- 1School of Public Health, Southern Medical University, Guangzhou, China
- 2Guangdong Provincial Institute of Public Health, Guangdong Provincial Center for Disease Control and Prevention, Guangzhou, China
- 3Guangdong Provincial Center for Disease Control and Prevention, Guangzhou, China
- 4Guangdong Workstation for Emerging Infectious Disease Control and Prevention, Guangzhou, China
- 5School of Public Health, Guangdong Pharmaceutical University, Guangzhou, China
- 6School of Public Health, Sun Yat-sen University, Guangzhou, Guangdong, China
- 7School of Medicine, Jinan University, Guangzhou, China
Background: The non-pharmaceutical interventions (NPIs) against COVID-19 may have affected the transmission of hand, foot and mouth disease (HFMD). We aimed to assess the impact of the NPIs on HFMD in the high epidemic area of HFMD, Guangdong Province.
Methods: The data of HFMD cases, etiological information, and meteorological factors in Guangdong from January 1, 2012, to December 31, 2021, were collected. Using a Bayesian structural time series (BSTS) model integrated counterfactual framework, we assessed the effect of NPIs on HFMD by different intervention periods, populations (gender, age, occupation), and cities. We further explored the correlation between the reduction of HFMD and socioeconomic factors in 21 cities.
Results: A total of 351,217 HFMD cases were reported and 455,327 cases were averted in Guangdong Province during 2020–2021 with a reduction of 84.94% (95%CI: 81.63–87.22%) in 2020 and 29.49% (95%CI: 15.26–39.54%) in 2021. The impact of NPIs on HFMD differed by age and gender. The effects of NPIs were more remarkable for children aged 0–2 years and scattered children. We found that the relative reductions in 21 cities were related to the composition ratio of children and COVID-19 incidence.
Conclusion: The reduction of HFMD incidence was significantly associated with COVID-19 NPIs, and school closure was an effective intervention to prevent HFMD outbreaks. Our findings will contribute to the development of HFMD prevention and control measures.
1 Introduction
Hand, foot and mouth disease (HFMD) is a widespread infectious disease that mainly affects children (1). The average annual number of HFMD cases reported in China from 2014 to 2019 was approximately 2.0 million (2). Guangdong has historically been a region with a high incidence of HFMD (3). The incidence of HFMD was about three times the national average, making it a major public health concern (4, 5). It has been reported that HFMD in China had semiannual peaks of activity, including a major peak in summer and a smaller peak in autumn (6). The incidence of HFMD remains high, threatening the health of children and causing a significant burden in China.
Coronavirus disease 2019 (COVID-19) which caused by SARS-CoV-2 is highly infectious (7). During the COVID-19 epidemic, China has adopted a series of non-pharmaceutical interventions (NPIs), such as school closure, wearing masks and enhancing personal hand hygiene, to control the spread of COVID-19 (8). Several studies have shown that the NPIs against the COVID-19 epidemic have co-benefits for the prevention of other infectious diseases. For example, the respiratory diseases decreased from 156.24 per 100,000 people during 2014–2019 to 145.12 in 2020 (9). Geng et al. found that the incidence of pertussis decreased by 76.49% in 2020, compared to the average incidence in 2017–2019 (10). Additionally, Zhao et al. showed that HFMD cases were reduced by 52.9% in 2020 (11). A study in Xi’an City found that HFMD cases decreased by 94.2% in the first half of 2020 (12). Xiao et al. found that HFMD has decreased by 83.9% compared to the average incidence in Guangdong Province during the anti-COVID-19 period (13). It was reported that the HFMD cases in China increased again in 2021, with reported cases of 1.35 million (vs. 0.76 million in 2020) (14, 15). Li′s study found that the incidence of HFMD in 2021 has higher than expected (12). However, there was less knowledge about the impact on HFMD with the NPIs during the different periods of COVID-19 epidemic.
In this study, based on large population surveillance data in the high epidemic area of HFMD, Guangdong Province, China, we aim to investigate the changing epidemic characteristics of HFMD in 2020–2021, the first two years during the COVID-19 pandemic. Then we quantified the effects of COVID-19 interventions on the HFMD epidemic in 2020–2021.
2 Methods
2.1 Study area and participants
Guangdong Province is located between 20°09′–25°31’ N latitude and 109°45′–117°20′ E longitude (16) in southern China, including 21 cities, with a population of 12.6 billion (17). It belongs to the East Asian monsoon region, with hot and rainy seasons (18). Guangdong is the province with the largest number of reported HFMD cases (19), ranking first among notifiable infectious diseases from 2010 to 2018 (20), and the cases were 418,300 in 2019, accounting for 21.9% of China (21, 22). HFMD has decreased significantly in the initial phase of COVID-19 epidemic (13), for the reason that Guangdong implemented strict NPIs such as travel restrictions, school closure, compulsory health quarantine, and regional lockdown. Thus, Guangdong would be an ideal site to study the effects of COVID-19 intervention on HFMD. Supplementary Figure S1 shows the distribution of 21 cities and populations in Guangdong Province in 2020. In this study, the study population was children aged 0–14 years.
2.2 Data collection
2.2.1 COVID-19 cases
The cases from January 1, 2020 to December 31, 2021 were obtained from the National Notifiable Infectious Diseases Reporting Information System (NNIDRIS) at Guangdong Provincial Center for Disease Control and Prevention.
2.2.2 NPIs and emergency response periods grading
The NPIs were collected from the official website and media reports including cases-based measures (quarantine and isolation), community measures (wearing masks, enhancing personal hand hygiene, and school closures), and travel-related measures. The government implemented Level 1 emergency response on January 23, 2020, after Guangdong Province reported the first case of COVID-19 on January 14, 2020. And then a series of NPIs such as canceling large-scale mass events, wearing face masks in public, and extending school holidays were taken.1 According to the study of Xiao et al. (13), we divided the period of 2020–2021 into four periods. Level 1 emergency response was weeks 4–8 in 2020, Level 2 was weeks 9–19, Level 3 was weeks 20–53 in 2020 and the whole of 2021 was divided into the Level 4 emergency response. The higher response level, the stricter the NPIs implemented.
2.2.3 HFMD cases
Data of daily HFMD cases aggregated for each of the 21 cities in Guangdong from January 1, 2012, to December 31, 2021, were obtained from the NNIDRIS. For this study, these daily HFMD cases were first organized into weekly data, and then categorized into different subgroups according to gender (male or female), age (0–2 years, 3–5 years, or 6–14 years), and occupation type (scattered children, kindergarten children or student).
2.2.4 HFMD etiological data
The data were collected from the Guangdong Province Acute Infectious Disease surveillance Information System from January 1, 2012, to December 31, 2021. We first divided the test results of the samples into negative, enterovirus A71 (EV-A71), coxsackievirus A16 (CV-A16) and others, and calculated the weekly total number of cases for each. Then, we calculated the composition ratio of EV-A71 cases and CV-A16 cases to the weekly total.
