- 1School of Public Health, Wannan Medical College, Wuhu, China
- 2Institutes of Brain Science, Wannan Medical College, Wuhu, China
- 3Department of Nursing, Anhui College of Traditional Chinese Medicine, Wuhu, China
- 4Nursing Department, Yijishan Hospital of Wannan Medical College, Wuhu, China
Objective: Medication adherence has a critical impact on the well-being of older adult patients with hypertension. As such, the current study aimed to investigate the mediating role of health literacy between frailty and medication adherence and the moderating role of educational level.
Methods: This cross-sectional study included patients admitted to the geriatric unit of a hospital. Participants were interviewed using the four-item Morisky Medication Adherence Scale, the Frailty Phenotype Scale, and the Health Literacy Management Scale. Spearman’s correlation coefficients were used to assess the association between variables. Mediation and moderated mediation analyses were performed using Process version 4.1 via Model 4 and 14, respectively.
Results: Data from 388 participants were analyzed. The median (IQR [P25–P75]) score for medication adherence was 4.00 (2.00–4.00). Results revealed that after controlling for age, sex, hypertension complication(s) and body mass index, frailty significantly contributed to medication adherence (βtotal −0.236 [95% confidence interval (CI) −0.333 to −0.140]). Medication adherence was influenced by frailty (βdirect −0.192 [95% CI −0.284 to −0.099]) both directly and indirectly through health literacy (βindirect −0.044 [95% CI −0.077 to −0.014]). Educational level moderated the pathway mediated by health literacy; more specifically, the conditional indirect effect between frailty and medication adherence was significant among older adult hypertensive patients with low, intermediate, and high educational levels (effect −0.052 [95% CI −0.092 to −0.106]; effect −0.041 [95% CI −0.071 to −0.012]; effect −0.026 [95% CI −0.051 to −0.006]). The relationship between frailty and medication adherence in older adult patients with hypertension was found to have mediating and moderating effects.
Conclusion: A moderated mediation model was proposed to investigate the effect of frailty on medication adherence. It was effective in strengthening medication adherence by improving health literacy and reducing frailty. More attention needs to be devoted to older adult patients with hypertension and low educational levels.
Introduction
The burden of disease due to hypertension remains high because it is the most important risk factor for all-cause mortality, disability, and global disability-adjusted life years (1). The prevalence of hypertension is significantly higher among older vs. younger individuals (2, 3). A pooled analysis of 104 million subjects found that, between 1990 and 2019, the prevalence and number of individuals with hypertension 30–79 years of age changed from 32% among females and 34% in males to 32% in females and 32% in males, and from 648 million to 1,278 million, respectively (4). A relatively recent national survey conducted in 2018 revealed that the weighted prevalence of hypertension among Chinese adults was 27.5 (5). The prevalence of hypertension in rural adults was higher than that in urban adults (29.4% vs. 25.7%, respectively) (6). With an increase in age among populations, the prevalence of hypertension has increased significantly, with >50% in 60–69 years and >60% in those ≥70 years of age (6). Studies have shown that most patients with hypertension worldwide do not meet blood pressure control standards, especially in low-income countries (4, 7, 8). Poor medication adherence is also a key factor (9). The prevalence of hypertension can be decreased in settings with a range of income levels by improving treatment and control, although there are significant differences in the rates of hypertension treatment and control across nations (4). We cannot reverse the trend in aging populations, which poses a serious threat to the burden of hypertension. However, measures can be taken to mitigate this burden, such as improving patient care and management and, specifically, increasing drug adherence.
Medication adherence refers to the consistency between patient medical adherence and physician recommendations (10). It is influenced by factors including patient-provider relationships, health literacy, age, sex, education, place of residence, income, frailty, family support, attitude, cost of medication, and comorbidities (11–14). Poor medication adherence is the leading cause of poor blood pressure control (15, 16). In one study, patients with good medication adherence were 45% more likely to achieve blood pressure control than those with poor adherence (17), and good medication adherence reduced the risk for cardiovascular outcomes by 37% (18). According to one study, more than one-third of cardiovascular fatalities among Chinese individuals are attributable to poor blood pressure management (19). Improved medication adherence is believed to have a substantially more significant impact on health than improving specific medical treatments/therapies (20), and enhanced medication adherence can significantly reduce cardiovascular events (21). In addition, according to the World Health Organization, poor adherence is the primary factor responsible for uncontrolled blood pressure (22). Therefore, increasing medication adherence in patients with hypertension is essential.
Frailty is defined as a reduction in physiological capacity and increase in vulnerability to stress, both of which are common in older individuals (23). At ages >60 and 80 years’, the prevalence of frailty increases to 15–20 and 30%, respectively (24). This has many similarities to individuals who are susceptible to hypertension. Frailty is an important determinant of longevity and quality of life among the older adult (25) and can be reversed, especially if detected early (26). A population-based study in China reported that the prevalence of frailty in older adults with hypertension was 13.8% (27). Hypertension is more likely to occur in fragile, older adult individuals (28). Frailty negatively affects blood pressure control in older adult patients with hypertension (29) as well as prognosis and adherence to therapy (11). The physical and mental health of older adult individuals are negatively affected due to the onset and development of frailty, which is frequently accompanied by several medical and mental illnesses such as anxiety, depression, cardiovascular disease, and cognitive impairment. Early recognition of frailty in older adult patients with hypertension and appropriate counseling will help ensure their quality of life (11). A possible explanation for this is that the degeneration of physiological functions in the older adult accelerates the progression of frailty, and the occurrence of frailty leads to further deterioration of physiological functions, resulting in the abnormal distribution and metabolism of drugs in the body, eventually increasing the occurrence of adverse drug reactions (30). In addition, frail patients tend to experience negative emotions that exacerbate adverse drug effects and may choose avoidance behaviors that translate into low medication compliance (30). Several studies have concluded that patients with frailty and chronic diseases exhibit poor medication adherence (24, 31, 32).
Health literacy refers to the ability of individuals to acquire, understand and use basic health information and health services so they are able to make the correct health decisions to promote and maintain their own health (33). It can also be condensed into the capacity to make decisions that would improve and preserve one’s well-being (34). Studies have shown that patient health literacy levels increase with educational level (35–37). Health literacy plays a significant role in facilitating the management and prevention of various chronic diseases, reducing the occurrence of various complications, and improving quality of life (38). Since the concept of health literacy was proposed, an increasing number of studies have addressed its relationship with medication adherence (39–42). High health literacy may enhance patient capacity for self-management and medication adherence (43). Studies have presented conflicting results regarding the association between medication adherence and health literacy, including a significant positive correlation (44–46), a significant negative correlation (47), and no significant correlation (48–50). Meanwhile, inadequate health literacy is a concern because it directly influences patient decisions to take medications (51). Compared with individuals with sufficient health literacy, inadequate health literacy has been associated with less optimal medication adherence (52, 53). Patients with low health literacy are more likely to misinterpret prescription label information, which can lead to adverse effects such as poor medication adherence (54). Conversely, better medication adherence and decreased likelihood of misinterpreting pharmaceutical recommendations have been associated with higher levels of health literacy (55). In addition, some studies have demonstrated an association between frailty and the absence of health literacy (56, 57). The association between adequate health literacy and a lower frequency of frailty was also supported by a recent study conducted in 2023 among older community-dwelling adults (58).
