CI: 0.03–0.57, p = 0.008) were independently associated with knowledge. Positive attitude (OR = 7.03, 95% CI: 2.92–16.96, p < 0.001), education (high school or technical secondary school, OR = 4.91, 95% CI: 1.63–14.73, p = 0.005; college and above, OR = 14.94, 95% CI: 3.51–63.58, p < 0.001), and shorter disease duration (3–6 months, OR = 0.40, 95% CI: 0.18–0.90, p = 0.026) were independently associated with better practice scores.
Conclusion: Household contacts of TB patients demonstrated insufficient knowledge, unfavorable attitude, and suboptimal practice toward TB prevention and management. Tailored interventions are needed to ensure information accessibility, especially for individuals living in suburban and rural areas.
Introduction
Tuberculosis (TB) is a communicable disease, which is caused by mycobacterium tuberculosis (1, 2). In 2021, an estimated 10.6 million people contracted TB, and 1.6 million died from the disease (1). In 2014 and 2015, the World Health Organization (WHO) and the United Nations (UN) adopted WHO’s end TB Strategy, aiming to eliminate the global TB epidemic by the year 2035 (3). China is one of the highest TB burden countries, with a total TB incidence of 55 per 100,000 and approximately 6,395,000 new tuberculosis cases in 2021 (4). It was estimated that China had the highest burden of latent tuberculosis infection (LTBI) in the world, with approximately 350 million persons living with the infection (5). Household contacts of TB patients are at a higher risk of developing TB due to prolonged and close exposure to source (6), with a prevalence of 5.2% in those ≥15 years old (7). Therefore, investigation and management of household contacts are discussed as essential parts of the TB prevention strategy (1, 8).
Knowledge, attitude, and practice (KAP) study is a structured method that provides access to quantitative and qualitative information regarding a known situation, might reveal misunderstandings or potential barriers to the implementation of healthcare practices, identify what is known and done about various health-related subjects, and plan new interventions (9, 10). It was demonstrated that the methodology of the KAP study could provide useful insight for TB management, as lower KAP scores were associated with delayed healthcare seeking (11). The majority of previous studies accessed KAP toward TB among healthcare workers or TB patients, reporting mostly encouraging results (2, 12–14). However, a recent study undertaken in India has found that compared to TB patients, household contacts had notably poorer knowledge (15). Based on that, KAP of TB prevention and management among household contacts needs to be further studied to develop effective interventions. In addition, this significance is amplified by the distinctive living arrangements found in Chinese families, where at least three generations live together and share the same spaces, making it imperative to gain insights into these dynamics (16).
Although China has made some progress in reducing TB cases, it is still far from achieving the goals of the end TB strategy. A study published in 2021 (17) reported the notable absence of tuberculosis-related training for health professionals and the lower efficacy of primary healthcare providers in referring and managing TB cases among the main healthcare challenges. In 2019, the State Council of China issued the new Healthy China Initiative 2019–2030, which included the Tuberculosis Control Action focused on patient-centered approach with greater attention to vulnerable and hard-to-reach populations (18). Moreover, in the most recent study conducted in Shanghai, China, close contact investigation proved to be at least partly effective strategy for TB control (19). Therefore, this study aimed to explore the KAP toward TB prevention and management among household contacts of TB patients in China. We hypothesized that practice patterns might be related to knowledge and/or attitude, and additional modifiable factors could be identified to plan specific educational interventions in the target population.
Materials and methods
Study design and participants
This cross-sectional quantitative study enrolled household contacts in Suzhou Hospital of Integrated Traditional Chinese and Western Medicine between September 2022 and January 2023. Inclusion criteria are as follows: (1) age ≥18 years and (2) living with TB patients for more than 7 days during the period between 3 months before the diagnosis of TB and 14 days after the start of treatment of TB. Exclusion criteria are as follows: (1) cognitive dysfunction and (2) combined serious life-threatening diseases. A maximum of two family members per patient were included in the survey. The study has been ethically approved by the Ethics Committee of Suzhou Hospital of Integrated Traditional Chinese and Western Medicine (2022-001), and informed consent was obtained from the study participants.
Questionnaire and quality control
The questionnaire was designed with reference to the related literature (2, 20, 21), and WHO guidelines on tuberculosis infection prevention and control: 2019 update, the Technical Guidelines for the Prevention and Management of Tuberculosis in China (22, 23), and the Guidelines for Primary Care of Tuberculosis (Expert Consensus) (24). The first draft was modified by comments from two experts. A pretest was carried out (n = 59), and Cronbach’s α was 0.829, indicating a good internal consistency.
