- 1Department of Nursing and Midwifery, Collage of Health Sciences, University of Doha for Science and Technology, Doha, Qatar
- 2Daphne Cockwell School of Nursing, Faculty of Community Services, Toronto Metropolitan University, Toronto, ON, Canada
- 3Department of Healthcare Management, College of Business Management, University of Doha for Science and Technology, Doha, Qatar
Background: The global healthcare landscape was profoundly impacted by the COVID-19 pandemic placing nurses squarely at the heart of this emergency. This review aimed to identify the factors correlated with nurses’ job satisfaction, the impact of their job satisfaction on both themselves and their patients, and to explore strategies that might have counteracted their job dissatisfaction during the COVID-19 pandemic.
Methods: The Joanna Briggs Institute (JBI) methodology for systematic reviews of prevalence and incidence was used in this review. The electronic databases of CINAHL, MEDLINE, SCOPUS, PsycINFO and Academic Search Complete were searched between January 2020 to February 2023.
Results: The literature review identified 23 studies from 20 countries on nurses’ job satisfaction during the COVID-19 pandemic. A pooled prevalence of 69.6% of nurses were satisfied with personal, environmental, and psychological factors influencing their job satisfaction. Job satisfaction improved psychological wellbeing and quality of life, while dissatisfaction was linked to turnover and mental health issues.
Conclusion: This systematic review elucidates key factors impacting nurses’ job satisfaction during the COVID-19 pandemic, its effects on healthcare provision, and the potential countermeasures for job dissatisfaction. Core influences include working conditions, staff relationships, and career opportunities. High job satisfaction correlates with improved patient care, reduced burnout, and greater staff retention.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023405947, the review title has been registered in PROSPERO and the registration number is CRD42023405947.
1 Introduction
The COVID-19 pandemic significantly affected multiple dimensions of healthcare systems across the globe, with nurses being at the epicenter of this crisis (1, 2). In the midst of the COVID-19 outbreak, nurses encountered distinct stressors encompassing both personal and professional spheres, which have the potential to substantially affect their levels of job satisfaction and intentions to remain in their positions (3). Nurses experiencing anxiety related to COVID-19 exhibited higher levels of work-related stress, greater inclination towards leaving their jobs (4). Furthermore, nurses reported a marked increase in their burnout level (5). As fundamental healthcare professionals accountable for patient care, nurses have grappled with unparalleled challenges that include an escalation in workload (6), scarcity of resources, vulnerability to infection (7), and emotional distress (8). The emotional toll from seeing increased patient morbidity and mortality during the pandemic, and the limited psychological support provided by the organization, significantly affected nurses’ emotional wellbeing and job satisfaction (9). Reduction in salaries and increased workload played a significant role as well, with adequate remuneration and acknowledgment acting as motivational factors (9).
Nurse’s job satisfaction during COVID-19 was a critical factor affecting their performance, productivity, and retention (10). Nurses experiencing low job satisfaction may be prone to burnout (11), reduced job performance (12), and increased likelihood of leaving the profession (10). Furthermore, job dissatisfaction may negatively impact nurses’ mental and physical health, exacerbating stress, anxiety, and other mental health conditions (1, 6, 10). Low job satisfaction among nurses during the COVID-19 pandemic could have had far-reaching consequences, not only for themselves but also for patient care and healthcare organizations as a whole (10).
Recognizing the significance of addressing job satisfaction among nurses, especially during the COVID-19 pandemic, the implementation of effective mitigation strategies is imperative (3, 13). These strategies may include promoting supportive work environments (8), providing adequate resources and training (7, 13), fostering open communication channels (14), and offering mental health support services (8).
Although the repercussions of the COVID-19 pandemic on various facets of healthcare and the welfare of healthcare professionals have been extensively acknowledged (8), there is a notable scarcity of exhaustive scholarly literature specifically zeroing in on nurses’ job satisfaction amidst this unparalleled crisis. Consequently, all-encompassing research, inclusive of systematic reviews scrutinizing the distinct impact of the pandemic on nurses’ job satisfaction, has been sparse. Holistic studies centered on nurses’ job satisfaction during the COVID-19 outbreak can furnish critical insights into the specific factors shaping job satisfaction levels, the ramifications of job discontentment on nurses’ wellbeing and the caliber of patient care, and the formulation of efficacious ameliorative strategies. Such research may guide evidence-based interventions and policies to bolster job satisfaction and foster the resilience of nurses, which in turn may catalyze the enhancement of healthcare delivery during and in the aftermath of the pandemic. The aim of this systematic review is to investigate how the COVID-19 pandemic affected nurses’ job satisfaction. Specifically, the review seeks to identify factors influencing job satisfaction, explore the consequences of job dissatisfaction on both nurses and their patients, and examine mitigation strategies employed to counteract job dissatisfaction during the pandemic.
2 Methods
This systematic review was conducted in accordance with the JBI methodology for systematic reviews of prevalence and incidence (15) and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (16). A priori protocol was registered in PROSPERO and the registration number is (CRD42023405947).
2.1 Search strategy
In March 2023, a three-step search strategy was used aimed at locating published studies in English. First, an initial limited search of MEDLINE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) was undertaken to identify articles on the topic. Text words contained in the titles and abstracts of relevant articles, and index terms used to describe the articles were used to develop a full search strategy.
In the second step in the search strategy, all identified keywords, index terms and MESH terms were adapted for each included database and/or information source. The following databases were searched: CINAHL, MEDLINE, SCOPUS, PsycINFO, and Academic Search Complete. The Boolean operators AND/OR were used to narrow or broaden the search using a combination of the keywords. Search terms included: (nurse or nurses or nursing) AND (“job satisfaction” or “work satisfaction” or “employee satisfaction”) AND (determinant or factor or cause or influence or influencer or predictor or mitigation or prevention or reduction). Finally, the reference lists of the included studies were searched manually to identify any relevant studies.
2.2 Study types and participants
Any primary experimental, quasi-experimental, cohort, or cross-sectional research studies that investigated job satisfaction among nurses during the COVID-19 pandemic were included. Studies published in English and between January 2020 to February 2023 were included as this was the time when COVID-19 was declared as a pandemic across the globe. Studies that investigated job satisfaction among nurses outside the COVID-19 pandemic period were excluded. Qualitative studies were also excluded.
