- 1Centre for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
- 2National Health Commission (NHC) Key Lab of Health Economics and Policy Research, Shandong University, Jinan, Shandong, China
- 3Shandong Center for Disease Control and Prevention, Jinan, Shandong, China
Background: Improving the quality of life (QoL) of older adults is becoming an important global issue. However, very few studies have been focused on the relationship between socioeconomic status (SES) and QoL in older adults with hypertension. The purpose of this study is to investigate (a) the status of QoL and (b) the mediating effect of social capital in the relationship between SES and QoL, among rural older adults with hypertension in China.
Methods: Using multistage stratified random sampling, a face-to-face questionnaire survey was conducted among rural older adults with hypertension in Shandong province of China from June to July 2021. Three typical measures representing SES were used, namely, annual household income, educational level, and employment status. Individual social capital and QoL were assessed by the Resource Generator-China Scale (RG—China) and a 34-item simplified Patient Report Outcome (PRO)-specific scale for older adults with hypertension, respectively. A total of 950 rural older adults with hypertension were included in the analysis. The mediation model based on bootstrap analyses was employed to explore the relationship between SES and QoL and the mediating role of social capital in the SES-QoL nexus.
Results: The sampled rural older adults with hypertension had an upper-middle level of QoL, and the average score was 132.57 ± 19.40. SES was positively correlated with both QoL and individual social capital; individual social capital was significantly positively correlated with QoL. Controlling for sociodemographic variables, SES was still significantly associated with individual social capital (β = 0.140, P < 0.001), and the higher the individual social capital, the better QoL (β = 0.153, P < 0.001). Individual social capital played a partially mediating role in the association between SES and QoL (indirect effect = 0.021, 95% CI: 0.010–0.038), which accounted for 9.38% of the total effect.
Conclusion: This study provides evidence that the effect of SES on QoL was partially mediated by individual social capital among rural older adults with hypertension in China. The government should pay more attention to the rural older hypertensive population with lower SES and strive to reduce the negative impact of poor SES on their QoL, based on effective strategies including improving their individual social capital.
Introduction
As one of the countries with the fastest population aging, China had 267.36 million people aged older than 60 years in 2020, accounting for 18.9% of the total population (1). It is estimated that the aging population will exceed 500 million, accounting for more than 35.1% by 2050 in China (2). Hypertension is a major public health concern due to its high prevalence and mortality rate, especially in China. According to a report by the World Health Organization (WHO), in 2019, ~60–70% of older adults suffered from hypertension, which is a major risk factor for many cardiovascular, cerebrovascular, and renal diseases (3, 4). The latest data showed that the prevalence rate of hypertension among older adults in China has exceeded 50% (5), and the prevalence rate and growth rate in rural areas were higher than in urban areas (6). However, the rural population was less likely to be aware of, treated for, and controlled for hypertension (6, 7). Therefore, hypertension has become one of the major public health issues in rural China.
With the increasing aging population and the extension of life expectancy, improving the quality of life (QoL) of older adults is becoming an important global issue. As an important indicator of studies on non-communicable chronic diseases (NCDs), QoL is a multidimensional concept encompassing a patient's emotional, physical, and social functional factors (8, 9). Many studies have explored the relationship between QoL and hypertension, which indicated that older adults with hypertension had a lower QoL than the general population (10), and advanced age and comorbidity were negatively associated with QoL (11, 12). In addition, another study in Shaanxi province, China, found that the urban population with hypertension might have better QoL than those from rural areas (13). However, most of the above studies have measured QoL using generic QoL instruments, such as SF-36 and EQ-5D, which did not include important disease-specific domains.
Chinese society is characterized by a stark rural–urban divide due to longstanding disparities in social welfare entitlement, socioeconomic positions, and health profiles between rural and urban residents in later life (14, 15). In fact, in rural China, individuals and families are strongly dependent on mutual social support, when life risks and difficulties occur. Especially for older adults, whose physical condition and working ability are gradually declining and their income is gradually decreasing, traditional rural social network and social capital, embedded in them, are an important guarantee for maintaining a certain standard of living and quality of life. For the rural population with hypertension in China, due to the lack of medical resources, weak health literacy, and health awareness, the extensive interventions and support of socialization forces have a far-reaching impact on their health and QoL. In such a situation, the faster population aging and high prevalence of hypertension in rural areas have posed great challenges to the realization of a healthy China. Therefore, how to improve the QoL of older adults with hypertension in rural areas deserves further attention.
Socioeconomic status (SES), commonly measured by income, education, and occupation, is an overall measure of the economic and social status of an individual or family relative to others (16). SES is also regarded as an important factor in determining an individual's quality of life (17). In the past decades, the relationship between SES and QoL has become an important research issue in the field of healthcare, and similar conclusions on the relationship between SES and QoL were drawn. Low SES has been found to be associated with poor QoL (18, 19). Other studies indicated that chronic disease patients with low SES had low QoL, and there was a differential association between chronic disease conditions and QoL across different SES positions (20, 21). However, there have been very few studies focusing on the relationship between SES and QoL in older adults with hypertension.
Studies on the relationship between social capital and health were mainly based on two different perspectives: “communitarian” and “social network resources”. From the view of communitarian, social capital is defined as the characteristics of social organizations, such as trust, norms, and networks, that can improve social effectiveness by promoting cooperation (22). From the social network resource perspective, social capital refers to the actual or potential resources occupied by the members of a social network or organization, from where the members can get support (23). At present, social capital has been recognized as a social determinant and health influencing factor, as well as an important factor in the prevention and control of chronic diseases (24–26). Studies on the relationship between social capital and the health status of a population with hypertension have disclosed that social capital plays a positive role in the prevention and treatment of hypertension (27, 28). However, very few of them have focused on the relationship between social capital and QoL, especially for those based on the view of social network resources. No study has used a resource generator (RG) scale to measure the individual social capital of older adults with hypertension.
Although previous studies have explored the relationship between SES and QoL, few studies have touched on the role of social capital in this relationship. Some studies have shown that SES not only has a direct impact on health status but also an indirect impact through changes in social capital. However, most of these studies were carried out on the whole older population, adolescents, and urban–rural residents (29–31), while few studies focused on older adults with hypertension. A study in China reported that the effect of SES on QoL is partially mediated through social support among older adults (29). Another study of Chinese Americans also showed that social support mediates the relationship between SES and QoL in breast cancer patients, and improving the level of social support can alleviate the health inequality associated with SES (32). The health ecological model points out that people's health status is determined by individual factors, social factors, and macroenvironmental factors (33). According to the causal distance between the influencing factors and health, the social factors in the health ecological model can be divided into the following aspects: the farthest factor such as macroenvironmental, the second farthest factor such as socioeconomic status, the middle factor such as interpersonal network or social capital, the proximal factor such as behavioral characteristics, and the core factors such as biological factors. Therefore, this study aims to explore the status of QoL and the mediating effect of social capital on the association between SES and QoL among older adults with hypertension in rural China.
