
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 October 2023
Sec. Environmental Health and Exposome
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1278516
This article is part of the Research Topic Synergistic Effects of Climate Change and Air Pollution on Health View all 13 articles
Background: Hand, foot, and mouth disease (HFMD) is a significant public health issue in China, and numerous studies have indicated a close association between HFMD incidence and meteorological factors. This study aims to investigate the relationship between meteorological factors and HFMD in Yangzhou City, Jiangsu Province, China.
Methods: HFMD case reports and meteorological data from Yangzhou City between 2017 and 2022 were extracted from the National Notifiable Infectious Disease Surveillance System and the Meteorological Data Sharing Service System, respectively. A generalized additive model (GAM) was employed to assess the exposure-response relationship between meteorological factors and HFMD. Subsequently, a distributed lag nonlinear model (DLNM) was used to explore the exposure-lag-effect of meteorological factors on HFMD.
Results: HFMD in Yangzhou City exhibits obvious seasonality and periodicity. There is an inverted “U” shaped relationship between average temperature and the risk of HFMD, with the maximum lag effect observed at a temperature of 25°C with lag 0 day (RR = 2.07, 95% CI: 1.74–2.47). As the duration of sunshine and relative humidity increase, the risk of HFMD continuously rises, with the maximum lag effect observed at a sunshine duration of 12.4 h with a lag of 14 days (RR = 2.10, 95% CI: 1.17–3.77), and a relative humidity of 28% with a lag of 14 days (RR = 1.21, 95% CI: 1.01–1.64). There is a “U” shaped relationship between average atmospheric pressure and the risk of HFMD, with the maximum effect observed at an atmospheric pressure of 989 hPa with no lag (RR = 1.45, 95% CI: 1.25–1.69). As precipitation increases, the risk of HFMD decreases, with the maximum effect observed at a precipitation of 151 mm with a lag of 14 days (RR = 1.45, 95% CI: 1.19–2.53).
Conclusion: Meteorological factors including average temperature, average atmospheric pressure, relative humidity, precipitation, and sunshine duration significantly influenced the risk of HFMD in Yangzhou City. Effective prevention measures for HFMD should be implemented, taking into account the local climate conditions.
Hand, foot, and mouth disease (HFMD) is an acute infectious disease caused by enteroviruses, primarily Coxsackievirus A16 (CV A16) and Enterovirus 71 (EV71). HFMD is characterized by the development of characteristic lesions on the hands, feet, and mouth. The transmission routes of HFMD mainly include contact transmission, respiratory transmission, and fecal-oral transmission. This disease predominantly affects children under the age of 5 (1, 2). The majority of patients with HFMD present with symptoms such as fever, as well as vesicular or popular eruptions on the hands, feet, and oral mucosa. The prognosis is generally favorable, with self-resolution occurring within approximately 1 week. However, a small proportion of patients may develop severe complications, including aseptic meningitis, encephalitis, pulmonary edema, and other severe manifestations. In rare cases, HFMD can progress to a critical condition and even result in death (3, 4). In recent years, the Asia-Pacific region has experienced frequent outbreaks of HFMD, posing a significant threat to the lives and health of children and adolescents in affected countries. These outbreaks have also imposed a substantial disease burden on the social and economic aspects of these nations (5–7).
Meteorological factors play a pivotal role in the transmission and epidemiology of infectious diseases, and they have been identified as significant risk factors contributing to the spread of HFMD (8–10), being a seasonal infectious disease, exhibits distinct patterns during specific periods in various regions and countries (11). Notably, several Asian countries, including Japan, Singapore, and mainland China, have observed a seasonal occurrence pattern of HFMD (12). Researchers from diverse countries and regions have conducted investigations on the influence of climate on HFMD, encompassing factors such as temperature, sunshine duration, relative humidity, wind speed, and precipitation. However, the findings from these studies exhibit some inconsistencies (13, 14). Analyzing the impact of meteorological factors on the incidence of HFMD can yield valuable insights for future prevention and control endeavors. The conclusions derived from such analyses can effectively guide the development of appropriate intervention measures.
It has been established that meteorological factors possess the capacity to exert a significant influence on the transmission and dissemination of HFMD, primarily by modulating the behavioral patterns of the pathogens or the hosts involved (15). The distributed lag nonlinear model (DLNM) can be employed to investigate the relationship between meteorological factors and HFMD. Meteorological factors such as temperature, humidity, and rainfall may exhibit certain associations with the incidence rate of HFMD. By utilizing the DLNM model, meteorological factors can be treated as independent variables, while the incidence rate of HFMD serves as the dependent variable. This model incorporates lag terms and nonlinear functions to capture the delayed effects of HFMD incidence and the nonlinear relationship with meteorological factors. The advantages of DLNM include its ability to address non-linear and delayed associations, such as exposure-lag-response, through cross-basis functions. Additionally, DLNM can automatically handle various regression function models such as linear models (LM), generalized linear models (GLM), and generalized additive models (GAM). A study conducted in Beijing utilizing a case-crossover design and DLNM revealed a non-linear relationship between temperature and hand, foot, and mouth disease (HFMD), indicating that the risk of HFMD increases with rising temperatures, with the highest risk observed at 25°C–27°C (16). Another study conducted in Sichuan Province using DLNM identified the interactive effects of meteorological factors and air pollutants on HFMD, highlighting that the combined presence of SO2 and high temperature and humidity exerted the strongest impact on HFMD (17). Laboratory and epidemiological research has also demonstrated the crucial role of humidity in the transmission of HFMD, with relative humidity accounting for over 84% of the impact on pediatric HFMD, and each 1% increase in relative humidity associated with a 0.34% increase in pediatric HFMD (18, 19). A study conducted in Vietnam demonstrated that an increase in average rainfall is associated with an increased risk of HFMD, an increase in 1 unit of rainfall was associated with a 0.5% increase of HFMD rate on the lag 1 and 6 days (20). A previous study indicated that diurnal temperature range altered the relationship between temperature and pediatric HFMD, with a higher diurnal temperature range associated with a greater risk of HFMD (21), another study found that climate indicators specific to certain cities, including temperature, sunshine duration, and atmospheric pressure, modified the relationship between relative humidity and HFMD, with an overall pooled humidity-HFMD relationship displaying an approximate U-shaped curve with substantial spatial heterogeneity (I2 = 77.8%), and a reference relative humidity of 70% associated with an RR value of 0.83 (22).
