- 1School of Nursing and Midwifery, Trinity College Dublin, Dublin, Ireland
- 2Jishou University School of Medicine, Jishou, China
- 3Hunan University of Medicine General Hospital, Huaihua, China
Background: As the population ages, the proportion of chronic diseases becomes more prevalent. This study aimed to investigate the current status of chronic diseases among the older people in home care (HC) and long-term care facilities (LTCFs) in China and to analyze its influencing factors.
Methods: This cross-sectional study was conducted between 2021 and 2022. A multi-stage stratified random sampling and census sampling approach was used in this survey of the health of 389 older people in HC and 202 older people in LTCFs from Western Hunan, respectively. The following instruments were included in the survey “International Resident Assessment Instrument for Home Care (interRAI-HC)” and the “International Resident Assessment Instrument for Long-Term Care Facilities (interRAI-LTCF).” Univariate analysis was used to examine the prevalence of chronic diseases among older people with different characteristics. Data were analyzed by IBM SPSS version 25.0 software. A p-value of <0.05 was considered statistically significant.
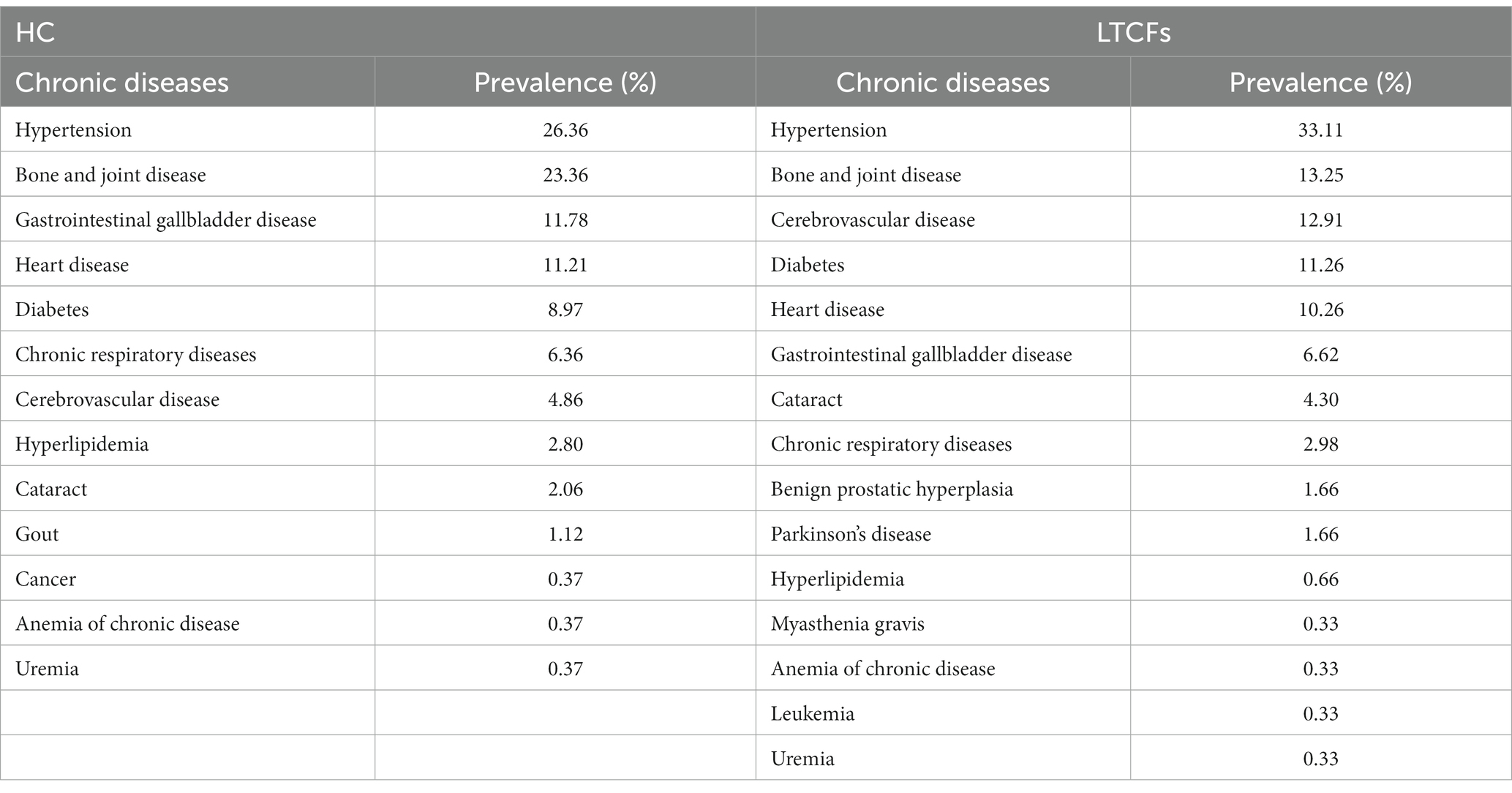
Results: The survey results showed that the prevalence of chronic diseases among older people in HC was 73.26% (95% CI, 68.85–77.68), and the top five chronic diseases were hypertension (26.36%), bone and joint disease (23.36%), gastrointestinal and gallbladder disease (11.78%), heart disease (11.21%), and diabetes (8.97%). The prevalence of chronic diseases among older people in LTCFs was 77.23% (95% CI, 77.23–83.06), and the top five chronic diseases were hypertension (33.11%), bone and joint disease (13.25%), cerebrovascular disease (12.91%), diabetes (11.26%), and heart disease (10.26%). The results showed that long time spent alone, having sleep disorders, and self-rated health status significantly increased HC in older people with the prevalence of chronic diseases (p < 0.05). Having marital status, non-healthy BMI, having sleep disorder, walking with the use of assistive devices, and self-rated health status significantly increased older people in LTCFs with the prevalence of chronic diseases (p < 0.05).
