
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 October 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1274253
This article is part of the Research Topic The Importance of the Body-Mind Relationship in Mental Functioning and Development of Body-Focused Disorders in Adolescence, volume II View all 10 articles
Background: A growing number of studies have suggested that adolescents’ prosocial behavior can protect against depression and anxiety. It is known that anxiety and depression are often comorbid. However, it remains unclear if when depression is present, prosocial behavior remains protective against anxiety, and if when anxiety is present, prosocial behavior remains protective against depression. The purpose of this study was to determine the association of anxiety and depressive with prosocial behavior.
Methods: A large representative sample of middle-school students was recruited for a cross-sectional study and completed standardized instruments (the Children’s Depression Inventory (CDI), Screen for Child Anxiety Related Emotional Disorders–Child version (SCARED-C), and Strengths and Difficulties Questionnaire (SDQ)). We used structural equation modeling (SEM) to examine the protective effect of prosocial behavior against anxiety when depression was present.
Results: A survey of 3,510 students was conducted, and the final analysis included 3,169 students, comprising 1,616 boys (51.0%) and 1,553 girls (49.0%), with a mean age of 13.09 years (SD = 1.31, range 11–16).The prevalence rates of anxiety and depression in early adolescents were 31.6 and 16.7%, respectively. More than two-thirds of depressed adolescents had comorbid anxiety, while more than one-third of anxious adolescents had comorbid depression. Regression models showed that compared with depressed adolescents, adolescents without depressive symptoms exhibited a significant negative correlation between prosocial behaviors and anxiety and depression (β = −0.01, p > 0.01, β = −0.06, p > 0.01; β = −0.11, p < 0.01, and β = −0.17, p < 0.01). There was no difference in the relationship between prosocial behavior and depression between anxious and non-anxious adolescents (p > 0.05).
Conclusion: Anxiety and depression are common in adolescence and are often comorbid disorders. However, the comorbidity is not symmetrical. Specifically, the protective effect of prosocial behavior against anxiety is weaker in depressed adolescents. Findings are discussed in light of related research and theory, and insights for intervention programs and future research are presented.
The prevalence rates of mental health problems have increased among adolescents worldwide, as high as 20.0% (1, 2). If left untreated, they tend to persist into adulthood and are associated with a range of adverse outcomes (3). Mental health problems account for 16% of the disease and injury burden among adolescents aged 10–19 years worldwide, according to statistics released by WHO in 2019. Thus, promoting mental health among adolescents is a public health priority (4).
Anxiety and depression are the most prevalent mental health problems in adolescence. Nearly 40% of adolescents reported having experienced anxiety symptoms, and 8.3% qualified for severe anxiety-related impairment (5). Anxiety is the sixth leading cause of disease and disability for adolescents aged 11–14 years and the ninth leading cause for those aged 15–19 years (6). A meta-analysis indicated that the prevalence of depressive symptoms in adolescents was18.4% before 2000 and was 26.3% after 2016 in China (7). More than half of adolescents who commit suicide may have had a depressive disorder at the time of death (8), and depression in adolescents is a primary risk factor for suicide (8). The high prevalence of anxiety and depression in adolescents and the high rates of disability require a focus on adolescent anxiety and depression.
Anxiety and depression often co-occur (9, 10). Diagnostic comorbidity rates reported in some clinical samples were as high as 75% (11, 12). Approximately 25–50% of depressed youth have anxiety, and approximately 10–15% of anxious youth have comorbid depression (13). Depressed youths with comorbid anxiety tend to have more severe depressive symptoms than no anxious depressed youths (13). Thus, the symptoms may be magnified in children and adolescents with comorbidities (13). However, individuals with a comorbid disorder also exhibit some unique characteristics. One study found that depressed youths tended to report high levels of depression and anxiety, while anxious youths tended to report relatively low levels of depression (14). Comorbidity may result in greater overall impairment, higher rates of suicide attempts and worse treatment outcomes (15, 16). A better understanding of the relationship between anxiety and depression is crucial for preventing comorbidities and mitigating their impact in depressed/anxious adolescents. Anxiety and depression share various risk and protective factors (17), individually, they might not exert the same level of influence on outcomes. Exploring risk and protective factors and determining their effects are important to prevent anxiety and depression in adolescents.
Prosocial behavior, often referred to as sociability, is a complex amalgamation of different types of social interactions (18). Prosocial behaviors are intended to benefit others, including helping, caring, cooperating, sharing, sympathizing and comforting (19). Recent meta-analyzes indicated that prosocial activities have a positive effect on well-being and reduce negative emotions. Prosocial behavior is socially respected, and the social rewards it accrues may, consequently, improve mood (20). Conversely, prosocial behavior may protect against negative feelings (21), depression and anxiety (22, 23). These studies have not considered the high rates of comorbidity observed. However, epidemiological studies suggest that comorbidity is universal, not exceptional; therefore, solely exploring the association of prosocial behaviors with a single mental health problem may not be comprehensive. It is essential to determine the association of depression and anxiety with prosocial behaviors in adolescents to elucidate internalizing problems in adolescents as well as to implement more optimal interventions for anxiety and depression. The present study aimed to investigate (a) the association between prosocial behavior and anxiety when depression was present, and (b) the association between prosocial behavior and depression when anxiety was present.
This cross-sectional study used a stratified random cluster sampling method to recruit students from junior high schools in the Pudong New Area, Shanghai, China, from September to November 2021. A total of 3,510 participants aged 11–16 years took part in the survey. After excluding the data of participants with invalid questionnaires, 3,169 participants were included in the final analysis, for a response rate of 90.3%.
Approval for the study was obtained from the Ethics Committee of Shanghai Pudong New Area Mental Health Center. The parents of all participants provided informed consent to participate in the study (PDJWLL2021030).
A custom-designed demographic questionnaire was used to collect the participants’ general information, including age, gender, monthly family income, marital relationship of parents (harmony/disharmony), family structure (nuclear family/extended family/other family structures), parenting style (consistent/inconsistent) and relationship with friends (good/acceptable/bad). Family economic status was categorized into three classes according to monthly family income: lower (less than ¥5,000), middle (¥5,000–10,000), and upper (more than ¥10,000).
Depressive symptoms were assessed using the Children’s Depression Inventory (CDI), which consists of 27 items. The CDI is a comprehensive multilayer assessment of depressive symptoms in children and adolescents and has five subscales: negative mood, interpersonal problems, ineffectiveness, anhedonia and negative self-esteem (24, 25). Participants were asked to indicate the presence of 27 problems in the last 2 weeks on a 3-point scale ranging from 0 (none) to 2 (distinct symptom). Higher scores indicate more depressive symptoms. In this study, participants with a cutoff score of 19 or higher were considered to have significant depressive symptoms. The CDI has good internal consistency, with Cronbach’s alpha coefficients ranging from 0.71 to 0.89 (26). The reliability and validity of this test in the Chinese population have been demonstrated (27). The Cronbach’s alpha coefficient of the CDI was good (0.88) in the present study.
