- 1Department of Health Sciences, University of Catanzaro “Magna Gracia”, Catanzaro, Italy
- 2Department of Experimental Medicine, University of Campania “Luigi Vanvitelli”, Naples, Italy
- 3Department of Pharmacy, Health and Nutritional Sciences, University of Calabria, Arcavacata of Rende, Cosenza, Italy
Introduction: This study explored the quality of sleep among university students in the South of Italy during the Covid-19 pandemic.
Methods: A cross-sectional study was conducted between March 2022 and January 2023 and involved students over the age of 18, who were invited to complete a self-administered questionnaire using an online application.
Results: Overall, 88% of men and 94.5% of women had Pittsburgh Sleep Quality Index (PSQI) scores of ≥5 and a mean PSQI score of 9.2 ± 3. Students with severe or extremely depression score, with sever or extremely stress score, male and who did not had Covid-19 infection were more likely to have a PSQI global score. Moreover, 62.6% of the students declared a reduction in social relations and 72.3% an increase in the use of social media during the pandemic period. The majority of respondents reported an extremely severe level of depression (68.1%), anxiety (84.4%) and stress (71.9%).
Conclusion: This finding indicate that a relevant percentage of students are poor sleepers with a higher overall PSQI score with depression and stress and underline the role the implementation of public health interventions to promote healthy life styles and in particular focus on the duration of long night sleep.
1 Introduction
It is well established that sleep is regulated by a set of physiologic and genetic processes, nonetheless many sleep behaviors are influenced by social, subjective and environmental factors. Generally, sleep occupies 20–40% of people’s days and good sleep patterns are markers of a well-off social status (1, 2).
Sleep disorders have a high prevalence in the general population (3) and have been found to be associated with obesity, weight disorders and metabolic syndrome (4, 5). Nonetheless there is evidence that people are not conscious and aware of the impact of these problems in daily routine (6). Quality of sleep, indeed, is associated with mental disorders and, together, these conditions are public health challenges because both of them have an important impact on individual and global wellness (6–9). Several studies have shown an association between inadequate sleep and frequent mental disorders and lack of sleep negatively affects health (10, 11). In particular, sleep quality and mental disorders have a bidirectional relationship over the life course (12), indeed, poor sleep quality is described as a significant predictor for the onset of depression, anxiety, alcohol abuse and psychosis (13, 14).
Although research most commonly focuses on the associations between insomnia and depression and anxiety, there is also evidence that problems of sleeping are associated with a variety of mental disorders. For example, poor sleep has also been associated with posttraumatic stress or eating disorders (15, 16). Relationship between sleep and mental disorder represents a potentially modifiable risk factor instead of a symptom–disease relationship (9).
In recent years, Covid-19 has changed sleep patterns, representing a source of stress (17, 18). The global effects of these factors are still unknown, on the one hand Covid-19 seems to have had negative effects on the sleep health, while conversely others have benefited of increased sun exposure and increased sleep during the pandemic (19–21). At the same time, quarantine reduced the daylight time for some people, influencing the synchronization of the circadian body clock, consequently worsening many people’s sleep and mood (22, 23). Moreover, during the first waves of pandemic, poor knowledge about Covid-19 has been associated with poor quality of sleep (24).
The determinants of sleep quality, including socio-demographic characteristics, behavioral and lifestyle factors, and mental health status had been largely explored in the literature, especially among university students (25, 26). To our knowledge, no studies had been conducted on the quality of sleep and mental disorders among university students from Southern of Italy during the Covid-19 pandemic. To address this research gap, the Theory of Unpleasant Symptoms (TOUS) has been employed (27). Following the TOUS, indeed, three categories of factors can influence the quality of sleep: physiological, psychological, and situational factors. The research question driving the present study is if quality of sleep of university students has been influenced by Covid-19 pandemic (situational factor), anxiety, stress and depression symptoms (psychological factors), and sleep latency, duration, efficiency and disturbance (physiological factors). Therefore, the aim of this study is to evaluate determinants of sleep quality on university students from Southern Italy in the context of the Covid-19 pandemic.
2 Materials and methods
2.1 Study population, sampling procedure and data collection
A cross-sectional study was conducted between March 2022 and January 2023 and involved students over the age of 18 enrolled at the Magna Graecia University of Catanzaro.
The required sample size was calculated before the beginning of the study, considering a 95% confidence interval, an alpha error of 5%, a response rate 50% and, since previous data were not available, poor sleep quality was assumed in 50% of students (28). Therefore, the minimum sample size was estimated to be 385 participants.
Data were collected anonymously using a self-administered online questionnaire using the Google Forms® online application. Each student was sent the questionnaire link via institutional email, which contained a brief summary of the study’s objectives, so that participants could decide whether to participate or not, and provide informed consent to participate in the survey. Only those who expressed their consent to participate in the survey and completed the questionnaire in all its parts have been included, since the questionnaire allowed to proceed only by completing all the questions before the final transmission. Furthermore, the questionnaire could be sent only once, in order to minimize the potential for repeated responses. Participants did not receive any form of payment or incentive for participating in this study. The study protocol was approved by the Ethics Committee of the Magna Graecia University of Catanzaro (Protocol n.107, 21 April 2022) and was conducted in accordance with the Declaration of Helsinki.
