- 1Faculty of Humanities and Arts, Macau University of Science and Technology, Taipa, Macau SAR, China
- 2Department of Hepatology, The 4th People's Hospital of Qinghai Province, Xining, Qinghai, China
- 3Operation Management Centre, Guangzhou Wanqu Cooperative Institute of Design, Guangzhou, Guangdong, China
- 4State Key Laboratory of Quality Research in Chinese Medicines, Macau University of Science and Technology, Taipa, Macau SAR, China
- 5Faculty of Chinese Medicine, Macau University of Science and Technology, Taipa, Macau SAR, China
- 6Guangdong-Hong Kong-Macao Joint Laboratory for Contaminants Exposure and Health, Guangzhou, Guangdong, China
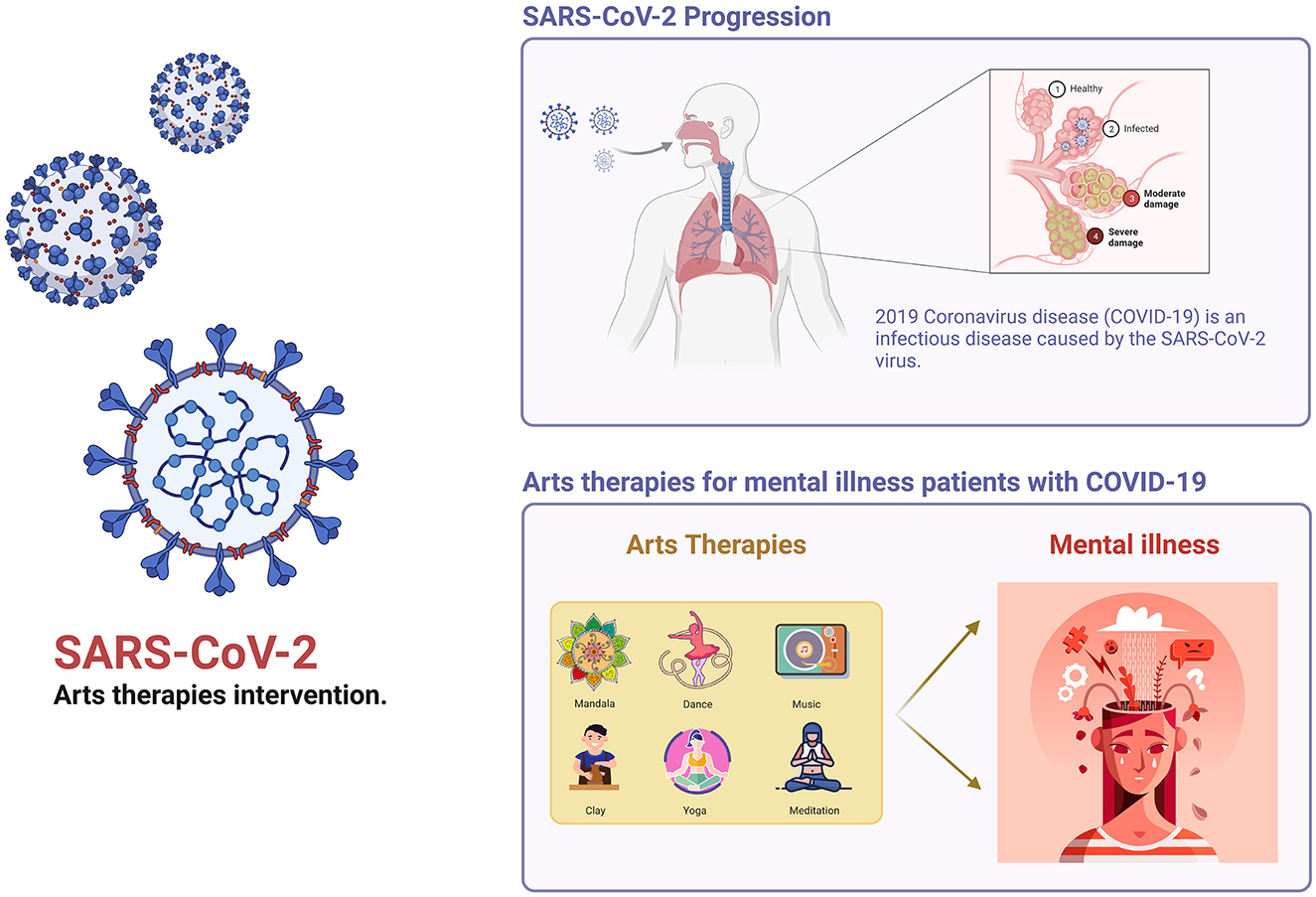
Background and objective: The COVID-19 global pandemic has necessitated the urgency for innovative mental health interventions. We performed a comprehensive review of the available literature on the utility and efficacy of arts therapies in treating mental health problems, with special emphasis on their deployment during the COVID-19 pandemic, aiming to provide some evidence for the application of this therapy.
Methods: The potential studies were systematically sourced from five authoritative databases: PubMed, Embase, the Cochrane Library, Web of Science, and the CNKI database. The evaluation of these studies was conducted based on stringent criteria, including validity, suitability, therapeutic potential, and consistency. Each piece of included literature was meticulously scored in accordance with these criteria, thus ensuring the inclusion of only the most robust studies in this review. The data from these Randomized Controlled Trials (RCTs) were carefully extracted using the PICO(S) framework, ensuring a comprehensive and systemic approach to data collection. In order to emphasize the variability in the effects of differing arts therapies on COVID-19-induced psychiatric disturbances, the sourced literature was systematically categorized and scrutinized based on distinct modalities.
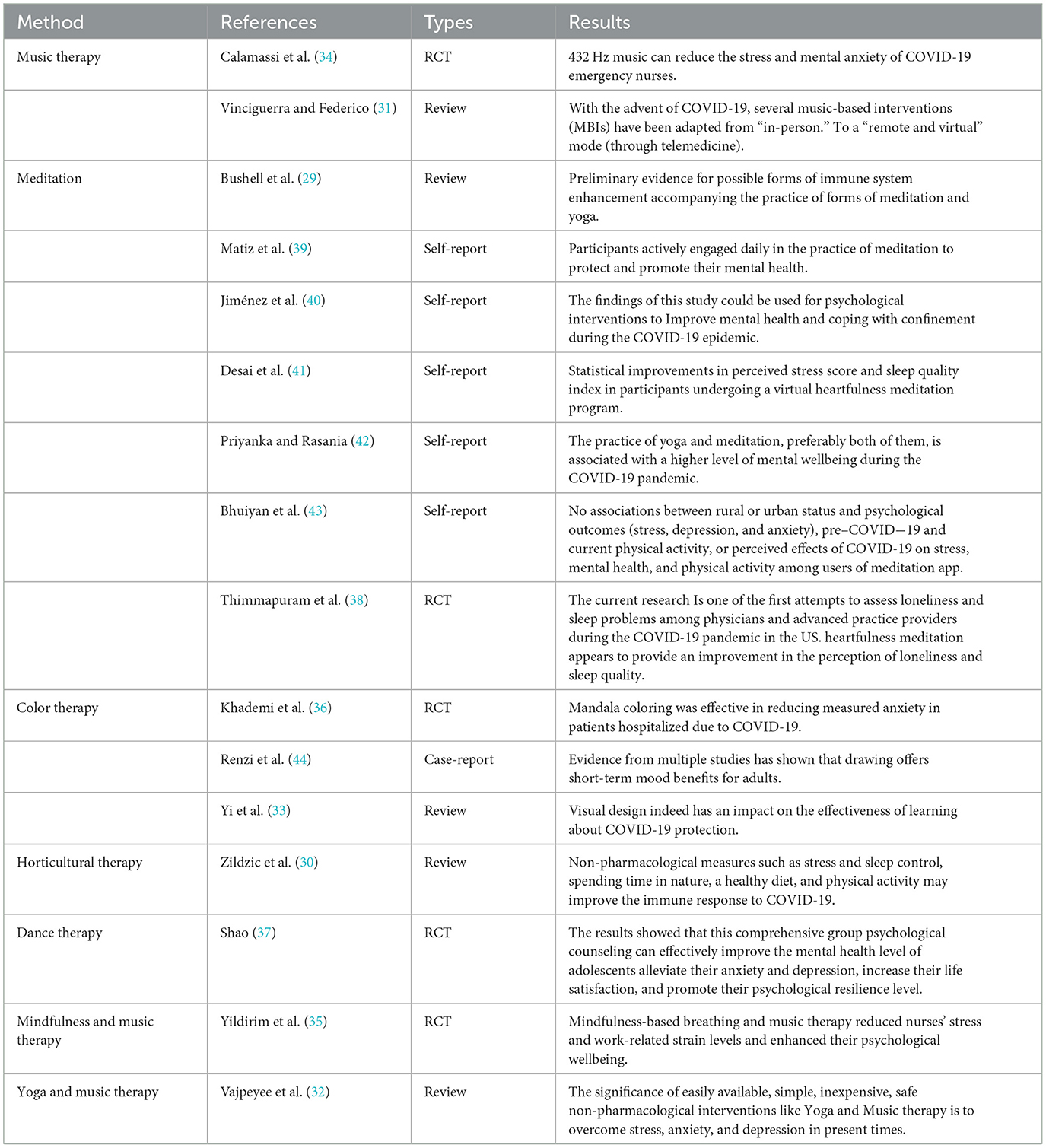
Results: Out of the 7,250 sourced articles, 16 satisfied the inclusion conditions. The therapies were predominantly meditation (n = 7), supplemented by individual studies on color therapy (n = 3), music therapy (n = 2), and single studies on horticultural therapy, dance therapy, mindfulness and music therapy, and yoga and music therapy (n = 4 collectively). These various forms of arts therapies had a positive short to medium-term impact on the mental health of COVID-19 patients. Besides improving patients' physical and mental health, these therapies can also be employed to mitigate mental health issues among healthcare professionals.
