
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 08 January 2024
Sec. Public Health and Nutrition
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1273594
This article is part of the Research Topic X-raying Zero Hunger (SDG2) Targets in Africa and Other Regions: Progress, Synergies, Opportunities, and Challenges View all 9 articles
Introduction: Undernutrition is a major health concern in many developing countries, and is one of the main health problems affecting children in Ethiopia. Although many children experience multiple relapses following the management of severe acute malnutrition, it is scarcely studied in Ethiopia.
Methods: A community-based cross-sectional study was conducted in Dessie, Kombolcha, and Haik towns among 6-59-month-old children enrolled and discharged from community-based acute malnutrition management (CMAM). The total sample size was 318 children, and data were collected from April 15, 2021, to May 14, 2021. The data were entered into EPI data version 4.4.1 before being exported and analyzed with SPSS version 25 software. A multivariate logistic regression analysis was performed, and a 95% confidence interval and p-value <0.05 were used to identify significantly associated variables. Additionally, the weight-for-height z-score (WHZ) was generated using the WHO Anthro 3.2.2 software.
Result: The overall acute malnutrition relapse after discharge from CMAM was 35.2% (6.6% relapsed to severe acute malnutrition and 28.6% relapsed to moderate acute malnutrition). The following variables were significantly associated with the relapse of acute malnutrition: child age (AOR: 3.08, 95% CI; 1.76, 5.39), diarrhea after discharge (AOR: 2.93, 95%CI; 1.51, 5.69), have not immunized (AOR: 3.05, 95% CI; 1.14, 8.23), MUAC at discharge (AOR: 3.16, 95% CI; 1.56, 6.40), and poorest and poor wealth index (AOR: 3.65, 95% CI; 1.45, 9.18) and (AOR: 2.73, 95% CI; 1.13, 6.59), respectively.
Conclusion: Over one-third of children treated with the CMAM program reverted to SAM or MAM. The age of the child, diarrhea after discharge, lack of immunization, MUAC at discharge (<13 cm), and poor and poorest wealth index were significantly associated with acute malnutrition relapse. Therefore, adequate health education and counseling services are essential for mothers to improve child immunization coverage and maintain adequate hygiene to prevent diarrhea. In addition, further experimental research is needed to investigate the effect of MUAC at discharge on the risk of acute malnutrition relapse.
Malnutrition in children refers to deficiencies, excesses, or imbalances in the nutrient intake. It addresses three groups of conditions: undernutrition, micronutrient-related malnutrition, and overweight or obesity (1). Malnutrition in children can be either acute (wasting) or chronic (stunting). Based on severity, acute malnutrition can be either moderate acute malnutrition (MAM) or severe acute malnutrition (SAM) (2, 3). Children with SAM are treated either in an outpatient therapeutic program or inpatient setting based on the age of the child, severity of malnutrition and the presence or absence of complications. Subsequently, they will be discharged from the therapeutic program when their weight-for-height/length (WHZ) is > − 2 Z-score, mid-upper-arm circumference (MUAC) is ≥12.5 cm, and there is no edema for at least 2 weeks (4).
Severe acute malnutrition is one of the most common causes of morbidity and mortality among children under 5 years of age worldwide. Children with SAM are 10 times more likely to die than non-malnourished children (5). According to the 2019 estimate, globally, 144 million under-5-year-old children were stunted, 47 million were wasted, and 38 million were overweight. Approximately 45% of deaths among children under 5 years of age are linked to undernutrition (1, 6, 7). Undernutrition is a major health concern in many developing countries, and is one of the main health problems affecting children in Ethiopia. Ethiopia has the second-highest malnutrition rate in sub-Saharan Africa (8). According to the 2016 Ethiopian Demographic and Health Survey, 37% of children under age 5 were stunted, 10% were wasted, 24% were underweight, and 1% were overweight (9).
Relapse after treatment for acute malnutrition is a serious health problem faced by humanitarian and developmental communities (10). Many children experience multiple relapses, and relapsed cases take longer to recover (11). Studies indicate that nearly half of all children who are successfully treated for malnutrition do not maintain their recovery for up to 12 months (12, 13). This situation undermines the cost-effectiveness of community-based management of acute malnutrition (CMAM) treatment programs by deploying limited resources to treat the same child multiple times. Furthermore, repeated episodes of severe acute malnutrition (SAM) increase the risk of death and long-term developmental problems and contributing to a persistently high rate of malnutrition (14).
Globally, the magnitude of malnutrition relapse ranges from 0 to 37%, and in Ethiopia, the re-admission (relapse) rate ranges from 2.6 to 37.5% (15–20). The risk of relapse or death was highest in the 3 months following release from the CMAM, with nearly half of all relapses to either moderate acute malnutrition or SAM occurring during the first 3 months of recovery (11). Child feeding practices, sex, food insecurity, lack of vitamin A supplements, prelacteal feeding, MUAC at discharge, complete vaccination, lower anthropometric measurements, and poor linear growth are the main factors contributing to the relapse of acute malnutrition (13, 21–23).
Recovered children are at a higher risk of acute malnutrition than children who have never been treated for acute malnutrition (20). Hence, identifying factors associated with relapses of acute malnutrition significantly contributes to achieving the national goal of ending all forms of malnutrition in Ethiopia by 2030 (24). However, relapse following treatment of severe acute malnutrition has rarely been measured across programs and research (23). Therefore, this study aimed to assess the prevalence of acute malnutrition relapse and its associated factors among 6–59 month-old children treated in the community-based acute malnutrition management program in Dessie, Kombolcha, and Haik towns.
A community-based cross-sectional study was conducted in Dessie, Kombolcha, and Hiak towns from April 15, 2021, to May 14, 2021.
This study was conducted in Dessie, Kombolcha, and Haik towns. These three towns are found in the South Wollo zone and are located 401, 373, and 426 km away from Addis Ababa, respectively. According to the Ethiopian Statistics Service 2022 population projection report, Dessie, Kombolcha, and Haik towns have a total of 431,004 residents, of whom 214,829 are men and 216,175 are women. Thirteen health centers in these towns (eight in Dessie city administration, four in Kombolcha town, and one in Haik town) deliver outpatient acute malnutrition management (CMAM) services.
All children who were treated in the CMAM program in Dessie, Kombolcha, and Haik towns.
All children aged 6 to 59 months who were treated in the CMAM program and discharged 4 to 54 weeks before data collection.
Children who had treatment outcomes other than recovery (defaulters, lost to follow-up, transfer out), and those with insufficient address information were excluded from the study.
The study included all (356) children who were treated for acute malnutrition in Dessie, Kombolcha, and Haik town health centers and were discharged within 4–54 weeks before the survey. Regarding the sampling procedure, the address information (Kebele, Ketene, name and sex of the child, name of the mother, and phone number) and baseline information about the treatment were obtained from the CMAM logbook. Health extension workers approached mother/caregiver at home. Confirmation of the study subjects was done by asking for the name, age, and sex of the child. Furthermore, the mother/caregiver confirmed that the child was enrolled in the CMAM program at a specified health facility.
Acute malnutrition relapse.
Socio-demographic characteristics: age of the mother, age of the child, education level of the mother, education level of the father, residence, occupation of the mother, and wealth index.