Methods
Study design and data collection
This study was conducted in Shandong province of China from June to July 2021. Shandong province, located on the eastern coast of China, is the third most economically developed province in China, and it has a population of more than 100 million people, of which 36.95% reside in rural areas (1). In total, 21.22 million people aged older than 60 years lived here in 2020, accounting for 20.9% of the total population (1).
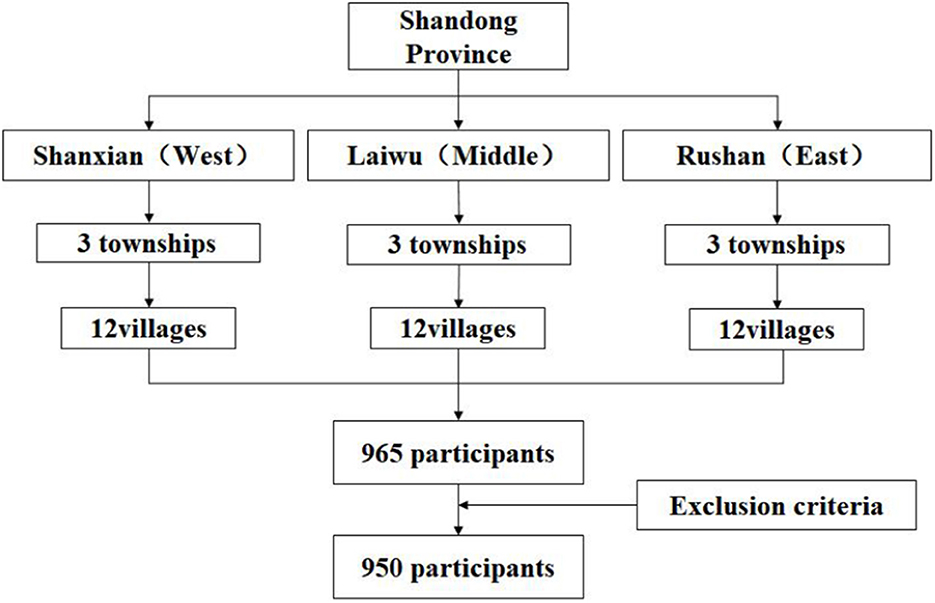
A multistage stratified random sampling framework was used to select participants (Figure 1). According to the socioeconomic levels and geographic location, three provincial counties were selected in Shandong province, namely, Rushan (high economic level, in the east), Laiwu (middle economic level, in the middle), and Shanxian (low economic level, in the west) to obtain a representative sample of older adults with hypertension in rural areas.
The sample size calculation was performed by the following formula: (N: sample size; : confidence interval, 95% confidence level; P: expected prevalence; δ: absolute error, r: relative error, δ = r × P). According to previous studies, the prevalence of hypertension was 53% among Chinese rural older adults (5); so in this study, P = 0.53, Zα/2= 1.96, δ = 0.06 × P = 0.032, α = 0.05. The required sample size was at least 935. Considering the loss and refusal of interviews, the final sample size of the survey was determined to be 960. In each county, older adults with hypertension were randomly selected and identified from the local hypertension registry system. Three townships were randomly selected within each county, and then, four villages were randomly selected within each sample township. Following that, 20–30 older adults with hypertension were randomly selected from each sample village. Finally, 965 older adults participated in the survey, and the number of valid questionnaires was 950 (98.4%).
All investigators received questionnaire survey training a few days before the formal survey. With the assistance of local community workers, skilled and trained teachers and graduate students from the Shandong University of China conducted structured face-to-face questionnaire interviews with the survey participants at the local village clinic or the office of the villagers' committee. The inclusion criteria of the participants were as follows: (1) previously diagnosed with hypertension; (2) at least 60 years old; (3) with an agreement to be investigated; and (4) able to communicate and express normally. The exclusion criteria of the participants were as follows: (1) without an agreement to be investigated; (2) poor mental state caused by a mental disorder or mental illness; and (3) unable to communicate normally due to cognitive impairment or audio–visual impairment.
The Ethics Review Board of the Center for Health Management and Policy Research, School of Public Health, Shandong University approved this study (No. ECCHMPSDU20210404), and it adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants prior to participating in this study.
Measures
Socioeconomic status
Three different measures of SES were used, namely, household income, educational level, and employment status, which have been extensively studied and validated (34, 35). Household income was collected by asking the participants to report specific income components, such as production income, wage income, transfer income, and others. Then, the respondents were also asked to report their total annual household income for validation of the sum of the components. Household income of participants was ranked from lowest to highest and divided into three groups (high = 2, middle = 1, and low = 0). Considering the actual conditions of older adults in rural China, their educational level was categorized into three groups, namely, middle school and above (high = 2), primary school (middle = 1), and illiteracy (low = 0). Employment status was categorized into three groups, namely, employed = 2, retired = 1, and unemployed = 0. Considering that in rural China, farmers view agricultural production labor as occupational work and the main source of household income, this study classified “engaged in agriculture production at present” as “employed”.
As the three SES indicators in China would not be highly correlated with each other, a single indicator cannot represent the overall SES (36). Therefore, we followed the previous studies to aggregate the above items to get a cumulative SES score (37–40). Scores are assigned to different household income levels, education levels, and employment status (39, 40). The total SES score ranges from 0 to 6, with higher scores indicating a higher socioeconomic status. In this study, the total SES score was classified into four categories, namely, lowest SES (scores ranging from 0 to 1), low SES (scores ranging from 2 to 3), high SES (scores ranging from 4 to 5), and highest SES (score is 6) (39, 40).
Quality of life
The 34-item simplified PRO-specific scale for older adults with hypertension, developed by Yang and Wang, was used to measure the health-related QoL of older adults with hypertension in the past week (41). Compared with the generic scale, it can more accurately measure the QoL of older adults with hypertension. The PRO scale is comprised of four dimensions, namely, physiology (11 items), psychology (12 items), society (6 items), and treatment (5 items). The physiology dimension is mainly concerned with physical symptoms and independence and cognitive conditions; the psychology dimension mainly includes paranoia, anxiety, depression, and hostility; the society dimension refers to social support and family role commitment; and the treatment dimension refers to compliance and satisfaction with treatment. It is worth noting that higher scores represent better QoL. The validity and reliability of this PRO scale have been assessed in older adults with hypertension, and it was considered to have good validity and reliability (41). Cronbach's α of this scale in the sample was 0.894.