Anxiety symptoms were assessed using the Screen for Child Anxiety Related Emotional Disorders–Child version (SCARED-C), which measures 41 symptoms. Participants are asked how often they had been bothered by each symptom over the previous 3 months. The response options are “almost never,” “sometimes,” and “often,” scored as 0, 1 and 2, respectively. The SCARED-C includes five subscales: generalized anxiety symptoms, separation anxiety symptoms, social anxiety symptoms, panic or somatic symptoms, and school avoidance (28, 29). A total score of 25 or more has been recommended to indicate significant clinical anxiety (30, 31). Good retesting reliability and validity for the SCARED-C have been confirmed in the Chinese population (32). The Cronbach’s alpha coefficient of this questionnaire was 0.84 in the present study.
Prosocial behavior was assessed using the prosocial scale of the Strengths and Difficulties Questionnaire (SDQ), which is a 25-item checklist (33). The SDQ is divided into five scales of five items each: conduct problems, emotional problems, hyperactivity, peer problems, and prosocial behavior (34). The prosocial scale assesses adolescents’ prosocial behavior. Items are rated on a 3-point Likert scale ranging from 0 to 2 (0 = never, 1 = sometimes, 2 = always). Higher scores indicate more prosocial behavior (35). There are three versions of this questionnaire: the parent version, the teacher version and the self-report version (36), and the self-report version was used in this study. The Chinese version of the SDQ has been demonstrated to have good reliability and validity in Chinese adolescents (37). The internal consistency of the prosocial behavior score (Cronbach’s alpha = 0.70) in the present study was sufficient.
Descriptive and inferential statistics were calculated using SPSS version 25.0 for Windows (SPSS, Inc., Chicago, IL, United States). AMOS24 (IBM Corporation, Armonk, NY, United States) was used for correlation analysis and regression analysis. Categorical variables are described as frequencies and percentages and were compared using the chi-square test. The internal consistency of the CDI, SCARED-C and the prosocial scale was evaluated using Cronbach’s alpha values. Pearson correlation analyzes were used to analyze relationships between study variables. A p value <0.05 was considered statistically significant, and all statistical tests were two-sided.
Structural equation modeling (SEM) was used to examine the relationships of latent variables. Model fit was evaluated using the chi-square test (χ2/df), root mean square error of approximation (RSMEA), comparative fit index (CFI), incremental fit index (IFI) and Tucker–Lewis index (TLI). Notably, χ2/df > 2 implies good model fit; RSMEA values <0.05 represent close model fit, and values >0.10 reflect poor model fit (38); and CFI, IFI, and TLI values >0.90 indicate good fit (39). The fit indices should be interpreted collectively. Standardized coefficients (β) were examined with regression path analyzes.
A survey of 3,510 students was conducted, and a total of 3,169 (90.3%) students were included in the final analysis. The sample consisted of 1,616 (51.0%) boys and 1,553 (49.0%) girls, with a mean age of 13.09 years (SD = 1.31, range 11–16). Descriptive statistics for all categorical variables are shown in Table 1. Most participants were from nuclear families (61.0%), had middle or upper family economic status (86.2%), maintained good relationships with their friends (62.1%), reported that their parents had a “good” relationship (88.5%), and reported experiencing a consistent parenting style (70.9%).
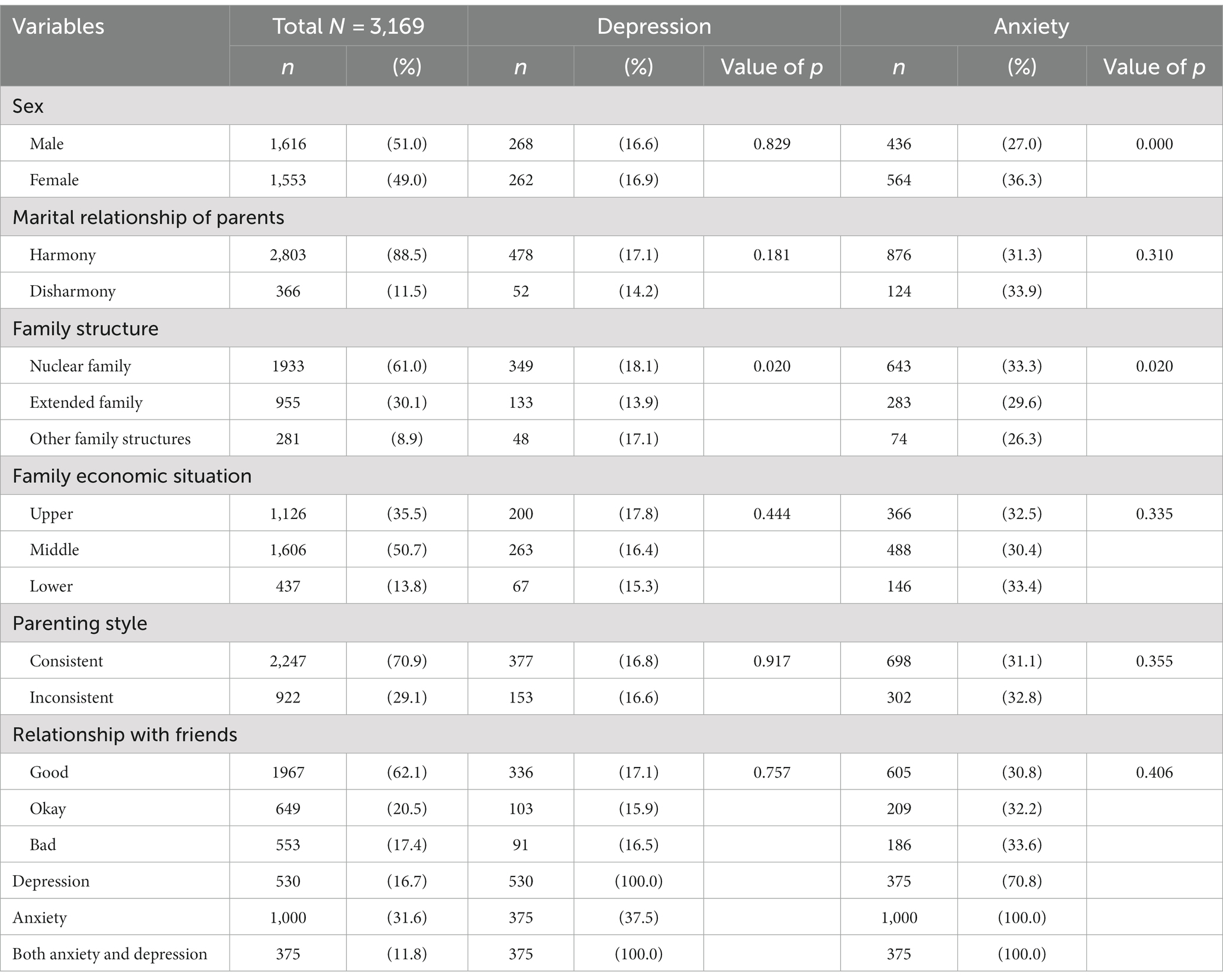
Table 1. Distribution of variables, and association with anxiety and depression among middle school students.