Conclusion: The COVID-19 pandemic has profound and long-lasting implications for public mental health. Diverse forms of arts therapies are potentially effective in addressing related psychiatric symptoms. The integration of artificial intelligence might further enhance the efficacy and scalability of arts therapies in future implementations.
1 Introduction
As of August 13, 2023, the cumulative number of COVID-19 cases and related variants reached 769 million globally. The global death amounted to 6.9 million, accounting for 0.08% of the global population (1). The COVID-19 pandemic has far-reaching impacts on various societal sectors, generates considerable stress among healthcare workers (2, 3), and induces significant emotional strain on the general population due to the extensive infection rates and associated mortality (4–6). This considerable burden leads to psychological and mental health problems, emanating not only from the physical symptoms of the disease but also from various stressors (7, 8).
The COVID-19 pandemic, as reported by the World Health Organization, has given rise to multitudinous stressors, which notably include economic hardships, disease prevalence, workforce reductions, and rigid governmental policies (9–11). Such stressors significantly exacerbate mental health issues, leading to a broad spectrum of psychological disorders. If these emerging psychological health challenges are not addressed promptly, they could escalate into severe conditions such as anxiety, depression, intense stress, profound sorrow, suicidal ideations, and feelings of isolation. These conditions may subsequently induce more severe disorders like eating disorders, obsessive-compulsive disorder, and traumatic stress responses, further weakening the body's immune responses (12). Affected demographics encompass individuals with pre-existing mental health conditions, women, parents, the older adult, racial minorities, children, college students, and military personnel, with those having a history of psychological disorders or predisposition to isolation exhibiting heightened vulnerability (13, 14).
In the context of recurring COVID-19 outbreaks and the concomitant governmental policies and quarantines, there was an increase in psychiatric symptoms across both infected and uninfected populations, which was further aggravated by a shortage of specialized medical facilities and the lack of immediate treatment options (15). This situation accentuated the need for practical, economical therapeutic strategies that extend beyond conventional pharmaceutical treatments. These strategies ought to effectively manage these symptoms and thus improve people's quality of life. Therefore, the time is ripe to consider the potential of alternative therapeutic interventions, such as art therapy, a well-established method, to address the psychological health issues resulting from COVID-19 and Post-Acute COVID-19 Syndrome.
This review primarily focused on utilizing arts therapies to treat psychological disorders in COVID-19 patients. According to the British Association for Art Therapy (BAAT), art therapy is “a form of psychotherapy that uses art media as its primary mode of expression and communication” to support individuals in distress (16). According to the American Art Therapy Association (AATA), Through integrative methods, art therapy engages the mind, body, and spirit in ways that are distinct from verbal articulation alone. Art Therapy offers numerous sub-disciplines to combat distinct mental ailments, frequently employing a variety of artistic mediums in both group and individual environments (17). The current review primarily concerns itself with the following research issues:
Which literature can be incorporated into the discussion about the effectiveness of arts therapies for the mental health problems of COVID-19 patients?
What distinct sub-therapies can effectively address specific mental health issues?
How can the efficiency of arts therapies be elevated in the future for large-scale populations?
review aims to contribute to the respective literature by identifying the mechanisms of action, consolidating the consensus on the effectiveness of arts therapies, discussing persisting issues in research design, and suggesting future steps for advancing the application of arts therapies in treating mental disorders (18, 19).
2 Materials and methods
2.1 Searching literature about the arts therapies
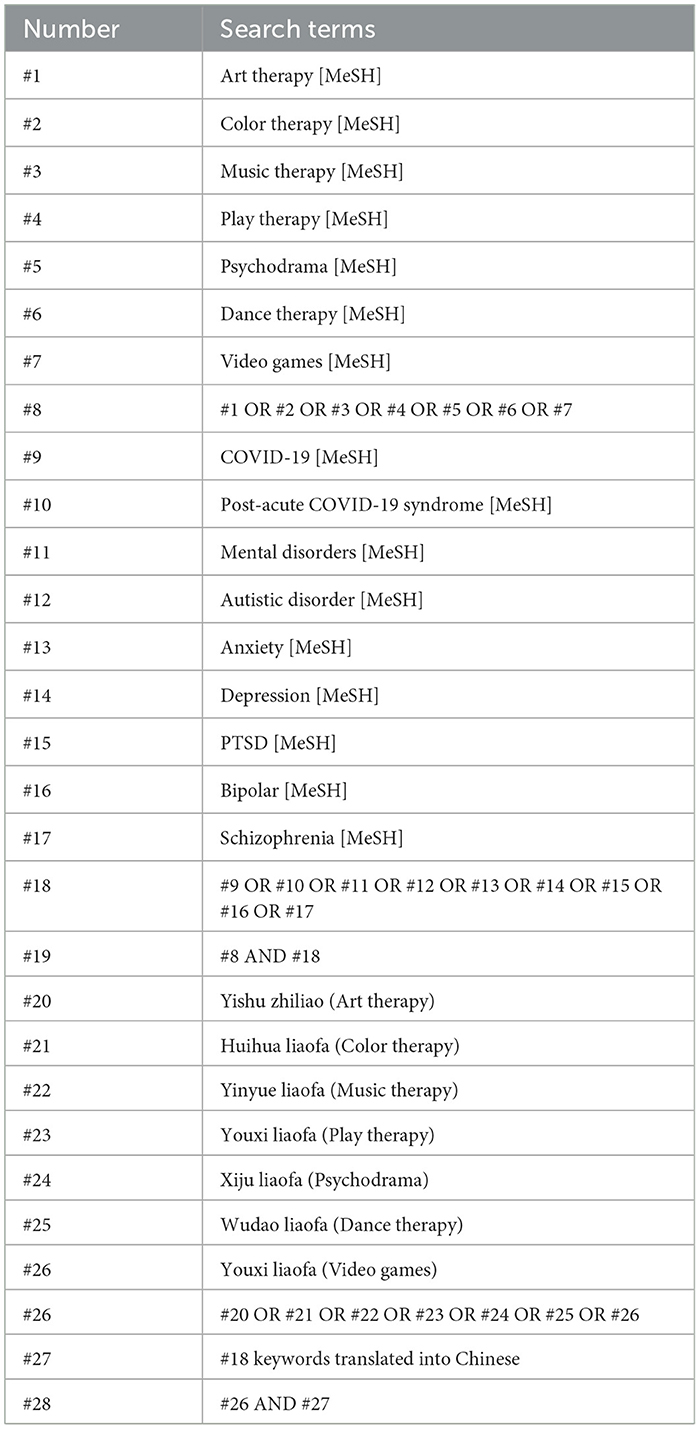
A methodical search was performed on PubMed, Cochrane Library databases, Embase, Web of Science, and CNKI databases to review the literature and identify relevant articles comprehensively. Utilizing MeSH tags such as “art therapy,” “music therapy,” “dance therapy,” “color therapy,” “play therapy,” “drama therapy,” and “video games”, these keywords were combined with terms like “COVID-19,” “Post-Acute COVID-19 Syndrome,” “mental disorder,” “autistic disorder,”, “schizophrenia,” “depression,” “bipolar disorder,” “anxiety,” and “post-traumatic stress disorder (PTSD).” The timeframe for this literature search was limited to articles published from January 2000 to July 2023, as further expounded in Table 1. Inclusion criteria mandated the incorporation of creative art therapies for mental illnesses by the categories delineated above. Any articles that were not available in the English language were consequently excluded from consideration.
