- 1Nelson R Mandela School of Clinical Medicine, University of KwaZulu-Natal, Durban, South Africa
- 2School of Health Sciences, University of Kwazulu-Natal, Durban, South Africa
The COVID-19 pandemic, triggered by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), rapidly became a worldwide emergency. How it was managed garnered both commendation and vehement censure. This crisis profoundly affected healthcare, the economy, education, and public confidence in scientific endeavors. Our primary aim was to scrutinize the shortcomings in the pandemic management and to articulate a more effective strategy for handling prospective pandemics. We delved into the errors encountered in the COVID-19 response and posited a holistic, evidence-grounded approach for future pandemic mitigation.
Introduction
In March 2020, the World Health Organization declared COVID-19 a global pandemic (1, 2). As of July 2023, there were 768 million reported cases and approximately 6.95 million COVID-19 fatalities (3). Subsequent waves, driven by variants such as Omicron, have further complicated an already uncertain situation, (4) as there was a growing concern about the potential diminished efficacy of vaccines (5).
Evaluating the global endeavors to contain the virus is paramount, informing future strategies and commemorating effective actions learned from past experiences. While regulatory bodies and public health experts have celebrated various interventions as successful, thoroughly examining their limitations is essential for enhancing future pandemic preparedness. Both governmental agencies and healthcare organizations must meticulously review their responses to formulate more effective public health policies.
A critical analysis encompassing a range of interventions and their subsequent outcomes, spanning health-related and economic dimensions, promises invaluable insights. Such an assessment can serve as a roadmap for optimizing future crisis response strategies and reducing the likelihood of repeating past mistakes. This paper briefly surveys the lessons that should have been drawn from previous respiratory virus pandemics. We then delve into the numerous deficiencies observed in our response to the COVID-19 pandemic, offering recommendations for a forward-looking approach that emphasizes a shift in pandemic response leadership from a clinician-centric model to a multidisciplinary one.
What we have learned from previous flu pandemics
Over the last century and beyond, pandemics such as the Spanish flu (1918), (6) SARS-Cov-1 in 2003 (7) and the Middle East respiratory syndrome (MERS) in 2012 (8) have occurred. However, SARS-Cov-1 and MERS were transmitted largely through close contacts (9–11) and these pandemics were relatively less severe. Spanish flu and COVID-19 are also spreaded via airborne transmission (12, 13).
Although SARS-Covid-1 is also transmitted via airborne particles, it appears not enough studies have been done to determine the exact mechanism for airborne transmission (14). COVID-19 (SARS-Co2-2) transmission in aeroplanes is similar to that of the influenza A(H1N1)virus, in that transmission occurs mainly via a short-range airborne route.
The reproductive number (R) for the Spanish Flu (15) was in a similar range to that of COVID-19 (16–19), although the 1918 pandemic was significantly more deadly, given that post-World War I, food shortages resulted in malnutrition and a lack of vitamin C, and antibiotics such as penicillin had not yet been discovered that could have controlled some secondary infections that proved to be lethal.
The 1918 influenza pandemic, caused by the H1N1 virus, provides valuable insights relevant to managing the COVID-19 pandemic. Markel et al. (20) demonstrated the profound impact of early intervention by comparing the disparate mortality rates in Philadelphia and St. Louis, each adopting different timelines for public health measures. St. Louis’s swift actions significantly reduced mortality, highlighting the importance of timely, decisive public health initiatives.
Moon (21) supported this observation, indicating that countries acting promptly before infection numbers surged achieved more favorable outcomes during the COVID-19 outbreak. The delayed pandemic declaration by the World Health Organization had adverse effects on early-affected countries, underscoring the critical role of timely action in public health crises.
The 1918 pandemic underscored the necessity of a robust public health infrastructure encompassing adequate staffing, medical equipment, and protective supplies. Nevertheless, many healthcare systems faced shortages of personal protective equipment and medical personnel during the COVID-19 pandemic, revealing gaps in pandemic preparedness.
Hobday and Cason (22) referenced the experience of Brooks Hospital near Boston to illustrate the potential benefits of open-air treatment, which resulted in lower mortality rates during the 1918 pandemic. While not universally applicable, this approach leverages natural light and improved ventilation, which could have been considered complementary to traditional healthcare settings during the COVID-19 pandemic.
The 1918 influenza pandemic imparts crucial lessons on early intervention, developing a resilient public health infrastructure, and exploring alternative treatment methods. These insights could have played a pivotal role in devising more effective strategies for managing the COVID-19 pandemic.
Assessing the mistakes
A reflective examination of past deficiencies offers valuable insights into significant weaknesses within the healthcare system, particularly in preparedness, resource allocation, and communication. Strategic allocation of resources to address these identified areas holds the promise of bolstering resilience and fortifying capabilities for improved crisis management in subsequent instances. In the interest of conciseness, our attention will be directed toward the more contentious aspects of the COVID-19 pandemic.
Reflecting on lockdowns
Lockdowns have emerged as a contentious yet often effective measure in controlling infectious diseases (23, 24). While some research underscores their efficacy, other studies advocate for a more nuanced strategy that considers factors such as timing and scale (25, 26). Notably, the broad application of lockdowns has come under scrutiny, particularly in the context of airborne diseases (27–29).
