- 1Department of Preventive Medicine and Public Health, University of Seville, Seville, Spain
- 2Department of Nursing, Pharmacology and Physiotherapy, University of Córdoba, Córdoba, Spain
- 3Research Group GE10 Clinical and Epidemiological Research in Primary Care, Instituto Maimónides de Investigación Biomédica de Córdoba (IMIBIC), Hospital Universitario Reina Sofía, Córdoba, Spain
Background: University students are a vulnerable population and faced a significant psychological impact from the COVID-19 pandemic. Therefore, this study aimed to determine the level of fear of COVID-19 among university students and to evaluate the possible relationship between fear of COVID-19 and socio-demographic, health-related determinants, variables related to the COVID-19 and variables related to the psychological impact of the COVID-19 pandemic.
Methods: We conducted a cross-sectional study between December 2020 and December 2021 on a sample of 950 university students from two universities in southern Spain. Participants completed a form that collected socio-demographic, health-related and COVID-related variables, a validated questionnaire related to the psychological impact of the COVID-19 pandemic and the fear of COVID Scale (FCV-19S). Descriptive, inferential, and multivariable linear regression analyzes were conducted.
Results: The mean FCV-19S score was 14.86 ± 5.16 points. The factors identified as predictors of FCV-19S were being female (p < 0.001), holding religious beliefs (p = 0.04), living in towns with over 10,000 inhabitants (p < 0.01), living with someone vulnerable to COVID-19 (p = 0.02), watching TV to keep informed about COVID-19 (p < 0.01), believing in a low probability of surviving if infected with COVID-19 (p < 0.001), having a higher level of death anxiety (p < 0.001) and suffering from insomnia (p < 0.001).
Conclusion: An average fear of COVID-19 score of 14.86 ± 5.16 points has been found among university students in Spain. These findings can aid in identifying specific factors contributing to fear of COVID-19 and in developing coping strategies to alleviate the stress of the pandemic.
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified as the cause of coronavirus disease 19 (COVID-19) in December 2019 (1). The rapid person-to-person transmission, as well as the severity of the virus across the globe (2), led to the implementation of several measures in Spain, including a general lockdown that started on March 15, 2020, and concluded on June 21, 2020. During this period of confinement, comprehensive measures were implemented, including the closure of restaurants, schools, universities, and workplaces which involved close physical contact. Governments also enforced physical distancing through quarantines, travel restrictions, and closures of various establishments such as theaters, cinemas, museums, and stadia. Remote work and online education became widespread, while the limited number of activities permitted included essential work, grocery shopping, caregiving, and medical visits (3). Nevertheless, during those 100 days of lockdown, there were 245,938 total confirmed cases of infection and 28,322 total deaths in Spain (4).
The lockdown period led not only a radical change in the population’s lifestyle (5), but also fear of COVID-19 (6) and a negative effect on mental health (7, 8) with reports of symptoms of common mental disorders in 35–50% of the population (9, 10). Fear, defined as an adaptive response to real or abstract threats which is crucial for survival (11), stands out as one of the most prevalent psychological reactions to pandemic diseases, and differs in responses to other disasters (12).
A multitude of adverse conditions, such as social isolation, uncertainty, chronic illness, financial hardships, disruptions to daily routines, and the loss of family members to COVID-19, particularly among the older adult, contributed to heightened levels of fear during the pandemic (13–16). This pervasive fear has had a profound and widespread impact on the mental health of millions of individuals worldwide (17). Several studies have investigated this impact on different groups (18–22), including university students, who were at risk due to the continued spread of the pandemic, strict isolation measures, and the restrictions on interpersonal relationships (23, 24).
In Spain, the level of fear of COVID-19 among university students (25) is higher than in other countries such as Turkey (26), China (27), Pakistan (28) or Russia and Belarus (29). Multiple studies worldwide performed in that population (30, 31) have shown the impact that fear of COVID-19 has on several psychological constructs. Thus, on the one hand, fear of COVID-19 plays a pivotal role in the initiation and progression of sleep difficulties, stress, panic and common mental disorders (32–37). On the other hand, death anxiety appears as an abnormal response when individuals experience fear regarding COVID-19 (38, 39). Additionally, previous studies reveal that other constructs such as social support, optimism, subjective happiness and resilience mitigates the fear of COVID-19, fostering better mental health in the battle against the virus (40–42).
Additionally, it is important to consider that the fear of COVID-19 has had an impact on the lifestyle habits of university students, such as resorting to increased alcohol or tobacco consumption as coping responses to the stressors associated with the COVID-19 pandemic (43), adopting less healthy dietary practices (44), and exhibiting a low level of physical activity (45).
The COVID-19 pandemic continues to pose significant health challenges (46, 47) and exerts an ongoing impact on a wide range of psychological responses in individuals (48), including university students (49). Despite the growing number of studies on the fear of COVID-19 worldwide, there is a noticeable gap in the scientific literature, to the best of our knowledge, particularly in terms of concurrently evaluating a variety of psychological constructs and assessing their influence in relation to the fear of COVID-19 among university students in Spain. Therefore, the present study aims to determine the level of fear of COVID-19 among university students and to evaluate the possible relationship between fear of COVID-19 and socio-demographic/health-related determinants, variables related to the COVID-19 and variables related to the psychological impact of the COVID-19 pandemic.
2. Materials and methods
2.1. Participants and procedure
We conducted a cross-sectional study among Spanish university students from December 2020 to December 2021.
The study was carried out in 12 different bachelor’s degree courses at two public universities located in the southern region of Spain, Andalusia. The majority of the students were taking degree courses in Health Sciences. Public university 1 had a total of 6,965 university students taking nine different bachelor’s degrees, while public university 2 contained a total of 1,417 university students studying for three different bachelor’s degrees. The exclusion criteria included students who did not fill out the questionnaires correctly, did not understand Spanish, were positive for COVID-19, and were on pharmacological and/or non-pharmacological therapy for anxiety.
The study population was assessed for suitability using Epidat version 4.2. (Ministry of Health, Xunta de Galicia, Galicia, Spain), which estimated a minimum sample size of 138 university students at a 95% confidence level, with an absolute precision of 1%, and a standard deviation of fear of COVID-19 of 6.04 points (50). The study subjects were selected by a non-probabilistic convenience sampling method and participated voluntarily in the study.
At both universities, the data collection was conducted during class hours. Before that, we had contacted the teachers responsible for the subjects involved so as to minimize the interferences in the correct development of the teaching methodology. The planned place, dates, and times to proceed with the data collection were agreed with the teachers. To maximize the response rate, the study was publicized during breaks between classes and on notice boards in common areas of various university faculties.
The students could complete the questionnaires easily by scanning a QR code of the URL of the Google Form with their smartphones. The questionnaires were created in Google Forms due to the advantages of being flexible, unlimited and free of charge (51). The form contained an informative letter emphasizing the voluntary and anonymous nature of the study, as well as an explicit consent form in which the university students agreed to cooperate and participate in the study.
Finally, data were collected from 1,162 students, and 950 completed all the questionnaire surveys, which satisfied the minimum sample size.
2.2. Measurements
2.2.1. Dependent variable: fear of COVID-19 scale (FCV-19S)
The level of emotional reactions of fear toward COVID-19 in individuals was assessed using the COVID-19 Fear Scale (FCV-19S) (30), validated in Spain (50). The scale involves responding to items on a 7-point Likert scale, ranging from ‘strongly disagree’ to ‘totally agree’, with scores ranging from 1 for ‘strongly disagree’ to 5 for ‘totally agree’. The total possible score ranges from 7 to 35, with a higher score indicating a higher level of fear toward COVID-19. The measure showed appropriate internal validity (Cronbach’s alpha: 0.83).
2.2.2. Independent variables
A self-administered survey containing questions concerning the following variables was used to collect the data:
2.2.2.1. Socio-demographic characteristics of Spanish university students
The socio-demographic data collected included the following: gender (women, men), age (18–24 years, 25–35 years, > 35 years), religious belief (yes, no), spiritual practice (yes, no), belief in life after death (yes, no), population of town/city (< 10,000 inhabitants, 10,000–100,000 inhabitants, > 100,000 inhabitants), type of housing (flat without balcony, terrace or courtyard; house without garden or courtyard; flat with balcony, terrace or courtyard; house with garden or courtyard) and number of people sharing the accommodation (not including the participant who answered).
2.2.2.2. Health-related determinants in Spanish university students
The health-related determinants collected included the following: leisure-time physical activity (I do no exercise - I spend my free time almost exclusively sitting down; I occasionally do sports or physical exercise; I do physical exercise several times a month; I do sports or physical exercise several times a week), current smoker (yes, no), frequency of alcohol consumption in the past 12 months (never, less than once a month, monthly, weekly, daily or almost daily) and self-assessed state of health in the past 12 months (very good, good, average, bad, very bad).
2.2.2.3. Variables related to COVID-19 in Spanish university students
The variables related to COVID-19 were collected from a previous study (52) and included the following: living with someone considered to be in a vulnerable group to COVID-19 (yes, no), watching television to stay informed about COVID-19 (little or not at all, only at specific times, most of the day), time spent using the Internet to stay informed about COVID-19 (little or not at all, only at specific times, most of the day), time spent using social networks to stay informed about COVID-19 (little or not at all, only at specific times, most of the day), time spent reading the press (newspapers) to stay informed about COVID-19 (little or not at all, only at specific times, most of the day) (Cronbach’s alpha of 0.62), the probability you think you have of surviving if you become infected with SARS-CoV-2 [5-point Likert scale ranging from 1 (no probability) to 5 (very high probability)], how effective you think preventive measures are to avoid infection with COVID-19 [5-point Likert scale ranging from 1 (not effective at all) to 5 (very effective)], and how satisfied you are with the measures adopted to control the COVID-19 pandemic [5-point Likert scale ranging from 1 (not satisfied at all) to 5 (very satisfied)]. Finally, to prevent the spread of COVID-19, the following items were used (never, rarely, sometimes, nearly always, always): (i) ‘I do not leave the house except to do the shopping or some other essential activity’, (ii) ‘If I have respiratory symptoms, I avoid close contact with other people by staying home’, (iii) ‘I keep a distance of at least 1.5 m from other people’, (iv) ‘When I sneeze or cough, I cover my mouth and nose with my elbow’, (v) ‘I avoid touching my eyes, nose and mouth with my hands’, (vi) ‘I use disposable tissues when sneezing or wiping my nose and throw them away after use’, (vii) ‘I wash my hands frequently’, (viii) ‘I use a mask’, (ix) ‘When I go outside, I mainly stay in outdoor spaces’ and (x) ‘I ventilate closed spaces frequently’ (Cronbach’s alpha of 0.83).
