- 1Department of Preventive Medicine, Shantou University Medical College, Shantou, Guangdong, China
- 2Faculty of Health Sciences and Sports, Macao Polytechnic University, Macao, Macao SAR, China
- 3Macao Polytechnic University, Peking University Health Science Center-Macao Polytechnic University Nursing Academy, Macao, Macao SAR, China
Background: Suicidal and self-injurious-related behaviors (SSIRBs) are a serious public health challenge in China. However, a comprehensive systematic review of psychosocial interventions for SSIRBs among Chinese adolescents has not been performed. To fill this gap, this systematic review and meta-analysis aimed to examine psychosocial interventions for SSIRBs among Chinese adolescents.
Methods: Eight international (PubMed, EMBASE, Cochrane Library, ScienceDirect, Clinical Trial, CINAHL, PsycINFO, and Web of Science) and four Chinese (Wanfang, SinoMed, CEPS, and CNKI) databases were searched from inception to 31 January 2023. Data extraction and quality assessment were independently conducted by two groups of researchers. Qualitative synthesis and meta-analysis were both used.
Results: The initial search yielded 16,872 titles. Of the 649 full texts reviewed, 19 intervention articles focusing on SSIRBs met the inclusion criteria. Thirteen out of the 19 included studies involved cognitive–behavioral therapy (CBT). Seven non-suicidal self-injury (NSSI) studies assessing self-injurious behaviors were included (six short-term studies and three long-term studies). Compared with long-term interventions [−1.30 (95% CI: –1.84, −0.76)], short-term psychosocial interventions had a higher standardized mean difference (SMD) value [1.86 (95% CI: –2.72, −0.99)]. Meta-regression showed an inverse relationship between the treatment response and sample size (slope = 0.068, Z = 2.914, p = 0.004) and proportion of females (slope = 1.096, Z = 5.848, p < 0.001). Subgroup analyses showed that compared with the “less than 1 month” group [−0.494 (−0.783, −0.205)], in the “immediate postintervention” group, the pooled estimate was significantly lower [−2.800 (−4.050, −1.550), p < 0.001].
Conclusion: Our review systematically summarized the key characteristics and effectiveness of existing psychosocial interventions for SSIRBs among Chinese adolescents. Short-term psychosocial interventions for NSSI were significantly effective in reducing self-injurious behavior scores, especially in the immediate postintervention period. More favorable treatment responses could be observed in both male and small samples.
1 Introduction
Approximately 800,000 persons die globally each year due to suicide, among whom approximately 60,000 are young people (1, 2). Suicide is the main cause of adolescent death (1), and approximately 1% to 18% of adolescents each year are diagnosed with suicidal and self-injurious-related behaviors (SSIRBs) (3, 4), including non-suicidal self-injury (NSSI), self-injurious behavior (SIB), suicide ideation (SI), and suicide attempts (SAs) (5–11), some of which are recognized as stages of the suicide continuum (12). Suicidal behaviors range from SI, suicide plans (SPs), and SAs to completed suicide (13). SI is widely accepted as a reflection of engagement in suicide-related behaviors (11). SAs are defined as potential self-injurious behaviors associated with at least some intent to die (14). Manifested as the deliberate, self-induced destruction of body tissues, the definition of NSSI as an essential component of SIB is based on the absence of suicidal intent (15). As the main component of SSIRBs, which are a severe public health problem (1, 16), suicide-related behaviors often lead to serious adverse consequences (17). These results are mainly reflected in personal psychological and physical pain as well as negative impacts on families and even communities (18).
In light of the above, many psychosocial intervention studies have been conducted in Western countries (19–21). For example, two previous studies demonstrated that internet-based cognitive–behavioral therapy (e-CBT) could reduce SI and alleviate symptoms of depression and despair (20, 21). A program from the Youth Aware of Mental Health (YAMH) in Europe found that the use of CBT significantly reduced SI and SAs among high school students (19). However, high-quality psychosocial intervention studies are rarely conducted among Chinese adolescents with SSIRBs. Moreover, early reviews also showed that both CBT and dialectical behavior therapy (DBT) were effective in treating individuals with SSIRBs (22, 23). However, due to language restrictions, Chinese intervention studies were rarely included in early systematic reviews and meta-analyses.
The rapid process of socialization, as well as the unique Chinese traditional cultural background and policies (24, 25), have had some impact on changes in suicide rates among adolescents (26, 27). There is accumulated evidence that the prevalence rates and mortality of SSIRBs are on the rise (28–30). Effective interventions and strategies that are suitable for China’s national conditions urgently need to be developed and implemented. Previous studies have shown that evidence-based interventions in clinical settings are effective (31, 32), but there is still a lack of high-quality systematic reviews and meta-analyses to guide interventions for Chinese adolescents with SSIRBs. At present, only a systematic scoping review in the Chinese population summarized the prevalence of and risk factors and interventions for NSSI (16). Nevertheless, several disadvantages need to be noted: first, only six databases were searched; second, a meta-analysis of interventions for NSSI was not performed; and third, only studies relating to NSSI were included.
From the above, no study has conducted a comprehensive and systematic review of psychosocial interventions for SSIRBs in China. To the best of our knowledge, this is the first study to systematically summarize psychosocial interventions for SSIRBs among Chinese adolescents. It might help us develop more authoritative intervention methods in the selection of treatment for SSIRBs, especially in intervening in NSSI among adolescents in China.
2 Materials and methods
This meta-analysis was prospectively registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY; registration number: 202350069) and was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
2.1 Eligibility criteria and outcome measures
According to the PICOS tool, the inclusion criteria were as follows: Participants (P): Chinese adolescents (up to and 18 years old) with SSIRBs (e.g., NSSI, SI, and SAs); intervention (I): psychosocial treatment (e.g., CBT, counseling, and systemic interventions); comparison (C): non-intervention or non-experimental group intervention (e.g., routine treatment and drug therapy); outcomes (O): effectiveness; and study design (S): randomized-controlled trials (RCTs), clinical-controlled trials (CCTs), and prepost studies. The exclusion criteria included (a) studies of Chinese adolescents with mental diseases, (b) studies using qualitative methods, and (c) non-Chinese or non-English studies. The main outcomes were the mean and standard deviation (SD) of scores on the SSIRB scale, such as the Questionnaire for Middle School Students’ Behavior (QMSSB) and the Adolescent Non-suicidal Self-injury Assessment Questionnaire (ANSAQ). Secondary outcomes were the mean and SD of scores on other symptom scales relating to hopelessness, depression, anxiety, and family function, such as the Chinese Family Function Scale (CFFS) and Middle School Students Depression Scale (MSSDS).
2.2 Search strategy and study selection
A literature search in both international (PubMed, EMBASE, Cochrane Library, ScienceDirect, Clinical Trial, CINAHL, PsycINFO, and Web of Science) and Chinese (Wanfang, SinoMed, CEPS, and CNKI) databases from inception to 31 January 2023 was independently conducted by two groups of researchers (JJL, WTG, WWR and NY, ZXW, and KIG L). To identify studies for review (33), the following subject and free terms were used: (“auto mutilat*“OR “cutt*” OR “headbang*” OR “overdos*” OR “selfdestruct*” OR “selfharm*” OR “selfimmolat*” OR “selfinflict*” OR “selfinjur*” OR “selfpoison*” OR “suicid*” OR “suicide, attempted” OR “suicidal ideation”) AND (“adolescent” OR “teen” OR “youth” OR “teenager”) AND (“China” OR “Chinese”). More detailed information is provided in Supplementary Figure S1.
The same two groups of researchers independently screened the titles and abstracts and then read the full texts of relevant publications for eligibility. Any discrepancy was discussed with another researcher (WIP P). The reference lists of the included articles, relevant systematic reviews, and meta-analyses were searched manually for additional studies (1, 33–50).
2.3 Data extraction
A predesigned Excel data collection sheet was used by the two groups of researchers to independently extract relevant data, including the following characteristics of studies and participants: first author, year of survey and publication, survey province, study type, sampling method, sample size, types of interventions in the control and experimental groups, setting, inclusion criteria, intervention duration, type of SSIRB, age range, mean and SD of participant age, number and proportion of males, definitions of various types of SSIRBs, and measurements.
According to a categorical criterion of psychosocial intervention (51), types of intervention were clustered into a new parent set and a subset. Data were extracted and double-checked independently by two researchers (KIG L and WWR). Disagreements were settled through discussion with another senior researcher (WIP P). To address the missing SD values, we substituted them with the average SD values reported from other RCTs that assessed the same treatment or outcome measures (52). GetData Graph Digitizer version 2.25.0.32 was used to extract related information presented in images.
2.4 Quality assessment and evidence level
The quality of the included studies was evaluated by quality assessment checklists based on study designs. RCT studies were evaluated by the Jadad scale (0–5 points) (53). CCT studies were assessed using the National Heart, Lung, and Blood Institute (NHLBI) tailored tool for controlled intervention studies (0–16 points) (54). The NHLBI checklist developed for before-after studies with no control group was used for pre–post studies (0–12 points) (54). The quality assessment was conducted under the assumption that each criterion contributed equally to study quality. Study quality was independently assessed by two reviewers (WWR and JJL). Disagreements were resolved through discussions with another researcher (KIG L).
2.5 Statistical analysis
2.5.1 Qualitative synthesis
Based on a qualitative analysis method, we synthesized the study traits, intervention attributes, and outcomes concerning the efficacy of the interventions.