In clinical practice, it is crucial to understand the potential mechanisms underlying these predictions and how they relate to medication adherence. In summary, the primary objective of current study was to determine the impact of frailty on medication adherence in older adult patients with hypertension; the second objective was to verify whether health literacy mediates the relationship between frailty and medication adherence; and the third objective was to assess the level of education as a moderating variable. The present study was prompted by lack of studies investigating the impact of frailty on medication adherence and health literacy. We established and verified a moderated mediation model based on two additional variables (i.e., health literacy and educational level). Therefore, our first hypothesis proposes that the association between frailty and medication adherence is significantly mediated by health literacy; the second proposes that the association between health literacy and medication adherence is moderated by educational level.
Materials and methods
Study design
A cross-sectional analytical observational design was used to explore the influence of frailty and health literacy on medication adherence among older individuals with hypertension, from June 1, 2019, to December 31, 2019, among geriatric inpatients at a hospital in Wuhu, China. Data were obtained using a questionnaire. This study was approved by the Institutional Research Ethics Committee, and informed consent was obtained from all subjects included in the study. Inpatients ≥60 years of age, who had already been diagnosed with hypertension, were recruited for this study. Individuals who were unwilling to participate in the study and could not express themselves clearly were excluded. Patients who fulfilled the inclusion criteria were selected daily through the admission system and face to face interviewed the next day, after which informed consent was obtained. Each Saturday, a questionnaire was administered to the recruited subjects. In total, 400 patients who fulfilled the criteria were initially recruited, 10 of whom refused to complete the questionnaire on Saturday, and 2 had already been discharged from hospital before completing the questionnaire. Ultimately, therefore, the final sample comprised 388 subjects, corresponding to a response rate of 97%.
Measures
Trained personnel were recruited to distribute and collect the paper questionnaires, explain the items to illiterate individuals, and record the questionnaire. The questionnaire recorded sociodemographic characteristics such as age, sex, smoking status, alcohol consumption status, height, weight, and educational level, as well as three specific scales.
Medication adherence was evaluated using the 4-item Morisky Medication Adherence Scale (MMAS-4), a reliable self-reported scale (59). Each item was assigned a score of 0 or 1 for “yes” or “no,” respectively. The total score ranged from 0 to 4, with higher scores indicating better medication adherence (45). The Cronbach’s α in the current study was 0.832, demonstrating the reliability of internal consistency.
Frailty was measured using the Frailty Phenotype Scale (FPS), developed by Fried and colleagues in 2001 (60) and widely used in clinical research (61). The Frailty Phenotype Scale was included in the Chinese Expert Consensus for Assessment and Intervention in Older Adult Patients with Frailty (62) and is also widely used by Chinese researchers (63–65). The Frailty Phenotype Scale consists of 5 items addressing unintentional weight loss, walking speed, grip strength, self-reported exhaustion, and physical activity. Each item was assigned a score of 0 or 1 corresponding to a response of “no” or “yes,” respectively. The cumulative score ranged from 0 to 5, with a higher score indicating a higher degree of frailty (66). The Cronbach’s α in the present study was 0.749, demonstrating the reliability of internal consistency.
Health literacy was evaluated using the Health Literacy Management Scale (HeLMS) proposed by Jordan et al. (67). The Chinese version of the HeLMS was adapted according to Chinese cultural customs and population characteristics to assess health literacy in patients with chronic diseases, especially hypertension (68). It comprises 24 items. Each item was scored on a five-point Likert scale (from totally unable or unwilling to without any difficulty or great willingness), with a total score of 120. A higher score indicated a higher level of health literacy. The Cronbach’s α in the current study was 0.917, demonstrating the reliability of internal consistency.
Statistical analysis
All statistical analyses were performed using SPSS version 25.0. Subject sociodemographic and clinical characteristics and study variables are described. Categorical variables are described as number (percentage), and numerical variables are expressed as mean with standard deviation (SD) or median (interquartile range [i.e., P25, P75]). The study variables were confirmed to have skewed distributions according to the Kolmogorov–Smirnov test, including frailty, health literacy, and medication adherence. Spearman’s correlation coefficients were used to assess associations among educational level, frailty, health literacy, and medication adherence. To statistically test for the presence of variance in the common methods, the Harman single factor test in SPSS v.25.0 and Confirmatory Factor Analysis in Mplus version 8.0 were performed. In addition, mediation analysis was performed to examine whether health literacy mediated the relationship between frailty and medication adherence (PROCESS 4.1, Model 4). Finally, a moderated mediation analysis was performed using PROCESS 4.1 (Model 14) to examine whether educational level moderated the relationship between health literacy and medication adherence. To confirm the moderating role of education level on health literacy and medication adherence, a simple slope test was performed to assess the relationship between health literacy and medication adherence at different educational levels. The indirect effect of mediation was estimated using a 5,000-sample bootstrapping method, with a significant effect indicated by a 95% confidence interval (CI) that did not include zero. Differences with p < 0.05 were considered to be statically significant.
Results
Common-method variance test
The results of the Harman single-factor test revealed that 6 factors had Eigenvalues >1, and the first common factor explained 26.71% (<40%) of total variation. The fitting indices of the confirmatory factor analysis were poor: root mean square error of approximation (i.e., “RMSEA”) = 0.200; comparative fit index (i.e., “CFI”) = 0.342; Tucker–Lewis index (i.e., “TLI”) = 0.298; and standardized root mean square residual (i.e., “SRMR”) = 0.237. Therefore, variance in the common method was not a concern.