The final questionnaire included four sections with 43 items in total (Supplementary material). The demographic characteristics included 12 items; the knowledge section included 11 items; the attitude section included 10 items; and the practice section included 10 items. For knowledge items, K1–10 scored 1 point for each correct answer, 0 points for a wrong answer or unclear; K11 was about the risk factors of TB, with “well informed,” “partially know,” and “do not know” were scored 2, 1, and 0, the knowledge scores ranging from 0 to 12 points. The attitude items were scored ranging from extremely positive (4 points) to extremely negative (0 points), while items A3 were not scored due to the lack of a clear positive or negative tendency; thus, the possible score range of attitude was 0–36 points. For the practice items, P1, P3, and P4, the presence of positive behavior was assigned 4 points, and the absence of it was assigned 0 points; for P2, the presence of negative behavior was assigned 0 points, and the absence of it was assigned 4 points; P5–9 were scored according to the perspective of positive behavior, ranging from “totally compliantly” (4 points) to “not compliantly at all” (0 points); P10 was to investigate the access to knowledge, which could not be assigned a score. Thus, the score range of the practice was also 0–36 points. According to Blooms’ cut-off point (25), knowledge, attitude, and practice scores of 60% or more of the theoretical total score were considered as “adequate knowledge” (≥7.2), “positive attitude” (≥21.6), and “proactive practice” (≥21.6).
