- 1Department of Ophthalmology, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, China
- 2Chinese Academy of Sciences Sichuan Translational Medicine Research Hospital, Chengdu, China
- 3Centre for Public Health, Queen’s University Belfast, Belfast, United Kingdom
- 4Stanford Centre on China’s Economy and Institutions, Stanford University, Stanford, CA, United States
- 5School of Financial and Management, Ningxia University, Yinchuan, China
- 6Department NEUROFARBA, University of Florence, Florence, Italy
- 7Orbis International, New York, NY, United States
- 8Affiliated Eye Hospital of Nanchang University, Nanchang, China
- 9Stanford University School of Medicine, Stanford University, Stanford, CA, United States
- 10Clearly Initiatives, London, United Kingdom
- 11Zhongshan Ophthalmic Centre, Sun Yat-sen University, Guangzhou, China
Objective: The measures implemented to control the spread of Coronavirus disease 2019 (COVID-19) could affect children’s mental and vision health. Youth particularly from minority and socioeconomically disadvantaged backgrounds were more likely to be impacted by these measures. This study aimed to examine the mental health of children with vision impairment and associated factors in North-western China during the COVID-19 pandemic.
Methods: A cross-sectional study was conducted among 2,036 secondary school children living in Ningxia Hui Autonomous Region. Participants completed a survey on sociodemographic and lifestyle information and answered the Chinese version of the 21-item Depression Anxiety Stress Scales (DASS-21) questionnaire. Presenting visual acuity was measured by a trained enumerator. Multivariate logistic regression analysis was used to identify potential risk factors for mental health problems.
Results: Responses from 1,992 (97.8%) children were included in the analysis after excluding those with incomplete mental health outcome data. The prevalence of depression, anxiety and stress symptoms within the dataset were 28.9, 46.4, and 22.3%, respectively. The distribution of children with different stress levels differed significantly between those with and without vision impairment (p = 0.03). Multivariable logistic regression analyses revealed that depression symptoms decreased with higher parental education (OR, 0.76, 95% confidence intervals (CI):0.63–0.96), longer sleep duration (OR, 0.90, 95% CI: 0.81–0.97) and longer study time (OR, 0.82, 95% CI: 0.74–0.91), whereas they increased with higher recreational screen time (OR, 1.19, 95% CI: 1.08–1.32). Anxiety symptoms decreased with higher parental education (OR, 0.80, 95% CI: 0.66–0.96) and increased with higher recreational screen time (OR, 1.15, 95% CI: 1.04–1.27) and being a left-behind child (OR, 1.26, 95% CI: 1.04–1.54). In addition, stress symptoms decreased with longer sleep duration (OR, 0.92, 95%CI: 0.85–0.99) and increased with higher number of siblings (OR, 1.10, 95% CI: 1.01–1.19), higher recreational screen time (OR, 1.15, 95% CI: 1.04–1.28) and older age (OR,1.12, 95% CI: 1.004–1.24).
Conclusion: A considerable proportion of our sample experienced mental health problems during the pandemic. Healthcare planners in China should consider interventions such as reducing recreational screen time, ensuring sufficient sleep, and timely detection of mental health symptoms among socioeconomically disadvantaged groups.
Introduction
In December 2019, a novel Coronavirus pandemic rapidly spread worldwide. Governments implemented various measures to control the pandemic on an international scale, such as restrictions on public activities, home quarantine, physical distancing, and school closures. Strict pandemic prevention measures led to a decrease in time spent outdoors and an increase in screen time (1, 2), which may have detrimentally impacted individuals’ vision and mental health during the COVID-19 pandemic (3–6).
Globally, one in seven 10 to 19-year-old children and young adults experience a mental disorder, and depression and anxiety disorders are among the leading causes of illness and disability among adolescents (7). When COVID-19 was declared an international public health emergency, children worldwide experienced dramatic disruptions to their daily lives, and the prevalence of depression and anxiety increased correspondingly. A systematic review of the global literature comprising 29 articles found that the prevalence of clinically-elevated depression and anxiety in children doubled compared with the pre-pandemic period, reaching 25.2 and 20.5%, respectively (8).
Ningxia is an autonomous region located in Northwest China with a population of 6.62 million, of which 38% are Hui ethnicity (9). Ningxia is a relatively undeveloped area, its disposable income per capita in 2020 was approximately RMB 27904 (US$3986), ranking 20th among 32 administrative regions in China (10). Ningxia reported the first COVID-19 cases in Jan 2020 (11), and all primary and secondary students in Ningxia were confined at home for almost 4 months with online school lessons (12). This led to increased screen time and reduced outdoor time, both of which have been shown to have a detrimental effect on children’s mental health (13, 14). Home confinement during the COVID-19 pandemic also increased the incidence and progression of myopia (5), which is the leading cause of children’s vision impairment and has also been shown to impact children’s mental health negatively (15).
These studies have significant implications for China as (i) vision impairment and myopia are among the most common health problems in Chinese students (16, 17); (ii) preliminary evidence also suggests an increased incidence and progression of myopia among children during the COVID-19 outbreak in China (1, 5); and (iii) the combination of the lockdown during the COVID-19 pandemic, uncorrected myopia, and subsequent unemployment and income reduction (18) may disproportionately affect the mental health of children from low socioeconomic status families (19). However, it is unclear how children’s mental health in rural China, especially rural minority populations, was affected by quarantine measures during COVID-19 and its association with the aforementioned factors. The Hui community, predominantly adherents of the Muslim faith, possesses a distinctive culture. They adhere to Islamic dietary laws and actively participate in various religious activities (20). In the rural part of Ningxia the Hui community is less educated and has a lower household per capita wealth compared to the Han community in the same region (21). Furthermore, given China’s relatively permissive birth-control policy for ethnic minorities, Hui households tend to have a higher number of dependent children compared to their Han counterparts (22). All these factors may contribute to the poor mental health of Hui people. Studies from Ningxia found that high religiosity was associated positively with mental disorders in older Hui people (23). Studies before COVID-19 indicated that adults women of Hui ethnicity in rural Ningxia experience more severe mental health symptoms including depression and anxiety than their Han counterparts (24). Children of Hui ethnicity from the Ningxia region are particularly vulnerable to behavioral and emotional problems (25, 26). Few studies have focused on investigating the mental health of children from the Hui ethnicity and other minority groups during the COVID-19 pandemic. Further, it is unclear how Hui children were affected psychologically during the pandemic.
