
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 24 November 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1275010
Introduction: Leprosy remains a major public health concern worldwide and one of the leading causes of disability. New cases of leprosy with grade 2 disability (G2D) often reflect delayed detection due to the limited capacity of the health system to recognize leprosy early. This study aimed to describe the epidemiology and G2D of leprosy among migrant and resident patients with leprosy in Guangdong province, China.
Methods: Data on newly diagnosed cases of leprosy were collected from the leprosy management information system in China. Descriptive statistical analysis was used to describe the status of G2D. Joinpoint regression model and logistic regression were performed to analyze the temporal trends and influencing factors for G2D.
Results: The G2D rate among migrant, resident, and total patients with leprosy was 17.5%, 18.7%, and 18.4%, respectively. The total G2D rate increased significantly from 18.0% in 2001 to 25.7% in 2021 (average annual per cent change: 2.5%). Multivariate analysis revealed that factors that negatively influence G2D between migrant and resident patients included delayed discovery time (migrants: OR = 2.57; residents: OR = 4.99) and nerve damage when diagnosed (migrants: OR = 9.40; residents: OR = 21.28).
Discussion: Our findings indicate that the targeted intervention measures implemented by our health system are urgently needed to improve the current situation, such as programs to promote early detection, strengthen awareness and skills of healthcare workers, and rehabilitation for disabled patients to improve their quality of life.
Hansen’s disease or leprosy is a neglected tropical disease (NTD) mainly caused by Mycobacterium leprae, a slow-growing Mycobacterium discovered by Hansen, which predominantly affects the skin, peripheral nerves, mucous membranes, liver, and kidney (1, 2). In 2008, Mycobacterium lepromatosis was identified as a new species and the second causal agent of leprosy. However, M. lepromatosis has been implicated in a small number of leprosy cases, and the clinical aspects of leprosy caused by M. lepromatosis are poorly characterized (3). Since 1982, the World Health Organization (WHO) has recommended multi-drug therapy (MDT), which has been used to treat more than 15 million patients in the last 30 years and has made leprosy a curable disease (4).
Although MDT has reduced the number of cases in treatment, it had less impact on the number of new cases. Despite the availability of health facilities, there continue to be barriers to early diagnosis and treatment of leprosy. The lack of awareness of the disease among the general population and many consultations—suggestive of ill-trained health staff in suspecting and managing a leprosy case—were associated with a longer diagnostic delay, thus contributing to the ongoing transmission and disability-related disease burden (5). There were 202,185 new cases of leprosy worldwide, with a new case detection rate of 25.9 per million population in 2019 (6). In China, according to statistics released by the National Center for Leprosy Control, a total of 521 new cases of leprosy were detected, with a new case detection rate of 0.037 per 100,000 population in 2018 (7).
Guangdong province is the most severe leprosy epidemic area, with the highest number of cases in history; records showed that 96,797 people were affected by leprosy by 2020, representing approximately one-fifth of all leprosy patients in China. Regarding the new cases reported in 2018, Guangdong province ranked third in the number of new cases reported (57 cases), trailing Yunnan (174 cases) and Guizhou province (61 cases). These three provinces accounted for 56.0% of newly detected cases in China (7). The epidemic has the potential to be underestimated. There may be cases of oligosymptomatic leprosy with subclinical infection without diagnosis. This underdiagnosis may lead to underreporting to the leprosy surveillance system.
As the first province in China in terms of floating population and GDP, Guangdong province has great attraction and development potential in household registration immigration. According to the Guangdong Statistical Yearbook 2021, approximately 28.15 million migrants live in Guangdong province, representing 22.3% of the total permanent population (8). Movement can be a strategy to achieve a higher standard of living and access to better employment, education, and health service infrastructure, mainly among resource-poor rural areas and urban centers (9). Migration can lead to changes in circumstances that influence the conditions and risks associated with disease transmission, particularly among the poor, who are disproportionately affected (9, 10). Therefore, migration has been identified as one of the social determinants that influence the transmission dynamics of NTDs, including leprosy, which was identified as an infection risk factor associated with poverty (11, 12).
To improve our understanding of the epidemic situation of leprosy between migrant and resident populations, we detailed the demographic, clinical, geographic characteristics, and temporal trend of patients with leprosy in Guangdong province, China, 2001–2021. We also evaluated the status of grade 2 disability (G2D) and its associated influencing factors among migrant and resident patients with leprosy.
Information on newly diagnosed leprosy cases were collected from the leprosy management information system (LEPMIS) in China. LEPMIS was designed by the Chinese government in 2010 and reports data on new, recurrent, and prevalent cases of leprosy (13). LEPMIS includes not only related information on disease discovery, diagnosis, and treatment, but also information on all aspects of leprosy management, including basic demographic information, source of infection, close contacts, follow-up after cure, etc. Therefore, LEPMIS was a detailed and comprehensive database that achieved lifelong leprosy cases and even contained information on death. Data from patients with leprosy from 2001 to 2021 were collected from paper files and uploaded to LEPMIS by staff from municipal, county, and district-level professional leprosy prevention and control institutions. Oral consent was obtained from each participant before the interview and each participant could decline to participate in this survey at any step.
