- 1Department of Biostatistics, School of Public Health, Southeast University, Nanjing, China
- 2Jiangsu Provincial Center for Disease Control and Prevention, Nanjing, China
- 3Medical Statistics and Analysis Center, Nanjing Drum Tower Hospital, Nanjing University Medical School, Nanjing, China
Introduction: In times of epidemic outbreaks, healthcare workers (HCWs) emerge as a particularly vulnerable group. This cross-sectional study endeavors to assess the COVID-19 infection rate among the primary HCWs in Jiangsu Province subsequent to the implementation of adjusted epidemic prevention and control strategies.
Methods: From January 17 to February 2, 2023, an extensive survey was conducted among primary HCWs in Jiangsu Province, employing a self-designed questionnaire. Logistic regression analysis was utilized to identify the factors associated with COVID-19 infection.
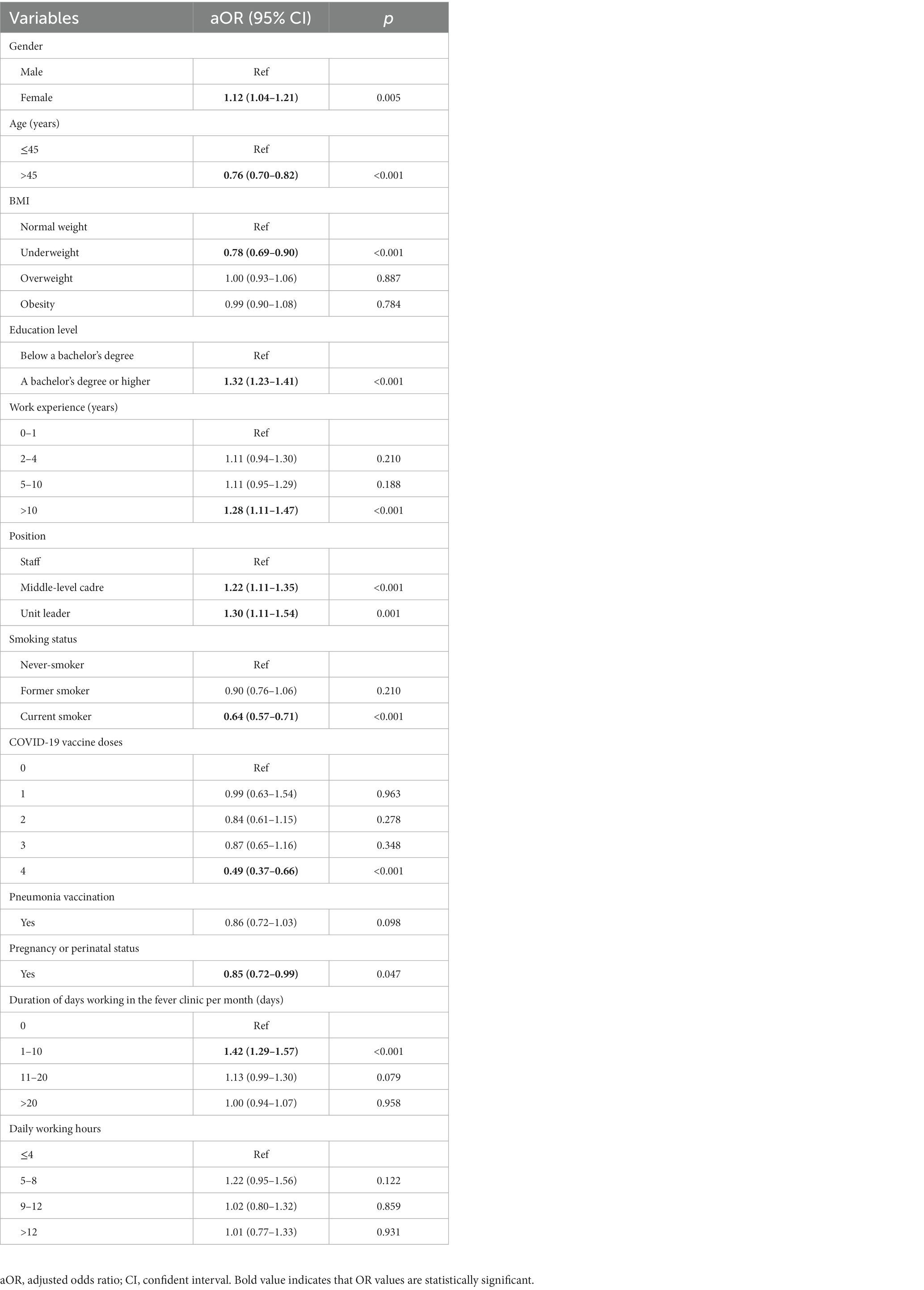
Results: The overall infection rate among primary HCWs stood at 81.05%, with a 95% confidence interval (CI) of 80.61–81.48%. Among those afflicted, cough, fatigue, and fever emerged as the three most prevalent symptoms, each with an incidence rate exceeding 80%. In the context of multivariate logistic regression, an elevated risk of COVID-19 infection was observed in correlation with female gender (adjusted odds ratio [aOR] = 1.12, 95% CI: 1.04–1.21), possessing a bachelor’s degree or higher (aOR = 1.32, 95% CI: 1.23–1.41), accumulating over 10 years of work experience (aOR = 1.28, 95% CI: 1.11–1.47), holding a middle-level cadre position (aOR = 1.22, 95% CI: 1.11–1.35), assuming the role of a unit leader (aOR = 1.30, 95% CI: 1.11–1.54), and working in a fever clinic for 1 to 10 days per month (aOR = 1.42, 95% CI: 1.29–1.57). Conversely, advanced age (aOR = 0.76, 95% CI: 0.70–0.82), being underweight (aOR = 0.78, 95% CI: 0.69–0.90), current smoking (aOR = 0.64, 95% CI: 0.57–0.71), receiving 4 doses of COVID-19 vaccine (aOR = 0.49, 95% CI: 0.37–0.66), and pregnancy or perinatal status (aOR = 0.85, 95% CI: 0.72–0.99) were associated with a diminished risk of infection.
