
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 22 September 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1265834
This article is part of the Research Topic Disparities in Mental Health View all 15 articles
Objective: This research dealt with investigating and measuring the contribution of the factors that impact depression in older adults living alone vs. those living with others (hereafter referred to as “not alone”) in China.
Design: This investigation adopts a cross-sectional research design. The dataset employed for this study comprises data from 2018 the Chinese Longitudinal Health Longevity Survey (CLHLS).
Setting: The research involved data sourced from China, specifically from 23 of its provinces. From the 8th CLHLS, 12,197 older adults were selected who met the study requirements.
Measures: Binary logistic regression models were established to delve into the primary factors impacting the depressive symptoms of the individuals. Furthermore, Fairlie models were employed to assess these factors between older adults living alone and those not living alone. This approach facilitated an in-depth analysis of their respective contributions.
Results: It was observed that the demographic of Chinese older adults exhibited depressive symptoms at a rate of 11.92%. Older adults who resided alone (15.76%) exhibited a higher prevalence of depressive symptoms in comparison to their counterparts living in not-alone settings (11.15%). Employing Fairlie decomposition analysis, it was determined that this observed disparity in depressive symptoms, amounting to 55.33% of the overall difference, could be primarily attributed to distinct factors. This encompassed variance in marital status (20.55%), years of school (4.63%), self-reported local income status (7.25%), self-reported sleep status (17.56%), and self-reported health status (4.24%).
Conclusion: The resulting data indicated that depressive symptoms exhibited an elevated prevalence in older adults living alone than in those living not alone. This discrepancy was predominantly attributed to variance in socioeconomic marital status, years of school, self-reported local income status, self-reported sleep status, and self-reported health status by living alone vs. not alone. Mitigating these influential factors could help develop targeted and meticulous intervention strategies, precisely tailored to improve the mental well-being of older adults at high risk.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. The common features of all the depressive disorders are sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function (1, 2). Because of false perceptions, nearly 60% of people with depression do not seek medical help and depression exerts a negative influence on the quality of life experienced by older adults (2). It primarily impacts older adults who are afflicted with chronic medical conditions and cognitive impairment. This condition precipitates personal distress, familial discord, and functional impairment, exacerbating the prognosis of various illnesses like diabetes, autoimmune disorders like rheumatoid arthritis, lupus, and cardiovascular diseases like coronary heart disease, hypertension (HTN), obesity, physiological aging, cancer, poor hearing, and poor health and heightening mortality rates (3, 4). Furthermore, it catalyzes suicidal tendencies, culminating in adverse health ramifications that result in a considerable burden on both families and society at large (5, 6).
Due to the accelerated process of global aging, the global population of older adults surpassed the 1 billion mark in 2021, constituting approximately 13.5% of the global populace. As projected by the World Health Organization, by the year 2030, an estimated one in six individuals will be age 60 years or older, underscoring the escalating significance of this demographic shift (7). As the country that long had the largest population worldwide, but is now the second largest and shrinking, China is facing an especially serious problem of an aging population. As per the findings of the seventh National Census conducted in 2021, the cohort of individuals aged 60 years and above within China has reached a substantial count of 260 million, comprising 18.7% of the entire population. Within this segment, individuals aged 65 years and above constitute 190 million individuals, equivalent to 13.5% of the total population (8). Projections indicate that the proportion of older adults aged 65 and above in the overall population will reach about 26.9% by the year 2050 (9).
Additionally, the implementation of the family planning policy in China has led to drastic declines in fertility, distinct from the demographic changes even in other countries with fertility declines over the past three decades. The 4 (older adults)–2 (a young or middle-aged couple)–1 (a child) family structure has become mainstream (10). Simultaneously, within contemporary society, adult children increasingly seek autonomy and their own personal “free space.” This trend has contributed to the erosion of the traditional family model characterized by multi-generational cohabitation involving three or even four generations. The functioning of family older-adult care is weakening and shifting to social eldercare services. In China, where cultural norms emphasize family structure and collective values, the family has traditionally served as a vital support system for older adults. As their spouses, cohabitants, or important friends die, the issue of older adults living alone has become a social concern and has garnered significant attention (11).
Are there differences in depressive symptoms between older adults living alone and not alone? Numerous investigations have established a robust correlation between loneliness in old age and the occurrence of depression (11, 12). A comprehensive review systematically elaborates on living alone may predispose individuals to an elevated susceptibility to psychiatric conditions such as depression, alcohol abuse, sleep disorders, personality disorders, and Alzheimer’s disease (4). One approach to preventing depression in older adults living alone is to identify factors distinguished from older adults living not alone. The factors may include sex, self-perceived financial status, marital status, educational level, living status, self-reported health status (SRH), quality of social relationships, smoking, and alcohol consumption (13–18). Therefore, we must explore the importance and contribution level of each factor between living alone and not alone, which will help us develop targeted measures to reduce depression in older adults living alone.
