
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health, 17 October 2023
Sec. Public Health Education and Promotion
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1265122
This article is part of the Research TopicPromoting Health and Addressing Disparities Amongst Indigenous PopulationsView all 20 articles
 Katherine A. Hirchak1*
Katherine A. Hirchak1* Oladunni Oluwoye1
Oladunni Oluwoye1 Melanie Nadeau2
Melanie Nadeau2 Meenakshi Richardson1,3
Meenakshi Richardson1,3 Kelsey Bajet1
Kelsey Bajet1 Mariah Brigman1
Mariah Brigman1 Jalene L. Herron4,5
Jalene L. Herron4,5 Alexandra Hernandez-Vallant4,5
Alexandra Hernandez-Vallant4,5 Angel Vasquez4
Angel Vasquez4 Cuong Pham6
Cuong Pham6 Karen Anderson Oliver7
Karen Anderson Oliver7 Paulette Baukol8
Paulette Baukol8 Kellie Webb9
Kellie Webb9 Lorenda Belone10
Lorenda Belone10 Michael G. McDonell1
Michael G. McDonell1 Kamilla L. Venner4,5
Kamilla L. Venner4,5 Aimee N. C. Campbell11
Aimee N. C. Campbell11Introduction: Dissemination and Implementation (D&I) science is growing among Indigenous communities. Indigenous communities are adapting and implementing evidence-based treatments for substance use disorders (SUD) to fit the needs of their communities. D&I science offers frameworks, models, and theories to increase implementation success, but research is needed to center Indigenous knowledge, enhancing D&I so that it is more applicable within Indigenous contexts. In this scoping review, we examined the current state of D&I science for SUD interventions among Indigenous communities and identified best-practice SUD implementation approaches.
Methods: PubMed and PsycINFO databases were queried for articles written in English, published in the United States, Canada, Australia, and New Zealand. We included key search terms for Indigenous populations and 35 content keywords. We categorized the data using the adapted and extended Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework that emphasizes equity and sustainability. RE-AIM has also been used as a primary model to consistently identify implementation outcomes.
Results: Twenty articles were identified from the original unduplicated count of over 24,000. Over half the articles discussed processes related to Reach, Adoption, and Implementation. Effectiveness was discussed by 50% of the studies (n = 10), with 25% of the articles discussing Maintenance/sustainability (n = 4). Findings also highlighted the importance of the application of each RE-AIM domain for meaningful, well-defined community-engaged approaches.
Conclusion: Finding indicated a need to prioritize Indigenous methods to culturally center, re-align and adapt Western treatments and frameworks to increase health equity and improve SUD treatment outcomes. Utility in the use of the modified RE-AIM and the continued modification for Indigenous communities was also noted.
Many Indigenous communities are interested in providing culturally responsive treatments for substance use disorders (SUD) to their communities (1). While alcohol and rates of other substance use varies greatly across Indigenous communities and reasons for these variation are complex (2–5), there is a need to understand how to better integrate culturally appropriate approaches specific to community and Tribal histories, culture, policy, and concepts of well-being and recovery to reduce the negative consequences of substance use more effectively (3–5). Over the last decade, research on evidence-based SUD treatments among Indigenous people has increased (e.g., motivational interviewing, community reinforcement approach, contingency management), which creates an opportunity to assess the strategies used to implement these treatments in community- and Tribal-based clinical settings (1, 6, 7).
In non-Indigenous focused research, dissemination and implementation (D&I) science models, frameworks, and strategies can guide and facilitate successful adoption, implementation, and sustainment of evidence-based practices to enhance participant outcomes. Indigenous D&I research is emerging and growing (8). Given the historical and ongoing harms created by extractive research practices, it is important that strategies related to implementation of SUD treatment use a community-engaged approach to facilitate equitable research partnerships (9) and work towards health equity.
Recent D&I and intervention research among Indigenous communities has commonly used a community-based participatory research (CBPR) framework to address chronic health conditions and health behaviors related to disease prevention [e.g., hypertension, cardiovascular disease, nutrition, substance misuse prevention and treatment (9) and wellness (10–12)]. CBPR has been widely adopted by Indigenous researchers and community research sites because the approach aligns with Indigenous values of centering the knowledge and expertise of the community, and the importance of Tribal sovereignty with applied outcomes that directly support culturally centered community wellbeing and capacity building. CBPR processes facilitate bi-directional learning and power-sharing between communities and researchers in every step of the process by addressing issues of equity, partnership voice and trust (11–14). While CBPR is thought of as an implementation approach, it has only more recently been conceptualized within the D&I context (15, 16).
Although there are numerous D&I frameworks, models, and theories to support program implementation (17), a commonly used framework to guide implementation outcomes is the Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) Framework (18, 19) which has recently been expanded to include considerations around contextual factors, longer-term sustainability, and equity (20, 21). RE-AIM is comprised of five domains, each of which reference a particular area of evaluation: Reach refers to the proportion and characteristics of people who are affected by and engaged in the intervention; Effectiveness is how well the intervention works in a given setting; Adoption is the proportion and representativeness of participating and non-participating providers and settings; Implementation is the extent to which the intervention is delivered as intended (e.g., fidelity); and Maintenance (or Sustainability) is the extent to which the intervention becomes part of routine practice, as well as the long-term impact of the intervention.
While RE-AIM has evolved and been used within a range of contexts over the years (19), misconceptions about the framework persist. These assumptions primarily fall within four areas: that RE-AIM is simply for evaluation, the framework privileges quantitative over qualitative data, all dimensions must be weighted the same, and that the Maintenance phase encompasses only 6 months (22). Recently published studies have clarified that when appropriate (22–25), RE-AIM can incorporate qualitative and mixed methods designs, is not restricted to evaluation, and can be applied during dissemination, adoption, planning, and implementation (23). In addition, the framework has been expanded to include greater emphasis on sustainability (e.g., implementation for more than 1 year, integrating internal and external factors influencing implementation success) and health equity (21). For practitioners and researchers, applying RE-AIM during different phases of the project, while also maintaining a health equity and sustainability lens, better supports a multi-level approach that addresses the evolving needs related to capacity, as well as barriers and facilitators that many programs, organizations, and minoritized communities face. For Indigenous communities, the inclusion of a health equity and sustainability lens is particularly relevant for SUD treatment given health disparities in substance use related health outcomes, funding and capacity difficulties faced by Tribal health organizations.