Thus, this study aimed to assess the mental health of Hui and Han children in rural Northwestern China using the Depression Anxiety Stress Scales (DASS-21) and to explore associations among mental health, vision impairment, and socioeconomic and lifestyle factors.
Methods
The protocol for this study was approved by the Institutional Review Boards at Stanford University (Protocol ID 52514) and Queen’s University Belfast (PFREC 19.25). Written informed consent was obtained from the parents of the students before data collection began. The study adhered to the tenets of the Declaration of Helsinki.
Study design and participants
This cross-sectional study was conducted in October 2021. The study was part of the See Well to stay In ScHool (SWISH) trial, designed to assess whether glasses distribution to myopic students in secondary school can increase academic high school attendance rates and improve mental health status in rural areas (27). As per the SWISH protocol, we aimed to screen 20,000 students of grade 7 and 8 from 120 secondary schools in Ningxia autonomous region. However, due to the outbreak of COVID-19 in Ningxia in October 2021, the included schools were temporarily closed. Fieldwork was suspended after 2,036 children from 13 schools in three counties were screened. After excluding participants with incomplete mental health data (n = 44), 1,992 participants (97.8%) were included in the analysis.
Measures
Field teams of 10 trained enumerators recruited from a local university administered a questionnaire to the children to collect data on sociodemographic status. Information was sought on age, gender, parental marital status, and whether or not they were a “left-behind child” [defined as children who live in their rural communities while one or both of their parents have migrated into cities for work over 6 months (28)], parental education level, and family wealth. In addition, questions were asked regarding lifestyle habits, including self-reported sleep time, study time, recreational screen time, and time spent on outdoor activities. Family wealth was measured by a pre-defined list of assets, including ownership of a private car, an apartment in the county, a refrigerator at home etc. We constructed a family wealth index by combining the self-reported assets using Principal Component Analysis (PCA) (29). The wealth index value was categorized in terciles and, used in the regression analysis. The lowest tercile was classified as poor, the highest was rich, and the rest were of average economic status.
Students were administered the Depression Anxiety Stress Scale (DASS-21) to determine their mental health (30). The DASS-21 is a self-reported measure of negative effects with three 7-item subscales (depression, anxiety, and stress). The responses were indicated using a 4-point Likert scale ranging from 0 (“does not apply to me at all”) to 3 (“applies to me very much or most of the time”), with higher scores indicating more negative experiences in the past week. Scores for each subscale were obtained by totaling the responses to the component items. DASS-21 has been previously used to assess mental health in Chinese populations (31).
After completing the questionnaires, the student’s visual acuity was assessed. The process has been described in detail by Wang et al. (32), and briefly included testing presenting visual acuity one eye at a time at a distance of 4 meters using the Early Treatment Diabetic Retinopathy tumbling E study chart (Precision Vision, La Salle, IL) in a well-lit, indoor area. Children with glasses were asked to wear them during the assessment. Visual acuity was recorded using logMAR (log of the Minimum Angle of Resolution) values. Presenting vision impairment was defined as better-eye presenting vision >0.3 logMAR.
Statistical analysis
All statistical analyses were performed using Stata 17.0 (Stata Corp., College Station, TX). Descriptive statistics were reported for the demographic data and prevalence of depression, anxiety, and stress symptoms among the participants. Associations between potential determinants and the symptoms of depression, anxiety and stress were investigated using univariable and multivariable logistic regression models. Odds ratios and 95% confidence intervals (CI) were also calculated. All variables with a p < 0.2 in the univariable logistic regression were included in the multivariable model. A two-tailed p < 0.05 was considered statistically significant.
Results
The study included 1,992 children (49.3% boys, with a mean age of 13.5 ± 0.88 years). Children from the Hui ethnic group formed 77.5% of the sample (n = 1,541), while the rest were from the majority Han group. About a third of the sample (n = 608, 30.5%) were left-behind children. Most children (n = 1,044, 52.4%) had at least one parent with 9 years or more education, and 1,002 (50.3%) were boarding at school.
Children spent an average of 0.88 ± 0.96 h per day on recreational screen time (including television, smartphones, laptops, and tablets). The average outdoor activities time, sleep time and study time after school were 0.91 ± 0.69 h, 9.65 ± 1.19 h and 1.15 ± 1.09 h per day, respectively. About a fifth of participants (20.3, 95%CI, 18.6–22.1%) had vision impairment (Table 1).