2.5.2 Meta-analysis
According to the duration of follow-up (55), studies were categorized into two periods in the meta-analysis: (1) short-term studies, which referred to studies in which the outcomes were assessed within 1 month after the intervention and (2) long-term studies, which encompassed studies in which the outcomes were evaluated at least 1 month after the intervention. Owing to the limitation of the number of included studies, more than three articles with the same SSIRBs and relevant self-injurious assessments were considered for meta-analysis. Given the different sampling methods, demographic characteristics, and instruments between studies, the estimates of self-injurious-related behavior scores were calculated as standardized mean differences (SMDs) using the Der Simonian and Laird random-effects model (56). Heterogeneity across studies was estimated with Cochran’s Q test and I2 statistics, with I2 ≥ 50% or a Cochran’s Q test value of p of <0.05 indicating significant heterogeneity (57). Subgroup analyses were conducted according to the following categorical variables: assessment period (“immediate postintervention” group vs. “less than 1 month” group), measurements [ANSAQ vs. QMSSB/Adolescent Self Harm Scale (ASHS) vs. others], definition of NSSI (DSM-V criteria vs. hospitalization vs. others), and geographic region (Eastern China vs. Western China, according to the National Bureau of Statistics of China). Meta-regression analyses were used to examine the associations between self-injurious-related behavior scores and the sample size, mean age, and sex ratio (female/male). Sensitivity analyses were conducted to explore the outlier studies. Funnel plots and Begg’s test were used to assess publication bias. The significance level was set at 0.05 (two-tailed). The meta-analyses were conducted using Comprehensive Meta-Analysis software, Version 2 (CMA, Biostat Inc., Englewood, New Jersey, USA) and RevMan software, Version 5.3.
3 Results
3.1 The overall characteristics of the included literature
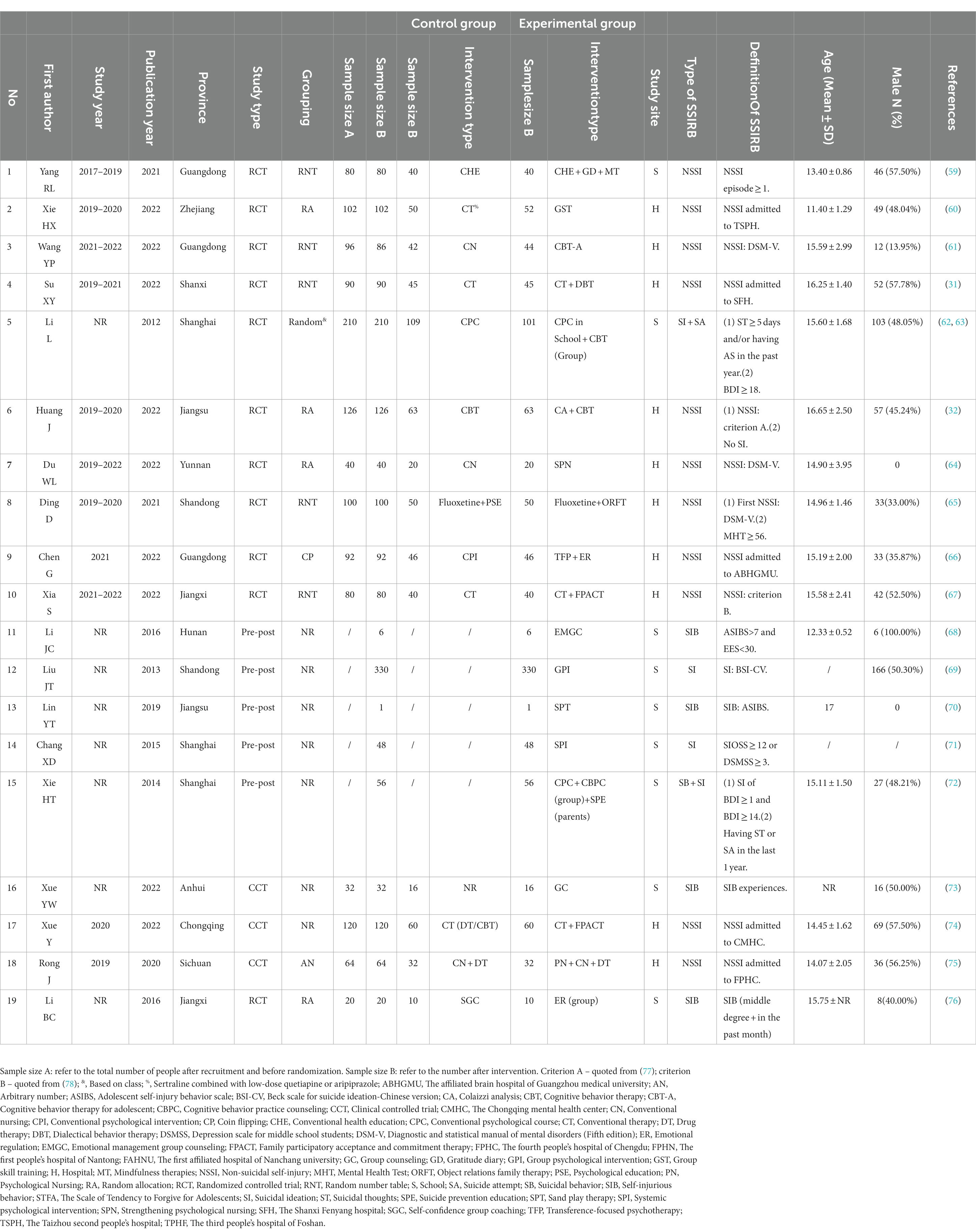
Altogether, 16,872 articles were screened. Of these articles, only 9,319 were deemed eligible after filtering based on titles and abstracts. After full-text screening, 19 studies with 1,683 participants (1,060 subjects in the intervention group and 623 subjects in the control group) met the selection criteria (Figure 1). The publication time ranged from 2012 to 2022. No relevant literature from Hong Kong, Macao, or Taiwan was eligible, but the included studies were distributed in different provinces of mainland China (Table 1).
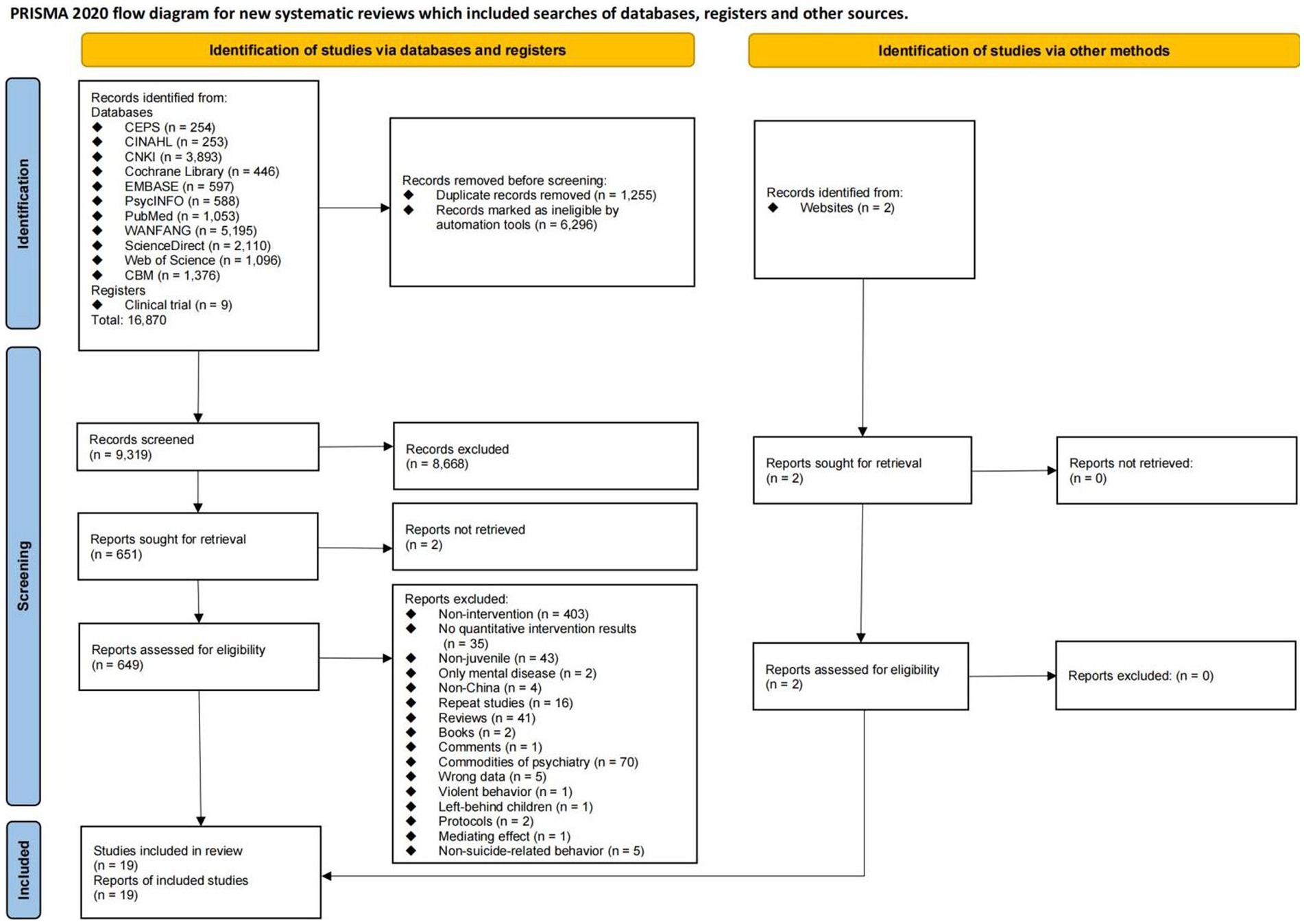
Figure 1. PRISMA flow diagram. From Page et al. (58).