2.3 Study selection
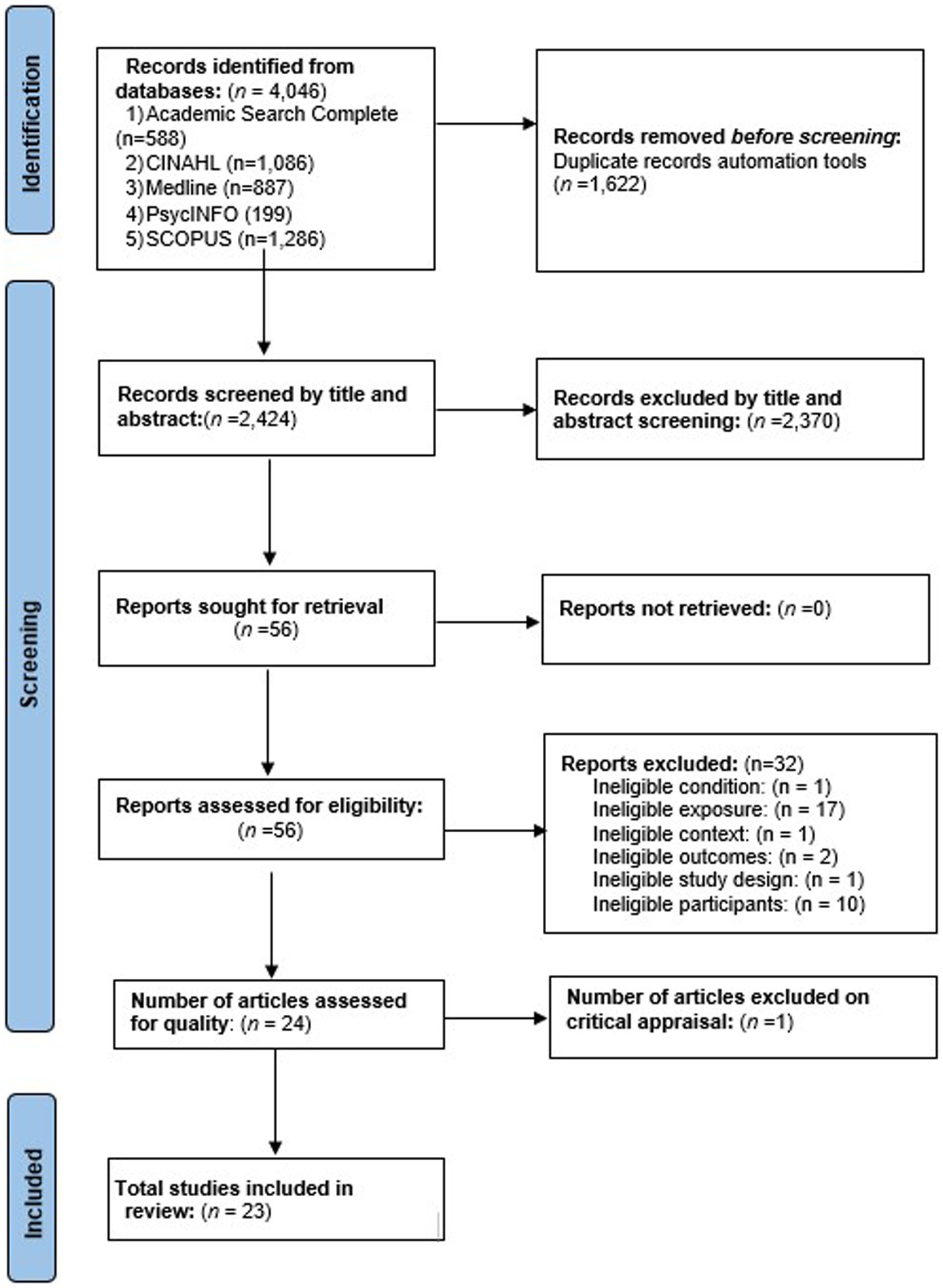
Following the search, all identified citations were collated and uploaded into EndNote version 20 (17) and duplicates were removed. Following a pilot test, titles and abstracts were screened by two independent reviewers (AA, YY) for assessment against the review’s inclusion criteria. Potentially relevant studies were retrieved in full, and their citation details imported into the JBI System for the Unified Management, Assessment and Review of Information (JBI SUMARI). The full text of selected citations was assessed in detail against the inclusion criteria by the two reviewers (AA, YY). Any disagreements that arose between the reviewers at each stage of the selection process was resolved through discussion. The results of the search and the study inclusion process were reported in full in the final systematic review and presented in a Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram (16). See Figure 1.
2.4 Assessment of methodological quality
Eligible studies were critically appraised independently by the two reviewers (AA, YY) at the study level for methodological quality using standardized critical appraisal instruments from JBI for experimental (18), quasi-experimental (19), and cross-sectional studies (20). The authors of papers were contacted to request missing or additional data for clarification, where required. Any disagreements that arose were resolved through discussion. The results of the critical appraisal were reported in narrative form and in a table (See Supplementary File 1). Not applicable or unclear answers were considered as not achieved. Any study that received a score of less than 50% on the quality assessment questions was excluded. The Supplementary File 1 shows the detailed methodological quality scores, the questions asked, and the answer key to each study according to the design.
2.5 Data extraction
Data extraction from the studies included in the review was carried out independently by the two reviewers (AA, YY) using the standardized data extraction tool for prevalence and incidence available in JBI SUMARI. To resolve extraction discrepancies, a third reviewer was consulted (VK). The data extracted included specific details about the condition, populations, study methods, and proportions of interest to the review specific objectives. For the purpose of meta-analysis, the pooling of estimates was executed by using JBI SUMARI. The transformation of data was done by applying a random-effects model that employed the Freeman–Tukey transformation. In order to assess heterogeneity, the standard I2 tests were judiciously employed. In situations where statistical pooling was deemed unfeasible, the outcomes were presented through a comprehensive narrative, supplemented with tables and figures in order to aid in the presentation of data.