2.2.2.4. General health questionnaire (GHQ-12)
The assessment of common mental disorders was conducted using the 12-item General Health Questionnaire (GHQ-12) (53), which was validated for the Spanish population (54, 55). The GHQ-12 utilizes a Likert-like scale with response options ranging from 0 (‘more than usual’) to 3 (‘much less than usual’). The scoring in the response categories followed the original GHQ method (56), where the first two response options were scored 0 and the last two received a score of 1, resulting in a bimodal score (0–0–1-1). The total score ranged from 0 to 12, with higher scores indicating a greater degree of psychological distress. The measure demonstrated adequate internal validity (Cronbach’s alpha of 0.90).
2.2.2.5. Duke-UNC functional social support questionnaire (DUKE-UNC-11)
The Duke-UNC-11 questionnaire (57), which was validated for use in Spanish populations (58), was utilized to collect information regarding perceived personal social support. The questionnaire comprises 11 items, each scored on a Likert-like scale ranging from 1 (‘much less than I would like’) to 5 (‘as much as I would like’). The total perceived social support score is obtained by adding together the scores of all 11 items, which range from 11 to 55, with higher scores indicating a greater level of perceived social support. Internal validity was adequate (Cronbach’s alpha of 0.90).
2.2.2.6. Death anxiety inventory (DAI)
The level of death anxiety was assessed using the Death Anxiety Inventory (DAI), which was initially developed in Spanish (59). The DAI consists of 20 items, and respondents rated their agreement with each item on a 5-point Likert scale ranging from 1 (‘totally disagree’) to 5 (‘totally agree’). The total possible score ranges from 20 to 100, with higher scores indicating a higher level of death anxiety. The DAI had excellent internal consistency in this sample (Cronbach’s alpha of 0.92).
2.2.2.7. Subjective happiness scale (SHS)
Subjective happiness was assessed using the Subjective Happiness Scale (SHS) (60), which has been validated for use in Spain (61). The scale comprises 4 items presented in a Likert format that measure global subjective happiness through self-rated statements or by comparing oneself to others. The Likert-type scale ranges from 1 (‘not at all’) to 7 (‘to a great extent’), and the total score ranges from 4 to 28 points. Higher scores on the SHS indicate greater levels of global subjective happiness. The scale has an adequate unitary structure and temporal stability, as confirmed in these samples (Cronbach’s alpha of 0.81).
2.2.2.8. Life orientation test-revised (LOT-R)
The Life Orientation Test-Revised (LOT-R) (62, 63), which has been adapted for use in Spanish (64, 65), was used to quantitatively assess the participants’ levels of optimism. The LOT-R comprises ten items, with three items measuring optimism (items 1, 4, and 10), three items measuring pessimism (items 3, 7, and 9), and four neutral filler items (items 2, 5, 6, and 8). Response options are on a Likert scale ranging from 0 (‘strongly disagree’) to 4 (‘strongly agree’), resulting in a total scale range of 0 to 24, which contains both the optimism scale and the inverted pessimism scale. Higher scores on the LOT-R indicate higher levels of optimism. The measure showed appropriate internal validity (Cronbach’s alpha of 0.68).
2.2.2.9. Connor-Davidson resilience scale (CD-RISC)
The level of resilience was measured using the Connor-Davidson Resilience Scale (CD-RISC), a 10-item scale developed by Campbell and Stein (66) and validated in Spain by Notario et al. (67). Each item is rated on a 5-point Likert scale ranging from 0 (‘not true at all’) to 4 (‘true nearly all the time’). The total score ranges from 0 to 40, with higher scores indicating higher levels of resilience. Cronbach’s alpha displayed a good internal consistency (Cronbach’s alpha of 0.84).
2.2.2.10. Athens insomnia scale (AIS-8)
The Athens Insomnia Scale (AIS-8) (68), validated in Spain (69), was used to measure insomnia. The scale consists of 8 items that assess various aspects of sleep difficulty, including sleep induction, night wakings, early morning waking, total sleep time, sleep quality, and the consequences of insomnia the following day, including its effects on functional capacity, well-being, and sleepiness. Responses are rated on a Likert scale from 0 (‘no problem’) to 3 (‘serious problem’). The total score ranges from 0 to 24 points, with higher scores indicating more severe insomnia. The measure showed appropriate internal validity (Cronbach’s alpha of 0.82).
2.3. Ethics statement
The study received approval from the clinical research ethics committee (approval number 316, reference 4845).
The study adhered to the principles of good clinical practice and followed the ethical guidelines outlined in the latest version of the Declaration of Helsinki, including the Oviedo agreement, as well as Law 14/2007, dated July 3, concerning Biomedical Research. The confidentiality of the data was strictly maintained at all times by ensuring the anonymity of the data on the database, in compliance with Organic Law 3/2018, dated December 5, on the Protection of Personal Data and guaranteeing digital rights.
2.4. Statistical analysis
Descriptive statistics were used to analyze both the categorical variables, including frequencies and percentages, and the quantitative variables, including means and standard deviations. The Kolmogorov–Smirnov test was also used to assess the normality of the variables. Student’s t and ANOVA tests were used to investigate the relationship between FCV-19S scores and the socio-demographic/health-related determinants, variables related to COVID-19 and variables related to the psychological impact of the COVID-19 pandemic, and Pearson’s correlation test was used for correlations between quantitative variables. The variables that demonstrated a statistically significant association with Fear of COVID-19 scores (p < 0.05) were later integrated into a multivariable linear regression model. The goodness of fit of the final model was assessed using the adjusted coefficient of determination R2. Validation of the collinearity conditions (through analysis of the variance inflation factor), normality, and independence of residuals was confirmed using the normality test and Durbin-Watson test, respectively. The IBM SPSS Statistical package version 26.0.0 (IBM Corp, Armonk, NY, United States), licensed to the University of Seville (Spain), was used to carried out the statistical analysis.
3. Results
3.1. Descriptive analysis of socio-demographic characteristics and health-related determinants in Spanish university students
We evaluated the data from 950 Spanish university students, mostly aged 18 to 24 years old (92.74%). Most of these students were women (74.11%), did not engage in spiritual practice (70.53%), lived in a town with over 100,000 inhabitants (44.00%), and their self-assessed state of health in the past 12 months was good (55.37%) (Table 1).
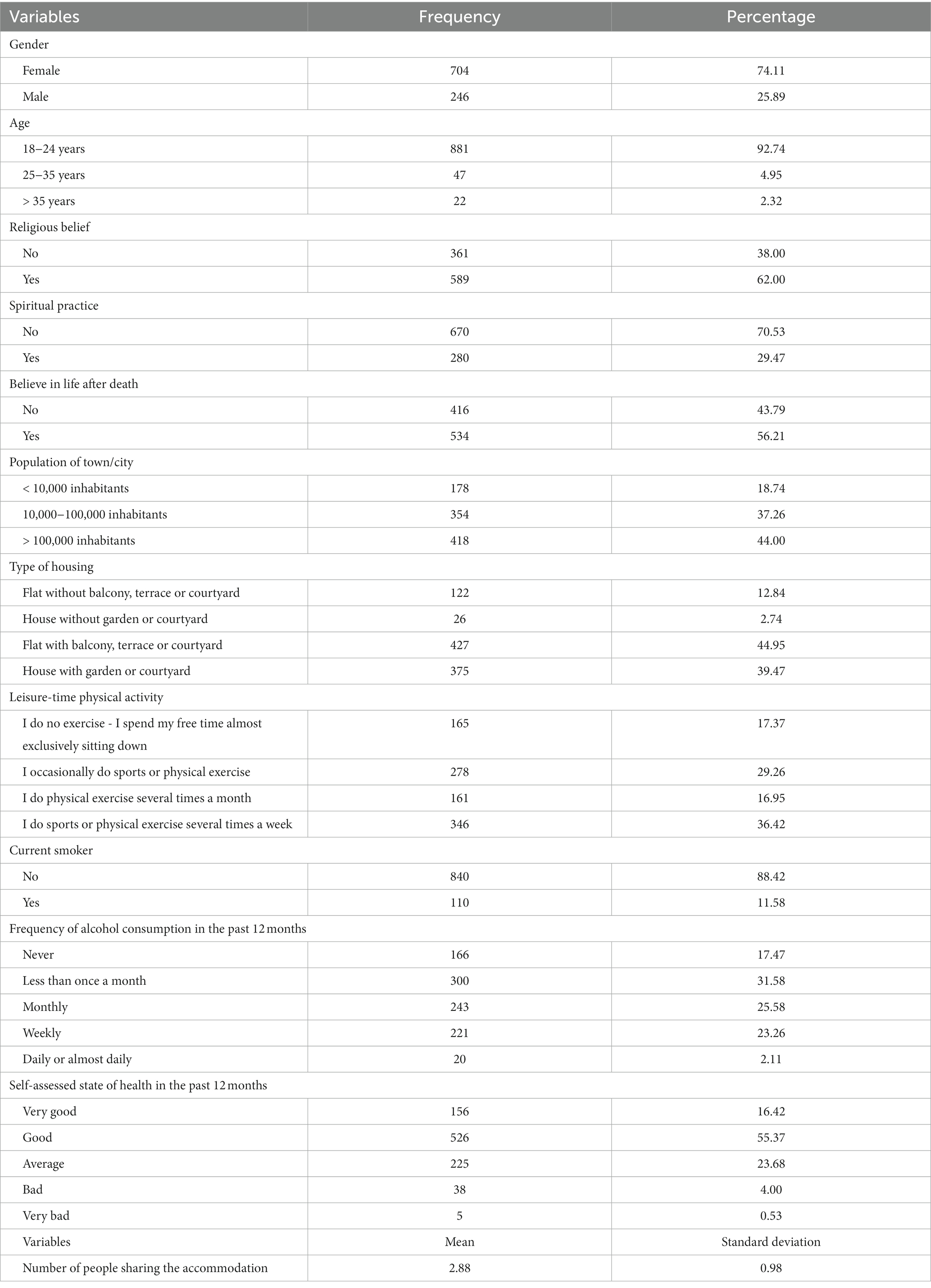
Table 1. Socio-demographic characteristics and health-related determinants of Spanish university students (n = 950).
3.2. Descriptive analysis of variables related to COVID-19 in Spanish university students
The majority of participants reported not living with someone considered to be in a group vulnerable to COVID-19 (56.11%), watching television only at specific times to stay informed about COVID-19 (64.95%), using the Internet only at specific times to stay informed about COVID-19 (58.95%), using social networks to stay informed about COVID-19 only at specific times (51.16%), and spending little or no time reading the press (newspapers) to stay informed about COVID-19 (67.58%). In addition to this, the participants felt that the probability of surviving if they became infected with COVID-19 were high (4.49 ± 0.72 points). Moreover, they considered the preventive measures to be moderately effective (3.06 ± 0.88 points) and were moderately satisfied (2.81 ± 0.99 points) with the measures adopted to control the COVID-19 pandemic in Spain.