Maternal reproductive health related factors: antenatal care (ANC) follow-up, place of delivery, age of the mother at marriage, family planning, number of children, birth interval, family size and multiple birth.
Child health related factors: diarrhea after management, fever after management, cough after management, chronic diseases, taking anti-helminthic drug, taking Vitamin A and immunization.
Environmental factors: distance from water source, hand hygiene, separate kitchen, and waste disposal.
Child and mother nutrition related factors: taking extra meals during pregnancy, breastfeeding within 1 hour, colostrum feeding, prelacteal feeding, exclusive breast feeding, frequency of breast feeding, separate complementary food preparation, food preparation training, and food aid.
Management related factors: duration of management, MUAC at discharge, WHZ at discharge, and duration (weeks) after discharge.
Acute malnutrition: MUAC <12.5 cm and/or WHZ <−2.
Severe acute malnutrition: MUAC <11.5 cm and/or presence of bilateral edema and/or WFL/H < −3, no medical complication and pass appetite test.
Moderate acute malnutrition: WHZ ≥ −3 Z-score to <−2 Z-score or MUAC ≥ 11.5 cm to <12.5 cm and no edema of both feet.
Relapse: MUAC <12.5 cm (both SAM and MAM) and/or bilateral edema and/or WHZ < −2 following discharge from the CMAM program.
Protected water source: water source from the pipe or modern well.
Food preparation training: mothers/caretakers who have received training in food preparation for children from health professionals, health extension workers, etc.
Wealth index: it was categorized into four quintiles (five groups), namely: poorest, poor, medium, rich, and richest, based on principal component analysis (PCA).
Data were collected using a semi-structured questionnaire designed after reviewing related articles (21–23, 25–37). Information related to the treatment and address of the participants was collected from the malnutrition registration logbook and medical records. After obtaining the address information, health extension workers accessed the participants and recorded the child’s current nutritional status and other related data. The weight of the children was measured using a well-calibrated, portable digital weight scale. A portable stadiometer was used to measure the height of the child, and an infantometer was used to measure the length of children under the age of two. MUAC of the child was measured using non-stretchable tape snugly at the midpoint of the arm. The wealth index was computed using fifteen items from the standard equity tool (38). The data were collected by nine trained health extension workers for four weeks and supervised by three MSc pediatric nursing professionals.
Data quality was ensured through the training of data collectors, regular supervision, immediate feedback, and spot-checking. Moreover, supervisors and principal investigators checked the completeness of the collected data daily. Pretesting of the questionnaire was undertaken on 5% (16) of the final sample size in Kutaber town.
All filled questionnaires were checked for completeness, consistency, and accuracy. The data were then entered into EPI data (version 4.4.1.0) and exported to SPSS version 25 software for analysis. Descriptive statistics (frequency table, pie chart, and bar graph) were performed to summarize the data. WHZ were generated using WHO Anthro software 3.2.2. Bivariate logistic regression was used to check variables associated with acute malnutrition relapse. Variables found to have a p-value ≤0.2 were further analyzed using multivariate logistic regression. Crude and adjusted odds ratio with 95% CI were computed, and variables that had a p-value <0.05 in the multivariate logistic regression were considered as significantly associated with the dependent variable. Furthermore, the model fitness was checked using the Hosmer and Lemeshow goodness-of-fit test, which gave a p-value of 0.28.
In the study areas, there were a total of 356 children treated for acute malnutrition and discharged within 4–54 weeks before the survey. Among those treated children, 318 were accessed and included in the analysis (Figure 1). The majority (59.1%) of mothers/caretakers were aged 25–34 years, with a mean ± SD of 30 ± 5.5 years. Over half (54.4%) of children were male and 49.7% were aged ≥24 months, with a mean ± SD of 27.9 ± 14 months. Nearly three-fourths (72.6%) of mothers/caretakers were housewives, 89.3% were married, 7.2% had a college or university education, and 88.7% were urban dwellers. Nearly one-third (31.4%) of fathers were daily laborers, 34% had primary education, and 22.3% of families had the lowest wealth index (Table 1).
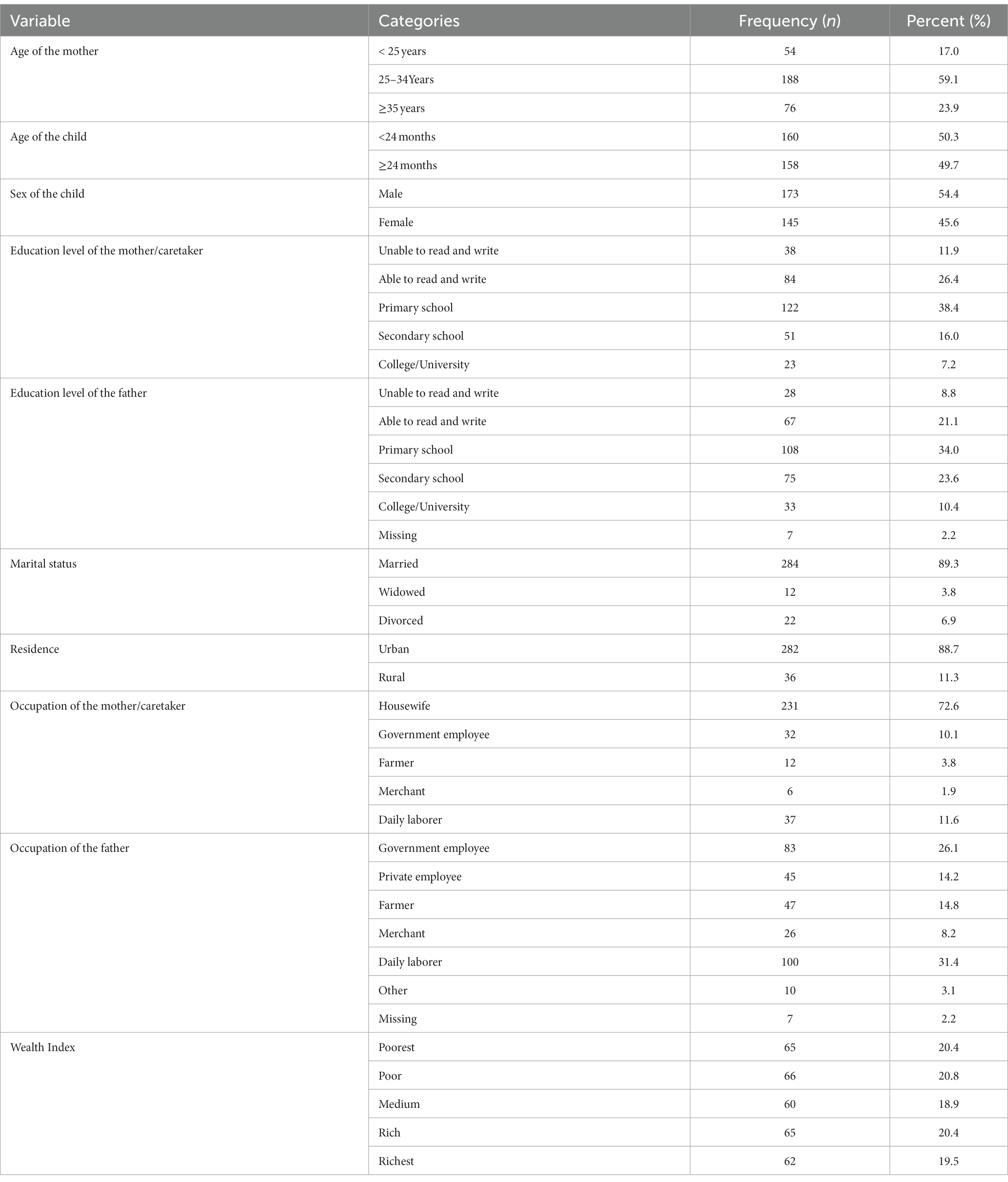
Table 1. Socio-demographic characteristics of the study participants in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia (N = 318).