Conclusion: There are differences in the prevalence and distribution of chronic diseases among older people in two different aged care models in China, and there are various risk factors for chronic diseases. Therefore, chronic disease healthcare strategies should be tailored to two different aged care models for older people. Further summary found that older people in HC spend a lot of time alone and suffer from loneliness, which ultimately causes psychological disorders. Thus, psychological adaptation interventions are needed for older people in HC. Besides, older people in LTCFs lack social support from their families (divorced/widowed) and have activity disorders (walking with the use of assistive devices). Thus, social adaptation interventions are needed for older people in LTCFs. This study provides a theoretical basis for the distribution of healthcare and the prevention and treatment of chronic diseases in Chinese older people.
1 Introduction
Population aging is one of the major trends in socio-demographic development, and it has become a major public health issue in China. China has the largest older population in the world (1). The older population aged 60 years and above account for 18.70% (264 million) of the total population in 2021 (2) and will enter the stage of severe aging in 2035 (3). The sudden increase in the older population causes the fact that older people are not only the main group of people suffering from chronic diseases, but they are also the main people group dying as a result of chronic diseases. The World Health Organization reported that chronic diseases account for 73.60% of all deaths worldwide (4), and such deaths are mainly concentrated in developing countries (5). Therefore, there is an urgent need to reduce and delay the prevalence of chronic diseases among older people in China.
Nursing healthcare is an effective method for reducing and delaying the prevalence of chronic diseases in the older people. However, it is based on the theoretical premise of analyzing and obtaining the key influencing factors of chronic diseases. Thus, key influencing factors of chronic diseases are urgently needed to be studied. Studies showed that chronic diseases can be prevented and intervened as early as possible, thus increasing life expectancy and reducing the incidence of major chronic diseases (6, 7). Ranjbaran surveyed 734 patients with type 2 diabetes and found that determinants of diet (8) and medication (9) adherence could be identified based on the health action process approach. The intervention was further designed based on obtained determinants and was found to effectively improve the diet and medication adherence of patients (10). In addition, perceived social support can improve patients’ quality of life and overcome cardiovascular diseases (11). Moreover, intervention measures based on PRECED-PROCED model can effectively improve the sleep quality of patients after coronary artery bypass grafting (12). May reported that older people in Netherlands with healthy lifestyles live longer (13). Danaei and Stanaway reported that being physically active, maintaining a normal body weight, avoiding smoking, and drinking moderately reduce the risk of total mortality and chronic diseases (14, 15). In contrast, lack of exercise (16), unhealthy diet (17), smoking (18), excessive alcohol consumption (19), and obesity (20) increase the risk of chronic diseases.
To respond to the problem of the aging population and chronic diseases, the Chinese government is currently aiming to develop long-term care (LTC) on the basis of home care (HC). However, there is currently a lack of sufficient understanding of chronic diseases among older people in two different aged care models in China. Thus, this study aimed to explore the status of chronic diseases in older people in Chinese home care and long-term care facilities (LTCFs). Through a systematic investigation of the current status of chronic diseases among the older people under different aged care models, chronic disease influencing factor models were developed. This study provides theoretical guidance for the development of appropriate healthcare strategies for older people.
2 Methods
2.1 Study design and participants
This cross-sectional study was conducted between 2021 and 2022. The older people in HC was based on the number of older population (N = 13.21 million) drawn from the seventh national population census of Hunan Province (21), of which 192,096 were in the urban areas of Western Hunan. The confidence level and sampling error were set as 95 and 5%, respectively. Thus, the sample size is 385 in this survey study. Using a multi-stage stratified random sampling method, three cities were selected from Western Hunan, three streets were randomly selected from each of the sample cities (a total of nine streets), and one community was randomly selected from each sample street (total of nine communities). At last, 30–50 cases of older people in HC randomly selected from each sample community were surveyed.
A census sampling approach was used to investigate the health of older people aged 60 years (n = 202) in all long-term care facilities (n = 12) from urban areas of Western Hunan. (1) Inclusion criteria: age ≥ 60 years and agreement to participate. (2) Exclusion criteria: people who are unconscious or unable to communicate and leave HC and LTCFs during the research period. The study was approved by the Institutional Ethics Committee and the Biomedical Ethics Committee. Additionally, all respondents were informed of the study objectives and an informed consent was obtained. Therefore, the final sample consisted of 389 older people in HC and 202 older people in LTCFs.
2.2 Research methods
The following instruments were included in the survey “International Resident Assessment Instrument for Home Care (interRAI-HC)” and the “International Resident Assessment Instrument for Long-Term Care Facilities (interRAI-LTCF).” The interRAI-HC and interRAI-LTCF Assessment Scale includes basic information and several dimensions of assessment: cognition, communication and vision, psychosocial wellbeing, functional status, disease diagnosis, and health conditions. These scales have been widely used around the world in more than 40 countries and regions. Moreover, they have been used to evaluate the care needs and health problems of older people, with high reliability and validity (22–25).
After obtaining the consent of the respondents, surveyors conducted face-to-face interviews using paper questionnaires, assisted by institutional management, nursing staff, or family members. The questionnaires were collected on-site and reviewed by two surveyors in order to add missing items as soon as possible.