In terms of actions taken to prevent the spread of COVID-19, the majority of Spanish university students reported always wearing a mask (85.69%), covering their mouth and nose with their elbow when coughing or sneezing (74.10%), and prioritizing outdoor spaces when going outside (71.58%) (Figure 1).
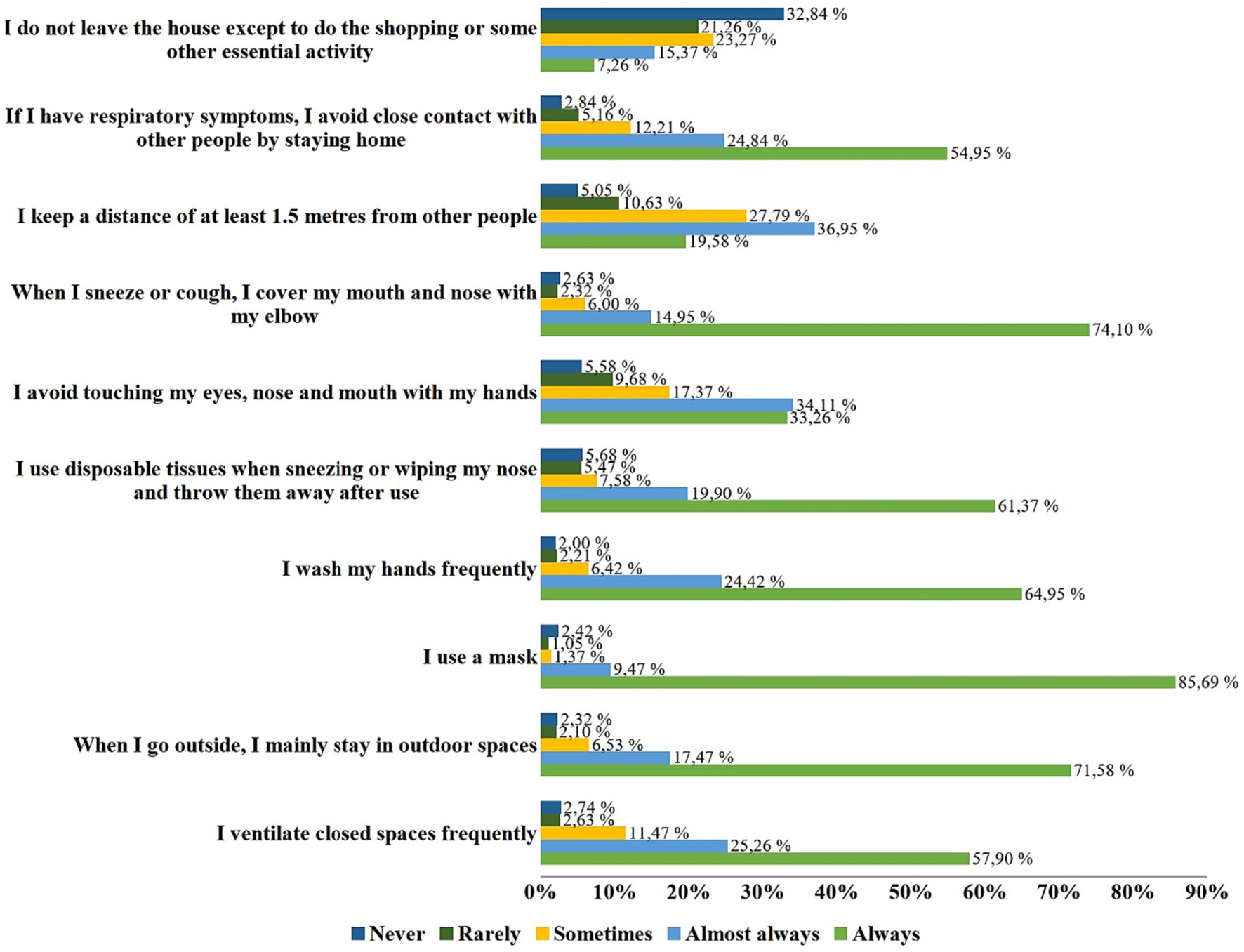
Figure 1. Actions to help preventing the spread of COVID-19 by Spanish university students (n = 950).
3.3. Descriptive and correlational analysis of fear of COVID-19 and variables related to the psychological impact of the COVID-19 pandemic
As shown in Table 2, the average fear of COVID-19 score among Spanish university students was found to be 14.86 ± 5.16 points and was positively correlated with common mental disorders (r = 0.680, p = 0.036) and death anxiety (r = 0.472, p < 0.001). On the contrary, fear of COVID-19 was negatively correlated with social support (r = −0.081, p = 0.012), optimism (r = −0.142, p < 0.001), resilience (r = −0.156, p < 0.001) and insomnia (r = −0.157, p < 0.001).
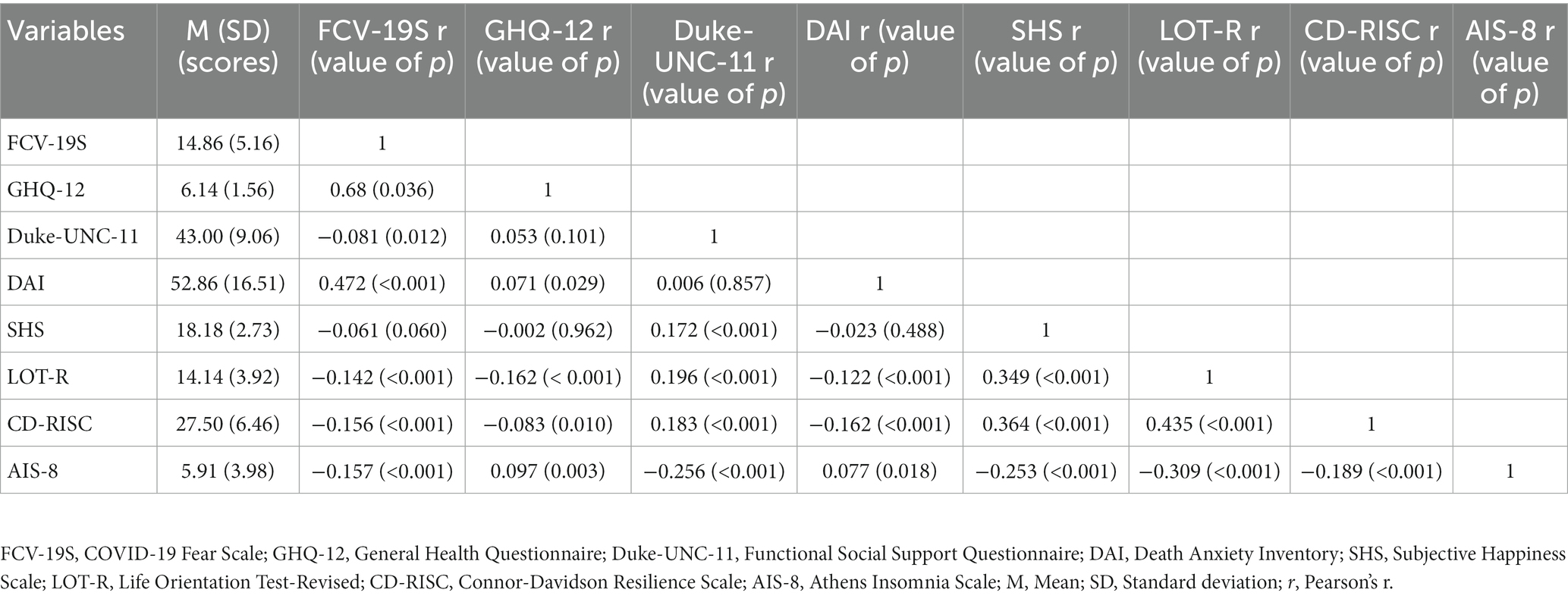
Table 2. Description and correlation between fear of COVID-19 and variables related to the psychological impact of the COVID-19 pandemic in Spanish university students (n = 950).
3.4. Relationship of the fear of COVID-19 with socio-demographic characteristics and health-related determinants in Spanish university students
Statistically significant differences in socio-demographic characteristics and health-related determinants among Spanish university students were observed (Table 3). A higher score of fear of COVID-19 was reported among females (t = −6.11, p < 0.0001), those who lived in a town with less than 10,000 inhabitants (F = 1.82, p = 0.009), those who practiced a religion (t = 0.24, p < 0.0001) and believed in life after death (t = −1.09, p = 0.018), and participants who reported a bad self-assessed state of health in the past 12 months (F = 2.07, p < 0.0001).
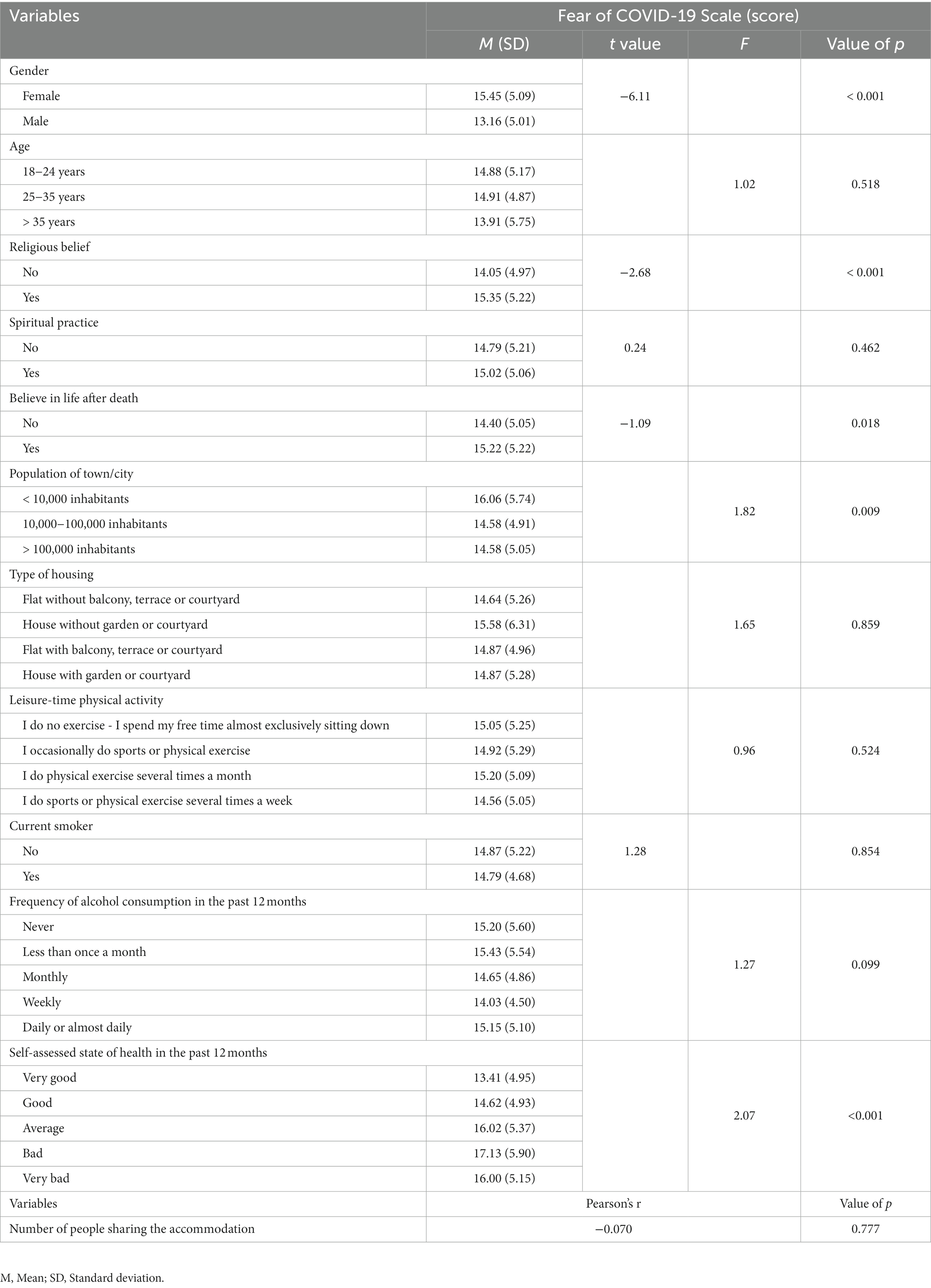
Table 3. Comparative analysis of participants’ Fear of COVID-19 scores and socio-demographic characteristics and health-related determinants in Spanish university students (n = 950).