Conclusion: Following the implementation of adjusted policies, a substantial proportion of primary HCWs in Jiangsu province contracted COVID-19. Female gender and younger age emerged as risk factors for COVID-19 infection, while no discernible link was established between professions and COVID-19 susceptibility. The receipt of COVID-19 vaccines demonstrated efficacy in curtailing the infection rate, underscoring the significance of bolstering prevention knowledge and heightening self-protective awareness among primary HCWs.
1 Introduction
Coronavirus disease 2019 (COVID-19), induced by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was initially identified among hospitalized patients in Wuhan, China, spanning December 2019 and January 2020 (1, 2). This viral pathogen underpins a potentially fatal illness, sparking profound global public health apprehensions. As of May 10, 2023, the World Health Organization’s records indicate a worldwide tally of over 765 million confirmed COVID-19 cases, encompassing in excess of 99 million cases documented in China (3).
In contrast to the general population, healthcare workers (HCWs) encounter a heightened risk of infection due to their close and direct exposure to individuals afflicted with COVID-19 (4–6). Particularly noteworthy, factors such as older age, male gender, Black individuals, Asian individuals, and minority ethnic groups, alongside underlying health conditions, contribute to an escalated risk of mortality within the HCW demographic (7–9). American participants who self-reported as African individuals and Latino participants are more likely to be at increased risk of infection and contribute to racial disparities in mortality due to living in neighborhoods with poor air quality (10), working in jobs that do not allow for telecommuting (9), or lack of access to medical care (11). As of August 10, 2021, among the 25 cross-sectional studies assessing COVID-19 prevalence, the combined prevalence of COVID-19 among HCWs, as determined through antibody tests, was found to be 7% (with 95% confidence intervals [CI]: 3–17%), in contrast to the prevalence of 11% (95% CI, 7–16%) observed in studies utilizing PCR tests (12). Among HCWs, instances of infection were predominantly observed in women and nurses, while a substantial proportion of fatalities were recorded among men and doctors (13).
On November 11 and December 7, 2022, the State Council’s Joint Prevention and Control Mechanism responded to the COVID-19 epidemic by introducing the “Twenty Measures” (14) and “Ten New Rules” (15). Notably, the “Ten New Rules” emphasize that nucleic acid testing for all staff should no longer be organized by administrative regions, thereby reducing both the extent and frequency of such testing. Additionally, the requirement for presenting evidence of negative nucleic acid results has been eliminated, except in cases involving specific institutions.
After the implementation of adjusted epidemic prevention and control strategies, the reported incidence of COVID-19 infection in China exhibited a noticeable upward trajectory, exerting a substantial impact on medical institutions across the nation. Nevertheless, primary HCWs persevered in their duties despite their own infections. To gain a comprehensive understanding of the situation surrounding primary HCWs infected with COVID-19 under the new prevention and control strategies, a survey was conducted through the basic public health service network of Jiangsu Province. The goal was to assess the prevalence and pinpoint the factors linked to COVID-19 infection among primary HCWs within Jiangsu Province amid the COVID-19 epidemic.
2 Materials and methods
2.1 Study subjects
In this cross-sectional study, the link to the questionnaire was disseminated to various categories of HCWs, including doctors, nurses, medical technicians, pharmacists, administrators, and other personnel, employed in primary healthcare institutions across the province. This distribution was facilitated through the basic public health service work network of Jiangsu Province on January 17, 2023. The IP address of each respondent during submission was recorded.
The research protocol obtained approval from the Ethics Committee of the Jiangsu Provincial Center for Disease Prevention and Control (JSJK2023-B010-01). Additionally, all participants volunteered for this study, and they signed the informed consent form at the outset of the questionnaire.
2.2 Definitions
After the implementation of adjusted COVID-19 prevention and control strategies, China has discontinued the universal requirement for nucleic acid testing in all individuals. In the context of this study, the term “infected” was delineated to encompass individuals meeting any of the following criteria: (1) testing positive for viral nucleic acid, (2) testing positive for antigens, (3) testing positive for both viral nucleic acid and antigens, or (4) displaying symptoms associated with COVID-19 but not undergoing nucleic acid or antigen testing. Furthermore, the term “uninfected” encompassed individuals meeting either of the following criteria: (1) displaying no positive outcomes in both viral nucleic acid testing and/or antigen testing, or (2) exhibiting no symptoms linked to COVID-19 and refraining from nucleic acid or antigen testing.
The body mass index (BMI) was calculated by dividing the weight in kilograms by the square of height in meters. The BMI classification criteria for Chinese adults are outlined as follows (16): underweight is defined as BMI < 18.5 kg/m2, normal weight is defined as BMI 18.5–23.9 kg/m2, overweight is defined as BMI 24.0–27.9 kg/m2, and obesity was defined as BMI ≥ 28.0 kg/m2.
2.3 Survey measures
The questionnaire used in this study was adapted from the second round of COVID-19 Infection Questionnaire released by China’s National Center for Disease Control and Prevention and Peking Union Medical College, which includes 45-items. In accordance with the Program for Prevention and Control of COVID-19 Infections (10th Edition, http://www.nhc.gov.cn/ylyjs/pqt/202301/32de5b2ff9bf4eaa88e75bdf7223a65a.shtml), the final questionnaire was confirmed in two rounds of discussions with five epidemiologists and statistical experts. The questionnaire consists of 78 obligatory questions, ensuring data integrity in this study. It comprises four sections: (1) Basic information: this includes demographic characteristics, past medical history, and lifestyle, (2) Vaccination status: this encompasses information about the doses and types of COVID-19 vaccine, influenza vaccine, pneumonia vaccine, (3) Clinical manifestations and COVID-19 outcomes: this section covers over ten symptoms such as fever, muscle aches, and cough, along with the duration of symptoms, hospital visits, and medications taken, and (4) Work burden: this includes factors like years of work experience, daily working hours, work-related stress, and whether individuals worked in a fever clinic.
Questionnaire completion and data collection were carried out based on the China’s largest online survey platform (Questionnaire Star, https://www.wjx.cn). Questionnaire Star is a professional service platform for electronic questionnaire design and data collection, which has been widely used by researchers. Designated personnel managed the export of the database through project-specific accounts.