Social capital
The Resource Generator China scale (RG-China), used in this study, has been developed to measure individual social capital for older rural-dwelling adults in China (42). It has been verified that RG-China has good validity and reliability in rural Chinese older adults (43, 44). RG-China has four dimensions, namely, domestic resources (eight items), expert advice (six items), personal skills (six items), and problem-solving resources (five items). Domestic resources refer to resources that can help or improve the quality of daily life; expert advice refers to resources that are helpful for medical treatment, financial management, and agricultural production; personal skills refer to the resources that provide domestic maintenance assistance and enrich entertainment activities; and problem-solving resources refer to resources that help solve personal or family problems and provide moral or material support. RG-China has 25 items, and each item has two levels of response: “yes” or “no”. The scores for the total scale and each sub-scale were calculated, and the higher the score, the more individual social capital. Cronbach's α of this scale in the sample was 0.835.
Other variables
Other variables can be classified into five categories in this study, namely, sociodemographic characteristics, health behavior and lifestyle, health service utilization characteristics, disease characteristics of hypertension, and hypertension-related knowledge. Sociodemographic characteristics included gender, age, marital status (married/cohabiting and single including never married, divorced, and widowed), and living arrangement (living alone or with others). Health-related behavior and lifestyle included alcohol drinking, cigarette smoking, physical exercise, BMI (<18.5, 18.5–23.9, 24–27.9, and ≥28), routine physical examination, and medication adherence. Health service utilization characteristics included outpatient and inpatient services received in the past year. Disease characteristics of hypertension included duration of hypertension, multimorbidity, and number of medicines taken. Hypertension-related knowledge of a 12-point scale was used to assess participants' awareness of hypertension treatment and blood pressure control, with scores of ≥7 indicating good awareness and scores of <7 indicating poor awareness (45).
Statistical analyses
Descriptive summary statistics were estimated for sociodemographic characteristics, such as SES, PRO dimensions, and RG-China dimensions. Means and standard deviations were calculated for continuous variables, and frequencies and percentages were calculated for categorical variables. The non-parametric Kruskal–Wallis test and Wilcoxon rank-sum test were conducted to test the difference in PRO scores among the subgroups, and Spearman correlation coefficients were used to test the correlations between socioeconomic status, social capital, and quality of life variables. All these analyses were performed using Stata 14.0 (Stata Corp, College Station, TX, USA).
Path analyses with regression function were performed to examine the direct effects of SES (predictor) on quality of life (outcome) and the mediating role of social capital (mediator) in this link. All regression coefficients were tested by the bias-corrected percentile bootstrap method. Specifically, we were interested in (1) the path coefficient from SES to social capital (coefficient a), (2) the path coefficient from social capital to QoL (coefficient b), and (3) the path coefficient from SES to quality of life with a mediator (coefficient c') and without a mediator (coefficient c). The focal parameters are presented in Figure 2. The mediation effect was quantified as a*b. We also used a bootstrapping strategy resampled 5,000 times to estimate the bias-corrected and accelerated 95% confidence intervals to test the indirect effects. If the 95% confidence interval did not include 0, it meant that the statistics were significant (46). The mediation model was tested with the PROCESS V.3.3 macro for SPSS. In the current study, model 4 was used to analyze the mediating effect. The model was defined as follows:
where Y is the dependent variable QoL, X is the independent variable SES, and M is the mediator variable social capital; a is the effect of SES on social capital, b is the effect of social capital on QoL, c is the total effect of SES on QoL, and c' is the direct effect of SES on QoL. Specifically, c = c' + a*b.
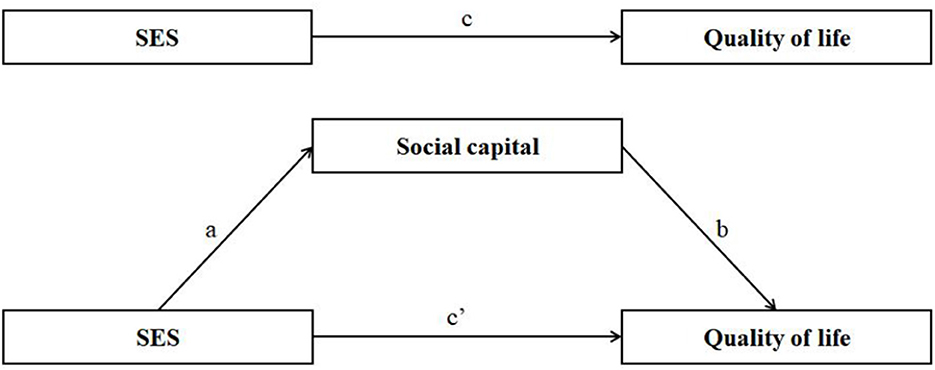
Figure 2. Mediation models. Path a, the coefficient from SES to social capital; path b, the coefficient from social capital to quality of life; path c, the coefficient from SES to quality of life without social capital; path c', the coefficient from SES to quality of life with social capital.
Results
Characteristics of the participants
Table 1 displays the characteristics of the participants. Their average age was 70.50 ± 6.11 years, and 61.3% of them were women. The majority of family caregivers had an education level below middle school (73.3%). The annual household income of 20.2% of them was more than 20,000 Chinese Yuan, while 58.0% reported an income level of <10,000 Chinese Yuan. More than half of the participants were employed, and they were mainly engaged in agricultural production labor. The proportions of non-smoking, non-drinking, exercise regularly, BMI > 24, routine health examination every year, and good medication adherence were 72.4, 67.1, 52.7, 72.3, 18.6, and 41.6%, respectively. The vast majority of participants did not utilize outpatient (52.1%) or inpatient (82.5%) services in the past year. In terms of the disease characteristics of hypertension, the proportion of participants also suffering from other diseases was 73.2%; more than half of them (52.6%) had been diagnosed with hypertension more than 10 years; and 67.6% of them took only one type of medicine (67.6%). In addition, approximately half of the participants had good awareness of hypertension treatment and blood pressure control.