The prevalence rates of anxiety and depression among middle school students were 31.6 and 16.7%, respectively. Boys had a lower prevalence of anxiety than girls (p < 0.05) but a similar prevalence of depression (p > 0.05). The prevalence rates of anxiety and depression were higher in participants from nuclear families than in those from large families and other types of families, and there were significant differences among family types (χ2 = 7.80, p = 0.020; χ2 = 7.85, p = 0.020). We found no significant difference in other variables (p > 0.05). More than two-thirds of students who met the threshold for depression as a primary condition also had anxiety symptoms, while more than one-third of students who met the threshold for anxiety as a primary condition also had depressive symptoms. The comorbidity rate of anxiety and depression was 11.8% among adolescents. See Table 1 for more details.
Table 2 summarized the correlations found between study variables with means and standard deviations for all continuous study variables. Prosocial behavior was negatively associated with anxiety, depression and SDQ-Externalized Problems (r = −0.177, p < 0.001; r = −0.359, p < 0.001; r = −0.392, p < 0.001). SDQ-Externalized Problems was positively associated with anxiety and depression (r = −0.452, p < 0.001; r = −0.615, p < 0.001). Anxiety was positively associated with depression (r = −0.589, p < 0.001).
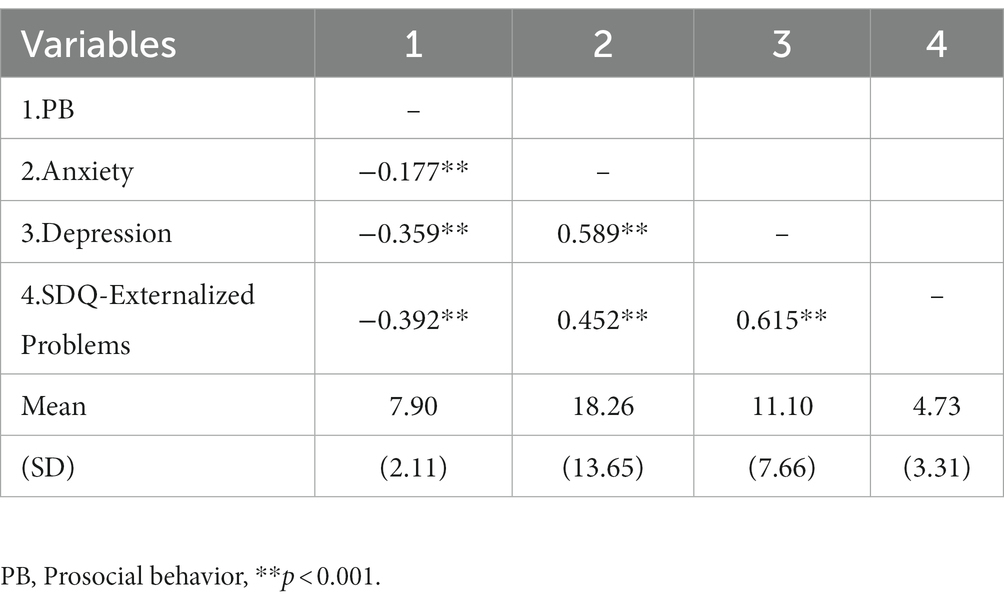
Table 2. Bivariate correlations between and descriptive statistics for all continuous study variables (r value).
The results showed that the overall model fit was acceptable (χ2/df = 7.754, RSMEA = 0.046, CFI = 0.990, IFI = 0.990, TLI = 0.964). The regression model showed that the correlations between adolescents’ externalizing problems and anxiety were significantly positive (β = −0.34, p < 0.001). As shown in Figure 1, among 2,639 middle school students without depressive symptoms, there was a significant negative correlation between prosocial behavior and anxiety (β = −0.11, p < 0.01), and prosocial behavior significantly negatively predicted the depressive symptom scores of middle school students (β = −0.17, p < 0.01). As shown in Figure 2, among the 530 middle school students with depressive symptoms, the correlation between prosocial behavior and anxiety was not statistically significant (β = −0.01, p > 0.01), and prosocial behavior did not significantly predict depressive symptoms in adolescents (β = −0.06, p > 0.01). As shown in Figures 1, 2, compared with adolescents without depression symptoms, adolescents with depressive symptoms did not exhibit a protective effect of prosocial behavior. While there was a significant negative correlation between prosocial behavior and anxiety symptoms among adolescents without depressive symptoms, this correlation was absent among adolescents with depressive symptoms. As shown in Figures 3, 4, there was no difference in the protective effect of prosocial behavior against depression between anxious and no anxious adolescents (p > 0.05).
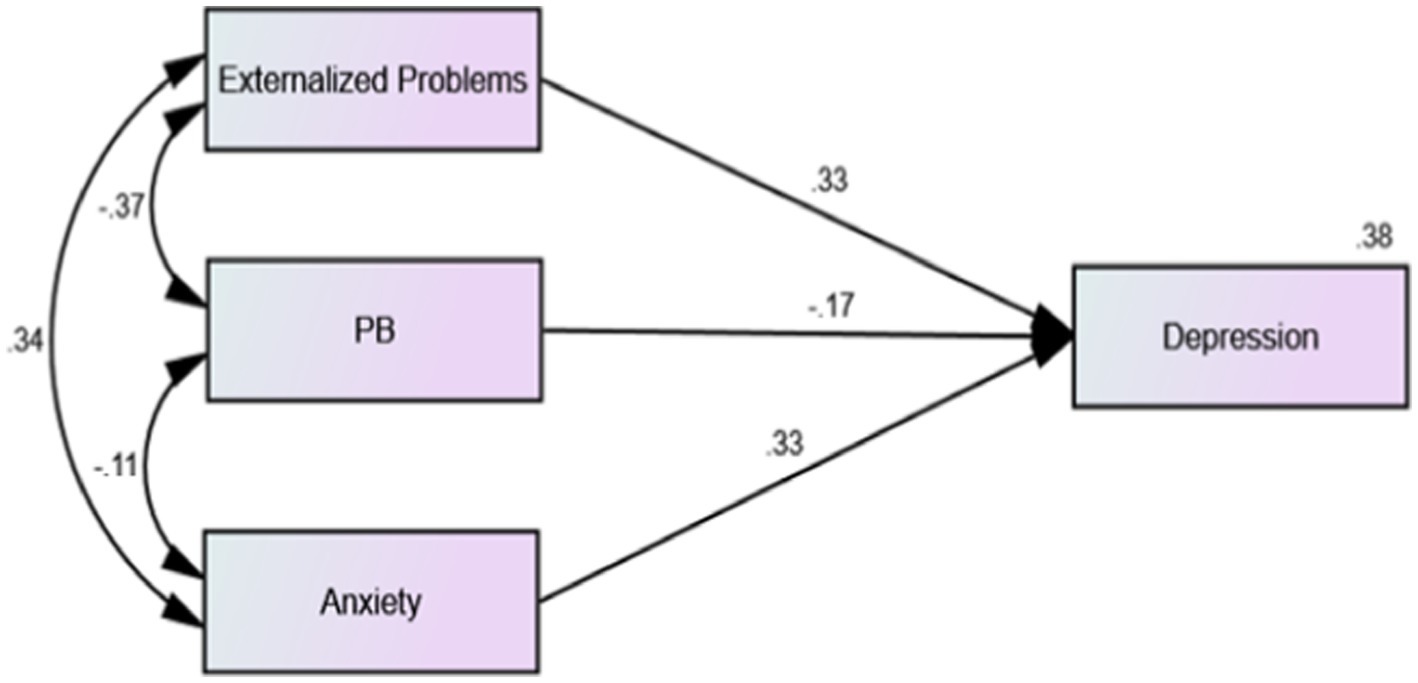
Figure 1. Regression model of external problems, prosocial behavior, anxiety and depression factors of middle school students without depressive symptoms.