3 Results
The literature search generated a total of 4,046 citations. Among these, 1,622 were identified as duplicates and were subsequently removed. The remaining 2,424 citations underwent a preliminary screening process, where titles and abstracts were examined for relevance according to the inclusion criteria. Based on this screening, 56 citations were selected for a comprehensive assessment involving full-text review. Within this subset of 56, 32 studies were also excluded for various reasons, including: ineligibility based on the condition under investigation (n = 1), exposure (n = 17), context (n = 1), outcomes (n = 2), study design (n = 1), and participant characteristics (n = 10). A critical appraisal was conducted on the remaining 24 studies, during which one study was further excluded due to a quality assessment score below the 50% threshold. Consequently, a total of 23 studies met the inclusion criteria and were incorporated in the final review.
3.1 Characteristics of included studies
The final selected studies were carried out from February 2020 to February 2022, during which the primary focus of data collection was in the peak period of the COVID-19 pandemic. Out of these, the majority of the included studies (21 out of 23) utilized a cross-sectional survey methodology. One study was open-label randomized controlled trial (21), and one study utilized a quasi-experimental design (22). The research had taken place across 20 different countries, with two of the studies being multi-national (23, 24). The countries that were part of this review included Bangladesh, Brazil, Canada, China, Egypt, Germany, Great Britain, Hong Kong, Iran, Israel, Italy, Philippines, Poland, Portugal, South Korea, Spain, Sweden, Switzerland, Turkey, and the United States. There was a diverse range in the number of participants in these studies, with the smallest sample consisting of 52 and the largest including 4,561 participants. The aggregate number of participants involved in all the studies exceeded 17,196. The settings in which these studies were conducted varied but mainly included hospital settings, specifically COVID-19 units, emergency departments, tertiary hospitals, isolation wards, inpatient hospital settings, outpatient clinics, and community facilities. Further details are provided in Supplementary File 2.
3.2 Level of job satisfaction
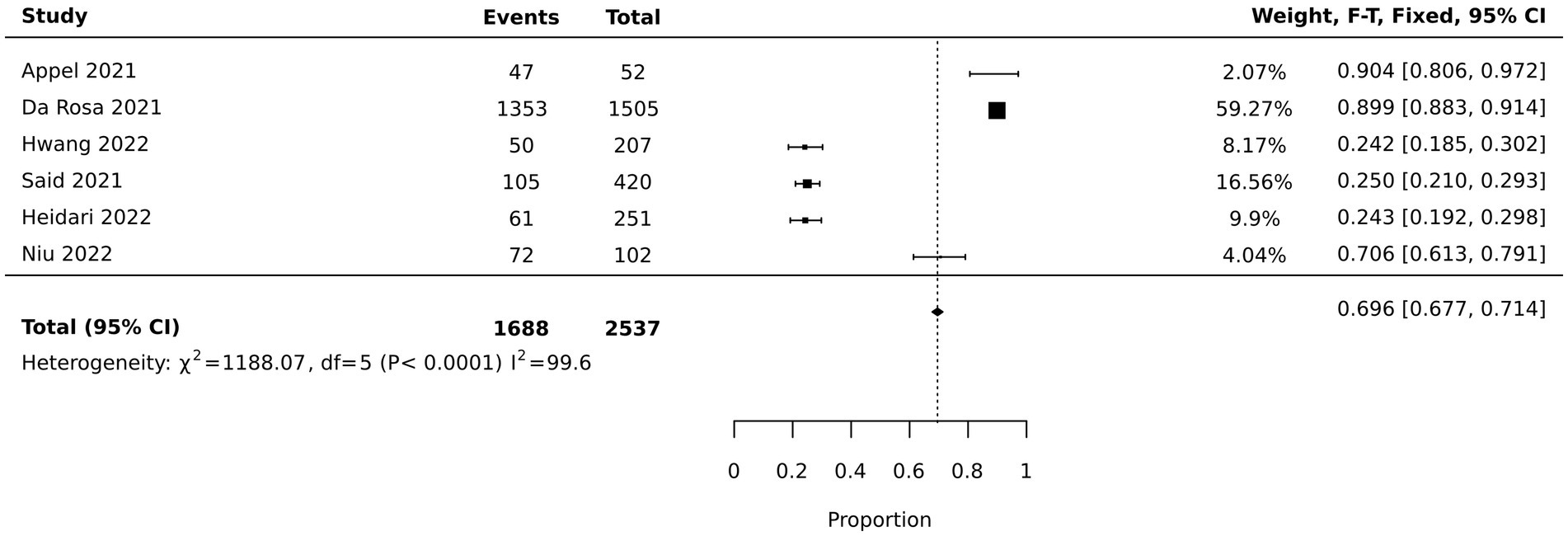
Six studies reported the percentage of nurses’ job satisfaction during the pandemic. Of these, two provided specific cutoff points on their respective scales to delineate job satisfaction (25, 26); three presented job satisfaction data in terms of prevalence percentages (27–29); and one study utilized a 10-point single-item scale and applied a median split to categorize nurses’ job satisfaction into high and low (30). The pooled data from these six studies indicated that 69.6% (95% CI: [67.7, 71.4%]) of nurses were satisfied with their jobs, as illustrated in Figure 2. Specifically, three of the studies reported that nurses’ satisfaction level was more than 70% (27, 29, 30). Three other studies reported that their job satisfaction was 24.2 to 25% (25, 26, 28). The remaining studies reported means and standard deviations without categorical description of job satisfaction levels. See Supplementary File 2.
3.3 Tools used to assess job satisfaction
The 23 included studies employed a diverse set of measurement tools to evaluate job satisfaction. Among these tools were the McCloskey/Mueller Satisfaction Scale (23, 26), the Minnesota Satisfaction Questionnaire (25), the Turkish Job Satisfaction Scale (31), the Job Satisfaction Scale (24), the Safety Attitudes Questionnaire (32), the Nursing Questionnaire on Organizational Health (22), and the Brayfield and Rothe’s 5-item Short Index of Job Satisfaction (33). Some of the researchers though opted for a single item scale to gauge job satisfaction (27, 29, 30, 34–38). Other researchers adapted subscales of existing questionnaires; for instance, four questions focusing on work satisfaction were adapted from Shaver and Lacey (39). The job satisfaction subscale of the UNIPSICO Battery was employed in a similar manner (14). Sampaio et al. used the job satisfaction dimension from the Copenhagen Psychosocial Questionnaire’s (40), while Goktas et al. employed a 5-point scale that was a refined version of Brayfield and Rothe’s scale (21). Savitsky et al. constituted an occupational satisfaction scale by utilizing items from the Minnesota Satisfaction Questionnaire, the Measure of Job Satisfaction, and other items (41). Finally, Barili et al. constructed an index “Satisfaction i” to measure job satisfaction derived from items extracted from the Labor Force Survey (42).