The vast majority (91.2%) of mothers attended ANC, 94% delivered in health facilities, and 72.6% utilized family planning at the time of data collection. One-fourth (23.9%) of children had diarrhea, 24.2% had fever, and 27.4% had cough after malnutrition treatment. Almost all children (98.1%) had no chronic disease, 31.1% took anthelmintic drugs, 87.7% took vitamin A, and 84.3% were immunized according to the schedule. The birth interval for half of the mothers (49.7%) was more than 2 years, 39.3% of the households had five people, and 97.2% of the deliveries were singletons. A quarter of the households (23%) had a round-trip of more than 30 min to fetch water, 85.2% had a separate kitchen, and 9.4% disposed waste in an open field (Table 2).
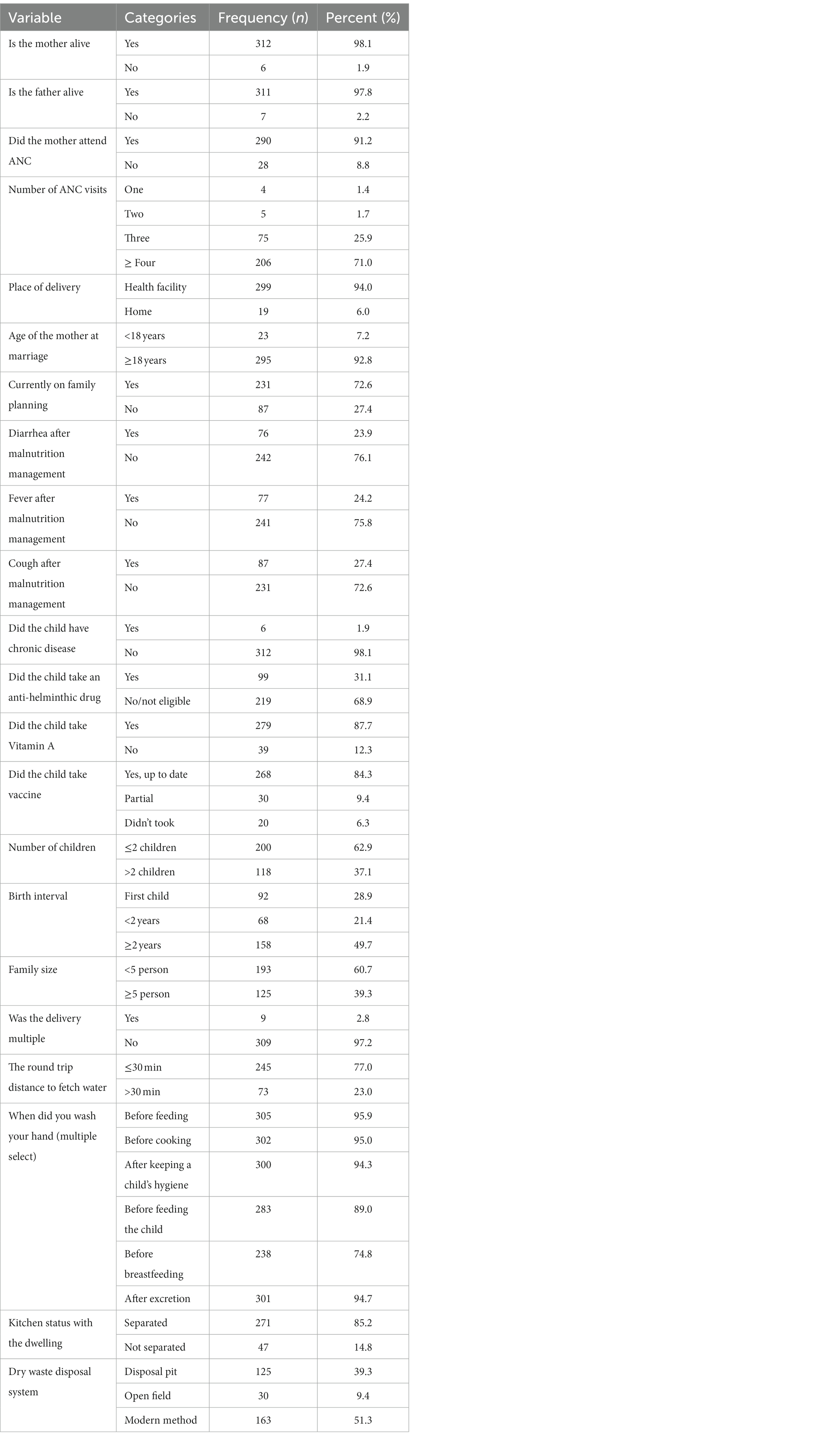
Table 2. Participant and environmental -related characteristics in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia (N = 318).
One-fourth (26.7%) of mothers ate extra meals while pregnant, 88.1% of children received colostrum, 91.2% exclusively breastfed for 6 months, and 84% of mothers/caregivers prepared food separately for the child. Almost one-tenth of the children (10.7%) received malnutrition treatment for 4 weeks, 26.1% had MUAC measurements of 13 cm, and 89.6% had a WHZ of −2 at discharge (Table 3). During the assessment, 3.8% of children had a MUAC measurement of <11.5 cm, 4.1% had a WHZ score of <−3, and 35.2% (95% CI; 29.9, 40.6%) of children had acute malnutrition (Figures 2, 3).