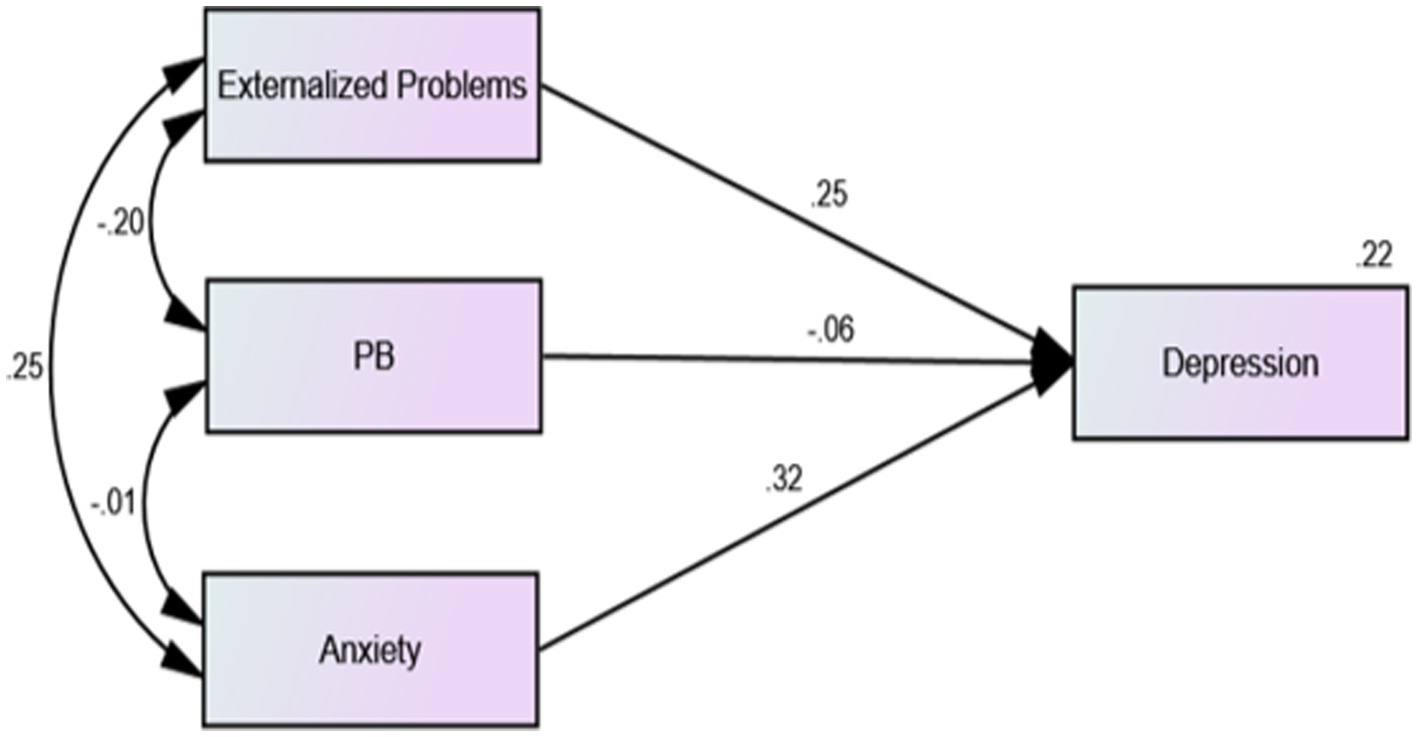
Figure 2. Regression model of external problems, prosocial behavior, anxiety and depression factors of middle school students with depressive symptoms.
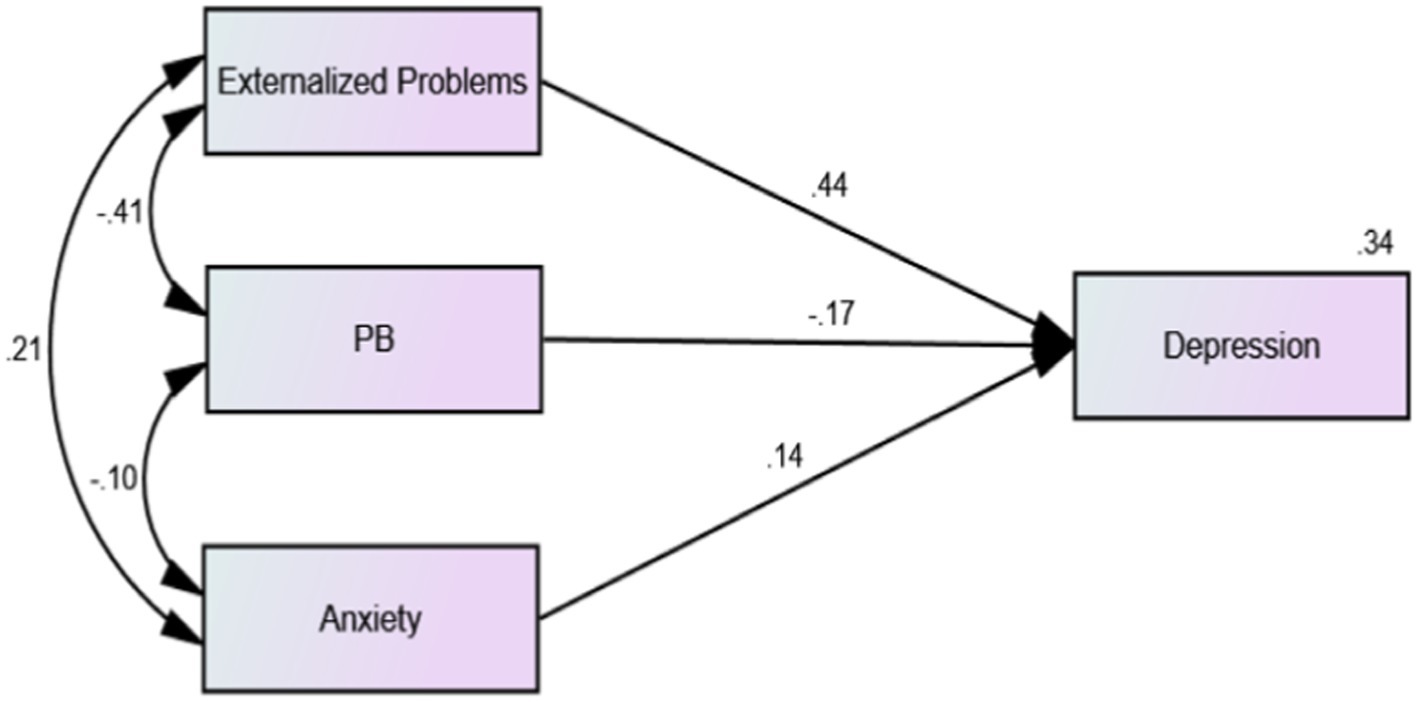
Figure 3. Regression model of external problems, prosocial behaviors, anxiety and depression factors of middle school students without anxiety symptoms.