3.2 Suicidal-related behaviors
3.2.1 Intervention targets
As shown in Figure 2, two studies focused on SI. Moreover, one study explored SI in conjunction with SAs. Another study examined SI combined with suicidality.
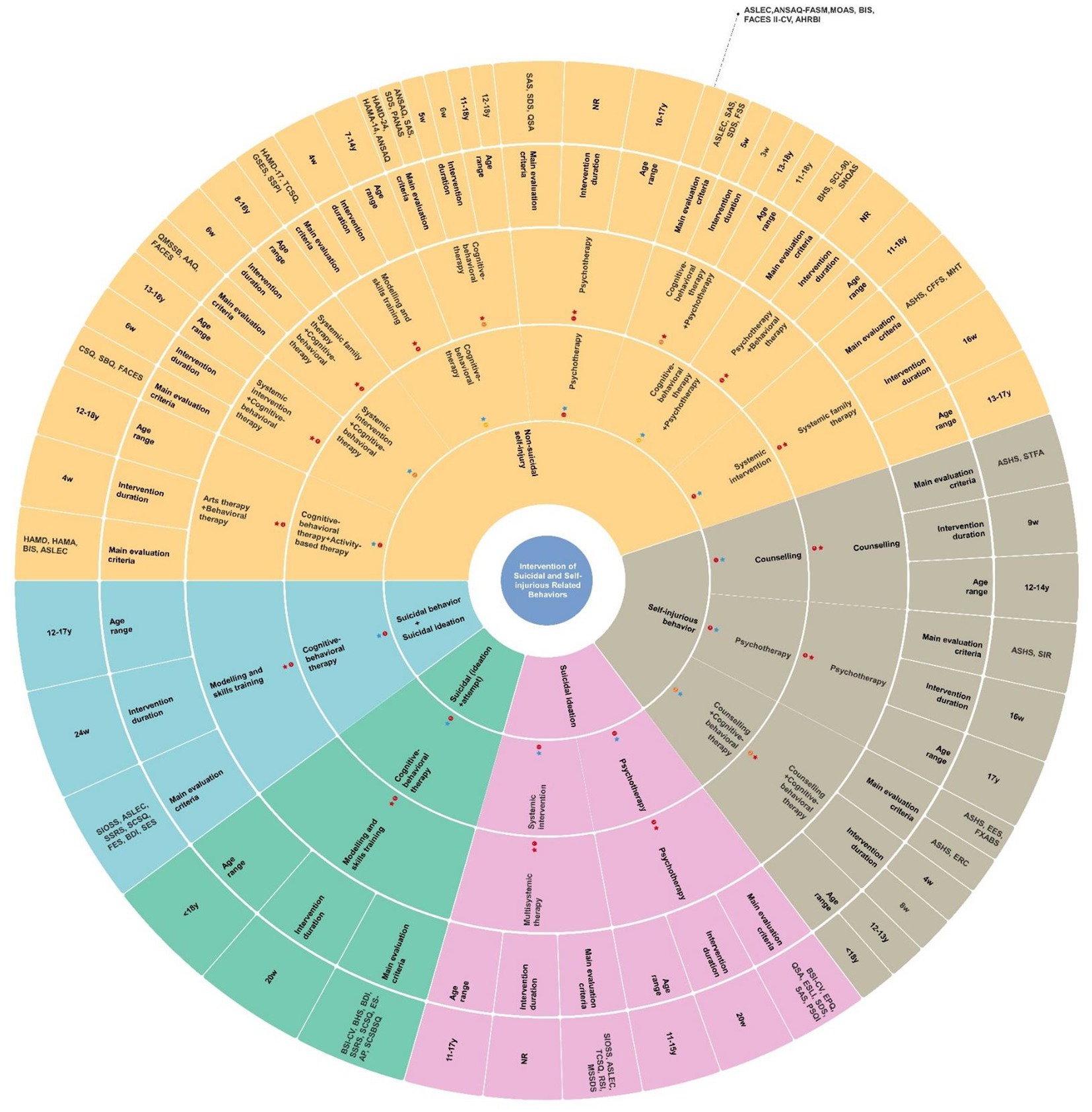
Figure 2. Intervention of suicidal and self-injurious related behaviors. 1 months = 4 weeks. Borders marked with “ ” belong to the large category of therapeutic approaches, while sub-category are tagged as “
” belong to the large category of therapeutic approaches, while sub-category are tagged as “ .”
.”  : means that there is one study.
: means that there is one study.  : means that there are two studies.
: means that there are two studies.  : means that there are three studies. ASLEC, Adolescent Self-rating Life Events Check List; AHRBI, Adolescent Health Related Risk Behavior Inventory; ASHS, Adolescent Self Harm Scale; AAQ, Acceptance and Action Questionnaire; ANSAQ, Adolescent Non-suicidal Self-injury Assessment Questionnaire; BHS, Beck Hopelessness Scale; BDI, Beck Depression Inventory; BSI-CV, Beck Scale for Suicide Ideation-Chinese Version; BIS, Barratt Impulsiveness Scale; CSQ, Coping Style Questionnaire; CFFS, Chinese Family Function Scale; MSSDS, Middle School Students Depression Scale; RSI, Rate of Suicide Ideation; ES-AP, Emotional Skills Assessment Process; EPQ, Eysenck’s Personality Questionnaire; ESLI, Emotional–Social Loneliness Inventory; EES, Emotional Expression Scale; ERC, Emotional regulation scale; FES, Family Environment Scale; FASM, Functional Assessment of Self ⁃ mutilation; GSES, General Self-Efficacy Scale; FXABS, Fan Xiaodong Affect Balance Scales; FSS, Frequency and Severity of Self-injury; FACES, Family Adaptability and Cohesion Evaluation Scale; HAMD-24, Hamilton Depression Scale 24-item; HAMA-14, Hamilton Anxiety Scale 14-item; MOAS, Modified Overt Aggression Scale; PANAS, Positive and Negative Affect Scale; PSQI, Pittsburgh Sleep Quality Index; QSA, Suicide Attitude Questionnaire; QMSSB, Questionnaire for Middle School Students’ Behavior; SSRS, Social Support Rating Scale; SCSQ, Simplified Coping Style Questionnaire; SSPI, Scale of Social function in Psychosis Inpatients; SIOSS, Self-rating Idea of Suicide Scale; SES, Self-Esteem Scale; SAS, Self-rating Anxiety Scale; SDS, Self-rating Depression Scale; SCL-90, Symptom Check List-90; SNQAS, Self-developed Nursing Quality Assessment Scale; SCSBSQ, Self-compiled Suicide Behavior Survey Questionnaire; SBQ, Self-injury Behavior Questionnaire; SS, Self-esteem Scale; SIR, Self-Injury Rate; STFA, Scale of Tendency to Forgive for Adolescents; TCSQ, Trait Coping Style Questionnaire.
: means that there are three studies. ASLEC, Adolescent Self-rating Life Events Check List; AHRBI, Adolescent Health Related Risk Behavior Inventory; ASHS, Adolescent Self Harm Scale; AAQ, Acceptance and Action Questionnaire; ANSAQ, Adolescent Non-suicidal Self-injury Assessment Questionnaire; BHS, Beck Hopelessness Scale; BDI, Beck Depression Inventory; BSI-CV, Beck Scale for Suicide Ideation-Chinese Version; BIS, Barratt Impulsiveness Scale; CSQ, Coping Style Questionnaire; CFFS, Chinese Family Function Scale; MSSDS, Middle School Students Depression Scale; RSI, Rate of Suicide Ideation; ES-AP, Emotional Skills Assessment Process; EPQ, Eysenck’s Personality Questionnaire; ESLI, Emotional–Social Loneliness Inventory; EES, Emotional Expression Scale; ERC, Emotional regulation scale; FES, Family Environment Scale; FASM, Functional Assessment of Self ⁃ mutilation; GSES, General Self-Efficacy Scale; FXABS, Fan Xiaodong Affect Balance Scales; FSS, Frequency and Severity of Self-injury; FACES, Family Adaptability and Cohesion Evaluation Scale; HAMD-24, Hamilton Depression Scale 24-item; HAMA-14, Hamilton Anxiety Scale 14-item; MOAS, Modified Overt Aggression Scale; PANAS, Positive and Negative Affect Scale; PSQI, Pittsburgh Sleep Quality Index; QSA, Suicide Attitude Questionnaire; QMSSB, Questionnaire for Middle School Students’ Behavior; SSRS, Social Support Rating Scale; SCSQ, Simplified Coping Style Questionnaire; SSPI, Scale of Social function in Psychosis Inpatients; SIOSS, Self-rating Idea of Suicide Scale; SES, Self-Esteem Scale; SAS, Self-rating Anxiety Scale; SDS, Self-rating Depression Scale; SCL-90, Symptom Check List-90; SNQAS, Self-developed Nursing Quality Assessment Scale; SCSBSQ, Self-compiled Suicide Behavior Survey Questionnaire; SBQ, Self-injury Behavior Questionnaire; SS, Self-esteem Scale; SIR, Self-Injury Rate; STFA, Scale of Tendency to Forgive for Adolescents; TCSQ, Trait Coping Style Questionnaire.