2.4 Statistical analysis
In accordance with prior research (17), the COVID-19 infection rate of the faculty and students at the School of Public Health in universities in Beijing, subsequent to the implementation of adjusted epidemic prevention and control strategies, was 77.89% before December 23, 2022. Assuming a prevalence of COVID-19 of 80%, a significance level (α) of 0.05, and a relative error of sampling of 3%, we estimated the sample size of each city to be 1,107 individuals, and there were 13 cities in the whole province, and considering the design effect of 2, the sample size was 28,782 individuals.
Continuous variables were expressed as means (standard deviation, SD), while categorical variables were presented as frequencies and percentages. Statistical differences between groups were assessed using two sample t-test for continuous variables and Pearson’s Chi-square test or Fisher’s exact test for categorical variables. To identify factors associated with COVID-19 infection among Primary HCWs, both univariate and multivariate logistic regression analyzes were conducted. Variables associated with infection at p ≤ 0.1 in the univariate analysis were included in the multivariate logistic stepwise regression analysis. The risk of COVID-19 infection was assessed with odds ratios (OR) and 95% CI, or adjusted odds ratios (aOR) and 95% CI. All statistical analyzes were performed using R software (R version 4.3.0). A two-sided p ≤ 0.05 was considered statistically significant.
3 Results
3.1 Participants
The average number of primary HCWs per primary healthcare institution in Jiangsu Province is 104. We randomly sampled 400 primary healthcare institutions and collected a total of 34,090 questionnaires between January 17 and February 2, with a roughly estimated response rate of 81.95%. After excluding questionnaires with logical errors or those completed in an unreasonable time frame (less than 300 s for infected individuals and less than 210 s for uninfected individuals), we ultimately acquired 31,482 valid questionnaires, constituting 92.3% of the total number of questionnaires.
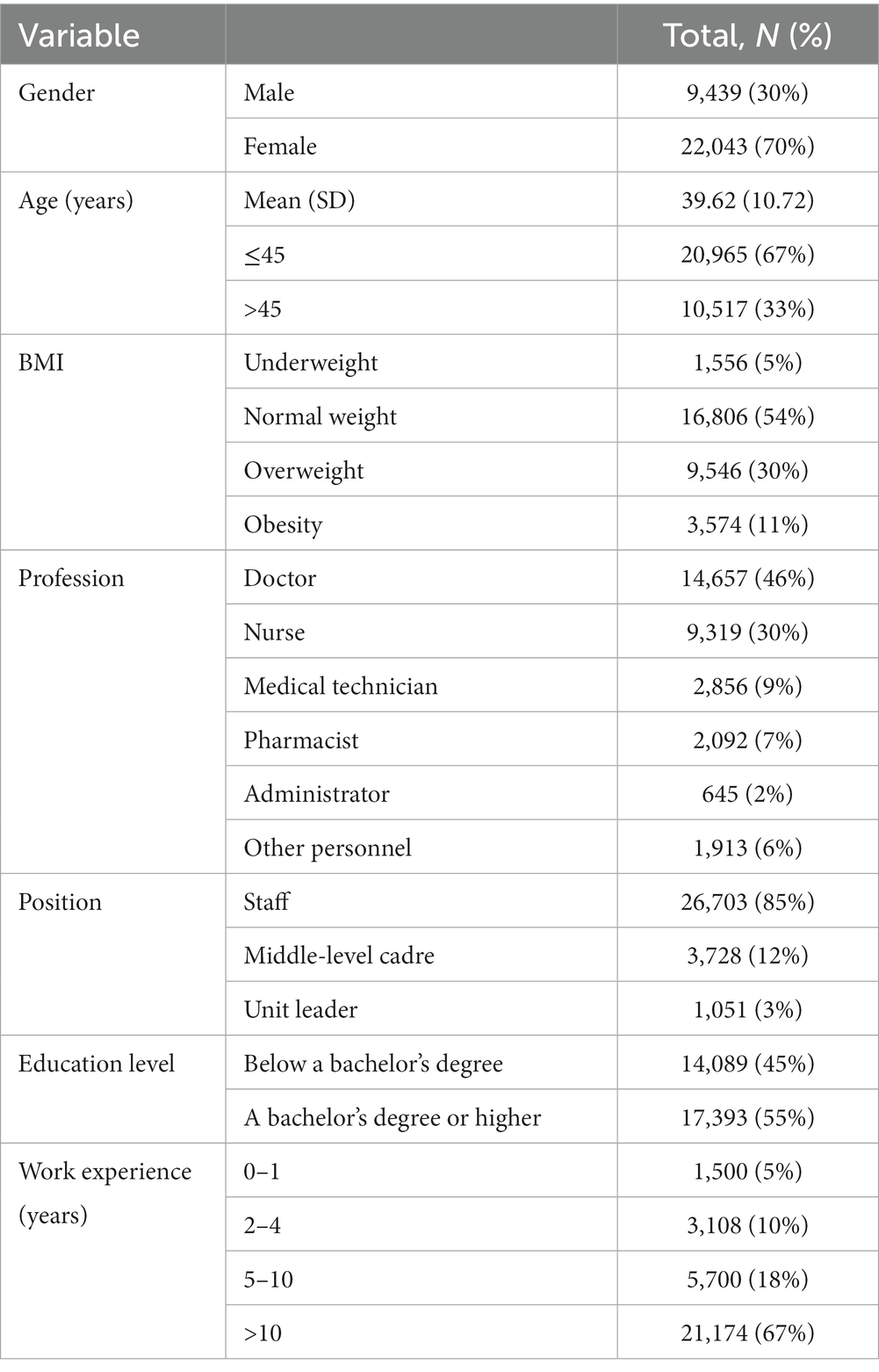
3.2 Demographic characteristics of primary HCWs
In this study, all results are analyzed based on the participation of 31,482 primary HCWs. The mean age was 39.62 years, with 67% falling within the age range of 45 years or younger, while the remaining 33% were older than 45 years. Of the participants, 9,439 (30%) were men and 22,043 (70%) were women. In total, 17,393 (55%) held a bachelor’s degree or higher, and the majority of participants were doctors (46%) and nurses (30%). For a comprehensive breakdown of the participants’ demographic characteristics, please refer to Table 1.