Since being classified as a Class C notifiable infectious disease in China in 2008 (23), HFMD has consistently ranked high in terms of reported cases and fatalities. The generalized additive model (GAM), a flexible and effective approach for parametric, non-parametric, and semi-parametric regression analysis, has been widely employed in time series studies and can be used to identify the relationships between meteorological factors and infectious diseases such as bacterial dysentery, mumps, and hemorrhagic fever with renal syndrome (24, 25).
In recent years, the incidence rate of HFMD in Yangzhou City has remained high, making it the leading notifiable infectious disease in the region (26). This study aims to describe the epidemiological trends of HFMD in Yangzhou City from 2017 to 2022. The GAM will be employed to explore the exposure-response relationship between meteorological factors and HFMD. Additionally, DLNM will be used to assess the exposure-lag-response effects of meteorological factors on HFMD.
Yangzhou, situated at the heart of Jiangsu Province, assumes a pivotal role in the advancement of the Yangtze River Economic Belt. Geographically, this city spans an expansive area of 6591.21 square kilometers and is demarcated into three districts, one county, and two county-level cities, as visually depicted in Figure 1. The climatic conditions in Yangzhou exhibit distinctive seasonal variations, characterized by copious precipitation, ample sunshine, and discernible shifts in wind patterns corresponding to the changing seasons. Notably, no reports have been documented regarding the influence of meteorological factors on HFMD and its predictive capabilities within the confines of Yangzhou. Consequently, it becomes imperative to comprehend the precise impact of meteorological factors on HFMD within the context of Yangzhou.
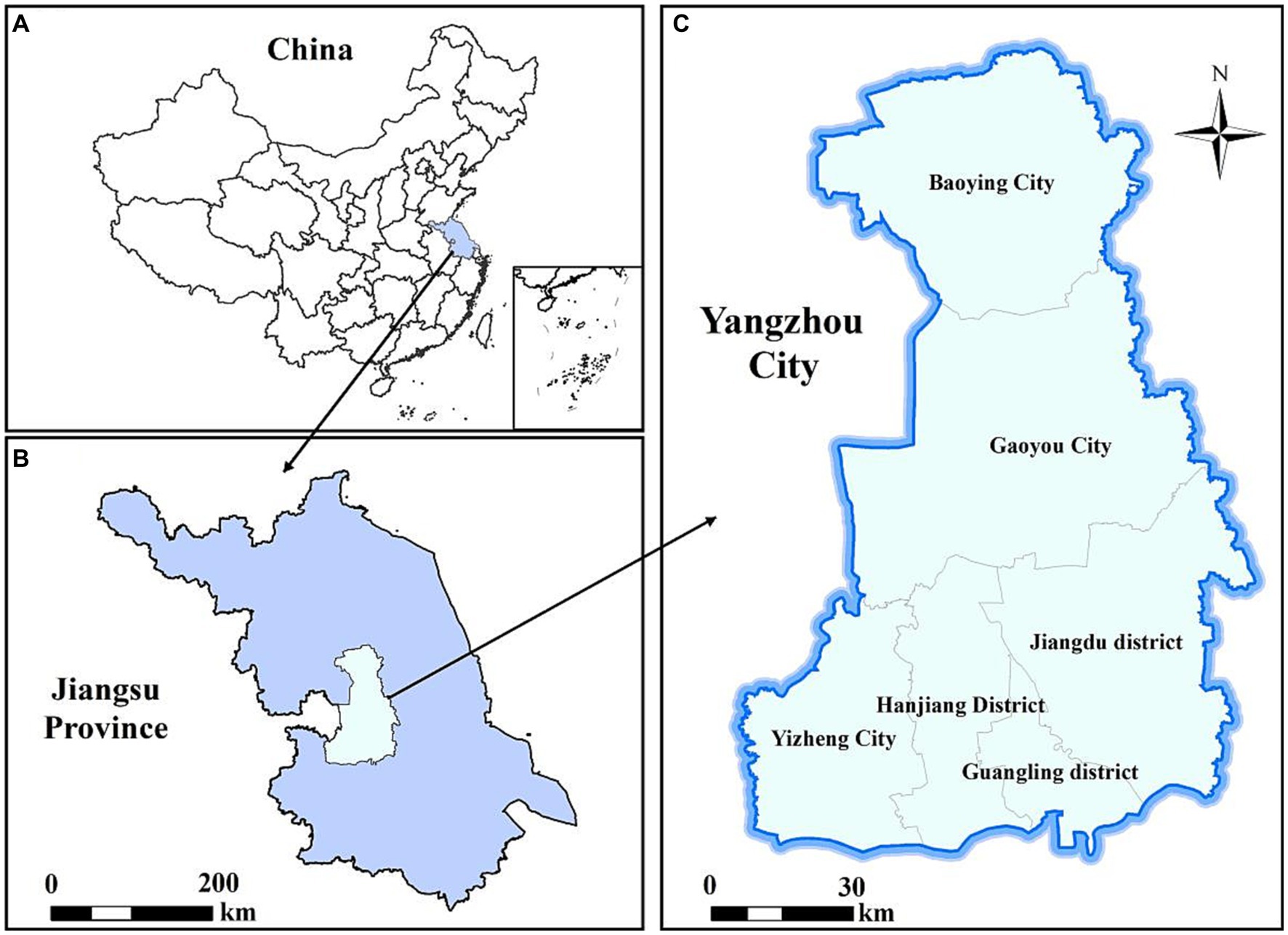
Figure 1. Geographical location of Yangzhou City, China. (A) China; (B) Jiangsu Province; (C) Yangzhou City.