3.2.2 Intervention area, year, and site
All four studies were geographically clustered in the eastern region of China. One study of an intervention for suicide-related behaviors was published every year. From 2012 to 2015, one article was retrieved for each year. All studies were performed at schools (Table 1).
3.2.3 Intervention approaches
All empirical studies used group therapy. In addition, as shown in Figure 2, three strategies (i.e., systemic interventions, psychotherapy, and CBT) were mentioned in the included studies, and CBT appeared in two studies.
3.2.4 Study quality
The majority of the three pre–post studies scored approximately 8 points out of a maximum score of 12 points. One article used a CCT design, which obtained 7 of 16 points (Supplementary Table S1).
3.3 Self-injurious behaviors
3.3.1 General self-injury
Between 2016 and 2022, four studies explored intervention strategies for self-injurious behavior (Figure 2). Distributed in the eastern and central parts of China, these studies were conducted in Hunan Province, Jiangxi Province, Anhui Province, and Jiangsu Province. All studies were also carried out at schools. Apart from one study that used individual therapy alone, the other three studies applied group therapy. Half of the studies used combination therapy (i.e., counseling and CBT). The two other studies used counseling and psychotherapy. One study adopted a CCT design (7 points). The score of another RCT study, which did not use the appropriate randomization sequence method, was 1 point. Additionally, the average score of study quality in two pre- and postintervention studies was 7 points.
3.3.2 Non-suicidal self-injury
3.3.2.1 Intervention targets
Eleven studies focusing on NSSI were included in our review. Since four studies did not perform self-injury behavior assessments, seven studies were included in the final meta-analysis. Ultimately, six short-term studies and three long-term studies were pooled and analyzed according to predefined criteria. Two of the included studies used the ANSAQ-behavioral questionnaire, followed by the ASHS in one study, the QMSSB in one study, the FASM-behavioral questionnaire in one study, the SBQ in one study, and the Self-developed Nursing Quality Assessment Scale (SNQAS)-Self-injury risk assessment in one study. The detailed self-injury-related measurements and psychosocial intervention strategies are summarized in Figure 2.
3.3.2.2 Intervention area, year, and site
Six studies were geographically concentrated in coastal cities, namely, Guangdong Province, Zhejiang Province, Jiangsu Province, and Shandong Province. Two studies were conducted in Central China, while another three studies were conducted in Western China. Only one study was published in 2020, and two studies were published in 2021. Then, most notably, the number of studies increased to eight in 2022, indicating an enormous growth trend of research interest. Furthermore, 10 studies were conducted in hospitals, with one study including a school sample.
3.3.2.3 Intervention approaches
Three studies applied family therapy to treat adolescents with NSSI. The most commonly used psychological intervention was CBT, which was used in six studies.
3.3.2.4 Study quality
Nine studies were classified as RCTs. The scores of most studies were greater than or equal to 2, but most studies did not use a double-blind method. Two studies utilized a CCT design, with an average score of 7. Overall, the study quality was acceptable (Supplementary Table S1).
3.3.2.5 Rating of outcomes in the included studies (short-term)
The risk of self-injury and functional scores of the adolescents in the experimental group significantly decreased and were lower than those of the adolescents in the control group (31, 32, 64, 65, 67, 74). Only one study used the ANSAQ (experimental group: 58.68 ± 8.67 vs. control group: 68.61 ± 10.57, p < 0.001) (31). Using systematic interventions, CBT, and psychotherapy alone or in combination, four studies reported not only a significantly reduced risk of self-injury among adolescents but also significantly increased scores for family intimacy and adaptability (32, 65, 67, 74). Su et al. showed that CBT could significantly improve the scores of the Self-rating Anxiety Scale (SAS) (Z = 2.171, p = 0.030), Self-rating Depression Scale (SDS) (Z = 2.285, p = 0.022), and Positive and Negative Affect Scale (PANAS) [positive emotions: (experimental group: 26.39 ± 2.86 vs. control group: 22.23 ± 2.63, p < 0.001); negative emotions: (experimental group: 29.91 ± 2.73 vs. control group: 33.01 ± 3.19, p < 0.001)] (31).
3.3.2.6 Rating of outcomes in the included studies (long-term)
There was a significant decrease in the risk of self-injury and impairment in functioning among adolescents who received psychological interventions compared to adolescents in the control group (31, 61, 65). Two studies reported significant improvements in depressive symptoms and anxiety symptoms after the intervention (31, 61). One study conducted by Ding’s team evaluated the efficacy at multiple time points after the intervention (65). The findings indicated that the self-injury scores in the experimental group significantly decreased (8 weeks: 14.5 ± 3.92 vs. 12 weeks: 13.32 ± 4.04 vs. 16 weeks: 8.62 ± 4.05).
3.3.2.7 Meta-analysis
3.3.2.7.1 Effectiveness in the short term
The combined SMD value of self-injurious behavior scores was −1.86 (95% CI: –2.72, − 0.99). Considerable heterogeneity was found (I2 = 95%, p < 0.001, Figure 3). However, no publication bias was found (Begg’s test = 1.503, p = 0.133, Figure 4). Based on sensitivity analysis, it was determined that the pooled SMD value of psychological interventions remained stable regardless of the exclusion of any single study (Supplementary Figure S2). The results of subgroup analyses using assessment periods showed that compared with the “less than 1 month” group [−0.494 (−0.783, −0.205)], in the “immediate postintervention” group, the pooled estimate was lower [−2.800 (−4.050, −1.550)]. As the sample size (slope = 0.068, Z = 2.914, p = 0.004) and proportion of females (slope = 1.096, Z = 5.848, p < 0.001) decreased, a more favorable treatment response was indicated (Supplementary Table S2).
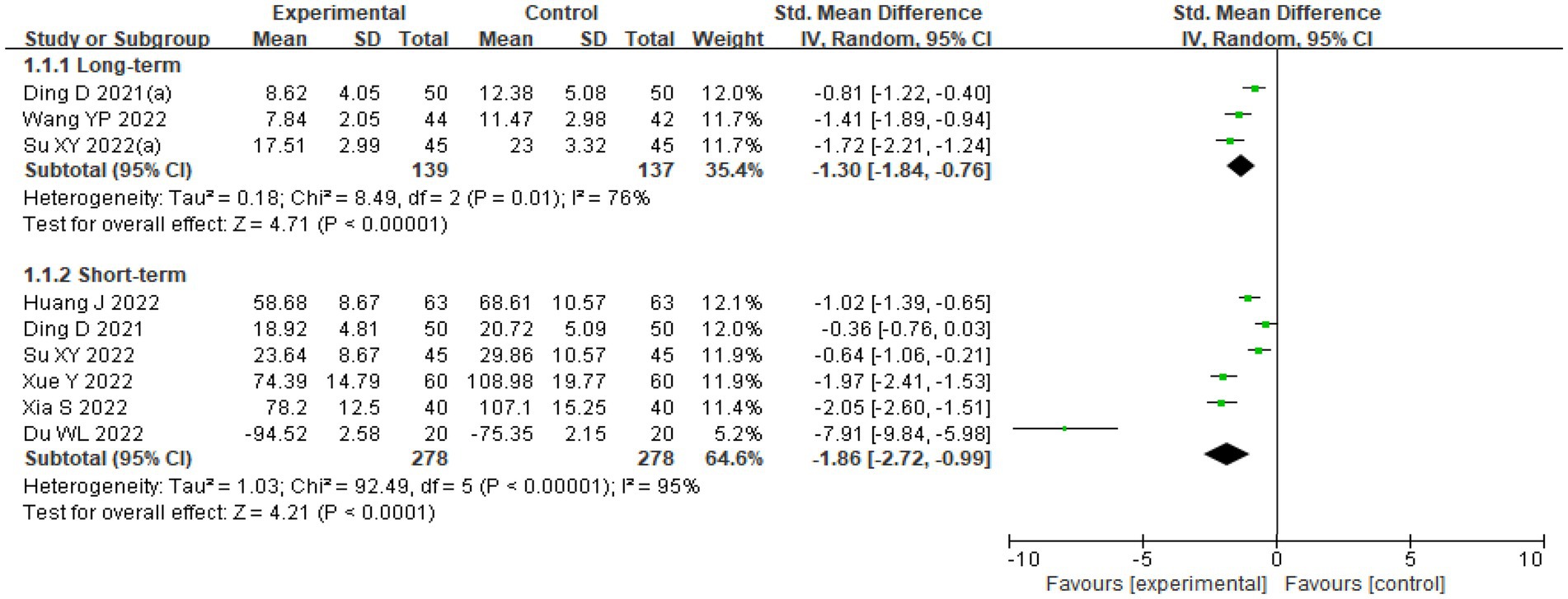
Figure 3. Effectiveness of interventions targeting NSSI. Ding D 2021(a) means the evaluation period: 16 weeks after intervention. Su XY 2022(a) means the evaluation period: 6 weeks after intervention.