The diagnosis of new leprosy was based on the Leprosy Diagnosis Standard WS291-2018 (14). Patients with clinical manifestations (skin lesions or peripheral nerve lesions) and positive laboratory tests for leprosy (skin smear test for bacteria or histological examination) were diagnosed as confirmed cases. Disability classification was based on the Disability Classification Standard for Leprosy, WHO, 1998 (15). In 1988, the WHO Expert Committee on Leprosy substantially simplified the disability grading system into a three-grade (0, 1, and 2) classification system (16). Patients with G2D have visible deformities (i.e., hand ulcers, absorption or contractures of the digits, plantar ulcers, callosities, foot drop, or claw) or severe visual impairment (i.e., cannot read the fingers at a distance of 6 m). Patients with grade 1 disability have loss of sensation or eye problems (irregular blinking) due to the presence of leprosy, but no visible deformities, including muscle weakness without clawing. Nerve involvement in leprosy is considered to occur when there are signs of pain or nerve thickening on palpation of the nerves, when there is loss of sensation according to the monofilament test, or when motor impairment is observed (17). Patients with grade 0 disability have no loss of sensation, no visible deformity, and no eye problems due to leprosy. In 1997, the eighth report of the WHO Expert Committee on Leprosy endorsed this grading system with the amendment that lagophthalmos, iridocyclitis, and corneal opacities should be included in the grade 2 criteria (18).
Migrant patients with leprosy were defined as patients with leprosy who live in other places for work or live outside the county or municipal district where their registered permanent residence is located. The assignment of independent variables in the multivariate analysis was as follows: (1) age: 1, <30; 2, 30–44; 3, 45–59; 4, ≥60. (2) Sex: 1, female; 2, male. (3) Nationality: 1, others; 2, Han. (4) Occupation: 1, students; 2, workers or office staff; 3, unemployment or retiree; 4, farmers or herders. (5) Marriage status: 1, unmarried; 2, married; 3, divorced or widowed. (6) Delayed discovery time: 1, ≤24 months; 2, >24 months. (7) Skin lesion when diagnosed: 1, ≤5; ≥6. (8) Leprosy reaction: 1, no; 2, yes. (9) Nervous lesions when diagnosed: 1, 0; 2, 1; 3, ≥2. (10) Treatment classification: 1, paucibacillary (PB), including indeterminate (I), tuberculoid (TT), and borderline-tuberculoid (BT) cases with negative skin smear test for bacteria, skin lesions ≤5 and nerve lesion ≤1; 2, multibacillary (MB), including lepromatous (LL), borderline-lepromatous (BL), and mid-borderline (BB) cases with positive skin smear test for bacteria, or cases with negative skin smear test for bacteria but skin lesions ≥6 or nerve lesions ≥2, or cases with lesions ≥1 and also have characteristics of size, sensory, or morphological losses of advanced leprosy patients.
A newly diagnosed leprosy case database was established in Excel 2010 (Microsoft Corp., Redmond, WA, United States), and the data were cleaned by logical error detection. Statistical analyses, including descriptive statistical analysis, chi-square test, bivariate and multiple logistic regression analysis, were performed using IBM SPSS Statistics 24.0 (IBM Corp., Armonk, NY, United States). Basic descriptive analyses, including frequency, percentage, and mean (SD), were used to describe demographic and clinical characteristics. Geographic distribution analysis was performed using MapInfo Professional version 11.0 (Pitney Bowes Software Inc.). Joinpoint regression analysis was performed using the Joinpoint Regression Program version 4.9.1.0 (Statistical Research and Applications Branch, National Cancer Institute).
No personally identifiable information was included in the database used for the analysis. All data included in the study were stored on a removable hard disk and unauthorized access to them was not possible.
Of the 1980 newly diagnosed cases of leprosy registered during the study period, 452 (22.8%) were migrant patients, while 1,528 (77.2%) were resident patients. The proportion of migrant cases increased from 9.0% in 2001 to 45.7% in 2021 in Guangdong, China (Figure 1). Among the 452 migrant patients, 328 from other provinces were relatively close in location [top five provinces: Hunan (74), Guizhou (55), Sichuan (48), Jiangxi (38), and Guangxi (34)], 116 from other areas of Guangdong, four from Hongkong, three from Indonesia, and one from Mali. Among 1,980 patients with leprosy, 1,302 (65.8%) were males. The vast majority (94.9%) were Han nationality and 1,105 cases were farmers or herders, representing 58.7%. Between 2001 and 2021, the average age of newly diagnosed patients with leprosy in Guangdong was 43.1 (SD = 18.0) years. During this period, 51 cases of pediatric patients (aged <14 years) were detected, with a male-to-female ratio of 1:3 (Table 1).