3.4 Factors affecting job satisfaction
The review concluded that several factors significantly contributed to better job satisfaction in nurses. These statistically significant factors were categorized into personal and demographic factors, work environment factors, and psychological and emotional factors.
3.4.1 Personal and demographic factors
Experience (37), lower education (33), and having a family (33, 36, 37, 42) were personal factors contributing to job satisfaction. Older age was generally associated with greater job satisfaction (32, 36, 37, 42), with an exception in one study (24). One study found that female nurses were less satisfied compared to male nurses (24). Financial matters, particularly salary and earnings satisfaction, were also important (33, 39, 42). Good health positively impacted job satisfaction (42), but COVID-19 infection, especially if led to hospitalization, had a negative impact (31, 42).
3.4.2 Work environment factors
The quality of the work environment, including supportive supervision (39), availability of resources (14, 33, 36), manageable workloads (14, 39), adequate staffing (32, 42), employer and coworker support (32), working in a community compared to hospital setting (41), and effective COVID-19 measures (14, 32, 36, 37, 42) were vital for job satisfaction. Conversely, working in a COVID-19 unit (30, 36, 38, 40, 43), job insecurity (14), or working overtime (42) negatively affected job satisfaction. Employment in government hospitals, training against workplace violence, job performance rewards (33), the geographical location of the health care facility, and perceived job importance (24) also contributed to nurses’ job satisfaction.
3.4.3 Psychological and emotional factors
Changes in work conditions, prestige, and commitment to nursing during COVID-19 negatively impacted job satisfaction (24). Anxiety (36), role conflicts, psychosomatic problems (14), and fear of COVID-19 infection (35) also contributed to decreased job satisfaction. Concerns regarding potential infection and stigma from working in high-risk areas like COVID-19 treatment centers further decreased job satisfaction (36). In contrast, positive behaviors, specifically discretionary efforts aimed at enhanced care for COVID-19 patients, and adaptability post-trauma led to post-traumatic growth and job satisfaction, had favorable effects.” (36, 39).
3.5 Consequences of job satisfaction
3.5.1 Positive consequences
Chong et al. shed light on the enhancement of psychological flexibility and mental wellbeing as positive outcomes of job satisfaction (23). Additionally, correlation was reported between better professional quality of life and higher job satisfaction (28, 29). Further, elevated job satisfaction was associated with improved quality of life and wellbeing in the workplace (40). Moreover, higher levels of job satisfaction had a positive impact on nurses’ organizational commitment and their inclination to provide care to COVID-19 patients (39).
3.5.2 Negative consequences
Conversely, job dissatisfaction was associated with several undesired consequences. For instance, job dissatisfaction during COVID-19 was found to be associated with higher turnover intentions (38). Job dissatisfaction was correlated with mental health issues (23). Depression and stress were specifically identified as detrimental consequences of low job satisfaction (27, 30, 34). Anxiety was reported to be negatively affected by low job satisfaction (27, 34, 37). Chowdhury et al. showed that job dissatisfaction resulted in increased workplace violence, bullying, and burnout (33). Moreover, Heidari et al. (25) expounded on burnout as a result of job dissatisfaction, specifically highlighting that emotional exhaustion and compromised personal accomplishment, as facets of burnout, were impacted.
3.6 Interventions to enhance job satisfaction during COVID-19
This review identified two studies that investigated the efficacy of interventions aimed at bolstering job satisfaction. Goktas et al. employed a randomized controlled experiment to assess the impact of disseminating motivational messages on the job satisfaction of emergency nurses amidst the COVID-19 pandemic (21). The experimental intervention entailed transmitting motivational text messages to participants in the intervention group three times daily. These messages were crafted to augment job satisfaction and communication skills while mitigating compassion fatigue. The findings of this study evinced a favorable effect of the intervention on the participants’ job satisfaction.
Similarly, Zaghini et al. utilized a longitudinal mixed-methods design to scrutinize the implementation of organizational proactive management interventions and their impact on nurses’ job satisfaction (22). The study gauged job satisfaction before and after the implementation of a spectrum of interventions. These interventions encompassed measures pertaining to the nursing work environment, staffing and workload adjustments, the enhancement of competence and learning, fostering a participatory approach and autonomy, unit-level strategies concerning COVID-19, and surveillance of healthcare nurses. The study ascertained that the execution of these organizational proactive management interventions positively influenced job satisfaction.
4 Discussion
The COVID-19 pandemic had a significant impact on all aspects of healthcare systems globally, including healthcare professionals who were in the front lines caring for patients with COVID-19 infections. Of particular concern, which is the subject of this systematic review, is the wellbeing of nurses who experienced serious stressors that had the potential to substantially affect their levels of job satisfaction and commitment to remain in their profession. While considerable number of research studies have been conducted on nurses’ job satisfaction during the COVID-19 pandemic, to our best knowledge, no studies had explored this subject systematically. In planning this systematic review, we believed that our review would provide critical insights into the specific factors during the pandemic that influenced nurses’ job satisfaction, and the impact of job dissatisfaction on their wellbeing and the consequential quality of patient care provided.