From an economic perspective, the consequences of stringent lockdowns have been substantial, resulting in business closures, job losses, and a global recession (30–32). In the United States, the estimated cost per prevented infection was $28,000, significantly impacting GDP (33).
Lockdowns also had notable repercussions on education and healthcare systems. These measures exacerbated educational inequalities, (34) and delays in non-COVID medical treatments were prevalent (35). The healthcare sector faced strains, particularly in terms of shortages in supplies and personnel, disproportionately affecting vulnerable communities (36). The interruption of educational activities impacted the quality and accessibility of learning, particularly in under-resourced regions (37).
Considering the social and economic trade-offs associated with lockdowns, a more nuanced, context-specific approach is imperative for future pandemic management. This approach should encompass financial assistance, mental health support, and targeted public health interventions. For instance, strategies effective in essential sectors, such as reducing public transport occupancy, could be adapted to other sectors to alleviate economic pressures. Telemedicine holds promise as an alternative for healthcare delivery. The psychological impact of lockdowns, particularly on vulnerable populations, should not be underestimated. Interventions such as open-air visits may help mitigate some of these emotional costs (38). The approach to social distancing and lockdown measures requires a balanced consideration of multiple factors, encompassing public health, economic, and psychological well-being.
Although some assert the effectiveness of cloth face masks in preventing the airborne transmission of COVID-19, (39, 40) multiple studies have found them to be ineffective in this regard (41–46) and have highlighted adverse effects associated with prolonged usage.
The regrettable outcome of this resulted in a deviation from established pandemic protocols, wherein fear was disseminated, fostering an unscientific perspective that characterized individuals as bio-hazards.
Reflecting on cigarette and alcohol bans
The approach to social distancing and lockdown measures requires a balanced consideration of multiple factors, encompassing public health, economic, and psychological well-being (47). However, these bans encountered criticism due to their perceived lack of well-founded rationale, especially given that existing lockdown protocols already restricted social interactions.
Several factors, including concerns about compromised immune systems and the potential for viral transmission through shared cigarettes, influenced the decision to prohibit the sale of these products. In South Africa, implementing such a policy led to cultural reactions, including the creation of a widely circulated parody song (48).
From a financial perspective, these bans had notable repercussions. Substantial revenue losses were observed, including foregone sin taxes, value-added taxes, and related income. Furthermore, illicit markets emerged for these banned items, exacerbating public health risks due to the poor quality and potential toxicity of the products. The bans also unintentionally gave rise to health issues, such as withdrawal symptoms and associated mental distress, for which sufficient addiction management support was often lacking.
An alternative strategy could have focused on educational initiatives aimed at informing the public about the specific health risks associated with smoking and alcohol consumption during the pandemic. Given that existing lockdown measures and restrictions on social gatherings were already in place to address many of the issues targeted by the substance bans, a more nuanced approach, incorporating public education, might have offered a more effective and less detrimental solution.
Reflecting on alternative treatment strategies and the misinterpretation of evidence-based medicine
In the first year of the COVID-19 pandemic, healthcare professionals explored various treatment options using repurposed drugs. By December 2020, a body of literature had emerged, comprising in vitro studies, case series, and observational research, which collectively suggested the potential efficacy of these drugs in treatment protocols. However, with the introduction of vaccines at the end of 2020, a media campaign arose that largely discredited the use of therapeutics. This campaign cited the absence of large randomized controlled trials (RCTs) and dismissed existing literature as lacking in quality.
Over decades, medical education has perpetuated the notion that research not conforming to the RCT framework is of inferior quality. The evidence-based medicine (EBM) pyramid concept has contributed to this perception, implying that research quality progresses linearly from observational studies at the base to meta-analyses at the apex. However, this presents a misleading viewpoint, as the pyramid primarily signifies increasing certainty levels, not necessarily research quality. Moreover, it neglects significant categories of research, including in silico, in vitro, and in vivo studies.
To rectify this misconception, Aldous et al. (49) introduced an alternative model known as the T-EBM Wheel. This model offers a more nuanced and adaptable framework for evaluating various forms of evidence, particularly valuable in the early phases of pandemics. Unlike the conventional EBM pyramid, which emphasizes a hierarchical structure, the T-EBM Wheel provides a more practical guide for clinicians and policymakers. It is important to note that the T-EBM Wheel builds upon the principles of the traditional hierarchical model and, as such, complements this established method.
This innovative model argues for a departure from traditional hierarchical models, advocating for an inclusive approach that accommodates multiple forms of evidence and embraces real-world clinical observations. In particular, it facilitates the exploration of repurposed drugs in pandemic contexts, potentially offering effective early treatment alternatives.
Reflecting on the lack of diverse thinking
The response to the COVID-19 pandemic has laid bare deficiencies in leadership and policy-making, notably regarding the limited diversity within decision-making groups. Initially, the global response was predominantly orchestrated by clinicians and bolstered by government officials. This narrow focus overlooked valuable contributions from social scientists, economists, legal specialists, and pure scientists, resulting in a restricted range of solutions and insufficient consideration of the broader societal impacts. It is essential to acknowledge that the importance of early involvement of Public Health specialists during a pandemic is not in dispute.