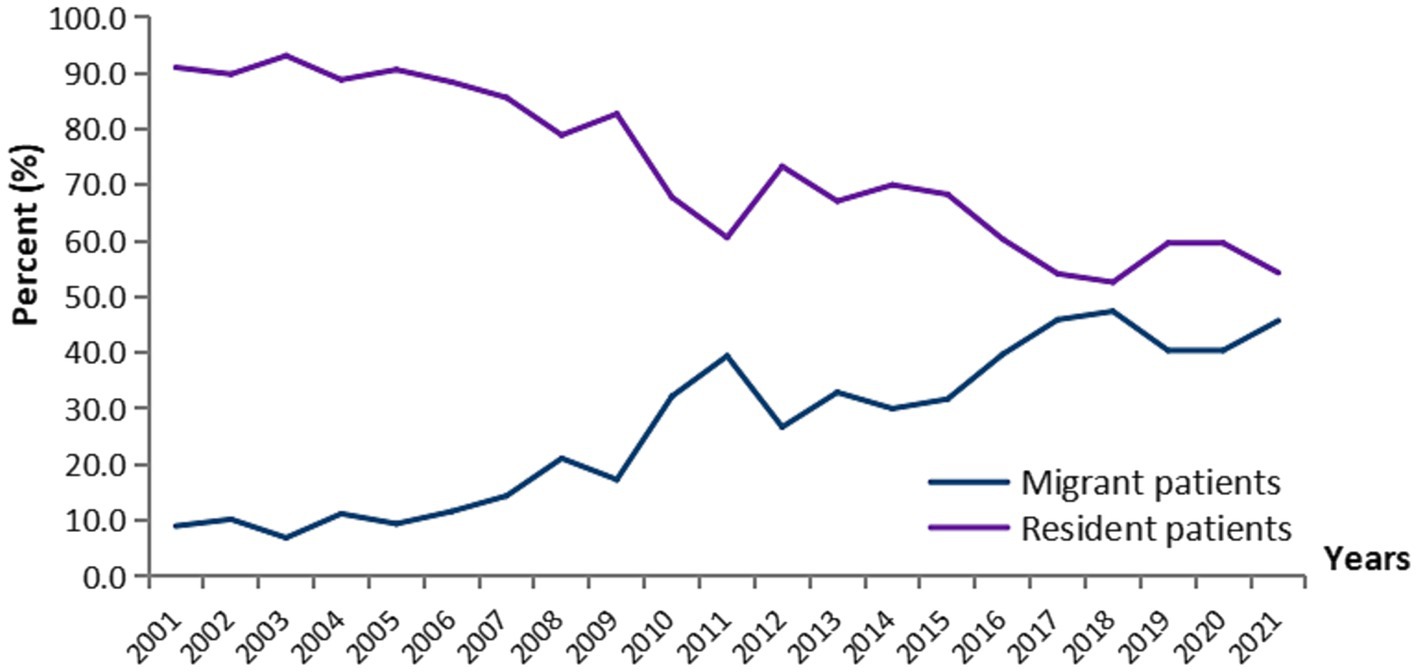
Figure 1. Trends of migrant and resident patients with leprosy in Guangdong province, China, 2001–2021.
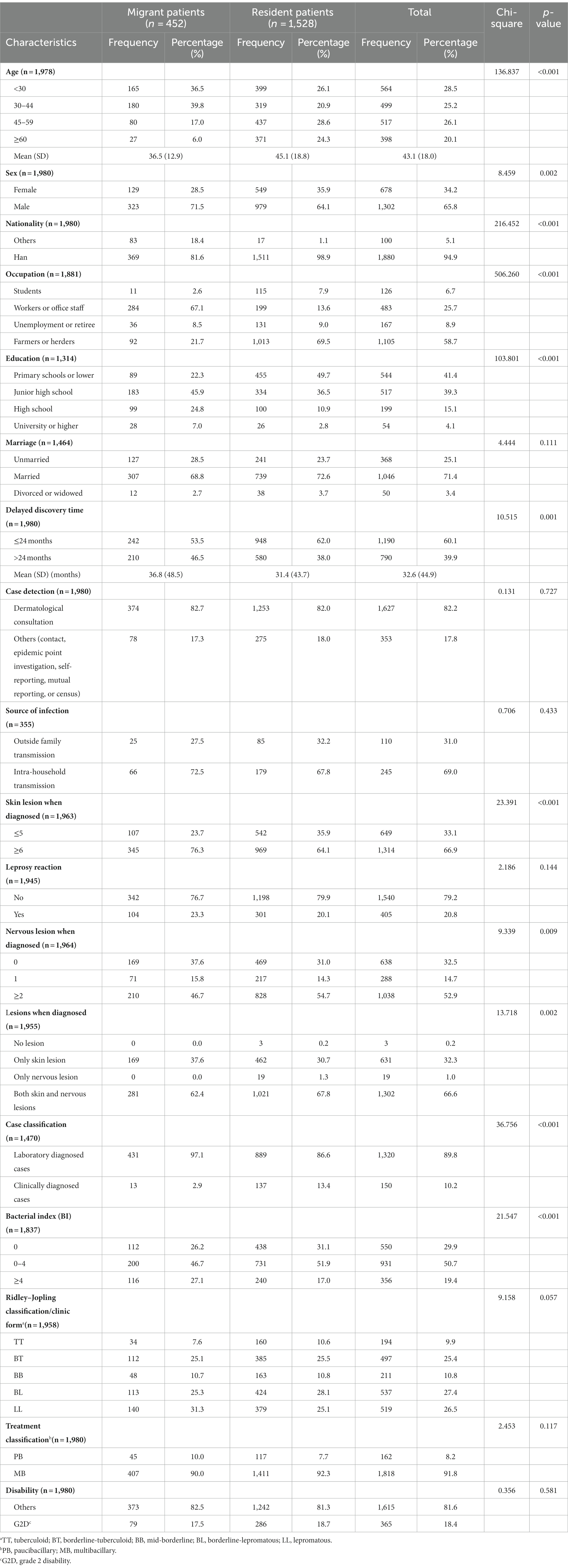
Table 1. Demographic and clinical characteristics of migrant and resident patients with leprosy in Guangdong, China, 2001–2021 (N = 1,980).