So further assessment of the elements that result in heightened depression in older adults living alone in comparison with those living with others (hereafter referred to as “not alone”) must be executed. Furthermore, this research attempted to establish a foundation for the formulation of effective policies aimed at managing the levels of depressive symptoms experienced by older adults. Therefore, the variance between older adults (aged 65+) living alone and those cohabitating was examined in China. To achieve this, the Chinese Longitudinal Health Longevity Survey (CLHLS) dataset was utilized. Initially, the study delved into the degree to which sociodemographic characteristics, personal lifestyle choices, and health statuses accounted for the variations in depressive symptoms among Chinese older adults living alone and not alone.
The data were retrieved from the 8th CLHLS (PKU Center for Healthy Aging and Development, 2020). Detailed information regarding the sources and design of the datasets can be accessed at https://opendata.pku.edu.cn/dataset.xhtml?persistentId=doi:10.18170/DVN/ WBO7LK (Accessed July 22, 2023). The CLHLS was executed by the Center for Healthy Ageing and Development Studies/National Development Research Institute of Peking University and was subjected to approval by the Ethics Committee of Peking University (No. IRB00001052-13074). The survey comprehensively spanned 23 of the provinces, encompassing approximately two-thirds of the geographical expanse of China. The focal demographic comprised individuals aged 65 years and above. The methodology involved two distinct questionnaires: one aimed at respondents who were alive and another tailored for family members of deceased older adults. The 8th iteration of the CLHLS took place from 2017 to 2018, involving interviews with a total of 15,874 older adults. We selected the participants who completed the full 10-question version of the Center for Epidemiology Studies Depression (CES-D) questionnaire were selected. The exclusion criteria encompassed individuals below the age of 65, as well as those who had not responded to measurements relating to depressive symptoms, demographic and sociological characteristics, personal lifestyle choices, or health status indicators. Finally, 12,197 respondents were selected for this study (Figure 1). Ultimately, including 2029 and 10,148 older adults living alone and not alone, respectively. The process utilized for the exclusion of non-relevant individuals is depicted in Figure 1.
The CES-D has been widely used as a practical depression screening tool by previous studies targeting older adults in China (19–21). In the 8th CLHLS, the CES-D-10 scale comprises 10 specific items such as “I was bothered by things that usually do not bother me,” “I did not feel like eating; my appetite was poor,” to comprehensive evaluation of the responders’ depression status. The response options for each item range from 0 (none of the time or rarely) to 3 (most or all the time) on the questionnaire. Higher scores represent more severe depressive symptom. The questionnaire was centered on assessing depressive symptoms within the context of the past week. In the same way that multiple previous studies defined a score of 10 as a threshold score, participants with a score greater than or equal to 10 were defined as experiencing depressive symptoms (20, 22). Although scoring above a 10 does not directly correlate with a formal diagnosis, it does indicate a need for direct clinical assessment (22).
Respondents were classified as alone or not alone based on whether they cohabited with family or spouse during the survey duration.
The reliability of the acquired data was enhanced further by accounting for multiple potential confounding factors. To acquire comprehensive factors spanning sociological attributes, demographic characteristics, sociological characteristics, personal lifestyle and health status were drawn from existing studies on depressive symptoms.
Age was classified as <70 years, 70–79 years, 80–89 years, 90–99 years, or > =100 years. The residence mainly included city, town, or rural. BMI was calculated by dividing weight (kg) by the square of height (m) and was divided into four categories: <18.5, 18.5–23.9, 24.0–27.9, and > =28.0. Education level was classified according to time in school as 0 years, 1–6 years, and ≥ 7 years.
Marital status included married and living with spouse, widowed, and others (including married but not living with a spouse, divorced, and never married). Self-reported local income status was divided into three categories: poor, average, and rich.
Personal lifestyle included smoking, drinking, exercise, and self-reported sleep status. Smoking, drinking, and exercise were categorized as “Yes” or “No” based on the responses to specific questions. Specifically, questions like “Do you currently drink alcohol,” “Do you presently smoke?” and “Do you do regular exercises?” Self-reported sleep status was based on the question “What do you think of your recent sleep situation?” and classified as Poor, Average, and Rich.
Health status included SRH, hypertension, heart disease, diabetes, and stroke. The assessment of SRH was contingent on the answer to the question “How do you rate your current health?” This was followed by the categorization of the resulting data as average (so-so), good (good or very good), and poor (bad or very bad). We carefully asked each person about the four types of chronic diseases—hypertension, heart disease, diabetes, and stroke—and each item was categorized as “Yes” or “No.”
