- 1Department of Health Promotion and Behavioral Sciences, University of Texas Health Science Center at Houston (UTHealth) School of Public Health, Houston, TX, United States
- 2Center for Health Promotion and Prevention Research, UTHealth School of Public Health, Houston, TX, United States
- 3Department of Health Promotion and Behavioral Sciences, UTHealth School of Public Health, Dallas, TX, United States
- 4ProSalud, Inc., Houston, TX, United States
Background: Despite CDC recommendations for breast and cervical cancer screening and HPV vaccination, cancer control behaviors are underutilized among low-income Latinas. Salud en Mis Manos (SEMM), adapted from Cultivando La Salud, is a community health worker- (CHW-) delivered evidence-based intervention (EBI), shown to increase breast and cervical cancer screening.
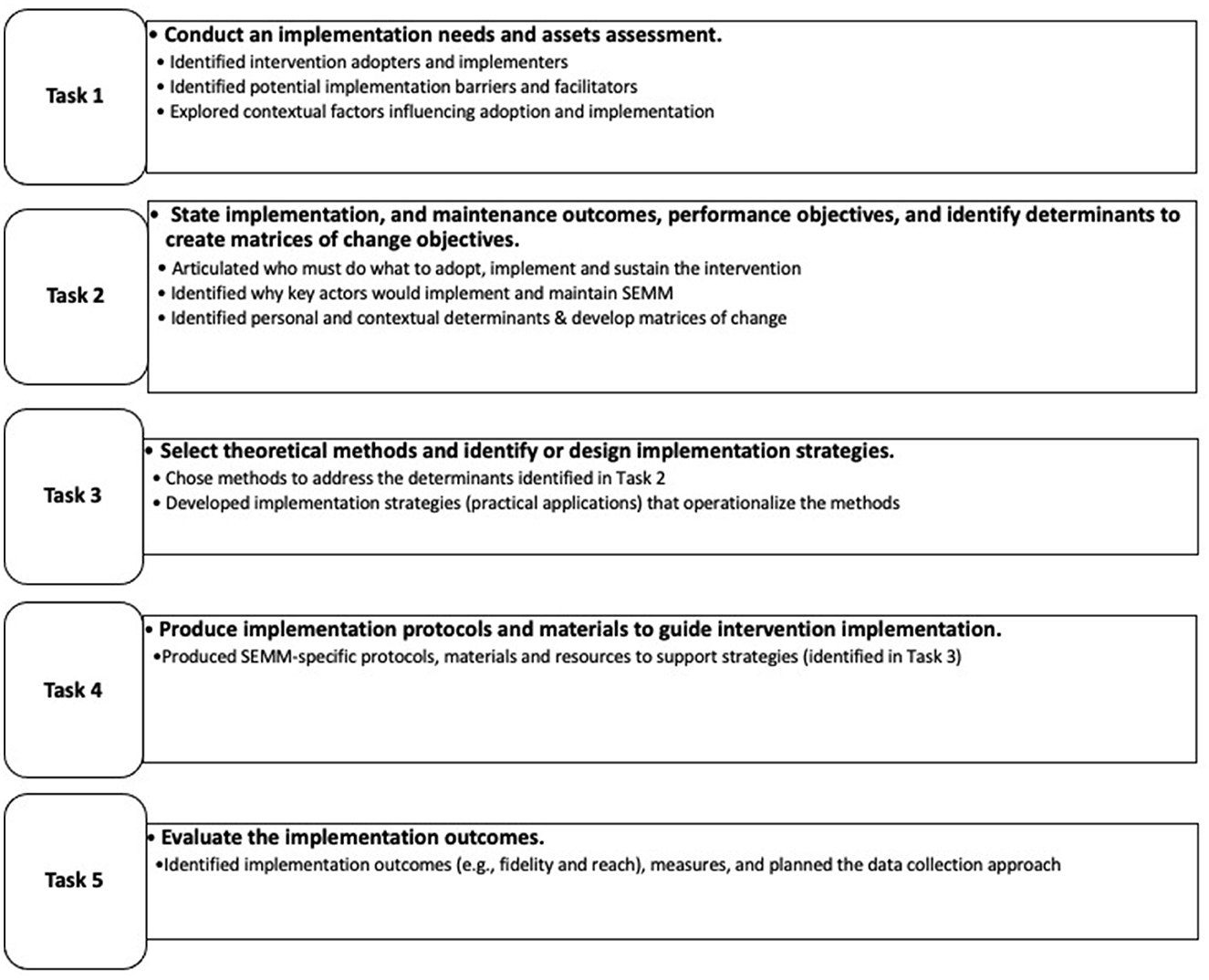
Methods: We used Implementation Mapping to create SEMM-Dissemination and Implementation Assistance (SEMM-DIA), a set of implementation strategies designed to support implementation and maintenance of SEMM in clinic settings. Specifically, we used Implementation Mapping's five iterative tasks to guide the use of theories and frameworks, evidence, new data, and stakeholder input to develop strategies to accelerate and improve implementation fidelity, reach, and maintenance of the SEMM intervention. The resulting implementation mapping logic model also guides the SEMM-DIA evaluation plan to assess reach, effectiveness, implementation, and maintenance.
Discussion: Increased use of implementation planning frameworks is necessary to accelerate the translation of EBIs to public health practice. This work demonstrates the application of Implementation Mapping to develop SEMM-DIA, providing a model for the development of other implementation strategies to support translation of evidence-based health promotion interventions into clinic settings.
Introduction
Despite the availability and effectiveness of evidence-based interventions (EBIs), their implementation and dissemination have been slow, resulting in limited reach (1), and missed opportunities for positive public health impact (2–4). Challenges to EBI adoption, implementation, and maintenance are multifactorial and multilevel, and are influenced by environmental and organization-level factors (e.g., resources and capacity), as well as individual implementer-level factors (e.g., skills or self-efficacy). Implementation support strategies designed to address the complex factors that influence EBI adoption, implementation, and maintenance can promote translation of behavioral intervention research to effective public health practice.
Implementation strategies provide guidance and support to EBI adopters and implementers, helping to ensure effective program delivery, including attention to fidelity, such that essential elements of the intervention are preserved as they are implemented within their organization's context. Implementation strategies must also build on organizations' assets and address organizations' needs (2–4). We used Implementation Mapping, a framework for planning and developing implementation strategies to accelerate and improve implementation and maintenance of Salud en Mis Manos (SEMM), an evidence-based community health worker (CHW)-delivered intervention shown to increase breast and cervical cancer screening among low-income Latinas (5, 6). The Implementation Mapping framework guides a systematic planning process that incorporates perspectives and experiences of multiple stakeholders and uses evidence and theory to inform development of implementation strategies (7). While the SEMM intervention addresses an important problem (underutilization of breast and cervical cancer screening) and has the potential to reduce breast cancer survival disparities and the disproportionate burden of cervical cancers among Latinas (compared with non-Hispanic whites; NHWs) (8), widespread implementation of SEMM has been slow.
Briefly, SEMM is an evidence-based intervention based on Cultivando la Salud (CLS), a CHW-delivered breast and cervical cancer screening behavioral intervention originally developed for Mexican-American women living in farmworkers communities (9, 10). Adaptations of SEMM for medically underserved Latinas in urban and suburban settings increased the behavioral intervention's generalizability to Latinas from diverse backgrounds and to those living in areas with different environmental and social contexts (6). SEMM intervention planners adapted the original CLS CHW-delivered education intervention and referral protocol (to deliver referrals to low-cost services) guided by the Intervention Mapping framework for adaptation (IM ADAPT). This systematic approach to intervention adaptation planning informed integration of theory, evidence, and formative work to ensure retention of salient elements while increasing relevance to the new population and setting. In addition, the SEMM adaptation included development of a telephone-based health coaching and navigation component delivered by health coach navigators trained to help women overcome structural and personal barriers to completing needed cancer prevention services. Based on a randomized controlled trial (Cancer Prevention and Research Institute of Texas, CPRIT award, PP110081), the adapted intervention effectively increased screening in the intervention compared with control groups for both mammogram (39.9 vs. 20.3%; p < 0.001) and Pap outcomes (55.8 vs. 27.4%; p < 0.001); intent-to-treat analyses were also significant (11). While proven effective, broad uptake and use of SEMM has been slow and implementation in clinical settings has been particularly limited.
We used Implementation Mapping, a systematic process for designing and tailoring implementation strategies to develop Salud en Mis Manos- Dissemination and Implementation Assistance (SEMM-DIA), a multifaceted implementation strategy, to support implementation of SEMM. This paper serves as a model for applying the Implementation Mapping framework to develop implementation strategies. In the case of SEMM-DIA, these strategies were designed to build capacity of clinic leadership and management, intervention champions, and CHWs to plan, manage, implement, and maintain SEMM.
Methods
Conceptual framework and theoretical basis for the development of the implementation strategy
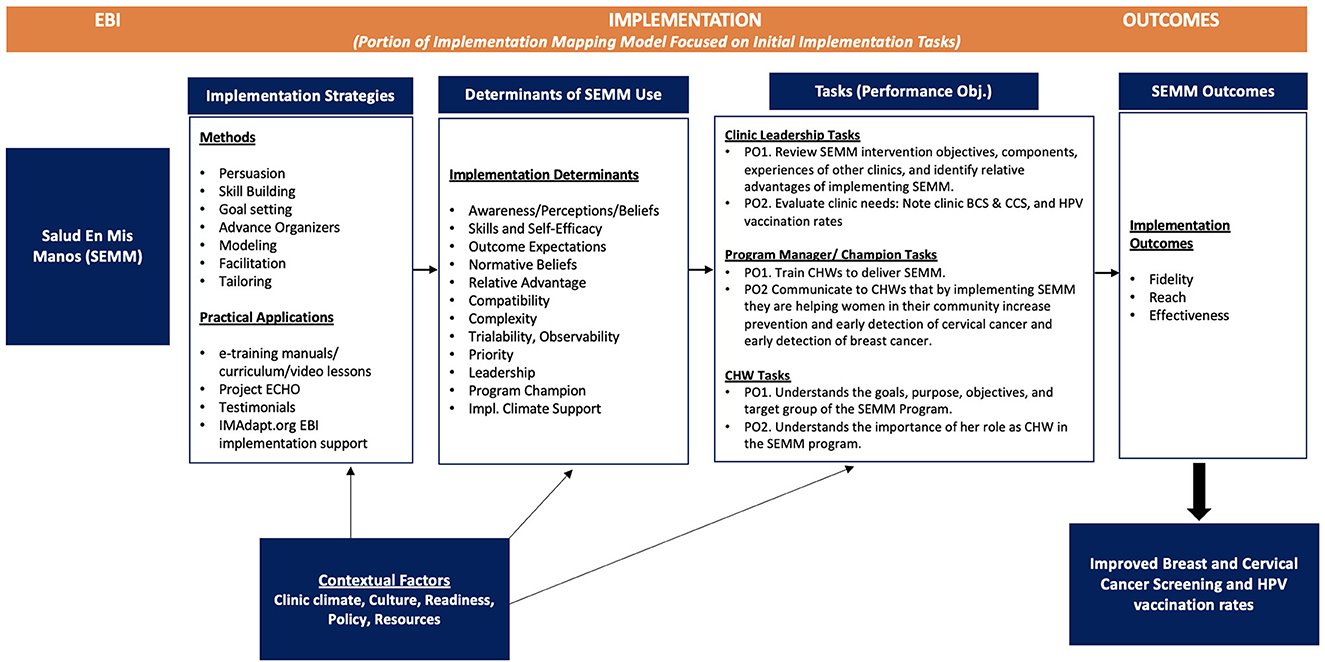
The Implementation Mapping framework includes five tasks that guide implementation strategy planners in the design and tailoring of implementation strategies. These tasks are described below (see Figure 1) (7). Implementation Mapping is a step-by-step protocol that incorporates empirical evidence, stakeholder input and feedback, and is informed by theories, models and frameworks. In the development of SEMM-DIA, we used the Implementation Mapping framework to help integrate behavioral theory [i.e., Social Cognitive Theory (SCT)], to identify behavioral determinants at multiple levels (e.g., organization and CHW) (12) and implementation frameworks, including the Interactive Systems Framework for Dissemination and Implementation (ISF) (13) and the Exploration, Preparation, Implementation, and Sustainment (EPIS) framework (14). To guide planning evaluation outcomes, we used RE-AIM, focusing on Reach, Effectiveness, Implementation, and Maintenance (intention) (1). All behavioral and Implementation Science theories and frameworks used to develop the SEMM-DIA implementation support strategy are summarized in Table 1.
