- 1Physician Assistant Program, Charles R. Drew University of Medicine and Science (CDU), Los Angeles, CA, United States
- 2Department of Psychiatry, Charles R. Drew University of Medicine and Science (CDU), Los Angeles, CA, United States
- 3Department of Family Medicine, Charles R. Drew University of Medicine and Science (CDU), Los Angeles, CA, United States
- 4Department of Family Medicine, University of California, Los Angeles (UCLA), Los Angeles, CA, United States
- 5Department of Internal Medicine, Charles R. Drew University of Medicine and Science (CDU), Los Angeles, CA, United States
Introduction: A high quality diet is vital in promoting wellbeing and ensuring good health, particularly for those living with chronic conditions. Older African Americans, already burdened with a higher prevalence of chronic conditions, also face a higher risk for suboptimal diets. The COVID-19 pandemic had lasting effects on access to healthy food for all Americans, but some demographic groups were disproportionately affected. Older African Americans, who already experienced reduced access to healthy food pre-pandemic, were particularly afflicted, but the full extent of the pandemic's impact on their food insecurity and food environment remains unclear.
Methods: To address this gap, we conducted a study among 102 older African Americans in South Los Angeles between October 2021 and July 2022 during the COVID-19 pandemic. Participants completed surveys on dietary intake, food insecurity, and neighborhood food environment. We measured dietary quality using the healthy eating index (HEI)-2015. The analysis included descriptive, bivariate chi-square, t-tests, analysis of variance, and multiple linear and logistic regression.
Results: While overall dietary quality was suboptimal, most participants met the guidelines for fruit and vegetable consumption. Food insecurity was associated with lower overall diet quality and lower total fruit and whole fruit intake. However, there was no association between food environment and diet quality.
Discussion: In light of our findings, further intervention is critical to improving diet quality, especially among older African Americans living with chronic conditions in the post-pandemic era.
1. Introduction
Chronic conditions such as heart disease, diabetes, and hypertension continue to rank as leading causes of morbidity and mortality among older Americans (1). There is well-established evidence that a high-quality diet plays an important role in preventing or slowing these diseases and promoting overall wellbeing (2–5). This is particularly important among older African Americans, who are disproportionately burdened with chronic conditions (1) and have historically reported suboptimal diets based on recommended guidelines (6–10). Prior studies suggest that access to healthy food significantly influences in diet quality (11–15). However, it remains unclear how changes in the experiences of food insecurity and the food environment impacted the diet quality of older African Americans during the COVID-19 pandemic. This is of considerable importance because chronic diseases may be exacerbated by diet changes experienced during this pandemic.
Food insecurity is a condition in which an individual lacks consistent access to enough nutritious food to live an active and healthy life (16). It is often caused by a lack of financial resources or inadequate access to healthy and affordable food options. Food insecurity is associated with poor diet quality, prevalence of chronic disease, and higher mortality rates (17–21). On the other hand, the food environment refers to the physical environment that influences access to healthy food options in a particular area or community (15). It includes factors such as the availability and affordability of high quality food, as well as the types of food outlets (such as grocery stores, convenience stores, fast food restaurants, and farmers' markets) present in the area. Particularly for low-income and minority communities, limited access to affordable and nutritious food options may significantly impact dietary habits and health outcomes (22–24).
A longitudinal study by Leung et al., (19) found a positive relationship between food insecurity and poor diet quality among adults over the age of 60 years. Furthermore, a systematic review and meta-analysis of existing literature by Gundersen and Ziliak (20) demonstrated that food insecurity was consistently associated with worse physical and mental health outcomes, including chronic diseases. The link between food insecurity and chronic diseases such as heart disease, diabetes, and hypertension was also observed among low-income participants in the National Health and Nutrition Examination Survey (NHANES) (21). Recognizing the negative impact of food insecurity on disease outcomes is critical now more than ever, considering the escalation of food insecurity during and post the COVID-19 pandemic (25, 26).
The COVID-19 pandemic exerted a disproportionate impact on food environments and food insecurity, particularly among vulnerable populations such as older adults, low-income individuals, and minorities (17, 25, 27–32). Notably, Dubowitz et al. (28) reported that among African American residents in a low-income food desert neighborhood, food insecurity increased from 21% in 2018 to 36% in 2020 as a result of the pandemic. Additionally, several studies quantified the number of food outlet closures in locations around the US (33–35). In Flint, MI, 173 food venues closed during the pandemic, with only 17 new venues taking their place (33). Locations with predominantly African American populations had three times the rate of emergency food outlet closures as other locations (33). Similarly San Diego county lost a net of 8% of its stores that accept electronic benefits transfer (EBT) payments, including one full-service supermarket (35). These closures, coupled with supply-chain shortages and business restrictions, significantly impacted access to healthy food options (31, 32, 36). The repercussions of these changes in the food landscape pose substantial challenges to vulnerable communities already facing food insecurity.
Recognizing the potential compromise to diet quality during the pandemic and the subsequent potential impact on the health status of older African Americans, our study aimed to examine the effects of food insecurity and food environment on their diet quality. Our hypothesis posited that (1) a lower food insecurity would be associated with higher diet quality, and (2) a favorable food environment would be associated with higher diet quality.
2. Materials and methods
2.1. Participants
The COVID-19, Food insecurity, Exercise, and Dietary history (C-FED) study was a cross-sectional sample of a larger intervention study focused on health behaviors in older African Americans in South LA during the COVID-19 pandemic (37). To be eligible for the parent study, participants had to identify as Black or African American and be at least 65 or 55 years old with a chronic condition. All participants enrolled in the parent study were eligible to take part in the C-FED study. A total of 118 participants opted to join the C-FED study and complete the study-related surveys between October 2021 and July 2022. Consistent with previous studies, we excluded individuals whose responses to the diet history questionnaire indicated improbable caloric intake (<500 kcal/day or >3,500 kcal/day for women; <800 kcal/day or >4,000 kcal/day for men) (38–40), resulting in an analytical dataset of 102 participants. Informed consent was obtained prior to their participation. The C-FED study was approved by the Charles R. Drew University of Medicine and Science IRB.
2.2. Surveys
Details on the methodology and design of the C-FED study are presented in a previous manuscript (37). Participants completed surveys on their own, through an online link, over the phone with a trained research assistant, or in person with a trained research assistant. The C-FED surveys consisted of the Diet History Questionnaire (DHQ) III, the National Center for Health Statistics six-item short form food security survey, and three questions about food environment. Socio-demographic and health information were obtained from the parent study questionnaires. Socio-demographic information included age, gender, education level, income, and living arrangement. Education level was categorized into three groups: high school degree or less, associate degree or some college, and college or post-graduate degree. Annual income was dichotomized using a cutoff of $50,000. For living arrangement, participants were asked if they lived alone (yes/no). Health information consisted of self-reported health, BMI, and chronic conditions. Health rating options included poor, fair, good, very good, and excellent. We combined groups with small numbers, resulting in the categories poor-fair, good, and very good-excellent. BMI was categorized according to clinical guidelines into healthy (18.5–24.9), overweight (25.0–29.9), and obese (≥30). We constructed the variable number of chronic health conditions by counting the number of health conditions that participants listed. This variable was categorized into 0, 1, or 2, and 3+ health conditions.