3.5. Comparison of the fear of COVID-19 and variables related to COVID-19 in Spanish university students
Fear of COVID-19 was higher in university students who lived with someone considered to be in a group vulnerable to COVID-19 (t = −2.24, p = 0.022), watched television, used the Internet and social networks most of the day to stay informed about COVID-19 (F = 3.41, p < 0.0001; F = 2.11, p = 0.010; F = 2.03, p < 0.0001, respectively), and spent only a short time reading the press (newspapers) to stay informed about COVID-19 (F = 2.03, p = 0.040). Lastly, a negative correlation was found between fear of COVID-19 and the probability of the participants believing they could survive if they became infected with COVID-19 (r = −0.580, p = 0.009; Table 4).
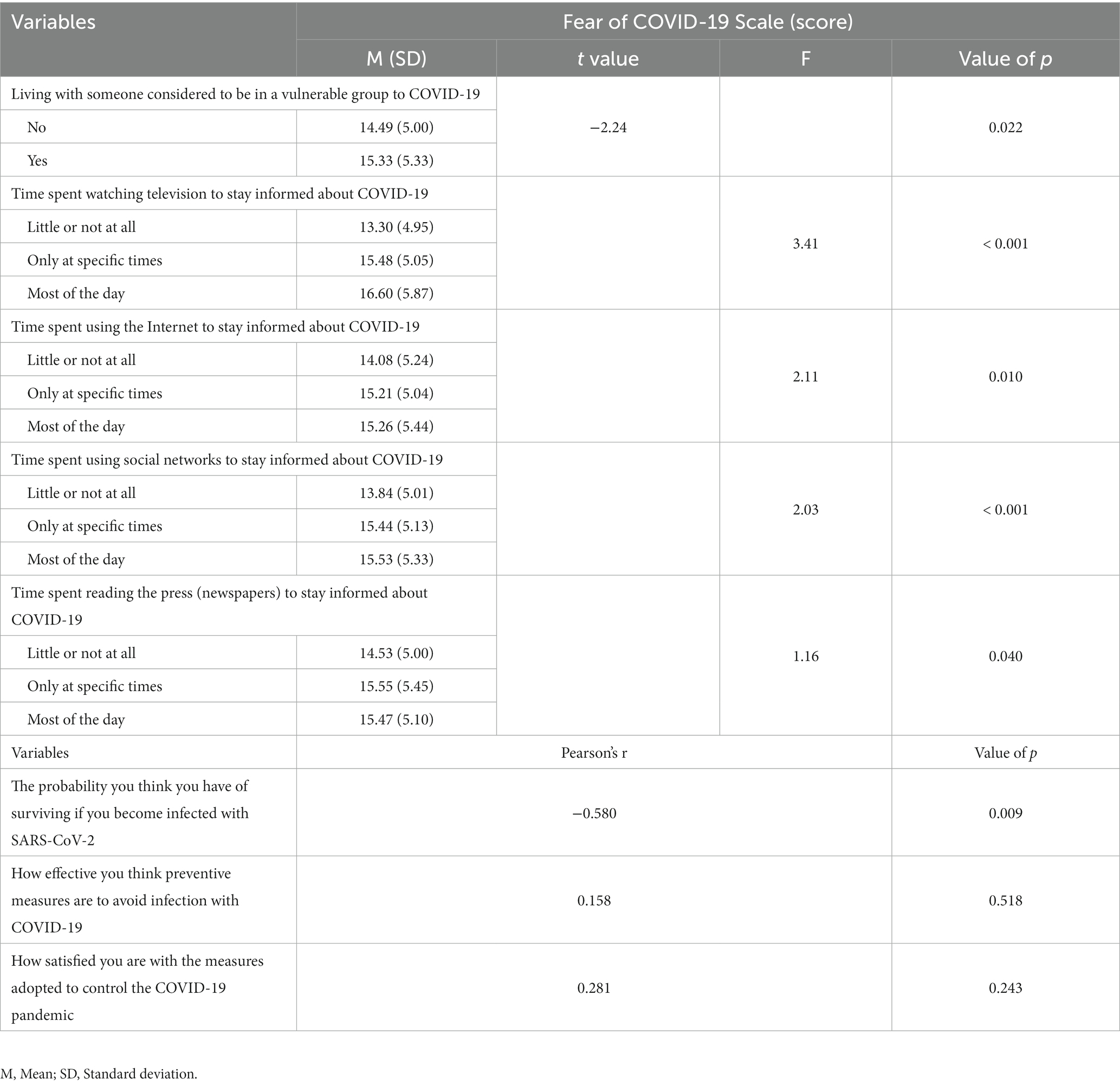
Table 4. Comparative analysis of participants’ fear of COVID-19 Scale scores and variables related to COVID-19 in Spanish university students (n = 950).
3.6. Multivariate linear regression model between fear of COVID-19 and independent variables in Spanish university students
The results of the multiple linear regression analyzes are shown in Tables 5, 6 (Adjusted R2 = 0.35). Fear of COVID-19 was determined by gender (t = 3.54, p < 0.001), religious beliefs (t = 2.00, p = 0.04), population of town/city (t = −3.33, t = −3.41, p < 0.01), living with someone considered to belong to a group vulnerable to COVID-19 (t = 2.26, p = 0.02), watching TV only at specific times (t = 5.38, p < 0.001) or most of the day (t = 3.27, p < 0.01) to stay informed about COVID-19, perceived probability of surviving a COVID-19 infection (t = −7.62, p < 0.001; Table 5), level of death anxiety (t = 14.88, p < 0.001) and level of insomnia (t = 4.43, p < 0.001; Table 6).
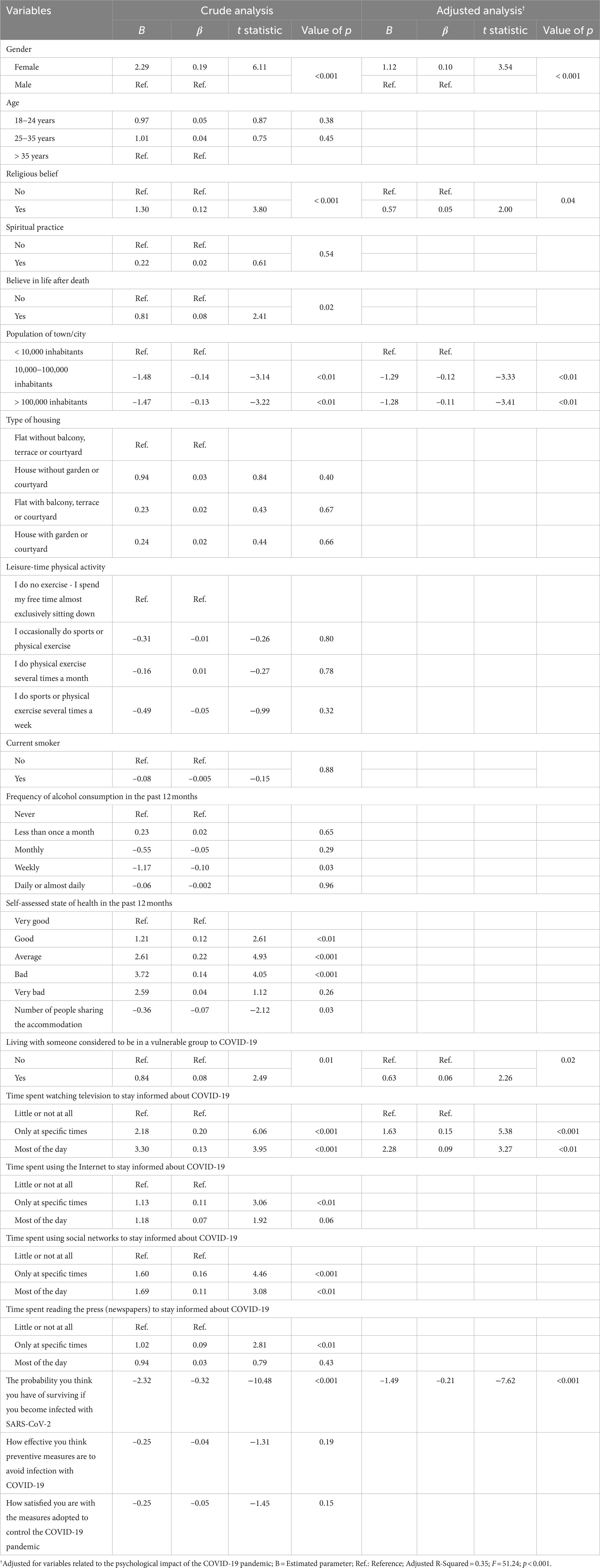
Table 5. Multivariate linear regression model between fear of COVID-19 scores and socio-demographic, health-related determinants and variables related to COVID-19 (n = 950).