4.1 Level and measurement of job satisfaction
The results from the meta-analysis indicated a bifurcation in the levels of nurses’ job satisfaction during the pandemic. While the pooled data from six studies showed that approximately 69.6% of nurses were satisfied with their jobs during the pandemic, there was a noticeable divergence between the studies. Half of these studies reported job satisfaction levels exceeding 70% (27, 29, 30), while the other half reported significantly lower levels between 24.2 to 25% (25, 26, 28). One possible explanation for this disparity could be the setting and context in which the studies were conducted. National policies regarding healthcare workers’ remuneration, workload, and support during the pandemic might have been different between different countries (43). The studies reporting higher levels of job satisfaction were primarily conducted in the USA, Brazil, and China. These nations, despite their economic and cultural differences, may have features in their healthcare systems that contribute positively to job satisfaction during the pandemic. In contrast, studies from Iran and Egypt reported lower satisfaction scores, potentially linked to economic challenges, healthcare resource limitations, and cultural perceptions of nursing. Notably, the job satisfaction scores from South Korea presented an unexpected outcome, with levels significantly lower than other countries. This anomaly could be reflective of the particularly high rates of burnout and workload experienced by healthcare providers in South Korea during the pandemic (44). Such stressful working conditions are likely to adversely affect job satisfaction and may have accounted for the distinct results observed in this context. As well, it is important to consider the cultural differences in the way people perceived the subjective questions about job satisfaction when comparing data across countries (45). To comprehensively understand the nuances of job satisfaction among healthcare professionals in these countries, further research is warranted. Such studies should delve into the interplay of economic, cultural, and systemic factors that contribute to these differences, considering the unique resilience measures and support systems for nurses that these nations may have implemented during the pandemic.
4.2 Factors affecting job satisfaction
The findings of this review indicated that job satisfaction among nurses was influenced by a combination of personal and demographic factors, work environment factors, and psychological and emotional factors. This is consistent with previous literature which has also shown the multidimensional nature of job satisfaction (46, 47).
Regarding personal and demographic factors, our review found that higher working experience (37), lower education preparation (33), and having a family (33, 36, 37, 42) were linked to higher job satisfaction. These findings may be attributed to the potential stability and familiarity that experience brings (48), and the support systems that families could provide (49). Moreover, this interpretation may explain why older age was generally associated with higher job satisfaction. Kovner et al. suggested that older nurses might have more realistic expectations and coping skills (50). However, Makowicz et al. found an exception regarding age, which suggested that other factors might have moderated the relationship between age and job satisfaction, which might require further studies (24).
Work environment factors were found to be vital in determining job satisfaction. Positive factors included supportive supervision, availability of resources, reasonable workloads, and effective COVID-19 measures (14, 32, 33, 36, 37, 39, 42). Our findings are consistent with the conclusions of Persefoni’s review (51), which synthesized evidence of a significant association between nurses’ job satisfaction and the quality of their work environment. Interestingly, nurses working in community settings were found to have higher job satisfaction than those in hospital settings (41), possibly due to lower patient acuity and more autonomous practice.
Conversely, psychological and emotional factors such as anxiety, role conflicts, and fear of COVID-19 infection contributed to reduced job satisfaction (14, 35, 36). This supports the findings of Lee and Jang (52), who identified that emotional status had a significant impact on nurses’ job satisfaction. Concerns regarding potential infection and stigma from working in high-risk areas like COVID-19 treatment centers further decreased job satisfaction (36), underscoring the significant impact of the pandemic on nurses’ psychological wellbeing and job satisfaction.
4.3 Consequences of job satisfaction
The consequences of job satisfaction among nurses, especially during the COVID-19 pandemic, are multifaceted and crucial to understand for the betterment of healthcare services. Chong et al. illustrated that higher job satisfaction was associated with an enhancement in psychological flexibility and mental wellbeing (23). This finding is critical for healthcare service quality, aligning with earlier research that underscored the role of mental wellbeing in healthcare professionals in determining patient care quality (53). Moreover, improved professional quality of life resulting from high job satisfaction (28, 29) reiterates the importance of maintaining a positive working environment for better service delivery. Sampaio et al. supported this by associating high job satisfaction with improved quality of life and workplace wellbeing (40). Notably, Sharif Nia et al. established that job satisfaction positively influenced nurses’ commitment to the organization and their willingness to provide care to COVID-19 patients (39). This is particularly significant in the context of a pandemic, as the commitment and dedication of healthcare professionals are paramount in handling healthcare crises (54).
On the contrary, job dissatisfaction has been linked to a plethora of negative consequences. Consistent with earlier research (55), Lavoie-Tremblay et al. found that job dissatisfaction during COVID-19 was associated with higher turnover intentions (38), which can be detrimental to healthcare systems that were already strained by the pandemic. Moreover, Chong et al. correlated job dissatisfaction with mental health issues (23), which is alarming considering the stress and emotional turmoil healthcare professionals already face in pandemic settings (56). Specific mental health issues like depression, anxiety burnout, and stress were also observed as consequences of low job satisfaction (25, 27, 30, 34, 37). Furthermore, the work of Chowdhury et al. showing an association between job dissatisfaction and increased workplace violence, bullying, and burnout (33) is particularly concerning.
The findings in this review elucidate the significant impact job satisfaction has on nurses’ mental wellbeing, professional quality of life, and dedication to care, especially during a health crisis like COVID-19. The negative consequences of job dissatisfaction, including mental health issues, turnover intentions, and burnout, are detrimental not only to healthcare professionals but also to the quality of healthcare delivery. As such, it is imperative that measures be implemented to improve job satisfaction among nurses, thereby positively influencing their wellbeing and the overall effectiveness of healthcare systems if future pandemics or health crises.
4.4 Interventions to enhance job satisfaction during pandemics
Regarding interventions aimed at enhancing job satisfaction during the COVID-19 pandemic, this systematic review identified two studies with promising outcomes. Goktas, Gezginci et al. used a randomized controlled experiment focusing on the use of motivational messages to improve job satisfaction among emergency nurses (21). This aligns with other research highlighting the positive impact of motivational messages in nurses’ life satisfaction (57). Another noteworthy study included in the review used a longitudinal mixed methods design to investigate the effects of organizational proactive management interventions (22). This is particularly relevant as several studies have stressed the importance of organizational support in improving nurse’ job satisfaction (58, 59).
Taken together, these findings underscore the importance of multifaceted approaches in enhancing job satisfaction among healthcare professionals during a health crisis such as the COVID-19 pandemic. Motivational support and comprehensive organizational interventions can be critical components in addressing the unique challenges faced by nurses and ensuring their mental wellbeing and satisfaction, which in turn can contribute to better patient care.