Patient characteristics
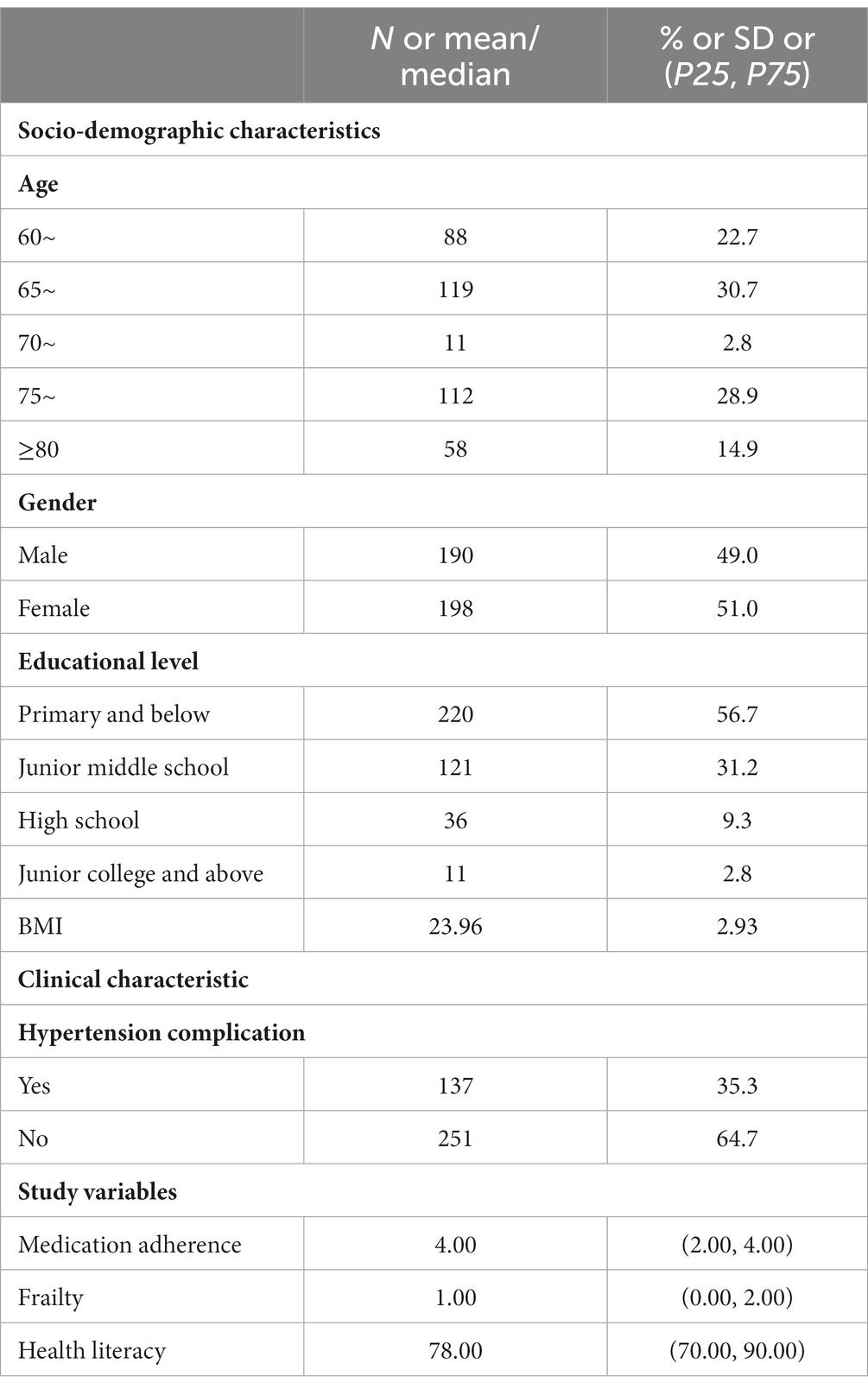
Subjects exhibited a mean (± SD) body mass index of 23.96 ± 2.93 kg/m2; 190 patients were male (49.0%), 47 had a high school diploma or higher (12.1%), and 119 (30.7%) were 65–70 years of age (Table 1). Based on diagnosis, 137 subjects developed hypertensive complications. In addition, the median (IQR [P25–P75]) scores for medication adherence, frailty and health literacy were 4.00 (2.00–4.00), 1.00 (0.00–2.00) and 78.00 (70.00–90.00), respectively.
Correlations among variables
The results of correlation analyses are summarized in Table 2. Medication adherence (rs = 0.196, p < 0.001), frailty (rs = −0.117, p < 0.05) and health literacy (rs = 0.354, p < 0.001) are all significantly correlated with educational level. Frailty (rs = −0.223, p < 0.001) and health literacy (rs = 0.301, p < 0.001) were both significantly correlated with medication adherence. In addition, a significant and negative correlation was found between frailty and health literacy (rs = −0.128, p < 0.05).
Testing for mediation
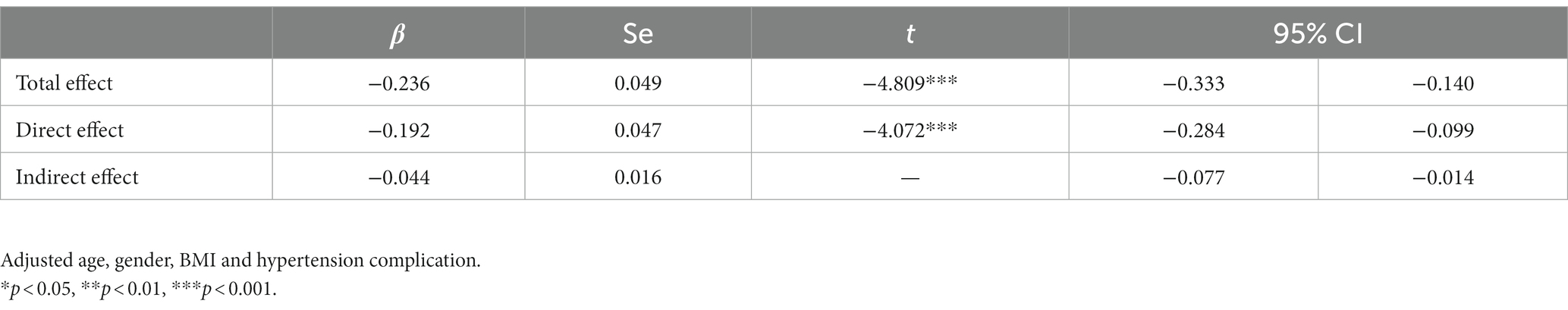
The mediating effects of health literacy are summarized in Table 3. Frailty exerted a significant negative effect on medication adherence (β = −0.236, t = −4.809, p < 0.001) and on health literacy (β = −1.583, t = −2.832, p < 0.01). When the mediating variable health literacy was added, the direct effect of frailty on medication adherence remained significant (β = −0.192, t = −4.072, p < 0.001), indicating partial mediation. Health literacy had a significant positive effect on medication adherence (β = 0.028, t = 6.583, p < 0.001). The partial mediation of health literacy was verified using the bootstrapping method, and the indirect effect accounted for 18.64% of the total effect (Table 4). Thus, this model indicated that the first hypothesis was fulfilled. More specifically, the relationship between frailty and medication adherence was partially mediated by health literacy, and frailty was associated with medication adherence both directly and indirectly through health literacy.