2.2 Survey instrument
The questions were grouped into five sections: (1) socio-demographic characteristics of students; (2) assessment of knowledge on Covid-19 infection and prevention measures; (3) information on the contagion from Covid-19; (4) assessment of sleep quality; (5) assessment of the level of anxiety, stress and depression.
The variables examined in the socio-demographic section included: gender, age, marital status, level of education, occupation, general information on family and home (having or not children, number of people in the household, size of the house, presence/absence of garden or balcony) and information on any changes to the occupation of participants during the Covid-19 pandemic (office work or smart working, face-to-face or distance learning).
Knowledge about Covid-19 infection was assessed through four questions regarding transmission routes and prevention measures. Collection of data on participants regarding the contagion from Covid-19 included having contracted or not Covid-19, having been forced or not to remain in a mandatory quarantine condition, having had close people who tested positive or not, having lost someone close due to Covid-19 eventual, effects that the emergency had had on their social relationships (decrease/improvement of social contacts and use of social media).
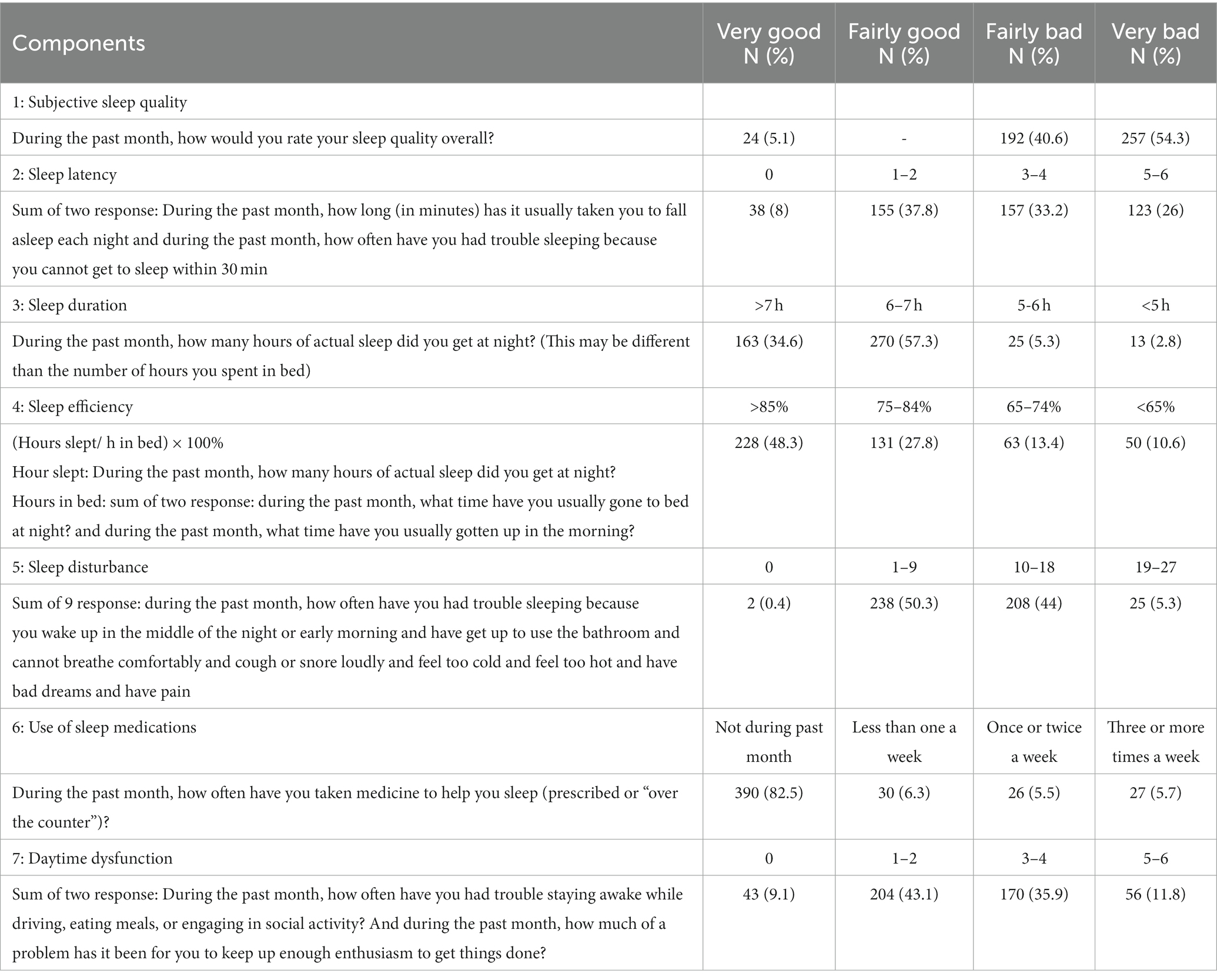
Sleep quality was assessed using the 19-item Pittsburgh Sleep Quality Index (PSQI) (29, 30). The PSQI is a self-administered questionnaire that evaluates the quality of sleep with questions about sleep in the previous month. The scale is made up of the following 7 components: subjective sleep quality (from Very good = 0 to Very bad = 3), sleep latency (sum of two questions describing time to fall asleep, each from 0 to 3), sleep duration (with a score from 0= >7 h to 3 = <5 h), routine sleep efficiency (calculated as (hours slept/h in bed) × 100%, with a score from 0= >85% to 3 = <65%), sleep disturbances (sum of nine questions, each with a score from 0 to 3, investigating trouble sleeping), use of sleep medications (from Not during past month = 0 to Three or more times a week = 3) and daytime dysfunctions (sum of two questions investigating staying awake and enthusiastic during the day, each from 0 to 3). By adding the scores of each section the final score between 0 and 21 is obtained with higher scores indicating a lower quality of sleep. A score ≥ 5 indicates a poor sleep, while <5 a good sleep.