The daily reported data on HFMD cases in Yangzhou City from 2017 to 2022 were obtained from the National Infectious Disease Information Monitoring and Reporting Management System. HFMD is classified as a Class C notifiable infectious disease, and all cases diagnosed by qualified doctors in hospitals at all levels nationwide are required to be reported through this system within 24 h. According to the HFMD diagnostic guidelines issued by the Chinese Ministry of Health, all HFMD cases are diagnosed based on clinical symptoms and laboratory test results. The information for each reported HFMD case includes a case number, gender, age, population category, date of onset, and residential address. The meteorological data used in this study was obtained from the China Meteorological Data Sharing Service System.1
Spearman’s rank correlation analysis is a non-parametric statistical method used to assess the correlation between two variables. The formula for Spearman’s rank correlation coefficient, denoted as rs, is as follows:
where rs represents the Spearman’s rank correlation coefficient, n represents the sample size, and di represents the difference in ranks between the two sets of data. The coefficient ranges from −1 to 1, where −1 indicates a perfect negative correlation, 0 indicates no correlation, and 1 indicates a perfect positive correlation. In this study, Spearman’s analysis was employed to evaluate the correlation between meteorological factors and the incidence rate of HFMD, in order to determine which meteorological factors may have an impact on the disease incidence rate.
Given the non-linear relationship between HFMD and meteorological factors, as well as the monthly periodicity of HFMD incidence, we applied a generalized additive model (GAM) to estimate the impact of meteorological parameters on monthly HFMD cases (27). GAM is helpful in determining the exposure-response relationships of various types of data, particularly when exploring non-parametric relationships (28). The dependent variable in this study is the cases of HFMD in Yangzhou city, which is a small probability event relative to the whole Yangzhou city population, and can be approximated as its obeying Poisson distribution, so the LOG function is chosen as the link function. In addition, as the spline function has strong ability to apply data and function transformation, and has certain overall smoothness, it is an ideal tool for function approximation, so the function corresponding to each independent variable in this study is set as the spline function, and the model is as follows:
Yt is the number of HFMD cases in month t; E(Yt) is the expected value of HFMD cases in month t; α is the constant term of the model; s() denotes the spline function; tl is used to control for long-term trends; ts is used to control for seasonal trends Xi denotes the independent variable (contemporaneous meteorological factors); df denotes the degrees of freedom on the spline function of the independent variable, obtained from generalized cross-validation.
It is used to quantitatively assess the “exposure-lag-effect” relationships between variables. The DLNM model builds upon the framework of traditional models by utilizing cross-basis functions, allowing for the simultaneous modeling of non-linear and lagged effects in exposure-response relationships. It has been widely employed in studying the associations between environmental exposures and infectious diseases (29). The model is as follows:
In the model, t represents the observation date, Yt represents the number of HFMD cases on day t, α represents the intercept, cb represents the cross-basis functions used to assess the non-linear relationship and lagged effects between meteorological factors and HFMD cases, ns represents natural cubic spline functions, M represents the study variables (various meteorological factors), Xi refers to other factors except M in the model to control the confounding effect. Time represents seasonal and long-term trends, and DOW refers to the day of the week effect. Based on the incubation period of HFMD and existing research (30, 31), set maximum lag days lag to 14.
From January 1, 2017, to December 31, 2022, a total of 23,652 cases of HFMD were reported in Yangzhou City. Among these cases, there were 13,858 male and 9,794 female patients. The annual reported cases were 5,935, 9,431, 4,437, 884, 1,765, and 1,200, exhibiting a pattern of “high-low” years. During the same period, the daily average temperature, atmospheric pressure, relative humidity, precipitation, and sunshine duration in Yangzhou City were 16.81°C (range: −6.5°C to −35.7°C), 1014.94 KPa (range: 999–1041.1 hPa), 74.19% (range: 28–100%), 2.83 mm (range: 0.1–156.2 mm), and 4.7 h (range: 0–12.6 h), respectively. Table 1 and Figure 2 summarize the basic information of HFMD cases and meteorological data. Figure 3 depicts the monthly distribution of HFMD cases in Yangzhou City.
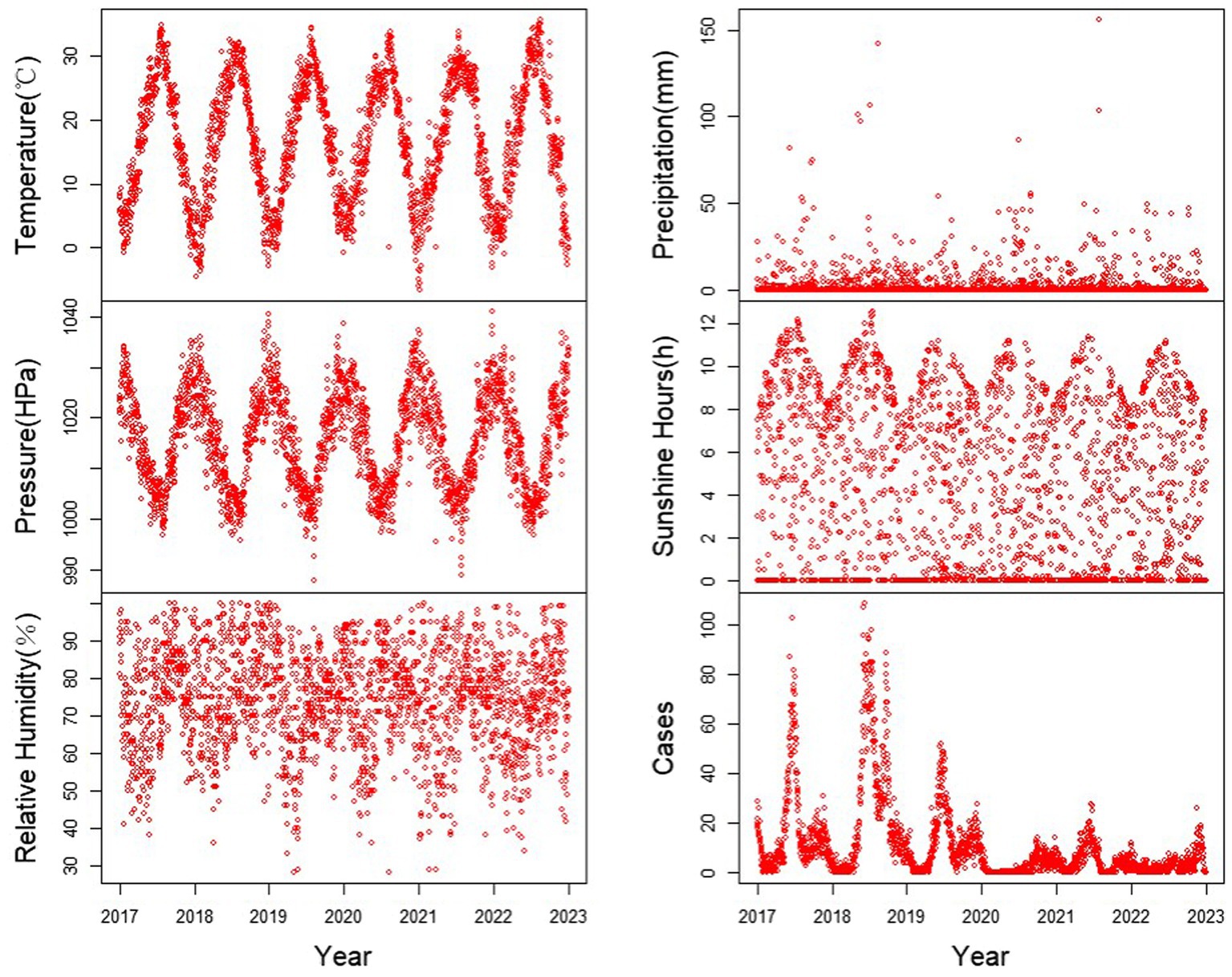
Figure 2. Time series of meteorological factors and number of HFMD cases in Yangzhou City, 2017–2022.
The Spearman correlation analysis matrix is presented in Table 2. In this study, temperature, relative humidity, precipitation, and sunshine duration showed positive correlations with the number of HFMD cases, while atmospheric pressure exhibited a negative correlation. Among these variables, temperature, atmospheric pressure, and precipitation were significantly correlated with HFMD cases (p < 0.05), while relative humidity and sunshine duration showed no statistically significant association (p > 0.05). Temperature had the highest correlation coefficient with HFMD cases (r = 0.37), followed by atmospheric pressure (r = −0.36).
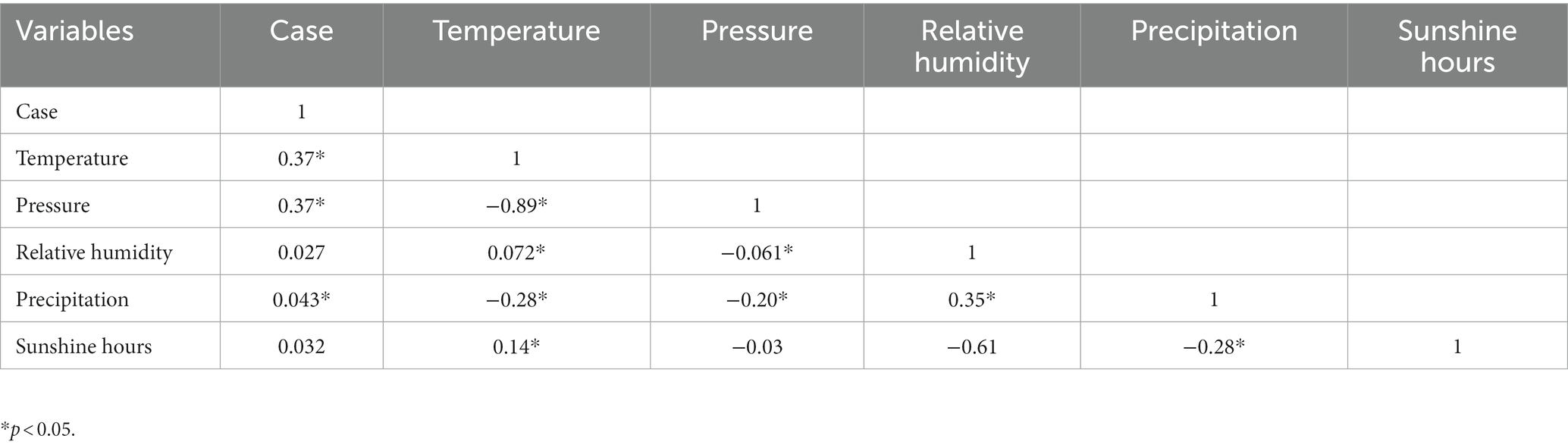
Table 2. Correlation analysis of meteorological factors, hand, foot and mouth disease cases in Yangzhou City.
The results of the generalized additive model are shown in Figure 4. It can be observed that temperature exhibits a “inverted U-shaped” relationship with the incidence rate of HFMD. As temperature increases, the risk of HFMD initially rises, reaching its peak around 17°C, and then decreases. Atmospheric pressure shows a “U-shaped” relationship with the incidence rate of HFMD. With increasing atmospheric pressure, the risk of HFMD initially decreases, reaching its lowest point around 1,016 KPa, and then increases again. Relative humidity and sunshine duration have similar response on the risk of HFMD, showing a predominantly linear relationship. As relative humidity and sunshine duration increase, the risk of HFMD also increases. On the other hand, the risk of HFMD decreases with increasing precipitation, which is contrary to the effects of relative humidity and sunshine duration.
We presented the exposure-lag-effect relationships between various meteorological factors and HFMD using a three-dimensional plot. Additionally, we depicted the cumulative effects at the maximum lag of 14 days (Figure 5).