The purpose of this scoping review is to inform future SUD evidence-based implementation research among Indigenous communities. A scoping review was identified by the study team as the appropriate approach because of the nascent nature of the state of the field. We sought to assess the existing evidence, clarify key concepts, and identify potential next steps to advance the science (26). While to our knowledge there are few completed published implementation trials for SUD interventions among Indigenous communities, we sought to inform future research and support practice change by examining a broad range of implementation strategies and processes among the more general Indigenous SUD treatment literature. Additionally, we reviewed whether Indigenous frameworks and worldviews have been centered in this work. Our guiding research question was what implementation processes or strategies are used among Indigenous communities for the uptake of evidence-based substance use treatment. We characterize the relevant research using the RE-AIM domains, contributing to previous work that has applied the framework with a focus on implementation (24, 25).
Literature searches and eligibility assessment occurred in June and July of 2021 using Preferred Reporting Items for Systematic reviews and Meta-Analysis guidelines [PRISMA-Equity; search activities were completed by author MR (27)]. The search strategy was conducted within PsycINFO and PubMed/Medline databases. The second step in the search protocol involved all combinations of our population and content keywords. Population keywords included words used to describe and identify Indigenous populations. There were more than 30 content keywords including reference to dissemination and implementation frameworks and approaches. Combinations of each population term and all content keywords were administered via advanced search options with selections made for peer-reviewed articles written in English.
Search keywords were either combined with “AND” or in one plain search phrase (e.g., American Indian and Alaska Native; Māori “AND” dissemination and implementation science; implementation strategies; Explore, Preparation, Implementation and Sustainment; health equity implementation framework; Indigenous Implementation Framework). For a complete list, please refer to the Supplementary materials. The third step in the research strategy was to take the references identified by all combinations of search terms from each database extraction and save them as Research Information Systems (RIS) text files that were then uploaded into COVIDENCE, a systematic review management software (28). Duplicates were identified and removed within the software system.
KH (descendent of the Eastern Shoshone Tribe/White, mixed European ancestry), MR (citizen of the Haliwa-Saponi Tribe), and KB (descendant of Filipino ancestry and immigrants) reviewed research articles for eligibility in COVIDENCE based on the title and the abstract. Study eligibility criteria was determined by the research team using knowledge of existing literature (e.g., anticipated state of the science), consideration of limitations of the research team (e.g., language capacity), and specific interest in SUD treatment implementation (29). Inclusion criteria were: (a) peer-reviewed, (b) written in English, (c) conducted with an Indigenous, adult (18 and older) population, (d) comprised of aims and outcomes related to substance misuse; (e) delivering an evidence-based intervention or practice based upon Western scientific criteria (e.g., efficacy or effectiveness randomized controlled trials), and (f) described one or more implementation processes or strategies. Exclusion criteria were: (a) studies completed entirely with non-Indigenous populations, (b) interventions intended for youth (younger than 18 years-old), (c) research that did not include outcomes related to substance use, and (d) research that did not discuss an evidence-based intervention (e.g., efficacy or effectiveness randomized controlled trials) for substance use. There was no exclusion based on publication date.
For articles which met initial eligibility criteria based on title and abstract, a full text review was conducted by KH and MR. Data extraction was completed by KH, MN (Turtle Mountain Band of Chippewa Indians), MR, KB, and MB (Spokane Tribe of Indians). Articles were initially reviewed independently and then underwent a second review by an alternate author to ensure validity and reliability of the extraction. None of the reviewers were individuals who had authored one of the articles. Consensus was determined and resolved by KH, MR, KB and MB. Final data review was carried out by KH and MR.
Once the final sample of articles was confirmed, the adapted RE-AIM framework was utilized for coding by two independent coders. While none of the studies were explicit D&I outcome studies, we coded the articles based upon what applied to the RE-AIM framework. This included articles that were clinical trials, methods papers, qualitative research, and case studies. Operational definitions based on the RE-AIM framework were identified and developed by the first author along with the review protocol (see Supplementary materials adapted from D’Lima et al. (30) and Shelton et al. (21)). The health equity and long-term sustainability extension codes were embedded within each existing domain. Codes were used to complete the data extraction within COVIDENCE, with final consensus completed in Excel.
For Reach, two questions were coded around the intended audience and who participated, as well as ways to better reach and engage the intended audience. Effectiveness was coded with three items related to whether the intervention was effective, if there had been any unintended consequences, and if intervention effectiveness was assessed over time. Adoption was assessed by three questions at the staff and setting level. This included application of the intervention and by whom, which staff were invited to participate versus excluded, and how staff were supported in delivering the intervention or could have been better supported. Implementation was assessed by six items ranging from efforts to culturally adapt the intervention, fidelity and delivery of the intervention, and costs. Maintenance was reviewed through the lens of sustainability of the intervention beyond 1 year and if multi-level contextual determinants were discussed that might impact sustainment.
The initial search produced 44,301 articles. After the removal of 19,379 duplicates, an additional 24,689 were deemed ineligible through title and abstract screening and 234 articles underwent full-text review. After the full text-review, 20 articles were identified for inclusion (see Figure 1). Just over one-third were methods or protocol papers and about half of the studies included a randomization component. Of the studies identified, 65% included AI/AN adults, 20% Aboriginal Australian adults, 10% First Nations adults, and 5% Native Hawaiian adults. The evidence-based SUD programs being implemented (sometimes in combination) included: nicotine replacement therapy (n = 8), motivational interviewing (n = 5), community reinforcement approach (n = 4), medications for opioid use disorder (n = 3), contingency management (n = 3), community reinforcement approach and family training (n = 2), and recovery housing (n = 1). Primary substance use outcomes included smoking cessation (n = 7), alcohol use (n = 6), more than one substance or not specified (n = 5), and opioid use (n = 3). All the interventions focused on the individual, with a little over half also having a family, community, or organizational component (n = 12). Only two of the studies intentionally included implementation strategies and existing dissemination and implementation frameworks, but this was integrated retrospectively (Table 1).