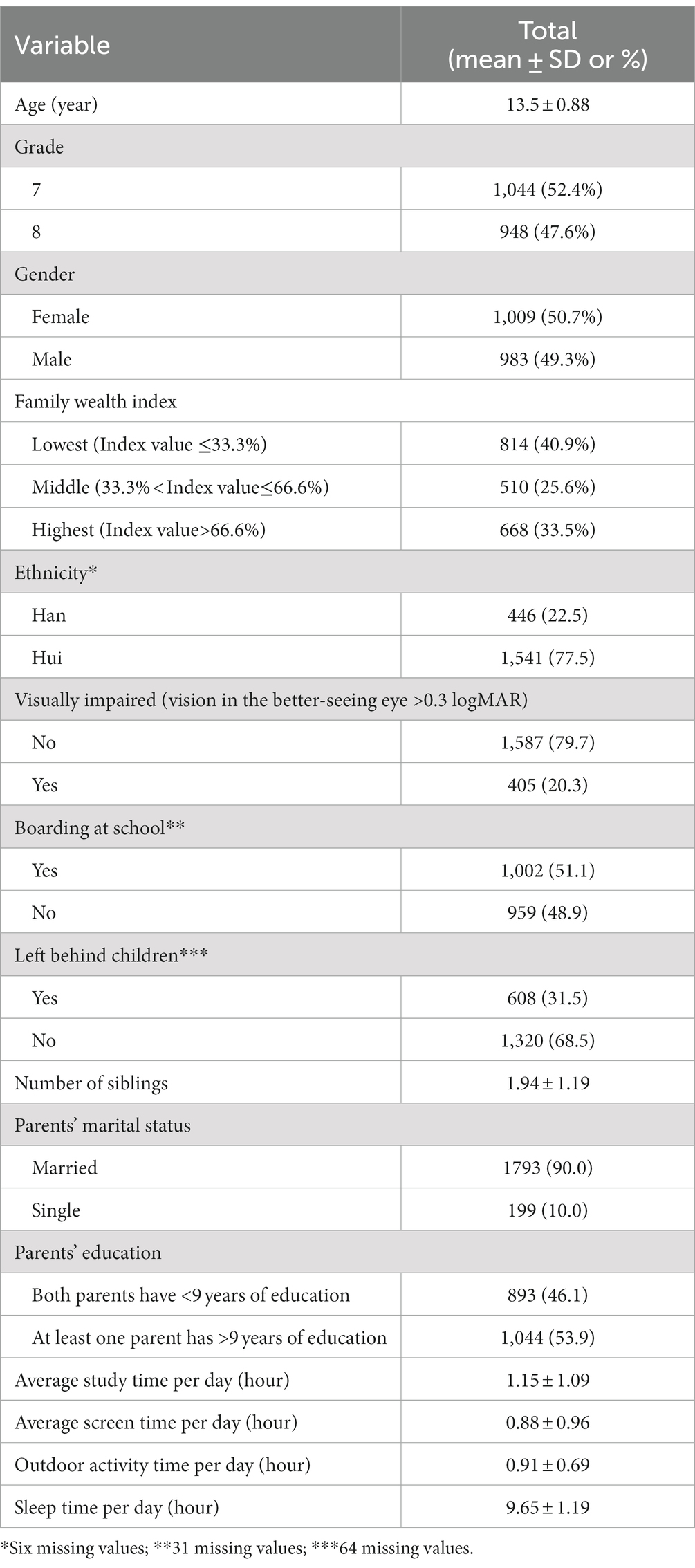
Table 1. Demographic and lifestyle characteristics of participants (N = 1,992) in a study of mental health in rural Chinese school-children.
The prevalence of symptoms of depression was 28.9% (95% CI, 26.3–30.2%), while the figures for anxiety and stress symptoms were 46.4% (95% CI, 44.2–48.6%) and 22.3% (95%CI, 20.5–24.2%) respectively. The prevalence of extremely severe stress symptoms was significantly higher in children with vision impairment than those with normal vision. However, no significant differences were observed in the level of depression and anxiety symptoms among children with or without vision impairment. Ethnicity was not associated with the prevalence of depression, anxiety, and stress symptoms (Table 2).
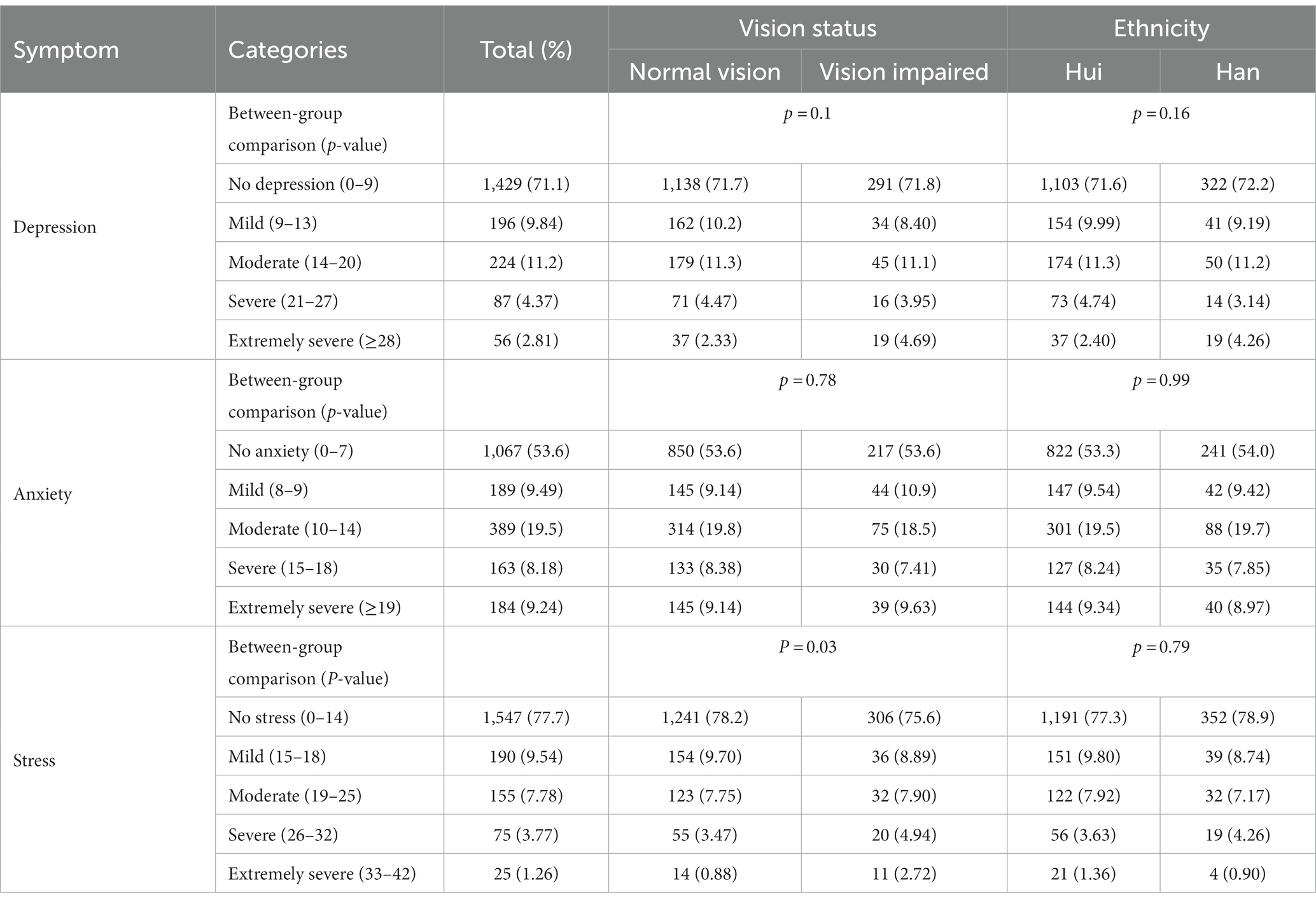
Table 2. Prevalence of depression, anxiety and stress symptoms among rural students in China on the DASS-21, stratified by vision impairment and ethnicity.