Testing for moderated mediation
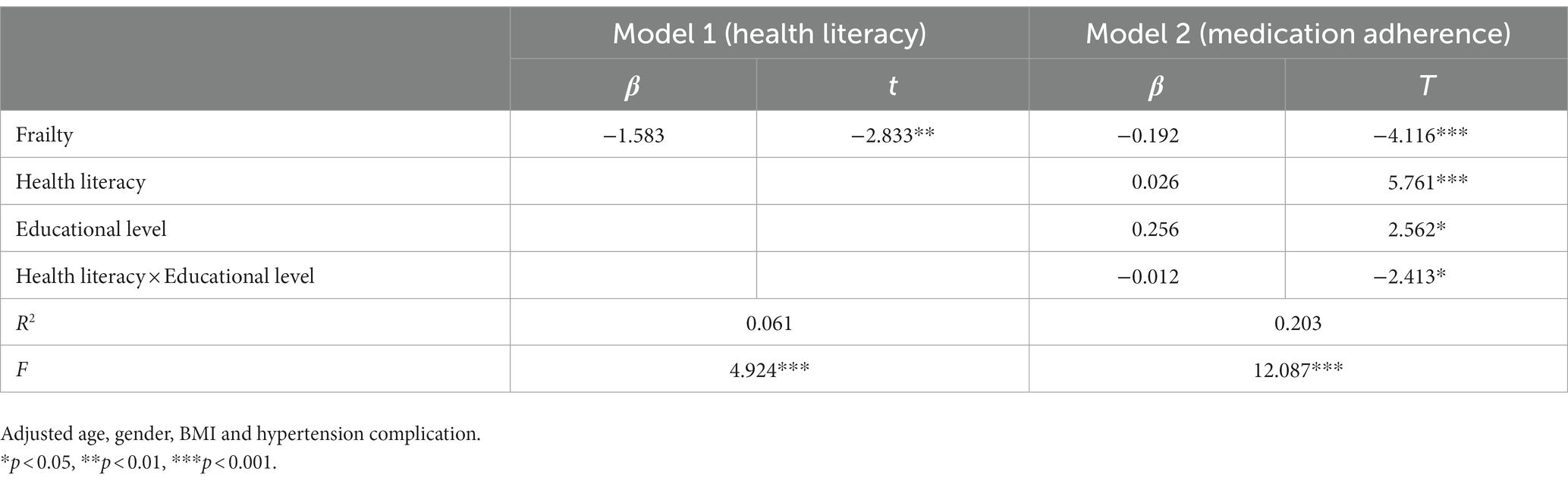
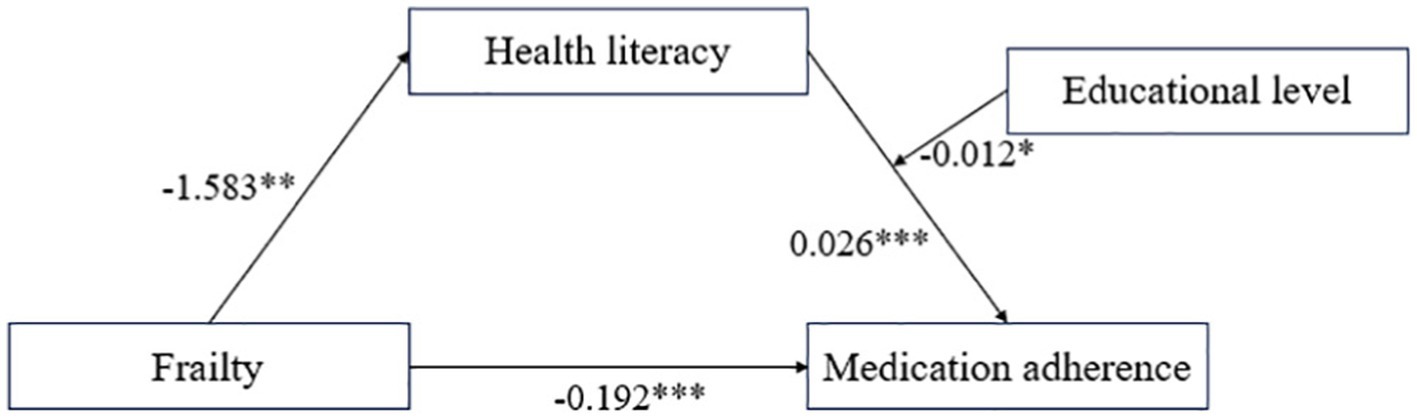
Educational level significantly moderated the indirect effect of frailty on medication adherence through health literacy (Tables 5, 6, Figure 1). Data reported in Table 5 show that health literacy was positively correlated with medication adherence (β = 0.026, t = 5.761, p < 0.001), and the interaction between health literacy and educational level exerted a significant negative effect on medication adherence (β = −0.012, t = −2.413, p < 0.05), while frailty had a significant negative effect on health literacy (β = −1.583, t = −2.833, p < 0.01). Furthermore, the direct effect of frailty on medication adherence was 0.192 (t = −4.116, p < 0.001). The path coefficients of the moderated mediation model are shown in Figure 1. The data revealed that the association between health literacy and medication adherence was stronger in individuals with low level(s) of education (β = 0.033, t = 5.953, p < 0.001) than in individuals with high levels of education (β = 0.017, t = 2.916, p < 0.01) (Figure 2). In addition, bias-corrected percentile bootstrap analysis confirmed that frailty indirectly influenced medication adherence through health literacy, which was moderated by different levels of education. Specifically, the conditional indirect effect between frailty and medication adherence was significant among individuals with all levels of education (low, effect −0.052 [95% CI −0.092 to −0.016]; medium, effect −0.041 [95% CI −0.071 to −0.012]; and high, effect −0.026 [95% CI −0.051 to −0.006]) (Table 6). The moderated mediation index was 0.019 (95% CI 0.003 to 0.043), confirming the effect of moderated mediation. In summary, these results confirm the second hypothesis. In other words, educational level moderated the relationship between health literacy and medication adherence. More specifically, health literacy had a significant positive predictive effect on medication adherence at different educational levels, and the positive predictive effect of health literacy on medication adherence gradually decreased with increasing educational level.
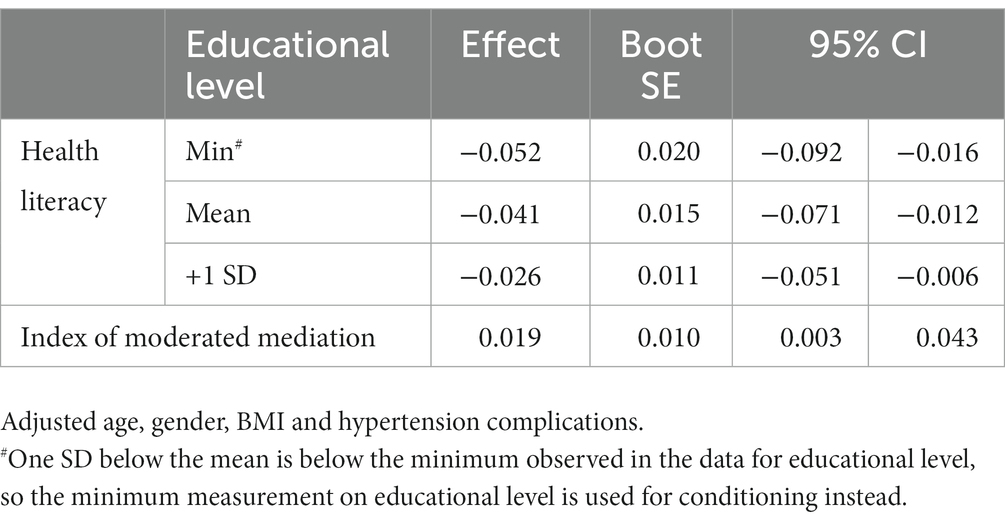
Table 6. Conditional indirect effect of educational level when health literacy mediated between frailty and medication adherence.