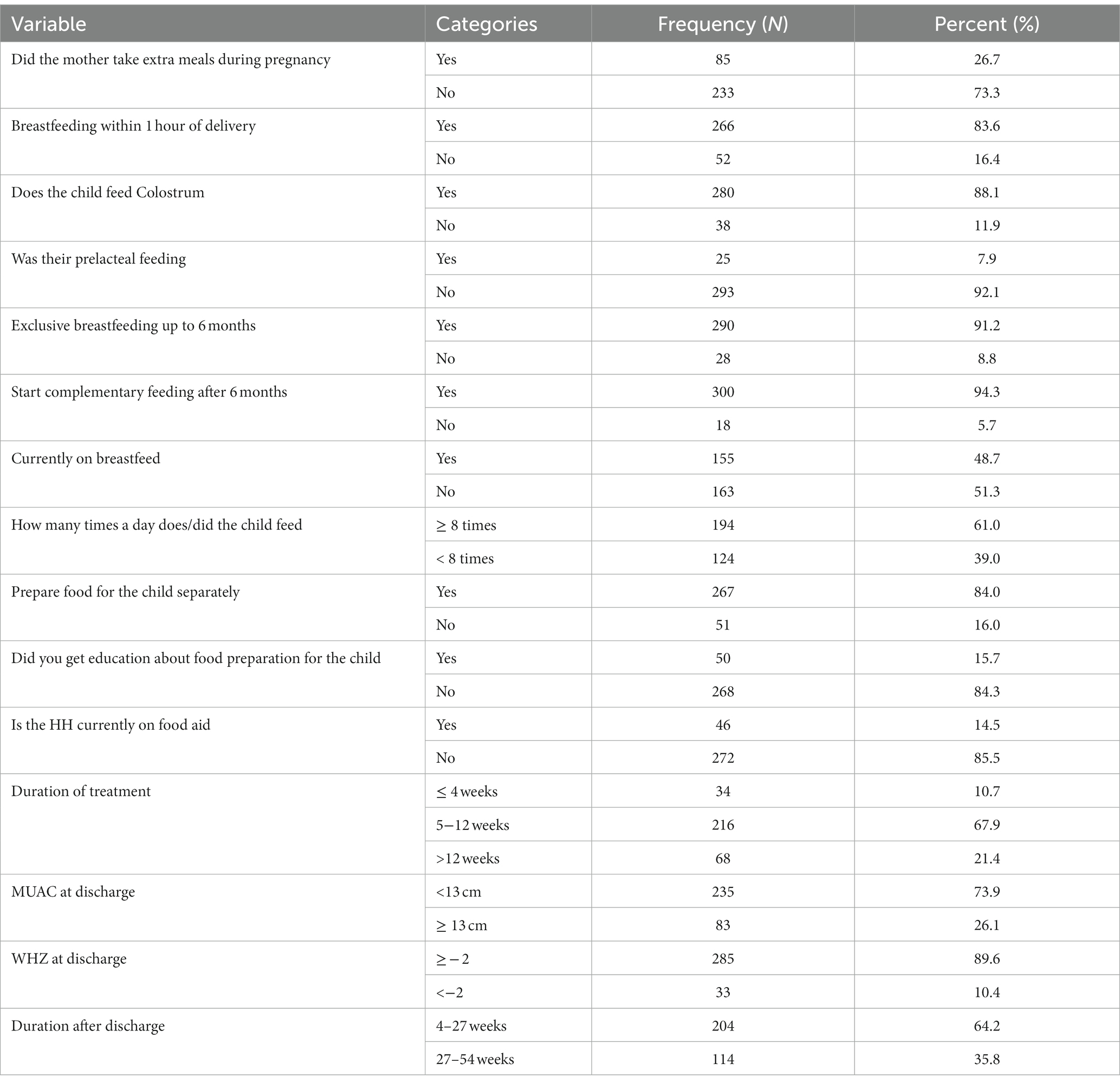
Table 3. Nutritional characteristics of the study participants in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia (N = 318).
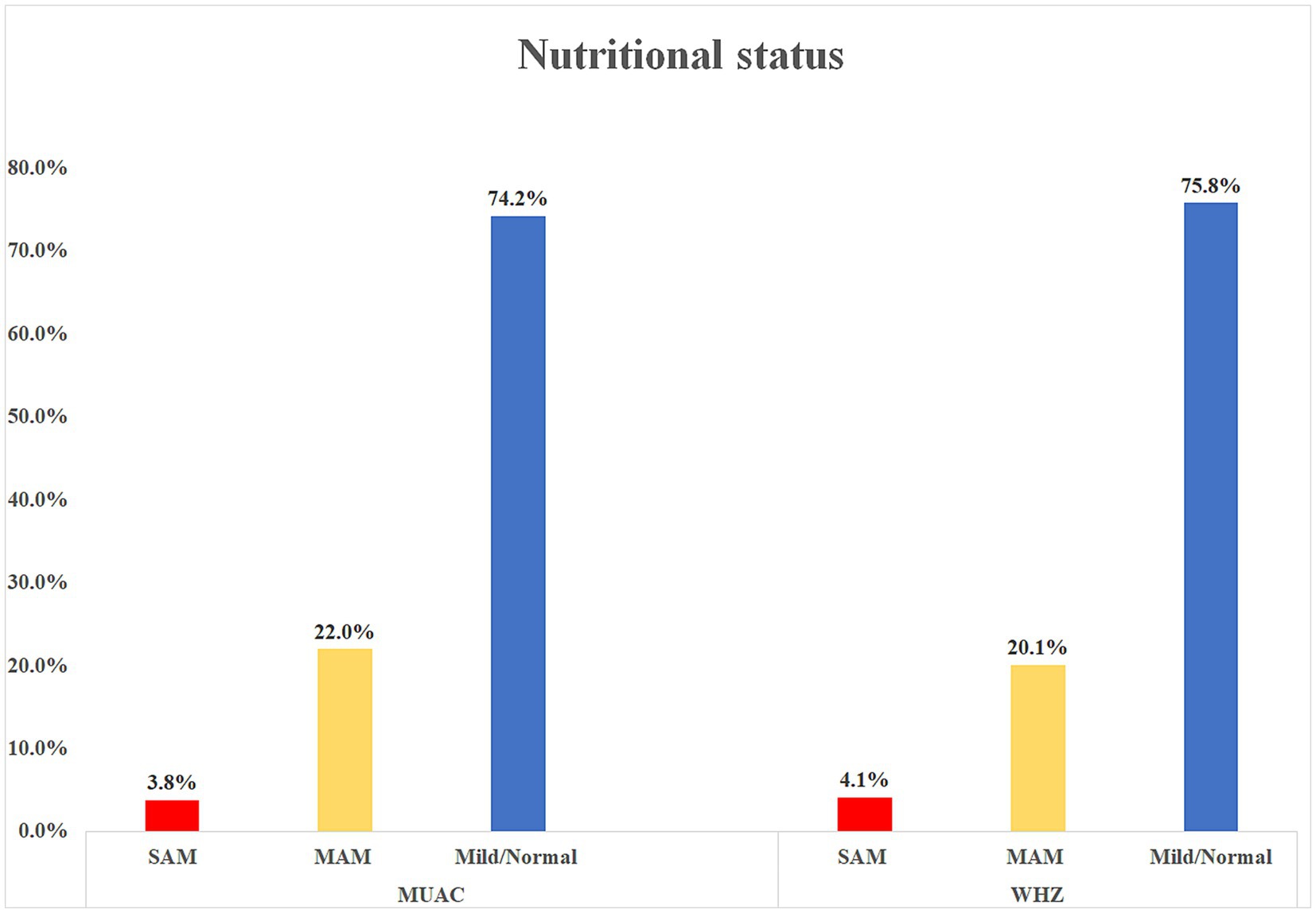
Figure 2. Nutritional status of children using MUAC and WHZ measurements in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia (N = 318).