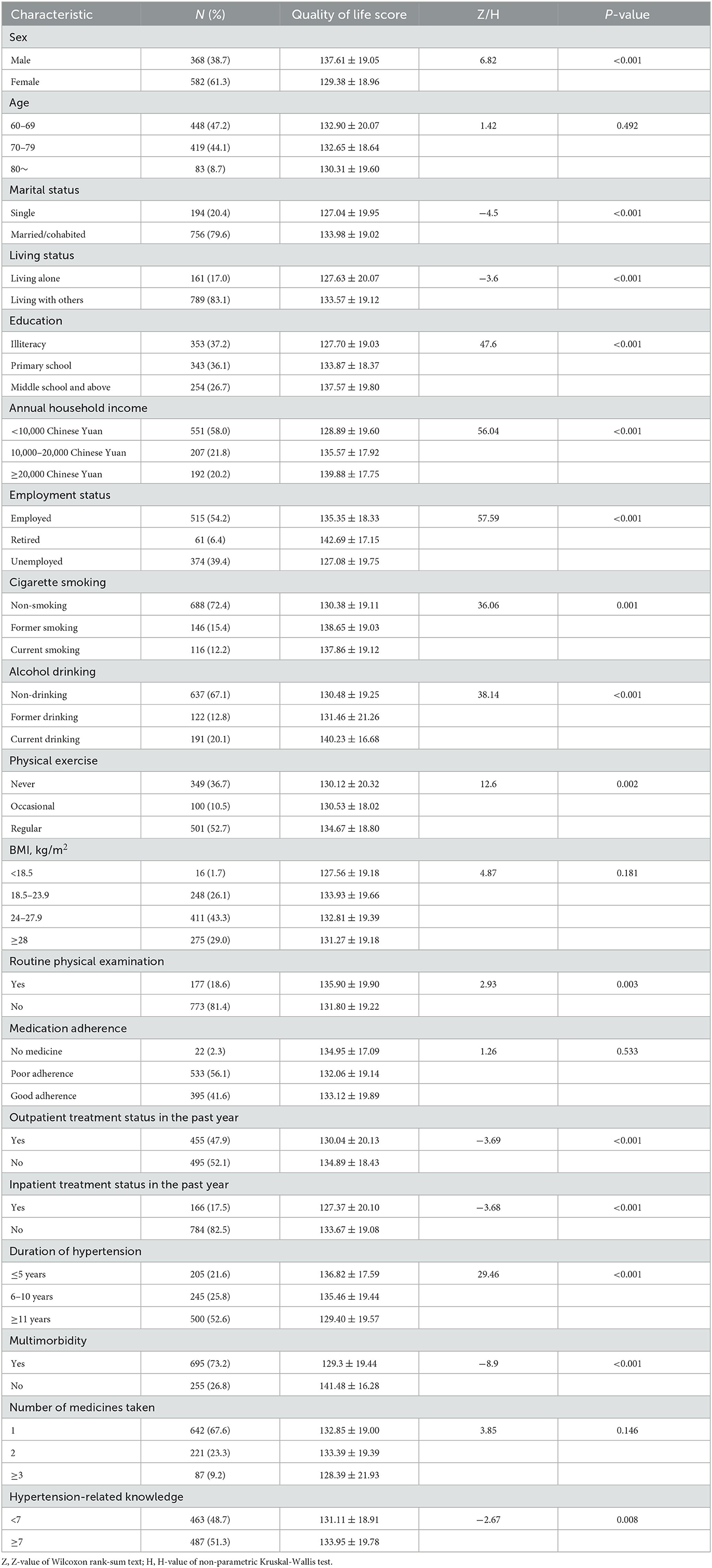
Table 1. Comparison of quality of life in rural older adults with hypertension by different characteristics.
Quality of life in rural older adults with hypertension with different characteristics
The QoL scores of most characteristic subgroups were distributed between 127 and 142. Statistical differences were revealed in the other variables except age, BMI, medication adherence, and number of medications taken. The participants had higher QoL scores, who belonged to the following characteristic subgroups: males, married/cohabited, living with others, having an education level of middle school and above, having a high annual household income, retired, former smoking, current drinking, physical exercise regularly, routine health examination every year, not utilizing outpatient or inpatient services in the past year, with hypertension <5 years, with no multimorbidity, and having good knowledge about hypertension.
Description analyses of SES, quality of life, and social capital
The mean score of the SES was 2.67 ± 1.70, and the proportions of lowest SES, low SES, high SES, and highest SES were 26.1, 41.5, 27.4, and 5.1%, respectively. The mean scores of the total social capital and four sub-dimensions were 18.66 ± 4.14, 6.98 ± 1.79 (domestic resource), 3.92 ± 1.52 (expert advice), 3.25 ± 1.46 (personal skills), and 4.51 ± 1.04 (problem-solving resources), respectively. The mean scores of the QoL and four sub-dimensions were 132.57 ± 19.40, 41.99 ± 8.32 (physiology), 49.86 ± 9.84 (psychology), 22.83 ± 4.49 (society), and 17.89 ± 4.98 (treatment), respectively.
Correlation analyses of SES, quality of life, and social capital
Table 2 provides the results of correlation analyses for SES, social capital, and QoL, respectively. SES was positively correlated with QoL (β = 0.330, P < 0.001) and social capital (β = 0.181, P < 0.001), respectively. Social capital was significantly positively correlated with QoL (β = 0.196, P < 0.001).
Analyses of the mediating effects
As shown in Table 3, three models were constructed to test the mediating role of social capital in the relationship between SES and QoL. Model 1 took SES as an independent variable, and QoL as the dependent variable. After controlling for other variables, SES was significantly associated with QoL (β = 0.227, P < 0.001). In model 2, SES was still taken as an independent variable, while social capital was used as a dependent variable. The results of model 2 showed that SES had a significant positive effect on social capital (β = 0.140, P < 0.001). When including social capital in model 3, the association between SES and QoL was still statistically significant, while the β coefficient decreased by 0.021 (β = 0.206, P < 0.001), compared with that in model 2; social capital was also significantly associated with QoL (β = 0.153, P < 0.001).