Discussion
In the current study, 233 (60.1%) subjects demonstrated good medication adherence. According to previous research, the percentage of patients with good adherence fluctuates significantly (69–71). This may be due to the diverse evaluation methods and different demographic characteristics (14). Numerous studies have demonstrated the effects of frailty on medication adherence (30–32), although few have focused on the potential mediators and regulatory mechanisms that represent how and when frailty occurs. Our data demonstrated that frailty was related to medication adherence both directly and indirectly through health literacy. The educational level of older patients with hypertension may moderate health and, thus, influence medication adherence.
Mediating role of health literacy
These results are consistent with previous studies reporting that frailty has a significant negative effect on health literacy (43, 58). The higher the frailty of the participant(s), the more their physiological capacity was reduced, which was associated with increased susceptibility to stressors, and the less likely they were able to obtain health-related information and, consequently, the lower their health literacy. Health literacy was a significant and positive predictor of treatment adherence, consistent with previous research findings (52, 53). People with low health literacy do not realize the importance of medication adherence, and they live an unhealthy lifestyle (15). Frailty had a negative and significant direct effect on medication adherence among older adult patients. Pharmacokinetics may partially explain this relationship. Due to changes in body fat lean tissue, and oxidative metabolic enzymes in frail patients, the distribution of drugs in the body and metabolism are prone to change, which predisposes to the occurrence of side effects and, in turn, poor medication adherence (30). Frailty in older adult patients is often associated with anxiety, depression, inadequate social support, lack of care, and supervision by others. When taking medication as prescribed by a physician, it is easier to exacerbate the adverse effects of taking the medication and even question the need to take the medication due to the lack of short-term efficacy, resulting in poor medication adherence (72). Health literacy is an inherent health promotion skill essential for processing medication information and taking medication correctly (73). Individuals with high health literacy are better able to receive, process, and understand health information; therefore, they participate more actively in decision-making and health actions, resulting in better medication adherence (74, 75). Inadequate health literacy is one of the main factors leading to poor medication adherence in patients with hypertension (46, 76). Therefore, improving health literacy has been suggested as an effective measure for improving medication adherence (76, 77).
Moderating role of educational level
Data from the present study revealed that participant educational level moderated the indirect effect between frailty and medication adherence. The moderating point was in the second half of the intermediate chain; more specifically, the relationship between health literacy and medication adherence depended on educational level. Compared with individuals with higher education levels, the indirect effect was stronger for individuals with a lower education level (Table 6). Medication adherence among individuals with higher education levels was generally higher than that among those with lower education levels (Figure 2), suggesting that more attention should be devoted to individuals with lower educational levels. This moderation could be due to the fact that individuals with higher levels of education already have higher health literacy (78–81) as well as higher medication adherence (20, 82–84), which was consistent with our analysis of the association between educational level and health literacy (rs = 0.354, p < 0.001) and medication adherence (rs = 0.196, p < 0.001). However, for individuals with lower levels of education, an increase in health literacy could have a stronger impact on improving medication adherence. Individuals with higher levels of education tend to have higher health demands than those with lower levels of education and tend to understand the importance of medication (85). Conversely, those with lower levels of education are more likely to make mistakes, have less medical knowledge, and have superstitious beliefs (85). Therefore, they are more likely to make poor decisions when experiencing health problems. Improving educational level is difficult for older adults. However, features that benefit from education can also improve medication adherence by designing easy-to-understand educational materials, breaking down multistep or complex skills into smaller steps, and encouraging the older population to repeat information in their own words, such as reading, learning, and applying new information and specific skills (i.e., background knowledge) (86, 87). In addition, creating a positive community environment for trusting the science and rejecting superstitious beliefs would be helpful in improving medication adherence.
Limitations and further research directions
Although the current study advances the understanding of the mediating and moderating mechanisms underlying the association between frailty and medication adherence among older adult individuals with hypertension, several limitations should be addressed. First, subjects were recruited from a single hospital, and the sample size was small; therefore, the results may not be generalizable to all older adult patients with hypertension. Further studies should be conducted in multicenter settings with sufficient sample sizes to ensure the generalizability of the conclusions. Second, this study used a cross-sectional design, which precluded the ability to infer causality. Longitudinal studies should be performed in the future to further verify the causal relationships between variables. Third, our data were self-reported, making them susceptible to a social desirability bias. Data for further studies should be obtained from objective tests or from multiple informants. Fourth, our study used a non-random sampling method, which has an unfavorable effect on the representativeness of the samples. We will use a more appropriate sampling method in the follow-up study.
Conclusion
Although some studies have focused on the relationship between frailty and medication, little attention has been devoted to the mediation and moderation mechanisms underlying this association in older adult patients with hypertension. Our results suggest that more attention should be paid to patients with frailty and low educational level to achieve a greater breakthrough in medication adherence in older adult patients with hypertension. The clinical implication for us is that we should focus on hypertensive patients with frail, hypertensive patients with low health literacy, and hypertensive patients with low education level to better control the blood pressure of older adult patients with hypertension.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Scientific Research and New Technology of Wannan Medical College Yijishan Hospital IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AW: Data curation, Writing – original draft, Writing – review & editing. JW: Data curation, Investigation, Writing – original draft, Writing – review & editing. LZ: Data curation, Writing – review & editing. WC: Investigation, Writing – review & editing. LW: Writing – review & editing, Investigation. XT: Conceptualization, Supervision, Writing – review & editing. YJ: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by National Natural Science Foundation of China (82003546), Natural Science Foundation of Anhui Province (1808085MH297), Anhui Province Quality Engineering Project (2020jyxm2086, 2022jyxm1699), Wannan Medical College Quality Engineering Project (2021jyxm43).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Collaborators, GBDRF. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1659–724. doi: 10.1016/S0140-6736(16)31679-8