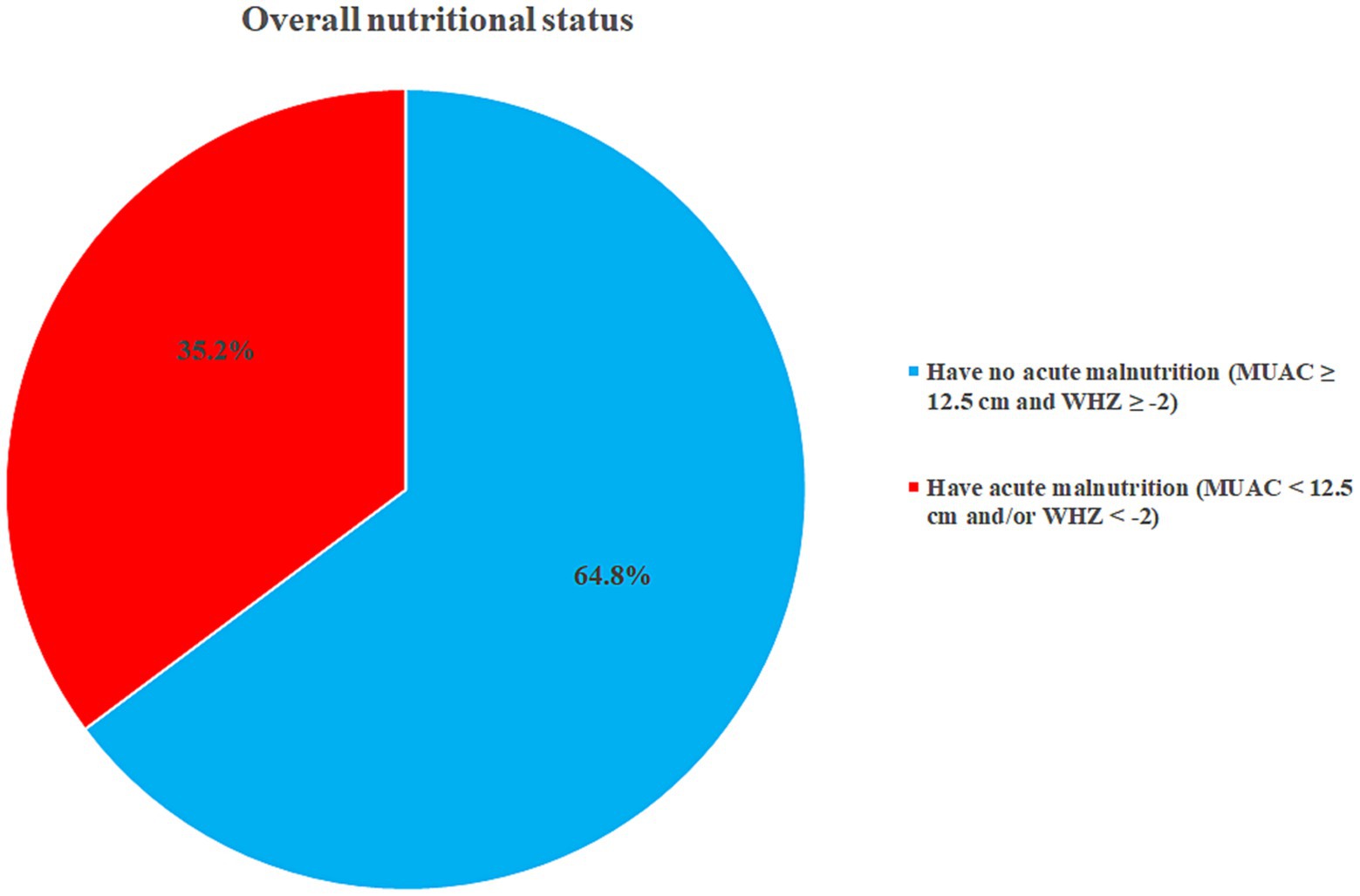
Figure 3. Overall nutritional status of children in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia (N = 318).
In the bivariate logistic regression, the age of the child, educational level of the mother, diarrhea after management, immunization status, birth space, MUAC at discharge, WHZ at discharge, duration after discharge, and wealth index had a p-value of ≤0.2. Further analysis of these variables in the multivariable logistic regression revealed that age of the child, immunization status, diarrhea after management, MUAC at discharge, and wealth index had a significant association with acute malnutrition relapse.
Children aged <24 months had higher odds of acute malnutrition relapse compared to ≥24 months-old children (AOR: 3.08, 95% CI; 1.76, 5.39). Likewise, children who had diarrhea after management were more likely to experience malnutrition relapse than those who did not (AOR: 2.93, 95% CI; 1.51, 5.69). Additionally, children who were not immunized had higher odds of acute malnutrition relapse than those children with full immunization (AOR: 3.05, 95% CI; 1.14, 8.23). Furthermore, children with a discharge MUAC of <13 cm had a higher risk of acute malnutrition relapse than those with a MUAC of ≥13 cm (AOR: 3.16, 95% CI: 1.56, 6.40). Finally, children from the poorest and poor families had higher odds of developing acute malnutrition relapse compared to children from the richest families [(AOR: 3.65, 95% CI; 1.45, 9.18) and (AOR: 2.73, 95% CI; 1.13, 6.59), respectively] (Table 4).
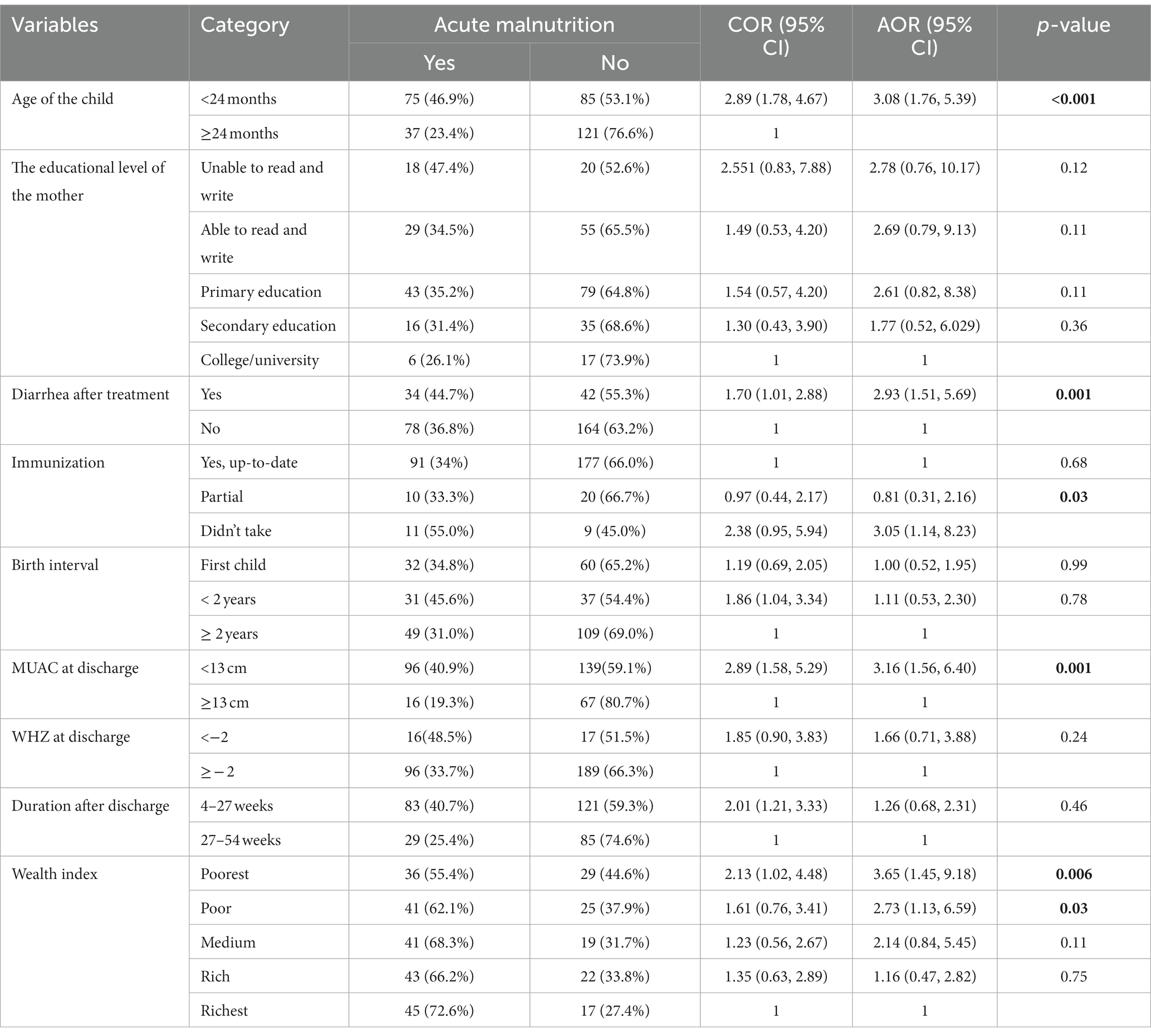
Table 4. Factors associated with acute malnutrition relapse in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia (N = 318).