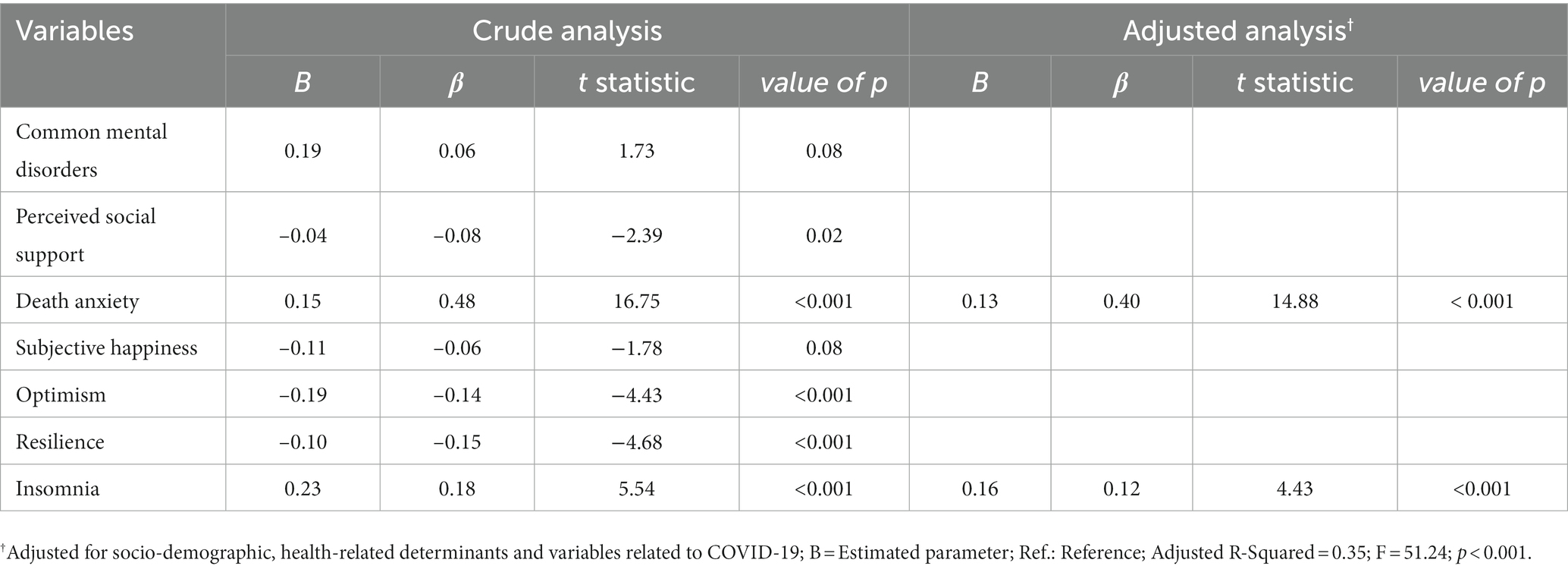
Table 6. Multivariate linear regression model between fear of COVID-19 scores and variables related to the psychological impact of the COVID-19 pandemic of Spanish university students (n = 950).
4. Discussion
4.1. Main findings
The present study presents a multidisciplinary approach to examine the relationship between fear of COVID-19 and multiple factors that may influence the psychological impact of the COVID-19 pandemic on Spanish university students. Overall, the study found that the average fear of COVID-19 score was 14.86 ± 5.16 points. Several factors were identified as predictors of fear of COVID-19, including being female, holding religious beliefs, residing in towns/cities with over 10,000 inhabitants, living with someone vulnerable to COVID-19, and watching TV to stay informed about COVID-19 either at specific times or for most of the day. Additionally, the higher the participants’ perceived probability of surviving a COVID-19 infection, the lower their fear of COVID-19 score. However, the fear of COVID-19 score increased with every one-point increase in the level of death anxiety and insomnia.
According to our results, the level of fear of COVID-19 among Spanish university students was found to be lower than that reported in other studies conducted in the same context in Spain (25, 70, 71). In contrast, other countries have reported higher average scores of fear of COVID-19, including China (27), Pakistan (28), Russia and Belarus (29) and Turkey (26). Spain was one of the countries in the world most affected by the first wave of the COVID-19 pandemic (72–74). The measures implemented by the Spanish government, autonomous communities and Spanish universities to ensure the safety and well-being of students during the COVID-19 pandemic (75, 76) may have contributed to reducing fear of COVID-19 in this population group. In fact, our study also found that the majority of participants reported engaging in preventive practices such as wearing masks, covering their mouth and nose with their elbow when coughing or sneezing, and always prioritizing outdoor spaces when going outside. In that context, measures such as limiting face-to-face attendance at universities (77), promoting online classes (78), and implementing health safety protocols (79) may have contributed to creating a sense of safety and confidence among students (80).
Fear of COVID-19 may have affected women and men differently (81), with women having a higher perceived risk of infection (82). Various studies have shown that women experienced higher levels of stress, anxiety, and depression related to the COVID-19 pandemic compared to men (83–85). It is also important to note that women often take on caregiving roles (86, 87) and work as front-line health-care workers (88), which put them at greater risk and vulnerability during COVID-19 pandemic (89).
One of the best-known coping strategies to deal with the negative effects that the COVID-19 pandemic had on the mental health of the population was having religious beliefs, attitudes, or practices (90–94). Nevertheless, our study participants who believed in a religion showed a higher score for fear of COVID-19, in line with other studies (95–97). According to Krok et al. (98), the fear of COVID-19 also intensified the effect of religiosity on meaning-making, leading individuals to seek religious activities for emotional support and coping strategies.
According to our results, university students who lived in a town/city with over 10,000 inhabitants had higher fear of COVID-19 scores, in agreement with other studies (99, 100). This may be because people living in urban areas may be more exposed to the virus due to the higher population density and more frequent social interactions (101).
We also found that university students who lived with someone considered to be in a high-risk group for COVID-19 experienced a significantly greater fear of COVID-19, in line with other studies (102, 103). It is likely that people experienced higher levels of anxiety due to the fear of infecting their sick relatives as well as from the fear of contracting SARS-CoV-2 coronavirus themselves (104). Watching TV to stay informed about COVID-19 was identified as another factor that contributed to the greater fear of COVID-19 among study participants. This finding is consistent with the idea that the coverage of COVID-19 in the mainstream media focused predominantly on negative issues (105), disseminating uncertainties about the virus, the global spread of the pandemic (106), the increasing number of cases and fatalities (107), government policies (108), and the rising demand for healthcare (109), all of which had psychological implications.
Finally, university students reported feeling less fear of COVID-19 if they believed they could survive the disease, whether they were already infected or might become infected in the future, in agreement with Tusey et al. (110). In fact, participants in the study by Mousavi et al. (111), who believed they had a low probability of surviving if infected with COVID-19 were more likely to practice preventive behavior. Considering that a significant majority of the participants in the present study were under 25 years of age, this is likely to be due to the scientific literature reporting high SARS-CoV-2 transmissibility but relatively low mortality rates in this age range (112–114). Nevertheless, survivors who had COVID-19 perceived the disease as a factor affecting their existence and reported having a fear of death (115–118). In fact, it is not surprising that death anxiety arises when individuals face the threat of death due to either experiencing or fearing COVID-19 (119). In this case, the effective utilization of mindfulness and coping strategies can assist individuals in managing stressful situations, decreasing negative emotions (120) and improving sleep quality (121). Fear plays a determinant factor in modifying normal sleep patterns (122, 123), and so the connection between the fear of COVID-19 and sleep problems could be linked to concerns about the contagious nature of the disease (124), as supported by other studies (125, 126). Nevertheless, when Cerqueira et al. (127) asked university students about the quality of their sleep in the COVID-19 pandemic, 55.7% described it as either ‘very good’ or ‘good in general’. In addition, Wright et al. (128) reported that during the lockdown period, time in bed increased by around 30 min on weekdays and 24 min at weekends, sleep timing regularity improved by approximately 12 min, and university students extended the duration of their sleep by about 50 min on weekdays and approximately 25 min at weekends, thereby reducing social jetlag. Leone et al. (129) attributed the improvement in weekday sleep duration and the reduction in social jetlag to a plausible explanation based on lifestyle changes associated with weaker social cues, such as work and class schedules becoming more flexible, delayed, or even absent. t.
4.2. Strengths and limitations
One of the major strengths of this study was its multidisciplinary approach, which explored the relationship between fear of COVID-19 and various factors that may have affected the psychological impact of the pandemic on Spanish university students, using a considerable number of validated questionnaires. Nevertheless, the study has several limitations. Firstly, its cross-sectional design means that no causal relationships can be established. Secondly, the study was conducted from December 2020 to December 2021, and therefore further research is needed to investigate how levels of fear of COVID-19 may have changed over time. Thirdly, the use of questionnaires as a data collection method is subject to the participants’ truthfulness in responding. For example, using self-report measures may not reflect people’s real opinions and feelings due to the demands of social desirability (130). Lastly, the study’s non-probabilistic convenience sample of university students from the southern region of Spain limits the generalizability of its findings.
4.3. Implications for research and practice
This study highlights the significance of fear of COVID-19 and its impact on the mental health of university students. Previous research has demonstrated that a significant proportion of Spanish university students suffer from mental health disorders (131), and that the COVID-19 pandemic exacerbated negative mental health outcomes (132). These findings can help to identify specific factors that contribute to the fear of COVID-19 and enable us to develop coping strategies to alleviate the stress caused by the pandemic. They may also help policymakers and health professionals in devising suitable strategies to address the pandemic’s long-term effects on mental health, for example, by emphasizing the need to enable universities to make decisions regarding changes to the curriculum and assessment methods that align with students’ well-being and mental health expectations (133). This could include flexible academic schedules, reduced workloads during future pandemics, and the option of distance-learning to accommodate students’ needs during a pandemic (134). Furthermore, the study suggests that universities may be an ideal environment for implementing health promotion programs focusing on mental health and well-being (135), as they allow students to develop coping skills and better understand how to manage fear during a pandemic.
5. Conclusion
A score of 14.86 ± 5.16 points was identified as the average level of fear of COVID-19 among university students in Spain. The main predictors of fear of COVID-19 are being female, having religious beliefs, living in towns/cities with over 10,000 inhabitants, living with someone vulnerable to COVID-19, watching TV to stay informed about COVID-19, believing in a low probability of survival if infected with COVID-19, and having a higher level of death anxiety and insomnia. The findings of this study, which identify numerous factors related to fear of COVID-19, can aid policymakers and health professionals in developing appropriate strategies to address the pandemic’s long-term effects on mental health. In addition, these findings can facilitate future research on coping strategies for university students facing the stress caused by a pandemic.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical Committee for Clinical Research of Cordoba (Spain) (approval number 316, reference 4845). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JC: conceptualization, methodology, and writing–original draft. JC and SP: data curation, data analysis, resources, visualization, project administration, methodology, and writing–reviewing and editing. SP: supervision. All authors contributed to the article and approved the submitted version.