2.3 Statistical analysis
The data entry and statistical analysis were performed using IBM SPSS Statistics for Windows version 25.0 (IBM Corp., Armonk, NY, United States). The measured data are expressed as mean ± standard deviation. Count data are expressed as proportion ratios or rates and 95% confidence intervals. Univariate analysis will be used to examine whether there are differences in the prevalence of chronic diseases among older people with different characteristics. Logistic regression analysis will be used to analyze the factors influencing chronic diseases among older people. A p-value of <0.05 was considered statistically significant.
3 Results
3.1 Basic information
For older people in HC, the mean age was (69.4 ± 7.4) years. There was a higher proportion of males (57.33%) than that of females (42.67%). The presence of marital history (married/divorced/widowed) was the highest percentage (98.20%). In addition, there are varying degrees of functional impairment among the older people. Specifically, 59.13, 28.53, and 6.17% of the older people had abnormal vision, sleep disorders, and swallowing disorders, respectively. See Table 1.
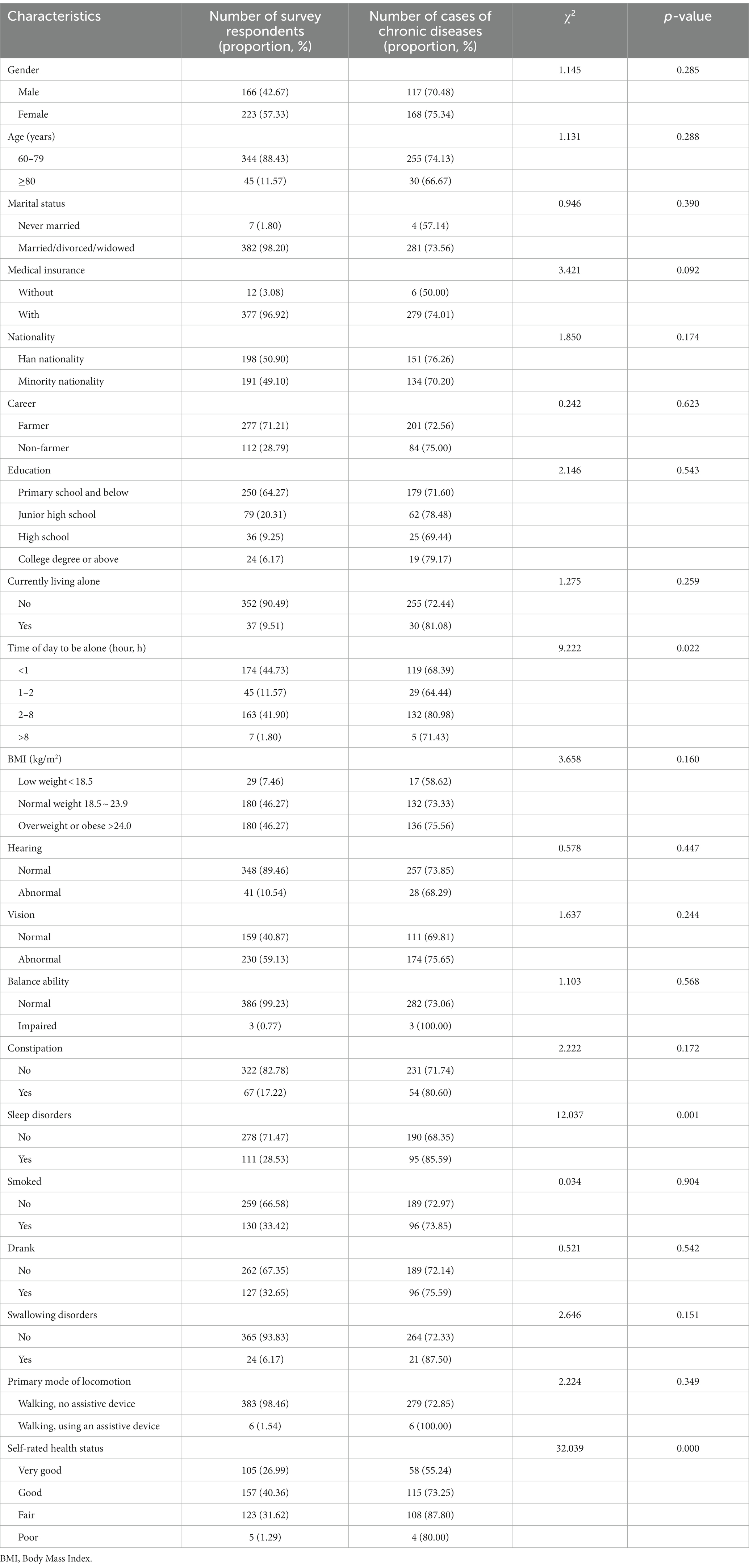
Table 1. The prevalence of chronic diseases among older people in HC with different characteristics.
For older people in LTCFs, the mean age was (79.1 ± 9.1) years. Its gender proportion was similar to that of HC. The majority of them are farmers (67.33%). The presence of marital history was the highest percentage (78.71%). Moreover, 67.82% of the older people had medical insurance. In addition, 35.64%, 55.45%, 47.52%, 37.62%, and 26.24% of older people had abnormal hearing, abnormal vision, impaired balance, sleep disorders, and swallowing disorders, respectively. See Table 2.