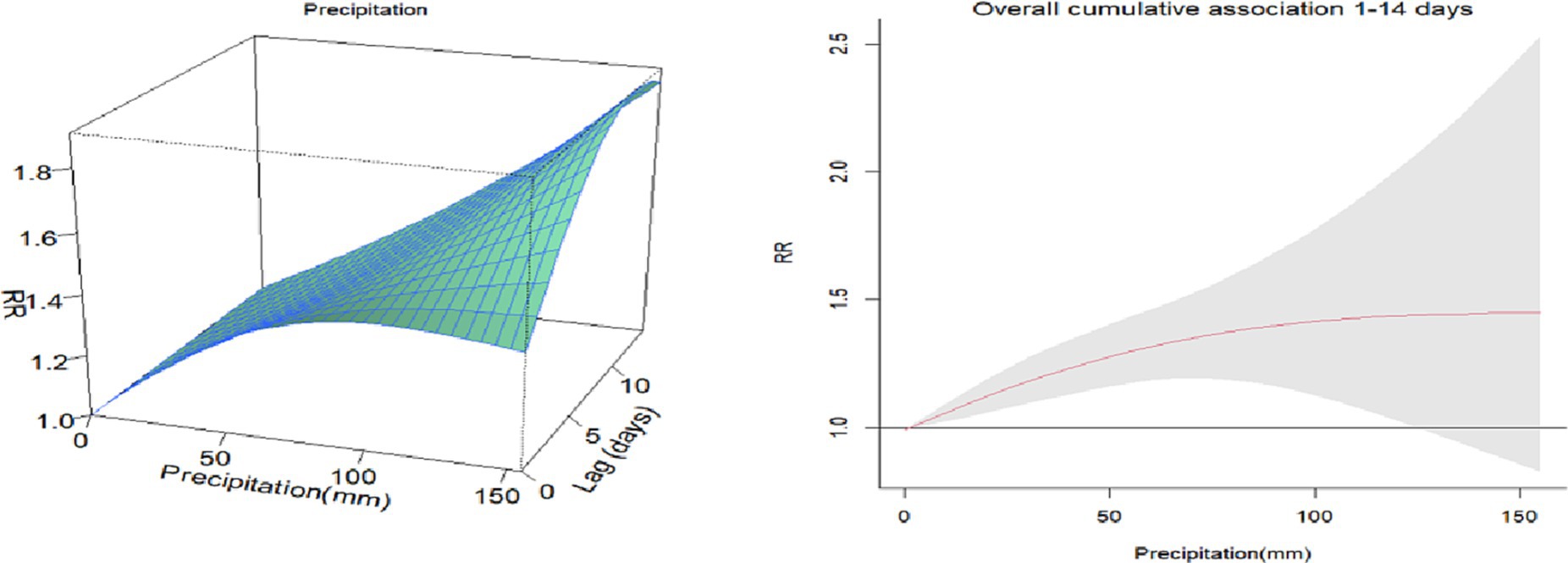
Figure 5. 3D plots and cumulative lag effect plots of the impacts of meteorological factors on the risk of HFMD.
The impact of temperature on HFMD at the maximum lag of 0 days showed that the highest relative risk (RR) value was observed at a temperature of −6°C (RR = 2.07, 95% CI: 1.74–2.47). Using the median temperature as the reference, the cumulative effect of temperature on HFMD approximately followed an inverted U-shaped curve. The maximum cumulative effect was observed at around 25°C (RR = 1.12, 95% CI: 1.05–1.23).
The impact of sunshine duration on HFMD at the maximum lag of 14 days was observed to be highest at 12.4 h (RR = 2.10, 95% CI: 1.17–3.77). Using the median sunshine duration as the reference, the cumulative effect of sunshine duration on HFMD gradually increased. The maximum cumulative effect was observed at 12.6 h of sunshine duration (RR = 2.08, 95% CI: 1.20–3.60).
The impact of relative humidity on HFMD at the maximum lag of 14 days was found to be highest at 28% (RR = 1.21, 95% CI: 1.01–1.64). Using the median relative humidity as the reference, the cumulative effect of relative humidity on HFMD exhibited an inverted U-shaped pattern. As relative humidity increased, the RR value initially increased and then decreased. The peak cumulative effect was observed at a relative humidity of 70% (RR = 2.01, 95% CI: 1.57–2.59).
The impact of atmospheric pressure on HFMD at the maximum lag of 0 days was found to be highest at 989 hPa (RR = 1.45, 95% CI: 1.25–1.69). Using the median atmospheric pressure as the reference, the cumulative effect of atmospheric pressure on HFMD gradually decreased. The maximum cumulative effect was observed at an atmospheric pressure of 990 hPa (RR = 3.79, 95% CI: 2.54–5.66).
The impact of precipitation on HFMD at the maximum lag of 14 days was found to be highest at 151 mm (RR = 1.90, 95% CI: 1.30–3.88). Using the median precipitation as the reference, the cumulative effect of precipitation on HFMD increased initially and then leveled off as precipitation … increased. The maximum cumulative effect was observed at a precipitation of 156 mm (RR = 1.45, 95% CI: 1.19–2.53).
Since its first reported case in New Zealand in 1957, HFMD has rapidly spread to most countries and regions worldwide. In China, HFMD has become a significant public health issue since 2008. The Chinese government has implemented a series of measures to address this problem, including strengthening surveillance and reporting systems, enhancing vaccine research and promotion, and improving public education and health campaigns. Despite some achievements, HFMD remains an important challenge in China, requiring continuous attention and efforts to combat it (32). The impact of meteorological factors on human health has received extensive attention and is closely associated with the occurrence and transmission of various infectious diseases (27, 33, 34). The aim of this study is to investigate the relationship between HFMD cases and meteorological factors, examining the impact of meteorological factors on HFMD from two temporal dimensions: monthly data and daily data.