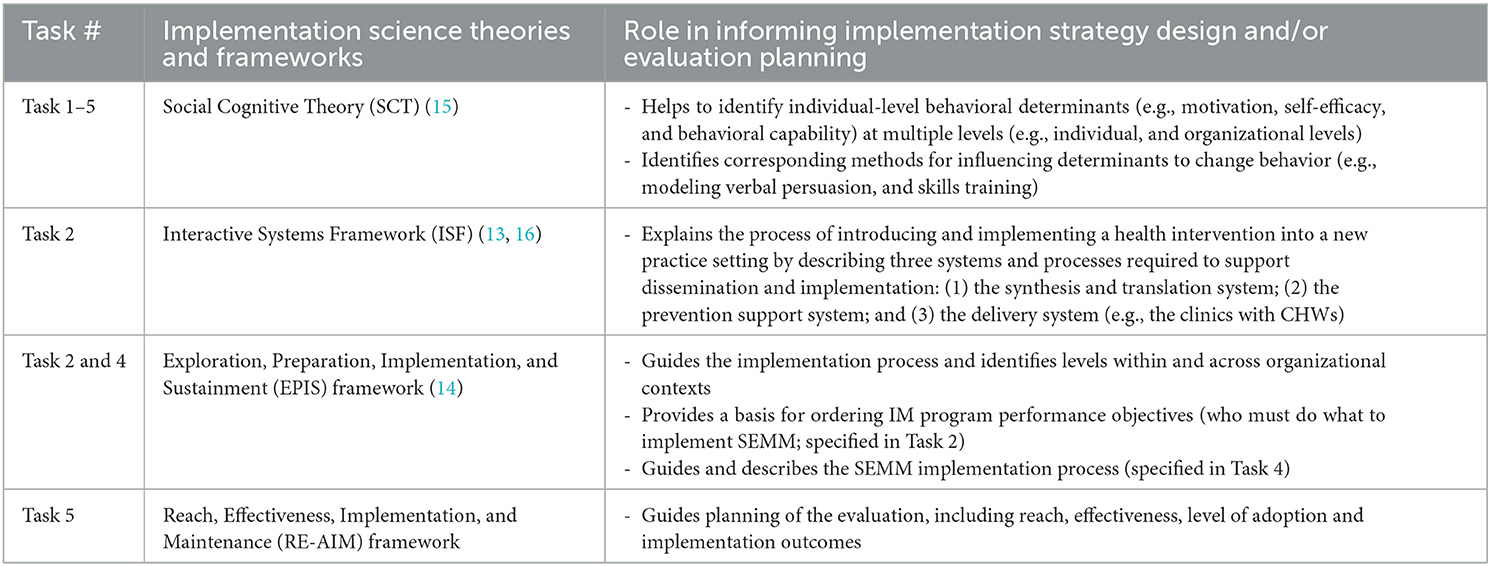
Table 1. Summary of theories, frameworks and models used to guide development of SEMM-DIA, an implementation intervention.
The Implementation Mapping planning process also supports a community-engaged approach to implementation strategy development, helping to integrate multiple stakeholder perspectives throughout development. Using a community-engagement approach, we included perspectives of stakeholders with previous experience implementing the SEMM intervention, as well as people with insight into the clinic practice setting (e.g., clinic leaders, clinic managers, and CHWs) who could also represent the patient perspective. Implementation stakeholders invited to participate in the planning process included managers working with The Breast and Cervical Cancer Collaborative of Texas, and representatives from the Centers for Disease Control and Prevention (CDC)-funded Texas Prevention Research Center Community Advisory Board (CAB). The CAB included community leaders representing community-based CHW organizations (e.g., ProSalud, Inc. and South Coastal Area Health Education Center; AHEC), and CHWs with substantial field experience working with Latinas on breast and cervical cancer screening interventions in Federally Qualified Health Centers (FQHCs) in the Greater Houston area. It also included staff and leaders at community health centers, many of whom provided insights into the patient populations they serve, such as patient's concerns regarding undergoing cancer screening and barriers to completing screening services.
Methods for each Implementation Mapping task
Task 1. Conduct an implementation needs and assets assessment
The research team conducted 12 semi-structured Zoom-based interviews with clinic personnel representing clinic leadership (e.g., CEO, Medical Director), mid-management (e.g., Clinic Program Manager, MA/Director of Program Development, and CHWs at four different Texas Community Health Centers. Participants were provided with a five-minute PowerPoint overview of the SEMM intervention prior to their interviews. Three interview guides were developed respectively for leadership, mid-level, and CHWs, informed by SCT, ISF and the Readiness heuristic, R = MC2 (readiness = motivation × innovation specific capacity × general capacity) (15). Interview questions focused on exploring clinic and program implementers' needs and assets (e.g., resources, infrastructure, and potential related experiences) that may influence SEMM implementation, such as: (1) What could be potential problems/barriers that you might face to implement the intervention? (2) Who would be involved in planning how the program would be incorporated into clinical workflows and practice? (3) What would make it easier to adopt and implement the intervention? and (4) What makes an organization ready (to take on a program like this/new programs)? Interviews were audio-recorded and professionally transcribed. Using an adapted rapid qualitative approach (RQA) (16), one independent reviewer (reviewer CC) analyzed all 12 interview transcriptions to identify potential implementation barriers and facilitators. Transcript data were tabulated in summary tables by content domain. For example, the question, “Your clinic has CHWs—can you tell me a bit about the program and how CHWs are used?” represents the domain “CHW utilization.” The data were then coded for potential barriers and facilitators. A second reviewer (reviewer PL) reviewed the summary tables for clarity. Both reviewers then met to discuss and reach consensus on any discrepancies. The data were stratified by implementer level (leadership, mid-level, CHW) and by theoretical constructs (e.g., complexity and staff capacity (Readiness constructs). To further examine the data, an in-depth content and thematic analysis is currently being conducted by the research team using a traditional qualitative analysis approach. Findings will help better understand which additional environmental factors should be considered for improved program implementation and maintenance (17–20).
We also used core processes adapted from Intervention Mapping to aid in the identification of barriers and facilitators to implementation (21). As described by Fernandez et al., “Core processes are a set of helpful actions or tools that can provide a systematic way to answer questions raised during the planning process and aid in the identification of potential barriers and facilitators to implementation” (21, 22). These core processes were used throughout the five tasks of implementation mapping where appropriate and were fundamental in Task 1. They included: (1) Brainstorm potential factors (i.e., barriers and facilitators) based on experience, past needs assessments, and published literature, (2) Use theories and frameworks, (3) Collect new data, and (4) Prioritize the most important and changeable factors. We considered both health behavior theory (i.e., SCT) and implementation science frameworks (i.e., Interactive Systems Framework and Organizational Readiness) during the identification of factors potentially influencing implementation. Doing so enabled the research team to confirm if the listed barriers and facilitators previously identified aligned with constructs from existing theoretical models. This step also informed the identification of additional constructs that were relevant in similar implementation efforts and allowed the research team to refine performance objectives (who must do what to implement SEMM). Finally, the research team integrated diverse perspectives provided by the CAB members.
Task 2. State implementation and maintenance outcomes, performance objectives, and identify determinants to create matrices of change objectives
In Task 2, based on the needs and assets assessment conducted in Task 1, the research team articulated performance objectives (who must do what to implement SEMM) as well as the potential factors (from theory, evidence, and new data) that might influence key actors' pre-implementation, implementation, and maintenance of SEMM. We developed matrices of specific change objectives by crossing performance objectives and determinants and asking, “what has to change in X determinant in order to accomplish this implementation performance objective.”
Task 3. Choose theoretical methods; and identify or design implementation strategies
In Task 3, we considered theoretical change methods (both those focused on changing behavior and those focused on influencing the implementation environment) that could address determinants identified in Task 2 (23, 24). We developed the implementation strategies by operationalizing the methods. We created practical applications of those methods such that they were feasible and appropriate for use in clinic settings. This task was also conducted in partnership with stakeholder engagement, e.g., those with previous experience implementing SEMM, as well as clinic and CHW experiences in general. The research team engaged CAB members monthly via Zoom to pose a series of questions/ideas/implementation strategies to CAB members to gain their insight into what resources would best serve and support clinic personnel with the implementation of SEMM. By working with clinic representatives, selection of implementation strategies took into consideration relevance and feasibility for different implementers in clinical settings.
Task 4. Produce implementation protocols and materials to guide intervention implementation
Following the planning of implementation strategies in Task 3, we identified, adapted, or produced the SEMM implementation protocols, materials, and tools to include in the SEMM-DIA implementation package. This task was also informed by the EPIS “meta” framework (14). This “meta” framework consists of five phases that we used to order SEMM-DIA performance objectives, including (1) Exploration (Prioritizing SEMM), (2) Preparation (Assessing clinic readiness), (3) Preparation for implementation of SEMM, (4) Implementation, and (5) Maintenance. Each phase was associated with clinic personnel responsible for that phase (i.e., clinic leadership, SEMM program manager and/or champion, and CHW). We also developed documentation to support clinic stakeholders' implementation planning and process monitoring of SEMM. The overarching goal of this implementation strategy package was to provide clear, user-friendly support to promote feasibility, and fidelity of implementation.