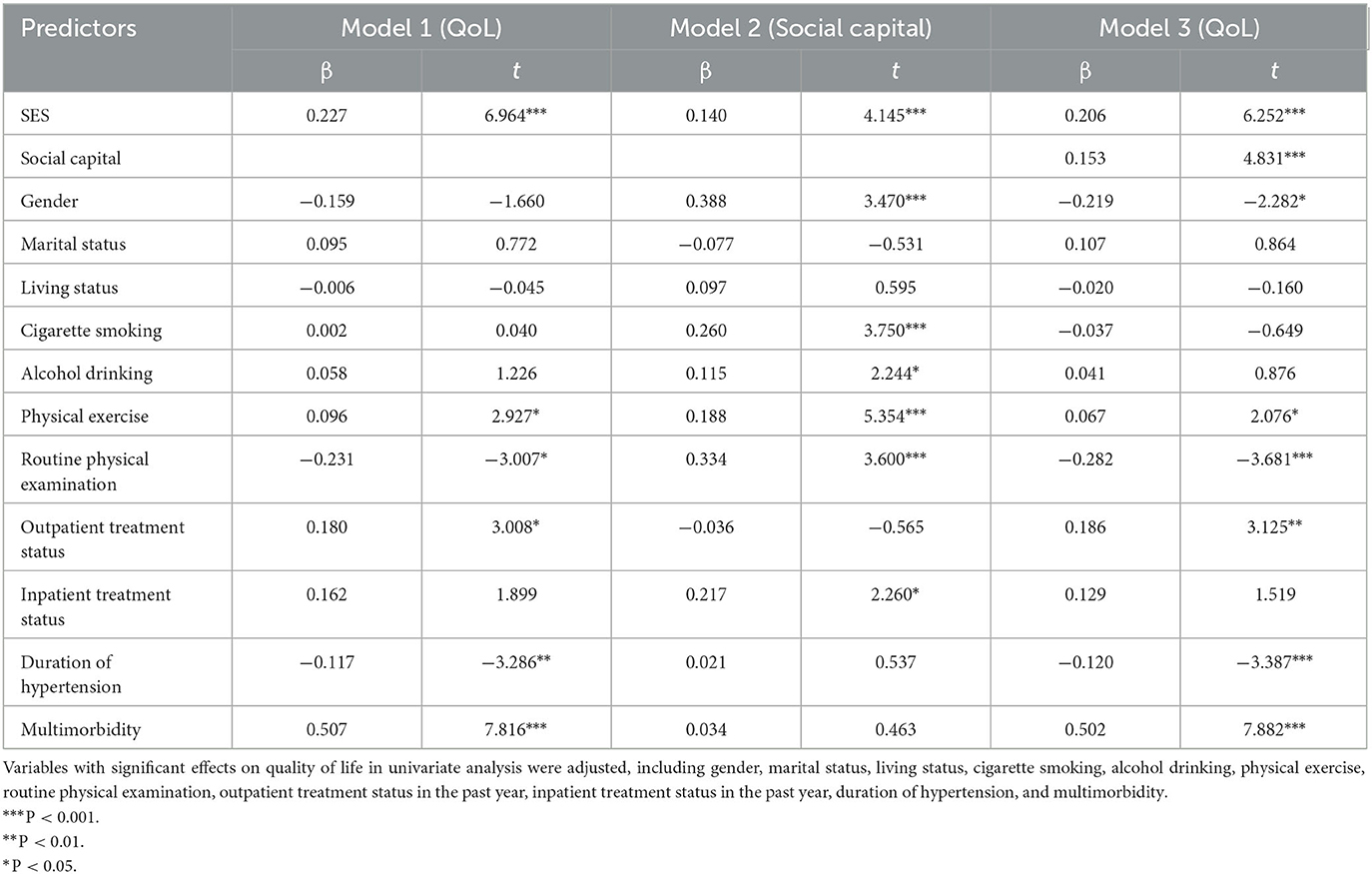
Table 3. Testing the mediation effect of social capital between SES and QoL among the participants in Shandong, China.
Therefore, we supposed that social capital may mediate the relationship between SES and QoL. The total effect, direct effect, and indirect effect of SES on QoL, with social capital as a mediator, are presented in Table 4. After controlling for potential confounders, the bootstrapping method was used to further verify the mediation effect, and the direct effect, indirect effect, and total effect were all statistically significant. Social capital played a partial mediating effect in the association between SES and QoL (indirect effect = 0.021, 95% CI: 0.010–0.038), and the mediating effect of social capital accounted for 9.38% of the total effect.
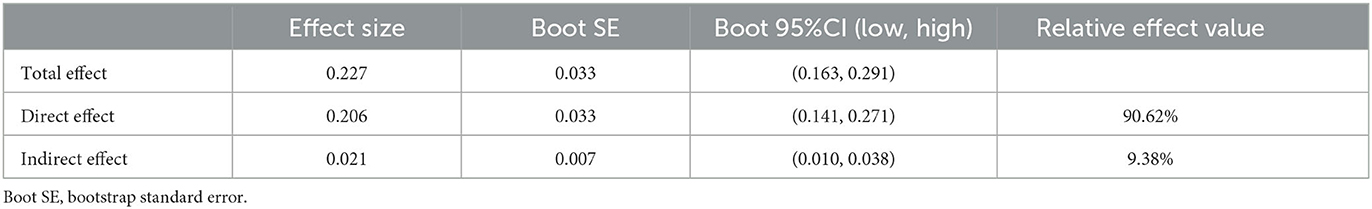
Table 4. Total effect, direct effect, and indirect effect of SES on QoL with social capital as mediator.
Discussion
To the best of our knowledge, this is the first study to explore the association of SES with QoL in rural older adults with hypertension in China, as well as the mediating effect of social capital. Our study demonstrated that SES was associated with QoL, and the effect of SES on QoL was partially mediated by social capital among rural older adults with hypertension.
The present study quantified the QoL of rural older adults with hypertension by using the PRO-specific scale for older adults with hypertension. The sampled rural older adults with hypertension had an upper-middle level of QoL, which was not completely consistent with previous studies using hypertension patient-specific QoL scales. A study used the QLICD-HY scale (quality of life instrument for a population with hypertension) to measure the QoL of the hypertensive population in Shaoyang city of Hunan province, which had a similar finding to this study (47). However, another study using the same scale found a lower level of QoL in the hypertensive population in Shanxi province (48). Focusing on older adults with hypertension, a study using the QLICD-HY scale reported that older adults with hypertension in Nanjing city had a higher QoL (49). In addition, most of the previous studies measured the QoL of hypertension using generic instruments and indicated that the rural hypertension population might have lower QoL than those in urban areas (13). The QoL in this study was inconsistent with other studies, which can be explained in the following three aspects. First, participants in the current study were older adults aged 60 years and older, while many previous studies included all adults older than 18 years. Second, there were some differences in the applicable population among different specific scales. Our study used the specific scale for older adults with hypertension, while the QLICD-HY scale was targeted at all age groups of the hypertension population. Finally, regional differences and urban–rural differences also affected the QoL of the population with hypertension.
This study revealed that SES was positively associated with QoL among rural older adults with hypertension. In other words, the Chinese rural older hypertensive population with a high level of SES had better QoL. This finding was consistent with previous research in Chinese older adults (50). Focusing on the population with hypertension, a study on the relationship between SES and mental health in the hypertensive population in Shandong province, China, reported that SES was positively correlated with mental health, which measured the SES by education background, occupation, and household income (39). Another study also showed that the risk of hypertension was different among people with different SES levels, the detection rate of hypertension was higher among people with lower education level, and the prevalence of hypertension in low-income people was higher than that in high-income people (51).
Our results indicated that there was a significant positive association between SES and social capital among rural older adults with hypertension. Similar findings have been disclosed by previous studies among adolescents, older adults, or rural–urban residents. A longitudinal study focusing on the impact of residents' SES on social capital, based on the data from China's General Social Survey, found that people with lower SES had worse social capital (52). Studies in other countries also indicated that people with higher SES had large-scale, high-quality, and more robust social relationship networks. Two possible reasons may be explained as follows: on one hand, SES determines the environment in which people live and work and the accessibility of health products and services (53). On the other hand, SES also affects people's psychological state and perception of the world around them (54).