3.3 The prevalence and determinants of COVID-19 infection
Following the implementation of adjusted epidemic prevention and control strategies, out of the 31,482 valid questionnaires, 25,516 respondents were infected with COVID-19 and 5,966 remained uninfected, yielding an infection rate of 81.05% (95% CI: 80.61–81.48%).
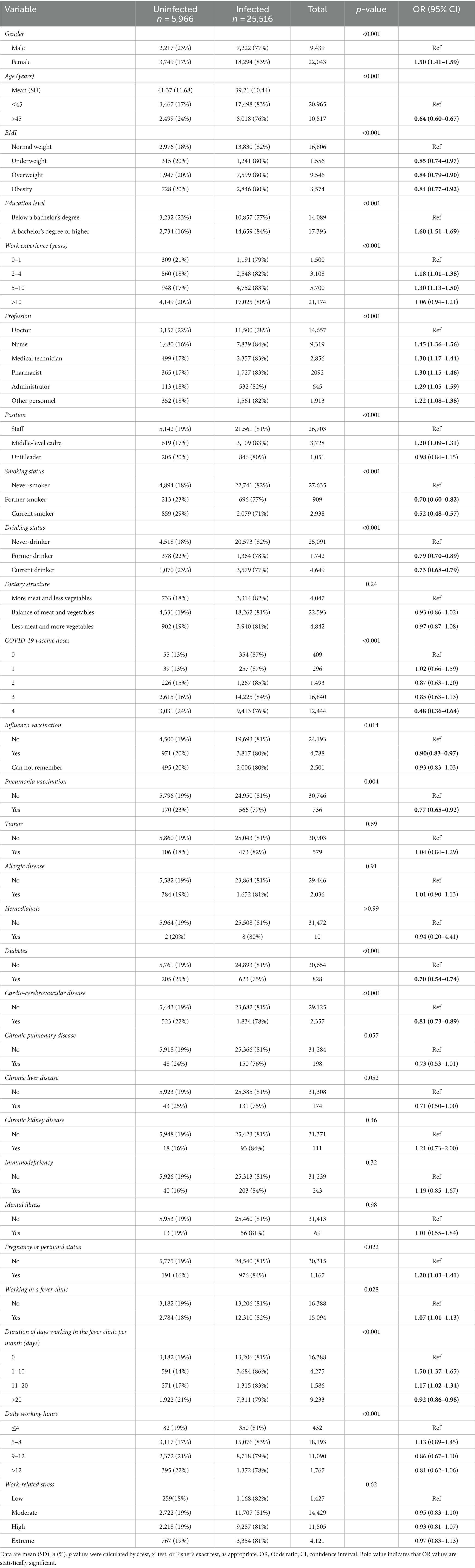
The in-depth analysis of the factors contributing to COVID-19 infection among the primary HCWs are presented in Table 2. The findings indicated that females exhibited a higher infection rate (83%) in comparison to males (77%). In the younger age group (≤ 45 years old), 83% of individuals were infected, while the infection rate among those over 45 years old was 76%. The prevalence of infection was more pronounced among participants with a bachelor’s degree or higher (84%) than those with below a bachelor’s degree (77%). Among all professional roles, nurses displayed the highest infection rate at 84%, while doctors exhibited the lowest rate at 78%. For primary HCWs who received 0, 1, 2, 3, and 4 doses of the COVID-19 vaccine, the corresponding infection rates were 87, 87, 85, 84, and 76%, with statistically significant differences observed between the infected and uninfected groups in terms of gender, age, education level, profession, and COVID-19 vaccine doses (p < 0.001).
No statistically significant differences were observed between the infected and uninfected groups in terms of dietary structure (p = 0.24), tumor (p = 0.69), allergic diseases (p = 0.91), hemodialysis (p > 0.99), chronic kidney disease (p = 0.46), immunodeficiency (p = 0.32), mental illness (p = 0.98), and work-related stress (p = 0.62). The individual characteristics of both the infected and uninfected groups are presented in Table 2.
3.4 Assessment of factors associated with COVID-19 infection among primary HCWs
The outcomes of multivariate logistic regression analysis are displayed in Table 3. The analysis revealed that an escalated risk of COVID-19 infection was correlated with female gender (aOR = 1.12, 95% CI: 1.04–1.21), possessing a bachelor’s degree or higher (aOR = 1.32, 95% CI: 1.23–1.41), accumulating over 10 years of work experience (aOR = 1.28, 95% CI: 1.11–1.47), holding a middle-level cadre position (aOR = 1.22, 95% CI: 1.11–1.35), assuming the role of a unit leader (aOR = 1.30, 95% CI: 1.11–1.54), and working in a fever clinic for 1 to 10 days per month (aOR = 1.42, 95% CI: 1.29–1.57). Conversely, advanced age (aOR = 0.76, 95% CI: 0.70–0.82), being underweight (aOR = 0.78, 95% CI: 0.69–0.90), current smoking (aOR = 0.64, 95% CI: 0.57–0.71), receiving 4 doses of COVID-19 vaccine (aOR = 0.49, 95% CI: 0.37–0.66), and pregnancy or perinatal status (aOR = 0.85, 95% CI: 0.72–0.99) were linked to a diminished risk of infection.