The possibility of participating in the study was discussed with pulmonary tuberculosis patients who were newly diagnosed during the study period. In addition to this, researchers presented the study to previously diagnosed patients who come to the hospital for follow-up visits. Upon agreeing, TB patients received letters from their family members with explanations and invitations to the study site to answer questionnaires. If the family member was present during the visit, they were invited to discuss the informed consent form and fill in the questionnaire right away. Before paper-based questionnaires were distributed in the consultation room, the research team assured participants that there were no right or wrong answers and encouraged them to truthfully fill out the questionnaire. Additionally, the team offered prompt assistance if any difficulties arose during the filling process. Subsequently, a statistician conducted quality control measures, in which any questionnaires that exhibited obvious logical errors or consistently selected the same option throughout were identified as invalid and excluded from the analysis. This rigorous process aimed to uphold the quality and validity of the data collected from the participants, enhancing the credibility of the study’s findings.
Sample size calculation
The sample size was calculated based on the item-respondent theory (26). A ratio of 1:10 is considered suitable according to this theory. Considering 31 KAP items of the questionnaire, the required sample size was 310. Considering a 20% drop-out rate, the final sample size was 388.
Statistical analysis
Stata 17.0 (Stata Corporation, College Station, TX, United States) was used for statistical analysis. The continuous variables with normal distribution were presented as means ± standard deviations (SD) and tested using an independent sample t-test or one-way analysis of variance (ANOVA). Continuous variables with skew