Previous studies have shown that there was a positive relationship between social capital and QoL among different population groups, including older adults, family caregivers, and patients with stroke, HIV/AIDS, and others (50, 55–60). Similarly, this study disclosed that social capital was linked to the QoL among rural older adults with hypertension. This finding is in line with a previous study from a cross-national analysis, which suggested that hypertensive population with a higher individual social capital had better hypertension management, thereby improving their QoL (28). Another longitudinal follow-up survey in rural China reported that baseline individual social capital positively affects the QoL in older adults with hypertension (44). However, the above studies were based on the communitarian view, without taking into account actual or potential resources within social networks. Therefore, through measuring social capital with RG-China, our study enriches the existing research on the relationship between social capital and QoL in the hypertensive population.
Furthermore, this study revealed that social capital played a significant mediating role between SES and QoL among rural older adults with hypertension, which is vital for improving QoL. The rural older adults with hypertension with higher SES were more likely to have more social network resources, which were associated with better QoL. With the improvement in SES, people's experiences of social activities will become richer, which is conducive to expanding their social network and enhancing their social capital. Higher social capital represents a higher frequency of social participation, a higher level of social trust, and a higher quality of material and emotional support (61, 62). On one hand, adequate social participation in daily life not only promotes physical and mental activities but also enhances daily activities, such as ability and cognition. On the other hand, social capital can also alleviate anxiety and depression. Therefore, social capital is a beneficial factor to improve QoL in both physical and psychological aspects. These findings suggest that the effects of SES on QoL were partially mediated by social capital. Based on the above results and the high prevalence of hypertension among older adults in rural China, it is imperative to take multifaceted management strategies to prevent and control hypertension among older adults. The rate of missed diagnosis of hypertension in China is as high as 57%, and only 9% are properly treated (63). Studies have shown that the low socioeconomic status groups are more likely to delay the diagnosis and treatment of hypertension (64). Therefore, the results of this study also have a certain reference value for rural older adults with undiagnosed hypertension. We suggest that primary healthcare should strengthen the screening for chronic non-communicable diseases such as hypertension among older adults, especially in those with low SES. Health providers can regularly carry out health education to provide disease prevention, treatment, and self-management knowledge for rural older adults. In addition, it is necessary for the rural communities to build some public facilities and activities and encourage the older adults to participate in social activities, so as to improve their social capital as possible.
Although this study extends the existing literature on QoL among rural older adults with hypertension, there are still several limitations to acknowledge. First, given the cross-sectional survey, the present analyses cannot identify the causal relationships between SES, social capital, and QoL. Further research will be conducted to explore the causality with longitudinal survey data. Second, our data were collected using a structured questionnaire based on self-reported information of the participants, which might be subjected to some recall bias. In addition, the measurement of SES in our study only included household income, educational level, and employment status and did not include other indicators that can measure SES. In future studies, we will consider including other indicators that can measure SES. Third, this study was conducted in rural areas of Shandong province, China, and caution should be taken when extending these results to other rural regions. However, owing to the many similarities of rural China regions, the results of this study still have relatively good reference value.
Conclusion
This study demonstrated that SES was positively associated with QoL, and the effect of SES on QoL was partially mediated by social capital among older adults with hypertension in rural China. The government and policymakers should pay more attention to those with lower SES and strive to reduce the negative impact of poor SES on their QoL, based on effective strategies including improving their social capital.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The Ethics Review Board of the Center for Health Management and Policy Research, School of Public Health, Shandong University approved this study (No. ECCHMPSDU20210404), and it adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants prior to participate in this study.
Author contributions
XS: conceptualization, critical revision, funding acquisition, supervision, writing—original draft preparation, and writing—reviewing and editing. YF: data curation, formal analysis, software, critical revision, writing—original draft preparation, and writing—reviewing and editing. SZ: data curation, formal analysis, and supervision. XG: data curation and supervision. ZL: data curation and supervision. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Shandong Provincial Natural Science Foundation, China (ZR2019MG013) and the Shandong University Multidisciplinary Research and Innovation Team of Young Scholars (2020QNQT019).
Acknowledgments
The authors would like to thank the officials of local health agencies and all participants and staff of the study site for their cooperation. The authors also would like to express gratitude to Nan Zhang of the University of Manchester for her helpful comments on the article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SES, Socioeconomic status; QoL, Quality of life.
References
1. The Seventh Census Committee. Communiqué of the Seventh National Population Census (No. 5) (2021). Available online at: http://www.stats.gov.cn/zt_18555/zdtjgz/zgrkpc/dqcrkpc/ggl/202302/t20230215_1904001.html (accessed May 6, 2022).
2. United Nations DESA, Population, Division,. World Population Ageing 2017: Highlights (2017). Available online at: https://www.un.org/development/desa/pd/node/3335 (accessed May 6, 2022).