2.3. Food insecurity
The food insecurity questionnaire reflects household level food insecurity. This measure has been previously validated as correctly classifying 97.7% of households in the U.S. (41, 42). It consists of six questions that ask about running out of food and skipping or cutting the size of meals. The total food insecurity score is calculated as the total number of items endorsed by the participant, such that the total possible score ranges from 0 to 6. A score of 0 indicated full food security, while scores ranging from 1 to 6 indicate increasing levels of food insecurity. We used a cutoff of 1 to dichotomize this variable into those with food insecurity (code = 1) and without food insecurity (code = 0).
2.4. Food environment
We asked three questions related to the food available in the neighborhood taken from the PhenX Toolkit (https://www.phenxtoolkit.org/protocols/view/210701). An assessment of these questions reported an internal reliability of 0.78 and test-retest reliability of 0.69 (43). Participants were instructed to consider their neighborhood as within 1 mile of their home. Participants were asked to rate their level of agreement with (1) The fresh fruits and vegetables in my neighborhood are of high quality, (2) A large selection of fresh fruits and vegetables is available in my neighborhood, and (3) A large selection of low-fat products is available in my neighborhood. Responses were on a 5-point Likert scale ranging from strongly disagree to strongly agree. Following instrument guidelines, we created an overall food environment score by taking the average of the scores of the three questions and rounding to the nearest integer. All food environment variables were categorized into three groups: disagree (scores <3), neutral (score = 3), and agree (scores > 3).
2.5. Outcome variables: diet quality
The DHQ is a comprehensive diet inventory. Participants were asked about the frequency and quantity of all types of foods consumed over the past 12 months. Diet quality was measured using the Healthy Eating Index-2015 (HEI), which was calculated based on responses on the DHQ. The HEI is a validated construct for assessing dietary intake (44). It consists of the sum of 10 sub scores, each of which reflect consumption of a particular food group or food category. A key feature of HEI is that scores are based on density, so it reflects the balance of food consumed across food groups. Thus, the total score reflects diet quality, as opposed to quantity.
The total score ranges from 0 to 100, with 100 reflecting the ideal diet according to the dietary recommendations of the USDA. The USDA suggests the following grading for total HEI scores: 90–100 = A; 80–89 = B; 70–79 = C; 60–69 = D; <60 = F (45). In addition, the score for overall HEI was normally distributed using the Shapiro-Wilk test and used in the analysis as continuous variable.
We focused on the diet quality indices that correspond to the neighborhood food environment questions: HEI sub scores for total fruit, whole fruit, vegetable, percent of calories from total fat, and percent of calories from saturated fat. Total fruit score includes 100% juices, while the whole fruit score includes all forms of fruit except juice. All the included HEI sub scores range from 0 to 5, with 5 indicating highest quality. Because the distributions of the HEI sub scores were highly skewed, we categorized these variables into those who achieved the maximum possible score (5) and those who did not (<5). The percentage of calories consumed from fat and from saturated fats were normally distributed per Shapiro-Wilk Tests and treated as continuous variables.
2.6. Statistical analysis
Descriptive statistics were used to depict the population characteristics. Categorical data were presented as number and percent. Continuous data were presented as mean and standard deviation for normally distributed variables and median and inter quartile range for skewed variables. For bivariate analyses, we used chi-squared tests to test for statistical significance between categorical variables, and t-test or analysis of variance (ANOVA) for associations between categorical and continuous normally distributed variables. We used multiple regression to test for statistical associations of food insecurity and food environment with diet quality. We used the overall food environment score in multiple regressions and controlled for variables that could be associated with diet quality: age, gender, education, living arrangement, physical health, BMI, and number of chronic conditions. Age was included in the model as a continuous variable; the other variables were included as categorical variables. To avoid multicollinearity, we did not include income in the models, due to its strong correlation with food insecurity. Our small sample size did not provide us with the power to investigate interactions.
The diet quality outcomes included total HEI, HEI sub scores of fruit, whole fruit, and vegetables, and percent of calories from fats and from saturated fats. Linear regression was used where the dependent outcome was a continuous normally distributed variable (total HEI, percent calories from saturated fat, and percent calories from fat), and logistic regression was used for categorical binary outcomes (HEI sub scores of fruit, whole fruit, and vegetables). For linear regressions, we present adjusted B coefficient and standard error (SE); for logistic regressions we report adjusted odds ratio and 95% confidence interval. The percent missing for any given variable was <5%, except for education level which was missing for 8%. We used listwise deletion for cases with missing data in multivariable regressions. Analyses were done using SAS 9.4, and a p < 0.05 was considered statistically significant.
3. Results
3.1. Participant characteristics
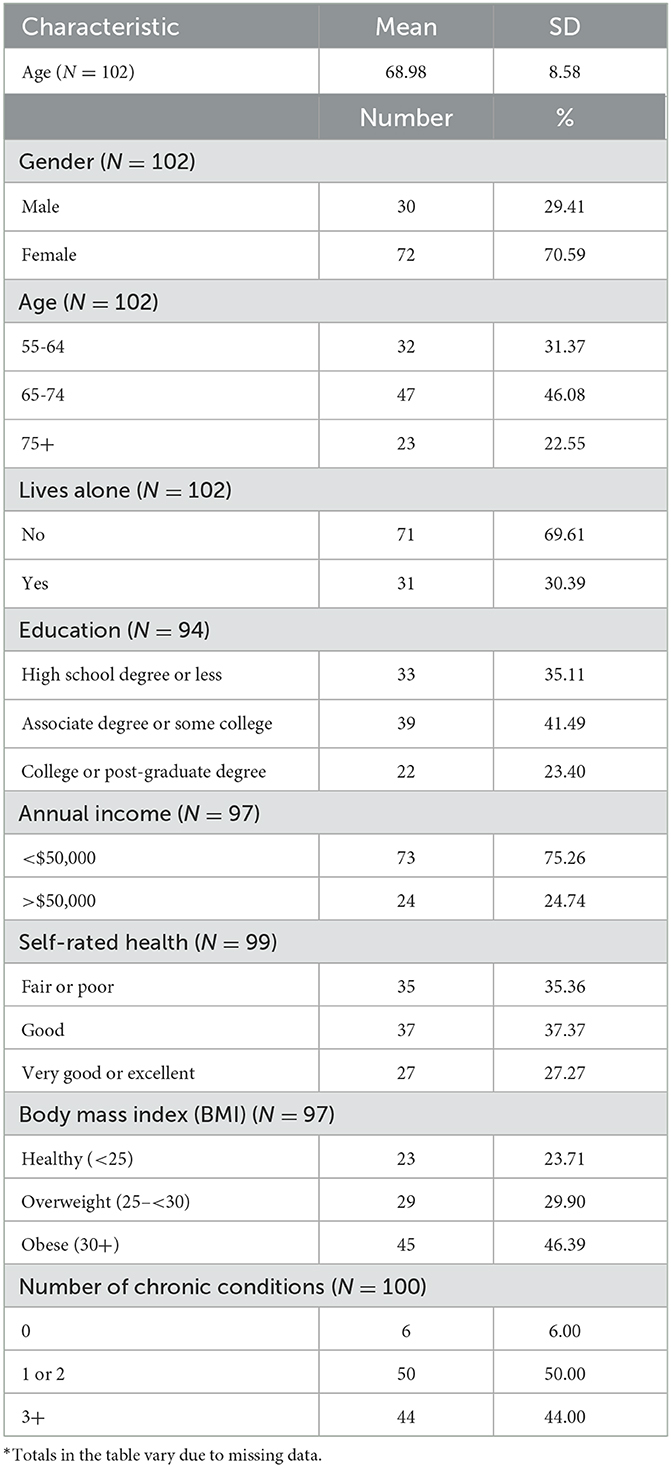
Participant ages were nearly evenly distributed (Table 1). Most participants were female (71%), did not live alone (70%), and had relatively low incomes with 75% reporting an annual income <$50,000. Thirty-five percent had an education level of high school degree or less, while 23% had a college or post-graduate degree. While 65% rated their health as very good, good, or better excellent, 76% were overweight or obese, and 94% had at least one chronic condition, with 44% having 3 or more. Sixty-three percent reported having hypertension, 25% COPD or asthma, 23% diabetes, and 9% heart disease.