distribution were presented as n (percentage) and tested using the Wilcoxon–Mann–Whitney test or Kruskal–Wallis analysis of variance. Categorical variables were presented as n (percentage). Pearson’s correlation tests were used to analyze the correlation between knowledge, attitude, and practice. Variables with p < 0.05 in the univariate logistic regression were included in the multivariate logistic regression. Multivariate logistic regression was conducted to determine the factors associated with KAP. A two-sided p < 0.05 was considered statistically significant.
Results
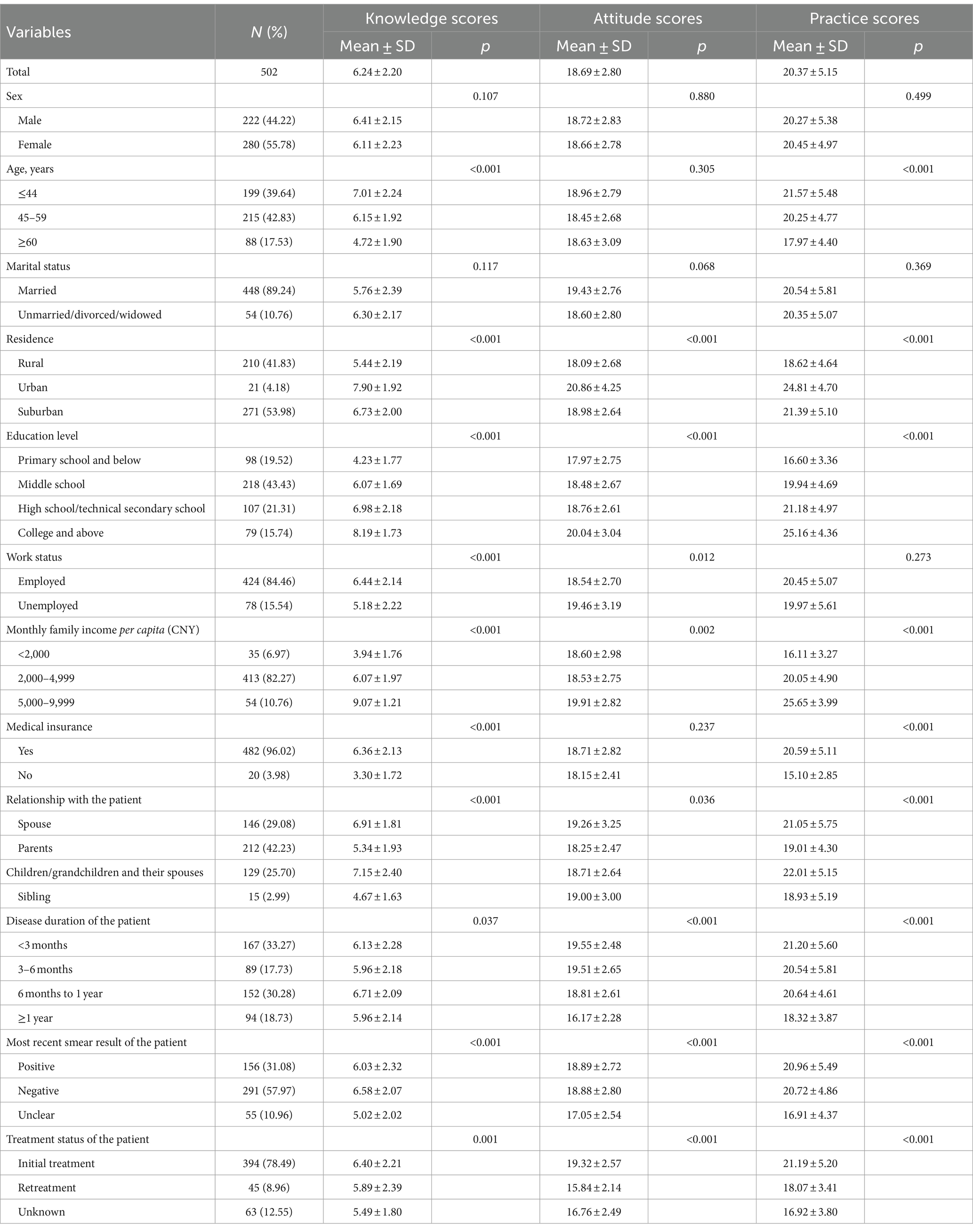
A total of 503 questionnaires were collected, and one of them was excluded due to obvious repetition of the same option, leaving 502 valid questionnaires (99.80%). Among the participants, 303 (60.36%) were aged ≥45 years old, 280 (55.78%) were females, 448 (89.24%) were married, and 210 (41.83%) were living in rural areas. For the relationships with TB patients, 212 (42.23%) and 146 (29.08%) were parents and spouses, respectively. Over half of the patients in their family were < 6 months after first diagnosed with TB (51.00%) and in initial treatment (78.49%) (Table 1).
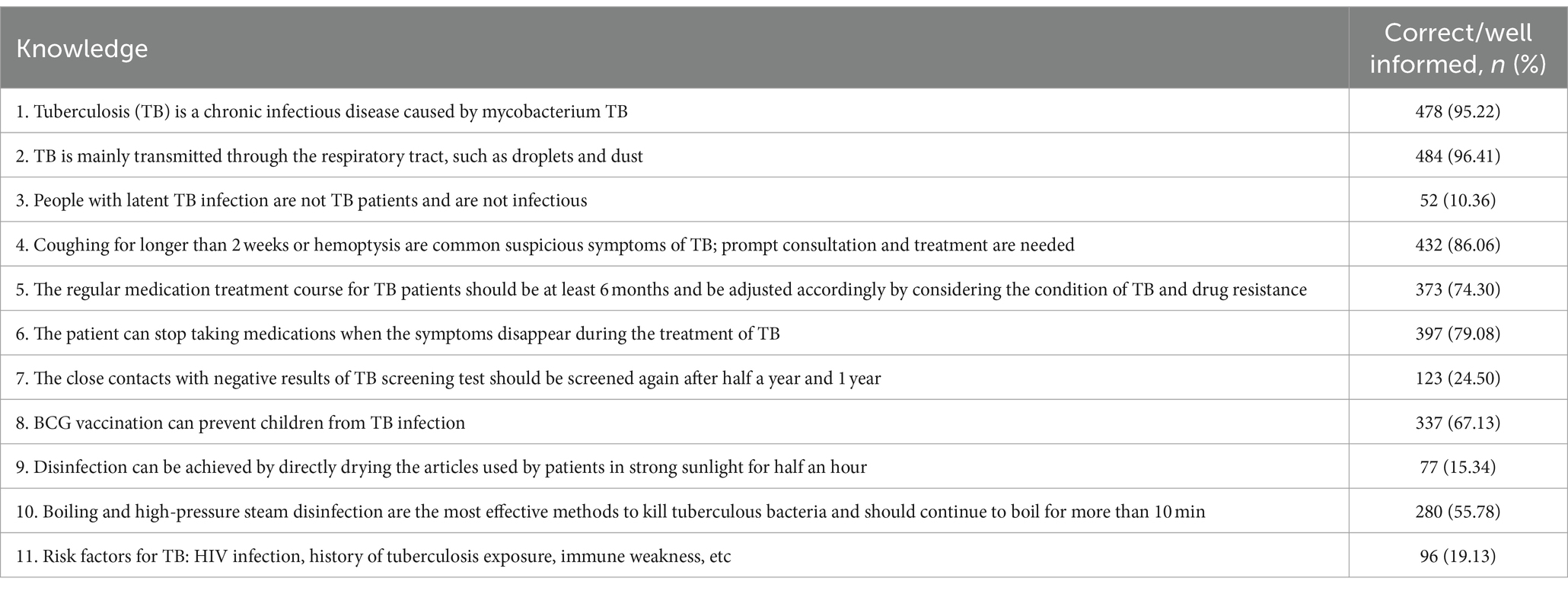
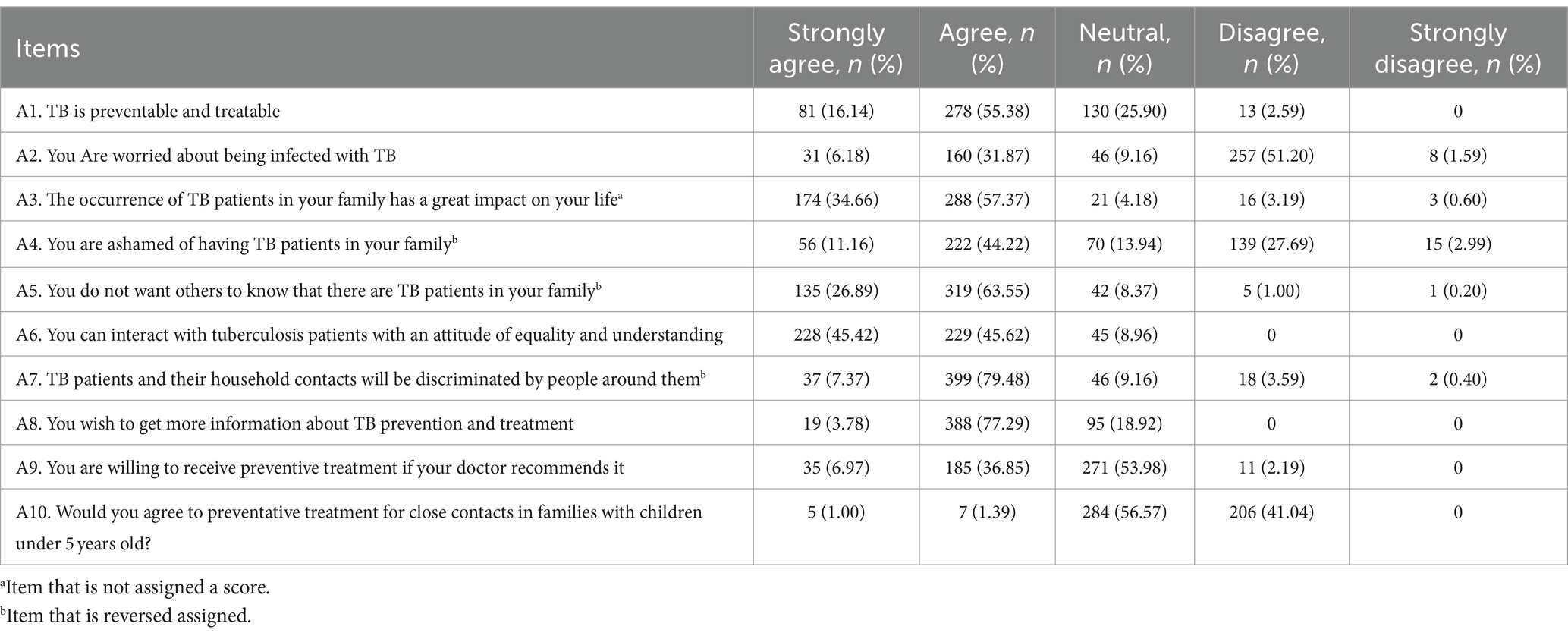
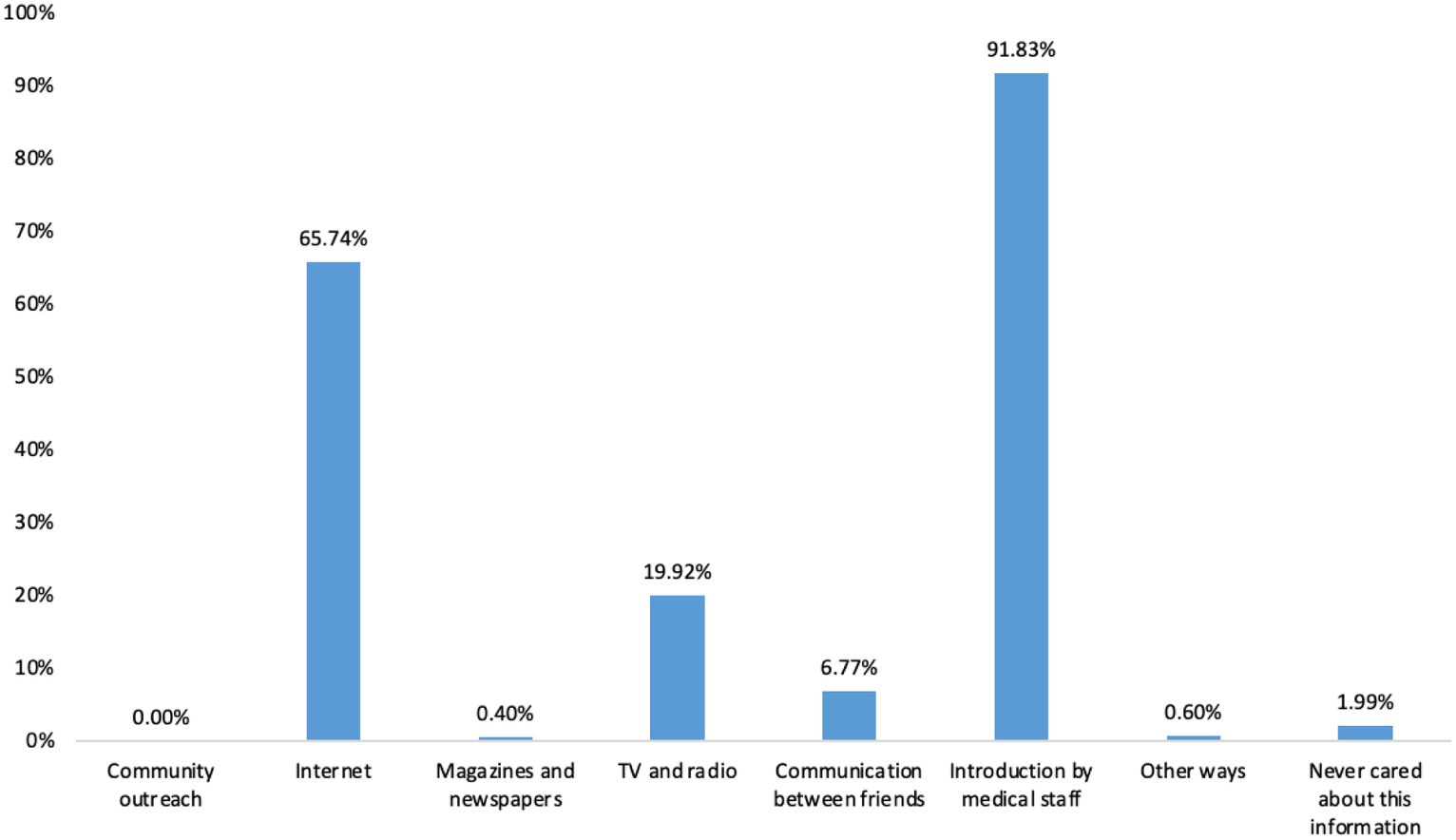
The scores of knowledge, attitude, and practice were 6.24 ± 2.20 (possible range: 0–12), 18.69 ± 2.80 (possible range: 0–36), and 20.37 ± 5.15 (possible range: 0–36), respectively. The knowledge, attitude, and practice scores were all varied among different education, family per capita income, relationship with the patient, and disease duration of the patient in their family (all p < 0.05) (Table 1). The knowledge item with the highest correct rate