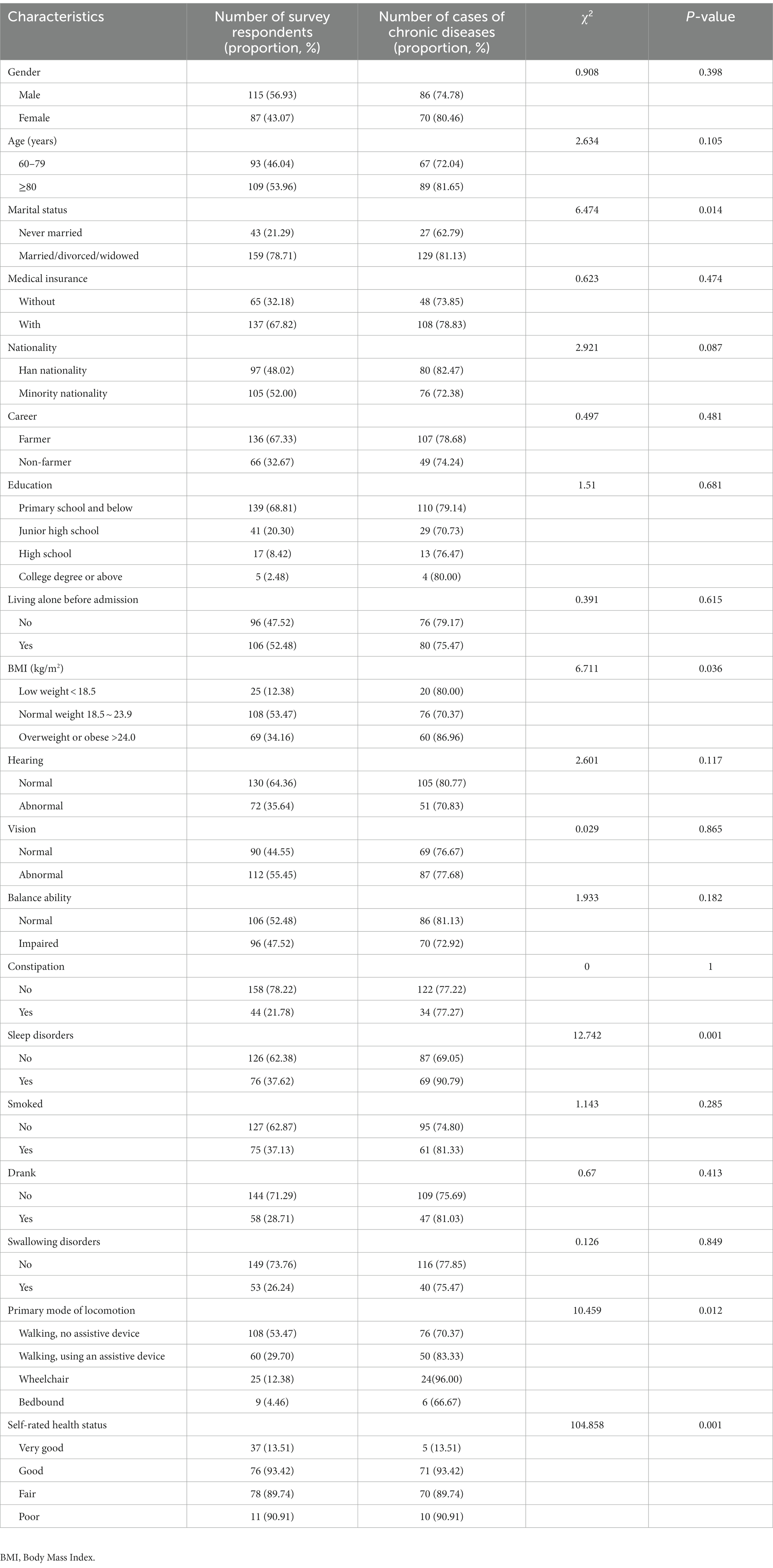
Table 2. The prevalence of chronic diseases among older people in LTCFs with different characteristics.
3.2 Current status of chronic diseases
The prevalence of chronic diseases among older people in HC was 73.26% (95% CI, 68.85–77.68), and 41.39% of older people suffered from two or more chronic diseases. The top five chronic diseases were hypertension (26.36%), bone and joint disease (23.36%), gastrointestinal and gallbladder disease (11.78%), heart disease (11.21%), and diabetes (8.97%). See Table 3.
The prevalence of chronic diseases among older people in LTCFs was 77.23% (95% CI, 77.23–83.06), and 43.56% of older people suffered from two or more chronic diseases. The top five chronic diseases were hypertension (33.11%), bone and joint disease (13.25%), cerebrovascular disease (12.91%), diabetes (11.26%), and heart disease (10.26%). See Table 3.