The proliferation of misinformation in the media and information blackouts due to government censorship (50–56) stifled dissenting scientific voices. This clinician-centric approach failed to account for diverse community needs, economic factors, and broader human rights concerns. For example, the initial emphasis on medical interventions like testing and vaccines failed to consider the social and economic repercussions. Vulnerable, low-income communities with limited access to healthcare were disproportionately affected. As circumstances evolved and trust eroded, it became evident that leadership needed to adopt a more comprehensive perspective.
The ivermectin (IVM)-Wheel introduced by Aldous et al. (49) illustrates that by 2022, there were discernible positive indications of efficacy evident across all categories of reports. Statistically positive findings could have provided valuable insights for using IVM-based treatment protocols. The positive results and inconclusive findings with positive signals could have served as foundational information for developing new IVM-based treatment strategies. Conversely, negative results would have indicated areas of treatment regimens requiring modification or avoidance.
Even flawed studies could have offered insights into aspects of treatment protocols that warranted cautious consideration. In cases where positive findings contradicted negative conclusions, such discrepancies could have pointed to components of treatment protocols that yielded positive effects.
The use of an IVM T-EBM Wheel (e.g., Figure 1) by decision-makers in the early stages of the pandemic could have played a pivotal role in expediting the mitigation of COVID-19. This underscores the importance of incorporating such frameworks into future pandemic response strategies.
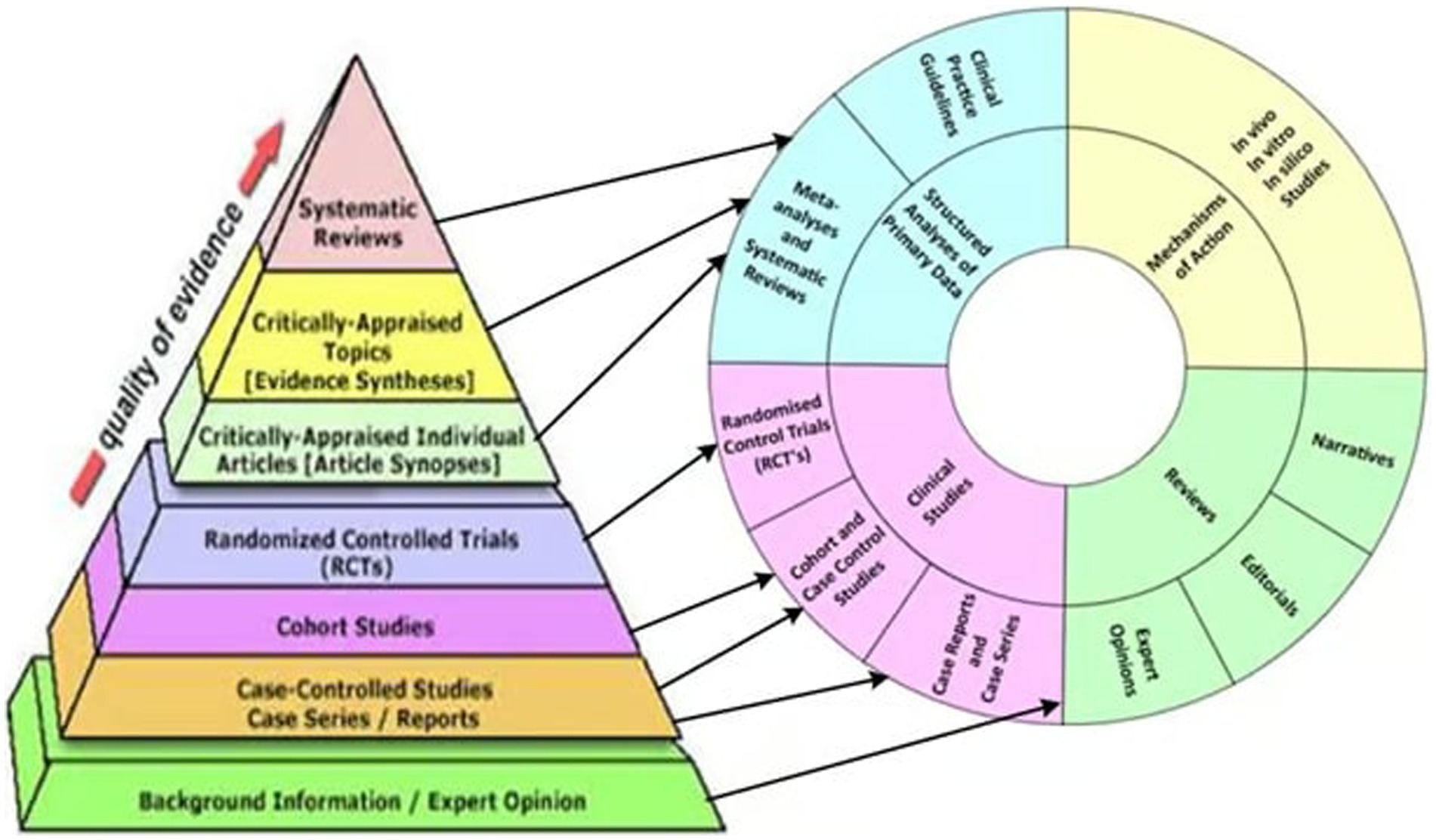
Figure 1. Correspondence of traditional evidence-based medicine pyramid with the two inner rings of the T-EBM wheel. Arrows show correspondences between levels of the pyramid and sections of the rings.