The search method was derived from the PubMed database and applied to additional databases. This formula was used consistently across all databases: (“Art Therapy”[Mesh]) OR “Music Therapy”[Mesh]) OR “Color Therapy”[Mesh]) OR “Play Therapy”[Mesh]) OR “Dance Therapy”[Mesh]) OR “Psychodrama”[Mesh]) OR “Video Games”[Mesh]) AND “COVID-19”[Mesh]) OR “Post-Acute COVID-19 Syndrome”[Mesh]) AND (“Mental Disorders”[Mesh]) OR “Autistic Disorder”[Mesh]) OR “Anxiety”[Mesh]) OR (“Depression”[Mesh] OR “Depressive Disorder”[Mesh])) OR “Stress Disorders, Post-Traumatic”[Mesh]) OR “Bipolar Disorder”[Mesh]) OR “Schizophrenia”[Mesh]).
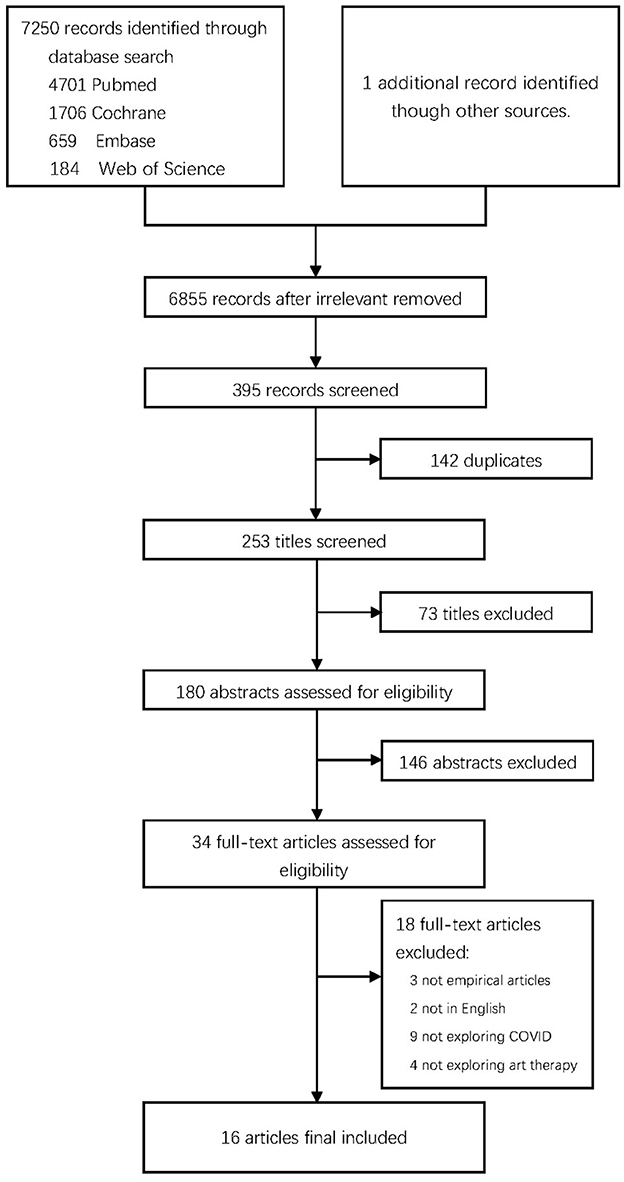
A total of 7,250 citations conforming to the search criteria were identified, from which 34 full texts underwent examination (refer to Table 1; Figure 1).
The framework illustrated in Figure 1 outlines the inclusion and exclusion criteria for the study. Articles were rigorously screened based on these criteria, posed as three questions: 1. Does the article's content pertain to COVID-19, post-COVID-19, and arts therapies or its sub-therapies? 2. Does the article provide relevant data to validate the application of arts therapies? 3. Does the article possess significant value? The first two questions guided the initial screening and subsequent literature review.
The third question was instrumental in determining the three exclusion criteria: 1. Insufficient value in the literature. 2. non-English literature. 3. Literature classified under “gray literature.” During the literature screening process, it became apparent that certain interventions were defined ambiguously, thereby complicating the differentiation between art psychotherapy applications and the mere utilization of art for recreational purposes or the acquisition of artistic skills. By adhering to this criterion, studies were assessed exclusively for their exploration of arts therapies, ensuring the elimination of any ambiguities in intervention classification.
We included papers relating to the MATISSE trial identified in the search to review them in light of the more exhaustive research (19, 20).
3 Results
3.1 Method of quality appraisal
Two independent reviewers, LXX and JW, were involved during the screening, eligibility, and inclusion review process. LXX was responsible for downloading and reviewing the screened articles, excluding irrelevant literature. The relevant literature was then forwarded to JW for eligibility review. JW assessed the eligibility of the literature to be included in the analyses. The literature that met the eligibility criteria underwent a double inspection by both LXX and JW.
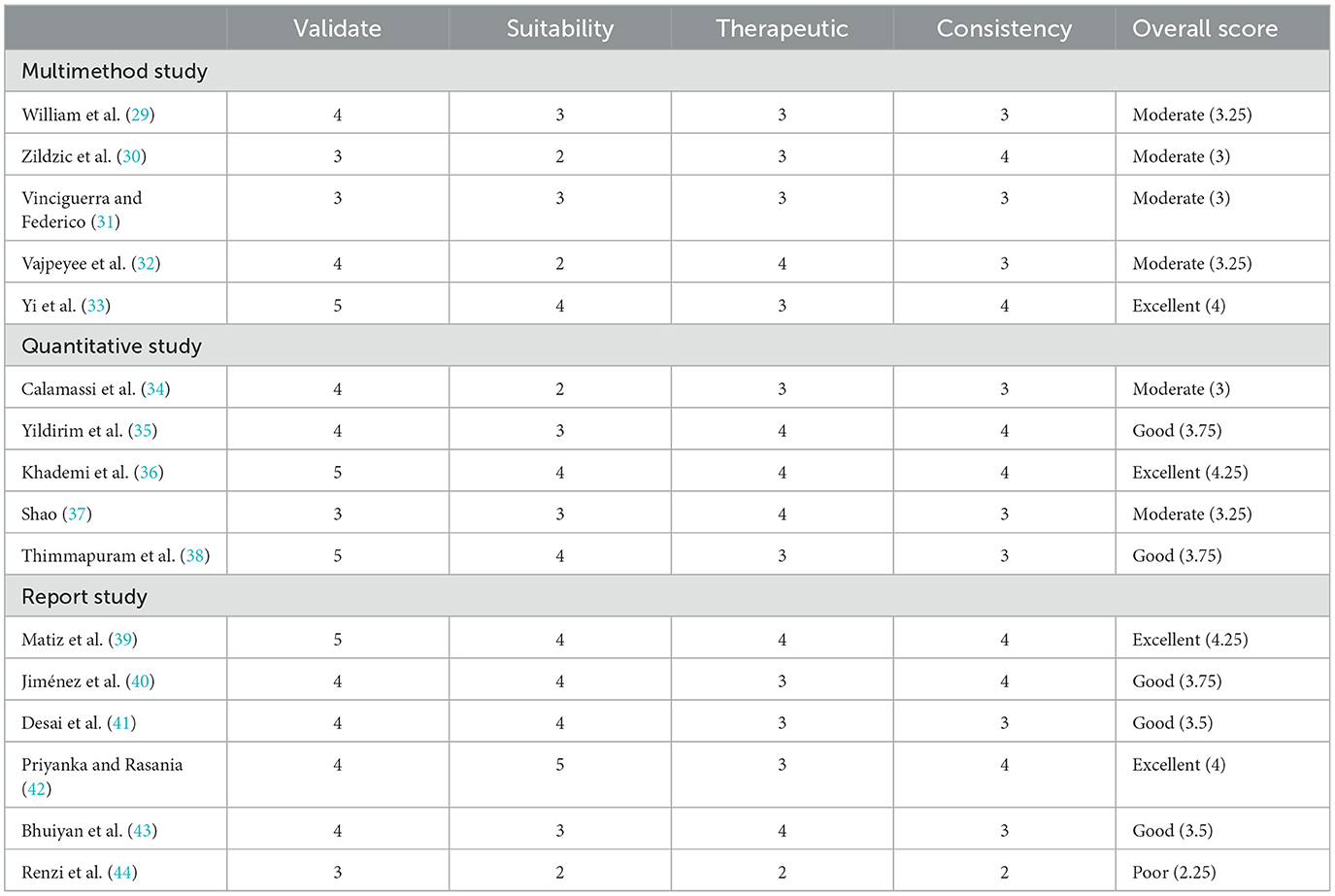
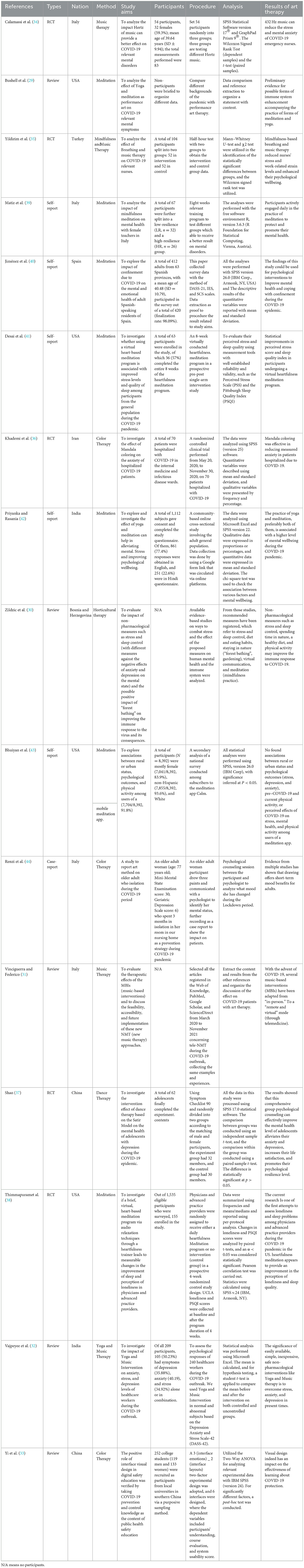
The 16 selected articles delivered precise data and research content. Their quality was evaluated by a multimethod framework established based on standardized criteria (21). This framework relied on multiple strategies to extract and analyze data and content from the pertinent references (22), incorporating qualitative (23), multi-method (24), target audience, and RCT strategies (25). The analysis method was updated in light of two papers (26, 27); in adherence to the Center for Review and Dissemination's recommendations, an extra researcher was included to solidify the framework (28). The finalized framework encompassed four primary quality categories, with each article being assessed based on these criteria: Validate, Suitability, Therapeutic, and Consistency. Scores were assigned to each category, and the average score of all four categories determined the article's overall quality rating and robustness as excellent, good, moderate, or poor. To resolve discrepancies in ratings, WJ and independent researchers conducted a calibration of quality ratings on samples from 16 studies (see Table 2); we used study design by PICO[S] to identify RCT data in these 16 studies (see Table 3).
LXX extracted data from each study using a grid that summarized information relevant to the goals of the review (Table 4). JW randomly selected the papers to double-check to avoid missing or inaccurate data.
In this review, we presented a descriptive synthesis of qualitative and methodological aspects of the papers considered in five quality categories.