3.5 Symptoms observed in infected patients
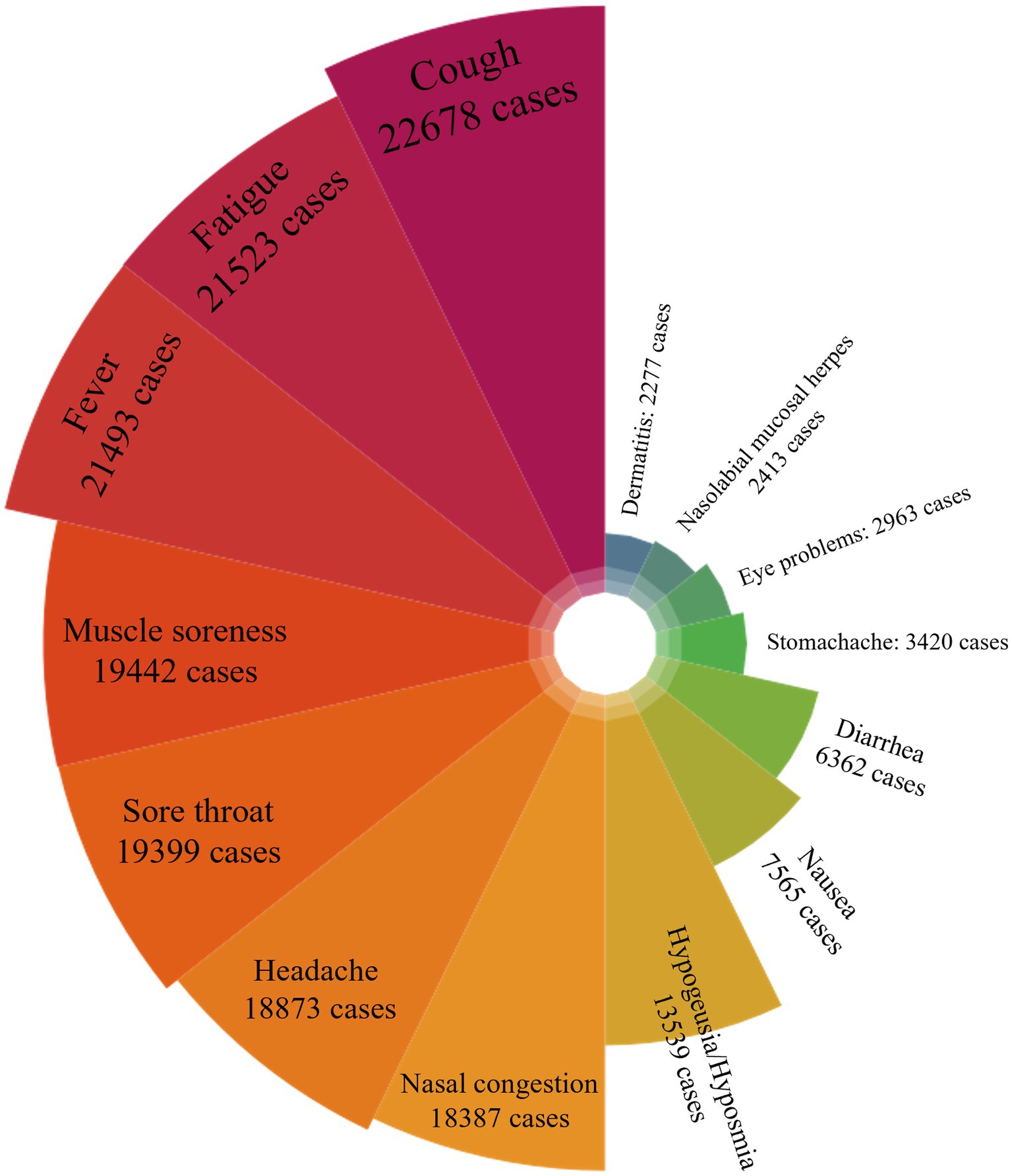
The symptoms observed in infected patients are presented in Figure 1. As per the survey, cough emerged as the most prevalent symptom among the infected patients, being reported by approximately 89% (22,678/25,516) of them. Following this, other frequently encountered symptoms included fatigue (21,523 [84%]) and fever (21,493 [84%]). For a more detailed account of the symptoms, please refer to the Supplementary material provided in an additional work document.
4 Discussion
This study offers the initial insight into the infection status of primary HCWs in Jiangsu Province, China, during the first wave of the COVID-19 epidemic, following the implementation of adjusted policies. By the conclusion of the survey, a mere 57 days after the issuance of the “Ten New Rules,” the aggregate infection rate among primary HCWs in Jiangsu province had surged to 81.05%. Li et al. conducted a comparable study and highlighted that COVID-19 infection in China was spreading at an accelerated pace compared to previous years, leading to a rapid escalation in infection rates among Chinese residents (18). The impending arrival of the Spring Festival (January 21) led to a notable surge in population movement, as individuals returned to their hometowns ahead of our survey commencement. This influx of travelers, including those who tested positive for viral nucleic acid or antigens, potentially played a role in the observed high infection rate.
In this study, the infection rate was higher among females (83%) in comparison to males (77%). Multivariate logistic regression analysis revealed that female gender constituted a risk factor for COVID-19 infection (aOR = 1.12). Existing research has consistently indicated that gender significantly influences the risk of COVID-19 infection across diverse workplaces. This trend is particularly noticeable in care-related occupations, where women tend to face elevated susceptibility to the risk of COVID-19 infection (19). In this outbreak, some primary HCWs will be dispatched from primary healthcare institutions in the province to conduct household follow-up visits to key populations in order to keep abreast of the development of the condition of positive people. This team is mainly undertaken by nursing staff, most of whom are young females, thus they indirectly increasing the chances of contact with exposures in society and have a higher risk of contracting COVID-19. In addition, women have more chances to come into contact with social infectious agents outside of working hours, such as shopping for groceries, going to the supermarket to buy household goods, and picking up and dropping off their children at school.
Notably, younger primary HCWs exhibited a higher likelihood of COVID-19 infection. Multivariate regression analysis unveiled an OR of 0.76 for individuals over 45 years old, in contrast to those aged 45 years or younger. This finding is in line with the research conducted by scientists in Madagascar (20). However, previous studies have consistently indicated that the risk of COVID-19 infection escalates significantly with advanced age (9, 21, 22). Research has demonstrated that advanced age independently correlates with a greater viral load, potentially linked to the decline of immune function among the older adult and the manifestation of less conspicuous symptoms (23). Another plausible interpretation for the outcomes of this study could be that younger individuals may have lowered their guard and exercised fewer precautions in their professional and daily lives due to an inadequate awareness of self-protection. Additionally, it is plausible that, drawing from prior studies (9, 21, 22), hospital administrators may have intentionally allocated tasks to older workers that did not require close contact with COVID-19 patients, or alternatively, permitted them to work remotely as a measure to minimize exposure (24). Further, the accelerated development of herd immunity within the younger population might potentially result in fewer severe cases (25).