Demographic and sociological characteristics, personal lifestyle choices, and health statuses were investigated using descriptive statistics. The distribution patterns of depressive symptoms among older adults living alone and those living in not-alone arrangements were analyzed using the chi-squared test. Subsequently, the binary logistic regression model was applied to assess the primary influencers of depressive symptoms within the contexts of both living conditions. These statistical analyses were executed utilizing SPSS 21.0 software. To further investigate the dynamics influencing and contributing to the divergence in depressive symptoms between older adults living alone and those cohabitating, the Fairlie model was employed. However, for the missing data of covariates, we used the multiple-imputation mothed to simulate, with each variable supplemented 10 times.
The software Stata MP16.0 was utilized for the assessment of data. The level of statistical significance was defined as 0.05.
Given that the dependent variable takes on two distinct values (a dichotomous variable), the Fairlie nonlinear decomposition approach was applied. This methodology allowed the decomposition of the variations in depressive symptoms by attributing them to different contributing factors. More details are provided in our previous studies (23, 24).
In total, this research involved 12,197 individuals. The outcomes of the descriptive statistical analyses for the older adults living alone and not alone in China are illustrated in Table 1. The resulting data indicated that 11.92% of these aged people had experienced depressive symptoms, while 88.08% had none. An elevated proportion of older adults living alone (15.76%) had experienced depressive symptoms in contrast to those living not alone (11.15%) (p < 0.001). The resulting data of a chi-squared test depicted variance in the distribution of the 10 covariates across the two living conditions. These encompassed: age, residence, sex, BMI, marital status, education level, self-reported local income status, self-reported sleep status, diabetes, and stroke.
The distribution of covariates was assessed across older adults living alone and those living with someone else with different depressive symptoms. The data are depicted in Table 2. The resulting data demonstrated that certain covariates exhibited dissimilar distribution patterns among older adults with and without depressive symptoms. These divergent characteristics were evident in the variables of sex, self-reported sleep status, self-reported health status, diabetes, and stroke.
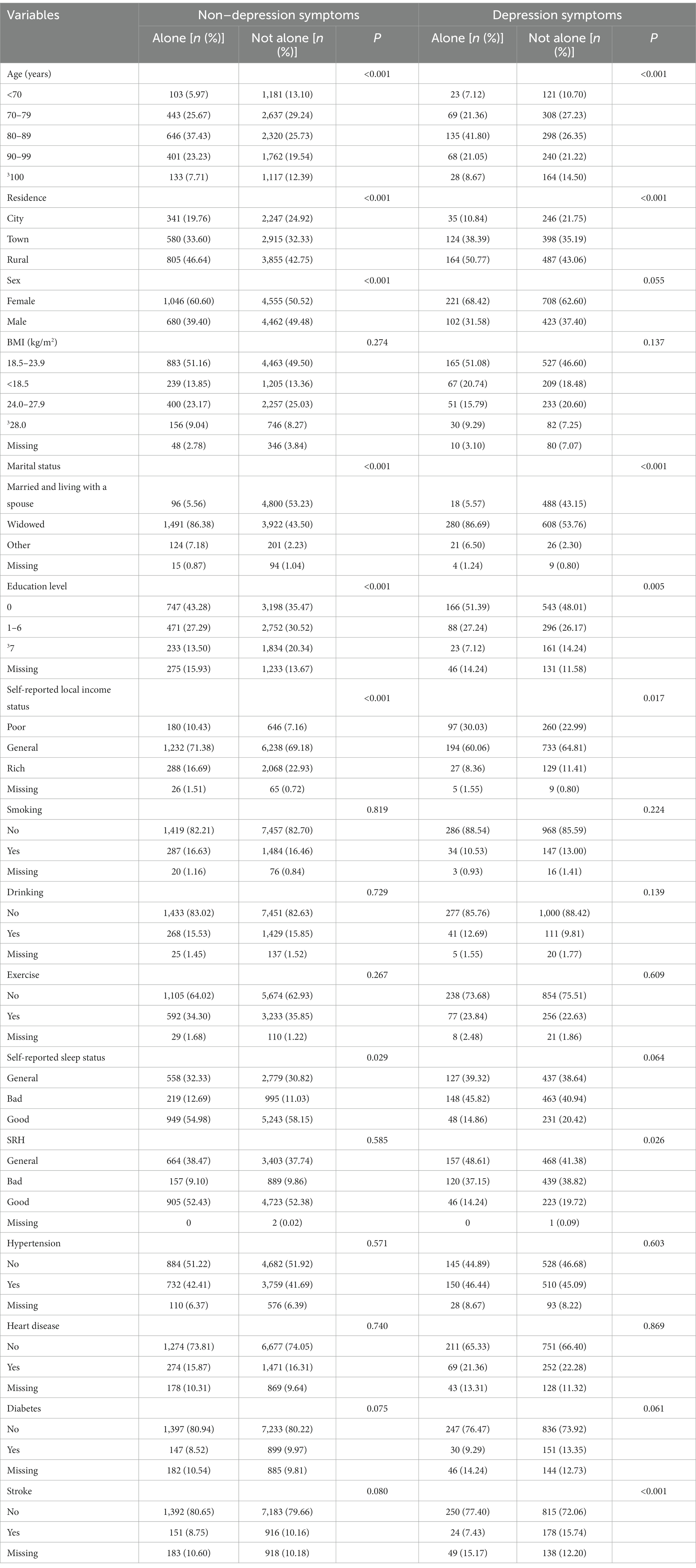
Table 2. Alone vs. not alone older adults differential in depression symptoms and non-depressive symptoms by selected background characteristics.