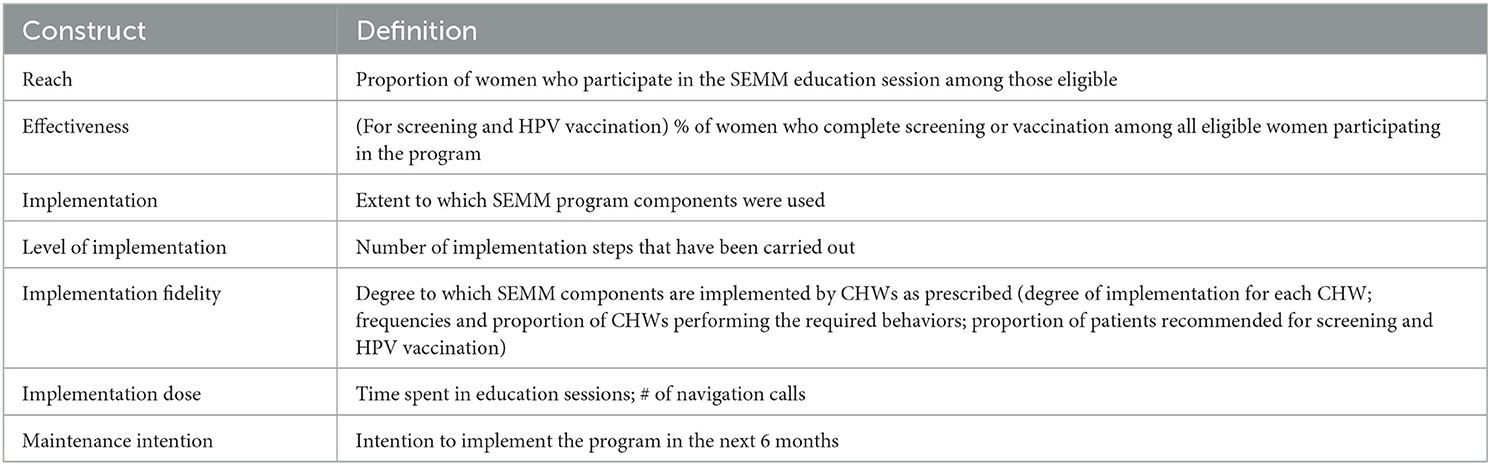
Task 5. Evaluate the implementation outcomes
Task 5 of Implementation Mapping focused on planning the evaluation of the SEMM-DIA implementation strategy, to assess the effect of SEMM-DIA on implementation outcomes, and on SEMM effectiveness outcomes (e.g., breast and cervical cancer screening and HPV vaccination). We also developed indicators and measures for the evaluation, informed by the matrices. Our evaluation plan included measures to assess organizational readiness for implementation, level of implementation, determinants of implementation, experiences with implementing SEMM, and implementation maintenance. Selection of mediators and moderators of implementation was guided by behavioral theoretical constructs based on SCT and ISF identified during the planning process.
Results
Task 1. Conduct needs and asset assessment
Stakeholder engagement played a critical role on the planning team (comprised of both stakeholders and research team members). The CAB weighed in on key actionable findings to ultimately inform implementation strategy development. Input from all CAB members during Zoom meetings helped to identify potential barriers and facilitators influencing the implementation and maintenance of the program. Included in these CAB meetings over the course of the needs assessment period were clinic leadership, clinic managers, as well as former SEMM CHW managers (heretofore referred to as SEMM champions).
Adopters and implementers
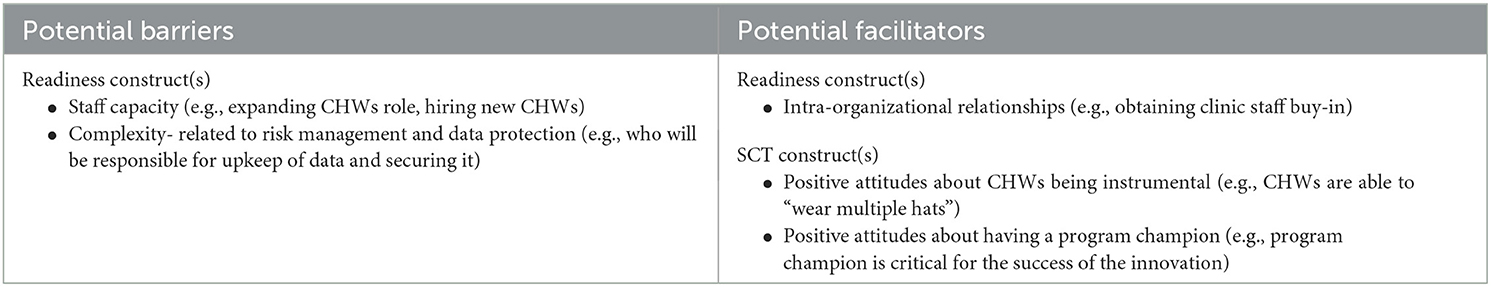
Potential barriers and facilitators to implementation corresponded to Readiness and SCT constructs. For example, related to Readiness, staff capacity, and complexity constructs were identified as potential barriers. Participants expressed concerns about staff capacity and the need to further expand CHWs' role for program implementation and having to hire new clinic staff, “What we need are new people to perform this role, I don't have people I could add more responsibility to.” Another potential barrier included complexity, as it is related to data management. Participants had concerns about data risk management and data protection (e.g., who will be responsible for acquiring and securing the program's database?).
Facilitators
Regarding potential facilitators, leadership participants stressed the importance of intra-organizational relationships, stating that obtaining clinic staff buy-in for intervention implementation is important, “I'd also gain the feedback from people who will implement it, so that we can be on the same page that we're going to do it.” Other potential facilitators related to SCT included positive attitudes among participants who recognized that having CHWs is instrumental, “Our community health workers are used in every capacity of the organization, from our clinic services, health education, outreach, they are the ones who are instrumental in doing the education and outreach activities for the clinics.” Participants emphasized CHWs' role as one that can “wear multiple hats” and therefore would likely be able to play various roles related to implementation. Positive attitudes also included the belief that having a SEMM champion is critical for its success. Of note, participants also discussed the need to develop communication strategies to facilitate SEMM intervention promotion and implementation by clinic staff, “This is what I can just easily send [referring to email templates] to the staff. This is what we're doing and how to refer a patient kind of things.”
Barriers
The planning team, including researchers and CAB stakeholders, (e.g., clinic staff, SEMM champions, and CHWs) prioritized which barriers needed to be addressed. Clinic participants provided insight into addressing implementation challenges and shared lessons learned and practical suggestions regarding factors affecting CHW implementation. For example, in one of the monthly CAB meetings, stakeholders validated the finding that CHWs do, in most cases, “wear multiple hats.” Stakeholders also added that when there is no CHW, they often have other staff (e.g., patient navigator, patient educators) who could (and do) serve in a similar role. While the original program was designed to focus on community outreach for identifying women in need of services, CAB members stressed the importance of in-reach (i.e., focusing on current clinic patients), in addition to outreach as an important way to identify women in need of screening and HPV vaccination.
CAB members also helped clarify who the potential implementers in clinic practice settings would likely be in the safety-net clinic context (e.g., FQHCs). CHW managers with extensive experience managing CHW training and CHW delivery provided insight into potential barriers and facilitators to managing CHWs. CAB members discussed the importance of SEMM champions engaging in weekly meetings with CHWs, in which they use effective facilitation skills, such as facilitating discussions between CHWs to encourage CHWs to share their work challenges and successes. For clinic-based implementation, by talking with SEMM managers who supervised clinic delivery of SEMM, we identified the importance for clinic leaders to understand their patient population's needs and to prioritize SEMM delivery, focusing on current patients (in-reach recruitment strategy), or focus on delivering SEMM to women in surrounding communities to enroll women in the SEMM intervention (outreach recruitment strategy). Table 2 presents an example of findings from the rapid qualitative analysis of interviews conducted at the leadership level.
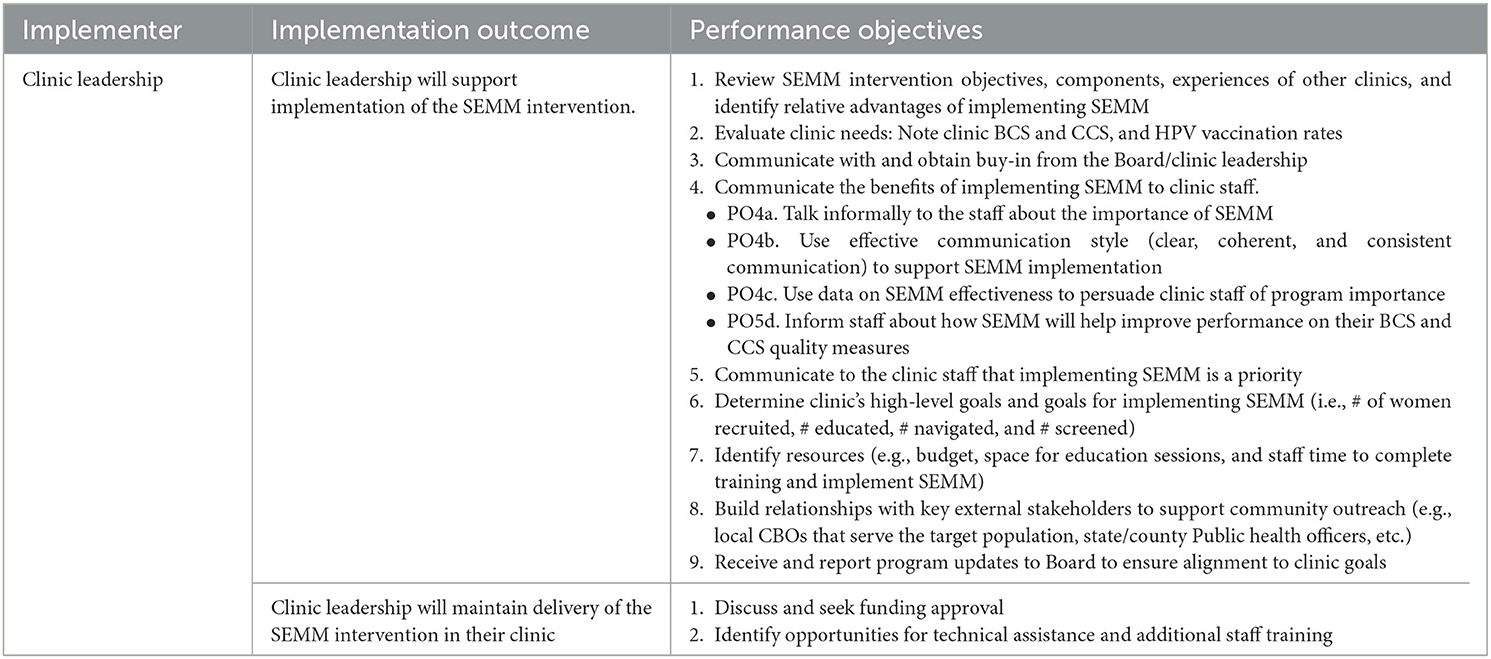
Task 2. Identify pre-implementation, implementation and maintenance outcomes, performance objectives, and determinants, and create matrices of change
Results of the needs and assets assessment helped inform the expected pre-implementation, implementation, and maintenance outcomes and to develop a list of specific actions, referred to here as performance objectives (POs), that each potential implementer (e.g., clinic leader, SEMM champions, CHW, and health coach navigator) needs to perform at each of the implementation stages (see Tables 3.1–3.3). Direct feedback from the clinic staff confirmed that implementation and maintenance of the SEMM intervention as a standard practice would require the endorsement of clinic leadership and commitment of resources, including an emphasis on dedicated personnel time.