3.3 One-way analysis of variance
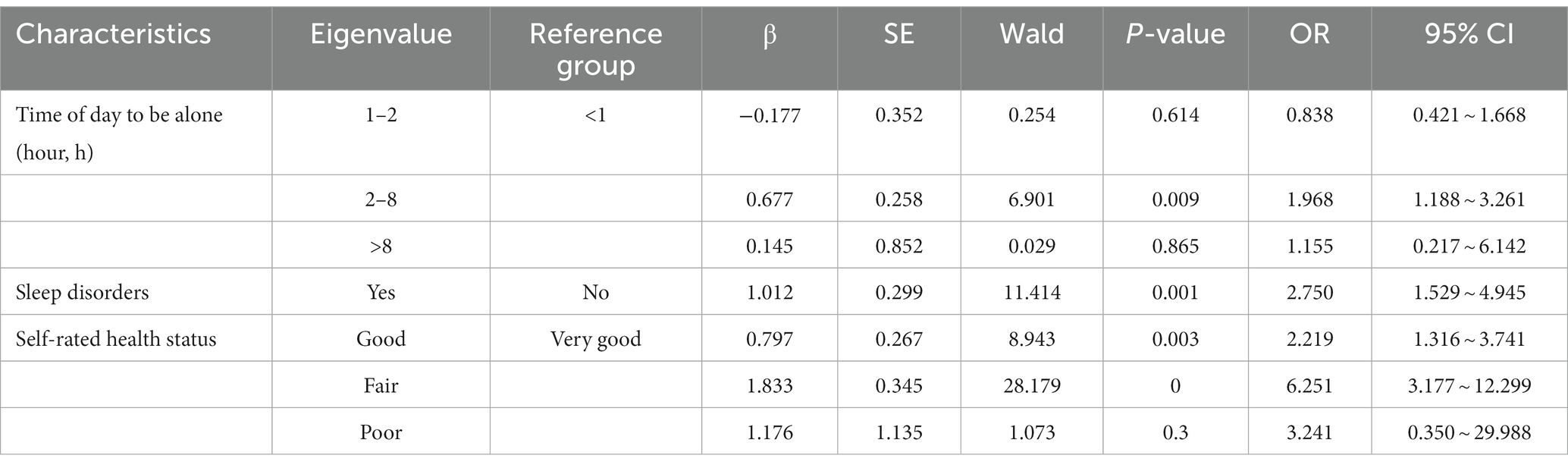
The results of the one-way analysis of variance showed that the time of day to be alone, sleep disorders, and self-rated health status of the older people in HC with chronic diseases were statistically significant (p < 0.05). See Table 1.
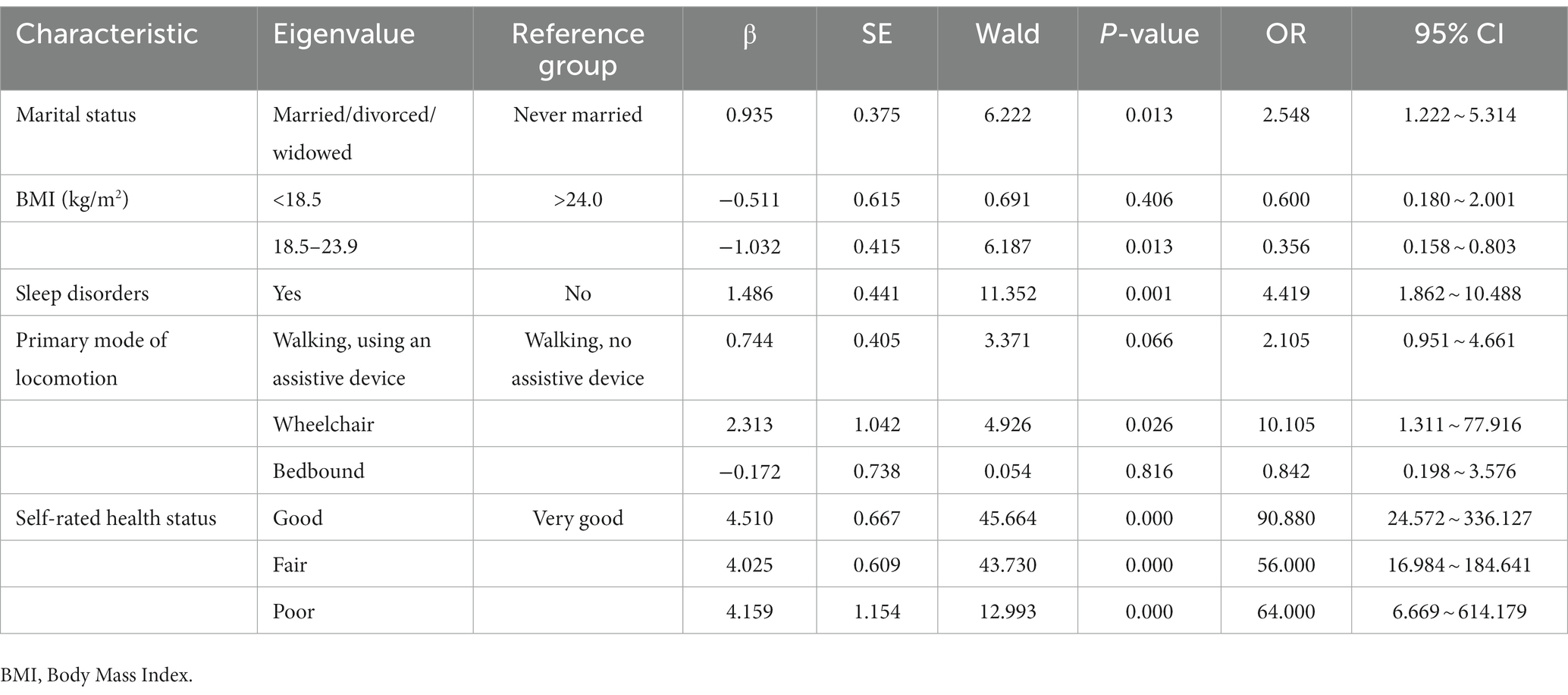
For the older people in LTCFs with chronic diseases, it showed that the marital status, BMI, sleep disorders, primary mode of locomotion, and self-rated health status of the older people in LTCFs with chronic diseases were statistically significant (p < 0.05). See Table 2.