3.2 Treatment method
The Taiwan Association for Art Therapy (TATA) believes that the expression of art therapy often utilizes mental images for reflection. That art involves the client applying their perceptions and senses. In contrast, the Hong Kong Association of Art Therapists (HKAAT) believes that Art Therapy is about using art as a communication tool. Through the therapeutic relationship, emotional, psychosocial, and developmental needs are addressed to effect lasting change. In summary, arts therapies' core lies in the driving force of art, which itself is diverse in its forms of expression; arts therapies encompass a variety of concepts, rendering it a complex therapeutic approach due to its diverse types (45). Commonly associated with psychology and psychiatry (46–50), arts therapies include music therapy (32, 51–53), mandala-color therapy (36, 54), creative art therapy (45, 55, 56), dance therapy (53, 57), play or game therapy (58–61), and meditation or yoga therapy (29, 39, 41, 42, 62, 63). These art therapies comprise proactive approaches—such as mandala coloring, dance therapy, and meditation therapy—where patients focus on the activity to divert negative mental attention. Conversely, reactive approaches like music therapy or art gallery-based projects entail patients receiving positive stimuli from external sources to benefit their mental health (64), the article presents a tabular representation that effectively illustrates the outcomes derived from the literature about the seven distinct therapeutic modalities (see Table 5).
Patterson and colleagues found that art therapy is typically divided into two methods: 94.4% of individuals receive art therapy from therapists, and 70.4% engage in group-based therapy with therapists (65). Art therapy treatments can be categorized as open-ended (47, 50, 66) or closed-loop (46). For controlled trials to establish the efficacy of arts therapies, participants must follow a stringent program directed by an art therapist. Individuals with severe symptoms typically necessitate lengthier interventions for optimum outcomes (47, 67, 68).
Through the examination of various therapeutic methodologies, it is evident that many individuals have encountered isolation within the framework of COVID-19 infection. Moreover, the implementation of diverse isolation policies by different nations, some involving prolonged periods of closure and seclusion, has resulted in concealed mental health issues among individuals residing in confined and inaccessible environments during isolation. These individuals often exhibit psychological sensitivity, irritability, and anxiety. However, it has been observed that arts therapy interventions can effectively mitigate or eliminate these psychological states and problems, thereby averting their progression into severe conditions over time. Art therapy has effectively reduced or eliminated certain psychological disorders and problems, mitigating the risk of these issues progressing into more severe states.
In summary, several arts therapy modalities vary in their respective intervention durations. As an illustration, engaging in activities such as listening to music and practicing meditation does not necessitate intricate apparatus or a particular setting. These therapeutic modalities can be employed amidst periods of illness and seclusion to modulate one's emotional state effectively.
3.3 The therapeutic of arts therapies
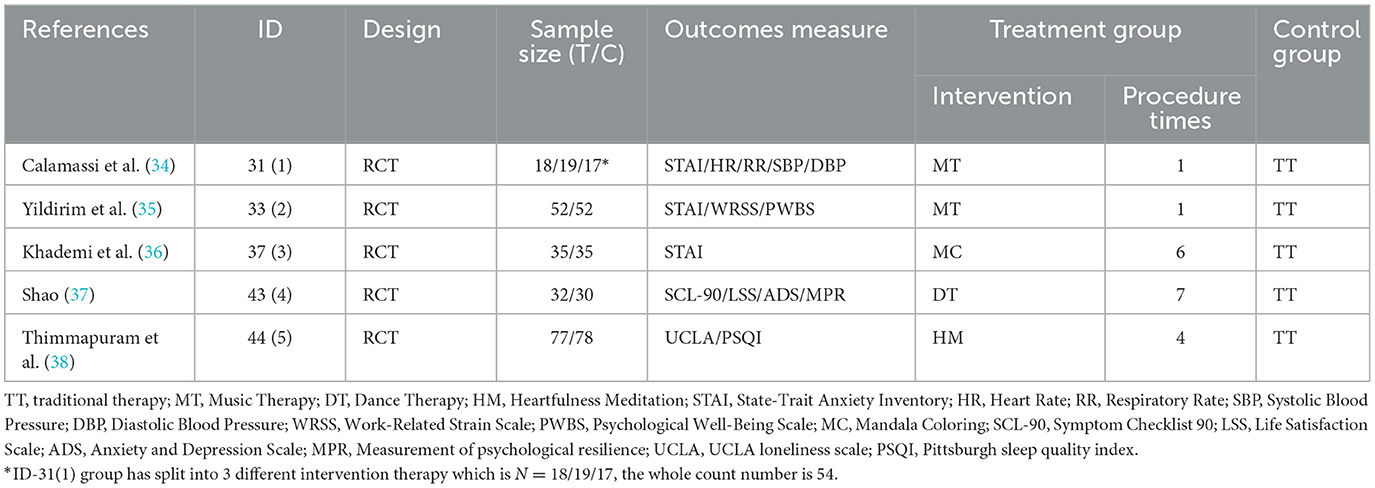
Five quantitative studies, including four randomized controlled trials (RCTs), assessed arts therapies' efficacy and therapeutic effects. The mental status of patients who received arts therapies over a specific period was compared to a control group undergoing traditional medication (34–38). Two studies focused on healthcare workers such as nurses involved in treating COVID-19 patients (34, 35), while the remaining three targeted patients with COVID-19 (36–38). These studies used various widely accepted therapeutic approaches to primarily measure quality of life outcomes and therapeutic effects, including art therapy (45), music therapy (34, 35), color therapy (36), dance therapy (37), and meditation therapy (38).