was “TB is mainly transmitted through the respiratory tract, such as droplets and dust” (K2), with a correct rate of 96.41%; the question with the lowest correct rate was “People with latent TB infection are not TB patients and are not infectious” (K3), with a correct rate of 10.36% (Table 2). For the attitude items, the highest rate of agree/strongly agree item was “You can get along with TB patients as an equal” (A6), with a rate of 91.04%; the item with the lowest rate of agree/strongly agree was “Would you agree to preventative treatment for close contacts in families with children under 5 years old?” (A10), with the rates of 2.39% (Table 3). Regarding the practice items, 95.22% of the participants went to hospitals for TB screening after the patient was diagnosed, and only 7.57% of the participants received preventive treatments (P3), 92.4% presented negative behavior of eating with the TB patient after he/she was diagnosed (P4) (Figure 1). Almost 70.72% of participants reported that they would pay attention to opening windows for ventilation air, washing hands frequently, and taking active physical exercise (P8). However, only 37.45% of participants reported that they would try their best to avoid direct contact with patients (P6) (Table 4). The main access for TB household contacts to learn about TB were media staff (91.83%), internet (65.74%), and TV and radios (19.92%) (Figure 2).
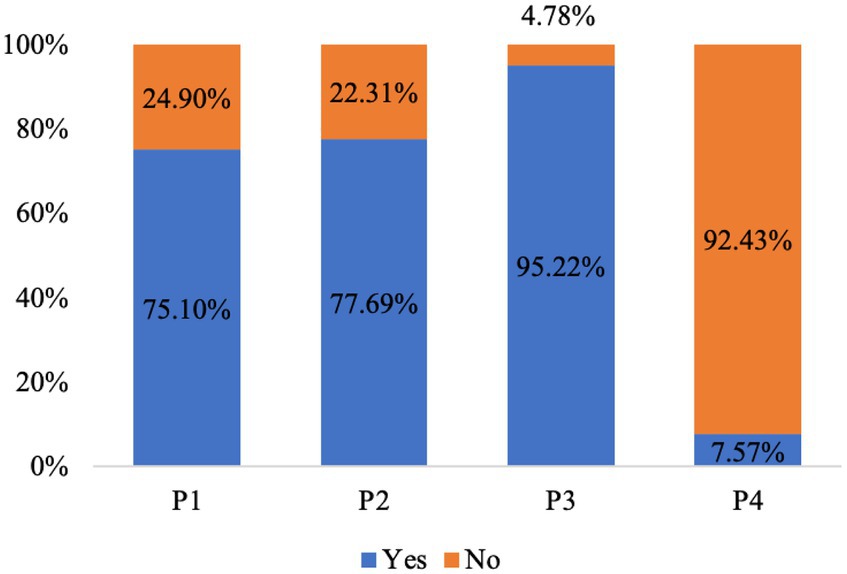
Figure 1. Practice of TB household contacts. P1. The TB patient in your household lives alone in one room. P2. You are still eating with the TB patient in your household after he/she was diagnosed. P3. Did you go to the hospital for TB screening after the patient was diagnosed? P4. Did you receive preventive treatment?