4.5 Implications
The results of this systematic review have several implications for management, policy, practice, education, and future research. Managers and policymakers should consider implementing interventions such as motivational messaging and organizational proactive management interventions, as identified in the review, to improve job satisfaction among nurses, especially during health crises. Implementing policies that address nurses’ work environment ensuring adequate staffing, and providing support and resources may lead to enhanced job satisfaction. In terms of practice, the emphasis should be on establishing supportive supervision, reasonable workloads, and effective health measures to create a conducive work environment. For education, training programs should focus on equipping nurses with the necessary skills to handle the psychological and emotional challenges of their profession, particularly during a pandemic. Educators should also aim at building resilience in nurses and teaching coping strategies. Furthermore, there is a need for standardized tools for assessing job satisfaction, as the review highlighted the use of diverse measurement tools. Future research should focus on understanding the long-term impact of pandemics on job satisfaction and mental health among healthcare professionals. It is essential to develop evidence-based interventions that may be effectively integrated into the healthcare system to bolster job satisfaction, which in turn, could lead to better patient care and wellbeing among healthcare professionals.
4.6 Review limitation
A potential limitation of this review was the exclusive consideration of English-language studies. The utilization of differing methods to measure job satisfaction may have also influenced the aggregation of all the investigations, complicating the production of a holistic conclusion. It is also important to note that despite the diligent search for relevant studies to include in this review, the systematic search process may not have captured all applicable research, leading to possible omissions.
5 Conclusion
In conclusion, job satisfaction among nurses is multifactorial and requires an integrated approach to address personal, workplace, and psychological dimensions. During the COVID-19 pandemic, it is especially crucial to ensure that nurses have adequate support and resources to maintain their job satisfaction and wellbeing. This review yielded three principal outcomes: identification of the elements that correlated with nurses’ job satisfaction; analysis of the impact of nurses’ job satisfaction on nurses themselves and their patients; and the exploration of counteractive strategies linked to job satisfaction among nurses during COVID-19. The review meticulously analyzed a range of factors, including working conditions, staff relationships, compensation, and career development opportunities, that are correlated with job satisfaction. It also critically assessed the consequences of job satisfaction levels on both nurses and patients, highlighting the linkages between high job satisfaction and inclination to provide nursing care, reduced nurse burnout, and increased retention rates among nursing staff. Additionally, in recognition of the unique challenges faced during the COVID-19 pandemic, the review investigated various strategies such as organizational support, mental health resources, enhanced communication, and adaptive work environments to mitigate job dissatisfaction among nurses.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
YY: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Writing – original draft. AA: Conceptualization, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. AA-H: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. VK: Conceptualization, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Open access was funded by the University of Doha for Science and Technology.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1285101/full#supplementary-material
References
1. Cotrin, P, Moura, W, Gambardela-Tkacz, CM, Pelloso, FC, Santos, LD, Carvalho, MDB, et al. Healthcare Workers in Brazil during the COVID-19 pandemic: a cross-sectional online survey. Inquiry. (2020) 57:1–11. doi: 10.1177/0046958020963711
2. Lupu, D, and Tiganasu, R. COVID-19 and the efficiency of health systems in Europe. Heal Econ Rev. (2022) 12:14. doi: 10.1186/s13561-022-00358-y
3. Senek, M, Robertson, S, Ryan, T, King, R, Wood, E, Taylor, B, et al. Determinants of nurse job dissatisfaction – findings from a cross-sectional survey analysis in the UK. BMC Nurs. (2020) 19:88. doi: 10.1186/s12912-020-00481-3
4. Ekingen, E, Teleş, M, Yıldız, A, and Yıldırım, M. Mediating effect of work stress in the relationship between fear of COVID-19 and nurses’ organizational and professional turnover intentions. Arch Psychiatr Nurs. (2023) 42:97–105. doi: 10.1016/j.apnu.2022.12.027
5. Rizzo, A, Yıldırım, M, Öztekin, GG, Carlo, AD, Nucera, G, Szarpak, Ł, et al. Nurse burnout before and during the COVID-19 pandemic: a systematic comparative review. Front Public Health. (2023) 11:1225431. doi: 10.3389/fpubh.2023.1225431
6. de Oliveira, SD. Health of nursing professionals: workload during the COVID-19 pandemic. Revista Brasileira de Medicina Do Trabalho. (2021) 18:464–71. doi: 10.47626/1679-4435-2020-600
7. Park, SH. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infect Chemother. (2020) 52:165–82. doi: 10.3947/ic.2020.52.2.165
8. Turale, S, and Nantsupawat, A. Clinician mental health, nursing shortages and the COVID-19 pandemic: crises within crises. Int Nurs Rev. (2021) 68:12–4. doi: 10.1111/inr.12674
9. Levi, P, and Moss, J. Intensive care unit nurses’ lived experiences of psychological stress and trauma caring for COVID-19 patients. Workplace Health Safety. (2022) 70:358–67. doi: 10.1177/21650799211064262