2.2.5 Meteorological data
Daily meteorological data were obtained from The China Meteorological Data Service Centre.2 If there is no meteorological monitoring station in the administrative region of a city, the meteorological monitoring station data of the nearest neighboring city will be used.
2.2.6 Sociodemographic and economic data
Population data for children aged 0–14, and per capita GDP for 21 cities were collected from the Guangdong Statistics Yearbook (see Footnote 1).
2.3 Statistical analysis
We used the Bayesian structural time series (BSTS) model to construct the counterfactual time series in 2020–2021, and compare the weekly counterfactual cases with observed cases which were further stratified by emergency response periods, population, and cities to evaluate the effects of NPIs on HFMD.
The BSTS model consists of the spike-and-slab method, Kalman filter, and Bayesian model averaging, and was specified as follows:
Eq. (1) is the observation equation, which connects the monitoring data yt with the potential d-dimensional state vector αt. Eq. (2) is the transition equation that governs the change of the state vector αt over time. In this study, yt is the number of HFMD cases in a certain week t, Zt is a d-dimensional output vector, μt is the control variable (weekly average temperature, weekly average relative humidity, and the weekly composition ratio of CV-A16). Some studies showed that the prevalence of HFMD is affected by meteorological parameters (23–26), which suggests temperature and relative humidity are significantly associated with HFMD incidence. Studies also found that increasing CV-A16 epidemic activity was observed recently in Guangdong (19). Hence, we incorporated them into the BSTS model. τt is the time trend control variable, and εt is the monitoring error. Tt. is a transformation matrix of d*d, Rt is a control matrix of controlling d*q, and ηt is a q-dimensional systematic error. The above state space equation integrates the linear regression, the seasonal trend, and the regression coefficients of covariates over the same period of the number of HFMD cases per week before the intervention, and the Bayesian prior distribution is used for fitting in the analysis process.
First, we fit data from 2012 to 2019 to evaluate the fit of the BSTS model. The data from 2012 to 2017 were used as training data, and the data from 2018 to 2019 were used to simulate. We evaluated the fit of the model using the Mean Absolute Percentage Error (MAPE) or R2 values, with lower MAPE values indicating better performance and higher R2 values indicating a better model fit. Then based on the MAPE or R2, the model has adjusted appropriately so that the accuracy of the model could meet the expected standard. Finally, we used the adjusted model to estimate the weekly counterfactual HFMD cases and evaluate the effects of NPIs on HFMD by comparing the predicted and observed cases from January 20, 2020 (week 4), to December 31, 2021 (week 53), taking into account seasonality and long-term trends in Guangdong Province. The formula is as follows:
In Eq. (3), represents the counterfactual HFMD cases in group a at week t and c = 0 represents the counterfactual HFMD cases. represents the number of observed cases in age group a at week t and c = 1 represents the observed cases. τ is the total age group. represents the magnitude of the reduction of the observed cases compared with the expected. We used the indicator “relative reduction” instead of to represent the effects. In addition, we estimated the relative reduction by gender, age, and occupation groups.
Furthermore, to explore the relationship between the relative reduction with COVID-19 incidence and socioeconomic status, we did a Spearman correlation analysis of the relative reduction with the number of COVID-19 cases, COVID-19 incidence, GDP per capita, and composition ratio of children aged 0–14 in 2020 and 2021, respectively.
In this study, a value of p of <0.05 was considered significant. We implemented the BSTS models using the “bsts” and “CausalImpact” packages in R soft (version 4.2.1).
3 Results
3.1 Epidemic of COVID-19 and implementation of NPIs
The epidemic curve was constructed according to the number of COVID-19 cases per week and the NPIs initiated at different times were also annotated in the Figure 1. We classified NPIs into three categories: case-based measures, community measures, and travel-related measures.
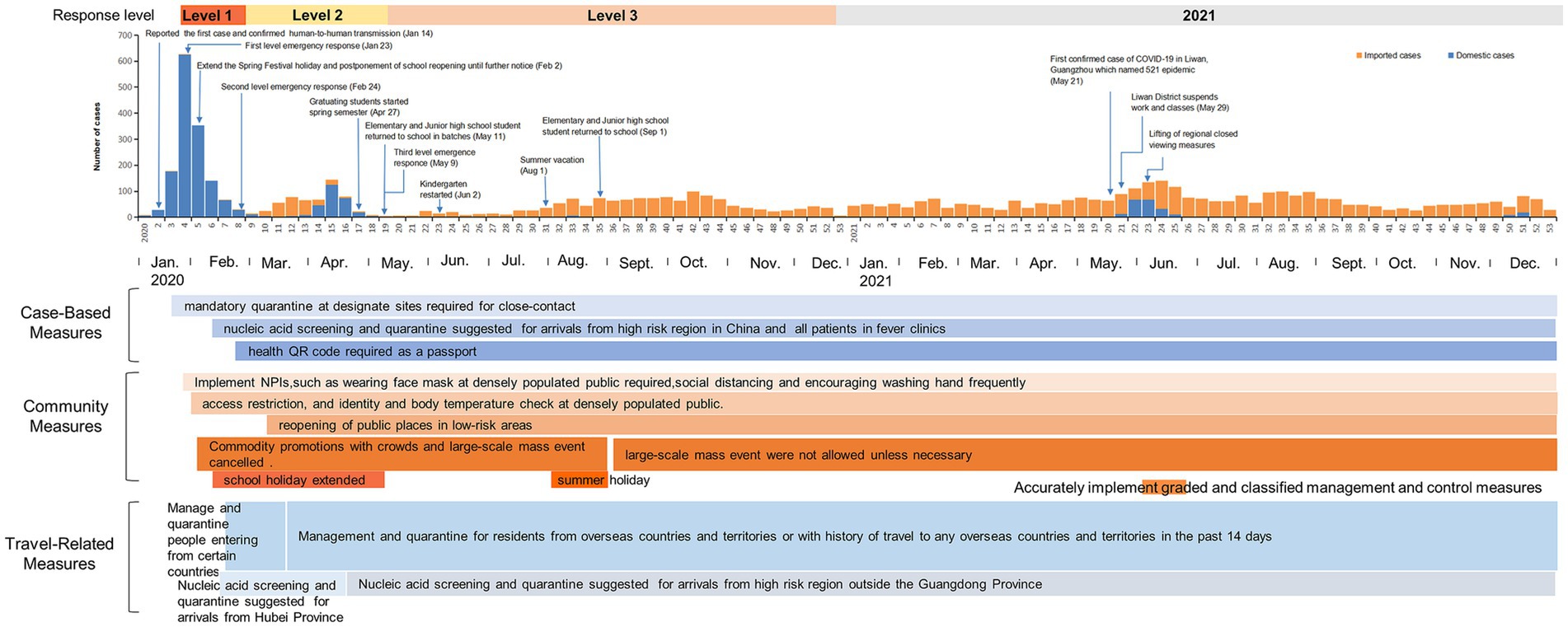
Figure 1. Epidemiological profile of COVID-19 and implementation of synchronous NPIs in Guangdong Province, China, 2020–2021.