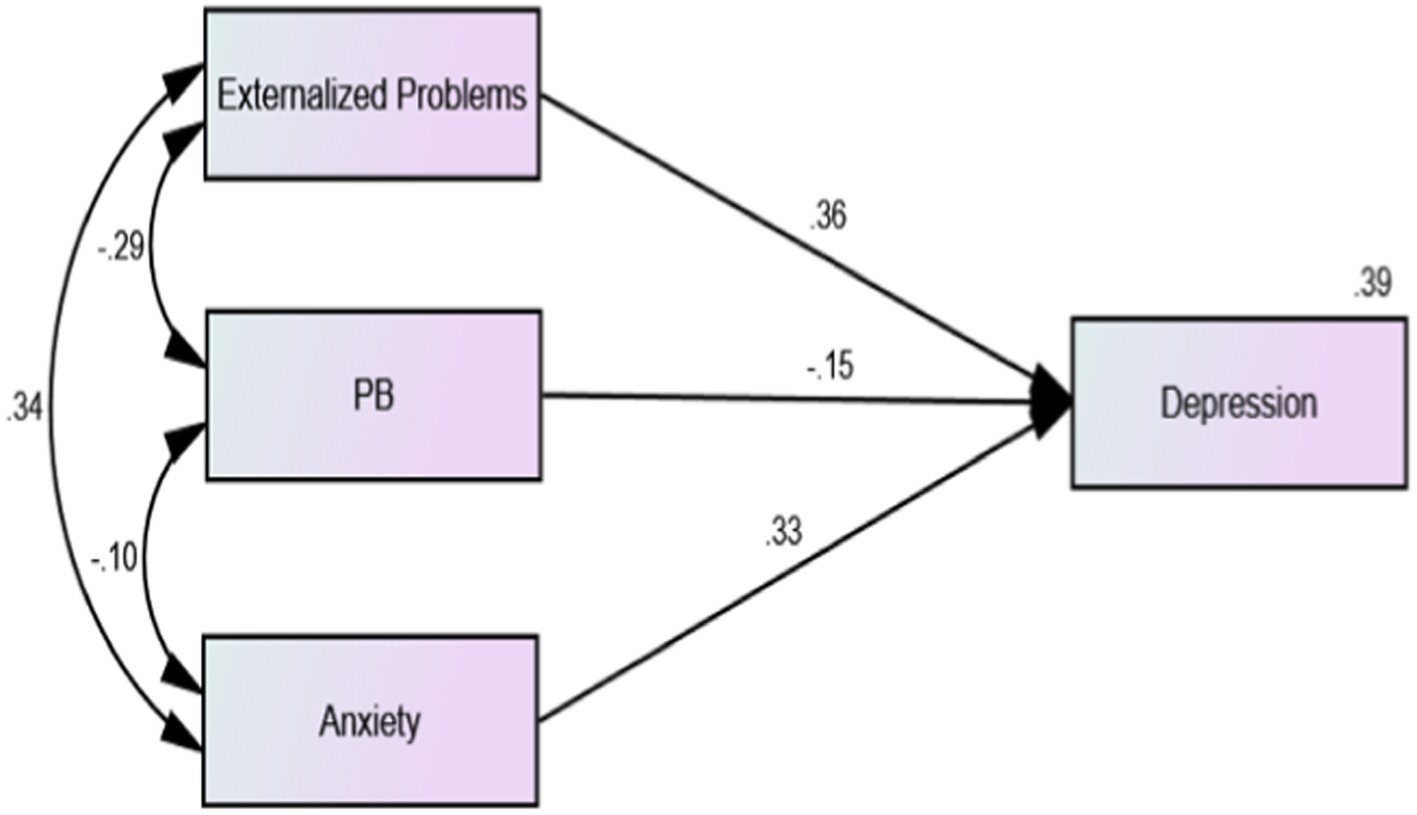
Figure 4. Regression model of external problems, prosocial behaviors, anxiety and depression factors of middle school students with anxiety symptoms.
We found that anxiety and depression were prevalent among adolescents, with prevalence rates of 31.6 and 16.7%, respectively. Adolescence is a high-risk period for the onset of mood disorders, particularly anxiety and depression (40). Adolescence is a period of upheaval and change in physical, cognitive, emotional and social factors (41). During this period, adolescents face many developmental challenges, such as the need for academic achievement, peer relationships and independence from parents (42). Female adolescents are more likely than males to suffer from mood and anxiety disorders (43). Similar to previous studies, our findings confirmed that there was a gender difference in the distribution of anxiety, with female adolescents having a higher prevalence of anxiety than male adolescents. However, we did not find a gender difference in the incidence of depression. Previous research has suggested that female adolescents are biased toward depressive symptoms due to gender differences in hormone levels during puberty (44, 45). The gender difference in depression is one of the strongest findings in psychopathology research (46). Considerable empirical and theoretical research has been conducted on gender differences in depression. However, the findings have been inconsistent. One study found that male adolescents have a higher risk of depression than female adolescents (47). There may be a gender-age pattern of depressive symptoms. Several studies have shown that during childhood, boys are more likely than girls to suffer from depression (48). The increased prevalence of depression in females is thought to occur between the ages of 13 and 15 years (49, 50). The age range of our study sample was 11 to 16 years. Differences in the age range of samples may have contributed to the inconsistent results regarding gender differences in adolescent depression. In addition to age, differences in other nonphysical factors, such as research instruments, cultures, regions, and social structure, may also be important factors leading to inconsistent findings and a comprehensive meta-analysis of gender differences in adolescent depression could be conducted in the future. We also noted that living in extended families may protect adolescents’ emotional health compared to living in nuclear families. One possible explanation is that adolescents in nuclear families receive less emotional support than those in extended families, as these children can draw upon grandparents as additional (or alternative) sources of attachment, reassurance and knowledge and possibly experience decreased parental stress (51).