For a more effective and equitable pandemic response, diverse disciplines must be included:
1. Social Scientists: They bring insights into human behavior, social dynamics, and cultural influences, which can improve the effectiveness of public health measures like vaccine distribution and adherence to safety protocols.
2. Legal Experts: They can guide the legal frameworks essential for a pandemic response, ensuring that measures are constitutionally sound and respect individual liberties.
3. Economists: They can assess the economic impact of interventions and recommend strategies to mitigate economic damage while ensuring equitable response.
4. Pure Scientists contribute to understanding the virus at a fundamental level, providing data that can inform public health policies and potential treatment or vaccination strategies.
5. Multidisciplinary Approach: Including experts from finance, health, humanities, and legal fields would lead to a more holistic understanding and effective control measures.
In the face of future pandemics, global leadership should make a concerted effort to prioritize diversity of thought. This entails actively seeking diverse perspectives, which will, in turn, develop more comprehensive strategies. These strategies should encompass enhanced health communication tailored to meet the diverse needs of various communities and the implementation of nuanced workplace safety measures.
Embracing a multidisciplinary approach is pivotal in achieving a more effective and inclusive response. Such an approach would be instrumental in addressing the multifaceted challenges of pandemics, spanning medical, social, legal, and economic dimensions. By incorporating a wide range of expertise and viewpoints, global leadership can better navigate the complexities of future crises and devise solutions that cater to the diverse array of challenges that pandemics invariably bring forth.
Holistic management
Alan Savory’s Holistic Management principles, applied globally in agriculture and conservation for over 40 years, have effectively balanced economic, social, and environmental elements (57–59). The emergence of the COVID-19 pandemic sparked discussions on adapting these principles for comprehensive pandemic management (60). Moreover, the literature indicates a broader trend shifting from reductionist to holistic models in various fields, including economics, health, and environmental management (61–64). General Stanley McChrystal emphasized the inadequacy of reductionist leadership in modern organizations (65).
This proposal put forth that future pandemics should be addressed holistically. In this approach, multidisciplinary advisory panels would seek optimal solutions that consider economic, social, and environmental factors related to the pathogen. Any proposed intervention would undergo analysis in terms of its advantages and disadvantages concerning these three critical dimensions. It is evident that the approach taken during the COVID-19 pandemic exhibited shortcomings in terms of economics, (66, 67) social aspects (30, 68) and the environmental context of the virus. For instance, isolating older adult individuals indoors instead of allowing them outdoor exposure had devastating effects (69).
Early evidence, including findings from the Diamond Princess outbreak, indicated that a significant majority of individuals (>85%) were asymptomatic to the virus (12, 70, 71). It is now known that asymptomatic individuals are less infectious than initially reported (72, 73). Despite such data, strict lockdowns were enforced globally, neglecting the potential for more nuanced strategies. As demonstrated during the 1918 Spanish flu pandemic, the impact of early intervention is crucial (20). In some instances, like South Africa, stringent lockdowns failed to contain the virus due to the widespread use of minibus taxis (74). By March 2022, over 98% of the South African population had been exposed to COVID-19 (75). In contrast, Sweden’s more balanced approach, (76, 77) resulted in better outcomes to those observed in the UK, which also opted for a hard lockdown (78).
Herein we argued that censoring dissenting views are counter productive. A prominent example of a dissenting voice from during COVID-19 is that of Dr. David Martin whose views were portrayed as outlandish. Although we are neutral about his claims, it remains to be seen to what extent the revelations by Dr. David Martin about the origin and handling of the COVID-19 pandemic hold true (79).
Conclusion
Centralized decision-making during the pandemic, primarily led by select scientists (pandem-icons) who self-appointed as the sole voices of reason, resulted in a narrow, reductionist approach. This approach neglected critical factors, such as economic and social impacts, ultimately leading to suboptimal outcomes (80). The absence of multidisciplinary advisory panels perpetuated these limitations at considerable costs (30, 81).
Concerns have emerged regarding legal immunities granted to vaccine manufacturers by global governments and entities like the WHO, raising questions about the potential for expedited processes at the expense of safety (82, 83). Even though the WHO officially declared the end of the pandemic on May 5th, 2023, there is still a need for a broader discussion on the extent of governmental influence. To address these issues, it is recommended to establish multidisciplinary pandemic advisory panels rooted in Holistic Management principles. The adoption of the “Totality of Evidence-Based Medicine (T-EBM) Wheel” approach (49) aims to provide a nuanced understanding of various factors, promoting more inclusive strategies.
Looking ahead, fostering transdisciplinarity, robust debates, and transparent collaboration is crucial. Societies worldwide are encouraged to actively engage in discussions that delineate the boundaries of governmental power, fostering a collaborative effort to chart a pathway characterized by informed choices. This approach seeks to secure our civil liberties and collective well-being. Our collective responsibility should aim to develop evidence-based and holistic responses to pandemics, aligning with a commitment to global well-being and preparedness for future challenges.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CA: Conceptualization, Writing – review & editing. HK: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank UKZN and NRF for funding. HK thank Alan Savory for introducing us to the concept of Holistic management during a workshop in 2021.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cruickshank, M, and Shaban, RZ. COVID-19: lessons to be learnt from a once-in-a-century global pandemic. J Clin Nurs. (2020) 29:3901–4. doi: 10.1111/jocn.15365
2. Zhou, M, Zhang, X, and Jieming, Q. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. (2020) 14:126–35. doi: 10.1007/s11684-020-0767-8