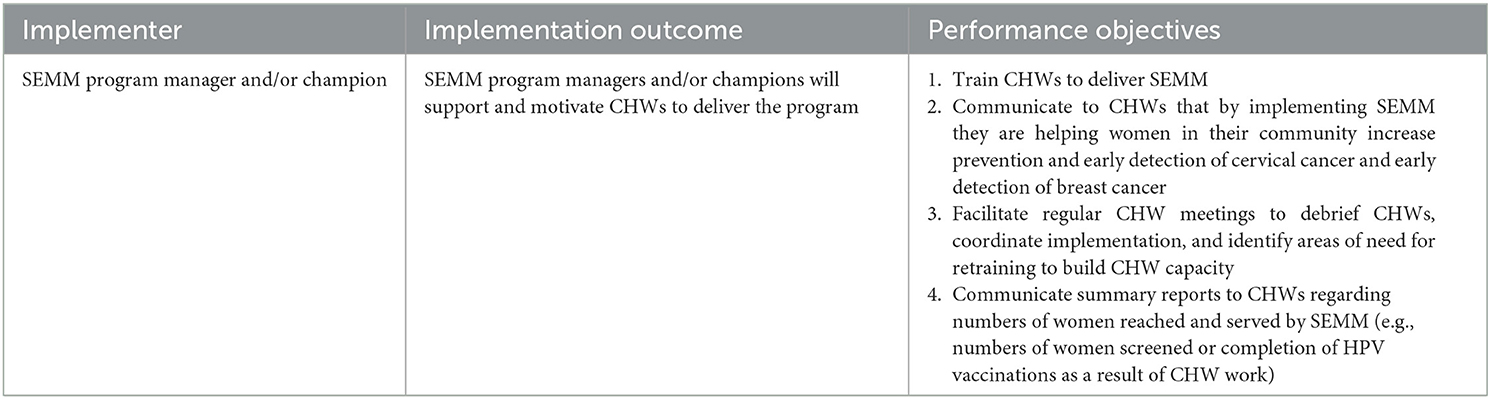
Table 3.2. Implementation outcomes and performance objectives: program manager/champion level (example).
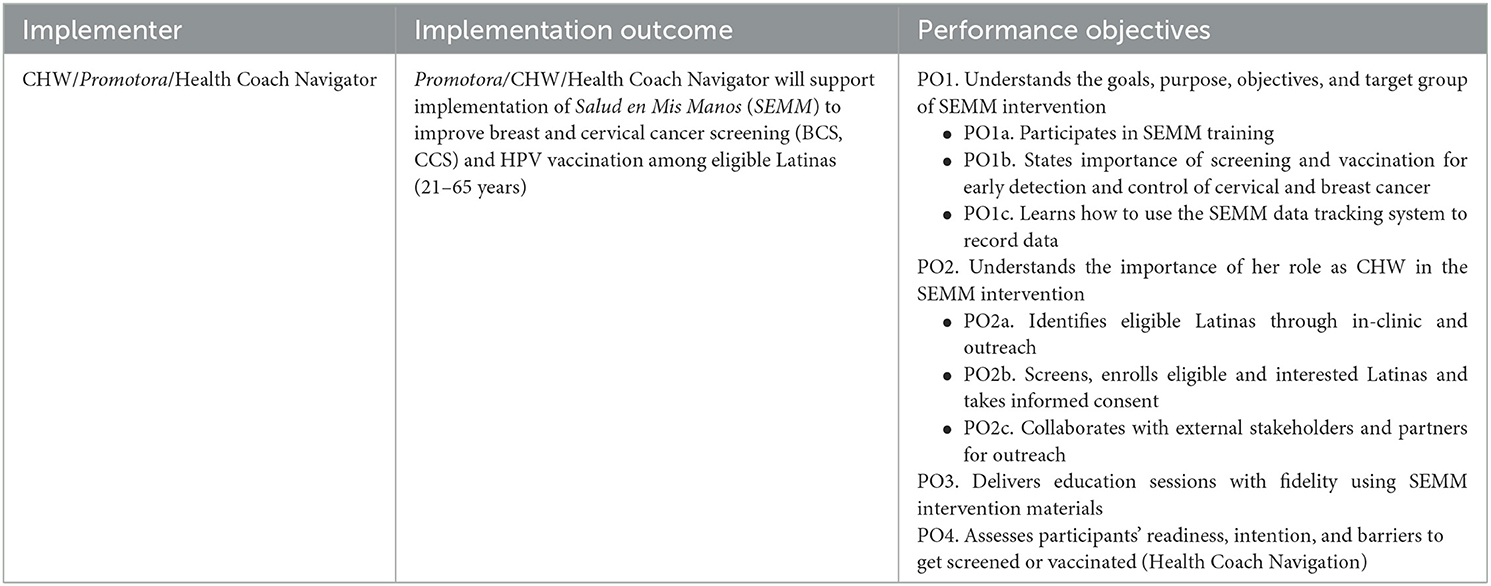
Table 3.3. Implementation outcomes and performance objectives: Promotora/CHW/Health Coach Navigator level (example).
Insights of research team members with previous and current experience managing implementation of the SEMM intervention were leveraged to help identify implementer-specific POs. For example, the POs of a designated manager related to providing guidance and support to CHWs, such as developing CHWs' clinic-based recruitment or community-based outreach plans. Other manager POs related to facilitating routine CHW meetings to address challenges and share successes, to provide continuous process monitoring to ensure CHWs reach under-screened or unvaccinated women most in need of the SEMM education and navigation support, and to sustain CHW motivation for the work.
Finally, the research team reviewed each implementer's POs and finalized the list of POs for clinic leaders, SEMM program managers and/or champions, and CHWs. Review of the POs by current intervention implementers led to the identification of missing and overlapping tasks. Tables 3.1–3.3 present examples of SEMM implementation and maintenance POs describing the specific actions for implementers (clinic leadership, SEMM program manager and/or champion, and CHWs). For the clinic leaders, for example, POs were identified by asking “What does the clinic leadership need to do to garner clinic Board of Directors' commitment of resources to support the program? What do clinic leaders need to do to plan the staffing to manage and deliver SEMM?”
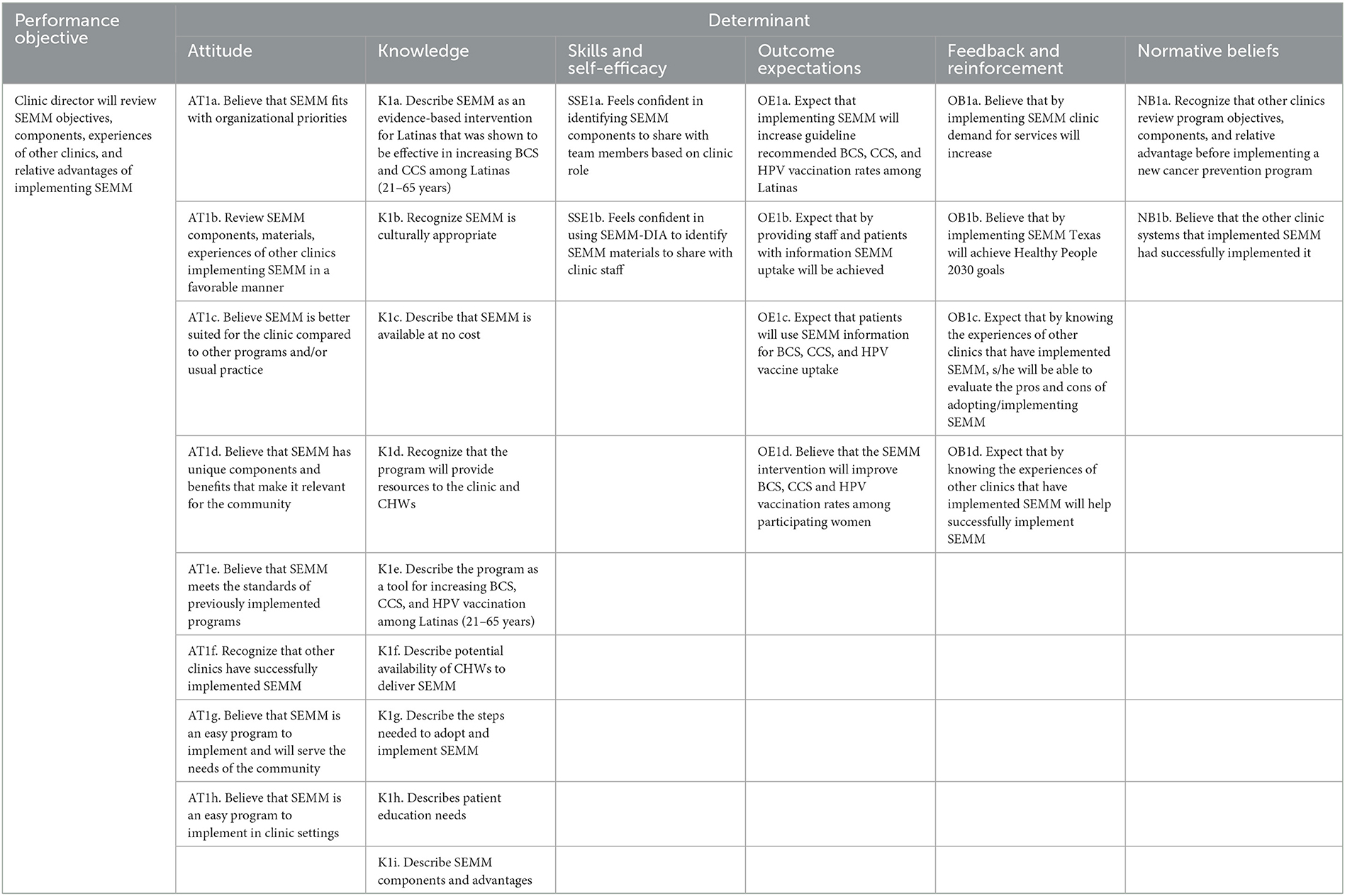
Next, the research team identified factors influencing implementation and developed the matrices of change objectives by crossing the selected behavioral and organizational determinants with identified performance objectives asking the question, “What needs to change for the implementers to accomplish the specific implementation performance objective?” The research team also considered behavioral science theories (e.g., SCT) and implementation science frameworks (e.g., ISF) in the identification of determinants and development of matrices of change (Table 4). For example, the ISF domain, “motivation,” guided the selection of specific attitudinal determinants expected to influence implementation and maintenance of the program. These included subconstructs, such as relative advantage, potential fit or compatibility, and the SEMM intervention's effectiveness in improving an important health problem prioritized by the clinic leadership (e.g., low cervical cancer screening rates and HPV vaccination rates). All ISF, and Readiness constructs from the R = MC2 heuristic (readiness= motivation × innovation specific capacity × general capacity) informed the types of implementers that may need to be involved to support implementation and deliver the program as well as the types of capacity needed for implementation to be successful (15). These matrices of change objectives served as the roadmap for designing the SEMM-DIA implementation strategies. Table 4 presents an example matrix for clinic leadership.