On the other hand, anxiety and depression are highly concurrent or sequential comorbidities. In some clinical samples, the correlation between dimensional measures of anxiety and depression symptoms was high (52), and the rate of diagnostic comorbidity was as high as 75% (11), with substantial comorbidity evident in both areas. We also found considerable levels of comorbid anxiety and depression in this large representative sample of Chinese adolescents. However, the comorbidity was commonly asymmetrical. That is, adolescents with a primary diagnosis of depression tended to have comorbid anxiety more often than adolescents with a primary diagnosis of anxiety experienced comorbid depression (13). This phenomenon was also confirmed in this study.
Most importantly, we analyzed the association between prosocial behavior and internalizing problems such as anxiety and depression. Our findings indicated that higher levels of prosocial behavior were associated with lower levels of anxiety and lower levels of depression. Specifically, prosocial behavior was negatively associated with anxiety and depression, consistent with some previous research (21–23), suggesting that prosocial behavior may prevent anxiety and depression. Prosocial behaviors are positive and friendly voluntary behaviors that an individual displays toward others. It is quite common during adolescence because during this period, opportunities for prosocial behaviors increase. Adolescents are especially sensitive to the quality and type of interactions they have with people in their social networks, and poor interpersonal interactions can lead to unfavorable mental health outcomes such as anxiety and depression (53). Previous research has shown that children who display high levels of prosocial behavior receive positive feedback and peer acceptance from their peers, and being liked and accepted by peers is associated with increased self-confidence and reduced anxiety and depression in children (54). Thus, prosocial behavior is important for forming and maintaining healthy relationships, and it can protect adolescents from maladjustment. Engaging in prosocial behaviors, especially with strangers, also promotes or stimulates the development of dominant personalities, which is especially important in early adolescence, as adolescents are developing character strengths that may continue to play a protective role in late adolescence and adulthood (55). In addition, according to response transformation theory, engaging in prosocial behaviors facilitates psychological adaptation through shifts in internal norms, values, and concepts of well-being as well as disengagement from self-focused psychological problems, such as anxiety and depression (56, 57). Prosocial behaviors, such as volunteering, leadership, and civic engagement, have often been incorporated into positive adolescent interventions, both as desired outcomes and as protective factors against future negative outcomes (58). All of the above findings suggest that adding prosocial behavior programs in schools may be beneficial. One school-based intervention study showed that when prosocial behavior was structurally added to the students’ curriculum, students’ mood level was significantly improved (59).
It is notable that the protective effect of prosocial behaviors against anxiety and depression may occur in both healthy and anxious adolescent populations. In further analyzes, we found that the protection of prosocial behavior against anxiety disappeared in individuals with depressive symptoms, but prosocial behavior still protected against depression in individuals with anxiety symptoms. Depression may have a greater impact on adolescents’ prosocial behaviors; they become more introverted, withdrawn and unable to exhibit warmth, compassion and helpfulness to others, resulting in decreased prosocial behavior. Individuals with low levels of prosocial behavior will experience more interpersonal problems and stress, making it difficult for them to stop negative self-thoughts and reflection and even aggravate these issues (60). This in turn increases the risk of depression and anxiety, resulting in a vicious cycle. Thus, treating depressive symptoms may be the first step for adolescents with depressive symptoms (e.g., through counseling interventions or medication). Alleviating the depressive symptoms of adolescents may help to restore the sensitivity provided by prosocial behavior and benefit from it.
Although our results indicated that prosocial behavior was negatively associated with depression and anxiety, these findings need to be verified in the future, especially in other adolescent samples. Inconsistent results have been reported in previous studies, particularly regarding the association between prosocial behavior and adolescent anxiety. For example, there is evidence that high levels of prosocial behavior protects against anxiety in girls (61). However, a recent meta-analysis showed that prosocial behavior was not related to anxiety (62). Another study showed that normative levels of anxiety were positively associated with prosocial behavior (63). In the future, research should focus on the association between prosocial behavior and adolescents’ internalizing problems from a more specific and multidimensional perspective.
Our study has two potential limitations. First, it had a cross-sectional design; therefore, we could not dynamically analyze the association between prosocial behaviors and internalizing problems. Second, all measures in the study were self-reported, potentially leading to shared method bias. Although adolescents were considered the best reporters of their internal states (such as anxiety and depression), future research should investigate a wider range of reporters (e.g., parents, teachers).
Anxiety and depression are common in adolescents and are often comorbid. Adolescents spend more time in school than in any other formal institutional institution. Therefore, schools play a key role in the development of adolescents in all aspects. For adolescents without depressive symptoms, adding prosocial behavior to educational goals may be beneficial for their emotional management. Increasing school support and cultivating adolescents’ self-esteem and hope can promote prosocial behavior. However, in adolescents who already have depressive symptoms, increasing prosocial behavior may not be the most effective method. Instead, depressive symptoms may first need to be structurally addressed.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Ethics Committees of Shanghai Pudong New Area Mental Health Center. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
XZ: Writing – original draft, Funding acquisition. TL: Data curation, Writing – original draft. GL: Methodology, Investigation, Software, Writing – review & editing. NZ: Investigation, Writing – original draft. XL: Formal analysis, Writing – original draft. YL: Software, Writing – original draft. YC: Writing – review & editing, Funding acquisition.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Excellent Youth Medical Talents Training Program of Pudong Health Bureau of Shanghai (PWRq2021-09), Science and Technology Development Fund Of Shanghai Pudong New Area (PKJ2017-Y67) and the Medical Discipline Construction Project of Pudong Health Committee of Shanghai Medical Discipline Construction Project of Pudong Health (PWYgy2021-02).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Zhao, M, and Hu, M. A multilevel model of the help-seeking behaviors among adolescents with mental health problems. Front Integr Neurosci. (2022) 16:946842. doi: 10.3389/fnint.2022.946842
2. Cui, Y, Li, F, Leckman, JF, Guo, L, Ke, X, Liu, J, et al. The prevalence of behavioral and emotional problems among Chinese school children and adolescents aged 6-16: a national survey. Eur Child Adolesc Psychiatry. (2021) 30:233–41. doi: 10.1007/s00787-020-01507-6
3. Rutter, M, Kim-Cohen, J, and Maughan, B. Continuities and discontinuities in psychopathology between childhood and adult life. J Child Psychol Psychiatry. (2006) 47:276–95. doi: 10.1111/j.1469-7610.2006.01614.x
4. Patel, V, Flisher, AJ, Hetrick, S, and McGorry, P. Mental health of young people: a global public-health challenge. Lancet. (2007) 369:1302–13. doi: 10.1016/S0140-6736(07)60368-7
5. Parodi, KB, Holt, MK, Green, JG, Porche, MV, Koenig, B, and Xuan, Z. Time trends and disparities in anxiety among adolescents, 2012–2018. Soc Psychiatry Psychiatr Epidemiol. (2021) 57:127–37. doi: 10.1007/s00127-021-02122-9
6. Kessler, RC, Angermeyer, M, Anthony, JC, De Graaf, R, Demyttenaere, K, Gasquet, I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's world mental health survey initiative. World Psychiatry. (2007) 6:168–76.