3. WHO. (2023b). ‘WHO coronavirus (COVID-19) dashboard’. Available at: https://covid19.who.int.
4. Damme, V, Wim, RD, Delamou, A, Ingelbeen, B, Wouters, E, Vanham, G, et al. The COVID-19 pandemic: diverse contexts; different epidemics—how and why? BMJ Glob Health. (2020) 5:e003098. doi: 10.1136/bmjgh-2020-003098
5. Markov, PV, Ghafari, M, Beer, M, Lythgoe, K, Simmonds, P, Stilianakis, NI, et al. The evolution of SARS-CoV-2. Nat Rev Microbiol. (2023) 21:361–79. doi: 10.1038/s41579-023-00878-2
6. Martini, M, Gazzaniga, V, Bragazzi, NL, and Barberis, I. The Spanish influenza pandemic: a lesson from history 100 years after 1918. J Prev Med Hyg. (2019) 60:E64–7. doi: 10.15167/2421-4248/jpmh2019.60.1.1205
7. LeDuc, JW, and Anita Barry, M. SARS, the first pandemic of the 21st Century. Emerg Infect Dis. (2004) 10:e26. doi: 10.3201/eid1011.040797_02
8. Rolston, KVI. Understanding Middle East respiratory syndrome. JAAPA. (2015) 28:52–4. doi: 10.1097/01.JAA.0000466591.41090.5e
9. Arslan, M, Bin, X, and El-Din, MG. Transmission of SARS-CoV-2 via fecal-oral and aerosols-borne routes: environmental dynamics and implications for wastewater management in underprivileged societies. Sci Total Environ. (2020) 743:140709. doi: 10.1016/j.scitotenv.2020.140709
10. Paden, CR, Yusof, MFBM, Al Hammadi, ZM, Queen, K, Tao, Y, Eltahir, YM, et al. Zoonotic origin and transmission of Middle East respiratory syndrome coronavirus in the UAE. Zoonoses Public Health. (2018) 65:322–33. doi: 10.1111/zph.12435
11. Wiboonchutikul, S, Manosuthi, W, and Sangsajja, C. Zero transmission of Middle East respiratory syndrome: lessons learned from Thailand. Clin Infect Dis. (2017) 64:S167–70. doi: 10.1093/cid/cix074
12. Morawska, L, Bahnfleth, W, Bluyssen, PM, Boerstra, A, Buonanno, G, Dancer, SJ, et al. Coronavirus disease 2019 and airborne transmission: science rejected, lives lost. Can society do better? Clin Infect Dis. (2023) 76:1854–9. doi: 10.1093/cid/ciad068
13. Wang, J, Alipour, M, Soligo, G, Roccon, A, De Paoli, M, Picano, F, et al. Short-range exposure to airborne virus transmission and current guidelines. Proc Natl Acad Sci. (2021) 118:e2105279118. doi: 10.1073/pnas.2105279118
14. Luo, Y, Li, Y, Xiao, S, and Lei, H. Comparative analysis of inflight transmission of SARS-CoV-2, influenza, and SARS-CoV-1. Epidemiol Infect. (2023) 151:e111. doi: 10.1017/S0950268823001012
15. Mills, CE, Robins, JM, and Lipsitch, M. Transmissibility of 1918 Pandemic Influenza’. Nature. (2004) 432:904–6. doi: 10.1038/nature03063
16. Karimizadeh, Z, Dowran, R, Mokhtari-azad, T, and Shafiei-Jandaghi, N-Z. The reproduction rate of severe acute respiratory syndrome coronavirus 2 different variants recently circulated in human: a narrative review. Eur J Med Res. (2023) 28:94. doi: 10.1186/s40001-023-01047-0
18. Petersen, E, Koopmans, M, Go, U, Hamer, DH, Petrosillo, N, Castelli, F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. (2020) 20:e238–44. doi: 10.1016/S1473-3099(20)30484-9
19. de Souza, AS, de Freitas Amorim, VM, Guardia, GDA, Dos Santos, FF, Ulrich, H, Galante, PAF, et al. Severe acute respiratory syndrome coronavirus 2 variants of concern: a perspective for emerging more transmissible and vaccine-resistant strains. Viruses. (2022) 14:827. doi: 10.3390/v14040827
20. Markel, H, Lipman, HB, Alexander Navarro, J, Sloan, A, Michalsen, JR, Stern, AM, et al. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. JAMA. (2007) 298:644–54. doi: 10.1001/JAMA.298.6.644
21. Moon, MJ. Fighting COVID-19 with agility, transparency, and participation: wicked policy problems and new governance challenges. Public Adm Rev. (2020) 80:651–6. doi: 10.1111/puar.13214
22. Hobday, RA, and Cason, JW. The open-air treatment of PANDEMIC INFLUENZA. Am J Public Health. (2009) 99:S236–42. doi: 10.2105/AJPH.2008.134627
23. Caristia, S, Ferranti, M, Skrami, E, Raffetti, E, Pierannunzio, D, Palladino, R, et al. Effect of national and local lockdowns on the control of COVID-19 pandemic: a rapid review. Epidemiol Prev. (2020) 44:60–8. doi: 10.19191/EP20.5-6.S2.104
24. Khanna, RC, Cicinelli, MV, Gilbert, SS, Honavar, SG, and Murthy, GSV. COVID-19 pandemic: lessons learned and future directions. Indian J Ophthalmol. (2020) 68:703–10. doi: 10.4103/ijo.IJO_843_20
25. Hu, Y, Kong, L, Yao, T, Chen, X, and Wei, D. Does lock-down of Wuhan effectively restrict early geographic spread of novel coronavirus epidemic during Chunyun in China? A spatial model study. BMC Public Health. (2021) 21:825. doi: 10.1186/s12889-021-10837-2
26. Zhang, X, Ji, Z, Zheng, Y, Ye, X, and Li, D. Evaluating the effect of City lock-down on controlling COVID-19 propagation through deep learning and network science models. Cities. (2020) 107:102869. doi: 10.1016/j.cities.2020.102869
27. Feltham, E, Forastiere, L, Alexander, M, and Christakis, NA. Mass gatherings for political expression had no discernible association with the local course of the COVID-19 pandemic in the USA in 2020 and 2021. Nat Hum Behav. (2023) 7:1708–28. doi: 10.1038/s41562-023-01654-1
28. Herby, J., Jonas Lars, K., and Hanke, S.H. (2023). ‘Did lockdowns work? The verdict on covid restrictions’ institute of economic affairs. Available at:https://iea.org.uk/publications/did-lockdowns-work-the-verdict-on-covid-restrictions/.