According to the findings of this study, the prevalence of overall acute malnutrition relapse among children treated in the CMAM program was 35.2% (95% CI, 30.2, 41.5%). 6.6% of the relapsed cases were SAM and 28.6% were MAM, indicating that more than one-fourth of the treated children had returned to MAM. Other studies conducted in Gambella region and Hadiya zone indicated a 10.1 and 9.6% relapse to SAM, respectively which is higher than the relapse reported in this study (6.6%) (39, 40). The discrepancy might be attributed to variations in the study design, setting and cultural and sociodemographic diferences. On the other side, comparable findings of overall acute malnutrition relapse were reported from studies conducted in Malawi (41%), Eastern Ethiopia (36.2%) and South Gondar, Ethiopia (34.3%) (11, 20, 41). However, studies in Burkina Faso (15.4%), a systematic review of low and middle-income countries (27.5%), and the United States (27%), all found a lower prevalence of relapse (22, 28, 42). To the contrary, a higher magnitude of relapse was reported from the study in the Democratic Republic of the Congo (44.2%) (43). These discrepancies might be attributed to the variations in the study design, duration of follow-up, study setting, and cultural and economic factors.
One of the significantly associated variables with the relapse of acute malnutrition was the child’s age. Children aged <24 months had higher odds of acute malnutrition relapse compared to children older than ≥24 months. Children under the age of two require more nutrition and energy for growth and development than at any other stage in their lives, making them more vulnerable to malnutrition (44). Similar studies from Nepal and Nigeria also reported that the age of children had an association with malnutrition (45, 46).
In this study, having diarrhea after discharge from malnutrition management was significantly associated with acute malnutrition relapse. Children who had diarrhea after discharge had higher odds of acute malnutrition relapse compared to children without diarrhea. Diarrhea contributes to malnutrition by reducing food intake, decreasing nutrient absorption, and increasing nutrient catabolism (47). This finding is consistent with other studies undertaken in Ethiopia (48) and Nigeria (49).
The immunization status of children had a significant association with acute malnutrition relapse. Children who were not immunized experienced a higher occurrence of acute malnutrition relapse compared to fully vaccinated children. Immunization protects children from a wide range of illnesses, including pneumonia and diarrhea, which can put them at risk of malnutrition. A significantly higher prevalence of malnutrition was found among children with incomplete vaccinations (50). Research findings in this regard illustrate the relationship between vaccination and nutritional status (50, 51).
Furthermore, the MUAC measurement of children at discharge showed significant associations with acute malnutrition relapse. Children with a MUAC measurement of <13 cm were more likely to have an acute malnutrition relapse compared to children with a MUAC measurement of ≥13 cm. Adequate nutritional achievement before discharge might enable the child to sustain their nutritional status. A similar study from Ethiopia and Nigeria also reported that the discharge MUAC of children was a significant predictor of relapse (40, 46).
Finally, the wealth index was reported to have a significant association with acute malnutrition relapse. Children from the poorest families had higher odds of developing an acute malnutrition relapse compared to children from the richest families. Poverty and malnutrition are deeply interrelated, and low socioeconomic status remains one of the most important predictors of child malnutrition (52). Related studies from India (53), Ethiopia (27, 54), and Bangladesh (55) reported similar results.
This study addresses the gross acute malnutrition relapses from 1 to 12 months following CMAM treatment. It did not figure out the relapse rate in relation to various periods. Therefore, further large-scale prospective cohort studies are needed to describe the relapse rate in various periods. Moreover, given that the study used a cross-sectional design, the associations observed in the study do not infer a causal relationship, and there might be recall biases for certain items.
Over one-third of children treated under the CMAM program reverted to SAM or MAM. The age of the child, diarrhea after discharge, immunization, MUAC at discharge, and wealth index were all significantly associated variables with acute malnutrition relapse. Therefore, adequate health education and counseling services are required for mothers to improve child immunization coverage and maintain adequate hygiene to prevent diarrhea. In addition, further experimental research is needed to investigate the effect of MUAC at discharge on the risk of acute malnutrition relapse.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical clearance and approval (RF: CMHS/47/13/13) were obtained from Wollo University College of Medicine and Health Sciences. Official letters were written to the respective health facilities and town administrations. Consent to review the medical records of study subjects was waived by the authorities of health facilities. Written informed consent was obtained from the mother/caretaker after thoroughly explaining the objectives of the study and the data were analyzed anonymously. Respondents had the right to not participate in or withdraw from the study at any stage, and compliance with the Declaration of Helsinki was ensured.
YY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZY: Investigation, Project administration, Software, Supervision, Validation, Visualization, Writing – review & editing. SN: Data curation, Investigation, Project administration, Supervision, Validation, Visualization, Writing – review & editing. DJ: Formal analysis, Investigation, Software, Supervision, Validation, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to acknowledge Wollo University for providing us with the opportunity to conduct this research project. Then we would like to express our deepest gratitude to all of the study participants, data collectors, and supervisors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ANC, Antenatal care; AOR; Adjusted odds ratio CI, Confidence interval; CMAM, Community based management of acute malnutrition; COR, Crude odds ratio; MAM, Moderate acute malnutrition; MUAC, Middle upper arm circumference; OR, Odds ratio; SAM, Sever acute malnutrition; SPSS, Statistical package for social science; WHZ, Weight for height Z-score.