3.4 Chronic disease influencing factor model
Chronic disease influencing factor models are developed based on the above investigation and logistic regression analysis. For the older people in HC with chronic diseases, it shows that long time spent alone, having sleep disorders, and self-rated health status significantly increased the prevalence of chronic diseases (p < 0.05). As older people spend more time alone throughout the day, their risk of chronic diseases increases more significantly. The prevalence of chronic diseases in older people who spend 2–8 h and > 8 h alone are 1.968 and 1.155 times than that of those who spend <1 h alone. The prevalence of chronic diseases in older people with sleep disorders is 2.750 times than that of those without sleep disorders. Besides, the prevalence of older people who have good, fair, and poor self-rated health status are 2.219, 6.251, and 3.241 times than that of those who have very good self-rated health status. See Table 4.
For the older people in LTCFs with chronic diseases, it shows that having marital status, non-healthy BMI, having sleep disorder, walking with the use of assistive devices, and self-rated health status significantly increased their prevalence (p < 0.05). The prevalence of chronic diseases of older people who are married/divorced/widowed is 2.548 times than that of those who have never been married. Furthermore, the risk of chronic diseases in older people also increases as BMI decreases, reaching a level of 0.600 times. The prevalence of chronic diseases in older people with sleep disorders is 4.419 times than that of those without sleep disorders. Among the primary modes of locomotion, the prevalence of chronic diseases of older people who walk with the use of assistive devices and wheelchairs are 2.105 and 10.105 times than that of those who walk without assistive devices. Besides, the prevalence of older people who have good, fair, and poor self-rated health status are 90.880, 56.000, and 64.000 times than that of those who have very good self-rated health status. See Table 5.
4 Discussion
In this study, the prevalence of chronic diseases among older people in HC and LTCFs was higher than 70.00%. This is significantly higher than that of developed countries, such as the United States (60.00%) (26), Germany (62.10%) (27), and Australia (66.30%) (28), and lower than that of in six low- and middle-income countries (80.59%) (29). These results demonstrate that the prevalence of chronic diseases is higher in low-income and middle-income countries than in developed countries (30). This is the result of complex social, economic, and behavioral factors at different development levels in various countries (31). In these two different aged care models, hypertension, bone and joint disease, heart disease, and diabetes were the most prevalent chronic diseases among older people in HC and LTCFs. Bone and joint diseases are caused by the mountainous areas where part of the respondents reside (32).
The prevention and treatment of chronic diseases in older people are more important to pay attention to risk factors because of the shortage of medical and care resources in China. In this study, one-way analysis of variance shows that the time of day to be alone, sleep disorders, and self-rated health status were the main risk influences on the prevalence of chronic diseases among older people in HC vs. marital status, BMI, sleep disorders, primary mode of locomotion, and self-rated health status for older people in LTCFs. People who are married/divorced/widowed are more likely to suffer from chronic diseases than those who have never been married, which is due to the heavy family and social responsibilities of older people with a marriage history (33–35). In addition, Qian (36) found that older people who sleep long at night and do not sleep during the day are more likely to suffer from diabetes. In this study, the association between sleep disorders and chronic disease is further confirmed, with sleep disorders significantly increasing the prevalence of chronic disease in older people. Besides, high prevalence of chronic diseases in older people who walk with the use of assistive devices and spend extensive periods alone. This is attributed to the decline of physiological functions as a result of aging in older people, causing them to exercise less and increasing their risk of developing chronic diseases (37). Besides, their long time alone and limited family support cause them more risk of chronic illnesses, both physically and mentally (38, 39).
The above studies prove that HC and LTCFs have different risk factors for chronic diseases in older people. Thus, older people under different aged care models need to propose corresponding healthcare strategies based on their characteristics. Further summary found that older people in HC spend a lot of time alone and then suffer from loneliness, which ultimately causes psychological disorders. Thus, psychological adaptation interventions are needed for older people in HC, such as psychotherapy, psychological counseling, psychological crisis intervention, and so on. Besides, older people in LTCFs lack social support from their families (divorced/widowed) and have activity disorders (walking with the use of assistive devices). Thus, social adaptation interventions are needed for older people in LTCFs, such as health education, changing poor lifestyles, providing social support, and so on. The above healthcare strategies are obtained through the chronic disease influencing factor model. This care strategy not only improves the quality of life of older people in two different aged care models but also optimizes the distribution of care resources between the two different aged care models.
This study used a cross-sectional study, which is one of the best ways to measure the prevalence of health outcomes and can study the associations between multiple exposures and outcomes (40). Nevertheless, it has some limitations. The cross-sectional study design limited the ability to infer causal relationships from the findings. Furthermore, cohort studies are required to determine causal relationships. Second, as the data are self-reported, they may influence participants’ responses and lead them to overestimate their abilities. In future studies, more objective indicators should be added.