Table 3 reveals the resulting data of the logistic model calculations for depressive symptoms by older adults living alone or not alone in China. Among older adults living alone, age (70–79, OR = 0.352, 95%CI = 0.171–0.722, 80–89:OR = 0.482, 95%CI = 0.240–0.966; 90–99:OR = 0.420, 95%CI = 0.198–0.893), self-reported local income status (average: OR = 0.016; 95%CI = 0.374–0.904), self-reported sleep status (good: OR = 0.262; 95%CI = 0.161–0.425), and SRH (good: OR = 0.297; 95%CI = 0.186–0.472) were noted to act as protective factors. In contrast, self-reported sleep status (bad: OR = 2.613; 95%CI = 1.762–3.874) and SRH (bad: OR = 2.723, 95%CI = 1.781–4.161) were noted to function as risk factors for depressive symptoms. Among older adults living not alone, education level (≥7: OR = 0.639, 95%CI = 0.477–0.856), self-reported local income status (average: OR = 0.406, 95%CI = 0.323–0.511; rich: OR = 0.319, 95%CI = 0.234–0.436), exercise (yes: OR = 0.687-95%CI = 0.563, 0.838), self-reported sleep status (good: OR = 0.396, 95%CI = 0.321–0.489), and SRH (good: OR = 0.524, 95%CI = 0.423–0.650) were protective factors, and marital status (widowed: OR = 1.382, 95%CI = 1.109–1.720), self-reported sleep status (bad: OR = 2.462, 95%CI = 2.015–3.010), SRH (bad, OR = 2.557, 95%CI = 2.080–3.143), and diabetes (yes: OR = 1.304, 95%CI = 1.011–1.682) were risk factors for depressive symptoms.
Hence, the differences in depressive symptoms observed between individuals living alone and those in not-alone arrangements in China can be attributed to 3 primary areas. First, age (70–79: OR = 0.352, 95%CI = 0.171–0.722; 80–89:OR = 0.482, 95%CI = 0.240–0.966; 90–99:OR = 0.420, 95%CI = 0.198–0.893) was a protective factor only in older adults living alone. Second, education level (≥7: OR = 0.639, 95%CI = 0.477–0.856), self-reported local income status (rich: OR = 0.319, 95%CI = 0.234–0.436), and (yes: OR = 0.687-95%CI = 0.563, 0.838) were observed to be protective factors only in older adults living not alone. Third, marital status (widowed, OR = 1.382) and diabetes (yes, OR = 1.304) were risk factors only in older adults living not alone.
Table 4 depicts the resulting data of the decomposition model of the variation in depressive symptoms across older adults living alone and not alone in China. The results showed that 55.33% of the difference in depressive symptoms was owing to observed factors, whereas 44.67% was owing to factors involving living alone and not alone and other unobserved factors. To ensure the robustness Fairlie model, a multiple-impute model was established for supplementary analysis (supplement Table S1). Among the observed factors, specific elements played a remarkable role in explaining the differences in depressive symptoms (p < 0.05). These factors included marital status (20.55%), education level (4.63%), self-reported local income status (7.25%), self-reported sleep status (17.56%), and SRH (4.24%).