2. Mozaffarian, D, Benjamin, EJ, Go, AS, Arnett, DK, Blaha, MJ, Cushman, M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. (2015) 131:e29–e322. doi: 10.1161/CIR.0000000000000152
3. Bavishi, C, Goel, S, and Messerli, FH. Isolated systolic hypertension: an update after SPRINT. Am J Med. (2016) 129:1251–8. doi: 10.1016/j.amjmed.2016.08.032
4. Collaboration NCDRF. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398:957–80. doi: 10.1016/S0140-6736(21)01330-1
5. China, WCRCHD. Report on cardiovascular health and diseases in China 2022: an updated summary. Chinese Circul J. (2023) 38:583–612. doi: 10.3969/j.issn.1000-3614.2023.06.001
6. Wang, YJ, Li, ZX, Gu, HQ, Zhai, Y, Zhou, Q, Jiang, Y, et al. China stroke statistics: an update on the 2019 report from the National Center for healthcare quality Management in Neurological Diseases, China National Clinical Research Center for neurological diseases, the Chinese Stroke Association, National Center for chronic and non-communicable disease control and prevention, Chinese Center for Disease Control and Prevention and institute for global neuroscience and stroke collaborations. Stroke Vasc Neurol. (2022) 7:415–50. doi: 10.1136/svn-2021-001374
7. Kayima, J, Wanyenze, RK, Katamba, A, Leontsini, E, and Nuwaha, F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord. (2013) 13:54. doi: 10.1186/1471-2261-13-54
8. Zhang, M, Shi, Y, Zhou, B, Huang, Z, Zhao, Z, Li, C, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ. (2023) 380:e071952. doi: 10.1136/bmj-2022-071952
9. Wilkinson, R, Garden, E, Nanyonga, RC, Squires, A, Nakaggwa, F, Schwartz, JI, et al. Causes of medication non-adherence and the acceptability of support strategies for people with hypertension in Uganda: a qualitative study. Int J Nurs Stud. (2022) 126:104143. doi: 10.1016/j.ijnurstu.2021.104143
10. Huang, J, Ding, S, Xiong, S, and Liu, Z. Medication adherence and associated factors in patients with type 2 diabetes: a structural equation model. Front Public Health. (2021) 9:730845. doi: 10.3389/fpubh.2021.730845
11. Chudiak, A, Jankowska-Polanska, B, and Uchmanowicz, I. Effect of frailty syndrome on treatment compliance in older hypertensive patients. Clin Interv Aging. (2017) 12:805–14. doi: 10.2147/CIA.S126526
12. Vong, SK, Kang, L, and Carter, SR. Consumers' self-reported adherence to directions for non-prescription medicines and the role of risk perception. Res Social Adm Pharm. (2022) 18:3929–38. doi: 10.1016/j.sapharm.2022.06.004
13. Mekonnen, HS, Gebrie, MH, Eyasu, KH, and Gelagay, AA. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacol Toxicol. (2017) 18:27. doi: 10.1186/s40360-017-0134-9
14. Wan, J, Wu, Y, Ma, Y, Tao, X, and Wang, A. Predictors of poor medication adherence of older people with hypertension. Nurs Open. (2022) 9:1370–8. doi: 10.1002/nop2.1183
15. Delavar, F, Pashaeypoor, S, and Negarandeh, R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: a randomized controlled trial. Patient Educ Couns. (2020) 103:336–42. doi: 10.1016/j.pec.2019.08.028
16. Poulter, NR, Borghi, C, Parati, G, Pathak, A, Toli, D, Williams, B, et al. Medication adherence in hypertension. J Hypertens. (2020) 38:579–87. doi: 10.1097/HJH.0000000000002294
17. Bramley, TJ, Gerbino, PP, Nightengale, BS, and Frech-Tamas, F. Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm. (2006) 12:239–45. doi: 10.18553/jmcp.2006.12.3.239
18. Corrao, G, Parodi, A, Nicotra, F, Zambon, A, Merlino, L, Cesana, G, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. (2011) 29:610–8. doi: 10.1097/HJH.0b013e328342ca97
19. Li, Y, Yang, L, Wang, L, Zhang, M, Huang, Z, Deng, Q, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. (2017) 227:516–23. doi: 10.1016/j.ijcard.2016.10.110
20. Jia, Q, Wang, H, Wang, L, and Wang, Y. Association of Health Literacy with Medication Adherence Mediated by cognitive function among the community-based elders with chronic disease in Beijing of China. Front Public Health. (2022) 10:824778. doi: 10.3389/fpubh.2022.824778
21. Kohlman-Trigoboff, D. Hypertension management in patients with vascular disease: an update. J Vasc Nurs. (2016) 34:87–92. doi: 10.1016/j.jvn.2016.01.002
22. Whitworth, JA, World Health Organization ISoHWG. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. (2003) 21:1983–92. doi: 10.1097/00004872-200311000-00002
23. Dent, E, Martin, FC, Bergman, H, Woo, J, Romero-Ortuno, R, and Walston, JD. Management of frailty: opportunities, challenges, and future directions. Lancet. (2019) 394:1376–86. doi: 10.1016/S0140-6736(19)31785-4
24. Jankowska-Polanska, B, Dudek, K, Szymanska-Chabowska, A, and Uchmanowicz, I. The influence of frailty syndrome on medication adherence among elderly patients with hypertension. Clin Interv Aging. (2016) 11:1781–90. doi: 10.2147/CIA.S113994
25. Gill, TM, Gahbauer, EA, Han, L, and Allore, HG. Trajectories of disability in the last year of life. N Engl J Med. (2010) 362:1173–80. doi: 10.1056/NEJMoa0909087
26. Rodriguez-Manas, L, and Fried, LP. Frailty in the clinical scenario. Lancet. (2015) 385:e7–9. doi: 10.1016/S0140-6736(14)61595-6
27. Ma, L, Chhetri, JK, Liu, P, Ji, T, Zhang, L, and Tang, Z. Epidemiological characteristics and related factors of frailty in older Chinese adults with hypertension: a population-based study. J Hypertens. (2020) 38:2192–7. doi: 10.1097/HJH.0000000000002650
28. Kang, MG, Kim, SW, Yoon, SJ, Choi, JY, Kim, KI, and Kim, CH. Association between frailty and hypertension prevalence, treatment, and control in the elderly Korean population. Sci Rep. (2017) 7:7542. doi: 10.1038/s41598-017-07449-5
29. Zeng, XZ, Jia, N, Meng, LB, Shi, J, Li, YY, Hu, JB, et al. A study on the prevalence and related factors of frailty and pre-frailty in the older population with hypertension in China: a national cross-sectional study. Front Cardiovasc Med. (2022) 9:1057361. doi: 10.3389/fcvm.2022.1057361
30. Hubbard, RE, O'Mahony, MS, and Woodhouse, KW. Medication prescribing in frail older people. Eur J Clin Pharmacol. (2013) 69:319–26. doi: 10.1007/s00228-012-1387-2
31. Sheppard, VB, Faul, LA, Luta, G, Clapp, JD, Yung, RL, Wang, JH, et al. Frailty and adherence to adjuvant hormonal therapy in older women with breast cancer: CALGB protocol 369901. J Clin Oncol. (2014) 32:2318–27. doi: 10.1200/JCO.2013.51.7367
32. Koizumi, Y, Hamazaki, Y, Okuro, M, Iritani, O, Yano, H, Higashikawa, T, et al. Association between hypertension status and the screening test for frailty in elderly community-dwelling Japanese. Hypertens Res. (2013) 36:639–44. doi: 10.1038/hr.2013.7
33. Nutbeam, D. The evolving concept of health literacy. Soc Sci Med. (2008) 67:2072–8. doi: 10.1016/j.socscimed.2008.09.050
34. Guzys, D, Kenny, A, Dickson-Swift, V, and Threlkeld, G. A critical review of population health literacy assessment. BMC Public Health. (2015) 15:215. doi: 10.1186/s12889-015-1551-6
35. Milne, RA, Puts, MT, Papadakos, J, Le, LW, Milne, VC, Hope, AJ, et al. Predictors of high eHealth literacy in primary lung Cancer survivors. J Cancer Educ. (2015) 30:685–92. doi: 10.1007/s13187-014-0744-5
36. Moon, Z, Zuchowski, M, Moss-Morris, R, Hunter, MS, Norton, S, and Hughes, LD. Disparities in access to mobile devices and e-health literacy among breast cancer survivors. Support Care Cancer. (2022) 30:117–26. doi: 10.1007/s00520-021-06407-2
37. Zhou, J, and Wang, C. Improving cancer survivors' e-health literacy via online health communities (OHCs): a social support perspective. J Cancer Surviv. (2020) 14:244–52. doi: 10.1007/s11764-019-00833-2
38. Prince, LY, Mears, SC, Watson, JC, and Hadden, KB. Health literacy evaluation of opioid patient education materials for Orthopaedic surgery. J Surg Orthop Adv. (2019) 28:232–6. doi: 10.3113/JSOA.2019.0232
39. Mosher, HJ, Lund, BC, Kripalani, S, and Kaboli, PJ. Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. J Health Commun. (2012) 17:241–51. doi: 10.1080/10810730.2012.712611
40. Bauer, AM, Schillinger, D, Parker, MM, Katon, W, Adler, N, Adams, AS, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the diabetes study of northern California (DISTANCE). J Gen Intern Med. (2013) 28:1181–7. doi: 10.1007/s11606-013-2402-8
41. O'Conor, R, Wolf, MS, Smith, SG, Martynenko, M, Vicencio, DP, Sano, M, et al. Health literacy, cognitive function, proper use, and adherence to inhaled asthma controller medications among older adults with asthma. Chest. (2015) 147:1307–15. doi: 10.1378/chest.14-0914