5 Conclusion
There are differences in the prevalence and distribution of chronic diseases among older people in two different aged care models in China. Moreover, there are various risk factors for chronic diseases. Therefore, chronic disease healthcare strategies should be tailored to two different aged care models for older people. Further summary found that older people in HC spend a lot of time alone and suffer from loneliness, which ultimately causes psychological disorders. Thus, psychological adaptation interventions are needed for older people in HC. Besides, older people in LTCFs lack social support from their families (divorced/widowed) and have activity disorders (walking with the use of assistive devices). Thus, social adaptation interventions are needed for older people in LTCFs. This study provides a theoretical basis for the distribution of healthcare and the prevention and treatment of chronic diseases in Chinese older people. It also can be considered as a starting point for further care needs and intervention research studies in chronic diseases among older people.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by Biomedical Ethics Committee of Jishou University (JSDX-2021-0027). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
FX: Funding acquisition, Writing – original draft, Writing – review & editing. QS: Formal analysis, Investigation, Writing – review & editing. JL: Funding acquisition, Investigation, Writing – review & editing. Z-yC: Formal analysis, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Hunan Provincial Social Science Fund (21YBA129) and the Hunan Provincial Innovation Foundation for Postgraduate (CX20211063). The funders had no direct role in the design, data collection, analysis, interpretation, or writing of the manuscript.
Acknowledgments
The authors thank the interRAI for their suggestions and help in this research and for the valuable support and cooperation of the respondents and family members, as well as LTCF managers and nursing staff.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Office for the coordination of humanitarian affairs. Global age watch index 2015, insight report. Available at: https://reliefweb.int/report/world/global-agewatch-index-2015-insight-report (Accessed September 9, 2015).
2. The central people's government of the People's Republic of China. The seventh national population census. Available at: http://www.gov.cn/xinwen/2021-05/11/content_5605760.htm (Accessed May 11, 2021).
3. National health commission of the People's Republic of China. Transcript of the 20 September 2022 press conference by the national health commission. Available at: http://www.nhc.gov.cn/xcs/s3574/202209/ee4dc20368b440a49d270a228f5b0ac1 (Accessed September 20, 2022).
4. World Health Organization. World health statistics 2021: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization (2021).
6. Li, Y, Schoufour, J, Wang, DD, Dhana, K, Pan, A, Liu, X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ. (2020) 368:l6669. doi: 10.1136/bmj.m456
7. Nyberg, ST, Singh-Manoux, A, Pentti, J, Madsen, IE, Sabia, S, Alfredsson, L, et al. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern Med. (2020) 180:760–8. doi: 10.1001/jamainternmed.2020.0618
8. Ranjbaran, S, Shojaeizadeh, D, Dehdari, T, Yaseri, M, and Shakibazadeh, E. Using health action process approach to determine diet adherence among patients with type 2 diabetes. J Educ Health Promot. (2020) 9:170. doi: 10.4103/jehp.jehp_175_20
9. Ranjbaran, S, Shojaeizadeh, D, Dehdari, T, Yaseri, M, and Shakibazadeh, E. Determinants of medication adherence among Iranian patients with type 2 diabetes: an application of health action process approach. Heliyon. (2020) 6:e04442. doi: 10.1016/j.heliyon.2020.e04442
10. Ranjbaran, S, Shojaeizadeh, D, Dehdari, T, Yaseri, M, and Shakibazadeh, E. The effectiveness of an intervention designed based on health action process approach on diet and medication adherence among patients with type 2 diabetes: a randomized controlled trial. Diabetol Metab Syndr. (2022) 14:1–10. doi: 10.1186/s13098-021-00773-x
11. Chollou, KM, Shirzadi, S, Pourrazavi, S, Babazadeh, T, and Ranjbaran, S. The role of perceived social support on quality of life in people with cardiovascular diseases. Ethiop J Health Sci. (2022) 32:1019–26. doi: 10.4314/ejhs.v32i5.17
12. Ranjbaran, S, Dehdari, T, Sadeghniiat-Haghighi, K, and Majdabadi, MM. Poor sleep quality in patients after coronary artery bypass graft surgery: an intervention study using the PRECEDE-PROCEED model. JTHC. (2015) 10:1–8.
13. May, AM, Struijk, EA, Fransen, HP, Onland-Moret, NC, de Wit, GA, Boer, JM, et al. The impact of a healthy lifestyle on disability-adjusted life years: a prospective cohort study. BMC Med. (2015) 13:1–9. doi: 10.1186/s12916-015-0287-6
14. Danaei, G, Ding, EL, Mozaffarian, D, Taylor, B, Rehm, J, Murray, CJ, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. (2009) 6:e1000058. doi: 10.1371/journal.pmed.1000058
15. Stanaway, JD, Afshin, A, Gakidou, E, Lim, SS, Abate, D, Abate, KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
16. Ding, D, Lawson, KD, Kolbe-Alexander, TL, Finkelstein, EA, Katzmarzyk, PT, Van Mechelen, W, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet. (2016) 388:1311–24. doi: 10.1016/S0140-6736(16)30383-X
17. He, Y, Li, Y, Yang, X, Hemler, EC, Fang, Y, Zhao, L, et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol. (2019) 7:540–8. doi: 10.1016/S2213-8587(19)30152-4
18. Zhou, M, Wang, H, Zeng, X, Yin, P, Zhu, J, Chen, W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
19. Wise, J. Large study is “robust” evidence of link between chronic heavy drinking and dementia. BMJ. (2018) 360:k814. doi: 10.1136/bmj.k1308
20. Barrett-Connor, EL. Obesity, atherosclerosis, and coronary artery disease. Ann Intern Med. (1985) 103:1010–9. doi: 10.7326/0003-4819-103-6-1010
21. Hunan Provincial Bureau of Statistics. The seventh national population census of Hunan province. Available at: http://tjj.hunan.gov.cn/hntj/wzzl/hnsdqcqgrkpc/qrptzgg/202105/t20210519_19054787.html (Accessed May 19, 2021).