We conducted an observational analysis of HFMD cases and meteorological data in Yangzhou City from 2017 to 2022. The study revealed that HFMD in Yangzhou City exhibits clear seasonality and periodicity, with a bimodal distribution: the onset of cases begins in May, with the first peak occurring in June and a smaller peak in August. Overall, HFMD has a higher incidence during the summer and autumn seasons, while it decreases during the winter and spring seasons. In terms of epidemic years, HFMD showed a high incidence from 2017 to 2019, followed by a decline likely influenced by the COVID-19 pandemic. These findings are consistent with studies conducted in other Provinces of China (35, 36).
The impact of meteorological factors on HFMD is believed to be influenced by the intricate interplay among the pathogen, environmental factors, and the host population (22). Our research findings have revealed a non-linear relationship, characterized by an “inverted U-shaped” curve, between the average temperature and the incidence of HFMD. This implies that the risk of HFMD tends to be lower at extremely low and high temperatures, while it is higher within the temperature range that is more conducive to disease transmission. The DLNM also revealed that the cumulative effect is highest at 25°C during the 14 days lag period. It is important to note that our research outcomes may diverge from studies conducted in other regions of China, where the relationship between average temperature and HFMD may exhibit an “M-shaped” pattern (37, 38). Moreover, we have also observed a positive correlation between relative humidity and the occurrence of HFMD. On one hand, in conditions of high relative humidity, the pathogens associated with HFMD may thrive, endure for longer durations, and exhibit heightened infectivity. On the other hand, elevated relative humidity can impede sweating and disrupt the metabolic processes in children. This finding aligns with research conducted in other regions of China.
Our study has also unveiled a U-shaped correlation between average atmospheric pressure and HFMD, albeit without the ability to definitively establish a causal relationship between the two. In terms of sunshine duration, our results show that there is a positive relationship between hand-foot-mouth disease and sunshine duration. As the duration of sunshine increases, the risk of HFMD escalates accordingly. It is worth noting that this conclusion contradicts the findings of other studies (39). Conversely, as precipitation levels rise, the risk of HFMD diminishes. This finding aligns with research conducted in other regions of China (40, 41). The reduced risk of HFMD with increased precipitation can plausibly be attributed to the unfavorable conditions for the survival of enteroviruses in high rainfall. Moreover, during periods of heavy precipitation, children may exhibit reduced inclination towards outdoor activities, thereby minimizing their exposure to the virus. Consequently, it is imperative to remain vigilant during periods characterized by high levels of sunshine duration and precipitation. The varying impact of meteorological factors on HFMD across different regions can be attributed to factors such as climate variations, disparities in viral strains, and divergent population behaviors among these regions (42).
This is the first study to explore the impact of meteorological conditions in Yangzhou City on the association with HFMD, expanding our understanding of the influence of meteorological factors on the risk of HFMD. Our research findings have practical implications in two aspects. Firstly, in the formulation of public health policies, our study results indicate that meteorological conditions affect the incidence rate of HFMD in Yangzhou City. For example, high rainfall and prolonged sunshine hours are associated with an increased incidence rate of HFMD, suggesting the need for different policies during the rainy season and dry season. Secondly, in the development of individual-level intervention measures, our research can serve as a reference. Children should develop healthy hygiene habits, such as washing hands before meals and after using the restroom. During HFMD outbreaks, parents or guardians should pay attention to reducing children’s outdoor activities. Additionally, it is necessary to check weather forecasts and air quality before going out.
However, this study has certain limitations. Firstly, time series analysis is an ecological study and may be susceptible to ecological fallacy. This study only focuses on the overall population and does not stratify by gender or pathogen. Secondly, the epidemic process of HFMD is influenced by both natural and social factors (43). Despite the paramount importance of meteorological factors in the transmission dynamics of HFMD, it is imperative to acknowledge that social behavior, economic factors, population mobility, and air quality may also exert significant influences on the occurrence and dissemination of the disease. Regrettably, our study did not encompass an examination of these multifaceted factors, thereby limiting the comprehensive understanding of the complex interplay between various determinants and the epidemiology of HFMD.
Meteorological factors such as average temperature, average atmospheric pressure, relative humidity, precipitation, and sunshine duration have a significant impact on the risk of HFMD in Yangzhou City. The relationship between average temperature and HFMD risk follows an inverted U-shaped pattern, while the relationship between average atmospheric pressure and HFMD risk exhibits a U-shaped pattern. The risk of HFMD continuously increases with increasing relative humidity and sunshine duration, while it gradually decreases with increasing precipitation, showing a negative correlation. Our study fills a research gap regarding the impact of meteorological factors on HFMD in Yangzhou City. These findings can provide scientific evidence for relevant authorities to implement preventive measures and offer practical recommendations for establishing an early warning and prevention system for infectious diseases.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
ZG: Writing – original draft, Writing – review & editing. YW: Data curation, Methodology, Project administration, Writing – original draft. YL: Conceptualization, Investigation, Software, Writing – review & editing. LZ: Funding acquisition, Validation, Writing – original draft, Writing – review & editing.