A total of 1,818 patients were diagnosed with MB leprosy, which represents 91.8%. According to Ridley–Jopling classification, patients with leprosy were more likely to be classified as having BL (537 patients, 27.4%), LL (519 patients, 26.5%), and BT (497 patients, 25.4%). Most patients have both skin lesions and nervous lesions (1,302 patients, 66.6%), and a positive skin smear test for bacteria [bacterial index (BI) >0: 1,287 patients, 70.1%] when diagnosed.
The results of the chi-square test showed that there was a significant difference between migrant and resident patients from different groups of age, sex, nationality, occupation, education, delayed discovery time, skin lesions when diagnosed, nervous lesions when diagnosed, case classification, and BI (p < 0.05) (Table 1).
The G2D rate of newly diagnosed migrant leprosy patients was 17.5% between 2001 and 2021, ranging from 0 (Chaozhou and the other six cities) to 50.0% in Heyuan (northern Guangdong) (Figure 2). In contrast, the rate of G2D of newly diagnosed resident patients with leprosy was 18.7 between 2001 and 2021, ranging from 9.5% in Chaozhou (eastern Guangdong) to 32.4% in Shaoguan (northern Guangdong) (Figure 2).
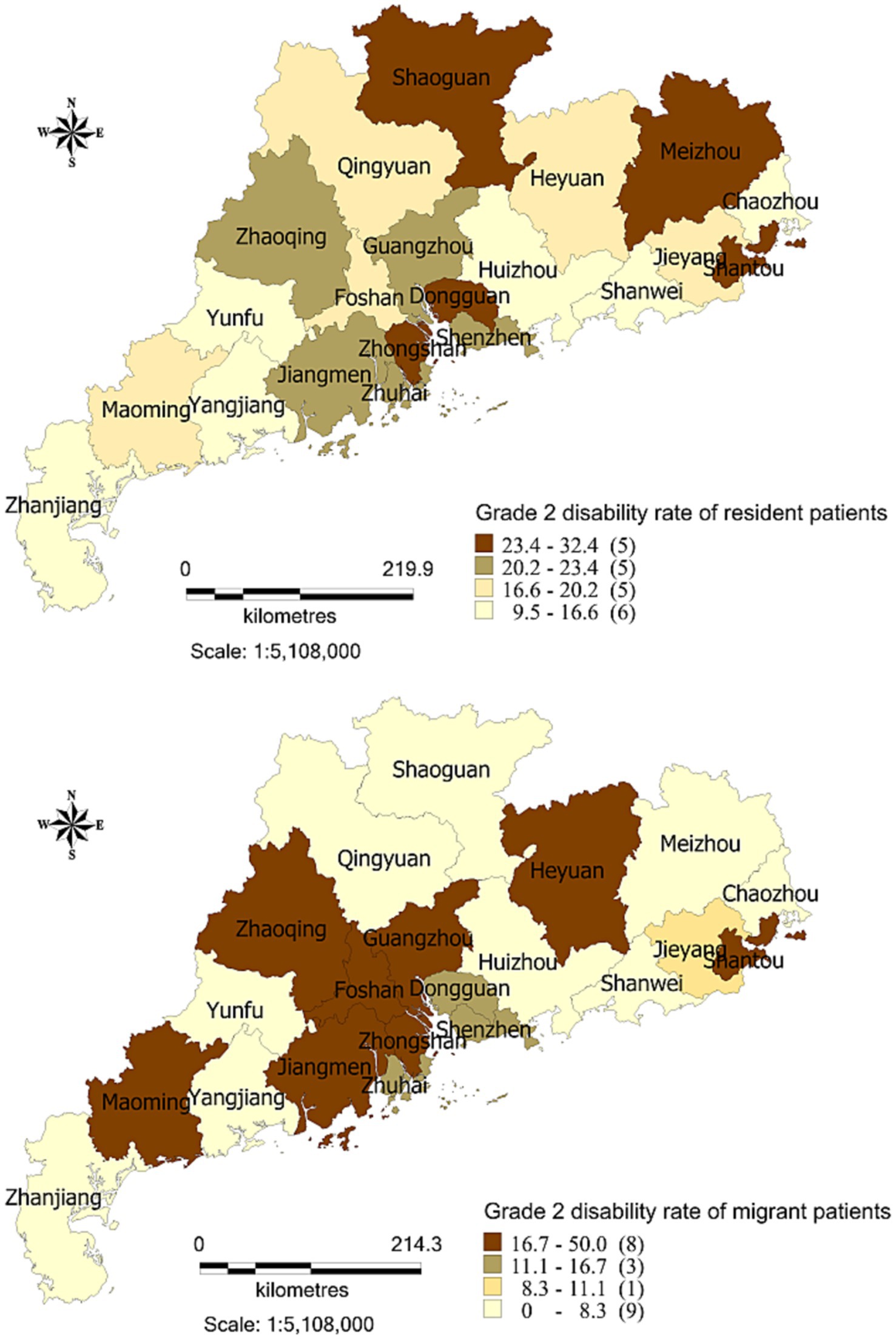
Figure 2. Geography distribution of the grade 2 disability rate between migrant and resident patients with leprosy in Guangdong province, China, 2001–2021.