3.2. Characteristics of participant diets
Participants consumed an estimated average (±SD) of 1,533 (±650) calories per day (Table 2). Approximately 32% (±7%) of calories came from fat, with 10% (±3%) from saturated fat. Medians (inter-quartile range) for consumption of proteins, fats, and carbohydrates were 60 (46), 51 (31), and 197 (125) grams, respectively. The average total HEI score was 68, which would earn a “D” by suggested USDA grading criteria (Table 2). Only 7% of participants had a total HEI score that would earn an “A” or “B”. Based on HEI component sub scores, most participants met the guidelines for total fruit (70%) and whole fruit (78%) consumption, while 39% met the guidelines for vegetable consumption. Most participants (70%) were food secure, but 30% had some level of food insecurity. Food environment was generally favorable. The majority of participants agreed with the statements about their neighborhood: the fresh fruits and vegetables were of high quality (69%); a large selection of fresh fruits and vegetables were available (73%); and a large selection of low-fat products were available (68%).
3.3. Associations between diet quality and food access (food environment and food insecurity)
3.3.1. Bivariate analyses
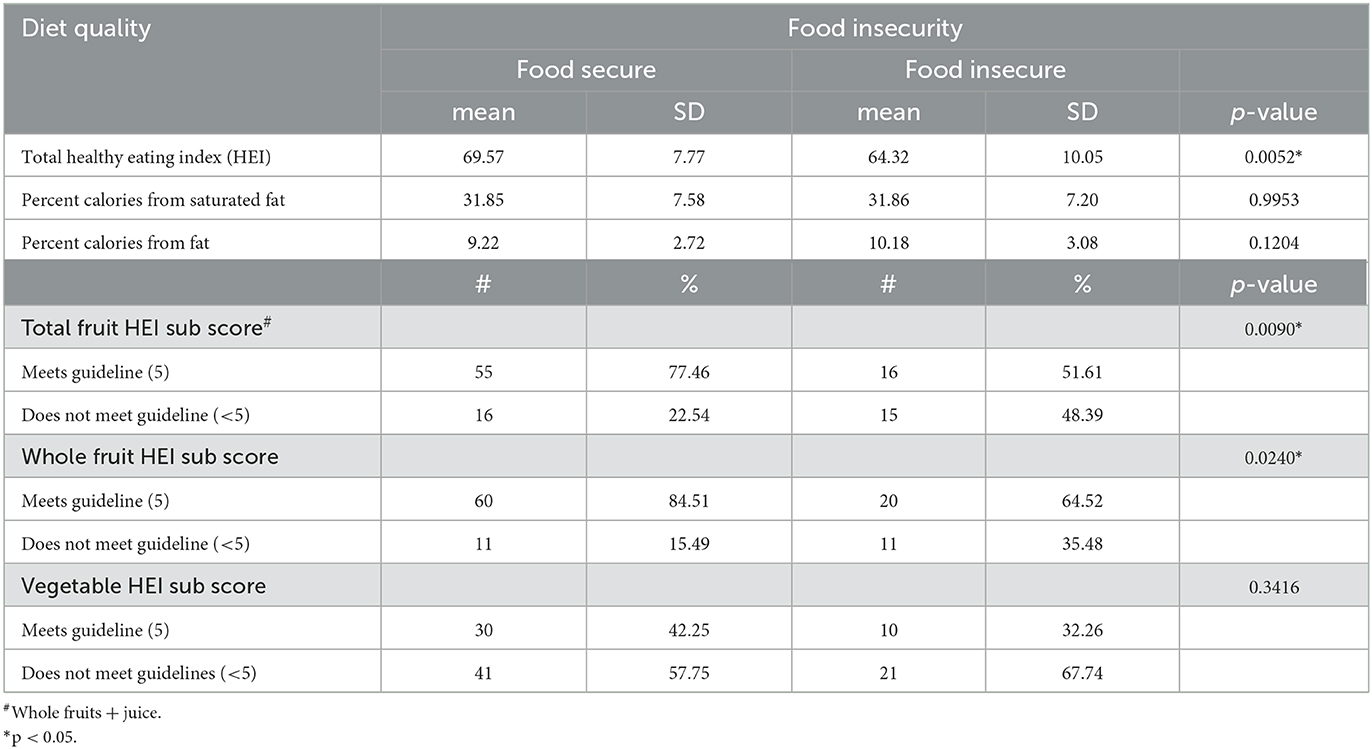
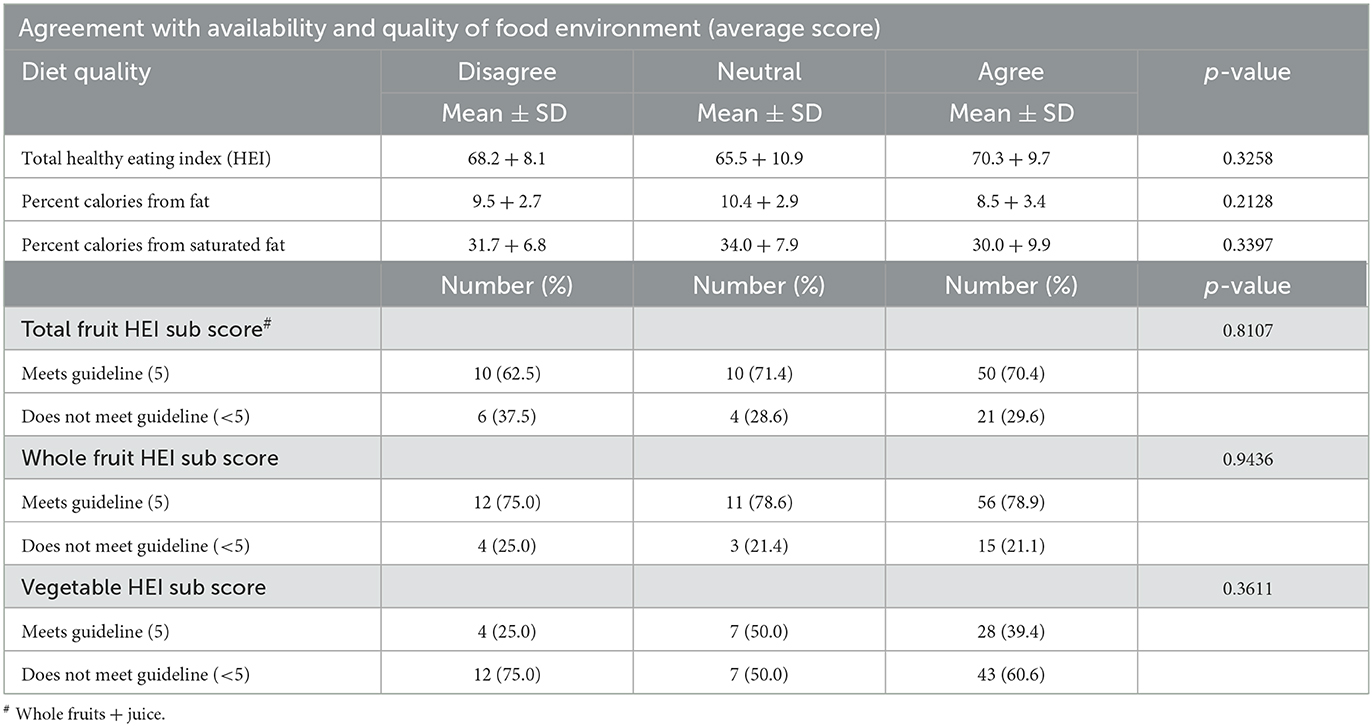
Food insecurity was significantly associated with total HEI (p = 0.0052) and with the total and whole fruit HEI sub scores (p = 0.0090, p = 0.0240, respectively) (Table 3). However, food insecurity was not significantly associated with percent of calories consumed from fats, or vegetable HEI. There was no significant association between the food environment and total HEI, % of calories consumed from fats, fruit HEI, or vegetable HEI (Table 4).