The shortened version of the Depression Anxiety Stress Scales (DASS-21) was used to assess anxiety, stress, and depression (28). The DASS-21 is a self-rating scale in which participants rate the frequency and severity of anxiety, stress, and depression. Depression is investigated by assessing dysphoria, anhedonia, lack of incentives, and low self-esteem; anxiety by somatic symptoms of physiological over-arousal and fear response; stress by irritability, impatience, tension, and arousal levels. Therefore, we will have: low positive affect (DASS-Depression), physiological hyper-activation (DASS-Anxiety) and negative affect (DASS-Stress). Subscale scores are calculated as the sum of responses to the seven items of each subscale and multiplied by 2 to satisfy the 42 items of the original scale (29). The cut-offs for defining moderate levels of depression, anxiety, and stress are ≥14, ≥10, and ≥ 19, respectively (31, 32).
2.3 Statistical analysis
Data were analyzed with descriptive (proportions, means, standard deviations) and inferential (bivariate and multivariate analysis) statistics using the Stata software version 15.1 (33). First, descriptive statistics were conducted to summarize the main characteristic of the sample. Second, a univariate analysis was performed using the chi-square test, student’s t-test and Fisher’s exact test to evaluate the association between several potential determinants and being a poor or good sleeper (poor sleeper = 0; good sleeper = 1) (Table 1). All independent variables considered potential determinants of quality of sleep (continuous) were introduced in the multivariate linear regression model constructed to identify factors associated with this outcome.
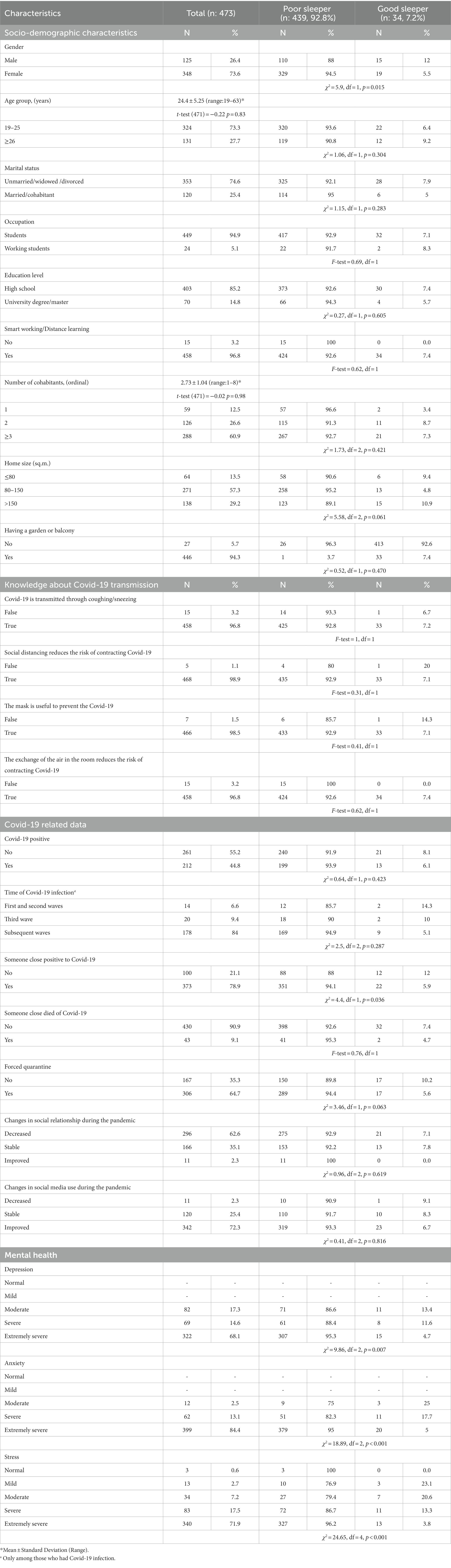
Table 1. Comparing poor and good sleepers according to socio-demographic characteristics, knowledge about Covid-19 transmission, Covid-19 related data and mental health.