Table 3 presents the PICO(S) framework, which illustrates the utilization of music therapy, dance therapy, mandala therapy, and meditation in addressing mental health issues among individuals affected by COVID-19. The results of five randomized controlled trials (RCTs) indicate that these therapeutic interventions have yielded positive outcomes. Notably, the scope of these outcomes extends beyond the patients themselves to include healthcare practitioners. The literature about these RCTs suggests that various forms of arts therapies have been employed with diverse populations. In these interventions, subjects were exposed to rigorous programs by medical professionals or art therapists.
The results suggested that ~6–12 days of arts therapies intervention can ameliorate mental symptoms, including anxiety, depression, and insomnia. Although the severity of various disorders differs from the control group, music, and color therapies typically enhance mild anxiety in patients or nurses swiftly. Dance and meditation therapies predominantly aim at moderate symptoms such as mild depression and sleep disturbances. Results demonstrate that these mid-level mental disorders usually necessitate consistent, long-term treatment to show comparable positive outcomes to the control group.
Preliminary conclusions from other studies imply that individuals with severe mental illness consequent to COVID-19 may not be optimally suited for exclusive arts therapies due to the many physiological symptoms associated with the virus. Persistent post-COVID-19 symptoms fluctuate in intensity, during which patients typically exhibit mental and physical symptoms (69). Research findings underscore the value of arts therapies as a supplementary approach for critically ill mental health patients within a clinical setting. Patients with schizophrenia, bipolar depression, or suicidal tendencies often necessitate auxiliary interventions like medications or electroconvulsive therapy (70–73).
3.4 Outcome measures
According to BAAT, AATA, TATA, and HKAAT, which collectively state that the drive for art is the biggest centerpiece in arts therapies, arts therapies serve as a bridge connecting patients to their inner worlds, with art therapists and the artistic process acting as catalysts for uncovering deep-seated emotional issues. Nevertheless, study findings indicate variability in results, frequently influenced by factors including the stage of professional treatment, prime physiological state, and acquaintance with art therapists and techniques. Therefore, precisely evaluating the impact of arts therapies on patients with mental disorders and potentially associated groups (e.g., individuals experiencing prolonged quarantine) remains a challenge (74, 75). Such a population faces a higher risk of mental illness due to enforced quarantine policies instead of voluntary compliance (76, 77). Large-scale events are often unpredictable and unplanned, sometimes resulting in insufficient resources during quarantine.
The primary outcome measures In three RCTs involving patients (36–38) may not fully encompass potential group dynamics or observations from individuals in quarantine with COVID-19-positive cases at risk of infection. These individuals often experience anxiety, nervousness, and restlessness (11); prompt arts therapies intervention could potentially inhibit further deterioration. This finding aligns with psychotherapy's emphasis on alleviating distress and fostering coping mechanisms rather than simply reducing symptoms (78). Secondary outcome measures in these RCTs included aspects such as social functioning, wellbeing, mentalization, and self-efficacy (79), which require a more comprehensive study. Furthermore, self-confidence and intra- and interpersonal connectedness are proposed as potential outcome measures for arts therapies.
3.5 Intervention design
Arts therapies can be a versatile supplementary approach for patients with different types of mental disorders (refer to Figure 2). Therefore, the statistical analysis of risk and mental status changes should be personalized according to the diverse participant groups. Future RCTs could be enhanced by stratifying the research populations based on the subtleties of mental health issues related to COVID-19. Recognizing distinct characteristics of patients and potential patients is crucial for subsequent studies. During mandatory quarantine, many individuals may experience changes in their typical mental behavior (11, 75, 80), underscoring the need for early intervention.
Art therapy, a non-invasive, cost-effective method with no associated side effects, can be administered early to potential patients in controlled quarantine. Employing techniques such as music intervention, mandala-color intervention, and web-based guided meditation developed by art therapists may yield benefits. Simultaneously, evaluations and statistics following MATISSE guidelines (46, 81) can be used to assess individuals' mental status during quarantine and for 7–14 days afterward, determining the potential reduction in the incidence of mental illness due to arts therapies.
The inclusion of regular follow-up periods in research may elucidate the long-term effects of arts therapies, which is not evidenced in the reviewed studies (23). In the MATISSE framework, transient improvements from arts therapies could be missed (16); hence, diligent data documentation—particularly at the onset, midpoint, and closure of the intervention—is vital to measure changes accurately.
4 Discussion
Amid the detrimental effects of the COVID-19 pandemic, existing literature acknowledges the far-reaching impact of the virus beyond physical health, with significant implications for global mental health. This reality necessitates urgent, in-depth research into therapeutic responses to manage pandemics' psychological repercussions. Enhanced understanding of psychological burdens across various populations would significantly facilitate this effort (2, 3). Present research emphasizes pandemics' impact on mental health (4–6), the manifestation of complex stressors such as economic hardship, disease epidemics, labor force reductions, and stringent government policies exacerbating global mental health crises (9–11). Thus, developing non-pharmacological treatments for mild to moderate psychological and mental health issues arises as a key research area.
To further alleviate this crisis, current research strives to broaden our understanding of psychiatric symptoms displayed by COVID-19-affected and unaffected populations, evaluating the effectiveness of different forms of art therapy in targeting mental illnesses. The findings underscore the urgent need to develop efficient and cost-effective treatment strategies, including variably time-intensive art therapy forms alongside traditional medication (15). A comparative analysis with prior studies presents a crucial evolution: While most studies have primarily explored health issues from a biomedical perspective, the inclusion of 16 art therapy papers illuminates the feasibility of alternative therapies for intervening mild-to-moderate psychological and mental health issues. This shift in focus, especially amidst COVID-19's substantial pressure on global mental health resources, is of paramount importance.
This review seeks to extend this newly adopted perspective, exploring art therapy's role and potential in managing mental health issues associated with COVID-19 and its sequelae. Consequently, this paper's narrative diverges from conventional treatment protocols, recognizing alternative therapeutic interventions' potential value.
Diletta et al. assert the necessity of artistic interventions for healthcare professionals in music therapy, suggesting telemedicine's applicability in the current context (31, 34). In meditation therapy, involving 11,273 of the 16 papers' subjects, William posits meditation and yoga can enhance the body's immune system to combat viruses (29). Desai et al. suggests meditation also improves sleep quality (41). While Bhuiyan reported no difference between rural or urban status concerning psychological issues (43), the majority of included meditation literature is based on quantitative questionnaire statistics, indicating a need for more RCTs to understand meditation's role across different ages and cultures. Khademi, Renzi, and Yi used mandala therapy and painting therapy, noting their dual capacity to alleviate patients' anxiety as tools for evaluating patients' mental states (33, 36, 44). Zildzic's et al. study deems horticultural therapy effective in ameliorating sleep and stress issues, as well as immune system problems during the COVID-19 pandemic (30). Lastly, Shao's study found dance therapy beneficial in managing adolescent anxiety and depression (37). However, traditional dance may not be suitable for all, particularly middle-aged and older adult individuals or post-COVID-19 patients. Manisha's proposal of a music-and-yoga combination demonstrates better efficacy for these demographics (32), indicating the need for further research into non-pharmacological alternative therapies customized for different populations. Examples for future study may be Qigong and Tai Chi.