42. Merritt, JL. Advances in orthotics for the patient with rheumatoid arthritis. J Rheumatol Suppl. (1987) 14:62–7.
43. Chen, YC, Chang, LC, Liu, CY, Ho, YF, Weng, SC, and Tsai, TI. The roles of social support and health literacy in self-management among patients with chronic kidney disease. J Nurs Scholarsh. (2018) 50:265–75. doi: 10.1111/jnu.12377
44. Muellers, KA, Chen, L, O'Conor, R, Wolf, MS, Federman, AD, and Wisnivesky, JP. Health literacy and medication adherence in COPD patients: when caregiver presence is not sufficient. COPD. (2019) 16:362–7. doi: 10.1080/15412555.2019.1665007
45. Zheng, F, Ding, S, Lai, L, Liu, X, Duan, Y, Shi, S, et al. Relationship between medication literacy and medication adherence in inpatients with coronary heart disease in Changsha, China. Front Pharmacol. (2019) 10:1537. doi: 10.3389/fphar.2019.01537
46. Lor, M, Koleck, TA, Bakken, S, Yoon, S, and Dunn Navarra, AM. Association between health literacy and medication adherence among Hispanics with hypertension. J Racial Ethn Health Disparities. (2019) 6:517–24. doi: 10.1007/s40615-018-00550-z
47. Persell, SD, Karmali, KN, Lee, JY, Lazar, D, Brown, T, Friesema, EM, et al. Associations between health literacy and medication self-management among community health center patients with uncontrolled hypertension. Patient Prefer Adherence. (2020) 14:87–95. doi: 10.2147/PPA.S226619
48. Lu, M, Ma, J, Lin, Y, Zhang, X, Shen, Y, and Xia, H. Relationship between patient's health literacy and adherence to coronary heart disease secondary prevention measures. J Clin Nurs. (2019) 28:2833–43. doi: 10.1111/jocn.14865
49. Huang, YM, Shiyanbola, OO, and Smith, PD. Association of health literacy and medication self-efficacy with medication adherence and diabetes control. Patient Prefer Adherence. (2018) 12:793–802. doi: 10.2147/PPA.S153312
50. Agarwal, P, Lin, J, Muellers, K, O'Conor, R, Wolf, M, Federman, AD, et al. A structural equation model of relationships of health literacy, illness and medication beliefs with medication adherence among patients with chronic obstructive pulmonary disease. Patient Educ Couns. (2021) 104:1445–50. doi: 10.1016/j.pec.2020.11.024
51. Meraz, R, McGee, J, Caldwell, EP, Ke, W, and Osteen, K. The impact of resilience, health literacy, and social support on medication adherence and self-care among adults with heart failure. J Cardiovasc Nurs. (2022) 38:415–24. doi: 10.1097/JCN.0000000000000948
52. Williams, KJ, Housten, AJ, and Coughlin, CC. Health literacy in pediatric dermatology: challenges and opportunities. Curr Opin Pediatr. (2023) 35:445–51. doi: 10.1097/MOP.0000000000001254
53. Matrisch, L, Grasshoff, H, Muller, A, Schinke, S, and Riemekasten, G. Therapy satisfaction and health literacy are key factors to improve medication adherence in systemic sclerosis. Scand J Rheumatol. (2023) 52:395–402. doi: 10.1080/03009742.2022.2111771
54. AbuAlreesh, A, and Alburikan, KA. Health literacy among patients with poor understanding of prescription drug label instructions in Saudi Arabia. Saudi Pharm J. (2019) 27:900–5. doi: 10.1016/j.jsps.2019.06.003
55. Cajita, MI, Cajita, TR, and Han, HR. Health literacy and heart failure: a systematic review. J Cardiovasc Nurs. (2016) 31:121–30. doi: 10.1097/JCN.0000000000000229
56. Shirooka, H, Nishiguchi, S, Fukutani, N, Adachi, D, Tashiro, Y, Hotta, T, et al. Association between comprehensive health literacy and frailty level in community-dwelling older adults: a cross-sectional study in Japan. Geriatr Gerontol Int. (2017) 17:804–9. doi: 10.1111/ggi.12793
57. Huang, CH, Lai, YC, Lee, YC, Teong, XT, Kuzuya, M, and Kuo, KM. Impact of health literacy on frailty among community-dwelling seniors. J Clin Med. (2018) 7:481. doi: 10.3390/jcm7120481
58. Uemura, K, Tsukasa, K, Watanabe, A, Okamoto, H, and Yamada, M. Association between community-level health literacy and frailty in community-dwelling older adults. Aging Clin Exp Res. (2023) 35:1253–61. doi: 10.1007/s40520-023-02405-y
59. Gynnild, MN, Aakeroy, R, Spigset, O, Askim, T, Beyer, MK, Ihle-Hansen, H, et al. Vascular risk factor control and adherence to secondary preventive medication after ischaemic stroke. J Intern Med. (2021) 289:355–68. doi: 10.1111/joim.13161
60. Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.M146
61. Hanlon, P, Faure, I, Corcoran, N, Butterly, E, Lewsey, J, McAllister, D, et al. Frailty measurement, prevalence, incidence, and clinical implications in people with diabetes: a systematic review and study-level meta-analysis. Lancet Healthy Longev. (2020) 1:e106–16. doi: 10.1016/S2666-7568(20)30014-3
62. CMA GMB. Chinese experts consensus on assessment and intervention for elderly patients with frailty. Chinese J Geriatr. (2017) 36:251–6. doi: 10.3760/cma.j.issn.0254-9026.2017.03.007
63. Qu, J, Zhou, T, Xue, M, Sun, H, Shen, Y, Chen, Y, et al. Correlation analysis of hemoglobin-to-red blood cell distribution width ratio and frailty in elderly patients with coronary heart disease. Front Cardiovasc Med. (2021) 8:728800. doi: 10.3389/fcvm.2021.728800
64. Liu, H, Li, D, Zhao, X, Fang, B, Zhang, Q, and Li, T. Longitudinal impact of frailty states and sleep duration on subsequent depressive symptoms of older adults. J Am Geriatr Soc. (2021) 69:1003–11. doi: 10.1111/jgs.16999
65. Cao, L, Zhou, Y, Liu, H, Shi, M, Wei, Y, and Xia, Y. Bidirectional longitudinal study of frailty and depressive symptoms among older Chinese adults. Front Aging Neurosci. (2022) 14:791971. doi: 10.3389/fnagi.2022.791971
66. Tarazona-Santabalbina, FJ, Gomez-Cabrera, MC, Perez-Ros, P, Martinez-Arnau, FM, Cabo, H, Tsaparas, K, et al. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: a randomized clinical trial. J Am Med Dir Assoc. (2016) 17:426–33. doi: 10.1016/j.jamda.2016.01.019
67. Jordan, JE, Buchbinder, R, Briggs, AM, Elsworth, GR, Busija, L, Batterham, R, et al. The health literacy management scale (HeLMS): a measure of an individual's capacity to seek, understand and use health information within the healthcare setting. Patient Educ Couns. (2013) 91:228–35. doi: 10.1016/j.pec.2013.01.013
68. Sun, HL. Development and preliminary application of scale on health literacy for patients with chronic Diease [D]. Shang Hai: Fudan University (2012).