1. WHO. Fact sheets - malnutrition - World Health Organization Available at: https://wwwwhoint/news-room/fact-sheets/detail/malnutrition
2. Organization WH. WHO child growth standards and the identification of severe acute malnutrition in infants and children: Joint statement by the World Health Organization and the United Nations Children's fund. Geneva: WHO (2009).
3. Action_agianst_hunger. Types of acute malnutrition - action against hunger. Available at: https://actionagainsthungerca/what-is-acute-malnutrition/types-of-acute-malnutrition/
4. Organization WH. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization (2013).
5. WHO. Children: Reducing mortality - World Health Organization. Available at: https://wwwwhoint/news-room/fact-sheets/detail/children-reducing-mortality
6. WHO. WHO | child malnutrition. available at: https://wwwwhoint/gho/child-malnutrition/en/
7. ACPF. For lack of will: Child hunger in Africa. Addis Ababa: African Child Policy Forum (ACPF) (2019).
8. OpenLearnCreate. Nutrition: 6. Common nutritional problems in Ethiopia. Available at: https://wwwopenedu/openlearncreate/mod/oucontent/viewphp?id=319&printable=1
9. EDHS E. Demographic and health survey 2016: Key indicators report, vol. 363. Reston, VA: The DHS Program ICF (2016). 364 p.
10. Stobaugh, HC, Rogers, BL, Webb, P, Rosenberg, IH, Thakwalakwa, C, Maleta, KM, et al. Household-level factors associated with relapse following discharge from treatment for moderate acute malnutrition. Br J Nutr. (2018) 119:1039–46. doi: 10.1017/S0007114518000363
11. Stobaugh, H, and Manary, M. Relapse after treatment for moderate acute malnutrition: Risk factors and interventions to prevent it, vol. 64. Tipperary: Field Exchange (2018).
12. RTI. New studies identify key factors to relapse of malnourished children in developing countries. Available at: https://wwwrtiorg/announcements/new-studies-identify-key-factors-relapse-malnourished-children-developing-countries
13. Stobaugh, HC, Rogers, BL, Rosenberg, IH, Webb, P, Maleta, KM, Manary, MJ, et al. Children with poor linear growth are at risk for repeated relapse to wasting after recovery from moderate acute malnutrition. J Nutr. (2018) 148:974–9. doi: 10.1093/jn/nxy033
14. Action_agianst_hunger. Relapse study - knowledge against hunger. Available at: http://wwwactionagainsthungerorg/research/sam-relapse
15. Fikrie, A, Alemayehu, A, and Gebremedhin, S. Treatment outcomes and factors affecting time-to-recovery from severe acute malnutrition in 6–59 months old children admitted to a stabilization center in southern Ethiopia: a retrospective cohort study. Ital J Pediatr. (2019) 45:46. doi: 10.1186/s13052-019-0642-x
16. Mengesha, MM, Deyessa, N, Tegegne, BS, and Dessie, Y. Treatment outcome and factors affecting time to recovery in children with severe acute malnutrition treated at outpatient therapeutic care program. Glob Health Action. (2016) 9:30704. doi: 10.3402/gha.v9.30704
17. Shanka, N, Lemma, S, and Abyu, D. Recovery rate and determinants in treatment of children with severe acute malnutrition using outpatient therapeutic feeding program in Kamba District, south West Ethiopia. J Nutr Disord Ther. (2015) 5:155. doi: 10.4172/2161-0509.1000155
18. Yohannes, T, Laelago, T, Ayele, M, and Tamrat, T. Mortality and morbidity trends and predictors of mortality in under-five children with severe acute malnutrition in Hadiya zone, South Ethiopia: a four-year retrospective review of hospital-based records (2012–2015). BMC Nutr. (2017) 3:18. doi: 10.1186/s40795-017-0135-5
19. Dubale, S, Negash, E, and Shuramu, M. Treatment outcomes and determinant factors of under-five children with malnutrition treated in Ilu aba Bor zone health facilities, south West Ethiopia. Biomed J Sci Tech Res. (2019) 20:14888–95. doi: 10.26717/BJSTR.2019.20.003425
20. Abitew, DB, Worku, A, Mulugeta, A, and Bazzano, AN. Rural children remain more at risk of acute malnutrition following exit from community based management of acute malnutrition program in South Gondar zone, Amhara region, Ethiopia: a comparative cross-sectional study. Peer J. (2020) 8:e8419. doi: 10.7717/peerj.8419
21. Abitew, DB, Yalew, AW, Bezabih, AM, and Bazzano, AN. Predictors of relapse of acute malnutrition following exit from community-based management program in Amhara region, Northwest Ethiopia: an unmatched case-control study. PLoS One. (2020) 15:e0231524. doi: 10.1371/journal.pone.0231524
22. Somassè, YE, Dramaix, M, Bahwere, P, and Donnen, P. Relapses from acute malnutrition and related factors in a community-based management programme in B urkina F Aso. Matern Child Nutr. (2016) 12:908–17. doi: 10.1111/mcn.12197
23. Stobaugh, HC, Mayberry, A, McGrath, M, Bahwere, P, Zagre, NM, Manary, MJ, et al. Relapse after severe acute malnutrition: a systematic literature review and secondary data analysis. Matern Child Nutr. (2019) 15:e12702. doi: 10.1111/mcn.12702
24. scalingupnutrition.org. Ethiopia commit to ending undernutrition by 2030 with the Seqota declaration. Available at: http://scalingupnutritionorg/news/ethiopia-commit-to-ending-under-nutrition-by-2030-with-the-seqota-declaration/
25. Dereje, N. Determinants of severe acute malnutrition among under five children in Shashogo Woreda, southern Ethiopia: a community based matched case control study. J Nutr Food Sci. (2014) 4:300. doi: 10.4172/2155-9600.1000300
26. Awoke, A, Ayana, M, and Gualu, T. Determinants of severe acute malnutrition among under five children in rural Enebsie Sarmidr District, east Gojjam zone, north West Ethiopia, 2016. BMC Nut. (2018) 4:4. doi: 10.1186/s40795-018-0211-5
27. Tekile, AK, Woya, AA, and Basha, GW. Prevalence of malnutrition and associated factors among under-five children in Ethiopia: evidence from the 2016 Ethiopia demographic and health survey. BMC Res Notes. (2019) 12:391. doi: 10.1186/s13104-019-4444-4
28. O’Sullivan, NP, Lelijveld, N, Rutishauser-Perera, A, Kerac, M, and James, P. Follow-up between 6 and 24 months after discharge from treatment for severe acute malnutrition in children aged 6-59 months: a systematic review. PloS one. (2018) 13:e0202053. doi: 10.1371/journal.pone.0202053
29. Ayana, AB, Hailemariam, TW, and Melke, AS. Determinants of acute malnutrition among children aged 6–59 months in public hospitals, Oromia region, West Ethiopia: a case–control study. BMC Nut. (2015) 1:34. doi: 10.1186/s40795-015-0031-9