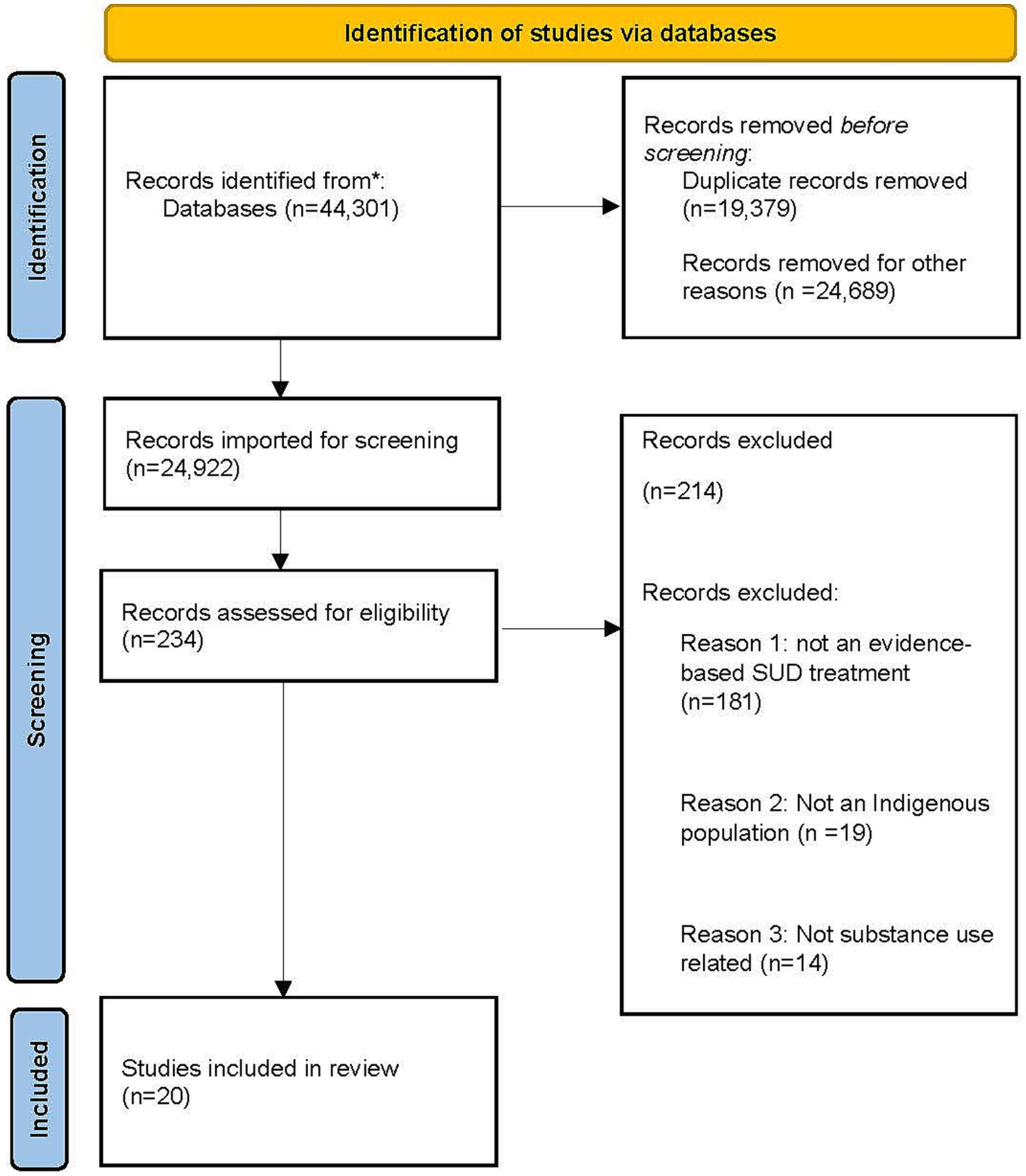
Figure 1. PRISMA flow diagram. Adapted from Page et al. (31).
Reach, Adoption, and Implementation were discussed by 60% of the studies. This was followed by Effectiveness (50% n = 10), with five studies discussing Maintenance/sustainability (25%, Table 2). Frequency and distribution of each of the domains coded in the literature are also presented (Figure 2). Below we provide descriptions of how the RE-AIM domain was characterized and include examples from the literature that highlight each domain. Definitions of domains and abbreviated summaries of examples can be found in Table 3.
Sixty percent of the studies reported Reach [n = 12; (33, 35–38, 40, 42, 45–48, 50)] with information mainly focused on inclusion and exclusion criteria for participants along with recruitment strategies (33, 35, 36, 40, 42, 45, 46, 48, 50). For example, Campbell and colleagues (35) noted that they recruited 58.8% (N = 40) out of the 68 clients that were eligible to participate in their study. In another study, the involvement of treatment providers from the community was also critical to Reach, with one study describing their recruitment efforts as including clinician referrals, radio newspaper, and digital (i.e., Facebook) ads, outreach at community events, and word-of-mouth (33). Reach was expanded in a pharmacist-led initiative through the Indian Health Service to increase access to medications for opioid use disorder [MOUD; (33)]. This was achieved by increasing the number of individuals initiated onto medications, poisoning awareness and procurement of naloxone kits that were distributed nationally. Other strategies around Reach included naloxone/drug take-back initiatives and engagement through culturally responsive educational tools (37).
Within the Reach domain, though not always referencing CBPR specifically, articles highlighted the importance of community buy-in and engaging collaborators on the project that were a part of the community and had knowledge of cultural protocols [e.g., how to appropriately greet an Elder; (50)]. Another common implementation strategy across studies was convening an advisory board (e.g., Community Advisory Board) or collaborative board to provide oversight on research activities, assist with recruitment and facilitate connections across organizations in the community. In one study, for example, the Community Advisory Board assisted in developing the culturally appropriate intervention title and how to brand the project in each community, identified and adapted measures, and guided focus groups to increase cultural acceptability of the intervention (40).
Trust was also emphasized in a few studies as another reason Reach was successful (36, 37). A trusting relationship between the participants and the research team was key. In these studies, it was argued that participants reported that they participated because they knew that the research team would manage their data with care, which speaks to data sovereignty and privacy. A unique aspect of Reach and trust was illustrated by a study completed in Australia (45). The authors described how “jealousy” played a significant role in recruitment. As reported by the authors, the spouses of participants were concerned that participation in research would provide opportunities for romantic infidelity. Research staff responded by developing strategies to make the intervention more welcoming and inclusive by providing opportunities to non-participating spouses. While specific to this community, this study demonstrates the importance of an engaged and flexible staff that can identify barriers and then develop solutions.