3.3.2. Multi-variable analyses
After controlling for age, gender, education, living arrangement, physical health, BMI, and number of chronic conditions, we still found no significant associations between the food environment and total diet quality or diet quality components (Table 5). The significant association between food insecurity and total HEI (p = 0.048), and the total fruit (p = 0.049) and whole fruit HEI (p = 0.030) sub scores persisted (Table 5). Of note, none of the controlled variables were significantly associated with total HEI, vegetables, or percent calories from saturated fats. Participants who lived alone were significantly less likely to meet the guidelines for total fruits (p = 0.007) and whole fruits (p = 0.018). Compared to those with high school education or less, those with a college degree consumed significantly more calories from fat (p = 0.022).
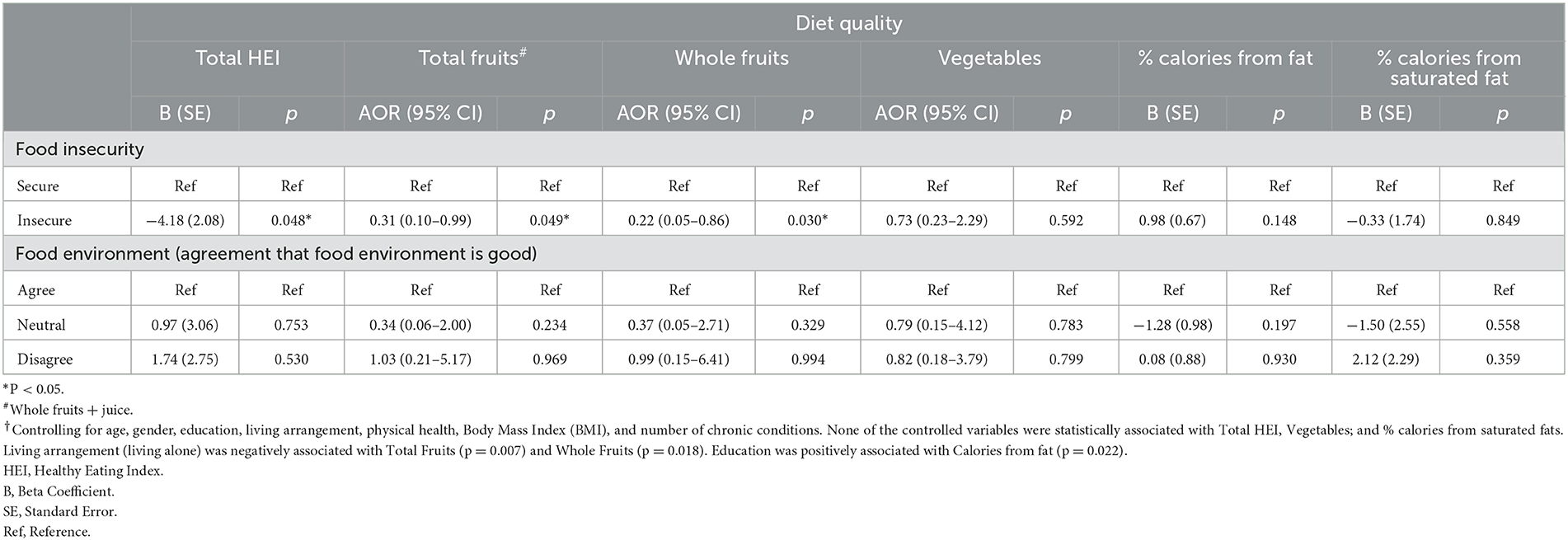
Table 5. Multivariable† associations between food insecurity and food environmentand diet quality: linear and logistic regressions (N = 85).
4. Discussion
Pre-pandemic studies found that older African Americans had poor overall diet quality and did not meet fruit, vegetable, and low-fat guidelines based on USDA recommendations (3, 7–9, 46–48). These findings are crucial because poor diet quality is associated with poor outcomes, including all-cause mortality (49–53). While studies on dietary habits during the COVID-19 pandemic have yielded mixed results (54–56), research specifically on older African Americans remain limited (57). Our study fills this gap by providing insights into the diet quality of older African Americans during the pandemic.
Our findings indicate that during the pandemic, older African Americans had poor diet quality. Specifically, the average total HEI score was 68, which would earn a “D” grade based on suggested USDA scoring. Only 7% of participants had a total HEI score that would earn an “A” or “B,” highlighting the pressing need for dietary improvements in this population. In contrast, over 60% of participants had fruit and vegetable scores that met the guidelines and received the maximum score of 5, which would earn an “A”. The Dietary Guidelines for Americans recommend that adults get 20–35% of their calories from fats and limit saturated fats to <10% of their caloric intake (58). While participants were close to the suggested limits for fat and saturated fat, with averages of 32.9% and 9.5% of calories coming from fat and saturated fat, respectively, they did meet the guidelines. Because the total HEI quality score is computed from all food sources, including fruits and vegetables, this finding suggests deficiencies in the other types of foods consumed.
Our findings underscore the complex and multifaceted determinants of dietary behavior during the pandemic. Our study focused on the impact of food insecurity and the food environment on diet quality. Building upon our previous work, which identified how attitudes toward COVID-19 influenced diet quality in underserved older African Americans (59), the current study expands our understanding of associations between food insecurity, the food environment, and diet quality in this vulnerable population during the pandemic.