Multivariate logistic regression analysis revealed that children with the following characteristics were less likely to have symptoms of depression: one or both parents having >9 years of education (OR, 0.78, 95% CI: 0.63–0.96, p = 0.02), those with longer sleep duration (OR, 0.90 95% CI: 0.81–0.97, p = 0.03) and study time (OR, per hour 0.82, 95% CI: 0.74–0.91, p = 0.03). Children with higher recreational screen time were significantly more likely (OR per additional hour 1.19, 95% CI: 1.08–1.32, p = 0.001) to have depression symptoms. Being a left-behind child also marginally increased the risk of depression (OR,1.26, 95% CI: 0.99–1.59, p = 0.057) (Table 3).
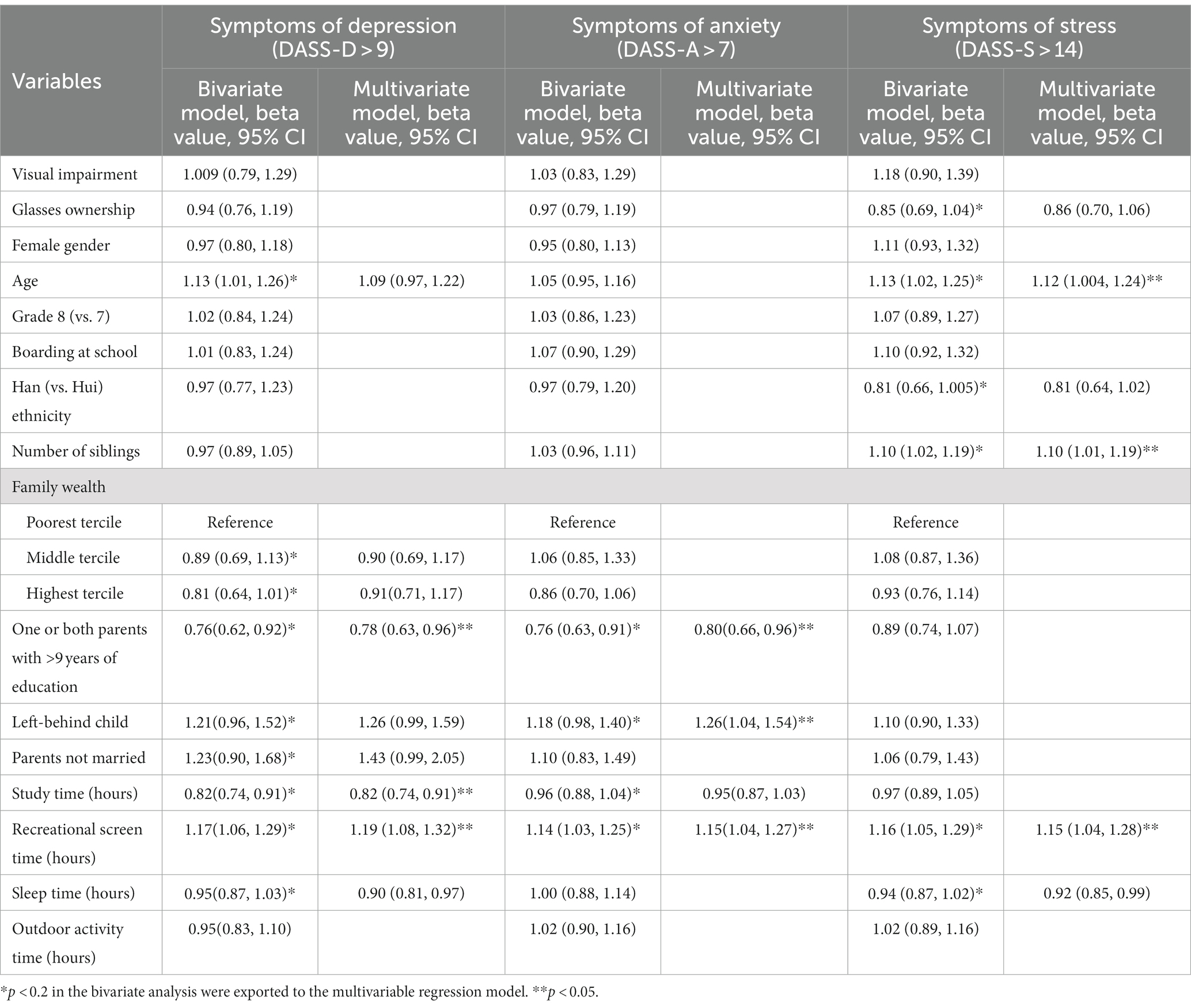
Table 3. Factors associated with symptoms of depression, anxiety, and stress among rural students in China.
Children with one or both parents having >9 years of education were significantly less likely (OR, 0.80, 95% CI: 0.66–0.96, p = 0.02) to have anxiety symptoms. Children with higher recreational screen time (OR per additional hour 1.15, 95% CI: 1.04–1.27, p = 0.004) and left-behind children were significantly more likely (OR, 1.26, 95% CI: 1.04–1.54, p = 0.016) to suffer from anxiety symptoms (Table 3).
Children with more siblings (OR per additional sibling 1.10, 95% CI: 1.01–1.19, p = 0.002), who engaged in higher recreational screen time (OR per hour, 1.15, 95% CI: 1.04–1.28, p = 0.009), and who were older (OR per year, 1.12, 95% CI: 1.004–1.24, p = 0.04) were significantly more likely to experience symptoms of stress. Children with longer sleep duration per day were significantly less likely (OR, 0.92, 95% CI: 0.85–0.99, p = 0.002) to have symptoms of stress. Ethnicity was not associated with any of the three mental health outcomes in regression models (Table 3).
Discussion
The current study provides insight into the mental health problems of secondary school children living in Northwestern rural China during COVID-19. Approximately a quarter of children experienced symptoms of depression and stress, and close to half of the sample experienced symptoms of anxiety. Modifiable factors, such as longer recreational screen time and shorter sleeping time, and sociodemographic factors, such as having parents with fewer years of education, being left-behind children, being older and having more siblings, were associated with poorer mental health.