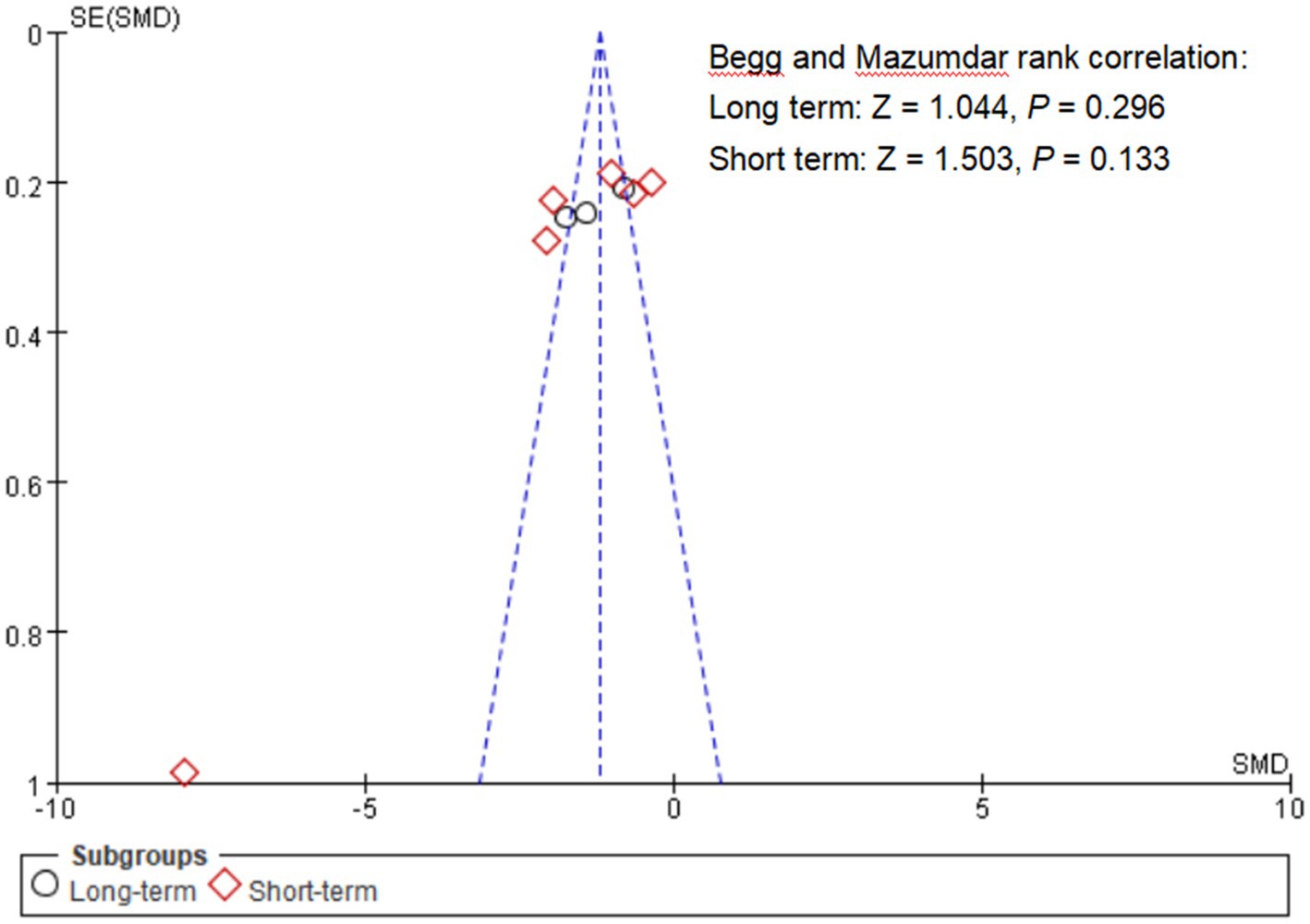
Figure 4. Funnel plot of publication bias. The x-axis represents the SMD for each study, while the y-axis is the standard error of the SMD. The dashed line represents the 95% confidence interval (CI).
3.3.2.7.2 Effectiveness in the long term
The pooled SMD value of self-injurious behavior scores was −1.30 (95% CI: –1.84, − 0.76), indicating relatively poor efficacy. The presence of pronounced heterogeneity was noted (I2 = 76%, p = 0.01, Figure 3). Publication bias was not found (Begg’s test = 1.044, p = 0.296, Figure 4). Given that a study reported the findings from multiple time points (65), the results from other time points were included as sensitivity analysis and showed stable results 8 weeks [− 1.35(− 1.80, − 0.89)] and 12 weeks [−1.30(− 1.85, − 0.75)]. The pooled SMD value of psychological status remained stable regardless of the exclusion of any single study (Supplementary Figure S3).
4 Discussion
This systematic review and meta-analysis provides the first comprehensive overview of the key features and effectiveness of interventions for SSIRBs among Chinese adolescents. The earliest included studies began in 2012 and were geographically distant from inland areas, with the duration of the intervention ranging from 3 to 20 weeks. Thirteen articles were published between 2019 and 2022, which corresponded to the onset of the COVID-19 pandemic (79). Therefore, the pandemic lockdown policy captured mental health workers’ attention toward SSIRBs among adolescents.
4.1 Interventions for SSIRBs
The psychosocial interventions applied in Chinese studies accounted for 5 out of the 10 major categories of psychological interventions (51). Similar to the outcomes of numerous interventions targeting SSIRBs (80–84), our research also showed that psychosocial therapy was effective. A previous study showed that counseling could reduce the occurrence of SAs (85), which was similar to the findings of our study that counseling could reduce self-injury scores. In addition, our study showed that 13 out of the 19 included studies involved CBT, which was considered as the most effective intervention toward suicide reattempts (86). A systematic review among adolescents also suggested that CBT was the only intervention that could effectively reduce the risk of SIB (83). CBT focuses on an individual’s psychological and behavioral patterns and helps them understand the negative factors of SSIRBs, reduce their paranoid thoughts, reshape their perception of personal control, and ultimately achieve the goal of reducing the recurrence of SSIRBs (51, 55). Our study also found that combination therapies, including those with CBT, were more commonly used than single therapy, especially combinations of CBT and psychotherapy (31, 32, 61, 62, 64, 66, 69, 70, 72). Consistent with our study, an early study revealed that CBT combined with psychotherapy could reduce the recurrence of self-injurious behavior over a long follow-up period (87, 88). Therefore, we believe that CBT is the most widely used intervention for treating Chinese adolescents with SSIRBs.
To date, few studies in other countries have applied activity-based therapy or systemic interventions for SSIRBs, which have been applied in Chinese adolescents (59, 65, 67, 71, 74). Other intervention approaches include relationship-based interventions, psychoeducation, group work with children, peer mentoring, and intensive service models. However, no research has proven the effectiveness of these five interventions on SSIRBs among Chinese adolescents. Therefore, more attention should be given to the evaluation of the application of these interventions in the Chinese population in future.
4.2 Meta-analysis for NSSI
Our study revealed that psychosocial interventions for NSSI were effective, especially in the short term. Significant short-term effects of psychosocial interventions were often reported (89–91) because they immediately restored patients’ psychophysiological balance. Although long-term psychosocial interventions were also effective in our study, the effects were attenuated compared with those of short-term interventions, which might have been affected by the number of included studies and the nature of the psychosocial intervention. Meta-regression analyses found that psychosocial interventions might be more effective for small samples and male populations. On the one hand, the intervention form of psychosocial interventions (e.g., CBT) makes it easier to implement and evaluate in a small sample. On the other hand, individual interventions can provide subjects with more attention and improve effectiveness (92, 93). Due to the influence of social and cultural factors and sex roles, men are more likely to suppress and conceal their mental health problems, and men are inclined to participate more actively in the CBT treatment process by providing clear goals, solving problems, and establishing specific strategies (94). Subgroup analysis revealed that the efficacy was significantly greater immediately after the intervention compared with 1 month after the intervention. The pattern of significant short-term effectiveness was generally reflected in psychosocial interventions (95–98). Future studies should focus on assessing the long-term effects of interventions to understand their lasting impact on individuals. This can help evaluate the effectiveness and sustainability of interventions, providing evidence-based decision-making for tailored interventions.
4.3 Implications for future interventions
The findings from our study demonstrated that both offline and face-to-face practices were adopted in traditional interventions, indicating that CBT could significantly reduce depression and anxiety scores. In addition, CBT combined with psychotherapy could significantly reduce feelings of despair in adolescents (31, 60–62, 72). Currently, numerous innovative methods and technologies are continuously emerging, such as virtual reality, mobile applications, and online intervention platforms (99) and have been applied to improve mental health (21, 99, 100). Early studies identified that SI in adults was improved after digital interventions (21, 100). However, one study using an online intervention found that the impact of e-CBT on anxiety and despair in individuals with SI was not significant (99). Therefore, the efficacy of digital interventions for SSIRBs is still unknown. The powerful features of ChatGPT provide researchers with new opportunities (101, 102), but ethical issues also need to be considered (103). Future studies can benefit from multidisciplinary research methods that integrate knowledge from disciplines such as psychology and biology to comprehensively understand the causes of SSIRBs and intervention potential (104). Multidisciplinary approaches offer interdisciplinary perspectives and encourage the development of a deep understanding and effective interventions for SSIRBs (105).
4.4 Strengths and limitations
A comprehensive literature search and complex statistical analyses were carried out. Furthermore, this review not only outlined the characteristics of psychosocial interventions for SSIRBs but also performed a meta-analysis of interventions for NSSI and filled the research gap on psychosocial interventions for SSIRBs among Chinese adolescents. Our research also disseminates the results provided by researchers in China to the international community. As an alternative to drug therapy, psychosocial therapy could not only avoid the hidden dangers of insufficient evidence regarding efficacy and safety but also reduce the occurrence of many adverse reactions (106). This helps to optimize resource allocation and improve intervention effectiveness. Nevertheless, some limitations should be acknowledged. First, owing to the limited number of long-term studies, the effectiveness of the research needs to be cautiously interpreted. Second, the quality of research needs to be improved. Last, as all the reviewed studies were from mainland China, these findings may not be generalizable to other ethnicities.