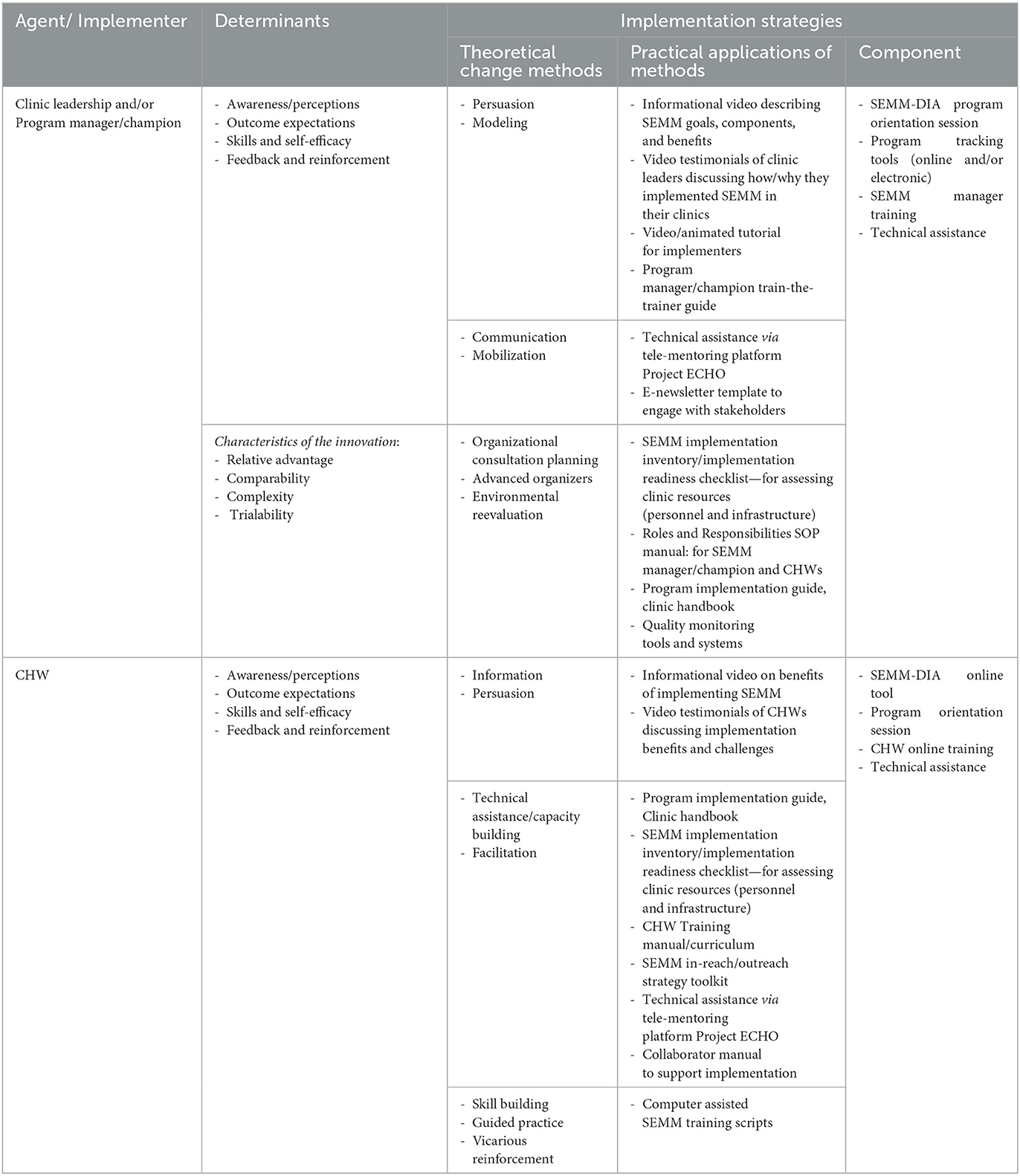
Task 3. Select theoretical methods and identify or design implementation strategies
The planning group selected evidence-based methods based on the targeted determinants and performance objectives, as well as informed by types of methods that have worked before to address identified implementation challenges (e.g., such as potential lack of motivation, capacity of staff to manage or deliver the program). For example, to address the potential skills and self-efficacy required of CHWs to implement SEMM, the team identified implementation strategies to target CHW training needs, targeting potential implementation threats (see Table 5). For example, the team identified the need to provide video testimonials of CHWs with previous experience implementing SEMM in their clinics. The research team would design the testimonial to show a CHW discussing how the SEMM training helped them to learn to deliver the intervention, and as a result, the implementer's satisfaction of seeing that their delivery of SEMM helped women they served to complete their breast and cervical cancer screenings, and HPV vaccinations. The previous implementers would also share their perspectives regarding the types of supporting materials and protocols (e.g., simple) that enabled CHWs to learn to deliver education and navigation support to patients. The testimonials also would include patients sharing their own positive experience with SEMM.
Based on their influence on determinants (e.g., attitudes, self-efficacy, and skills; see Table 4) and contextual factors, guided by SCT, the team identified behavioral change methods (e.g., modeling verbal persuasion, and communication). These methods were operationalized to guide adaptation of the existing CHW manager trainings. For example, CHW manager trainings included a train-the-trainer guide with step-by-step demonstrations of how to facilitate CHW peer learning (e.g., modeling). Trainings were adapted to build the CHW manager's capacity to supervise CHW delivery of SEMM, and to facilitate peer learning and peer support strategies during regular CHW team meetings. Empowerment and support of CHWs, managers and leadership were also addressed by planning testimonials based on positive experiences of previous program implementers who share benefits of promoting the intervention within their clinic systems (e.g., helping to meet performance measures for cervical cancer screening) and benefiting their communities by addressing high priority problems in vulnerable communities. The implementation support planning process, therefore, not only provided practical support (e.g., knowledge and resource transfer to potential users), but also included implementation strategies and theoretically informed methods to help address both implementation challenges and user-related determinants of implementation (e.g., capacity to deliver SEMM, outcome expectations that SEMM will help women they serve to complete screenings and HPV vaccinations, and motivation to implement the program).
Task 4. Produce implementation protocols and materials to guide intervention implementation
The fourth task of the Implementation Mapping process included designing the SEMM-DIA implementation strategy materials, protocols, and training. This involved describing the SEMM-DIA design document, creating the SEMM-DIA resource inventory, designing the SEMM-DIA website, and programming the SEMM-DIA website.
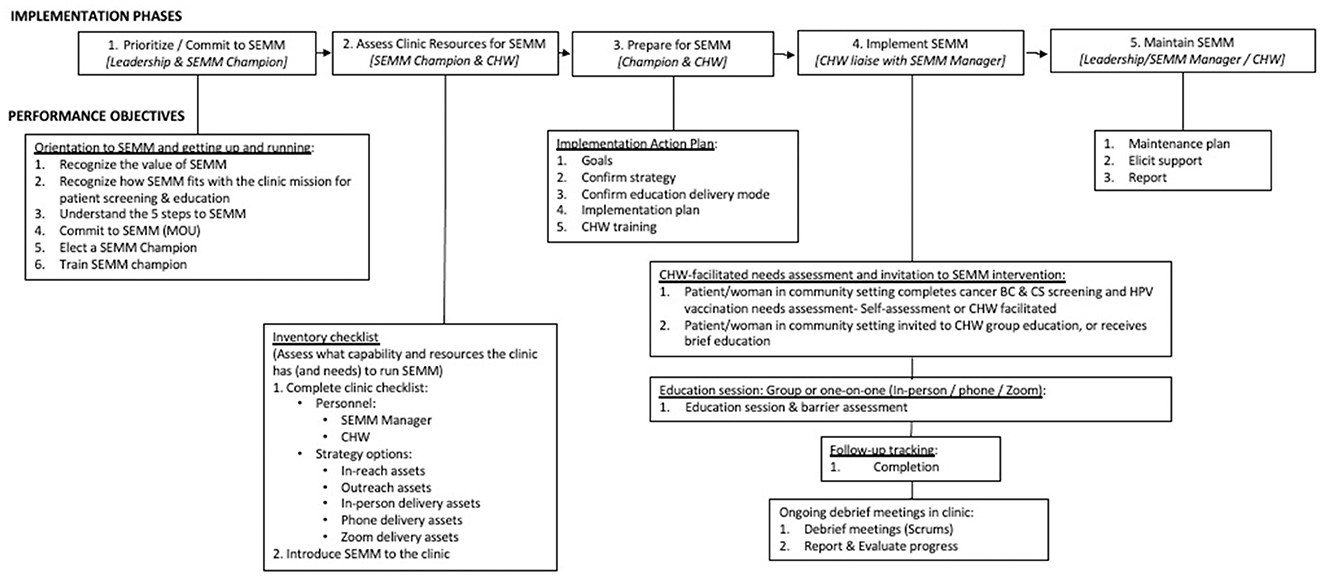
SEMM-DIA design document
SEMM-DIA is a multi-faceted multi-component implementation strategy. The SEMM-DIA design document was derived from the matrices of change objectives developed in Task 2 (Figure 2). It represents a top-level conceptualization of how SEMM-DIA functions. The performance objectives were ordered in a chronological sequence according to when they would occur during implementation (Table 6). On review, these performance objectives suggested a natural clustering that corresponded approximately to the Exploration, Preparation, Implementation, and Sustainment (EPIS) framework (14). This overriding “meta” implementation framework comprised five phases to support SEMM implementation and maintenance. These phases were (1) Exploration (prioritizing SEMM), (2) Preparation (assessing clinic readiness), (3) Preparation for implementation of SEMM, (4) Implementation, and (5) Sustainment (or maintenance). Each phase was associated with clinic personnel responsible for that phase (i.e., clinic leadership, SEMM champion, CHWs and health coach navigators).
The SEMM-DIA design document lists performance objectives embedded within this framework in thematic clusters representing: (1) Orientation; (2) Inventory checklist (for the implementer to assess delivery capacity and patient/community outreach needs); (3) Clinic Implementation Action Plan; (4) SEMM components: CHW-delivered education and referrals and health coach navigator-delivered barrier mitigation to help women overcome personal and system-level barriers to accessing and using clinic services; and (5) Maintenance planning (Figure 2). This provides a context for when the performance objective occurs within the SEMM-DIA implementation process. Each performance objective refers to resources that are required to complete the objective, represented as row numbers within the SEMM-DIA resource inventory.