Studies in Chile (33), Bangladesh (34), and Palestine (35) using the same mental health questionnaire as our study found a much higher prevalence of symptoms of depression, anxiety, and stress. However, all these studies collected data through online questionnaires, which will make the study participants non-representative. The prevalence of depression and anxiety in the current study was higher than reported in a systematic review, which found that the pooled prevalence of depression and anxiety symptoms among Chinese children during COVID-19 were 22 and 25%, respectively (36). Even though Ningxia was one of the less severely impacted areas of China (37), our study suggests that children may still have been affected by negative experiences related to fear of infection, lack of personal contact with friends, increased screen time and reduced outdoor time during the pandemic, and thus, experienced more depression and anxiety symptoms.
Measures such as school closures and the transition to online studies contributed to the increased use of screen-based media for education and recreation (38–40). Screen-based sedentary behaviors have been recognized as a significant contributor to adverse outcomes such as mental health problems (41), obesity (42), and myopia (43). The average recreational screen time reported in the current study was less than an hour per day, much less than previous studies conducted in other parts of China, and yet had a significant association with increased mental health symptoms (44). According to guidelines issued by the Health Department of China during the COVID-19 pandemic, secondary school children should be exposed to no more than 4 h of online study and 1 h of recreational screen time per day (45). Our findings may help inform stakeholders considering interventions such as developing a family media plan (46) to mitigate the potential risks to children’s mental health of screen use.
We identified shorter study time and sleep duration as two potentially modifiable risk factors associated with poorer mental health. Given that many intermediate school children in rural China aspire to continue to academic high schools, which requires a high entrance examination score, spending less time studying might have caused anxiety over educational prospects. Many Chinese adolescents were already not meeting the recommended sleep time of 8–10 h per night before the pandemic (47). Children with excessive screen time leading to shorter sleep duration (48), going to bed late and taking a long time to fall asleep during the pandemic are all associated with adverse physical and mental health outcomes (49, 50). Hence, public health messages regarding the importance of healthy sleep schedules should be disseminated to children and parents.
Previous reviews, including studies of Christian populations, have indicated that religious involvement is correlated with better mental health (51). With its Islamic practices, the Hui ethnicity might be hypothesized to protect against mental health problems. However, economic development and education in recent years in China have led to reduced emphasis on religious practices among some Hui (52). This trend of cultural integration may have contributed to the lack of significant differences in the prevalence of the three mental health symptoms between Hui and Han children.
Our findings suggest that vision impairment was not associated with symptoms of depression and anxiety, which is inconsistent with a recent systematic review (15). The daily outdoor time of the children included in this study was far below the 2 h per day suggested by the National Health Commission of the People’s Republic of China (45). Furthermore, despite studies showing that outdoor activities can relieve anxiety and stress (53, 54), we did not find the same associations. Hence, we hypothesize that the disruption in lifestyle habits during the pandemic had greater detrimental effects on mental health than vision impairment. During the COVID-19 pandemic, learning activities in secondary schools alternated from face-to-face to online if there were new COVID cases. In the face-to-face context, children with vision impairment might have experienced stress due to difficulty in seeing the material on a blackboard, and the ensuing academic pressures. In addition, during COVID-19, the transition of traditional class to online one was a challenge to students due to technology-related issues (55), and lack of interaction with teachers and fellow students (56).
Children from socioeconomically disadvantaged families and those left behind at home were more likely to experience mental health symptoms than their peers without these issues (57, 58). Left-behind children are usually cared for by their grandparents, and inadequate parental care may impact children’s physical and mental health (58). Additionally, left-behind children’s families may have suffered reductions in income due to the pandemic. Amidst the lockdown in 2020, around 25 million rural migrants in China found themselves either unemployed or in a state of anticipation, awaiting the opportunity to return to work (59). Many migrant parents fail to maintain a strong and healthy parent–child relationship (60). While the lockdown created an opportunity for parents and left-behind children to spend more time together, repeating separations and reunions with caregivers is stressful. This may have disrupted left-behind children’s attachment behaviors during the pandemic (61).
Interestingly, children with more siblings were more likely to report stress on the DASS-21 than those with fewer siblings or no siblings. This is consistent with a previous study that found that children with siblings were more likely to develop symptoms of anxiety and depression compared to only-children during COVID-19 (62). Studies before COVID-19 found better mental health status in children with siblings compared to children without siblings (63, 64). In addition to effecting health, COVID-19 severely decreased employment and income (59, 65). Underprivileged students may not have access to resources such as the internet, which are essential for their learning (66). We hypothesize that, families with fewer children may have had fewer economic burdens and could provide more attention and support to children, but these attitudes and beliefs could also be contextualized in decades-long single-child family restrictions.
Strengths of the current study include the focus on China’s relatively less-studied rural west, particularly the Hui ethnic group, about whose mental health epidemiology relatively little is known. A large sample of children was recruited, with high rates of participation, reducing risk of bias, and a well-recognized tool, validated in China, was used to assess mental health symptoms.
Several limitations of this study should also be noted. Firstly, the sample was taken from 3 counties only and might not represent children throughout Ningxia Hui Autonomous Region. Secondly, recall and reporting bias might have occurred, with variables such as sleep time and recreational screen time being self-reported. In addition, the individual history and family history of psychiatric disorders were not collected, which might confound the association between mental health symptoms and risk factors. Finally, as this study was cross-sectional, we could not establish a causal relationship between mental health and risk factors. Despite the limitations, this is the first study investigating the mental health of Hui children and identified several modifiable risk factors of potential interest to policymakers.
Conclusion
Our results showed that a considerable proportion of these children in Northwestern China experienced depression, anxiety, and stress symptoms during the COVID-19 pandemic. Healthcare planners in China should consider interventions such as reducing recreational screen time, ensuring sufficient sleep, and timely detection of mental health symptoms among socioeconomically disadvantaged groups.