3. Chantakeeree C, Sormunen M, Estola M, Jullamate P, Turunen H. Factors affecting quality of life among older adults with hypertension in urban and rural areas in Thailand: a cross-sectional study. Int J Aging Hum Dev. (2022) 95:222–44. doi: 10.1177/00914150211050880
4. Olsen MHD, Angell SYM, Asma SD, Boutouyrie PP, Burger DP, Chirinos JAP, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. (2016) 388:2665–712. doi: 10.1016/S0140-6736(16)31134-5
5. China CW. Report on cardiovascular health and diseases Burden in China: an updated summary of 2020. Chin Circul J. (2021) 36:521–45. doi: 10.3969/j.issn.1000-3614.2021.06.001
6. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. (2017) 390:2549–58. doi: 10.1016/S0140-6736(17)32478-9
7. Li H, Meng QY, Sun XY, Salter A, Briggs NE, Hiller JE. Prevalence, awareness, treatment, and control of hypertension in rural China: results from Shandong Province. J Hypertens. (2010) 28:432–8. doi: 10.1097/HJH.0b013e328334b39e
8. Carr AJ, Gibson B, Robinson PG. Measuring quality of life: is quality of life determined by expectations or experience? BMJ. (2001) 322:1240–3. doi: 10.1136/bmj.322.7296.1240
9. Xiao M, Zhang F, Xiao N, Bu X, Tang X, Long Q. Health-related quality of life of hypertension patients: a population-based cross-sectional study in Chongqing, China. Int J Environ Res Public Health. (2019) 16:348. doi: 10.3390/ijerph16132348
10. Zheng E, Xu J, Xu J, Zeng X, Tan WJ, Li J, et al. Health-related quality of life and its influencing factors for elderly patients with hypertension: evidence from Heilongjiang Province, China. Front Public Health. (2021) 9:654822. doi: 10.3389/fpubh.2021.654822
11. Mannan A, Akter KM, Akter F, Chy N, Alam N, Pinky SD, et al. Association between comorbidity and health-related quality of life in a hypertensive population: a hospital-based study in Bangladesh. BMC Public Health. (2022) 22:181. doi: 10.1186/s12889-022-12562-w
12. Huong NT, Ha L, Tien TQ. Determinants of health-related quality of life among elderly: evidence from Chi Linh Town, Vietnam. Asia Pac J Public Health. (2017) 29:84S–93S. doi: 10.1177/1010539517704041
13. Zhang YL, Zhou ZL, Gao JM, Wang D, Zhang Q, Zhou ZY, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv Res. (2016) 16:277. doi: 10.1186/s12913-016-1536-x
14. Zhang N, Nazroo J, Vanhoutte B. The relationship between rural to urban migration in China and risk of depression in later life: an investigation of life course effects. Soc Sci Med. (2021) 270:113637. doi: 10.1016/j.socscimed.2020.113637
15. Zhang J, Chandola T, Zhang N. Understanding the longitudinal dynamics of rural-urban mental health disparities in later life in China. Aging Ment Health. (2023) 27:1419–28. doi: 10.1080/13607863.2022.2098912
16. Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. (1999) 896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x
17. Razzaque A, Nahar L, Akter KM, Kim SP. Socio-demographic differentials of adult health indicators in Matlab, Bangladesh: self-rated health, health state, quality of life and disability level. Glob Health Action. (2010) 3:4618. doi: 10.3402/gha.v3i0.4618
18. Lubetkin EI, Jia HM, Franks P, Gold MR. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: Examining the EQ-5D in the U.S. general population. Qual of Life Res. (2005) 14:2187–96. doi: 10.1007/s11136-005-8028-5
19. Mielck A, Vogelmann M, Leidl R. Health-related quality of life and socioeconomic status: inequalities among adults with a chronic disease. Health Qual Life Outcomes. (2014) 12:58. doi: 10.1186/1477-7525-12-58
20. Mielck A, Reitmeir P, Vogelmann M, Leidl R. Impact of educational level on health-related quality of life (HRQL): results from Germany based on the EuroQol 5D (EQ-5D). Eur J Public Health. (2013) 23:45–9. doi: 10.1093/eurpub/ckr206
21. Stafford M, Soljak M, Pledge V, Mindell J. Socio-economic differences in the health-related quality of life impact of cardiovascular conditions. Eur J Public Health. (2012) 22:301–5. doi: 10.1093/eurpub/ckr007
22. Putnam RD. Bowling Alone: The Collapse and Revival of American Community. New York, NY: Simon & Schuster (2000).
23. Bourdieu P. The Forms of Capital Richardson J G. Handbook of Theory and Research for the Sociology of Education. New York, NY: Green wood Press (1986).
24. Ma T, Wu N, Xia J, Gao B, Yu C, Li N. The effects of social capital on depressive symptoms of elderly patients with chronic diseases in urbanized communities. J Sichuan Univ. (2019) 50:561–5. doi: 10.13464/j.scuxbyxb.2019.04.020
25. Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. (2015) 69:1021–8. doi: 10.1136/jech-2015-205868
26. Rodgers J, Valuev AV, Hswen Y, Subramanian SV. Social capital and physical health: an updated review of the literature for 2007-2018. Soc Sci Med. (2019) 236:112360. doi: 10.1016/j.socscimed.2019.112360
27. Lu X, Juon H, He X, Dallal CM, Wang MQ, Lee S. The association between perceived stress and hypertension among Asian Americans: does social support and social network make a difference? J Community Health. (2019) 44:451–62. doi: 10.1007/s10900-018-00612-7
28. Palafox B, Goryakin Y, Stuckler D, Suhrcke M, Balabanova D, Alhabib KF, et al. Does greater individual social capital improve the management of hypertension? Cross-national analysis of 61 229 individuals in 21 countries. BMJ Glob Health. (2017) 2:e443. doi: 10.1136/bmjgh-2017-000443
29. Hou L,. Study on the influencing pathway between socio-economic status quality of life based on the health ecological model (Master, Shanxi Medical University) (2020). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1020751261.nh&DbName=CMFD2020 (accessed May 6, 2022).
30. Zhang J, Hong L, Ma G. Socioeconomic status, peer social capital, and quality of life of high school students during COVID-19: a mediation analysis. Appl Res Qual Life. (2022) 17:3005–21. doi: 10.1007/s11482-022-10050-2
31. Addae EA. The mediating role of social capital in the relationship between socioeconomic status and adolescent wellbeing: evidence from Ghana. BMC Public Health. (2020) 20:20. doi: 10.1186/s12889-019-8142-x
32. You J, Wang C, Yeung N, Lu Q. Socioeconomic status and quality of life among Chinese American breast cancer survivors: the mediating roles of social support and social constraints. Psychooncology. (2018) 27:1742–9. doi: 10.1002/pon.4719
33. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. (1988) 15:351–77. doi: 10.1177/109019818801500401
34. Li Z, Li J, Fu P, Chen Y, Jing Z, Yuan Y, et al. Family doctor contract services and health-related quality of life among patients with chronic diseases in rural China: what is the role of socioeconomic status? Int J Equity Health. (2021) 20:191. doi: 10.1186/s12939-021-01530-2
35. Falagas ME, Zarkadoulia EA, Pliatsika PA, Panos G. Socioeconomic status (SES) as a determinant of adherence to treatment in HIV infected patients: a systematic review of the literature. Retrovirology. (2008) 5:13. doi: 10.1186/1742-4690-5-13
36. Pan Y, Chen R, Li Z, Li H, Zhao X, Liu L, et al. Socioeconomic status and the quality of acute stroke care: the china national stroke registry. Stroke. (2016) 47:2836–42. doi: 10.1161/STROKEAHA.116.013292
37. Shi L, Tao L, Chen N, Liang H. Relationship between socioeconomic status and cognitive ability among Chinese older adults: the moderating role of social support. Int J Equity Health. (2023) 22:70. doi: 10.1186/s12939-023-01887-6
38. Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, et al. Impact of multiple social determinants of health on incident stroke. Stroke. (2020) 51:2445–53. doi: 10.1161/STROKEAHA.120.028530
39. Zhang X, Zhou C, Jing Z, Xu Q. Studying on the relationship between mental health and socioeconomic status among hypertensive patients in Shandong. Chin Health Serv Manag. (2019) 36:219–23.