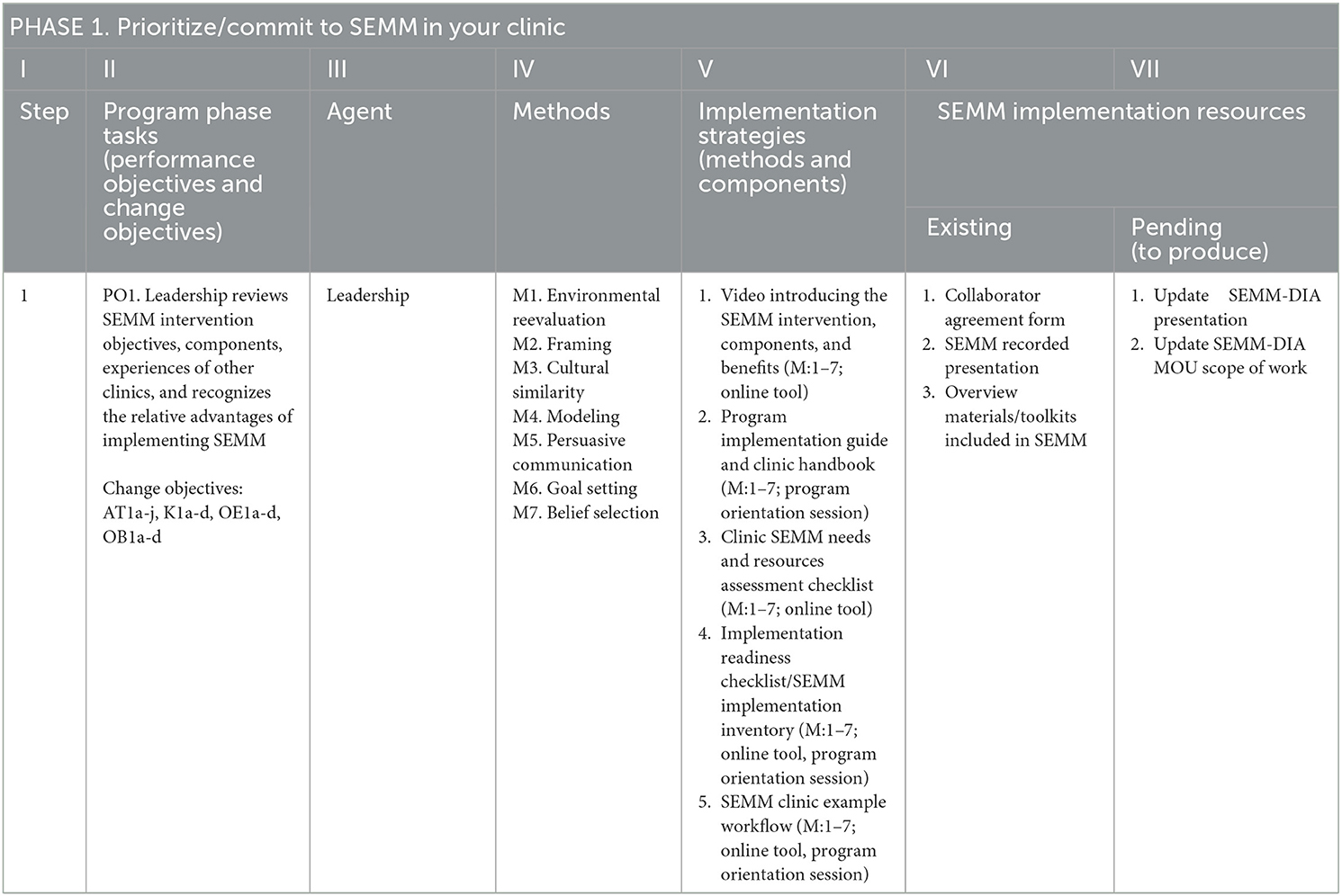
SEMM-DIA resource inventory
The SEMM-DIA resource inventory lists the resources that enable clinic personnel to complete each performance objective in SEMM-DIA (Table 6). The inventory provides information on the phase and performance objectives, agent (responsible clinic personnel), methods and strategies (from Step 3), and the SEMM implementation resources. The resources include written information about SEMM, a clinic inventory form to assess readiness for SEMM, a training curriculum for SEMM champions and CHWs, a template SEMM preparation plan, a CHW screening and tracking form, CHW patient and community awareness educational materials, and template maintenance plan (Figure 3). The resources are categorized as either “Existing” implementation resources (those implementation materials that had already been developed) that could be adopted or adapted, (such as CHW delivery guides) or as “Pending” resources (those in need of development; Table 6, Columns 6 and 7). This provides guidance on what pre-existing SEMM resources (again see Figure 3) could be leveraged in the SEMM-DIA development effort and to identify the extent of resource development required.
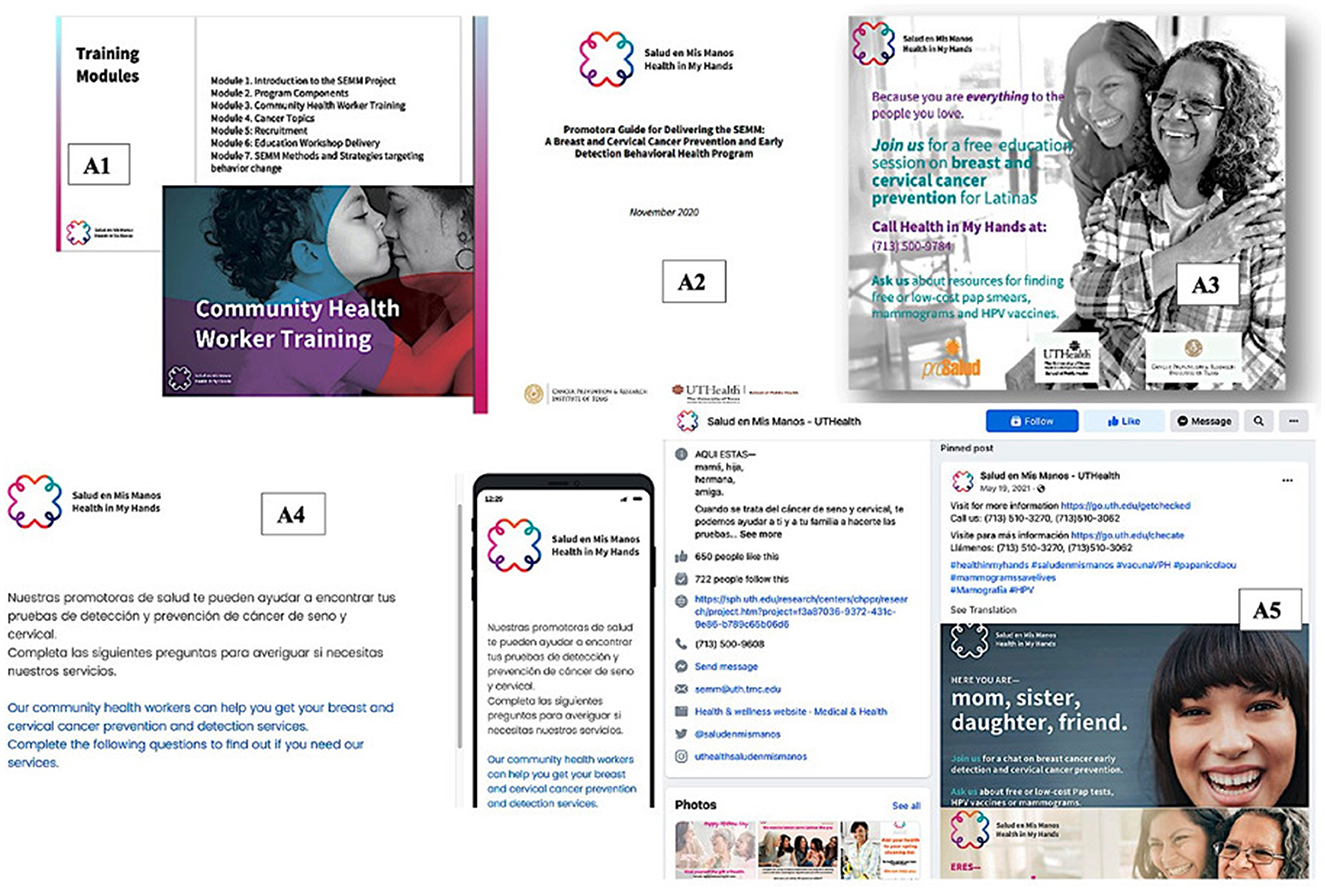
Figure 3. Sample of existing SEMM Resources to Support CHW Training, Community Outreach, and Recruitment to the SEMM Intervention: (A1) CHW Training Curriculum, (A2) CHW Guide for Delivering SEMM Education Intervention, (A3) SEMM Promotional Print Material, (A4) SEMM Participant Needs Assessment, and (A5) SEMM Social Media.
SEMM-DIA implementation support resources were designed to align with the varied implementation delivery goals, including if the priority for SEMM implementation was on “In-reach” (engaging existing patients within a clinic), or “out-reach” (engaging the broader community). Further materials, and tools were designed to facilitate varying delivery modalities including CHW-mediated one-on-one or group-based SEMM education and varying delivery channels including in-person, phone-based, or video-conference platforms.
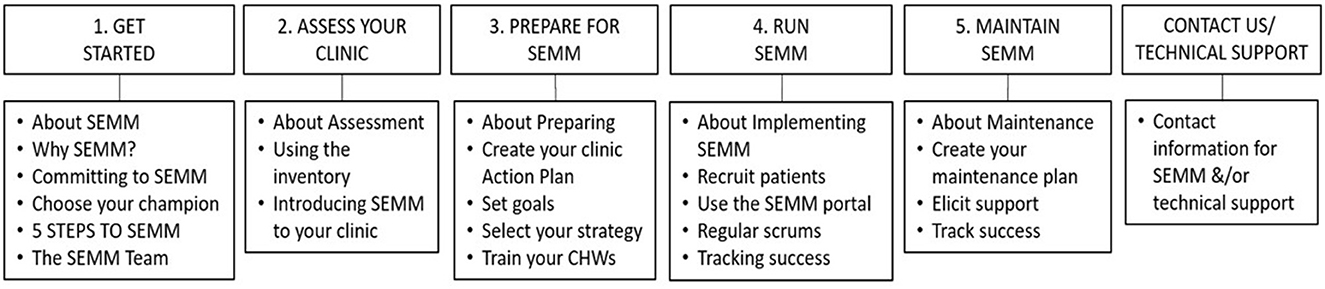
SEMM-DIA website design
The SEMM-DIA website was designed to be a multi-faceted multi-component implementation support strategy to guide planning and implementation of the SEMM EBI. A design document was developed to be the “blueprint” to guide construction of the SEMM-DIA website. The document was informed by the previous implementation planning tasks and describes the website's purpose and context, functional parameters (protocols, activities, and flow), design features, and resources (associated materials and assets to support adoption, implementation, and maintenance).
The SEMM-DIA website was designed as an asynchronous, easily accessible, and user-friendly online guide and reference to SEMM implementation. The website guidance was designed to support navigation through the “5 steps to SEMM” in accordance with the SEMM-DIA design document (Figure 4). Development was also informed by clinic staff's preference for a simple, form-based approach that could be easily integrated into CHW workflow. They preferred to be able to download needed forms for use in the clinic or community rather than use of mHealth or technology-dependent applications for real-time use with patients (e.g., electronic data collection surveys or decision support tools). Thus, to enable accomplishment of each step the website was designed to provide SEMM resources for download (e.g., pdf forms that are the core of the SEMM screening and education for CHWs to use as hardcopy versions) or streaming (e.g., testimonial videos) in a manner that provided context and rationale for use within the SEMM-DIA design document. The website was designed to accommodate the needs of relevant clinic stakeholders including clinic leadership, SEMM champions, and CHWs.
SEMM-DIA website programming
SEMM-DIA website programming was guided by the design document which provided the specifications previously described, priority audience (e.g., program adopters, SEMM champions, CHWs, or health coach navigators), scripts (e.g., for video testimonials planned for creation), and images (e.g., stock photos, or existing program photographs). In addition, a SEMM-DIA description, and specific instructions of each element in the SEMM-DIA plan, were provided to the SEMM-DIA website developers. This included the existing graphic design assets to retain the same look and feel of the original intervention design. Figure 3 provides a sample of the SEMM material design “look and feel,” as used in existing SEMM CHW training curriculum, recruitment, and community outreach materials.