4.1. Diet quality and food insecurity
Before the COVID-19 pandemic, food insecurity was already more prevalent among African Americans and had been linked to poorer diet quality (12, 19, 20). The pandemic further exacerbated this issue, with widespread reports of food insecurity among older adults, and particularly impacting racial/ethnic minority groups (28, 29, 60, 61). Dubowitz et al. (28) examined the impact of COVID-19 shutdowns on food insecurity among predominantly African American adults living in an under-resourced community. They found that despite steady declines since 2011, food insecurity increased from 21% in 2018 to 36% in 2020 and skyrocketed to 80% due to the pandemic. This heightened level of food insecurity is a critical concern, as previous research has associated food insecurity with chronic disease (3, 21, 62–65).
In previous studies, food insecurity was found to be associated with lower consumption of fruits and vegetables and recommended nutrients, as well as a higher likelihood of consuming a high-fat, and high-calorie diet (11, 14, 23, 66–69). However, our study found that food insecurity was specifically associated with lower consumption of whole and total fruits, but not vegetable or fat consumption. The observed association between food insecurity and reduced consumption of whole fruits underscores the necessity for focused interventions to enhance access to these nutritious options, which offer the added benefit of high fiber content. Moreover, our study revealed that fewer older African Americans met the guidelines for vegetable consumption compared to those meeting the guidelines for fruits, emphasizing the significance of interventions targeting vegetable intake as well. Although our study did not find a significant association between food insecurity and vegetable or low-fat food consumption, we interpret this result with caution due to our smaller sample size. Indeed, the lack of association might also be attributed to the lower efforts to meet overall dietary guidelines.
Overall, these findings underscore the critical importance of addressing food insecurity and improving access to nutritious foods, especially fruits and vegetables, to enhance the diet quality and overall health outcomes for older African Americans.
4.2. Diet quality and the food environment
In addition to the high prevalence of food insecurity, African Americans were already facing other challenges that contributed to poor diet quality before the pandemic, such as a lack of access to healthy food options, including fruits, vegetables and low-fat options (15, 24, 70). A study conducted by Zenk et al. (70) found that older African Americans had limited access to supermarkets and grocery stores that offer fresh and healthy food options, leading to what has been termed as “food deserts”. Interestingly, in our study, the availability or absence of healthy foods in the neighborhood did not impact the diet quality of our participants. It is worth noting that during the pandemic, local government initiatives such as the Senior Meal Emergency Response Program were put in place to increase access to food. Such efforts may have impacted participants' perceptions of food availability. However, we did not assess individuals' participation in these programs.
Our findings suggest that the mere availability of food and/or high quality foods in the neighborhood does not translate to healthy diets. This finding is consistent with previous literature (71, 72). The consumption of healthy diets is influenced by additional factors such as cost, skills, and availability of food preparation time, and transportation (11, 71, 73). A systematic review of the contribution of food prices on diet quality found that foods of lower nutritional value and lower-quality diets were generally more affordable per calorie and tended to be selected by groups of lower socioeconomic status (11). Furthermore, numerous other factors can hinder the consumption of healthy diets. In a qualitative study, African American adults noted that barriers to healthy eating included a perception of departing from the cultural heritage, lack of support from family and friends, lack of information, and preferences for the taste of foods considered unhealthy (74). Additionally, older African Americans managing hypertension reported challenges sorting through dietary advice from different sources and implementing dietary changes that would support multiple chronic conditions (75).
Addressing the complexities of the dietary behaviors of older African Americans requires a comprehensive approach that considers various factors, including affordability, accessibility, cultural influences, and social support. By understanding these multifaceted barriers, we can design targeted interventions to foster healthier dietary behaviors and improve overall health outcomes within this vulnerable population.
4.3. Influence of the pandemic
Restrictions during the pandemic caused disruptions in the food supply chain, reduced workforce, and shopping limitations, which affected the availability and affordability of healthy food options in some neighborhoods (76–81). Economic instability caused by the pandemic increased the risk of food insecurity for many households, which was especially pronounced in communities of color that already face higher rates of food insecurity and limited access to healthy food options due to systemic inequities and structural racism (30).
Older adults were particularly affected by the pandemic's restrictions, facing challenges in grocery shopping and limited access to fresh and nutritious foods. As a result, reliance on pre-packaged meals, often high in unhealthy ingredients, increased due to their longer shelf-life (78, 79). For older African Americans, who are more likely to live in food deserts and have limited access to healthy and affordable food options, the closure of senior centers and other community sites that provide free or reduced-price meals contributed to food insecurity. Furthermore, in the thick of the pandemic, reliance on food delivery put older African Americans at a disadvantage as they are less likely to have access to reliable internet, technology equipment and skills to make this possible (77, 82).
A systematic review by Trude et. al. (77) highlighted the barriers and facilitators of access to healthy food in low-income households during the COVID-19 pandemic. The primary barriers to equitable access were cost and limited availability of online grocery opportunities in food desserts. Although the perception of lack of control in food selection discouraged online grocery shopping, convenience and lower perceived stress were reported as benefits. However, older adults who lacked access to online grocery shopping during the extreme period of the pandemic shopped less frequently and/or relied on others to shop for them (78).
Our study shows that the diet of underserved older African Americans was far from optimal during the thick of the COVID-19 pandemic despite meeting some diet quality indices. Given the established link between poor overall diet quality and chronic disease (2, 3), this is particularly important in our cohort, which had a noteworthy prevalence of overweight or obesity (76%), hypertension (63%), COPD or asthma (25%), diabetes (23%) and heart disease (9%).
4.4. Limitations and strengths
Although our participants met the requirement for total fruit and total vegetable consumption, this was not enough to improve their overall diet quality. Additionally, the neighborhood availability of healthy fruits, vegetables, and low-fat products did not impact their overall diet quality. These findings should be interpreted with caution as the individual, community, and national responses to support older adults temporarily during the pandemic were not considered in this study. Additionally, our smaller sample size and convenience sample may limit generalizability. There is also a possibility of recall bias due to the self-reporting of the variables. Despite these limitations, a strength of our study is that it illuminates the comprehensive dietary quality in older African Americans, a marginalized and understudied population. Additionally, our study used validated, standardized questionnaires and a detailed dietary intake methodology. Our study emphasizes the need for further investigations into the influence of access to healthy food on diet quality post-pandemic. As one of the few studies focusing on this population, our results have implications for future interventions targeting diet quality in underserved older African Americans.
5. Conclusion
Factors associated with suboptimal diets in older African Americans during the COVID-19 pandemic are complex and multifaceted, encompassing both individual and environmental influences. Our research contributes valuable insights into the dietary challenges faced by this vulnerable population, highlighting the need for targeted interventions addressing access, affordability, and education on healthy food choices. As we navigate the post-pandemic era, it is imperative to recognize the importance of promoting equitable access to nutritious food options, particularly for older African Americans who are disproportionately affected by food insecurity and limited access to healthy foods.
Future research should further investigate the influence of individual and environmental factors on dietary quality among underserved older African Americans, considering broader support systems and societal responses. By understanding these multifaceted determinants, we can develop more effective strategies to improve diet quality, enhance health outcomes, and promote overall wellbeing within this vulnerable population. Addressing these disparities will require a comprehensive and collaborative approach involving policymakers, community organizations, healthcare providers, and other stakeholders.