The need for flexibility in participant engagement strategies, and the ability to pivot based on community-generated solutions for health equity in substance use accessibility and capacity was, in fact, described across studies. For example, Orr and colleagues (47) initially intended to recruit AI/AN college students for their tobacco cessation program. However, recruitment efforts led to only 9 college students enrolling. The researchers then turned their recruitment strategy to Quitlines in states that had higher AI/AN rural populations (e.g., Alaska, New Mexico) and were able to complete their recruitment efforts. Another study identified recruitment challenges due to staff not having the time to recruit at the site, a short recruitment window, and eligibility criteria that were too stringent (38). One study team discussed needing to make changes to recruitment strategies when participants were screened eligible but declined to participate. Of note, the reasons for declining varied but were both practical and directly related to the research fit in the community. For example, participants reported not being comfortable with randomization, lack of interest in research, a preference for another type of treatment, and study location that was too far away (50).
Out of the 20 studies reviewed, ten (50%) of them reported outcomes related to intervention effectiveness (1, 34, 36, 38, 40, 41, 45, 48–50). There were several studies where the primary outcome was tobacco cessation [n = 7; (32, 36, 38, 45, 47–49)]. In a tobacco cessation program for pregnant Aboriginal women, self-reported 12-week 7-day point-prevalence abstinence was 13.6% (38). In another smoking cessation study integrated across two geographically and culturally distinct Aboriginal primary care settings, no statistically significant difference was observed in quit rates, but the study was also statistically underpowered (45). Although the quit rate varied, up to 43% of patients were tobacco free for 3 months across a healthcare system with five locations serving Native Hawaiian people (49).
Interventions addressing alcohol and other substance use also resulted in favorable outcomes. In a study assessing the effectiveness of Motivational Interviewing and Community Reinforcement Approach among a Tribal community in the Southwest United States, at 8 months, percent days abstinent had increased for both alcohol and cannabis, as well as other substances [excluding tobacco; (47)]. In the primary outcome clinical trial of Motivational Interviewing and Community Reinforcement Approach, participants in both the treatment, and treatment as usual (TAU), improved in percent days abstinent and substance use severity [MICRA PDA =72.63%, TAU = 73.62%; (1)]. At the three-month follow up in another study, Aboriginal participants in the Community Reinforcement Approach intervention had significantly reduced their alcohol use. There were also reductions in frequency of days of alcohol consumed and number of drinks consumed per drinking day based on pre- and post- self-report (34).
Sixty percent of the studies described processes and outcomes related to Adoption [n = 12; (1, 32, 36–38, 40–42, 44, 47–49)]. At the staff level, authors highlighted strategies, for and barriers to, Adoption. Including enhancements to Adoption focused on the staff members themselves. While some studies had specific inclusion and exclusion criteria for staff (32, 38, 48), Indigenous staff and level of staff buy-in were highlighted as the key to increasing Adoption (37, 41, 44). The duration of the intervention also impacted Adoption. While shorter interventions are generally considered easier to Adopt, some of the studies highlighted that shorter project duration among Indigenous communities actually inhibited long-term Adoption and more time was needed to build relationships (36, 38, 40). Recommendations to increase Adoption included hiring qualified study staff who were trusted community members cross-trained to facilitate coverage (38). Also, the quality of the Tribal-organization and university partnership and the need for relationship-building at all levels was of noted importance, for managing potential distrust of research by the community, as well as to facilitate approval processes from multiple entities (1, 33, 41, 46).
At the organizational level, Adoption was discussed in the context of recruitment success, with higher recruitment translating to better adoption (36, 41, 45). One study focused on tobacco cessation located at a healthcare system with different locations across the Hawaiian Islands. Differences in adoption by site were explained by barriers such as lower level of administrative or clinical support, staff turnover, and lower organizational readiness to adopt a new protocol or service (49). Although the authors initially assumed locations would be similar because they were within the same health system, each of the five locations evidenced variation in community needs, representation on the governing board, use of their medical record system, or attitudes toward medications for tobacco cessation (49).
Facilitators of Implementation were described at both the internal (i.e., organizational) and external levels, with 60% of studies touching upon this [n = 12; (1, 33–35, 37, 38, 40–43, 46, 47, 49)]. Organizations face an array of internal challenges (e.g., shifting priorities and reduced funding) along with external factors that impact what types of interventions may be supported or can be reimbursed. Authors discussed strategies related to the need for capacity building within and outside of the organization, having champions at multiple levels within (e.g., direct service, supervisor levels) and outside of the organization [e.g., Tribal leadership; (1, 40, 41, 49, 50)] and holding information meetings about the intervention for service providers outside of the organization (i.e., community members and leaders). Within the organization, it was recommended that there be on-going face-to-face communication between research staff and site staff and sharing of information and lessons from Implementation including monthly ongoing technical assistance/facilitation (1, 35, 38, 40, 41, 45).
Modifications to the intervention to enhance acceptability, integration, and implementation included cultural adaptations tailored to each setting. Making cultural adaptations to evidence-based substance use disorder treatment was described as a more holistic approach that sits within the cultural framework of the partnering community. This can take the form of integrating appropriate representation (e.g., art, study staff from the community) knowledge, and Indigenous worldviews into the evidence-based treatment which may also increase engagement and adoption (33, 42, 43, 50) (Table 1). Seventy-five percent of the studies (n = 15) mentioned culturally adapting the intervention, but only 15.0% (n = 3) described a specific framework guiding the adaptations made. While 90% of the studies mentioned a process of community engagement, only one-third of the studies explicitly stated the use of CBPR. Of those, there was no description or definition of how CBPR was being interpreted. None of the studies explicitly identified an Indigenous framework used as a part of the program implementation or intervention adaptation.
Examples of the commonly described cultural adaptation processes and methods included: focus groups, having members of the community lead the intervention, and culturally adapting materials (e.g., including Indigenous languages or pictures that represent the community). One study was initiated when a Tribal elected official contacted the researchers following the development of a community sober living house to assist with evaluation of feasibility, acceptability, and effectiveness (42). The study was unique in that the residents culturally adapted the model and the implementation processes in real time. The communal nature of the sober living house aligned with Tribal culture, and participants were able to include cultural activities (e.g., sweat lodge, talking circles with the inclusion of sacred objects like feathers, and drumming circles). Further modifications included the house being run by the residents who decided all activities, house rules and procedures. The house was also inclusive of non-Tribal members, so that anyone would have a home if they needed one, reflecting the Tribe’s values of providing social support and resources to those most in need (42).