Throughout the 21-year period, the G2D rate increased significantly over time, from 18.0% in 2001 to 25.7% in 2021 [average annual per cent change (AAPC) 2.5, 95% CI: 1.0–3.9]. Among 1,528 resident patients, 286 cases of leprosy with G2D were reported; the G2D rate also increased significantly over time from 12.7% in 2005 to 36.8% in 2021 (AAPC 5.0, 95% CI: 3.5–6.6) (Table 2).
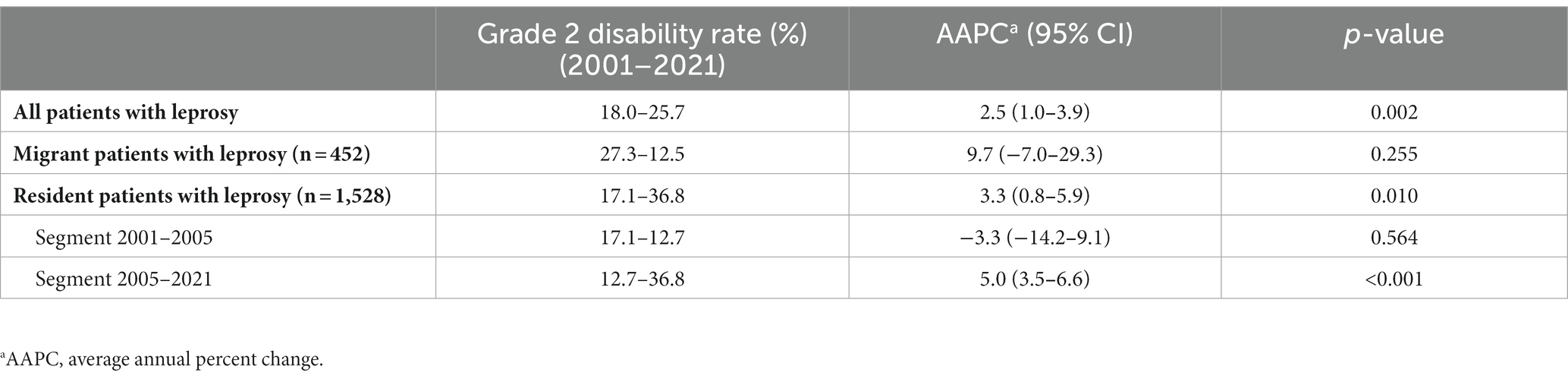
Table 2. Joinpoint regression analysis of the trend for grade 2 disability rate among migrant and resident leprosy patients in Guangdong province, China, 2001–2021 (N = 1,980).
Univariate logistic regression analysis showed that age (≥60, migrant: OR = 3.50, 95% CI: 1.24–9.89; resident: OR = 2.25, 95% CI: 1.56–3.24), delayed discovery time (>24 months, migrant: OR = 3.46, 95% CI: 2.04–5.87; resident: OR = 3.78, 95% CI: 2.89–4.95), nerve lesions when diagnosed (≥2, migrant: OR = 11.38, 95% CI:4.78–27.08; resident: OR = 15.73, 95% CI: 8.70–28.44), and treatment classification (MB, migrant: OR = 10.42, 95% CI: 1.41–76.88; resident: OR = 7.06, 95% CI: 2.58–19.29) were the influencing factors for G2D for both migrant and resident patients with leprosy (Table 3).
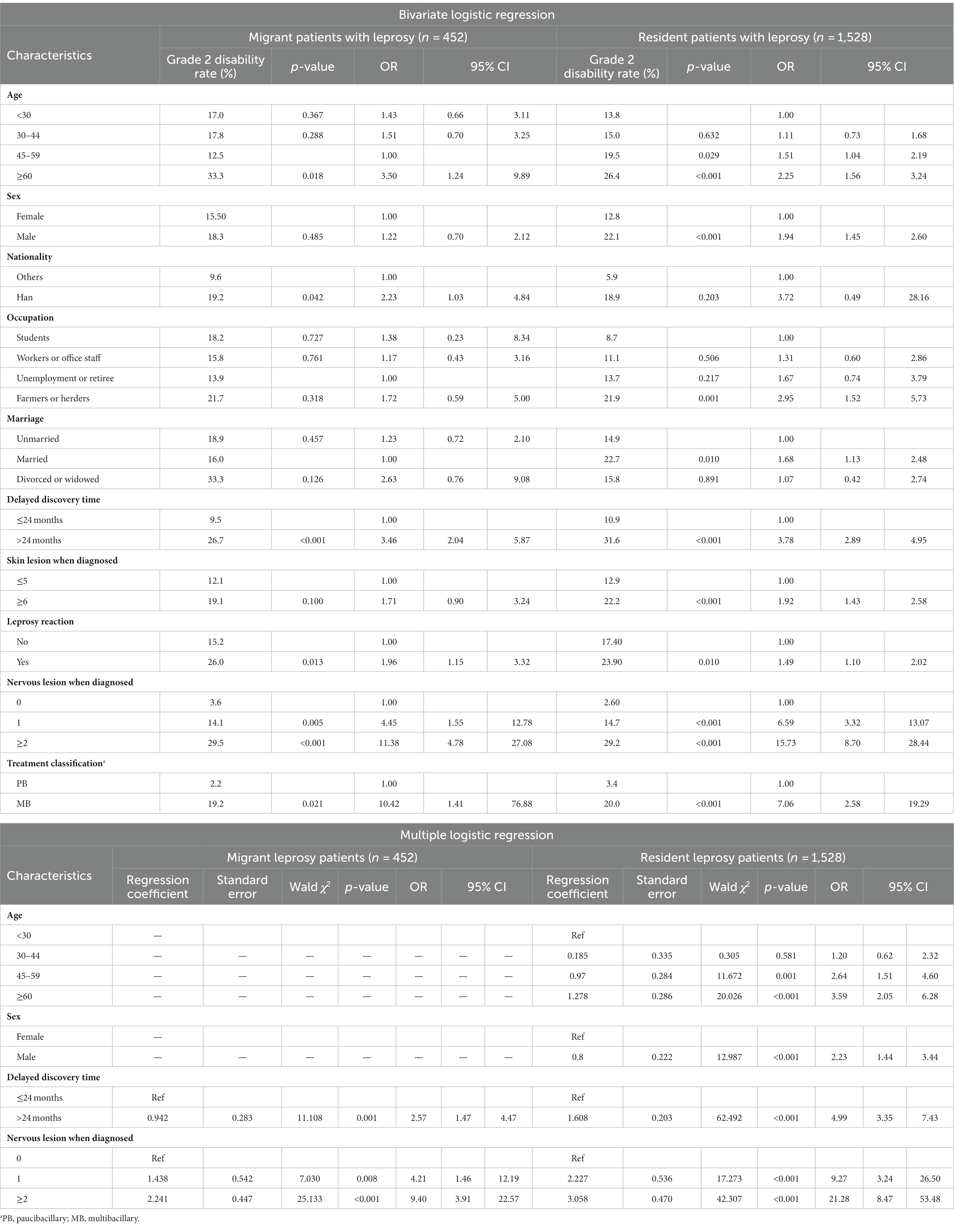
Table 3. Bivariate and multiple logistic regression analysis of grade 2 disability among migrant and resident patients with leprosy in Guangdong province, China, 2001–2021 (N = 1,980).
Multivariate analysis revealed that factors that influence G2D in migrant patients with leprosy were the delayed discovery time (>24 months, OR = 2.57, 95% CI: 1.47–4.47), and nerve damage when diagnosed (≥2, OR = 9.40, 95% CI: 3.91–22.57). Meanwhile, in resident patients with leprosy, the influencing factors for G2D were age [≥60, OR = 3.59, 95% CI: 2.05–6.28, sex (male, OR = 2.23, 95% CI: 1.44–3.44)], delayed discovery time (>24 months, OR = 4.99, 95% CI: 2.35–7.43), and nerve lesion when diagnosed (≥2, OR = 21.28, 95% CI: 8.47–53.48) (Table 3).
With the worldwide implementation of WHO MDT in the 1980s, the global burden of leprosy has decreased. However, a certain number of new patients with leprosy with G2D are still found when diagnosed, reflecting a failure in early detection of leprosy and indicating that transmission continues (19). Of the 121 countries that submitted data to the WHO on G2D in 2020, 68 