10. Sihvola, S, Nurmeksela, A, Mikkonen, S, Peltokoski, J, and Kvist, T. Resilience, job satisfaction, intentions to leave nursing and quality of care among nurses during the COVID-19 pandemic - a questionnaire study. BMC Health Serv Res. (2023) 23:632. doi: 10.1186/s12913-023-09648-5
11. Galanis, P, Vraka, I, Fragkou, D, Bilali, A, and Kaitelidou, D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. (2021) 77:3286–302. doi: 10.1111/jan.14839
12. Hoşgör, H, and Yaman, M. Investigation of the relationship between psychological resilience and job performance in Turkish nurses during the Covid-19 pandemic in terms of descriptive characteristics. J Nurs Manag. (2022) 30:44–52. doi: 10.1111/jonm.13477
13. Yasin, YM, Khraim, F, and Kehyayan, V. Job satisfaction among expatriate nurses during the COVID-19 pandemic: a cross-sectional study. Int Nurs Rev. (2023) 11:12847. doi: 10.1111/inr.12847
14. Gimenez-Espert, MDC, Prado-Gasco, V, and Soto-Rubio, A. Psychosocial risks, work engagement, and job satisfaction of nurses during COVID-19 pandemic. Front Public Health. (2020) 8:566896. doi: 10.3389/fpubh.2020.566896
15. Munn, Z, Moola, S, Lisy, K, Riitano, D, and Tufanaru, C In: E Aromataris and Z Munn, editors. Systematic reviews of prevalence and incidence : JBI manual for evidence synthesis Joanna Briggs Institute (2020)
16. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
18. Barker, TH, Stone, JC, Sears, K, Klugar, M, Tufanaru, C, Leonardi-Bee, J, et al. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evidence Synth. (2023) 21:494–506. doi: 10.11124/JBIES-22-00430
19. Tufanaru, C, Munn, Z, Aromataris, E, Campbell, J, and Hopp, L. Systematic reviews of effectiveness. E Aromataris and Z Munn, (Eds.) JBI manual for Evidence Synthesis: JBI ; (2020)
20. Moola, S, Munn, Z, Tufanaru, C, Aromataris, E, Sears, K, Sfetcu, R, et al. In: E Aromataris and Z Munn, editors. Systematic reviews of etiology and risk : Manual for Evidence Synthesis (2020)
21. Goktas, S, Gezginci, E, and Kartal, H. The effects of motivational messages sent to emergency nurses during the COVID-19 pandemic on job satisfaction, compassion fatigue, and communication skills: a randomized controlled trial. J Emerg Nurs. (2022) 48:547–58. doi: 10.1016/j.jen.2022.06.001
22. Zaghini, F, Fiorini, J, Livigni, L, Carrabs, G, and Sili, A. A mixed methods study of an organization’s approach to the COVID-19 health care crisis. Nurs Outlook. (2021) 69:793–804. doi: 10.1016/j.outlook.2021.05.008
23. Chong, YY, Frey, E, Chien, WT, Cheng, HY, and Gloster, AT. The role of psychological flexibility in the relationships between burnout, job satisfaction, and mental health among nurses in combatting COVID-19: a two-region survey. J Nurs Scholarsh. (2023) 55:1068–81. doi: 10.1111/jnu.12874
24. Makowicz, D, Lisowicz, K, Bryniarski, K, Dziubaszewska, R, Makowicz, N, and Dobrowolska, B. The impact of the COVID-19 pandemic on job satisfaction among professionally active nurses in five European countries. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.1006049
25. Heidari, S, Parizad, N, Goli, R, Mam-Qaderi, M, and Hassanpour, A. Job satisfaction and its relationship with burnout among nurses working in COVID-19 wards: a descriptive correlational study. Ann Med Surg. (2022) 82:82. doi: 10.1016/j.amsu.2022.104591
26. Said, RM, and El-Shafei, DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City. Egypt Environ Sci Pollut Res. (2021) 28:8791–801. doi: 10.1007/s11356-020-11235-8
27. Da Rosa, P, Brown, R, Pravecek, B, Carotta, C, Garcia, AS, Carson, P, et al. Factors associated with nurses emotional distress during the COVID-19 pandemic. Appl Nurs Res. (2021) 62:151502. doi: 10.1016/j.apnr.2021.151502
28. Hwang, E. Factors affecting the quality of work life of nurses at tertiary general hospitals in the context of the COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:84718. doi: 10.3390/ijerph19084718
29. Niu, A, Li, P, Duan, P, Ding, L, Xu, S, Yang, Y, et al. Professional quality of life in nurses on the frontline against COVID-19. J Nurs Manag. (2022) 30:1115–24. doi: 10.1111/jonm.13620
30. Appel, AP, Carvalho, A, and Santos, RPD. Prevalence and factors associated with anxiety, depression and stress in a COVID-19 nursing team. Revista Gaucha de Enfermagem. (2021) 42:e20200403. doi: 10.1590/1983-1447.2021.20200403
31. Işıklı, AG, Şen, H, and Soydaş, D. Assessment of psychological resilience, job satisfaction, and fear level of nurses infected and not infected with the COVID-19 virus. J Psychiatr Nurs. (2021) 12:281–7. doi: 10.14744/phd.2021.57983
32. Malinowska-Lipień, I, Wadas, T, Gabryś, T, Kózka, M, Gniadek, A, Brzostek, T, et al. Evaluating polish nurses’ working conditions and patient safety during the COVID-19 pandemic. Int Nurs Rev. (2022) 69:239–48. doi: 10.1111/inr.12724
33. Chowdhury, SR, Kabir, H, Mazumder, S, Akter, N, Chowdhury, MR, and Hossain, A. Workplace violence, bullying, burnout, job satisfaction and their correlation with depression among Bangladeshi nurses: a cross-sectional survey during the COVID-19 pandemic. PLoS One. (2022) 17:e0274965. doi: 10.1371/journal.pone.0274965
34. Gorini, A, Giuliani, M, Fiabane, E, Bonomi, A, Gabanelli, P, Pierobon, A, et al. Prevalence of psychopathological symptoms and their determinants in four healthcare workers’ categories during the second year of COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:712. doi: 10.3390/ijerph192013712
35. Labrague, LJ, and Santos, JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. (2021) 29:395–403. doi: 10.1111/jonm.13168
36. Yeung, NCY, Wong, ELY, Cheung, AWL, Leung, CSY, Yeoh, EK, and Wong, SYS. Finding the positives from the COVID-19 pandemic: factors associated with posttraumatic growth among nurses in Hong Kong. Eur J Psychotraumatol. (2022) 13:5346. doi: 10.1080/20008198.2021.2005346