Through PICO(S), we conducted a structured data extraction from the five included RCTs, encompassing 445 subjects. Three RCTs used the STAI scale for anxiety, with the remaining using the WRSS for work stress and PWBS for mental health status (34–36). Calamassi's RCT also measured heart rate, respiratory rate, and blood pressure to validate meditation's effects (34), whereas other RCTs used varying scales to evaluate life satisfaction, anxiety, depression, loneliness, sleep quality, and psychological wellbeing (37, 38). All RCTs effectively evaluated the effectiveness of different art therapy subtypes, though underscored the need to balance the patient-to-practitioner ratio.
Collectively, these studies underscore the growing promise of treatments for COVID-19-related mental health disorders. Given the broad COVID-19 patient base, a large number of people suffer from mental health issues. Factors such as isolation and closure render individuals psychologically vulnerable, making teletherapy an invaluable asset. However, the number of psychologists is inadequate to maintain a one-to-one counseling ratio. In this context, we propose a hypothesis: Could artificial intelligence assist psychologists and extend the reach of art therapy?
As the number of patients with NCCP-associated psychiatric disorders increases, traditional art therapies such as painting and music face limitations. The technical complexity and time-consuming nature of traditional painting techniques make it challenging to manage large numbers of patients simultaneously. Similarly, music therapy struggles with selecting suitable music and designing tailored schedules for diverse patient populations. Therefore, while art therapy effectively serves as a non-pharmacological psychotherapeutic form, it lacks the capacity to treat numerous individuals simultaneously. We propose a potentially transformative conjecture: Combining Artificial Intelligence (AI) technologies could bring substantial impacts to the field of art therapy, enhancing its effectiveness, adaptability, and inclusiveness. However, given AI's nascent nature, extensive investigations and empirical analyses are necessary to fully explore and substantiate AI's potential application in art therapy.
The present review is subject to several limitations that warrant acknowledgment. Firstly, the investigation was restricted to studies written in English, thus limiting our sample range. Therefore, it is possible that we missed valuable insights from studies published in other languages. Consequently, our findings may not entirely reflect or apply to non-English speaking populations, introducing potential research bias.
Secondly, the term “mental disorders” encompasses a diverse range of diagnostic categories, implying the presence of unique differences within this group, which our reviewed studies might not have comprehensively explored. While our review attempted to provide a broad perspective, it is important to consider these inherent variations.
Thirdly, the rapidly evolving policies in different countries pose a formidable challenge to literature selection for reviews like this. To mitigate a scarcity of pertinent literature, we selected references applicable and discussable at the time of writing. Nevertheless, future studies may need to update the included literature, reflecting sudden changes in respective countries' policies.
Lastly, considering the small sample size and limited number of studies, we advocate for a prudent interpretation of the qualitative results. The conclusions drawn might not be fully representative of the broader population due to our sample's limited size. It is worth noting that only four studies were evaluated as excellent, further limiting the robustness of our conclusions. This limitation might potentially create a gap in our understanding of arts therapies' full potential in the global response to the COVID-19 pandemic.
5 Conclusions
In conclusion, based on the available literature, arts therapies have demonstrated long-standing effectiveness as a mental health intervention, suggesting potential advantages in addressing mental health concerns among individuals affected by COVID-19. Furthermore, scholarly investigations have indicated that it also plays a significant role in mitigating stress levels among healthcare professionals. The present study provides additional support for the efficacy of arts therapies in promoting the mental wellbeing of individuals affected by COVID-19, as evidenced by our analysis of Randomized Controlled Trials (RCTs). The results of our overlay visualization experiment reveal a notable shift in research emphasis from individual mental disorders to the wider mental health consequences of the COVID-19 pandemic. Additionally, there is a renewed scholarly interest in exploring the potential therapeutic benefits of meditation. The present analysis cautiously examines the potential efficacy of arts therapies as a treatment modality for mental health concerns arising from COVID-19. However, it is imperative to conduct additional specialized research to establish the validity of this assumption conclusively.
Author contributions
XL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZZ: Writing – original draft. XS: Writing – original draft. CH: Writing – review & editing. JW: Supervision, Writing – review & editing, Conceptualization, Data curation. QW: Investigation, Writing – review & editing, Supervision, Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Validation, Visualization. GH: Investigation, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Science and Technology Development Fund, Macau SAR (No: 0098/2021/A2) and the Science and Technology Planning Project of Guangdong Province (2020B1212030008).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. COVID-19 Weekly Epidemiological Update. (2023). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-−17-august-2023 (accessed March 19, 2023).
2. Eissazade N, Shalbafan M, Saeed F, Hemmati D, Askari S, Sayed Mirramazani M, et al. The impact of the COVID-19 pandemic on Iranian psychiatric trainees' and early career psychiatrists' well-being, work conditions, and education. Acad Psychiatry. (2022) 46:710–7. doi: 10.1007/s40596-022-01674-5
3. Xu X, Zhang J, Fang R, Liu H, Zhou W, She Y, et al. Evaluation of the mental health status of community frontline medical workers after the normalized management of COVID-19 in Sichuan, China. Front Psychiatry. (2023) 14:1198822. doi: 10.3389/fpsyt.2023.1198822
4. Adiukwu F, Kamalzadeh L, Pinto da Costa M, Ransing R, de Filippis R, Pereira-Sanchez V, et al. The grief experience during the COVID-19 pandemic across different cultures. Ann Gen Psychiatry. (2022) 21:18. doi: 10.1186/s12991-022-00397-z
5. Ullah I, Khan KS, Ali I, Ullah AR, Mukhtar S, de Filippis R, et al. Depression and anxiety among Pakistani healthcare workers amid COVID-19 pandemic: a qualitative study. Ann Med Surg. (2022) 78:103863. doi: 10.1016/j.amsu.2022.103863
6. Ashiq MAR, Gupta PS, Jubayer Biswas MAA, Ahmed N, Sultana MstS, Ghosh B, et al. Depression, anxiety, stress, and fear of COVID-19 among Bangladeshi medical students during the first wave of the pandemic: a mixed-methods study. Front Psychiatry. (2023) 14:1142724. doi: 10.3389/fpsyt.2023.1142724
7. Anteneh RM, Dessie AM, Azanaw MM, Anley DT, Melese BD, Feleke SF, et al. The psychological impact of COVID-19 pandemic and associated factors among college and university students in Ethiopia: a systematic review and meta-analysis, 2022. Front Public Health. (2023) 11:1136031. doi: 10.3389/fpubh.2023.1136031
8. Zenba Y, Kobayashi A, Imai T. Psychological distress is affected by fear of COVID-19 via lifestyle disruption and leisure restriction among older adults in Japan: a cross-sectional study. Front Public Health. (2023) 11:1264088. doi: 10.3389/fpubh.2023.1264088
9. Tahmasebi S, Khosh E, Esmaeilzadeh A. The outlook for diagnostic purposes of the 2019-novel coronavirus disease. J Cell Physiol. (2020) 235:9211–29. doi: 10.1002/jcp.29804
10. World Health Organization. Yoshi Shimizu. #HealthyAtHome - Mental Health. Available online at: https://www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome—mental-health?gclid=EAIaIQobChMIjdvml-zbgQMVzfxMAh2lZgDFEAAYASAAEgLG2PD_BwE (accessed March 19, 2023).
11. Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. (2021) 18:2470. doi: 10.3390/ijerph18052470
12. Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Research. (2020) 9:636. doi: 10.12688/f1000research.24457.1
13. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. (2020) 291:113264. doi: 10.1016/j.psychres.2020.113264
14. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
15. Boden M, Zimmerman L, Azevedo KJ, Ruzek JI, Gala S, Abdel Magid HS, et al. We are addressing the mental health impact of COVID-19 through population health. Clin Psychol Rev. (2021) 85:102006. doi: 10.1016/j.cpr.2021.102006
16. British Association of Art Therapists. What is Art Therapy? (2015). Available online at: http://www.baat.org/About-Art-Therapy (accessed November 22, 2023).