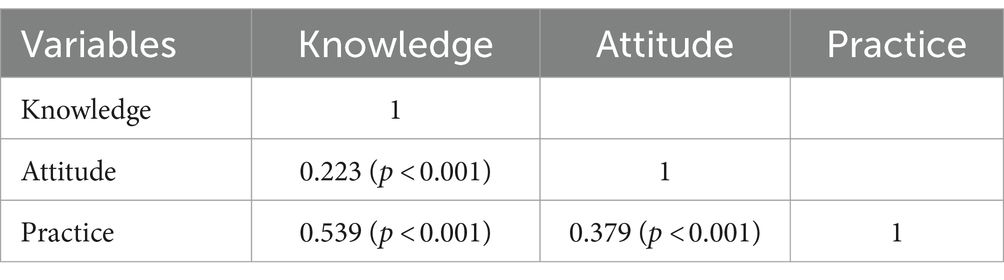
Knowledge was positively correlated with attitude (r = 0.223, p < 0.001) and practice (r = 0.539, p < 0.001), and attitude was positively correlated with practice (r = 0.379, p < 0.001) (Table 5). Suburban (OR = 0.18, 95% CI: 0.04–0.79, p = 0.023) and rural (OR = 0.12, 95% CI: 0.03–0.57, p = 0.008) were independently associated with knowledge. College and above (OR = 5.28, 95% CI: 1.55–17.99, p = 0.008) was associated with attitude. Positive attitude (OR = 7.03, 95% CI: 2.92–16.96, p < 0.001), high school or technical secondary school (OR = 4.91, 95% CI: 1.63–14.73, p = 0.005), and college and above (OR = 14.94, 95% CI: 3.51–63.58, p < 0.001), monthly income of 5,000–9,999 CNY (OR = 14.26, 95% CI: 2.04–99.44, p = 0.007) and disease duration of the patients with 3–6 months (OR = 0.40, 95% CI: 0.18–0.90, p = 0.026) were associated with practice (Table 6).
It also showed differences in knowledge, attitude, and practice dimensions across residences (Supplementary Table S1). For knowledge items, the scores for basic knowledge of TB, TB treatment-related knowledge, and contacts’ knowledge of TB prevention were significantly different among participants from urban, rural and suburban areas (all p < 0.05).
Discussion
This study found insufficient knowledge, unfavorable attitude, and suboptimal practice toward TB prevention and management among household contacts of TB patients in China. The majority of preventive measures violations, such as 92.4% of participants eating together with the TB patient even before the treatment started and 37.45% not trying to avoid direct contact with patients, were most probably explained by the inability to change living arrangements. In-hospital education was identified as a primary (and sometimes only) source of information regarding TB management. These results might help the establishment of prevention measures for the promotion of healthy lifestyles and TB management among household contacts.
A few previous studies undertaken among household contacts of TB patients reported varied results, from poor knowledge, but positive attitude in India (15) to acceptable knowledge/attitude with poor practice in Malaysia (27). This disparity could be attributed to variations in racial, geographical, and cultural characteristics of the populations studied, as well as the differences in the approach to the questionnaire. Nevertheless, some common points were also demonstrated, such as the fact that good knowledge, positive attitude, and proactive practice toward TB were significantly higher among those with higher education, which is also consistent with studies undertaken among TB patients (11), general population (12), university students (28), and social media users (29). Another common observation is the difference between urban and rural populations, with urban residents more likely to have adequate knowledge, favorable attitudes, or good practices toward TB (29–31). In the present study In the present study, knowledge scores itself were notably higher in urban residents compared to rural (7.90 ± 1.92 vs. 5.44 ± 2.19, p < 0.001). Although the percentage of urban residents in our study was low, due to the generally lower prevalence, suburban and rural residence was still independently associated with lower knowledge scores. It necessitates the clear need for educational interventions designed and implemented specifically for rural and suburban areas to facilitate a better understanding of tuberculosis prevention and management.
Violations of TM prevention measures, found in the present study, are most likely equally preconditioned by lower education and income levels of participants, higher number of people living in the same household, and their physical inability to change living arrangements; those features are somewhat typical for rural China, calling for integral systematic changes at all levels (32, 33). However, some improvements might be possible to implement on a local plane. For one thing, in this study, comparing to spouses of the TB patients, the attitude score of their parents, children, and grandchildren was significantly lower; it suggests that the relationship with the patient could play a motivating role in education and tailored intervention might improve the attitude of the household contacts with different family relationships, resulting in the better practice. Aside from that, in-hospital education was identified as a primary source of information for study participants, sometimes being the only source. The results also found that knowledge, attitude, and practice were positively related to each other, consistent with the notion that adequate knowledge is associated with good practices among general populations. Thus, this study emphasizes the importance of effectively communicating essential information to household contacts during hospital visits and even stronger need for alternative ways to reach family members who are unable to visit the hospital. Efforts made to improve KAP toward TB should prioritize individuals with lower education levels, those with a lower socio-economic status, and members of the family other than their spouse.