5 Conclusion
In conclusion, our review systematically summarized the key characteristics and effectiveness of existing psychosocial interventions for SSIRBs among Chinese adolescents. CBT is the most widely used intervention for treating Chinese adolescents with NSSI. Short-term psychosocial interventions for NSSI were significantly effective in reducing self-injurious behavior scores, especially in the immediate postintervention period. More favorable treatment responses could be observed in both male and small samples. Future interventions and research should prioritize individualization, innovation, long-term outcome tracking, multidisciplinary approaches, and international collaborations.
Author contributions
JL: Formal analysis, Writing – original draft, Writing – review & editing. WG: Methodology, Software, Writing – review & editing. NY: Data curation, Writing – review & editing. WP: Data curation, Writing – review & editing. GL: Methodology, Project administration, Writing – review & editing. WR: Methodology, Project administration, Resources, Supervision, Writing – review & editing. ZW: Data curation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the SUMC Scientific Research Foundation for Talents (SRFT, No. 510858060) and the Guangdong-Macau Youth Talent Exchange Program (No. 002–14202212).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1281696/full#supplementary-material
References
1. Wasserman, D, Carli, V, Iosue, M, Javed, A, and Herrman, H. Suicide prevention in childhood and adolescence: a narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia Pac Psychiatry. (2021) 13:e12452. doi: 10.1111/appy.12452
2. World Health Organization. Suicide worldwide in 2019: Global health estimates. (2021) Available at: https://www.who.int/publications/i/item/9789240026643
3. Geoffroy, MC, Bouchard, S, Per, M, Khoury, B, Chartrand, E, Renaud, J, et al. Prevalence of suicidal ideation and self-harm behaviours in children aged 12 years and younger: a systematic review and meta-analysis. Lancet Psychiatry. (2022) 9:703–14. doi: 10.1016/s2215-0366(22)00193-6
4. Rao, WW, Lin, X, Liu, H, Yang, C, and Wang, S. Suicidal ideation and self-harm behaviours in children aged 12 years or younger. Lancet Psychiatry. (2022) 9:855. doi: 10.1016/s2215-0366(22)00319-4
5. Ortin-Peralta, A, Sheftall, AH, Osborn, A, and Miranda, R. Severity and transition of suicidal Behaviors in childhood: sex, racial, and ethnic differences in the adolescent brain cognitive development (ABCD) study. J Adolesc Health. (2023) 73:724–30. doi: 10.1016/j.jadohealth.2023.05.026
6. Liu, RT, Walsh, RFL, Sheehan, AE, Cheek, SM, and Sanzari, CM. Prevalence and correlates of suicide and nonsuicidal self-injury in children: a systematic review and Meta-analysis. JAMA Psychiatry. (2022) 79:718–26. doi: 10.1001/jamapsychiatry.2022.1256
7. Liu, X, Huang, Y, and Liu, Y. Prevalence, distribution, and associated factors of suicide attempts in young adolescents: school-based data from 40 low-income and middle-income countries. PLoS One. (2018) 13:e0207823. doi: 10.1371/journal.pone.0207823
8. DeVille, DC, Whalen, D, Breslin, FJ, Morris, AS, Khalsa, SS, Paulus, MP, et al. Prevalence and family-related factors associated with suicidal ideation, suicide attempts, and self-injury in children aged 9 to 10 years. JAMA Netw Open. (2020) 3:e1920956. doi: 10.1001/jamanetworkopen.2019.20956
9. Nock, MK, Green, JG, Hwang, I, McLaughlin, KA, Sampson, NA, Zaslavsky, AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. (2013) 70:300–10. doi: 10.1001/2013.jamapsychiatry.55
10. Iskric, A, Ceniti, AK, Bergmans, Y, McInerney, S, and Rizvi, SJ. Alexithymia and self-harm: a review of nonsuicidal self-injury, suicidal ideation, and suicide attempts. Psychiatry Res. (2020):288. doi: 10.1016/j.psychres.2020.112920
11. Office of the Surgeon General (US); National Action Alliance for Suicide Prevention (US). 2012 National Strategy for suicide prevention: Goals and objectives for action: A report of the U.S. surgeon general and of the National Action Alliance for suicide prevention. Washington, DC: US Department of Health & Human Services (US) (2012).
12. Sveticic, J, and Leo, DD. The hypothesis of a continuum in suicidality: a discussion on its validity and practical implications. Ment Illn. (2012) 4:73–8. doi: 10.4081/mi.2012.e15
13. Bai, W, Liu, Z, Jiang, Y, Zhang, Q, Rao, W, Cheung, T, et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. (2021) 11:552. doi: 10.1038/s41398-021-01671-6
14. Turecki, G, and Brent, DA. Suicide and suicidal behaviour. Lancet. (2016) 387:1227–39. doi: 10.1016/S0140-6736(15)00234-2
15. Nock, MK, and Favazza, AR. Nonsuicidal self-injury: Definition and classification. Understanding nonsuicidal self-injury: Origins, assessment, and treatment. Washington, DC: American Psychological Association; (2009). 9–18.
16. Qu, D, Wen, X, Liu, B, Zhang, X, He, Y, Chen, D, et al. Non-suicidal self-injury in Chinese population: a scoping review of prevalence, method, risk factors and preventive interventions. Lancet Regional Health. (2023) 37:100794. doi: 10.1016/j.lanwpc.2023.100794
17. Hamza, CA, Stewart, SL, and Willoughby, T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clin Psychol Rev. (2012) 32:482–95. doi: 10.1016/j.cpr.2012.05.003
18. Jordans, M, Rathod, S, Fekadu, A, Medhin, G, Kigozi, F, Kohrt, B, et al. Suicidal ideation and behaviour among community and health care seeking populations in five low- and middle-income countries: a cross-sectional study. Epidemiol Psychiatr Sci. (2018) 27:393–402. doi: 10.1017/s2045796017000038
19. Wasserman, D, Hoven, CW, Wasserman, C, Wall, M, Eisenberg, R, Hadlaczky, G, et al. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet. (2015) 385:1536–44. doi: 10.1016/S0140-6736(14)61213-7
20. Hetrick, S, Yuen, HP, Cox, G, Bendall, S, Yung, A, Pirkis, J, et al. Does cognitive behavioural therapy have a role in improving problem solving and coping in adolescents with suicidal ideation? Cognit. Behav. Therapist. (2014) 7:e13. doi: 10.1017/S1754470X14000129
21. Robinson, J, Hetrick, S, Cox, G, Bendall, S, Yuen, HP, Yung, A, et al. Can an internet-based intervention reduce suicidal ideation, depression and hopelessness among secondary school students: results from a pilot study. Early Interv Psychiatry. (2016) 10:28–35. doi: 10.1111/eip.12137
22. Backer, HS, Miller, AL, and van den Bosch, LM. Dialectical behaviour therapy for adolescents: a literature review. Tijdschr Psychiatr. (2009) 51:31–41.
23. Spirito, A, Esposito-Smythers, C, Wolff, J, and Uhl, K. Cognitive-behavioral therapy for adolescent depression and suicidality. Child Adolesc Psychiatr Clin N Am. (2011) 20:191–204. doi: 10.1016/j.chc.2011.01.012
24. Stack, S. Contributing factors to suicide: political, social, cultural and economic. Prev Med. (2021) 152:106498. doi: 10.1016/j.ypmed.2021.106498
25. Al-Sharifi, A, Krynicki, CR, and Upthegrove, R. Self-harm and ethnicity: a systematic review. Int J Soc Psychiatry. (2015) 61:600–12. doi: 10.1177/0020764015573085
26. Lange, S, Cayetano, C, Jiang, H, Tausch, A, and Oliveira e Souza, R. Contextual factors associated with country-level suicide mortality in the Americas, 2000–2019: a cross-sectional ecological study. Lancet Regional Health. (2023) 20:100450. doi: 10.1016/j.lana.2023.100450
27. Choi, NG, Marti, CN, and Choi, BY. Job loss, financial strain, and housing problems as suicide precipitants: associations with other life stressors. Population Health. (2022) 19:101243. doi: 10.1016/j.ssmph.2022.101243
28. Tian, Y, Luan, M, Chen, H, and Zhang, J. Temporal trend in suicide mortality for Chinese adolescents, 2008 to 2021. JAMA Pediatr. (2023) 177:1224–1226. doi: 10.1001/jamapediatrics.2023.3062
29. Liu, XC, Chen, H, Liu, ZZ, Wang, JY, and Jia, CX. Prevalence of suicidal behaviour and associated factors in a large sample of Chinese adolescents. Epidemiol Psychiatr Sci. (2019) 28:280–9. doi: 10.1017/S2045796017000488
30. Lang, J, and Yao, Y. Prevalence of nonsuicidal self-injury in Chinese middle school and high school students: a meta-analysis. Medicine. (2018) 97:e12916. doi: 10.1097/MD.0000000000012916
31. Su, X, He, J, Zhang, X, Zhang, L, and Men, J. Application of dialectical behavior therapy in adolescents with non-suicidal self-injury (in Chinese). Chin Nurs Res. (2022) 36:3922–5. doi: 10.12102/j.issn.1009-6493.2022.21.029
32. Huang, J, Cheng, X, Zhu, X, and Li, X. Colaizzi analysis combined with cognitive-behavior therapy for adolescent non-suicidal self-injury and its effect on Barratt score and MOAS (in Chinese). The Journal of Practical Medicine. (2022) 38:360–5. doi: 10.3969/j.issn.1006-5725.2022.03.019
33. Hawton, K, Witt, KG, Taylor Salisbury, TL, Arensman, E, Gunnell, D, Townsend, E, et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev. (2015) 2015:CD012013. doi: 10.1002/14651858.CD012013
34. Ding, D. Research progress of dialectical behavior therapy in the treatment of non-suicidal self-injury (in Chinese). Chongqing: ChongQing Medical University (2020).