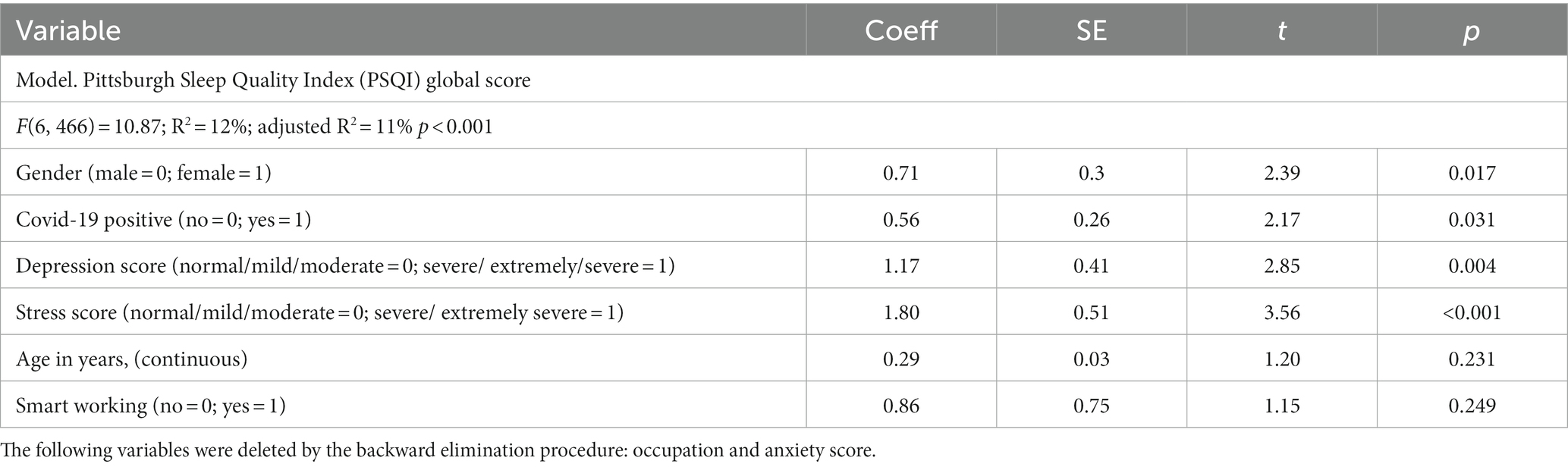
In the multivariate linear model the following independent variables, which were judged to potentially have influence on the above mentioned outcome (Model), were included: gender (male = 0, female = 1); age in years (continuous); occupation (students = 1, working students = 2); smart working/distance learning (no = 0,yes = 1); Covid-19 infection (no = 0,yes = 1); anxiety score
(normal/mild/moderate = 0; severe/extremely severe = 1); depression score (normal/mild/moderate = 0;severe/extremely severe = 1); stress score (normal/mild/moderate = 0; severe/extremely severe = 1).
Backward stepwise procedures were applied, including in the final models only the characteristics that provided a significant explanation of the outcomes, with a threshold of p-values of 0.2 for entering and of 0.4 for being retained. Standardized regression coefficients (β) were presented. All analyses were two-sided and the level of statistical significance was set at p equal to or less than 0.05.
3 Results
Of the 930 university students invited, 473 agreed to participate in the survey, with a response rate of 50.9%. The main characteristics of the examined sample are reported in Table 1. A large majority of participants were women (73.6%), with a mean age of 24.4 (range = 19–63 ± 5.25), and 74.6% were unmarried, widowed or divorced. Among the respondents, 14.8% had already another degree, 5.1% had a working activity and, the majority, during the pandemic, attended distance learning (96.8%). Moreover, 62.6% of the students declared a reduction in social activities and 72.3% an increase in the use of social media. 60.9% of respondents had more than two cohabitants, and most of respondents (94.3%) had an outdoor space (garden or balcony). Quarantine was imposed on 64.7% of them, and 78.9% of respondents had someone close who was positive to Covid-19. In addition, 9.1% had experience of someone close who died for Covid-19 infection. 44.8% of participants had the Covid-19 infection, the majority of them (84%) after the third wave. The investigation of students’ knowledge showed that almost all participants were aware that Covid-19 transmission occurs through coughing or sneezing, that it is reduced by air exchange (96.8%), and that social distancing and masks prevent Covid-19 infection (>98%). The majority of respondents reported an extremely severe level of depression (68.1%), anxiety (84.4%) and stress (71.9%).