3.2 Epidemiological trend of HFMD
The epidemiological trend of HFMD during 2012–2021 was presented in Supplementary Figure S2. We found the HFMD has seasonality and periodicity, with two peaks per year, and the incidence remained high until 2020. The major peak is in May–July and the smaller peak is in September–October.
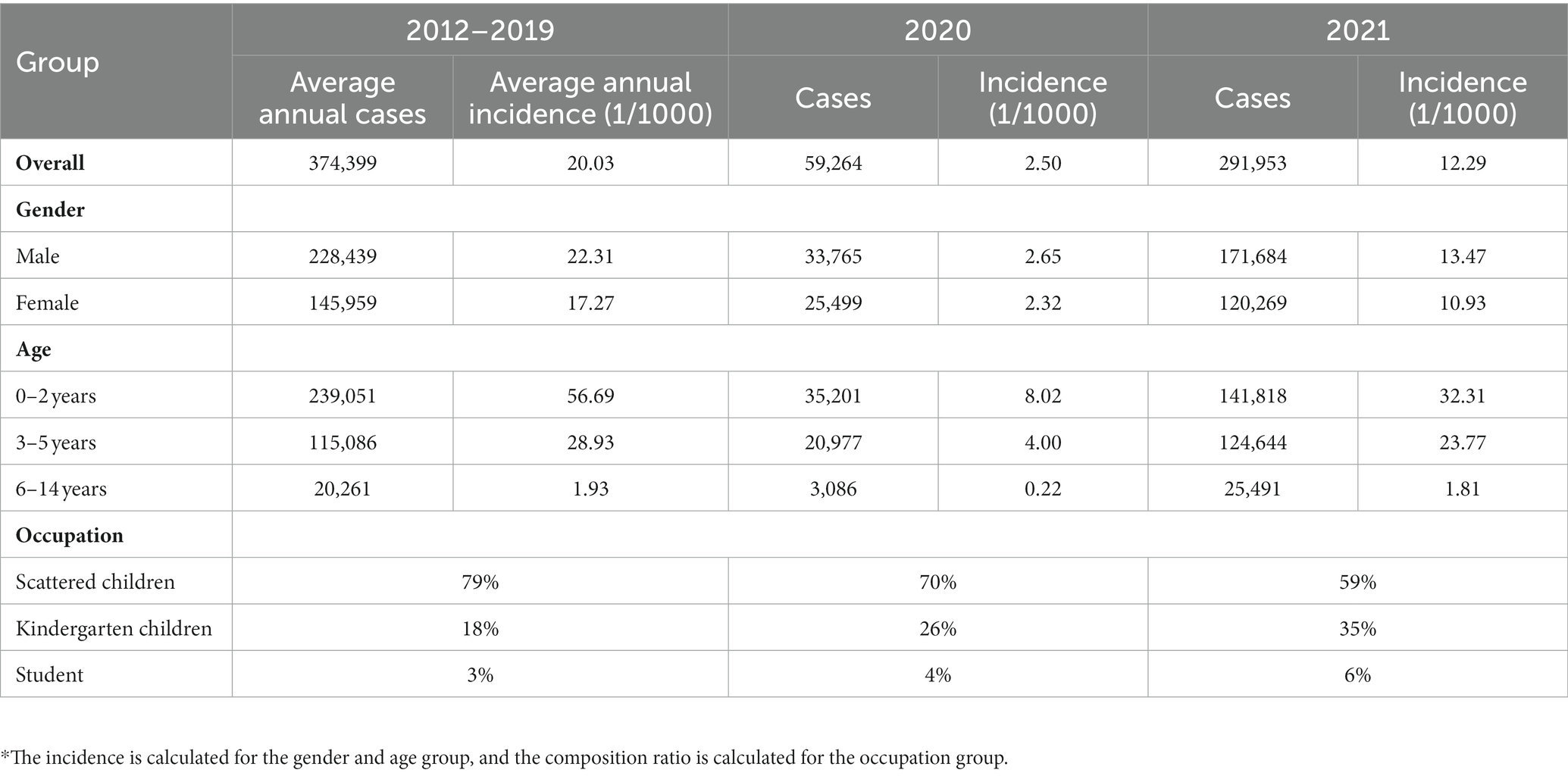
Table 1 showed the cases and incidence of HFMD by gender, age, and occupation group. Overall, Guangdong reported 59,264 and 291,953 cases in 2020 and 2021, respectively, which was lower than the annual cases in 2012–2019. The incidence was 2.50/1000 in 2020 and was 12.29/1000 in 2021 which was lower than the annual incidence in 2012–2019. We found that the incidence in male was higher than in female. Among the age groups, the HFMD incidence in 2020 and 2021 was lower than the annual incidence of 2012–2019. The incidence in children aged 0–2 and 3–5 years was significantly higher than in those aged 6–14 years. Furthermore, the proportion of scattered children was the most.
3.3 The impact of the NPIs
Figure 2 and Table 2 showed the comparison of the observed and predicted HFMD cases by week during 2020–2021. We found that the observed cases were lower than the predicted counterfactual cases in 2020–2021. In addition, the major peak disappeared and the smaller peak was delayed in 2020. The BSTS model showed that the relative reduction of HFMD cases in Level 1 was 91.10% (95% CI: -∞–97.95%), corresponding to 4,537 averted cases. The relative reduction in Level 2 was 98.28% (95% CI: 97.18–98.74%), averting 67,011 cases. At Level 3, the relative reduction was 82.00% (95% CI: 78.34–84.59%) averting 262,664 cases. While the relative reduction had declined to 29.49% (95% CI: 15.26–39.54%) in 2021, corresponding to 121,115 cases averted (Table 2).