22. Hirdes, JP, Ljunggren, G, Morris, JN, Frijters, DH, Soveri, HF, Gray, L, et al. Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res. (2008) 8:1–11. doi: 10.1186/1472-6963-8-277
23. Kim, H, Jung, YI, Sung, M, Lee, JY, Yoon, JY, and Yoon, JL. Reliability of the interRAI long term care facilities (LTCF) and interRAI home care (HC). Geriatr Gerontol Int. (2015) 15:220–8. doi: 10.1111/ggi.12330
24. Morris, JN, Berg, K, Bjorkgren, M, Costa, AP, Declercq, A, Finne-Soveri, UH, et al. InterRAI long-term care facilities (LTCF) assessment form and user's manual : Washington, DC: Australian Edition (2011), 25–30.
25. Liu, Y, Zhang, S, Chen, P, Feng, D, Tian, J, and Wang, X. Application of interRAI HC to analyze health issues and related caring needs among Chinese community-dwelling elders. Chin Nurs Manag. (2016) 16:1448–52. doi: 10.3969/j.issn.1672-1756.2016.11.003
26. Centers for Disease Control and Prevention. Chronic diseases in America (2019). Available at: https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm (Accessed April 15, 2019).
27. Puth, M-T, Weckbecker, K, Schmid, M, and Münster, E. Prevalence of multimorbidity in Germany: impact of age and educational level in a cross-sectional study on 19,294 adults. BMC Public Health. (2017) 17:826. doi: 10.1186/s12889-017-4833-3
28. Harrison, C, Britt, H, Miller, G, and Henderson, J. Prevalence of chronic conditions in Australia. PLoS One. (2013) 8:e67494. doi: 10.1371/journal.pone.0067494
29. Vancampfort, D, Stubbs, B, and Koyanagi, A. Physical chronic conditions, multimorbidity and sedentary behavior amongst middle-aged and older adults in six low-and middle-income countries. Int J Behav Nutr Phys Act. (2017) 14:1–13. doi: 10.1186/s12966-017-0602-z
30. World Health Organization. Preventing chronic diseases: a vital investment. Public Health Agency of Canada. Geneva: World Health Organization (2005).
31. Banatvala, N, and Donaldson, L. Chronic diseases in developing countries. Lancet. (2007) 370:2076–8. doi: 10.1016/S0140-6736(07)61877-7
32. Xie, F, Li, J, Song, W, Liu, Q, Jiang, S, Chen, Z-Y, et al. Long-term care facility and its elderly chronic diseases in Jishou: insights into underdeveloped area of China. Inquiry. (2022) 59:00469580221128735. doi: 10.1177/00469580221128735
33. Gong, CH, Kendig, H, and He, X. Factors predicting health services use among older people in China: an analysis of the China health and retirement longitudinal study 2013. BMC Health Serv Res. (2016) 16:63. doi: 10.1186/s12913-016-1307-8
34. Abukhdeir, HF, Caplan, LS, Reese, L, and Alema-Mensah, E. Factors affecting the prevalence of chronic diseases in Palestinian people: an analysis of data from the Palestinian Central Bureau of Statistics. East Mediterr Health J. (2013) 19:307–13.
35. Brennan-Olsen, SL, Cook, S, Leech, MT, and Bowe, SJ. Prevalence of arthritis according to age, sex and socioeconomic status in six low and middle income countries: analysis of data from the World Health Organization study on global AGEing and adult health (SAGE) wave 1. BMC Musculoskelet Disord. (2017) 18:1–12. doi: 10.1186/s12891-017-1624-z
36. Zhang, S, Xie, L, Yu, H, Zhang, W, and Qian, B. Association between nighttime-daytime sleep patterns and chronic diseases in Chinese elderly population: a community-based cross-sectional study. BMC Geriatr. (2019) 19:1–10. doi: 10.1186/s12877-019-1136-9
37. Feng, K, Pu, X, Tang, G, Tang, X, and He, Z. Prevalence and influencing factors of common chronic diseases among the elderly in Chongqing. Chinese Health Service Management. (2018) 35:713.
38. Kharicha, K, Iliffe, S, Harari, D, Swift, C, Gillmann, G, and Stuck, AE. Health risk appraisal in older people 1: are older people living alone an ‘at-risk’ group? Br J Gen Pract. (2007) 57:271–6.
39. McInnis, GJ, and White, JH. A phenomenological exploration of loneliness in the older adult. Arch Psychiatr Nurs. (2001) 15:128–39. doi: 10.1053/apnu.2001.23751
Keywords: older people, home care, long term care facilities, chronic disease, influencing factors
Citation: Xie F, Shu Q, Li J and Chen Z-y (2023) An exploration of status of chronic diseases and its influencing factors of older people in Chinese home care and long-term care facilities: a cross-sectional study. Front. Public Health. 11:1321681. doi: 10.3389/fpubh.2023.1321681
Edited by:
Giuseppe Caminiti, Università telematica San Raffaele, ItalyReviewed by:
Soheila Ranjbaran, Sarab Faculty of Medical Sciences, IranDaisy Volmer, University of Tartu, Estonia
Sup Amornpinyo, Khon Kaen University, Thailand
Copyright © 2023 Xie, Shu, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingxia Shu, MjUxMjg2ODQzMkBxcS5jb20=; Jinxiu Li, MjQwNzY3Nzk1OEBxcS5jb20=
 Fen Xie
Fen Xie Qingxia Shu
Qingxia Shu Jinxiu Li
Jinxiu Li Zheng-ying Chen2
Zheng-ying Chen2