Data availability statement
The dataset of this article will be uploaded to Queen’s University Belfast Research Portal and further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Stanford University and Queen’s University Belfast. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
DL: Conceptualization, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. VC: Conceptualization, Formal analysis, Methodology, Writing – review & editing, Supervision. HW: Conceptualization, Methodology, Writing – review & editing, Project administration, Validation. HZ: Methodology, Project administration, Writing – review & editing. GV: Methodology, Writing – review & editing, Formal analysis. NW: Writing – review & editing, Conceptualization. BX: Writing – review & editing, Project administration. MS: Writing – review & editing, Conceptualization, Methodology. XS: Conceptualization, Methodology, Writing – review & editing. GM: Conceptualization, Writing – review & editing, Funding acquisition, Resources. MB: Conceptualization, Funding acquisition, Writing – review & editing. SM: Writing – review & editing, Methodology. SR: Methodology, Writing – review & editing, Conceptualization, Funding acquisition. NC: Conceptualization, Funding acquisition, Writing – review & editing, Project administration, Resources, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Medical Research Council (No. R1087CPH) and Clearly Initiatives (No. R2657CPH).
Conflict of interest
MS has received research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, National Institute of Mental Health, National Institute of Aging, Patient Centered Outcomes Research Institute, Johnson and Johnson, and the Brain and Behavior Research Foundation. She was on the advisory board for Sunovion and Skyland Trail, was a consultant for Johnson and Johnson, Alkermes, Neumora, AbbVie, Karuna Therapeutics, Inc., and Boehringer-Ingelheim. She received honoraria from the American Academy of Child and Adolescent Psychiatry, and royalties from American Psychiatric Association Publishing and Thrive Global. GM is the research director of Clearly Initiatives and contributed to the design of this study. BX received a Ph.D. scholarship from Clearly Initiatives.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhang, X, Cheung, SS, Chan, H-N, Zhang, Y, Wang, YM, Yip, BH, et al. Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: a population-based prospective study. Br J Ophthalmol. (2021) 106:1772–8. doi: 10.1136/bjophthalmol-2021-319307
2. Silva, DR, Werneck, AO, Malta, DC, Souza-Júnior, PRB, Azevedo, LO, Barros, MBA, et al. Incidence of physical inactivity and excessive screen time during the first wave of the COVID-19 pandemic in Brazil: what are the most affected population groups? Ann Epidemiol. (2021) 62:30–5. doi: 10.1016/j.annepidem.2021.05.001
3. Gerdes, ME, Aistis, LA, Sachs, NA, Williams, M, Roberts, JD, and Rosenberg Goldstein, RE. Reducing anxiety with nature and gardening (RANG): evaluating the impacts of gardening and outdoor activities on anxiety among US adults during the COVID-19 pandemic. Int J Environ Health Res. (2022) 19:5121. doi: 10.3390/ijerph19095121
4. Haider, S, Smith, L, Markovic, L, Schuch, FB, Sadarangani, KP, Lopez Sanchez, GF, et al. Associations between physical activity, sitting time, and time spent outdoors with mental health during the first COVID-19 lock down in Austria. Int J Environ Res Public Health. (2021) 18:9168. doi: 10.3390/ijerph18179168
5. Wang, J, Li, Y, Musch, DC, Wei, N, Qi, X, Ding, G, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. (2021) 139:293–300. doi: 10.1001/jamaophthalmol.2020.6239
6. Martínez-Líbano, J, Yeomans, MM, González Campusano, N, and Campos, FE. Emotional exhaustion and mental health in a sample of Chilean social science students during the COVID-19 pandemic. Psocial. (2021) 7:69–81.
7. World Health Organization. Adolescent mental health. (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed October 18, 2022).
8. Racine, N, McArthur, BA, Cooke, JE, Eirich, R, Zhu, J, and Madigan, S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. (2021) 175:1142–50. doi: 10.1001/jamapediatrics.2021.2482
9. National Bureau of Statistics. China statistical yearbook. (2021). Available at: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.htm.
10. Ministry of Education of the People's Republic of China. National statistical bulletin on the development of education. (2020). Available at: http://www.moe.gov.cn/jyb_sjzl/sjzl_fztjgb/202108/t20210827_555004.html (Accessed September 24, 2022).
11. Health Commission of Ningxia Hui Autonomous Region. The treatment of the first pneumonia patient infected with the novel coronavirus in Ningxia. (2020). Available at: http://wsjkw.nx.gov.cn/sy_279/jknx/xwbd/202001/t20200123_2821729.html (Accessed June 28, 2022).
12. Education Department of Ningxia Hui Autonomous Region. School reopening dates of Ningxia Hui autonomous region. (2020). Available at: http://jyt.nx.gov.cn/xwdt/gzdt/202104/t20210407_2701759.html (Accessed June 28, 2022).
13. Yue, J, Zang, X, Le, Y, and An, Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr Psychol. (2020) 41:5723–30. doi: 10.1007/s12144-020-01191-4
14. Li, W, Zhang, Y, Wang, J, Ozaki, A, Wang, Q, Chen, Y, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. (2021) 175:313–6. doi: 10.1001/jamapediatrics.2020.5499
15. Li, D, Chan, VF, Virgili, G, Piyasena, P, Negash, H, Whitestone, N, et al. Impact of vision impairment and ocular morbidity and their treatment on depression and anxiety in children: a systematic review. Ophthalmology. (2022) 129:1152–70. doi: 10.1016/j.ophtha.2022.05.020
16. Sun, H-P, Li, A, Xu, Y, and Pan, C-W. Secular trends of reduced visual acuity from 1985 to 2010 and disease burden projection for 2020 and 2030 among primary and secondary school students in China. JAMA Ophthalmol. (2015) 133:262–8. doi: 10.1001/jamaophthalmol.2014.4899
17. The State Council of The People's Republic of China. Majority of students are nearsighted. (2019). Available at: http://english.www.gov.cn/state_council/ministries/2019/04/30/content_281476636681446.htm (Accessed January 18, 2022).
18. Che, L, Du, H, and Chan, KW. Unequal pain: a sketch of the impact of the Covid-19 pandemic on migrants’ employment in China. Eurasian Geogr Econ. (2020) 61:448–63. doi: 10.1080/15387216.2020.1791726
19. Li, W, Wang, Z, Wang, G, Ip, P, Sun, X, Jiang, Y, et al. Socioeconomic inequality in child mental health during the COVID-19 pandemic: first evidence from China. J Affect Disord. (2021) 287:8–14. doi: 10.1016/j.jad.2021.03.009
20. Dodge, CH. The everything understanding Islam book: a complete and easy to read guide to Muslim beliefs, practices, traditions, and culture Simon & Schuster (2003).