Data availability statement
The datasets presented in this article are not publicly available as they are still in progress. Queries and requests to access the finalized datasets should be directed to bHVjeWtpYmVAY2RyZXd1LmVkdQ==.
Ethics statement
This study was approved by the Institutional Review Board of Charles R. Drew University of Medicine and Science. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LK: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing. KS: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Visualization, Writing—original draft, Writing—review & editing. MB: Methodology, Supervision, Writing—review & editing. MS: Conceptualization, Data curation, Supervision, Validation, Writing—review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Institute of Minority Health and Health Disparities under award numbers U54MD007598 and S21 MD000103. In addition, as a scholar of the Clinical Research Education and Career Development (CRECD) program at Charles R. Drew University of Medicine and Science, LK's efforts were supported by the NIMHD/NIH Award number R25 MD007610.
Acknowledgments
The authors acknowledge Adaobi Bosah, YuFu Kuo, Edward Adinkrah, and Humberto Sanchez for their support in data collection. The authors would also like to thank the study participants for sharing their time and effort.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
One of the authors declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Centers for Disease Control and Prevention National Center for Health Statistics. National Vital Statistics System, Mortality 2018-2021 on CDC WONDER Online Database, released in 2021. In:Data Data are from the Multiple Cause of Death Files 2018-2021 as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Available online at: http://wonder.cdc.gov/ucd-icd10-expanded.html (accessed February 20, 2023).
2. Rodriguez-Monforte M, Flores-Mateo G, Sanchez E. Dietary patterns and CVD: a systematic review and meta-analysis of observational studies. Br J Nutr. (2015) 114:1341–59. doi: 10.1017/S0007114515003177
3. Zhao H, Andreyeva T. Diet quality and health in Older Americans. Nutrients. (2022) 14:1198. doi: 10.3390/nu14061198
4. Morze J, Danielewicz A, Hoffmann G, Schwingshackl L. Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: a second update of a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. (2020) 120:1998–2031. doi: 10.1016/j.jand.2020.08.076
5. Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. J Am Med Assoc. (2017) 317:912–24. doi: 10.1001/jama.2017.0947
6. Bowman SA. Socioeconomic characteristics, dietary and lifestyle patterns, and health and weight status of older adults in NHANES, 1999-2002: a comparison of Caucasians and African Americans. J Nutr Elder. (2009) 28:30–46. doi: 10.1080/01639360802633938
7. Deierlein AL, Morland KB, Scanlin K, Wong S, Spark A. Diet quality of urban older adults age 60 to 99 years: the cardiovascular health of seniors and built environment study. J Acad Nutr Diet. (2014) 114:279–87. doi: 10.1016/j.jand.2013.09.002
8. Hsiao PY, Mitchell DC, Coffman DL, Allman RM, Locher JL, Sawyer P, et al. Dietary patterns and diet quality among diverse older adults: the University of Alabama at Birmingham Study of Aging. J Nutr Health Aging. (2013) 17:19–25. doi: 10.1007/s12603-012-0082-4
9. Kibe LW, Bazargan M. Fruit and vegetable intake among older African American and Hispanic adults with cardiovascular risk factors. Gerontol Geriatr Med. (2022) 8:23337214211057730. doi: 10.1177/23337214211057730
10. Long T, Zhang K, Chen Y, Wu C. Trends in diet quality among older US adults From 2001 to 2018. JAMA Network Open. (2022) 5:e221880. doi: 10.1001/jamanetworkopen.2022.1880
11. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. (2015) 73:643–60. doi: 10.1093/nutrit/nuv027
12. Wilcox S, Sharpe PA, Liese AD, Dunn CG, Hutto B. Socioeconomic factors associated with diet quality and meeting dietary guidelines in disadvantaged neighborhoods in the Southeast United States. Ethn Health. (2020) 25:1115–31. doi: 10.1080/13557858.2018.1493434
13. Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. (2012) 18:1172–87. doi: 10.1016/j.healthplace.2012.05.006
14. Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. (2014) 114:1943–53. doi: 10.1016/j.jand.2014.06.353
15. Larson NI, Story MT, Nelson MC. Neighborhood environments. Disparities in access to healthy foods in the US. Am J Prev Med. (2009) 36:74–81. doi: 10.1016/j.amepre.2008.09.025
16. Coleman-Jensen A, Gregory C, Singh A. Household food security in the United States in 2013 (September 1, 2014). In: USDA-ERS Economic Research Report Number 173. Available online at: https://ssrn.com/abstract=2504067; http://dx.doi.org/10.2139/ssrn.2504067 (accessed February 1, 2023).
17. Walker RJ, Chawla A, Garacci E, Williams JS, Mendez C, Ozieh MN, et al. Assessing the relationship between food insecurity and mortality among US adults. Ann Epidemiol. (2019) 32:43–8. doi: 10.1016/j.annepidem.2019.01.014
18. Banerjee S, Radak T, Khubchandani J, Dunn P. Food insecurity and mortality in American adults: results from the NHANES-linked mortality study. Health Promot Pract. (2021) 22:204–14. doi: 10.1177/1524839920945927
19. Leung CW, Wolfson JA. Food insecurity among older adults: 10-year national trends and associations with diet quality. J Am Geriatr Soc. (2021) 69:964–71. doi: 10.1111/jgs.16971
20. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. (2015) 34:1830–9. doi: 10.1377/hlthaff.2015.0645
21. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income nhanes participants. J Nutr. (2010) 140:304–10. doi: 10.3945/jn.109.112573
22. Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn Dis. (2006) 16:275–80. Available online at: https://www.jstor.org/stable/48666828
23. Zenk SN, Odoms-Young AM, Dallas C, Hardy E, Watkins A, Hoskins-Wroten J, et al. “You have to hunt for the fruits, the vegetables”: Environmental barriers and adaptive strategies to acquire food in a low-income African American neighborhood. Health Educ Behav. (2011) 38:282–92. doi: 10.1177/1090198110372877
24. Rimkus L, Isgor Z, Ohri-Vachaspati P, Zenk SN, Powell LM, Barker DC, et al. Disparities in the availability and price of low-fat and higher-fat milk in US food stores by community characteristics. J Acad Nutr Diet. (2015) 115:1975–85. doi: 10.1016/j.jand.2015.04.002
25. Nagata JM, Seligman HK, Weiser SD. Perspective: the convergence of Coronavirus Disease 2019 (COVID-19) and food insecurity in the United States. Adv Nutr. (2020) 12:287–90. doi: 10.1093/advances/nmaa126
26. Mayasari NR, Ho DKN, Lundy DJ, Skalny AV, Tinkov AA, Teng IC, et al. Impacts of the COVID-19 pandemic on food security and diet-related lifestyle behaviors: an analytical study of google trends-based query volumes. Nutrients. (2020) 12:3103. doi: 10.3390/nu12103103