17. Chung J, Woods-Giscombe C. Influence of dosage and type of music therapy in symptom management and rehabilitation for individuals with schizophrenia. Issues Ment Health Nurs. (2016) 37:631–41. doi: 10.1080/01612840.2016.1181125
18. Potash JS, Ho RTH, Chick JKY, Au Yeung FSW. Viewing and engaging in an art therapy exhibit by people living with mental illness: implications for empathy and social change. Public Health. (2013) 127:735–44. doi: 10.1016/j.puhe.2013.05.004
19. Leurent B, Killaspy H, Osborn DP, Crawford MJ, Hoadley A, Waller D, et al. Moderating factors for the effectiveness of group art therapy for schizophrenia: secondary analysis of data from the MATISSE randomised controlled trial. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1703–10. doi: 10.1007/s00127-014-0876-2
20. Holttum S, Huet V. The MATISSE trial–A critique. SAGE Open. (2014) 4:215824401453293. doi: 10.1177/2158244014532930
21. Centre for Reviews and Dissemination. Systematic reviews: CRD's guidance for undertaking reviews in health care. New York, NY: York Publishing Services Ltd (2008).
22. Sale JEM, Brazil K. A strategy to identify critical appraisal criteria for primary mixed-method studies. Qual Quant. (2004) 38:351–65. doi: 10.1023/B:QUQU.0000043126.25329.85
23. Critical Appraisal Skills Programme (CASP). Qualitative Research Checklists. (2015). Available online at: http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf (accessed November 22, 2023).
24. Pluye P, Robert E, Cargo M, et al. Proposal: A Mixed Methods Appraisal Tool for Systematic Mixed Studies Reviews. (2015). Available online at: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/84371689/MMAT%202011%20criteria%20and%20tutorial%202011-06-29updated2014.08.21.pdf (accessed November 22, 2023).
25. Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. (2010) 340:c869. doi: 10.1136/bmj.c869
26. Attard A, Larkin M. Art therapy for people with psychosis: a narrative review of the literature. Lancet Psychiatry. (2016) 3:1067–78. doi: 10.1016/S2215-0366(16)30146-8
27. Chancellor B, Duncan A, Chatterjee A. Art therapy for Alzheimer's disease and other dementias. J Alzheimers Dis. (2014) 39:1–11. doi: 10.3233/JAD-131295
28. Tacconelli E. Systematic reviews: CRD's guidance for undertaking reviews in health care. Lancet Infect Dis. (2010) 10:226. doi: 10.1016/S1473-3099(10)70065-7
29. Bushell W, Castle R, Williams MA, Brouwer KC, Tanzi RE, Chopra D, et al. Meditation and yoga practices as potential adjunctive treatment of SARS-CoV-2 infection and COVID-19: a brief overview of key subjects. J Altern Complement Med. (2020) 26:547–56. doi: 10.1089/acm.2020.0177
30. Zildzic M, Salihefendic D, Masic I. Non-pharmacological measures in the prevention and treatment of COVID-19 infection. Med Arch. (2021) 75:307–12. doi: 10.5455/medarh.2021.75.307-312
31. Vinciguerra C, Federico A. Neurological music therapy during the COVID-19 outbreak: updates and future challenges. Neurol Sci. (2022) 43:3473–8. doi: 10.1007/s10072-022-05957-5
32. Vajpeyee M, Tiwari S, Jain K, Modi P, Bhandari P, Monga G, et al. Yoga and music intervention to reduce depression, anxiety, and stress during COVID-19 outbreak on healthcare workers. Int J Soc Psychiatry. (2022) 68:798–807. doi: 10.1177/00207640211006742
33. Yi M, Bao D, Mo Y. Exploring the role of visual design in digital public health safety education. Int J Environ Res Public Health. (2021) 18:7965. doi: 10.3390/ijerph18157965
34. Calamassi D, Li Vigni ML, Fumagalli C, Gheri F, Pomponi GP, Bambi S. The Listening to music tuned to 440 Hz versus 432 Hz to reduce anxiety and stress in emergency nurses during the COVID-19 pandemic: a double-blind, randomized controlled pilot study. Acta Biomed. (2022) 93:e2022149. doi: 10.23750/abm.v93iS2.12915
35. Yildirim D, Çiriş Yildiz C. The effect of mindfulness-based breathing and music therapy practice on nurses' stress, work-related strain, and psychological well-being during the COVID-19 pandemic: a randomized controlled trial. Holist Nurs Pract. (2022) 36:156–65. doi: 10.1097/HNP.0000000000000511
36. Khademi F, Rassouli M, Rafiei F, Moayedi S, Torres M, Marzban N, et al. The effect of mandala colouring on anxiety in hospitalized COVID-19 patients: A randomized controlled clinical trial. Int J Ment Health Nurs. (2021) 30:1437–44. doi: 10.1111/inm.12901
37. Shao S. Intervention effect of dance therapy based on the Satir model on the mental health of adolescents during the COVID-19 epidemic. Psychiatr Danub. (2021) 33:411–7. doi: 10.24869/psyd.2021.411
38. Thimmapuram J, Pargament R, Bell T, Schurk H, Madhusudhan DK. Heartfulness meditation improves loneliness and sleep in physicians and advance practice providers during COVID-19 pandemic. Hosp Pract (1995). (2021) 49:194–202. doi: 10.1080/21548331.2021.1896858
39. Matiz A, Fabbro F, Paschetto A, Cantone D, Paolone AR, Crescentini C. Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. Int J Environ Res Public Health. (2020) 17:6450. doi: 10.3390/ijerph17186450
40. Jiménez Ó, Sánchez-Sánchez LC, García-Montes JM. Psychological Impact of COVID-19 Confinement and Its Relationship with Meditation. Int J Environ Res Public Health. (2020) 17:6642. doi: 10.3390/ijerph17186642
41. Desai K, Gupta P, Parikh P, Desai A. Impact of virtual heartfulness meditation program on stress, quality of sleep, and psychological wellbeing during the COVID-19 pandemic: a mixed-method study. Int J Environ Res Public Health. (2021) 18:11114. doi: 10.3390/ijerph182111114
42. Priyanka, Rasania SK. A cross–sectional study of mental wellbeing with practice of yoga and meditation during COVID-19 pandemic. J Family Med Prim Care. (2021) 10:1576–1581. doi: 10.4103/jfmpc.jfmpc_2367_20
43. Bhuiyan N, Puzia M, Stecher C, Huberty J. Associations between rural or urban status, health outcomes and behaviors, and COVID-19 perceptions among meditation app users: longitudinal survey study. JMIR Mhealth Uhealth. (2021) 9:e26037. doi: 10.2196/26037
44. Renzi A, Verrusio W, Evangelista A, Messina M, Gaj F, Cacciafesta M. Using drawings to express and represent one's emotional experience during the coronavirus disease 2019 pandemic: a case report of a woman living in a nursing home. Psychogeriatrics. (2021) 21:118–20. doi: 10.1111/psyg.12638
45. Chiang M, Reid-Varley WB, Fan X. Creative art therapy for mental illness. Psychiatry Res. (2019) 275:129–36. doi: 10.1016/j.psychres.2019.03.025
46. Crawford MJ, Killaspy H, Kalaitzaki E, Barrett B, Byford S, Patterson S, et al. The MATISSE study: a randomised trial of group art therapy for people with schizophrenia. BMC Psychiatry. (2010) 10:65. doi: 10.1186/1471-244X-10-65
47. Gajić GM. Group art therapy as adjunct therapy for the treatment of schizophrenic patients in day hospital. Vojnosanit Pregl. (2013) 70:1065–9. doi: 10.2298/VSP1311065M
48. Banks L. Free to talk about violence: a description of art therapy with a male service user in a low secure unit. Int J Art Therapy. (2012) 17:13–24. doi: 10.1080/17454832.2012.658578