countries reported 7,198 new G2D cases, which represents 5.7% of 127,396 new cases of leprosy worldwide (20). Although leprosy has a steadily low prevalence in China, the rate of G2D among new cases of leprosy was 17.7% in 2020, while our research showed that the rate of G2D was 18.4% in Guangdong province, China, between 2001 and 2021. Although leprosy cases with G2D have been diagnosed and reported, cases of oligosymptomatic leprosy with subclinical infection can easily be overlooked. Therefore, it leads to underdiagnosis, underreporting to the surveillance system, and an underestimation of the leprosy epidemic.
Leprosy remains one of the leading causes of deformity and physical disability. Our study showed the same influencing factors for G2D among migrant and resident patients with leprosy, including delayed discovery and nervous lesions when diagnosed. The burden of leprosy G2D in new cases often indicates a delayed detection, often due to a lack of awareness in the community of early signs of leprosy, a delay in seeking care, or the limited capacity of the health system to recognize leprosy early (20). Srinivas et al. (21) found that delayed diagnosis is a major challenge in the leprosy program in India. Patient delay and healthcare provider delay have been significant risk factors for disability among adult cases of leprosy. Moreover, since a large proportion of cases with disabilities ignored initial symptoms as they believed that symptoms would disappear by themselves, patient delay became the main reason for the risk of disability.
Nervous lesions when diagnosed were another influencing factor for G2D among migrant and resident patients with leprosy. Due to bacterial proliferation or the immunologic response of the host to these bacilli or both, there is some degree of irreversible peripheral nerve damage in virtually all patients with leprosy. If not treated effectively, widespread destruction of the mixed peripheral nerve trunks can result in widespread skin anesthesia and widespread permanent muscle paralysis that affects the face, hands, and feet (22). Meanwhile, peripheral nerve trunks remove the sensation of pain. The lack of pain feedback allows patients with leprosy to damage and deform themselves. Most of the deformities attributed to leprosy are caused by this secondary damage (1).