29. Herby, J, Jonung, L, and Hanke, SH. A literature review and Meta-analysis of the effects of lockdowns on COVID-19 mortality. Maryland: Johns Hopkins University (2022).
30. Bhattacharya, S, Smark, C, and Mir, M. COVID 19: social, financial and economic implications. Australas Account Bus Finance J. (2021) 15:1–4. doi: 10.14453/aabfj.v15i1.1
31. Nicola, M, Alsafi, Z, Sohrabi, C, Ahmed Kerwan, A, Al-Jabir, CI, Agha, M, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. (2020) 78:185–93. doi: 10.1016/j.ijsu.2020.04.018
32. Ozili, PK, and Arun, T. Spillover of COVID-19: impact on the global economy. SSRN Scholarly Paper: Rochester, NY (2020).
33. Tellis, GJ, Sood, A, Nair, S, and Sood, N. Lockdown without loss? A natural experiment of net payoffs from COVID-19 lockdowns. J Public Policy Mark. (2023) 42:133–51. doi: 10.1177/07439156221143954
34. Onyema, EM, Eucheria, NC, Obafemi, FA, Sen, S, Atonye, FG, Sharma, A, et al. Impact of coronavirus pandemic on education. J Educ Pract. (2020) 11:108. doi: 10.7176/JEP/11-13-12
35. Kapitsinis, N. The underlying factors of excess mortality in 2020: a cross-country analysis of pre-pandemic healthcare conditions and strategies to cope with COVID-19. BMC Health Serv Res. (2021) 21:1197. doi: 10.1186/s12913-021-07169-7
36. Jakovljevic, M, Bjedov, S, Jaksic, N, and Jakovljevic, I. COVID-19 Pandemia and public and global mental health from the perspective of Global Health Securit. Psychiatr Danub. (2020) 32:6–14. doi: 10.24869/psyd.2020.6
37. Spaull, N, and Van Der Berg, S. ‘Counting the cost: COVID-19 school closures in South Africa and its impact on children’. South African journal of. Child Educ. (2020) 10:a924. doi: 10.4102/sajce.v10i1.924
38. López-Castro, T, Brandt, L, Anthonipillai, N, Espinosa, A, and Melara, R. Experiences, impacts and mental health functioning during a COVID-19 outbreak and lockdown: data from a diverse New York city sample of college students. PLoS One. (2021) 16:e0249768. doi: 10.1371/journal.pone.0249768
39. Jefferson, T, Dooley, L, Ferroni, E, Al-Ansary, LA, van Driel, ML, Bawazeer, GA, et al. ‘Physical Interventions to Interrupt or Reduce the Spread of Respiratory Viruses’. Cochrane Database of Systematic Reviews, no. 1. (2023) doi: 10.1002/14651858.CD006207.pub6
40. Mehr, J, Kim, ST, Xu, C, Li, H, and Rose, G. ‘Efficacy and Use of Cloth Masks: A Scoping Review’. Cureus. (2020) doi: 10.7759/cureus.10423
41. Høeg, TB, González-Dambrauskas, S, and Prasad, V. ‘Does Equipoise Exist for Masking Children for COVID-19?’ Public Health Pract. (2023) 6:100428. doi: 10.1016/j.puhip.2023.100428
42. Kisielinski, K, Hirsch, O, Wagner, S, Wojtasik, B, Funken, S, Klosterhalfen, B, et al. ‘Physio-Metabolic and Clinical Consequences of Wearing Face Masks—Systematic Review with Meta-Analysis and Comprehensive Evaluation’. Front Public Health (2023) 11. doi: 10.3389/fpubh.2023.1125150
43. Kisielinski, K, Wagner, S, Hirsch, O, Klosterhalfen, B, and Prescher, A. ‘Possible Toxicity of Chronic Carbon Dioxide Exposure Associated with Face Mask Use, Particularly in Pregnant Women, Children and Adolescents - A Scoping Review’. Heliyon (2023) 9:e14117. doi: 10.1016/j.heliyon.2023.e14117
44. Radonovich, LJ, Simberkoff, MS, Bessesen, MT, Brown, AC, Cummings, DA, Gaydos, CA, et al. ‘N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial’. JAMA. (2019) 322:824–33. doi: 10.1001/jama.2019.11645
45. Sharma, SK, Mishra, M, and Mudgal, SK. ‘Efficacy of Cloth Face Mask in Prevention of Novel Coronavirus Infection Transmission: A Systematic Review and Meta-Analysis’. J. Educ. Health Promot. (2020) 9:192. doi: 10.4103/jehp.jehp_533_20
46. Wang, Y, Deng, Z, and Shi, D.‘How Effective Is a Mask in Preventing COVID‐19 Infection?’ Medical Devices & Sensors. (2021) 4:e10163. doi: 10.1002/mds3.10163
47. Villiers, D, Charl, DC, and Van Zijl, W. The south African Government’s response to COVID-19. J Public Budg Account Financ Manag. (2020) 32:797–811. doi: 10.1108/JPBAFM-07-2020-0120
48. Hurrell, Max. (2023). ‘Max Hurrell-ZOL (unofficial music video by the Kiffness)-YouTube’. Available at: https://www.youtube.com/watch?v=UshEeyv8YZM.