21. Gustafsson, B, and Sai, D. Why is there no income gap between the hui Muslim minority and the Han majority in rural Ningxia, China? China Q. (2014) 220:968–87. doi: 10.1017/S0305741014001131
22. Jin, Y, Hu, W, and Wang, D. Fertility transition of Han and ethnic minorities in China: a tale of convergence and variation. Chin J Sociol. (2023) 9:522–52. doi: 10.1177/2057150X231207916
23. Wang, Z, Koenig, HG, Zhang, Y, Ma, W, and Huang, Y. Religious involvement and mental disorders in mainland China. PLoS One. (2015) 10:e0128800. doi: 10.1371/journal.pone.0128800
24. Wang, C, Li, H, Li, L, Xu, D, Kane, RL, and Meng, Q. Health literacy and ethnic disparities in health-related quality of life among rural women: results from a Chinese poor minority area. Health Qual Life Outcomes. (2013) 11:1–9. doi: 10.1186/1477-7525-11-153
25. Yu, X, Wang, L, Liu, M, Li, Q, and Dai, X. Externalizing behavior problems among hui ethnicity left-behind children in rural China: a cross-sectional study. Psychiatry Investig. (2022) 19:289–301. doi: 10.30773/pi.2021.0119
26. Yu, X, Wang, LL, Liu, MM, Li, QL, Dai, XY, and Li, LG. Internalizing behavior problems among the left-behind children of the hui nationality in rural China: a cross-sectional study. Psychol Res Behav Manag. (2022) 15:887–902. doi: 10.2147/prbm.S347639
27. Correcting myopia among secondary school children to increase academic high school attendance rates in rural communities. Available at: https://ClinicalTrials.gov/show/NCT04077086.
28. The Ministry of Education of the People's Republic of China. The evaluation indexes and monitoring system of education in China. (2015). Available at: http://www.moe.gov.cn/srcsite/A03/s182/201509/t20150907_206014.html (Accessed September 13, 2022).
29. Vyas, S, and Kumaranayake, L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. (2006) 21:459–68. doi: 10.1093/heapol/czl029
30. Lovibond, PF, and Lovibond, SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
31. Wang, K, Shi, H-S, Geng, F-L, Zou, LQ, Tan, SP, Wang, Y, et al. Cross-cultural validation of the depression anxiety stress scale–21 in China. Psychol Assess. (2016) 28:e88:–e100. doi: 10.1037/pas0000207
32. Wang, H, Barket, B, Du, S, Friesen, D, Kohrman, E, Tok, E, et al. The prevalence and correlates of vision impairment and glasses ownership among ethnic minority and Han schoolchildren in rural China. PLoS One. (2021) 16:e0256565. doi: 10.1371/journal.pone.0256565
33. Martínez-Líbano, J, Torres-Vallejos, J, Oyanedel, JC, González-Campusano, N, Calderón-Herrera, G, and Yeomans-Cabrera, M-M. Prevalence and variables associated with depression, anxiety, and stress among Chilean higher education students, post-pandemic. Front Psych. (2023) 14:1139946. doi: 10.3389/fpsyt.2023.1139946
34. Afrin, S, Nasrullah, S, Dalal, K, Tasnim, Z, Benzadid, MS, Humayara, F, et al. Mental health status of adolescents in-home quarantine: a multi-region, cross-sectional study during COVID-19 pandemic in Bangladesh. BMC Psychol. (2022) 10:116. doi: 10.1186/s40359-022-00819-3
35. Radwan, E, Radwan, A, Radwan, W, and Pandey, D. Prevalence of depression, anxiety and stress during the COVID-19 pandemic: a cross-sectional study among Palestinian students (10–18 years). BMC Psychol. (2021) 9:187. doi: 10.1186/s40359-021-00688-2
36. Chai, J, Xu, H, An, N, Zhang, P, Liu, F, He, S, et al. The prevalence of mental problems for Chinese children and adolescents during COVID-19 in China: a systematic review and Meta-analysis. Front Pediatr. (2021) 9:661796. doi: 10.3389/fped.2021.661796
37. Health Commission of Ningxia Hui Autonomous Region. Covid-19 situation of Ningxia Hui autonomous region of 30th September, 2021. (2021). Available at: http://wsjkw.nx.gov.cn/sy_279/yqfkdt/yqsd/202110/t20211001_3072246.html (Accessed June 28, 2022).
38. Pišot, S, Milovanović, I, Šimunič, B, Gentile, A, Bosnar, K, Prot, F, et al. Maintaining everyday life praxis in the time of COVID-19 pandemic measures (ELP-COVID-19 survey). Eur J Pub Health. (2020) 30:1181–6. doi: 10.1093/eurpub/ckaa157
39. Guan, H, Okely, AD, Aguilar-Farias, N, del Pozo Cruz, B, Draper, CE, el Hamdouchi, A, et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolesc Health. (2020) 4:416–8. doi: 10.1016/S2352-4642(20)30131-0
40. Xiang, M, Zhang, Z, and Kuwahara, K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. (2020) 63:531–2. doi: 10.1016/j.pcad.2020.04.013
41. Domingues-Montanari, S. Clinical and psychological effects of excessive screen time on children. J Paediatr Child Health. (2017) 53:333–8. doi: 10.1111/jpc.13462
42. Tremblay, MS, LeBlanc, AG, Janssen, I, Kho, ME, Hicks, A, Murumets, K, et al. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab. (2011) 36:59–64. doi: 10.1139/H11-012
43. Foreman, J, Salim, AT, Praveen, A, Fonseka, D, Ting, DSW, Guang He, M, et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit Health. (2021) 3:e806–18. doi: 10.1016/S2589-7500(21)00135-7
44. Xiao, S, Yan, Z, and Zhao, L. Physical activity, screen time, and mood disturbance among Chinese adolescents during COVID-19. J Psychosoc Nurs Ment. (2021) 59:14–20. doi: 10.3928/02793695-20201104-04
45. Health Department of China. Guideline of myopia prevention of adolescents and children during the COVID-19 pandemic. (2020). Available at: http://www.nhc.gov.cn/jkj/s5899tg/202004/8258621038d346659a64c69b06f46405.shtml.