The author (s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Solomon, T , Lewthwaite, P , Perera, D , Cardosa, MJ , McMinn, P , and Ooi, MH . Virology, epidemiology, pathogenesis, and control of enterovirus 71. Lancet Infect Dis. (2010) 10:778–90. doi: 10.1016/s1473-3099(10)70194-8
2. Xing, W , Liao, Q , Viboud, C , Zhang, J , Sun, J , Wu, JT, et al. Hand, foot, and mouth disease in China, 2008–2012: an epidemiological study. Lancet Infect Dis. (2014) 14:308–18. doi: 10.1016/s1473-3099(13)70342-6
3. Liu, B , Luo, L , Yan, S , Wen, T , Bai, W , Li, H, et al. Clinical features for mild hand, foot and mouth disease in China. PLoS One. (2015) 10:e0135503. doi: 10.1371/journal.pone.0135503
4. Cai, K , Wang, Y , Guo, Z , Yu, H , Li, H , Zhang, L, et al. Clinical characteristics and managements of severe hand, foot and mouth disease caused by enterovirus A71 and coxsackievirus A16 in Shanghai. Infect Dis. (2019) 19:285. doi: 10.1186/s12879-019-3878-6
5. Puenpa, J , Wanlapakorn, N , Vongpunsawad, S , and Poovorawan, Y . The history of enterovirus A71 outbreaks and molecular epidemiology in the Asia-Pacific region. J Biomed Sci. (2019) 26:75. doi: 10.1186/s12929-019-0573-2
6. Sabanathan, S , Tan le, V , Thwaites, L , Wills, B , Qui, PT , and Rogier van Doorn, H . Enterovirus 71 related severe hand, foot and mouth disease outbreaks in South-East Asia: current situation and ongoing challenges. J Epidemiol Community Health. (2014) 68:500–2. doi: 10.1136/jech-2014-203836
7. Han, Y , Ji, H , Shen, W , Duan, C , Cui, T , Chen, L, et al. Disease burden in patients with severe hand, foot, and mouth disease in Jiangsu Province: a cross-sectional study. Hum Vaccin Immunother. (2022) 18:2049168. doi: 10.1080/21645515.2022.2049168
8. Grassly, NC , and Fraser, C . Seasonal infectious disease epidemiology. Proc Biol Sci. (2006) 273:2541–50. doi: 10.1098/rspb.2006.3604
9. Cherrie, MPC , Nichols, G , Iacono, GL , Sarran, C , Hajat, S , and Fleming, LE . Pathogen seasonality and links with weather in England and Wales: a big data time series analysis. BMC Public Health. (2018) 18:1067. doi: 10.1186/s12889-018-5931-6
10. Sumi, A , Toyoda, S , Kanou, K , Fujimoto, T , Mise, K , Kohei, Y, et al. Association between meteorological factors and reported cases of hand, foot, and mouth disease from 2000 to 2015 in Japan. Epidemiol Infect. (2017) 145:2896–911. doi: 10.1017/s0950268817001820
11. Koh, WM , Bogich, T , Siegel, K , Jin, J , Chong, EY , Tan, CY, et al. The epidemiology of hand, foot and mouth disease in Asia: a systematic review and analysis. Pediatr Infect Dis J. (2016) 35:e285–300. doi: 10.1097/inf.0000000000001242
12. Chen, Y , Badaruddin, H , Lee, VJ , Cutter, J , and Cook, AR . The effect of school closure on hand, foot, and mouth disease transmission in Singapore: a modeling approach. Am J Trop Med Hyg. (2018) 99:1625–32. doi: 10.4269/ajtmh.18-0099
13. Chen, S , Liu, X , Wu, Y , Xu, G , Zhang, X , Mei, S, et al. The application of meteorological data and search index data in improving the prediction of HFMD: a study of two cities in Guangdong Province, China. Sci Total Environ. (2019) 652:1013–21. doi: 10.1016/j.scitotenv.2018.10.304
14. Song, C , He, Y , Bo, Y , Wang, J , Ren, Z , and Yang, H . Risk assessment and mapping of hand, foot, and mouth disease at the county level in mainland China using spatiotemporal zero-inflated Bayesian hierarchical models. Int J Environ Res Public Health. (2018) 15:1476. doi: 10.3390/ijerph15071476
15. Cheng, Q , Bai, L , Zhang, Y , Zhang, H , Wang, S , Xie, M, et al. Ambient temperature, humidity and hand, foot, and mouth disease: a systematic review and meta-analysis. Sci Total Environ. (2018) 625:828–36. doi: 10.1016/j.scitotenv.2018.01.006
16. Xu, M , Yu, W , Tong, S , Jia, L , Liang, F , and Pan, X . Non-linear association between exposure to ambient temperature and Children’s hand-foot-and-mouth disease in Beijing, China. PLoS One. (2015) 10:e0126171. doi: 10.1371/journal.pone.0126171
17. Huang, J , Ma, Y , Lv, Q , Liu, Y , Zhang, T , Yin, F, et al. Interactive effects of meteorological factors and air pollutants on hand, foot, and mouth disease in Chengdu. BMJ Open. (2022) 12:e067127. doi: 10.1136/bmjopen-2022-067127
18. Yang, H , Wu, J , Cheng, J , Wang, X , Wen, L , Li, K, et al. Is high relative humidity associated with childhood hand, foot, and mouth disease in rural and urban areas? Public Health. (2017) 142:201–7. doi: 10.1016/j.puhe.2015.03.018
19. Abad, FX , Pintó, RM , and Bosch, A . Survival of enteric viruses on environmental fomites. Appl Environ Microbiol. (1994) 60:3704–10. doi: 10.1128/aem.60.10.3704-3710.1994
20. Nguyen, HX , Chu, C , Nguyen, HLT , Nguyen, HT , Do, CM , Rutherford, S, et al. Temporal and spatial analysis of hand, foot, and mouth disease in relation to climate factors: a study in the Mekong Delta region, Vietnam. Sci Total Environ. (2017) 581-582:766–72. doi: 10.1016/j.scitotenv.2017.01.006
21. Hu, Y , Liu, F , Zhao, X , Ma, Y , Lan, T , Yang, F, et al. The modification effect of the diurnal temperature range on the exposure-response relationship between temperature and pediatric hand. Sci Total Environ. (2020) 722:137921. doi: 10.1016/j.scitotenv.2020.137921
22. Bo, Z , Ma, Y , Chang, Z , Zhang, T , Liu, F , Zhao, X, et al. The spatial heterogeneity of the associations between relative humidity and pediatric hand. Sci Total Environ. (2020) 707:136103. doi: 10.1016/j.scitotenv.2019.136103