The Implementation Mapping planning process helped incorporate guidance from theoretical frameworks and informed the design and content of all the SEMM-DIA implementation strategies, including the SEMM-DIA website, as well as technical assistance strategies such as an initial program orientation session with clinics (either in-person or virtually), the SEMM-DIA Project ECHO tele-mentoring series, and IMAdapt.org to support EBI and implementation strategy adaptation. These additional individual technical assistance strategies are accessible via the online SEMM-DIA website. The implementation strategies embedded within the SEMM-DIA website component are the ones highlighted in this paper.
Task 5. Evaluation the implementation outcomes
In Task 5, design of the evaluation plan focused on determining the effect of the SEMM-DIA implementation strategy on implementation outcomes, as well as the overall effectiveness of the SEMM intervention on increasing breast and cervical cancer screening and HPV vaccination rates. We will conduct a hybrid type 2 effectiveness-implementation group randomized trial to determine effectiveness and compare the effect of SEMM-DIA vs. Usual Implementation Practice (usual practice) on Reach, Effectiveness, Implementation, and Maintenance of SEMM, focusing on intentions to maintain SEMM due to the time constraints on evaluating long-term maintenance outcomes (25). These primary outcomes (four of the five RE-AIM dimensions) are defined in Table 7. A cost-effectiveness analysis to produce data on the economic details of SEMM-DIA implementation in clinic practice settings is planned as part of a future phase of this study.
To guide the overall evaluation, the planners articulated implementation evaluation questions to assess whether the SEMM-DIA implementation strategy influenced implementation determinants and outcomes such as fidelity of the SEMM implementation plan. Other implementation questions included whether SEMM-DIA was acceptable to the program implementers (e.g., implementer satisfaction), and did SEMM reach the priority implementers as planned. At the SEMM intervention level, process evaluation questions focused on whether each implementer delivered the intervention as planned (e.g., assessing fidelity of CHW implementation of SEMM), and whether the intervention reached the intended priority population (e.g., women overdue for breast and cervical cancer screenings, or HPV vaccination).
Implementation facilitators and barriers identified in Task 1 (needs and assets assessments) helped to identify potential mediators and moderators for the evaluation plan. In the selection of determinants and the development of matrices of change objectives, which focused on “what needs to change in the determinants (e.g., attitudes, skills, knowledge),” the research team had considered behavioral science theories, such as SCT. Consequently, the evaluation plan also selected measures to evaluate targeted individual-level constructs identified, such as to evaluate the effect of CHW training on implementers' knowledge, skills, self-efficacy, and outcome expectations.
In addition, implementation science frameworks (e.g., Integrated Systems Framework; ISF) that guided synthesis of the formative work conducted in Task 1, and informed implementation planning, consequently informed evaluation planning. Specifically, we identified the contextual factors of implementation to include in the evaluation plan at the organizational level, such as organizational readiness. Using the heuristic for organizational readiness—motivation × innovation-specific capacity × general capacity, (R = MC2) from ISF—we identified important constructs to include in the evaluation plan related to motivation (e.g., relative advantage, compatibility, complexity, priority), general capacity (e.g., culture, resource utilization, leadership, staff capacity), and innovation-specific capacity (e.g., knowledge/skills/abilities, program champion). Thus, the matrices developed in tasks 1–4 served as a road map to guide development of the evaluation plan.
Finally, the research team developed a logic model to provide a graphical representation of how strategies influence implementation and effectiveness of outcomes as part of the process for planning implementation strategies (Figure 5). This Implementation Mapping logic model illustrates the planned linkages between the implementation strategy, mechanisms, determinants of implementation, and proximal and distal implementation outcomes, thus helping describe the SEMM-DIA strategy's mechanisms of change. The logic model begins with the intervention (SEMM) on the far left and progresses to implementation strategies that deliver change methods. The research team designed these strategies to influence determinants, which in turn effect change in the implementation behaviors and conditions, leading to implementation.
This logic model thus helps to define our SEMM-DIA implementation outcomes as well as SEMM effectiveness outcomes (breast, cervical and HPV vaccination), to be examined in the planned hybrid type 2 study. The comprehensive SEMM-DIA implementation support plan facilitates implementation of the SEMM intervention as planned (increasing implementation fidelity) among a priority population in need of the program (increasing efficiency in reach, minimizing over-inclusion and under-inclusion of the target population). The logic model also represents how the plan results in an intervention that effectively increases breast and cervical cancer screening, and HPV vaccination among underserved Latinas. Finally, the logic model is especially useful for communicating both the evaluation outcomes, and the causal mechanisms of the SEMM implementation and evaluation plan to non-academic clinic or community partners.
Discussion
Effective and feasible implementation strategies are needed to increase the use of evidence-based cancer prevention and control interventions in community and health care settings. Implementation support is also needed to promote implementation with fidelity to retain effectiveness when EBIs are translated from research to practice. This paper described the use of Implementation Mapping to plan a multifaceted implementation strategy for the delivery of an effective breast and cervical cancer screening intervention targeting Latinas. The development of SEMM-DIA provides an opportunity to illustrate how Implementation Mapping can help implementation strategy planners use theory, evidence, and community engagement to inform strategy selection and tailoring. The use of Implementation Mapping also results in a logic model that presents a graphic depiction of the planned linkages between the implementation strategy, mechanisms, determinants of implementation and proximal and distal implementation outcomes, helping to describe the SEMM-DIA strategy's mechanisms of change.
A major strength of this work is that it provides a model for developing a multi-component, multi-level implementation support strategy to enable the implementation of a CHW delivered intervention in clinical settings (26, 27). CHW-delivered peer-to-peer behavioral interventions and patient navigation are recognized strategies to increase access to and utilization of preventive health care services, serving as effective approaches to increase parity for medically underserved ethnic and racial minorities (28–37). However, there are notable gaps in implementation and maintenance of such EBIs. The Implementation Mapping process used to plan SEMM-DIA provides a model to help identify common challenges to implementation and maintenance specific to CHW-delivered interventions, and provides an example for strategies selected, or designed, to address these CHW intervention-specific implementation challenges. Strategies identified may benefit other CHW-delivered interventions, these include: (1) provide online CHW training materials to help maintain continuity of the program when there is CHW turnover, (2) embed materials developed to promote the program to reduce difficulty accessing materials in a timely manner, and (3) provide CHW manager training materials, to develop manager capacity to deliver CHW training, and provide continuous support and motivation to CHWs (9, 28, 38).
Another major strength of this work is the integration of multiple stakeholders in the planning process, using a collaborative approach (39–43). Implementation Mapping includes, as a foundational principle, the integration of implementers, community partners and other interested parties in the strategy development process. This includes people with experience delivering and managing the SEMM intervention (or similar CHW interventions), as well as other stakeholders and implementers (e.g., clinic leaders at FQHCs, clinic managers, and CHWs working in clinic settings). The importance of integrating stakeholders with extensive experience delivering and managing SEMM-specifically also helped to identify potential problems future implementers might encounter, and thus helped develop and select needed implementation support strategies. The SEMM-DIA planning team members with extensive experience managing and delivering SEMM provided their perspectives to planning and design decisions, such as identifying existing protocols and materials and resources that proved successful in supporting implementation that were leveraged in the design of SEMM-DIA. By engaging stakeholders with different roles and from different clinic settings, we were able to develop relevant and feasible methods and strategies with consideration of multiple perspectives and contingencies, ensuring that the implementation strategies addressed the needs and resources of the different organizations and the communities they served. Thus, throughout the process, we provided tailored options within the implementation strategies to influence different determinants and performance objectives for different types of users. The approach helped maximize generalizability of the SEMM-DIA design to a variety of potential users, as well as to diverse clinic and environmental contexts.
A challenge to this collaborative approach was scheduling meetings with clinic leadership and health care providers who often have competing priorities (e.g., during this study, clinic stakeholders' time was limited due to the COVID-19 pandemic). We learned that conducting regular virtual meetings with CAB members was essential to ensure inclusion of community stakeholders' perspectives. In addition, we used an iterative engagement process, circling back to different stakeholders to integrate their insights and feedback at key decision points, enabling participation by clinic coordinators and CHWs during the intervention development process, but also cognizant of their limited time.
The existing SEMM-DIA strategy is primarily focused on implementation and maintenance. Since this project works with clinics who have already expressed some interest in SEMM, the strategy does not include a major focus on clinic leaders' initial decision to adopt SEMM. The research team focused on designing SEMM-DIA to support the pre-implementation phase following initial adoption, to ensure SEMM alignment with the clinic organization's goals and capacity, as well as to facilitate SEMM implementation within their clinic organization. This assumed that the clinic leadership had made a decision to adopt SEMM. Thus, we focused on developing implementation support for clinic leaders, managers and CHWs rather than on supporting leadership in a decision process to adopt SEMM. Future research is needed to examine the effect of the SEMM-DIA intervention on promoting adoption of SEMM as well as program maintenance. Further, because the implementation support system is designed as a multi-component multi-faceted implementation strategy, primarily within an online website, CHWs with limited technology skills may have difficulty accessing it, increasing reliance on SEMM CHW champions to provide SEMM-DIA resources to CHWs. Planned pilot testing of SEMM-DIA will help identify initial challenges, and pilot results will be used to identify solutions and further refine the implementation support strategies. Finally, ongoing evaluation will examine SEMM-DIA implementation outcomes, such as usability, feasibility, and acceptability, and SEMM intervention outcomes (e.g., completion of overdue breast and cervical cancer screenings, and HPV vaccination). To understand the degree of implementation, and degree of engagement with the SEMM-DIA dissemination and implementation support strategy, we will continuously monitor program implementation and stakeholder (clinic implementers) engagement. We will assess use of implementation materials and resources by clinic implementers through surveys and in-depth interviews. For the intervention group (SEMM-DIA study arm), we will also analyze implementers and decision makers' user data captured by SEMM-DIA (e.g., use, pathways, and Google Analytics), to examine the level of engagement with this implementation assistance. Because each clinic may use the SEMM-DIA implementation support differently (selecting elements that they decide will help their organization to implement SEMM effectively in their own clinic context and for the population they serve), there is not a predetermined “right” way to use SEMM-DIA. Therefore, in this study we will seek to identify potential mechanisms by which SEMM-DIA promotes fidelity in implementation outcomes and effectiveness of SEMM. Implementation monitoring and evaluation of the use of the implementation strategies will inform future adaptations of SEMM-DIA. Future SEMM-DIA implementation research will also include an implementation planning goal to develop and evaluate implementation strategies focused on supporting SEMM adoption, and will monitor maintenance over a longer period, to further improve widespread diffusion of SEMM.
In summary, we used Implementation Mapping to plan SEMM-DIA, a multifaceted implementation strategy (set of strategies). This paper describes the application of Implementation Mapping to develop implementation support strategies embedded in the SEMM-DIA website to serve as an example of how a systematic protocol can help apply theory and evidence for implementation strategy selection and development, describe the expected mechanisms of action of implementation strategies, and provide a framework for evaluation of implementation and effectiveness outcomes. Importantly, this approach integrates theory, empirical evidence, and EBI stakeholders' perspectives to develop relevant methods and implementation strategies, as well as to promote fidelity of implementation in the new adoption context. To promote implementation of evidence-based behavioral interventions into community practice, increased reporting of processes used to select and tailor and develop implementation strategies are needed. This paper begins to fill that gap (44).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MF, LS, and RS contributed to the conception and design of the study. LS, MF, PL, EA, CC, AA, and RS wrote sections of the first draft of the manuscript. LS, RC, and CC conducted interviews. CC and MA performed the qualitative analysis for the study's needs assessment. LS, EA, and MG summarized findings representing previous experience of SEMM implementers on the team. LS led final writing of the manuscript with substantive contributions from MF, RS, and CM. AA led final revision changes and responses to reviewers during the resubmission process and finalized all tables and figures. PL finalized all citations. LS and MF read and approved the final manuscript.