Of the 1,980 cases of leprosy registered during the study period, 452 (22.8%) were migrant patients. Similarly to our previous research, the migrant cases originated mainly from two areas: the provinces surrounding Guangdong (Hunan and Jiangxi) and the southwestern provinces (Guizhou, Sichuan, and Guangxi), which have the highest incidence of leprosy in China (23). Due to the long incubation period of leprosy and the failure of current testing method to detect leprosy early, these migrants were identified and treated only after they migrated to Guangdong province, thus resulted in continued transmission between provinces in Chinese territory. We also found that the G2D rate among migrant patients with leprosy was 17.5%, which is related to delayed discovery and nervous lesions. Early diagnosis of leprosy can lead to breaking the chain of transmission and reducing the number of G2D cases (24, 25). Thus, the key point of resolve epidemiological problem is to fix the inability to diagnose in early period of leprosy. However, an accurate and timely diagnosis of the disease is still a challenge (26). Skin slit smear acid-fast staining is rapid and economic but has very low sensitivity and specificity. Definitive diagnosis of leprosy by clinic and pathological features requires experienced physicians. Quantitative polymerase chain reaction (qPCR) holds promise as a simple and sensitive diagnostic tool, but the infrastructure, such as equipment and trained professionals, is still a barrier to implementing qPCR in resource-limited settings (27). Early diagnosis and followed by effective treatment is crucial to avoiding continued transmission and controlling the disease, the need for more accurate tools for the detection and confirmation of leprosy among suspected individuals and more effective treatment regimens are indeed urgent.
Our study also found that all migrant patients with leprosy had skin or nervous lesion when diagnosed, nearly one quarter had leprosy reactions, and about one fifth had visible deformities. The pronounced damage and permanent disabilities frequently caused patients with leprosy to suffer stigma and prejudice. The management of migrant patients with leprosy has been an important issue for current leprosy prevention and control. Possible reasons for this are that patients with leprosy may fear discrimination to seek medical care. Otherwise, changing job and address frequently reduced the convenience to professional leprosy prevention and control institutions for treatment because of more time and transportation cost.
There are some limitations to this study. First, this study is a cross-sectional study, therefore, we were unable to draw causal inferences. Second, the clinical histories of some participants were incomplete due to the loss of records throughout the 21 years period, and the information of treatment classification was collected from LEPMIS which followed the instruction of WHO-MDT classification of leprosy treatment and the Leprosy Diagnosis Standard WS291-2018 in China, which may outdated and reduces the complexity of the disease. Third, although patients claim that their current address is the place where they live, work, and receive treatment, we cannot exclude individuals who work only in places other than their municipality as migrants. Furthermore, it is not known whether the infection occurred at the place of primary residence or at the present address due to the long incubation period of leprosy.
To reduce delay and promote early diagnosis, we have implemented leprosy symptom monitoring programs in Guangdong province since 2017. We propose eight early symptoms of leprosy. If doctors in medical institutions find suspected cases of leprosy, the cases can be referred to a local leprosy-designated diagnosis and treatment center for professional diagnosis and treatment through the “Guangdong Suspected Leprosy Symptom Monitoring System.” However, this is not enough; early case detection campaigns, such as active surveys in endemic areas, should be carried out periodically (21). Furthermore, continuing education programs for healthcare workers and the community should also place greater emphasis on raising awareness of the disease (19). Meanwhile, disability prevention and rehabilitation, even after effective treatment, remain essential for patients with leprosy with deformity to improve their quality of life, which is why we plan to establish a provincial-level leprosy correction surgery and rehabilitation center in the future.
The data analyzed in this study is subject to the following licenses/restrictions: Leprosy Control Department of Dermatology Hospital, Southern Medical University. Requests to access these datasets should be directed to XW, V3hoXzIxNzczQDE2My5jb20=.
The studies involving humans were approved by Medical Ethics Committee of Dermatology Hospital of Southern Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
LC: Writing – original draft, Data curation. DZ: Writing – review & editing. ML: Writing – review & editing. MZ: Writing – review & editing. BY: Writing – review & editing. XW: Conceptualization, Funding acquisition, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Medical Science and Technology Foundation of Guangdong Province (C2021061); Guangzhou Municipal Science and Technology Project (202102080056).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hastings, RC, Gillis, TP, Krahenbuhl, JL, and Franzblau, SG. Leprosy. Clin Microbiol Rev. (1988) 1:330–48. doi: 10.1128/CMR.1.3.330
2. Chhabra, N, Grover, C, Singal, A, Bhattacharya, SN, and Kaur, R. Leprosy scenario at a tertiary level hospital in Delhi: a 5 years retrospective study. Indian J Dermatol. (2015) 60:55–9. doi: 10.4103/0019-5154.147793
3. Deps, P, and Collin, SM. Mycobacterium lepromatosis as a second agent of Hansen’s disease. Front Microbiol. (2021) 12:698588. doi: 10.3389/fmicb.2021.698588
4. Noordeen, SK . History of chemotherapy of leprosy. Clin Dermatol. (2016) 34:32–6. doi: 10.1016/j.clindermatol.2015.10.016
5. Gomez, L, Rivera, A, Vidal, Y, Bilbao, J, Kasang, C, Parisi, S, et al. Factors associated with the delay of diagnosis of leprosy in northeastern Colombia: a quantitative analysis. Trop Med Int Health. (2018) 23:193–8. doi: 10.1111/tmi.13023
6. World Health Organization . Global leprosy (Hansen disease) update, 2019: time to step-up prevention initiatives. Geneva: World Health Organization (2019). p. 389–412.
7. Le, W, Wen, SP, Wen, YM, Heng, G, Sheng, WH, and Sheng, CX. Epidemiological characteristics of leprosy in China, 2018. Int J Dermatol Venereol. (2020) 3:27–30. doi: 10.1097/JD9.0000000000000065
8. Statistics Bureau of Guangdong Province . Guangdong statistical yearbook. Guangzhou: Statistics Bureau of Guangdong Province (2021).