49. Aldous, Coleen, Oldfield, Philip, Dancis, Jerome, and Dancis, Barry. (2023). ‘New approach for evaluating evidence in a pandemic: the totality of evidence wheel’. Available at: https://www.trialsitenews.com/a/new-approach-for-evaluating-evidence-in-a-pandemic-the-totality-of-evidence-wheel-abff2a0c.
50. Bhattacharya, Jay. (2023). The government censored me and other scientists. We fought Back—and won.’ Available at:https://www.thefp.com/p/i-fought-government-censorship-and-won.
51. Canada Global Affairs. (2020). ‘Media freedom and COVID-19’. Available at: https://www.international.gc.ca/world-monde/issues_development-enjeux_developpement/human_rights-droits_homme/policy-orientation-COVID-19.aspx?lang=eng.
52. Christenson, Josh. (2023). ‘CIA tried to pay off analysts to Bury COVID lab leak findings: whistleblower’. Available at: https://nypost.com/2023/09/12/cia-tried-to-pay-off-analysts-to-bury-covid-lab-leak-findings-whistleblower/.
53. Cole, Devan. (2023). ‘What to know about the order blocking the Biden administration from communicating with social media companies’. Available at: https://www.cnn.com/2023/07/06/politics/social-media-misinformation-biden-administration-injunction-explainer/index.html.
54. Kenny, Chris. (2023). “Utterly appalling: government censored COVID posts that were actually true ”. Available at: https://www.skynews.com.au/opinion/chris-kenny/utterly-appalling-government-censored-covid-posts-that-were-actually-true/video/340e76e27e9f43a9830d2abc0c71be87.
55. Showalter, Monica. (2023). ‘As COVID recrudesces, major meta-study questioning lockdowns is censored’. Available at: https://www.americanthinker.com/blog/2023/09/as_covid_recrudesces_major_metastudy_questioning_lockdowns_is_censored.html.
56. Team Investigations. (2023). ‘Secretive Covid disinformation unit worked with security services’. Available at: https://www.telegraph.co.uk/news/2023/09/01/secretive-covid-disinformation-unit-security-services/.
57. Hanselka, CW, Savory, A, and Butterfield, J. Holistic management: a new framework for decision making. Washington, DC: Island Press (1999).
58. Savory, A, Jody TH=Butterfield. Holistic management: a common sense revolution to restore our environment. Washington, DC: Island Press (1999).
59. Savory Institute. (2023). ‘Our team Savory institute’. Available at: https://savory.global/team/.
60. Gosnell, H, Grimm, K, and Goldstein, BE. A half century of holistic management: what does the evidence reveal? Agric Hum Values. (2020) 37:849–67. doi: 10.1007/s10460-020-10016-w
61. Barrera, JF. Holistic pest management In: D PerezStaples, F DiazFleischer, P Montoya, and MT Vera, editors. Area-wide management of fruit fly pests. Florida: CRC Press (2019). 281–300.
62. Constantinou, C, Kolokotroni, O, Mosquera, MC, Heraclides, A, Demetriou, C, Karayiannis, P, et al. Developing a holistic contingency plan: challenges and dilemmas for cancer patients during the COVID-19. Cancer Med. (2020) 9:6082–92. doi: 10.1002/cam4.3271
63. Ponte, B, Costas, J, Puche, J, De La Fuente, D, and Pino, R. Holism versus reductionism in supply chain management: an economic analysis. Decis Support Syst. (2016) 86:83–94. doi: 10.1016/j.dss.2016.03.010
64. Rodriguez, NJI. A comparative analysis of holistic marine management regimes and ecosystem approach in marine spatial planning in developed countries. Ocean Coast Manag. (2017) 137:185–97. doi: 10.1016/j.ocecoaman.2016.12.023
65. McChrystal, Stanley (US Army, retired General), Tantum Collins, and Chris Fussel. (2015). Team of teams: new rules of engagement for a complex world. Available at:https://www.mcchrystalgroup.com/team-of-teams/.