27. Higashi RT, Sood A, Conrado AB, Shahan KL, Leonard T, Pruitt SL. Experiences of increased food insecurity, economic and psychological distress during the COVID-19 pandemic among Supplemental Nutrition Assistance Program-enrolled food pantry clients. Public Health Nutr. (2022) 25:1027–37. doi: 10.1017/S1368980021004717
28. Dubowitz T, Dastidar MG, Troxel WM, Beckman R, Nugroho A, Siddiqi S, et al. Food insecurity in a low-income, predominantly African American cohort following the COVID-19 pandemic. Am J Public Health. (2021) 111:494–7. doi: 10.2105/AJPH.2020.306041
29. Lauren BN, Silver ER, Faye AS, Rogers AM, Woo-Baidal JA, Ozanne EM, et al. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. (2021) 24:3929–36. doi: 10.1017/S1368980021000355
30. Dennard E, Kristjansson E, Tchangalova N, Totton S, Winham D, O'Connor A. Food insecurity among African Americans in the United States: a scoping review. PLoS ONE. (2022) 17:e0274434. doi: 10.1371/journal.pone.0274434
31. Otten JJ, Averill MM, Spiker ML. Food security and food access during the COVID-19 pandemic: Impacts, adaptations, and looking ahead. JPEN J Parenter Enteral Nutr. (2023) 47 Suppl 1:S11–5. doi: 10.1002/jpen.2445
32. Pakravan-Charvadeh MR, Mohammadi-Nasrabadi F, Gholamrezai S, Vatanparast H, Flora C, Nabavi-Pelesaraei A. The short-term effects of COVID-19 outbreak on dietary diversity and food security status of Iranian households (A case study in Tehran province). J Clean Prod. (2021) 281:124537. doi: 10.1016/j.jclepro.2020.124537
33. Bell A, Taylor DE. A vanishing food infrastructure: the closure of food outlets in flint in a pandemic era. Am Behav Sci. (2023). doi: 10.1177/00027642221142202
34. Yi SS, Ali SH, Russo RG, Foster V, Radee A, Chong S, et al. COVID-19 Leads to dramatic changes in the food retail environment in New York City: May–July 2020. J Immigr Minor Health. (2022) 24:31–7. doi: 10.1007/s10903-021-01230-7
35. Lowery BC, Swayne MR, Castro I, Embury J. Mapping EBT store closures during the COVID-19 pandemic in a low-income, food-insecure community in San Diego. Prev Chronic Dis. (2022) 19:E37. doi: 10.5888/pcd19.210410
36. Larson N, Alexander T, Slaughter-Acey JC, Berge J, Widome R, Neumark-Sztainer D. Barriers to accessing healthy food and food assistance during the COVID-19 pandemic and racial justice uprisings: a mixed-methods investigation of emerging adults' experiences. J Acad Nutr Diet. (2021) 121:1679–94. doi: 10.1016/j.jand.2021.05.018
37. Kibe LW, Bosah A, Schrode KM, Kuo Y, Shaheen M, Adinkra E, et al. Assessing food access, exercise, and dietary history among older african american parishioners during the COVID-19 pandemic (C-FED study): design, opportunities, challenges, and lessons learned. J Racial Ethn Health Disparities. (2023). doi: 10.1007/s40615-023-01657-8
38. Montgomery MP, Kamel F, Pericak-Vance MA, Haines JL, Postel EA, Agarwal A, et al. Overall diet quality and age-related macular degeneration. Ophthalmic Epidemiol. (2010) 17:58–65. doi: 10.3109/09286580903450353
39. Golmohammadi M, Zarrin R, Ayremlou P. Adaptation and validity assessment of a diet quality index for patients with type 2 diabetes. J Diabetes Metabol Dis. (2020) 19:1027–36. doi: 10.1007/s40200-020-00601-5
40. Hengeveld LM, Wijnhoven HA, Olthof MR, Brouwer IA, Harris TB, Kritchevsky SB, et al. Prospective associations of poor diet quality with long-term incidence of protein-energy malnutrition in community-dwelling older adults: the health, aging, and body composition (Health ABC) study. Am J Clin Nutr. (2018) 107:155–64. doi: 10.1093/ajcn/nqx020
41. Bickel G NM, Price C, Hamilton W, Cook J. Guide to measuring household food security revised 2000. In: US Department of Agriculture. Alexandria, VA. (2010). doi: 10.22004/ag.econ.337157
42. Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the household food security scale. Am J Public Health. (1999) 89:1231–4. doi: 10.2105/AJPH.89.8.1231
43. Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. (2007) 165:858–67. doi: 10.1093/aje/kwm040
44. Reedy J, Lerman JL, Krebs-Smith SM, Kirkpatrick SI, Pannucci TE, Wilson MM, et al. Evaluation of the healthy eating index-2015. J Acad Nutr Diet. (2018) 118:1622–33. doi: 10.1016/j.jand.2018.05.019
45. National Cancer Institute. Visualizing and Interpreting HEI Scores. Available online at: https://epi.grants.cancer.gov/hei/interpret-visualize-hei-scores.html (accessed June 7, 2022).
46. Wang Y, Chen X. Between-group differences in nutrition- and health-related psychosocial factors among US adults and their associations with diet, exercise, and weight status. J Acad Nutr Diet. (2012) 112:486–98. doi: 10.1016/j.jand.2011.12.003
47. Vergis S, Schiffer L, White T, Mcleod A, Khudeira N, Demott A, et al. Diet quality and nutrient intake of urban overweight and obese primarily African American older adults with osteoarthritis. Nutrients. (2018) 10:485. doi: 10.3390/nu10040485
48. Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in state-specific adult fruit and vegetable consumption — United States, 2015. MMWR Morbidity and Mortality Weekly Report. (2017) 66:1241–7. doi: 10.15585/mmwr.mm6645a1
49. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. (2017) 46:1029–56. doi: 10.1093/ije/dyw319
50. Yu D, Sonderman J, Buchowski MS, Mclaughlin JK, Shu X-O, Steinwandel M, et al. Healthy eating and risks of total and cause-specific death among low-income populations of African-Americans and other adults in the Southeastern United States: a prospective cohort study. PLoS Med. (2015) 12:e1001830. doi: 10.1371/journal.pmed.1001830
51. English LK, Ard JD, Bailey RL, Bates M, Bazzano LA, Boushey CJ, et al. Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open. (2021) 4:e2122277. doi: 10.1001/jamanetworkopen.2021.22277
52. Hays JC, Keller HH, Ostbye T. The effects of nutrition-related factors on four-year mortality among a biracial sample of community-dwelling elders in the North Carolina piedmont. J Nutr Elder. (2005) 25:41–67. doi: 10.1300/J052v25n02_04
53. Boggs DA, Ban Y, Palmer JR, Rosenberg L. Higher diet quality is inversely associated with mortality in African-American women. J Nutr. (2015) 145:547–54. doi: 10.3945/jn.114.195735
54. Mignogna C, Costanzo S, Ghulam A, Cerletti C, Donati MB, de Gaetano G, et al. Impact of nationwide lockdowns resulting from the first wave of the COVID-19 pandemic on food intake, eating behaviours and diet quality: a systematic review. Adv Nutr. (2021) 13:388–423. doi: 10.1093/advances/nmab130
55. Ruggiero E, Mignogna C, Costanzo S, Persichillo M, Di Castelnuovo A, Esposito S, et al. Changes in the consumption of foods characterising the Mediterranean dietary pattern and major correlates during the COVID-19 confinement in Italy: results from two cohort studies. Int J Food Sci Nutr. (2021) 72:1105–17. doi: 10.1080/09637486.2021.1895726