Acknowledgments
Our gratitude goes to all the students who participated in the current study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhu, N, Zhang, D, Wang, W, Li, X, Yang, B, Song, J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/nejmoa2001017
2. World Health Organization. Coronavirus disease (COVID-19) pandemic. Geneva: World Health Organization. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (Accessed September 1, 2023).
3. Agencia Estatal Boletín Oficial del Estado. (2020). Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. Available at: https://www.boe.es/buscar/doc.php?id=BOE-A-2020-3692 (Accessed September 1, 2023).
4. World Health Organization. Coronavirus disease 2019 (COVID-19) situation report–153. (2023). Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200621-covid-19-sitrep-153.pdf?sfvrsn=c896464d_2 (Accessed September 1, 2023).
5. Jiménez-Pavón, D, Carbonell-Baeza, A, and Lavie, CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Dis. (2020) 63:386–8. doi: 10.1016/j.pcad.2020.03.009
6. Saraf, A, Sathe, H, Mishra, K, and John, S. A cross-sectional study of psychological distress and fear of COVID-19 in the general population of India during lockdown. Ann Ind Psychiatr. (2020) 4:181. doi: 10.4103/aip.aip_54_20
7. Chen, P, Mao, L, Nassis, GP, Harmer, P, Ainsworth, BE, and Li, F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. (2020) 9:103–4. doi: 10.1016/j.jshs.2020.02.001
8. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, Ho, CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
9. Planchuelo, Á, Odriozola, P, Irurtia, MJ, and de Luis, R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J Affect Disord. (2020) 277:842–9. doi: 10.1016/j.jad.2020.09.018
10. Odriozola, P, Planchuelo, Á, Irurtia, MJ, and De Luis, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. (2020) 290:113108. doi: 10.1016/j.psychres.2020.113108
11. Gullone, E. The development of normal fear. Clin Psychol Rev. (2000) 20:429–51. doi: 10.1016/s0272-7358(99)00034-3
12. Ahorsu, DK, Lin, C-Y, and Pakpour, AH. The association between health status and insomnia, mental health, and preventive behaviors: the mediating role of fear of COVID-19. Gerontol Geriatr Med. (2020) 6:233372142096608. doi: 10.1177/2333721420966081
13. Tzur Bitan, D, Grossman-Giron, A, Bloch, Y, Mayer, Y, Shiffman, N, and Mendlovic, S. Fear of COVID-19 scale: psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. (2020) 289:113100. doi: 10.1016/j.psychres.2020.113100
14. Coelho, CM, Suttiwan, P, Arato, N, and Zsido, AN. On the nature of fear and anxiety triggered by COVID-19. Front Psychol. (2020) 11:581314. doi: 10.3389/fpsyg.2020.581314
15. Satici, B, Gocet-Tekin, E, Deniz, ME, and Satici, SA. Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addict. (2021) 19:1980–8. doi: 10.1007/s11469-020-00294-0
16. Smith, BM, Twohy, AJ, and Smith, GS. Psychological inflexibility and intolerance of uncertainty moderate the relationship between social isolation and mental health outcomes during COVID-19. J Contextual Behav Sci. (2020) 18:162–74. doi: 10.1016/j.jcbs.2020.09.005
17. Mahmud, MS, Talukder, MU, and Rahman, SM. Does ‘fear of COVID-19’ trigger future career anxiety? An empirical investigation considering depression from COVID-19 as a mediator. Int J Soc Psychiatry. (2021) 67:35–45. doi: 10.1177/0020764020935488
18. Barello, S, Palamenghi, L, and Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. (2020) 290:113129. doi: 10.1016/j.psychres.2020.113129
19. Dubey, S, Biswas, P, Ghosh, R, Chatterjee, S, Dubey, MJ, Chatterjee, S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. (2020) 14:779–88. doi: 10.1016/j.dsx.2020.05.035
20. Garnier-Crussard, A, Forestier, E, Gilbert, T, and Krolak-Salmon, P. Novel coronavirus (COVID-19) epidemic: what are the risks for older patients? J Am Geriatr Soc. (2020) 68:939–40. doi: 10.1111/jgs.16407
21. Li, S, Wang, Y, Xue, J, Zhao, N, and Zhu, T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health. (2020) 17:2032. doi: 10.3390/ijerph17062032
22. Lima, CKT, Carvalho, PMM, Lima, IAAS, Nunes, JVAO, Saraiva, JS, de Souza, RI, et al. The emotional impact of coronavirus 2019-nCoV (new coronavirus disease). Psychiatry Res. (2020) 287:112915. doi: 10.1016/j.psychres.2020.112915
23. Son, C, Hegde, S, Smith, A, Wang, X, and Sasangohar, F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. (2020) 22:e21279. doi: 10.2196/21279
24. Nania, T, Dellafiore, F, Caruso, R, and Barello, S. Risk and protective factors for psychological distress among Italian university students during the COVID-19 pandemic: the beneficial role of health engagement. Int J Soc Psychiatry. (2021) 67:102–3. doi: 10.1177/0020764020945729
25. Muyor, J, Caravaca, F, and Fernández, JS. COVID-19 fear, resilience, social support, anxiety, and suicide among college students in Spain. Int J Environ Res Public Health. (2021) 18:8156. doi: 10.3390/ijerph18158156
26. Yeni Elbay, R, Yılmaz, H, Çifteci, K, and Karadere, E. The psychological effects of COVID 19 on medical and non-medical university students. Psychiatr Danub. (2021) 33:126–31.
27. Yang, W, Li, P, Huang, Y, Yang, X, Mu, W, Jing, W, et al. Cross-cultural adaptation and validation of the fear of COVID-19 scale for Chinese university students: a cross-sectional study. Int J Environ Res Public Health. (2022) 19:8624. doi: 10.3390/ijerph19148624
28. Green, ZA, Noor, U, Ahmed, F, and Himayat, L. Validation of the fear of COVID-19 scale in a sample of Pakistan’s university students and future directions. Psychol Rep. (2022) 125:2709–32. doi: 10.1177/00332941211016754
29. Reznik, A, Gritsenko, V, Konstantinov, V, Khamenka, N, and Isralowitz, R. COVID-19 fear in eastern Europe: validation of the fear of COVID-19 scale. Int J Ment Health Addict. (2021) 19:1903–8. doi: 10.1007/s11469-020-00283-3
30. Ahorsu, DK, Lin, C-Y, Imani, V, Saffari, M, Griffiths, MD, and Pakpour, AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. (2022) 20:1537–45. doi: 10.1007/s11469-020-00270-8
31. Sakib, N, Bhuiyan, AKMI, Hossain, S, Al Mamun, F, Hosen, I, Abdullah, AH, et al. Psychometric validation of the Bangla fear of COVID-19 scale: confirmatory factor analysis and Rasch analysis. Int J Ment Health Addict. (2022) 20:2623–34. doi: 10.1007/s11469-020-00289-x
32. Fang, H, Tu, S, Sheng, J, and Shao, A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. (2019) 23:2324–32. doi: 10.1111/jcmm.14170
33. Ahmed, MZ, Ahmed, O, Aibao, Z, Hanbin, S, Siyu, L, and Ahmad, A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr. (2020) 51:102092. doi: 10.1016/j.ajp.2020.102092
34. Redeker, NS, Conley, S, Anderson, G, Cline, J, Andrews, L, Mohsenin, V, et al. Effects of cognitive behavioral therapy for insomnia on sleep, symptoms, stress, and autonomic function among patients with heart failure. Behav Sleep Med. (2020) 18:190–202. doi: 10.1080/15402002.2018.1546709
35. Rubin, GJ, and Wessely, S. The psychological effects of quarantining a city. BMJ. (2020) 368:m313. doi: 10.1136/bmj.m313
36. Siddique, RF, Ahmed, O, and Hossain, KN. Relationship between the fear of COVID-19 disease and sleep quality: the mediating role of stress. Heliyon. (2021) 7:e07033. doi: 10.1016/j.heliyon.2021.e07033
37. Han, B, Ma, C, Liu, Z, Jiang, R, Zhang, T, Wang, Y, et al. Perceived psychological feelings make important contributions to the symptoms of common mental disorders of medical staff during the COVID-19. Front Psych. (2022) 12:8610. doi: 10.3389/fpsyt.2021.738610
38. Menzies, RE, and Menzies, RG. Death anxiety in the time of COVID-19: theoretical explanations and clinical implications. Cogn Behav Therap. (2020) 13:e19. doi: 10.1017/s1754470x20000215
39. Menzies, RE, Neimeyer, RA, and Menzies, RG. Death anxiety, loss, and grief in the time of COVID-19. Behav Change. (2020) 37:111–5. doi: 10.1017/bec.2020.10
40. Alnazly, E, Khraisat, OM, Al-Bashaireh, AM, and Bryant, CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. (2021) 16:e0247679. doi: 10.1371/journal.pone.0247679
41. Alves, MP, Costa, V, Cunha, AI, Carvalho, P, and Loureiro, MJ. Optimism and fear of COVID-19 in higher education students: the mediating role of general anxiety. Psychol Health Med. (2023) 28:241–52. doi: 10.1080/13548506.2022.2073376
42. Satici, SA, Kayis, AR, Satici, B, Griffiths, MD, and Can, G. Resilience, hope, and subjective happiness among the Turkish population: fear of COVID-19 as a mediator. Int J Ment Health Addict. (2023) 21:803–18. doi: 10.1007/s11469-020-00443-5
43. Gritsenko, V, Skugarevsky, O, Konstantinov, V, Khamenka, N, Marinova, T, Reznik, A, et al. COVID 19 fear, stress, anxiety, and substance use among Russian and Belarusian university students. Int J Ment Health Addict. (2021) 19:2362–8. doi: 10.1007/s11469-020-00330-z
44. Grande, M, and Doyle-Baker, P. Fear of COVID-19 effects on university student’s health behaviours: the FRESH study. Int J Kinesiol Sports Sci. (2021) 9:52. doi: 10.7575/aiac.ijkss.v.9n.3p52
45. Cardoso, JPP, Afonso, MVR, Mendes, BF, Vieira, ER, Pereira, WF, Dias-Peixoto, MF, et al. Fear of COVID-19 influences physical activity practice: a study in a Brazilian sample. Psychol Health Med. (2023) 28:232–40. doi: 10.1080/13548506.2022.2072916
46. Basseal, JM, Bennett, CM, Collignon, P, Currie, BJ, Durrheim, DN, Leask, J, et al. Key lessons from the COVID-19 public health response in Australia. Lancet Reg Health West Pac. (2023) 30:100616. doi: 10.1016/j.lanwpc.2022.100616
47. Yeboah, H, and Yaya, S. Health and economic implications of the ongoing coronavirus disease (COVID-19) pandemic on women and children in Africa. Reprod Health. (2023) 20:70. doi: 10.1186/s12978-023-01616-w
48. Mauz, E, Walther, L, Junker, S, Kersjes, C, Damerow, S, Eicher, S, et al. Time trends in mental health indicators in Germany’s adult population before and during the COVID-19 pandemic. Front Public Health. (2023) 11:1065938. doi: 10.3389/fpubh.2023.1065938
49. Kohls, E, Guenthner, L, Baldofski, S, Brock, T, Schuhr, J, and Rummel-Kluge, C. Two years COVID-19 pandemic: development of university students’ mental health 2020–2022. Front Psych. (2023) 14:1122256. doi: 10.3389/fpsyt.2023.1122256
50. Martínez-Lorca, M, Martínez-Lorca, A, Criado-Álvarez, JJ, Armesilla, MDC, and Latorre, JM. The fear of COVID-19 scale: validation in spanish university students. Psychiatry Res. (2020) 293:113350. doi: 10.1016/j.psychres.2020.113350
51. Abundis-Espinosa, VM. Beneficios de las encuestas electrónicas como apoyo para la investigación. Tlatemoani. (2016) 7:168–86.