Analyzing the quality of sleep of students, it emerged that 88% of men and 94.5% of women had PSQI scores ≥5 and a mean PSQI score of 9.2 ± 3. Tables 1, 2 highlight the results of the univariate and multivariate analyses of the outcome of interest. Univariate analysis shows significant differences according to several characteristics. In particular, PSQI was higher in women, in those who had someone close who tested positive for Covid-19, in students who had forced quarantine, and among subjects with extremely severe levels of depression, anxiety and stress (Table 1).
The results of the multivariate analysis showed that students with severe or extremely severe depression score, with severe or extremely severe stress score, who were females and who had contracted Covid-19 infection were more likely to have a high PSQI global score (Model in Table 2).
As summarized in Table 3, more than half of respondents (54.3%) had very bad subjective sleep quality in the previous month. In particular, more than half of students had difficulty in sleep initiation within 30 min 3 times or more per month (59.2%), and only 34.6% of participants reported long sleep duration lasting >7 h. Almost half of the students perceived a sleep efficiency >85% in the previous month (48.3%). Moreover, almost half of students (49.3%) reported to have experienced sleep disturbances one or two times a week (waking up or going to the bathroom in the middle of the night, not being able to breathe well, coughing or snoring, feeling hot or cold, having bad dreams or pain). Furthermore, 17.5% said they had taken medication as a sleep aid, and one half (47.7%) reported difficulty in staying awake while driving or eating meals or with maintaining their enthusiasm while completing their duties in the previous month.
4 Discussion
As highlighted by the World Health Organization (34), during the Covid-19 pandemic, there was a potential risk of increase in mental illness. All the worries, resulting from the almost inevitable health risks and social distancing, could have had a major impact on daily functioning and nighttime sleep. These scenarios impacted individuals’ daily routines, emotional wellbeing, sleep quality and mental health, leading to changes in sleep patterns, representing a source of stress. The present study provides results on the sleep quality of students during the pandemic and on several factors that can affect the quality of sleep.
Almost all participants demonstrated an optimal knowledge about the transmission of Covid-19. Indeed, data collection was conducted in 2022–2023, when the major waves of the pandemic were over in Italy and people were well informed on how to avoid infection. Although strong knowledge about Covid-19 has been associated with less psychological distress and with better quality of sleep during the first waves of pandemic (24, 35), reported findings are not consistent with previous studies since no association has been reported between knowledge on Covid-19 and sleep quality or psychological distress in the current epidemiological context. It has been observed that more than half of students had difficulty in sleep initiation and only one third reported long sleep duration (lasting >7 h), particularly in women. These results are similar to those reported in college students in USA, respectively 48 and 36.7% (36). Indeed, almost half of our students declared to have experienced sleep disturbances and this frequency is higher than that reported in a similar population (30%) (36). One half of participants declared to have experienced difficulty in staying awake while driving or eating meals or with maintaining their enthusiasm while completing their duties in the previous month, and even this sleep component is in contrast with what reported (25%) in a similar group (36).
The prevalence of poor sleepers in our population (92.8%) is higher than that reported in two similar Italian studies (around 75%) (37, 38) and significantly higher than that reported in German (36.9%) (39) and Chinese students (66.2%) (40).
In our study the mean PSQI global score (9.2 ± 3) is significantly higher in comparison with similar studies that used the same scale to evaluate the quality of sleep during lockdown in Italian students (PSQI mean score from 5.8 to 6.7) (41–43) and in USA students (PSQI mean score around 7.5) (44, 45).
In addition to the interpretation of the PSQI total score, the detailing of results on the domains of this instrument is worth discussing. In our study the mean of sleep latency is 1.8 ± 0.92 which is similar to the results reported in the same period by Benham et al. (1.49 ± 1) (44), Romero Blanco et al. (1.54 ± 1.06) (46) and Somma et al. (1.49 ± 1) (43); moreover, in our population it was revealed an increase in daytime dysfunction (1.5 ± 0.82) compared to the studies of Viselli et al. and Somma et al. (1.21 ± 8 and 1.24 ± 0.70) (42, 43). Mean sleep disturbance in our study was 1.5 ± 0.6, which is higher in comparison with Romero-Blanco et al. (1.12 ± 0.43) (46) and Somma et al. (1.14 ± 0.45) (43), whereas use of sleep medication is the same reported by Benham et al. (0.3 ± 0.82) (44). In line with the literature (38, 44, 46), college students reported a decrease in sleep duration (0.8 ± 0.67 in our study) and sleep efficiency (0.9 ± 1.01 in our study).
The present study also found a strong association, recently documented also in the Italian population (42, 47), between those who have poor sleep quality and psychological distress. The majority of respondents reported an extremely severe level of depression (68.1%), anxiety (84.4%) and stress (71.9%), in contrast with the study of Najafi Kalyani et al. (48) reporting lower severe level of depression (14.7%), anxiety (32.4%) and stress (24.8%). In the study of Najafi Kalyani et al. (48) a statistically significant relationship was found between the student’s stress levels and sleep quality (p < 0.001), which was confirmed by our study. We observed that the change in sleep quality (PSQI global score) was stronger in participants with a high DASS-21 score, similar to previous Italian studies in students and general population, in particular in the South of Italy (41, 49).