This study has some limitations. First of all, it is a single-center study with limited sample size. Most importantly, the study was undertaken in the hospital and thus excluded family members who were unable to commute. Second, self-reported questionnaires were used for the measurement of KAP, which may produce information bias. Third, there may be some confounding factors, for example, the KAP of the TB patients, and the health education practice provided by healthcare providers, which were not measured in this study. Despite the limitations, the findings might provide implications for the development of TB education programs and intervention strategies for household contacts of TB patients in China.
In conclusion, this study demonstrated insufficient knowledge, unsatisfactory attitude, and suboptimal practice toward TB prevention and management among household contacts. Tailored interventions are needed to ensure information accessibility, especially for individuals living in suburban and rural areas.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Suzhou Hospital of Integrated Traditional Chinese and Western Medicine (2022-001). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JW and YZ carried out the studies, participated in collecting data, and drafted the manuscript. PZ and XH performed the statistical analysis and participated in its design. FX participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1249971/full#supplementary-material
References
1. World Health Organization . (2022). World Health Organization: global tuberculosis report. Available at: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022
2. Abu-Humaidan, AHA , Tarazi, A , Hamadneh, Y , Al-Leimon, A , Al-Leimon, O , Aljahalin, M, et al. Knowledge, attitudes, and practices toward tuberculosis among Jordanian university students. Front Public Health. (2022) 10:1055037. doi: 10.3389/fpubh.2022.1055037
3. World Health Organization . The end TB strategy. Geneva: World Health Organization (2014) Available at: https://www.who.int/publications/i/item/WHO-HTM-TB-2015.19.
4. Zhang, W . Incidence of tuberculosis in China 2011–2021. Available at: https://www.statista.com/statistics/239095/cases-of-tuberculosis-in-china/#:~:text=In%202021%2C20the20number%20of,lowest%20value%20in%20recent%20years
5. Houben, RM , and Dodd, PJ . The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med. (2016) 13:e1002152. doi: 10.1371/journal.pmed.1002152
6. Fox, GJ , Barry, SE , Britton, WJ , and Marks, GB . Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J. (2013) 41:140–56. doi: 10.1183/09031936.00070812
7. Velen, K , Shingde, RV , Ho, J , and Fox, GJ . The effectiveness of contact investigation among contacts of tuberculosis patients: a systematic review and meta-analysis. Eur Respir J. (2021) 58:2100266. doi: 10.1183/13993003.00266-2021
8. United Nations General Assembly . Resolution A/RES/73/3: political declaration of the high-level meeting of the general assembly on the fight against tuberculosis. New York: United Nations General Assembly (2018) Available at: https://digitallibrary.un.org/record/1649568?ln=en.
9. Andrade, C , Menon, V , Ameen, S , and Kumar, PS . Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian J Psychol Med. (2020) 42:478–81. doi: 10.1177/0253717620946111
10. Rakhshani, T , Dada, M , Kashfi, SM , Kamyab, A , and Jeihooni, AK . The effect of educational intervention on knowledge, attitude, and practice of women towards breast cancer screening. Int J Breast Cancer. (2022) 2022:5697739–8. doi: 10.1155/2022/5697739
11. Makgopa, S , and Madiba, S . Tuberculosis knowledge and delayed health care seeking among new diagnosed tuberculosis patients in primary health facilities in an Urban District, South Africa. Health Serv Insights. (2021) 14:11786329211054035. doi: 10.1177/11786329211054035
12. Datiko, DG , Habte, D , Jerene, D , and Suarez, P . Knowledge, attitudes, and practices related to TB among the general population of Ethiopia: findings from a national cross-sectional survey. PLoS One. (2019) 14:e0224196. doi: 10.1371/journal.pone.0224196
13. Alotaibi, B , Yassin, Y , Mushi, A , Maashi, F , Thomas, A , Mohamed, G, et al. Tuberculosis knowledge, attitude and practice among healthcare workers during the 2016 hajj. PLoS One. (2019) 14:e0210913. doi: 10.1371/journal.pone.0210913
14. Kigozi, NG , Heunis, JC , Engelbrecht, MC , Janse van Rensburg, AP , and van Rensburg, H . Tuberculosis knowledge, attitudes and practices of patients at primary health care facilities in a South African metropolitan: research towards improved health education. BMC Public Health. (2017) 17:795. doi: 10.1186/s12889-017-4825-3
15. Joyce Mary, A . Knowledge, attitude and practices regarding yuberculosis among people diagnosed with tuberculosis and their immediate household contacts in an Urban Health Care Centre in Vellore In: Dissertation. Vellore: Christian Medical College (2020)
16. Wang, M , Yang, Y , Liu, M , and Yu, H . Intergenerational factors influencing household cohabitation in urban China: Chengdu. Int J Environ Res Public Health. (2021) 18:4289. doi: 10.3390/ijerph18084289
17. Long, Q , Guo, L , Jiang, W , Huan, S , and Tang, S . Ending tuberculosis in China: health system challenges. Lancet Public Health. (2021) 6:e948–53. doi: 10.1016/s2468-2667(21)00203-6
18. Zhang, H , Liu, X , Xu, C , Hu, D , Li, X , Li, T, et al. Guiding tuberculosis control through the healthy China initiative 2019–2030. China CDC Wkly. (2020) 2:948–50. doi: 10.46234/ccdcw2020.236
19. Zhou, M , Wang, L , Li, M , Zou, J , Li, Y , Li, J, et al. Contact investigation of tuberculosis in Shanghai, China: a 13-year cohort. Tuberculosis. (2023) 139:102323. doi: 10.1016/j.tube.2023.102323
20. Bashorun, AO , Linda, C , Omoleke, S , Kendall, L , Donkor, SD , Kinteh, MA, et al. Knowledge, attitude and practice towards tuberculosis in Gambia: a nation-wide cross-sectional survey. BMC Public Health. (2020) 20:1566. doi: 10.1186/s12889-020-09685-3
21. Gil, N , López, L , Rodríguez, D , Rondón, M , Betancourt, A , Gutiérrez, B, et al. Myths and realities about knowledge, attitudes and practices of household contacts of tuberculosis patients. Int J Tuberc Lung Dis. (2018) 22:1293–9. doi: 10.5588/ijtld.17.0886
22. WHO Guidelines Approved by the Guidelines Review Committee . WHO guidelines on tuberculosis infection prevention and control: 2019 update. Geneva: World Health Organization (2019).