66. Chenli, M, Bannerman, S, and Abrokwah, E. Reviewing the global economic impacts and mitigating measures of COVID-19. Total Qual Manag Bus Excell. (2022) 33:1573–87. doi: 10.1080/14783363.2021.1981130
67. Garcia, MA, Thierry, AD, and Pendergrast, CB. The devastating economic impact of COVID-19 on older black and Latinx adults: implications for health and well-being. J Gerontol B Psychol Sci Soc Sci. (2022) 77:1501–7. doi: 10.1093/geronb/gbab218
68. Müller, SR, Delahunty, F, and Matz, SC. The impact of the early stages of COVID-19 on mental health in the United States, Germany, and the United Kingdom. J Pers Soc Psychol. (2023) 124:620–39. doi: 10.1037/pspp0000459
69. Chidambaram, Priya. (2022). ‘Over 200,000 residents and staff in long-term care facilities have died from COVID-19 | KFF’. Available at: https://www.kff.org/policy-watch/over-200000-residents-and-staff-in-long-term-care-facilities-have-died-from-COVID-19/.
70. Hao, X, Cheng, S, Degang, W, Tangchun, W, Lin, X, and Wang, C. Reconstruction of the full transmission dynamics of COVID-19 in Wuhan. Nature. (2020) 584:420–4. doi: 10.1038/S41586-020-2554-8
71. Morawska, L, and Milton, DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19). Clin Infect Dis. (2020) 71:2311–3. doi: 10.1093/CID/CIAA939
72. Byambasuren, O, Cardona, M, Bell, K, Clark, J, McLaws, M-L, and Glasziou, P. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: systematic review and Meta-analysis. J Assoc Med Microbiol Infect Dis Can. (2020) 5:223–34. doi: 10.3138/jammi-2020-0030
73. Tayyar, R, Kiener, MA, Liang, JW, Contreras, G, Rodriguez-Nava, G, Zimmet, AN, et al. Low infectivity among asymptomatic patients with a positive severe acute respiratory coronavirus virus 2 (SARS-CoV-2) admission test at a tertiary care center, 2020–2022. Infect Control Hosp Epidemiol. (2023) 25:1–3. doi: 10.1017/ice.2023.210
74. Reuters. (2020). ‘Minibus drivers in South Africa strike over coronavirus funding’. Available at: https://www.voanews.com/a/COVID-19-pandemic_minibus-drivers-south-africa-strike-over-coronavirus-funding/6191527.html.
75. Bingham, J, Cable, R, Coleman, C, Glatt, TN, Grebe, E, Mhlanga, L, et al. Estimates of prevalence of anti-SARS-CoV-2 antibodies among blood donors in South Africa in march 2022. Res Sq. (2022) 26:rs.3.rs-1687679. doi: 10.21203/RS.3.RS-1687679/V1
76. Britschgi, Christian. (2023). ‘Study: Sweden’s “laissez faire” pandemic policies paid off’. Available at: https://reason.com/2023/08/29/study-swedens-laissez-faire-pandemic-policies-paid-off/.
77. Norberg, Johan. (2023). ‘Sweden during the pandemic | Cato institute’. Available at: https://www.cato.org/policy-analysis/sweden-during-pandemic.
78. Georank. (2020). ‘Sweden vs the United Kingdom coronavirus cases: day by day comparison’. Available at: https://georank.org/covid/sweden/united-kingdom.
79. Martin, David. (2023). Covid summit-European Union parliament. Available at:https://rumble.com/v2ncp8w-dr-david-e.-martin-phd-covid-summit-european-union-parliament-may-2023.html.
80. Joubert, M, Guenther, L, Metcalfe, J, Riedlinger, M, Chakraborty, A, Gascoigne, T, et al. `Pandem-icons’ — exploring the characteristics of highly visible scientists during the COVID-19 pandemic. J Sci Commun. (2023) 22:A04. doi: 10.22323/2.22010204
81. Caro, JC, Clark, AE, D’Ambrosio, C, and Vogele, C. The impact of COVID-19 lockdown stringency on loneliness in five European countries. Soc Sci Med. (2022) 314:115492. doi: 10.1016/j.socscimed.2022.115492
82. Lintern, Shaun. (2020). ‘Pfizer given protection from legal action over coronavirus vaccine by UK government’. Available at: https://www.independent.co.uk/news/health/coronavirus-pfizer-vaccine-legal-indemnity-safety-ministers-b1765124.html.
Keywords: pandemic management, lockdowns, evidence based medicine, COVID-19, holistic health, holistic management
Citation: Aldous C and Kruger HG (2023) Interrogating the lack of diversity of thought in the pandemic response that led to mistakes - holistic evidence-based approach to deal with future pandemics. Front. Public Health. 11:1310210. doi: 10.3389/fpubh.2023.1310210
Edited by:
Nicolai Savaskan, District Office Neukölln of Berlin Neukölln, GermanyReviewed by:
Emanuel Wiggerich, Stadt Oberhausen - Gesundheitsamt, GermanyBenedikt M. J. Lampl, Regensburg Department of Public Health, Germany
Copyright © 2023 Aldous and Kruger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hendrik G. Kruger, a3J1Z2VyQHVrem4uYWMuemE=
 Colleen Aldous
Colleen Aldous Hendrik G. Kruger
Hendrik G. Kruger