Sleep and stress are closely linked, at multiple levels, with current evidence supporting a bidirectional association between sleep and stress (50). Furthermore, the worsening of sleep quality is directly related to the motivation of university students (51).
This study presents some potential limitations that need to be dealt with before interpreting the results. First, the analyses were based on cross-sectional data, and therefore, the nature of the associations limited us from drawing definitive causal conclusions about the observed relationships between determinants and quality of sleep. Second, respondents may have been influenced to give the most “desirable” answers, and this may have produced overestimation of the quality of sleep. Third, this study was conducted after the major waves of the pandemic in Italy and questions were asked to investigate the quality of sleep during the pandemic period, therefore, the time occurred may have had an influence on the recall of sleep quality. Fourth, the majority of the sample was composed by students in Southern Italy from a single university, and our sample might not be completely representative of the Italian students or other populations or age groups such as not students young adults. Fifth, there was potential bias attributable to the use of a self-reporting instrument, recall bias and social desirability bias, and we were unable to accurately reflect the participants’ responses about actual sleep quality or mental health status. Moreover, self-reported data and the use of a cross-sectional design may limit the generalizability of the findings. Additionally, the study did not explore potential confounding factors that could influence sleep quality, such as pre-existing medical conditions, medication use, substance use, or prior sleep disorders. Finally, it was not possible to collect information on students who refused to participate in the study, which may have different characteristics than the study participants. Although those who chose to not participate may have a different quality of sleep or mental health status, which could affect the generalization of results, our response rate was sufficiently high to suggest that no substantial differences in the estimates would have been introduced by the results on non-responders.
In conclusion, a relevant percentage of students are poor sleepers with a higher overall PSQI score associated with depression and stress. Future studies should monitor sleep quality in a wider sample of students involving multiple universities and including additional determinants of sleep quality, such as obesity, current smoking status and binge drinking. The results of this study suggest the implementation of public health interventions to follow-up people with poor quality of sleep and promote healthy life styles focusing on the duration of night sleep.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Magna Graecia University of Catanzaro. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SA: Conceptualization, Data curation, Investigation, Writing – original draft. VS: Formal analysis, Resources, Writing – original draft. GP: Formal analysis, Resources, Writing – original draft. LL: Data curation, Writing – original draft. GDG: Formal analysis, Writing – original draft. CGAN: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors wish to thank all participating students for taking part to the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Grandner, MA. Sleep, health, and society. Sleep Med Clin. (2017) 12:1–22. doi: 10.1016/j.jsmc.2016.10.012
2. Williams, SJ. Sleep and society: sociological ventures into the un(known). 1st ed. London: Routledge (2005).
3. Kerkhof, GA. Epidemiology of sleep and sleep disorders in the Netherlands. Sleep Med. (2017) 30:229–39. doi: 10.1016/j.sleep.2016.09.015
4. Zhu, B, Wang, Y, Yuan, J, Mu, Y, Chen, P, Srimoragot, M, et al. Associations between sleep variability and cardiometabolic health: a systematic review. Sleep Med Rev. (2022) 66:101688. doi: 10.1016/j.smrv.2022.101688
5. Pileggi, C, Lotito, F, Bianco, A, Nobile, CG, and Pavia, M. Relationship between chronic short sleep duration and childhood body mass index: a school-based cross-sectional study. PLoS One. (2013) 8:e66689. doi: 10.1371/journale.pone.0066680
6. Chattu, VK, Manzar, MD, Kumary, S, Burman, D, Spence, DW, and Pandi-Perumal, SR. The global problem of insufficient sleep and its serious public health implications. Healthcare. (2018) 7:1. doi: 10.3390/healthcare7010001
7. Hale, L, Troxel, W, and Buysse, DJ. Sleep health: an opportunity for public health to address health equity. Annu Rev Public Health. (2020) 41:81–99. doi: 10.1146/annurev-publhealth-040119-094412
8. Scott, AJ, Webb, TL, Martyn-St James, M, Rowse, G, and Weich, S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. (2021) 60:101556. doi: 10.1016/j.smrv.2021.101556