Although funding is a core aspect of Implementation, it was not frequently discussed. Many of the studies did not directly specify the costs of delivering the evidence-based treatment, and, when funding was discussed, studies highlighted that it had enhanced Implementation efforts. For example, one study described how the total budget was dispersed across partnering communities during the duration of the research project and that this had been one of the major strengths of the collaboration [e.g., $1.8 million budget over 6 years for contingency management; (48)]. The authors of a multi-component intervention for smoking cessation among pregnant Aboriginal women did not list the entire cost of the intervention and delivery but noted that each site received $6,000 to support delivery of the intervention and staff contribution (38). In another study assessing recovery housing, Oxford Houses were argued to be self-sustaining and a lower cost option for post-treatment or recovery maintenance because each resident contributed to the cost of running the home. Professional staff were not employed (Oxford houses are operated by the residents) and residents’ rent typically amounted to about $100 per week (42).
Maintenance, or Sustainability, was the least discussed across studies with 20% of the articles including some discussion around this domain [n = 4; (39, 40, 44, 49)]. Multi-level factors related to sustainment suggested by a few authors included societal and policy forces (e.g., racism, historical trauma, poverty, and discrimination) but these components were not directly assessed within the studies (1, 41, 44, 45, 50). The studies that did highlight Sustainability also speculated on activities that may support or hinder the long-term delivery of the intervention. Authors also described future plans for program sustainment (39).
One qualitative study that examined a program delivering medications for opioid use disorder emphasized the need for community education and buy-in around harm reduction strategies to effectively sustain program activities. The need for education and training related to these medications was especially important to inform family members about how the medications worked to support treatment and how they were different from other types of opioids and illicit drugs (e.g., some family members were unsupportive of methadone maintenance treatment). Among those interviewed, there was a belief that the long-term impact of the medication for opioid use disorder program had been to increase cleanliness/safety (e.g., reduction in discarded needles) and reduce crime (e.g., burglary, vandalism) in the community. The program had already been on-going for 5 years by the time of publication, so institutionalization of the program was achieved, but the specifics of how this was accomplished were not discussed in detail (44).
In this scoping review, we assessed implementation strategies and processes employed by researchers and Indigenous communities to enhance the uptake and delivery of evidence-based substance use disorder treatments, applying a widely used public health framework, RE-AIM: Reach, Effectiveness, Adoption, Implementation, and Maintenance. Across eligible studies, the most often discussed processes were Implementation, Reach, and Adoption followed by Effectiveness and Maintenance/sustainability. Of the 10 studies that described Effectiveness, all but one intervention led to statistically significant improved substance use outcomes. The present study highlights the need for additional implementation research with Indigenous communities to better understand implementation strategies and outcomes that will support the integration of evidence-based practices to address substance use disorders.
Many of the studies referenced the importance of a community engaged or CBPR approach but few defined or detailed what this meant or how the CBPR methods were applied. Several articles also mentioned having a Community Advisory Board or Research Review Board, which are key principles of CBPR, but how exactly this was developed and deployed remained unclear (for examples see 51, 52). Additionally, most of the studies did not outline the use of specific frameworks, or dissemination and implementation theories and models. Future research should be model-driven and systematically describe the methods used with Indigenous communities to support this emerging knowledge base. Strategies and approaches in D&I research must also be pursued thoughtfully so that an emphasis or privileging of Western worldviews does not hinder the use or development of Indigenous frameworks to braid collaborations [e.g., the Indigenist-Stress Coping Model (53), the Two-Eyed Seeing approach (54) or the He Pikinga Waiora Implementation Framework; (55)]. As noted by McCuistian and Colleagues (56), a need exists for a well-specified model and plan for community engagement and CBPR approaches with minoritized communities. This is likely to support reach and engagement within the community and ensure that the intervention is desired and integrated appropriately for and with the community. Prior evidence also suggests that this may lead to improved intervention effectiveness (57).
A primary challenge to sustainability from the studies assessed in this review was lack of or insufficient funding. Lack of program sustainment creates further issues around trust between researchers and communities (e.g., when programs or research projects are visible in the community and then suddenly disappear when the funding ends). Challenges in program sustainment also inhibit the ability to truly impact health equity (58). Additionally, we found that despite the large sample of articles identified through the initial search, there were few that described implementation research specifically for SUD treatments with Indigenous communities. More work is needed that is culturally congruent or grounded (and specifies the methods for conceptual grounding) to increase both the literature on implementation strategies as well as the literature on evidence-based treatments.
Another component of our analysis was related to health equity and the integration of Indigenous frameworks. Findings indicated that while some of the articles intended to positively impact substance use outcomes, many did not discuss the multi-level determinants necessary for interventions to work [e.g., the social determinants of health or the importance of overall improved quality of life; (57)]. A few authors suggested that societal and policy forces (e.g., racism, historical trauma, poverty, and discrimination) should be considered (1, 41, 44, 45, 50), but it was not explicit as to how the interventions might seek to address these factors. It is important that future SUD treatment research is placed within the larger colonial-settler context so that Indigenous people are not further stigmatized or blamed for the consequences of colonization and to ensure that meaningful systems change occurs.
There were notable strengths of this review and several limitations. Reviewers may not have extracted all relevant data for the specified domain due to lack of clarity or explicit description within the article. However, our analysis of these data included independent assessment from at least two reviewers and consensus building across reviewers to increase scientific rigor. Second, this research was focused on evidence-based treatments and used a Western framework to structure the review. This may have reduced our ability to examine community-centered approaches. While our final sample included 20 articles, the initial unduplicated count was close to 25,000. We believe this was due to the extensive population and content search terms (35+; see Supplementary materials). Future studies may want to include fewer keywords and more focused search terms to summarize any recent literature accordingly, as this research area continues to grow. Although we used the PRISMA-Equity Extension checklist, future research might consider the development of an a priori review protocol. Despite this, a strength of this review was the extensive assessment of implementation strategies and processes used by researchers and communities to effectively increase the health and well-being of Indigenous people.