Due to the high incidence of infections among young people, this may cause a significant short-term shock to the healthcare service, leading to greater strain on the healthcare system. Although there were differences in infection rates between men and women, both groups exhibited a higher infection rate. Therefore, before the next outbreak, it is necessary to have a back-up population and to adopt a shift system for primary HCWs, which may avoid a shortage of critical care staff or a breakdown of the entire healthcare system.
Upon adjusting for age, gender, and other confounding factors, we observed a notable decrease in the relative risk of COVID-19 infection associated with the administration of a fourth dose of COVID-19 vaccine. In comparison to individuals who had never received the COVID-19 vaccine, those who had received four doses exhibited an OR of 0.49. From December 1, 2022 to February 6, 2023, the prevalent strains of the new coronavirus in China were BA.5.2.48 and BF.7.14, both subbranches of the Omicron variant BA.5 (26). Researches have established that a two-dose regimen of BNT162b2 conferred 95% protection against COVID-19 in persons 16 years of age or older (27), a third dose of the COVID-19 vaccine offers effective protection against Omicron (28, 29), although these protection wane over time, a fourth dose has the potential to restore antibody levels (30). BNT162b2 vaccine has been shown to be highly effective in preventing COVID-19 symptomatic infections, as well as for the more serious outcomes: hospitalization, severe illness, and death (31). Among adults older than 55 years who had received 3 doses of BNT162b2, immunogenicity against Omicron BA.1 increased considerably with the omicron BA.1–adapted BNT162b2 vaccines than with the original dose of BNT162b2 (32). In our study, the collective infection rate among primary HCWs reached 81.05%. Conversely, among those who had received the fourth dose of the COVID-19 vaccine, the infection rate diminished to 76%. However, only 40% of primary HCWs had received the fourth dose of the vaccine, with 2% of primary HCWs either had received a single dose or remained unvaccinated. This suggested the necessity for maintaining COVID-19 vaccination, the need for prompt promotion of COVID-19 booster immunization for HCWs and gradually extension of such efforts to the entire population. This approach will not only safeguard HCWs but also curtail the risk of potential nosocomial infections among hospitalized patients.
Among all professional roles, nurses exhibited the highest infection (84%), while doctors had the lowest rate at 78%. The average age of nurses stood at 35.08 years, contrasted with the average age of non-nurse staff at 41.52 years. Given that younger age has emerged as a risk factor for COVID-19 infection in this study, the observed age discrepancy could potentially contribute to the elevated infection rate observed among nurses. Univariate analysis outcomes indicated that nurses, medical technicians, pharmacists, administrators, and others faced a heightened risk of COVID-19 infection compared to doctors. However, after accounting for confounding factors, no discernible association surfaced between professions and COVID-19 infection among primary HCWs, aligning with other studies (20, 33). While other research (5, 34–37) has demonstrated that frontline HCWs in close proximity to COVID-19 patients encounter significantly greater infection risks, our study did not yield this evidence. This could be attributed to the release of the “Ten New Rules” in China, which eliminated the requirement for centralized isolation for positive patients, opting for home isolation whenever possible. Moreover, mandatory nucleic acid testing was abolished. Consequently, a significant number of asymptomatic cases are present, escalating the risk of exposure in the absence of proper personal protective equipment (PPE) (38, 39). It has been confirmed that exposure to COVID-19-positive family members or co-workers considerably amplifies the risk of COVID-19 infection (33, 40). Although hospitals make it mandatory for primary HCWs to wear PPE, which is impossible to be worn at all times, so primary HCWs can be exposed in the community or infected at home. Collective transmission within households might be a primary factor fueling the rapid dissemination of this epidemic.
This study possessed several strengths: the respondents were HCWs in primary healthcare institutions, ensuring easy access to samples that were highly cooperative. Moreover, the majority of respondents possessed both preventive and medical knowledge, enhancing the accuracy of self-reported results. The quality of response data demonstrated a high level of accuracy, contributing to the reliability of the findings. Additionally, the study indirectly provided insight into the infection rate of a specific group.
However, our study did entail certain limitations. Firstly, given that nucleic acid testing is no longer obligatory, the group of individuals who displayed no COVID-19-related symptoms and did not undergo nucleic acid or antigen testing might encompass asymptomatic cases. Consequently, the self-reported overall infection rate among the subjects examined in this study might potentially underestimate the actual infection rate. Secondly, our questionnaire was not designed to be comprehensive enough, for example, it lacked information on travel modes, compliance with precautionary measures, and the extent of PPE utilization, all of which could constitute significant factors influencing virus transmission. Thirdly, as a cross-sectional survey, our study’s scope was limited to a snapshot in time, preventing the capture of the dynamic progression of the epidemic, and due to the online self-administered format, we did not capture critically ill patients or those who died and older adult people may not be proficient in cell phone operation, potentially leading to selection bias. Fourthly, although a pre-survey was conducted with our team and 20 graduate students majoring in public health before the actual survey to revise the question formulation, the final questionnaire was filled out remotely and lacked on-site communication and explanation, and thus there may have been a certain bias in the understanding of the same question between the questionnaire filler and researchers.
5 Conclusion
Our study aimed to assess the prevalence and pinpoint the factors linked to COVID-19 infection among primary HCWs in Jiangsu Province subsequent to the implementation of adjusted epidemic prevention and control strategies. The results showed that the overall infection rate among primary HCWs stood at 81.05%, with a 95% CI of 80.61–81.48%. Being younger and female primary HCWs were noted risk factors for COVID-19 infection, and COVID-19 vaccines can significantly mitigate the infection rate. In conclusion, assessment of infection risks confronted by HCWs during the initial wave of the COVID-19 epidemic, after the implementation of adjusted epidemic prevention and control strategies, stands to improve preparedness for timely protective actions in anticipation of subsequent epidemic waves. This proactive approach will be instrumental in substantially curtailing the occurrence of re-positive HCWs and reducing the infection rate within the broader population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Jiangsu Provincial Center for Disease Prevention and Control (Reference number: JSJK2023-B010-01). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BL: Data curation, Formal analysis, Software, Writing – original draft, Investigation. RM: Data curation, Formal analysis, Software, Writing – original draft, Investigation. JX: Investigation, Project administration, Resources, Supervision, Writing – review & editing. YZ: Investigation, Project administration, Resources, Supervision, Writing – review & editing. HG: Funding acquisition, Investigation, Resources, Supervision, Writing – review & editing. HC: Data curation, Investigation, Software, Writing – review & editing. PM: Investigation, Software, Writing – review & editing. YQ: Investigation, Software, Writing – review & editing. BX: Funding acquisition, Investigation, Writing – review & editing. YS: Conceptualization, Writing – review & editing, Investigation, Supervision, Resources. BC: Conceptualization, Writing – review & editing, Data curation, Investigation, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by Health Commission of Nanjing, China (ZKX22019) and the 2022 annual open project of Jiangsu Provincial Primary Health Development and General Practice Medical Education Research Center (No. 2022A02).