9. Blackwelder, A, Hoskins, M, and Huber, L. Effect of inadequate sleep on frequent mental distress. Prev Chronic Dis. (2021) 18:E61. doi: 10.5888/pcd18.200573
10. Peltzer, K, and Pengpid, S. Self-reported sleep duration and its correlates with sociodemographics, health behaviours, poor mental health, and chronic conditions in rural persons 40 years and older in South Africa. Int J Environ Res Public Health. (2018) 15:1357. doi: 10.3390/ijerph15071357
11. Wang, S, Wu, Y, Ungvari, GS, Ng, CH, Forester, BP, Gatchel, JR, et al. Sleep duration and its association with demographics, lifestyle factors, poor mental health and chronic diseases in older Chinese adults. Psychiatry Res. (2017) 257:212–8. doi: 10.1016/j.psychres.2017.07.036
12. Lo Martire, V, Caruso, D, Palagini, L, Zoccoli, G, and Bastianini, S. Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev. (2019) 117:65–77. doi: 10.1016/j.neubiorev.2019.08.024
13. Hertenstein, E, Feige, B, Gmeiner, T, Kienzler, C, Spiegelhalder, K, Johann, A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
14. Baglioni, C, Battagliese, G, Feige, B, Spiegelhalder, K, Nissen, C, Voderholzer, U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
15. El-Solh, AA, Riaz, U, and Roberts, J. Sleep disorders in patients with posttraumatic stress disorder. Chest. (2018) 154:427–39. doi: 10.1016/j.chest.2018.04.007
16. Allison, KC, Spaeth, A, and Hopkins, CM. Sleep and eating disorders. Curr Psychiatry Rep. (2016) 18:92. doi: 10.1007/s11920-016-0728-8
17. Werner, A, Kater, MJ, Schlarb, AA, and Lohaus, A. Sleep and stress in times of the COVID-19 pandemic: the role of personal resources. Appl Psychol Health Well Being. (2021) 13:935–51. doi: 10.1111/aphw.12281
18. Limongi, F, Siviero, P, Trevisan, C, Noale, M, Catalani, F, Ceolin, C, et al. Changes in sleep quality and sleep disturbances in the general population from before to during the COVID-19 lockdown: a systematic review and meta-analysis. Front Psych. (2023) 14:1166815. doi: 10.3389/fpsyt.2023.1166815
19. Altena, E, Baglioni, C, Espie, CA, Ellis, J, Gavrilo, D, Holzinger, B, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I academy. J Sleep Res. (2020) 4:e13052. doi: 10.1111/jsr.13052
20. Gao, C, and Scullin, MK. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. (2020) 73:1–10. doi: 10.1016/j.sleep.2020.06.032
21. Wright, KP Jr, Linton, SK, Withrow, D, Casiraghi, L, Lanza, SM, Iglesia, H, et al. Sleep in university students prior to and during COVID-19 stay-at-home orders. Curr Biol. (2020) 30:R797–8. doi: 10.1016/j.cub.2020.06.022
22. McClung, CA. How might circadian rhythms control mood? Let me count the ways. Biol Psychiatry. (2013) 74:242–9. doi: 10.1016/j.biopsych.2013.02.019
23. Vadnie, CA, and McClung, CA. Circadian rhythm disturbances in mood disorders: insights into the role of the suprachiasmatic nucleus. Neural Plast. (2017) 2017:1504507–28. doi: 10.1155/2017/1504507
24. Yang, H, Shi, R, Chi, Y, Qiao, Z, Wu, Y, Zhu, Z, et al. Knowledge, anxiety, depression, and sleep quality among medical staff in central south areas of China during the break of COVID-19: does the level of hospitals make a difference? Front Psych. (2021) 12:714870. doi: 10.3389/fpsyt.2021.714870
25. Zhang, L, Zheng, H, Yi, M, Zhang, Y, Cai, G, Li, C, et al. Prediction of sleep quality among university students after analyzing lifestyles, sports habits, and mental health. Front Psych. (2022) 13:927619. doi: 10.3389/fpsyt.2022.927619
26. Schmickler, JM, Blaschke, S, Robbins, R, and Mess, F. Determinants of sleep quality: a cross-sectional study in university students. Int J Environ Res Public Health. (2023) 20:2019. doi: 10.3390/ijerph20032019
27. Lenz, ER, Pugh, LC, Milligan, RA, Gift, A, and Suppe, F. The middle-range theory of unpleasant symptoms: an up-date. Adv Nurs Sci. (1997) 19:14–27. doi: 10.1097/00012272-199703000-00003
28. Aday, LA, and Cornelius, LJ. Designing and conducting health surveys: A comprehensive guide. 3rd ed. San Francisco, CA, USA: Jossey-Bass Publisher (2000).
29. Buysse, DJ, Reynolds, CF, Monk, TH, Berman, SR, and Kupfer, DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
30. Curcio, G, Tempesta, D, Scarlata, S, Marzano, C, Moroni, F, Rossini, PM, et al. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurol Sci. (2013) 34:511–9. doi: 10.1007/s10072-012-1085-y
31. Bottesi, G, Ghisi, M, Altoè, G, Conforti, E, Melli, G, and Sica, C. The Italian version of the depression anxiety stress Scales-21: factor structure and psychometric properties on community and clinical samples. Compr Psychiatry. (2015) 60:170–81. doi: 10.1016/j.comppsych.2015.04.005
32. Lovibond, SH, and Lovibond, PF. Depression anxiety stress scales. Sydney: The Psychology Foundation of Australia Inc (1996).
33. Stata Corporation. Stata reference manual release 15.1; Stata corporation. College Station, TX, USA: Stata Corporation (2017).
34. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. (2020) Available at: (https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1).