23. Technical guidelines for tuberculosis control in China. Available at: https://tb.chinacdc.cn/xxjlg/202111/W020211119672904030470.pdf
24. Chinese Medical Association, Journal of Chinese Medical Association, General Practice Branch of Chinese Medical Association . Tuberculosis primary-level diagnosis and treatment guidelines. Chin J Gen Pract. (2019) 18:709–17. doi: 10.3760/cma.j.issn.1671-7368.2019.08.002
25. Agonafir, M , Assefa, Y , Girmachew, F , and Jerene, D . Factors affectinsg the utilization of Xpert MTB/RIF assay among TB clinic health workers in Addis Ababa. J Clin Tuberc Other Mycobact Dis. (2018) 12:48–53. doi: 10.1016/j.jctube.2018.06.007
26. Naqvi, AA , Hassali, MA , Rizvi, M , Zehra, A , Nisa, ZU , Islam, MA, et al. Validation of the general medication adherence scale in Pakistani patients with rheumatoid arthritis. Front Pharmacol. (2020) 11:1039. doi: 10.3389/fphar.2020.01039
27. Loh, SY , Zakaria, R , and Mohamad, N . Knowledge, attitude, and stigma on tuberculosis and the associated factors for attitude among tuberculosis contacts in Malaysia. Medeni Med J. (2023) 38:45–53. doi: 10.4274/MMJ.galenos.2023.14478
28. Puspitasari, IM , Sinuraya, RK , Aminudin, AN , and Kamilah, RR . Knowledge, attitudes, and preventative behavior toward tuberculosis in university students in Indonesia. Infect Drug Resist. (2022) 15:4721–33. doi: 10.2147/idr.S365852
29. Mahmud, S , Mohsin, M , Irfan, SH , Muyeed, A , and Islam, A . Knowledge, attitude, practices, and determinants of them toward tuberculosis among social media users in Bangladesh: a cross-sectional study. PLoS One. (2022) 17:e0275344. doi: 10.1371/journal.pone.0275344
30. Adane, K , Spigt, M , Johanna, L , Noortje, D , Abera, SF , and Dinant, GJ . Tuberculosis knowledge, attitudes, and practices among northern Ethiopian prisoners: implications for TB control efforts. PLoS One. (2017) 12:e0174692. doi: 10.1371/journal.pone.0174692
31. Bati, J , Legesse, M , and Medhin, G . Community's knowledge, attitudes and practices about tuberculosis in Itang special district, Gambella Region, South Western Ethiopia. BMC Public Health. (2013) 13:734. doi: 10.1186/1471-2458-13-734
32. Wang, H , Zhao, Q , Bai, Y , Zhang, L , and Yu, X . Poverty and subjective poverty in rural China. Soc Indic Res. (2020) 150:219–42. doi: 10.1007/s11205-020-02303-0
Keywords: tuberculosis, household contacts, prevention, management, knowledge, attitude, practice
Citation: Zhang Y, Wu J, Hui X, Zhang P and Xue F (2024) Knowledge, attitude, and practice toward tuberculosis prevention and management among household contacts in Suzhou Hospital, Jiangsu province, China. Front. Public Health. 12:1249971. doi: 10.3389/fpubh.2024.1249971
Edited by:
Adwoa Asante-Poku, University of Ghana, GhanaReviewed by:
Lawrence Ulu Ogbonnaya, Ebonyi State University, NigeriaThabang Manyaapelo, Africa Health Research Institute (AHRI), South Africa
Copyright © 2024 Zhang, Wu, Hui, Zhang and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingwen Wu, d3VqaW5nd2VucGpAMTYzLmNvbQ==
 Yuping Zhang
Yuping Zhang Jingwen Wu
Jingwen Wu