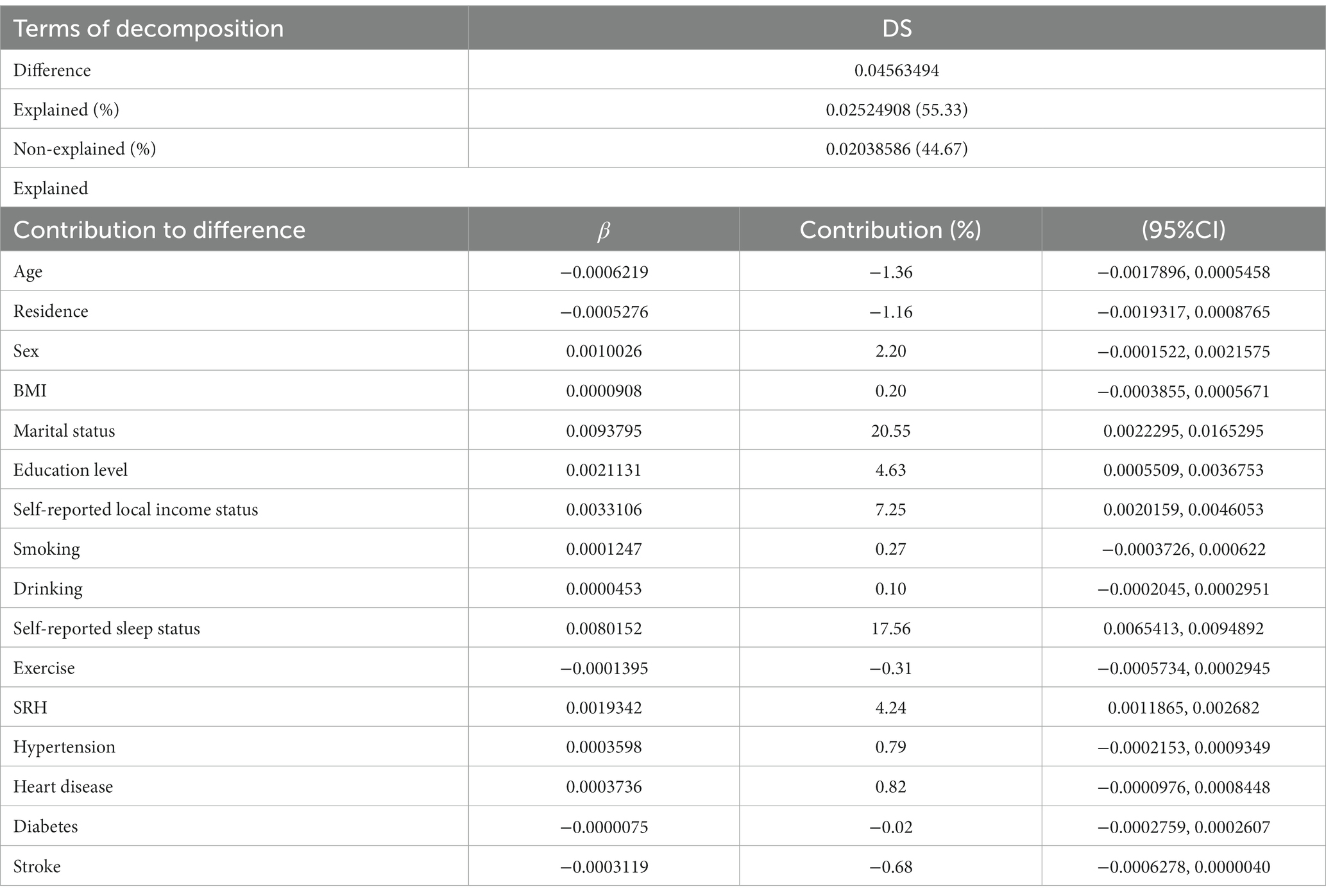
Table 4. Fairlie decomposition of depressive symptoms disparity between older adults living alone and not alone in China.
This research delved into the relationship between specific factors (e.g., demographic characteristics, sociological characteristics, and health status) and depressive symptoms among older adults living alone and not alone in China. Additionally, the study quantified the degree to which these factors contributed to the discernible variations in depressive symptoms among older adults. This investigation substantiated the presence of remarkable differences in depressive symptoms between older adults living alone and those cohabitating in not-alone arrangements within China.
This study showed that the prevalence of depressive symptoms among Chinese older adults (age ≥ 65) was 11.92%. Notably, this prevalence was considerably lower than that reported in a meta-analysis which indicated a prevalence of approximately 23.6% for depressive symptoms among Chinese older adults aged over 60 (25). The prevalence was recorded to be higher among older adults living alone (15.76%) than among older adults living not alone (11.15%), which was aligned with the data acquired through prior investigation of depressive symptoms among older adults in China (26, 27). This is mainly because living alone makes it easier to experience social isolation, and cognitive decline, which are risk factors for depression according to previous research (28–30). Additionally, the 4.61%-point difference in the prevalence of depressive symptoms between alone and not alone suggested that medical personnel must pay attention to older adults living alone and provide them with more professional support to alleviate any anxiety or depression.