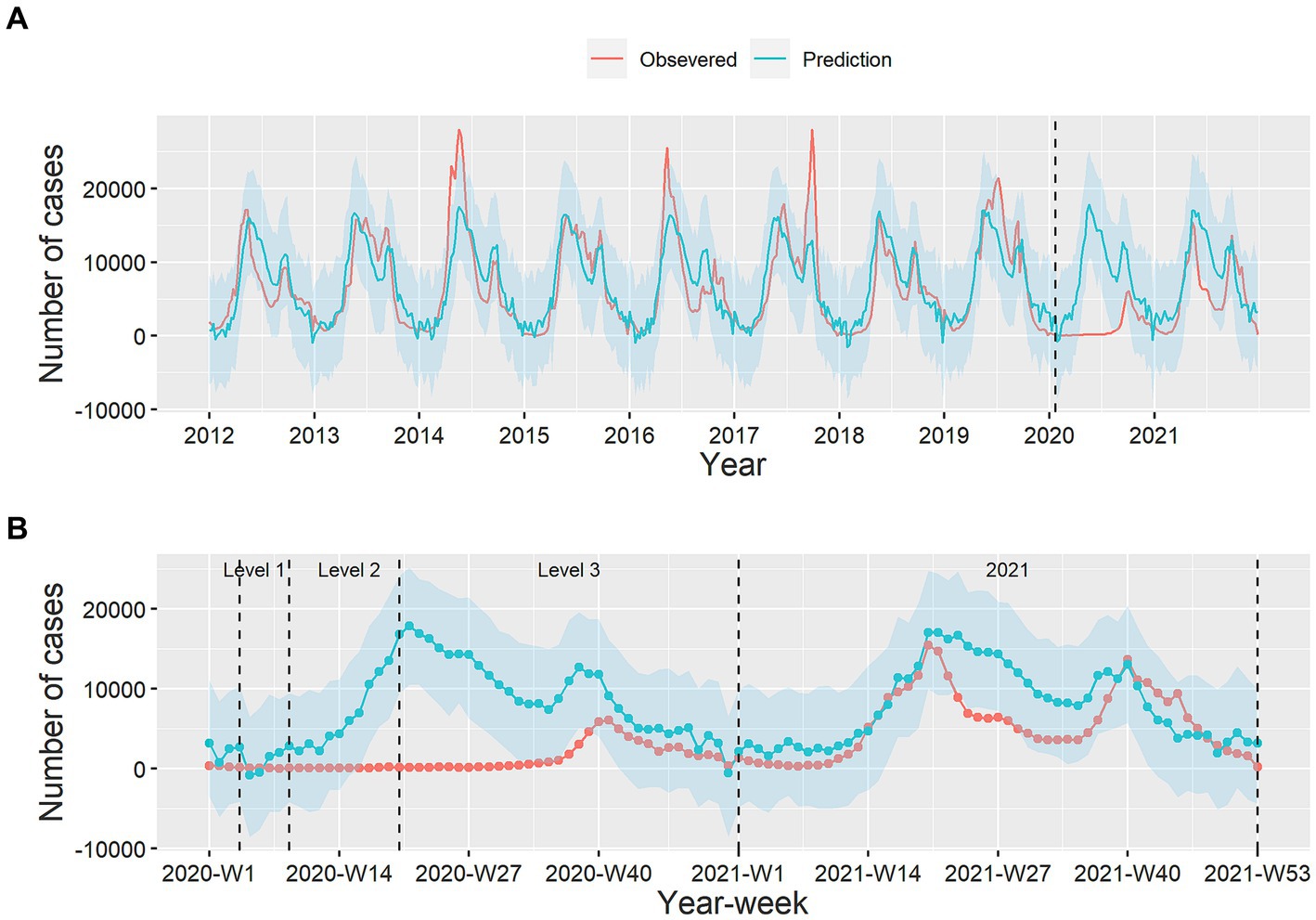
Figure 2. The weekly counts of observed and predicted HFMD cases. Plot (A) is the weekly time-series of observed and predicted HFMD cases during 2012–2021, and plot (B) is the comparison of observed HFMD cases with prediction in the 4 periods. Red line: observed cases, blue line: predicted cases, blue shadow: 95% confidence interval for prediction.
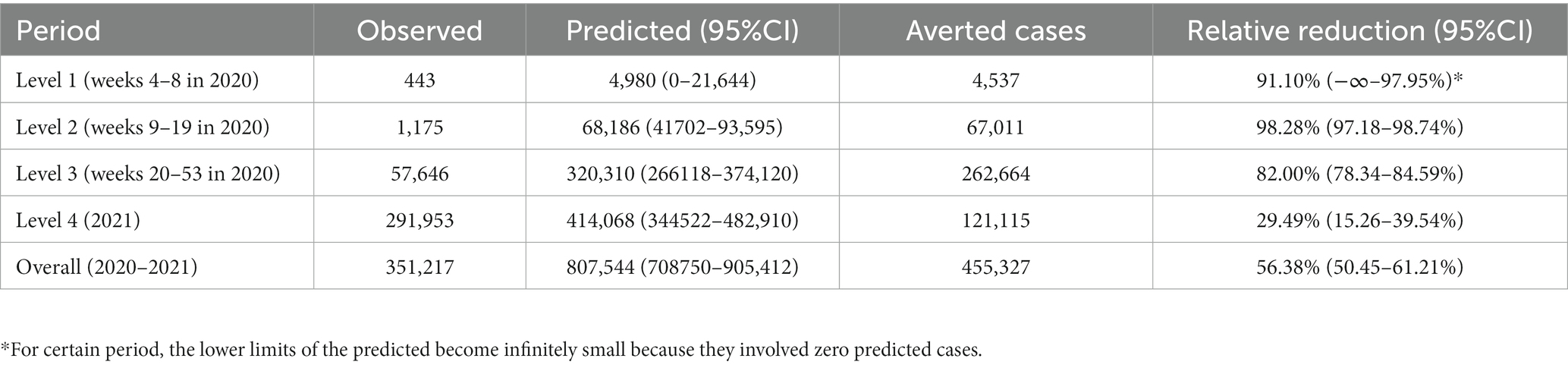
Table 2. The relative reduction of HFMD incidence during four periods in Guangdong Province in 2020–2021.
3.4 The impact of NPIs by group
Figure 3 and Supplementary Table S1 presented the relative reduction of HFMD cases by gender, age, and occupation during 2020–2021. The relative reduction in male was similar to that in female. In all three age groups, the greatest relative reduction was at Level 2, with 97.88% (95% CI: 96.65–98.45%), 99.12% (95% CI: 98.25–99.41%), and 97.56% (95% CI: 95.35–98.33%), respectively. The relative reduction of 0–2 years was larger than that of 3–5 years and 6–14 years during Level 1–Level 4 except Level 2. The counterfactual HFMD cases in 2021 in children aged 3–5 years and 6–14 years were higher than the observed cases. The situation in different occupations was similar to that in age group, with the greatest relative reduction in both cases at Level 2, which was 97.79% (95% CI: 96.30–98.44%), 99.35% (95% CI: 99.13–99.68%), and 97.55% (95% CI: 96.28–98.20%), respectively. The relative reduction among kindergarten children was higher than scattered children and student in Level 1 and Level 2, whereas that of scattered children was larger than that of kindergarten children and students during Level 3 to Level 4 period. The observed cases of kindergarten children and student were more than predicted in 2021.