40. Xie C, Qin C, Wang G, Yu C, Wang J, Dai L, et al. Relationship between socioeconomic status and the prevalence of cardiovascular disease among retired residents living in a communtiy, Shanghai. Chin J Epidemiol. (2014) 35:500–4. doi: 10.3760/cma.j.issn.0254-6450.2014.05.007
41. Yang C,. Development evaluation of patient reported outcomes for elderly hypertension patients (Master, Shandong University) (2015). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1015368435.nh&DbName=CMFD2016 (accessed May 6, 2022).
42. Sun XJ, Liu K, Webber M, Shi LZ. Individual social capital and health-related quality of life among older rural Chinese. Ageing Soc. (2017) 37:221–42. doi: 10.1017/S0144686X15001099
43. Liu K, Zhang N, Li Y, Sun X. Revision and evaluation of the rural elderly resource generator scale. J Shandong Univ. (2015) 53:87–91. doi: 10.6040/j.issn.1671-7554.0.2014.531
44. Liu S,. The effects of individual social capital on the health-related quality of life among rural seniors with hypertension (Master, Shandong University) (2021). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1021041736.nh&DbName=CMFD2022 (accessed May 6, 2022).
45. Lan H,. The study on knowledge, attitude, practice of hypertension among the middle-aged elderly denizens in Anqing rural communities (Master, Anhui Medical University) (2016). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1016138838.nh&DbName=CMFD2016 (accessed May 6, 2022).
46. Bolin JH. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. J Educ Measur. (2014) 51:335–7. doi: 10.1111/jedm.12050
47. Wang Y, Wang C, Zhan H, Huang M, Chen S. Research on life quality evaluation of hypertension Patients in Hunan province. Soft Sci Health. (2017) 31:60–4.
48. Che X,. Influential factors intervention study on quality of life in patients with essential hypertension (Master, Shanxi Medical University) (2019). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1019611638.nh&DbName=CMFD2019 (accessed May 6, 2022).
49. Wu X,. Study on quality of life its influencing factors of elderly hypertensive patients in community (Master, Southeast University) (2019). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1020801056.nh&DbName=CMFD2020 (accessed May 6, 2022).
50. Yang Y, Wang S, Chen L, Luo M, Xue L, Cui D, et al. Socioeconomic status, social capital, health risk behaviors, and health-related quality of life among Chinese older adults. Health Qual Life Outcom. (2020) 18:291. doi: 10.1186/s12955-020-01540-8
51. Leng B,. The effect of socioeconomic status on hypertension among Chongqing residents (Master, Chongqing Medical University) (2015). Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=1016008595.nh&DbName=CMFD2016 (accessed May 6, 2022).
52. Li T, Zhou J, Jin X, Shi Y. Determinants of social capital: the subjective economic status perspective. Econ Res J. (2021) 56:191–205.
53. Jiang Y, Hesser JE. Associations between health-related quality of life and demographics and health risks. Results from Rhode Island's 2002 behavioral risk factor survey. Health Qual Life Outcomes. (2006) 4:14. doi: 10.1186/1477-7525-4-14
54. Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol. (2011) 62:501–30. doi: 10.1146/annurev.psych.031809.130711
55. Lucumi DI, Gomez LF, Brownson RC, Parra DC. Social capital, socioeconomic status, and health-related quality of life among older adults in Bogota (Colombia). J Aging Health. (2015) 27:730–50. doi: 10.1177/0898264314556616
56. Zhang B, Conner KO, Meng H, Tu N, Liu D, Chen Y. Social support and quality of life among rural family caregivers of persons with severe mental illness in Sichuan Province, China: mediating roles of care burden and loneliness. Qual Life Res. (2021) 30:1881–90. doi: 10.1007/s11136-021-02793-6
57. Ji K, Bai Z, Zhao Y, Sang L, Wang D, Chen R. Relationship between social capital and quality of life among adult stroke patients: a cross-sectional study in Anhui Province, China. Health Qual Life Outcom. (2022) 20:19. doi: 10.1186/s12955-022-01925-x
58. Ma Y, Qin X, Chen R, Li N, Chen R, Hu Z. Impact of individual-level social capital on quality of life among AIDS patients in China. PLoS ONE. (2012) 7:e48888. doi: 10.1371/journal.pone.0048888
59. Rimaz S, Mohammad K, Dastoorpoor M, Jamshidi E, Majdzadeh R. Investigation of relationship between social capital and quality of life in multiple sclerosis patients. Glob J Health Sci. (2014) 6:261–72. doi: 10.5539/gjhs.v6n6p261
60. Boehm A, Eisenberg E, Lampel S. The contribution of social capital and coping strategies to functioning and quality of life of patients with fibromyalgia. Clin J Pain. (2011) 27:233–9. doi: 10.1097/AJP.0b013e3181fdabcf
61. Flores EC, Fuhr DC, Bayer AM, Lescano AG, Thorogood N, Simms V. Mental health impact of social capital interventions: a systematic review. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:107–19. doi: 10.1007/s00127-017-1469-7
62. Gupta R, Kaur M, Islam S, Mohan V, Mony P, Kumar R, et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. (2017) 30:373–81. doi: 10.1093/ajh/hpw169
63. Mauer N, Geldsetzer P, Manne-Goehler J, Davies JI, Stokes AC, McConnell M, et al. Longitudinal evidence on treatment discontinuation, adherence, and loss of hypertension control in four middle-income countries. Sci Transl Med. (2022) 14:i9522. doi: 10.1126/scitranslmed.abi9522
64. Rahman M, Syed EH, Islam MJ, Mostofa MG, Saadat KA. Association of socioeconomic status with diagnosis, treatment and control of hypertension in diabetic hypertensive individuals in Bangladesh: a population-based cross-sectional study. JRSM Open. (2015) 6:442833206. doi: 10.1177/2054270415608118
Keywords: socioeconomic status, quality of life, social capital, older adults with hypertension, rural, China
Citation: Fu Y, Zhang S, Guo X, Lu Z and Sun X (2023) Socioeconomic status and quality of life among older adults with hypertension in rural Shandong, China: a mediating effect of social capital. Front. Public Health 11:1248291. doi: 10.3389/fpubh.2023.1248291
Received: 27 June 2023; Accepted: 18 September 2023;
Published: 17 October 2023.
Edited by:
Maria Giné-Garriga, Ramon Llull University, SpainReviewed by:
Bo Hou, Bradford Teaching Hospitals NHS Foundation Trust, United KingdomWeidong Huang, Harbin Medical University, China
Copyright © 2023 Fu, Zhang, Guo, Lu and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaojie Sun, eGlhb2ppZXN1bkBzZHUuZWR1LmNu
 Yingjie Fu
Yingjie Fu Shuo Zhang1,2
Shuo Zhang1,2 Xiaojie Sun
Xiaojie Sun