Our logistic regression analysis revealed further differences between the covariates of depressive symptoms in Chinese older adults living alone and not alone. Age, marital status, education level, self-reported local income status, exercise, self-reported sleep status, SRH, and diabetes were associated with the presence of depressive symptoms, similar to the findings of other researchers (6, 31). Specifically, older adults living not alone but widowed had more depressive symptoms because this group lives with their children’s family and had negative interactions with family members because of the generation gap. In China, older adults are often required to care for their grandchildren, which leads to restrictions on social interactions (32). The group living not alone with shorter learning time had more depressive symptoms. This was likely because older adults with higher education time can find more ways to release their emotions and seek more ways like the Internet to treat depression symptoms, which was inconsistent with previous studies (33). Poor self-reported local income status would increase the risk of depressive symptoms, which can be attributed to the fact that older adults with lower income have lower life quality and limited access to treatment for depressive symptoms and other mental health issues (32, 34). The results indicated that lack of sleep was associated with more depressive symptoms in older adults, this was associated with cognitive decline which was confirmed to be prone to depression (35). SRH was based on subjective perceptions of their health, so Poor SRH means they were more dissatisfied with their health and found it difficult to actively participate in their lives (36). Additionally, incongruent with other findings (11, 37), the older adults living alone in this study were less likely to have depressive symptoms; however, the specific reasons for this require further investigation.
The results of the Fairlie model showed that this part of the difference was related to marital status (20.55%), education level (4.63%), self-reported local income status (7.25%), self-reported sleep status (17.56%), and SRH (4.24%). All factors were intervenable. If these intervening factors could be improved, the difference in depressive symptoms between Chinese older adults living alone and not alone could be reduced by about 55.33%. Thus, our study can provide targeted measures to reduce depression in older adults living alone according to the results of the Fairlie model. First, we should help older adults develop healthy lifestyles (i.e., regular exercise, and dietary patterns) while ensuring adequate sleep time and participation in social activities. Second, we should enhance protection for older adults living in poverty, especially in terms of health and other relevant aspects. Third, the government should pay attention to targeted older adults in need and encourage more young people to pay attention to the health of the targeted older adults through publicity, especially younger older adults who live alone, older adults who do not live alone but who have been widowed, and less educated older adults who do not live alone and in poverty. They should be offered an appropriate tilt in health insurance policies, and targeted assistance and aid programs should be formulated for them.
This research was limited in certain respects. First, the definition of depressive symptoms was based on the CES-D-10 scale, which, although widely validated and boasting good reliability, remains reliant on self-reporting, thus introducing potential inaccuracies in contrast to medical diagnoses. Second, the domain of factors influencing depressive symptoms is multifaceted, and while this research encompassed a subset of indicators, other significant variables (such as polypharmacy, dementia, osteoporosis, osteoarthritis, etc.) might not have been accounted for. Last, the expansive older adult population of China poses a challenge, as the CLHLS dataset utilized in this study covers only a fraction of this demographic and therefore cannot fully cover the entirety of older adults within the country.
The study findings contribute novel insights into the distinctions between older adults living alone and those living not alone within China. These results are poised to play a pivotal role in the refinement and establishment of mental health prevention and treatment policies targeted toward older adults in China. By accurately identifying the factors that influence living alone versus not alone conditions and their varying impacts on depressive symptoms, the groundwork is laid for the development of targeted and precise intervention strategies, aimed at enhancing the mental well-being of high-risk segments of the older adults. Ultimately, the problem of living alone and not alone differences in depressive symptoms will be effectively addressed.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
The data for this study were taken from the CLHLS, which is organized by the Center for Healthy Aging and Development Studies at Peking University and has been approved by the Research Ethics Committees of Peking University and Duke University. The data analyzed here are available in the public domain, and therefore, separate ethical approval was not required for this study.
CH: Formal Analysis, Funding acquisition, Project administration, Writing – original draft. ZD: Conceptualization, Data curation, Formal Analysis, Writing – original draft. HL: Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – original draft. SL: Conceptualization, Methodology, Project administration, Writing – review & editing. MD: Data curation, Investigation, Project administration, Writing – review & editing. TL: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. LY: Data curation, Project administration, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was sponsored by the Shanghai Sailing Program, Prediction of psychological stress of urban major infectious disease groups based on multi-agent modeling, 21YF1457500.