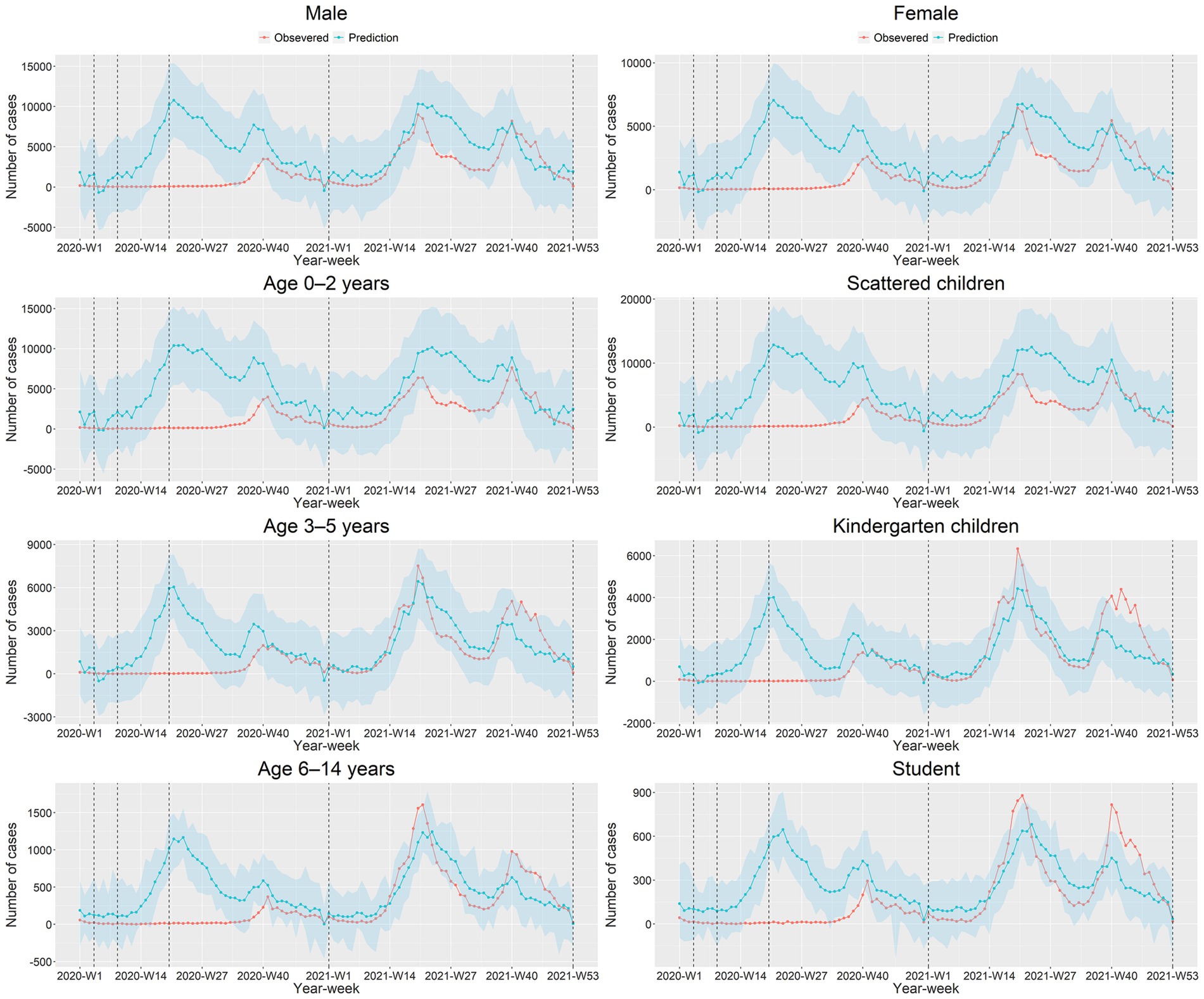
Figure 3. The observed and predicted HFMD cases by gender, age, and occupation during 2020–2021 in Guangdong Province.
3.5 The impact of the NPIs by city
Supplementary Figure S3 presented the comparison between observed and predicted HFMD cases in 21 cities by week. We noticed that the observed cases were lower than predicted in 2020, and the major peak disappeared and the smaller peak appeared later in each city. However, the observed cases were higher than predicted at the smaller peak of HFMD prevalence in some cities in 2021, such as Guangzhou and Foshan.
3.6 Correlation analysis
As shown in Supplementary Figures S4A,B were the relative reduction in 21 cities in Guangdong Province in 2020 and 2021, respectively. We found that the relative reduction was even larger in non-Pearl River Delta region. Supplementary Figures S4C,D represent the correlation analysis of relative reduction with log COVID-19 cases, per capita GDP, the incidence of COVID-19 (1/100000), and composition ratio of children aged 0–14 years in 2020 and 2021, respectively. The relative reduction was positively related (ρ = 0.61) to the composition ratio of children aged 0–14years in 2020. The results showed a negative correlation between the relative reduction in log COVID-19 cases (ρ = −0.49) and the incidence of COVID-19 (1/100000) in 2021 (ρ = −0.49).
4 Discussion
In this study, we observed that HFMD incidence in Guangdong decreased dramatically after the implementation of strict COVID-19 NPIs in 2020, and increased slightly in 2021 with certain relaxing of NPIs. The reduction of HFMD varied by periods and populations, and the effect was associated with COVID-19 incidence. This study has provided evidence that the implementation of NPIs is effective in mitigating the transmission of HFMD and that the stricter the NPIs, the greater the reduction. The results would help to develop the prevention strategy for the HFMD epidemic.
4.1 Impact of the NPIs
The characteristics of the epidemic have changed in 2020. HFMD in Guangdong province reached its lowest level in a decade due to the strict NPIs against COVID-19. The observed cases were significantly lower than the counterfactual predicted cases. The major peak disappeared, with only one epidemic peak in the autumn. The results were consistent with the findings of previous studies (27, 28). Niu et al. found that the effective reproduction number of HFMD decreased to 0 after the implementation of NPIs (27). These measures could reduce the transmission capacity of HFMD. However, with the decreased of stringency of NPIs, the number of HFMD cases gradually rose and returned to a higher level in 2021.
The relative reduction of HFMD cases was 56.38% (95%CI: 50.45–61.21%) in 2020–2021, which was lower than in the Xi’an study (12). We observed that the implementation of NPIs had a significant effect on HFMD in Guangdong, China, especially in 2020 when the interventions were more stringent. This finding was similar to that of Zhao et al. (11) and Li et al. (12), who found a remarkable decrease in HFMD cases since the implementation of NPIs in 2020. The main modes of transmission of HFMD include fecal-oral transmission, respiratory transmission and contact transmission (29, 30). And during the COVID-19 epidemic, some NPIs such as mask wearing, frequent hand washing and social distancing restrictions were implemented, which reduced the transmission of HFMD (31, 32). This suggested that developing good hygiene habits can effectively reduce HFMD, which needs attention from schools and parents. The largest reductions were in Level 1 and 2 periods, and the smallest in 2021, at 29.49%. Large-scale school closures occurred in Level 1 and 2 periods, while school closures only applied in epidemic areas during specific periods in 2021. This indicates that school closure may be an important NPI to control HFMD (33). Kindergartens are the common sites for HFMD outbreaks for they are the most socially dense environments (34–37), making it easy for HFMD to spread among children. A previous study showed that school closure reduced transmission by more than 50% (38). Hence, it is necessary for the government to consider closing schools to contain the outbreak. The largest reduction was at Level 2 rather than Level 1, possibly because of the delayed effect of the NPIs on HFMD transmission (13). Our results provided evidence that the implementation of stricter NPIs would provide better protection for children aged 0–14 years old, and suggested that it is important for schools and parents to develop good hygiene habits in children.