56. Bin Zarah A, Enriquez-Marulanda J, Andrade JM. Relationship between dietary habits, food attitudes and food security status among adults living within the United States three months post-mandated quarantine: a cross-sectional study. Nutrients. (2020) 12:3468. doi: 10.3390/nu12113468
57. Nicklett EJ, Johnson KE, Troy LM, Vartak M, Reiter A. Food access, diet quality, and nutritional status of older adults during COVID-19: a scoping review. Front Public Health. (2021) 9:763994. doi: 10.3389/fpubh.2021.763994
58. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025, 9th Edition. (2020). Available online at: DietaryGuidelines.gov (accessed February 1, 2023)
59. Kibe LW, Bazargan M, Bosah A, Schrode KM, Kuo Y, Andikrah E, et al. Diet quality of older African Americans: impact of knowledge and perceived threat of COVID-19. Int J Environ Res Public Health. (2023) 20:5274. doi: 10.3390/ijerph20075274
60. Ankuda CK, Fogel J, Kelley AS, Byhoff E. Patterns of material hardship and food insecurity among older adults during the COVID-19 pandemic. J Gen Intern Med. (2021) 36:3639–41. doi: 10.1007/s11606-021-06905-3
61. Morales DX, Morales SA, Beltran TF. Racial/ethnic disparities in household food insecurity during the COVID-19 pandemic: a nationally representative study. J Racial Ethn Health Disparities. (2021) 8:1300–14. doi: 10.1007/s40615-020-00892-7
62. Seligman HK, Tschann J, Jacobs EA, Fernandez A, López A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. (2012) 35:233–8. doi: 10.2337/dc11-1627
63. Pereira MHQ, Pereira M, Campos GC, Molina MCB. Food insecurity and nutritional status among older adults: a systematic review. Nutr Rev. (2022) 80:631–44. doi: 10.1093/nutrit/nuab044
64. Vaccaro JA, Huffman FG. Sex and race/ethnic disparities in food security and chronic diseases in US older adults. Gerontol Geriatr Med. (2017) 3:2333721417718344. doi: 10.1177/2333721417718344
65. Jih J, Stijacic-Cenzer I, Seligman HK, Boscardin WJ, Nguyen TT, Ritchie CS. Chronic disease burden predicts food insecurity among older adults. Public Health Nutr. (2018) 21:1737–42. doi: 10.1017/S1368980017004062
66. Lee JS, Frongillo EA. Nutritional and health consequences are associated with food insecurity among US elderly persons. J Nutr. (2001) 131:1503–9. doi: 10.1093/jn/131.5.1503
67. Choi YJ, Crimmins EM, Kim JK, Ailshire JA. Food and nutrient intake and diet quality among older Americans. Public Health Nutr. (2021) 24:1638–47. doi: 10.1017/S1368980021000586
68. Drisdelle C, Kestens Y, Hamelin AM, Mercille G. Disparities in access to healthy diets: how food security and food shopping behaviors relate to fruit and vegetable intake. J Acad Nutr Diet. (2020) 120:1847–58. doi: 10.1016/j.jand.2020.03.020
69. Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutr. (2004) 7:1081–8. doi: 10.1079/PHN2004648
70. Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W. Health promoting community design/nutrition neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am J Health Promot. (2009) 23:255–64. doi: 10.4278/ajhp.071204127
71. Widener MJ. Spatial access to food: retiring the food desert metaphor. Physiol Behav. (2018) 193:257–60. doi: 10.1016/j.physbeh.2018.02.032
72. Dubowitz T, Ncube C, Leuschner K, Tharp-Gilliam S. A natural experiment opportunity in two low-income urban food desert communities: research design, community engagement methods, and baseline results. Health Educ Behav. (2015) 42:87S−96S. doi: 10.1177/1090198115570048
73. Drewnowski A, Darmon N, Briend A. Replacing fats and sweets with vegetables and fruits - a question of cost. Am J Public Health. (2004) 94:1555–9. doi: 10.2105/AJPH.94.9.1555
74. James D. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: application of a culturally sensitive model. Ethn Health. (2004) 9:349–67. doi: 10.1080/1355785042000285375
75. Jones LM, Moss KO, Mitchell J, Still C, Hawkins J, Tang E, et al. Challenges to dietary hypertension self-management as described by a sample of African American older adults. Worldviews Evid Based Nurs. (2022) 19:64–72. doi: 10.1111/wvn.12555
76. Boyacι-Gündüz CP, Ibrahim SA, Wei OC, Galanakis CM. Transformation of the food sector: security and resilience during the COVID-19 pandemic. Foods. (2021) 10:497. doi: 10.3390/foods10030497
77. Trude ACB, Lowery CM, Ali SH, Vedovato GM. An equity-oriented systematic review of online grocery shopping among low-income populations: implications for policy and research. Nutr Rev. (2022) 80:1294–310. doi: 10.1093/nutrit/nuab122
78. Palmer F, Jung SE, Shahan MK, Ellis A. P66 Understanding how the COVID-19 pandemic influenced older adults' grocery shopping habits. J Nutr Educ Behav. (2021) 53:S54–5. doi: 10.1016/j.jneb.2021.04.125
79. Murphy B, Benson T, McCloat A, Mooney E, Elliott C, Dean M, et al. Changes in consumers' food practices during the COVID-19 lockdown, implications for diet quality and the food system: a cross-continental comparison. Nutrients. (2020) 13:20. doi: 10.3390/nu13010020
80. Alabi MO, Ngwenyama O. Food security and disruptions of the global food supply chains during COVID-19: building smarter food supply chains for post COVID-19 era. Br Food J. (2023) 125:167–85. doi: 10.1108/BFJ-03-2021-0333
81. Fu J. 'I felt like I failed': inflation puts healthy food out of reach for millions of Americans. In: The Guardian. (2022). Available at: https://www.theguardian.com/environment/2022/sep/30/inflation-healthy-food-eating-america?utm_source=Dornsife+School+of+Public+Health+Communications&utm_campaigN=cdb940349e-EMAIL_CAMPAIGN_2018_07_30_02_14_COPY_02&utm_medium=email&utm_term=0_fa9e5b0e03-cdb940349e-302144008&mc_cid=cdb940349e&mc_eid=3045c9f514 (accessed June 7, 2022).
Keywords: COVID-19, diet quality, food insecurity, food environment, African American, older adults, healthy eating index
Citation: Kibe LW, Schrode K, Bazargan M and Shaheen M (2023) Impact of food insecurity and food environment on the diet quality of older African Americans during the COVID-19 pandemic. Front. Public Health 11:1268961. doi: 10.3389/fpubh.2023.1268961
Received: 28 July 2023; Accepted: 12 October 2023;
Published: 14 November 2023.
Edited by:
Lené Levy-Storms, University of California, Los Angeles, United StatesReviewed by:
Mingke Wang, Naval Medical University, ChinaMohammad Reza Pakravan-Charvadeh, Lorestan University, Iran
Copyright © 2023 Kibe, Schrode, Bazargan and Shaheen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucy W. Kibe, bHVjeWtpYmVAY2RyZXd1LmVkdQ==
 Lucy W. Kibe
Lucy W. Kibe Katrina Schrode
Katrina Schrode Mohsen Bazargan
Mohsen Bazargan Magda Shaheen
Magda Shaheen