35. Fan, CW, Drumheller, K, Chen, IH, and Huang, HH. College students' sleep difficulty during COVID-19 and correlated stressors: a large-scale cross-sessional survey study. Sleep Epidemiol. (2021) 1:100004. doi: 10.1016/j.sleepe.2021.100004
36. Becker, SP, Jarrett, MA, Luebbe, AM, Garner, AA, Burns, GL, and Kofler, MJ. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health. (2018) 4:174–81. doi: 10.1016/j.sleh.2018.01.001
37. D'orsogna, T, Halson, SL, and Oehmen, R. Poor sleep quality during COVID-19 pandemic restrictions associated with reduced psychological wellbeing in healthcare students. Chronobiol Int. (2023) 40:438–49. doi: 10.1080/07420528.2023.2186127
38. Marelli, S, Castelnuovo, A, Somma, A, Castronovo, V, Mombelli, S, Bottoni, D, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. (2021) 268:8–15. doi: 10.1007/s00415-020-10056-6
39. Schlarb, AA, Claßen, M, Hellmann, SM, Vögele, C, and Gulewitsch, MD. Sleep and somatic complaints in university students. J PainRes. (2017) 10:1189–99. doi: 10.2147/JPR.S125421
40. Zhang, Y, Peters, A, and Chen, G. Perceived stress mediates the associations between sleep quality and symptoms of anxiety and depression among college nursing students. Int J Nurs Educ Scholarsh. (2018) 15:ijnes-2017-0020. doi: 10.1515/ijnes-2017-0020
41. Cellini, N, Canale, N, Mioni, G, and Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. (2020) 29:e13074. doi: 10.1111/jsr.13074
42. Viselli, L, Salfi, F, D'Atri, A, Amicucci, G, and Ferrara, M. Sleep quality, insomnia symptoms, and depressive symptomatology among Italian university students before and during the Covid-19 lockdown. Int J Environ Res Public Health. (2021) 18:13346. doi: 10.3390/ijerph182413346
43. Somma, A, Marelli, S, Gialdi, G, Castelnuovo, A, Mombelli, S, Ferini-Strambi, L, et al. Latent changes in perceived quality of sleep related to the COVID-19 quarantine measures in Italian university students: understanding the role of personality and internalizing symptoms. Med J Clin Psychol. (2020) 8:1–22. doi: 10.6092/2282-1619/mjcp-2550
44. Benham, G. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health. (2021) 37:504–15. doi: 10.1002/smi.3016
45. Vargas, PA, and Robles, E. Asthma and allergy as risk factors for suicidal behavior among young adults. J Am Coll Health. (2019) 67:97–112. doi: 10.1080/07448481.2018.1462822
46. Romero-Blanco, C, Rodríguez-Almagro, J, Onieva-Zafra, MD, Parra-Fernández, ML, Prado-Laguna, MDC, and Hernández-Martínez, A. Sleep pattern changes in nursing students during the COVID-19 lockdown. Int J Environ Res Public Health. (2020) 17:5222. doi: 10.3390/ijerph17145222
47. Casagrande, M, Favieri, F, Tambelli, R, and Forte, G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. (2020) 75:12–20. doi: 10.1016/j.sleep.2020.05.011
48. Najafi Kalyani, M, Jamshidi, N, Salami, J, and Pourjam, E. Investigation of the relationship between psychological variables and sleep quality in students of medical sciences. Depress Res Treat. (2017) 2017:7143547–6. doi: 10.1155/2017/7143547
49. Franceschini, C, Musetti, A, Zenesini, C, Palagini, L, Scarpelli, S, Quattropani, MC, et al. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Front Psychol. (2020) 11:574475. doi: 10.3389/fpsyg.2020.574475
50. Kalmbach, DA, Anderson, JR, and Drake, CL. The impact of stress on sleep: pathogenic sleepreactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. (2018) 27:e12710. doi: 10.1111/jsr.12710
Keywords: quality sleep, students, Covid-19, mental health, survey
Citation: Angelillo S, Sansone V, Paduano G, Lateano L, Di Giuseppe G and Nobile CGA (2024) The quality of sleep: evaluation among university students. Front. Public Health. 11:1270426. doi: 10.3389/fpubh.2023.1270426
Edited by:
Nyi Nyi Naing, Sultan Zainal Abidin University, MalaysiaReviewed by:
Pei-Lin Yang, University of Washington, United StatesNasr Chalghaf, University of Gafsa, Tunisia
Yaosheng Liu, Chinese PLA General Hospital, China
Copyright © 2024 Angelillo, Sansone, Paduano, Lateano, Di Giuseppe and Nobile. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carmelo Giuseppe Angelo Nobile, Y2FybWVsby5ub2JpbGVAdW5pY2FsLml0
 Silvia Angelillo
Silvia Angelillo Vincenza Sansone
Vincenza Sansone Giovanna Paduano
Giovanna Paduano Ludovica Lateano1
Ludovica Lateano1 Gabriella Di Giuseppe
Gabriella Di Giuseppe