Among Indigenous communities, the field of D&I is expanding. Research partnerships have led to the implementation of culturally adapted evidence-based treatments for substance use disorders that are more in alignment with culture and holistic conceptualizations of health and well-being. Given the continued growth in the field, we provide 6 broad recommendations from our findings to move the science forward. (1) The need for more SUD interventions among Indigenous communities that also include ways to address or reduce the disproportionate health inequities related to the social determinants of health that contribute to substance use. (2) While some studies addressed factors related to Implementation, Reach, Adoption and Effectiveness, very few addressed Maintenance/sustainability, which could reflect insufficient or lack of long-term funding for research as well as insufficient resources more broadly within Indigenous communities. More community generated and sustained funding is required. (3) Additional thoughtfulness and application of the extended RE-AIM to include a greater emphasis on equity and sustainability in D&I and treatment research among Indigenous communities was lacking. Future research could consider opportunities to expand RE-AIM to include adaptations to the domains that support the use of the framework specifically within Indigenous communities. (4) The field could benefit from a comprehensive discussion on applying Indigenous frameworks and worldviews within the context of Western D&I frameworks, models or theories. (5) CBPR plays an important role in D&I with Indigenous communities and our findings highlighted the need for more detailed descriptions of how this work is defined, employed, and assessed within partnerships. (6) Local research capacity building and front-loading engagement activities are needed to help with Reach, Adoption, and sustainment. Successful research partnerships require attention to trust and long-term relationship building. As models of sustainability evolve in the broader D&I community to reflect the challenges in the fit between interventions and local context, we hope that there will be more application of these methods and techniques to ensure interventions serve the needs of Indigenous communities.
KH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Investigation. OO: Conceptualization, Methodology, Writing – review & editing. MN: Conceptualization, Formal analysis, Methodology, Writing – review & editing. MR: Data curation, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. KB: Data curation, Formal analysis, Methodology, Software, Writing – review & editing. MB: Data curation, Formal analysis, Methodology, Writing – review & editing. JH: Conceptualization, Writing – review & editing. AH-V: Conceptualization, Writing – review & editing. AV: Conceptualization, Writing – review & editing. CP: Conceptualization, Writing – review & editing. KO: Conceptualization, Writing – review & editing. PB: Conceptualization, Writing – review & editing. KW: Writing – review & editing. LB: Writing – review & editing. MM: Writing – review & editing. KV: Conceptualization, Writing – review & editing, Data curation, Methodology. AC: Conceptualization, Writing – review & editing, Data curation, Methodology.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding for this study was provided by grants from the National Institute of Drug Abuse (1UG1DA049468-01; PI: Page; UG1 DA013035, PIs: Rotrosen, Nunes; & R25 DA035163-09, PI: Masson) and the National Institute on Alcohol Abuse and Alcoholism (K01 AA028831-01, PI: Hirchak; T32 AA018108, PI: Witkiewitz).
The publication of the paper would not have been possible without the support and guidance of many wonderful people. We would also like to thank all the Indigenous communities for their leadership in research. A special acknowledgement is also due to the University of California-San Francisco Learning for Early Careers in Addiction & Diversity (LEAD) Team and Fellows. Much gratitude to the late James L. Sorensen. Dr. Sorensen’s many decades of mentorship and work endure. His endless encouragement and warmth will always be remembered and appreciated.
KO was employed at KEAO Consulting LLC. KV currently has a conflict-of-interest management plan at the University of New Mexico.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1265122/full#supplementary-material
1. Venner, KL, Serier, K, Sarafin, R, Greenfield, BL, Hirchak, K, Smith, JE, et al. Culturally tailored evidence-based substance use disorder treatments are efficacious with an American Indian southwest tribe: an open-label pilot-feasibility randomized controlled trial. Addiction. (2020) 116:949–60. doi: 10.1111/add.15191
2. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2020 national survey on drug use and health [internet]. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration (2021).
3. Greenfield, BL, and Venner, KL. Review of substance use disorder treatment research in Indian country: future directions to strive toward health equity. Am J Drug Alcohol Abuse. (2012) 38:483–92. doi: 10.3109/00952990.2012.702170
4. Burlew, AK, Copeland, VC, Ahuama-Jonas, C, and Calsyn, DA. Does cultural adaptation have a role in substance abuse treatment? Soc Work Public Health. (2013) 28:440–60. doi: 10.1080/19371918.2013.774811
5. Walter, M, and Carroll, SR. Indigenous data sovereignty, governance and the link to indigenous policy In: M Walter, T Kukutai, SR Carroll, and D Rodriguez-Lonebear, editors. Indigenous data sovereignty and policy [internet]. 1st ed. London: Routledge (2020)
6. McDonell, MG, Skalisky, J, Burduli, E, Foote, A, Granbois, A, Smoker, K, et al. The rewarding recovery study: a randomized controlled trial of incentives for alcohol and drug abstinence with a rural American Indian community. Addiction. (2021) 116:1569–79. doi: 10.1111/add.15349
7. McDonell, MG, Hirchak, KA, Herron, J, Lyons, AJ, Alcover, KC, Shaw, J, et al. Effect of incentives for alcohol abstinence in partnership with 3 American Indian and Alaska native communities: a randomized clinical trial. JAMA Psychiatry. (2021) 78:599–606. doi: 10.1001/jamapsychiatry.2020.4768
8. Blue Bird Jernigan, V, D’Amico, EJ, and Keawe’aimoku Kaholokula, J. Prevention research with indigenous communities to expedite dissemination and implementation efforts. Prev Sci Off J Soc Prev Res. (2020) 21:74–82. doi: 10.1007/s11121-018-0951-0
9. Holt, CL, and Chambers, DA. Opportunities and challenges in conducting community-engaged dissemination/implementation research. Transl Behav Med. (2017) 7:389–92. doi: 10.1007/s13142-017-0520-2
10. Rae, R, Belone, L, Tafoya, E, Yepa, M, Cohoe-Belone, B, Burbank, I, et al. Family listening/circle program: the experience of community action projects to promote family and community wellness in three tribal communities in New Mexico. Front Public Health. (2023) 11:1091751. doi: 10.3389/fpubh.2023.1091751
11. Werito, V, and Belone, L. Research from a Diné -centered perspective and the development of a community-based participatory research partnership. Health Educ Behav. (2021) 48:361–70. doi: 10.1177/10901981211011926
12. Walters, KL, Johnson-Jennings, M, Stroud, S, Rasmus, S, Charles, B, John, S, et al. Growing from our roots: strategies for developing culturally grounded health promotion interventions in American Indian, Alaska native, and native Hawaiian communities. Prev Sci. (2020) 21:54–64. doi: 10.1007/s11121-018-0952-z
13. Wallerstein, N, and Duran, B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. (2010) 100:S40–6. doi: 10.2105/AJPH.2009.184036
14. Dickerson, D, Baldwin, JA, Belcourt, A, Belone, L, Gittelsohn, J, Keawe’aimoku Kaholokula, J, et al. Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prev Sci. (2020) 21:33–42. doi: 10.1007/s11121-018-0926-1
15. Sacca, L, Shegog, R, Hernandez, B, Peskin, M, Rushing, SC, Jessen, C, et al. Barriers, frameworks, and mitigating strategies influencing the dissemination and implementation of health promotion interventions in indigenous communities: a scoping review. Implement Sci. (2022) 17:18. doi: 10.1186/s13012-022-01190-y
16. Belone, L, Rae, R, Hirchak, KA, Cohoe-Belone, B, Orosco, A, Shendo, K, et al. Dissemination of an American Indian culturally centered community-based participatory research family listening program: implications for global indigenous well-being. Genealogy. (2020) 4:99. doi: 10.3390/genealogy4040099
17. Nilsen, P. Making sense of implementation theories, models and frameworks. Implement Sci. (2015) 10:53. doi: 10.1186/s13012-015-0242-0
18. Glasgow, RE, Vogt, TM, and Boles, SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89:1322–7. doi: 10.2105/ajph.89.9.1322
19. Glasgow, RE, Harden, SM, Gaglio, B, Rabin, B, Smith, ML, Porter, GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. (2019) 7:64. doi: 10.3389/fpubh.2019.00064
20. McCreight, MS, Rabin, BA, Glasgow, RE, Ayele, RA, Leonard, CA, Gilmartin, HM, et al. Using the practical, robust implementation and sustainability model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl Behav Med. (2019) 9:1002–11. doi: 10.1093/tbm/ibz085
21. Shelton, RC, Chambers, DA, and Glasgow, RE. An extension of RE-AIM to enhance sustainability: addressing dynamic context and promoting health equity over time. Front Public Health. (2020) 8:134. doi: 10.3389/fpubh.2020.00134