7. Li, J-Y, Li, J, Liang, J-H, Qian, S, Jia, R-X, Wang, Y-Q, et al. Depressive symptoms among children and adolescents in China: a systematic review and Meta-analysis. Med Sci Monit. (2019) 25:7459–70. doi: 10.12659/MSM.916774
8. Thapar, A, Collishaw, S, Pine, DS, and Thapar, AK. Depression in adolescence. Lancet. (2012) 379:1056–67. doi: 10.1016/S0140-6736(11)60871-4
9. Essau, CA . Comorbidity of depressive disorders among adolescents in community and clinical settings. Psychiatry Res. (2008) 158:35–42. doi: 10.1016/j.psychres.2007.09.007
10. Garber, J, and Weersing, VR. Comorbidity of anxiety and depression in youth: implications for treatment and prevention. Clin Psychol (New York). (2010) 17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x
11. Sørensen, MJ, Nissen, JB, Mors, O, and Thomsen, PH. Age and gender differences in depressive symptomatology and comorbidity: an incident sample of psychiatrically admitted children. J Affect Disord. (2005) 84:85–91. doi: 10.1016/j.jad.2004.09.003
12. Cummings, CM, Caporino, NE, and Kendall, PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. (2014) 140:816–45. doi: 10.1037/a0034733
13. Axelson, DA, and Birmaher, B. Relation between anxiety and depressive disorders in childhood and adolescence. Depress Anxiety. (2001) 14:67–78. doi: 10.1002/da.1048
14. Ferdinand, RF, de Nijs, PFA, van Lier, P, and Verhulst, FC. Latent class analysis of anxiety and depressive symptoms in referred adolescents. J Affect Disord. (2005) 88:299–306. doi: 10.1016/j.jad.2005.08.004
15. Lewinsohn, PM, Rohde, P, and Seeley, JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. J Am Acad Child Adolesc Psychiatry. (1995) 34:510–9. doi: 10.1097/00004583-199504000-00018
16. Karlsson, L, Pelkonen, M, Ruuttu, T, Kiviruusu, O, Heila, H, Holi, M, et al. Current comorbidity among consecutive adolescent psychiatric outpatients with DSM-IV mood disorders. Eur Child Adolesc Psychiatry. (2006) 15:220–31. doi: 10.1007/s00787-006-0526-7
17. Epkins, CC, and Heckler, DR. Integrating etiological models of social anxiety and depression in youth: evidence for a cumulative interpersonal risk model. Clin Child Fam Psychol Rev. (2011) 14:329–76. doi: 10.1007/s10567-011-0101-8
18. Walsh, JJ, Christoffel, DJ, Wu, X, Pomrenze, MB, and Malenka, RC. Dissecting neural mechanisms of prosocial behaviors. Curr Opin Neurobiol. (2021) 68:9–14. doi: 10.1016/j.conb.2020.11.006
19. Penner, LA, Dovidio, JF, Piliavin, JA, and Schroeder, DA. Prosocial behavior: multilevel perspectives. Annu Rev Psychol. (2005) 56:365–92. doi: 10.1146/annurev.psych.56.091103.070141
20. Hay, DF . Prosocial development. J Child Psychol Psychiatry. (1994) 35:29–71. doi: 10.1111/j.1469-7610.1994.tb01132.x
21. Adam, SS, and Grant, M. Doing good buffers against feeling bad: prosocial impact compensates for negative task and self-evaluations. Organ Behav Hum Decis Process. (2010) 111:13–22. doi: 10.1016/j.obhdp.2009.07.003
22. Haroz, EE, Murray, LK, Bolton, P, Betancourt, T, and Bass, JK. Adolescent resilience in northern Uganda: the role of social support and prosocial behavior in reducing mental health problems. J Res Adolesc. (2013) 23:138–48. doi: 10.1111/j.1532-7795.2012.00802.x
23. Fujiwara, T . The role of altruistic behavior in generalized anxiety disorder and major depression among adults in the United States. J Affect Disord. (2007) 101:219–25. doi: 10.1016/j.jad.2006.11.024
25. Watson, HJ, Egan, SJ, Limburg, K, and Hoiles, KJ. Normative data for female adolescents with eating disorders on the Children's depression inventory. Int J Eat Disord. (2014) 47:666–70. doi: 10.1002/eat.22294
26. Ivarsson, T, Svalander, P, and Litlere, O. The Children's depression inventory (CDI) as measure of depression in Swedish adolescents. A normative study. Nord J Psychiatry. (2006) 60:220–6. doi: 10.1080/08039480600636395
27. Wang, L, Feng, Z, Yang, G, Yang, Y, Dai, Q, Hu, C, et al. The epidemiological characteristics of depressive symptoms in the left-behind children and adolescents of Chongqing in China. J Affect Disord. (2015) 177:36–41. doi: 10.1016/j.jad.2015.01.002
28. Hale, WW, Raaijmakers, Q, Muris, P, and Meeus, W. Psychometric properties of the screen for child anxiety related emotional disorders (SCARED) in the general adolescent population. J Am Acad Child Adolesc Psychiatry. (2005) 44:283–90. doi: 10.1097/00004583-200503000-00013
29. Dirks, MA, Weersing, VR, Warnick, E, Gonzalez, A, Alton, M, Dauser, C, et al. Parent and youth report of youth anxiety: evidence for measurement invariance. J Child Psychol Psychiatry. (2014) 55:284–91. doi: 10.1111/jcpp.12159
30. Birmaher, B, Khetarpal, S, Brent, D, Cully, M, Balach, L, Kaufman, J, et al. The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. (1997) 36:545–53. doi: 10.1097/00004583-199704000-00018
31. Rappaport, BI, Pagliaccio, D, Pine, DS, Klein, DN, and Jarcho, JM. Discriminant validity, diagnostic utility, and parent-child agreement on the screen for child anxiety related emotional disorders (SCARED) in treatment-and non-treatment-seeking youth. J Anxiety Disord. (2017) 51:22–31. doi: 10.1016/j.janxdis.2017.08.006
32. Su, L, Wang, K, Fan, F, Su, Y, and Gao, X. Reliability and validity of the screen for child anxiety related emotional disorders (SCARED) in Chinese children. J Anxiety Disord. (2008) 22:612–21. doi: 10.1016/j.janxdis.2007.05.011
33. Goodman, R, Meltzer, H, and Bailey, V. The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. (1998) 7:125–30. doi: 10.1007/s007870050057
34. Goodman, R . The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
35. Basel El-Khodary, MS . The mediating role of trait emotional intelligence, prosocial behaviour, parental support and parental psychological control on the relationship between war trauma, and PTSD and depression. J Res Pers. (2019) 81:246–56. doi: 10.1016/j.jrp.2019.06.004