We thank the Center for Healthy Ageing and Development Studies at Peking University for organizing the CLHLS and all the participants, investigators, and assistants of the CLHLS.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1265834/full#supplementary-material
1. Tang, T, Jiang, J, and Tang, X. Prevalence of depressive symptoms among older adults in mainland China: a systematic review and meta-analysis. J Affect Disord. (2021) 293:379–90. doi: 10.1016/j.jad.2021.06.050
2. Marwaha, S, Palmer, E, Suppes, T, Cons, E, Young, AH, and Upthegrove, R. (2023). Novel and emerging treatments for major depression. Lancet. 401, 141–153. doi: 10.1016/S0140-6736(22)02080-3
3. Alexopoulos, GS. Depression in the elderly. Lancet. (2005) 365:1961–70. doi: 10.1016/S0140-6736(05)66665-2
4. Mushtaq, R, Shoib, S, Shah, T, and Mushtaq, S. Relationship between loneliness, psychiatric disorders and physical health? A review on the psychological aspects of loneliness. J Clin Diagn Res. (2014) 8:WE01–4. doi: 10.7860/JCDR/2014/10077.4828
5. Gonyea, JG, Curley, A, Melekis, K, Levine, N, and Lee, Y. Loneliness and depression among older adults in urban subsidized housing. J Aging Health. (2018) 30:458–74. doi: 10.1177/0898264316682908
6. Holwerda, TJ, van Tilburg, TGV, Deeg, DJH, Schutter, N, Van, R, Dekker, J, et al. Impact of loneliness and depression on mortality: results from the longitudinal ageing study Amsterdam. Br J Psychiatry. (2016) 209:127–34. doi: 10.1192/bjp.bp.115.168005
8. Guo, Y, Wang, T, Ge, T, and Jiang, Q. Prevalence of self-care disability among older adults in China. BMC Geriatr. (2022) 22:775. doi: 10.1186/s12877-022-03412-w
9. Fang, EF, Scheibye-Knudsen, M, Jahn, HJ, Li, J, Ling, L, Guo, H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
10. Zeng, Y, and Wang, Z. (2004). Changes in residential arrangements for old adults of Chinese families. Chin. J. Popul. Sci. 5, 4–10. doi:doi: 10.3969/j.issn.1000-7881.2004.05.001
11. Ormstad, H, Eilertsen, G, Heir, T, and Sandvik, L. Personality traits and the risk of becoming lonely in old age: a 5-year follow-up study. Health Qual Life Outcomes. (2020) 18:47. doi: 10.1186/s12955-020-01303-5
12. Qiu, QW, Qian, S, Li, JY, Jia, RX, and Xu, Y. Risk factors for depressive symptoms among older Chinese adults: a meta-analysis. J Affect Disord. (2020) 277:341–6. doi: 10.1016/j.jad.2020.08.036
13. Yujia, Z. Huaiming, Yi, Wei, Shen, et al. association of empty nest with depressive symptom in a Chinese elderly population: a cross-sectional study. J Affect Disord. (2015) 187:218–23. doi: 10.1016/j.jad.2015.08.031
14. Zhao, D, Hu, C, Chen, J, Dong, B, Ren, Q, Yu, D, et al. Risk factors of geriatric depression in rural China based on a generalized estimating equation. Int Psychogeriatr. (2018) 30:1489–97. doi: 10.1017/S1041610218000030
15. Wu, KY, Liu, CY, Chau, YL, and Chang, CM. Transient ischemic attack and incidence of depression in old age: evidence from a population-based analysis in Taiwan. Am J Geriatr Psychiatry. (2010) 18:382–7. doi: 10.1097/JGP.0b013e3181cabab1
16. Gong, Y, Wen, X, Guan, C, Wang, Z, and Liang, Y. The associations between family characteristics and depressive symptoms in older adults: a community-based survey in rural China. Int Psychogeriatr. (2012) 24:1226–34. doi: 10.1017/S1041610211002663
17. Cohen-Mansfield, J, Hazan, H, Lerman, Y, and Shalom, V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr. (2016) 28:557–76. doi: 10.1017/S1041610215001532
18. Chu, HS, Oh, J, and Lee, K. The relationship between living arrangements and sleep quality in older adults: gender differences. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19073893
19. Eli, B, Zhou, Y, Chen, Y, Huang, X, and Liu, Z. Symptom structure of depression in older adults on the Qinghai-Tibet plateau: a network analysis. Int J Environ Res Public Health. (2022) 19:13810. doi: 10.3390/ijerph192113810
20. Yuan, Y, Wang, K, Wang, Z, Zheng, H, Ma, Z, Liu, R, et al. Ambient ozone exposure and depression among middle-aged and older adults: Nationwide longitudinal evidence in China. Int J Hyg Environ Health. (2023) 251:114185. doi: 10.1016/j.ijheh.2023.114185
21. Zhang, X, Yan, G, Feng, Q, Razzaq, A, and Abbas, A. Ecological sustainability and households’ wellbeing: linking households’ non-traditional fuel choices with reduced depression in rural China. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph192315639