37. Yeung, NCY, Wong, ELY, Cheung, AWL, Yeoh, EK, and Wong, SYS. Feeling anxious amid the COVID-19 pandemic: factors associated with anxiety symptoms among nurses in Hong Kong. Front Psychol. (2021) 12:748575. doi: 10.3389/fpsyg.2021.748575
38. Lavoie-Tremblay, M, Gélinas, C, Aubé, T, Tchouaket, E, Tremblay, D, Gagnon, MP, et al. Influence of caring for COVID-19 patients on nurse’s turnover, work satisfaction and quality of care. J Nurs Manag. (2022) 30:33–43. doi: 10.1111/jonm.13462
39. Sharif Nia, H, Arslan, G, Naghavi, N, Sivarajan Froelicher, E, Kaveh, O, Pahlevan Sharif, S, et al. A model of nurses’ intention to care of patients with COVID-19: mediating roles of job satisfaction and organisational commitment. J Clin Nurs. (2021) 30:1684–93. doi: 10.1111/jocn.15723
40. Sampaio, F, Salgado, R, Antonini, M, Delmas, P, Oulevey Bachmann, A, Gilles, I, et al. Workplace wellbeing and quality of life perceived by Portuguese nurses during the COVID-19 pandemic: the role of protective factors and stressors. Int J Environ Res Public Health. (2022) 19:4231. doi: 10.3390/ijerph192114231
41. Savitsky, B, Radomislensky, I, and Hendel, T. Nurses’ occupational satisfaction during Covid-19 pandemic. Appl Nurs Res. (2021) 59:151416. doi: 10.1016/j.apnr.2021.151416
42. Barili, E, Bertoli, P, Grembi, V, and Rattini, V. Job satisfaction among healthcare workers in the aftermath of the COVID-19 pandemic. PLoS One. (2022) 17:e0275334. doi: 10.1371/journal.pone.0275334
43. Llop-Gironés, A, Vračar, A, Llop-Gironés, G, Benach, J, Angeli-Silva, L, Jaimez, L, et al. Employment and working conditions of nurses: where and how health inequalities have increased during the COVID-19 pandemic? Hum Resour Health. (2021) 19:112. doi: 10.1186/s12960-021-00651-7
44. Jihn, C-H, Kim, B, and Kim, KS. Predictors of burnout in hospital health workers during the COVID-19 outbreak in South Korea. Int J Environ Res Public Health. (2021) 18:720. doi: 10.3390/ijerph182111720
45. Hauff, S, Richter, NF, and Tressin, T. Situational job characteristics and job satisfaction: the moderating role of national culture. Int Bus Rev. (2015) 24:710–23. doi: 10.1016/j.ibusrev.2015.01.003
46. Yasin, YM, Kerr, MS, Wong, CA, and Bélanger, CH. Factors affecting nurses’ job satisfaction in rural and urban acute care settings: a PRISMA systematic review. J Adv Nurs. (2020) 76:963–79. doi: 10.1111/jan.14293
47. Lu, H, Barriball, KL, Zhang, X, and While, AE. Job satisfaction among hospital nurses revisited: a systematic review. Int J Nurs Stud. (2012) 49:1017–38. doi: 10.1016/j.ijnurstu.2011.11.009
48. Chien, WT, and Yick, SY. An investigation of nurses’ job satisfaction in a private hospital and its correlates. Open Nurs J. (2016) 10:99–112. doi: 10.2174/1874434601610010099
49. Chan, XW, Kalliath, P, Chan, C, and Kalliath, T. How does family support facilitate job satisfaction? Investigating the chain mediating effects of work-family enrichment and job-related well-being. Stress Health. (2020) 36:97–104. doi: 10.1002/smi.2918
50. Kovner, CT, Brewer, CS, Greene, W, and Fairchild, S. Understanding new registered nurses’ intent to stay at their jobs. Nurs Econ. (2009) 27:81–98.
51. Persefoni, L. Nurses perceptions of their professional practice environment in relation to job satisfaction: a review of quantitative studies. Health Sci J. (2014) 8:298–317.
52. Lee, M, and Jang, K-S. Nurses’ emotions, emotional labor, and job satisfaction. Int J Workplace Health Manag. (2020) 13:16–31. doi: 10.1108/IJWHM-01-2019-0012
53. Utriainen, K, Ala-Mursula, L, and Kyngäs, H. Hospital nurses’ wellbeing at work: a theoretical model. J Nurs Manag. (2015) 23:736–43. doi: 10.1111/jonm.12203
54. Choi, KR, Skrine Jeffers, K, and Cynthia, LM. Nursing and the novel coronavirus: risks and responsibilities in a global outbreak. J Adv Nurs. (2020) 76:1486–7. doi: 10.1111/jan.14369
55. Yasin, YM, Kerr, MS, Wong, CA, and Bélanger, CH. Factors affecting job satisfaction among acute care nurses working in rural and urban settings. J Adv Nurs. (2020) 76:2359–68. doi: 10.1111/jan.14449
56. Greenberg, N, Docherty, M, Gnanapragasam, S, and Wessely, S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. (2020) 368:m1211. doi: 10.1136/bmj.m1211
57. Köse, S, Gezginci, E, Göktaş, S, and Murat, M. The effectiveness of motivational messages to intensive care unit nurses during the COVID-19 pandemic. Intens Crit Care Nurs. (2022) 69:103161. doi: 10.1016/j.iccn.2021.103161
58. Chang, CS. Moderating effects of nurses’ organizational support on the relationship between job satisfaction and organizational commitment. West J Nurs Res. (2015) 37:724–45. doi: 10.1177/0193945914530047
Keywords: job satisfaction, COVID-19, systematic review, healthy work environment, healthcare management
Citation: Yasin YM, Alomari A, Al-Hamad A and Kehyayan V (2024) The impact of COVID-19 on nurses’ job satisfaction: a systematic review and meta-analysis. Front. Public Health. 11:1285101. doi: 10.3389/fpubh.2023.1285101
Edited by:
Murat Yildirim, Ağrı İbrahim Çeçen University, TürkiyeReviewed by:
Rita de Cássia Akutsu, University of Brasilia, BrazilHamid Sharif-Nia, Mazandaran University of Medical Sciences, Iran
Copyright © 2024 Yasin, Alomari, Al-Hamad and Kehyayan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yasin M. Yasin, eWFzaW4ueWFzaW5AdWRzdC5lZHUucWE=
†ORCID: Yasin M. Yasin, https://orcid.org/0000-0003-0599-7180
Albara Alomari, https://orcid.org/0000-0001-7693-4617
Areej Al-Hamad, https://orcid.org/0000-0002-6400-0750
Vahe Kehyayan, https://orcid.org/0000-0002-2462-7399
 Yasin M. Yasin
Yasin M. Yasin Albara Alomari
Albara Alomari Areej Al-Hamad2†
Areej Al-Hamad2† Vahe Kehyayan
Vahe Kehyayan