4.2 Impact of the NPIs by gender, age, and occupation
We observed that the relative reduction in male was similar to that in female. In terms of age groups, the best protection was observed in the 0–2 years group, whose highest reduction was 97.88% (96.65–98.45%) in Level 2. Our study suggested that NPIs such as home isolation can significantly reduce the cases of children under 2 years old. Previous studies have shown that children under 2 years old were more likely to be infected with HFMD, so strengthening the protection of children under 2 years old may be the key issue for the HFMD control (33). Furthermore, we found that the observed cases in children aged 3–5 and 6–14 years old were higher than expected in 2021. One possible reason for this shift may be that, with the under-controlled epidemic and relaxing NPIs, people participated in more economic and social activities (39, 40), which increased the interpersonal contacts and the risk of HFMD transmission (41, 42). In terms of occupation groups, the largest reduction occurred in Level 1 or Level 2, and the kindergarten children and student rebounded in 2021. It may be associated with the school reopen (11, 43). Luca et al. showed that school closure can reduce the spread of infectious diseases, but it would obtain a rebound effect when schools reopened after the closure (44). As the interventions against COVID-19 are relaxed and children return to school, the HFMD epidemic is likely to rise to higher levels. It is important for the government to increase the health knowledge of parents about HFMD (45) and adopt some NPIs (such as home isolation and school closure) to control it. In addition, some virus showed periodicity on the scale of 1 or 2 years (46). The rebound in 2021 may be related to the changes in the type of virus circulating. In conclusion, the effect was greater for 0–2 years than for others. If necessary, school closure may be effective in controlling the HFMD epidemics.
4.3 Impact of the NPIs on different regions
The observed HFMD cases decreased to varying degrees compared with the counterfactual cases in 21 cities in 2020. This may be related to the stringency of the implementation effects of the NPIs in different regions. HFMD rebounded mainly in the Pearl River Delta region in 2021, which may be related to the high mobility of the population and more interpersonal contact with people (42) after the relaxation of the implementation of NPIs (12).
The correlation analysis showed that the reduction of HFMD was positively related to the proportion of children aged 0–14 in 2020. The implementation of NPIs has prevented children from being exposed to HFMD virus, resulting in the decrease in the infection (28). Furthermore, our study showed that the reduction of HFMD was negatively related to the COVID-19 cases and incidence in 2021, meaning that regions with more stringent NPIs have fewer COVID-19 cases and a greater reduction in HFMD.
4.4 The strength and limitations
Using multi-source data from 21 cities in Guangdong Province from 2012 to 2021, we quantitatively assessed the effects of COVID-19 NPIs on HFMD. In addition, we incorporated influencing factors such as aetiological and meteorological data into the model to provide more reliable results. Our study has several limitations. First, HFMD cases may have been underdiagnosed and underreported to some extent in 2020–2021 due to the fear of COVID-19 infection preventing people from going to a hospital, or some medical institutions may not operate regularly. Second, this study is an ecological research design, the direct effect of a specific non-pharmaceutical intervention on HFMD needs further study. Third, the effect of EV-A71 vaccination was not considered in this study. Previous studies (47, 48) have shown that the EV-A71 vaccine provides good protection against EV-A71-associated HFMD, while showing limited effectiveness against non-EV-A71-associated HFMD. Additionally, one study also (49) found that the overall incidence of HFMD did not decrease after EV-A71 vaccination, although the EV-A71-associated HFMD cases decreased significantly. The EV-A71 vaccination may have a small effect on the overall incidence, so the impact of vaccination on the prevalence of HFMD was not considered in this study. Finally, there may be some uncertainty in estimating the reduction in cases of HFMD due to different periods of school closure.
5 Conclusion
This study demonstrated the effects of NPIs in reducing HFMD cases during COVID-19 epidemic in Guangdong Province, which varied in different intervention periods, populations and regions. Our study suggests that timely school closures are an effective way to prevent the HFMD outbreak, and NPIs such as hand washing and mask-wearing would significantly reduce the transmission of HFMD. This study has provided a vivid case to the response of HFMD and these findings will help the policy makers in the prevention and control of HFMD.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the dataset used in the study is not public available, while it was available from the corresponding author. Requests to access these datasets should be directed to JPX, anBlbmd4QDE2My5jb20=; MZ, NDA5NzgyMDc4QHFxLmNvbQ==.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Guangdong Provincial Center for Disease Control and Prevention (No. W96-027 E-202104). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
LZ: Data curation, Formal analysis, Methodology, Visualization, Writing – original draft. FY: Data curation, Formal analysis, Visualization, Writing – original draft. ZZ: Writing – review & editing. WLZ: Writing – review & editing. ZR: Writing – review & editing. JH: Formal analysis, Visualization, Writing – review & editing. XL: Writing – review & editing. JZ: Methodology, Writing – review & editing. BZ: Writing – review & editing. YHL: Data curation, Visualization, Writing – review & editing. YQ: Writing – review & editing. QZ: Visualization, Writing – review & editing. ZH: Visualization, Writing – review & editing. YYL: Data curation, Writing – review & editing. XH: Writing – review & editing. WYZ: Writing – review & editing. JQX: Writing – review & editing. YL: Funding acquisition, Writing – review & editing. QC: Writing – review & editing. JPX: Data curation, Funding acquisition, Methodology, Resources, Writing – review & editing. MZ: Data curation, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by National Natural Science Foundation of China (82373636), Guangdong Natural Science and Technology Project (2023A1515011921), the Key Area Research and Development Program of Guangdong Province (2022A1111090004), and Medical Science and Technology Research Fund of Guangdong Province (B2023033).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1307321/full#supplementary-material
Abbreviations
HFMD, Hand, foot and mouth disease; COVID-19, Coronavirus disease 2019; NPIs, non-pharmaceutical interventions; NNIDRIS, National Notifiable Infectious Diseases Reporting Information System; EV-A71, enterovirus A71; CVA16, coxsackievirus A16; BSTS, Bayesian structural time series; MAPE, Mean Absolute Percentage Error.