9. Murto, C, Kaplan, C, Ariza, L, Schwarz, K, Alencar, CH, Da, CL, et al. Factors associated with migration in individuals affected by leprosy, Maranhão, Brazil: an exploratory cross-sectional study. J Trop Med. (2013) 2013:495076. doi: 10.1155/2013/495076
10. Allotey, P, Reidpath, DD, and Pokhrel, S. Social sciences research in neglected tropical diseases 1: the ongoing neglect in the neglected tropical diseases. Health Res Policy Syst. (2010) 8:32. doi: 10.1186/1478-4505-8-32
11. Anantharam, P, Emerson, LE, Bilcha, KD, Fairley, JK, and Tesfaye, AB. Undernutrition, food insecurity, and leprosy in North Gondar Zone, Ethiopia: a case-control study to identify infection risk factors associated with poverty. PLoS Negl Trop Dis. (2021) 15:e9456. doi: 10.1371/journal.pntd.0009456
12. Aagaard-Hansen, J, Nombela, N, and Alvar, J. Population movement: a key factor in the epidemiology of neglected tropical diseases. Trop Med Int Health. (2010) 15:1281–8. doi: 10.1111/j.1365-3156.2010.02629.x
13. Zhang, QP, Li, G, Li, C, Lin, ZX, and Chen, P. Epidemiological situation of leprosy in a province in China: a long time to diagnosis and a high rate of deformity. BMC Public Health. (2020) 20:1790. doi: 10.1186/s12889-020-09933-6
14. National Health and Family Planning Commission of the People’s Republic of China . Diagnosis for leprosy WS 291-2018. (2018).
15. World Health Organization . Expert committee on leprosy (seventh report). WHO technical report series, No. 874. Geneva: World Health Organization (1998).
16. World Health Organization . WHO expert committee on leprosy (meeting held in Geneva from 17 to 24 November 1987): sixth report. Geneva: World Health Organization (1988).
17. Oliveira, DT, Sherlock, J, Melo, EV, Rollemberg, KC, Paixão, TR, Abuawad, YG, et al. Clinical variables associated with leprosy reactions and persistence of physical impairment. Rev Soc Bras Med Trop. (2013) 46:600–4. doi: 10.1590/0037-8682-0100-2013
19. Chaptini, C, and Marshman, G. Leprosy: a review on elimination, reducing the disease burden, and future research. Lepr Rev. (2015) 86:307–15. doi: 10.47276/lr.86.4.307
20. World Health Organization . Global leprosy (Hansen disease) update, 2020: impact of COVID-19 on the global leprosy control. Geneva: World Health Organization (2020).
21. Srinivas, G, Muthuvel, T, Lal, V, Vaikundanathan, K, Schwienhorst-Stich, EM, and Kasang, C. Risk of disability among adult leprosy cases and determinants of delay in diagnosis in five states of India: a case-control study. PLoS Negl Trop Dis. (2019) 13:e7495. doi: 10.1371/journal.pntd.0007495
22. Raposo, MT, Reis, MC, Caminha, A, Heukelbach, J, Parker, LA, Pastor-Valero, M, et al. Grade 2 disabilities in leprosy patients from Brazil: need for follow-up after completion of multidrug therapy. PLoS Negl Trop Dis. (2018) 12:e6645. doi: 10.1371/journal.pntd.0006645
23. Zheng, DC, Li, M, Sun, XF, Wang, XH, and Chen, YF. Epidemiological analysis and discussion of strategies regarding prevention of leprosy in migrating population in Guangdong province. J Diagn Ther Derm Venereol. (2010) 17:152–4.
24. Zhu, J, Shi, C, Yang, D, Liu, Y, Chen, J, Ye, M, et al. Internal migration and leprosy in Shanghai from 2000 to 2019: an epidemiological study of new cases. Acta Derm Venereol. (2021) 101:v459. doi: 10.2340/00015555-3821
25. Murto, C, Ariza, L, Alencar, CH, Chichava, OA, Oliveira, AR, Kaplan, C, et al. Migration among individuals with leprosy: a population-based study in Central Brazil. Cad Saude Publica. (2014) 30:487–501. doi: 10.1590/0102-311X00005913
26. Yuan, YH, Liu, J, You, YG, Chen, XH, Yuan, LC, Wen, Y, et al. Transcriptomic analysis of Mycobacterium leprae-stimulated response in peripheral blood mononuclear cells reveal potential biomarkers for early diagnosis of leprosy. Front Cell Infect Microbiol. (2021) 11:714396. doi: 10.3389/fcimb.2021.714396
Keywords: leprosy, migrant, grade 2 disability, influencing factors, cross-sectional study
Citation: Chen L, Zheng D, Li M, Zeng M, Yang B and Wang X (2023) Epidemiology and grade 2 disability of leprosy among migrant and resident patients in Guangdong: an unignorable continued transmission of leprosy. Front. Public Health. 11:1275010. doi: 10.3389/fpubh.2023.1275010
Received: 11 August 2023; Accepted: 06 November 2023;
Published: 24 November 2023.
Edited by:
Neusa Sakai Valente, University of São Paulo, BrazilReviewed by:
Maria Pena, Health Resources and Services Administration, United StatesCopyright © 2023 Chen, Zheng, Li, Zeng, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohua Wang, V3hoXzIxNzczQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.