52. Parrado, A, and León, J. COVID-19: Factores asociados al malestar emocional y morbilidad psíquica en población española. Rev Esp Salud Pública. (2020) 4:e1–e16.
53. Goldberg, DP, and Hillier, VF. A scaled version of the general health questionnaire. Psychol Med. (1979) 9:139–45. doi: 10.1017/s0033291700021644
54. Goldberg, DP, and Williams, P. Cuestionario de Salud General GHQ (General Health Questionnaire): Guía para el usuario de las distintas versiones. Barcelona: Masson (1996). 163 p.
55. Sánchez-López, MP, and Dresch, V. The 12-item general health questionnaire (GHQ-12): reliability, external validity and factor structure in the Spanish population. Psicothema. (2008) 20:839–43.
56. Goldberg, DP, Gater, R, Sartorius, N, Ustun, TB, Piccinelli, M, Gureje, O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. (1997) 27:191–7. doi: 10.1017/s0033291796004242
57. Broadhead, WE, Gehlbach, SH, De Gruy, FV, and Kaplan, BH. The Duke-UNC functional social support questionnaire: measurement of social support in family medicine patients. Med Care. (1988) 26:709–23. doi: 10.1097/00005650-198807000-00006
58. Bellón, JA, Delgado, A, Luna del Castillo, JD, and Lardelli, P. Validez y fiabilidad del cuestionario de apoyo social funcional Duke-UNC-11. Aten Primaria. (1996) 18:153–63.
59. Tomás-Sábado, J, and Gómez-Benito, J. Construction and validation of the death anxiety inventory (DAI). Eur J Psychol Assess. (2005) 21:108–14. doi: 10.1027/1015-5759.21.2.108
60. Lyubomirsky, S, and Lepper, HS. A measure of subjective happiness: preliminary reliability and construct validation. Soc Indic Res. (1999) 46:137–55. doi: 10.1023/a:1006824100041
61. Extremera, N, and Fernández-Berrocal, P. The subjective happiness scale: translation and preliminary psychometric evaluation of a Spanish version. Soc Indic Res. (2014) 119:473–81. doi: 10.1007/s11205-013-0497-2
62. Scheier, MF, Carver, CS, and Bridges, MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol. (1994) 67:1063–78. doi: 10.1037/0022-3514.67.6.1063
63. Glaesmer, H, Rief, W, Martin, A, Mewes, R, Brähler, E, Zenger, M, et al. Psychometric properties and population-based norms of the life orientation test revised (LOT-R): psychometric properties of the LOT-R. Br J Health Psychol. (2012) 17:432–45. doi: 10.1111/j.2044-8287.2011.02046.x
64. Ferrando, PJ, Chico, E, and Tous, JM. Propiedades psicométricas del test de optimismo Life Orientation Test. Psicothema. (2002) 14:673–80.
65. Cano, FJ, Sanduvete, S, Chacón, S, Rodríguez, L, García, J, Antuña, MA, et al. Factor structure of the Spanish version of the life orientation test-revised (LOT-R): testing several models. Int J Clin Health Psychol. (2015) 15:139–48. doi: 10.1016/j.ijchp.2015.01.003
66. Campbell, L, and Stein, MB. Psychometric analysis and refinement of the Connor-davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. (2007) 20:1019–28. doi: 10.1002/jts.20271
67. Notario, B, Solera, M, Serrano, MD, Bartolomé, R, García, J, and Martínez, V. Reliability and validity of the Spanish version of the 10-item Connor-Davidson resilience scale (10-item CD-RISC) in young adults. Health Qual Life Outcomes. (2011) 9:63. doi: 10.1186/1477-7525-9-63
68. Soldatos, CR, Dikeos, DG, and Paparrigopoulos, TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. (2000) 48:555–60. doi: 10.1016/s0022-3999(00)00095-7
69. Gómez-Benito, J, Ruiz, C, and Guilera, G. A Spanish version of the Athens insomnia scale. Qual Life Res. (2011) 20:931–7. doi: 10.1007/s11136-010-9827-x
70. Morales-Rodríguez, FM. Fear, stress, resilience and coping strategies during COVID-19 in Spanish university students. Sustainability. (2021) 13:5824. doi: 10.3390/su13115824
71. Cantero, PA, Rodríguez, M, Moraleda, E, Polonio, B, and Marcos, F. Analysis of fear post COVID in first-year students after the incorporation to the classroom: descriptive study in university students of health sciences. Healthcare (Basel). (2021) 9:1621. doi: 10.3390/healthcare9121621
72. Khafaie, MA, and Rahim, F. Cross-country comparison of case fatality rates of COVID-19/SARS-COV-2. Osong Public Health Res Perspect. (2020) 11:74–80. doi: 10.24171/j.phrp.2020.11.2.03
73. Verelst, F, Kuylen, E, and Beutels, P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, march 2020. Euro Surveill. (2020) 25:2000323. doi: 10.2807/1560-7917.ES.2020.25.13.2000323
74. Rodríguez, M, Rivas, L, Quiles, JL, Redondo, D, Aranda, P, Llopis, J, et al. The spread of SARS-CoV-2 in Spain: hygiene habits, sociodemographic profile, mobility patterns and comorbidities. Environ Res. (2021) 192:110223. doi: 10.1016/j.envres.2020.110223
75. Legido, H, Mateos, JT, Campos, VR, Gea, M, Muntaner, C, and McKee, M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. (2020) 5:e251–2. doi: 10.1016/S2468-2667(20)30060-8
76. Government of Spain. Royal decree, of march 14, declaring the state of alarm for the management of the health crisis situation caused by COVID-19. Madrid: Spain (2020).
77. Díaz, RM, Caravaca, F, Martín, MC, and De la Fuente, YM. Anxiety levels among social work students during the COVID-19 lockdown in Spain. Soc Work Health Care. (2020) 59:681–93. doi: 10.1080/00981389.2020.1859044
78. Verde, A, and Valero, JM. Teaching and learning modalities in higher education during the pandemic: responses to coronavirus disease 2019 from Spain. Front Psychol. (2021) 12:648592. doi: 10.3389/fpsyg.2021.648592
79. Aguilar, AJ, de la Hoz, ML, Oltra, L, Ruiz, DP, and Martínez, MD. Impact of COVID-19 protocols on IEQ and students’ perception within educational buildings in southern Spain. Build Res Inf. (2022) 50:755–70. doi: 10.1080/09613218.2022.2082356
80. Tuells, J, Egoavil, CM, Pena, MA, Montagud, AC, Montagud, E, Caballero, P, et al. Seroprevalence study and cross-sectional survey on COVID-19 for a plan to reopen the university of Alicante (Spain). Int J Environ Res Public Health. (2021) 18:1908. doi: 10.3390/ijerph18041908
81. Abdelghani, M, Hassan, MS, Elgohary, HM, and Fouad, E. Exploring the factors associated with coronaphobia among physicians during the COVID-19 outbreak in Egypt. Egypt J Neurol Psychiatr Neurosurg. (2021) 57:105. doi: 10.1186/s41983-021-00357-6
82. Ding, Y, Du, X, Li, Q, Zhang, M, Zhang, Q, Tan, X, et al. Risk perception of coronavirus disease 2019 (COVID-19) and its related factors among college students in China during quarantine. PLoS One. (2020) 15:e0237626. doi: 10.1371/journal.pone.0237626
83. Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. (2020) 51:102076. doi: 10.1016/j.ajp.2020.102076
84. Zhou, SJ, Zhang, LG, Wang, LL, Guo, ZC, Wang, JQ, Chen, JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. (2020) 29:749–58. doi: 10.1007/s00787-020-01541-4
85. Wang, Y, Di, Y, Ye, J, and Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. (2021) 26:13–22. doi: 10.1080/13548506.2020.1746817
86. Bauer, JM, and Sousa-Poza, A. Impacts of informal caregiving on caregiver employment, health, and family. J Popul Ageing. (2015) 8:113–45. doi: 10.1007/s12062-015-9116-0
87. Cohen, SA, Sabik, NJ, Cook, SK, Azzoli, AB, and Mendez-Luck, CA. Differences within differences: gender inequalities in caregiving intensity vary by race and ethnicity in informal caregivers. J Cross Cult Gerontol. (2019) 34:245–63. doi: 10.1007/s10823-019-09381-9
88. Boniol, M, McIsaac, M, Xu, L, Wulijiç, T, Diallo, K, and Campbell, J. Gender equity in the health workforce: Analysis of 104 countries. Geneva: World Health Organization (2019).
89. Almeida, M, Shrestha, AD, Stojanac, D, and Miller, LJ. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. (2020) 23:741–8. doi: 10.1007/s00737-020-01092-2
90. Koenig, HG. Spirituality in patient care: Why, how, when, and what. Radnor: Templeton Foundation Press (2007). 264 p.