Funding
This publication was supported by the Centers for Disease Control (CDC) and Prevention, Health Promotion and Disease Prevention Research Center (Cooperative Agreement Number 1U48DP006408-01-00) and by the Cancer Prevention Research Institute of Texas (CPRIT): Salud en Mis Manos: Delivering Evidence-Based Breast & Cervical Cancer Prevention Services to Latinas in Underserved Texas South and Gulf Coast Communities (CPRIT Number PP190061).
Acknowledgments
Thank you to the members of our Texas Prevention Research Center Community Advisory Board for their guidance and support in developing SEMM-DIA.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control (CDC) and Prevention or the Cancer Prevention Research Institute of Texas.
References
1. Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health. (2012) 102:1274–81. doi: 10.2105/AJPH.2012.300755
2. Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. (2011) 104:510–20. doi: 10.1258/jrsm.2011.110180
3. World Health Organization. Nine Steps for Developing a Scaling-up Strategy. Geneva: World Health Organization (2010).
4. Peters DH, Tran NT, Adam T. Implementation Research in Health: A Practical Guide. Geneva: World Health Organization (2013).
5. Fernandez ME, Gonzales A, Tortolero G, Partida S, Bartholomew LK. Cultivando la Salud: a breast and cervical cancer screening program for Hispanic farmworker women. In:Bartholomew LK, Markham CM, Ruiter RA, Fernandez ME, Kok G, Parcel G, , editors. Planning Health Promotion Programs, 4th ed ed. San Francisco, CA: Jossey Bass (2016), p. 606–45.
6. Savas LS, Atkinson JS, Figueroa-Solis E, Valdes A, Morales P, Castle PE, et al. A lay health worker intervention to improve breast and cervical cancer screening among Latinas in El Paso, Texas: a randomized control trial. Prevent Med. (2021) 145:106446. doi: 10.1016/j.ypmed.2021.106446
7. Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. doi: 10.3389/fpubh.2019.00158
8. Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, et al. Annual report to the nation on the status of cancer, 1975-2009, featuring the burden and trends in human papillomavirus(HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. (2013) 105:175–201. doi: 10.1093/jnci/djs491
9. Fernandez ME, Gonzales A, Tortolero-Luna G, Williams J, Saavedra-Embesi M, Chan W, et al. Effectiveness of Cultivando la Salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am J Public Health. (2009) 99:936–43. doi: 10.2105/AJPH.2008.136713
10. Fernandez ME, Gonzales A, Tortolero G, Partida S, Bartholomew LK. Cultivando la Salud: a breast and cervical cancer screening program for Hispanic farmworker women. In:Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, , editors. Intervention Mapping: Designing Theory- and Evidence -Based Health Promotion Programs. San Francisco, CA: Jossey Bass (2006). p. 606–45.
11. Savas LS, Heredia NI, Coan SP, Fernandez ME. Outcome Evaluation of a Community Health Worker-Delivered Breast and Cervical Cancer Screening Intervention Targeting Low Income Hispanics. Advancing the Science of Cancer in Latinos. San Antonio, TX (2018).
12. Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. (1998) 13:623–49. doi: 10.1080/08870449808407422
13. Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. (2008) 41:171–81. doi: 10.1007/s10464-008-9174-z
14. Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implement Sci. (2019) 14:1. doi: 10.1186/s13012-018-0842-6
15. Scaccia JP, Cook BS, Lamont A, Wandersman A, Castellow J, Katz J, et al. A practical implementation science heuristic for organizational readiness: R= MC2. J Community Psychol. (2015) 43:484–501. doi: 10.1002/jcop.21698
16. Hamilton AB. Qualitative Methods in Rapid Turn-Around Health Services Research. National Cyberseminar Series: Spotlight on Women's Health. Washington, DC: US Department of Veterans Affair (VA) (2013).
17. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
18. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed. Thousand Oaks, CA: Sage Publications, Inc (1994), p. xiv, 338–xiv.
19. Charmaz K. ‘Discovering' chronic illness: using grounded theory. Soc Sci Med. (1990) 30:1161–72. doi: 10.1016/0277-9536(90)90256-R
20. Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Approaches, 2nd ed. Thousand Oaks, CA: Sage Publications, Inc (2007), p. xvii, 395–xvii.
21. Fernandez ME, Damschroder L, Balasubramanian B. Understanding barriers and facilitators for implementation across settings. In:Weiner BJ, Lewis CC, Sherr K, , editors. Practical Implementation Science. New York, NY: Springer Publishing Company (2022), p. 97–132. doi: 10.1891/9780826186935.0005
22. Ruiter RAC, Crutzen R. Core processes: how to use evidence, theories, and research in planning behavior change interventions. Front Public Health. (2020) 8:247. doi: 10.3389/fpubh.2020.00247
23. Kok G, Gottlieb NH, Peters GJ, Mullen PD, Parcel GS, Ruiter RA, et al. A taxonomy of behaviour change methods: an Intervention Mapping approach. Health Psychol Rev. (2016) 10:297–312. doi: 10.1080/17437199.2015.1077155
24. Bartholomew Eldredge LK, Markham CM, Kok G, Ruiter RA, Parcel GS, editors. Intervention Mapping Step 3: Program Design. San Francisco, CA: Jossey-Bass (2016).
25. Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. (2012) 50:217–26. doi: 10.1097/MLR.0b013e3182408812
26. Williams LB, Shelton BJ, Gomez ML, Al-Mrayat YD, Studts JL. Using implementation science to disseminate a lung cancer screening education intervention through community health workers. J Community Health. (2021) 46:165–73. doi: 10.1007/s10900-020-00864-2
27. Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev. (2013) 2013:Cd010414. doi: 10.1002/14651858.CD010414
28. Roland KB, Milliken EL, Rohan EA, DeGroff A, White S, Melillo S, et al. Use of community health workers and patient navigators to improve cancer outcomes among patients served by Federally Qualified Health Centers: a systematic literature review. Health Equity. (2017) 1:61–76. doi: 10.1089/heq.2017.0001
29. Acevedo-Polakovich ID, Niec LN, Barnet ML, Bell KM. Incorporating natural helpers to address service disparities for young children with conduct problems. Child Youth Serv Rev. (2013) 35:1463–7. doi: 10.1016/j.childyouth.2013.06.003
30. Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci. (2013) 1:170–91. doi: 10.1177/2167702612463566
31. Stacciarini JM, Rosa A, Ortiz M, Munari DB, Uicab G, Balam M. Promotoras in mental health: a review of English, Spanish, and Portuguese literature. Fam Community Health. (2012) 35:92–102. doi: 10.1097/FCH.0b013e3182464f65
32. Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. (1995) 3:19–30.
33. Freund KM, Battaglia TA, Calhoun E, Darnell JS, Dudley DJ, Fiscella K, et al. Impact of patient navigation on timely cancer care: the patient navigation research program. J Natl Cancer Inst. (2014) 106:dju115. doi: 10.1093/jnci/dju115
34. Jandorf L, Gutierrez Y, Lopez J, Christie J, Itzkowitz SH. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. (2005) 82:216–24. doi: 10.1093/jurban/jti046
35. Lasser KE, Murillo J, Lisboa S, Casimir AN, Valley-Shah L, Emmons KM, et al. Colorectal cancer screening among ethnically diverse, low-income patients: a randomized controlled trial. Arch Intern Med. (2011) 171:906–12. doi: 10.1001/archinternmed.2011.201
36. Robinson-White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: a systematic review. Cancer Nurs. (2010) 33:127–40. doi: 10.1097/NCC.0b013e3181c40401
37. Rodday AM, Parsons SK, Snyder F, Simon MA, Llanos AA, Warren-Mears V, et al. Impact of patient navigation in eliminating economic disparities in cancer care. Cancer. (2015) 121:4025–34. doi: 10.1002/cncr.29612
38. Barnett ML, Lau AS, Miranda J. Lay health worker involvement in evidence-based treatment delivery: a conceptual model to address disparities in care. AnnuRevClinPsychol. (2018) 14:185–208. doi: 10.1146/annurev-clinpsy-050817-084825
39. Cabassa LJ, Gomes AP, Meyreles Q, Capitelli L, Younge R, Dragatsi D, et al. Using the collaborative intervention planning framework to adapt a health-care manager intervention to a new population and provider group to improve the health of people with serious mental illness. Implement Sci. (2014) 9:178. doi: 10.1186/s13012-014-0178-9
40. Ramanadhan S, Davis MM, Armstrong R, Baquero B, Ko LK, Leng JC, et al. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control. (2018) 29:363–9. doi: 10.1007/s10552-018-1008-1
41. Blachman-Demner DR, Wiley TRA, Chambers DA. Fostering integrated approaches to dissemination and implementation and community engaged research. Transl Behav Med. (2017) 7:543–6. doi: 10.1007/s13142-017-0527-8
42. Hawe P. Lessons from complex interventions to improve health. Ann Rev Public Health. (2015) 36:307–23. doi: 10.1146/annurev-publhealth-031912-114421
43. Pinto RM, Park S, Miles R, Ong PN. Community engagement in dissemination and implementation models: a narrative review. Implement Res Pract. (2021) 2. doi: 10.1177/2633489520985305
Keywords: Implementation Mapping, implementation strategy, health equity, community health workers, cancer prevention, cervical screening, mammography, HPV vaccination
Citation: Savas LS, Loomba P, Shegog R, Alaniz A, Costa C, Adlparvar E, Allicock MA, Chenier R, Goetz M, Markham CM and Fernandez ME (2023) Using Implementation Mapping to increase uptake and use of Salud en Mis Manos: A breast and cervical cancer screening and HPV vaccination intervention for Latinas. Front. Public Health 11:966553. doi: 10.3389/fpubh.2023.966553
Received: 11 June 2022; Accepted: 20 February 2023;
Published: 15 March 2023.
Edited by:
Deanna Kepka, The University of Utah, United StatesReviewed by:
Colleen Barbero, Centers for Disease Control and Prevention (CDC), United StatesIsabel Roth, University of North Carolina at Chapel Hill, United States
Copyright © 2023 Savas, Loomba, Shegog, Alaniz, Costa, Adlparvar, Allicock, Chenier, Goetz, Markham and Fernandez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lara S. Savas, bGFyYS5zdGF1YkB1dGgudG1jLmVkdQ==
 Lara S. Savas
Lara S. Savas Preena Loomba1,2
Preena Loomba1,2 Ross Shegog
Ross Shegog Angelita Alaniz
Angelita Alaniz Crystal Costa
Crystal Costa Emily Adlparvar
Emily Adlparvar Roshanda Chenier
Roshanda Chenier Christine M. Markham
Christine M. Markham Maria E. Fernandez
Maria E. Fernandez