23. MoHotP China . Hand, foot and mouth disease prevention and control guide (2009). Available at: http://www.gov.cn/gzdt/2009-06/04/content_1332078.htm
24. Hao, J , Yang, Z , Huang, S , Yang, W , Zhu, Z , Tian, L, et al. The association between short-term exposure to ambient air pollution and the incidence of mumps in Wuhan. Environ Res. (2019) 177:108660. doi: 10.1016/j.envres.2019.108660
25. Gopalkrishna, V , Patil, PR , Patil, GP , and Chitambar, SD . Circulation of multiple enterovirus serotypes causing hand, foot and mouth disease in India. J Med Microbiol. (2012) 61:420–5. doi: 10.1099/jmm.0.036400-0
26. Liu, WJ , Zhou, LP , Dong, YY , Xu, CH , Cui, LB , and Wu, Q . Epidemiological characterization of hand, foot and mouth disease in Yangzhou City, China, 2014–2017. Chin J Health Inspec. (2019) 29:2272–5. doi: 10.3760/cma.j.cn112150-20200512-00721
27. Du, Z , Lawrence, WR , Zhang, W , Zhang, D , Yu, S , and Hao, Y . Interactions between climate factors and air pollution on daily HFMD cases: a time series study in Guangdong, China. Sci Total Environ. (2019) 656:1358–64. Epub 2019/01/11. doi: 10.1016/j.scitotenv.2018.11.391
28. Hastie, T , and Tibshirani, R . Generalized additive models for medical research. Stat Methods Med Res. (1995) 4:187–96. doi: 10.1177/096228029500400302
29. Gasparrini, A , Armstrong, B , and Kenward, MG . Distributed lag non-linear models. Stat Med. (2010) 29:2224–34. doi: 10.1002/sim.3940
30. Liu, Z , Meng, Y , Xiang, H , Lu, Y , and Liu, S . Association of short-term exposure to meteorological factors and risk of hand, foot, and mouth disease: a systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17:8017. doi: 10.3390/ijerph17218017
31. Xiao, X , Gasparrini, A , Huang, J , Liao, Q , Liu, F , Yin, F, et al. The exposure-response relationship between temperature and childhood hand, foot and mouth disease: a multicity study from mainland China. Environ Int. (2017) 100:102–9. doi: 10.1016/j.envint.2016.11.021
32. Zhu, L , Wang, X , Guo, Y , Xu, J , Xue, F , and Liu, Y . Assessment of temperature effect on childhood hand, foot and mouth disease incidence (0–5 years) and associated effect modifiers: a 17 cities study in Shandong Province, China, 2007–2012. Sci Total Environ. (2016) 551–552:452–9. doi: 10.1016/j.scitotenv.2016.01.173
33. Peng, L , Zhao, X , Tao, Y , Mi, S , Huang, J , and Zhang, Q . The effects of air pollution and meteorological factors on measles cases in Lanzhou. Environ Sci Pollut Res. (2020) 27:13524–33. doi: 10.1007/s11356-020-07903-4
34. Yu, G , Li, Y , Cai, J , Yu, D , Tang, J , Zhai, W, et al. Short-term effects of meteorological factors and air pollution on childhood hand-foot-mouth disease in Guilin, China. Sci Total Environ. (2019) 646:460–70. doi: 10.1016/j.scitotenv.2018.07.329
35. Hu, H , Ge, W , and Yan, J . Analysis of the epidemiologic characteristics of children with hand, foot and mouth disease in China. Iran J Public Health. (2023) 52:773–9. doi: 10.18502/ijph.v52i4.12450
36. Wang, W , Rosenberg, MW , Chen, H , Gong, S , Yang, M , and Deng, D . Epidemiological characteristics and spatiotemporal patterns of hand, foot, and mouth disease in Hubei, China from 2009 to 2019. PLoS One. (2023) 18:e0287539. doi: 10.1371/journal.pone.0287539
37. Qi, H , Chen, Y , Xu, D , Su, H , Zhan, L , Xu, Z, et al. Impact of meteorological factors on the incidence of childhood hand, foot, and mouth disease (HFMD) analyzed by DLNMs-based time series approach. Infect Dis Poverty. (2018) 7:7. doi: 10.1186/s40249-018-0388-5
38. Luan, G , Liu, S , Zhang, W , Zhai, L , Zhang, Y , Sun, L, et al. Estimating the influence of high temperature on hand, foot, and mouth disease incidence in China. Environ Sci Pollut Res Int. (2023) 30:1477–84. doi: 10.1007/s11356-022-22038-4
39. Xu, J , Yang, M , Zhao, Z , Wang, M , Guo, Z , Zhu, Y, et al. Meteorological factors and the transmissibility of hand, foot, and mouth disease in Xiamen City, China. Front Med. (2021) 7:597375. doi: 10.3389/fmed.2020.597375
40. Zhu, H , Chen, S , Liang, R , Feng, Y , Joldosh, A , Xie, Z, et al. Study of the influence of meteorological factors on HFMD and prediction based on the LSTM algorithm in Fuzhou. Infect Dis. (2023) 23:299. doi: 10.1186/s12879-023-08184-1
41. Wang, Y , Feng, Z , Yang, Y , Self, S , Gao, Y , Longini, IM, et al. Hand, foot, and mouth disease in China: patterns of spread and transmissibility. Epidemiology. (2011) 22:781–92. doi: 10.1097/EDE.0b013e318231d67a
42. Peng, H , Chen, Z , Cai, L , Liao, J , Zheng, K , Li, S, et al. Relationship between meteorological factors, air pollutants and hand, foot and mouth disease from 2014 to 2020. BMC Public Health. (2022) 22:998. doi: 10.1186/s12889-022-13365-9
Keywords: hand, foot and mouth disease, meteorological factors, generalized additive model, distributed lag nonlinear model, China
Citation: Guo Z, Wang Y, Li Y and Zhou L (2023) Impact of meteorological factors on the incidence of hand-foot-mouth disease in Yangzhou from 2017 to 2022: a time series study. Front. Public Health. 11:1278516. doi: 10.3389/fpubh.2023.1278516
Received: 16 August 2023; Accepted: 26 September 2023;
Published: 10 October 2023.
Edited by:
Zhaobin Sun, Chinese Academy of Meteorological Sciences, ChinaReviewed by:
Yike Shen, University of Texas at Arlington, United StatesCopyright © 2023 Guo, Wang, Li and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luojing Zhou, MTgwNTEwNjMwODhAeXp1LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.