69. Shi, S, Shen, Z, Duan, Y, Ding, S, and Zhong, Z. Association between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. (2019) 10:822. doi: 10.3389/fphar.2019.00822
70. Jankowska-Polanska, B, Chudiak, A, Uchmanowicz, I, Dudek, K, and Mazur, G. Selected factors affecting adherence in the pharmacological treatment of arterial hypertension. Patient Prefer Adherence. (2017) 11:363–71. doi: 10.2147/PPA.S127407
71. Uchmanowicz, B, Jankowska, EA, Uchmanowicz, I, and Morisky, DE. Self-reported medication adherence measured with Morisky medication adherence scales and its determinants in hypertensive patients aged >/=60 years: a systematic review and Meta-analysis. Front Pharmacol. (2019) 10:168. doi: 10.3389/fphar.2019.00168
72. Bautista, LE, Vera-Cala, LM, Colombo, C, and Smith, P. Symptoms of depression and anxiety and adherence to antihypertensive medication. Am J Hypertens. (2012) 25:505–11. doi: 10.1038/ajh.2011.256
73. Guo, A, Jin, H, Mao, J, Zhu, W, Zhou, Y, Ge, X, et al. Impact of health literacy and social support on medication adherence in patients with hypertension: a cross-sectional community-based study. BMC Cardiovasc Disord. (2023) 23:93. doi: 10.1186/s12872-023-03117-x
74. Martin, LR, Williams, SL, Haskard, KB, and Dimatteo, MR. The challenge of patient adherence. Ther Clin Risk Manag. (2005) 1:189–99. doi: 10.2147/tcrm.s12160382
75. Roebuck, MC, Liberman, JN, Gemmill-Toyama, M, and Brennan, TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood). (2011) 30:91–9. doi: 10.1377/hlthaff.2009.1087
76. Zhang, NJ, Terry, A, and McHorney, CA. Impact of health literacy on medication adherence: a systematic review and meta-analysis. Ann Pharmacother. (2014) 48:741–51. doi: 10.1177/1060028014526562
77. Caballero, J, Jacobs, RJ, and Ownby, RL. Development of a computerized intervention to improve health literacy in older Hispanics with type 2 diabetes using a pharmacist supervised comprehensive medication management. PLoS One. (2022) 17:e0263264. doi: 10.1371/journal.pone.0263264
78. Estrela, M, Semedo, G, Roque, F, Ferreira, PL, and Herdeiro, MT. Sociodemographic determinants of digital health literacy: a systematic review and meta-analysis. Int J Med Inform. (2023) 177:105124. doi: 10.1016/j.ijmedinf.2023.105124
79. Jansen, T, Rademakers, J, Waverijn, G, Verheij, R, Osborne, R, and Heijmans, M. The role of health literacy in explaining the association between educational attainment and the use of out-of-hours primary care services in chronically ill people: a survey study. BMC Health Serv Res. (2018) 18:394. doi: 10.1186/s12913-018-3197-4
80. Holt, KA, Overgaard, D, Engel, LV, and Kayser, L. Health literacy, digital literacy and eHealth literacy in Danish nursing students at entry and graduate level: a cross sectional study. BMC Nurs. (2020) 19:22. doi: 10.1186/s12912-020-00418-w
81. Almoajel, A, Alshamrani, S, and Alyabsi, M. The relationship between e-health literacy and breast Cancer literacy among Saudi women. Front Public Health. (2022) 10:841102. doi: 10.3389/fpubh.2022.841102
82. Ozen, N, Cinar, FI, Askin, D, Mut, D, and Turker, T. Nonadherence in hemodialysis patients and related factors: a multicenter study. J Nurs Res. (2019) 27:e36. doi: 10.1097/jnr.0000000000000309
83. Singh, R, Kumari, P, Prashar, A, Sardana, O, and Singh, V. Assessment of medication adherence among type-2 diabetes mellitus in a tertiary care hospital of North India. Environ Sci Pollut Res Int. (2022) 29:24951–5. doi: 10.1007/s11356-021-17434-1
84. Napolitano, F, Napolitano, P, Angelillo, IF, and Collaborative, WG. Medication adherence among patients with chronic conditions in Italy. Eur J Pub Health. (2016) 26:48–52. doi: 10.1093/eurpub/ckv147
85. Al-Tarawneh, F, Ali, T, Al-Tarawneh, A, Altwalbeh, D, Gogazeh, E, Bdair, O, et al. Study of adherence level and the relationship between treatment adherence, and superstitious thinking related to health issues among chronic disease patients in southern Jordan: cross-sectional study. Patient Prefer Adherence. (2023) 17:605–14. doi: 10.2147/PPA.S390997
86. Li, RB. Analysis of the influence mechanism of health literacy on Residents' health level. Beijing: Central University of Finance and Economics (2022).
Keywords: older adult patients, hypertension, frailty, health literacy, medication adherence, educational level
Citation: Wang A, Wan J, Zhu L, Chang W, Wen L, Tao X and Jin Y (2023) Frailty and medication adherence among older adult patients with hypertension: a moderated mediation model. Front. Public Health. 11:1283416. doi: 10.3389/fpubh.2023.1283416
Edited by:
Mojtaba Vaismoradi, Nord University, NorwayReviewed by:
Juan Du, Capital Medical University, ChinaAbbas Mardani, Iran University of Medical Sciences, Iran
Copyright © 2023 Wang, Wan, Zhu, Chang, Wen, Tao and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiubin Tao, NDQyMDk2NTU2QHFxLmNvbQ==; Yuelong Jin, amlueWwwODAzQHdubWMuZWR1LmNu
†These authors have contributed equally to this work
 Anshi Wang
Anshi Wang Jingjing Wan3†
Jingjing Wan3† Yuelong Jin
Yuelong Jin