91. Ano, GG, and Vasconcelles, EB. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. (2005) 61:461–80. doi: 10.1002/jclp.20049
92. Lucchetti, G, Góes, LG, Amaral, SG, Ganadjian, GT, Andrade, I, Almeida, PO, et al. Spirituality, religiosity and the mental health consequences of social isolation during Covid-19 pandemic. Int J Soc Psychiatry. (2021) 67:672–9. doi: 10.1177/0020764020970996
93. Pirutinsky, S, Cherniak, AD, and Rosmarin, DH. COVID-19, mental health, and religious coping among American orthodox Jews. J Relig Health. (2020) 59:2288–301. doi: 10.1007/s10943-020-01070-z
94. Yıldırım, M, Arslan, G, and Alkahtani, AM. Do fear of COVID-19 and religious coping predict depression, anxiety, and stress among the Arab population during health crisis? Death Stud. (2022) 46:2070–6. doi: 10.1080/07481187.2021.1882617
95. Jaspal, R, Lopes, B, and Lopes, P. Fear, social isolation and compulsive buying in response to COVID-19 in a religiously diverse UK sample. Ment Health Relig Cult. (2020) 23:427–42. doi: 10.1080/13674676.2020.1784119
96. Prazeres, F, Passos, L, Simões, JA, Simões, P, Martins, C, and Teixeira, A. COVID-19-related fear and anxiety: spiritual-religious coping in healthcare workers in Portugal. Int J Environ Res Public Health. (2020) 18:220. doi: 10.3390/ijerph18010220
97. Rajkumar, RP. The relationship between pre-pandemic measures of religiosity and psychological responses to the COVID-19 pandemic: a secondary analysis of data from a multi-country study. Cureus. (2021) 13:e20013. doi: 10.7759/cureus.20013
98. Krok, D, Zarzycka, B, and Telka, E. Religiosity, meaning-making and the fear of COVID-19 affecting well-being among late adolescents in Poland: a moderated mediation model. J Relig Health. (2021) 60:3265–81. doi: 10.1007/s10943-021-01375-7
99. Nair, D, Rajmohan, V, and Tm, R. Impact of COVID-19 lockdown on lifestyle and psychosocial stress - an online survey. Kerala J Psychiatry. (2020) 33:194. doi: 10.30834/kjp.33.1.2020.194
100. Gaur, G, Sharma, M, Kundu, M, Sekhon, H, and Chauhan, N. Fear of COVID-19 among the Indian youth: a cross-sectional study. J Educ Health Promot. (2021) 10:340. doi: 10.4103/jehp.jehp_1455_20
101. Ganasegeran, K, Jamil, MFA, Ch’ng, ASH, Looi, I, and Peariasamy, KM. Influence of population density for COVID-19 spread in Malaysia: an ecological study. Int J Environ Res Public Health. (2021) 18:9866. doi: 10.3390/ijerph18189866
102. Mertens, G, Gerritsen, L, Duijndam, S, Salemink, E, and Engelhard, IM. Fear of the coronavirus (COVID-19): predictors in an online study conducted in march 2020. J Anxiety Disord. (2020) 74:102258. doi: 10.1016/j.janxdis.2020.102258
103. Cerda, AA, and García, LY. Factors explaining the fear of being infected with COVID-19. Health Expect. (2022) 25:506–12. doi: 10.1111/hex.13274
104. Baldi, E, and Savastano, S. Fear of contagion: one of the most devious enemies to fight during the COVID-19 pandemic. Disaster Med Public Health Prep. (2021) 15:e8–9. doi: 10.1017/dmp.2020.338
105. Cowper, A. Covid-19: are we getting the communications right? BMJ. (2020) 368:m919. doi: 10.1136/bmj.m919
106. Wang, Y, Wang, Y, Chen, Y, and Qin, Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. (2020) 92:568–76. doi: 10.1002/jmv.25748
107. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) in the United States. (2020). Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html (Accessed April 28, 2023).
108. Lazzerini, M, and Putoto, G. COVID-19 in Italy: momentous decisions and many uncertainties. Lancet Glob Health. (2020) 8:e641–2. doi: 10.1016/S2214-109X(20)30110-8
109. Rosenbaum, L. Facing covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. (2020) 382:1873–5. doi: 10.1056/NEJMp2005492
110. Tusev, A, Tonon, L, and Capella, M. The initial mental health effects of the covid-19 pandemic across some Ecuadorian provinces. Investigatio. (2020) 15:11–24. doi: 10.31095/investigatio.2020.15.2
111. Mousavi, SH, Delshad, MH, Acuti, C, Bhandari, D, Ozaki, A, Pourhaji, F, et al. Community behavioral and perceived responses in the COVID-19 outbreak in Afghanistan: a cross-sectional study. Disaster Med Public Health Prep. (2021) 16:1–7. doi: 10.1017/dmp.2021.135
112. Acuti, C, Flacco, ME, Cappadona, R, Bravi, F, Mantovani, L, and Manzoli, L. SARS-CoV-2 pandemic: an overview. Adv Biol Regul. (2020) 77:100736. doi: 10.1016/j.jbior.2020.100736
113. Tran, HTT, Nguyen, MH, Pham, TTM, Kim, GB, Nguyen, HT, Nguyen, N-M, et al. Predictors of eHealth literacy and its associations with preventive behaviors, fear of COVID-19, anxiety, and depression among undergraduate nursing students: a cross-sectional survey. Int J Environ Res Public Health. (2022) 19:3766. doi: 10.3390/ijerph19073766
114. Perez-Saez, J, Lauer, SA, Kaiser, L, Regard, S, Delaporte, E, Guessous, I, et al. Serology-informed estimates of SARS-CoV-2 infection fatality risk in Geneva, Switzerland. Lancet Infect Dis. (2021) 21:e69–70. doi: 10.1016/S1473-3099(20)30584-3
115. Aliakbari, M, Eisazadeh, F, and Aghajanbigloo, S. Psychological consequences of patients with coronavirus (COVID- 19): a qualitative study. Iran J Health Psychol. (2019) 2:9–20. doi: 10.30473/ijohp.2020.52395.1074
116. Sun, N, Wei, L, Shi, S, Jiao, D, Song, R, Ma, L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. (2020) 48:592–8. doi: 10.1016/j.ajic.2020.03.018
117. Son, H-M, Choi, W-H, Hwang, Y-H, and Yang, H-R. The lived experiences of COVID-19 patients in South Korea: a qualitative study. Int J Environ Res Public Health. (2021) 18:7419. doi: 10.3390/ijerph18147419
118. Muslu, L, Kolutek, R, and Fidan, G. Experiences of COVID-19 survivors: a qualitative study based on Watson’s theory of human caring. Nurs Health Sci. (2022) 24:774–84. doi: 10.1111/nhs.12979
119. Özgüç, S, Kaplan Serin, E, and Tanriverdi, D. Death anxiety associated with coronavirus (COVID-19) disease: a systematic review and meta-analysis. Omega (Westport). (2021) 8:503. doi: 10.1177/00302228211050503
120. Sadri Damirchi, E, Mojarrad, A, Pireinaladin, S, and Grjibovski, AM. The role of self-talk in predicting death anxiety, obsessive-compulsive disorder, and coping strategies in the face of coronavirus disease (COVID-19). Iran J Psychiatry. (2020) 15:182–8. doi: 10.18502/ijps.v15i3.3810
121. Zhao, Y, Liu, J-E, Lewis, FM, Nie, Z-H, Qiu, H, Han, J, et al. Effects of mindfulness-based cognitive therapy on breast cancer survivors with insomnia: a randomised controlled trial. Eur J Cancer Care (Engl). (2020) 29:e13259. doi: 10.1111/ecc.13259
122. Medina, O, Sánchez, N, Conejo, J, Fraguas, D, and Arango, C. Alteraciones del sueño en los trastornos psiquiátricos. Rev Colomb Psiquiatr. (2007) 36:701–17.
123. Krystal, AD. Psychiatric disorders and sleep. Neurol Clin. (2012) 30:1389–413. doi: 10.1016/j.ncl.2012.08.018
124. Jahrami, H, BaHammam, AS, AlGahtani, H, Ebrahim, A, Faris, M, AlEid, K, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. (2021) 25:503–11. doi: 10.1007/s11325-020-02135-9
125. Xiao, H, Zhang, Y, Kong, D, Li, S, and Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. (2020) 26:e923549. doi: 10.12659/MSM.923549
126. Zhang, C, Yang, L, Liu, S, Ma, S, Wang, Y, Cai, Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psych. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
127. Cerqueira, TRDC, Batista, SG, de Mello, EB, DosSantos, MF, and Tuñas, ITC. Impact of the COVID-19 pandemic on stress, sleep, and oral health in university students. Front Pain Res (Lausanne). (2021) 2:264. doi: 10.3389/fpain.2021.744264
128. Wright, KP Jr, Linton, SK, Withrow, D, Casiraghi, L, Lanza, SM, Iglesia, H, et al. Sleep in university students prior to and during COVID-19 stay-at-home orders. Curr Biol. (2020) 30:R797–8. doi: 10.1016/j.cub.2020.06.022
129. Leone, MJ, Sigman, M, and Golombek, DA. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol. (2020) 30:R930–1. doi: 10.1016/j.cub.2020.07.015
130. Smith, BJ, and Lim, MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract. (2020) 30:8. doi: 10.17061/phrp3022008
131. Ballester, L, Alayo, I, Vilagut, G, Almenara, J, Cebrià, AI, Echeburúa, E, et al. Mental disorders in Spanish university students: prevalence, age-of-onset, severe role impairment and mental health treatment. J Affect Disord. (2020) 273:604–13. doi: 10.1016/j.jad.2020.04.050
132. Boden, M, Zimmerman, L, Azevedo, KJ, Ruzek, JI, Gala, S, Abdel Magid, HS, et al. Addressing the mental health impact of COVID-19 through population health. Clin Psychol Rev. (2021) 85:102006. doi: 10.1016/j.cpr.2021.102006
133. Longhurst, GJ, Stone, DM, Dulohery, K, Scully, D, Campbell, T, and Smith, CF. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid-19 pandemic. Anat Sci Educ. (2020) 13:301–11. doi: 10.1002/ase.1967
134. Majrashi, A, Khalil, A, Nagshabandi, EA, and Majrashi, A. Stressors and coping strategies among nursing students during the COVID-19 pandemic: scoping review. Nurs Rep. (2021) 11:444–59. doi: 10.3390/nursrep11020042
Keywords: COVID-19, fear, public health, Spain, students
Citation: Cebrino J and Portero de la Cruz S (2023) Psychological impact of COVID-19 and determinants among Spanish university students. Front. Public Health. 11:1252849. doi: 10.3389/fpubh.2023.1252849
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Kunhua Lee, National Tsing Hua University, TaiwanSardar Imran, Independent Researcher, Khulna, Bangladesh
Yifan Zhang, South China Normal University, China
Nor Azlili Hassan, Universiti Tunku Abdul Rahman, Malaysia
Martin Noe-Grijalva, Cesar Vallejo University, Peru
Copyright © 2023 Cebrino and Portero de la Cruz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvia Portero de la Cruz, bjkycG9jcnNAdWNvLmVz
 Jesús Cebrino
Jesús Cebrino Silvia Portero de la Cruz
Silvia Portero de la Cruz