49. Hung C-C, Ku Y-W. Influencing and moderating factors analyzed in the group art therapy of two schizophrenic inpatients. Biomedicine. (2015) 5:24. doi: 10.7603/s40681-015-0024-7
50. Michaelides D. An understanding of negative reflective functioning, the image and the art psychotherapeutic group. Int J Art Therapy. (2012) 17:45–53. doi: 10.1080/17454832.2012.694107
51. Gómez-Romero M, Jiménez-Palomares M, Rodríguez-Mansilla J, Flores-Nieto A, Garrido-Ardila EM, González López-Arza MV. Benefits of music therapy on behaviour disorders in subjects diagnosed with dementia: a systematic review. Neurologia. (2017) 32:253–63. doi: 10.1016/j.nrl.2014.11.001
52. Solanki MS, Zafar M, Rastogi R. Music as a therapy: role in psychiatry. Asian J Psychiatr. (2013) 6:193–9. doi: 10.1016/j.ajp.2012.12.001
53. Pereira APS, Marinho V, Gupta D, Magalhaes F, Ayares C, Teixeira S. Music therapy and dance as gait rehabilitation in patients with Parkinson disease: a review of evidence. J Geriatr Psychiatry Neurol. (2019) 32:49–56. doi: 10.1177/0891988718819858
54. Liu C, Chen H, Liu C-Y, Lin R-T, Chiou W-K. Cooperative and individual mandala drawing have different effects on mindfulness, spirituality, and subjective well-being. Front Psychol. (2020) 11:564430. doi: 10.3389/fpsyg.2020.564430
55. Emblad SYM, Mukaetova-Ladinska EB. Creative Art Therapy As A Non-Pharmacological Intervention For Dementia: A Systematic Review. J Alzheimers Dis Rep. (2021) 5:353–64. doi: 10.3233/ADR-201002
56. Raybin JL, Krajicek M. Creative arts therapy in the context of children with cancer: a concept analysis. J Pediatr Oncol Nurs. (2020) 37:82–90. doi: 10.1177/1043454219878397
57. Karkou V, Meekums B. Dance movement therapy for dementia. Cochrane Database Syst Rev. (2017) 2:CD011022. doi: 10.1002/14651858.CD011022.pub2
58. Li WHC, Chung JOK, Ho KY, Kwok BMC. Play interventions to reduce anxiety and negative emotions in hospitalized children. BMC Pediatr. (2016) 16:36. doi: 10.1186/s12887-016-0570-5
59. Marcus D. Play therapy with young children. Ind J Pediatr. (1992) 59:53–60. doi: 10.1007/BF02760898
60. Choi Y-H, Paik N-J. Mobile game-based virtual reality program for upper extremity stroke rehabilitation. J Vis Exp. (2018) 133:56241. doi: 10.3791/56241
61. Wilkinson N, Ang RP, Goh DH. Online video game therapy for mental health concerns: a review. Int J Soc Psychiatry. (2008) 54:370–82. doi: 10.1177/0020764008091659
62. Saeed SA, Cunningham K, Bloch RM. Depression and anxiety disorders: benefits of exercise, yoga, and meditation. Am Fam Phys. (2019) 99:620–7.
63. Saeed SA, Cunningham K, Bloch RM. Exercise, yoga, and meditation for depressive and anxiety disorders. Am Fam Phys. (2010) 81:981–6.
64. Colbert S, Cooke A, Camic PM, Springham N. The art-gallery as a resource for recovery for people who have experienced psychosis. Arts Psychotherapy. (2013) 40:250–6. doi: 10.1016/j.aip.2013.03.003
65. Patterson S, Debate J, Anju S, Waller D, Crawford MJ. Provision and practice of art therapy for people with schizophrenia: results of a national survey. J Ment Health. (2011) 20:328–35. doi: 10.3109/09638237.2011.556163
66. de Morais AH, Roecker S, Salvagioni DAJ, Eler GJ. Significance of clay art therapy for psychiatric patients admitted in a day hospital. Invest Educ Enferm. (2014) 32:128–38. doi: 10.17533/udea.iee.v32n1a15
67. de Morais AH, Dalécio MAN, Vizmann S, Bueno VLR de C, Roecker S, Salvagioni DAJ, et al. Effect on scores of depression and anxiety in psychiatric patients after clay work in a day hospital. Arts Psychotherapy. (2014) 41:205–10. doi: 10.1016/j.aip.2014.02.002
68. Montag C, Haase L, Seidel D, Bayerl M, Gallinat J, Herrmann U, et al. pilot RCT of psychodynamic group art therapy for patients in acute psychotic episodes: feasibility, impact on symptoms and mentalising capacity. PLoS ONE. (2014) 9:e112348. doi: 10.1371/journal.pone.0112348
69. Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. (2021) 114:428–42. doi: 10.1177/01410768211032850
70. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:611–27. doi: 10.1016/S2215-0366(20)30203-0
71. Sinclair DJM, Zhao S, Qi F, Nyakyoma K, Kwong JSW, Adams CE. Electroconvulsive therapy for treatment-resistant schizophrenia. Schizophr Bull. (2019) 45:730–2. doi: 10.1093/schbul/sbz037
72. Perugi G, Medda P, Toni C, Mariani MG, Socci C, Mauri M. The role of electroconvulsive therapy (ECT) in bipolar disorder: effectiveness in 522 patients with bipolar depression, mixed-state, mania and catatonic features. Curr Neuropharmacol. (2017) 15:359–71. doi: 10.2174/1570159X14666161017233642
73. Rönnqvist I, Nilsson FK, Nordenskjöld A. Electroconvulsive therapy and the risk of suicide in hospitalized patients with major depressive disorder. JAMA Netw Open. (2021) 4:e2116589. doi: 10.1001/jamanetworkopen.2021.16589
74. Wells CR, Townsend JP, Pandey A, Moghadas SM, Krieger G, Singer B, et al. Optimal COVID-19 quarantine and testing strategies. Nat Commun. (2021) 12:356. doi: 10.1038/s41467-020-20742-8
75. Ferreira LN, Pereira LN, da Fé Brás M, Ilchuk K. Quality of life under the COVID-19 quarantine. Qual Life Res. (2021) 30:1389–405. doi: 10.1007/s11136-020-02724-x
76. Maner M, LeMasters K, Lao J, Cowell M, Nowotny K, Cloud D, et al. COVID-19 in corrections: Quarantine of incarcerated people. PLoS ONE. (2021) 16:e0257842. doi: 10.1371/journal.pone.0257842
77. Park HW. Seven principles of quarantine for the COVID-19 pandemic. J Korean Med Sci. (2021) 36:e147. doi: 10.3346/jkms.2021.36.e147
78. Kazdin AE. Evidence-based treatments: challenges and priorities for practice and research. Child Adolesc Psychiatr Clin N Am. (2004) 13:923–40, vii. doi: 10.1016/j.chc.2004.04.002
79. Luo X, Zhang Z, Zheng Z, Ye Q, Wang J, Wu Q, et al. Art therapy as an adjuvant treatment for schizophrenia: A protocol for an updated systematic review and subgroup meta-analysis of randomized clinical trials following the PRISMA guidelines. Medicine. (2022) 101:e30935. doi: 10.1097/MD.0000000000030935
80. Lindert J, Jakubauskiene M, Bilsen J. The COVID-19 disaster and mental health-assessing, responding and recovering. Eur J Public Health. (2021) 31:iv31–5. doi: 10.1093/eurpub/ckab153
Keywords: mental disorders, COVID-19, Post-Acute COVID-19 Syndrome, arts therapies, psychotherapy
Citation: Luo X, Zhang Z, Shi X, He C, Wang J, Wu Q and Huang G (2023) Arts therapies for mental disorders in COVID-19 patients: a comprehensive review. Front. Public Health 11:1289545. doi: 10.3389/fpubh.2023.1289545
Received: 06 September 2023; Accepted: 13 November 2023;
Published: 04 December 2023.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Carlos Laranjeira, Polytechnic Institute of Leiria, PortugalNoah Hass-Cohen, Alliant International University-San Diego, United States
Copyright © 2023 Luo, Zhang, Shi, He, Wang, Wu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jue Wang, d2FuZ2p1ZUBtdXN0LmVkdS5tbw==; Qibiao Wu, cWJ3dUBtdXN0LmVkdS5tbw==; Guanghui Huang, Z2hodWFuZzFAbXVzdC5lZHUubW8=
†These authors have contributed equally to this work
 Xuexing Luo
Xuexing Luo Zheyu Zhang1†
Zheyu Zhang1† Jue Wang
Jue Wang Qibiao Wu
Qibiao Wu Guanghui Huang
Guanghui Huang