30. Asres, DT, Prasad, RP, and Ayele, TA. Recovery time and associated factors of severe acute malnutrition among children in Bahir Dar city, Northwest Ethiopia: an institution based retrospective cohort study. BMC Nut. (2018) 4:17. doi: 10.1186/s40795-018-0224-0
31. Asfaw, M, Wondaferash, M, Taha, M, and Dube, L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. (2015) 15:41. doi: 10.1186/s12889-015-1370-9
32. Abuka, T, Jembere, D, and Tsegaw, D. Determinants for acute malnutrition among under-five children at public health facilities in Gedeo zone, Ethiopia: a case-control study. Pediatr Ther. (2017) 7:1000317. doi: 10.4172/2161-0665.1000317
33. Mena, MB, Dedefo, MG, and Billoro, BB. Treatment outcome of severe acute malnutrition and its determinants among pediatric patients in West Ethiopia. Int J Pediatr. (2018) 2018:1–7. doi: 10.1155/2018/8686501
34. Seid, A, Seyoum, B, and Mesfin, F. Determinants of acute malnutrition among children aged 6–59 months in public health facilities of pastoralist community, Afar region, Northeast Ethiopia: a case control study. J Nutr Metab. (2017) 2017:1–7. doi: 10.1155/2017/7265972
35. Hassen, SL, Astatkie, A, Mekonnen, TC, and Bogale, GG. Survival status and its determinants among under-five children with severe acute malnutrition admitted to inpatient therapeutic feeding centers in south Wollo zone, Amhara region, Ethiopia. J Nutr Metab. (2019) 2019:1–9. doi: 10.1155/2019/2643531
36. Massa, D, Woldemichael, K, Tsehayneh, B, and Tesfay, A. Treatment outcome of severe acute malnutrition and determinants of survival in northern Ethiopia: a prospective cohort study. Int. J Nutr Metab. (2016) 8:12–23. doi: 10.5897/IJNAM2015.0193
37. Chang, CY, Trehan, I, Wang, RJ, Thakwalakwa, C, Maleta, K, Deitchler, M, et al. Children successfully treated for moderate acute malnutrition remain at risk for malnutrition and death in the subsequent year after recovery. J Nutr. (2013) 143:215–20. doi: 10.3945/jn.112.168047
38. Ethiopia. Ethiopia - equity tool. Available at: https://www.equitytool.org/wp-content/uploads/2018/01/Ethiopia-DHS-2016-2nd-survey-EquityTool_2018.01.05.pdf
39. Teshale, EB, Nigatu, YD, and Delbiso, TD. Relapse of severe acute malnutrition among children discharged from outpatient therapeutic program in western Ethiopia. BMC Pediatr. (2023) 23:441. doi: 10.1186/s12887-023-04269-7
40. Lambebo, A, Temiru, D, and Belachew, T. Frequency of relapse for severe acute malnutrition and associated factors among under five children admitted to health facilities in Hadiya zone, South Ethiopia. PloS One. (2021) 16:e0249232. doi: 10.1371/journal.pone.0249232
41. Alyi, M, Roba, KT, Ketema, I, Habte, S, Goshu, AT, Mehadi, A, et al. Relapse of acute malnutrition and associated factors after discharge from nutrition stabilization centers among children in eastern Ethiopia. Front Nutr. (2023) 10:1095523. doi: 10.3389/fnut.2023.1095523
42. Manary, M. Relapse after treatment of MAM: Should we be concerned? Are we using our resources well? Vienna: International Atomic Energy Agency (2014).
43. Grellety, E, Babakazo, P, Bangana, A, Mwamba, G, Lezama, I, Zagre, NM, et al. Effects of unconditional cash transfers on the outcome of treatment for severe acute malnutrition (SAM): a cluster-randomised trial in the Democratic Republic of the Congo. BMC Med. (2017) 15:87. doi: 10.1186/s12916-017-0848-y
44. Feng, J, Gong, Z, Wang, Y, Huo, J, and Zhuo, Q. Complementary feeding and malnutrition among infants and young children aged 6–23 months in rural areas of China. Nutrients. (2022) 14:1807. doi: 10.3390/nu14091807
45. Ghimire, U, Aryal, BK, Gupta, AK, and Sapkota, S. Severe acute malnutrition and its associated factors among children under-five years: a facility-based cross-sectional study. BMC Pediatr. (2020) 20:249–9. doi: 10.1186/s12887-020-02154-1
46. Bliznashka, L, Grantz, KH, Botton, J, Berthé, F, Garba, S, Hanson, KE, et al. Burden and risk factors for relapse following successful treatment of uncomplicated severe acute malnutrition in young children: secondary analysis from a randomised trial in Niger. Matern Child Nutr. (2022) 18:e13400. doi: 10.1111/mcn.13400
47. Nel, E. Diarrhoea and malnutrition. South Afr J Clin Nutr. (2010) 23:15–8. doi: 10.1080/16070658.2010.11734262
48. Girma, T, James, PT, Abdissa, A, Luo, H, Getu, Y, Fantaye, Y, et al. Nutrition status and morbidity of Ethiopian children after recovery from severe acute malnutrition: prospective matched cohort study. PLoS One. (2022) 17:e0264719. doi: 10.1371/journal.pone.0264719
49. Adegoke, O, Arif, S, Bahwere, P, Harb, J, Hug, J, Jasper, P, et al. Incidence of severe acute malnutrition after treatment: a prospective matched cohort study in Sokoto, Nigeria. Matern Child Nutr. (2021) 17:e13070. doi: 10.1111/mcn.13070
50. Solis-Soto, MT, Paudel, D, and Nicoli, F. Relationship between vaccination and nutritional status in children. Demogr Res. (2020) 42:1–14. doi: 10.4054/DemRes.2020.42.1
51. Shinsugi, C, and Mizumoto, A. Associations of nutritional status with full immunization coverage and safe hygiene practices among Thai children aged 12–59 months. Nutrients. (2021) 14:34. doi: 10.3390/nu14010034
52. Siddiqui, F, Salam, RA, Lassi, ZS, and Das, JK. The intertwined relationship between malnutrition and poverty. Front Public Health. (2020) 8:453. doi: 10.3389/fpubh.2020.00453
53. Olwedo, MA, Mworozi, E, Bachou, H, and Orach, CG. Factors associated with malnutrition among children in internally displaced person\'s camps, northern Uganda. Afr Health Sci. (2008) 8:244–52.
54. Abate, KH, and Belachew, T. Chronic malnutrition among under five children of Ethiopia may not be economic. A systematic review and meta-analysis. Ethiop J Health Sci. (2019) 29:265–77. doi: 10.4314/ejhs.v29i2.14
Keywords: relapse, acute malnutrition, CMAM, under-five, associated factors, Ethiopia
Citation: Yitayew YA, Yalew ZM, Nebiyu S and Jember DA (2024) Acute malnutrition relapse and associated factors among 6–59 months old children treated in the community-based management of acute malnutrition in Dessie, Kombolcha, and Haik towns, Northeast Ethiopia. Front. Public Health. 11:1273594. doi: 10.3389/fpubh.2023.1273594
Received: 03 October 2023; Accepted: 11 December 2023;
Published: 08 January 2024.
Edited by:
Oluwaseun Ariyo, University of Ibadan, NigeriaReviewed by:
Olukunmi Omobolanle Balogun, St. Luke's International University, JapanCopyright © 2024 Yitayew, Yalew, Nebiyu and Jember. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yibeltal Asmamaw Yitayew, eWliaWUuYXNtYW1hdzIxQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.