22. RE-AIM [Internet]. Available at: https://re-aim.org/ (Accessed March 14, 2023).
23. Holtrop, JS, Estabrooks, PA, Gaglio, B, Harden, SM, Kessler, RS, King, DK, et al. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Transl Sci. (2021) 5:e126. doi: 10.1017/cts.2021.789
24. Glasgow, RE, Battaglia, C, McCreight, M, Ayele, RA, and Rabin, BA. Making implementation science more rapid: use of the RE-AIM framework for mid-course adaptations across five health services research projects in the veterans health administration. Front Public Health. (2020) 8:194. doi: 10.3389/fpubh.2020.00194
25. Heelan, KA, Abbey, BM, Bartee, RT, Estabrooks, PA, Malmkar, A, Jacobs, T, et al. Packaging of a pediatric weight management intervention and implementation blueprint for rural and Micropolitan communities: the Nebraska CORD 3.0 project. Child Obes. (2021) 17:S-62–9. doi: 10.1089/chi.2021.0171
26. Munn, Z, Peters, MDJ, Stern, C, Tufanaru, C, McArthur, A, and Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. (2018) 18:143. doi: 10.1186/s12874-018-0611-x
27. Welch, V, Petticrew, M, Tugwell, P, Moher, D, O’Neill, J, Waters, E, et al. PRISMA-equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. (2012) 9:e1001333. doi: 10.1371/journal.pmed.1001333
28. Covidence [internet]. Melbourne, Australia: Veritas Health Innovation; (2023). Available at: www.covidence.org
29. Levac, D, Colquhoun, H, and O’Brien, KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
30. D’Lima, D, Soukup, T, and Hull, L. Evaluating the application of the RE-AIM planning and evaluation framework: an updated systematic review and exploration of pragmatic application. Front Public Health. (2022) 9:755738. doi: 10.3389/fpubh.2021.755738
31. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement an update guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
32. Bar-Zeev, Y, Bonevski, B, Bovill, M, Gruppetta, M, Oldmeadow, C, Palazzi, K, et al. The indigenous counselling and nicotine (ICAN) QUIT in pregnancy pilot study protocol: a feasibility step-wedge cluster randomised trial to improve health providers’ management of smoking during pregnancy. BMJ Open. (2017) 7:e016095. doi: 10.1136/bmjopen-2017-016095
33. Burduli, E, Skalisky, J, Hirchak, K, Orr, MF, Foote, A, Granbois, A, et al. Contingency management intervention targeting co-addiction of alcohol and drugs among American Indian adults: design, methodology, and baseline data. Clin Trials. (2018) 15:587–99. doi: 10.1177/1740774518796151
34. Calabria, B, Shakeshaft, AP, Clifford, A, Stone, C, Clare, PJ, Allan, J, et al. Reducing drug and alcohol use and improving well-being for indigenous and non-indigenous Australians using the community reinforcement approach: a feasibility and acceptability study. Int J Psychol. (2020) 55:88–95. doi: 10.1002/ijop.12603
35. Campbell, ANC, Turrigiano, E, Moore, M, Miele, GM, Rieckmann, T, Hu, MC, et al. Acceptability of a web-based community reinforcement approach for substance use disorders with treatment-seeking American Indians/Alaska natives. Community Ment Health J. (2015) 51:393–403. doi: 10.1007/s10597-014-9764-1
36. Daley, CM, Daley, SM, Pacheco, CM, Smith, TE, Talawyma, M, McCloskey, C, et al. Feasibility of implementing the all nations breath of life culturally tailored smoking cessation program for American Indians in multi-tribal urban communities. Nicotine Tob Res. (2018) 20:552–60. doi: 10.1093/ntr/ntx030
37. Duvivier, H, Gustafson, S, Greutman, M, Jangchup, T, Harden, AK, Reinhard, A, et al. Indian Health Service pharmacists engaged in opioid safety initiatives and expanding access to naloxone. J Am Pharm Assoc. (2017) 57:S135–40. doi: 10.1016/j.japh.2017.01.005
38. Gould, GS, Bovill, M, Pollock, L, Bonevski, B, Gruppetta, M, Atkins, L, et al. Feasibility and acceptability of indigenous counselling and nicotine (ICAN) QUIT in pregnancy multicomponent implementation intervention and study design for Australian indigenous pregnant women: a pilot cluster randomised step-wedge trial. Addict Behav. (2019) 90:176–90. doi: 10.1016/j.addbeh.2018.10.036
39. Hanson, JD, Oziel, K, Sarche, M, MacLehose, RF, Rosenman, R, and Buchwald, D. A culturally tailored intervention to reduce risk of alcohol-exposed pregnancies in American Indian communities: rationale, design, and methods. Contemp Clin Trials. (2021) 104:106351. doi: 10.1016/j.cct.2021.106351
40. Hirchak, KA, Hernandez-Vallant, A, Herron, J, Cloud, V, Tonigan, JS, McCrady, B, et al. Aligning three substance use disorder interventions among a tribe in the Southwest United States: pilot feasibility for cultural re-centering, dissemination, and implementation. J Ethn Subst Abus. (2020) 21:1219–35. doi: 10.1080/15332640.2020.1836701
41. Hirchak, KA, Jansen, K, Lyons, AJ, Herron, J, Bergerson, D, Shaw, J, et al. Lessons shared: implementation of a randomized clinical trial for alcohol use disorders with five American Indian and Alaska native communities. Collab J Community-Based Res Pract. (2021) 4:5. doi: 10.33596/coll.76
42. Jason, LA, Kassanits, J, Reilly, A, Bobak, T, Guerrero, M, Stevens, E, et al. A promising recovery housing model for American Indian communities. J Community Psychol. (2019) 47:1926–36. doi: 10.1002/jcop.22237