Footnotes
References
1. CDC. Hand, foot, and mouth disease(HFMD). (2021). Available at: https://www.cdc.gov/hand-foot-mouth/index.html
2. National Health Commission of the People's Republic of China. Epidemic situation of notifiable infectious diseases in China. (2021). Available at: http://www.nhc.gov.cn/jkj/
3. Deng, T, Huang, Y, Yu, S, Gu, J, Huang, C, Xiao, G, et al. Spatial-temporal clusters and risk factors of hand, foot, and mouth disease at the district level in Guangdong Province, China. PLoS One. (2013) 8:e56943. doi: 10.1371/journal.pone.0056943
4. National Health Commission of the People's Republic of China. National overview of statutory infectious disease outbreaks in 2019. (2019). Available at: http://www.nhc.gov.cn/jkj/s3578/202004/b1519e1bc1a944fc8ec176db600f68d1.shtml
5. Health Commission of Guangdong Province. Guangdong provincial health commission announces 2019 Province's statutory reported infectious disease outbreaks. (2019). Available at: http://wsjkw.gd.gov.cn/gkmlpt/content/2/2897/post_2897686.html#2571
6. Xing, W, Liao, Q, Viboud, C, Zhang, J, Sun, J, Wu, JT, et al. Hand, foot, and mouth disease in China, 2008-12: an epidemiological study. Lancet Infect Dis. (2014) 14:308–18. doi: 10.1016/s1473-3099(13)70342-6
7. CDC. Coronavirus disease 2019 (COVID-19). (2021). Available at: https://www.cdc.gov/dotw/covid-19/index.html
8. Health Commission of Guangdong Province. Make every effort to prevent and control the epidemic of novel coronavirus infection. (2022). Available at: http://wsjkw.gd.gov.cn/
9. Geng, MJ, Zhang, HY, Yu, LJ, Lv, CL, Wang, T, Che, TL, et al. Changes in notifiable infectious disease incidence in China during the COVID-19 pandemic. Nat Commun. (2021) 12:6923. doi: 10.1038/s41467-021-27292-7
10. Geng, Y, and Zhang, L. Impact of non-pharmaceutical interventions during COVID-19 pandemic on pertussis, scarlet fever and hand-foot-mouth disease in China. J Infect. (2022) 84:e13–5. doi: 10.1016/j.jinf.2021.12.023
11. Zhao, Z, Zheng, C, Qi, H, Chen, Y, Ward, MP, Liu, F, et al. Impact of the coronavirus disease 2019 interventions on the incidence of hand, foot, and mouth disease in mainland China. Lancet Regional Health Western Pacific. (2022) 20:100362. doi: 10.1016/j.lanwpc.2021.100362
12. Shen, L, Sun, M, Song, S, Hu, Q, Wang, N, Ou, G, et al. The impact of anti-COVID-19 nonpharmaceutical interventions on hand, foot, and mouth disease-a spatiotemporal perspective in Xi'an, northwestern China. J Med Virol. (2022) 94:3121–32. doi: 10.1002/jmv.27715
13. Xiao, J, Dai, J, Hu, J, Liu, T, Gong, D, Li, X, et al. Co-benefits of nonpharmaceutical intervention against COVID-19 on infectious diseases in China: a large population-based observational study. Lancet Regional Health Western Pacific. (2021) 17:100282. doi: 10.1016/j.lanwpc.2021.100282
14. National Health Commission of the People's Republic of China. National epidemiological profile of statutory infectious diseases in 2021. (2022). Available at: http://www.nhc.gov.cn/jkj/s3578/202204/4fd88a291d914abf8f7a91f6333567e1.shtml
15. National Health Commission of the People's Republic of China. National epidemiological profile of statutory infectious diseases in 2020. (2021). Available from: http://www.nhc.gov.cn/jkj/s3578/202103/f1a448b7df7d4760976fea6d55834966.shtml
16. People's Government of Guangdong Province. Overview of Guangdong Province. (2022). Available at: http://www.gd.gov.cn/zjgd/sqgk/zrdl/index.html
17. Guangdong statistical yearbook. Main population indicators. (2021). Available at: http://tjnj.gdstats.gov.cn:8080/tjnj/2021/directory/03/html/03-01.htm
18. The Central People's Government of the People's Republic of China. Introduction to Guangdong Province. (2022). Available at: http://www.gov.cn/guoqing/2019-01/28/content_5361692.htm
19. Yi, L, Zeng, H, Zheng, H, Peng, J, Guo, X, Liu, L, et al. Molecular surveillance of coxsackievirus A16 in southern China, 2008-2019. Arch Virol. (2021) 166:1653–9. doi: 10.1007/s00705-021-05052-8
20. Health Commission of Guangdong Province. Report of notifiable infectious diseases in Guangdong Province. (2021). Available at: http://wsjkw.gd.gov.cn/
21. National Health Commission of the People's Republic of China. Overview of notifiable infectious diseases in China in 2019. (2019). Available at: http://www.nhc.gov.cn/jkj/s6873/202004/b1519e1bc1a944fc8ec176db600f68d1.shtml
22. Health Commission of Guangdong Province. The Health Commission of Guangdong Province announced the status of notifiable infectious diseases in 2019. (2019). Available at: http://wsjkw.gd.gov.cn/zwyw_yqxx/content/post_2897686.html
23. Ji, XY, Huang, LY, Song, J, Fei, CN, Liu, J, and Liu, H. Short-term effects of meteorological factors, air pollution, and sunspot on childhood hand, foot, and mouth disease in Tianjin, China: a new time series regression, 2014-2018. Environ Sci Pollut Res Int. (2020) 27:37022–35. doi: 10.1007/s11356-020-09794-x
24. Du, Z, Lawrence, WR, Zhang, W, Zhang, D, Yu, S, and Hao, Y. Bayesian spatiotemporal analysis for association of environmental factors with hand, foot, and mouth disease in Guangdong, China. Sci Rep. (2018) 8:15147. doi: 10.1038/s41598-018-33109-3
25. Wang, Y, Lai, Y, Du, Z, Zhang, W, Feng, C, Li, R, et al. Spatiotemporal distribution of hand, foot, and mouth disease in Guangdong Province, China and potential predictors, 2009−2012. Int J Environ Res Public Health. (2019) 16:1191. doi: 10.3390/ijerph16071191
26. Van Pham, H, Phan, UTN, and Pham, ANQ. Meteorological factors associated with hand, foot and mouth disease in a central highlands province in Viet Nam: an ecological study. Western Pacific Surveillance Response J. (2019) 10:18–23. doi: 10.5365/wpsar.2017.8.1.003
27. Niu, Y, Luo, L, Rui, J, Yang, S, Deng, B, Zhao, Z, et al. Control measures during the COVID-19 outbreak reduced the transmission of hand, foot, and mouth disease. J. Safety Sci. Resilience. (2021) 2:63–8. doi: 10.1016/j.jnlssr.2021.06.002
28. Wu, K, Ma, X, Liu, H, Zheng, J, Zhou, R, Yuan, Z, et al. Effects of different levels of non-pharmaceutical interventions on hand, foot and mouth disease in Guangzhou, China. BMC Public Health. (2022) 22:2398. doi: 10.1186/s12889-022-14850-x