35. Doty, B, Bass, J, Ryan, T, Zhang, A, and Wilcox, H. Systematic review of suicide prevention studies with data on youth and young adults living in low-income and middle-income countries. BMJ Open. (2022) 12:e055000. doi: 10.1136/bmjopen-2021-055000
36. Mo, PKH, Ko, TT, and Xin, MQ. School-based gatekeeper training programmes in enhancing gatekeepers’ cognitions and behaviours for adolescent suicide prevention: a systematic review. Child Adolesc Psychiatry Ment Health. (2018) 12:29. doi: 10.1186/s13034-018-0233-4
37. Brann, KL, Baker, D, Smith-Millman, MK, Watt, SJ, and DiOrio, C. A meta-analysis of suicide prevention programs for school-aged youth. Child Youth Serv Rev. (2021) 121:105826. doi: 10.1016/j.childyouth.2020.105826
38. Corcoran, J, Dattalo, P, Crowley, M, Brown, E, and Grindle, L. A systematic review of psychosocial interventions for suicidal adolescents. Child Youth Serv Rev. (2011) 33:2112–8. doi: 10.1016/j.childyouth.2011.06.017
39. Huang, R, Ding, L, and Huang, M. The Synopsis, influential factors and intervention of the non-suicidal self-injury behavior among the adolescences (in Chinese). Chin J Clin Psych. (2013) 21:965–7. doi: 10.16128/j.cnki.1005-3611.2013.06.008
40. Liu, X. Review on influencing factors and crisis intervention of suicide among adolescents (in Chinese). Chin J Prevent Control Chronic Diseases. (2011) 19:212–4. doi: 10.16386/j.cjpccd.issn.1004-6194.2011.02.001
41. Witt, KG, Hetrick, SE, Rajaram, G, Hazell, P, Taylor Salisbury, TL, Townsend, E, et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev. (2021) 3:CD013667:33677832. doi: 10.1002/14651858.CD013667.pub2
42. Cheng, Q, Zhang, X, Lui, C, and Yip, PSF. Suicide research in mainland China, Hong Kong, and Macau over three decades. Crisis. (2021) 42:455–64. doi: 10.1027/0227-5910/a000743
43. Mirjami Pelkonen LKaMM. Adolescent suicide: epidemiology, psychological theories, risk factors, and prevention. Curr Pediatr Rev. (2011) 7:52–67. doi: 10.2174/157339611795429080
44. Lin, M, Li, P, and Lu, Q. Current research status of non-suicidal self-injury in adolescents (in Chinese). J Psychiatry. (2018) 31:67–70. doi: 10.3969/j.jssn.2095-9346.2018.01.020
45. Zhou, X, and Jiang, W. Current research status on non-suicidal self- injury behavior among adolescents (in Chinese). J Psychiatry. (2021) 34:381–4. doi: 10.3969/j.issn.2095.9346.2021.04.024
46. Liu, RT, Scopelliti, KM, Pittman, SK, and Zamora, AS. Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry. (2018) 5:51–64. doi: 10.1016/S2215-0366(17)30469-8
47. Liang, J, and Liang, H. A review of the causes of NSSI in adolescents and the effects of intervention (in Chinese). Psychol Magazine. (2022) 17:220–2. doi: 10.19738/j.cnki.psy.2022.19.070
48. Wang, Y, He, W, Liang, L, Wen, H, Wang, H, and Huang, G. Application of dialectical behavior therapy in adolescents with non-suicidal self-injury behaviors (in Chinese). Sichuan Mental Health. (2021) 34:92–6. doi: 10.11886/scjsws20200915002
49. Liu, T, Wang, G, and Liu, T. Research on crisis intervention hotline intervention for adolescent suicide (in Chinese). World Latest Med Inform. (2022) 22:100–8. doi: 10.3969/j.issn.1671-3141.2022.015.024
50. Tang, C, and Li, Z. Interventional treatment for adolescent depression and suicide (in Chinese). Young Society. (2014) 550:61–2.
51. Macdonald, G, Livingstone, N, Hanratty, J, McCartan, C, Cotmore, R, Cary, M, et al. The effectiveness, acceptability and cost-effectiveness of psychosocial interventions for maltreated children and adolescents: an evidence synthesis. Health Technol Assess. (2016) 20:1–508. doi: 10.3310/hta20690 27678342
52. Leucht, S, Komossa, K, Rummel-Kluge, C, Corves, C, Hunger, H, Schmid, F, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. (2009) 166:152–63. doi: 10.1176/appi.ajp.2008.08030368
53. Jadad, AR, Moore, RA, Carroll, D, Jenkinson, C, Reynolds, DJ, Gavaghan, DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17:1–12. doi: 10.1016/0197-2456(95)00134-4
54. National Heart Lung and Blood Institute. Study quality assessment tools. (2021). Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Accessed August 17, 2023)
55. Li, M, Rao, W, Su, Y, Sul, Y, Caron, G, D'Arcy, C, et al. Psychological interventions for loneliness and social isolation among older adults during medical pandemics: a systematic review and meta-analysis. Age Ageing. (2023) 52:afad076. doi: 10.1093/ageing/afad076
56. Borenstein, M, Hedges, LV, Higgins, JP, and Rothstein, HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
57. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
58. Page, JM, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
59. Yang, R, Wei, Y, and Xiang, X. Intervention effect of gratitude diary combined with mindfulness training on non suicidal self injury behavior in adolescents (in Chinese). Nursing Integrat Trad Chin Western Med. (2021) 7:100–2.
60. Xie, H, Chu, J, Chen, Q, Zhang, M, and Xu, Y. The effect of group skills training on adolescents'non-suicidal self-injury self-injury and self-efficacy (in Chinese). Maternal Child Health Care China. (2022) 37:1704–7. doi: 10.19829/j.zgfybj.issn.1001-4411.2022.09.042
61. Wang, Y, Liang, J, Pan, J, Wang, X, Liao, Q, Li, R, et al. Application of adolescent cognitive behavior therapy in adolescent non-suicidal self-injury (in Chinese). Chin Evid Based Nurs. (2022) 8:1921–6. doi: 10.12102/j.issn.2095-8668.2022.14.015
62. Li, L. Intervention study on high-risk youth suicide (in Chinese). Hubei: Central China Normal University (2012).
63. Yang, J, Xie, B, Zhu, Z, Zhang, Q, Peng, Y, Han, H, et al. A school-based indicated prevention study for suicide in adolescents with high risk (in Chinese). Chin J Clin. (2012) 16:4704–14. doi: 10.3877/cma.j.issn.1674-0785.2012.16.042
64. Du, W. Analysis of psychological nursing countermeasures for non-suicidal self-injury patients (in Chinese). Womens Health. (2022) 51:159–60. doi: 10.3969/j.issn.1674-6074.2022.51.067
65. Ding, D. Study on the effect of object relations family therapy on nonsuicidal self-injury adolescents (in Chinese). Shandong: Shandong University Of Traditional Chinese Medicine (2021).
66. Chen, G, Zhou, H, and Zheng, M. Application of transference-focused psychotherapy combined with emotional regulation group intervention in the psychological intervention of adolescent patients with non-suicidal self-injury behaviors. Smart Healthcare. (2022) 8:213–7. doi: 10.19335/j.cnki.2096-1219.2022.26.051
67. Xia, S, and Shi, S. Effect of family participatory acceptance and commitment therapy on adolescents with non-suicidal self-injury. J Doctors. (2022):28.
68. Li, J. Intervention of emotion management group Counseling on non-suicidal self -injury (in Chinese). Hunan: Hunan Normal University (2016).
69. Liu, J. The personal risk factors for suicidal ideation and the effects of group psychological intervention in junior high students (in Chinese). Shandong: Shandong Normal University (2013).
70. Lin, Y. A study on the status of self-harm of senior high school students and the intervention of sandplay therapy (in Chinese). Jiangsu: Yangzhou University (2019).
71. Chang, X, Yuan, D, Xu, Y, Jin, X, Li, G, Shi, J, et al. Intervention study of suicidal ideation and depression for junior high school students (in Chinese). Chin J Health Psychol. (2015) 23:132–6. doi: 10.13342/j.cnki.cjhp.2015.01.038
72. Xie, H, Wang, Q, Sun, L, Zhou, D, Jia, Y, and Wang, Z. Psychosocial interventions affect on students with high risk of suicide (in Chinese). J Clin Psychiatry. (2014) 24:90–3.
73. Xue, Y. Research on the relationship between forgiveness tendency and self-injury behavior in junior high school students and intervention study (in Chinese). Anhui: Huaibei Normal University (2022).
74. Xue, Y, Zhou, X, Fan, Z, Wu, Q, and Liu, H. Application of family participatory acceptance and commitment therapy in the adolescent patients with non-suicidal self-injury (in Chinese). Chongqing Med. (2022) 51:1131–4. doi: 10.3969/j.issn.1671-8348.2022.07.010
75. Rong, J. Analysis of psychological nursing strategies for adolescent non suicidal self injury patients (in Chinese). Super Baby. (2020) 13:172.