43. Kiepek, N, Hancock, L, Toppozini, D, Cromarty, H, Morgan, A, and Kelly, L. Facilitating medical withdrawal from opiates in rural Ontario. Rural Remote Health. (2012) 12:2193. doi: 10.22605/RRH2193
44. Landry, M, Veilleux, N, Arseneault, JE, Abboud, S, Barrieau, A, and Bélanger, M. Impact of a methadone maintenance program on an aboriginal community: a qualitative study: Table 1. CMAJ Open. (2016) 4:E431–5. doi: 10.9778/cmajo.20150076
45. Marley, JV, Kitaura, T, Atkinson, D, Metcalf, S, Maguire, GP, and Gray, D. Clinical trials in a remote aboriginal setting: lessons from the BOABS smoking cessation study. BMC Public Health. (2014) 14:579. doi: 10.1186/1471-2458-14-579
46. McDonell, MG, Nepom, JR, Leickly, E, Suchy-Dicey, A, Hirchak, K, Echo-Hawk, A, et al. A culturally-tailored behavioral intervention trial for alcohol use disorders in three American Indian communities: rationale, design, and methods. Contemp Clin Trials. (2015) 47:93–100. doi: 10.1016/j.cct.2015.12.010
47. Orr, MF, Burduli, E, Hirchak, KA, Walsh Dotson, JA, Young, SL, Nelson, L, et al. Culturally-tailored text-messaging intervention for smoking cessation in rural American Indian communities: rationale, design, and methods. Contemp Clin Trials Commun. (2019) 15:100363. doi: 10.1016/j.conctc.2019.100363
48. Patten, CA, Lando, HA, Desnoyers, CA, Barrows, Y, Klejka, J, Decker, PA, et al. The healthy pregnancies project: study protocol and baseline characteristics for a cluster-randomized controlled trial of a community intervention to reduce tobacco use among Alaska native pregnant women. Contemp Clin Trials. (2019) 78:116–25. doi: 10.1016/j.cct.2019.01.012
49. Santos, LA, Braun, KL, and Kamuela Ae’a, LS. Institutionalizing a comprehensive tobacco-cessation protocol in an indigenous health system: lessons learned. Prog Community Health Partnersh. (2008) 2:279–89. doi: 10.1353/cpr.0.0038
50. Venner, KL, Greenfield, BL, Hagler, KJ, Simmons, J, Lupee, D, Homer, E, et al. Pilot outcome results of culturally adapted evidence-based substance use disorder treatment with a southwest tribe. Addict Behav Rep. (2016) 3:21–7. doi: 10.1016/j.abrep.2015.11.002
51. Hirchak, KA, Nadeau, M, Vasquez, A, Hernandez-Vallant, A, Smith, K, Pham, C, et al. Centering culture in the treatment of opioid use disorder with American Indian and Alaska native communities: contributions from a National Collaborative Board. Am J Community Psychol. (2023) 71:174–83. doi: 10.1002/ajcp.12620
52. Yuan, NP, Mayer, BM, Joshweseoma, L, Clichee, D, and Teufel-Shone, NI. Development of guidelines to improve the effectiveness of community advisory boards in health research. Prog Community Health Partnersh. (2020) 14:259–69. doi: 10.1353/cpr.2020.0026
53. Walters, KL, and Simoni, JM. Reconceptualizing native women’s health: an “Indigenist” stress-coping model. Am J Public Health. (2002) 92:520–4. doi: 10.2105/AJPH.92.4.520
54. Venner, KL, Donovan, DM, Campbell, ANC, Wendt, DC, Rieckmann, T, Radin, SM, et al. Future directions for medication assisted treatment for opioid use disorder with American Indian/Alaska natives. Addict Behav. (2018) 86:111–7. doi: 10.1016/j.addbeh.2018.05.017
55. Oetzel, J, Scott, N, Hudson, M, Masters-Awatere, B, Rarere, M, Foote, J, et al. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Glob Health. (2017) 13:69. doi: 10.1186/s12992-017-0295-8
56. McCuistian, C, Peteet, B, Burlew, K, and Jacquez, F. Sexual health interventions for racial/ethnic minorities using community-based participatory research: a systematic review. Health Educ Behav. (2023) 50:107–20. doi: 10.1177/10901981211008378
57. O’Mara-Eves, A, Brunton, G, Oliver, S, Kavanagh, J, Jamal, F, and Thomas, J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. BMC Public Health. (2015) 15:129. doi: 10.1186/s12889-015-1352-y
Keywords: dissemination and implementation science, indigenous research methods, community-based participatory research, American Indian and Alaska native adults, indigenous, scoping review, cultural centering
Citation: Hirchak KA, Oluwoye O, Nadeau M, Richardson M, Bajet K, Brigman M, Herron JL, Hernandez-Vallant A, Vasquez A, Pham C, Oliver KA, Baukol P, Webb K, Belone L, McDonell MG, Venner KL and Campbell ANC (2023) Coming together for something good: recommendations from a scoping review for dissemination and implementation science to improve indigenous substance use disorder treatment. Front. Public Health. 11:1265122. doi: 10.3389/fpubh.2023.1265122
Received: 21 July 2023; Accepted: 29 September 2023;
Published: 17 October 2023.
Edited by:
Eduardo Vasconez, University of the Americas, EcuadorReviewed by:
Alberto Rodriguez Lorenzana, University of the Americas, EcuadorCopyright © 2023 Hirchak, Oluwoye, Nadeau, Richardson, Bajet, Brigman, Herron, Hernandez-Vallant, Vasquez, Pham, Oliver, Baukol, Webb, Belone, McDonell, Venner and Campbell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katherine A. Hirchak, S2F0aGVyaW5lLmhpcmNoYWtAd3N1LmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.