Acknowledgments
The authors would like to thank Professor Qiao-Hong Chen from California State University, Fresno, for her valuable proofreading assistance in refining this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1297770/full#supplementary-material
Abbreviations
aOR, adjusted Odds Ratio; BMI, Body Mass Index; CI, Confidence Interval; COVID-19, Coronavirus Disease 2019; HCWs, Healthcare Workers; OR, Odds Ratio; PPE, Personal Protective Equipment; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; SD, Standard Deviation.
References
1. Zhu, N, Zhang, D, Wang, W, Li, X, Yang, B, Song, J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. Huang, C, Wang, Y, Li, X, Ren, L, Zhao, J, Hu, Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China The Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
3. WHO. Coronavirus Disease (COVID-19) Dashboard Available at: https://covid19.who.int/ (accessed May 10, 2023).
4. Black, JRM, Bailey, C, Przewrocka, J, Dijkstra, KK, and Swanton, C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. (2020) 395:1418–20. doi: 10.1016/S0140-6736(20)30917-X
5. Iversen, K, Bundgaard, H, Hasselbalch, RB, Kristensen, JH, Nielsen, PB, Pries-Heje, M, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. (2020) 20:1401–8. doi: 10.1016/S1473-3099(20)30589-2
6. Zheng, L, Wang, X, Zhou, C, Liu, Q, Li, S, Sun, Q, et al. Analysis of the infection status of healthcare Workers in Wuhan during the COVID-19 outbreak: a cross-sectional study. Clin Infect Dis. (2020) 71:2109–13. doi: 10.1093/cid/ciaa588
7. Kirby, T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. (2020) 8:547–8. doi: 10.1016/S2213-2600(20)30228-9
8. Hughes, MM, Groenewold, MR, Lessem, SE, and Xu, K. Update: characteristics of health care personnel with COVID-19 - United States, February 12-July 16, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1364–8. doi: 10.15585/mmwr.mm6938a3
9. Rozenfeld, Y, Beam, J, Maier, H, Haggerson, W, Boudreau, K, Carlson, J, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. (2020) 19:126. doi: 10.1186/s12939-020-01242-z
10. Rosofsky, A, Levy, JI, Zanobetti, A, Janulewicz, P, and Fabian, MP. Temporal trends in air pollution exposure inequality in Massachusetts. Environ Res. (2018) 161:76–86. doi: 10.1016/j.envres.2017.10.028
11. Riley, WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. (2012) 123:167–74.
12. Dzinamarira, T, Murewanhema, G, Mhango, M, Iradukunda, PG, Chitungo, I, Mashora, M, et al. COVID-19 prevalence among healthcare workers. A systematic review and Meta-analysis. Int J Environ Res Public Health. (2022) 19:146. doi: 10.3390/ijerph19010146
13. Soham, B, Ronnie, EB, Murtaza, K, Muath, A, Daniel, KO, Yara, B, et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health. (2020) 5:e003097. doi: 10.1136/bmjgh-2020-003097
14. COVID-19 Prevention and Control Measures. Notice on Further Optimizing the Precision of COVID-19 Prevention and Control Measures for Scientific Implementation. Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202211/ed9d123bbfe14e738402d846290049ea.shtml (accessed May 22, 2023).
15. Prevent and Control the COVID-19 Outbreak. Notice on Further Optimizing the Implementation of Measures to Prevent and Control the COVID-19 Outbreak. Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202212/8278e7a7aee34e5bb378f0e0fc94e0f0.shtml (accessed May 22, 2023).
16. Bei-Fan, Z. China tCM-aGoWGoOi. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Asia Pac J Clin Nutr. (2002) 11:S685–93. doi: 10.1046/j.1440-6047.11.s8.9.x
17. Wei, Y, Gao, W, Zhang, L, Wang, S, Zhan, S, Ren, T, et al. Epidemiological survey of 2019-nCoV infection in staff and students in some public health schools in China. Chin J Epidemiol. (2023) 44:175–83. doi: 10.3760/cma.j.cn112338-20221231-01092
18. Li, Y, Wang, S, Yang, N, Shi, Y, Yang, Y, Zhu, Z, et al. Analysis on the factors associated with COVID-19 infection among Chinese residents after the implementation of the 10 new rules to optimize COVID-19 response: a cross-sectional study. Front Public Health. (2023) 11:11. doi: 10.3389/fpubh.2023.1197889
19. Lee, J. The gendered outbreak of COVID-19 in South Korea. Fem Econ. (2022) 28:89–111. doi: 10.1080/13545701.2022.2057565
20. Ratovoson, R, Raberahona, M, Razafimahatratra, R, Randriamanantsoa, L, Andriamasy, EH, Herindrainy, P, et al. SARS-CoV-2 infection rate in Antananarivo frontline health care workers, Madagascar. Influenza Other Respir Viruses. (2022) 16:994–1003. doi: 10.1111/irv.13022
21. Hu, L, Chen, S, Fu, Y, Gao, Z, Long, H, Ren, H-w, et al. Risk factors associated with clinical outcomes in 323 coronavirus disease 2019 (COVID-19) hospitalized patients in Wuhan, China. Clin Infect Dis. 71:2089–98. doi: 10.1093/cid/ciaa539
22. Zhou, F, Yu, T, Du, R, Fan, G, Liu, Y, Liu, Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
23. Feng, C, Hong, S, Fan, R, Shi, X, Ma, Z, Li, C, et al. Age and sex differences among mildly symptomatic and asymptomatic patients with omicron infection in 2022 in Shanghai, China. J Multidiscip Healthc. (2022) 15:1909–19. doi: 10.2147/JMDH.S375724
24. Robles-Pérez, E, González-Díaz, B, Miranda-García, M, and Borja-Aburto, VH. Infection and death by COVID-19 in a cohort of healthcare workers in Mexico. Scand J Work Environ Health. (2021) 47:349–55. doi: 10.5271/sjweh.3970
25. Mbow, M, Lell, B, Jochems, SP, Cisse, B, Mboup, S, Dewals, BG, et al. COVID-19 in Africa: dampening the storm? Science. (2020) 369:624–6. doi: 10.1126/science.abd3902
26. National COVID-19 Infection Situation. National COVID-19 Infection Situation. Available at: https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_13141/202302/t20230208_263674.html (accessed May 22, 2023).