76. Li, B. Analysis and intervention of non-suicidal self-injury in middle SCHOOI students (in Chinese). Jiangxi: Jiangxi Normal University (2016).
77. Halicka, J, and Kiejna, A. Non-suicidal self-injury (NSSI) and suicidal: criteria differentiation. Adv Clin Exp Med. (2018) 27:257–61. doi: 10.17219/acem/66353
78. Chen, H, Pan, B, Zhang, C, Guo, Y, Zhou, J, and Wang, X. Revision of the non-suicidal self-injury behavior scale for adolescents with mental disorder. J Central South Univ. (2022) 47:301–8. doi: 10.11817/j.issn.1672-7347.2022.210549
79. Xiang, Y-T, Li, W, Zhang, Q, Jin, Y, Rao, W-W, Zeng, L-N, et al. Timely research papers about COVID-19 in China. Lancet. (2020) 395:684–5. doi: 10.1016/s0140-6736(20)30375-5
80. Robinson, J, Bailey, E, Witt, K, Stefanac, N, Milner, A, Currier, D, et al. What works in youth suicide prevention? Syst Rev Meta-Analysis EClinicalMedicine. (2018) 4-5:52–91. doi: 10.1016/j.eclinm.2018.10.004
81. Kothgassner, OD, Robinson, K, Goreis, A, Ougrin, D, and Plener, PL. Does treatment method matter? A meta-analysis of the past 20 years of research on therapeutic interventions for self-harm and suicidal ideation in adolescents. Borderline Pers Disord Emot Dysregul. (2020) 7:9. doi: 10.1186/s40479-020-00123-9
82. Yuan, SNV, Kwok, KHR, and Ougrin, D. Treatment engagement in specific psychological treatment vs. treatment as usual for adolescents with self-harm: systematic review and meta-analysis. Front Psychol. (2019) 10:104. doi: 10.3389/fpsyg.2019.00104
83. Iyengar, U, Snowden, N, Asarnow, JR, Moran, P, Tranah, T, and Ougrin, D. A further look at therapeutic interventions for suicide attempts and self-harm in adolescents: An updated systematic review of randomized controlled trials. Front Psych. (2018) 9:583. doi: 10.3389/fpsyt.2018.00583 30532713
84. Hetrick, SE, Robinson, J, Spittal, MJ, and Carter, G. Effective psychological and psychosocial approaches to reduce repetition of self-harm: a systematic review, meta-analysis and meta-regression. BMJ Open. (2016) 6:e011024. doi: 10.1136/bmjopen-2016-011024
85. Dinh-Zarr, TB, Goss, CW, Heitman, E, Roberts, IG, and DiGuiseppi, C. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. (2004) 3:CD001857. doi: 10.1002/14651858.CD001857.pub2 CD001857
86. Jeong, H, Yim, HW, Lee, SY, Potenza, MN, and Kim, NJ. Effectiveness of psychotherapy on prevention of suicidal re-attempts in psychiatric emergencies: a systematic review and network Meta-analysis of randomized controlled trials. Psychother Psychosom. (2023) 92:152–61. doi: 10.1159/000529753
87. Hawton, K, Witt, KG, Taylor Salisbury, TL, Arensman, E, Gunnell, D, Hazell, P, et al. Psychosocial interventions for self-harm in adults. Cochrane Database Syst Rev. (2016) 5:CD012189. doi: 10.1002/14651858.CD012189
88. Witt, KG, Hetrick, SE, Rajaram, G, Hazell, P, Taylor Salisbury, TL, Townsend, E, et al. Psychosocial interventions for self-harm in adults. Cochrane Database Syst Rev. (2021) 4:CD013668. doi: 10.1002/14651858.CD013668.pub2 CD013668
89. Schäfer, SK, Thomas, LM, Lindner, S, and Lieb, K. World Health Organization's low-intensity psychosocial interventions: a systematic review and meta-analysis of the effects of problem management plus and step-by-step. World Psychiatry. (2023) 22:449–62. doi: 10.1002/wps.21129 37713578
90. Rodríguez-Rivas, ME, Cangas, AJ, Martin, A, Romo, J, Pérez, JC, Valdebenito, S, et al. Reducing stigma toward people with serious mental illness through a virtual reality intervention: a randomized controlled trial. Games Health J. (2023). doi: 10.1089/g4h.2023.0118
91. Farrell, SF, Edmunds, D, Fletcher, J, Martine, H, Mohamed, H, Liimatainen, J, et al. Effectiveness of psychological interventions delivered by physiotherapists in the management of neck pain: a systematic review with meta-analysis. Pain Rep. (2023) 8:e1076. doi: 10.1097/pr9.0000000000001076
92. Ownsworth, T, Fleming, J, Shum, D, Kuipers, P, and Strong, J. Comparison of individual, group and combined intervention formats in a randomized controlled trial for facilitating goal attainment and improving psychosocial function following acquired brain injury. J Rehabil Med. (2008) 40:81–8. doi: 10.2340/16501977-0124
93. Kennedy, BM, Paeratakul, S, Champagne, CM, Ryan, DH, Harsha, DW, McGee, B, et al. A pilot church-based weight loss program for African-American adults using church members as health educators: a comparison of individual and group intervention. Ethn Dis. (2005) 15:373–8.
94. Eagly, AH, and Revelle, W. Understanding the magnitude of psychological differences between women and Men requires seeing the Forest and the trees. Perspect Psychol Sci. (2022) 17:1339–58. doi: 10.1177/17456916211046006
95. Menon, V, and Vijayakumar, L. Interventions for attempted suicide. Curr Opin Psychiatry. (2022) 35:317–23. doi: 10.1097/yco.0000000000000807
96. Nahlén, BC. A meta-review of systematic reviews and meta-analyses on outcomes of psychosocial interventions in heart failure. Front Psych. (2023) 14:1095665. doi: 10.3389/fpsyt.2023.1095665 36970265
97. Biagianti, B, Foti, G, Di Liberto, A, Bressi, C, and Brambilla, P. CBT-informed psychological interventions for adult patients with anxiety and depression symptoms: a narrative review of digital treatment options. J Affect Disord. (2023) 325:682–94. doi: 10.1016/j.jad.2023.01.057
98. Belloni, S, Arrigoni, C, Arcidiacono, MA, Baroni, I, Conte, G, Dellafiore, F, et al. A systematic review of systematic reviews and pooled meta-analysis on psychosocial interventions for improving Cancer-related fatigue. Semin Oncol Nurs. (2023) 39:151354. doi: 10.1016/j.soncn.2022.151354 36379818
99. Sander, LB, Beisemann, M, Doebler, P, Micklitz, HM, Kerkhof, A, Cuijpers, P, et al. The effects of internet-based cognitive Behavioral therapy for suicidal ideation or behaviors on depression, anxiety, and hopelessness in individuals with suicidal ideation: systematic review and Meta-analysis of individual participant data. J Med Internet Res. (2023) 25:e46771. doi: 10.2196/46771
100. Torok, M, Han, J, Baker, S, Werner-Seidler, A, Wong, I, Larsen, ME, et al. Suicide prevention using self-guided digital interventions: a systematic review and meta-analysis of randomised controlled trials. Lancet Digit Health. (2020) 2:e25–36. doi: 10.1016/s2589-7500(19)30199-2
101. Elyoseph, Z, and Levkovich, I. Beyond human expertise: the promise and limitations of ChatGPT in suicide risk assessment. Front Psych. (2023) 14:1213141. doi: 10.3389/fpsyt.2023
102. Schnell, K, and Stein, M. Diagnostics and therapy 24/7? Artificial intelligence as a challenge and opportunity in psychiatry and psychotherapy. Psychiatr Prax. (2021) 48:S5–S10. doi: 10.1055/a-1364-5565
103. Wang, C, Liu, S, Yang, H, Guo, J, Wu, Y, and Liu, J. Ethical considerations of using ChatGPT in health care. J Med Internet Res. (2023) 25:e48009. doi: 10.2196/48009
104. Minshawi, NF, Hurwitz, S, Morriss, D, and McDougle, CJ. Multidisciplinary assessment and treatment of self-injurious behavior in autism spectrum disorder and intellectual disability: integration of psychological and biological theory and approach. J Autism Dev Disord. (2015) 45:1541–68. doi: 10.1007/s10803-014-2307-3
105. Ding, OJ, and Kennedy, GJ. Understanding vulnerability to late-life suicide. Curr Psychiatry Rep. (2021) 23:58. doi: 10.1007/s11920-021-01268-2
Keywords: psychosocial intervention, suicide, self-injurious behavior, adolescent, China
Citation: Lu J, Gao W, Wang Z, Yang N, Pang WIP, In Lok GK and Rao W (2023) Psychosocial interventions for suicidal and self-injurious-related behaviors among adolescents: a systematic review and meta-analysis of Chinese practices. Front. Public Health. 11:1281696. doi: 10.3389/fpubh.2023.1281696
Edited by:
Rasmieh Al-amer, Western Sydney University, AustraliaReviewed by:
Rafael Fernandez Castillo, University of Granada, SpainM. David Rudd, University of Memphis, United States
Copyright © 2023 Lu, Gao, Wang, Yang, Pang, In Lok and Rao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Grace Ka In Lok, a2lsb2tAbXB1LmVkdS5tbw==; Wenwang Rao, cmFvd3dAc3R1LmVkdS5jbg==
 Junjie Lu
Junjie Lu Wanting Gao1
Wanting Gao1 Zexin Wang
Zexin Wang Weng Ian Phoenix Pang
Weng Ian Phoenix Pang Wenwang Rao
Wenwang Rao