36. Goodman, R . Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. (2001) 40:1337–45. doi: 10.1097/00004583-200111000-00015
37. Du, Y, Kou, J, and Coghill, D. The validity, reliability and normative scores of the parent, teacher and self report versions of the strengths and difficulties questionnaire in China. Child Adolesc Psychiatry Ment Health. (2008) 2:8. doi: 10.1186/1753-2000-2-8
38. Michael, RC, and Browne, W. Alternative ways of assessing model fit. Sociol Methods Res. (1992) 21:230–58. doi: 10.1177/0049124192021002005
39. Li-tze Hu, PMB . Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
40. Schacter, HL, and Margolin, G. When it feels good to give: depressive symptoms, daily prosocial behavior, and adolescent mood. Emotion. (2019) 19:923–7. doi: 10.1037/emo0000494
41. Griffin, A . Adolescent neurological development and implications for health and well-being. Healthcare. (2017) 5:62. doi: 10.3390/healthcare5040062
42. Zarrett, N, and Eccles, J. The passage to adulthood: challenges of late adolescence. New Dir Youth Dev. (2006) 2006:13–28. doi: 10.1002/yd.179
43. Merikangas, KR, He, J-p, Burstein, M, Swanson, SA, Avenevoli, S, Cui, L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. (2010) 49:980–9. doi: 10.1016/j.jaac.2010.05.017
44. Weller, EB, Kloos, A, Kang, J, and Weller, RA. Depression in children and adolescents: does gender make a difference? Curr Psychiatry Rep. (2006) 8:108–14. doi: 10.1007/s11920-006-0007-1
45. Paus, T, Keshavan, M, and Giedd, JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. (2008) 9:947–57. doi: 10.1038/nrn2513
46. Bebbington, P . The origins of sex differences in depressive disorder: bridging the gap. Int Rev Psychiatry. (2009) 8:295–332. doi: 10.3109/09540269609051547
47. Verboom, CE, Sijtsema, JJ, Verhulst, FC, Penninx, BW, and Ormel, J. Longitudinal associations between depressive problems, academic performance, and social functioning in adolescent boys and girls. Dev Psychol. (2014) 50:247–57. doi: 10.1037/a0032547
48. Cyranowski, JM, Frank, E, Young, E, and Shear, MK. Shear MK adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry. (2000) 57:21–7. doi: 10.1001/archpsyc.57.1.21
49. Hankin, BL, Abramson, LY, Moffitt, TE, Silva, PA, McGee, R, and Angell, KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. (1998) 107:128–40. doi: 10.1037/0021-843X.107.1.128
50. Twenge, JM, and Nolen-Hoeksema, S. Age, gender, race, socioeconomic status, and birth cohort difference on the children's depression inventory: a meta-analysis. J Abnorm Psychol. (2002) 111:578–88. doi: 10.1037/0021-843X.111.4.578
51. Hwang, HJ, and St James-Roberts, I. Emotional and behavioural problems in primary school children from nuclear and extended families in Korea. J Child Psychol Psychiatry. (1998) 39:973–9. doi: 10.1111/1469-7610.00400
52. Stark, KD, and Laurent, J. Joint factor analysis of the Children's depression inventory and the revised Children's manifest anxiety scale. J Clin Child Psychol. (2001) 30:552–67. doi: 10.1207/S15374424JCCP3004_11
53. Masten, CL, Eisenberger, NI, Borofsky, LA, Pfeifer, JH, McNealy, K, Mazziotta, JC, et al. Neural correlates of social exclusion during adolescence: understanding the distress of peer rejection. Soc Cogn Affect Neurosci. (2009) 4:143–57. doi: 10.1093/scan/nsp007
54. TS, BRB, Rubin-Smith, J, Fitzmaurice, GM, and Gilman, SE. Sierra Leone's former child soldiers: a longitudinal study of risk, protective factors, and mental health. J Am Acad Child Adolesc Psychiatry. (2010) 49:606–15. doi: 10.1016/j.jaac.2010.03.008
55. Padilla-Walker, LM, Millett, MA, and Memmott-Elison, MK. Can helping others strengthen teens? Character strengths as mediators between prosocial behavior and adolescents’ internalizing symptoms. J Adolesc. (2020) 79:70–80. doi: 10.1016/j.adolescence.2020.01.001
56. CE, SMS . Helping others helps oneself: response shift effects in peer support. Soc Sci Med. (1999) 48:1563–75. doi: 10.1016/S0277-9536(99)00049-0
57. MA, SCS . Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. (1999) 48:1507–15. doi: 10.1016/S0277-9536(99)00045-3
58. Ciocanel, O, Power, K, Eriksen, A, and Gillings, K. Effectiveness of positive youth development interventions: a meta-analysis of randomized controlled trials. J Youth Adolesc. (2016) 46:483–504. doi: 10.1007/s10964-016-0555-6
59. Berger, R, Benatov, J, Cuadros, R, VanNattan, J, and Gelkopf, M. Enhancing resiliency and promoting prosocial behavior among Tanzanian primary-school students: a school-based intervention. Transcult Psychiatry. (2018) 55:821–45. doi: 10.1177/1363461518793749
60. Fehr, E, and Fischbacher, U. The nature of human altruism. Nat Rev Neurosci. (2003) 425:785–91. doi: 10.1038/nature02043
61. Flynn, E, Ehrenreich, SE, Beron, KJ, and Underwood, MK. Prosocial behavior: long-term trajectories and psychosocial outcomes. Soc Dev. (2015) 24:462–82. doi: 10.1111/sode.12100
62. Memmott-Elison, MK, Holmgren, HG, Padilla-Walker, LM, and Hawkins, AJ. Associations between prosocial behavior, externalizing behaviors, and internalizing symptoms during adolescence: a meta-analysis. J Adolesc. (2020) 80:98–114. doi: 10.1016/j.adolescence.2020.01.012
Keywords: prosocial behavior, anxiety, depression, adolescent, emotion
Citation: Zhang X, Lv T, Leavey G, Zhu N, Li X, Li Y and Chen Y (2023) Does depression affect the association between prosocial behavior and anxiety? A cross-sectional study of students in China. Front. Public Health. 11:1274253. doi: 10.3389/fpubh.2023.1274253
Received: 10 August 2023; Accepted: 27 September 2023;
Published: 10 October 2023.
Edited by:
Stefania Cella, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Marco Scotto Rosato, University of Campania Luigi Vanvitelli, ItalyCopyright © 2023 Zhang, Lv, Leavey, Zhu, Li, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanhua Chen, Y2hlbnloQHNoc3BkancuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.