27. Polack, FP, Thomas, SJ, Kitchin, N, Absalon, J, Gurtman, A, Lockhart, S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. (2020) 383:2603–15. doi: 10.1056/NEJMoa2034577
28. Andrews, N, Stowe, J, Kirsebom, F, Toffa, S, Rickeard, T, Gallagher, E, et al. Covid-19 vaccine effectiveness against the omicron (B.1.1.529) variant. N Engl J Med. (2022) 386:1532–46. doi: 10.1056/NEJMoa2119451
29. Moreira, ED, Kitchin, N, Xu, X, Dychter, SS, Lockhart, S, Gurtman, A, et al. Safety and efficacy of a third dose of BNT162b2 Covid-19 vaccine. N Engl J Med. (2022) 386:1910–21. doi: 10.1056/NEJMoa2200674
30. Regev-Yochay, G, Gonen, T, Gilboa, M, Mandelboim, M, Indenbaum, V, Amit, S, et al. Efficacy of a fourth dose of Covid-19 mRNA vaccine against omicron. N Engl J Med. (2022) 386:1377–80. doi: 10.1056/NEJMc2202542
31. Dagan, N, Barda, N, Kepten, E, Miron, O, Perchik, S, Perchik, S, et al. BNT162b2 mRNA Covid-19 vaccine in a Nationwide mass vaccination setting. N Engl J Med. (2021) 384:1412–23. doi: 10.1056/NEJMoa2101765
32. Winokur, P, Gayed, J, Fitz-Patrick, D, Thomas, SJ, Diya, O, Lockhart, S, et al. Bivalent omicron BA.1–adapted BNT162b2 booster in adults older than 55 years. N Engl J Med. (2023) 388:214–27. doi: 10.1056/NEJMoa2213082
33. Bahrs, C, Weis, S, Kesselmeier, M, Ankert, J, Hagel, S, Beier, S, et al. Non-patient-related SARS-CoV-2 exposure from colleagues and household members poses the highest infection risk for hospital employees in a German university hospital: follow-up of the prospective co-HCW seroprevalence study. Infection. (2023) 51:1051–9. doi: 10.1007/s15010-023-01995-z
34. Modenese, A, Casolari, L, Rossi, G, Della Vecchia, E, Glieca, F, D’Elia, C, et al. Factors associated with SARS-CoV-2 infection risk among healthcare Workers of an Italian University Hospital. Healthcare. (2021) 9:1495. doi: 10.3390/healthcare9111495
35. Misra-Hebert, AD, Jehi, L, Ji, X, Nowacki, AS, Gordon, S, Terpeluk, P, et al. Impact of the COVID-19 pandemic on healthcare workers’ risk of infection and outcomes in a large, integrated health system. J Gen Intern Med. (2020) 35:3293–301. doi: 10.1007/s11606-020-06171-9
36. Stephen, RI, Olumoh, J, Tyndall, J, and Oyelola, A. Risk factors for COVID-19 infection among healthcare Workers in North-East Nigeria. Healthcare. (2022) 10:1919. doi: 10.3390/healthcare10101919
37. Nguyen, LH, Drew, DA, Graham, MS, Joshi, AD, Guo, C-G, Ma, W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. (2020) 5:e475–83. doi: 10.1016/S2468-2667(20)30164-X
38. Torjesen, I. Covid-19: appropriate PPE prevents infections in doctors in frontline roles, study shows. BMJ. (2020) 369:m2330. doi: 10.1136/bmj.m2330
39. Zhao, Y, Liang, W, Luo, Y, Chen, Y, Liang, P, Zhong, R, et al. Personal protective equipment protecting healthcare workers in the Chinese epicentre of COVID-19. Clin Microbiol Infect. (2020) 26:1716–8. doi: 10.1016/j.cmi.2020.07.029
Keywords: healthcare workers, COVID-19, infection, China, influencing factors
Citation: Lu B, Ma R, Xu J, Zhang Y, Guo H, Chen H, Miao P, Qian Y, Xu B, Shen Y and Chen B (2023) Primary healthcare workers’ COVID-19 infection status following implementation of adjusted epidemic prevention and control strategies: a cross-sectional study in Jiangsu, China. Front. Public Health. 11:1297770. doi: 10.3389/fpubh.2023.1297770
Edited by:
Khem Pokhrel, Development and Research Service International Nepal, NepalReviewed by:
Dipak Prasad Upadhyaya, Case Western Reserve University, United StatesPatrick M. D’Aoust, University of Ottawa, Canada
Copyright © 2023 Lu, Ma, Xu, Zhang, Guo, Chen, Miao, Qian, Xu, Shen and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ya Shen, MTIwNTkyNDk4QHFxLmNvbQ==; Bingwei Chen, ZHJjaGVuYndAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Beier Lu
Beier Lu Rongji Ma
Rongji Ma Jinshui Xu
Jinshui Xu Yongjie Zhang
Yongjie Zhang Haijian Guo
Haijian Guo Hualing Chen
Hualing Chen Pengcheng Miao
Pengcheng Miao Yongkang Qian
Yongkang Qian Biyun Xu
Biyun Xu Ya Shen
Ya Shen Bingwei Chen
Bingwei Chen