46. Hill, D, Ameenuddin, N, Reid Chassiakos, YL, Corinn Cross, MD, Jeffrey Hutchinson, MD, Alanna Levine, MD, et al. Media and young minds. Pediatrics. (2016) 138:e20162591. doi: 10.1542/peds.2016-2591
47. Ying, L, Zhu, X, Haegele, J, and Wen, Y. Movement in high school: proportion of Chinese adolescents meeting 24-hour movement guidelines. Int J Environ Res Public Health. (2020) 17:2395. doi: 10.3390/ijerph17072395
48. Feng, Q, Zhang, Q-l, Du, Y, Ye, Y-l, and He, Q-q. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One. (2014) 9:e100914. doi: 10.1371/journal.pone.0100914
49. Chaput, J-P, Gray, CE, Poitras, VJ, Carson, V, Gruber, R, Olds, T, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. (2016) 41:S266–82. doi: 10.1139/apnm-2015-0627
50. Bruni, O, Malorgio, E, Doria, M, Finotti, E, Spruyt, K, Melegari, MG, et al. Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Med. (2022) 91:166–74. doi: 10.1016/j.sleep.2021.02.003
51. Bonelli, RM, and Koenig, HG. Mental disorders, religion and spirituality 1990 to 2010: a systematic evidence-based review. J Relig Health. (2013) 52:657–73. doi: 10.1007/s10943-013-9691-4
52. Shimbo, A. The lifestyle transformation of Hui Muslim women in China: a comparison of modern and Islamic education. J Contemp East Asia Stud. (2017) 6:42–61. doi: 10.1080/24761028.2017.1312756
53. Stigsdotter, UK, Ekholm, O, Schipperijn, J, Toftager, M, Kamper-Jørgensen, F, and Randrup, TB. Health promoting outdoor environments-associations between green space, and health, health-related quality of life and stress based on a Danish national representative survey. Scand J Public Health. (2010) 38:411–7. doi: 10.1177/1403494810367468
54. Beyer, KM, Kaltenbach, A, Szabo, A, Bogar, S, Nieto, FJ, and Malecki, KM. Exposure to neighborhood green space and mental health: evidence from the survey of the health of Wisconsin. Int J Environ Res Public Health. (2014) 11:3453–72. doi: 10.3390/ijerph110303453
55. Niemi, HM, and Kousa, P. A case study of Students' and Teachers' perceptions in a Finnish high school during the COVID pandemic. Int J Technol Educ Sci. (2020) 4:352–69. doi: 10.46328/ijtes.v4i4.167
56. Anderson, T. Getting the mix right again: An updated and theoretical rationale for interaction. Int Rev Res Open Distance Learn. (2003) 4:1–14. doi: 10.19173/irrodl.v4i2.149
57. Reiss, F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. (2013) 90:24–31. doi: 10.1016/j.socscimed.2013.04.026
58. Wu, W, Qu, G, Wang, L, Tang, X, and Sun, YH. Meta-analysis of the mental health status of left-behind children in China. J Paediatr Child Health. (2019) 55:260–70. doi: 10.1111/jpc.14349
59. International Labour Organization. China: rapid assessment of the impact of COVID-19 on employment. (2020). Available at: https://www.ilo.org/emppolicy/areas/covid/WCMS_752056/lang--en/index.htm (Accessed October 3, 2022).
60. Guo, J, Ren, X, Wang, X, Qu, Z, Zhou, Q, Ran, C, et al. Depression among migrant and left-behind children in China in relation to the quality of parent-child and teacher-child relationships. PLoS One. (2015) 10:e0145606. doi: 10.1371/journal.pone.0145606
61. Farnfield, S, and Holmes, P. The Routledge handbook of attachment: assessment. London: Routledge (2014).
62. Cao, Y, Huang, L, Si, T, Wang, NQ, Qu, M, and Zhang, XY. The role of only-child status in the psychological impact of COVID-19 on mental health of Chinese adolescents. J Affect Disord. (2021) 282:316–21. doi: 10.1016/j.jad.2020.12.113
63. Fan, M. Effects of the “one-child” policy and the number of children in families on the mental health of children in China. Rev Cercet Interv Soc. (2016) 52:105–29.
64. Liu, J, Sekine, M, Tatsuse, T, Fujimura, Y, Hamanishi, S, and Zheng, X. Association among number, order and type of siblings and adolescent mental health at age 12. Pediatr Int. (2015) 57:849–55. doi: 10.1111/ped.12629
65. Argabright, ST, Tran, KT, Visoki, E, DiDomenico, GE, Moore, TM, and Barzilay, R. COVID-19-related financial strain and adolescent mental health. Lancet Reg Health. (2022) 16:100391. doi: 10.1016/j.lana.2022.100391
Keywords: mental health, children, vision impairment, rural China, COVID-19
Citation: Li D, Chan VF, Wang H, Zhang H, Virgili G, Whitestone N, Xiao B, Singh MK, She X, Mackenzie G, Boswell M, Mavi S, Rozelle S and Congdon N (2024) Depression, anxiety, stress symptoms and their determinants among secondary students with vision impairment in rural Northwestern China during the COVID-19 pandemic. Front. Public Health. 11:1282826. doi: 10.3389/fpubh.2023.1282826
Edited by:
Lisa Chiara Fellin, University of Bergamo, ItalyReviewed by:
Jonathan Martínez-Líbano, Andres Bello University, ChileMaría-Mercedes Yeomans-Cabrera, Universidad de las Américas, Chile
Copyright © 2024 Li, Chan, Wang, Zhang, Virgili, Whitestone, Xiao, Singh, She, Mackenzie, Boswell, Mavi, Rozelle and Congdon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ving Fai Chan, di5jaGFuQHF1Yi5hYy51aw==; Nathan Congdon, bmNvbmdkb24xQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Dongfeng Li
Dongfeng Li Ving Fai Chan3*†
Ving Fai Chan3*† Huan Wang
Huan Wang Manpreet K. Singh
Manpreet K. Singh Xinshu She
Xinshu She Scott Rozelle
Scott Rozelle Nathan Congdon
Nathan Congdon