29. National Health Commission of the People's Republic of China. Hand-foot-and-mouth disease diagnosis and treatment guidelines (2018 edition). (2018). Available at: http://www.nhc.gov.cn/yzygj/s3594q/201805/5db274d8697a41ea84e88eedd8bf8f63.shtml
30. Sun, L, Lin, H, Lin, J, He, J, Deng, A, Kang, M, et al. Evaluating the transmission routes of hand, foot, and mouth disease in Guangdong, China. Am J Infect Control. (2016) 44:e13–4. doi: 10.1016/j.ajic.2015.04.202
31. Zhang, D, Li, Z, Zhang, W, Guo, P, Ma, Z, Chen, Q, et al. Hand-washing: the Main strategy for avoiding hand, foot and mouth disease. Int J Environ Res Public Health. (2016) 13:610. doi: 10.3390/ijerph13060610
32. Ruan, F, Yang, T, Ma, H, Jin, Y, Song, S, Fontaine, RE, et al. Risk factors for hand, foot, and mouth disease and herpangina and the preventive effect of hand-washing. Pediatrics. (2011) 127:e898–904. doi: 10.1542/peds.2010-1497
33. Le, J, Hong, J, Zhao, Z, Chen, Y, Hu, Y, Chang, Z, et al. Age-specific transmission for different virus serotypes of hand, foot and mouth disease and the impact of interventions in East China, 2009-2015. Heliyon. (2022) 8:e12042. doi: 10.1016/j.heliyon.2022.e12042
34. Gatwood, J, Meltzer, MI, Messonnier, M, Ortega-Sanchez, IR, Balkrishnan, R, and Prosser, LA. Seasonal influenza vaccination of healthy working-age adults: a review of economic evaluations. Drugs. (2012) 72:35–48. doi: 10.2165/11597310-000000000-00000
35. Kar, BR, Dwibedi, B, and Kar, SK. An outbreak of hand, foot and mouth disease in Bhubaneswar, Odisha. Indian Pediatr. (2013) 50:139–42. doi: 10.1007/s13312-013-0033-0
36. Gemmetto, V, Barrat, A, and Cattuto, C. Mitigation of infectious disease at school: targeted class closure vs school closure. BMC Infect Dis. (2014) 14:695. doi: 10.1186/s12879-014-0695-9
37. Russell, ES, Zheteyeva, Y, Gao, H, Shi, J, Rainey, JJ, Thoroughman, D, et al. Reactive school closure during increased influenza-like illness (ILI) activity in Western Kentucky, 2013: a field evaluation of effect on ILI incidence and economic and social consequences for families. Open Forum Infect Dis. (2016) 3:ofw113. doi: 10.1093/ofid/ofw113
38. Earn, DJ, He, D, Loeb, MB, Fonseca, K, Lee, BE, and Dushoff, J. Effects of school closure on incidence of pandemic influenza in Alberta, Canada. Ann Intern Med. (2012) 156:173–81. doi: 10.7326/0003-4819-156-3-201202070-00005
39. People’s Government of Guangdong Province. Macroeconomic performance of Guangdong in 2020. (2020). Available at: http://www.gd.gov.cn/zwgk/sjfb/sjkx/content/post_3184233.html
40. People's Government of Guangdong Province. Implementation opinions of Guangdong COVID-19 prevention and Control Headquarters on normalizing COVID-19 prevention and control. (2020). Available at: https://www.gd.gov.cn/gdywdt/zwzt/yqfk/gdzxd/content/post_2994035.html
41. Zhang, J, Litvinova, M, Liang, Y, Zheng, W, Shi, H, Vespignani, A, et al. The impact of relaxing interventions on human contact patterns and SARS-CoV-2 transmission in China. Sci Adv. (2021) 7:eabe2584. doi: 10.1126/sciadv.abe2584
42. Liu, J, Chen, Y, Hu, P, Gan, L, Tan, Q, Huang, X, et al. Caregivers: the potential infection resources for the sustaining epidemic of hand, foot, and mouth disease/herpangina in Guangdong, China? Archives Public Health. (2021) 79:54. doi: 10.1186/s13690-021-00574-8
43. Chen, Y, Badaruddin, H, Lee, VJ, Cutter, J, and Cook, AR. The effect of school closure on hand, foot, and mouth disease transmission in Singapore: a modeling approach. Am J Trop Med Hyg. (2018) 99:1625–32. doi: 10.4269/ajtmh.18-0099
44. Luca, G, Kerckhove, KV, Coletti, P, Poletto, C, Bossuyt, N, Hens, N, et al. The impact of regular school closure on seasonal influenza epidemics: a data-driven spatial transmission model for Belgium. BMC Infect Dis. (2018) 18:29. doi: 10.1186/s12879-017-2934-3
45. Kua, JA, and Pang, J. The epidemiological risk factors of hand, foot, mouth disease among children in Singapore: a retrospective case-control study. PLoS One. (2020) 15:e0236711. doi: 10.1371/journal.pone.0236711
46. Wu, H, Xue, M, Wu, C, Lu, Q, Ding, Z, Wang, X, et al. Trend of hand, foot, and mouth disease from 2010 to 2021 and estimation of the reduction in enterovirus 71 infection after vaccine use in Zhejiang Province, China. PLoS One. (2022) 17:e0274421. doi: 10.1371/journal.pone.0274421
47. Head, JR, Collender, PA, Lewnard, JA, Skaff, NK, Li, L, Cheng, Q, et al. Early evidence of inactivated enterovirus 71 vaccine impact against hand, foot, and mouth disease in a major Center of Ongoing Transmission in China, 2011-2018: a longitudinal surveillance study. Clin Infect Dis. (2020) 71:3088–95. doi: 10.1093/cid/ciz1188
48. Xiao, J, Zhu, Q, Yang, F, Zeng, S, Zhu, Z, Gong, D, et al. The impact of enterovirus A71 vaccination program on hand, foot, and mouth disease in Guangdong, China: a longitudinal surveillance study. J Infect. (2022) 85:428–35. doi: 10.1016/j.jinf.2022.06.020
Keywords: HFMD, COVID-19, SARS-CoV-2, non-pharmaceutical interventions, impact, BSTS
Citation: Zhang L, Yang F, Zhu Z, Zeng W, Rong Z, Hu J, Li X, Zhao J, Zeng B, Li Y, Quan Y, Zhang Q, Huang Z, Li Y, Huang X, Zheng W, Xu J, Li Y, Chen Q, Xiao J and Zhang M (2024) Assessing the impact of COVID-19 interventions on the hand, foot and mouth disease in Guangdong Province, China: a Bayesian modeling study. Front. Public Health. 11:1307321. doi: 10.3389/fpubh.2023.1307321
Edited by:
Hung-Yao Ho, Chang Gung University, TaiwanReviewed by:
Jimin Sun, Zhejiang Provincial Center for Disease Control and Prevention (Zhejiang CDC), ChinaXianfeng Zhou, Jiangxi University of Traditional Chinese Medicine, China
Copyright © 2024 Zhang, Yang, Zhu, Zeng, Rong, Hu, Li, Zhao, Zeng, Li, Quan, Zhang, Huang, Li, Huang, Zheng, Xu, Li, Chen, Xiao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianpeng Xiao, anBlbmd4QDE2My5jb20=; Meng Zhang, NDA5NzgyMDc4QHFxLmNvbQ==
†These authors have contributed equally to this work
 Li Zhang1,2†
Li Zhang1,2† Jianxiong Hu
Jianxiong Hu Biao Zeng
Biao Zeng Yihan Li
Yihan Li Jianpeng Xiao
Jianpeng Xiao