22. Andresen, EM, Malmgren, JA, Carter, WB, and Patrick, DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
23. Yuan, L, Zhao, Z, Wang, J, Du, M, Xiao, Y, Liu, L, et al. Decomposition and comparative analysis of the prevalence of and factors associated with smoking between the rural and urban elderly population in China: a national cross-sectional study. Front Public Health. (2022) 10:824587. doi: 10.3389/fpubh.2022.824587
24. Yuan, L, Xu, Q, Gui, J, Liu, Y, Lin, F, Zhao, Z, et al. Decomposition and comparative analysis of differences in depressive symptoms between urban and rural older adults: evidence from a national survey. Int Psychogeriatr. (2023) 2:1–12. doi: 10.1017/S1041610223000078
25. Li, D, Zhang, DJ, Shao, JJ, Qi, XD, and Tian, L. A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Arch Gerontol Geriatr. (2014) 58:1–9. doi: 10.1016/j.archger.2013.07.016
26. Lin, Y, Zhang, Q, Wang, T, and Zeng, Z. Effect of living arrangements on cognitive function in Chinese elders: a longitudinal observational study. BMJ Open. (2022) 12:e050410. doi: 10.1136/bmjopen-2021-050410
27. Zhang, Y, Liu, Z, Zhang, L, Zhu, P, Wang, X, and Huang, Y. Association of living arrangements with depressive symptoms among older adults in China: a cross-sectional study. BMC Public Health. (2019) 19:1017. doi: 10.1186/s12889-019-7350-8
28. Carbone, E, Piras, F, Pellegrini, FF, Caffarra, P, and Borella, E. Individual differences among older adults with mild and moderate dementia in social and emotional loneliness and their associations with cognitive and psychological functioning. BMC Geriatr. (2022) 22:859–72. doi: 10.1186/s12877-022-03517-2
29. Wu, D, Liu, F, and Huang, S. Assessment of the relationship between living alone and the risk of depression based on longitudinal studies: a systematic review and meta-analysis. Front Psych. (2022) 13:954857. doi: 10.3389/fpsyt.2022.954857
30. Yang, X, Qi, S, Wang, M, Calhoun, VD, Sui, J, Li, T, et al. Subtypes of depression characterized by different cognitive decline and brain activity alterations. J Psychiatr Res. (2021) 138:413–9. doi: 10.1016/j.jpsychires.2021.04.023
31. Chen, Y. Risk factors for depression among older adults living alone in Shanghai. China Psychogeriatr. (2022) 22:780–5. doi: 10.1111/psyg.12882
32. Ding, Y, Chen, L, and Zhang, Z. The relationship between social participation and depressive symptoms among Chinese middle-aged and older adults: a cross-lagged panel analysis. Front Public Health. (2022) 10:996606. doi: 10.3389/fpubh.2022.996606
33. Shen, T, Li, D, Hu, Z, Li, J, and Wei, X. The impact of social support on the quality of life among older adults in China: an empirical study based on the 2020 CFPS. Front Public Health. (2022) 10:914707. doi: 10.3389/fpubh.2022.914707
34. Guo, X, Meng, Z, Huang, G, Fan, J, Zhou, W, Ling, W, et al. Meta-analysis of the prevalence of anxiety disorders in mainland China from 2000 to 2015. Sci Rep. (2016) 6:28033. doi: 10.1038/srep28033
35. Meng, W, Gao, T, Zhong, Y, and Ge, L. Association between sleep and cognition of older adults in rural areas: a cross-sectional study. Inquiry. (2023) 60:004695802311718–9. doi: 10.1177/00469580231171820
36. Liu, H, Fan, X, Luo, H, Zhou, Z, Shen, C, Hu, N, et al. Comparison of depressive symptoms and its influencing factors among the elderly in urban and rural areas: evidence from the China health and retirement longitudinal study (CHARLS). Int J Environ Res Public Health. (2021) 18:3886. doi: 10.3390/ijerph18083886
Keywords: depressive symptoms, older adults, living status, China, Fairlie decomposition
Citation: Hu C, Dai Z, Liu H, Liu S, Du M, Liu T and Yuan L (2023) Decomposition and comparative analysis of depressive symptoms between older adults living alone and with others in China. Front. Public Health. 11:1265834. doi: 10.3389/fpubh.2023.1265834
Received: 24 July 2023; Accepted: 05 September 2023;
Published: 22 September 2023.
Edited by:
Farnam Mohebi, University of California, Berkeley, United StatesReviewed by:
Carlo Lazzari, International Centre for Healthcare and Medical Education, United KingdomCopyright © 2023 Hu, Dai, Liu, Liu, Du, Liu and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Yuan, eXVhbmxlaWd6QDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.